ARDS Acute Respiratory Distress Syndrome Criteria ACUTE onset




- Slides: 22
ARDS

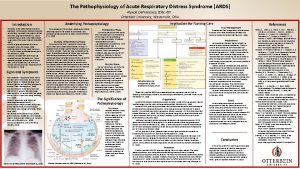
Acute Respiratory Distress Syndrome �Criteria: �ACUTE onset of bilateral infiltrates on chest x ray � Within a week of insult � Noncardiogenic pulmonary edema �Low ratio of Pa. O 2: Fi. O 2 � Partial pressure of arterial oxygen to fraction of inspired oxygen � Pa. O 2 = 80 -100 mm. Hg � Fi. O 2 = 0. 21
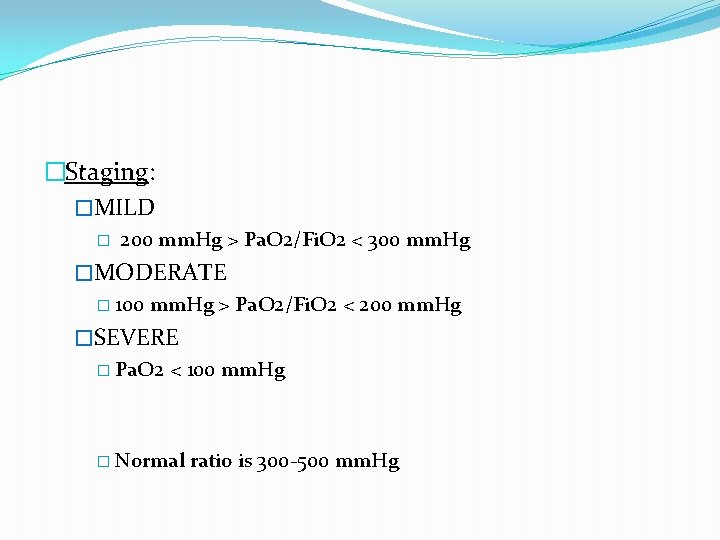
�Staging: �MILD � 200 mm. Hg > Pa. O 2/Fi. O 2 < 300 mm. Hg �MODERATE � 100 mm. Hg > Pa. O 2/Fi. O 2 < 200 mm. Hg �SEVERE � Pa. O 2 < 100 mm. Hg � Normal ratio is 300 -500 mm. Hg
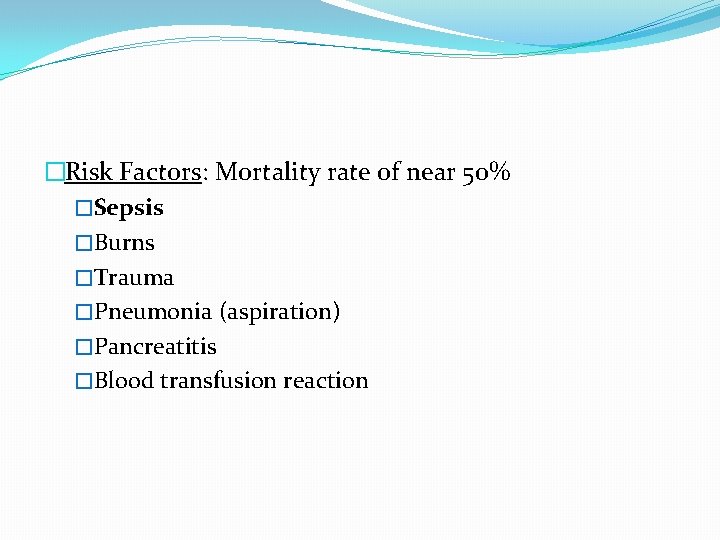
�Risk Factors: Mortality rate of near 50% �Sepsis �Burns �Trauma �Pneumonia (aspiration) �Pancreatitis �Blood transfusion reaction
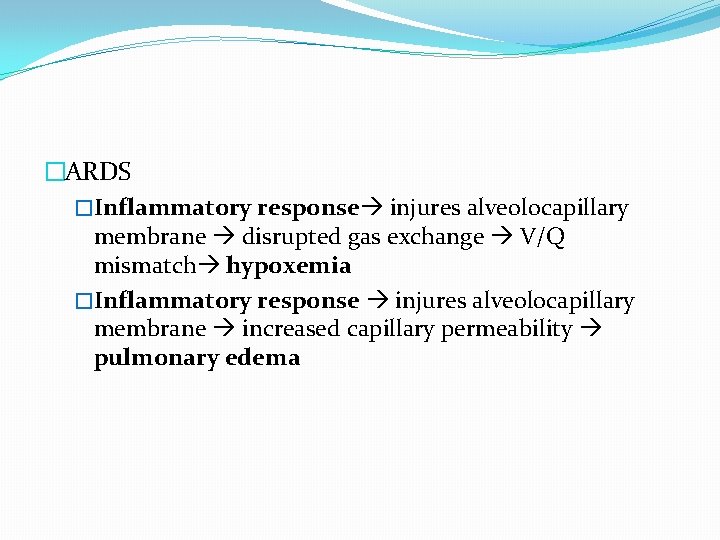
�ARDS �Inflammatory response injures alveolocapillary membrane disrupted gas exchange V/Q mismatch hypoxemia �Inflammatory response injures alveolocapillary membrane increased capillary permeability pulmonary edema
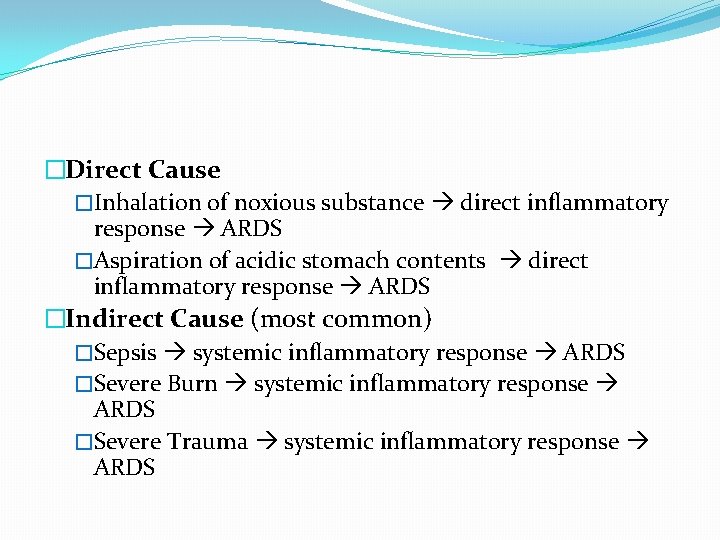
�Direct Cause �Inhalation of noxious substance direct inflammatory response ARDS �Aspiration of acidic stomach contents direct inflammatory response ARDS �Indirect Cause (most common) �Sepsis systemic inflammatory response ARDS �Severe Burn systemic inflammatory response ARDS �Severe Trauma systemic inflammatory response ARDS

Diagnostics 1) Chest Radiograph: acute bilateral infiltrates 2) ABGs 3) Measurement of TNF, IL-8, CBC 3) BNP: <100 pg/m. L (general guideline, not always accurate) -exclusion diagnostic 4) Echocardiogram -exclusion diagnostic 5) Lung Testing -exclusion diagnostic 6) Clinical Symptoms
�Phases: �Exudative (Inflammatory) � 6 -12 hours after insult (range of up to 72 hours) � Neutrophil activation � Release of inflammatory mediators (proteolytic enzymes, free radicals, platelet aggregates) � Pulmonary edema; Pulmonary hemorrhage � Decreased surfactant production � Alveolar collapse � Hypercapnia; Hypoxemia onset
�Proliferative � Commonly within 3 days. (range of 3 -21 days) � Pulmonary edema resolved � Exudate accumulates hyaline membrane � Rapid cellular proliferation � Hypoxemia worsens �Fibrotic � Can occur concurrently with proliferative phase or be delayed to 2 -3 weeks after initial insult � Commonly within 7 days. � Remodeling and Fibrosis occur � Decreased lung compliance � Extreme V/Q mismatch � Respiratory Failure MODS
�Clinical Manifestations: � Early signs � Dyspnea, inspiratory crackles, chest infiltrates on x ray seen within 24 -48 hours �Dyspnea ; hypoxemia onset; poor response to O 2 supplementation �Hyperventilation respiratory alkalosis �Decreased tissue perfusion; metabolic acidosis �Decreased tidal volume labored respirations hypoventilation �Respiratory acidosis; worsening hypoxemia �Hypotension, shock, respiratory failure, MODS, death
�Treatment: �Mechanical ventilation with PEEP �Supplemental supportive therapies � Vasopressors, fluid resuscitation if appropriate �Possible use of low dose corticosteroids during initial inflammatory phase. Not during later phases. �Treatment of underlying cause � Antibiotics to treat known infection or prophylactically
Gas Transport �Delivery of oxygen � 1) ventilation of oxygen to the lungs � 2) diffusion of oxygen from alveoli to the capillaries � 3) perfusion by arterial blood � 4) diffusion of oxygenated blood from capillaries to cells �Delivery of carbon dioxide � 1) diffusion of carbon dioxide from cells to capillaries � 2) perfusion by venous blood � 3) diffusion of carbon dioxide to alveoli � 4) removal of carbon dioxide during expiration
Oxygen Transport �Alveolocapillary membrane �Ideal medium for oxygen transport �Pressure of oxygen within in alveoli is greater than the pressure within the capillary blood allows for rapid oxygen transport �Oxygen dissolves within the plasma and exerts a pressure (measured as Pa. O 2) �Oxygen moves from the plasma to RBCs and binds with Hgb until Hgb is saturated �Diffusion continues until equilibrium is reached � PAO 2 = Pa. O 2
Alveolar Gas Equation �PAO 2 = Fi. O 2 (Patm-PH 2 O) – Pa. CO 2/R � 0. 21 (760 mm. Hg – 47 mm. Hg) – 40/0. 8 �Sa. O 2 = proportion/percentage of hemoglobin saturated with oxygen 92 -100% �Pa. O 2 = amount of oxygen within the plasma (measured as a pressure/tension) 80 -100 mm. Hg �Pa. CO 2 = amount of carbon dioxide within the plasma (measured as a pressure/tension) 35 -45 mm. Hg

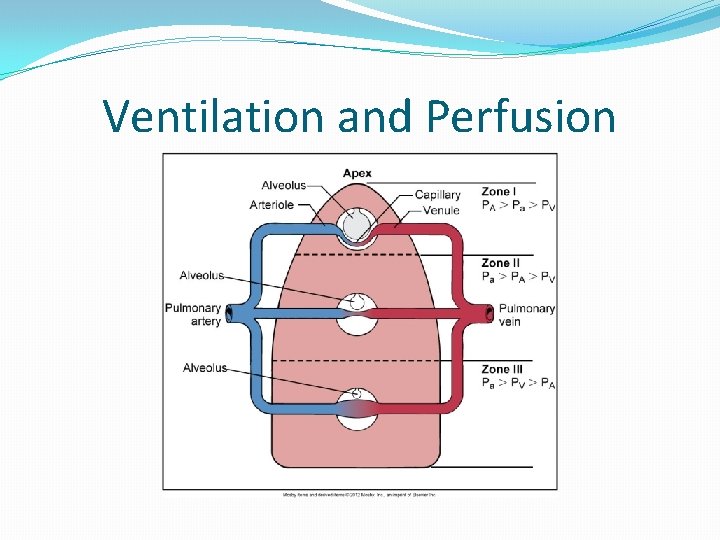
Ventilation and Perfusion �V = Ventilation Q = Perfusion �Dependent on body position �Ventilation exceeds perfusion in the apex �Perfusion exceeds ventilation in the base �More variation between the apex and the base occurs related to perfusion �V/Q ratio is higher in the apex � 0. 8/1 = 0. 8
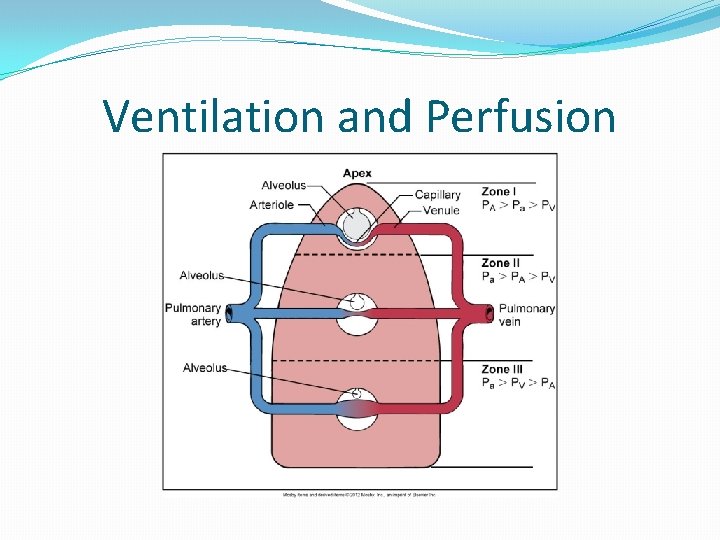
Ventilation and Perfusion
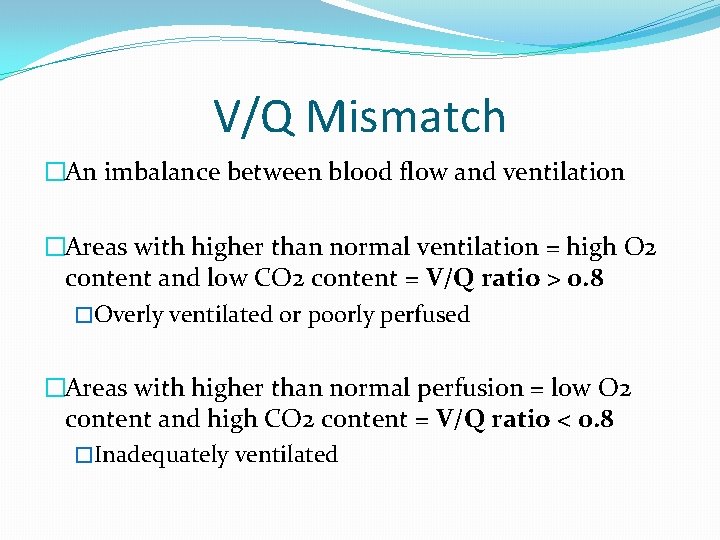
V/Q Mismatch �An imbalance between blood flow and ventilation �Areas with higher than normal ventilation = high O 2 content and low CO 2 content = V/Q ratio > 0. 8 �Overly ventilated or poorly perfused �Areas with higher than normal perfusion = low O 2 content and high CO 2 content = V/Q ratio < 0. 8 �Inadequately ventilated
�(V) Ventilation �Alveoli filled with air are ventilated. Alveoli that are collapsed or filled with anything besides air are not ventilated. Ventilated alveoli undergo gas exchange; nonventilated do not. �(Q) Perfusion �Alveoli are surrounded by a membrane of capillaries. These capillaries descend from the pulmonary arteries. Capillaries with adequate blood in them are perfused. Perfused capillaries are capable of gas exchange; non-perfused do not.

 Respiratory distress nasal flaring
Respiratory distress nasal flaring Respiratory distress
Respiratory distress Respiratory distress
Respiratory distress Ards management
Ards management Ards leczenie
Ards leczenie Jama 2017
Jama 2017 Ards
Ards Kryteria berlińskie ards
Kryteria berlińskie ards Prof dr cem yıldırım
Prof dr cem yıldırım Static compliance calculation
Static compliance calculation What is peep in ventilator
What is peep in ventilator Ards permissive hypercapnia
Ards permissive hypercapnia Ards definition
Ards definition Ards
Ards Respiratory zone vs conducting zone
Respiratory zone vs conducting zone Acute upper respiratory infection unspecified คือ
Acute upper respiratory infection unspecified คือ Acute liver failure criteria
Acute liver failure criteria Ranson criteria for acute pancreatitis
Ranson criteria for acute pancreatitis Acute liver failure criteria
Acute liver failure criteria Pancreatitis score
Pancreatitis score Hepatic coma stages
Hepatic coma stages Acute pancreatitis diagnosis criteria
Acute pancreatitis diagnosis criteria Ransons criteria
Ransons criteria