Acute Respiratory Distress Syndrome Jason D Sciarretta M






- Slides: 24
Acute Respiratory Distress Syndrome Jason D. Sciarretta, M. D. Critical Care Conference October 13, 2010
History ARDS n The syndrome of acute pulmonary failure was recognized during World War I n “The acute onset of severe respiratory distress and cyanosis that was refractory to oxygen therapy and associated with diffuse CXR abnormality and decreased lung compliance” – Ashbaugh DG. Acute Respiratory distress in Adults. Lancet 1967
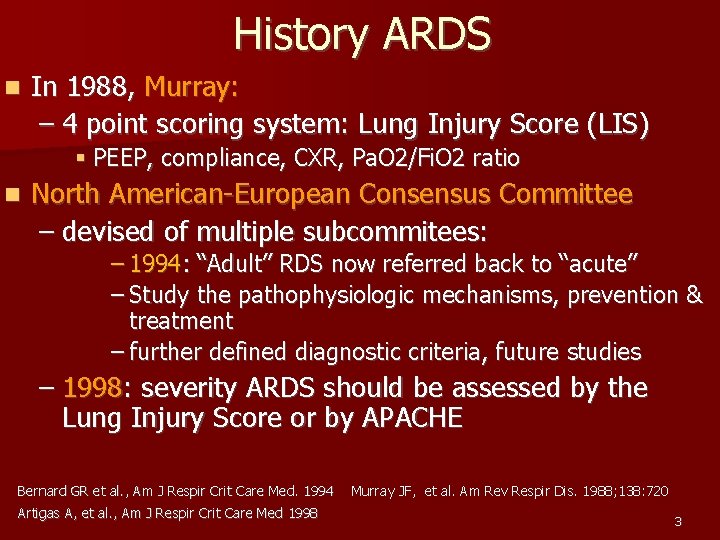
History ARDS n In 1988, Murray: – 4 point scoring system: Lung Injury Score (LIS) § PEEP, compliance, CXR, Pa. O 2/Fi. O 2 ratio n North American-European Consensus Committee – devised of multiple subcommitees: – 1994: “Adult” RDS now referred back to “acute” – Study the pathophysiologic mechanisms, prevention & treatment – further defined diagnostic criteria, future studies – 1998: severity ARDS should be assessed by the Lung Injury Score or by APACHE Bernard GR et al. , Am J Respir Crit Care Med. 1994 Murray JF, et al. Am Rev Respir Dis. 1988; 138: 720 Bernard GR et al. , Am J Respir Crit Care Med. 1994 Artigas A, et al. , Am J Respir Crit Care Med 1998 3
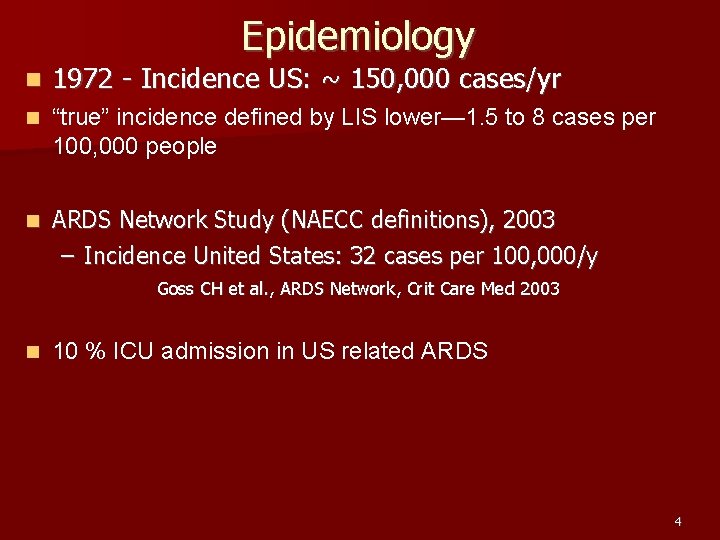
Epidemiology n 1972 - Incidence US: ~ 150, 000 cases/yr n “true” incidence defined by LIS lower— 1. 5 to 8 cases per 100, 000 people n ARDS Network Study (NAECC definitions), 2003 – Incidence United States: 32 cases per 100, 000/y Goss CH et al. , ARDS Network, Crit Care Med 2003 n 10 % ICU admission in US related ARDS 4
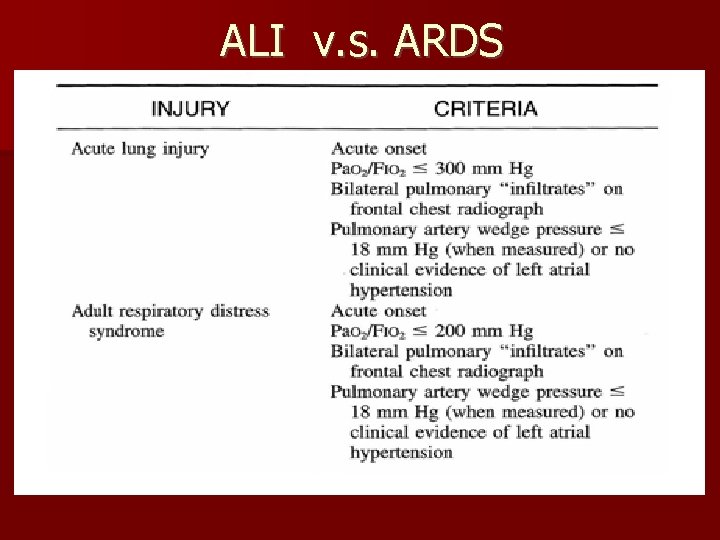
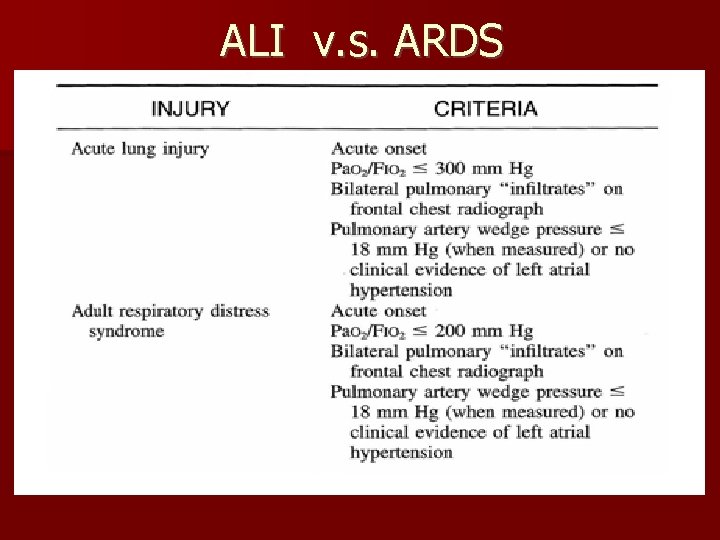
ALI v. s. ARDS
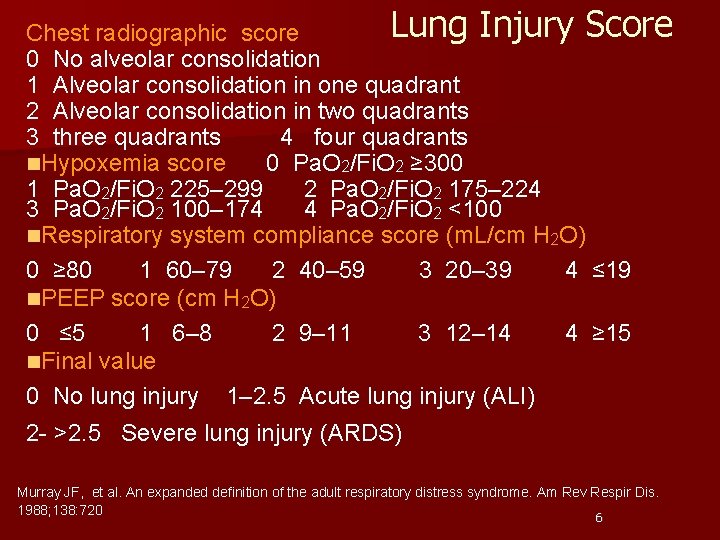
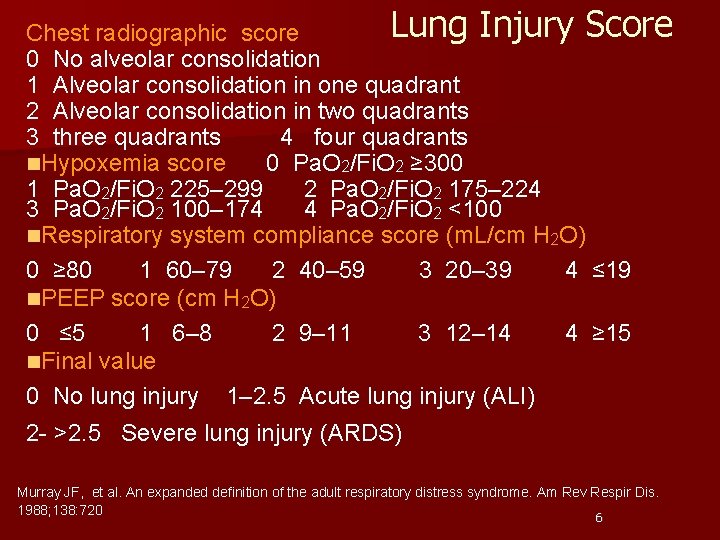
Lung Injury Score Chest radiographic score 0 No alveolar consolidation 1 Alveolar consolidation in one quadrant 2 Alveolar consolidation in two quadrants 3 three quadrants 4 four quadrants n. Hypoxemia score 0 Pa. O 2/Fi. O 2 ≥ 300 1 Pa. O 2/Fi. O 2 225– 299 2 Pa. O 2/Fi. O 2 175– 224 3 Pa. O 2/Fi. O 2 100– 174 4 Pa. O 2/Fi. O 2 <100 n. Respiratory system compliance score (m. L/cm H 2 O) 0 ≥ 80 1 60– 79 2 40– 59 3 20– 39 4 ≤ 19 n. PEEP score (cm H 2 O) 0 ≤ 5 1 6– 8 2 9– 11 3 12– 14 4 ≥ 15 n. Final value 0 No lung injury 1– 2. 5 Acute lung injury (ALI) 2 - >2. 5 Severe lung injury (ARDS) Murray JF, et al. An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis. 1988; 138: 720 6
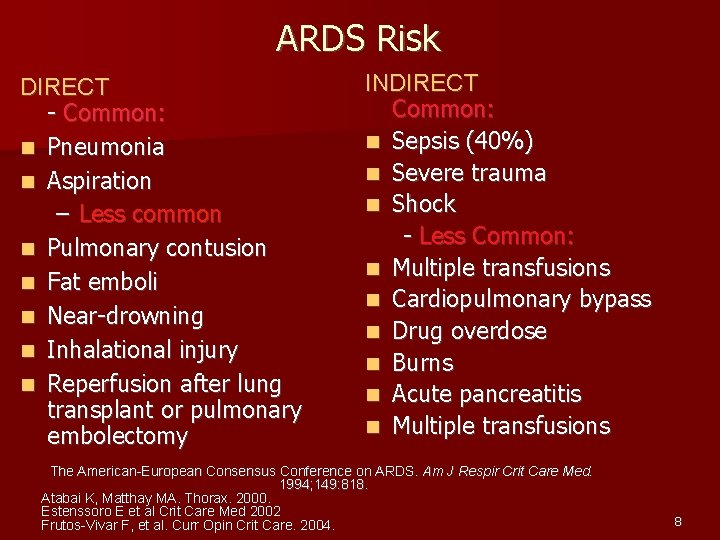
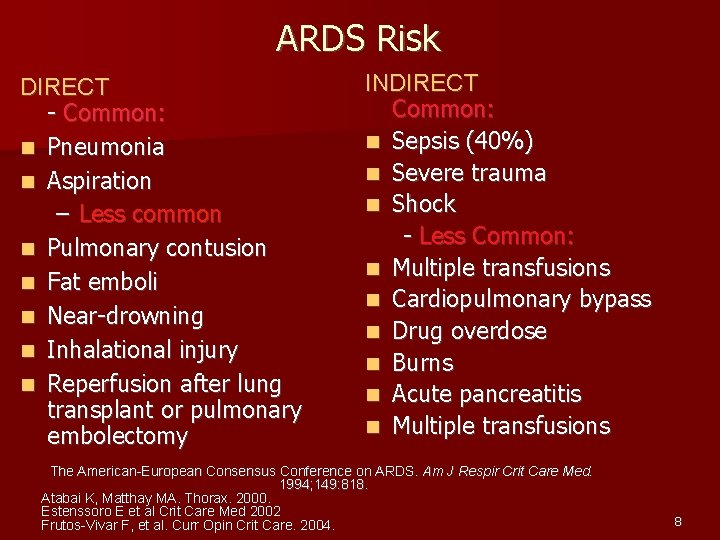
ARDS Risk DIRECT - Common: n Pneumonia n Aspiration – Less common n Pulmonary contusion n Fat emboli n Near-drowning n Inhalational injury n Reperfusion after lung transplant or pulmonary embolectomy INDIRECT Common: n Sepsis (40%) n Severe trauma n Shock - Less Common: n Multiple transfusions n Cardiopulmonary bypass n Drug overdose n Burns n Acute pancreatitis n Multiple transfusions The American-European Consensus Conference on ARDS. Am J Respir Crit Care Med. 1994; 149: 818. Atabai K, Matthay MA. Thorax. 2000. Estenssoro E et al Crit Care Med 2002 Frutos-Vivar F, et al. Curr Opin Crit Care. 2004. 8
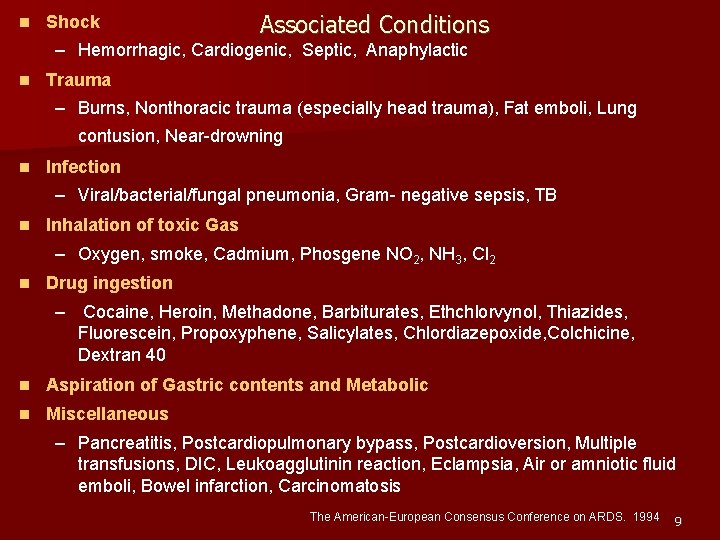
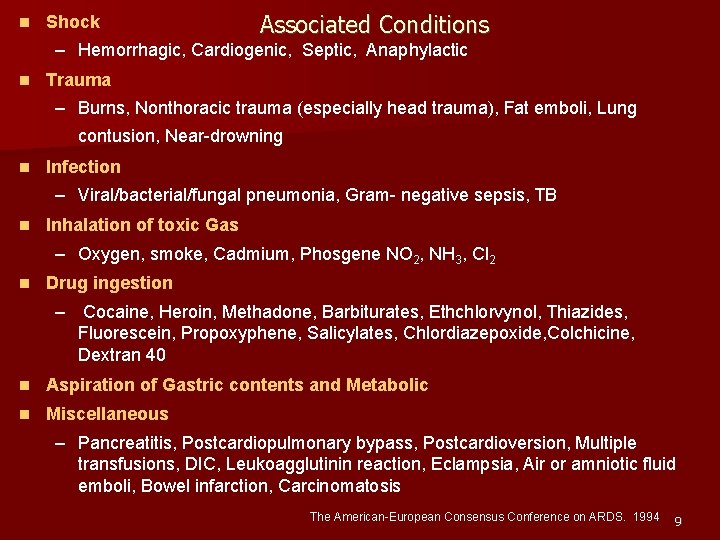
n Shock Associated Conditions – Hemorrhagic, Cardiogenic, Septic, Anaphylactic n Trauma – Burns, Nonthoracic trauma (especially head trauma), Fat emboli, Lung contusion, Near-drowning n Infection – Viral/bacterial/fungal pneumonia, Gram- negative sepsis, TB n Inhalation of toxic Gas – Oxygen, smoke, Cadmium, Phosgene NO 2, NH 3, Cl 2 n Drug ingestion – Cocaine, Heroin, Methadone, Barbiturates, Ethchlorvynol, Thiazides, Fluorescein, Propoxyphene, Salicylates, Chlordiazepoxide, Colchicine, Dextran 40 n Aspiration of Gastric contents and Metabolic n Miscellaneous – Pancreatitis, Postcardiopulmonary bypass, Postcardioversion, Multiple transfusions, DIC, Leukoagglutinin reaction, Eclampsia, Air or amniotic fluid emboli, Bowel infarction, Carcinomatosis The American-European Consensus Conference on ARDS. 1994 9
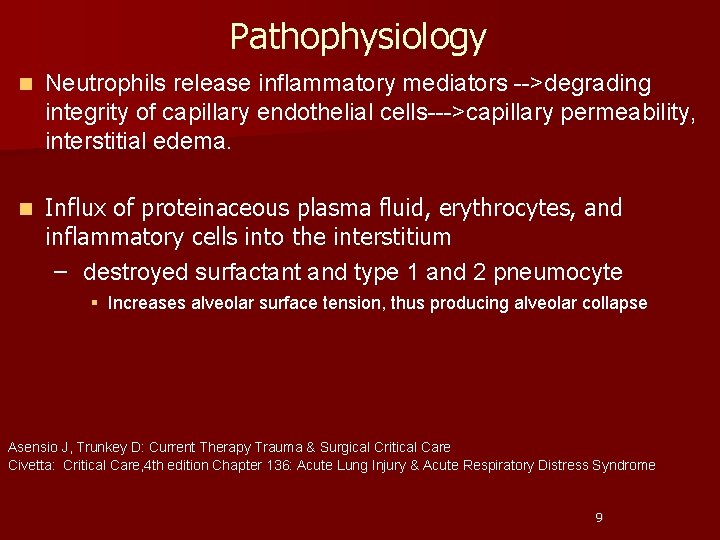
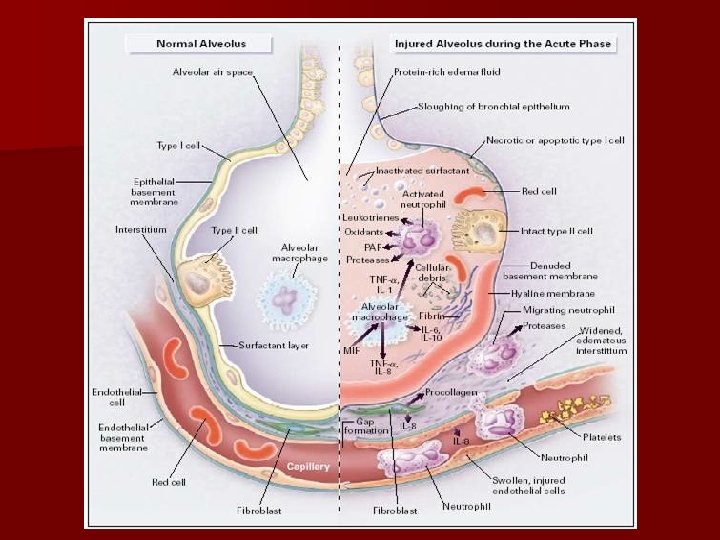
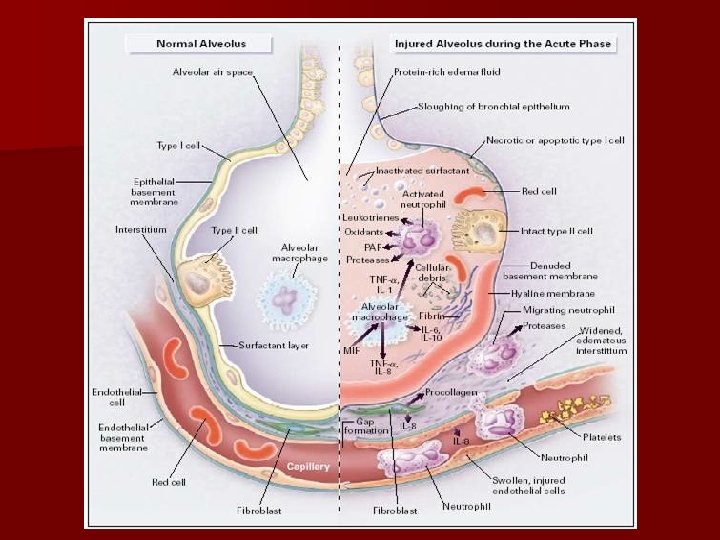
Pathophysiology n Neutrophils release inflammatory mediators -->degrading integrity of capillary endothelial cells--->capillary permeability, interstitial edema. n Influx of proteinaceous plasma fluid, erythrocytes, and inflammatory cells into the interstitium – destroyed surfactant and type 1 and 2 pneumocyte § Increases alveolar surface tension, thus producing alveolar collapse Asensio J, Trunkey D: Current Therapy Trauma & Surgical Critical Care Civetta: Critical Care, 4 th edition Chapter 136: Acute Lung Injury & Acute Respiratory Distress Syndrome 9
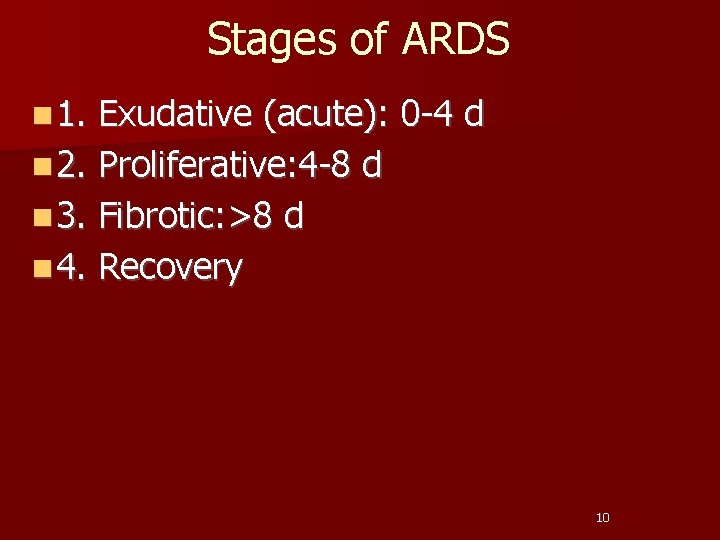
Stages of ARDS n 1. Exudative (acute): 0 -4 d n 2. Proliferative: 4 -8 d n 3. Fibrotic: >8 d n 4. Recovery 10
11
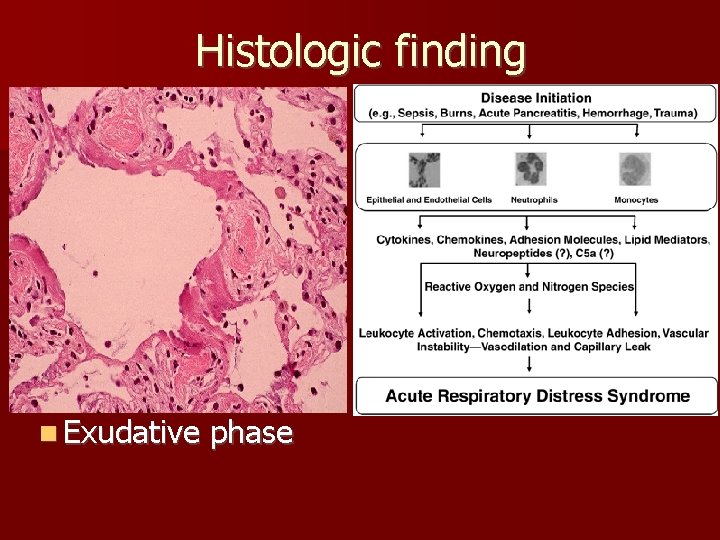
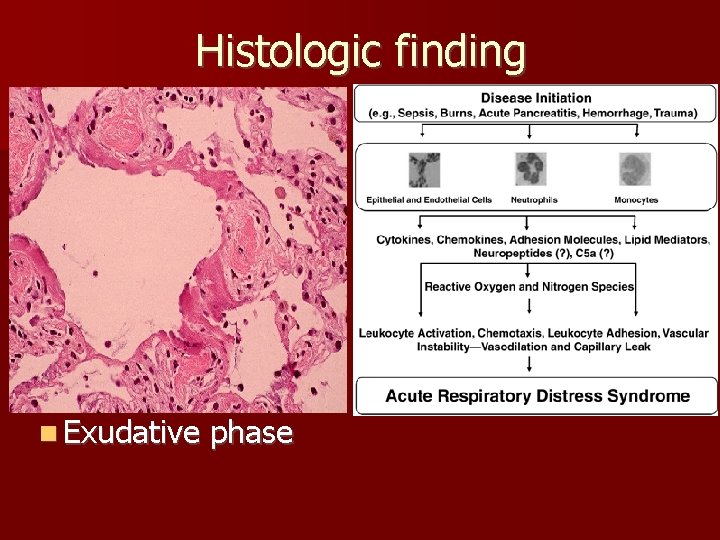
Histologic finding n Exudative phase

Histologic findings n early proliferative stage: type 2 pneumocytic proliferation, widening septa & interstitial fibroblast proliferation. n late proliferative stage: extensive fibroblast proliferation: incorporation of the hyaline membranes

Plasma Biologic Markers Predictive of a Poor Outcome Acute inflammation Endothelial injury Epithelial type II cell Adhesion molecule IL-6, IL-8 v. WF antigen Surfactant protein-D Intercellular adhesion molecule (ICAM-1) Neutrophil-endothelial Soluble TNF receptors I & II (s. TNFRI/II) interation Procoagulant activity Protein C Plasminogen activator inhibitor-1 Fibrinolytic activity 5 Ware LB, Crit Care Med. 2005

Clinical Progression n Phase 1: Acute Injury • • Normal physical examination and chest radiograph Tachycardia, tachypnea, and respiratory alkalosis develop n Phase 2: Latent Period • Lasts ~ 6– 48 h after injury: remains clinical stable • Hyperventilation & hypocapnia persist; mild increase work breathing • Minor abnormalities on physical examination and chest radiograph n Phase 3: Acute Respiratory Failure • Decreased lung compliance: marked tachypnea & dyspnea • Diffuse infiltrates on chest radiograph • High-pitched crackles heard throughout all lung fields n Phase 4: Severe Abnormalities • Severe hypoxemia unresponsive to therapy • Metabolic and respiratory acidosis • lethargy, obtunded Gomez AC: Pulmonary insufficiency in non-thoracic trauma [discussion]. J Trauma. 1968; 8: 666 15
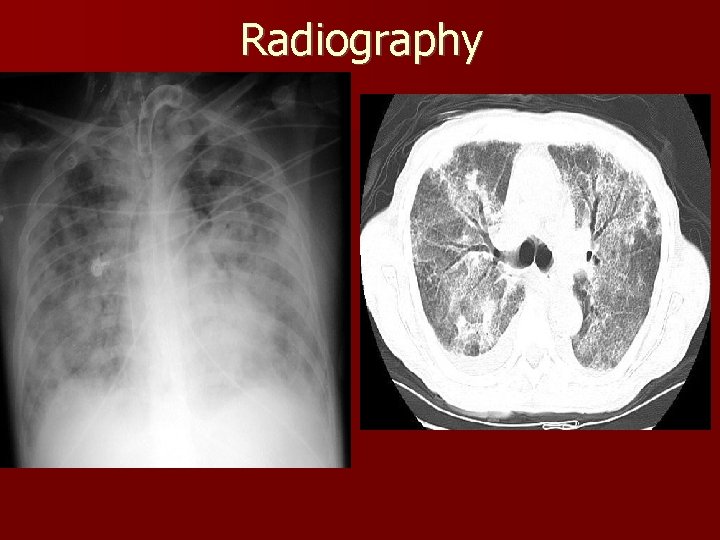
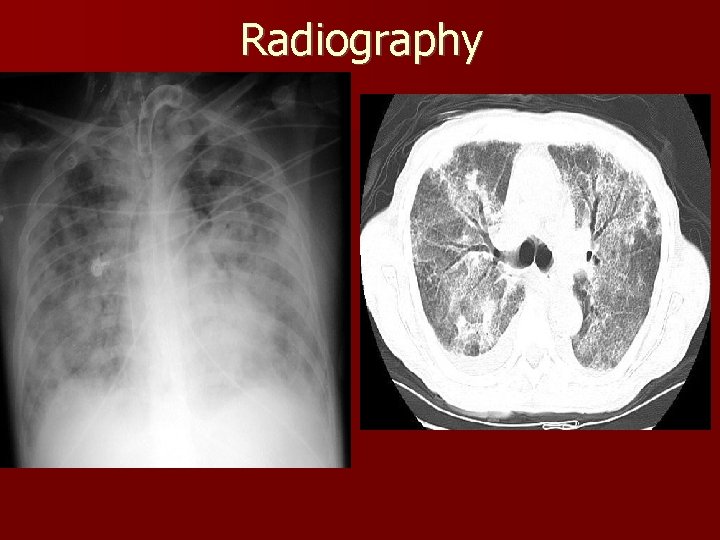
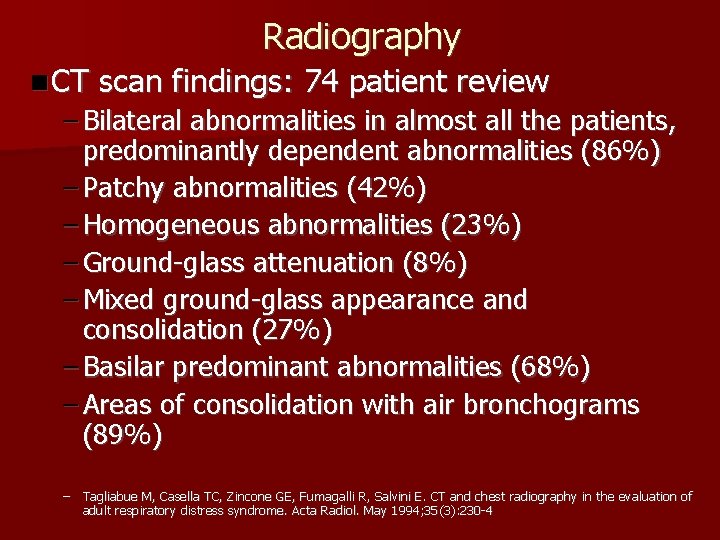
Radiography
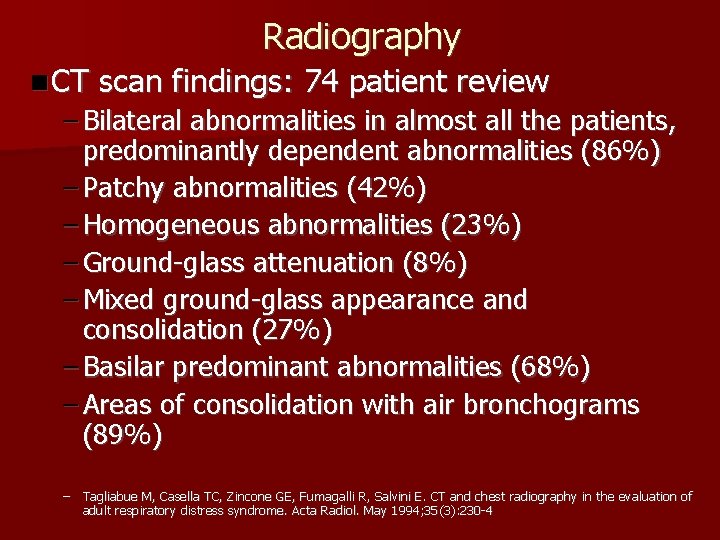
Radiography n CT scan findings: 74 patient review – Bilateral abnormalities in almost all the patients, predominantly dependent abnormalities (86%) – Patchy abnormalities (42%) – Homogeneous abnormalities (23%) – Ground-glass attenuation (8%) – Mixed ground-glass appearance and consolidation (27%) – Basilar predominant abnormalities (68%) – Areas of consolidation with air bronchograms (89%) – Tagliabue M, Casella TC, Zincone GE, Fumagalli R, Salvini E. CT and chest radiography in the evaluation of adult respiratory distress syndrome. Acta Radiol. May 1994; 35(3): 230 -4

Clinical Risk Factors Predictive of Poor Outcomes n Independent predictors repeatedly: higher mortality rates – Severity of the illness – Non-pulmonary organ dysfunction – Comorbid diseases, Sepsis, Liver dysfunction/cirrhosis – Advanced age n Other independent risk factors: – Organ transplantation – HIV infection and Immunosuppression – Active malignancy – Mechanisms of lung injury – Barotrauma – Fio 2 (High) – Atabai K, Matthay MA. Thorax. 2000. Ware LB. Crit Care Med. 2005. Ferguson ND, et al. Crit Care Med. 2005. 18
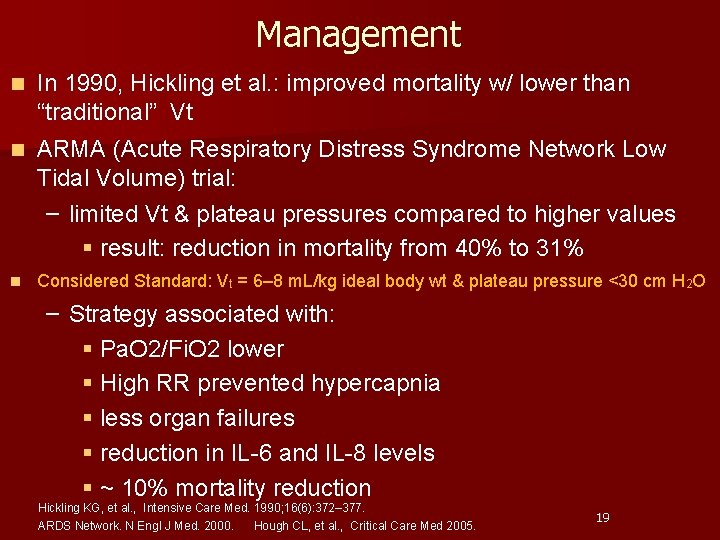
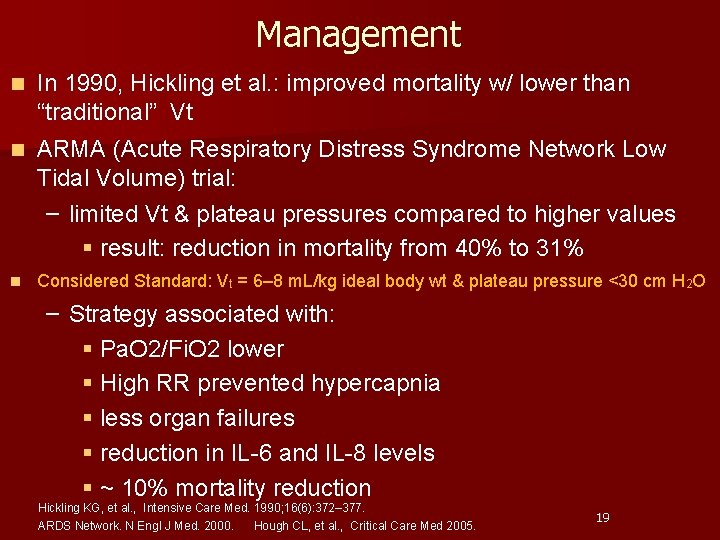
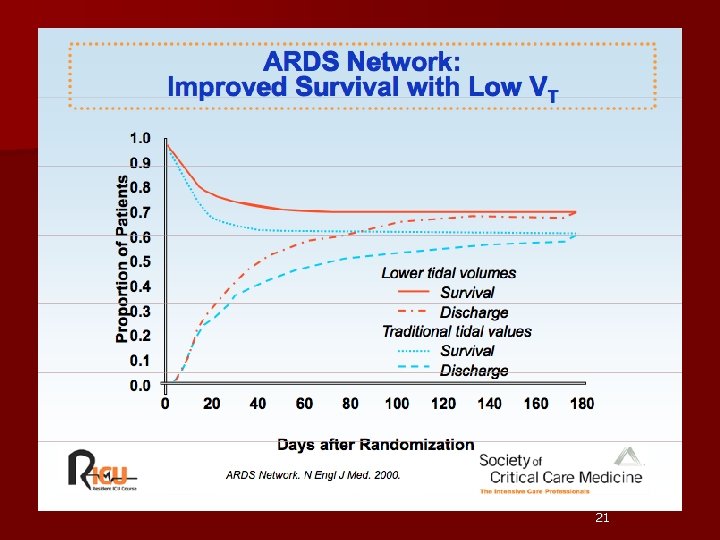
Management n In 1990, Hickling et al. : improved mortality w/ lower than “traditional” Vt n ARMA (Acute Respiratory Distress Syndrome Network Low Tidal Volume) trial: – limited Vt & plateau pressures compared to higher values § result: reduction in mortality from 40% to 31% n Considered Standard: Vt = 6– 8 m. L/kg ideal body wt & plateau pressure <30 cm H 2 O – Strategy associated with: § Pa. O 2/Fi. O 2 lower § High RR prevented hypercapnia § less organ failures § reduction in IL-6 and IL-8 levels § ~ 10% mortality reduction Hickling KG, et al. , Intensive Care Med. 1990; 16(6): 372– 377. ARDS Network. N Engl J Med. 2000. Hough CL, et al. , Critical Care Med 2005. 19
Non-Ventilatory Base Strategies n Inhaled Nitric Oxide – selectively vasodilates pulmonary capillaries – anti-inflammatory properties n Prone Positioning n Steroids: ? controversial n Further Investigations: – Liquid Ventilation – Surfactant Davis JW. et al, J Trauma. 2007 May; 62(5): 1201 -6. 20
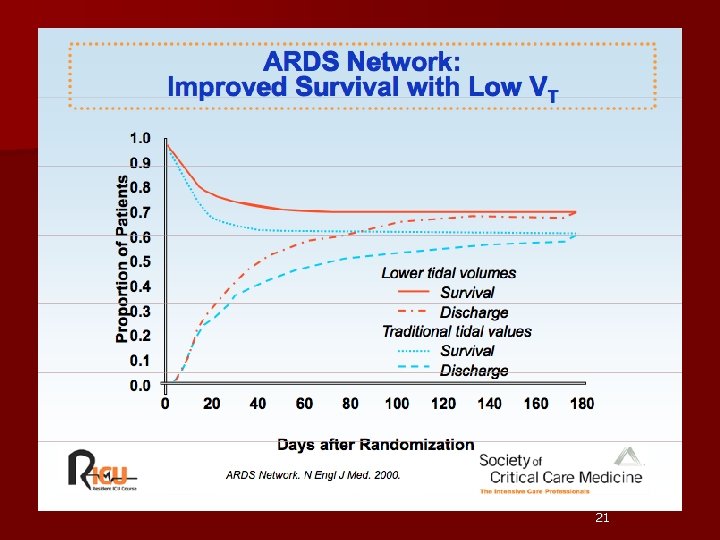
21
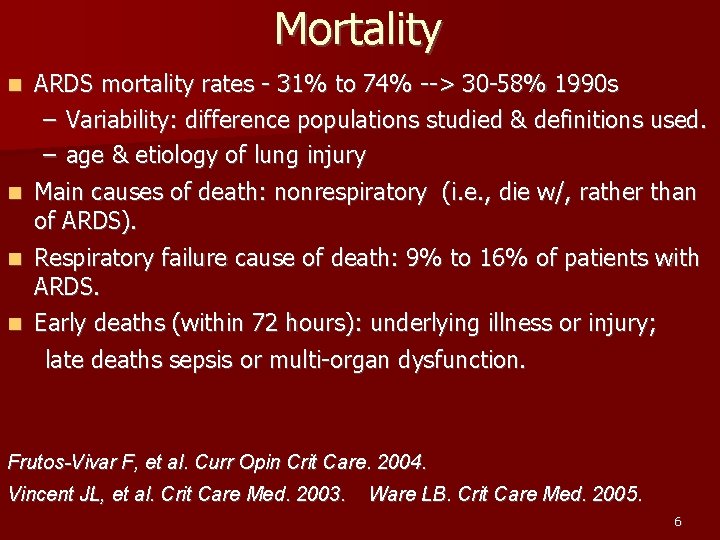
Mortality n ARDS mortality rates - 31% to 74% --> 30 -58% 1990 s – Variability: difference populations studied & definitions used. – age & etiology of lung injury Main causes of death: nonrespiratory (i. e. , die w/, rather than of ARDS). n Respiratory failure cause of death: 9% to 16% of patients with ARDS. n Early deaths (within 72 hours): underlying illness or injury; n late deaths sepsis or multi-organ dysfunction. Frutos-Vivar F, et al. Curr Opin Crit Care. 2004. Vincent JL, et al. Crit Care Med. 2003. Ware LB. Crit Care Med. 2005. 6

One-year Outcomes in Survivors of ARDS Persistent functional limitation • Extrapulmonary diseases (primarily): Muscle wasting and weakness (corticosteroid-induced & critical-illness-associated myopathy), • Intrinsic pulmonary morbidity (5%): Bronchiolitis obliterans organizing pneumonia Herridge MS, et al. N Engl J Med. 2003. 18

Long term outcomes n Outcomes variable n Lung mechanics may return to normal 1 year – gas exchange abnormalities may persist n Spirometry normal at 6 months n Mild to moderate: Quality of Life n 78% patients return to work Mc. Hugh LG, et al. Recovery of function in survivors of the acute respiratory distress syndrome. Am J Respir Crit Care Med. 1994; 150: 90. Herridge MS, Cheung AM, Tansey CM, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003; 348: 683 24
 Respiratory distress
Respiratory distress Respiratory distress nasal flaring
Respiratory distress nasal flaring Respiratory distress
Respiratory distress Protective reflexes
Protective reflexes Respiratory zone vs conducting zone
Respiratory zone vs conducting zone Acute coronary syndrome
Acute coronary syndrome Acute radiation syndrome
Acute radiation syndrome Firas mussa md
Firas mussa md Grading of meconium stained liquor ppt
Grading of meconium stained liquor ppt Direct costs of financial distress
Direct costs of financial distress Distress words survival
Distress words survival Paragraph on stress
Paragraph on stress Featal distress
Featal distress Meaning of eustress
Meaning of eustress Suds thermometer
Suds thermometer Jenna alexis
Jenna alexis Emotional thermometer
Emotional thermometer Distress signal x1
Distress signal x1 Pearlin's theory of psychological distress
Pearlin's theory of psychological distress Message relay sample
Message relay sample Contoh distress
Contoh distress Meaning of eustress
Meaning of eustress What is a archetypes
What is a archetypes 6 senses
6 senses Causes of decreased fetal movement
Causes of decreased fetal movement