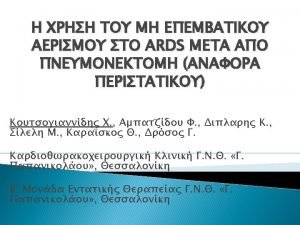
NonECMO rescue therapies for ARDS Division of Pulmonary



- Slides: 50
Non-ECMO rescue therapies for ARDS Division of Pulmonary, Allergy and Critical care medicine Department of Internal medicine Pusan National University Yangsan Hospital Hye Ju Yeo
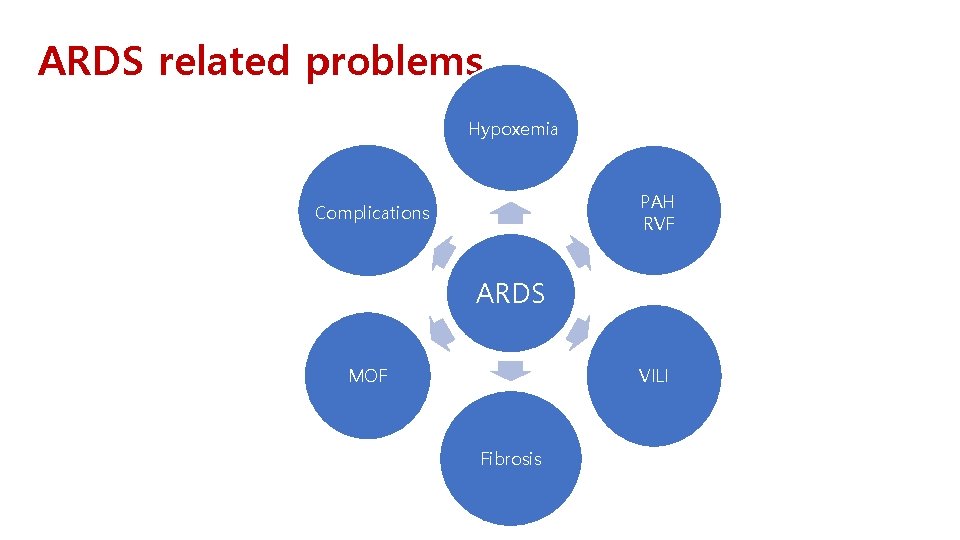
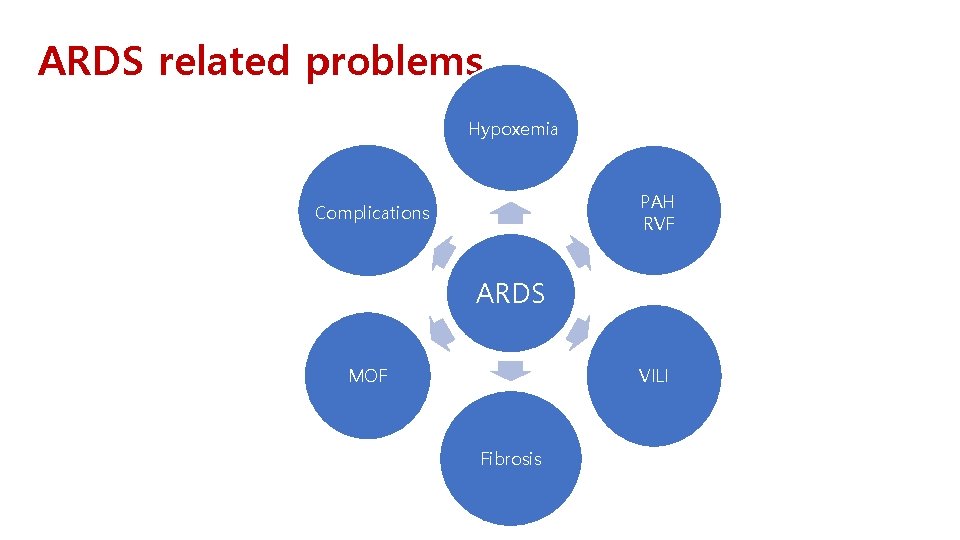
ARDS related problems Hypoxemia PAH RVF Complications ARDS VILI MOF Fibrosis
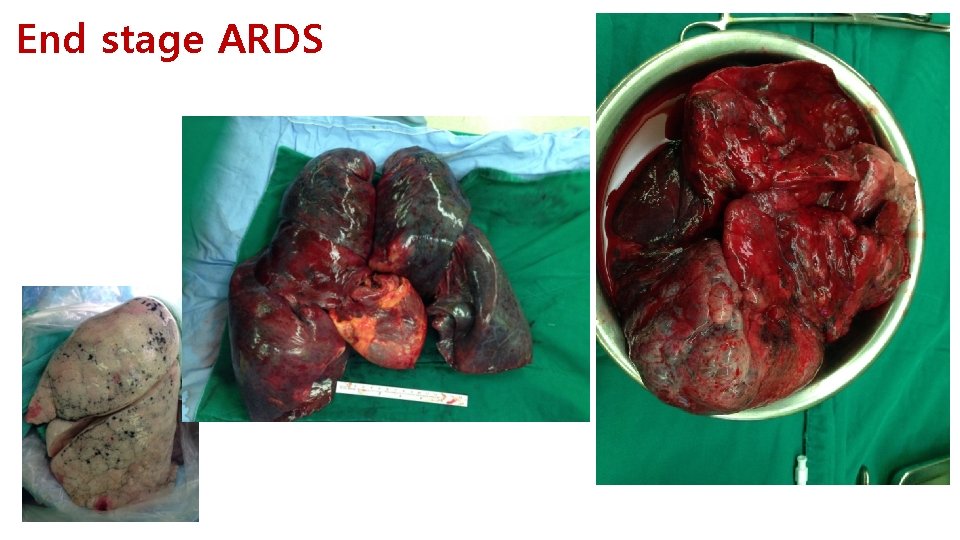
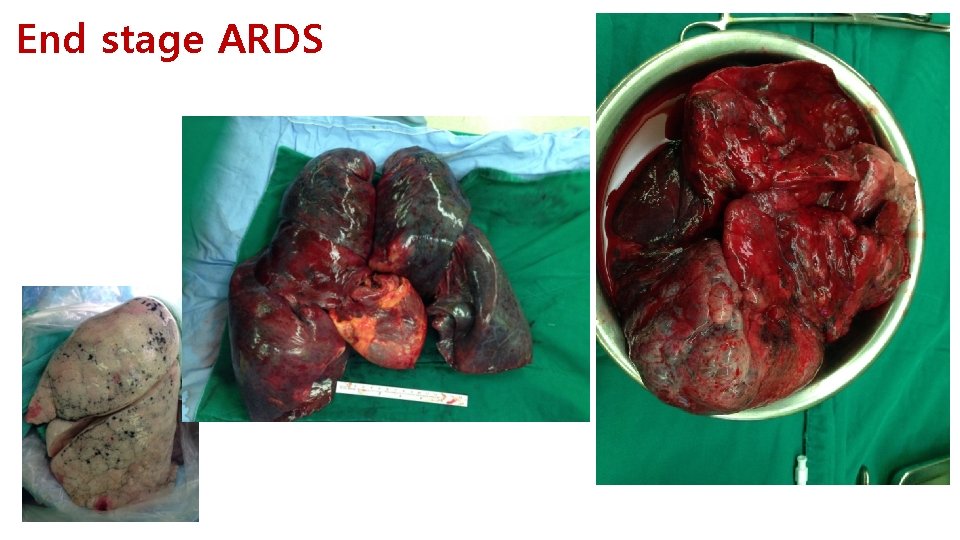
End stage ARDS
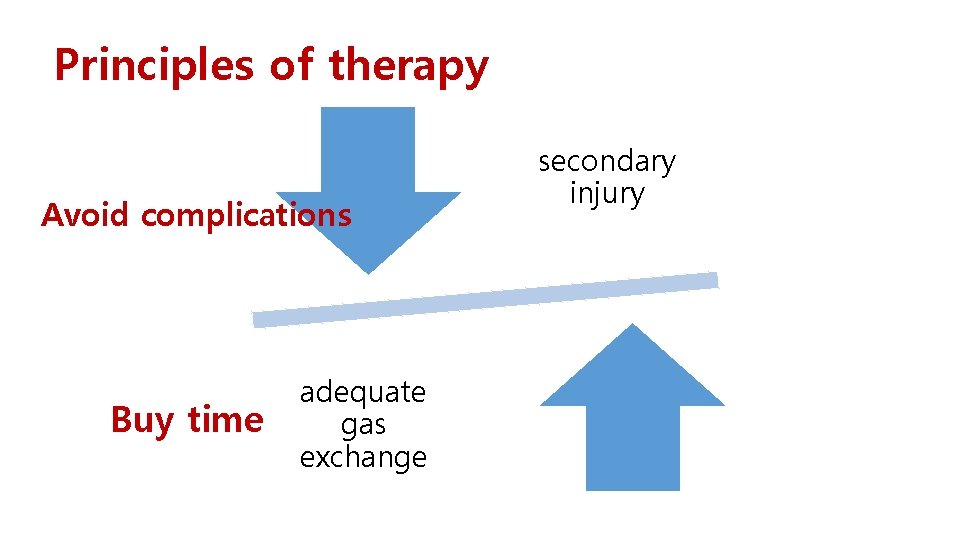
Principles of therapy Avoid complications Buy time adequate gas exchange secondary injury
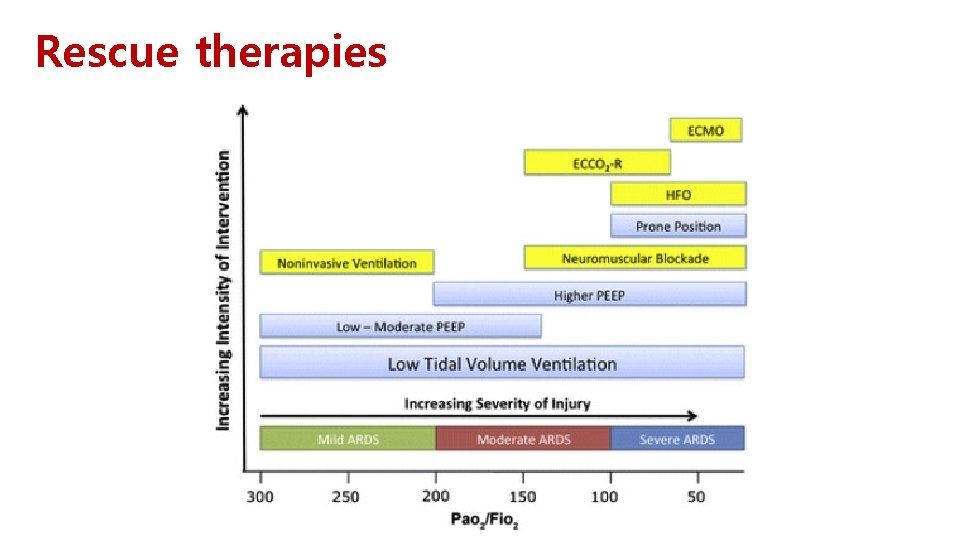
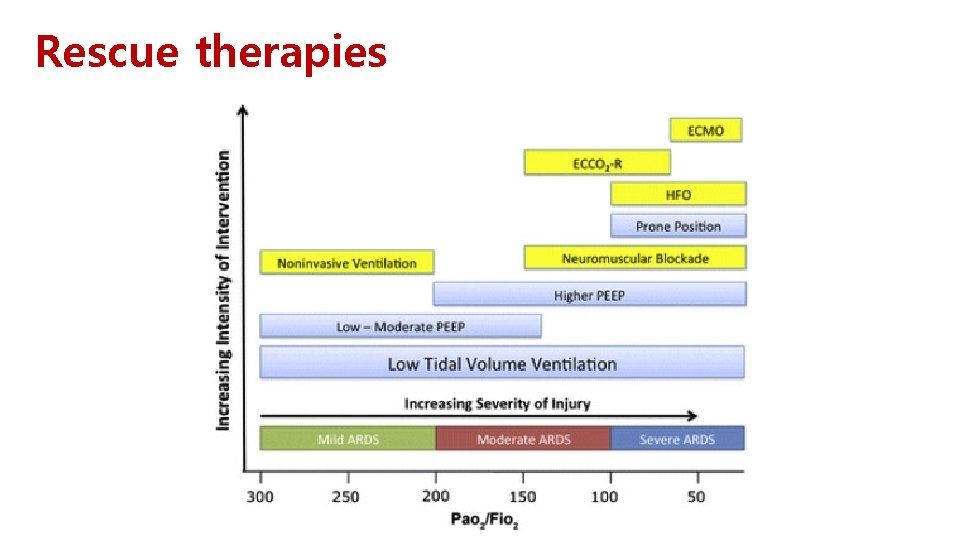
Rescue therapies
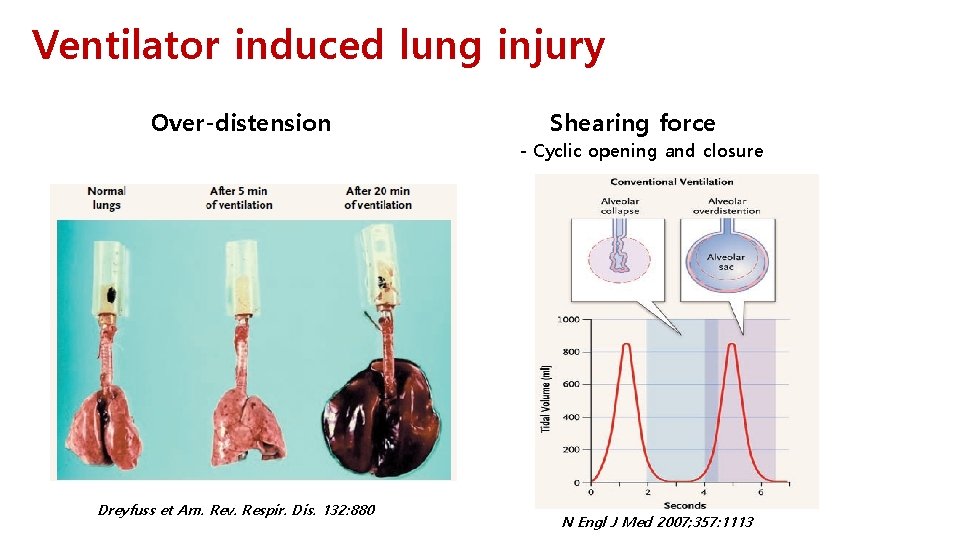
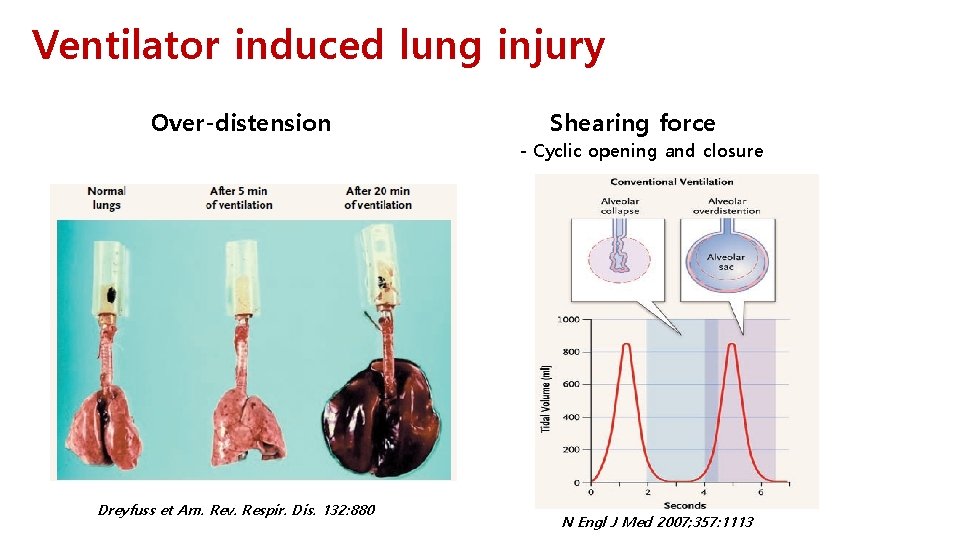
Ventilator induced lung injury Over-distension Shearing force - Cyclic opening and closure Dreyfuss et Am. Rev. Respir. Dis. 132: 880 N Engl J Med 2007; 357: 1113
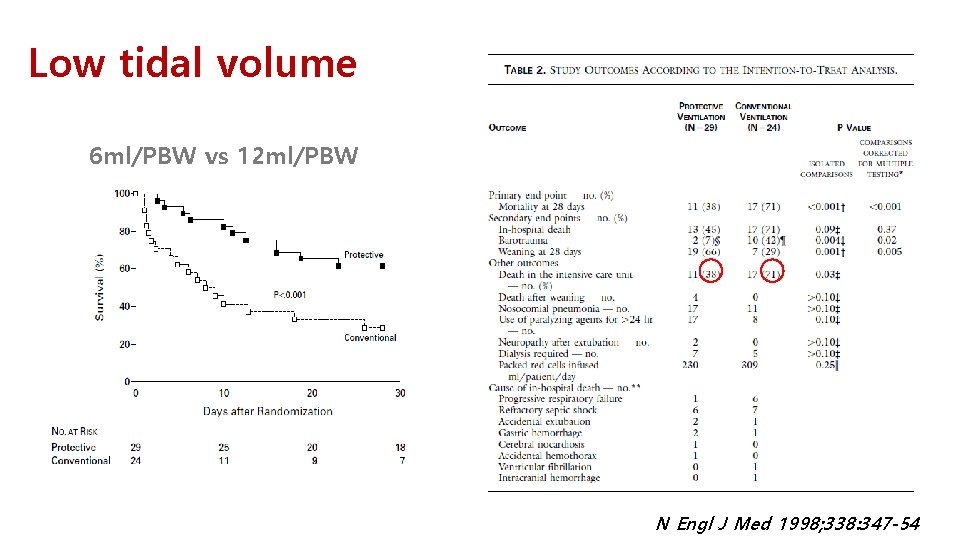
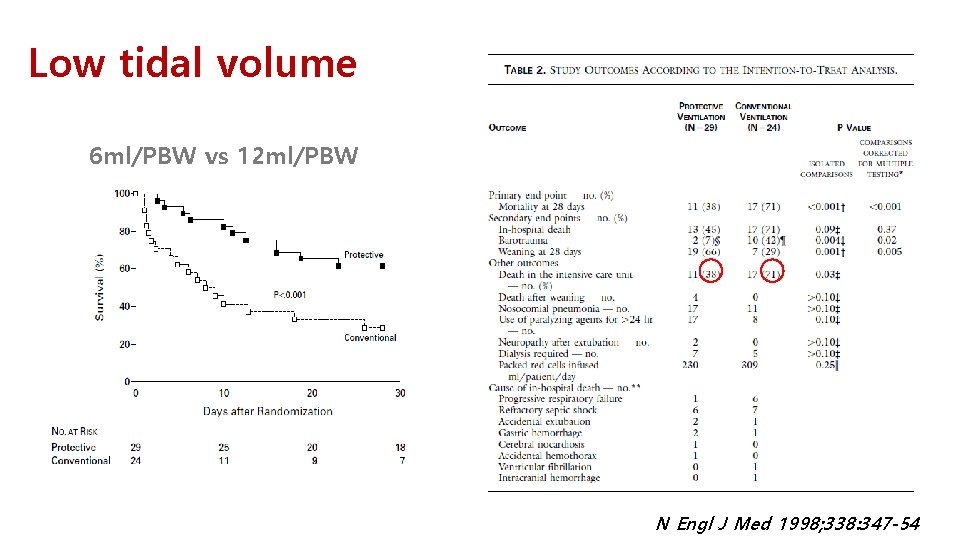
Low tidal volume 6 ml/PBW vs 12 ml/PBW N Engl J Med 1998; 338: 347 -54
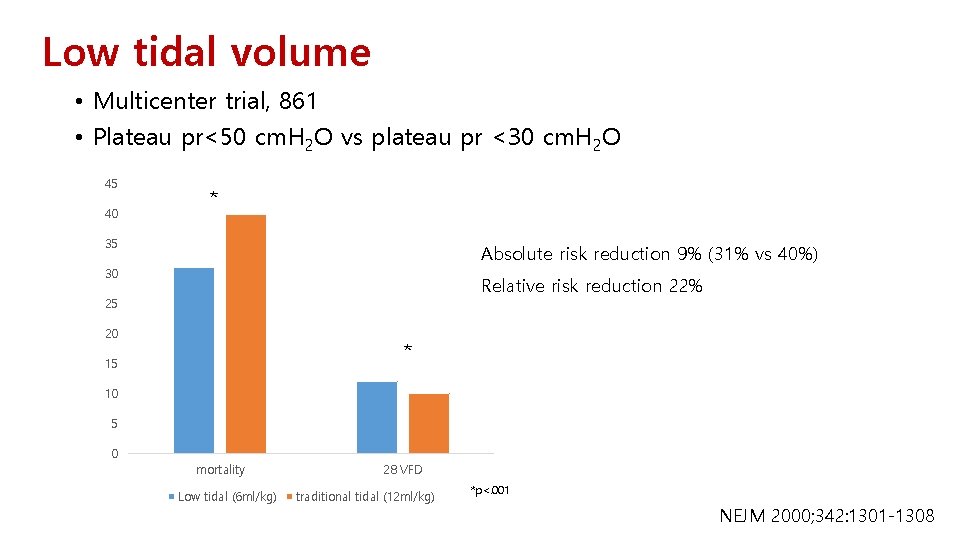
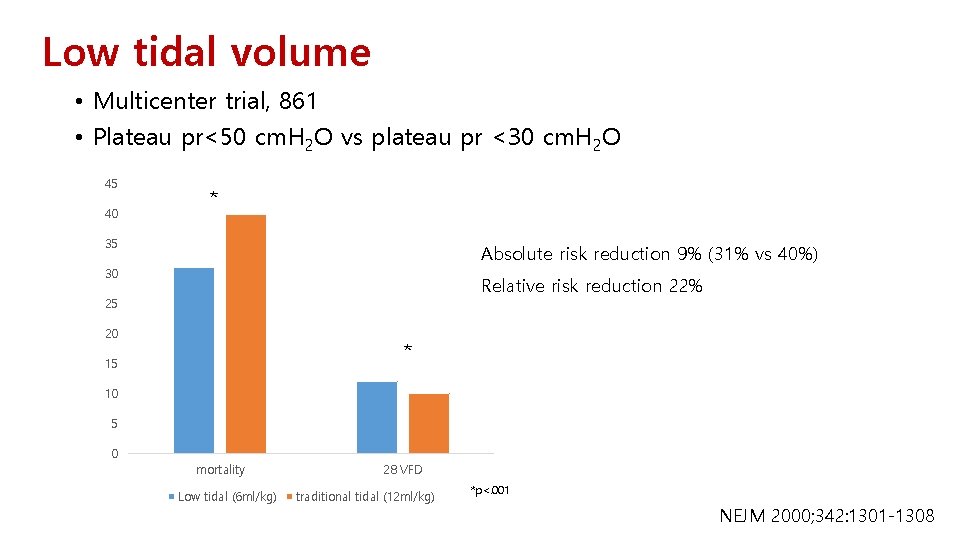
Low tidal volume • Multicenter trial, 861 • Plateau pr<50 cm. H 2 O vs plateau pr <30 cm. H 2 O 45 40 * 35 Absolute risk reduction 9% (31% vs 40%) 30 Relative risk reduction 22% 25 20 * 15 10 5 0 mortality Low tidal (6 ml/kg) 28 VFD traditional tidal (12 ml/kg) *p<. 001 NEJM 2000; 342: 1301 -1308
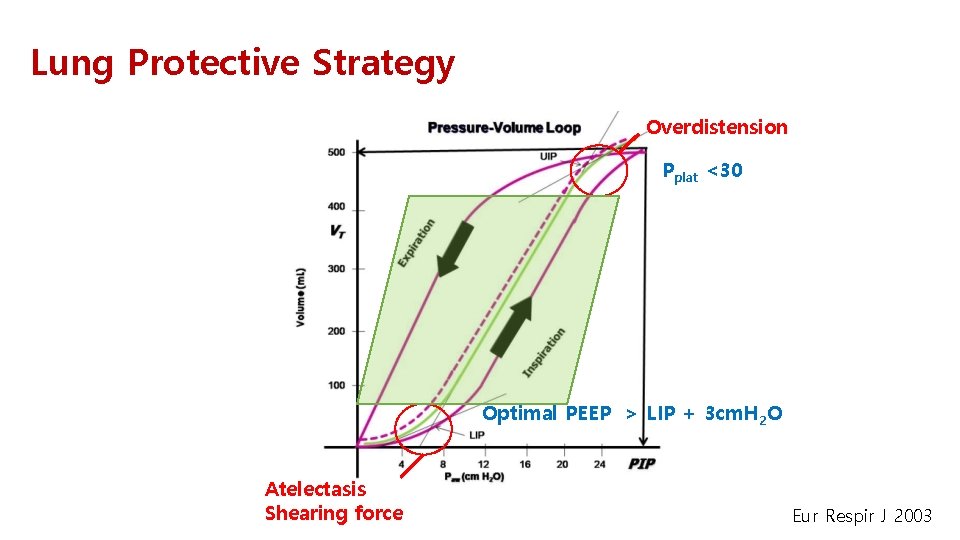
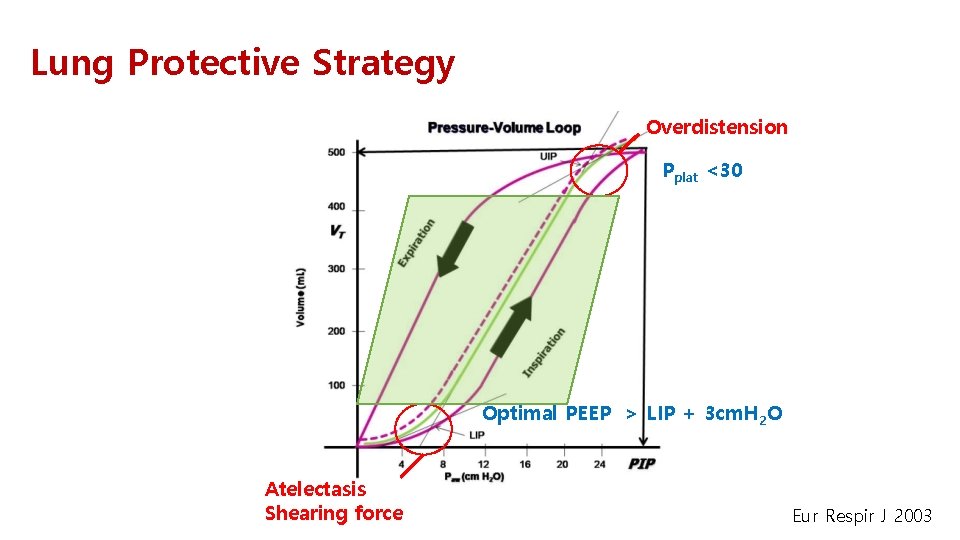
Lung Protective Strategy Overdistension Pplat <30 Optimal PEEP > LIP + 3 cm. H 2 O Atelectasis Shearing force Eur Respir J 2003
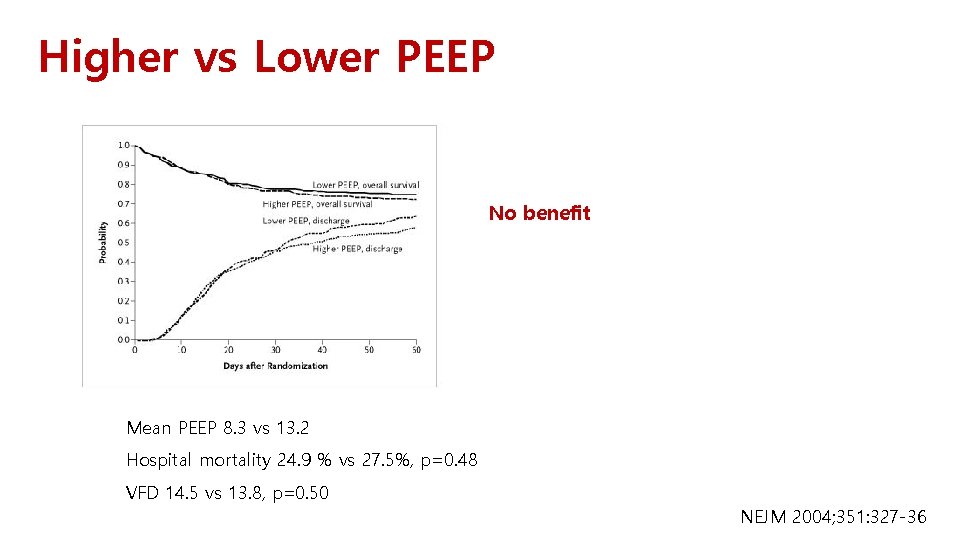
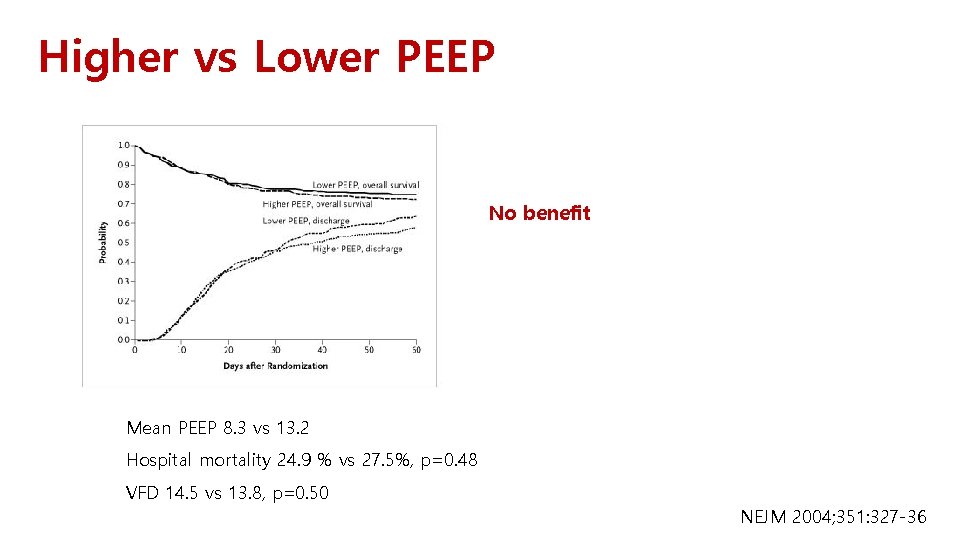
Higher vs Lower PEEP No benefit Mean PEEP 8. 3 vs 13. 2 Hospital mortality 24. 9 % vs 27. 5%, p=0. 48 VFD 14. 5 vs 13. 8, p=0. 50 NEJM 2004; 351: 327 -36
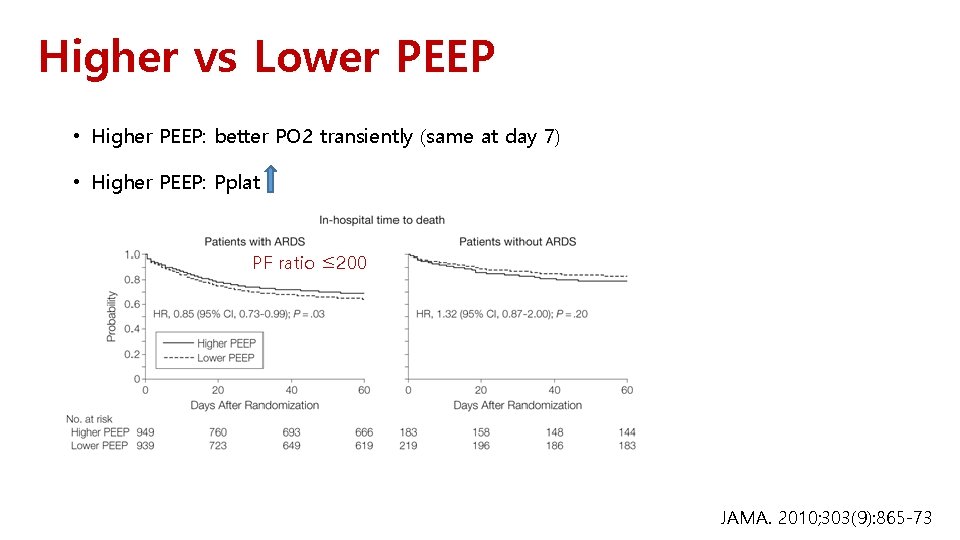
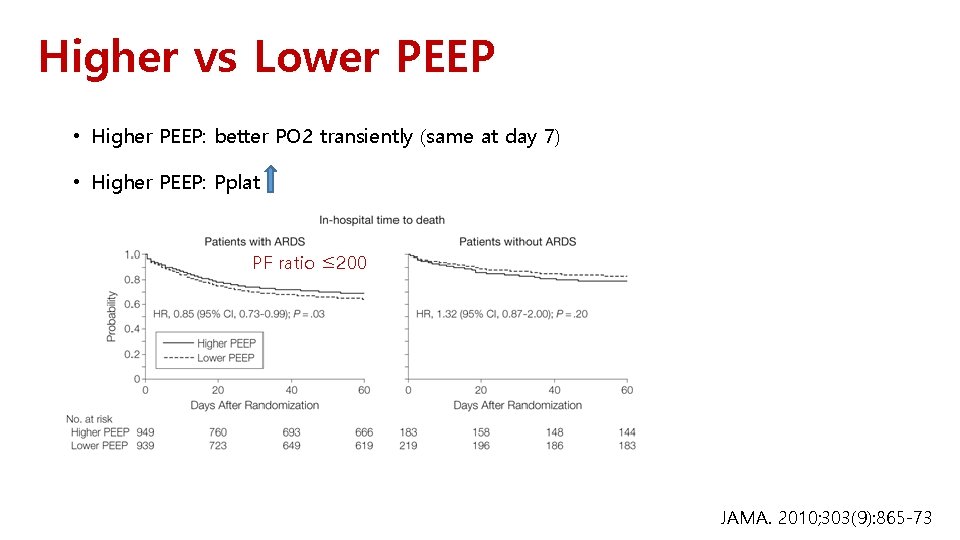
Higher vs Lower PEEP • Higher PEEP: better PO 2 transiently (same at day 7) • Higher PEEP: Pplat PF ratio ≤ 200 JAMA. 2010; 303(9): 865 -73
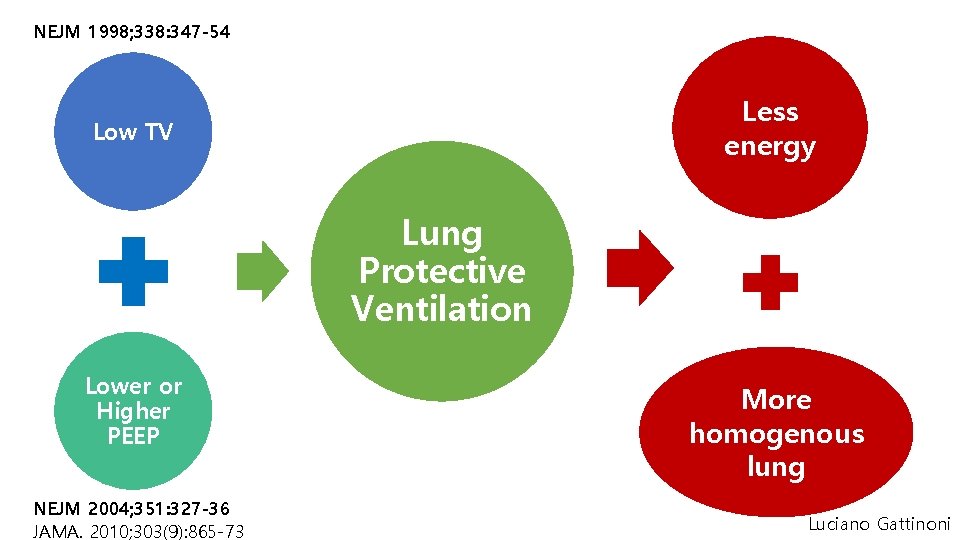
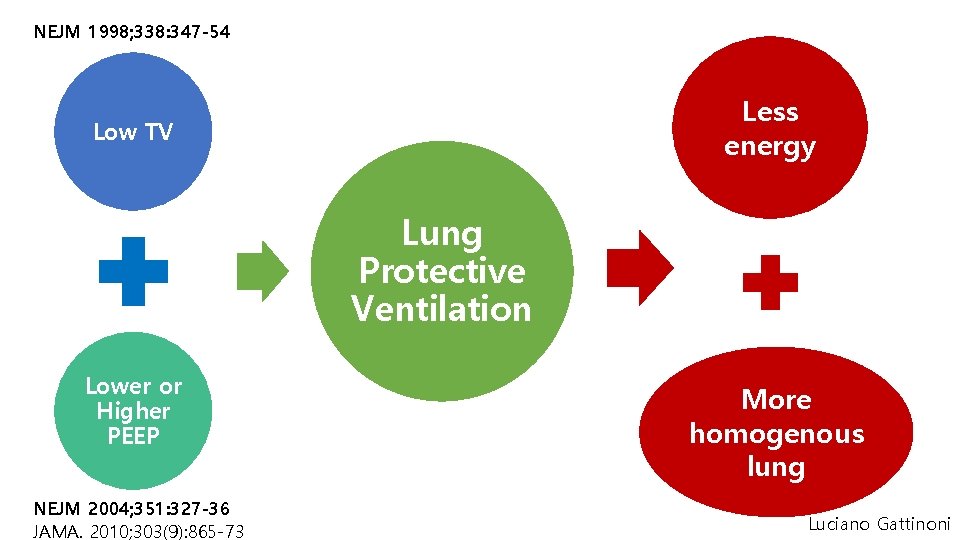
NEJM 1998; 338: 347 -54 Less energy Low TV Lung Protective Ventilation Lower or Higher PEEP NEJM 2004; 351: 327 -36 JAMA. 2010; 303(9): 865 -73 More homogenous lung Luciano Gattinoni
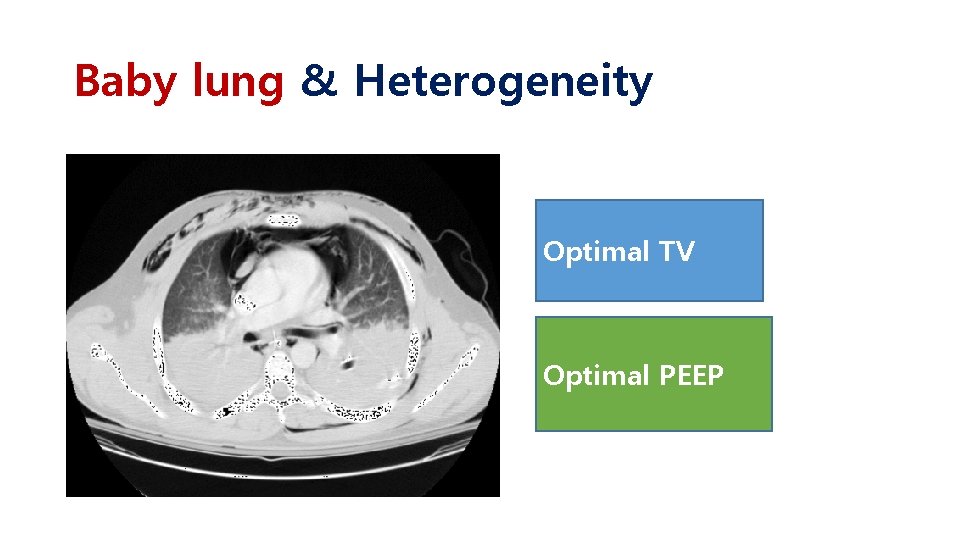
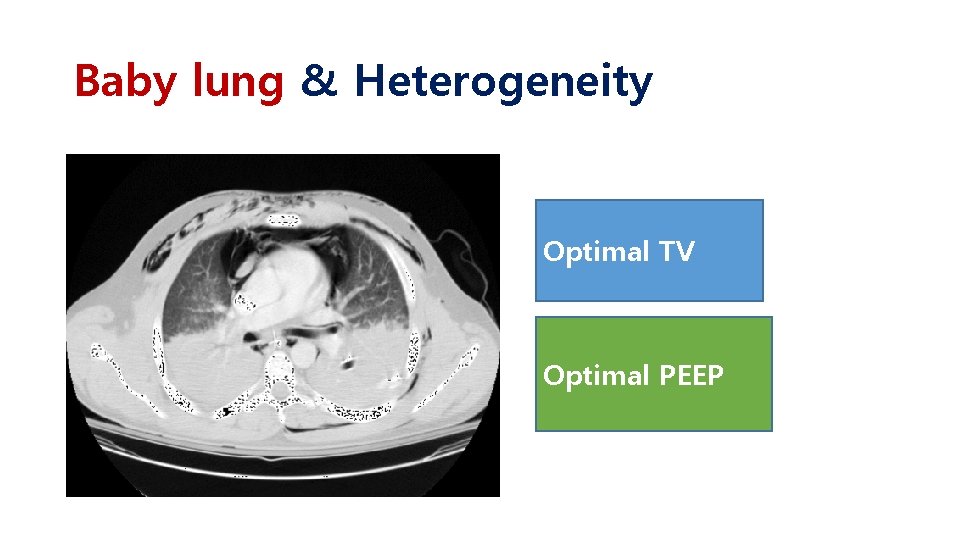
Baby lung & Heterogeneity Optimal TV Optimal PEEP
Protect baby lung • Low tidal volume • ultraprotective ventilation + ECCO 2 R • NMBA • ECMO
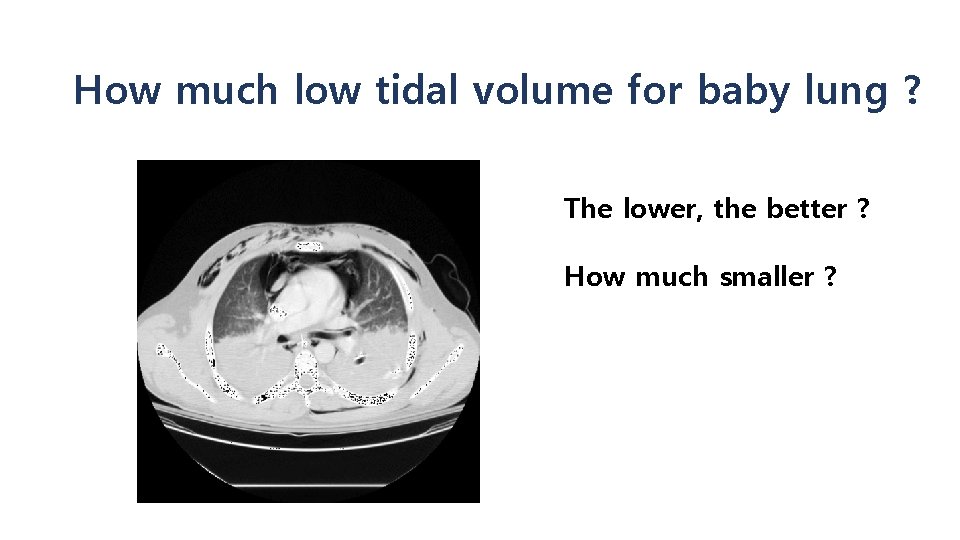
How much low tidal volume for baby lung ? The lower, the better ? How much smaller ?
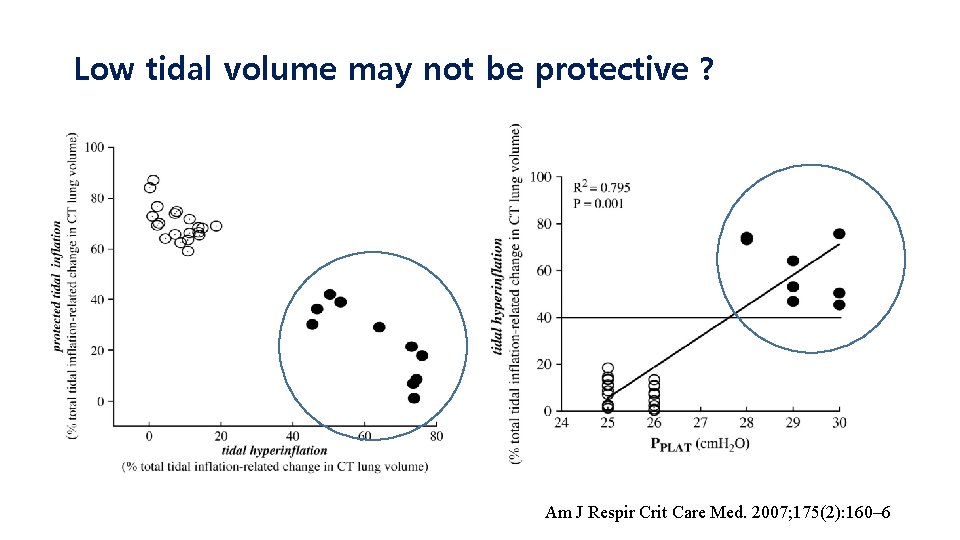
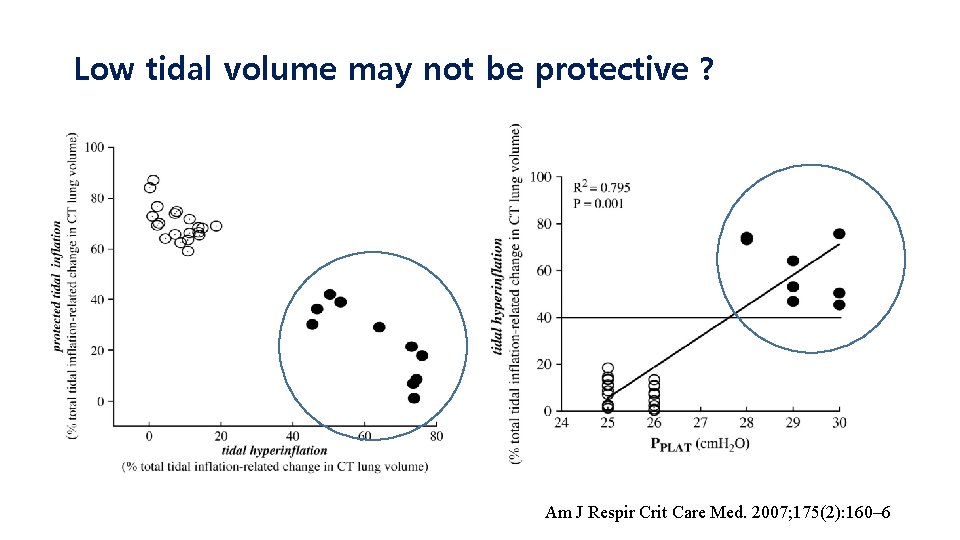
Low tidal volume may not be protective ? Am J Respir Crit Care Med. 2007; 175(2): 160– 6
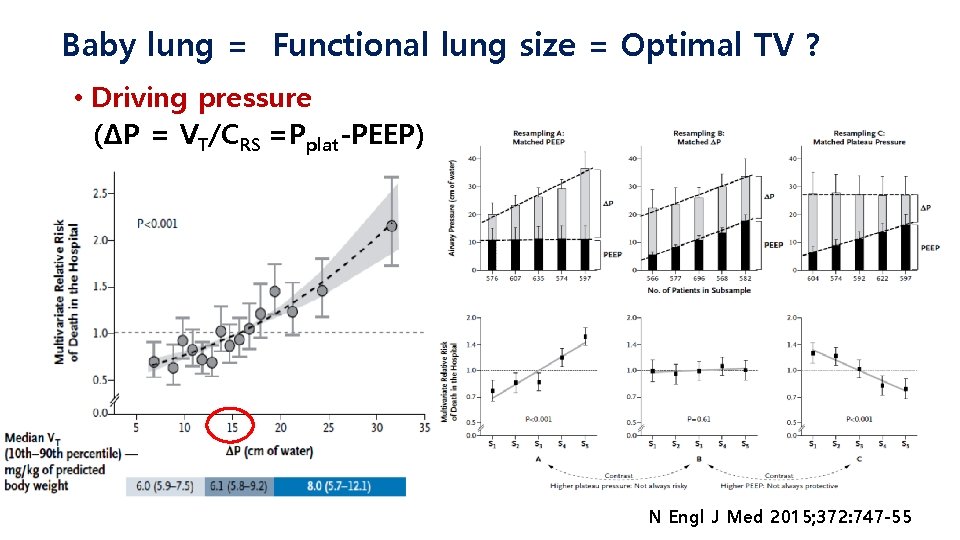
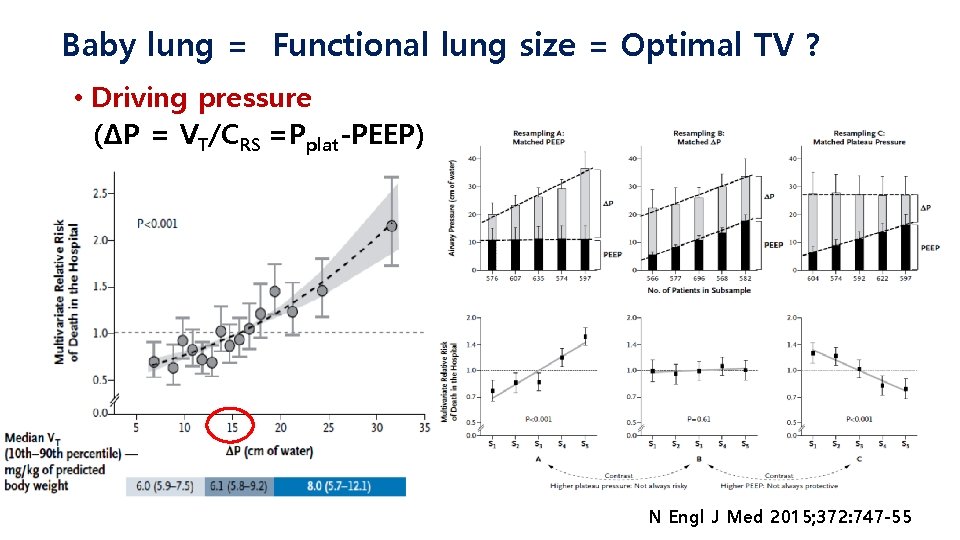
Baby lung = Functional lung size = Optimal TV ? • Driving pressure (ΔP = VT/CRS =Pplat-PEEP) N Engl J Med 2015; 372: 747 -55
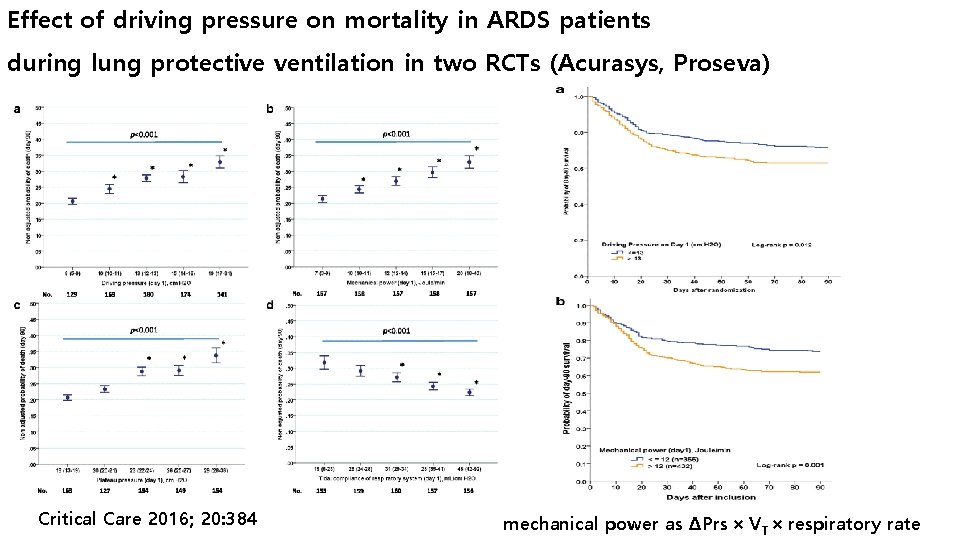
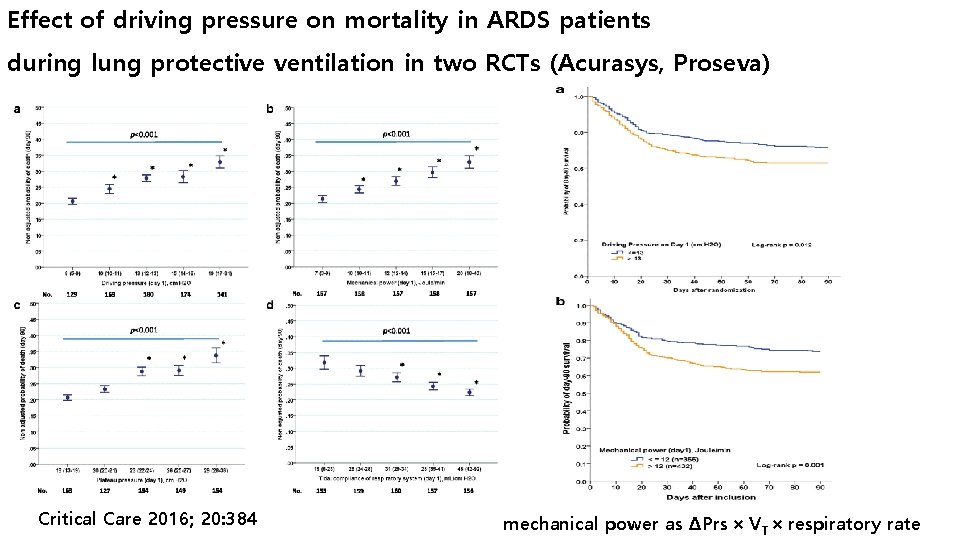
Effect of driving pressure on mortality in ARDS patients during lung protective ventilation in two RCTs (Acurasys, Proseva) Critical Care 2016; 20: 384 mechanical power as ΔPrs × VT × respiratory rate
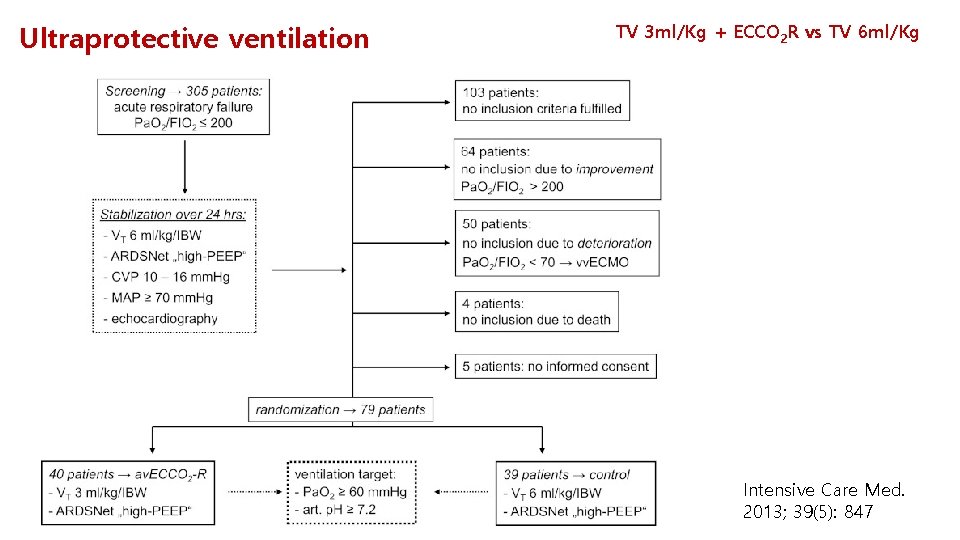
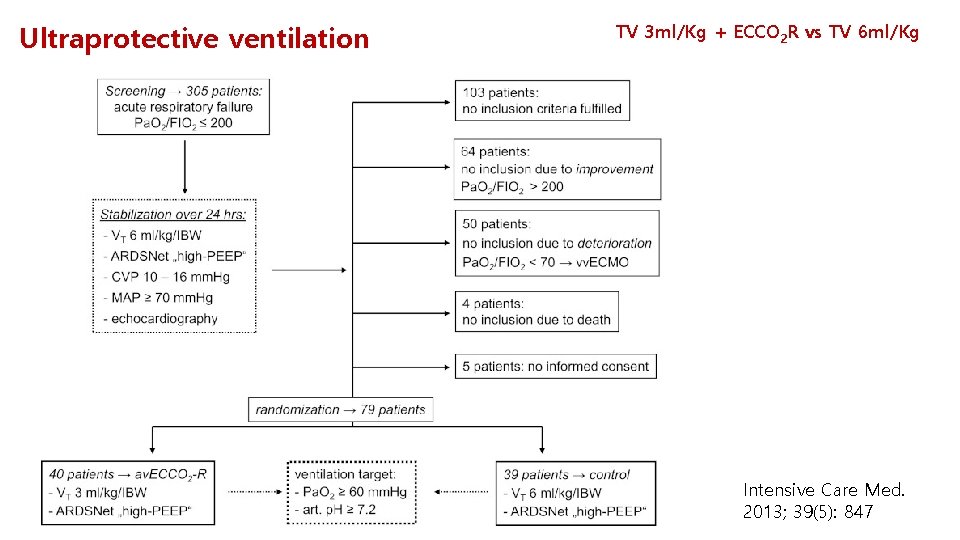
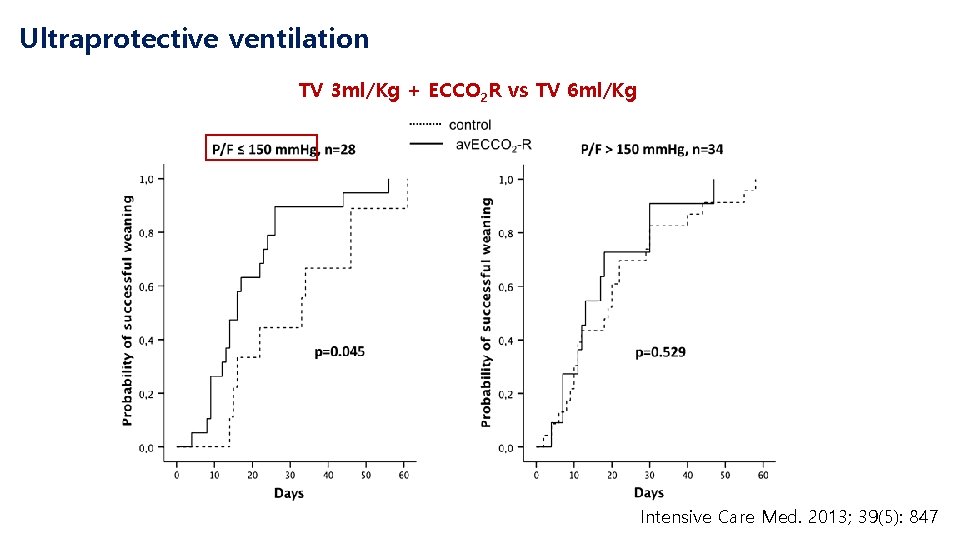
Ultraprotective ventilation TV 3 ml/Kg + ECCO 2 R vs TV 6 ml/Kg Intensive Care Med. 2013; 39(5): 847
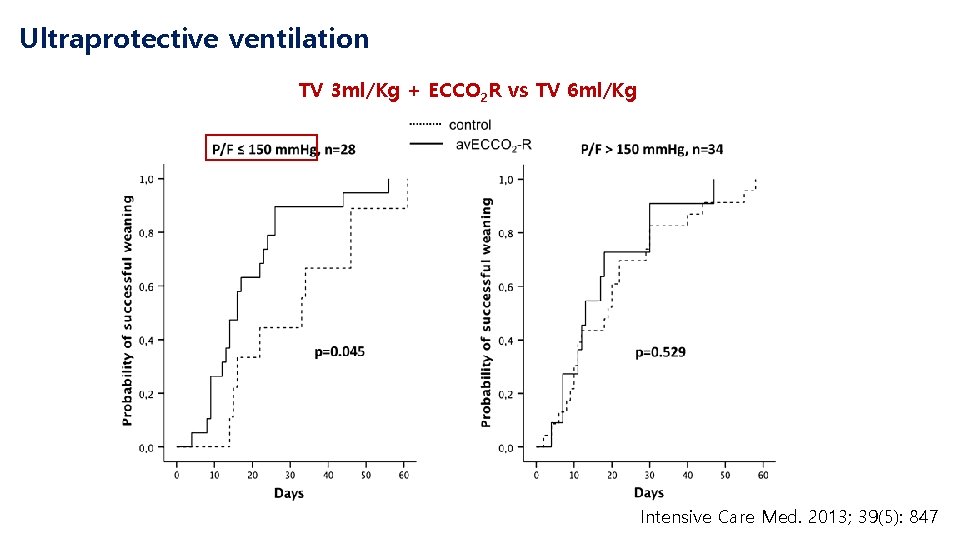
Ultraprotective ventilation TV 3 ml/Kg + ECCO 2 R vs TV 6 ml/Kg Intensive Care Med. 2013; 39(5): 847
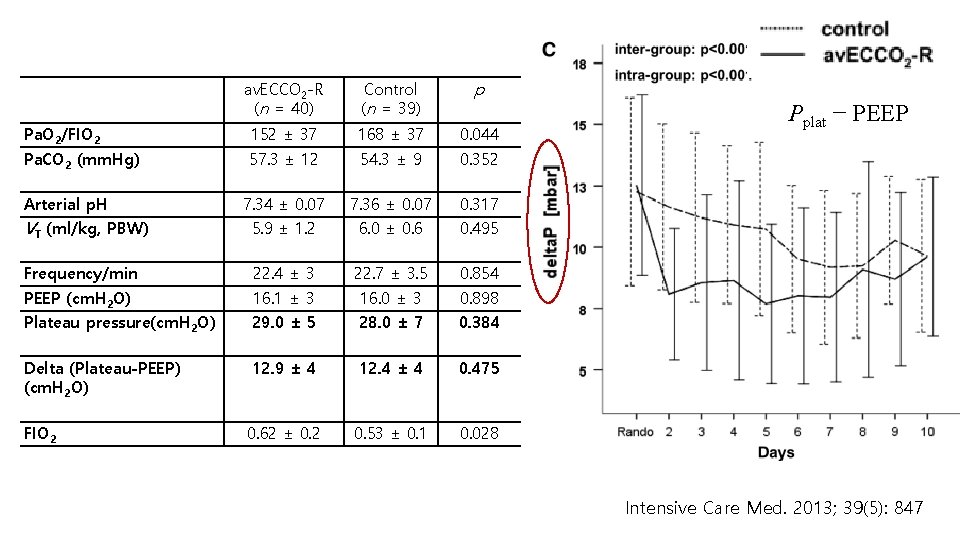
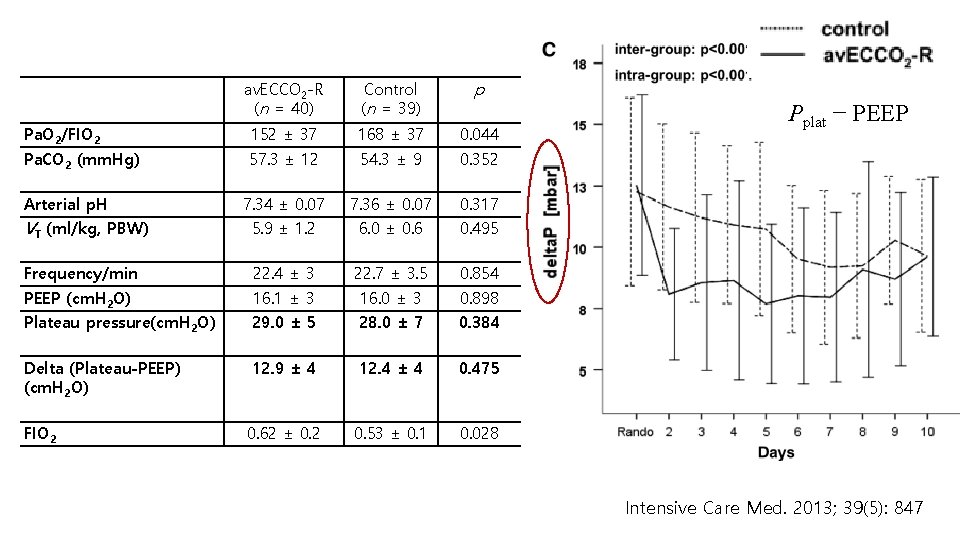
av. ECCO 2 -R (n = 40) Control (n = 39) p Pa. O 2/FIO 2 152 ± 37 168 ± 37 0. 044 Pa. CO 2 (mm. Hg) 57. 3 ± 12 54. 3 ± 9 0. 352 7. 34 ± 0. 07 7. 36 ± 0. 07 0. 317 VT (ml/kg, PBW) 5. 9 ± 1. 2 6. 0 ± 0. 6 0. 495 Frequency/min 22. 4 ± 3 22. 7 ± 3. 5 0. 854 PEEP (cm. H 2 O) 16. 1 ± 3 16. 0 ± 3 0. 898 Plateau pressure(cm. H 2 O) 29. 0 ± 5 28. 0 ± 7 0. 384 Delta (Plateau-PEEP) (cm. H 2 O) 12. 9 ± 4 12. 4 ± 4 0. 475 FIO 2 0. 62 ± 0. 2 0. 53 ± 0. 1 0. 028 Arterial p. H Pplat − PEEP Intensive Care Med. 2013; 39(5): 847
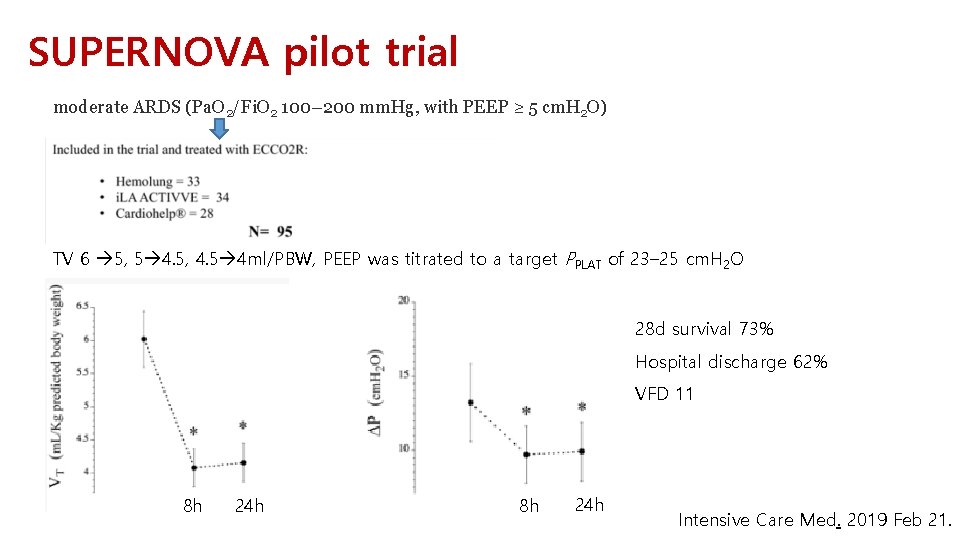
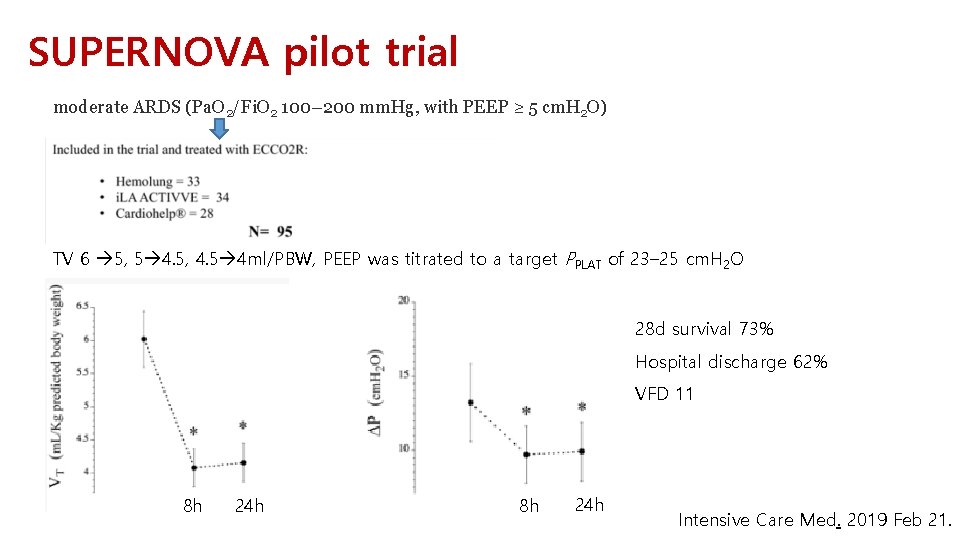
SUPERNOVA pilot trial moderate ARDS (Pa. O 2/Fi. O 2 100– 200 mm. Hg, with PEEP ≥ 5 cm. H 2 O) TV 6 5, 5 4. 5, 4. 5 4 ml/PBW, PEEP was titrated to a target PPLAT of 23– 25 cm. H 2 O 28 d survival 73% Hospital discharge 62% VFD 11 8 h 24 h Intensive Care Med. 2019 Feb 21.

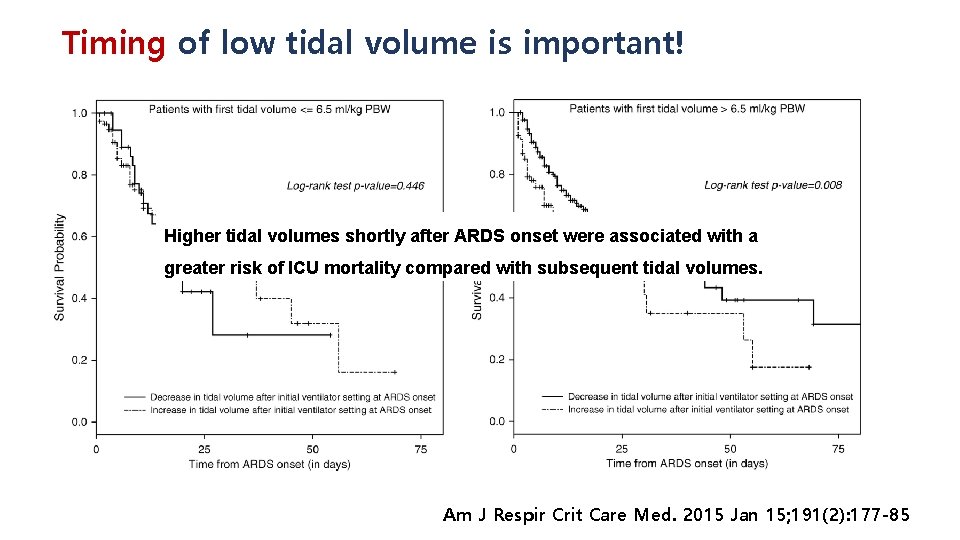
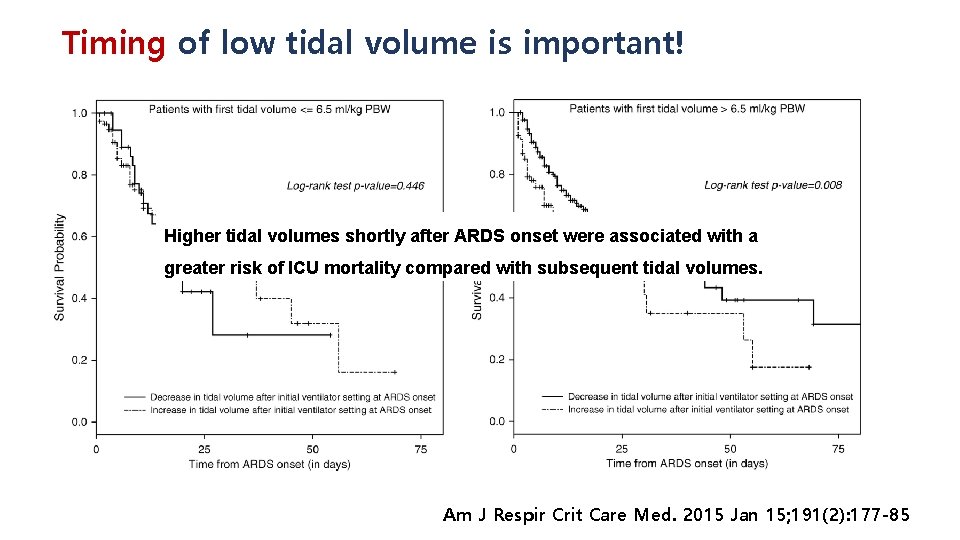
Timing of low tidal volume is important! Higher tidal volumes shortly after ARDS onset were associated with a greater risk of ICU mortality compared with subsequent tidal volumes. Am J Respir Crit Care Med. 2015 Jan 15; 191(2): 177 -85
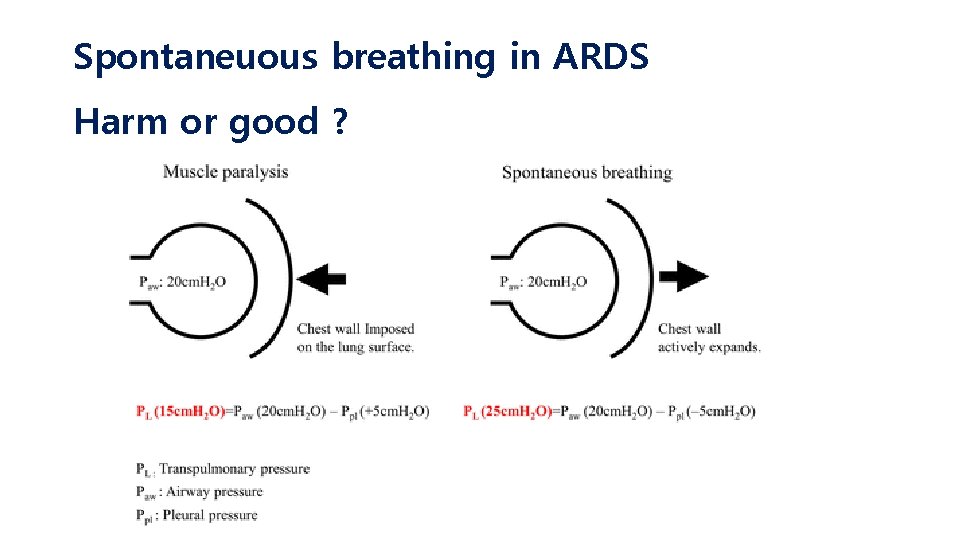
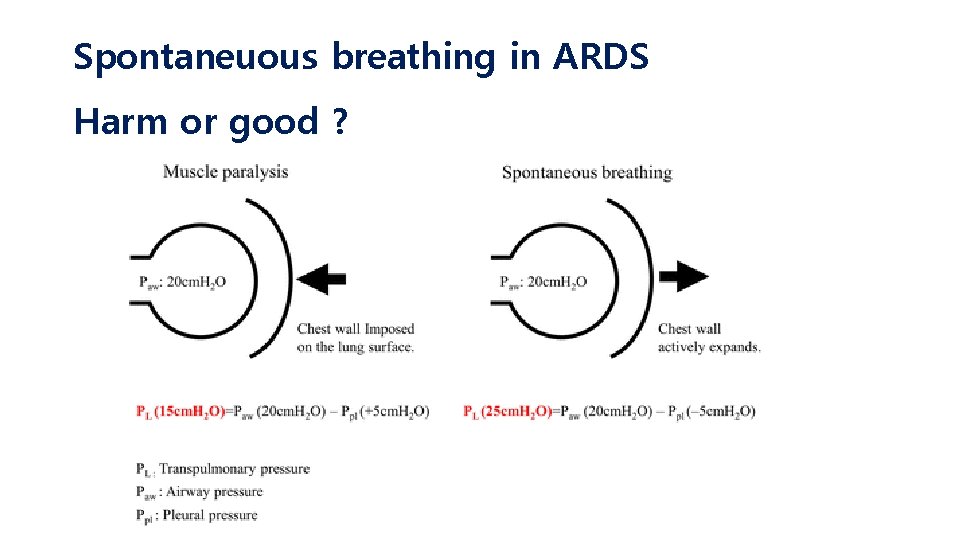
Spontaneuous breathing in ARDS Harm or good ?
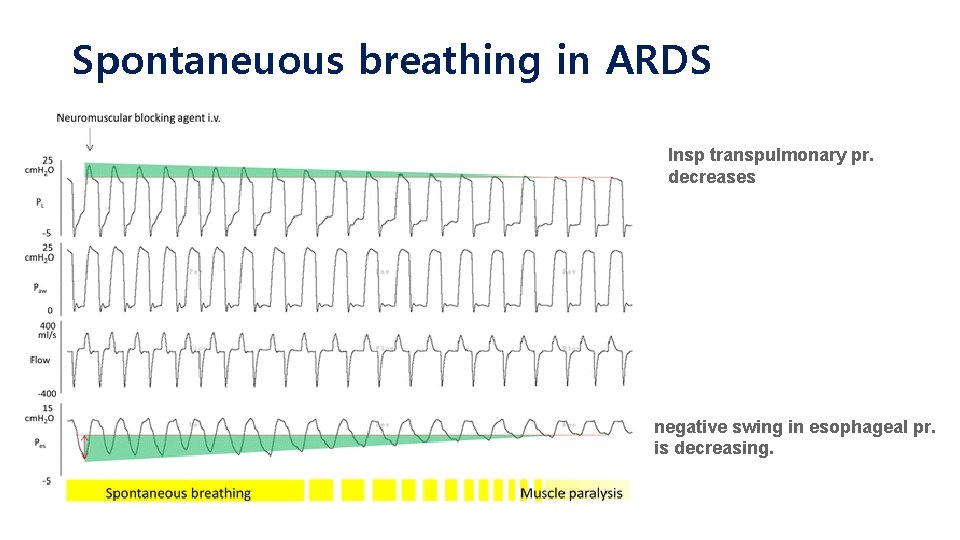
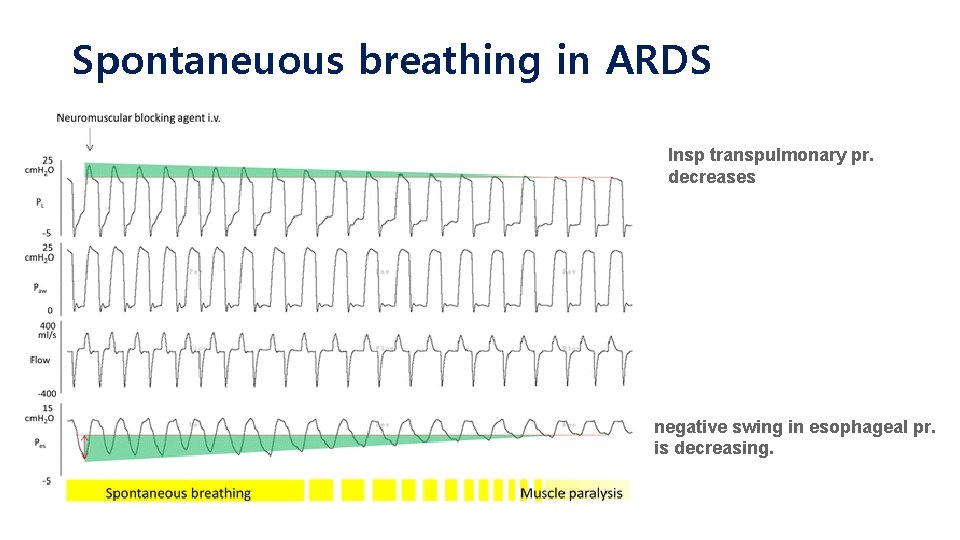
Spontaneuous breathing in ARDS Insp transpulmonary pr. decreases negative swing in esophageal pr. is decreasing.
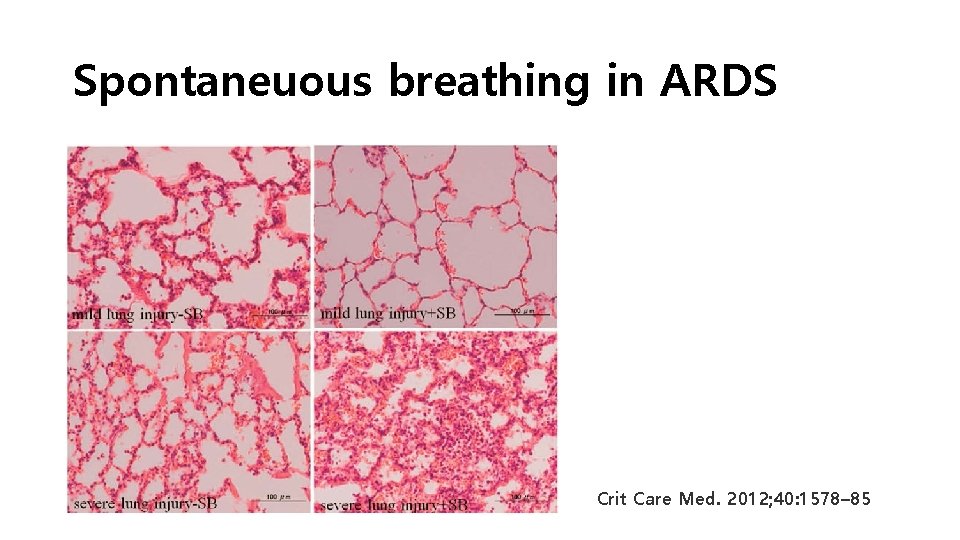
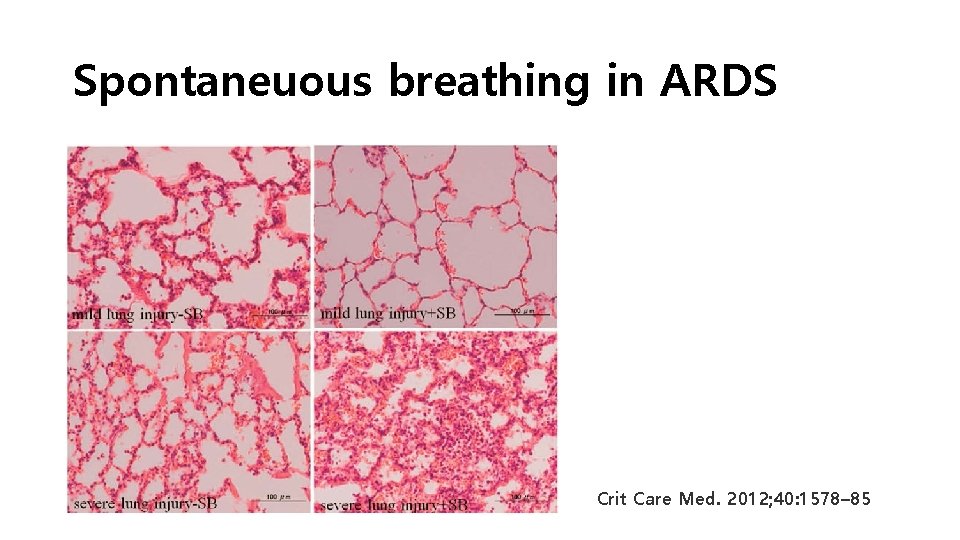
Spontaneuous breathing in ARDS Crit Care Med. 2012; 40: 1578– 85
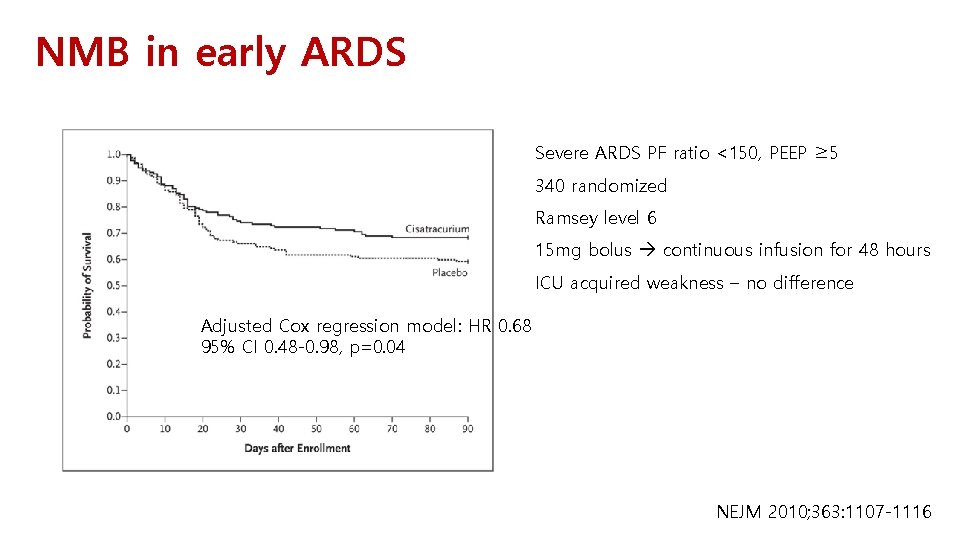
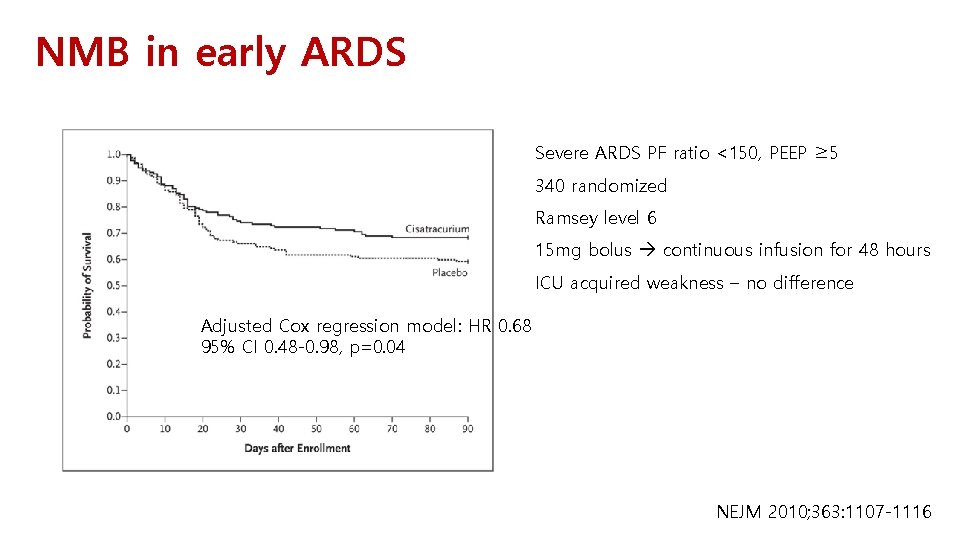
NMB in early ARDS Severe ARDS PF ratio <150, PEEP ≥ 5 340 randomized Ramsey level 6 15 mg bolus continuous infusion for 48 hours ICU acquired weakness – no difference Adjusted Cox regression model: HR 0. 68 95% CI 0. 48 -0. 98, p=0. 04 NEJM 2010; 363: 1107 -1116
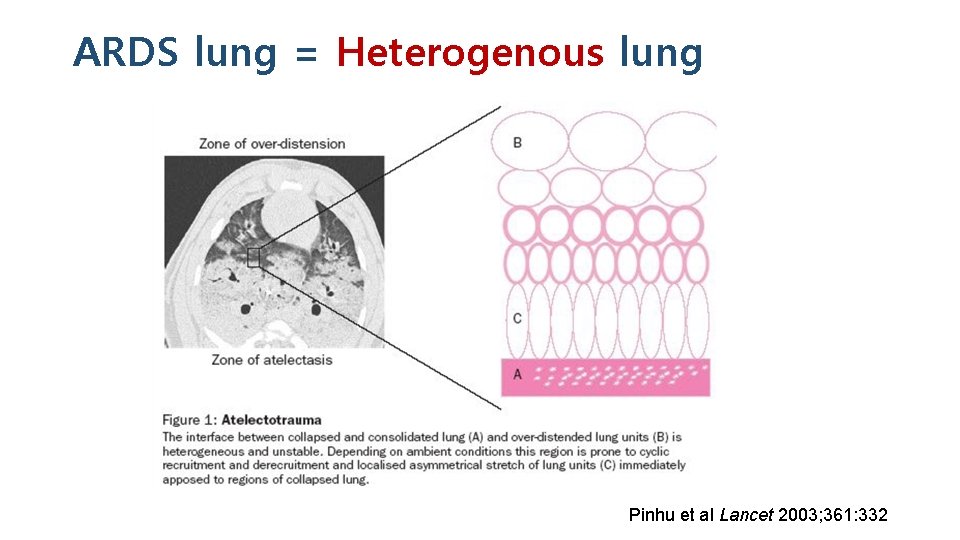
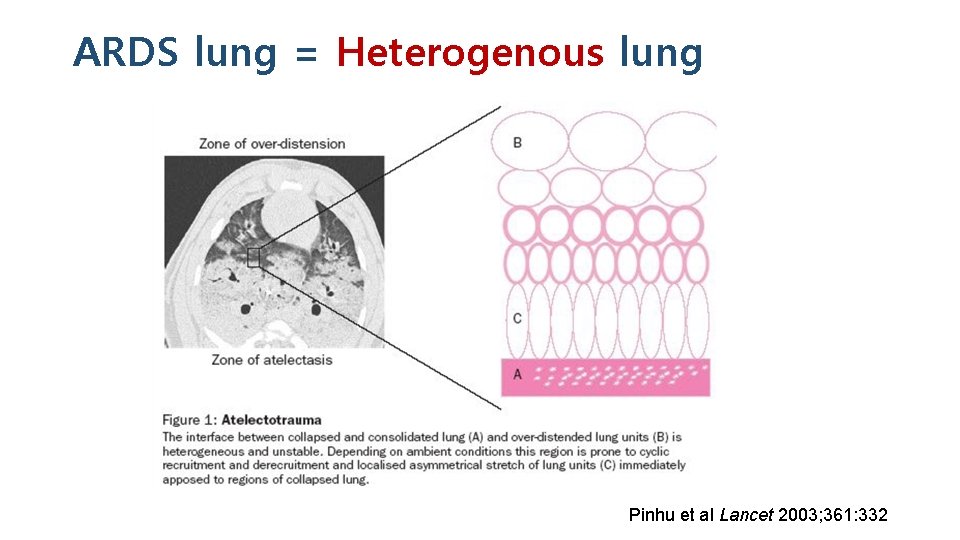
ARDS lung = Heterogenous lung Pinhu et al Lancet 2003; 361: 332
From heterogeneity to homogeniety • Prone position • Recruitment • HFOV • APRV
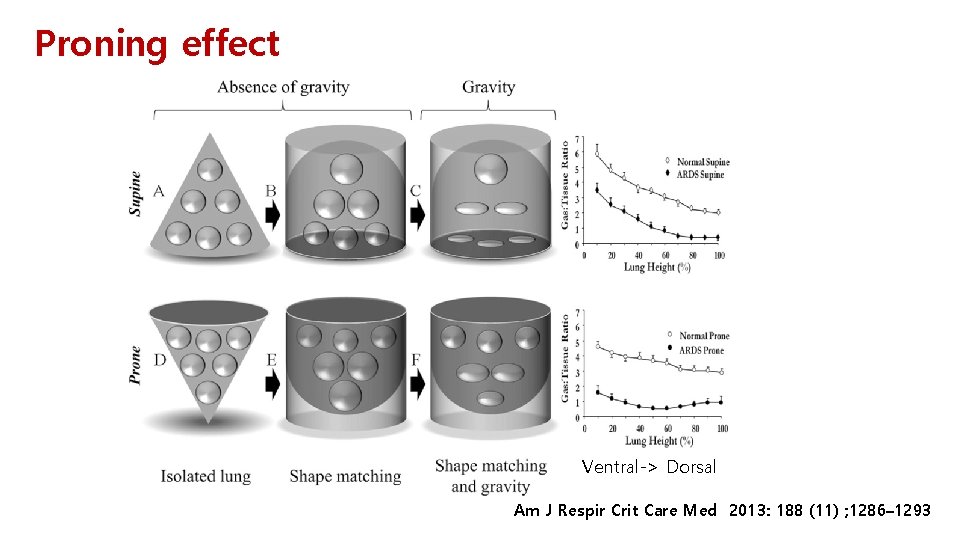
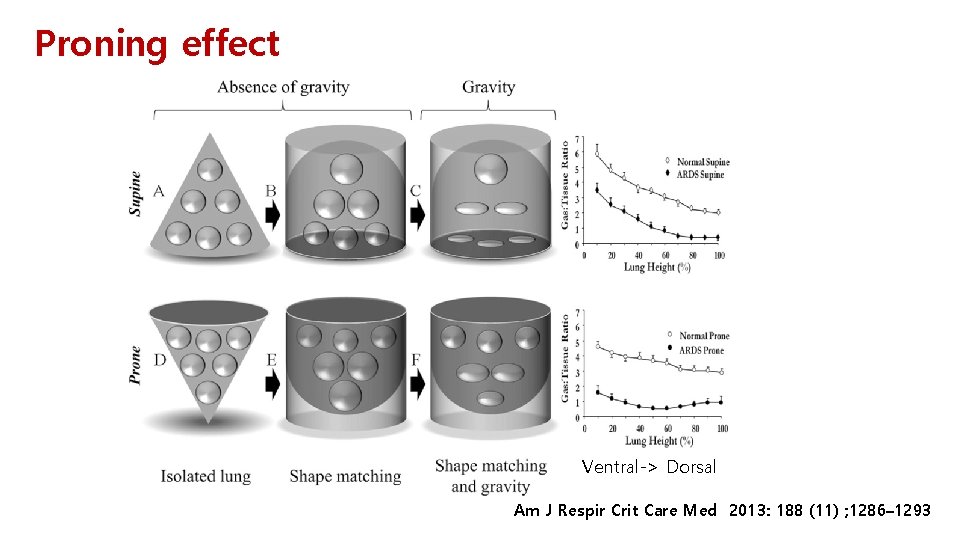
Proning effect Ventral-> Dorsal Am J Respir Crit Care Med 2013: 188 (11) ; 1286– 1293
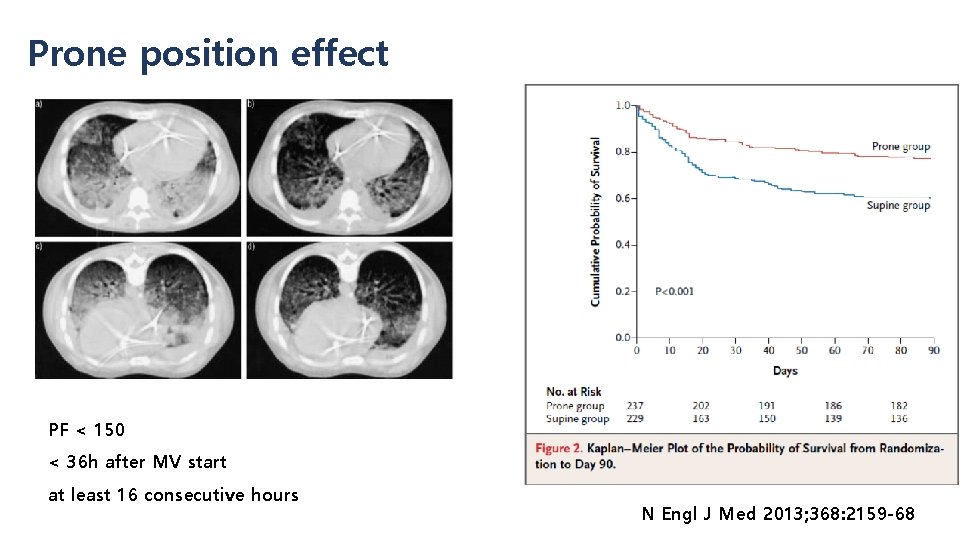
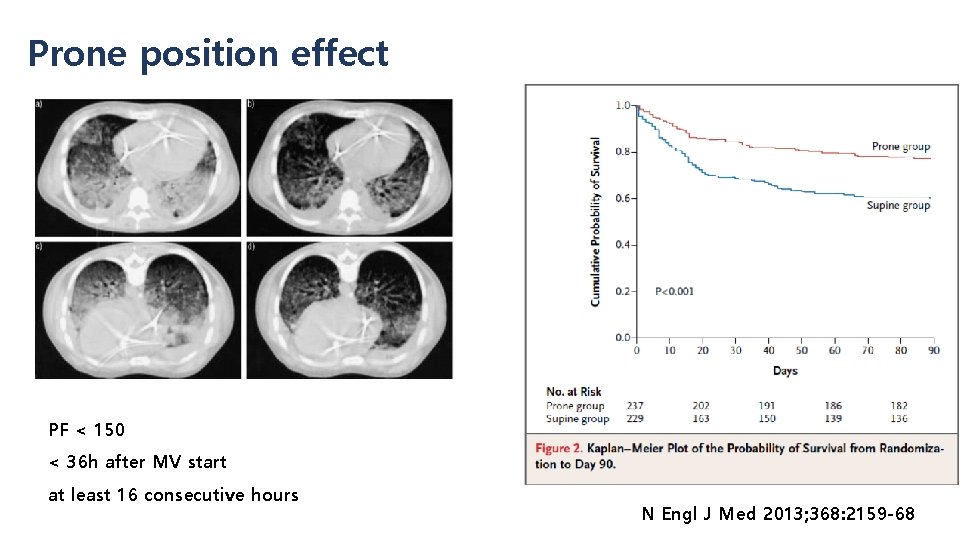
Prone position effect PF < 150 < 36 h after MV start at least 16 consecutive hours N Engl J Med 2013; 368: 2159 -68
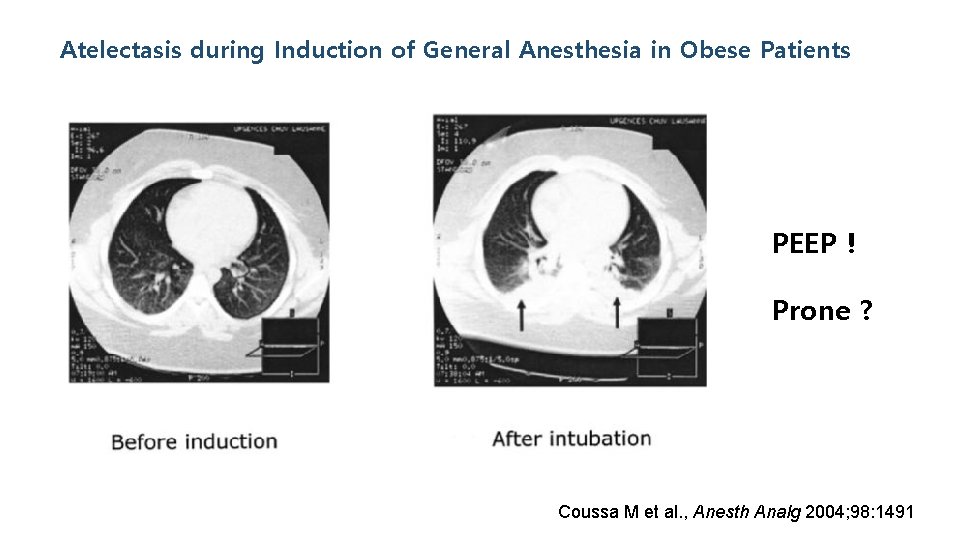
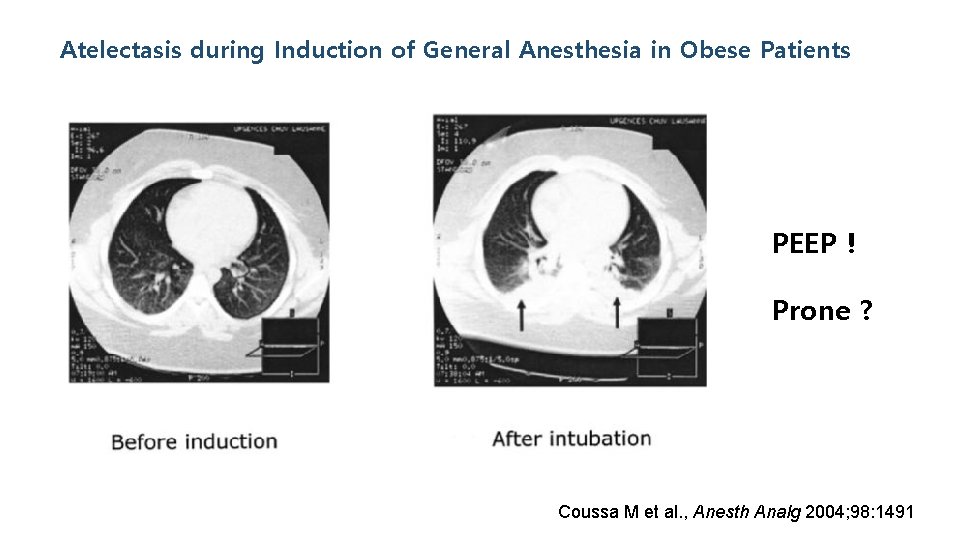
Atelectasis during Induction of General Anesthesia in Obese Patients PEEP ! Prone ? Coussa M et al. , Anesth Analg 2004; 98: 1491
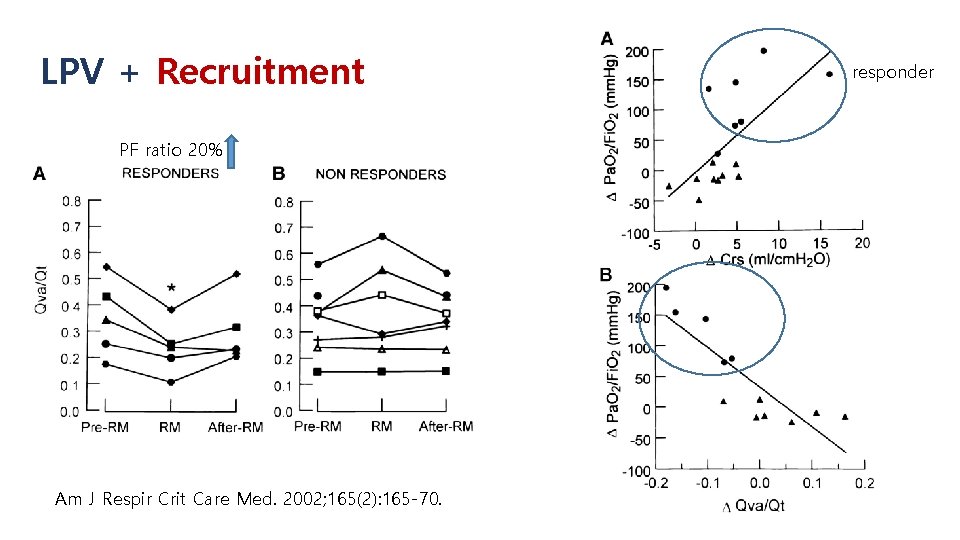
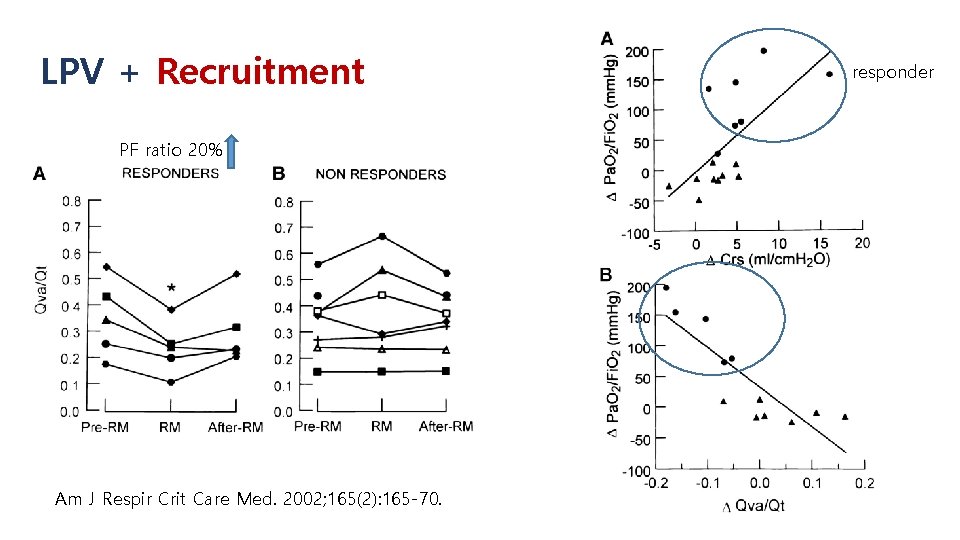
LPV + Recruitment PF ratio 20% Am J Respir Crit Care Med. 2002; 165(2): 165 -70. responder
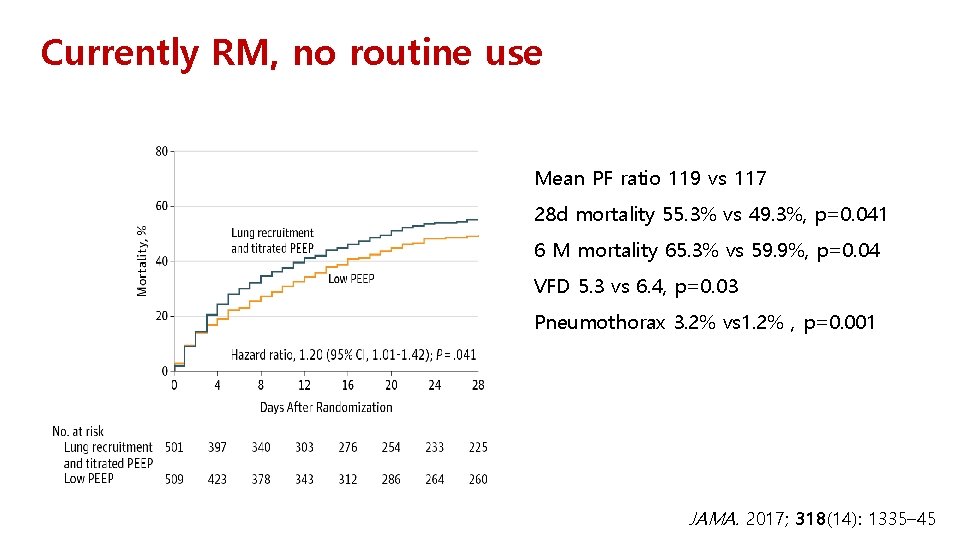
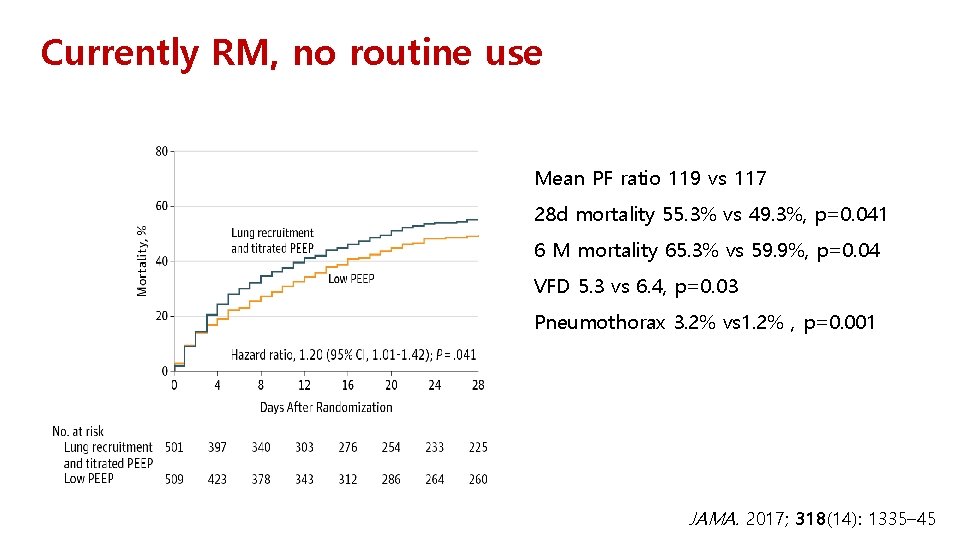
Currently RM, no routine use Mean PF ratio 119 vs 117 28 d mortality 55. 3% vs 49. 3%, p=0. 041 6 M mortality 65. 3% vs 59. 9%, p=0. 04 VFD 5. 3 vs 6. 4, p=0. 03 Pneumothorax 3. 2% vs 1. 2% , p=0. 001 JAMA. 2017; 318(14): 1335– 45
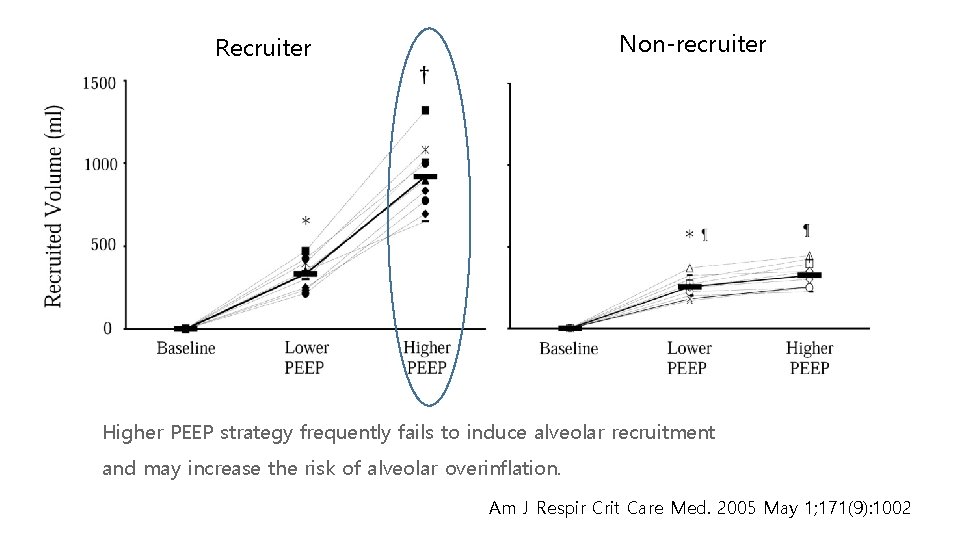
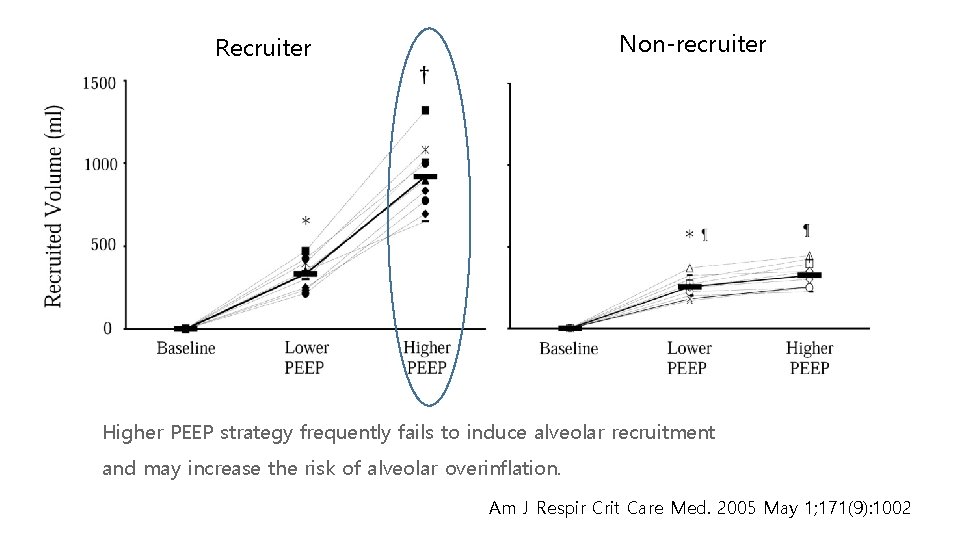
Non-recruiter Recruiter Higher PEEP strategy frequently fails to induce alveolar recruitment and may increase the risk of alveolar overinflation. Am J Respir Crit Care Med. 2005 May 1; 171(9): 1002
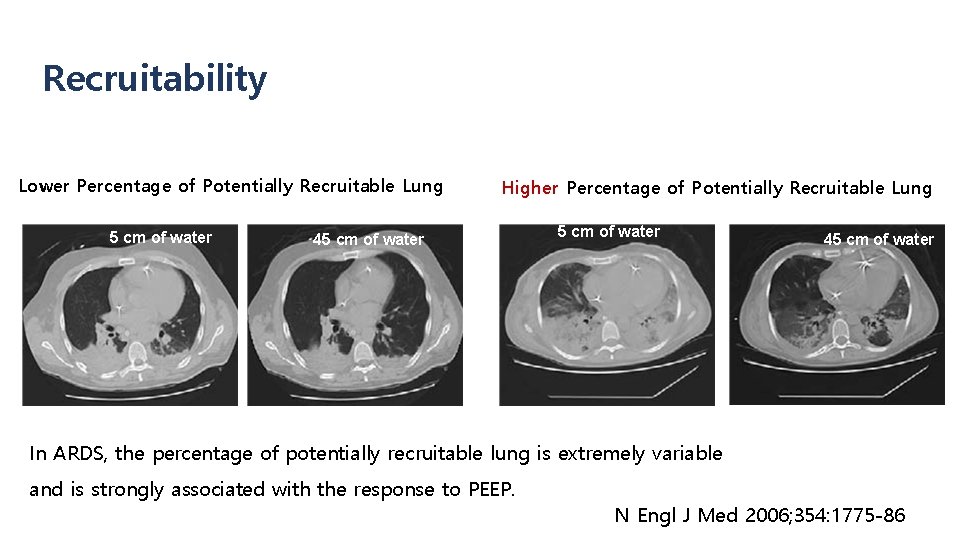
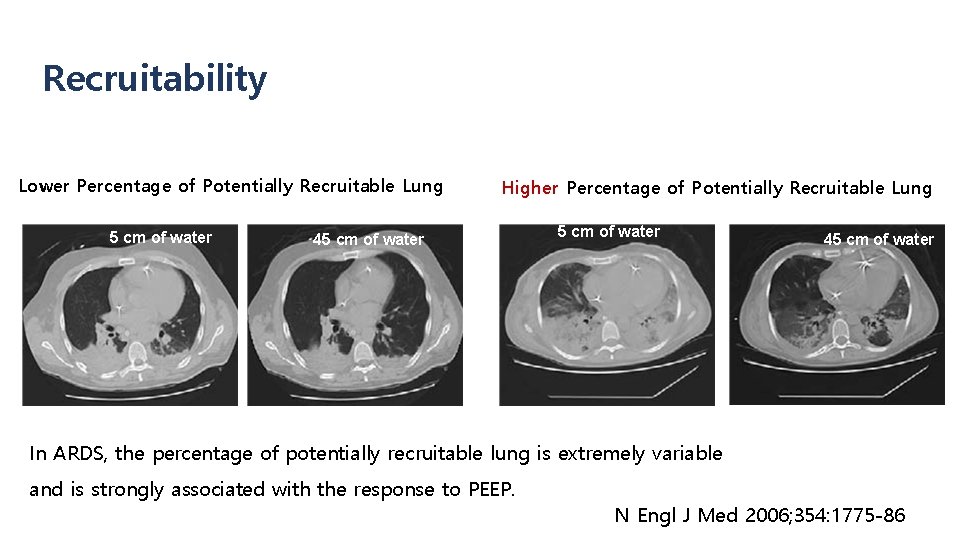
Recruitability Lower Percentage of Potentially Recruitable Lung 5 cm of water Higher Percentage of Potentially Recruitable Lung 45 cm of water In ARDS, the percentage of potentially recruitable lung is extremely variable and is strongly associated with the response to PEEP. N Engl J Med 2006; 354: 1775 -86
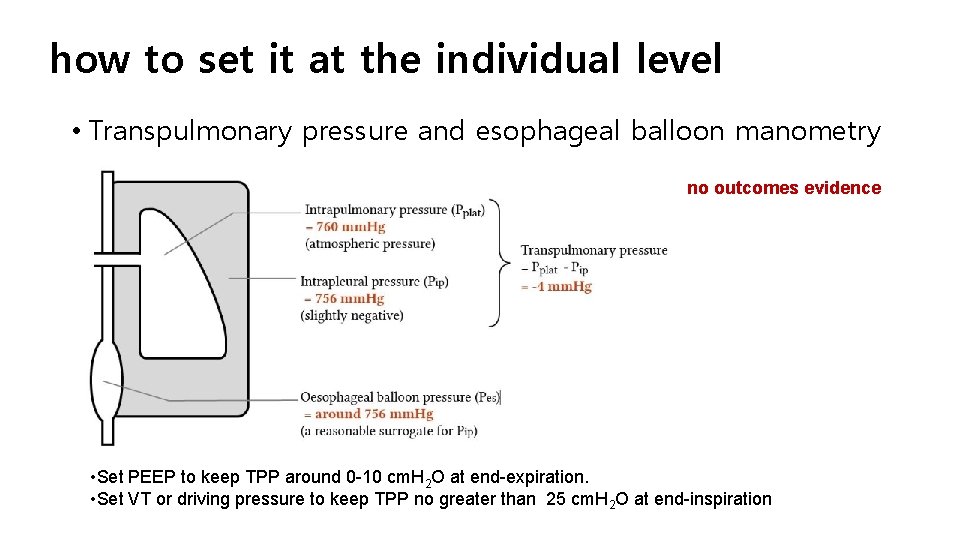
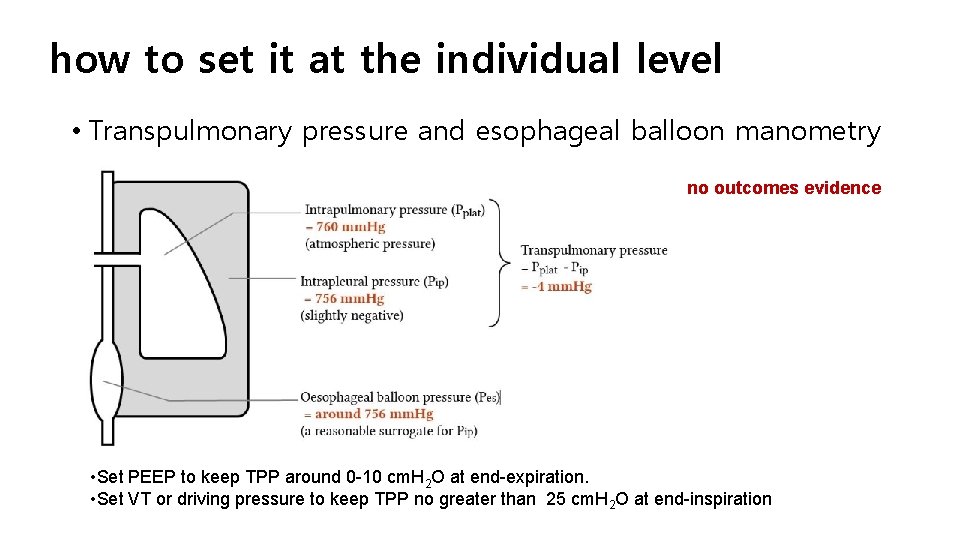
how to set it at the individual level • Transpulmonary pressure and esophageal balloon manometry no outcomes evidence • Set PEEP to keep TPP around 0 -10 cm. H 2 O at end-expiration. • Set VT or driving pressure to keep TPP no greater than 25 cm. H 2 O at end-inspiration

Electrical impedance tomography no outcomes evidence
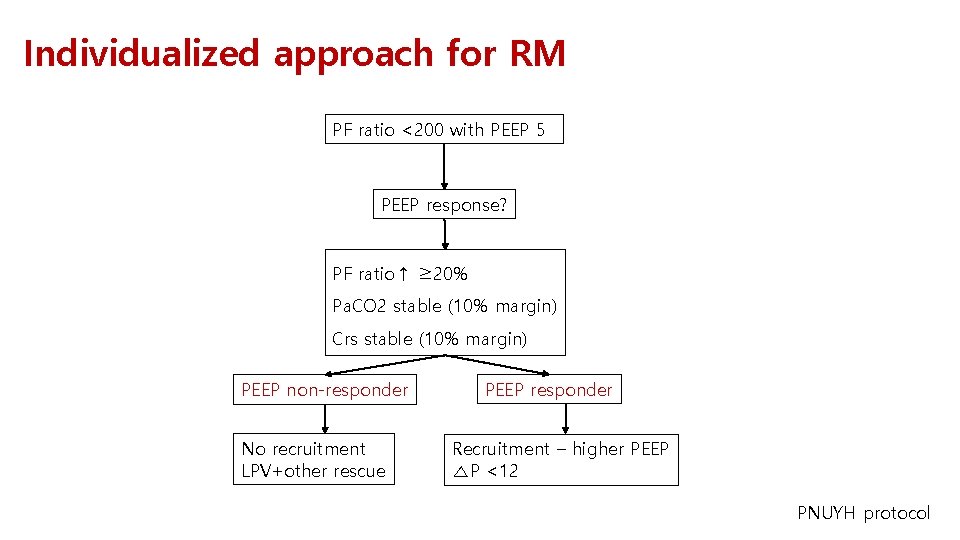
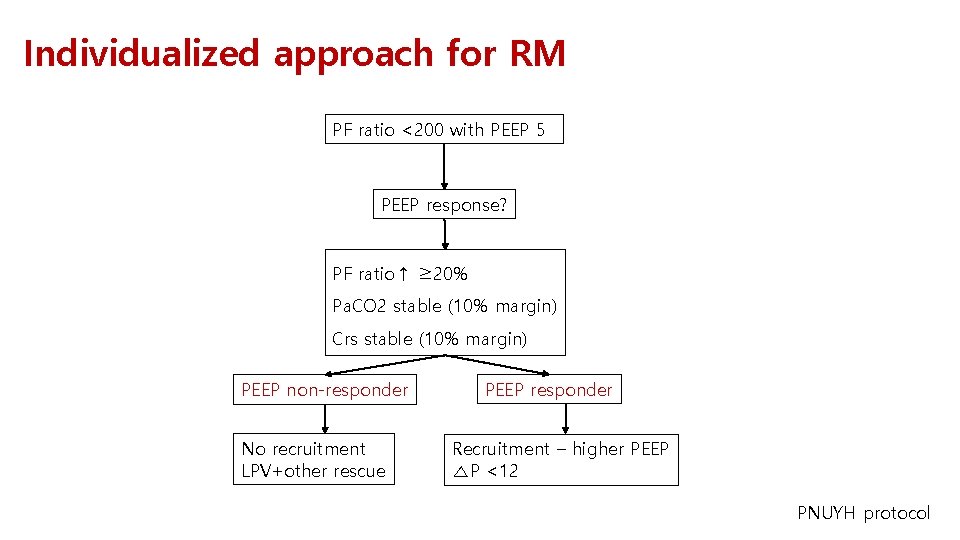
Individualized approach for RM PF ratio <200 with PEEP 5 PEEP response? PF ratio↑ ≥ 20% Pa. CO 2 stable (10% margin) Crs stable (10% margin) PEEP non-responder No recruitment LPV+other rescue PEEP responder Recruitment – higher PEEP △P <12 PNUYH protocol
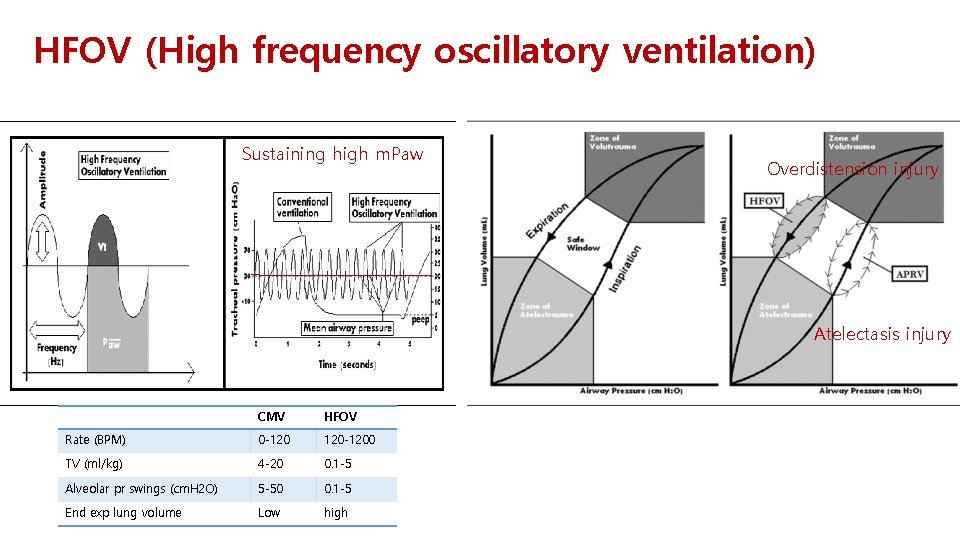
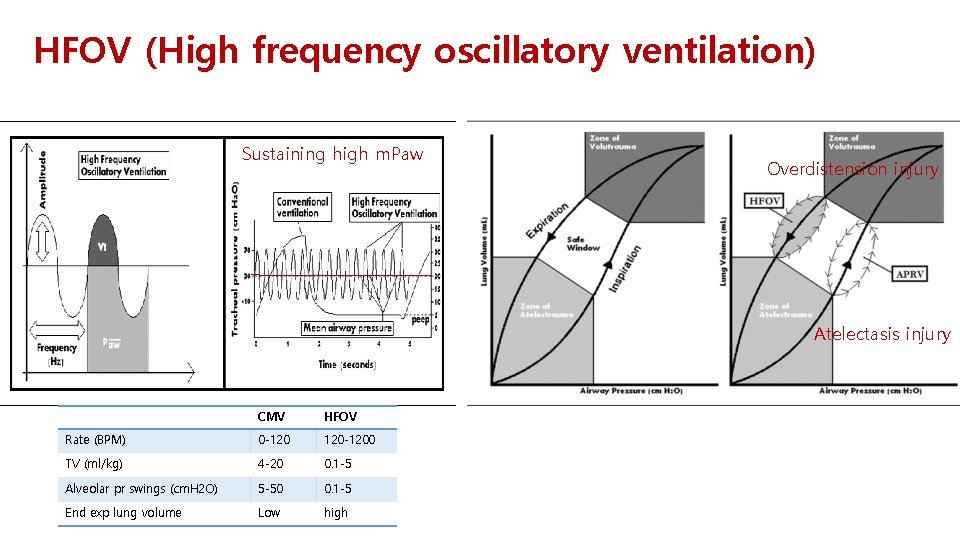
HFOV (High frequency oscillatory ventilation) Sustaining high m. Paw Overdistension injury Atelectasis injury CMV HFOV Rate (BPM) 0 -120 120 -1200 TV (ml/kg) 4 -20 0. 1 -5 Alveolar pr swings (cm. H 2 O) 5 -50 0. 1 -5 End exp lung volume Low high
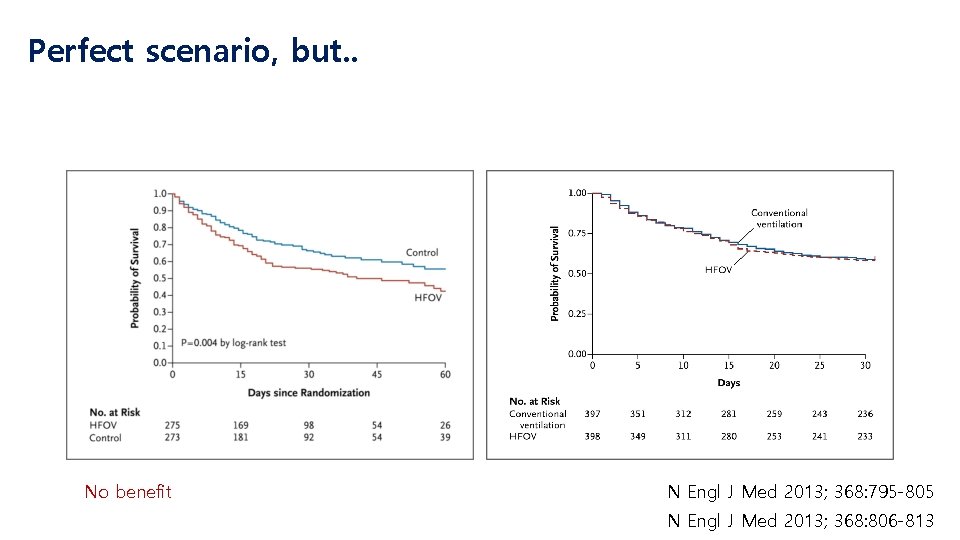
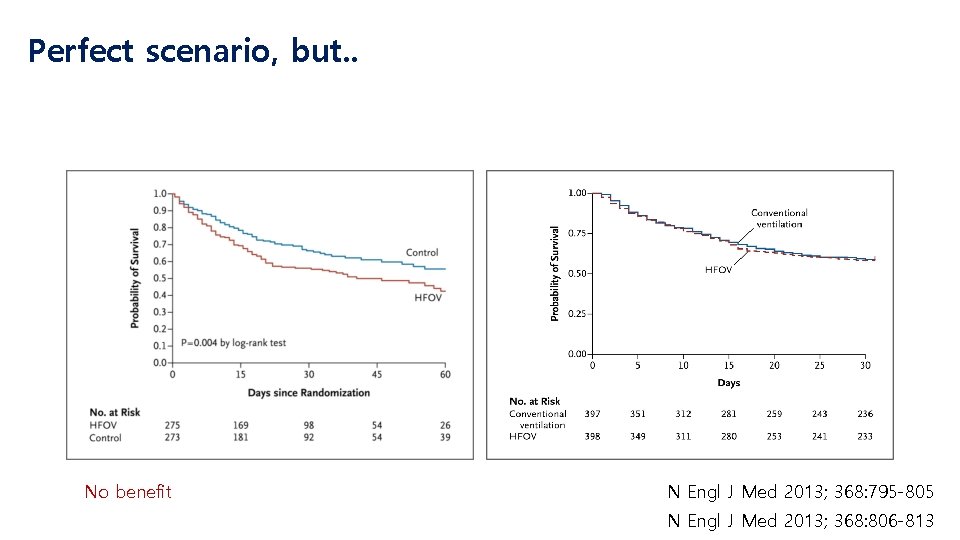
Perfect scenario, but. . No benefit N Engl J Med 2013; 368: 795 -805 N Engl J Med 2013; 368: 806 -813
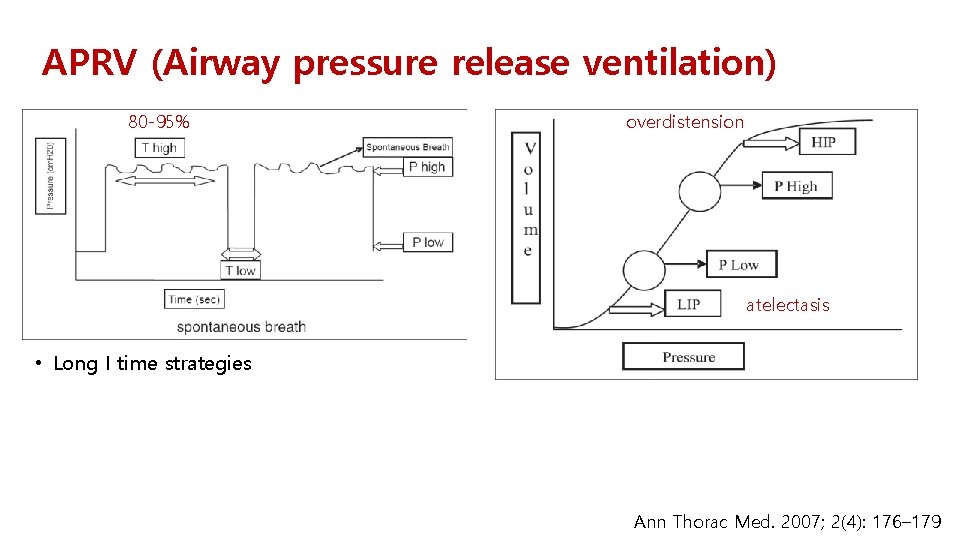
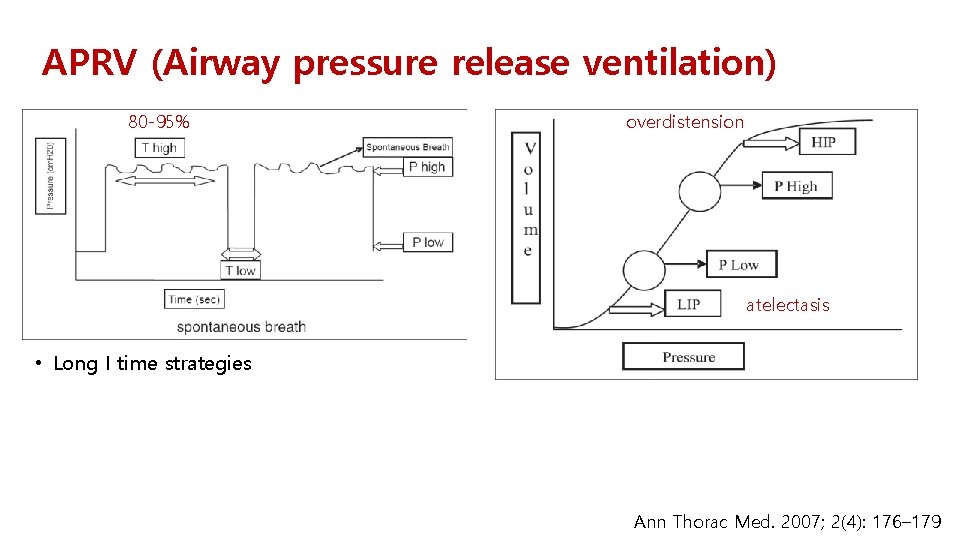
APRV (Airway pressure release ventilation) 80 -95% overdistension atelectasis • Long I time strategies Ann Thorac Med. 2007; 2(4): 176– 179
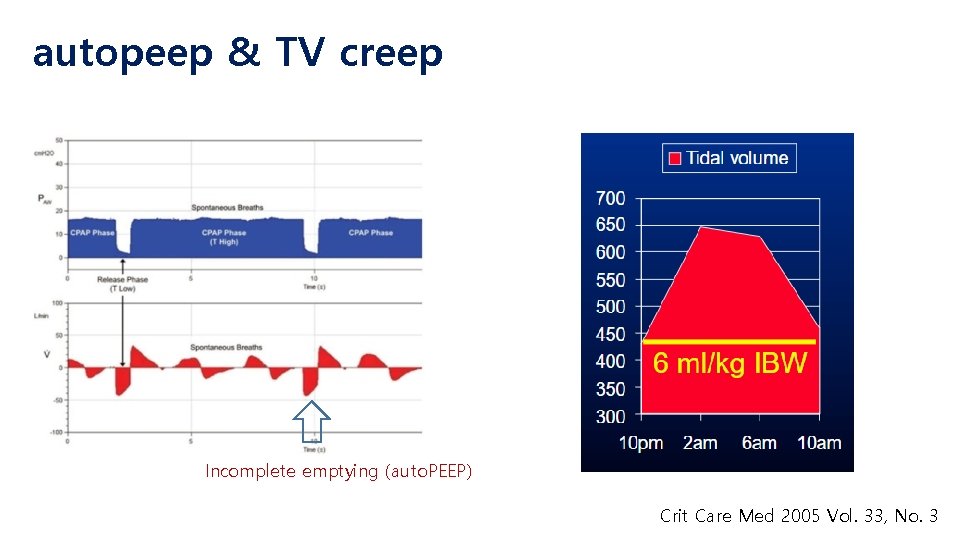
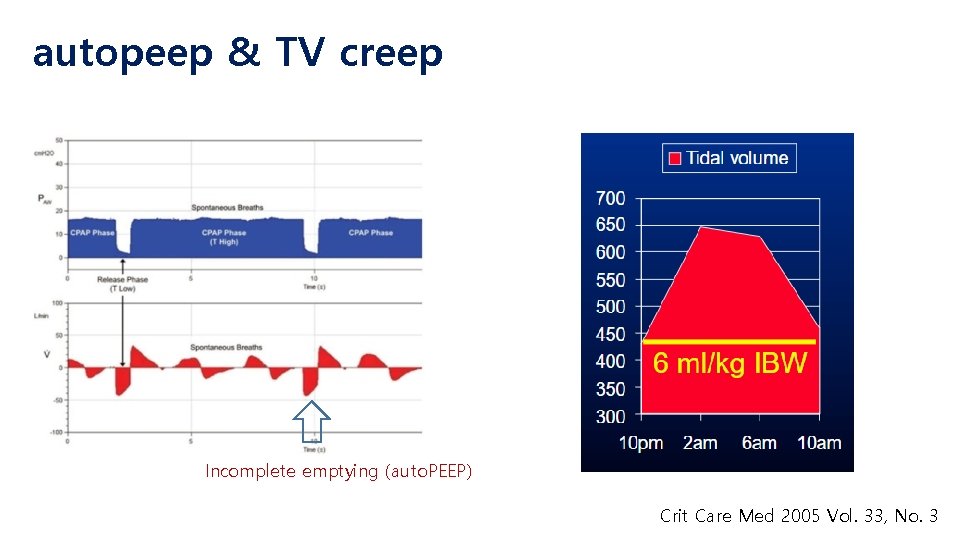
autopeep & TV creep Incomplete emptying (auto. PEEP) Crit Care Med 2005 Vol. 33, No. 3
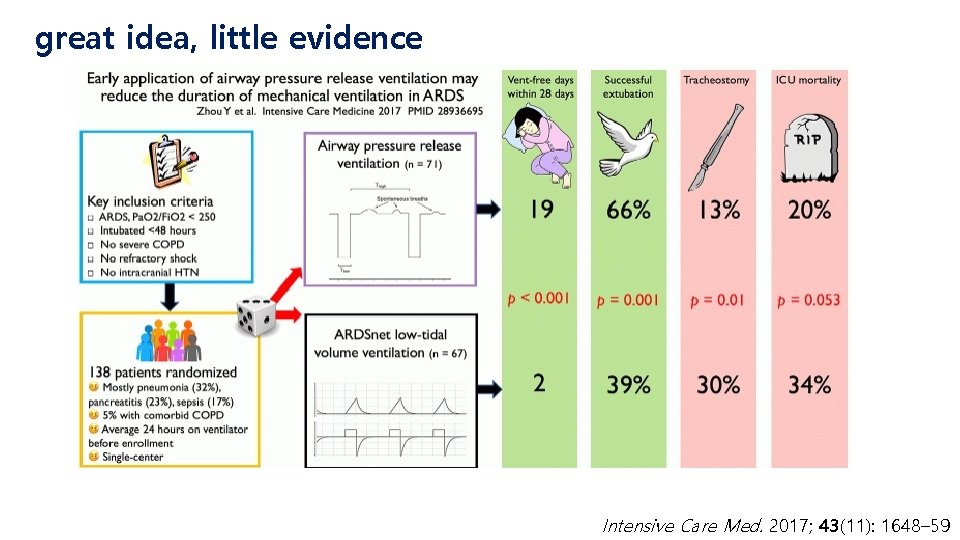
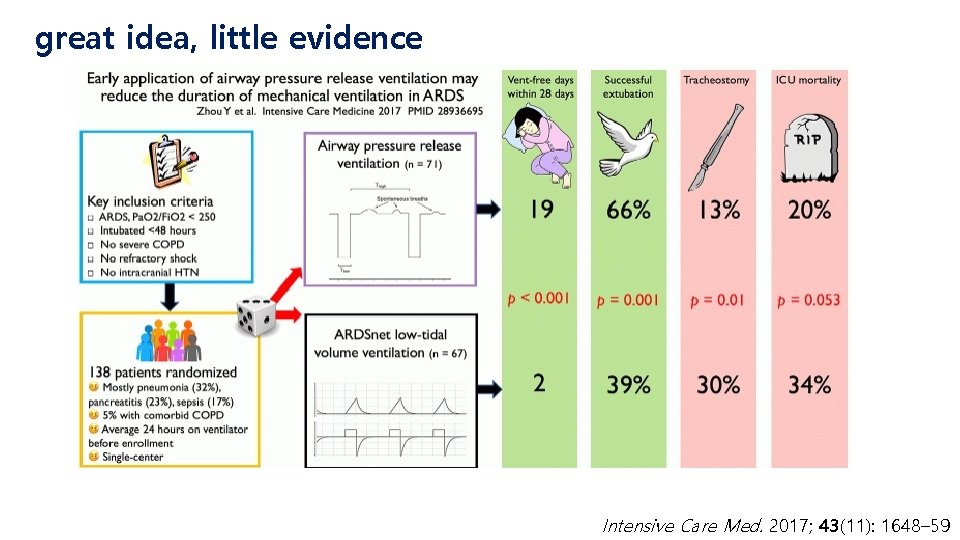
great idea, little evidence Intensive Care Med. 2017; 43(11): 1648– 59
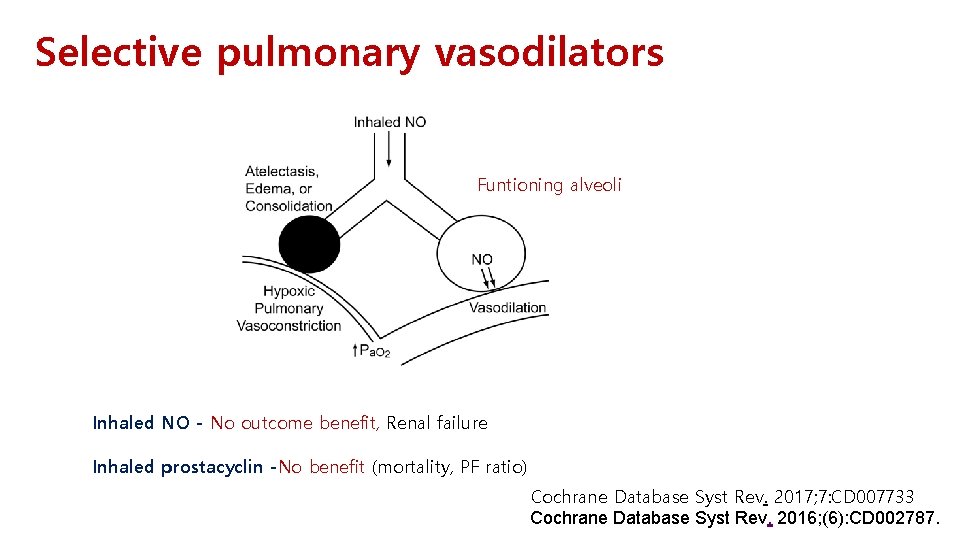
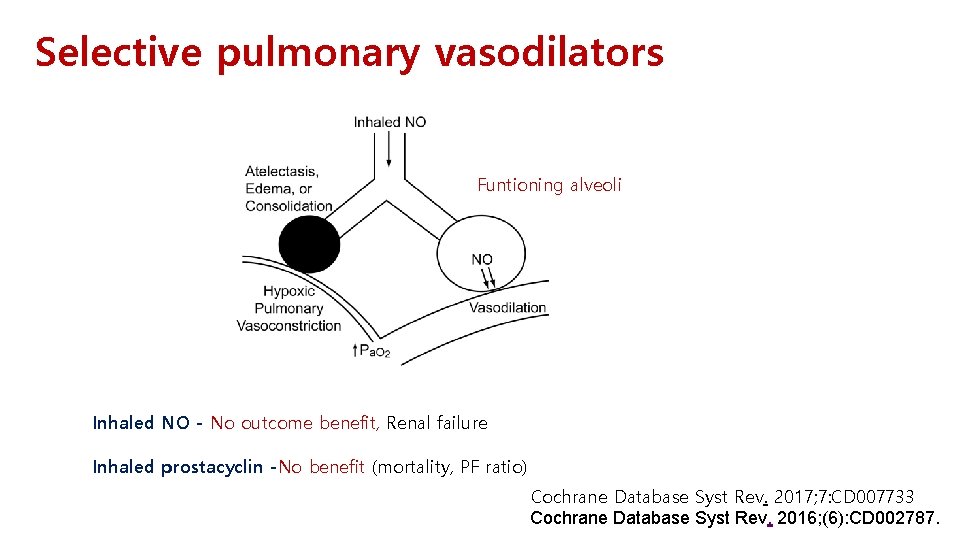
Selective pulmonary vasodilators Funtioning alveoli Inhaled NO - No outcome benefit, Renal failure Inhaled prostacyclin -No benefit (mortality, PF ratio) Cochrane Database Syst Rev. 2017; 7: CD 007733 Cochrane Database Syst Rev. 2016; (6): CD 002787.
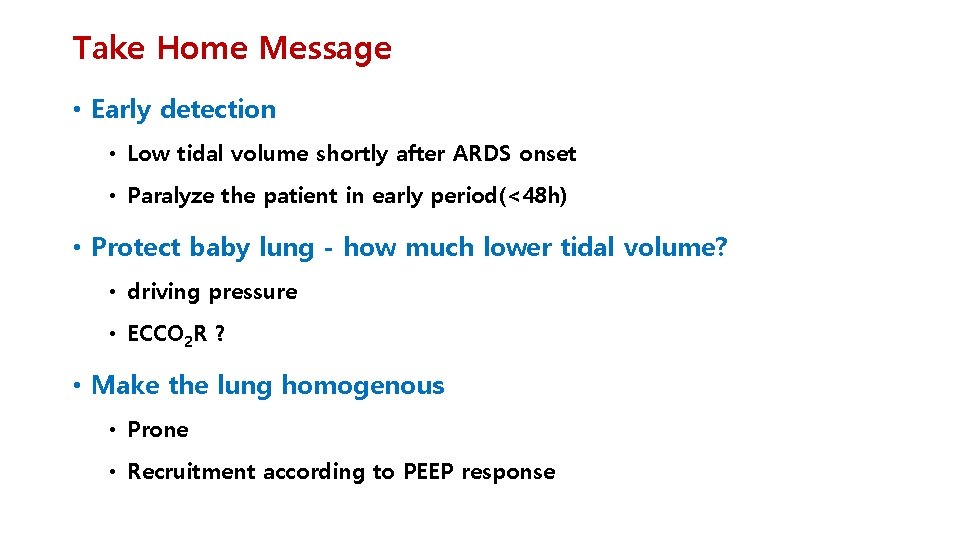
Take Home Message • Early detection • Low tidal volume shortly after ARDS onset • Paralyze the patient in early period(<48 h) • Protect baby lung - how much lower tidal volume? • driving pressure • ECCO 2 R ? • Make the lung homogenous • Prone • Recruitment according to PEEP response
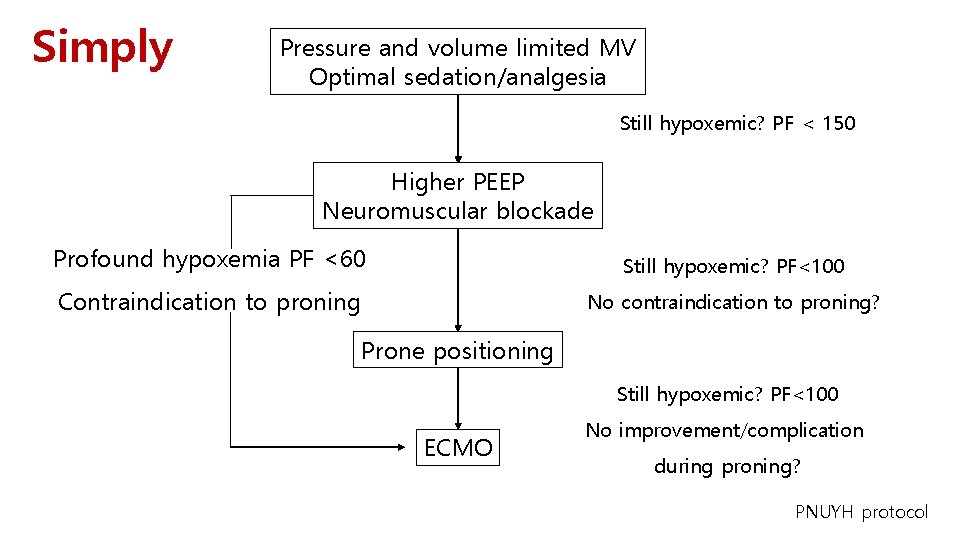
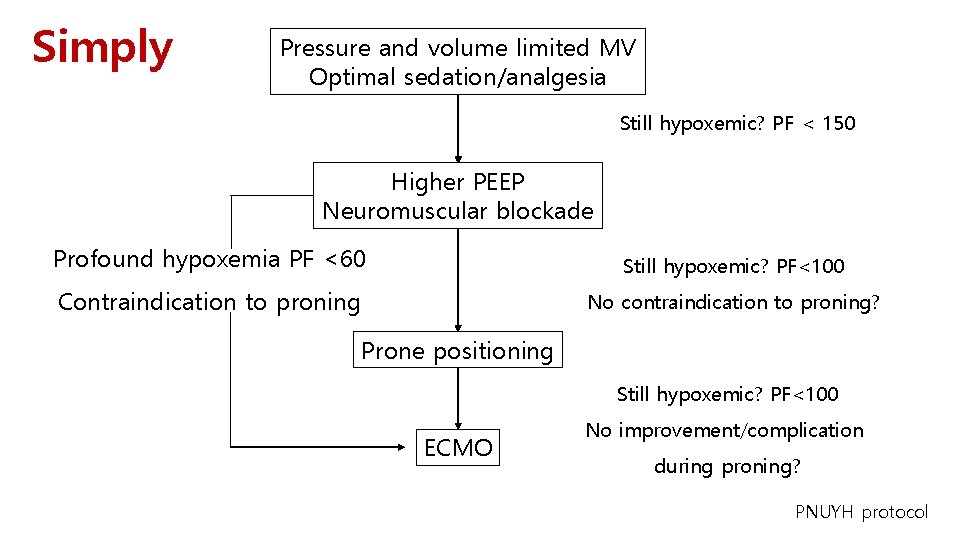
Simply Pressure and volume limited MV Optimal sedation/analgesia Still hypoxemic? PF < 150 Higher PEEP Neuromuscular blockade Profound hypoxemia PF <60 Still hypoxemic? PF<100 Contraindication to proning No contraindication to proning? Prone positioning Still hypoxemic? PF<100 ECMO No improvement/complication during proning? PNUYH protocol

It’s not easy but it’s worth it
Thank you for your attention
 Systematic desensitization therapy
Systematic desensitization therapy Tension diagonal swift water rescue
Tension diagonal swift water rescue Mutlu kartal
Mutlu kartal Ards net
Ards net Berlin definition of ards 2012
Berlin definition of ards 2012 Ards permissive hypercapnia
Ards permissive hypercapnia Ards definition
Ards definition Ards
Ards Ards management
Ards management Ards leczenie
Ards leczenie Ards
Ards Ards
Ards Kryteria berlińskie ards
Kryteria berlińskie ards Biomedical therapies are provided by
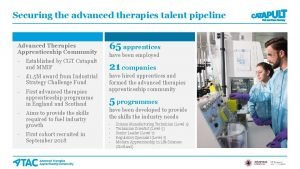
Biomedical therapies are provided by Advanced therapies apprenticeship community
Advanced therapies apprenticeship community Insight therapies involve verbal interactions
Insight therapies involve verbal interactions Pharmacological and parenteral therapies
Pharmacological and parenteral therapies Trafford psychological services
Trafford psychological services Stiriti ayur therapies
Stiriti ayur therapies The biomedical treatment most widely used today is
The biomedical treatment most widely used today is Astellas gene therapies
Astellas gene therapies Chapter 32 complementary and alternative therapies
Chapter 32 complementary and alternative therapies Trafford psychological therapies
Trafford psychological therapies Humanistic therapy aims to
Humanistic therapy aims to Talking therapies westminster
Talking therapies westminster Pvu
Pvu Trafford psychological therapies
Trafford psychological therapies Trafford psychological therapies
Trafford psychological therapies Air therapy in naturopathy ppt
Air therapy in naturopathy ppt Both psychoanalysis and humanistic therapy stress
Both psychoanalysis and humanistic therapy stress Biomedical therapy techniques
Biomedical therapy techniques Bodywork and movement therapies
Bodywork and movement therapies Therapies that directly affect the biological functioning
Therapies that directly affect the biological functioning Acceleration behavioral therapies
Acceleration behavioral therapies Module 73 the biomedical therapies
Module 73 the biomedical therapies Synthetic dividend
Synthetic dividend Long and short division
Long and short division Divide using synthetic division
Divide using synthetic division 369 times 2
369 times 2 Bris för vuxna
Bris för vuxna Mat för unga idrottare
Mat för unga idrottare Gumman cirkel
Gumman cirkel Svenskt ramverk för digital samverkan
Svenskt ramverk för digital samverkan Etik och ledarskap etisk kod för chefer
Etik och ledarskap etisk kod för chefer Datorkunskap för nybörjare
Datorkunskap för nybörjare Fredsgudinnan
Fredsgudinnan Ellika andolf
Ellika andolf Rita perspektiv
Rita perspektiv Kontinuitetshantering
Kontinuitetshantering Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Bästa kameran för astrofoto
Bästa kameran för astrofoto