INVASIVE MECHANICAL VENTILATION D Sara Salarian Why ventilate
- Slides: 43
INVASIVE MECHANICAL VENTILATION D. Sara Salarian,
Why ventilate? Improve oxygenation Increase/maintain minute ventilation and help CO 2 clearance Decrease work of breathing Protect airway Nov 2006 Kishore P. Critical Care Conference
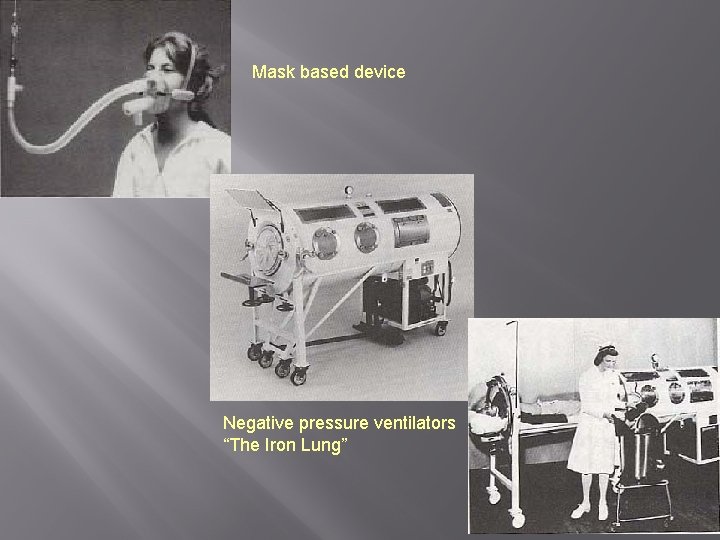
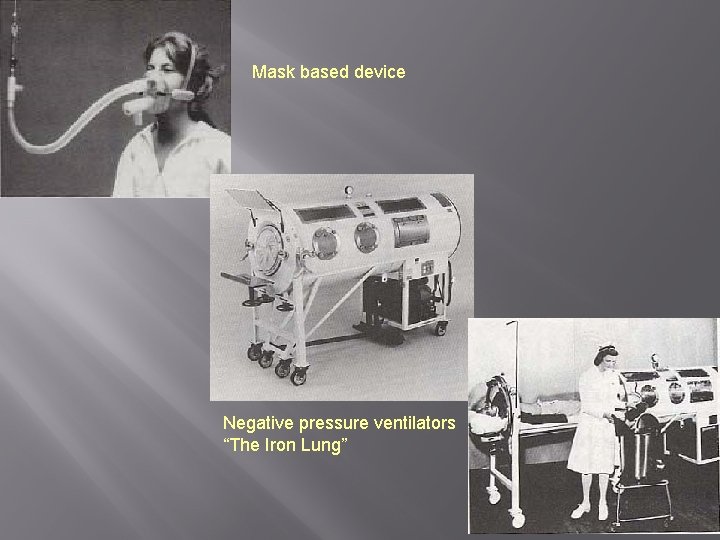
Mask based device Negative pressure ventilators “The Iron Lung”
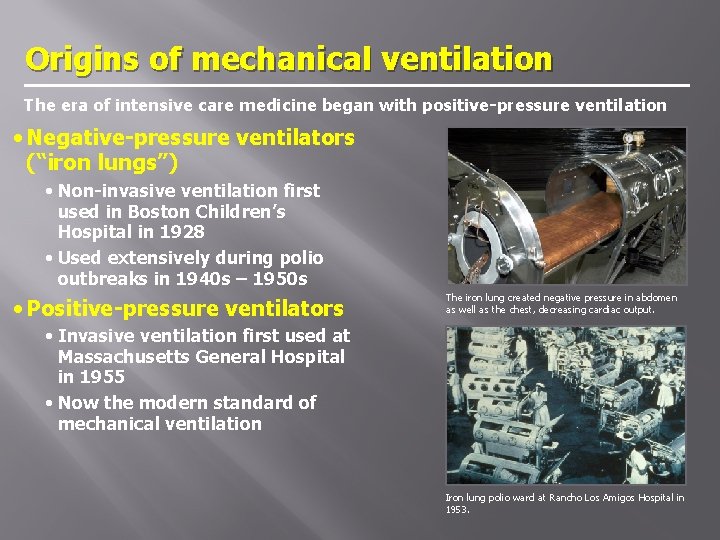
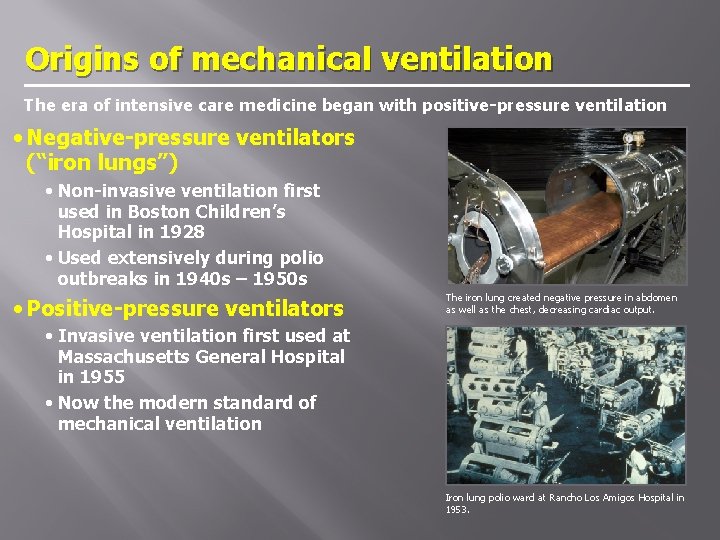
Origins of mechanical ventilation The era of intensive care medicine began with positive-pressure ventilation • Negative-pressure ventilators (“iron lungs”) • Non-invasive ventilation first used in Boston Children’s Hospital in 1928 • Used extensively during polio outbreaks in 1940 s – 1950 s • Positive-pressure ventilators The iron lung created negative pressure in abdomen as well as the chest, decreasing cardiac output. • Invasive ventilation first used at Massachusetts General Hospital in 1955 • Now the modern standard of mechanical ventilation Iron lung polio ward at Rancho Los Amigos Hospital in 1953.
Modes of Mechanical Ventilation Spontaneous/Controlled/Dual Controlled Mechanical Ventilation (CMV) Assist Control (AC)/Volume Control (VC) Intermittent Mandatory Ventilation (SIMV) Pressure Control (PCV) Pressure Support Ventilation (PSV)
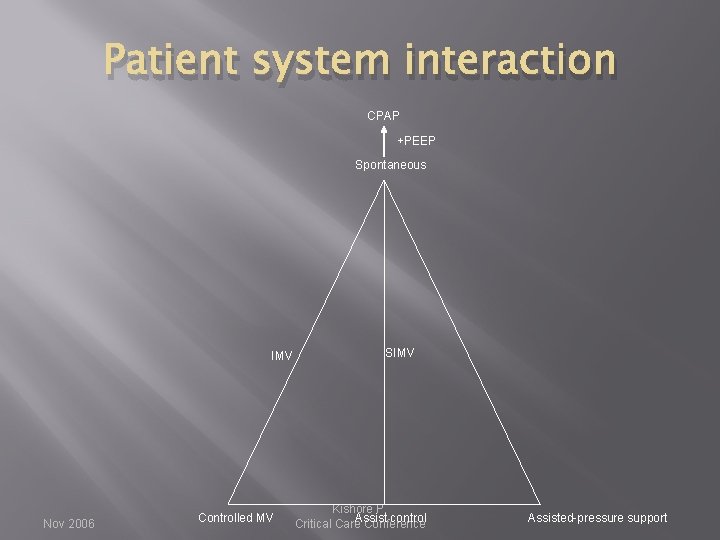
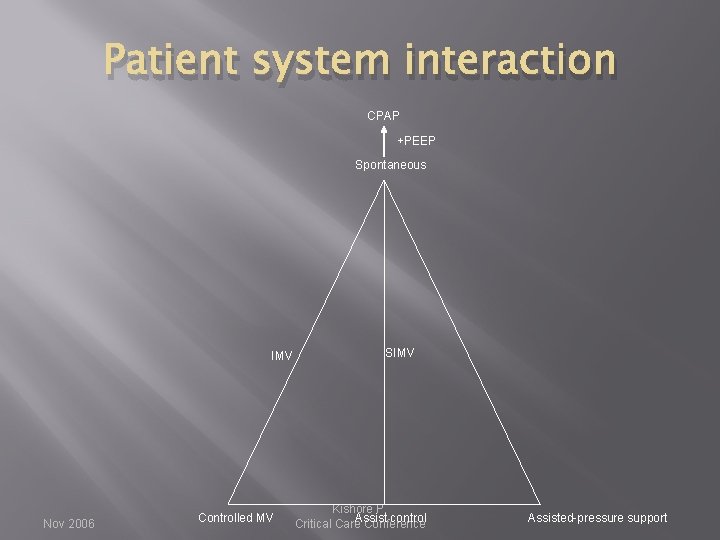
Patient system interaction CPAP +PEEP Spontaneous IMV Nov 2006 Controlled MV SIMV Kishore P. control Critical Care. Assist Conference Assisted-pressure support
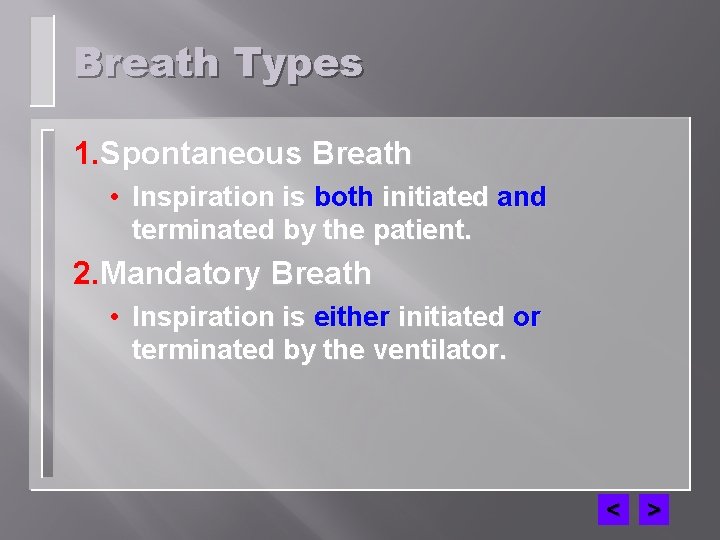
Breath Types 1. Spontaneous Breath • Inspiration is both initiated and terminated by the patient. 2. Mandatory Breath • Inspiration is either initiated or terminated by the ventilator. < >
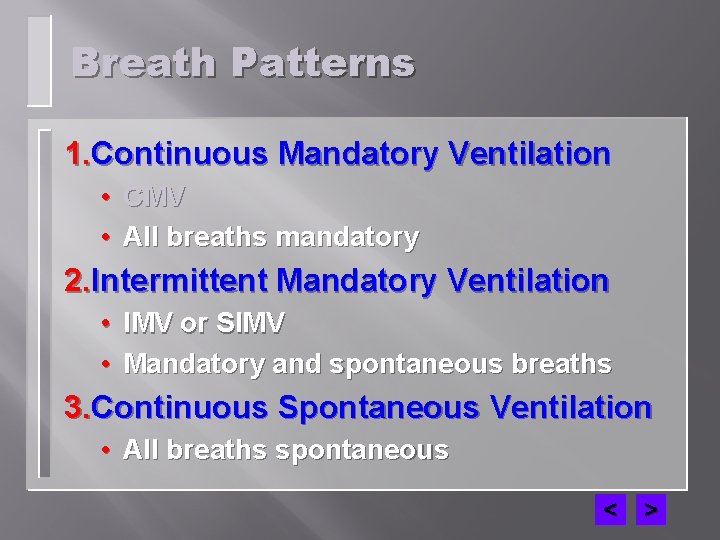
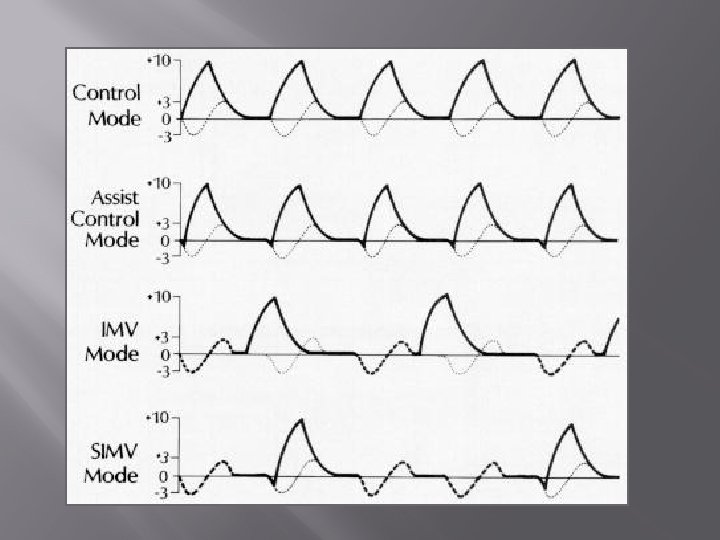
Breath Patterns 1. Continuous Mandatory Ventilation • CMV • All breaths mandatory 2. Intermittent Mandatory Ventilation • IMV or SIMV • Mandatory and spontaneous breaths 3. Continuous Spontaneous Ventilation • All breaths spontaneous < >
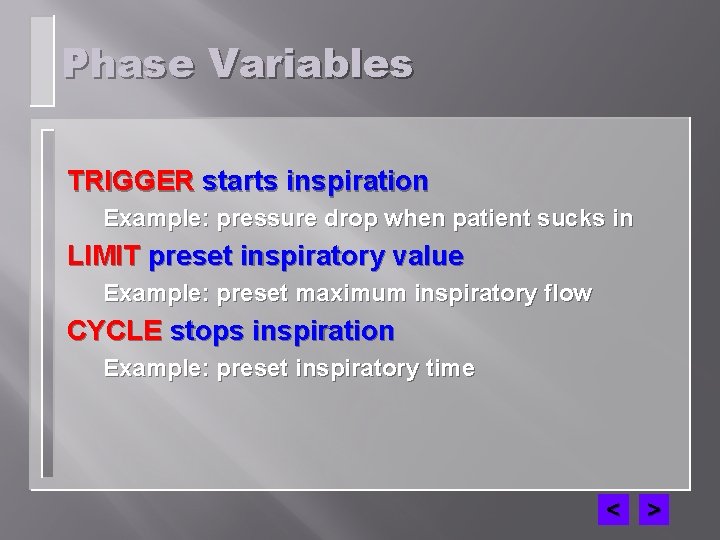
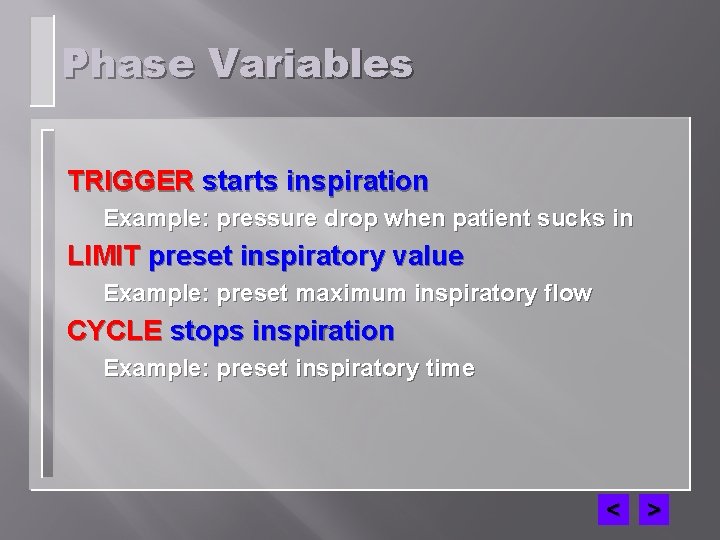
Phase Variables TRIGGER starts inspiration Example: pressure drop when patient sucks in LIMIT preset inspiratory value Example: preset maximum inspiratory flow CYCLE stops inspiration Example: preset inspiratory time < >
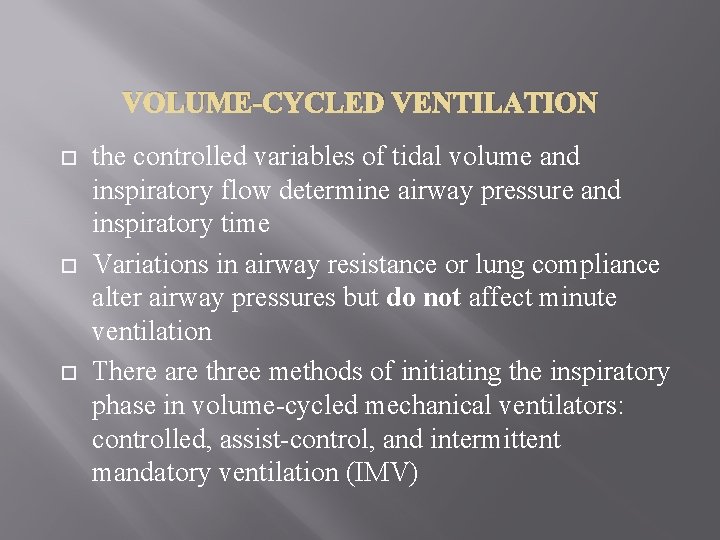
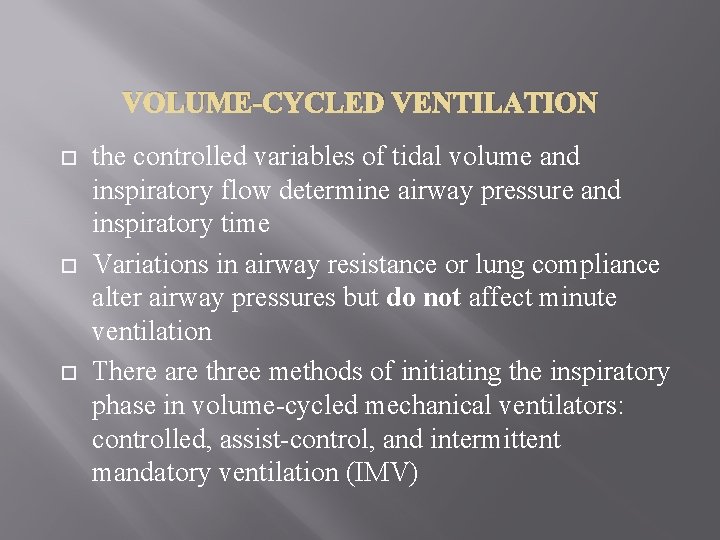
VOLUME-CYCLED VENTILATION the controlled variables of tidal volume and inspiratory flow determine airway pressure and inspiratory time Variations in airway resistance or lung compliance alter airway pressures but do not affect minute ventilation There are three methods of initiating the inspiratory phase in volume-cycled mechanical ventilators: controlled, assist-control, and intermittent mandatory ventilation (IMV)
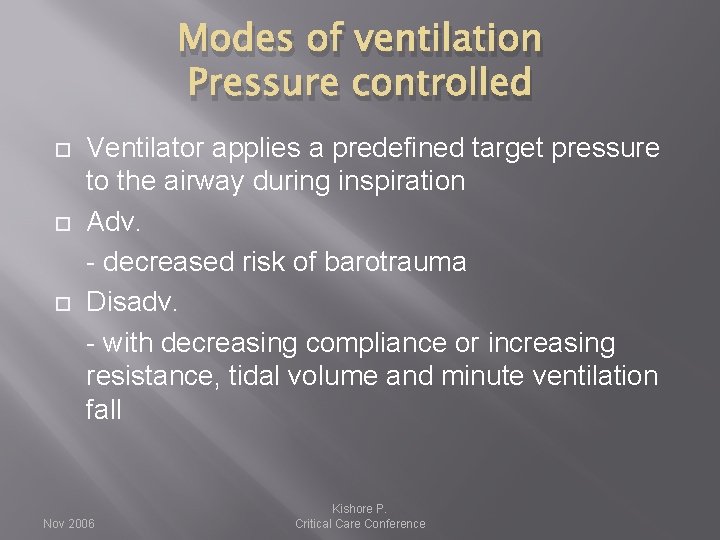
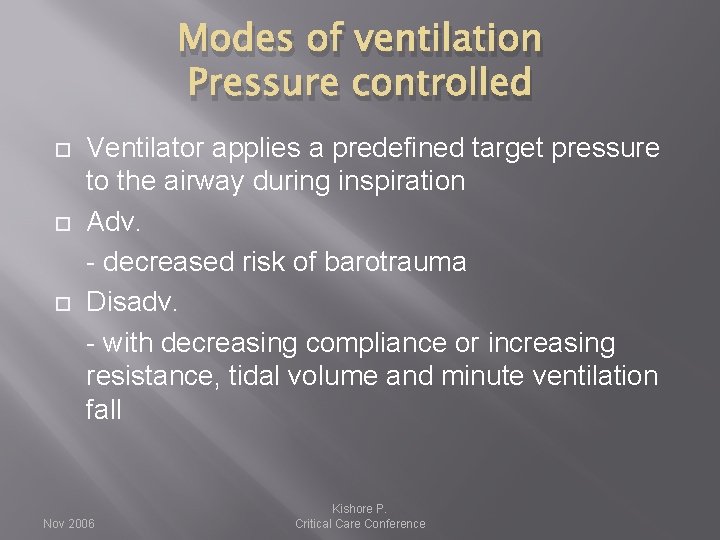
Modes of ventilation Pressure controlled Ventilator applies a predefined target pressure to the airway during inspiration Adv. - decreased risk of barotrauma Disadv. - with decreasing compliance or increasing resistance, tidal volume and minute ventilation fall Nov 2006 Kishore P. Critical Care Conference
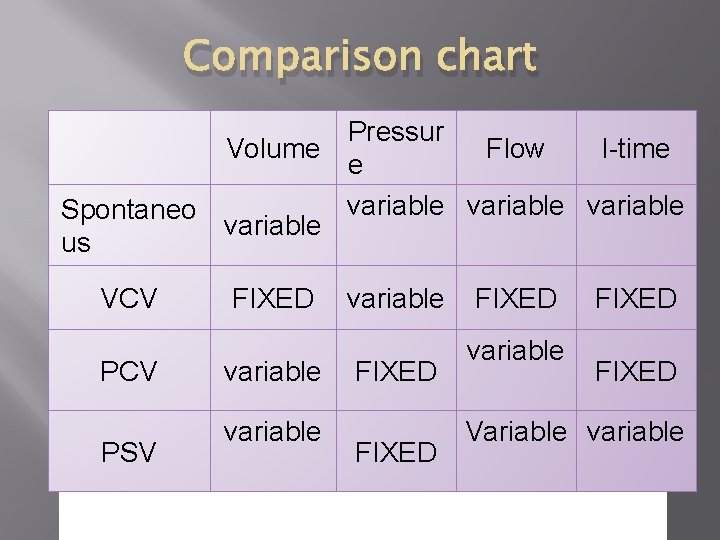
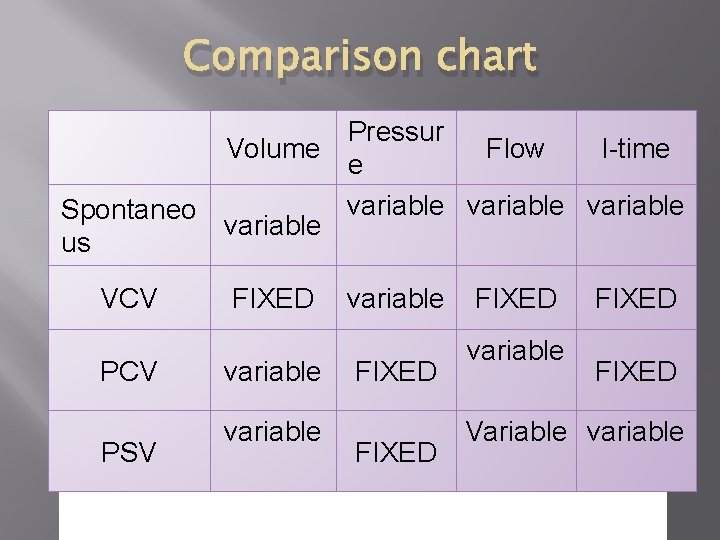
Comparison chart Pressur Volume Flow I-time e variable Spontaneo variable us VCV PSV FIXED variable FIXED variable FIXED Variable variable
MODES OF PPV
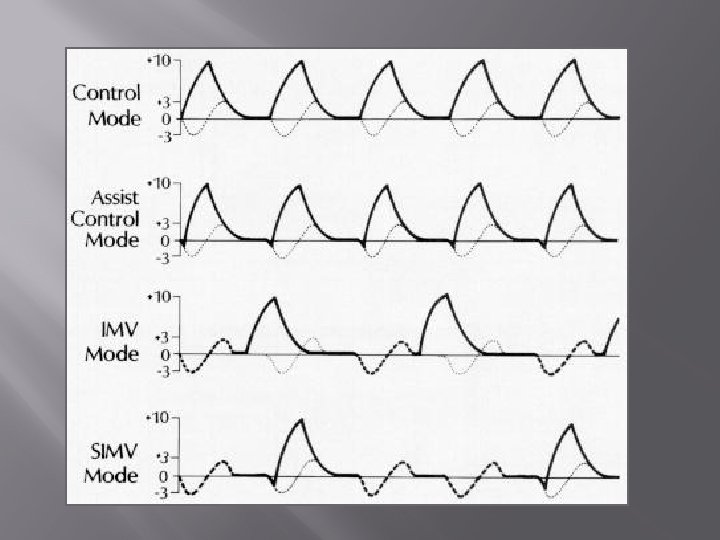
Controlled mechanical ventilation (CMV) minute ventilation is completely dependent upon the rate and tidal volume set on the ventilator. Any respiratory efforts made by the patient do not contribute to minute ventilation Controlled ventilation is the required ventilatory mode in patients who are making no respiratory effort (eg, spinal cord injury or drug overdose and those who have been subjected to pharmacologic paralysis).
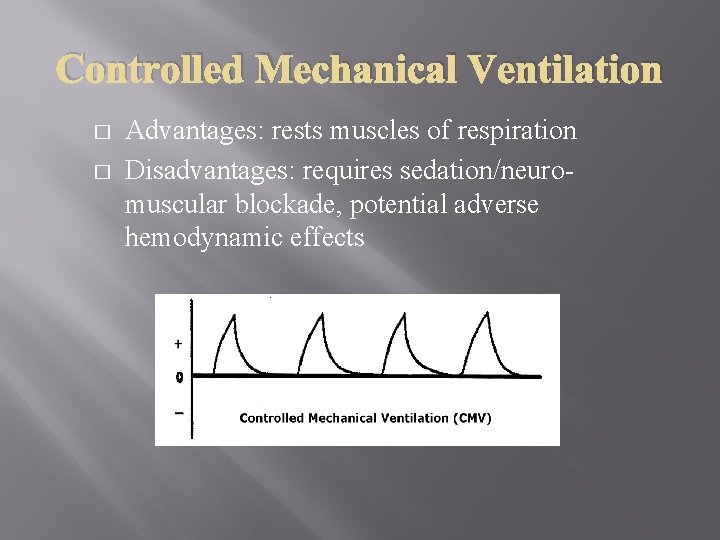
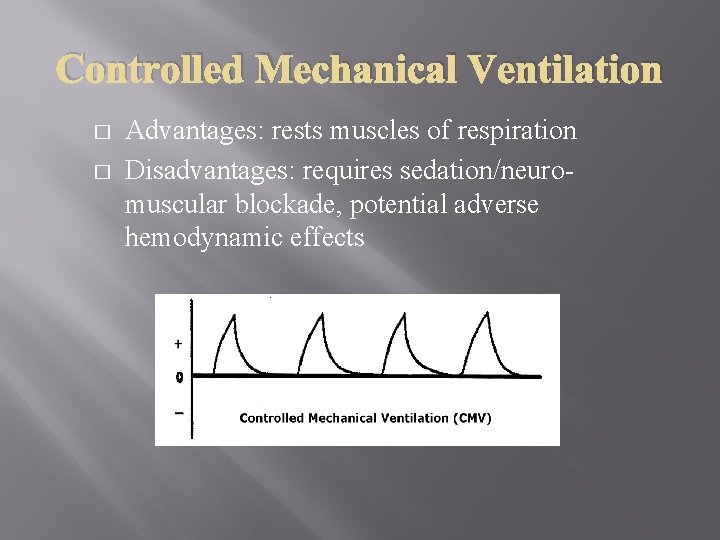
Controlled Mechanical Ventilation � � Advantages: rests muscles of respiration Disadvantages: requires sedation/neuromuscular blockade, potential adverse hemodynamic effects
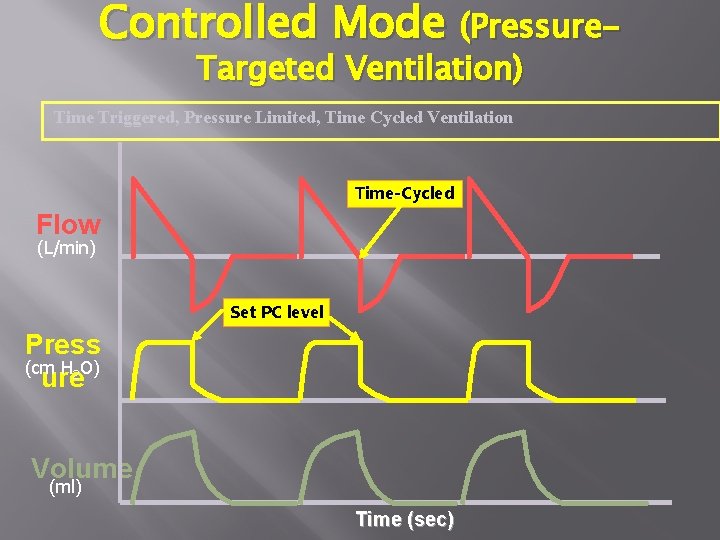
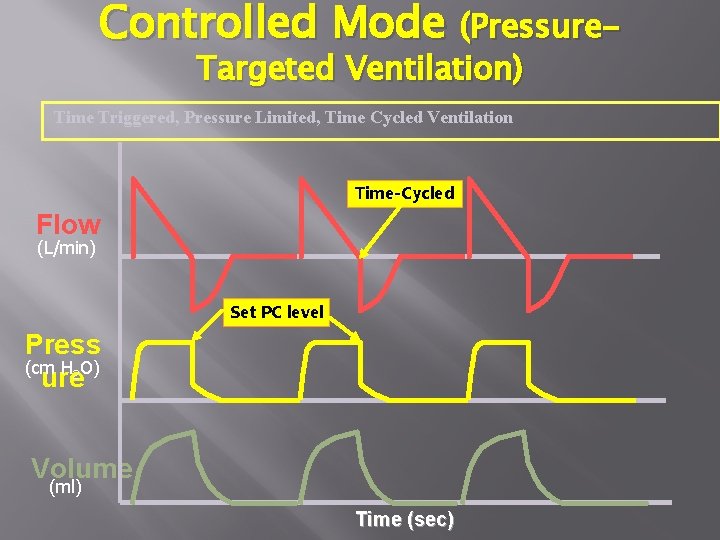
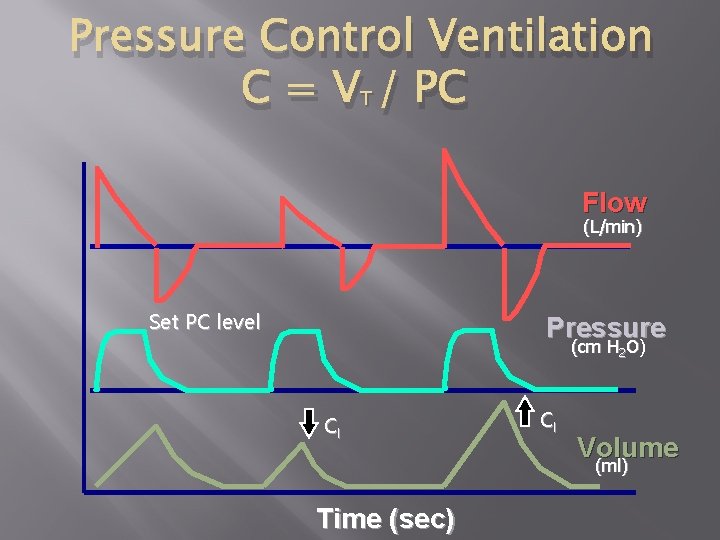
Controlled Mode (Pressure. Targeted Ventilation) Time Triggered, Pressure Limited, Time Cycled Ventilation Time-Cycled Time- Flow (L/min) Set PC level Press (cm H 2 O) ure Volume (ml) Time (sec)
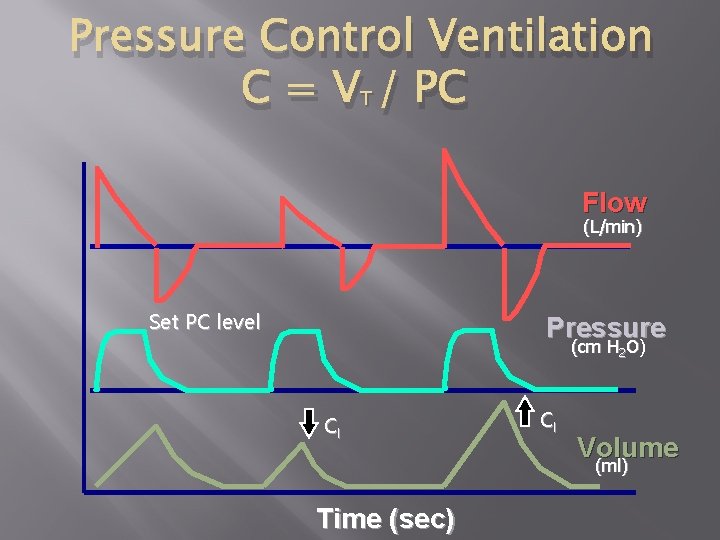
Pressure Control Ventilation C = VT / PC Flow (L/min) Set PC level Pressure (cm H 2 O) Cl Cl Volume (ml) Time (sec)
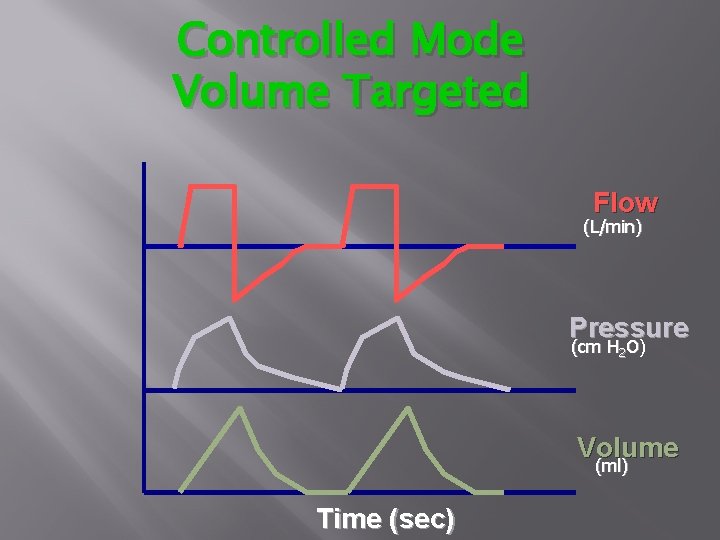
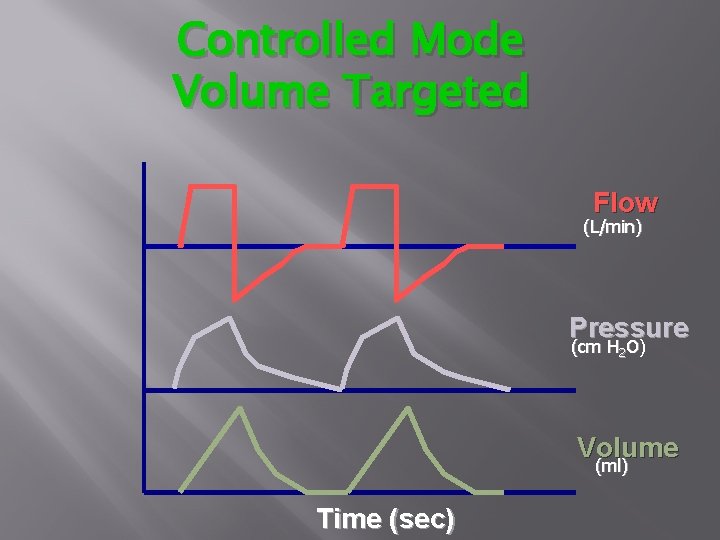
Controlled Mode Volume Targeted Flow (L/min) Pressure (cm H 2 O) Volume (ml) Time (sec)
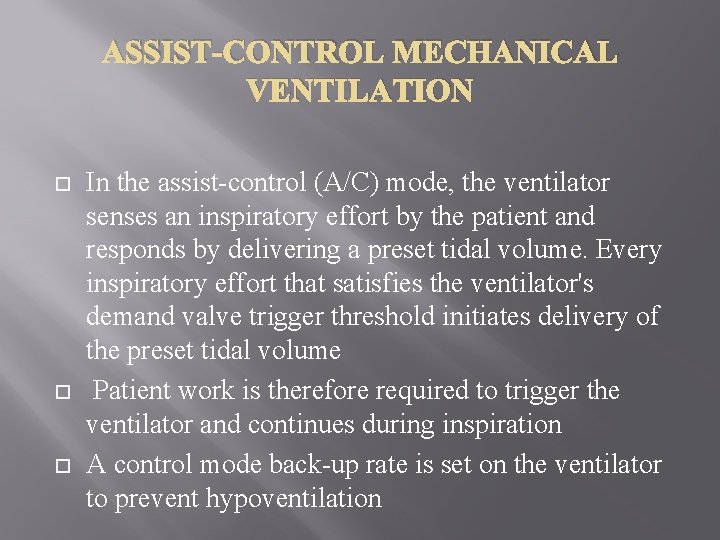
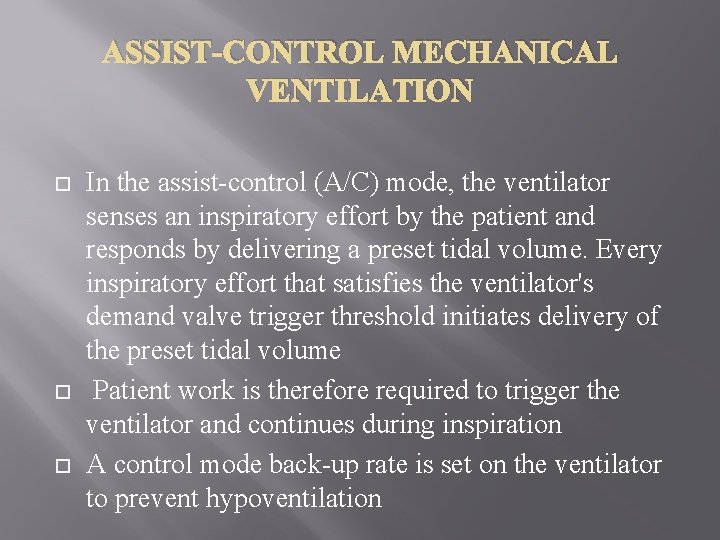
ASSIST-CONTROL MECHANICAL VENTILATION In the assist-control (A/C) mode, the ventilator senses an inspiratory effort by the patient and responds by delivering a preset tidal volume. Every inspiratory effort that satisfies the ventilator's demand valve trigger threshold initiates delivery of the preset tidal volume Patient work is therefore required to trigger the ventilator and continues during inspiration A control mode back-up rate is set on the ventilator to prevent hypoventilation
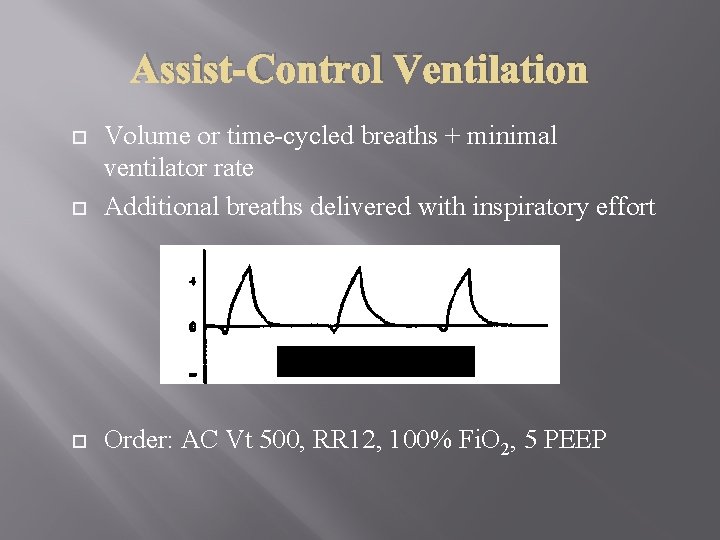
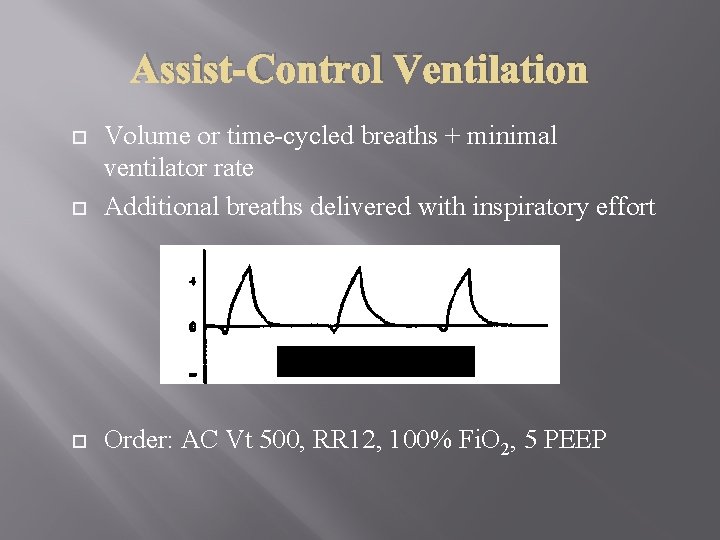
Assist-Control Ventilation Volume or time-cycled breaths + minimal ventilator rate Additional breaths delivered with inspiratory effort Order: AC Vt 500, RR 12, 100% Fi. O 2, 5 PEEP
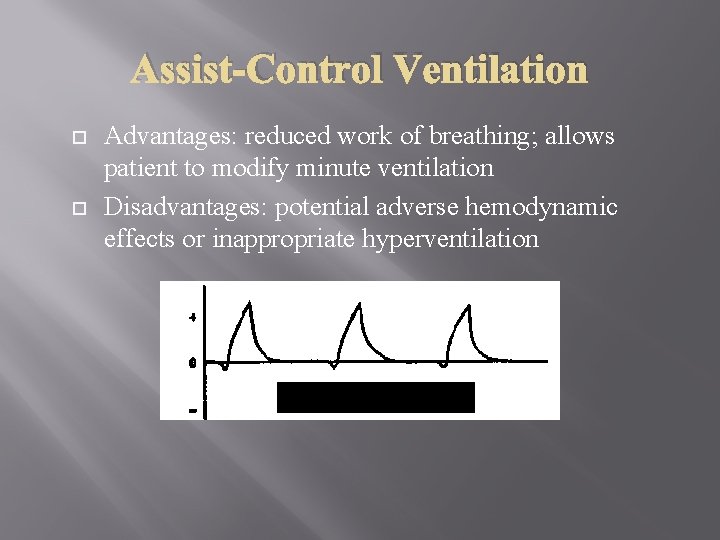
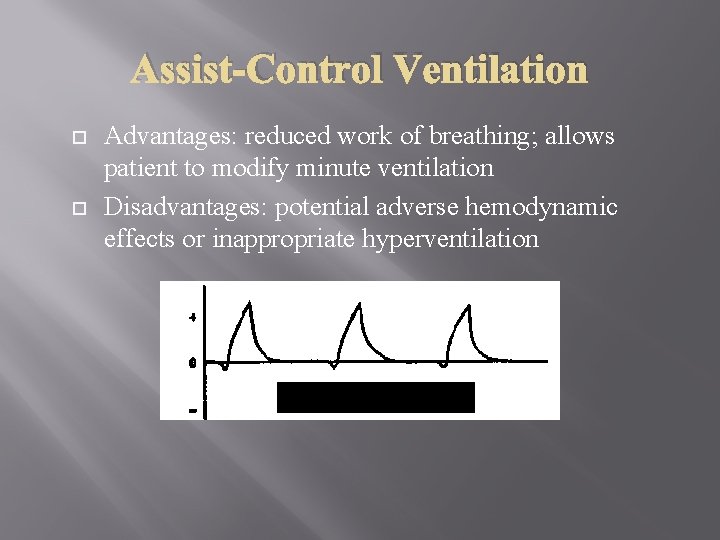
Assist-Control Ventilation Advantages: reduced work of breathing; allows patient to modify minute ventilation Disadvantages: potential adverse hemodynamic effects or inappropriate hyperventilation
INTERMITTENT MANDATORY VENTILATION � � With intermittent mandatory ventilation (IMV), the degree of ventilatory support is determined by the selected IMV rate. At regular intervals, the ventilator delivers a breath based upon a preset tidal volume and rate. In addition, the patient is allowed to breathe spontaneously through the ventilator circuit at a tidal volume and rate determined according to need and capacity. Most present day ventilators synchronize the intermittent ventilator breaths with inspiratory effort by the patient, a modality termed synchronized IMV or SIMV. However, this modification requires a trigger modality
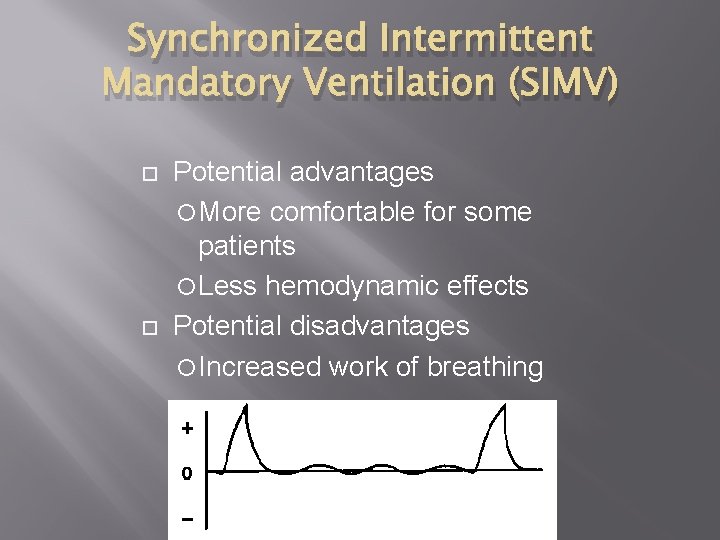
Synchronized Intermittent Mandatory Ventilation (SIMV) Potential advantages More comfortable for some patients Less hemodynamic effects Potential disadvantages Increased work of breathing
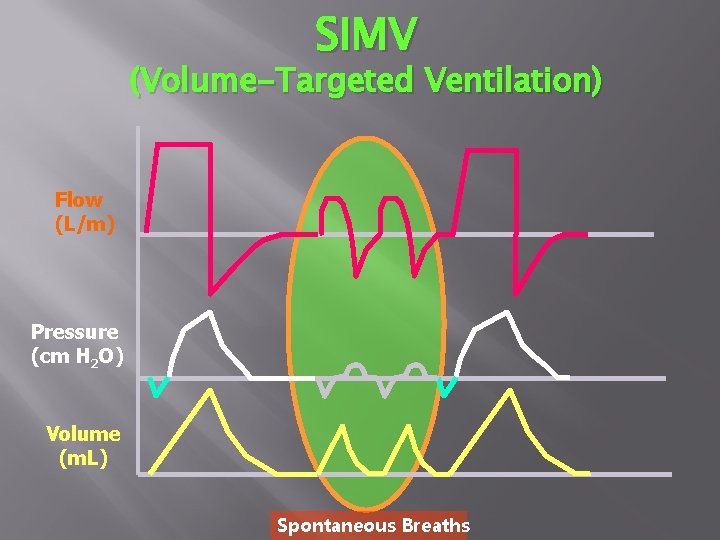
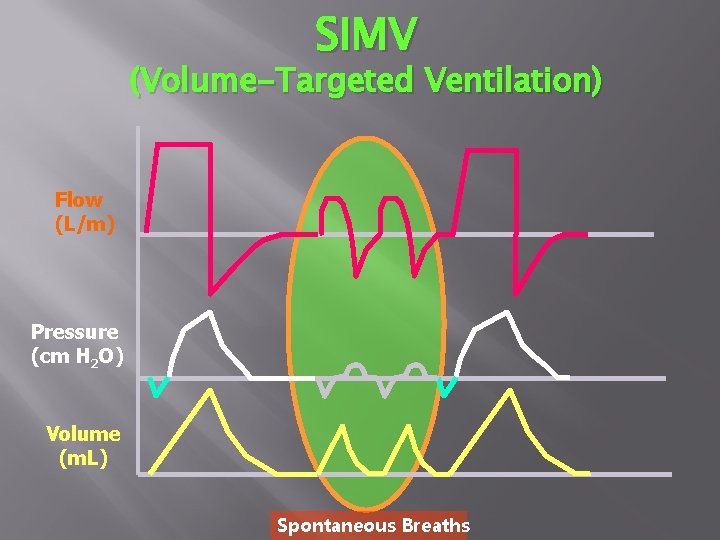
SIMV (Volume-Targeted Ventilation) Flow (L/m) Pressure (cm H 2 O) Volume (m. L) Spontaneous Breaths
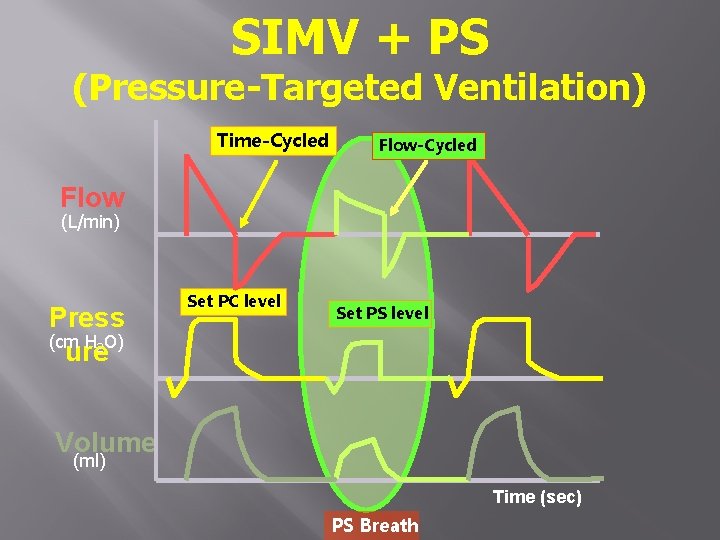
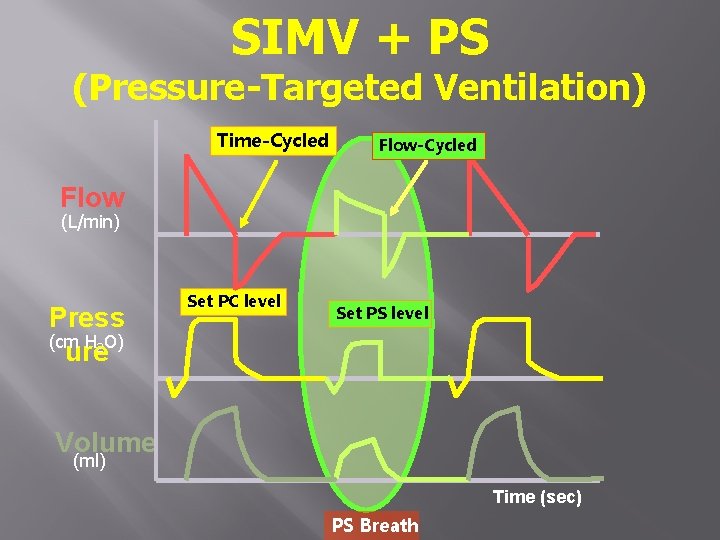
SIMV + PS (Pressure-Targeted Ventilation) Time-Cycled Flow (L/min) Press (cm H 2 O) ure Set PC level Set PS level Volume (ml) Time (sec) PS Breath
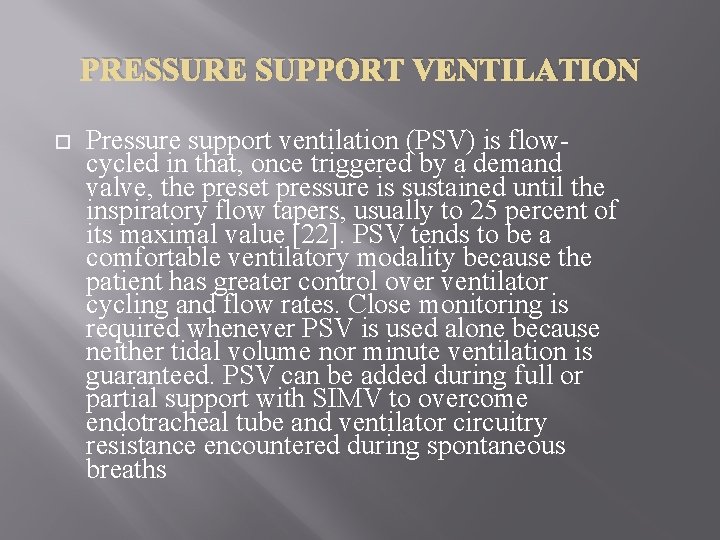
PRESSURE SUPPORT VENTILATION Pressure support ventilation (PSV) is flowcycled in that, once triggered by a demand valve, the preset pressure is sustained until the inspiratory flow tapers, usually to 25 percent of its maximal value [22]. PSV tends to be a comfortable ventilatory modality because the patient has greater control over ventilator cycling and flow rates. Close monitoring is required whenever PSV is used alone because neither tidal volume nor minute ventilation is guaranteed. PSV can be added during full or partial support with SIMV to overcome endotracheal tube and ventilator circuitry resistance encountered during spontaneous breaths
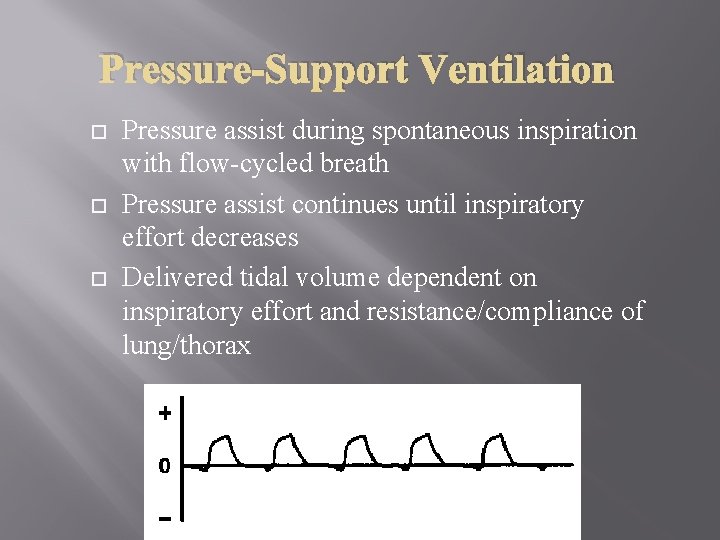
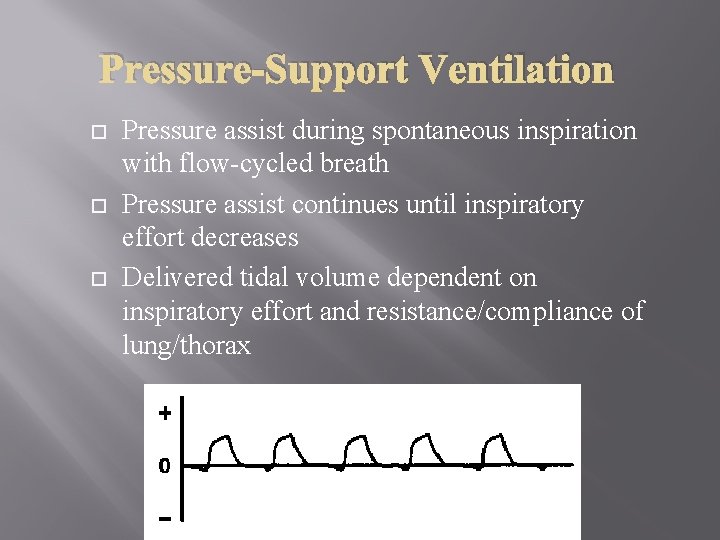
Pressure-Support Ventilation Pressure assist during spontaneous inspiration with flow-cycled breath Pressure assist continues until inspiratory effort decreases Delivered tidal volume dependent on inspiratory effort and resistance/compliance of lung/thorax Order: PS 10, PEEP 0, 50% Fi. O
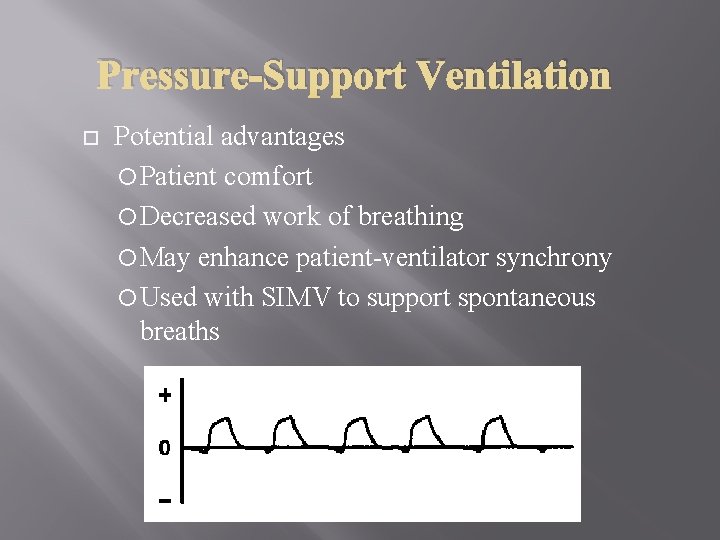
Pressure-Support Ventilation Potential advantages Patient comfort Decreased work of breathing May enhance patient-ventilator synchrony Used with SIMV to support spontaneous breaths
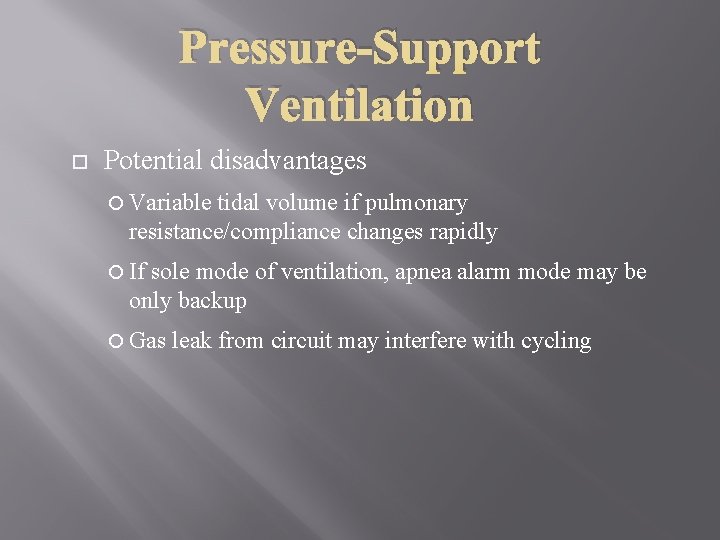
Pressure-Support Ventilation Potential disadvantages Variable tidal volume if pulmonary resistance/compliance changes rapidly If sole mode of ventilation, apnea alarm mode may be only backup Gas leak from circuit may interfere with cycling
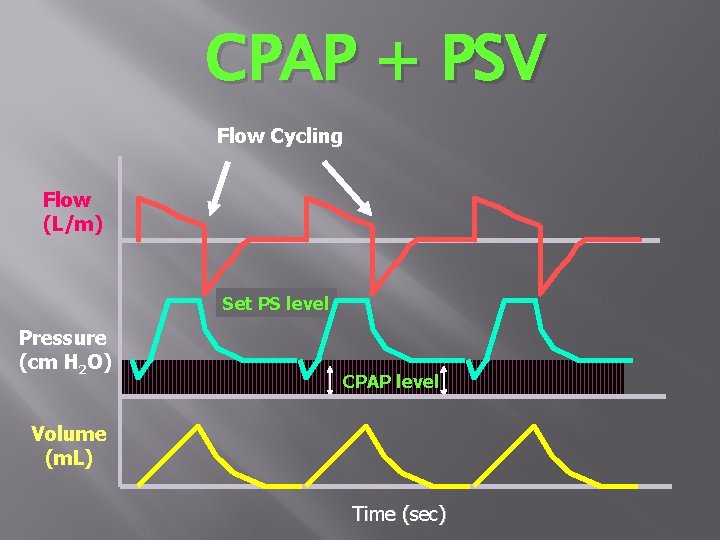
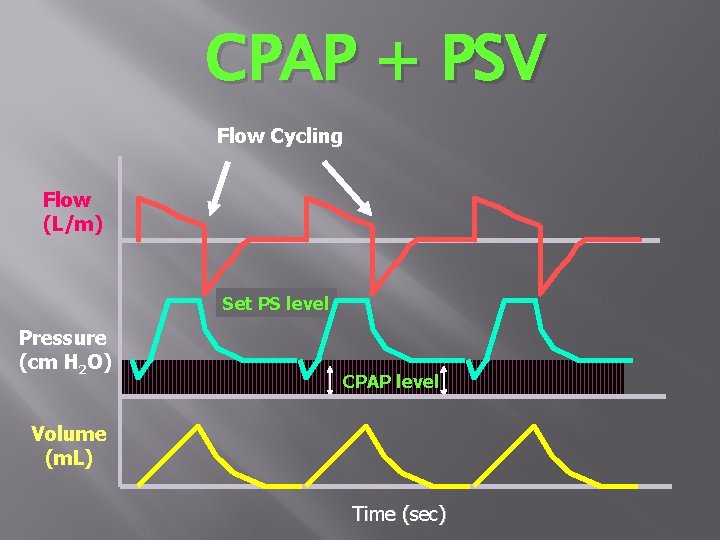
CPAP + PSV Flow Cycling Flow (L/m) Set PS level Pressure (cm H 2 O) CPAP level Volume (m. L) Time (sec)
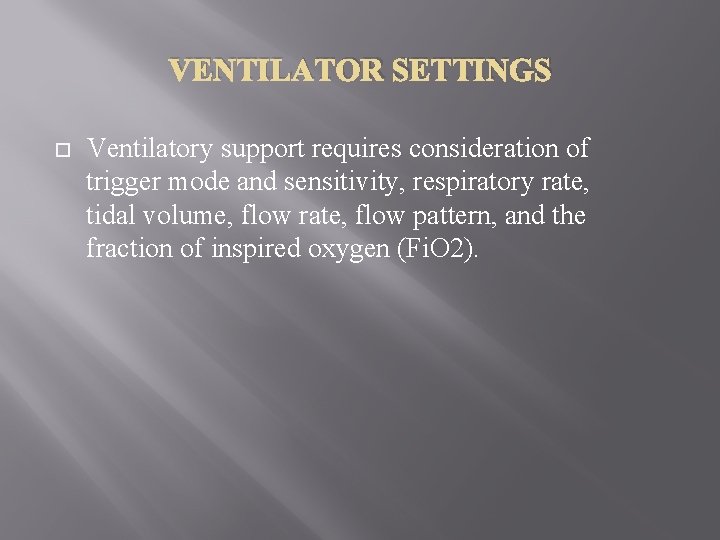
VENTILATOR SETTINGS Ventilatory support requires consideration of trigger mode and sensitivity, respiratory rate, tidal volume, flow rate, flow pattern, and the fraction of inspired oxygen (Fi. O 2).
Ventilator Settings Mode Rate Volume (VT) Pressure FIO 2 PEEP I: E
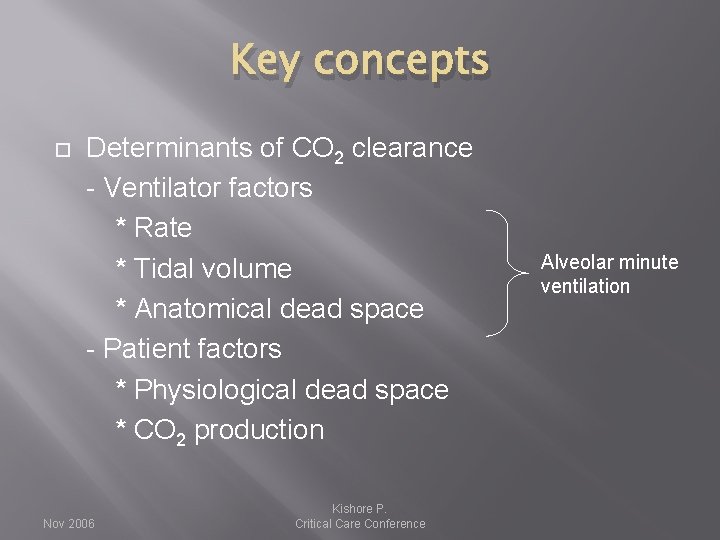
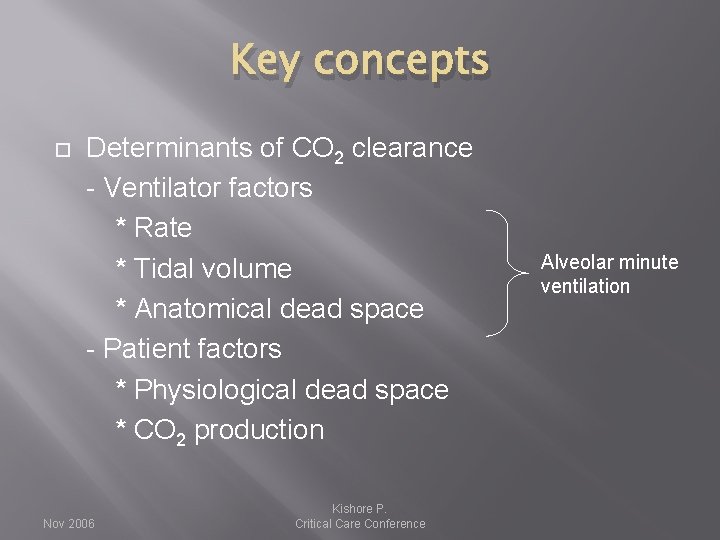
Key concepts Determinants of CO 2 clearance - Ventilator factors * Rate * Tidal volume * Anatomical dead space - Patient factors * Physiological dead space * CO 2 production Nov 2006 Kishore P. Critical Care Conference Alveolar minute ventilation
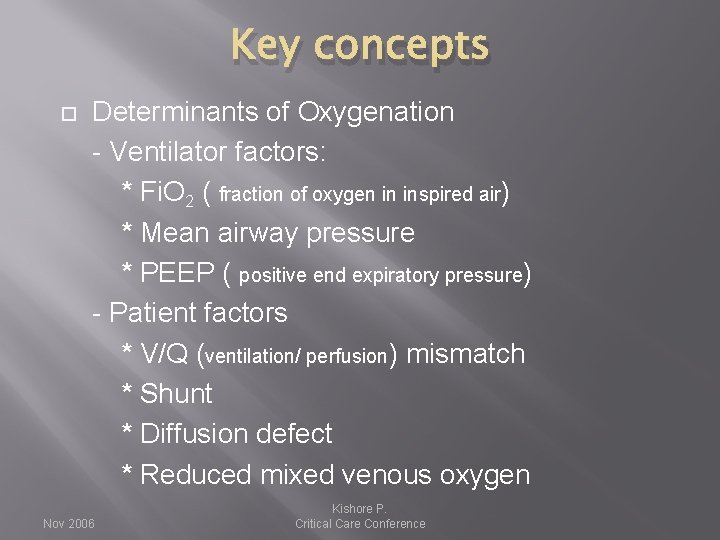
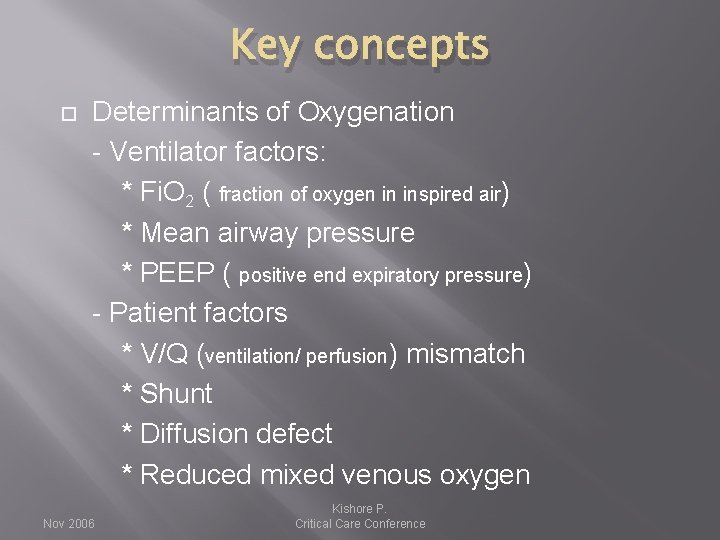
Key concepts Determinants of Oxygenation - Ventilator factors: * Fi. O 2 ( fraction of oxygen in inspired air) * Mean airway pressure * PEEP ( positive end expiratory pressure) - Patient factors * V/Q (ventilation/ perfusion) mismatch * Shunt * Diffusion defect * Reduced mixed venous oxygen Nov 2006 Kishore P. Critical Care Conference
Adjust Fi. O 2 and PEEP according to Pa. O 2 and Sp. O 2 Adjust TV and rate according to PCO 2 and p. H Nov 2006 Kishore P. Critical Care Conference
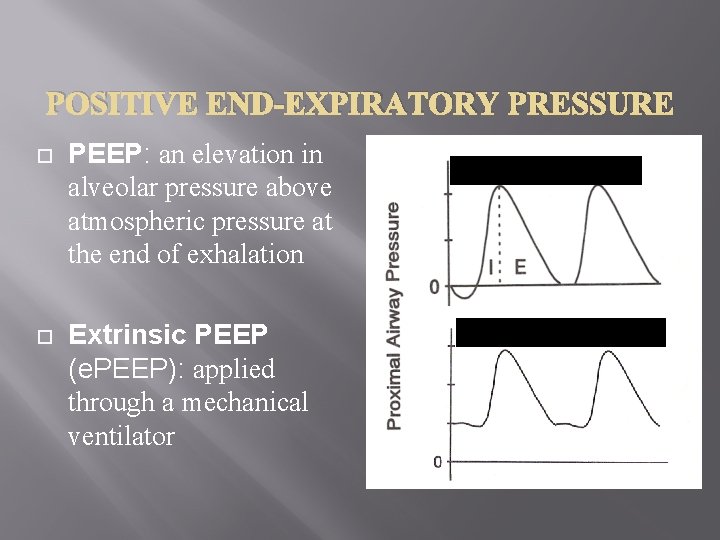
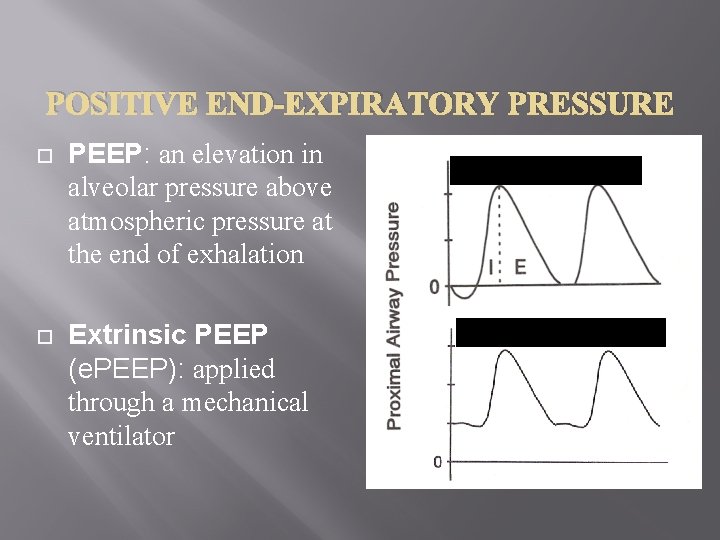
POSITIVE END-EXPIRATORY PRESSURE PEEP: an elevation in alveolar pressure above atmospheric pressure at the end of exhalation Extrinsic PEEP (e. PEEP): applied through a mechanical ventilator ACV without PEEP ACV with PEEP
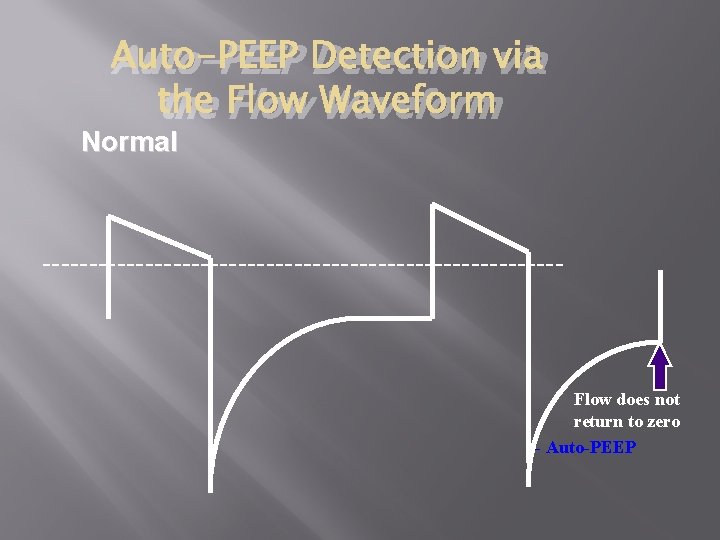
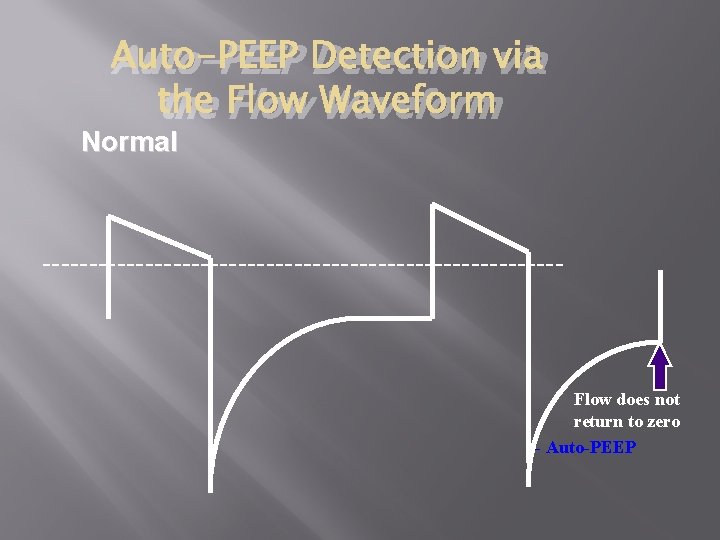
Auto-PEEP Detection via the Flow Waveform Normal ---------------------------- Flow does not return to zero - Auto-PEEP
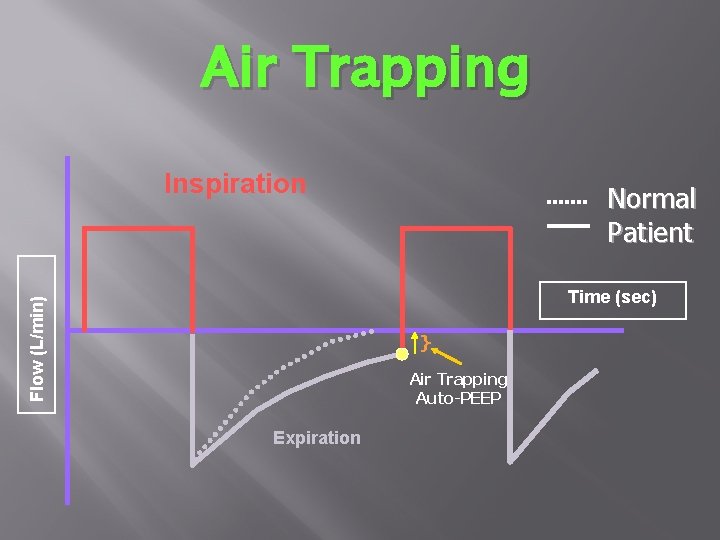
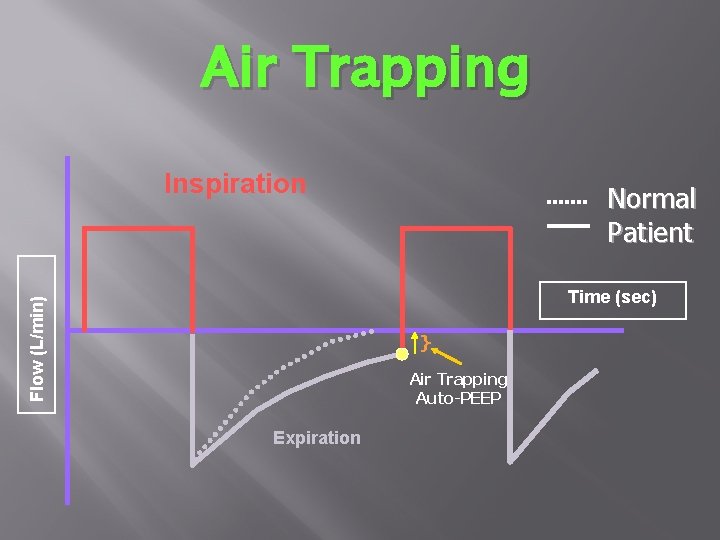
Air Trapping Inspiration Normal Patient Flow (L/min) Time (sec) } Air Trapping Auto-PEEP Expiration
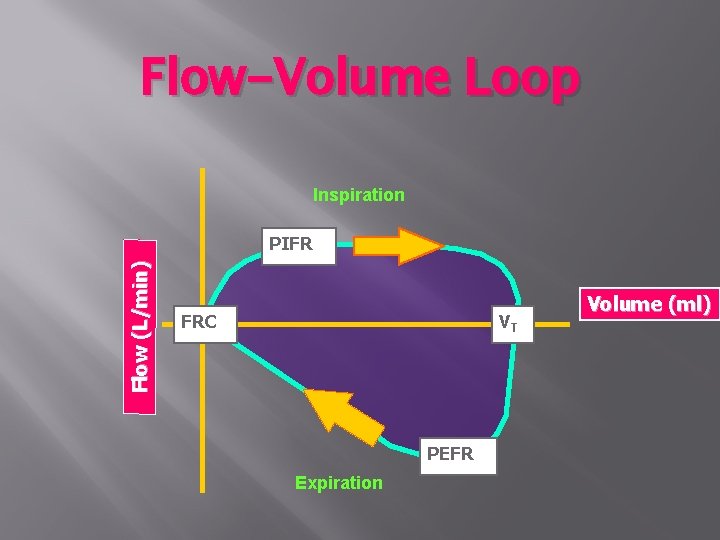
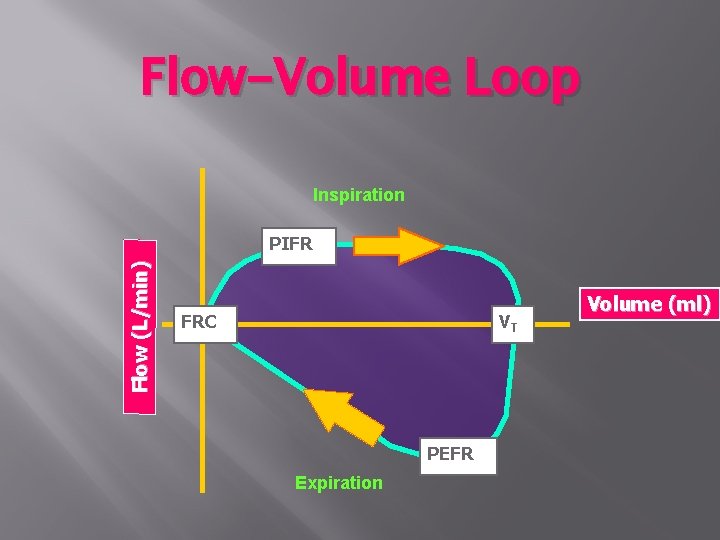
Flow-Volume Loop Inspiration Flow (L/min) PIFR FRC VT PEFR Expiration Volume (ml)
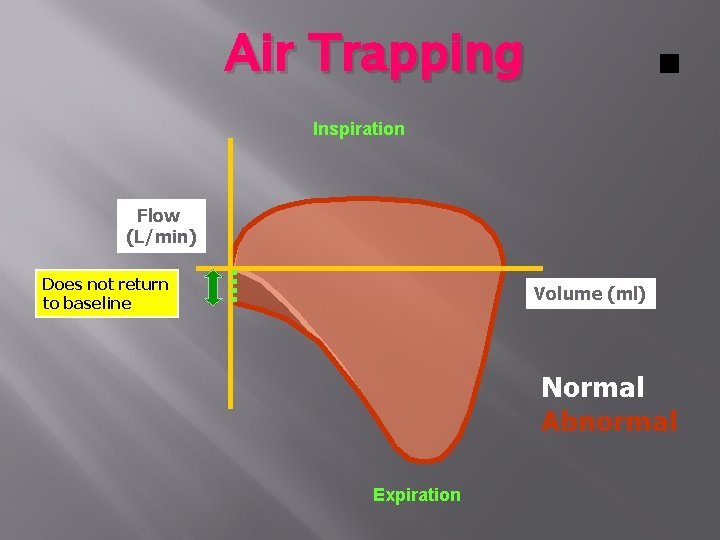
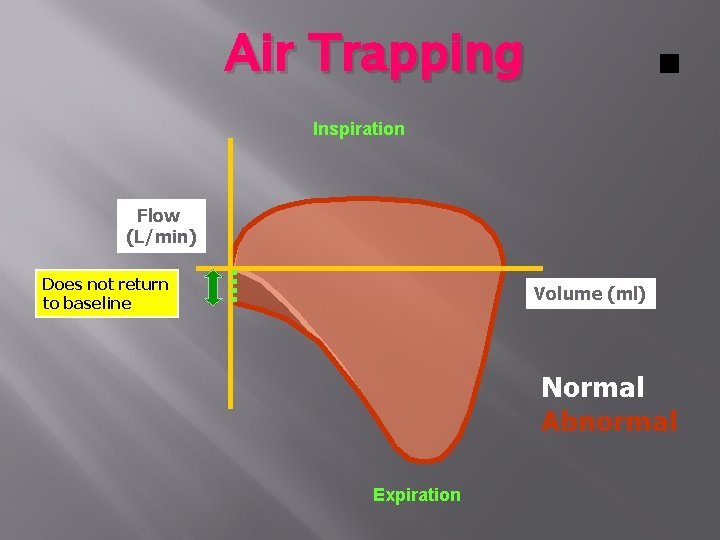
Air Trapping Inspiration Flow (L/min) Does not return to baseline Volume (ml) Normal Abnormal Expiration
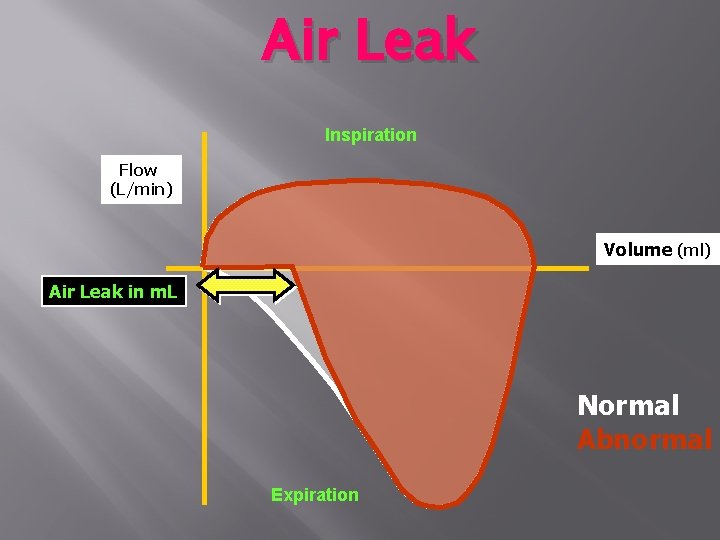
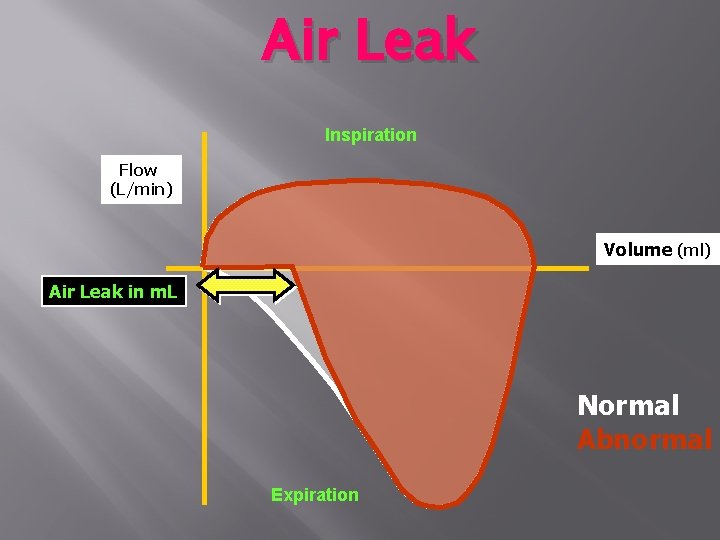
Air Leak Inspiration Flow (L/min) Volume (ml) Air Leak in m. L Normal Abnormal Expiration
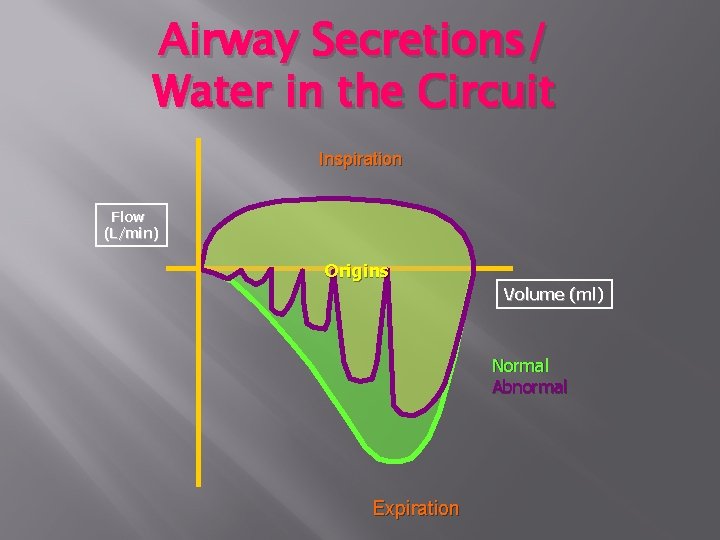
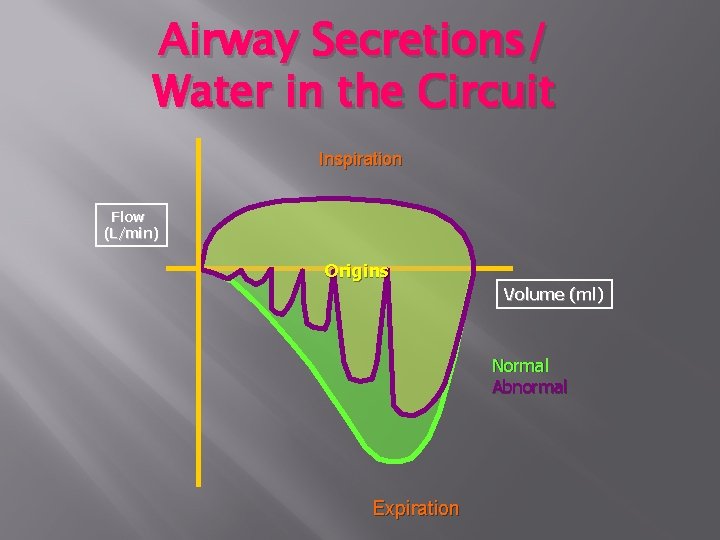
Airway Secretions/ Water in the Circuit Inspiration Flow (L/min) Origins Volume (ml) Normal Abnormal Expiration