ACUTE RESPIRATORY DISTRESS SYNDROME ARDS Oea Khairsyaf Acute


- Slides: 23
ACUTE RESPIRATORY DISTRESS SYNDROME ( ARDS ) Oea Khairsyaf
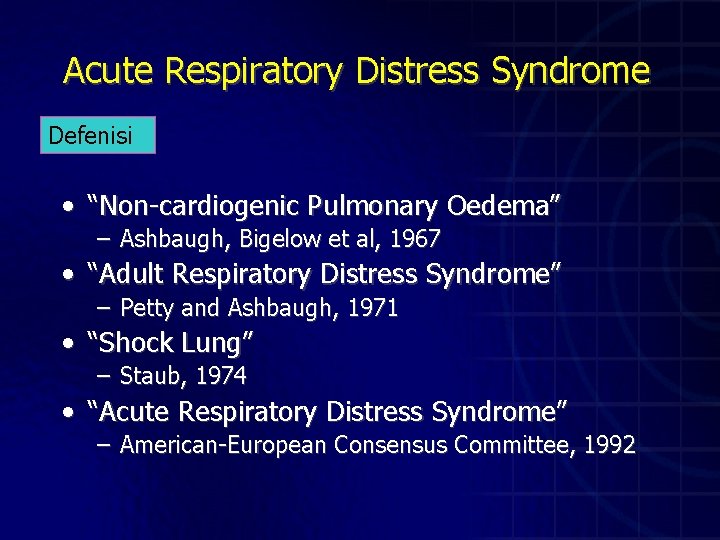
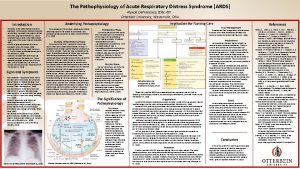
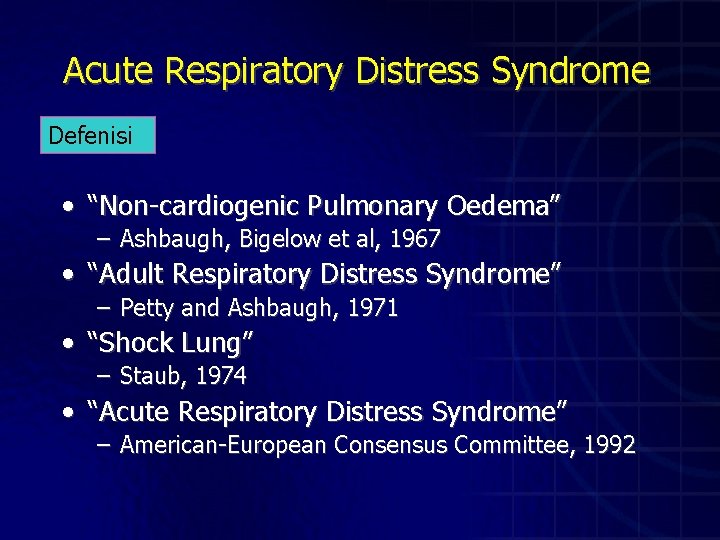
Acute Respiratory Distress Syndrome Defenisi • “Non-cardiogenic Pulmonary Oedema” – Ashbaugh, Bigelow et al, 1967 • “Adult Respiratory Distress Syndrome” – Petty and Ashbaugh, 1971 • “Shock Lung” – Staub, 1974 • “Acute Respiratory Distress Syndrome” – American-European Consensus Committee, 1992
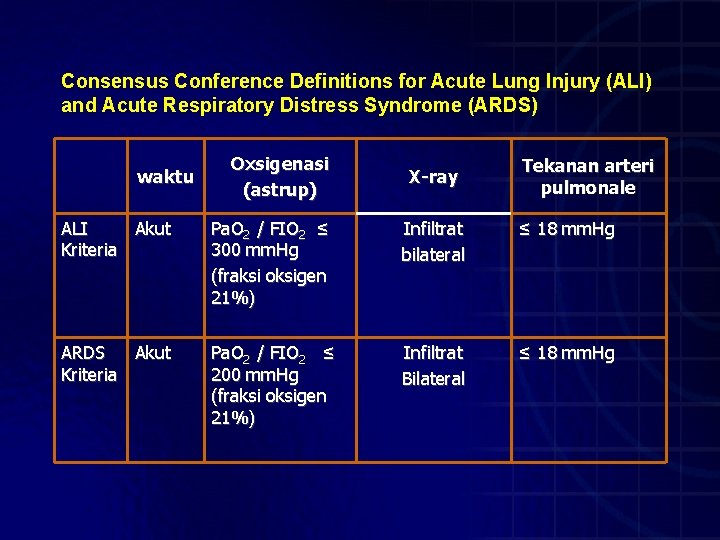
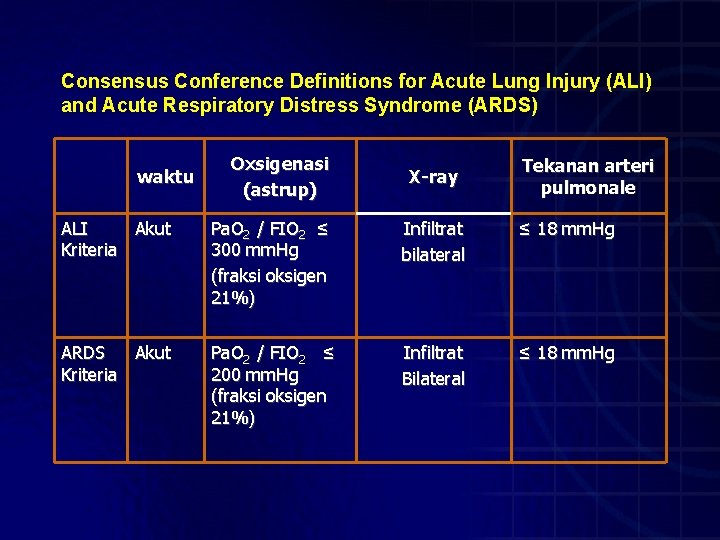
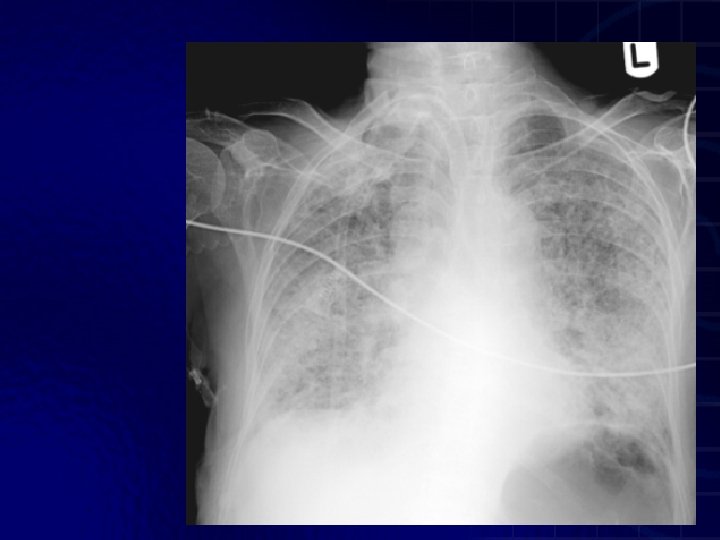
Consensus Conference Definitions for Acute Lung Injury (ALI) and Acute Respiratory Distress Syndrome (ARDS) waktu Oxsigenasi (astrup) X-ray Tekanan arteri pulmonale ALI Akut Kriteria Pa. O 2 / FIO 2 ≤ 300 mm. Hg (fraksi oksigen 21%) Infiltrat bilateral ≤ 18 mm. Hg ARDS Akut Kriteria Pa. O 2 / FIO 2 ≤ 200 mm. Hg (fraksi oksigen 21%) Infiltrat Bilateral ≤ 18 mm. Hg
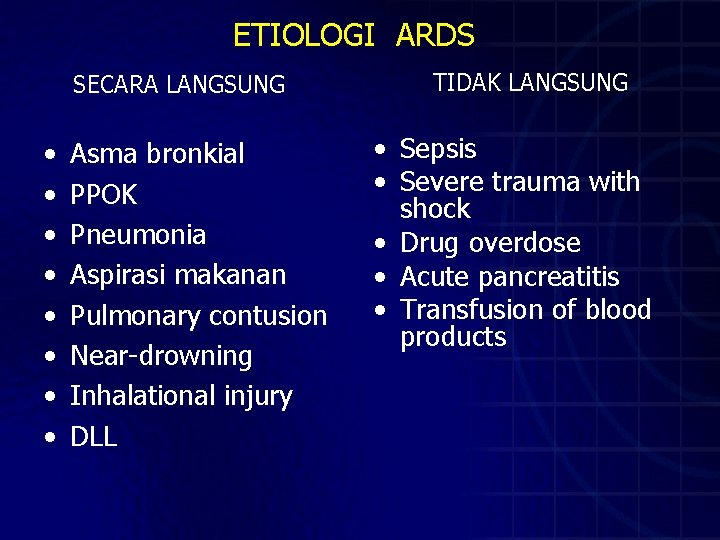
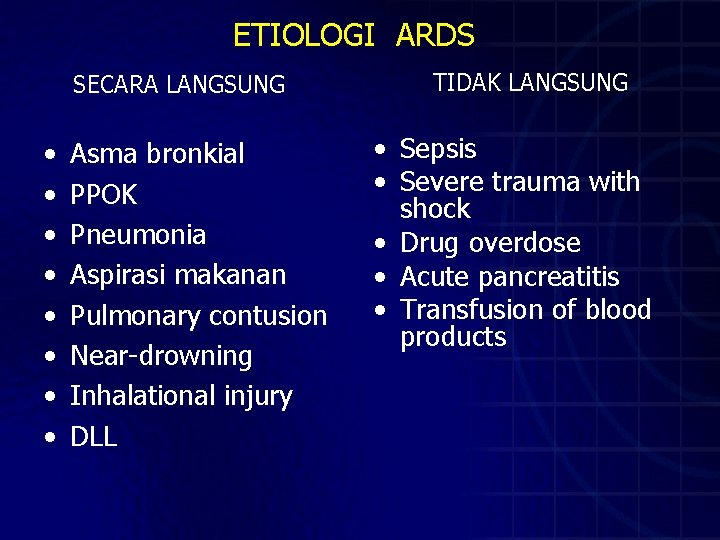
ETIOLOGI ARDS SECARA LANGSUNG • • Asma bronkial PPOK Pneumonia Aspirasi makanan Pulmonary contusion Near-drowning Inhalational injury DLL TIDAK LANGSUNG • Sepsis • Severe trauma with shock • Drug overdose • Acute pancreatitis • Transfusion of blood products
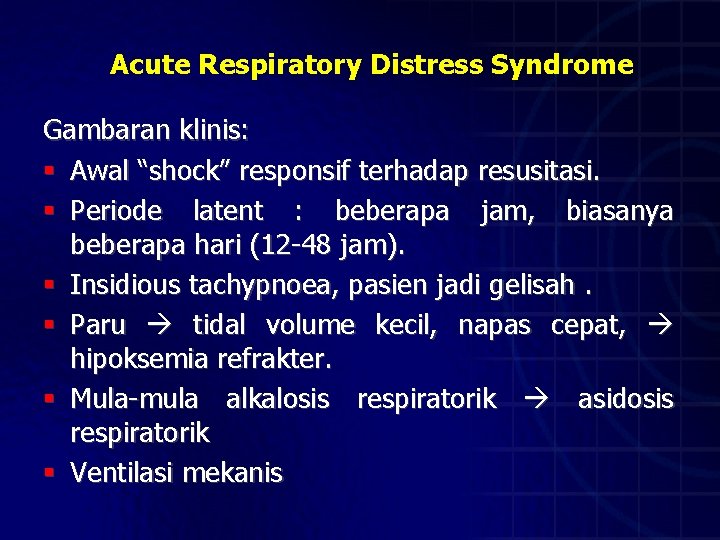
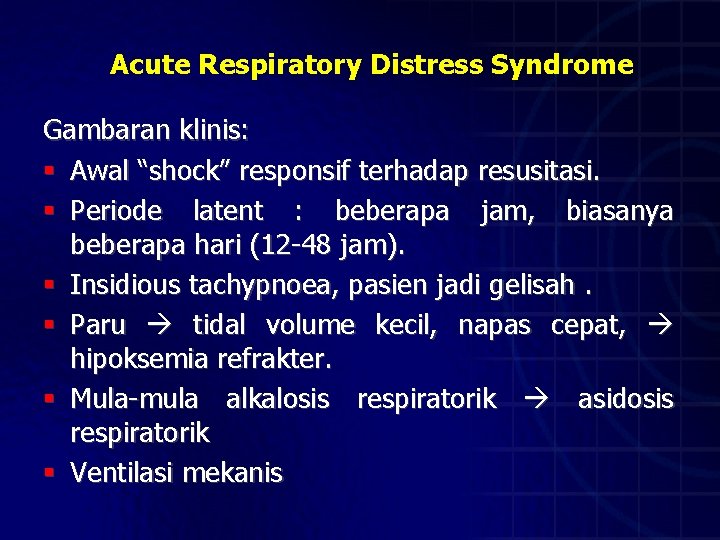
Acute Respiratory Distress Syndrome Gambaran klinis: § Awal “shock” responsif terhadap resusitasi. § Periode latent : beberapa jam, biasanya beberapa hari (12 -48 jam). § Insidious tachypnoea, pasien jadi gelisah. § Paru tidal volume kecil, napas cepat, hipoksemia refrakter. § Mula-mula alkalosis respiratorik asidosis respiratorik § Ventilasi mekanis
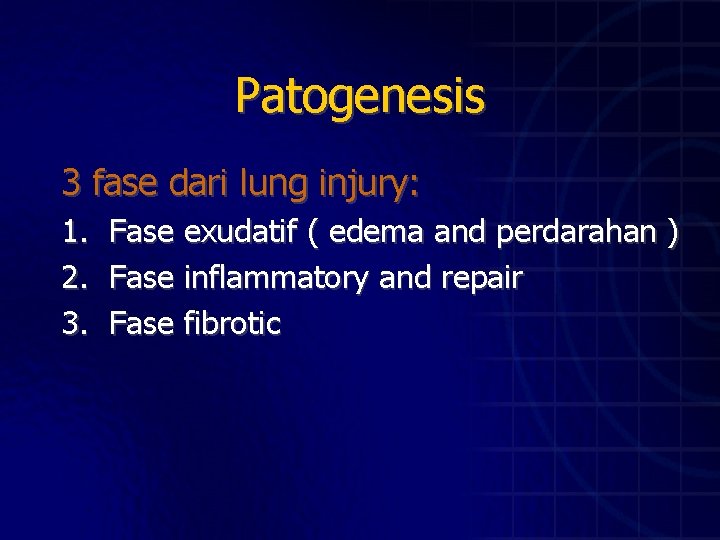
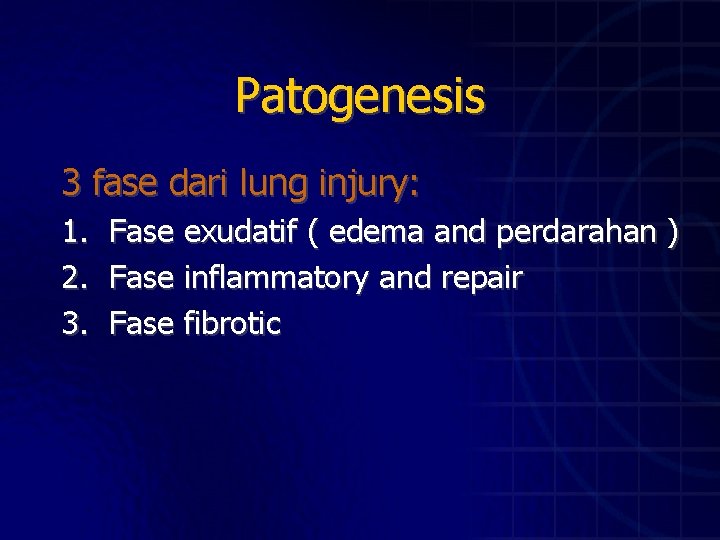
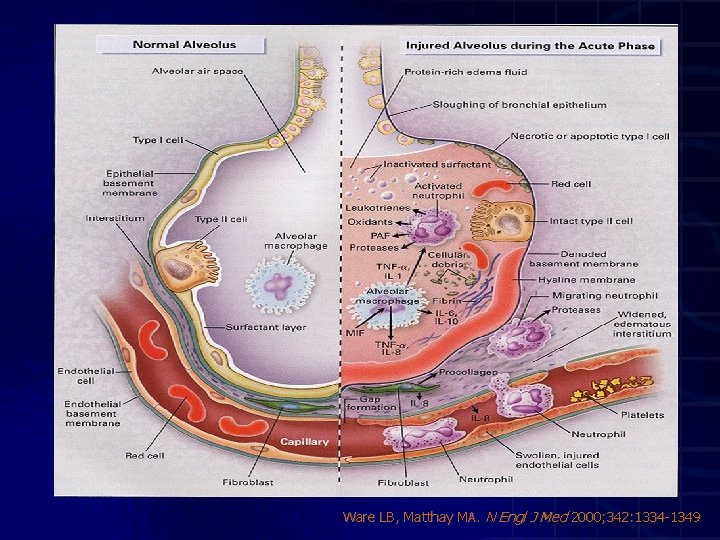
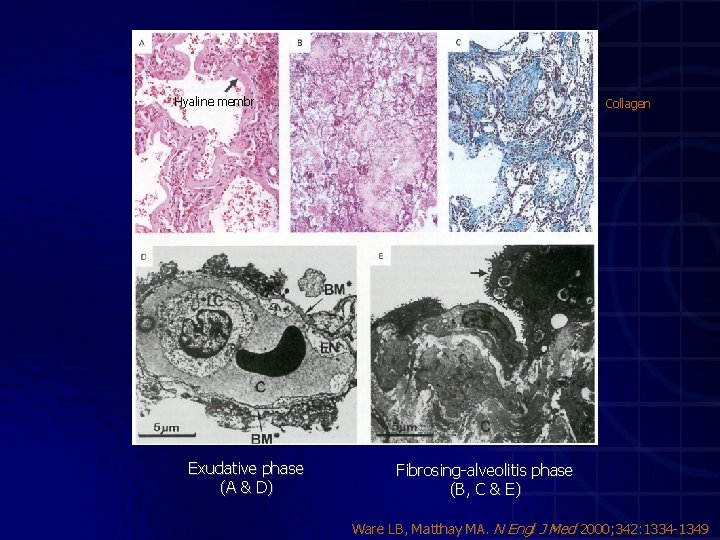
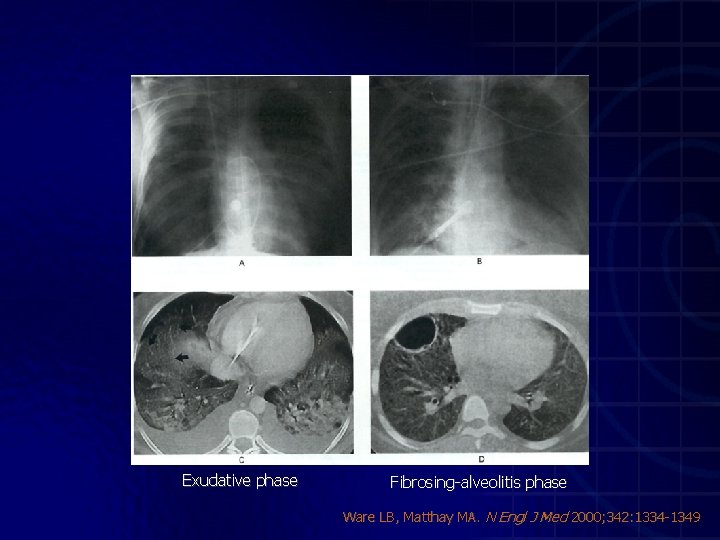
Patogenesis 3 fase dari lung injury: 1. Fase exudatif ( edema and perdarahan ) 2. Fase inflammatory and repair 3. Fase fibrotic
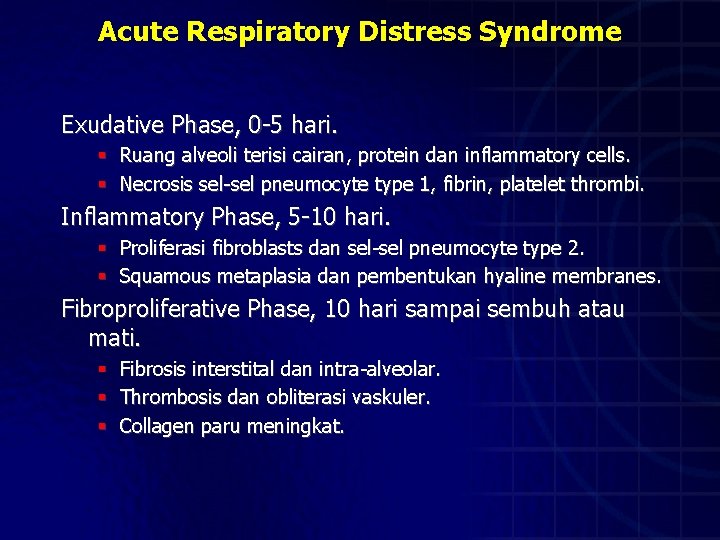
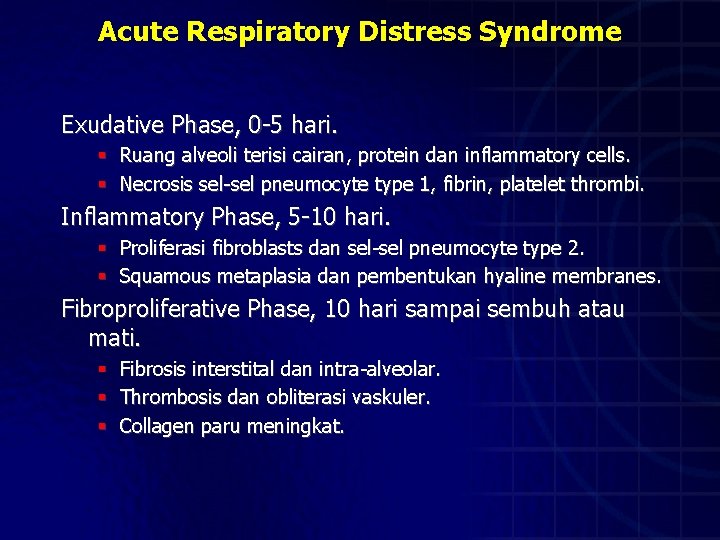
Acute Respiratory Distress Syndrome Exudative Phase, 0 -5 hari. § Ruang alveoli terisi cairan, protein dan inflammatory cells. § Necrosis sel-sel pneumocyte type 1, fibrin, platelet thrombi. Inflammatory Phase, 5 -10 hari. § Proliferasi fibroblasts dan sel-sel pneumocyte type 2. § Squamous metaplasia dan pembentukan hyaline membranes. Fibroproliferative Phase, 10 hari sampai sembuh atau mati. § § § Fibrosis interstital dan intra-alveolar. Thrombosis dan obliterasi vaskuler. Collagen paru meningkat.
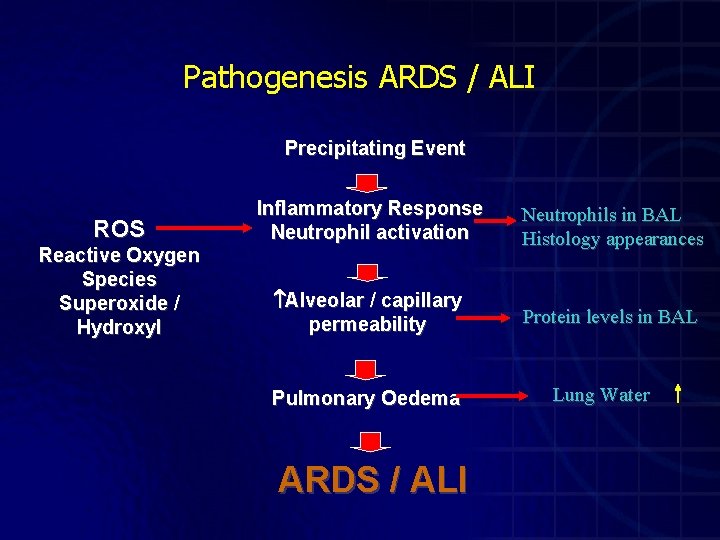
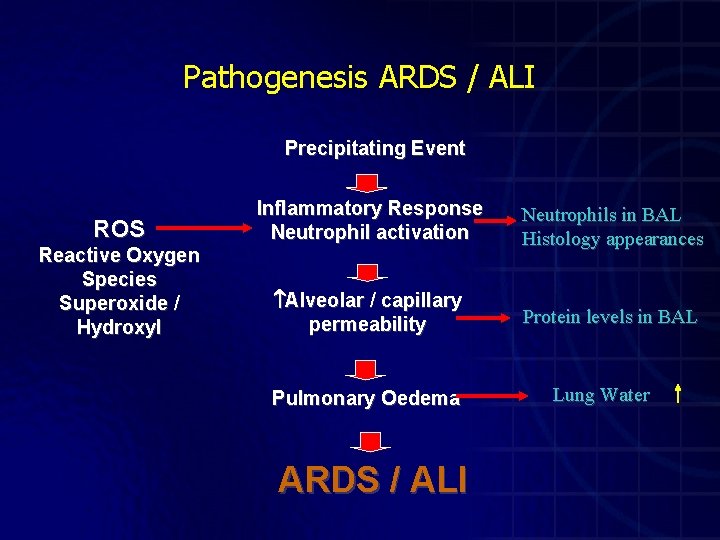
Pathogenesis ARDS / ALI Precipitating Event ROS Reactive Oxygen Species Superoxide / Hydroxyl Inflammatory Response Neutrophil activation Neutrophils in BAL Histology appearances Alveolar / capillary permeability Protein levels in BAL Pulmonary Oedema ARDS / ALI Lung Water
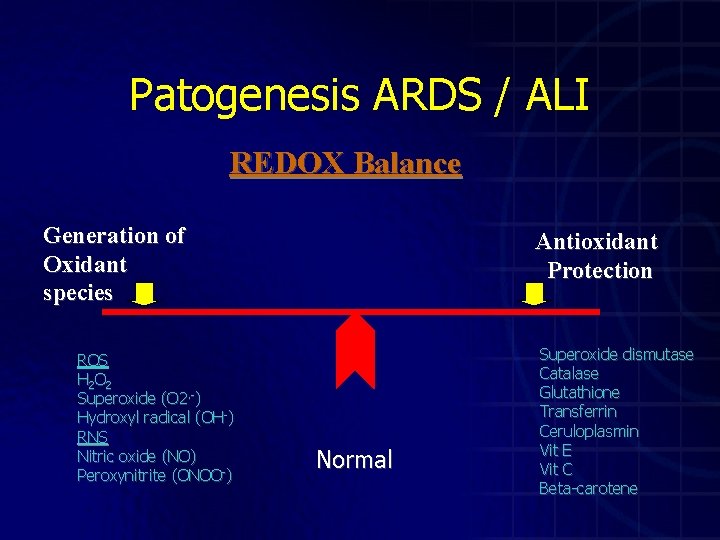
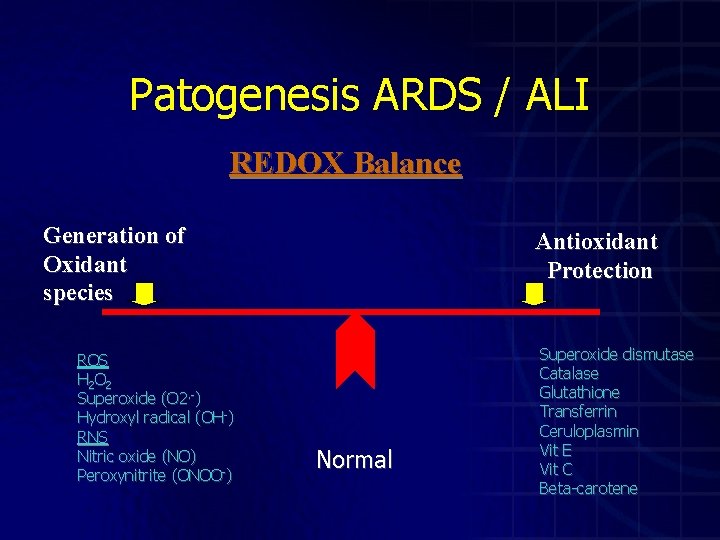
Patogenesis ARDS / ALI REDOX Balance Generation of Oxidant species ROS H 2 O 2 Superoxide (O 2. -) Hydroxyl radical (OH-) RNS Nitric oxide (NO) Peroxynitrite (ONOO-) Antioxidant Protection Normal Superoxide dismutase Catalase Glutathione Transferrin Ceruloplasmin Vit E Vit C Beta-carotene
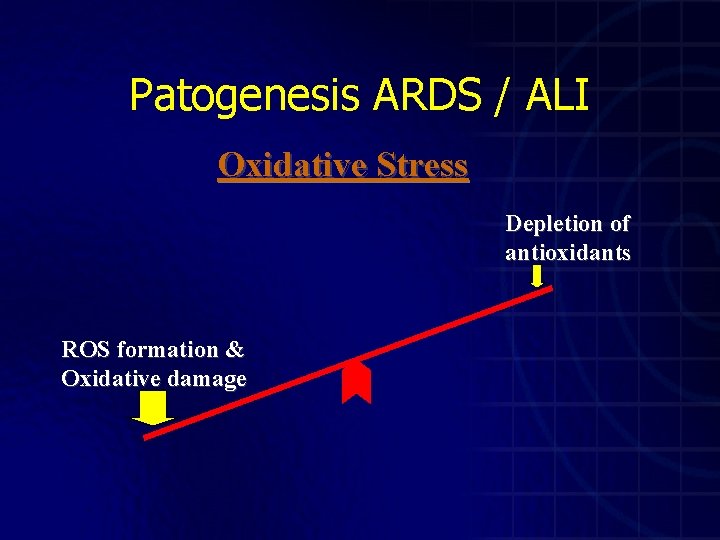
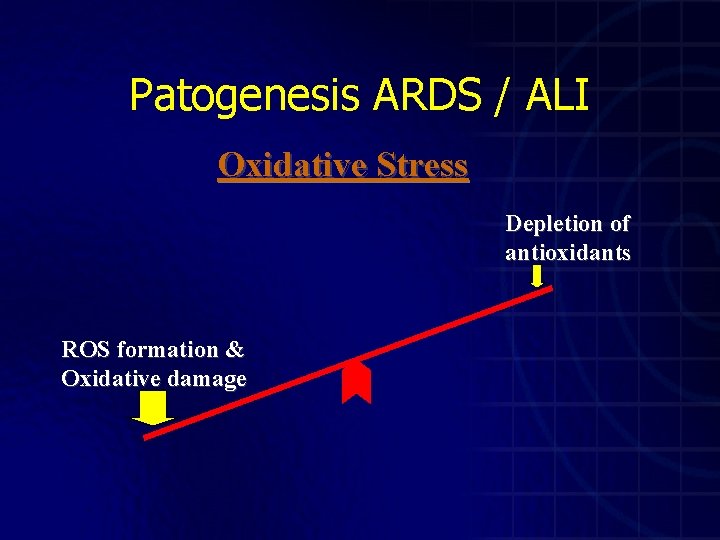
Patogenesis ARDS / ALI Oxidative Stress Depletion of antioxidants ROS formation & Oxidative damage
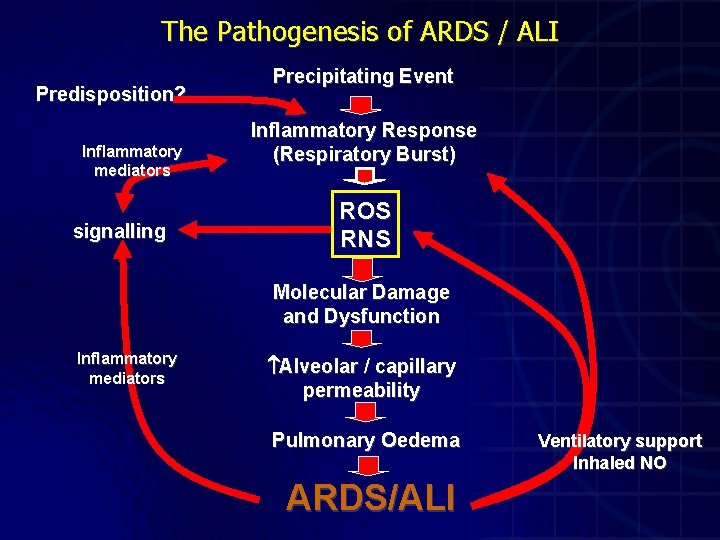
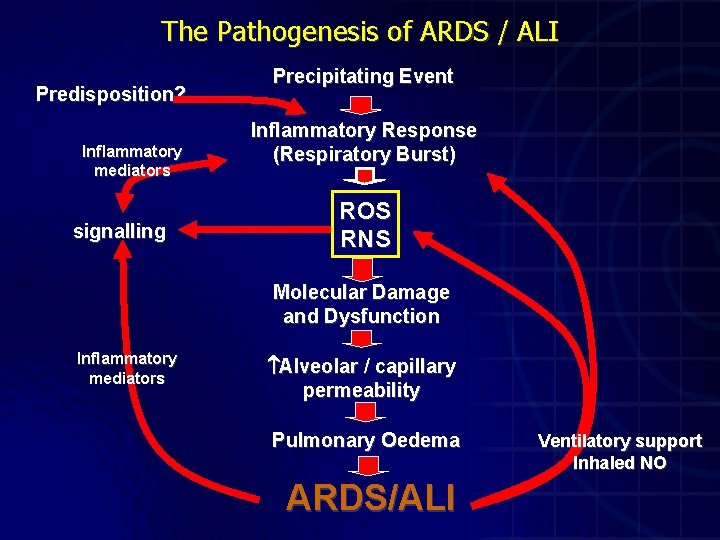
The Pathogenesis of ARDS / ALI Predisposition? Inflammatory mediators signalling Precipitating Event Inflammatory Response (Respiratory Burst) ROS RNS Molecular Damage and Dysfunction Inflammatory mediators Alveolar / capillary permeability Pulmonary Oedema ARDS/ALI Ventilatory support Inhaled NO
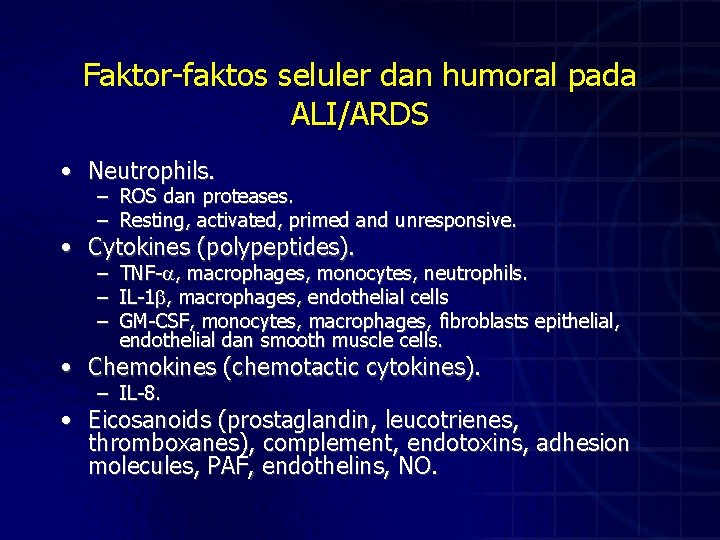
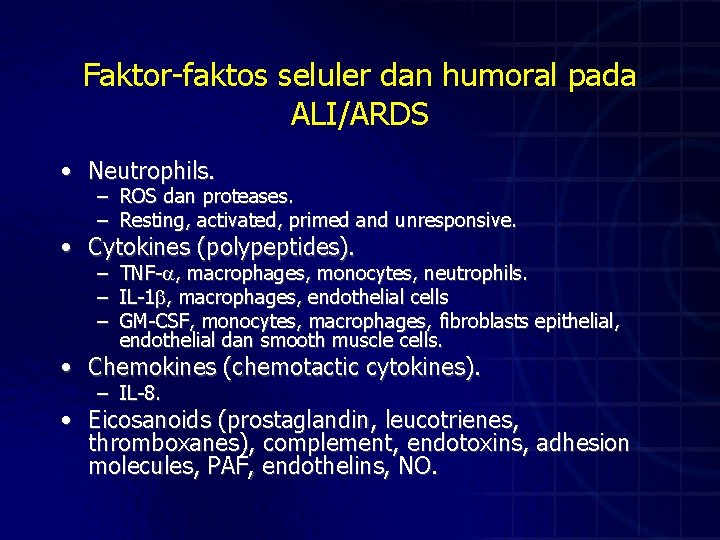
Faktor-faktos seluler dan humoral pada ALI/ARDS • Neutrophils. – – ROS dan proteases. Resting, activated, primed and unresponsive. – – – TNF- , macrophages, monocytes, neutrophils. IL-1 , macrophages, endothelial cells GM-CSF, monocytes, macrophages, fibroblasts epithelial, endothelial dan smooth muscle cells. • Cytokines (polypeptides). • Chemokines (chemotactic cytokines). – IL-8. • Eicosanoids (prostaglandin, leucotrienes, thromboxanes), complement, endotoxins, adhesion molecules, PAF, endothelins, NO.
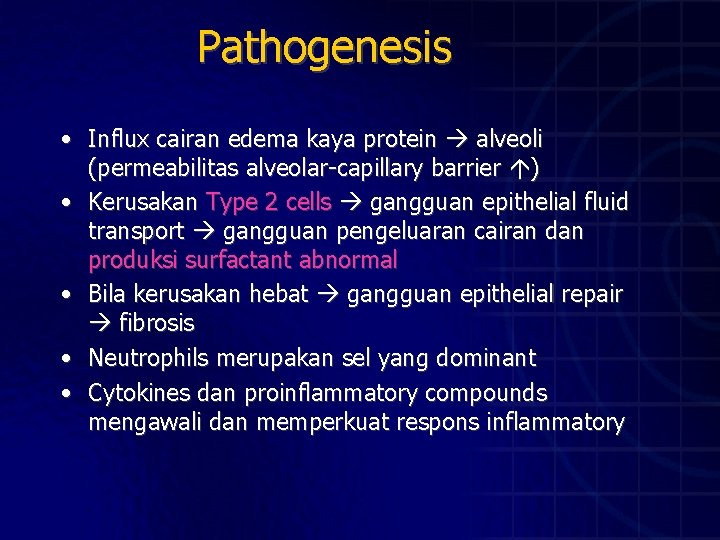
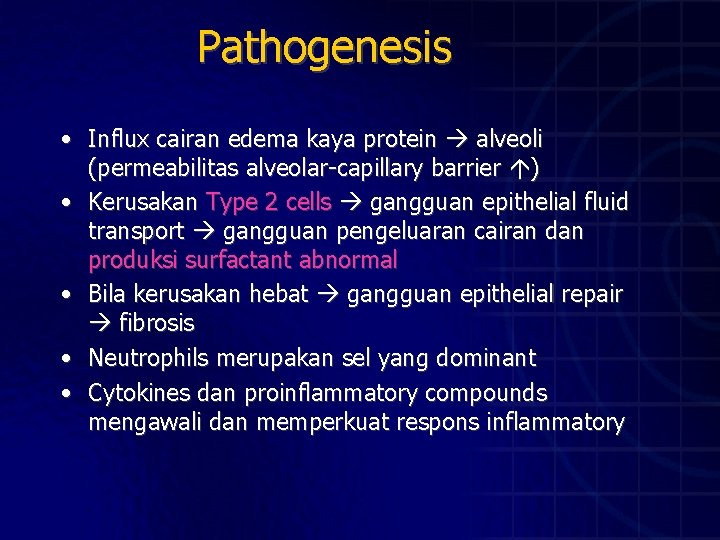
Pathogenesis • Influx cairan edema kaya protein alveoli (permeabilitas alveolar-capillary barrier ) • Kerusakan Type 2 cells gangguan epithelial fluid transport gangguan pengeluaran cairan dan produksi surfactant abnormal • Bila kerusakan hebat gangguan epithelial repair fibrosis • Neutrophils merupakan sel yang dominant • Cytokines dan proinflammatory compounds mengawali dan memperkuat respons inflammatory
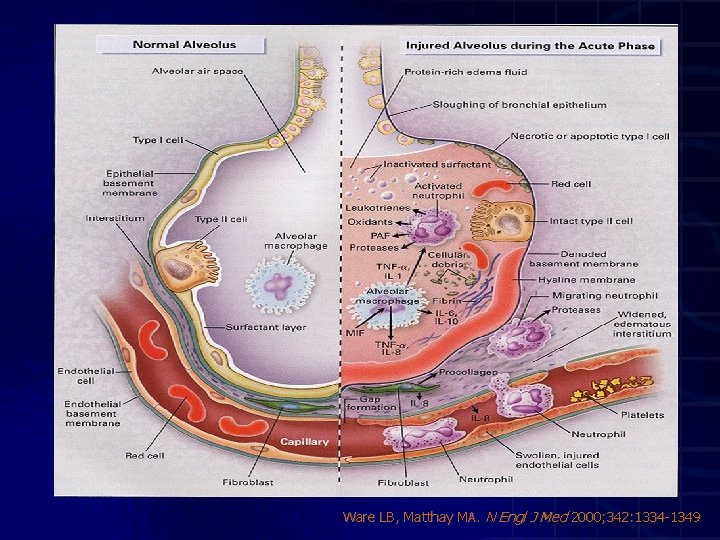
Ware LB, Matthay MA. N Engl J Med 2000; 342: 1334 -1349
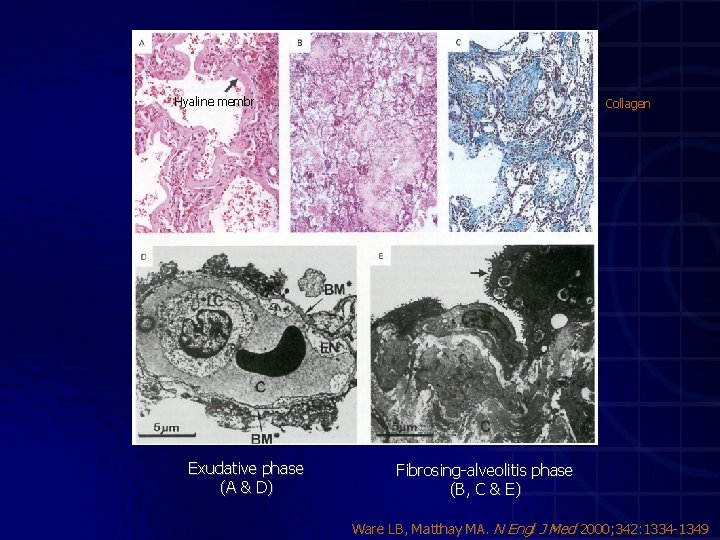
Hyaline membr Exudative phase (A & D) Collagen Fibrosing-alveolitis phase (B, C & E) Ware LB, Matthay MA. N Engl J Med 2000; 342: 1334 -1349
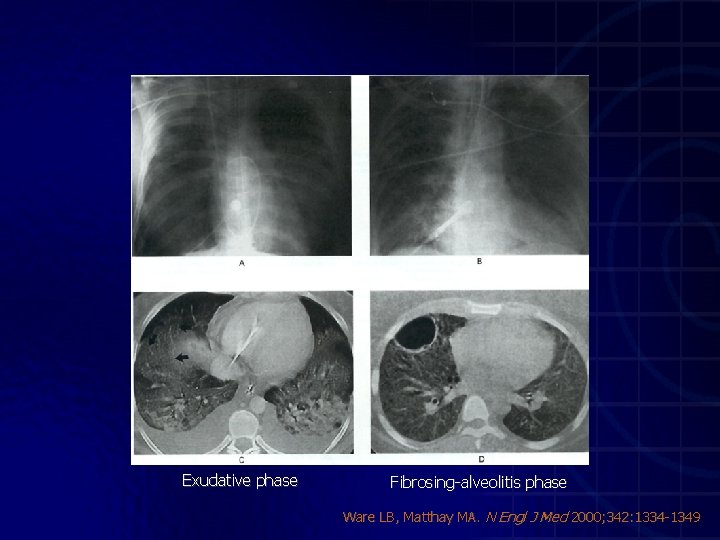
Exudative phase Fibrosing-alveolitis phase Ware LB, Matthay MA. N Engl J Med 2000; 342: 1334 -1349
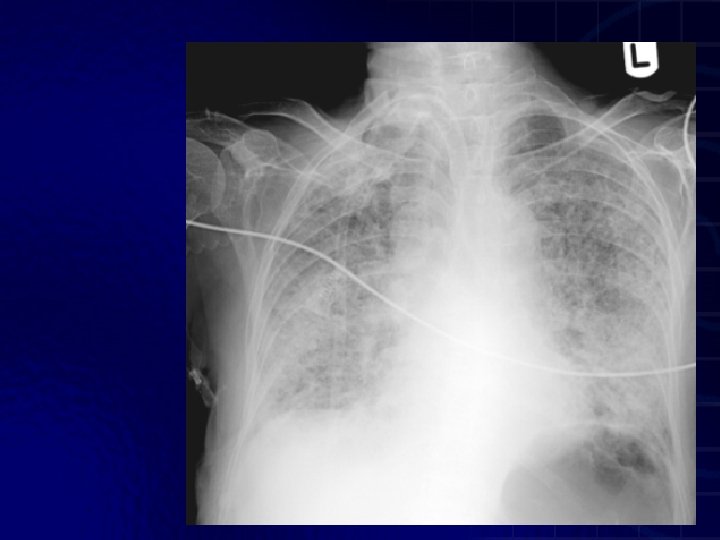
ARDS
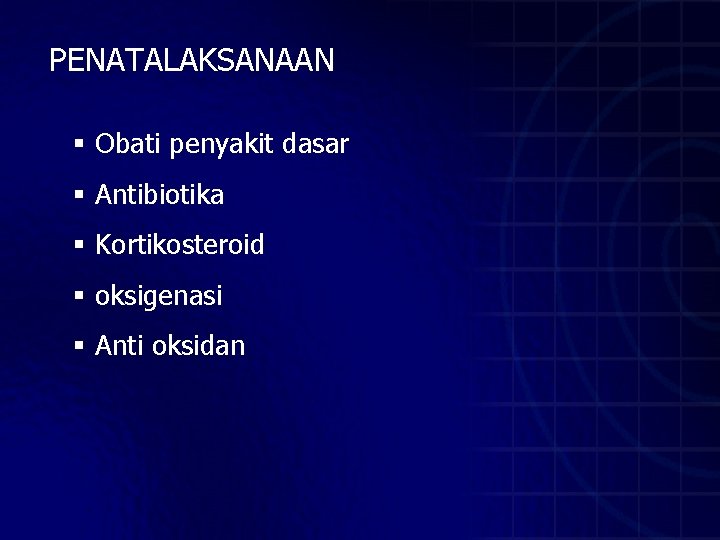
PENATALAKSANAAN § Obati penyakit dasar § Antibiotika § Kortikosteroid § oksigenasi § Anti oksidan
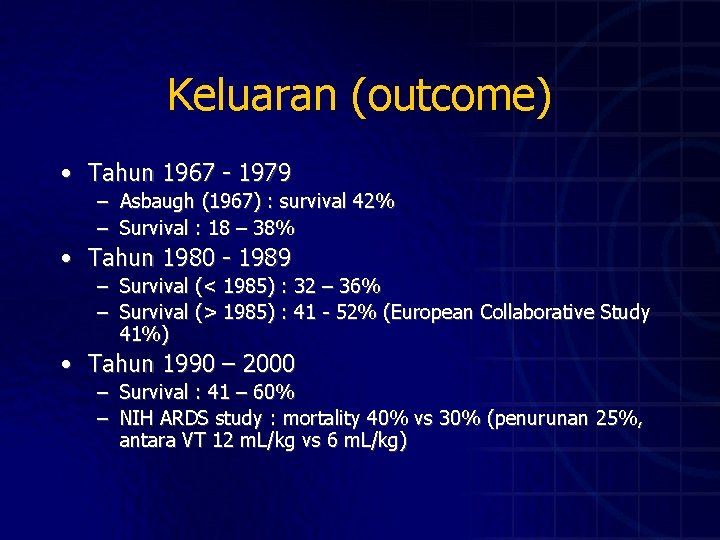
Keluaran (outcome) • Tahun 1967 - 1979 – Asbaugh (1967) : survival 42% – Survival : 18 – 38% • Tahun 1980 - 1989 – Survival (< 1985) : 32 – 36% – Survival (> 1985) : 41 - 52% (European Collaborative Study 41%) • Tahun 1990 – 2000 – Survival : 41 – 60% – NIH ARDS study : mortality 40% vs 30% (penurunan 25%, antara VT 12 m. L/kg vs 6 m. L/kg)
Outcome Jangka Panjang pada Survivors (1 -1, 5 tahun pasca ARDS) Sequelae pulmoner Majoritas, fungsi paru kembali hampir normal Gangguan residual: • • • restrictive ventilatory defect (biasanya ringan), Hipertensi pulmoner (ringan), airflow limitation ( bronchial hyperactivity) Gangguan pada exercise testing lebih bermakna (setara pasien COPD berat) Derajat gangguan ~ umur, riwayat merokok, ventlasi mekanis berkepanjangan
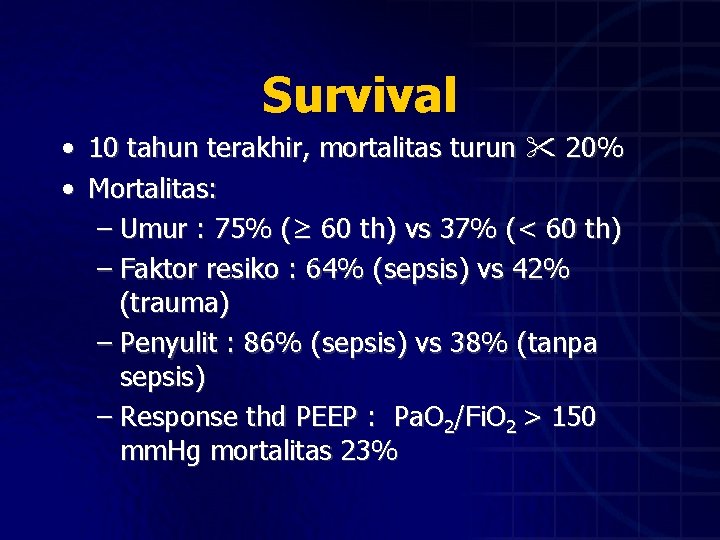
Survival • 10 tahun terakhir, mortalitas turun 20% • Mortalitas: – Umur : 75% (≥ 60 th) vs 37% (< 60 th) – Faktor resiko : 64% (sepsis) vs 42% (trauma) – Penyulit : 86% (sepsis) vs 38% (tanpa sepsis) – Response thd PEEP : Pa. O 2/Fi. O 2 > 150 mm. Hg mortalitas 23%

TERIMA KASIH

 Respiratory distress
Respiratory distress Respiratory distress
Respiratory distress Respiratory distress nasal flaring
Respiratory distress nasal flaring Ards
Ards Kryteria berlińskie ards
Kryteria berlińskie ards Prof dr cem yıldırım
Prof dr cem yıldırım Ards net
Ards net Ardsnet protocol
Ardsnet protocol Ards permissive hypercapnia
Ards permissive hypercapnia Ards definition
Ards definition Ards
Ards Ards management
Ards management Krzywa dysocjacji oksyhemoglobiny
Krzywa dysocjacji oksyhemoglobiny Ards
Ards What is the conducting zone of the respiratory system
What is the conducting zone of the respiratory system Acute upper respiratory infection unspecified คือ
Acute upper respiratory infection unspecified คือ Acute coronary syndrome
Acute coronary syndrome Acute radiation syndrome
Acute radiation syndrome Firas mussa
Firas mussa Oea jupas sample
Oea jupas sample Oea choice trust
Oea choice trust Preterito y copreterito
Preterito y copreterito Jupas slp sample
Jupas slp sample Obrm login
Obrm login