HYPER CALCEMIA Yazan Karim 2021 Pharmacy Candidate Roosevelt

- Slides: 44
HYPER CALCEMIA Yazan Karim 2021 Pharmacy Candidate Roosevelt University
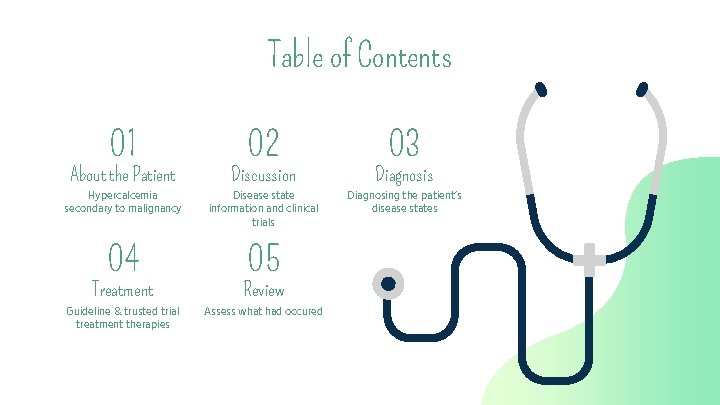
Table of Contents 01 02 03 About the Patient Discussion Diagnosis Hypercalcemia secondary to malignancy Disease state information and clinical trials Diagnosing the patient’s disease states 04 05 Treatment Review Guideline & trusted trial treatment therapies Assess what had occured
01 About the Patient Disease states, admission, and pertinent information
Our Patient - NB Reason of admission The patient states that she began having black colored stools 4 -5 days ago. Patient has never experienced GI bleeding before. She denies nausea/vomiting, constipation, straining w/ BMs, or abdominal pain. Our focus today We will specifically look at hypercalcemia in this patient. The pathophysiology, etiology, and treatment options. We will also look at relevant trials and guidelines about it. She has had hypercalcemia dating back to 08/2020.
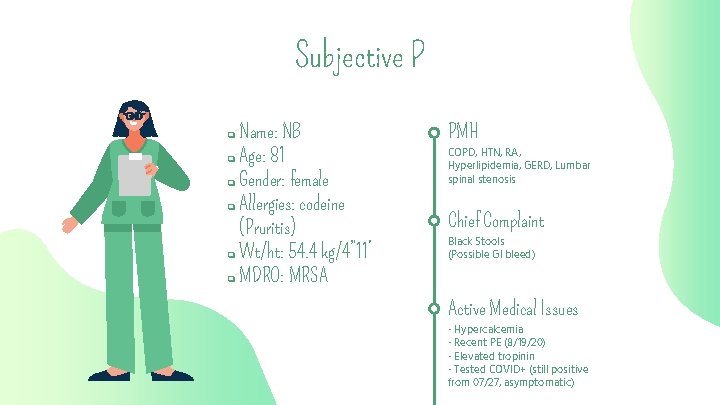
Subjective P Name: NB ❏ Age: 81 ❏ Gender: female ❏ Allergies: codeine (Pruritis) ❏ Wt/ht: 54. 4 kg/4” 11’ ❏ MDRO: MRSA ❏ PMH COPD, HTN, RA, Hyperlipidemia, GERD, Lumbar spinal stenosis Chief Complaint Black Stools (Possible GI bleed) Active Medical Issues - Hypercalcemia - Recent PE (8/19/20) - Elevated tropinin - Tested COVID+ (still positive from 07/27, asymptomatic)
Family History Father Mother Brother Glaucoma, COPD Heart disease, cancer (esophageal) Cancer – Lung / Head & neck
Social History - Former smoker: 1 PPD x 30 years - Alochol use: Yes, occasionally (no amount listed) - Illicit drug use: No - Caffeine: N/A
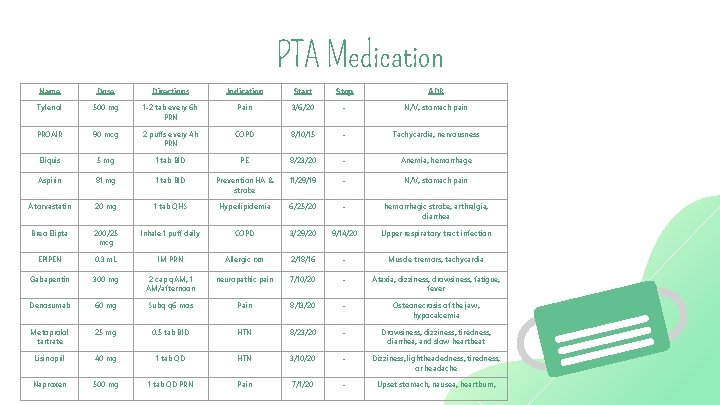
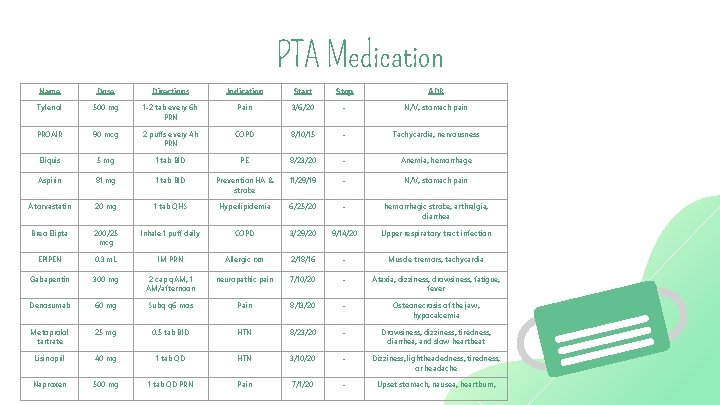
PTA Medication Name Dose Directions Indication Start Stop ADR Tylenol 500 mg 1 -2 tab every 6 h PRN Pain 3/6/20 - N/V, stomach pain PROAIR 90 mcg 2 puffs every 4 h PRN COPD 8/10/15 - Tachycardia, nervousness Eliquis 5 mg 1 tab BID PE 8/23/20 - Anemia, hemorrhage Aspirin 81 mg 1 tab BID Prevention HA & stroke 11/29/19 - N/V, stomach pain Atorvastatin 20 mg 1 tab QHS Hyperlipidemia 6/25/20 - hemorrhagic stroke, arthralgia, diarrhea Breo Elipta 200/25 mcg Inhale 1 puff daily COPD 3/29/20 9/14/20 Upper respiratory tract infection EPIPEN 0. 3 m. L IM PRN Allergic rxn 2/18/16 - Muscle tremors, tachycardia Gabapentin 300 mg 2 cap q. AM, 1 AM/afternoon neuropathic pain 7/10/20 - Ataxia, dizziness, drowsiness, fatigue, fever Denosumab 60 mg Subq q 6 mos Pain 8/13/20 - Osteonecrosis of the jaw, hypocalcemia Metoprolol tartrate 25 mg 0. 5 tab BID HTN 8/23/20 - Drowsiness, dizziness, tiredness, diarrhea, and slow heartbeat Lisinopril 40 mg 1 tab QD HTN 3/10/20 - Dizziness, lightheadedness, tiredness, or headache Naproxen 500 mg 1 tab QD PRN Pain 7/1/20 - Upset stomach, nausea, heartburn,
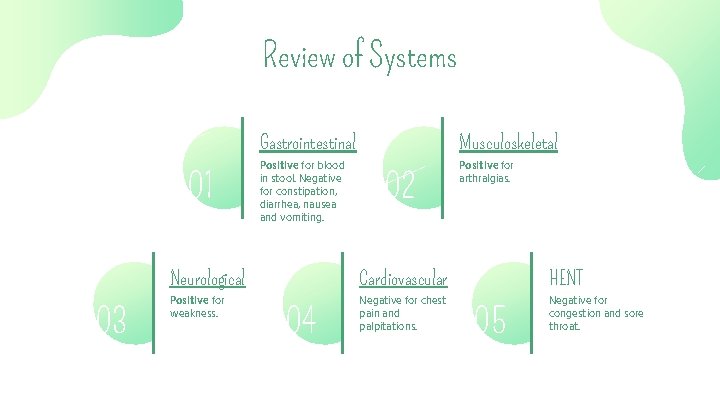
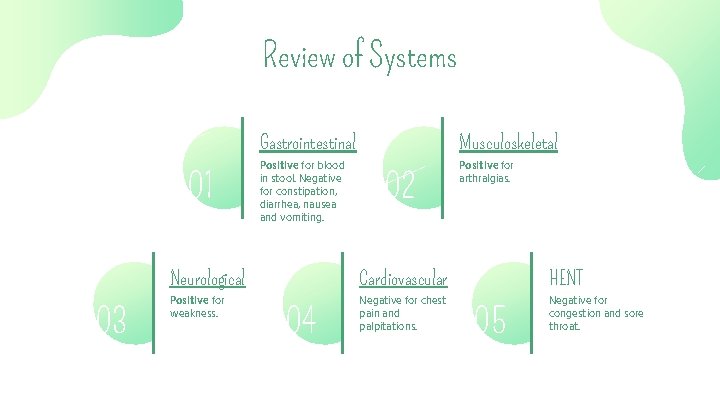
Review of Systems 01 03 Gastrointestinal Musculoskeletal Positive for blood in stool. Negative for constipation, diarrhea, nausea and vomiting. Positive for arthralgias. 02 Neurological Cardiovascular HENT Positive for weakness. Negative for chest pain and palpitations. Negative for congestion and sore throat. 04 05
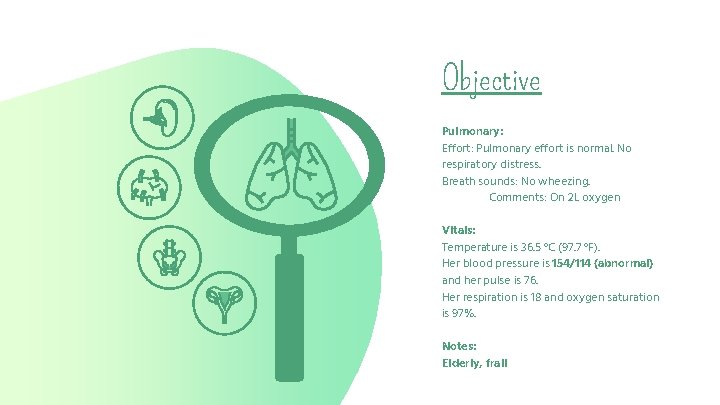
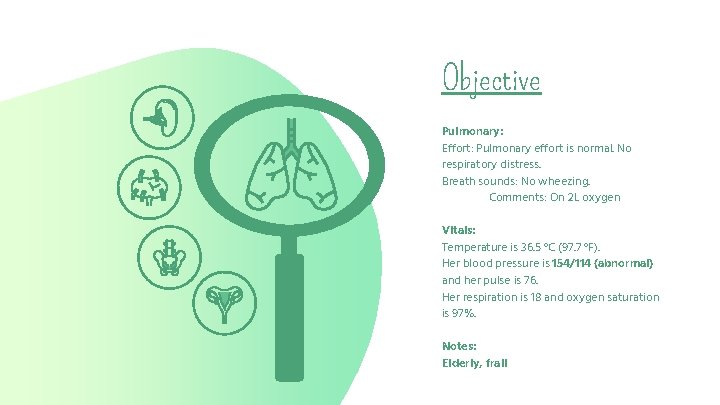
Objective Pulmonary: Effort: Pulmonary effort is normal. No respiratory distress. Breath sounds: No wheezing. Comments: On 2 L oxygen Vitals: Temperature is 36. 5 °C (97. 7 °F). Her blood pressure is 154/114 (abnormal) and her pulse is 76. Her respiration is 18 and oxygen saturation is 97%. Notes: Elderly, frail
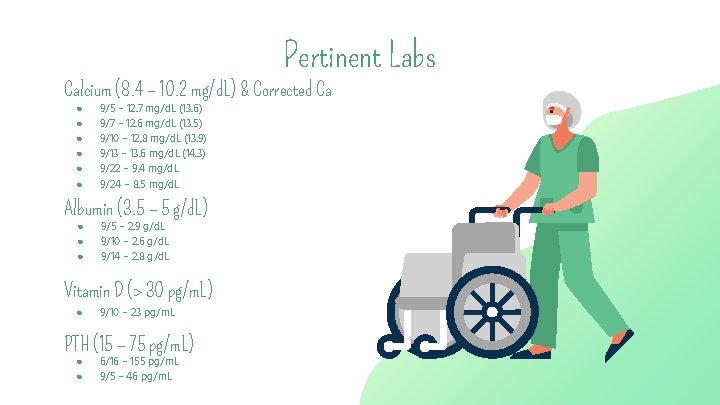
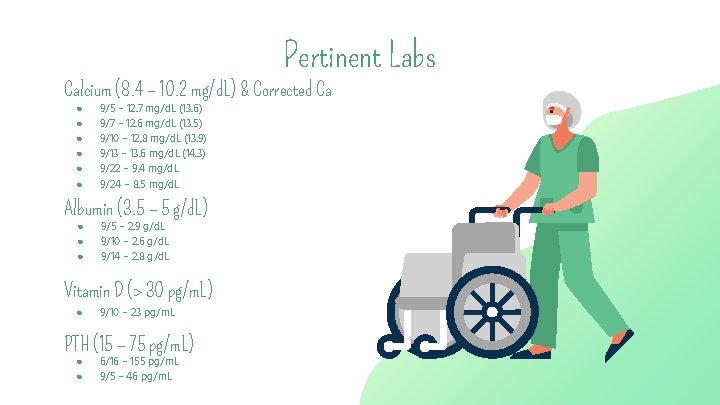
Pertinent Labs Calcium (8. 4 – 10. 2 mg/d. L) & Corrected Ca ● ● ● 9/5 – 12. 7 mg/d. L (13. 6) 9/7 – 12. 6 mg/d. L (13. 5) 9/10 – 12. 8 mg/d. L (13. 9) 9/13 – 13. 6 mg/d. L (14. 3) 9/22 – 9. 4 mg/d. L 9/24 – 8. 5 mg/d. L Albumin (3. 5 – 5 g/d. L) ● ● ● 9/5 – 2. 9 g/d. L 9/10 – 2. 6 g/d. L 9/14 – 2. 8 g/d. L Vitamin D (> 30 pg/m. L) ● 9/10 – 23 pg/m. L PTH (15 – 75 pg/m. L) ● ● 6/16 – 155 pg/m. L 9/5 – 46 pg/m. L
Hypercalcemia Disease State 1
Role of Calcium in the Body • Preservation and function of cell membranes • Propagation of neuromuscular activity • Regulation of endocrine and exocrine secretory functions • Blood coagulation cascade • Platelet adhesion process • Bone metabolism • Muscle cell excitation/contraction coupling • Mediation of the electrophysiologic slowchannel response in cardiac and smooth-muscle tissue Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
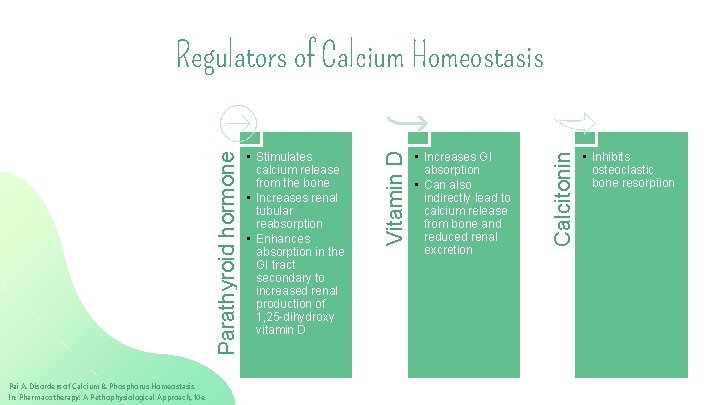
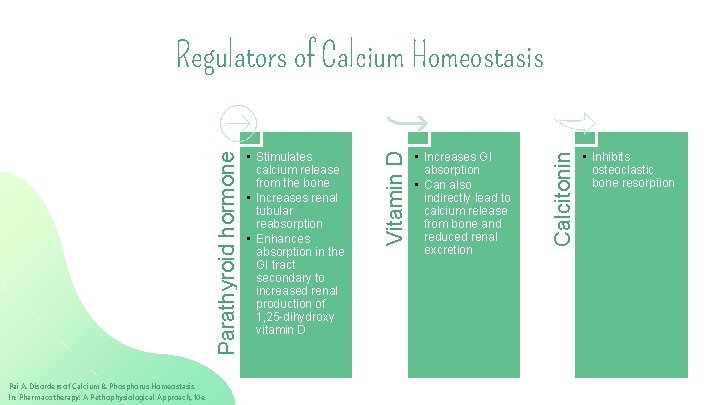
Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e • Increases GI absorption • Can also indirectly lead to calcium release from bone and reduced renal excretion Calcitonin • Stimulates calcium release from the bone • Increases renal tubular reabsorption • Enhances absorption in the GI tract secondary to increased renal production of 1, 25 -dihydroxy vitamin D Vitamin D Parathyroid hormone Regulators of Calcium Homeostasis • Inhibits osteoclastic bone resorption
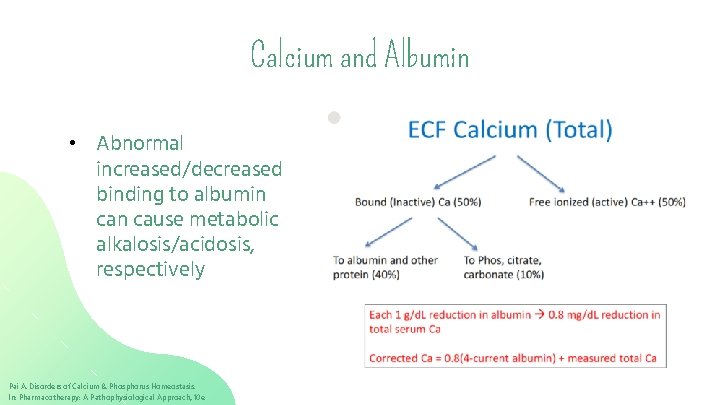
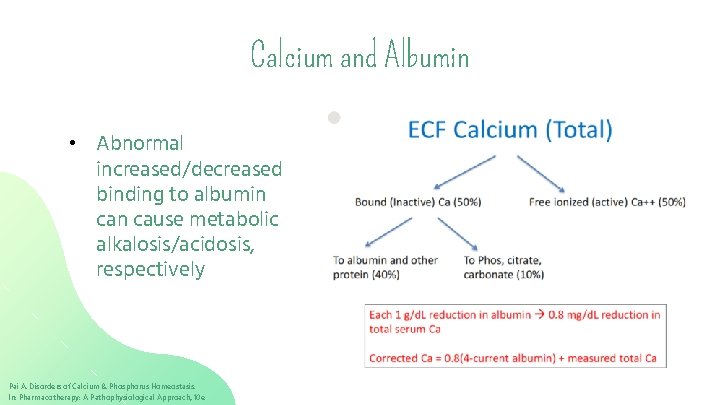
Calcium and Albumin • Abnormal increased/decreased binding to albumin cause metabolic alkalosis/acidosis, respectively Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
Assessment #1 • FS is 58 F admitted to the ER and her lab values are Ca: 7. 8 mg/d. L Albumin: 2. 5 g/d. L • What is her corrected calcium? A) 8. 5 B) 9 C) 9. 5 D) 10 Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
Definitions & Etiologies • Total serum calcium more than 10. 5 mg/d. L • Most common causes of hypercalcemia are cancer (15 -70% of cancer patients at some point in their disease) and primary hyperparathyroidism • Other causes of chronic hypercalcemia include medications, endocrine and granulomatous disorders, physical immobilization, high boneturnover states (adolescence and Paget disease), and rhabdomyolysis Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
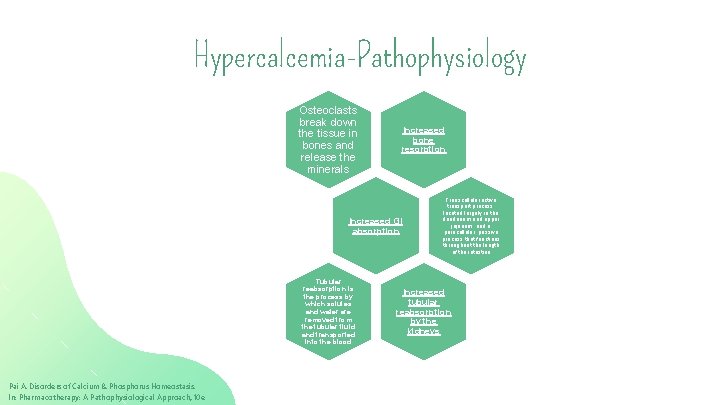
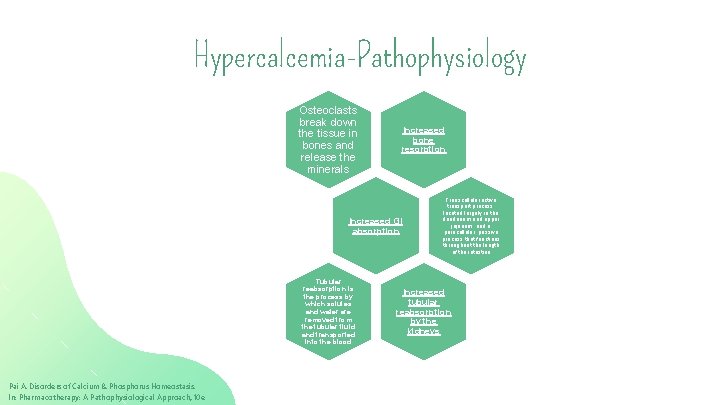
Hypercalcemia-Pathophysiology Osteoclasts break down the tissue in bones and release the minerals Increased bone resorption Increased GI absorption Tubular reabsorption is the process by which solutes and water are removed from the tubular fluid and transported into the blood Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e Transcellular active transport process, located largely in the duodenum and upper jejunum; and a paracellular, passive process that functions throughout the length of the intestine Increased tubular reabsorption by the kidneys
Hypercalcemia-Pathophysiology in Malignancy • • • Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e Tumors secrete PTH-related protein (PTHr. P), which binds to the PTH receptors in bone and renal tissues, leading to increased bone resorption and renal tubular reabsorption Tumors can also secrete substances such as vitamin D, transforming growth factor, interleukins, prostaglandins, interferon, tumor necrosis factor, and granulocyte-macrophage colony-stimulating factor, which are associated with the development of hypercalcemia Most frequent types of malignancy associated with hypercalcemia are carcinomas of the lung and breast
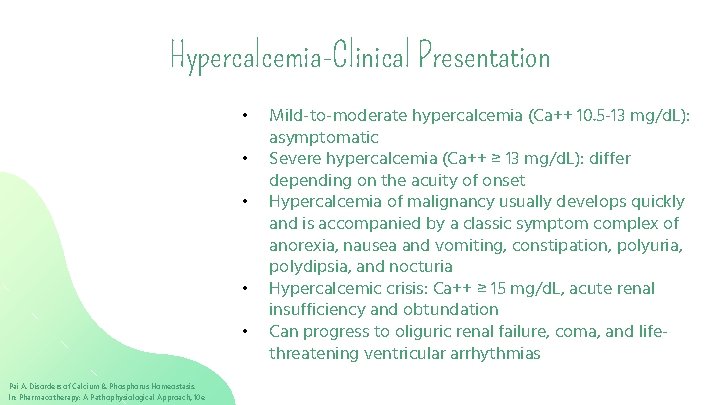
Hypercalcemia-Clinical Presentation • • • Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e Mild-to-moderate hypercalcemia (Ca++ 10. 5 -13 mg/d. L): asymptomatic Severe hypercalcemia (Ca++ ≥ 13 mg/d. L): differ depending on the acuity of onset Hypercalcemia of malignancy usually develops quickly and is accompanied by a classic symptom complex of anorexia, nausea and vomiting, constipation, polyuria, polydipsia, and nocturia Hypercalcemic crisis: Ca++ ≥ 15 mg/d. L, acute renal insufficiency and obtundation Can progress to oliguric renal failure, coma, and lifethreatening ventricular arrhythmias
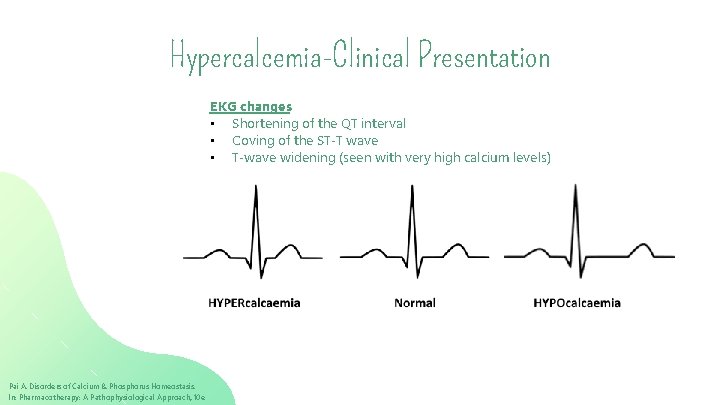
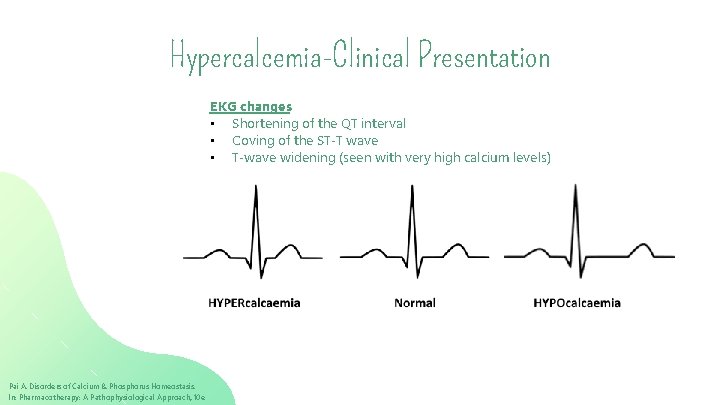
Hypercalcemia-Clinical Presentation EKG changes • Shortening of the QT interval • Coving of the ST-T wave • T-wave widening (seen with very high calcium levels) Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
Chronic Hypercalcemia-Complications • Metastatic calcification • Hypercalciuria • Chronic renal insufficiency secondary to interstitial nephroncalcinosis • Calcium and/or calcium–phosphorus complex deposition in blood vessels and multiple organs • Calcium deposits in atherosclerotic lesions contribute to cardiac disease Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
Hypercalcemia-Treatment • Indication for treatment are dependent on Severity of hypercalcemia Acuity of hypercalcemia Requiring emergent treatment • Goals of therapy Reverse signs and symptoms Restore normocalcemia (hours-days) Underlying cause of hypercalcemia Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
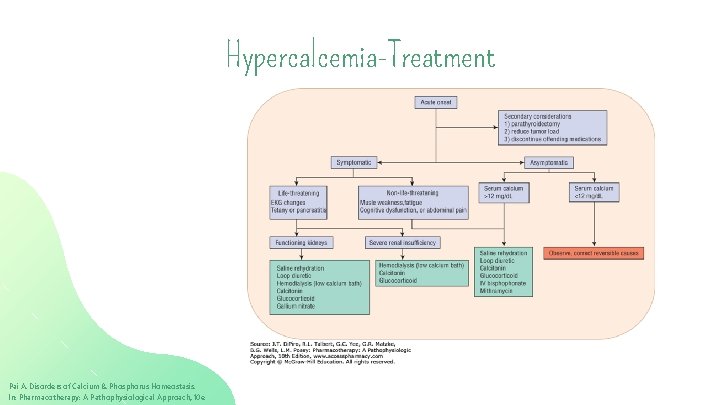
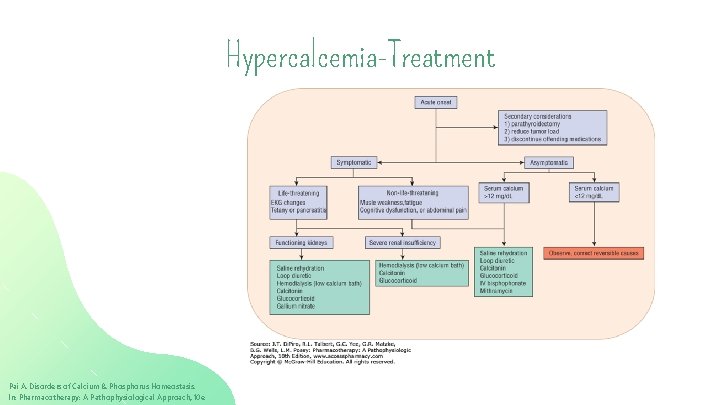
Hypercalcemia-Treatment Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
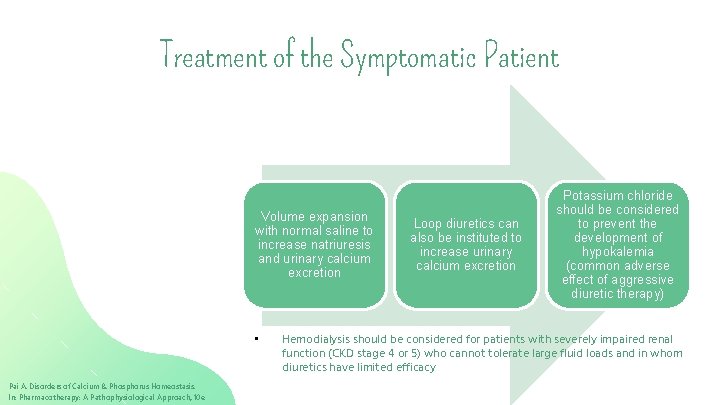
Treatment of the Symptomatic Patient Volume expansion with normal saline to increase natriuresis and urinary calcium excretion • Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e Loop diuretics can also be instituted to increase urinary calcium excretion Potassium chloride should be considered to prevent the development of hypokalemia (common adverse effect of aggressive diuretic therapy) Hemodialysis should be considered for patients with severely impaired renal function (CKD stage 4 or 5) who cannot tolerate large fluid loads and in whom diuretics have limited efficacy
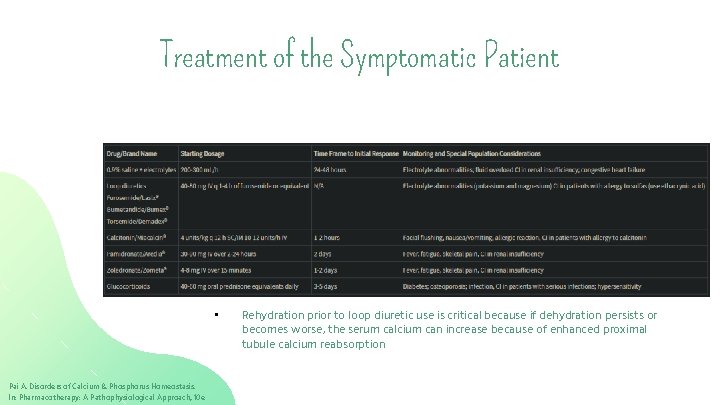
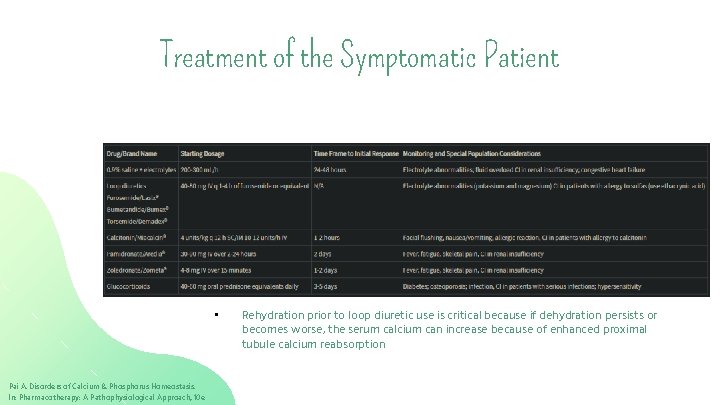
Treatment of the Symptomatic Patient • Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e Rehydration prior to loop diuretic use is critical because if dehydration persists or becomes worse, the serum calcium can increase because of enhanced proximal tubule calcium reabsorption
Treatment of the Asymptomatic Patient Treatment Considerations • Comorbid disease states (such as renal insufficiency, diabetes, infection, etc) • How quickly calcium needs to be decreased • Ease of Use • Cost of therapy Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
Hypercalcemia-Treatment 2 Calcitonin • Indicated for rapid decrease of calcium for patients in whom saline hydration is contraindicated (such as CHF or moderatesevere renal insufficiency) • Decreases serum calcium concentrations, primarily by inhibiting bone resorption but can also reduce renal tubular reabsorption of calcium • Rapid onset of action and reduces calcium levels in 1 -2 days • May be administered subcutaneously, intramuscularly or intranasally (synthetic; has lower potency and shorter duration) • Adverse effects mainly seen with IV administration, which is no longer recommended; tachyphylaxis can be seen if therapy continues for > 4 months • Test dose prior to first dose is recommended ( to test for allergic reaction) Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
Hypercalcemia-Treatment 2 Bisphonates (pamidronate and zoledronic acid) • First line therapy for cancer-associated hypercalcemia • Block bone resorption by rendering the hydroxyapatite crystal of bone mineral resistant to hydrolysis by phosphatases, inhibiting osteoclast precursors from attaching to the mineralized matrix, thus blocking their transformation into mature functioning osteoclasts • Onset of action: effects seen within 2 days with greatest effect seen at about 7 days after therapy • Duration of therapy: usually 2 -3 weeks (up to 4 -5 weeks with zoledronic acid) Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
Hypercalcemia-Treatment 2 Bisphonates (continued) • Dosing 1) Pamidronate is 30 to 90 mg as an IV infusion given over 2 to 24 hours 2) Zoledronic acid 4 -8 mg given over 15 minutes • Adverse Effects Fever (with IV therapy) Use caution in patients with moderatesevere renal insufficiency Osteonecrosis of the jaw Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
Hypercalcemia-Treatment 2 Denosumab • Monoclonal antibody that inhibits the receptor activator of nuclear factor kappa-light-chain-enhancer of activated B cells (NF -κB) ligand (RANKL) thereby preventing osteoclast formation leading to decreased bone resorption and increased bone mass • Onset of action : Effects seen at 9 days post-therapy with maximum effect seen at ~23 days post-therapy • Duration of therapy: appx 100 days • Dosing: 120 mg subcutaneously every 4 weeks (give additional doses of 120 mg on day 8 and 15 during the first month) • Adverse effects: Osteonecrosis of the jaw, severe, symptomatic hypocalcemia has been reported in CKD Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
Hypercalcemia-Treatment 2 Corticosteroids • Prednisone or an equivalent have been used • Work by reducing GI calcium absorption • Onset of action: 3 -5 days for normalized serum calcium levels • Dosing: 40 -60 mg daily of prednisone (or equivalent) • Disadvantages of corticosteroid therapy are its relatively slow onset of action and the potential for diabetes mellitus, osteoporosis, and increased susceptibility to infection Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
Hypercalcemia-Treatment 2 Cinacalcet • Binds to the calcium sensing receptor and increases the sensitivity for receptor activation by extracellular calcium resulting in reduced PTH and serum calcium concentrations • Onset of action: ~ 1 week • Dosing: starting dose is 30 mg PO BID; dosage is titrated every 2 to 4 weeks in 30 -mg increments until the desired serum calcium level is achieved • Adverse effects: nausea, vomiting, diarrhea, fatigue Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
Treatment of Nephrolithiasis Chronic Hypercalciuria and Hypercalcemia • • • Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e Sodium citrate Prevents stone formation by alkalinizing the urine Need to be taken multiple times per day Thiazide diuretics Commonly used to prevent stone formation Decrease urinary calcium excretion Shock wave lithotripsy Disintegrate stones allowing for urinary removal Pain and expensive procedure
Assessment #2 • Signs and symptoms of hypocalcemia include: A) Fatigue, weakness, and lethargy B) Anorexia, nausea, and vomiting C) Irritability, confusion, and psychosis D) Impaired kidney function, kidney stones, and polyuria Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
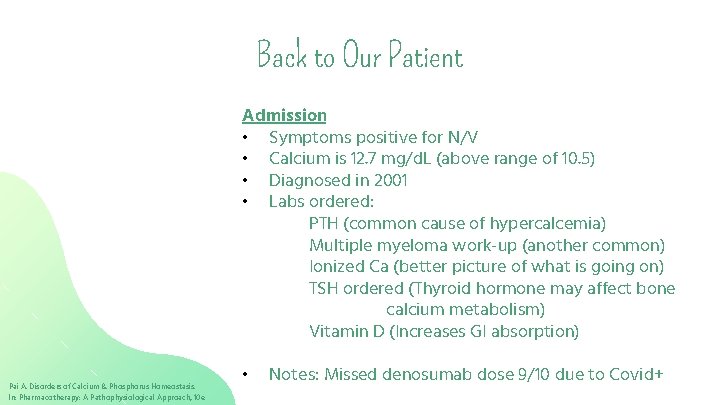
Back to Our Patient Admission • Symptoms positive for N/V • Calcium is 12. 7 mg/d. L (above range of 10. 5) • Diagnosed in 2001 • Labs ordered: PTH (common cause of hypercalcemia) Multiple myeloma work-up (another common) Ionized Ca (better picture of what is going on) TSH ordered (Thyroid hormone may affect bone calcium metabolism) Vitamin D (Increases GI absorption) Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e • Notes: Missed denosumab dose 9/10 due to Covid+
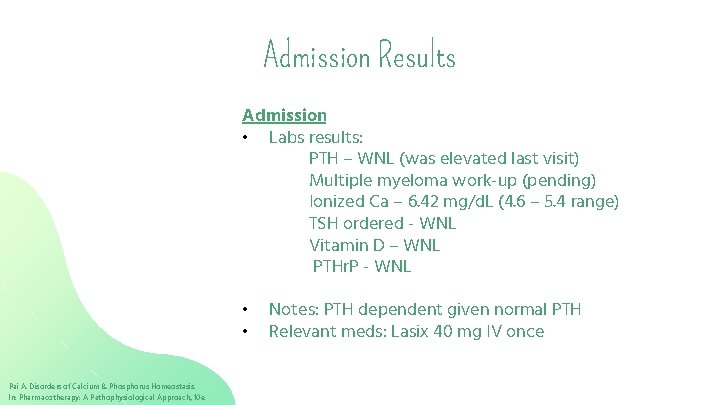
Admission Results Admission • Labs results: PTH – WNL (was elevated last visit) Multiple myeloma work-up (pending) Ionized Ca – 6. 42 mg/d. L (4. 6 – 5. 4 range) TSH ordered - WNL Vitamin D – WNL PTHr. P - WNL • • Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e Notes: PTH dependent given normal PTH Relevant meds: Lasix 40 mg IV once
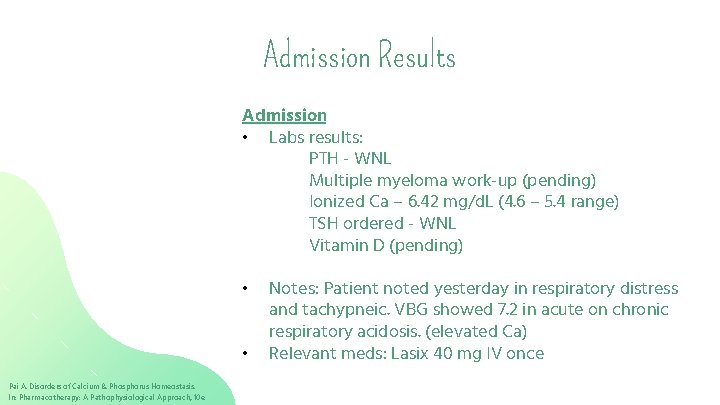
Admission Results Admission • Labs results: PTH - WNL Multiple myeloma work-up (pending) Ionized Ca – 6. 42 mg/d. L (4. 6 – 5. 4 range) TSH ordered - WNL Vitamin D (pending) • • Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e Notes: Patient noted yesterday in respiratory distress and tachypneic. VBG showed 7. 2 in acute on chronic respiratory acidosis. (elevated Ca) Relevant meds: Lasix 40 mg IV once
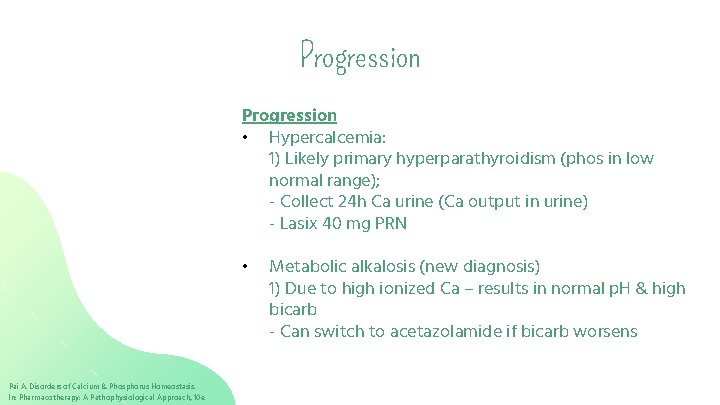
Progression • Hypercalcemia: 1) Likely primary hyperparathyroidism (phos in low normal range); - Collect 24 h Ca urine (Ca output in urine) - Lasix 40 mg PRN • Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e Metabolic alkalosis (new diagnosis) 1) Due to high ionized Ca – results in normal p. H & high bicarb - Can switch to acetazolamide if bicarb worsens
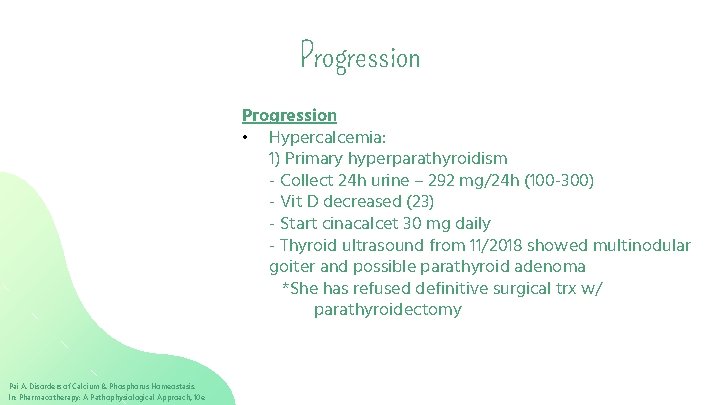
Progression • Hypercalcemia: 1) Primary hyperparathyroidism - Collect 24 h urine – 292 mg/24 h (100 -300) - Vit D decreased (23) - Start cinacalcet 30 mg daily - Thyroid ultrasound from 11/2018 showed multinodular goiter and possible parathyroid adenoma *She has refused definitive surgical trx w/ parathyroidectomy Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
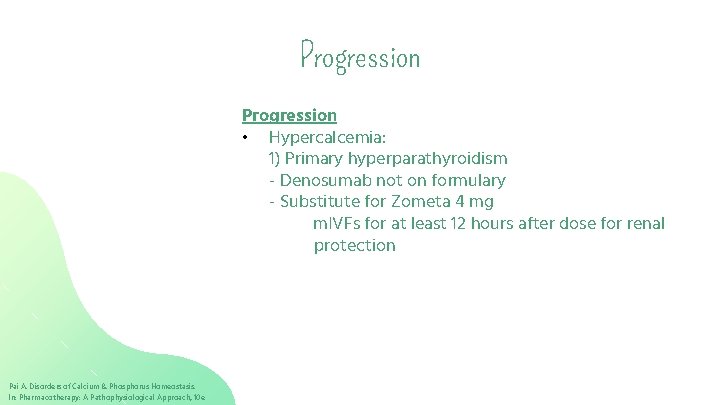
Progression • Hypercalcemia: 1) Primary hyperparathyroidism - Denosumab not on formulary - Substitute for Zometa 4 mg m. IVFs for at least 12 hours after dose for renal protection Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
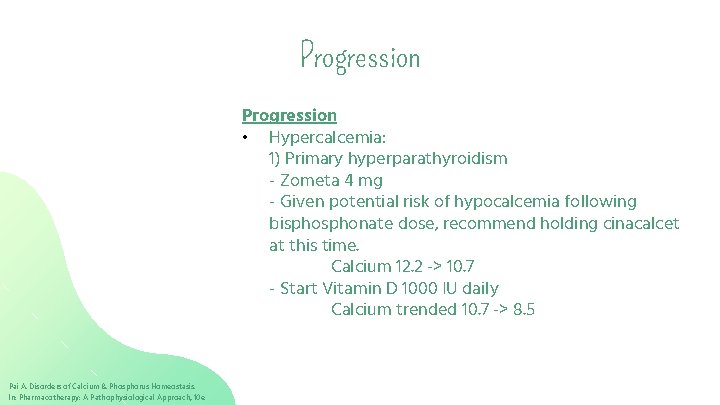
Progression • Hypercalcemia: 1) Primary hyperparathyroidism - Zometa 4 mg - Given potential risk of hypocalcemia following bisphonate dose, recommend holding cinacalcet at this time. Calcium 12. 2 -> 10. 7 - Start Vitamin D 1000 IU daily Calcium trended 10. 7 -> 8. 5 Pai A. Disorders of Calcium & Phosphorus Homeostasis. In: Pharmacotherapy: A Pathophysiological Approach, 10 e
Conclusions • Severe acute hypercalcemia can result in cardiac arrhythmias, whereas chronic hypercalcemia can lead to calcium deposition in soft tissues including blood vessels and the kidney. • The correction of hypercalcemia can include multiple pharmacotherapeutic modalities such as hydration, diuretics, bisphonates, and steroids, depending on the etiology and acuity of the hypercalcemia.

References ● Pai AA. Pharmacotherapy: A Pathophysiologic Approach, 11 e. Access. Pharmacy. https: //accesspharmacy. mhmedical. com/content. aspx? bookid=2577. Published 2020. Accessed September 25, 2020. ● Lexi-Drugs. Lexicomp. Wolters Kluwer Health, Inc. Riverwoods, IL. Available at http: //online. lexi. com. Accessed September 25, 2020.
 Yazan karim
Yazan karim Yazan karim
Yazan karim Material project
Material project Gazeteye yazı yazan haber toplayan kimse
Gazeteye yazı yazan haber toplayan kimse Karim dahia
Karim dahia Dr adiwarman karim
Dr adiwarman karim Contoh urf
Contoh urf Karim benali
Karim benali Prof. dr. karim fereidooni herkunft
Prof. dr. karim fereidooni herkunft Transitions for thesis statements
Transitions for thesis statements Cyk algorithm step by step
Cyk algorithm step by step Karim emile bitar
Karim emile bitar Riyas karim
Riyas karim Keistimewaan al quran
Keistimewaan al quran Karim daho
Karim daho Meneladani asmaul husna al karim
Meneladani asmaul husna al karim Dr azmat karim
Dr azmat karim Dr karim aref
Dr karim aref Al karim artinya
Al karim artinya Karim massoud
Karim massoud Rehnuma karim
Rehnuma karim Evelin karim aziz
Evelin karim aziz Image uml
Image uml Mining frequent patterns without candidate generation
Mining frequent patterns without candidate generation Candidate journey definition
Candidate journey definition Alien flight student program
Alien flight student program Candidate generation in apriori algorithm
Candidate generation in apriori algorithm Prinsip etika kandidat
Prinsip etika kandidat Inductive bias of candidate elimination algorithm
Inductive bias of candidate elimination algorithm Mining frequent patterns without candidate generation
Mining frequent patterns without candidate generation Candidate entry information checklist dse
Candidate entry information checklist dse Recruiter call script to client
Recruiter call script to client Define system analysis
Define system analysis Ibm talent gateway
Ibm talent gateway Gate.aon/candidate
Gate.aon/candidate Relational database design normalization
Relational database design normalization Nupoc salary
Nupoc salary The manchurian candidate
The manchurian candidate Websams ghs
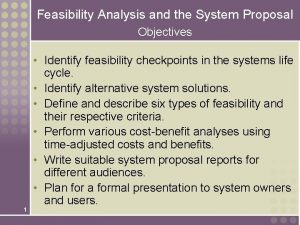
Websams ghs The main objectives of a detailed system proposal are to
The main objectives of a detailed system proposal are to Video phone block diagram
Video phone block diagram Usna candidate information system
Usna candidate information system Online proctored exams candidate guidelines peoplecert
Online proctored exams candidate guidelines peoplecert Candidate self service portal
Candidate self service portal The candidate-elimination algorithm represents the
The candidate-elimination algorithm represents the