ICU Curriculum Acute Respiratory Distress Syndrome Clinical Case



![Ventilator strategies Increasing inspiratory time Airway pressure release ventilation [APRV] Prone Ventilation Ventilator strategies Increasing inspiratory time Airway pressure release ventilation [APRV] Prone Ventilation](https://slidetodoc.com/presentation_image_h2/01255458a970868bc145ebe0c1ceba32/image-24.jpg)


- Slides: 31
ICU Curriculum Acute Respiratory Distress Syndrome
Clinical Case 35 year old lady with history of diabetes who was admitted to an outside hospital with 1 week of cough and shortness of breath. She was intubated there and transferred here for further management of her hypoxemic respiratory failure. BP: 130 s/80 s HR: 120 RR: 28 Temp: 100 Sp 02: 80% on 100% Fi 02 VC| RR 20 | Tidal volume 500 | PEEP: 15 | Fi 02: 100%
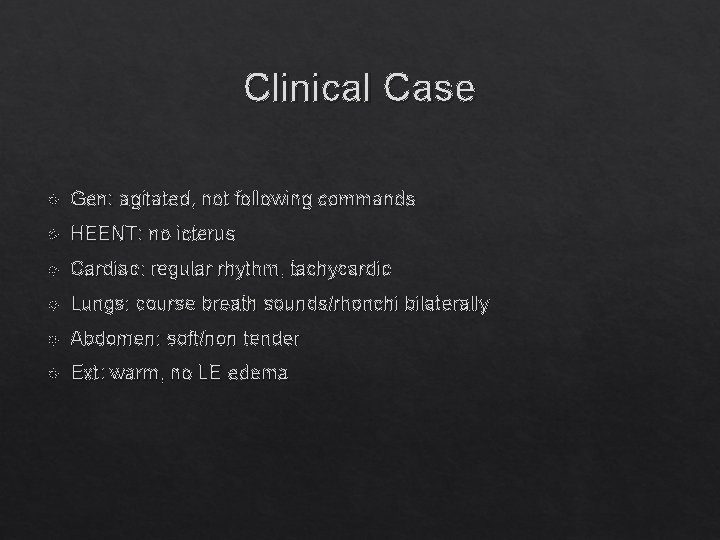
Clinical Case Gen: agitated, not following commands HEENT: no icterus Cardiac: regular rhythm, tachycardic Lungs: course breath sounds/rhonchi bilaterally Abdomen: soft/non tender Ext: warm, no LE edema
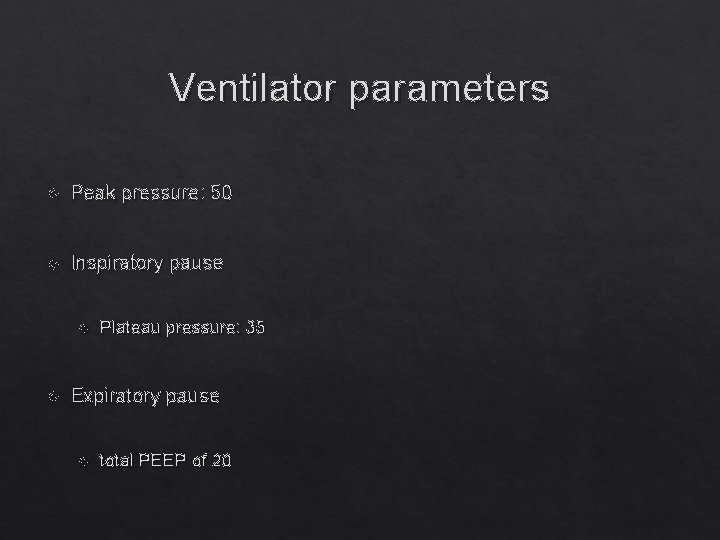
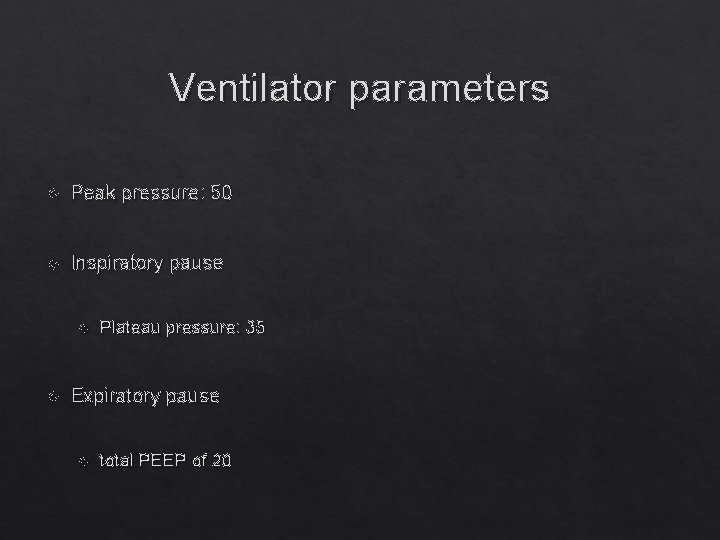
Ventilator parameters Peak pressure: 50 Inspiratory pause Plateau pressure: 35 Expiratory pause total PEEP of 20
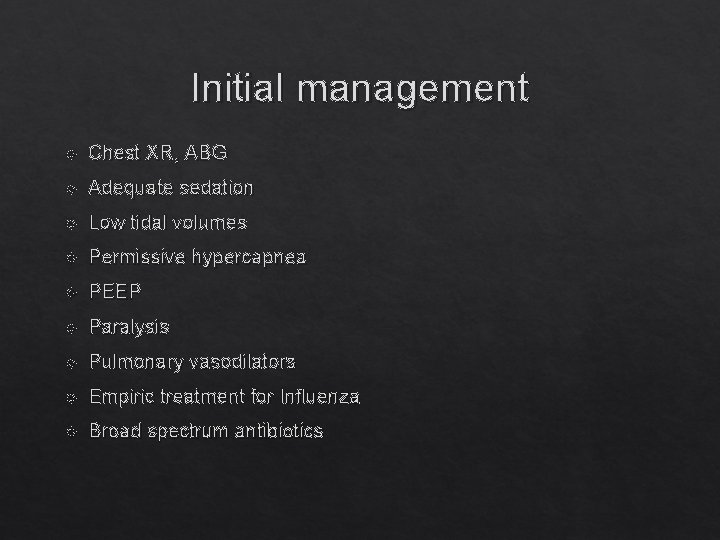
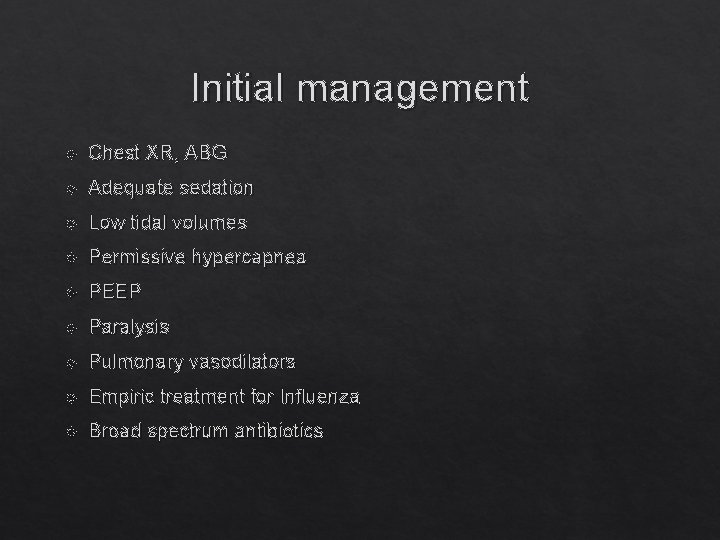
Initial management Chest XR, ABG Adequate sedation Low tidal volumes Permissive hypercapnea PEEP Paralysis Pulmonary vasodilators Empiric treatment for Influenza Broad spectrum antibiotics
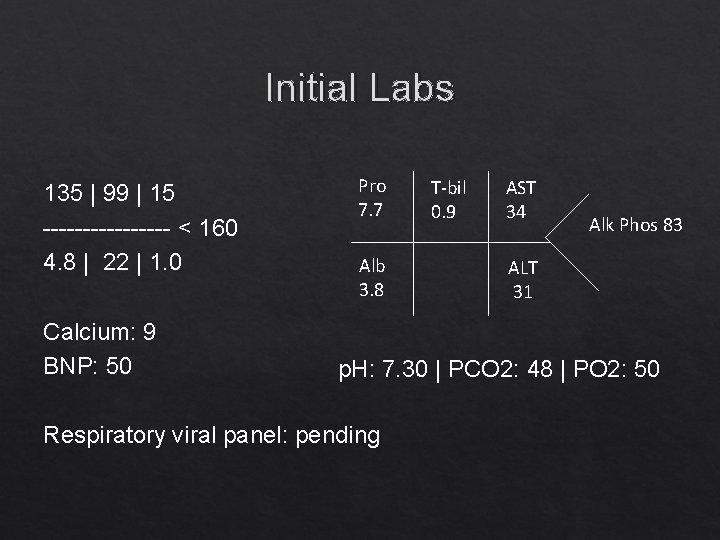
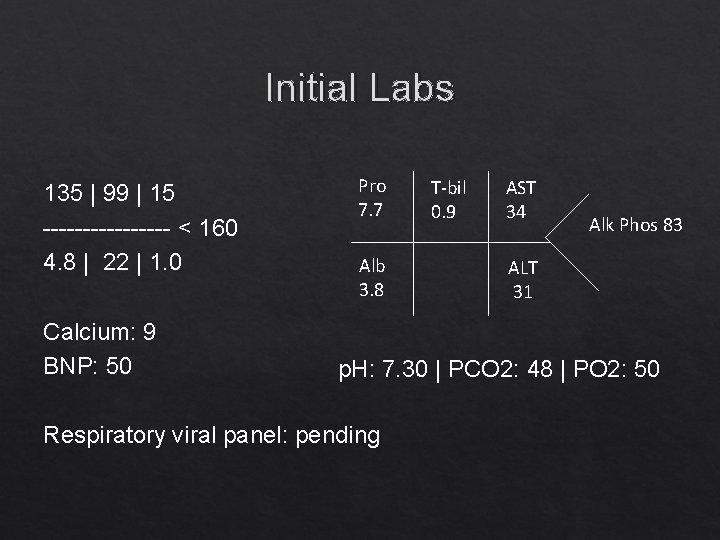
Initial Labs 135 | 99 | 15 -------- < 160 4. 8 | 22 | 1. 0 Calcium: 9 BNP: 50 Pro 7. 7 Alb 3. 8 T-bil 0. 9 AST 34 Alk Phos 83 ALT 31 p. H: 7. 30 | PCO 2: 48 | PO 2: 50 Respiratory viral panel: pending

Differential Diagnosis Noncardiogenic pulmonary edema/ARDS Infection Left heart failure Diffuse alveolar hemorrhage Acute eosinophilic pneumonia Acute interstitial pneumonia Pulmonary alveolar proteinosis Organizing pneumonia Hypersensitivity pneumonitis Leukemic infiltration Drug toxicity Aspiration TRALI Fat embolism
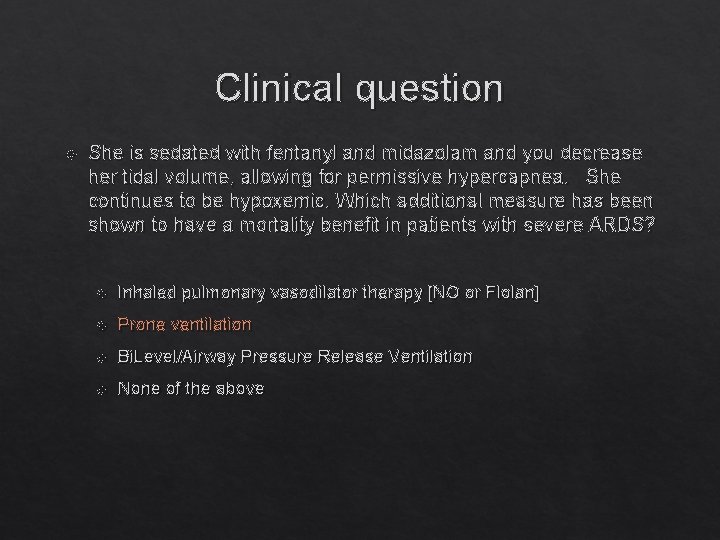
Clinical question She is sedated with fentanyl and midazolam and you decrease her tidal volume, allowing for permissive hypercapnea. She continues to be hypoxemic. Which additional measure has been shown to have a mortality benefit in patients with severe ARDS? Inhaled pulmonary vasodilator therapy [NO or Flolan] Prone ventilation Bi. Level/Airway Pressure Release Ventilation None of the above
ARDS Definition Acute onset Bilateral infiltrates consistent with pulmonary edema Exclude cardiogenic pulmonary edema
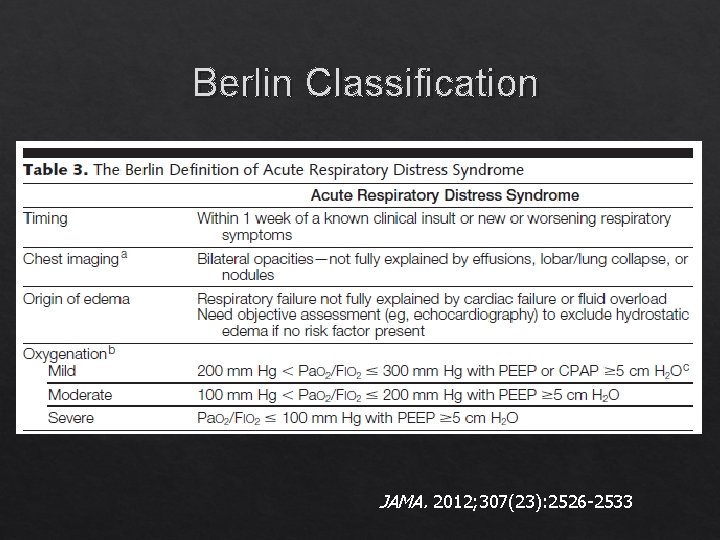
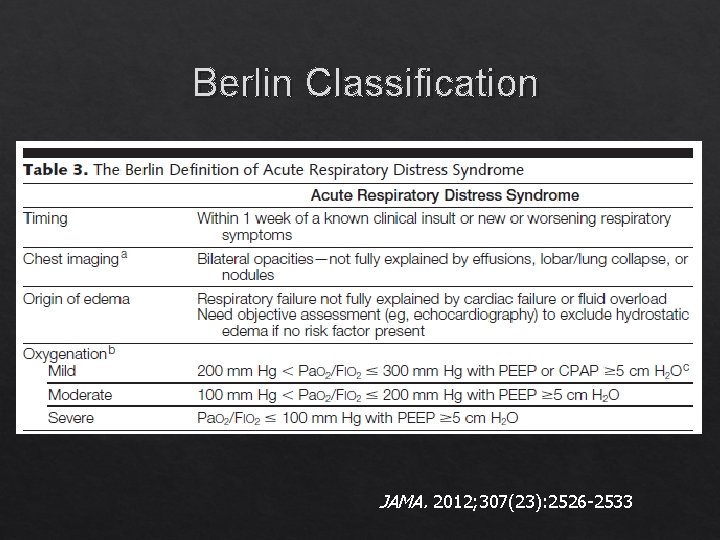
Berlin Classification JAMA. 2012; 307(23): 2526 -2533
Precipitating Causes ARDS is a final common pathway to a wide range of precipitants. Can divide precipitating causes into 2 groups: Direct (pulmonary) Indirect (extrapulmonary)
Pulmonary Causes Bacterial pneumonia Viral pneumonia Aspiration of gastric contents Trauma with lung contusion Near drowning Pneumocystis pneumonia Smoke inhalation Crack lung
Indirect (Extrapulmonary) Causes Acute pancreatitis TRALI Post cardiopulmonary bypass Severe sepsis Toxic ingestions Trauma with fractures and fat embolism
Pathogenesis and Pathology Early exudative phase Interstitial and alveolar edema capillary congestion intra-alveolar hemorrhage May be an inflammatory cell infiltrate Over the ensuing days, hyaline membranes form. Diffuse alveolar damage with necrosis of type 1 alveolar epithelial cells
Pathogenesis and Pathology Late proliferative phase Disordered lung healing As early as 7 -10 days after lung injury May result in extensive fibrosis Type 2 alveolar cells proliferate, fibroblasts become more numerous Clinical findings: large dead space fraction high minute ventilation pulmonary hypertension Reduced lung compliance Less responsive to PEEP


PEEP in ARDS Helps decrease requirements for high Fi. O 2 by alveolar recruitment Ideal level of PEEP is based on the individual patient. Beneficial effects: recruitment, improved oxygenation Detrimental effects: over distention, barotrauma, decreased venous return with decrease cardiac output.
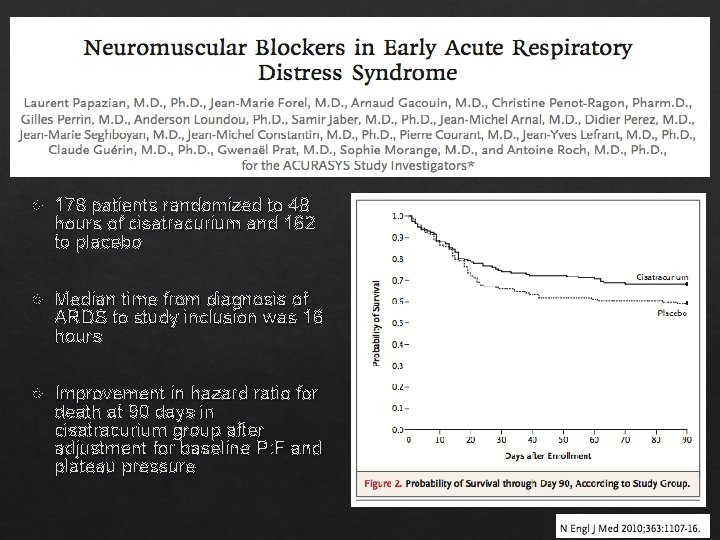
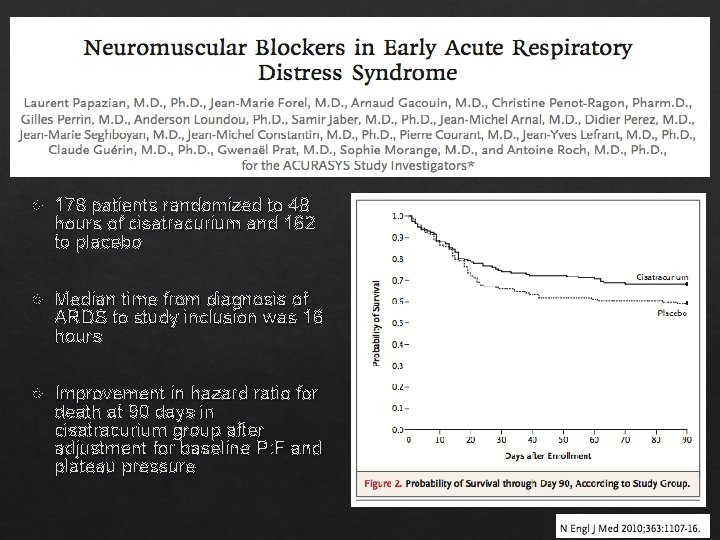
178 patients randomized to 48 hours of cisatracurium and 162 to placebo Median time from diagnosis of ARDS to study inclusion was 16 hours Improvement in hazard ratio for death at 90 days in cisatracurium group after adjustment for baseline P: F and plateau pressure
Inhaled vasodilators Should not be abruptly stopped, wean by 50% Nitric oxide Usual dose is 20 parts per million [ppm] Epoprostenol [Flolan] Starting dose is 20, 000 ng/m. L
Inhaled vasodilators Induces selective vasodilatation in ventilated lung areas and redistributes blood flow Reduces pulmonary hypertension Improves oxygenation in the first 24 hours No randomized trials that show a mortality benefit
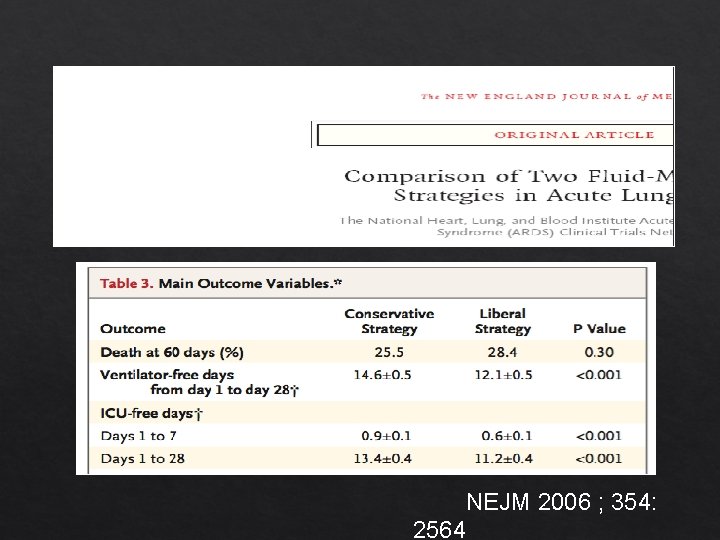
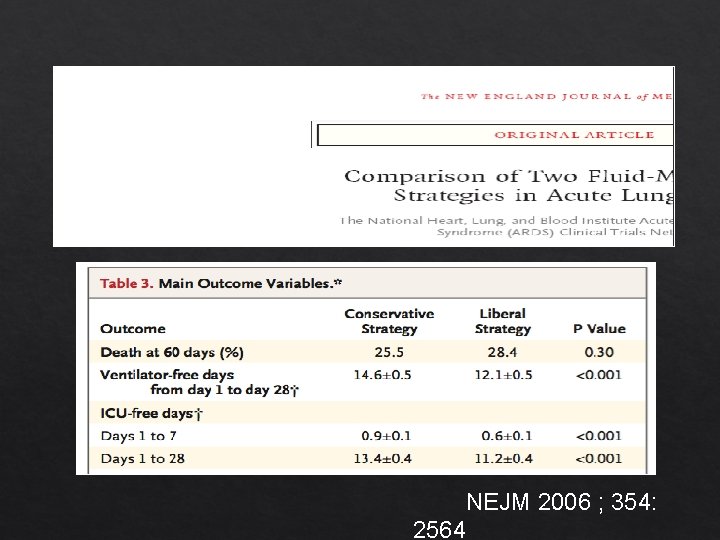
NEJM 2006 ; 354: 2564
![Ventilator strategies Increasing inspiratory time Airway pressure release ventilation APRV Prone Ventilation Ventilator strategies Increasing inspiratory time Airway pressure release ventilation [APRV] Prone Ventilation](https://slidetodoc.com/presentation_image_h2/01255458a970868bc145ebe0c1ceba32/image-24.jpg)
Ventilator strategies Increasing inspiratory time Airway pressure release ventilation [APRV] Prone Ventilation

Prone Ventilation • Decreases shunt perfusion • Improves V/Q matching • Improves oxygenation • Difficult to care for catheters and ETT • Concern for development of pressure ulcers and facial edema • Need for increased sedation
ECMO Indications for consideration of VV-ECMO in acute respiratory failure: Potentially reversible, single organ (lung) disease (AKI not a contraindication) PF <50 for >3 hours despite ventilator optimization and use of adjunctive measures OR PF <80 for >6 hours despite attempted optimization OR p. H <7. 20 with predominantly respiratory component despite attempted optimization OR Plateau pressure persistently >30 despite attempted optimization (Relative) Contra-indications: Poor pre-ECMO functional status Length of mechanical ventilation >7 days Acute intracranial hemorrhage Advanced multi-organ failure Early referral is key. ECMO team should be involved early to enhance collaborative decision making about propriety of initiating extracorporeal therapy.
Summary Treat underlying etiology Adequate sedation Negative fluid balance Paralysis Inhaled pulmonary vasodilators No randomized trials that show mortality benefit Alternative ventilator strategies Prone ventilation
Clinical question She is sedated with fentanyl and midazolam and you decrease her tidal volume, allowing for permissive hypercapnea. She continues to be hypoxemic. Which additional measure has been shown to have a mortality benefit in patients with severe ARDS? Inhaled pulmonary vasodilator therapy [NO or Flolan] Prone ventilation Bi. Level/Airway Pressure Release Ventilation None of the above
Clinical question She is sedated with fentanyl and midazolam and you decrease her tidal volume, allowing for permissive hypercapnea. She continues to be hypoxemic. Which additional measure has been shown to have a mortality benefit in patients with severe ARDS? Inhaled pulmonary vasodilator therapy [NO or Flolan] Prone ventilation Bi. Level/Airway Pressure Release Ventilation None of the above

 Respiratory distress
Respiratory distress Respiratory distress
Respiratory distress Respiratory distress nasal flaring
Respiratory distress nasal flaring Icu case presentation
Icu case presentation Icu case presentation
Icu case presentation Icu case presentation
Icu case presentation Broncheols
Broncheols Cholecystitis pathogenesis
Cholecystitis pathogenesis Periodontitis apicalis acuta
Periodontitis apicalis acuta Conducting zone and respiratory zone
Conducting zone and respiratory zone Acute coronary syndrome
Acute coronary syndrome Acute radiation syndrome
Acute radiation syndrome Firas mussa md
Firas mussa md Best case worst case average case
Best case worst case average case Severe acute malnutrition case presentation
Severe acute malnutrition case presentation Unfolding clinical reasoning case study
Unfolding clinical reasoning case study Kebutuhan tenaga perawat menurut depkes
Kebutuhan tenaga perawat menurut depkes Sas escala
Sas escala Icu localization
Icu localization Icu tersier adalah
Icu tersier adalah Icu university zambia
Icu university zambia 5hs and 5ts
5hs and 5ts Pressors icu
Pressors icu Nivel de conciencia escala
Nivel de conciencia escala Language
Language Cam icu escala
Cam icu escala Cheetah nicom interpretation
Cheetah nicom interpretation Cam icu
Cam icu Concept of intensive care unit
Concept of intensive care unit Icu orientation
Icu orientation Icu for dummies
Icu for dummies Information and communications university
Information and communications university