Hemorrhage Definition Classification Terminologies Clinical manifestations Pathophysiology Investigations
- Slides: 42
Hemorrhage
• Definition • Classification • Terminologies • Clinical manifestations • Pathophysiology • Investigations • Management 2
Definitions of Hemorrhage Discharge of blood from the vascular compartment to the exterior of the body or into non vascular body spaces. The escape of large amounts of blood from the blood vessels, normally due to injury. The bleeding may be internal or external. (www. ferring. com/therapeutic/gastro/GLOSSARY. htm ) Hemorrhage (alternate spelling is Haemorrhage) is the medical term referring to the presence of blood in the interstitial tissues. (en. wikipedia. org/wiki/Haemorrhage )
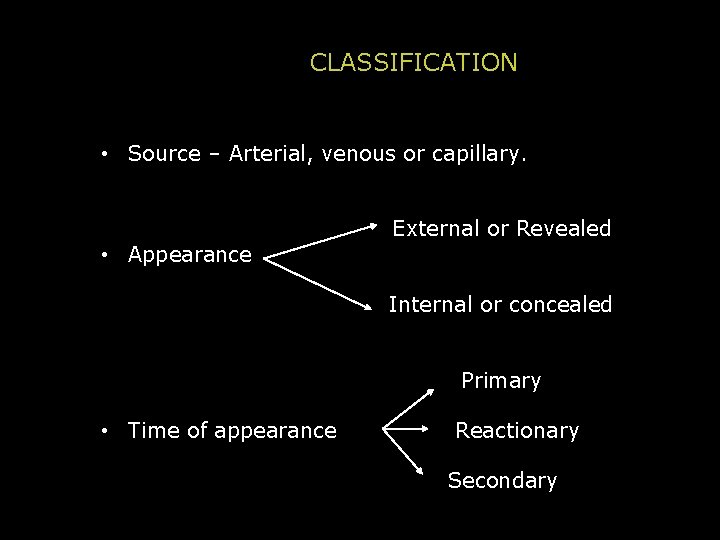
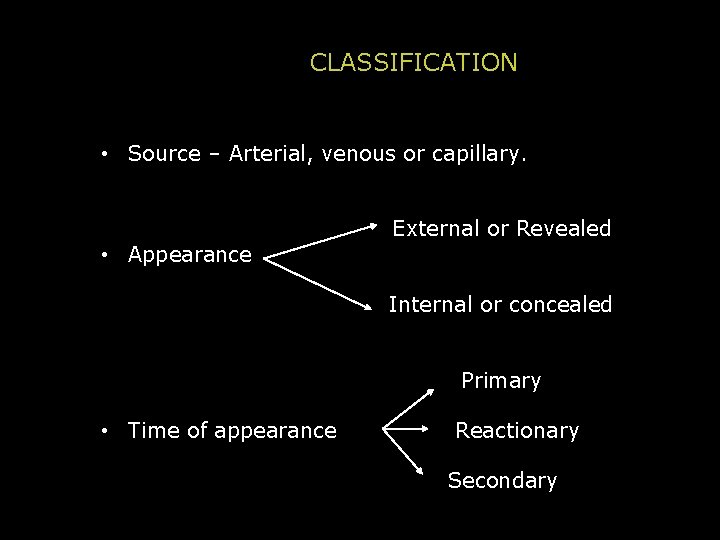
CLASSIFICATION • Source – Arterial, venous or capillary. • Appearance External or Revealed Internal or concealed Primary • Time of appearance Reactionary Secondary
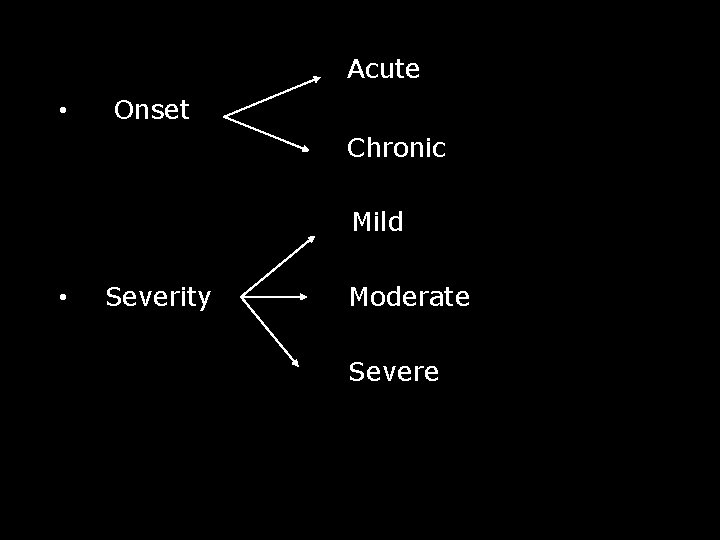
Acute • Onset Chronic Mild • Severity Moderate Severe
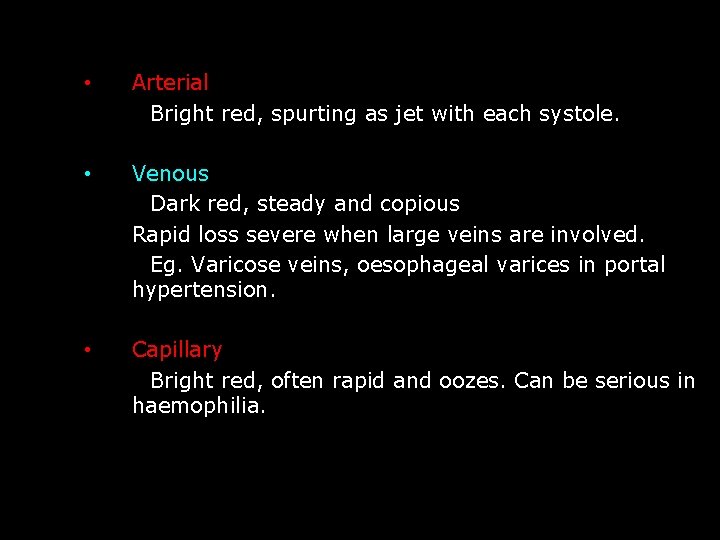
• Arterial Bright red, spurting as jet with each systole. • Venous Dark red, steady and copious Rapid loss severe when large veins are involved. Eg. Varicose veins, oesophageal varices in portal hypertension. • Capillary Bright red, often rapid and oozes. Can be serious in haemophilia.
• Primary Haemorrhage At the time of injury or operation. • Reactionary Haemorrhage Follows primary haemorrhage within 4 to 6 hours. Causes (1) Slipping of ligature (2) Dislodgement of clot (3) Cessation of reflex vasospasm. Raise in BP, restlessness. . . • Secondary Haemorrhage Occurs in 7 to 14 days because of infection and sloughing of vessel wall (usually artery). Predisposing factors are pressure of a draining tube, the presence of a fragment of bone, a ligature in an infected area
• Mild haemorrhage Blood loss is less than 500 ml. E. g. after dental extraction. • Moderate haemorrhage: Loss is upto 2 L. Initially BP falls but is restored by increased PR. • Severe haemorrhage: Could be more than 2 L. Due to positive feed back mechanism BP falls significantly hence is lethal.
Terminologies • hematoma: when large of amount of blood accumulates in soft tissue. • Petechiae: minute 1 to 2 mm hemorrhage into skin, mucous membranes or serosal surfaces. • Purpura: slightly larger (3 to 5 mm) hemorrhages. • Ecchymoses: larger 1 to 2 cm subcutaneous hematomas (bruises).
NORMAL PHYSIOLOGY OF HAEMOSTASIS • Haemostasis may be thought of as a tightly regulated system of interdependent factors. • Performance of even the most minor surgical procedure depends on a complex, interdependent set of events resulting in formation of a stable clot.
• Haemostasis consists of 3 phases: – Vascular phase – Platelet phase – Coagulation phase • The first two phases constitute primary haemostasis and the coagulation phase constitute the secondary haemostasis
Vascular constriction phase: • It is the initial vascular response to injury at the capillary level. • It is dependent upon local contraction of smooth muscle that has a reflex response to various stimuli. • Initial vascular constriction occurs prior to platelet adherence at the site of injury. • Vasoconstriction is subsequently linked to platelet plug and fibrin formation.
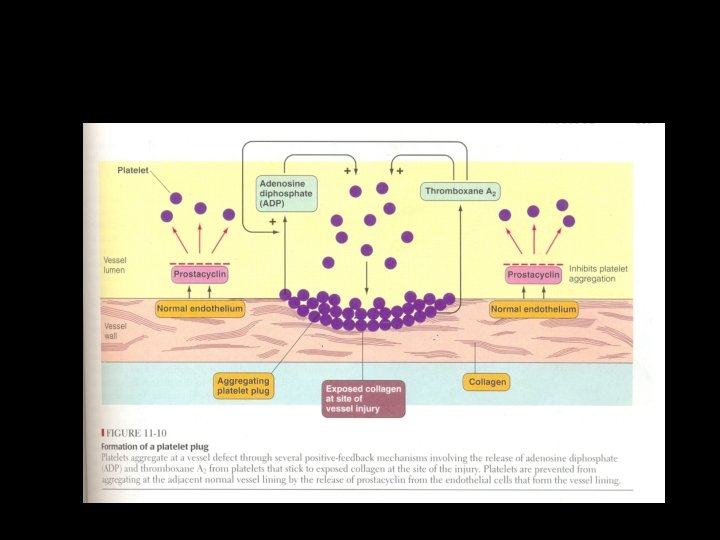
Platelet Phase • Platelet are 2µm diameter fragments of megakaryocytes and number 2 lakh to 4 lakh / cumm in circulating blood with a life span of 7 -9 days. • Injury to the intima exposes the endothelial collagen to which platelets adhere within 16 seconds of the traumatic event. • This also requires von Willebrand factor.
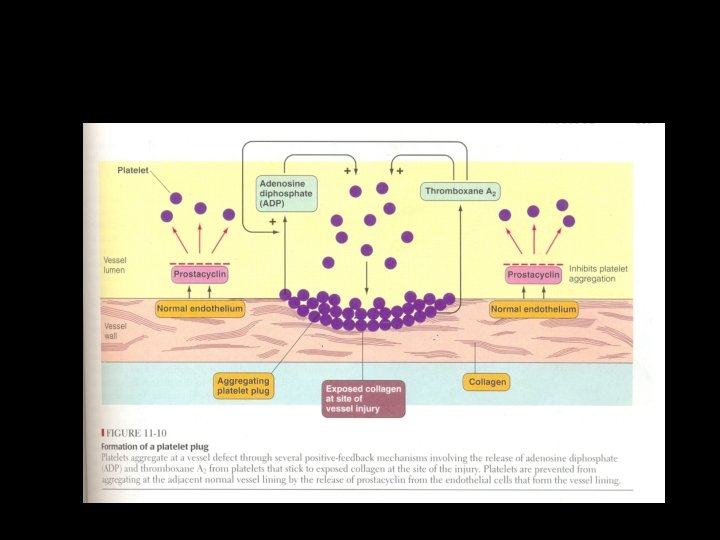
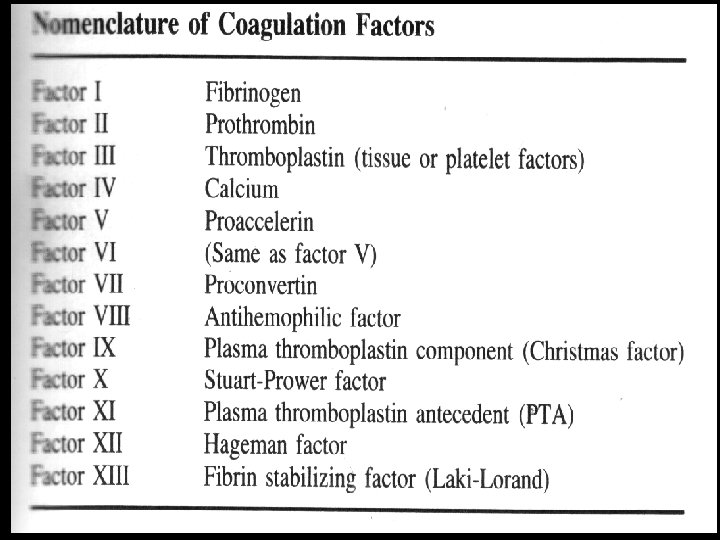
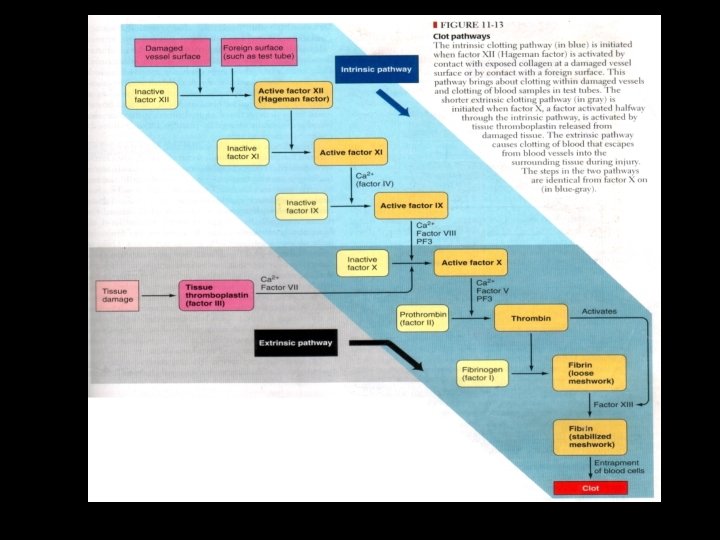
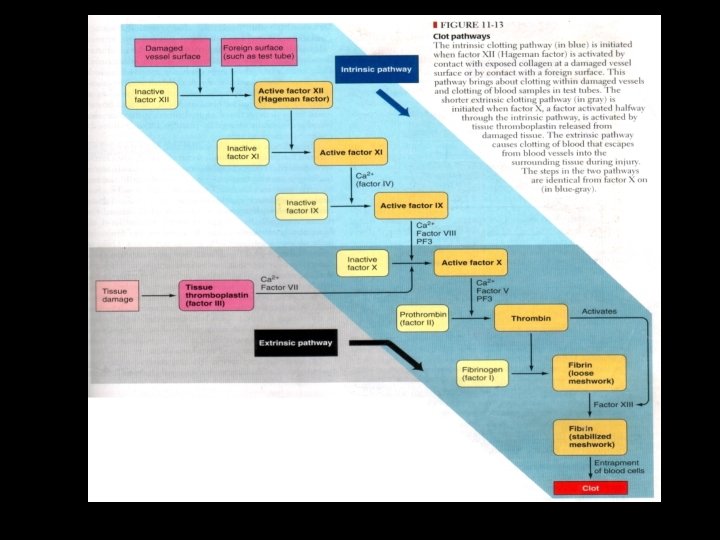
The coagulation phase and formation of the fibrin clot: • Coagulation is a process by which prothrombin is converted into the proteolytic enzyme thrombin. • Which in turn cleaves the fibrinogen molecule to form insoluble fibrin in order to stabilize and add to the platelet plug. • Traditional concept of the clotting system evolved from the test tube analysis and follows two pathways.
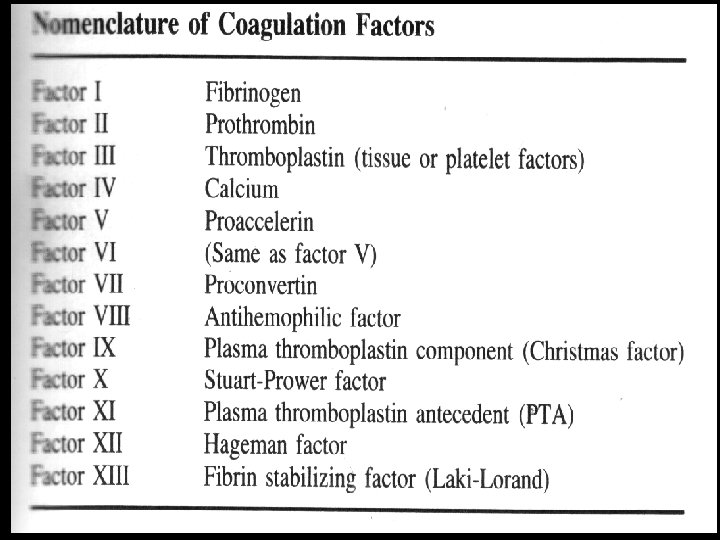
Essential steps in coaugulation: • Formation of prothrombin activator in response to vessel or tissue injury. • Conversion of prothrombin to thrombin in presence of prothrombin activator. • Conversion of fibrinogen to fibrin.
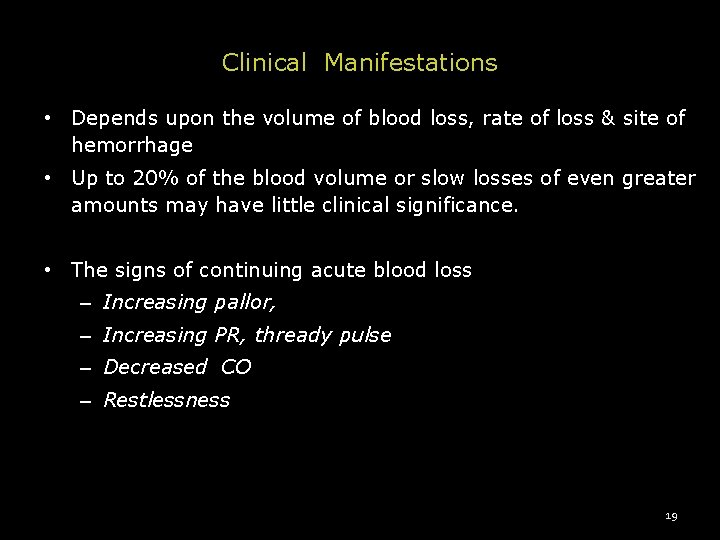
Clinical Manifestations • Depends upon the volume of blood loss, rate of loss & site of hemorrhage • Up to 20% of the blood volume or slow losses of even greater amounts may have little clinical significance. • The signs of continuing acute blood loss – Increasing pallor, – Increasing PR, thready pulse – Decreased CO – Restlessness 19
Clinical Manifestations • These are accompanied by - Cold and clammy skin - Empty veins - Thirst, tinnitus and blindness - oliguria/ anuria the subject goes deeper into shock. 20
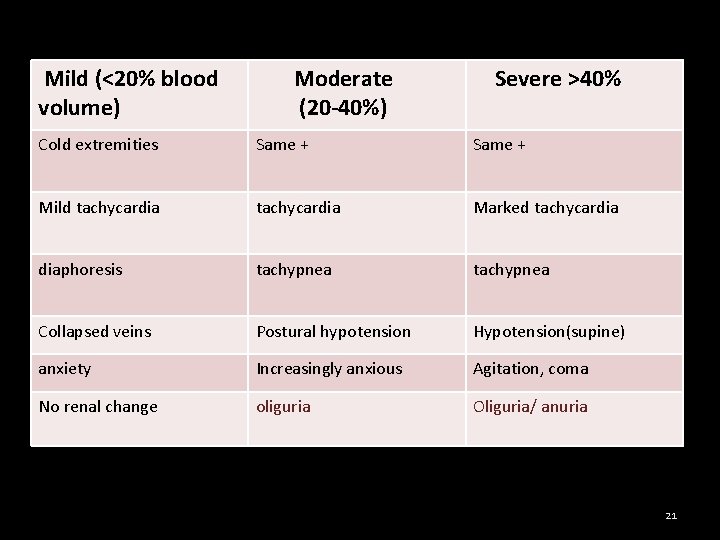
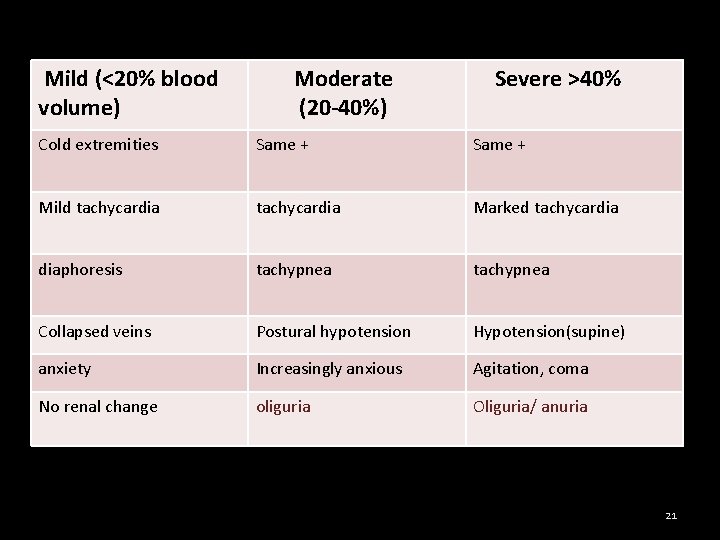
Mild (<20% blood volume) Moderate (20 -40%) Severe >40% Cold extremities Same + Mild tachycardia Marked tachycardia diaphoresis tachypnea Collapsed veins Postural hypotension Hypotension(supine) anxiety Increasingly anxious Agitation, coma No renal change oliguria Oliguria/ anuria 21
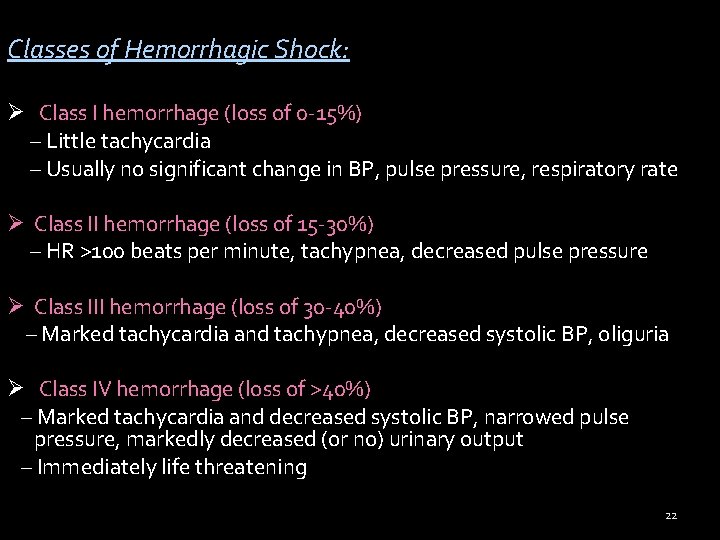
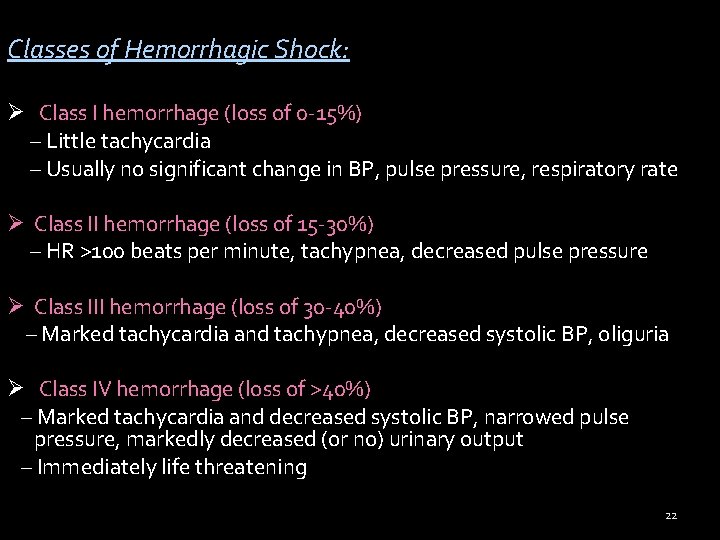
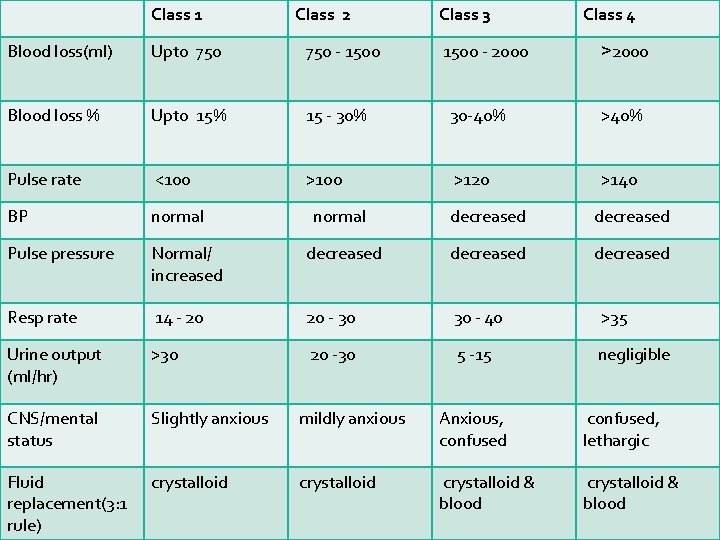
Classes of Hemorrhagic Shock: Ø Class I hemorrhage (loss of 0 -15%) – Little tachycardia – Usually no significant change in BP, pulse pressure, respiratory rate Ø Class II hemorrhage (loss of 15 -30%) – HR >100 beats per minute, tachypnea, decreased pulse pressure Ø Class III hemorrhage (loss of 30 -40%) – Marked tachycardia and tachypnea, decreased systolic BP, oliguria Ø Class IV hemorrhage (loss of >40%) – Marked tachycardia and decreased systolic BP, narrowed pulse pressure, markedly decreased (or no) urinary output – Immediately life threatening 22
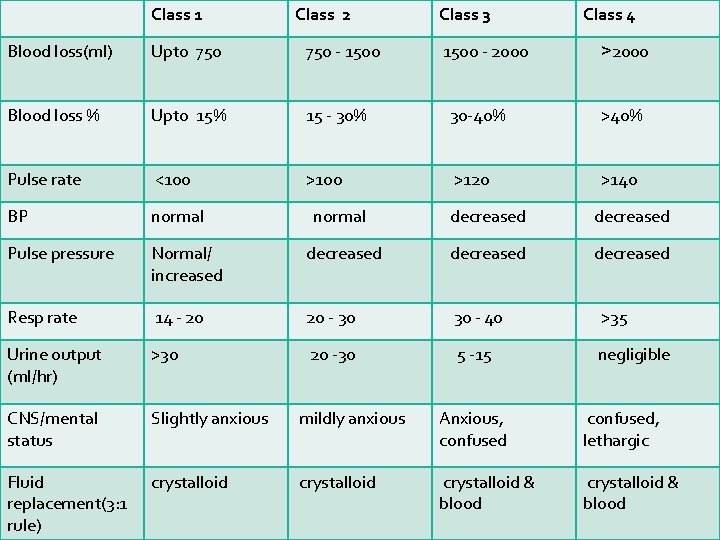
Class 1 Class 2 Class 3 1500 - 2000 Class 4 Blood loss(ml) Upto 750 - 1500 Blood loss % Upto 15% 15 - 30% 30 -40% >40% Pulse rate <100 >120 >140 BP normal Pulse pressure >2000 normal decreased Normal/ increased decreased Resp rate 14 - 20 20 - 30 30 - 40 >35 Urine output (ml/hr) >30 20 -30 5 -15 negligible CNS/mental status Slightly anxious mildly anxious Anxious, confused, lethargic Fluid replacement(3: 1 rule) crystalloid & blood 23
Body response How ? . . . .
PATHOPHYSIOLOGY Body response to hemorrhage may be classified as: 1) Early changes ( first 48 hrs) 2) Late changes (after 48 hrs) Early changes (first 48 hrs) Vaso-vagal syncope: sighing, sweating deep rapid breathing pallor, giddiness, fainting BP ↓ PR = 30 to 40/ min. - alarm signal indicating that the safety margin is exceeded.
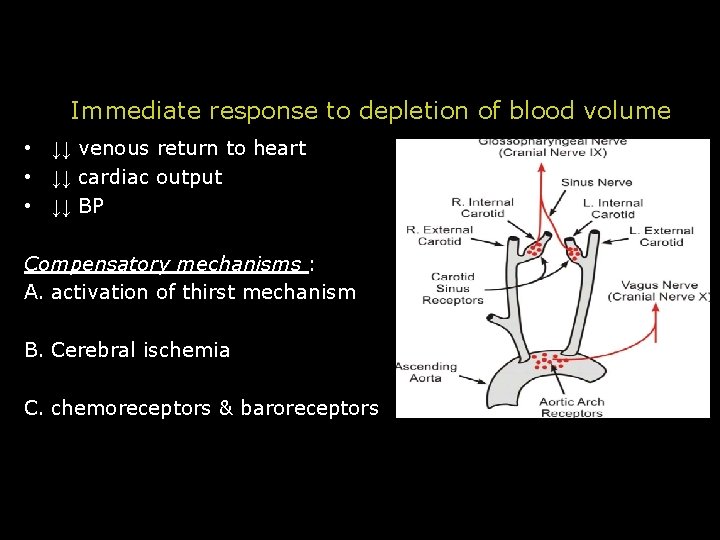
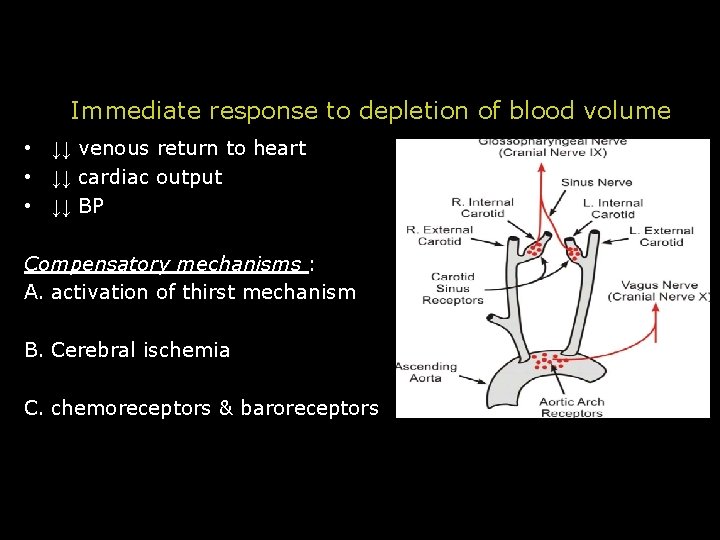
Immediate response to depletion of blood volume • ↓↓ venous return to heart • ↓↓ cardiac output • ↓↓ BP Compensatory mechanisms : A. activation of thirst mechanism B. Cerebral ischemia C. chemoreceptors & baroreceptors
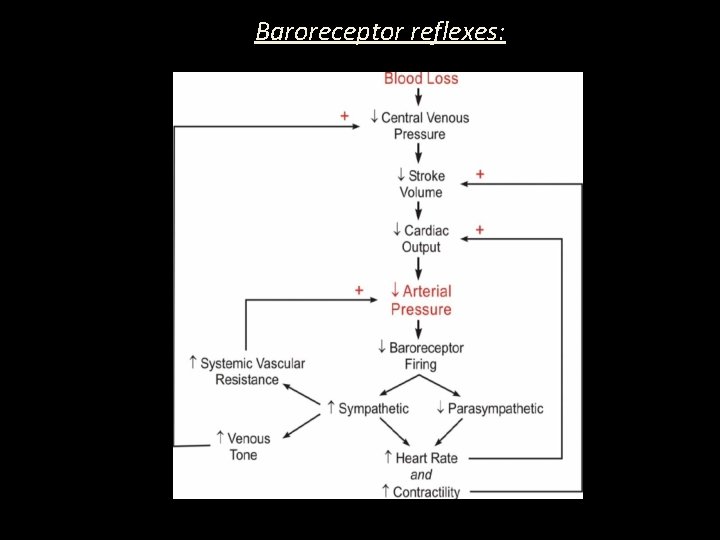
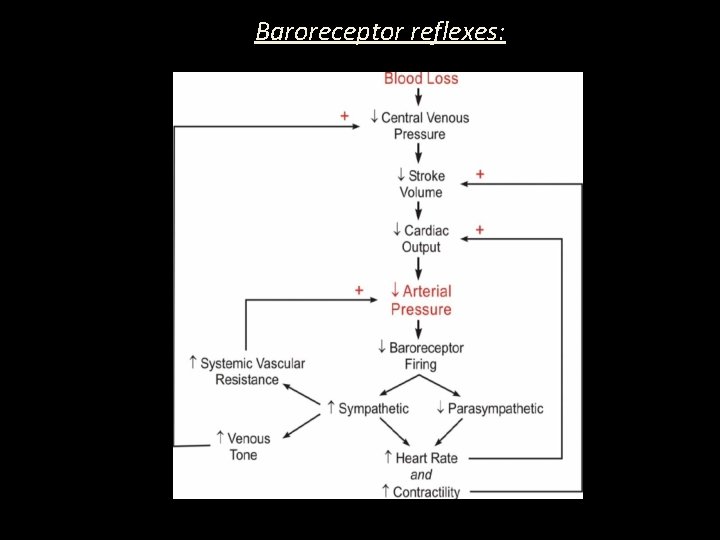
Baroreceptor reflexes:
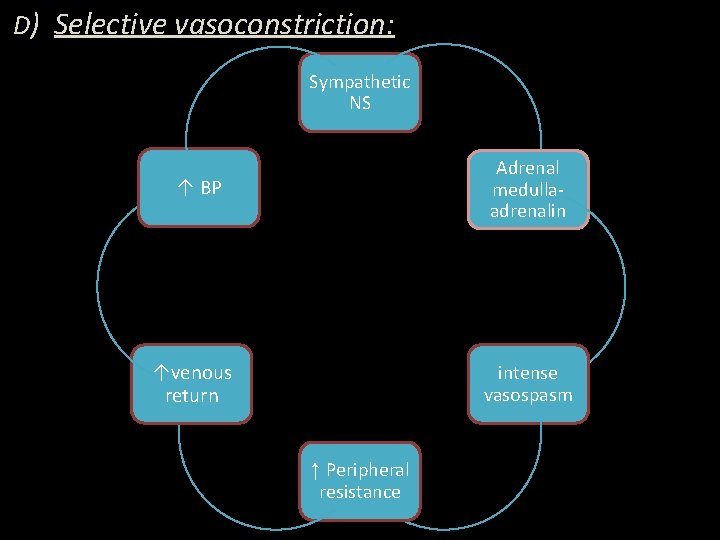
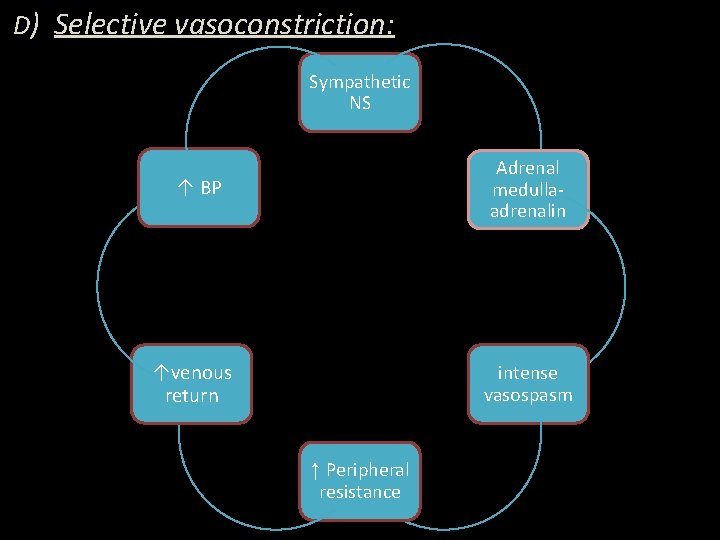
D) Selective vasoconstriction: Sympathetic NS Adrenal medullaadrenalin ↑ BP ↑venous return intense vasospasm ↑ Peripheral resistance
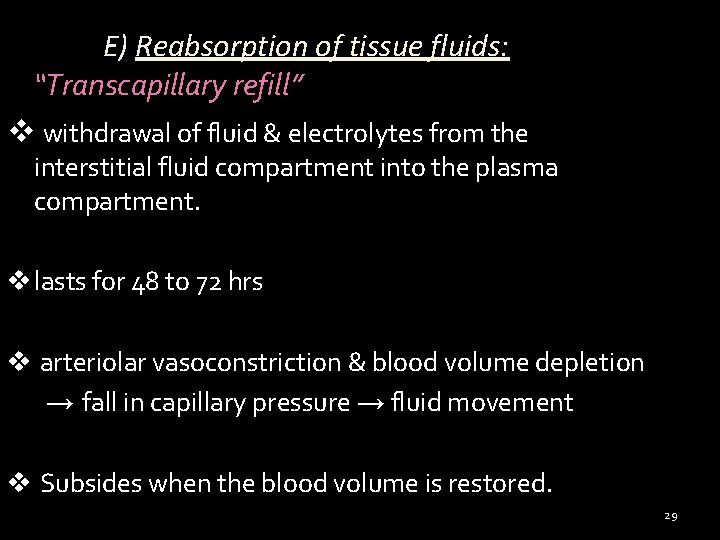
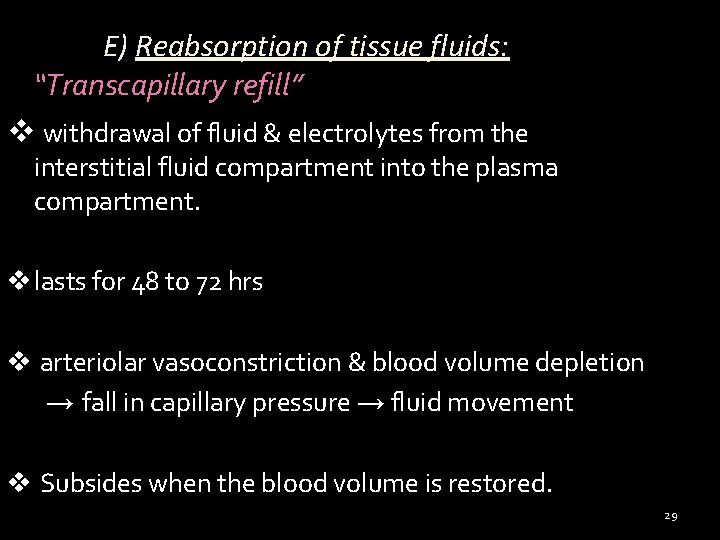
E) Reabsorption of tissue fluids: “Transcapillary refill” v withdrawal of fluid & electrolytes from the interstitial fluid compartment into the plasma compartment. v lasts for 48 to 72 hrs v arteriolar vasoconstriction & blood volume depletion → fall in capillary pressure → fluid movement v Subsides when the blood volume is restored. 29
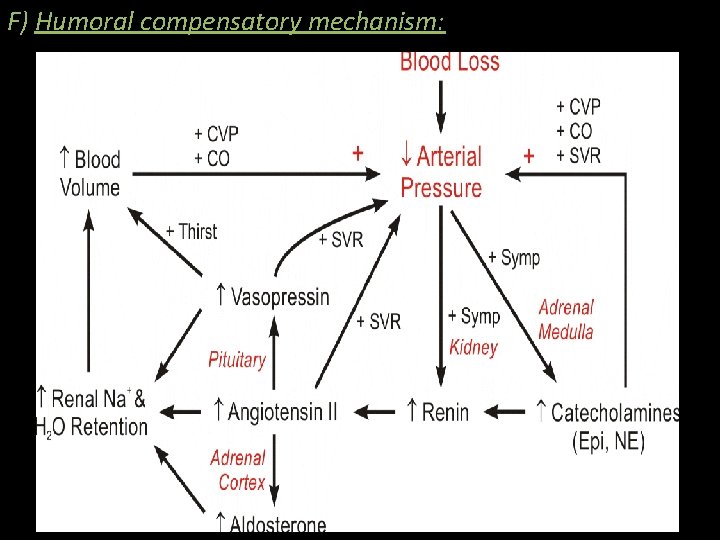
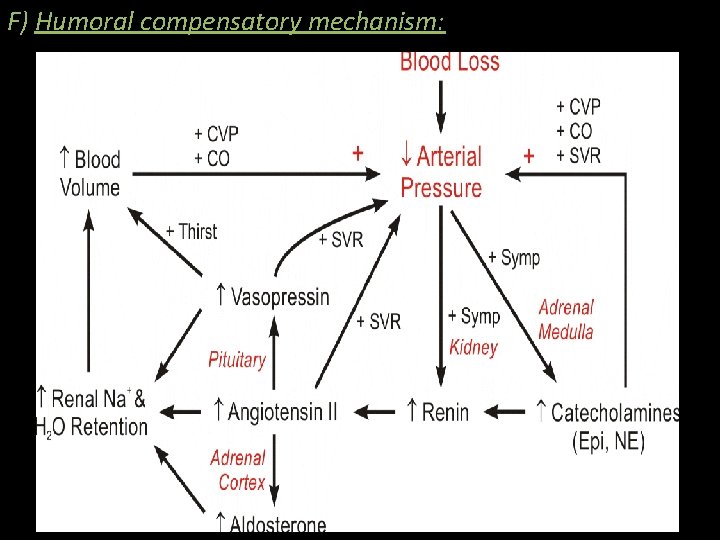
F) Humoral compensatory mechanism: 30
Renin-angiotensin mechanism is activated with further vasoconstriction & aldosterone release, causing salt & water retention. G) Release of ADH decreases the volume & urine concentration H) Shortening of coagulation time activation of fibrinolytic system sludging & leucocytosis 31
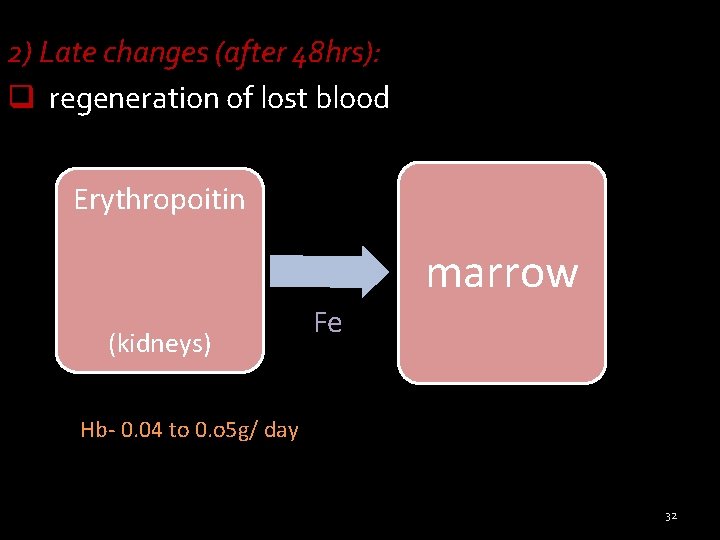
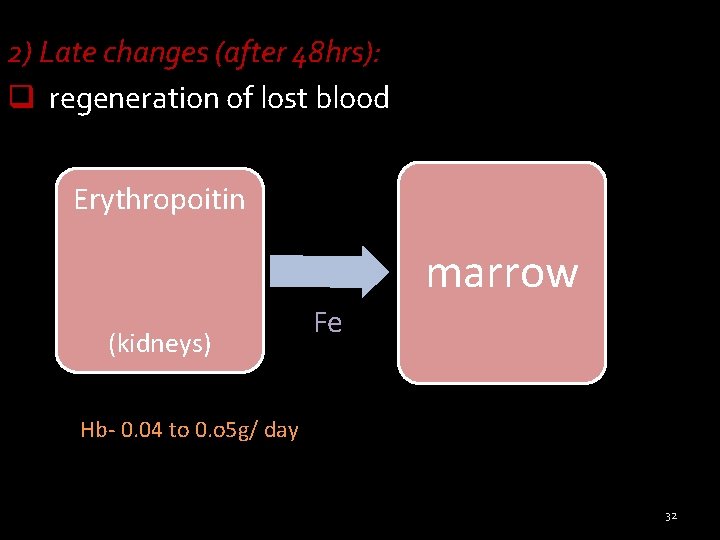
2) Late changes (after 48 hrs): q regeneration of lost blood Erythropoitin marrow (kidneys) Fe Hb- 0. 04 to 0. o 5 g/ day 32
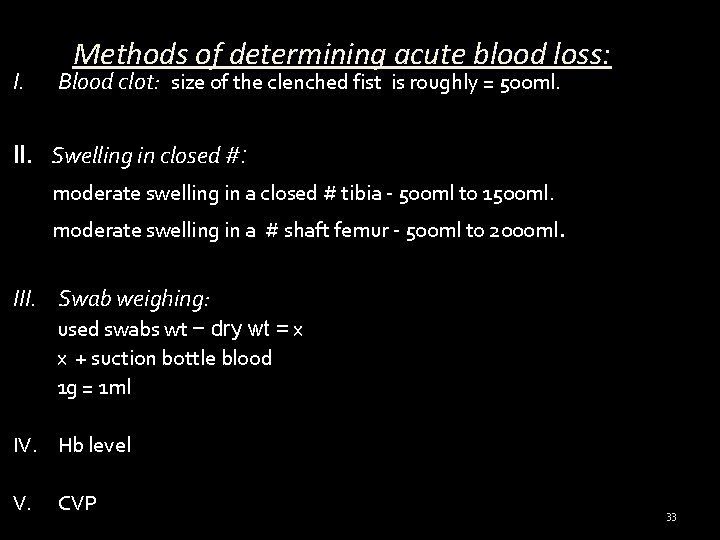
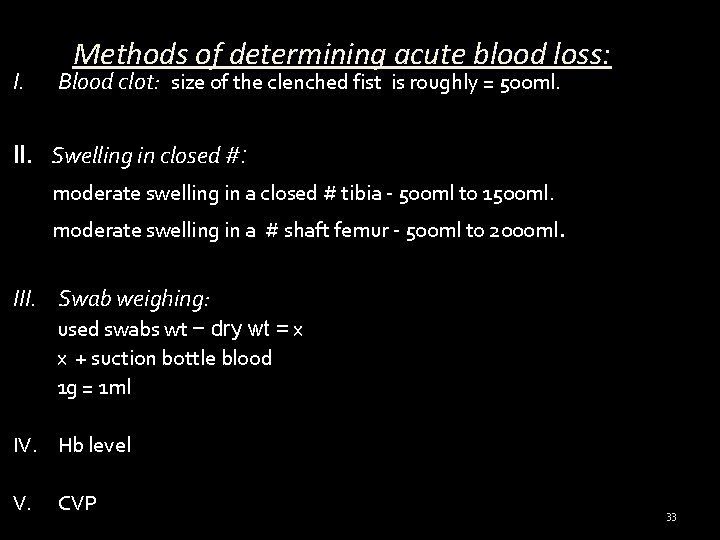
I. Methods of determining acute blood loss: Blood clot: size of the clenched fist is roughly = 500 ml. II. Swelling in closed #: moderate swelling in a closed # tibia - 500 ml to 1500 ml. moderate swelling in a # shaft femur - 500 ml to 2000 ml. III. Swab weighing: used swabs wt − dry wt = x x + suction bottle blood 1 g = 1 ml IV. Hb level V. CVP 33
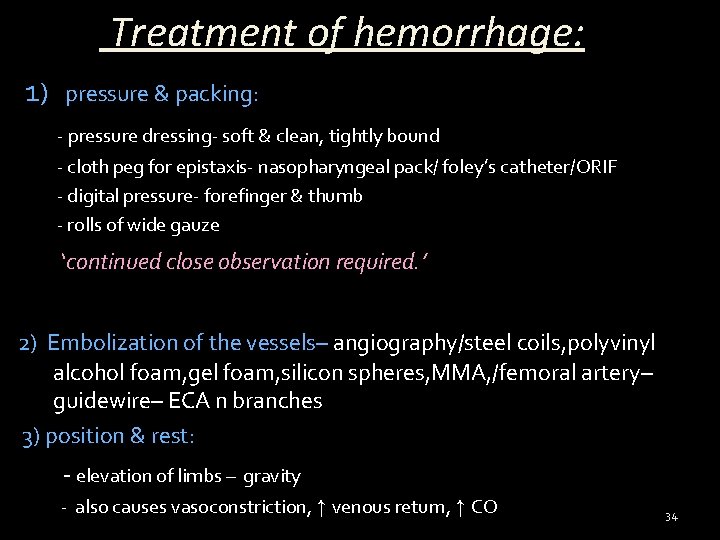
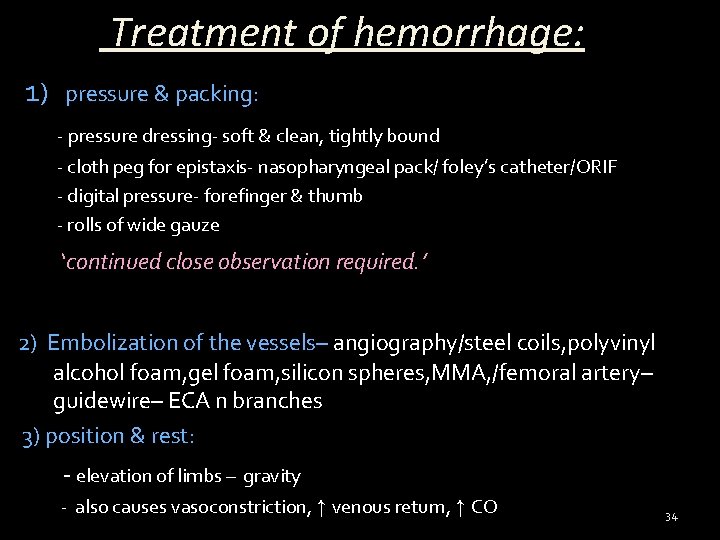
Treatment of hemorrhage: 1) pressure & packing: - pressure dressing- soft & clean, tightly bound - cloth peg for epistaxis- nasopharyngeal pack/ foley’s catheter/ORIF - digital pressure- forefinger & thumb - rolls of wide gauze ‘continued close observation required. ’ 2) Embolization of the vessels– angiography/steel coils, polyvinyl alcohol foam, gel foam, silicon spheres, MMA, /femoral artery– guidewire– ECA n branches 3) position & rest: - elevation of limbs – gravity - also causes vasoconstriction, ↑ venous return, ↑ CO 34
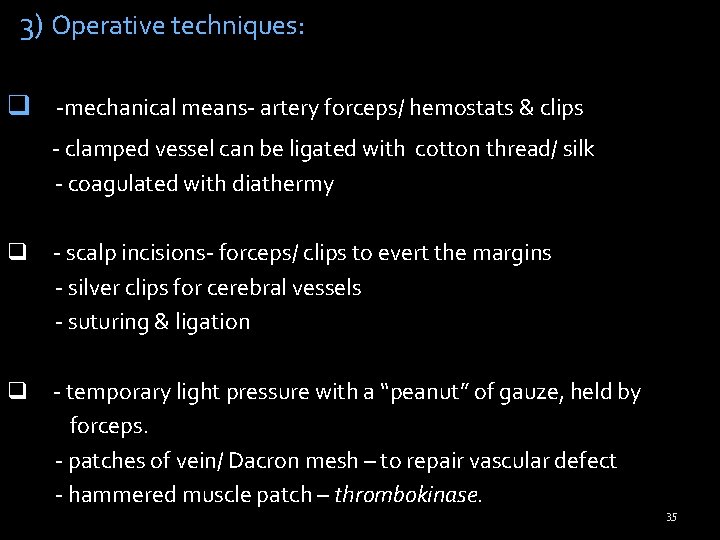
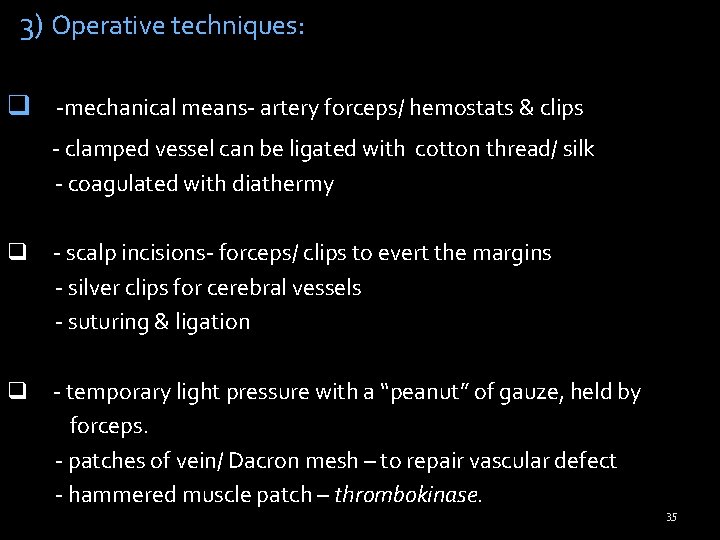
3) Operative techniques: q -mechanical means- artery forceps/ hemostats & clips - clamped vessel can be ligated with cotton thread/ silk - coagulated with diathermy q - scalp incisions- forceps/ clips to evert the margins - silver clips for cerebral vessels - suturing & ligation q - temporary light pressure with a “peanut” of gauze, held by forceps. - patches of vein/ Dacron mesh – to repair vascular defect - hammered muscle patch – thrombokinase. 35
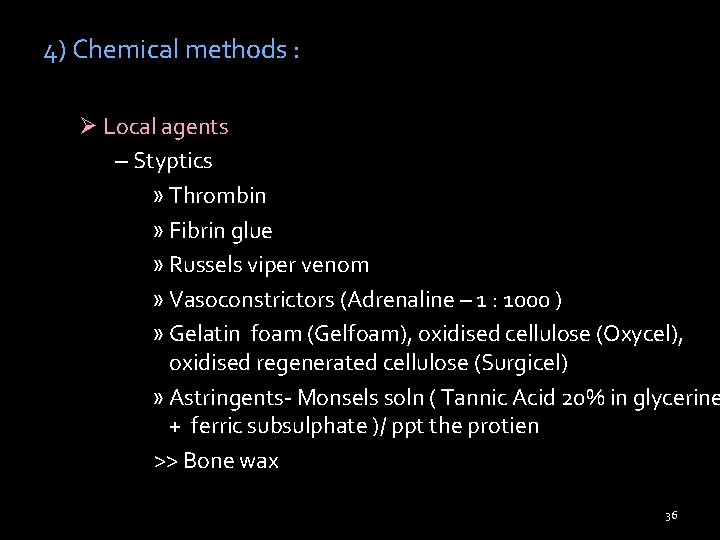
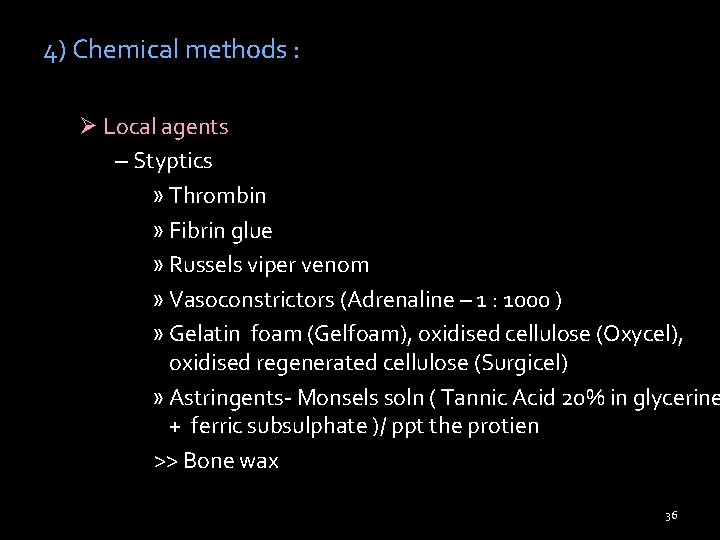
4) Chemical methods : Ø Local agents – Styptics » Thrombin » Fibrin glue » Russels viper venom » Vasoconstrictors (Adrenaline – 1 : 1000 ) » Gelatin foam (Gelfoam), oxidised cellulose (Oxycel), oxidised regenerated cellulose (Surgicel) » Astringents- Monsels soln ( Tannic Acid 20% in glycerine + ferric subsulphate )/ ppt the protien >> Bone wax 36
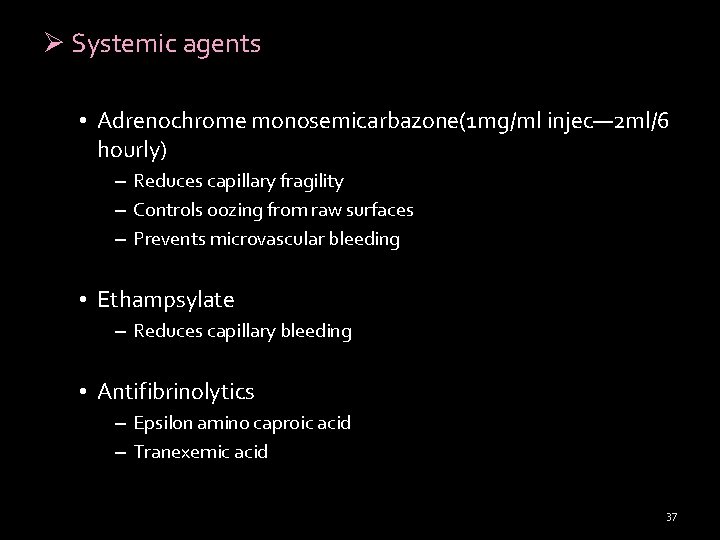
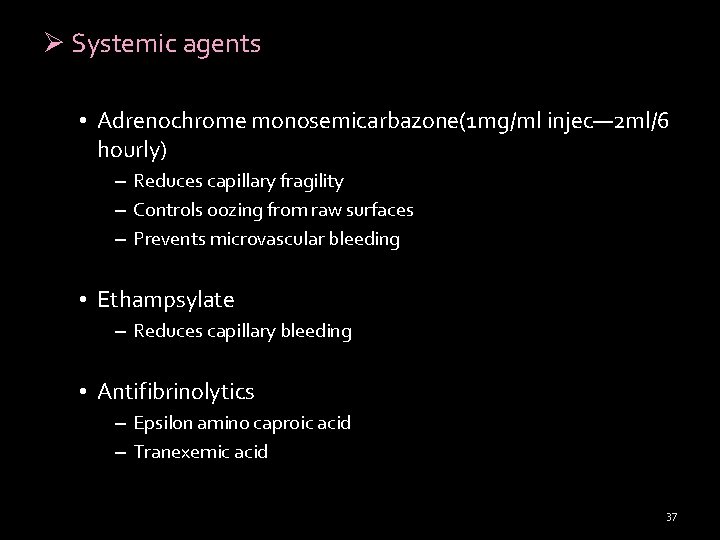
Ø Systemic agents • Adrenochrome monosemicarbazone(1 mg/ml injec— 2 ml/6 hourly) – Reduces capillary fragility – Controls oozing from raw surfaces – Prevents microvascular bleeding • Ethampsylate – Reduces capillary bleeding • Antifibrinolytics – Epsilon amino caproic acid – Tranexemic acid 37
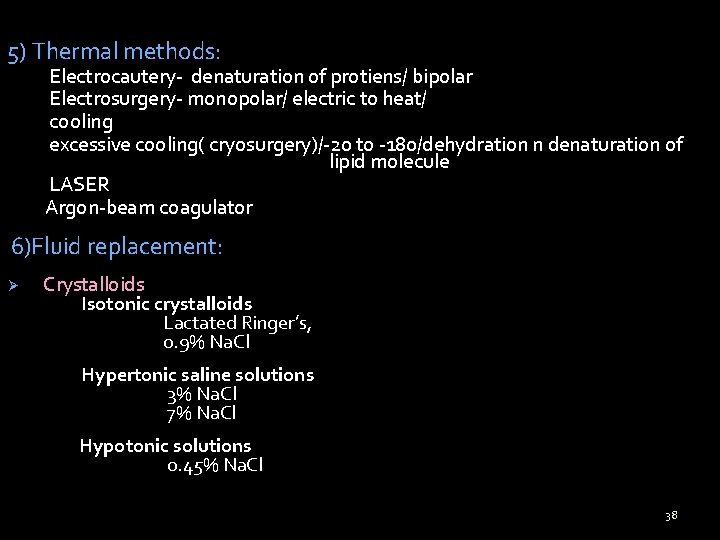
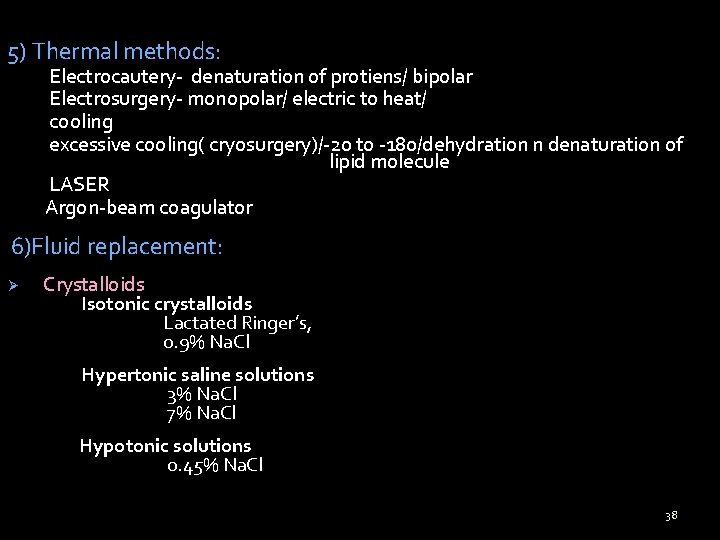
5) Thermal methods: Electrocautery- denaturation of protiens/ bipolar Electrosurgery- monopolar/ electric to heat/ cooling excessive cooling( cryosurgery)/-20 to -180/dehydration n denaturation of lipid molecule LASER Argon-beam coagulator 6)Fluid replacement: Ø Crystalloids Isotonic crystalloids Lactated Ringer’s, 0. 9% Na. Cl Hypertonic saline solutions 3% Na. Cl 7% Na. Cl Hypotonic solutions 0. 45% Na. Cl 38
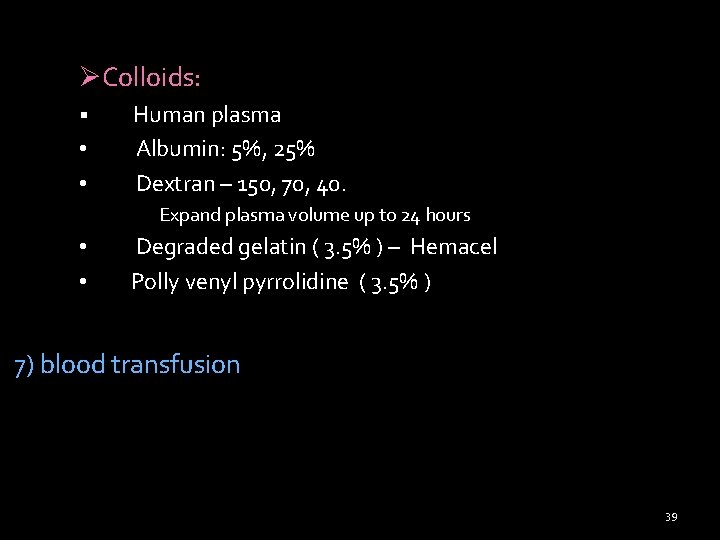
ØColloids: § • • Human plasma Albumin: 5%, 25% Dextran – 150, 70, 40. Expand plasma volume up to 24 hours • • Degraded gelatin ( 3. 5% ) – Hemacel Polly venyl pyrrolidine ( 3. 5% ) 7) blood transfusion 39
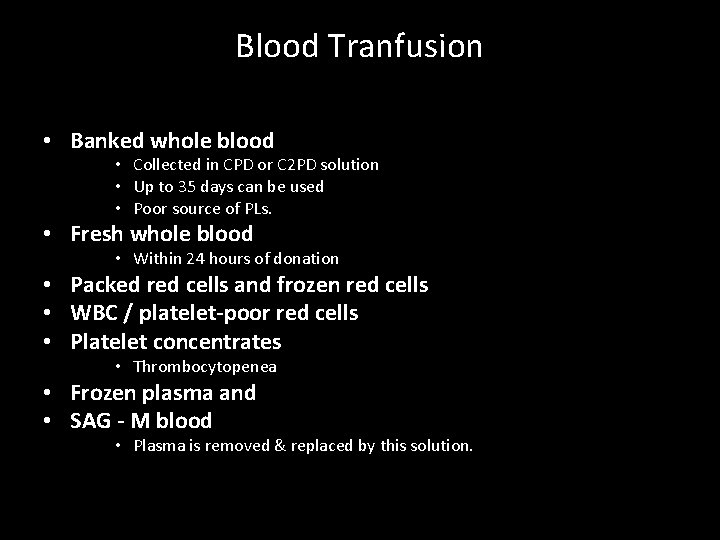
Blood Tranfusion • Banked whole blood • Collected in CPD or C 2 PD solution • Up to 35 days can be used • Poor source of PLs. • Fresh whole blood • Within 24 hours of donation • Packed red cells and frozen red cells • WBC / platelet-poor red cells • Platelet concentrates • Thrombocytopenea • Frozen plasma and • SAG - M blood • Plasma is removed & replaced by this solution.
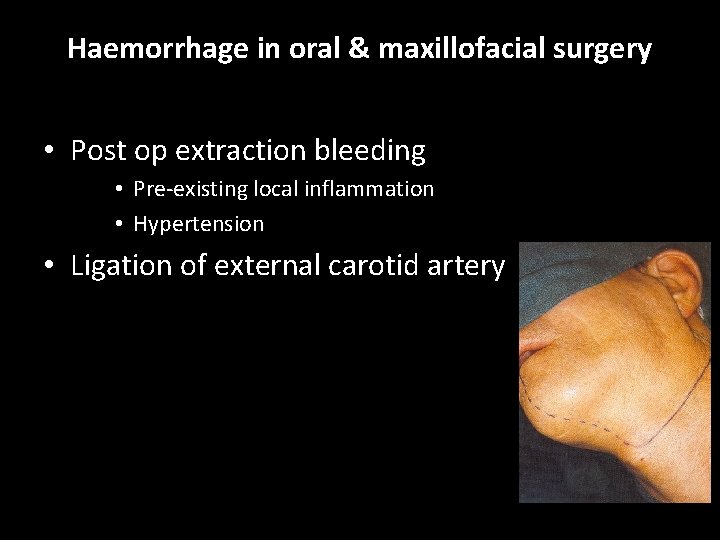
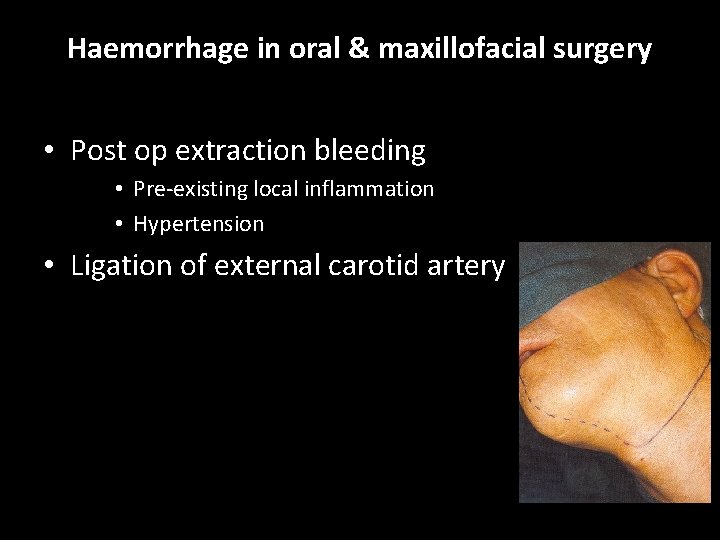
Haemorrhage in oral & maxillofacial surgery • Post op extraction bleeding • Pre-existing local inflammation • Hypertension • Ligation of external carotid artery
Haemorrhage in oral & maxillofacial surgery • Haemorrhage during the operation • • • Planning of the incision to avoid large blood vessels. Securing of blood vessels with haemostats. Hemostasis through the application of pressure with swabs The use of hemostatic agents (chemical) Hypotensive anaesthesia and vasoconstriction
 Itsm terms and terminologies
Itsm terms and terminologies Ethical hacking terminologies
Ethical hacking terminologies Security terminologies and principle
Security terminologies and principle Basic research terminology
Basic research terminology Homozygous dominant
Homozygous dominant Parenthetical referencing
Parenthetical referencing Antipartum hemorrhage
Antipartum hemorrhage Classes of hemorrhagic shock
Classes of hemorrhagic shock Hypercalcemia nephrogenic di
Hypercalcemia nephrogenic di Rheumatoid arthritis extra-articular manifestations
Rheumatoid arthritis extra-articular manifestations Spirit of jealousy manifestations
Spirit of jealousy manifestations Skin manifestations of hypothyroidism
Skin manifestations of hypothyroidism Swan neck deformity
Swan neck deformity Chapitre 3 l'énergie et ses manifestations
Chapitre 3 l'énergie et ses manifestations Fetomaternal hemorrhage
Fetomaternal hemorrhage B lynch suture
B lynch suture Pph treatment algorithm
Pph treatment algorithm Brain hemorrhage
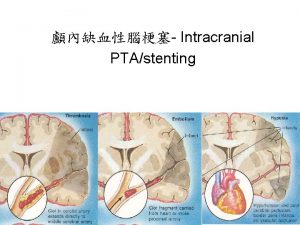
Brain hemorrhage Raina flores sex
Raina flores sex Complications of hydrocephalus
Complications of hydrocephalus Recreationary
Recreationary Lochia smell
Lochia smell Hunt and hess score
Hunt and hess score Post tonsillectomy hemorrhage
Post tonsillectomy hemorrhage Post tonsillectomy hemorrhage
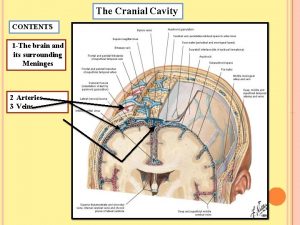
Post tonsillectomy hemorrhage Blood supply of dura mater
Blood supply of dura mater Secondary postpartum haemorrhage
Secondary postpartum haemorrhage Waiter's tip deformity
Waiter's tip deformity Antipartum hemorrhage
Antipartum hemorrhage Management of hemorrhage
Management of hemorrhage Management of hemorrhage
Management of hemorrhage Management of hemorrhage
Management of hemorrhage Triad of death
Triad of death Subconjunctival hemorrhage
Subconjunctival hemorrhage Hemorrhage
Hemorrhage Postpartum hemorrhage
Postpartum hemorrhage Hemorrhage
Hemorrhage Hemorrhage
Hemorrhage Gastroesophageal sphincter
Gastroesophageal sphincter Tracey whitley novant health
Tracey whitley novant health Homan signs
Homan signs Stamca
Stamca Rubeosis of iris
Rubeosis of iris