Hypoxia Respiratory Failure and Altered Mental Status Alicia







- Slides: 58
Hypoxia, Respiratory Failure and Altered Mental Status Alicia M. Mohr, MD Surgical Fundamentals Session 2 July 21, 2006
Objectives • To learn a logical method for determining the nature of respiratory failure and its treatment • To determine if a patient requires intubation and ventilation • To learn the differential diagnosis and treatment of altered mental status
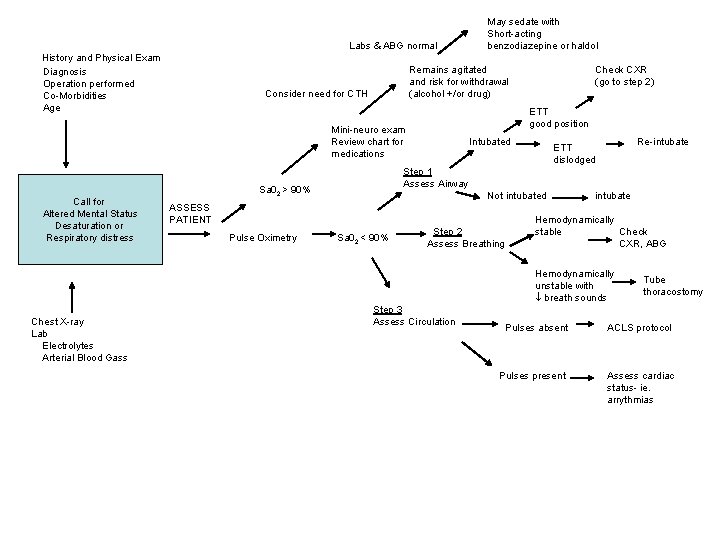
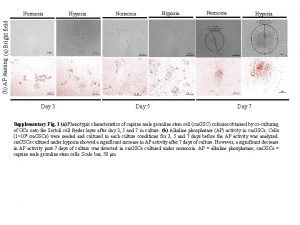
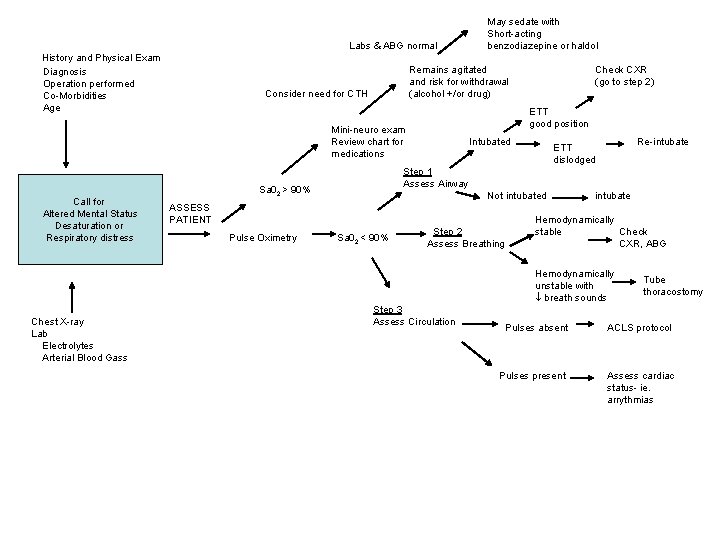
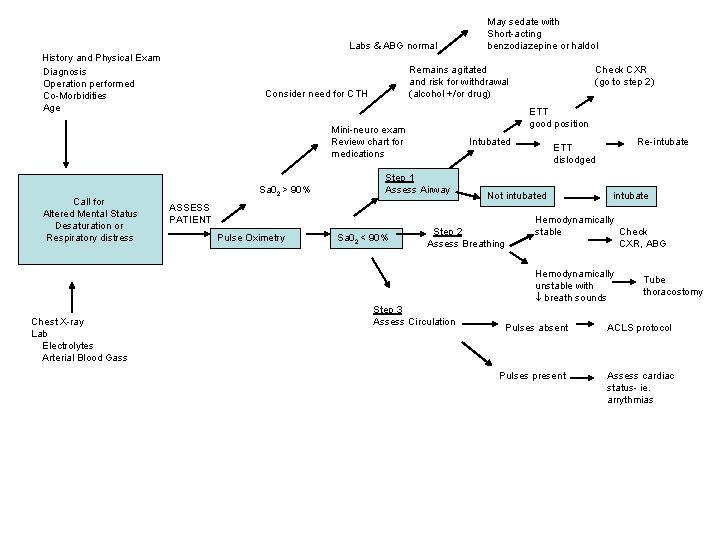
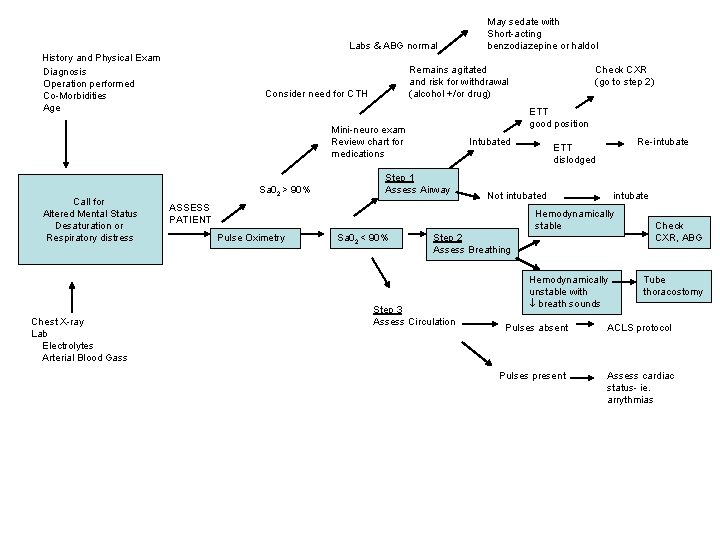
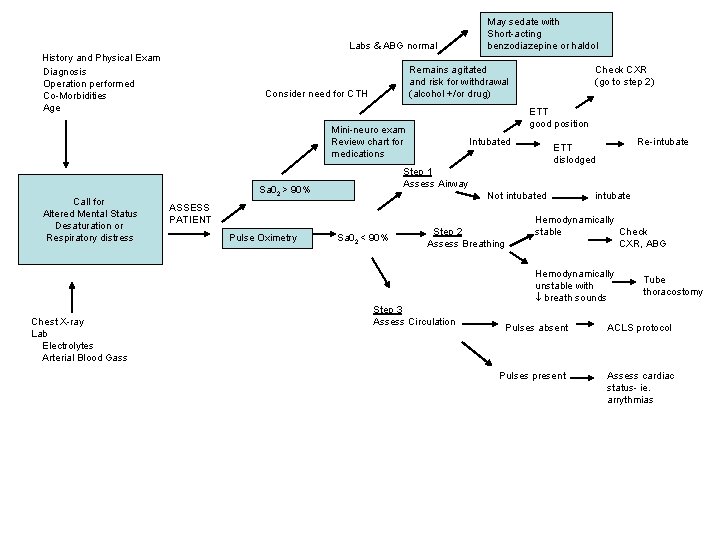
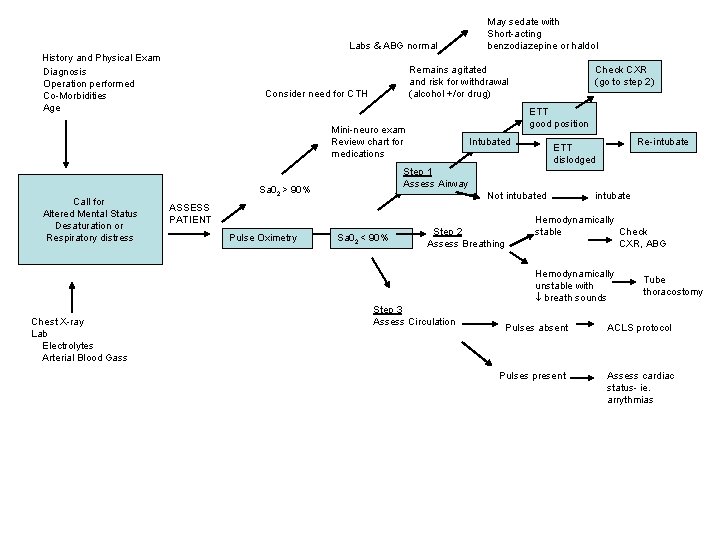
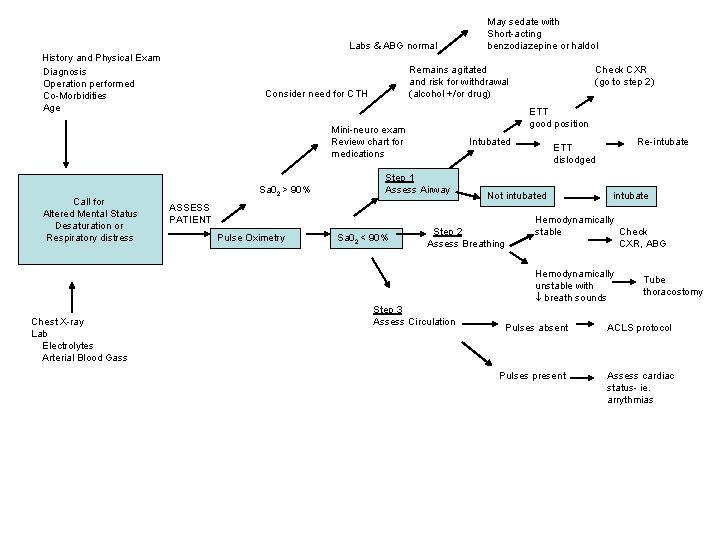
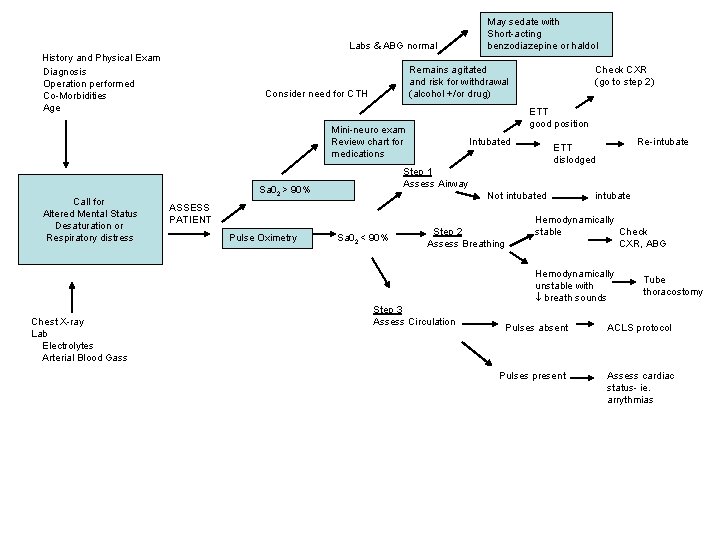
Labs & ABG normal History and Physical Exam Diagnosis Operation performed Co-Morbidities Age Remains agitated and risk for withdrawal (alcohol +/or drug) Consider need for CTH Intubated Re-intubate ETT dislodged Step 1 Assess Airway Sa 02 > 90% Not intubated ASSESS PATIENT Pulse Oximetry Check CXR (go to step 2) ETT good position Mini-neuro exam Review chart for medications Call for Altered Mental Status Desaturation or Respiratory distress May sedate with Short-acting benzodiazepine or haldol Sa 02 < 90% Step 2 Assess Breathing intubate Hemodynamically stable Check CXR, ABG Hemodynamically unstable with breath sounds Chest X-ray Lab Electrolytes Arterial Blood Gass Step 3 Assess Circulation Tube thoracostomy Pulses absent ACLS protocol Pulses present Assess cardiac status- ie. arrythmias
History
History • • Can’t catch my breath Lightedheadedness Usually acute onset Minimal symptoms
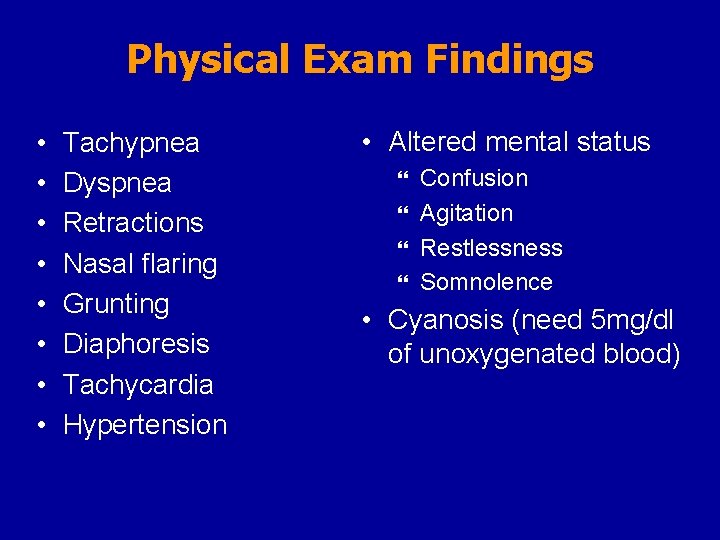
Physical Exam Findings
Physical Exam Findings • • Tachypnea Dyspnea Retractions Nasal flaring Grunting Diaphoresis Tachycardia Hypertension • Altered mental status Confusion } Agitation } Restlessness } Somnolence } • Cyanosis (need 5 mg/dl of unoxygenated blood)
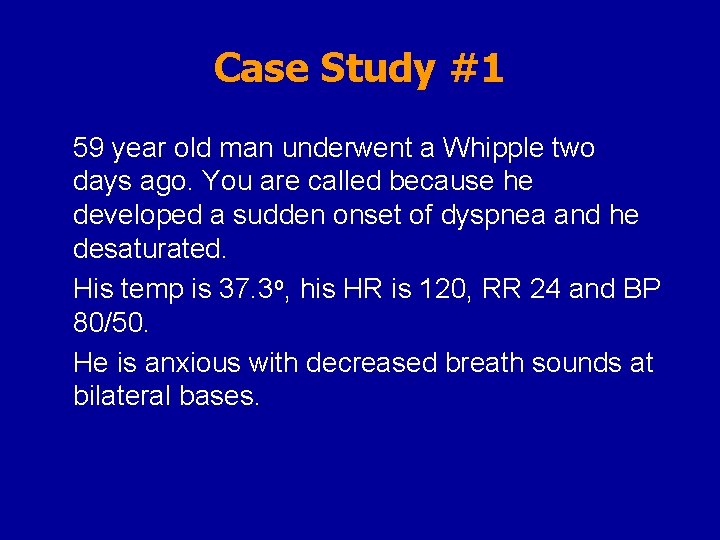
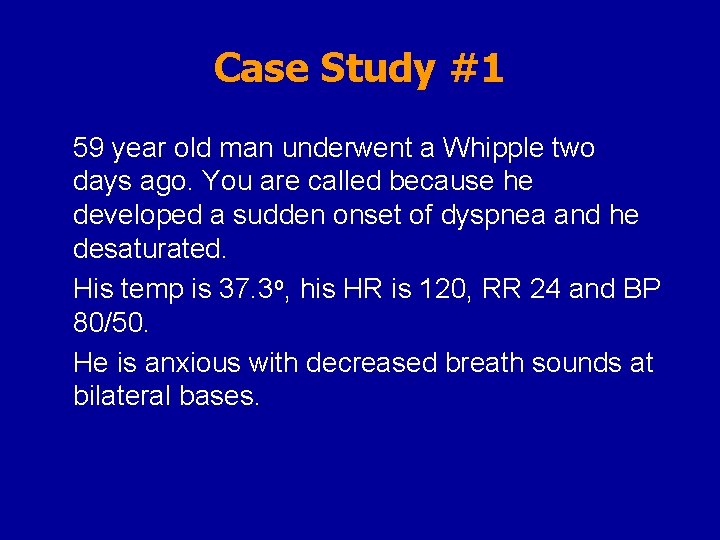
Case Study #1 59 year old man underwent a Whipple two days ago. You are called because he developed a sudden onset of dyspnea and he desaturated. His temp is 37. 3 o, his HR is 120, RR 24 and BP 80/50. He is anxious with decreased breath sounds at bilateral bases.
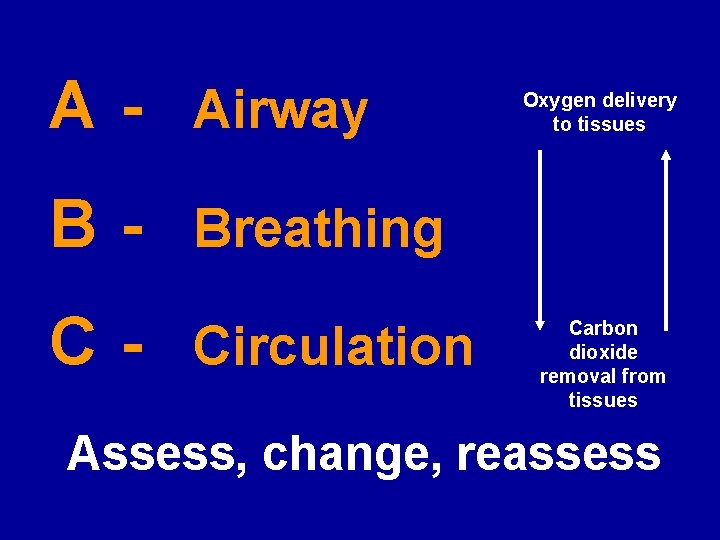
A - Airway Oxygen delivery to tissues B - Breathing C - Circulation Carbon dioxide removal from tissues Assess, change, reassess
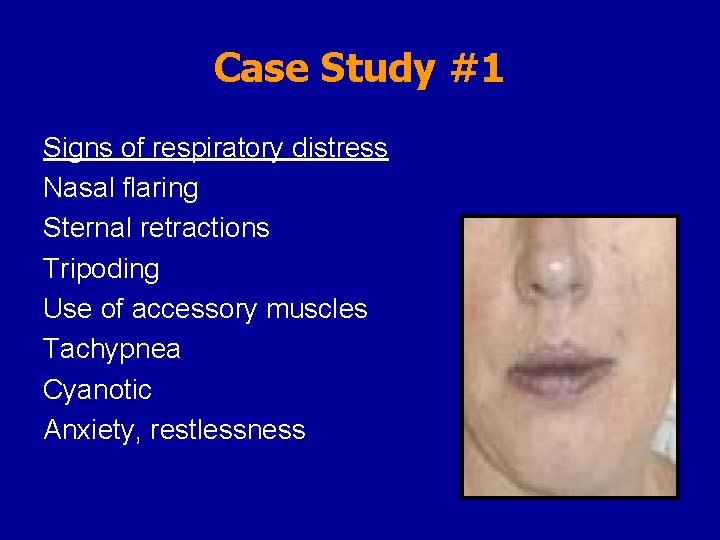
Case Study #1 Signs of respiratory distress Nasal flaring Sternal retractions Tripoding Use of accessory muscles Tachypnea Cyanotic Anxiety, restlessness
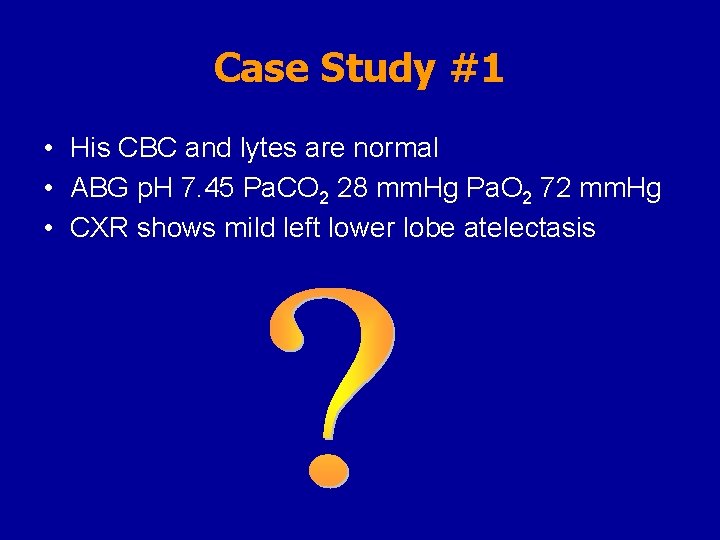
Case Study #1 • His CBC and lytes are normal • ABG p. H 7. 45 Pa. CO 2 28 mm. Hg Pa. O 2 72 mm. Hg • CXR shows mild left lower lobe atelectasis
Indications for Intubation
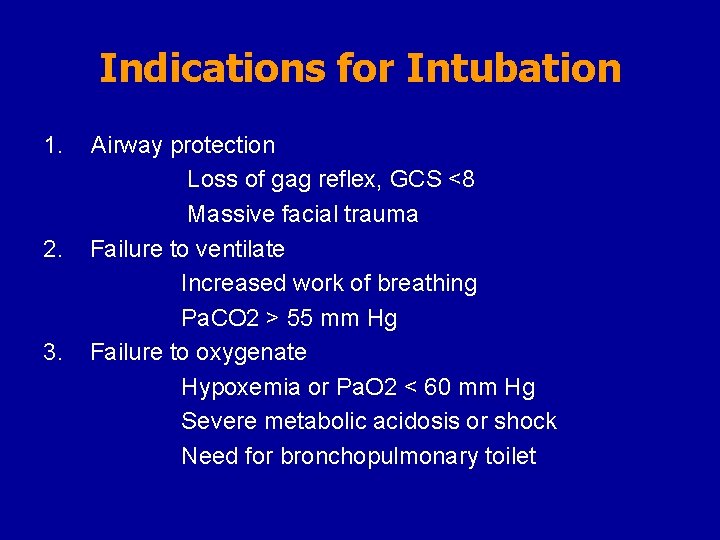
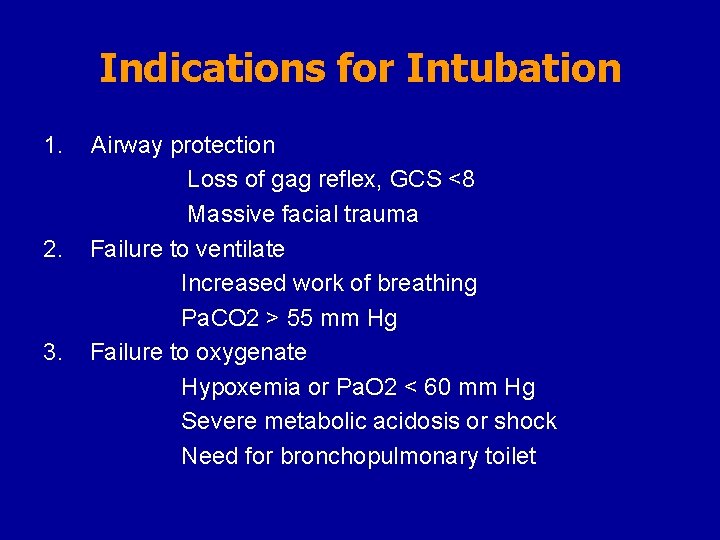
Indications for Intubation 1. 2. 3. Airway protection Loss of gag reflex, GCS <8 Massive facial trauma Failure to ventilate Increased work of breathing Pa. CO 2 > 55 mm Hg Failure to oxygenate Hypoxemia or Pa. O 2 < 60 mm Hg Severe metabolic acidosis or shock Need for bronchopulmonary toilet
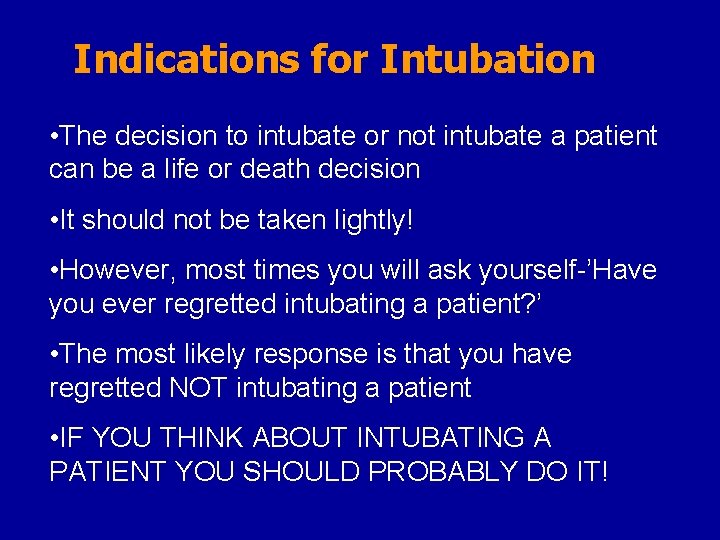
Indications for Intubation • The decision to intubate or not intubate a patient can be a life or death decision • It should not be taken lightly! • However, most times you will ask yourself-’Have you ever regretted intubating a patient? ’ • The most likely response is that you have regretted NOT intubating a patient • IF YOU THINK ABOUT INTUBATING A PATIENT YOU SHOULD PROBABLY DO IT!
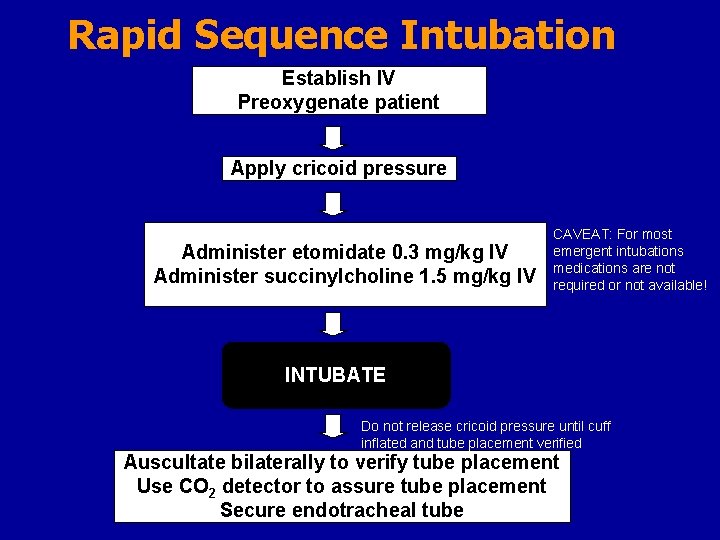
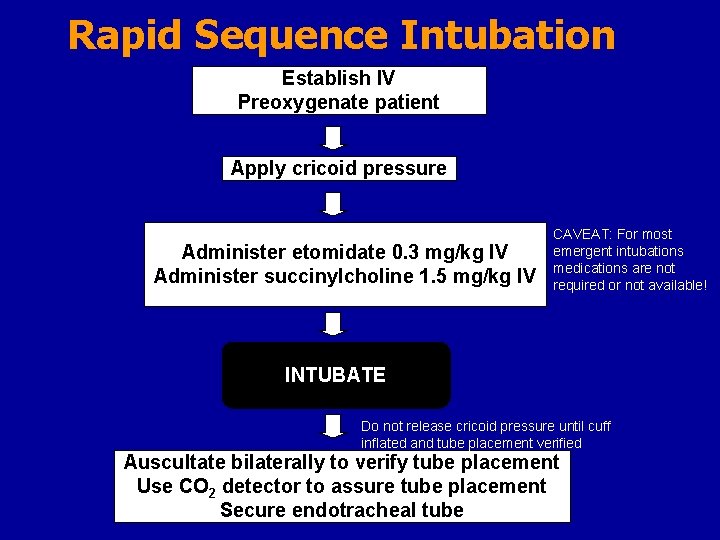
Rapid Sequence Intubation Establish IV Preoxygenate patient Apply cricoid pressure Administer etomidate 0. 3 mg/kg IV Administer succinylcholine 1. 5 mg/kg IV CAVEAT: For most emergent intubations medications are not required or not available! INTUBATE Do not release cricoid pressure until cuff inflated and tube placement verified Auscultate bilaterally to verify tube placement Use CO 2 detector to assure tube placement Secure endotracheal tube

Case Study #1 • His CBC and lytes are normal • ABG p. H 7. 45 Pa. CO 2 28 mm. Hg Pa. O 2 72 mm. Hg • CXR shows mild left lower lobe atelectasis
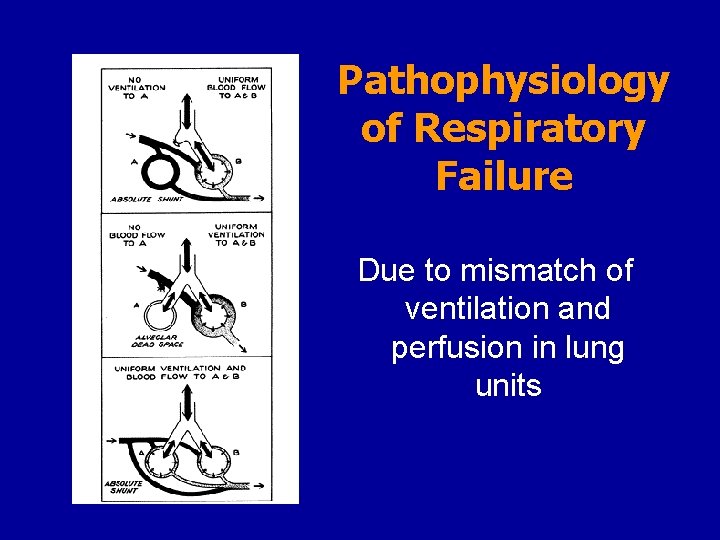
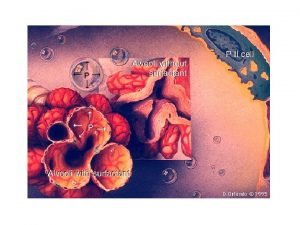
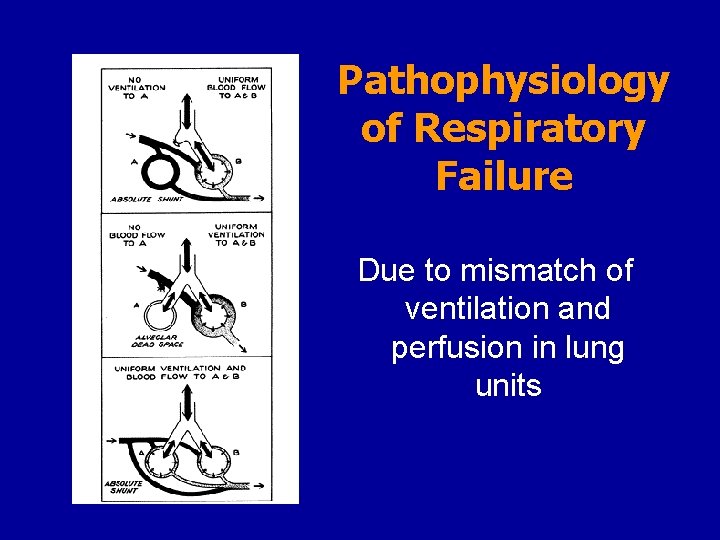
Pathophysiology of Respiratory Failure Due to mismatch of ventilation and perfusion in lung units
Labs & ABG normal History and Physical Exam Diagnosis Operation performed Co-Morbidities Age Remains agitated and risk for withdrawal (alcohol +/or drug) Consider need for CTH Call for Altered Mental Status Desaturation or Respiratory distress Intubated Step 1 Assess Airway Sa 02 < 90% Step 2 Assess Breathing Re-intubate ETT dislodged Not intubated ASSESS PATIENT Pulse Oximetry Check CXR (go to step 2) ETT good position Mini-neuro exam Review chart for medications Sa 02 > 90% May sedate with Short-acting benzodiazepine or haldol intubate Hemodynamically stable Check CXR, ABG Hemodynamically unstable with breath sounds Chest X-ray Lab Electrolytes Arterial Blood Gass Step 3 Assess Circulation Tube thoracostomy Pulses absent ACLS protocol Pulses present Assess cardiac status- ie. arrythmias
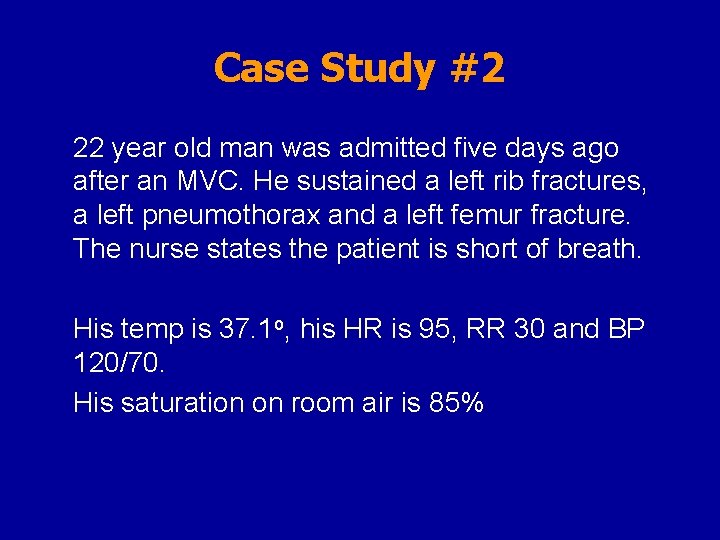
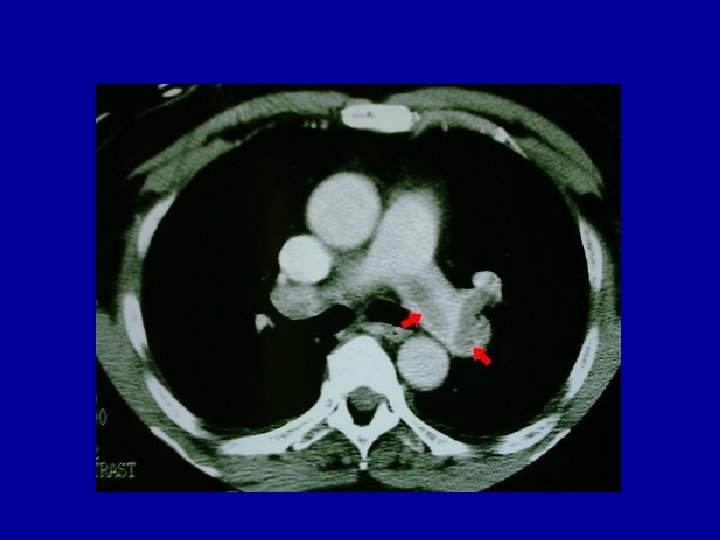
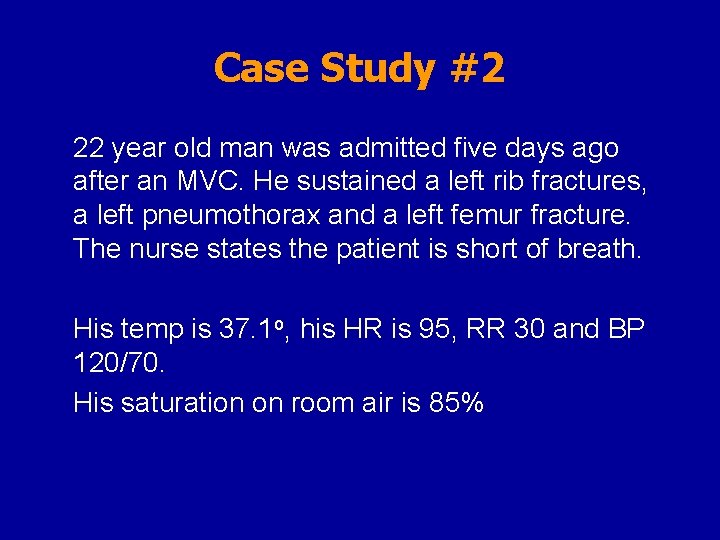
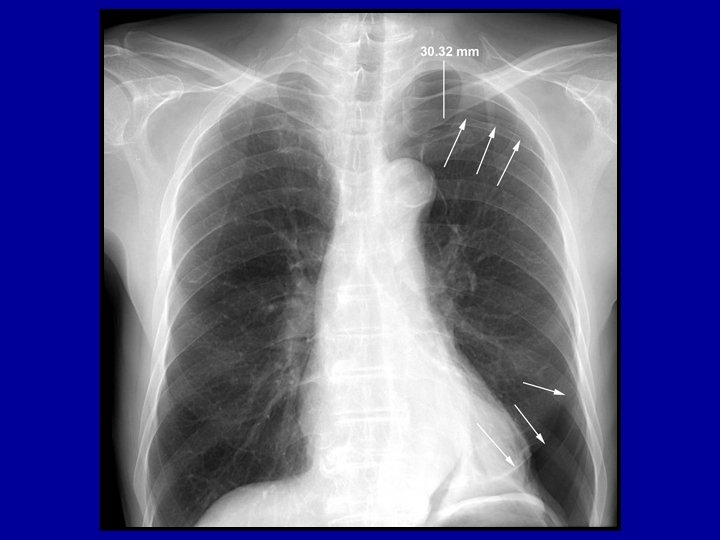
Case Study #2 22 year old man was admitted five days ago after an MVC. He sustained a left rib fractures, a left pneumothorax and a left femur fracture. The nurse states the patient is short of breath. His temp is 37. 1 o, his HR is 95, RR 30 and BP 120/70. His saturation on room air is 85%
Differential Diagnosis
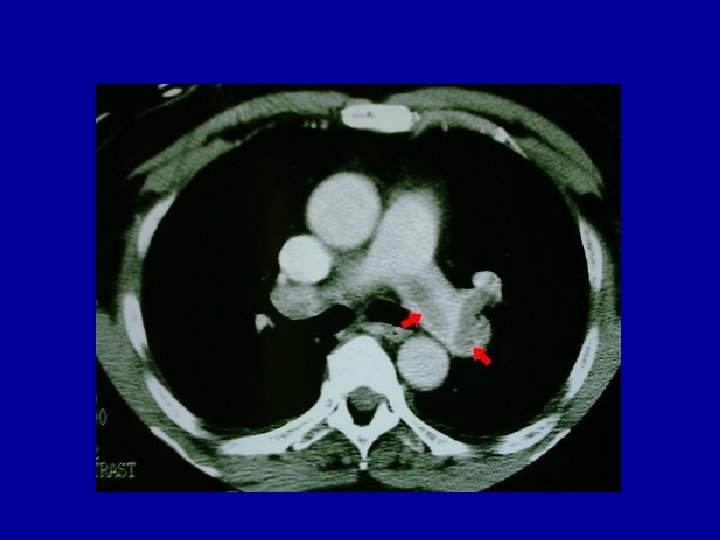
Differential Diagnosis • • Pneumothorax Pneumonia Lobar collapse Pulmonary embolus
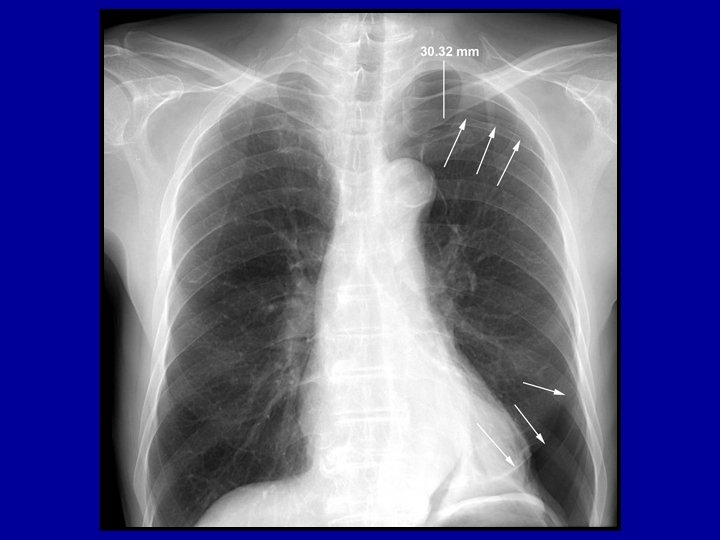





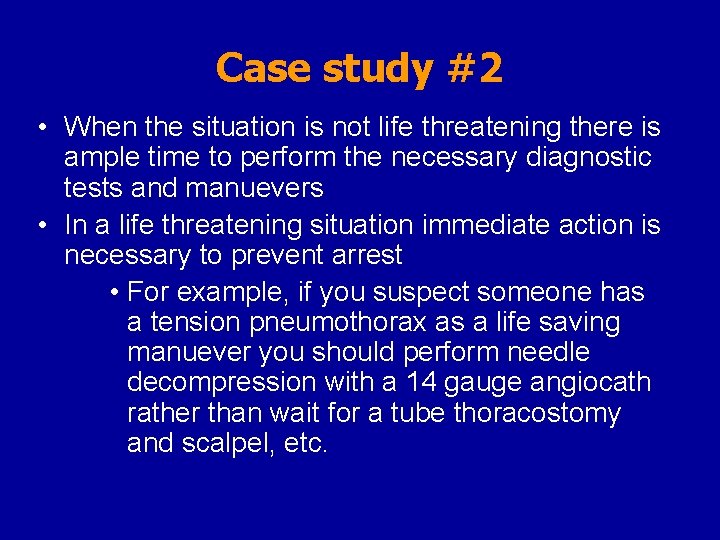
Case study #2 • When the situation is not life threatening there is ample time to perform the necessary diagnostic tests and manuevers • In a life threatening situation immediate action is necessary to prevent arrest • For example, if you suspect someone has a tension pneumothorax as a life saving manuever you should perform needle decompression with a 14 gauge angiocath rather than wait for a tube thoracostomy and scalpel, etc.
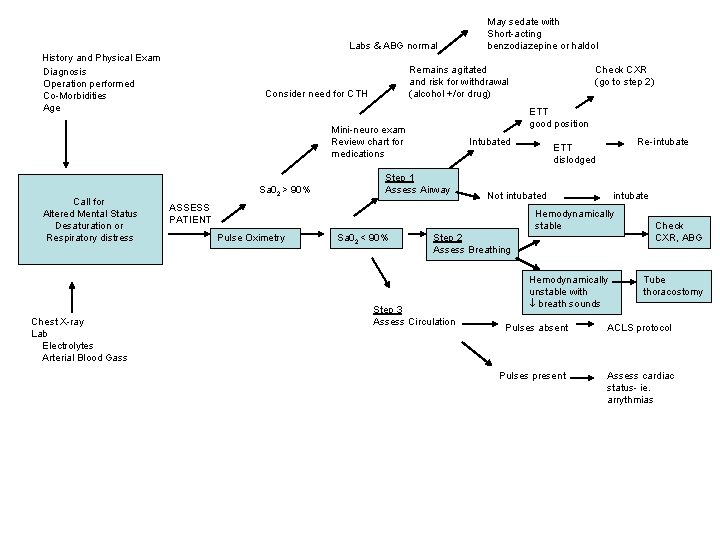
Labs & ABG normal History and Physical Exam Diagnosis Operation performed Co-Morbidities Age Remains agitated and risk for withdrawal (alcohol +/or drug) Consider need for CTH Call for Altered Mental Status Desaturation or Respiratory distress Chest X-ray Lab Electrolytes Arterial Blood Gass Check CXR (go to step 2) ETT good position Mini-neuro exam Review chart for medications Sa 02 > 90% May sedate with Short-acting benzodiazepine or haldol Intubated Step 1 Assess Airway Re-intubate ETT dislodged Not intubated ASSESS PATIENT intubate Hemodynamically stable Pulse Oximetry Sa 02 < 90% Step 2 Assess Breathing Step 3 Assess Circulation Hemodynamically unstable with breath sounds Check CXR, ABG Tube thoracostomy Pulses absent ACLS protocol Pulses present Assess cardiac status- ie. arrythmias
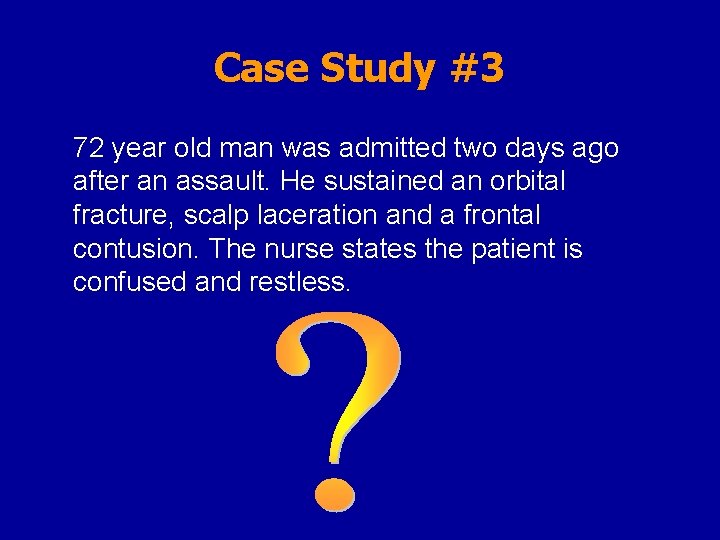
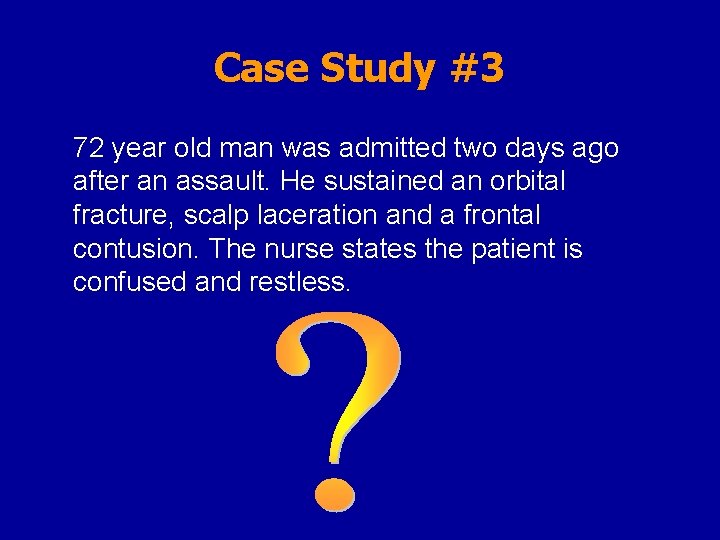
Case Study #3 72 year old man was admitted two days ago after an assault. He sustained an orbital fracture, scalp laceration and a frontal contusion. The nurse states the patient is confused and restless.
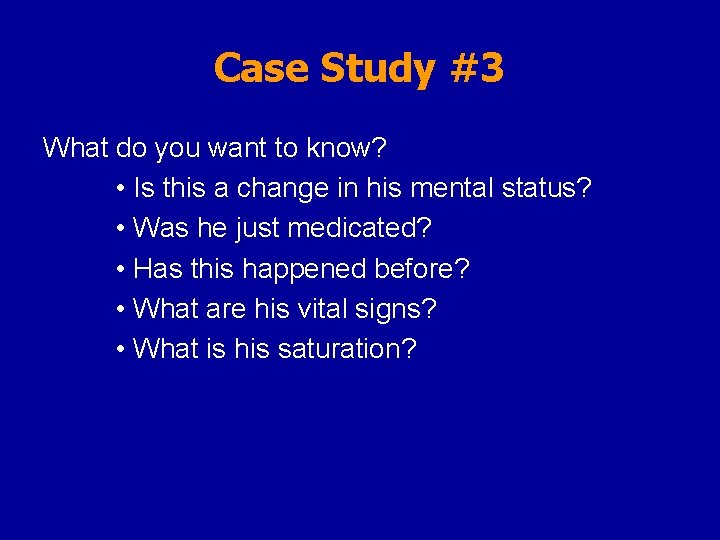
Case Study #3 What do you want to know? • Is this a change in his mental status? • Was he just medicated? • Has this happened before? • What are his vital signs? • What is his saturation?
Altered Mental Status Five major causes: • Metabolic derangement • Drug toxicity/overdose/withdrawal • Infectious • Strutural abnormality • Psychiatric
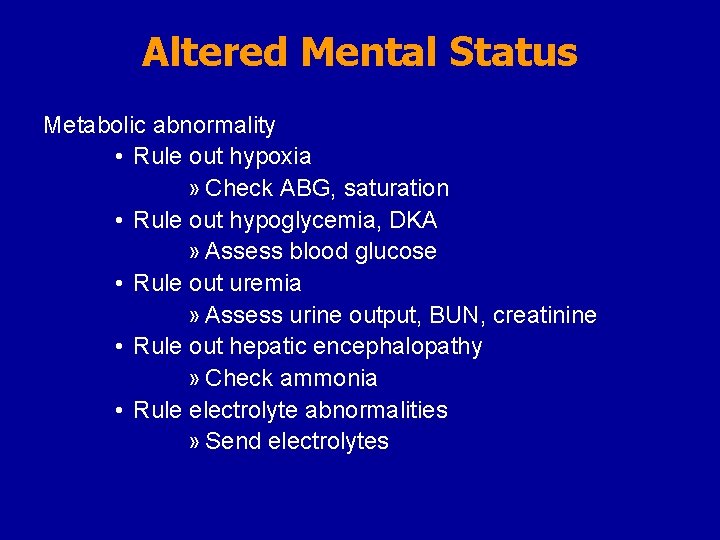
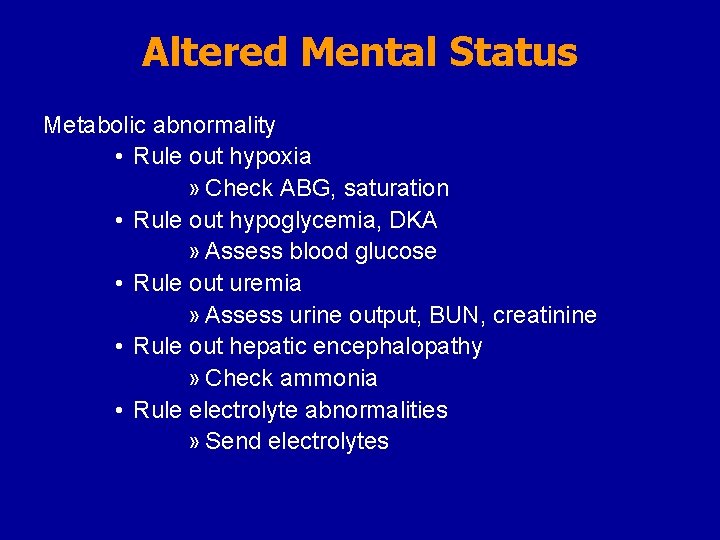
Altered Mental Status Metabolic abnormality • Rule out hypoxia » Check ABG, saturation • Rule out hypoglycemia, DKA » Assess blood glucose • Rule out uremia » Assess urine output, BUN, creatinine • Rule out hepatic encephalopathy » Check ammonia • Rule electrolyte abnormalities » Send electrolytes
Altered Mental Status Structural abnormality • Assess GCS • Assess for suspected head injury • Assess for focal neurologic deficits • Assess for possible post-ictal state • Emergent CT head
Altered Mental Status Infectious cause • Assess for post operative sepsis • Assess risk of meningitis • Assess need for CT
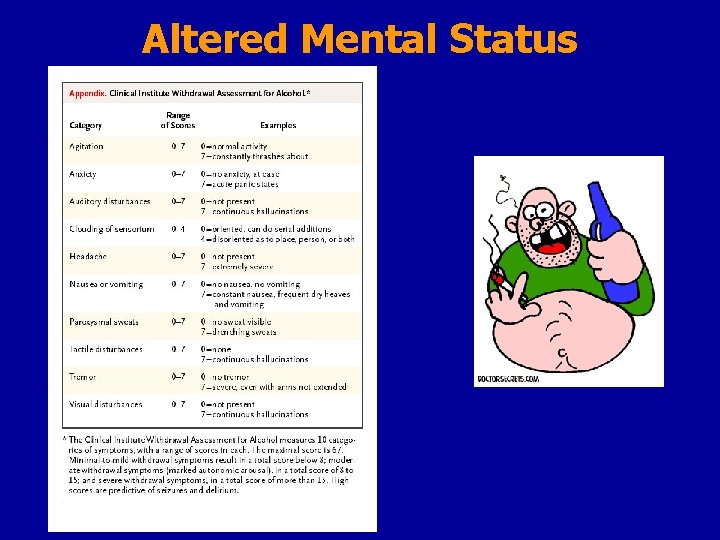
Altered Mental Status Drug toxicity/overdose/withdrawal • Assess recent prescribed medications • Assess for potential self prescribed medications • Check pupils • Check for sweating, agitation, hallucinations • Assess HR and blood pressure • May prescribe narcan or naloxone if OD • May prescribe benzodiazepine if withdrawal
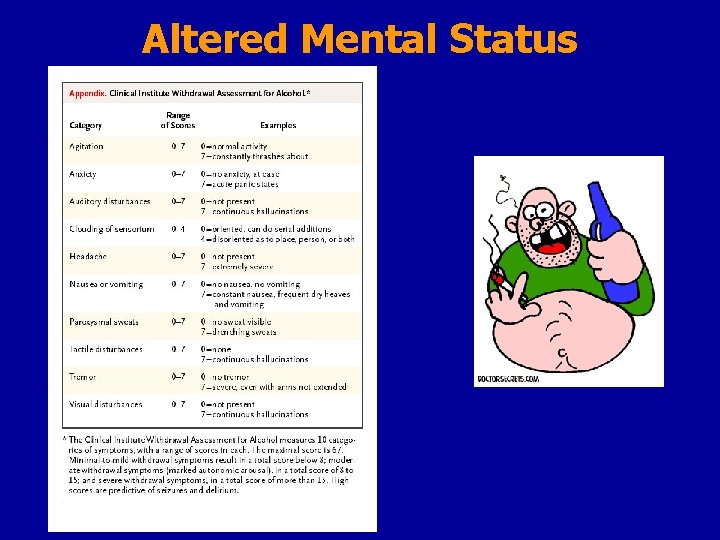
Altered Mental Status
Altered Mental Status Psychiatric cause • Assess for hallucinations • Assess for delusions • Mini-neuro exam
Labs & ABG normal History and Physical Exam Diagnosis Operation performed Co-Morbidities Age Remains agitated and risk for withdrawal (alcohol +/or drug) Consider need for CTH Intubated Re-intubate ETT dislodged Step 1 Assess Airway Sa 02 > 90% Not intubated ASSESS PATIENT Pulse Oximetry Check CXR (go to step 2) ETT good position Mini-neuro exam Review chart for medications Call for Altered Mental Status Desaturation or Respiratory distress May sedate with Short-acting benzodiazepine or haldol Sa 02 < 90% Step 2 Assess Breathing intubate Hemodynamically stable Check CXR, ABG Hemodynamically unstable with breath sounds Chest X-ray Lab Electrolytes Arterial Blood Gass Step 3 Assess Circulation Tube thoracostomy Pulses absent ACLS protocol Pulses present Assess cardiac status- ie. arrythmias
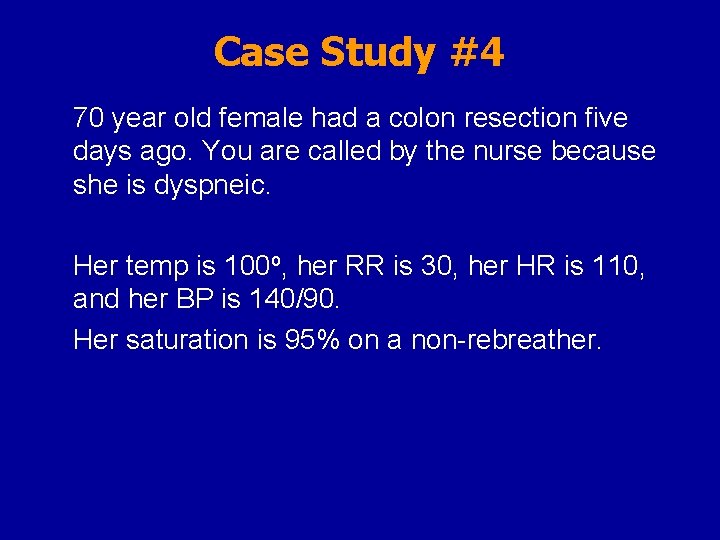
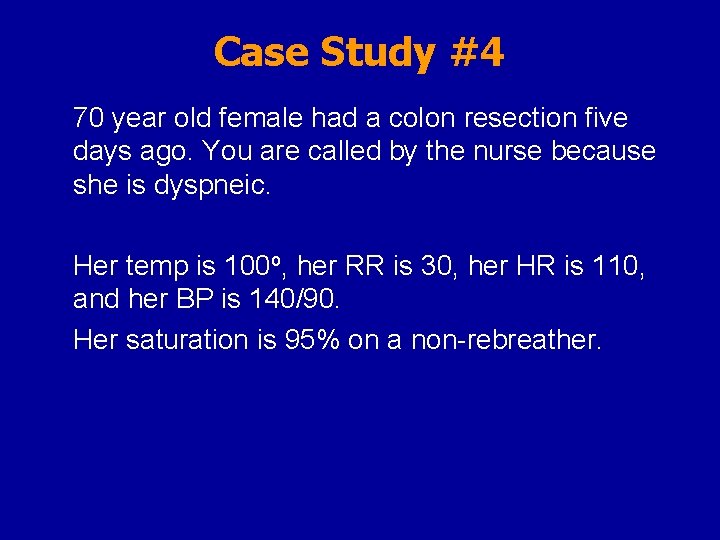
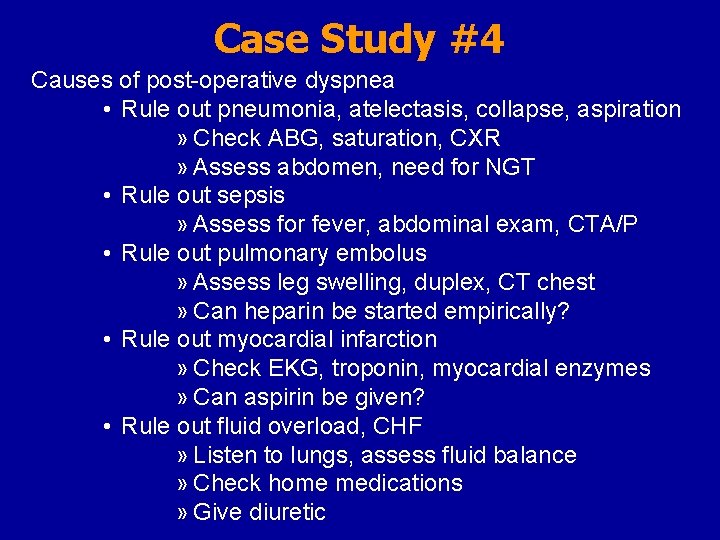
Case Study #4 70 year old female had a colon resection five days ago. You are called by the nurse because she is dyspneic. Her temp is 100 o, her RR is 30, her HR is 110, and her BP is 140/90. Her saturation is 95% on a non-rebreather.
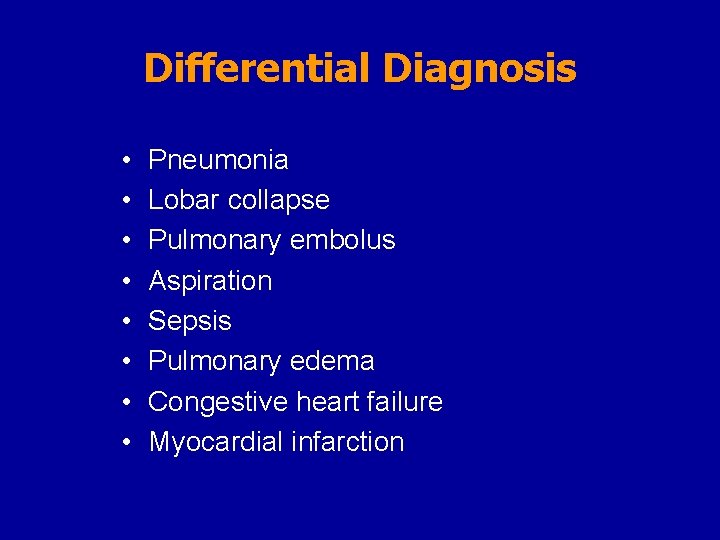
Differential Diagnosis
Differential Diagnosis • • Pneumonia Lobar collapse Pulmonary embolus Aspiration Sepsis Pulmonary edema Congestive heart failure Myocardial infarction
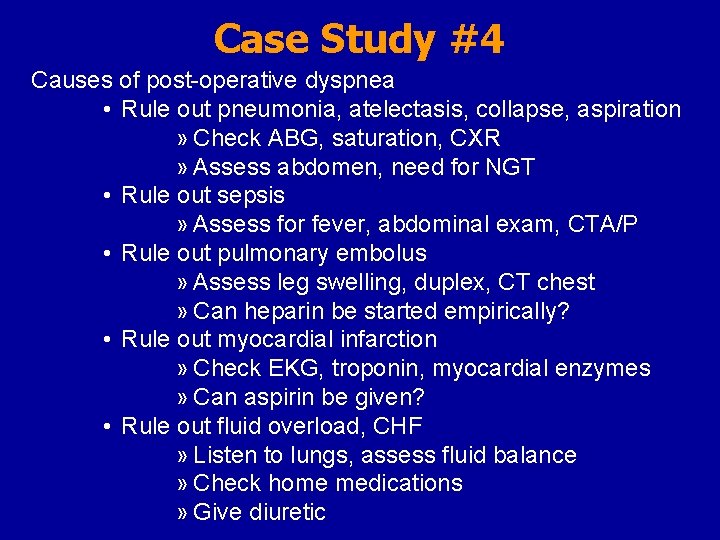
Case Study #4 Causes of post-operative dyspnea • Rule out pneumonia, atelectasis, collapse, aspiration » Check ABG, saturation, CXR » Assess abdomen, need for NGT • Rule out sepsis » Assess for fever, abdominal exam, CTA/P • Rule out pulmonary embolus » Assess leg swelling, duplex, CT chest » Can heparin be started empirically? • Rule out myocardial infarction » Check EKG, troponin, myocardial enzymes » Can aspirin be given? • Rule out fluid overload, CHF » Listen to lungs, assess fluid balance » Check home medications » Give diuretic
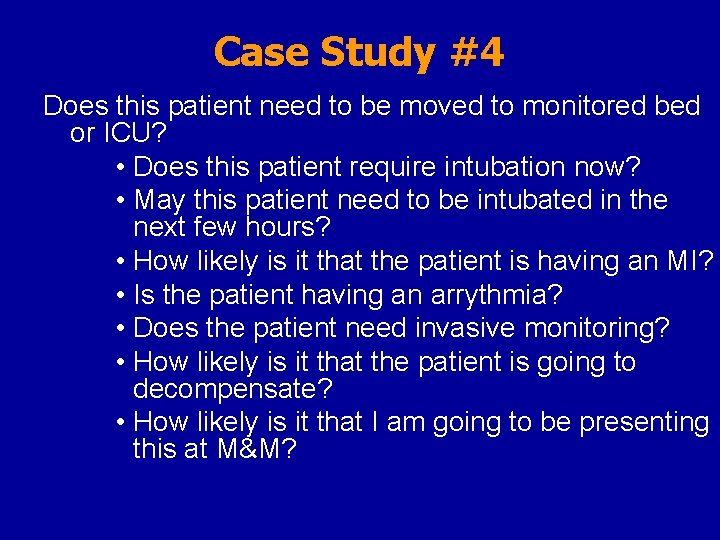
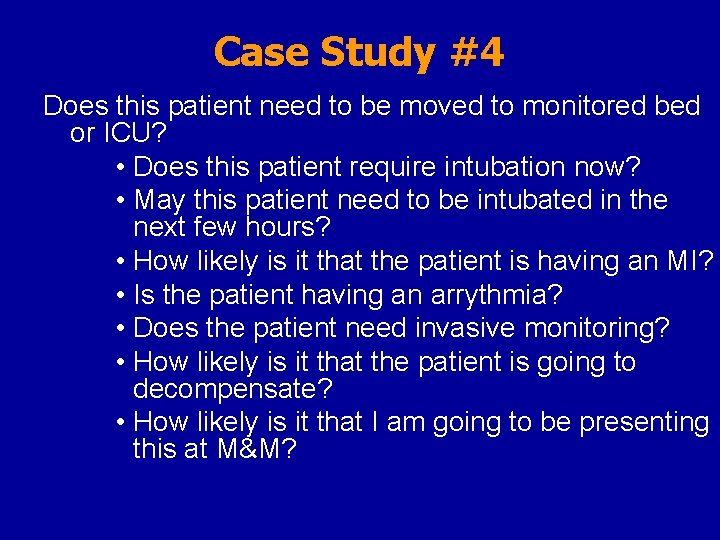
Case Study #4 Does this patient need to be moved to monitored bed or ICU? • Does this patient require intubation now? • May this patient need to be intubated in the next few hours? • How likely is it that the patient is having an MI? • Is the patient having an arrythmia? • Does the patient need invasive monitoring? • How likely is it that the patient is going to decompensate? • How likely is it that I am going to be presenting this at M&M?
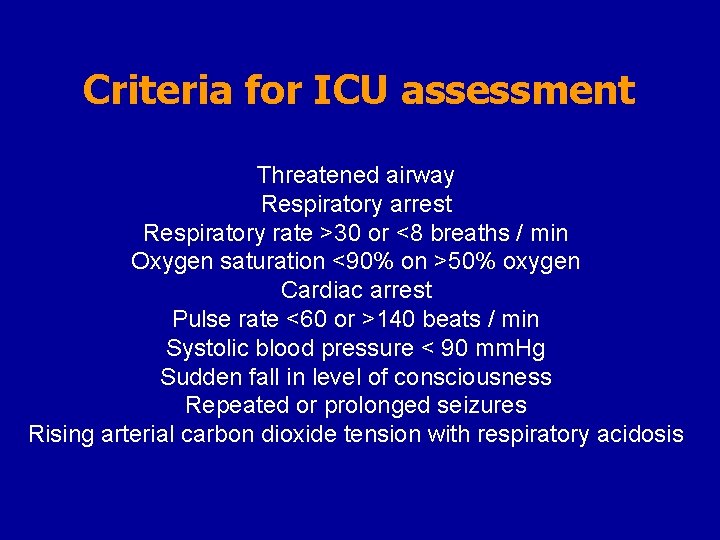
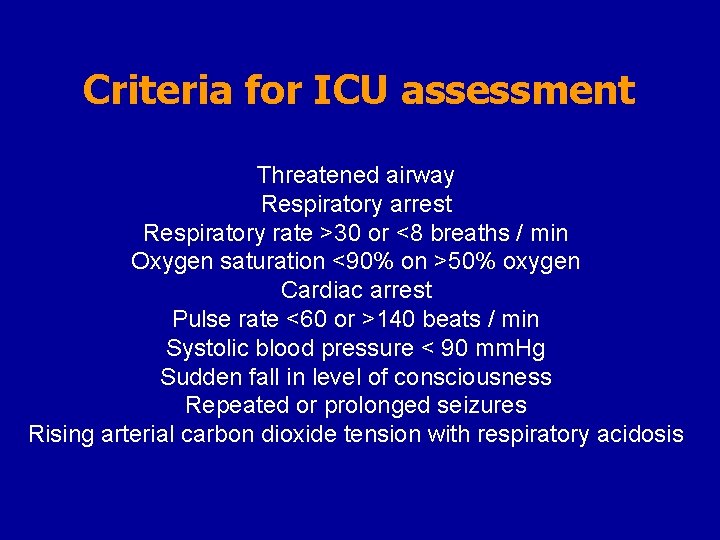
Criteria for ICU assessment Threatened airway Respiratory arrest Respiratory rate >30 or <8 breaths / min Oxygen saturation <90% on >50% oxygen Cardiac arrest Pulse rate <60 or >140 beats / min Systolic blood pressure < 90 mm. Hg Sudden fall in level of consciousness Repeated or prolonged seizures Rising arterial carbon dioxide tension with respiratory acidosis
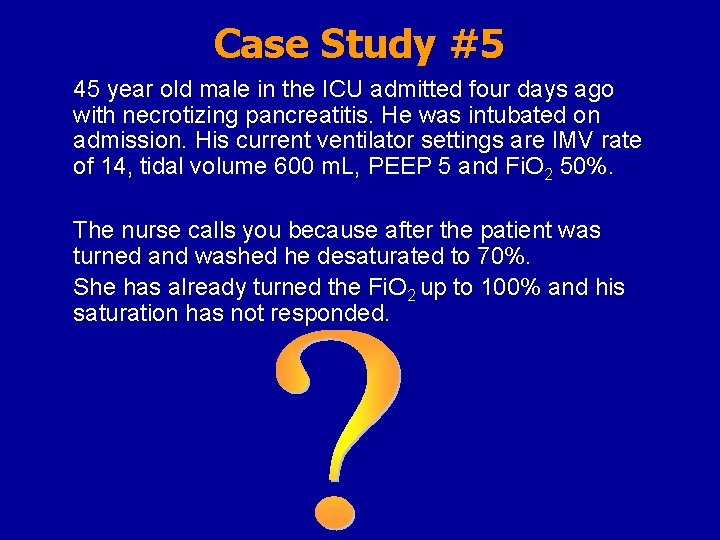
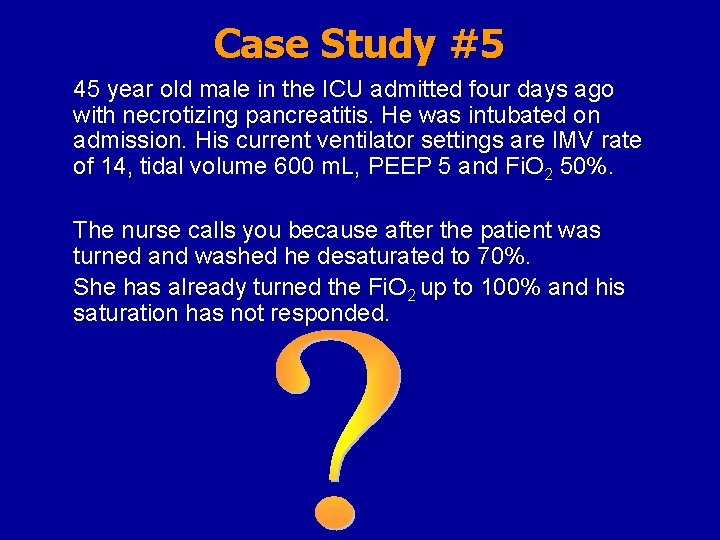
Case Study #5 45 year old male in the ICU admitted four days ago with necrotizing pancreatitis. He was intubated on admission. His current ventilator settings are IMV rate of 14, tidal volume 600 m. L, PEEP 5 and Fi. O 2 50%. The nurse calls you because after the patient was turned and washed he desaturated to 70%. She has already turned the Fi. O 2 up to 100% and his saturation has not responded.
Differential Diagnosis
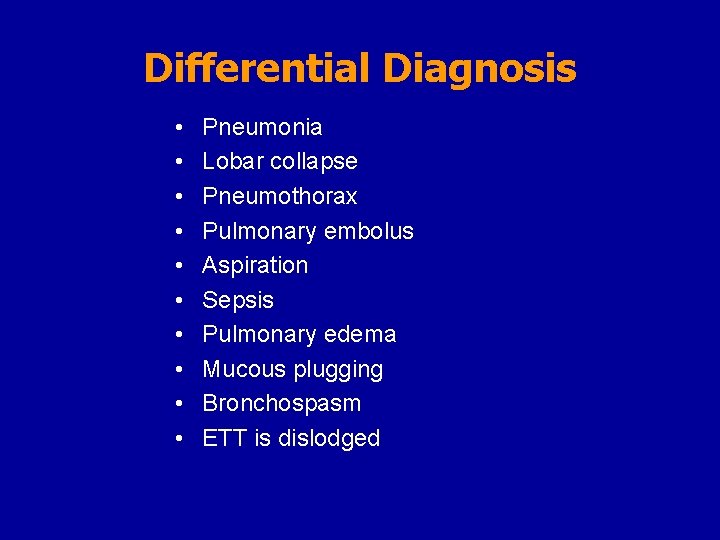
Differential Diagnosis • • • Pneumonia Lobar collapse Pneumothorax Pulmonary embolus Aspiration Sepsis Pulmonary edema Mucous plugging Bronchospasm ETT is dislodged
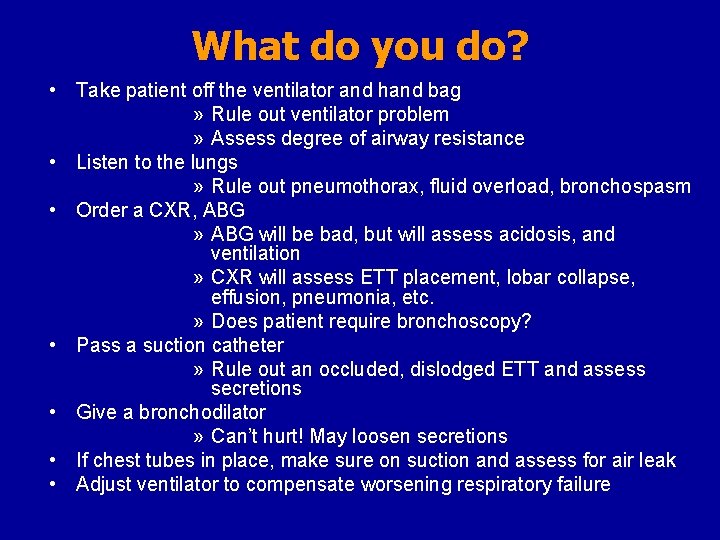
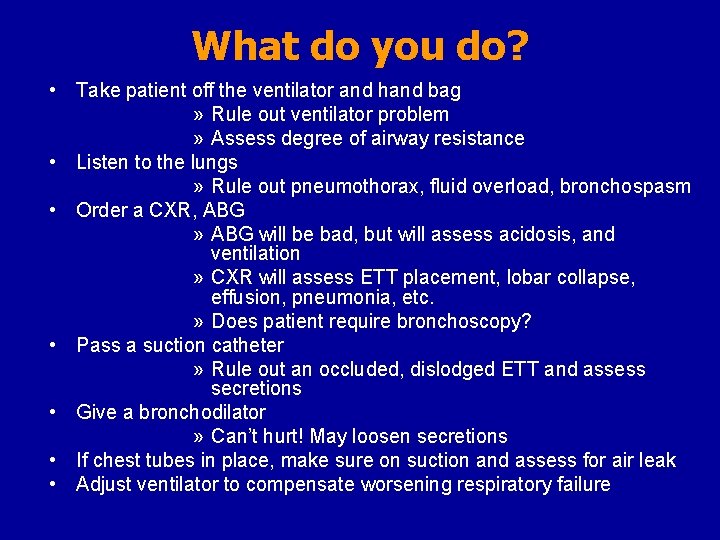
What do you do? • Take patient off the ventilator and hand bag » Rule out ventilator problem » Assess degree of airway resistance • Listen to the lungs » Rule out pneumothorax, fluid overload, bronchospasm • Order a CXR, ABG » ABG will be bad, but will assess acidosis, and ventilation » CXR will assess ETT placement, lobar collapse, effusion, pneumonia, etc. » Does patient require bronchoscopy? • Pass a suction catheter » Rule out an occluded, dislodged ETT and assess secretions • Give a bronchodilator » Can’t hurt! May loosen secretions • If chest tubes in place, make sure on suction and assess for air leak • Adjust ventilator to compensate worsening respiratory failure
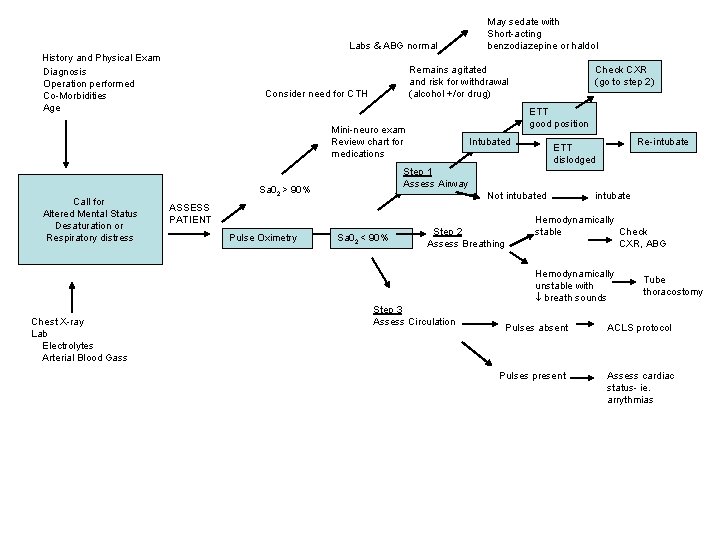
Labs & ABG normal History and Physical Exam Diagnosis Operation performed Co-Morbidities Age Remains agitated and risk for withdrawal (alcohol +/or drug) Consider need for CTH Intubated Re-intubate ETT dislodged Step 1 Assess Airway Sa 02 > 90% Not intubated ASSESS PATIENT Pulse Oximetry Check CXR (go to step 2) ETT good position Mini-neuro exam Review chart for medications Call for Altered Mental Status Desaturation or Respiratory distress May sedate with Short-acting benzodiazepine or haldol Sa 02 < 90% Step 2 Assess Breathing intubate Hemodynamically stable Check CXR, ABG Hemodynamically unstable with breath sounds Chest X-ray Lab Electrolytes Arterial Blood Gass Step 3 Assess Circulation Tube thoracostomy Pulses absent ACLS protocol Pulses present Assess cardiac status- ie. arrythmias

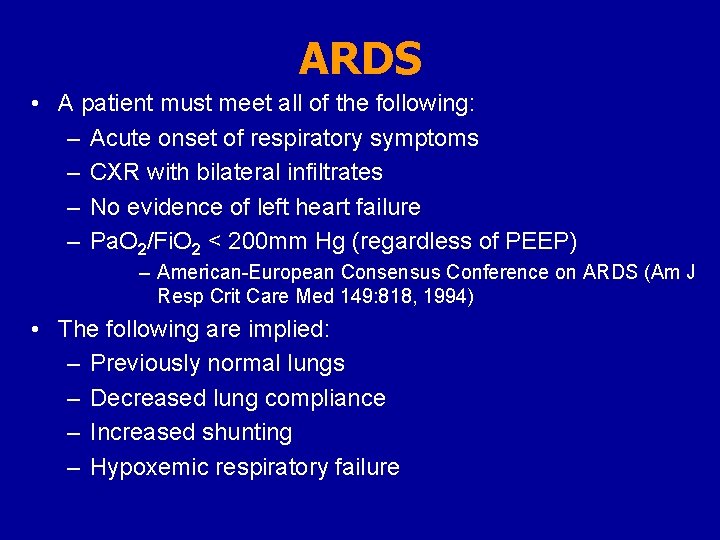
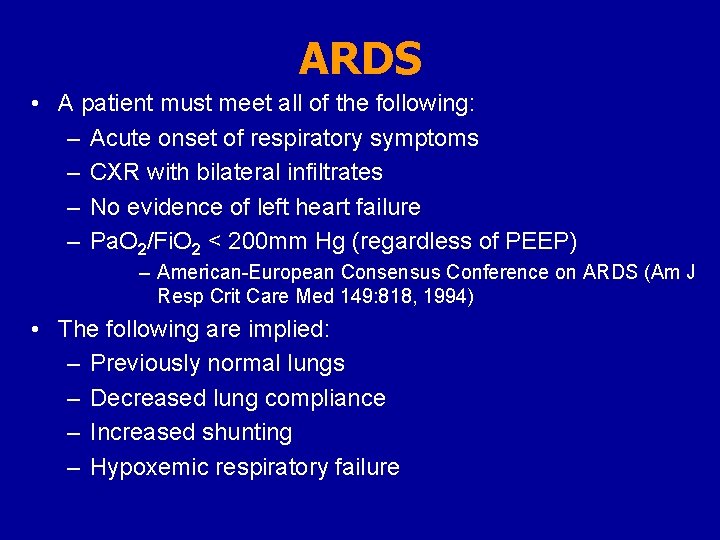
ARDS • A patient must meet all of the following: – Acute onset of respiratory symptoms – CXR with bilateral infiltrates – No evidence of left heart failure – Pa. O 2/Fi. O 2 < 200 mm Hg (regardless of PEEP) – American-European Consensus Conference on ARDS (Am J Resp Crit Care Med 149: 818, 1994) • The following are implied: – Previously normal lungs – Decreased lung compliance – Increased shunting – Hypoxemic respiratory failure
 Capture beat
Capture beat Failure to pace
Failure to pace Ductile fracture mechanism
Ductile fracture mechanism Decrd
Decrd Hypoventilation
Hypoventilation Hypoxaemia vs hypoxia
Hypoxaemia vs hypoxia Baltic sea hypoxia
Baltic sea hypoxia Dr halvax lászló
Dr halvax lászló Haemoglobin
Haemoglobin Diffusion hypoxia slideshare
Diffusion hypoxia slideshare Second gas effect
Second gas effect Hemoglobina
Hemoglobina Hypoximia
Hypoximia Type 1 resp failure
Type 1 resp failure Pink puffer
Pink puffer Hypercapnic respiratory failure
Hypercapnic respiratory failure Priyanka breathing
Priyanka breathing Types of respiratory failure
Types of respiratory failure Complications of respiratory failure
Complications of respiratory failure Respiratory zone and conducting zone
Respiratory zone and conducting zone Mental health and mental illness chapter 20
Mental health and mental illness chapter 20 Psychomotor activity in mse
Psychomotor activity in mse Thought content examples
Thought content examples Pemeriksaan psikiatri
Pemeriksaan psikiatri Preservasi jiwa adalah
Preservasi jiwa adalah Linear thought process mental status
Linear thought process mental status Heidi combs
Heidi combs A full mental status examination example
A full mental status examination example Mental status examination purpose
Mental status examination purpose Dysdiadochokinesia test
Dysdiadochokinesia test St louis mental status exam
St louis mental status exam Coastmap ems
Coastmap ems Mental state examination example
Mental state examination example Perubahan status mental
Perubahan status mental Coastmap ems
Coastmap ems Mental health jeopardy
Mental health jeopardy Mosby items and derived items
Mosby items and derived items Altered cellular and tissue biology
Altered cellular and tissue biology What happened to esperanza at the carnival?
What happened to esperanza at the carnival? Judy believes that her fate
Judy believes that her fate Altered state of consciousness psychology
Altered state of consciousness psychology An altered state of consciousness
An altered state of consciousness Modular tube feeding
Modular tube feeding Dietary adjustments after a gastrectomy are influenced by
Dietary adjustments after a gastrectomy are influenced by Altered cognition in older adults is commonly attributed to
Altered cognition in older adults is commonly attributed to Ap psychology states of consciousness
Ap psychology states of consciousness Altered state of consciousness psychology
Altered state of consciousness psychology Altered state of consciousness psychology
Altered state of consciousness psychology Altered cast technique diagram
Altered cast technique diagram Crash course altered states
Crash course altered states Hypnotic states
Hypnotic states Can fingerprints be altered or disguised
Can fingerprints be altered or disguised La rueda de color
La rueda de color What are fossils
What are fossils Lesson quiz 7-1 altered states of consciousness
Lesson quiz 7-1 altered states of consciousness Altered state of conciousness
Altered state of conciousness Sex altered state of consciousness
Sex altered state of consciousness Best impression material for partial dentures
Best impression material for partial dentures Altered fossil
Altered fossil