Hepatitis Dr Minoo Saeidi Isfahan University of Medical


- Slides: 49
Hepatitis Dr. Minoo Saeidi Isfahan University of Medical Sciences
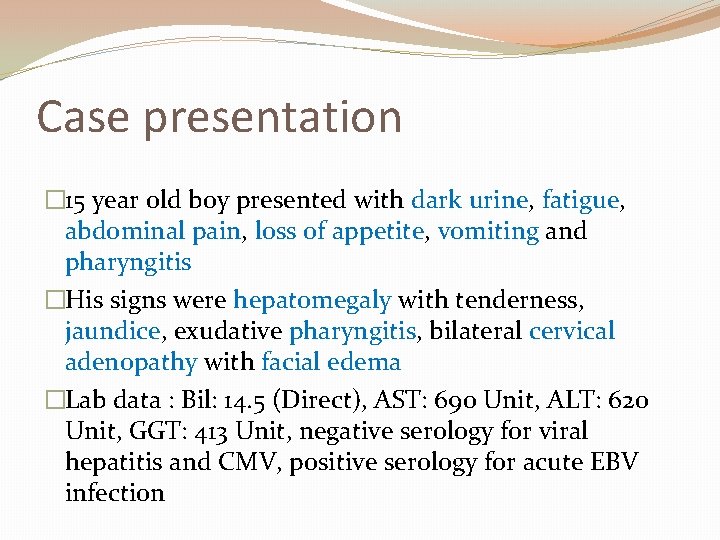
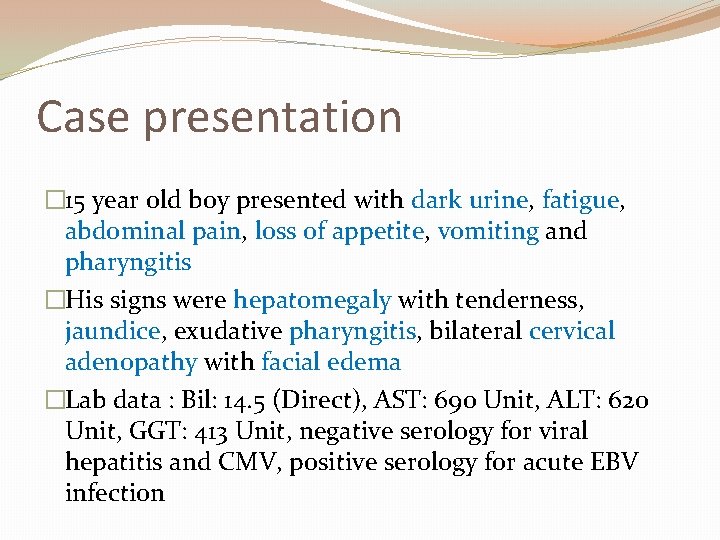
Case presentation � 15 year old boy presented with dark urine, fatigue, abdominal pain, loss of appetite, vomiting and pharyngitis �His signs were hepatomegaly with tenderness, jaundice, exudative pharyngitis, bilateral cervical adenopathy with facial edema �Lab data : Bil: 14. 5 (Direct), AST: 690 Unit, ALT: 620 Unit, GGT: 413 Unit, negative serology for viral hepatitis and CMV, positive serology for acute EBV infection
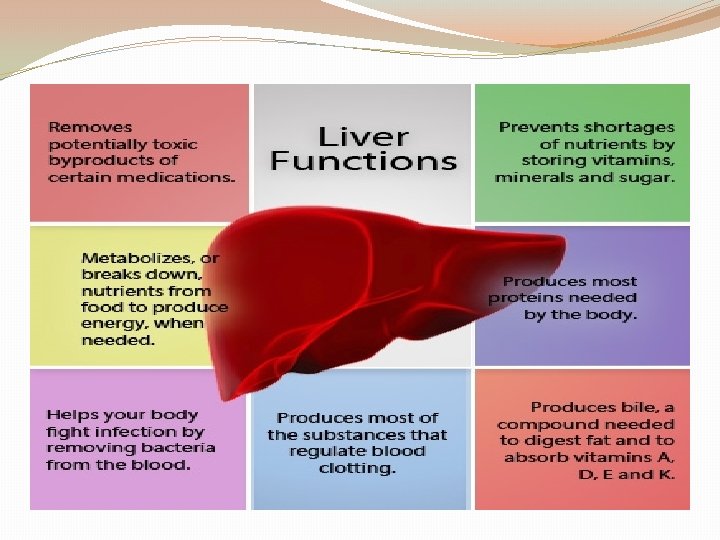
Definition �Presence of inflammatory cells in the liver �Elevated liver enzymes �Different causes (viruses, toxins, autoimmunity, drugs, shock, anoxia, Wilson, metabolic diseases) �Self limited or progressive �Acute or chronic
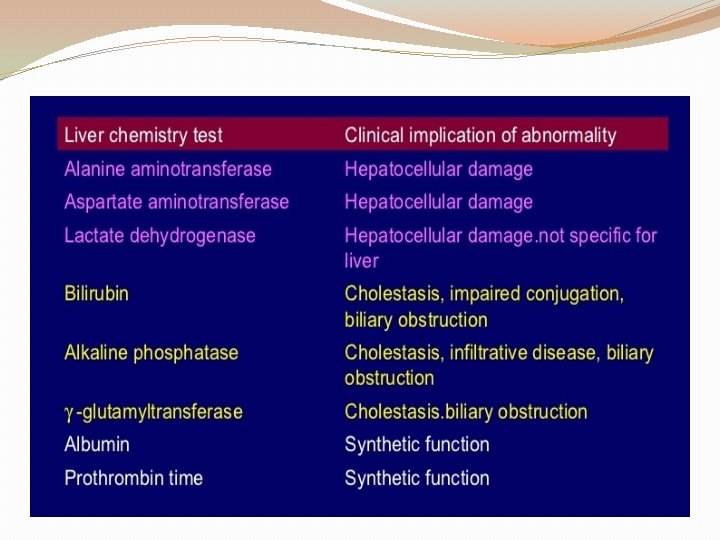
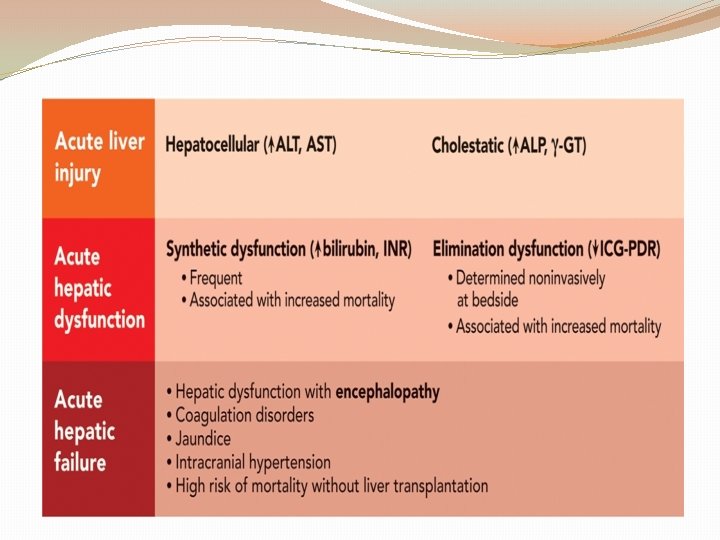
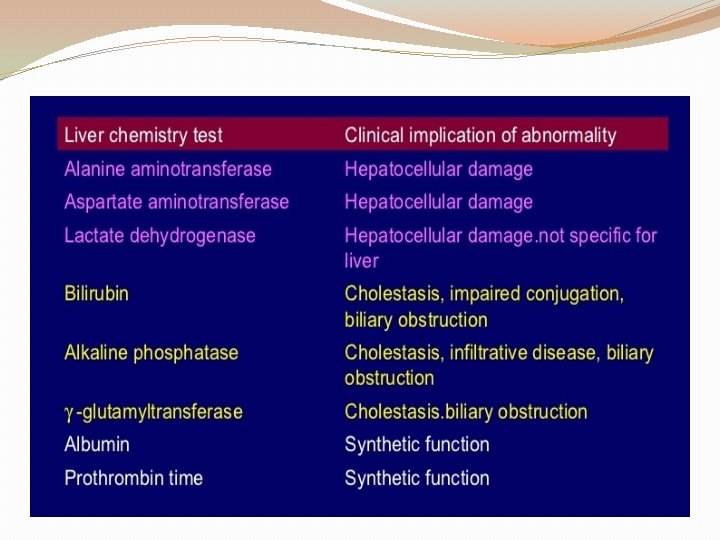
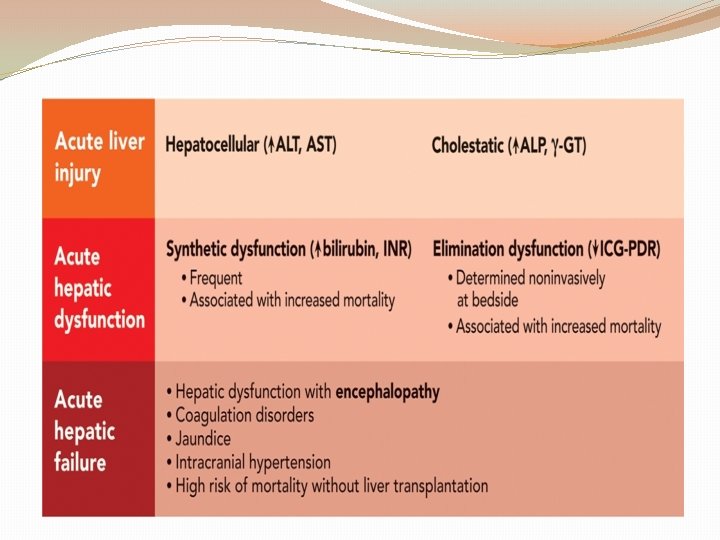
pathophysiology �Direct cellular injury that elevates serum liver enzyme levels �cholestasis that causes jaundice and hyperbilirubinemia �Inadequate liver function that lowers serum albumin levels and prolongs the prothrombin time (PT)
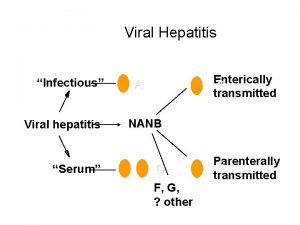
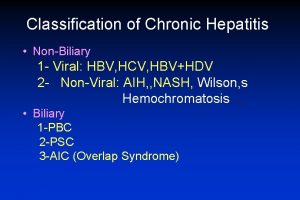
Causes �Acute (HAV, HEV, HBV, HCV, HDV, EBV, CMV, HSV, VZV, Adenovirus, Entrovirus, E coli, toxoplasmosis, leptospirosis, alcohol, Amantia toxin, paracetamol, autoimmunity, metabolic disorders like as Wilson) �Chronic (HBV, HCV, HDV, autoimmunity, nitrofurantoin, ketoconazole, isoniazid, metyldopa, alcohol, metabolic disorders like as Wilson, alfa 1 antitrypsin deficiency, galactosemia, tyrosinemia, IBD)
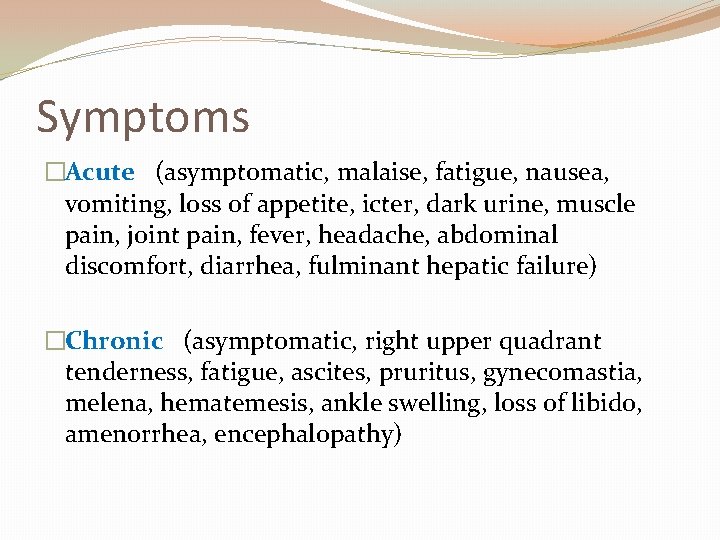
Symptoms �Acute (asymptomatic, malaise, fatigue, nausea, vomiting, loss of appetite, icter, dark urine, muscle pain, joint pain, fever, headache, abdominal discomfort, diarrhea, fulminant hepatic failure) �Chronic (asymptomatic, right upper quadrant tenderness, fatigue, ascites, pruritus, gynecomastia, melena, hematemesis, ankle swelling, loss of libido, amenorrhea, encephalopathy)
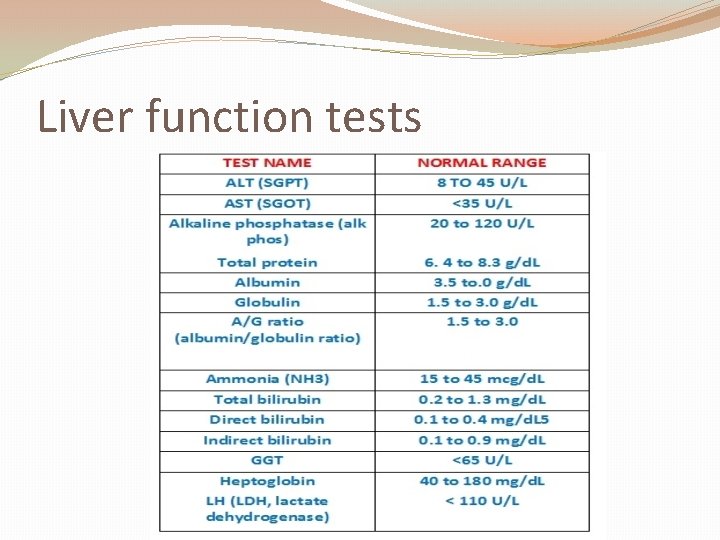
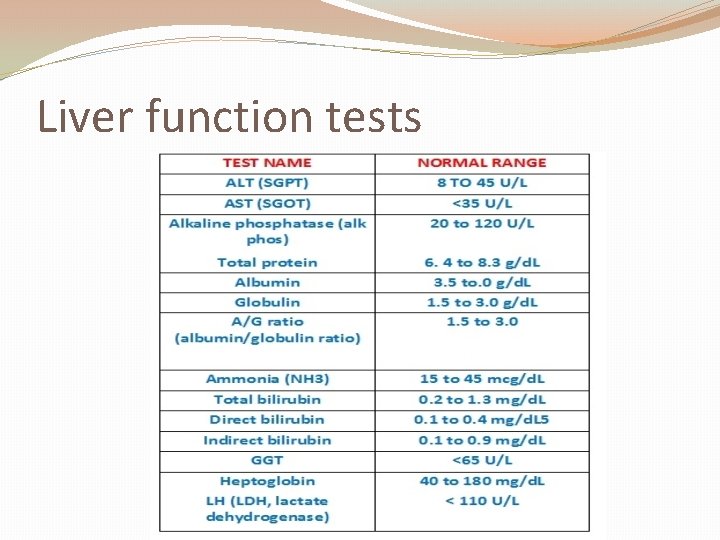
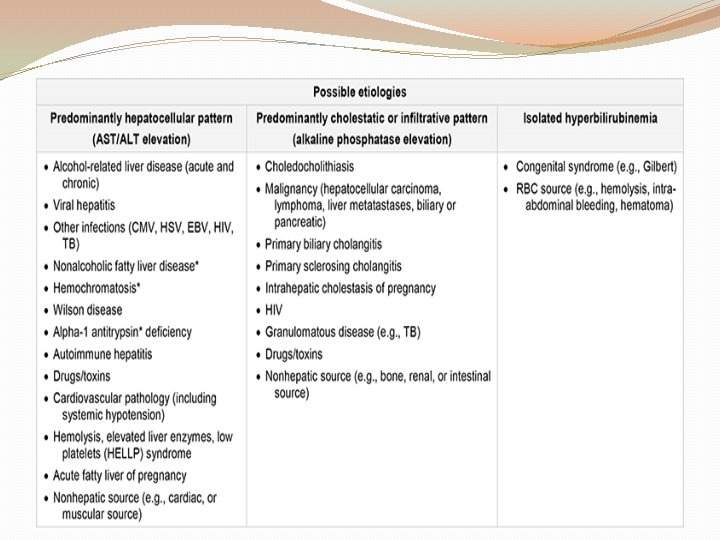
Liver function tests
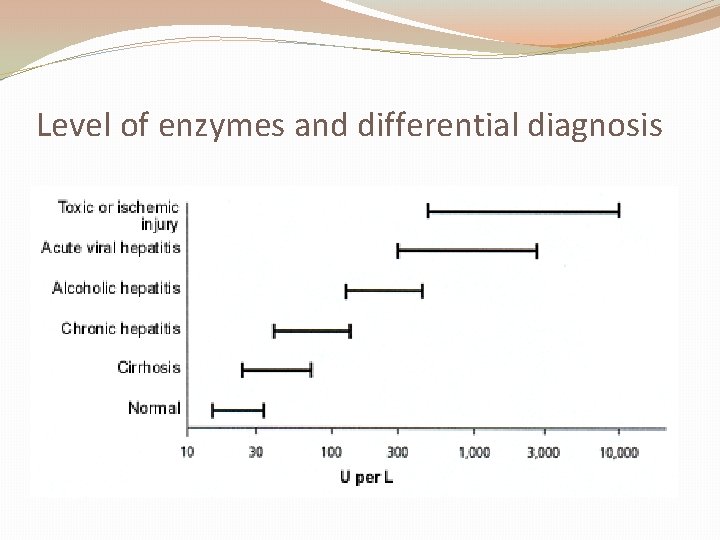
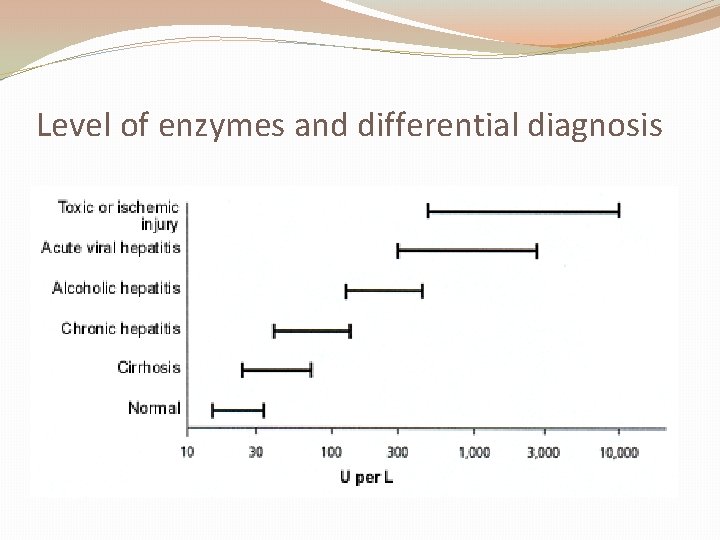
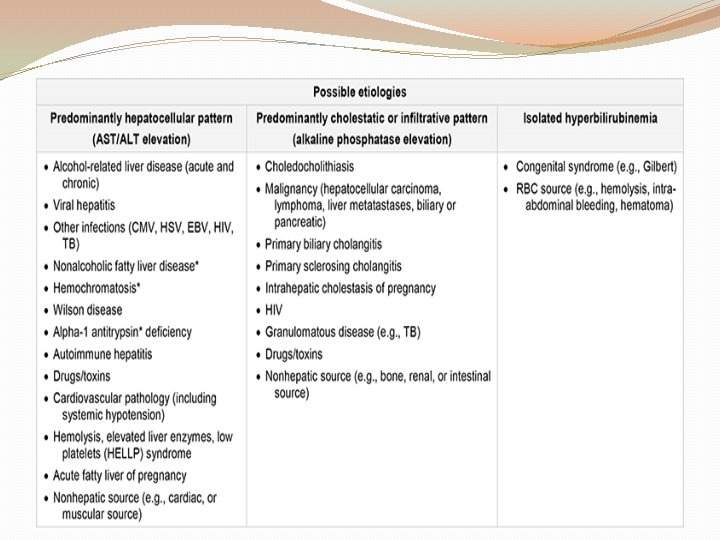
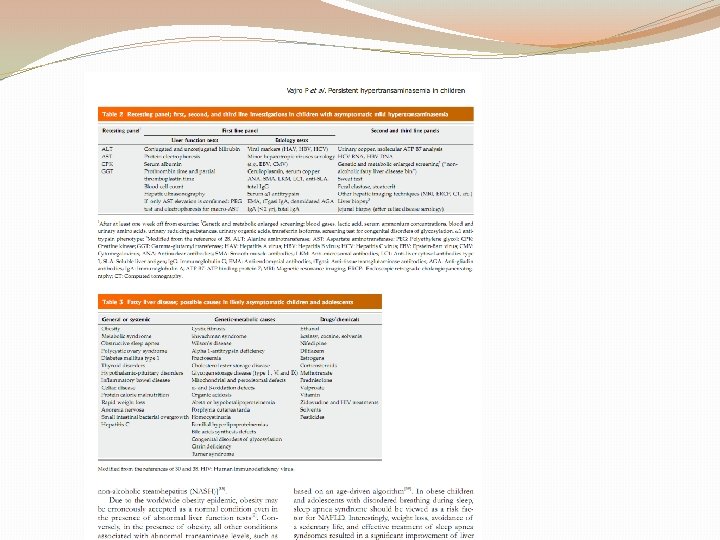
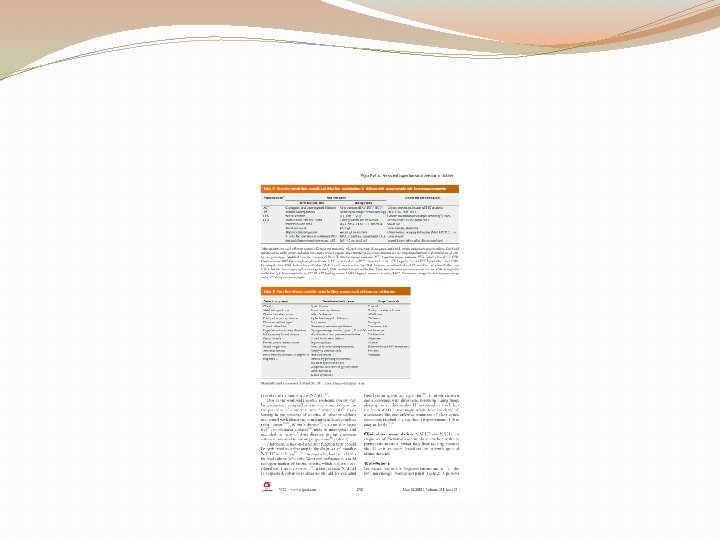
Level of enzymes and differential diagnosis
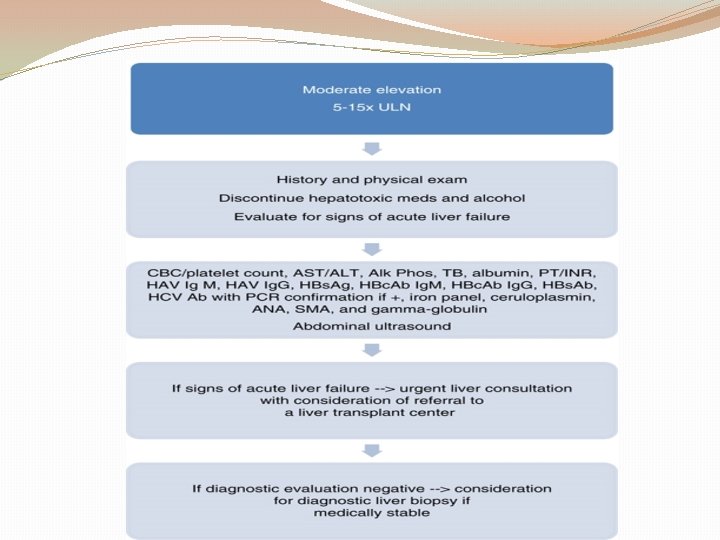
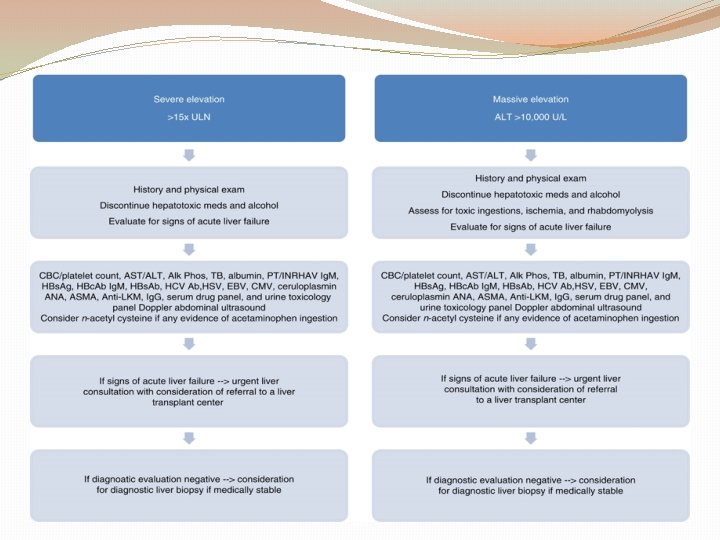
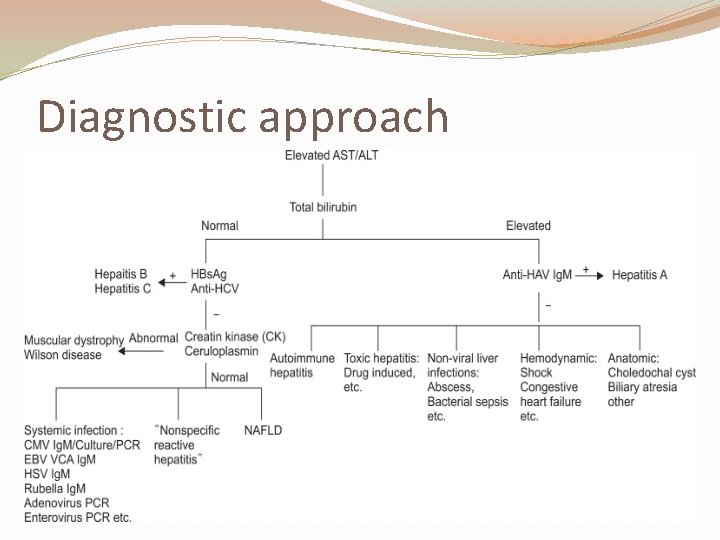
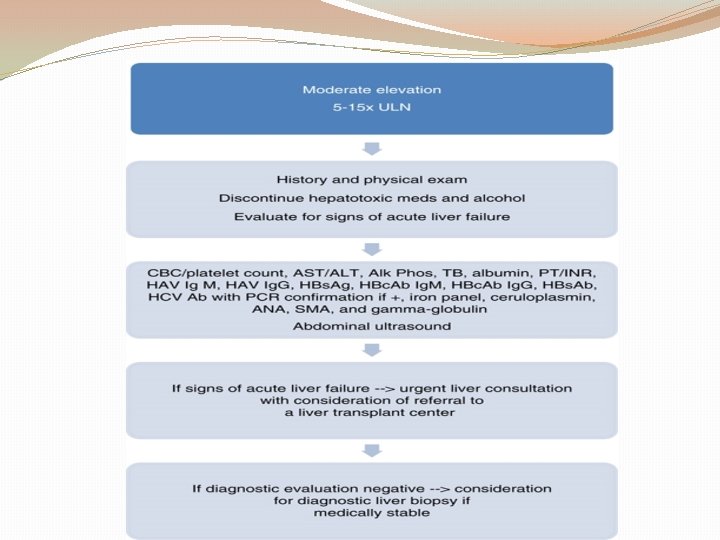
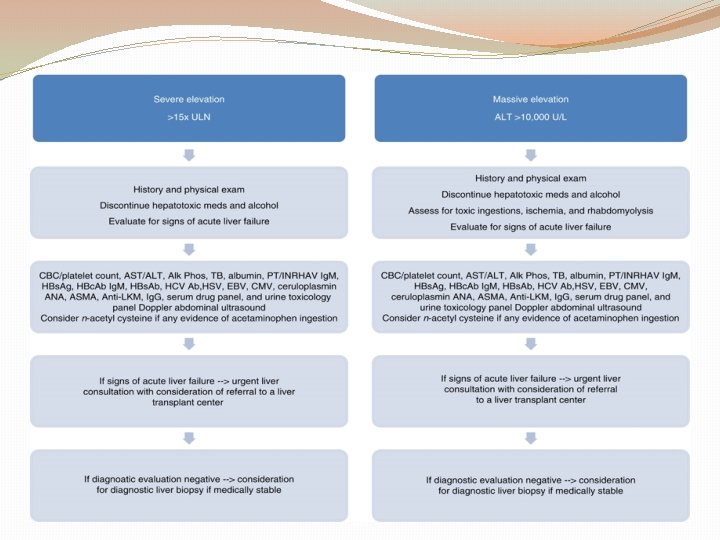
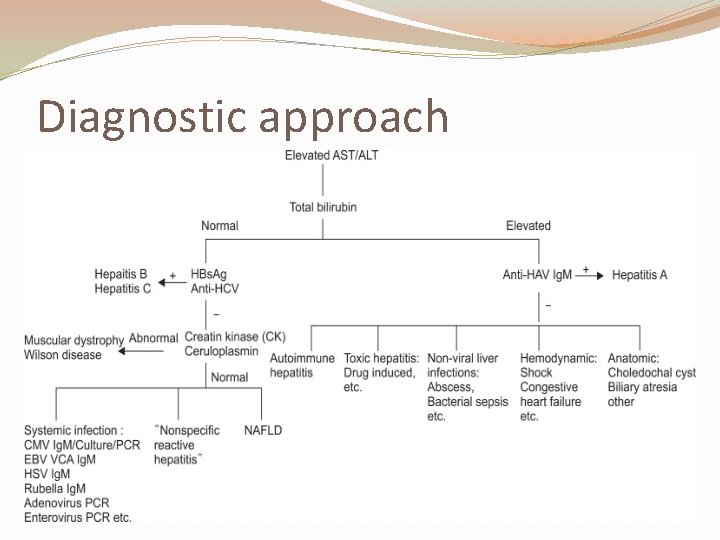
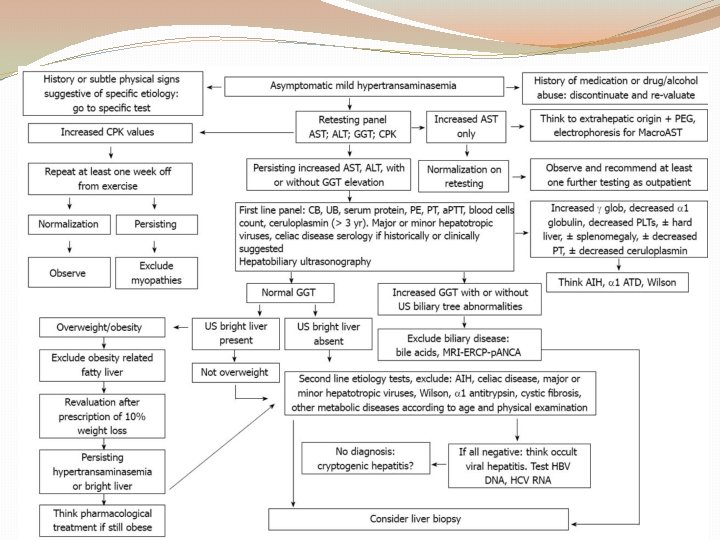
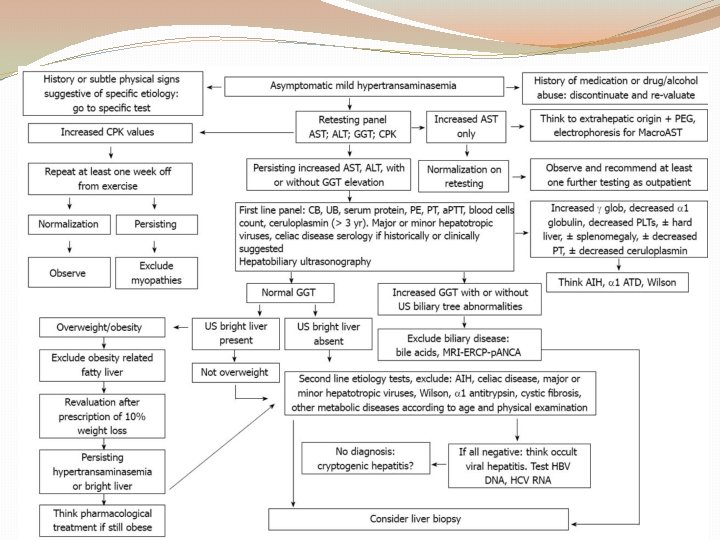
Diagnostic approach
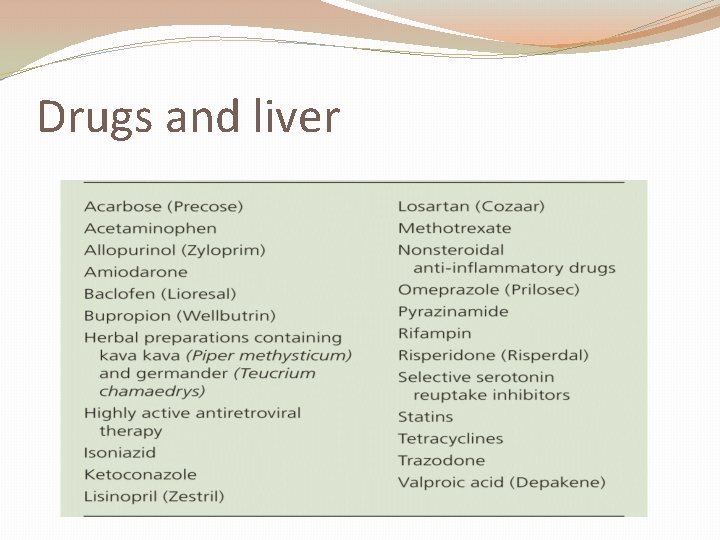
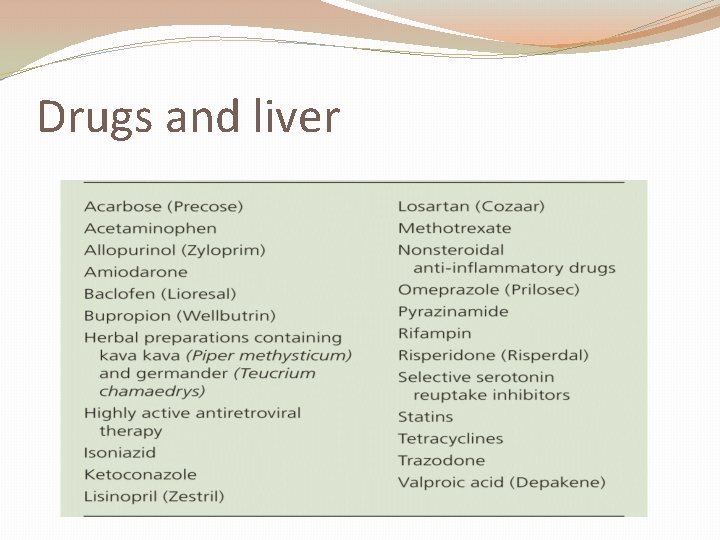
Drugs and liver
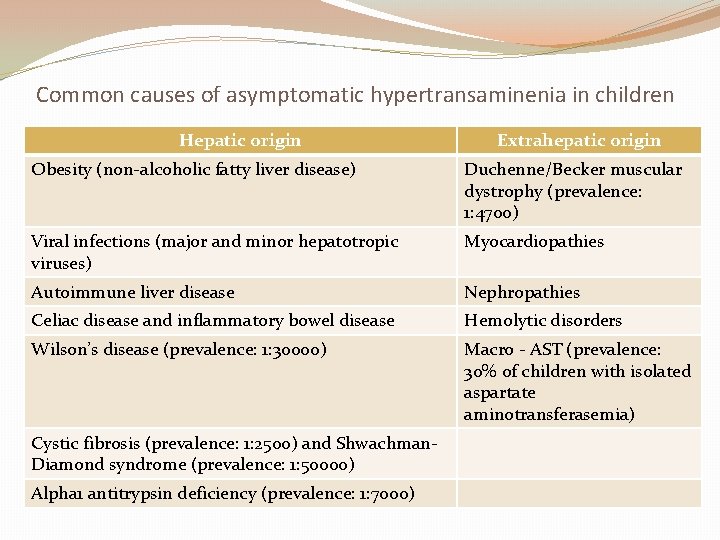
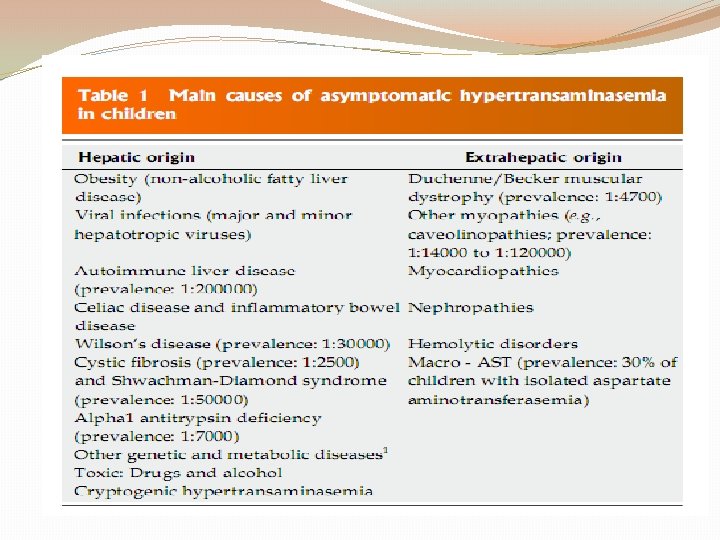
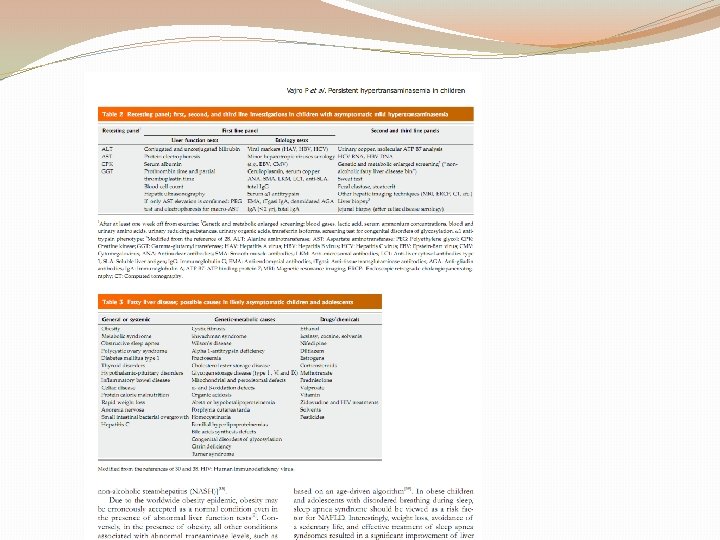
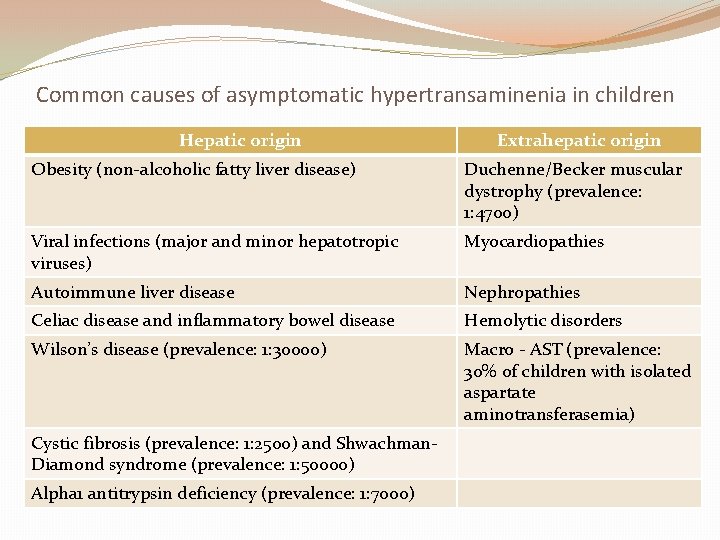
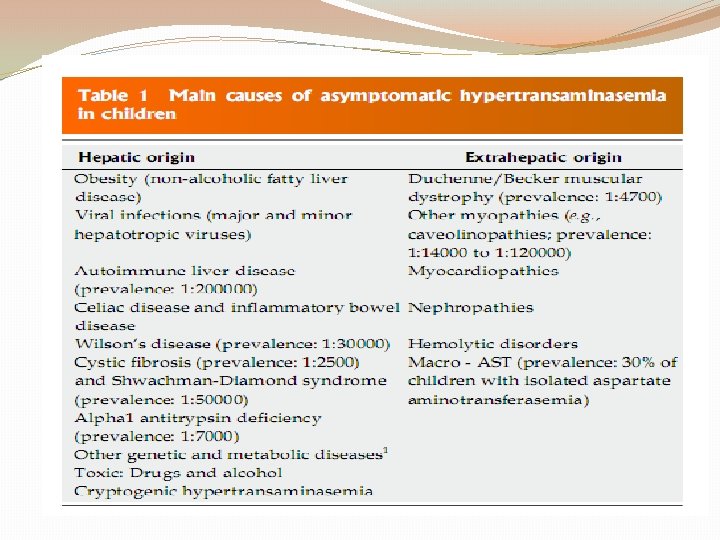
Common causes of asymptomatic hypertransaminenia in children Hepatic origin Extrahepatic origin Obesity (non-alcoholic fatty liver disease) Duchenne/Becker muscular dystrophy (prevalence: 1: 4700) Viral infections (major and minor hepatotropic viruses) Myocardiopathies Autoimmune liver disease Nephropathies Celiac disease and inflammatory bowel disease Hemolytic disorders Wilson’s disease (prevalence: 1: 30000) Macro - AST (prevalence: 30% of children with isolated aspartate aminotransferasemia) Cystic fibrosis (prevalence: 1: 2500) and Shwachman. Diamond syndrome (prevalence: 1: 50000) Alpha 1 antitrypsin deficiency (prevalence: 1: 7000)
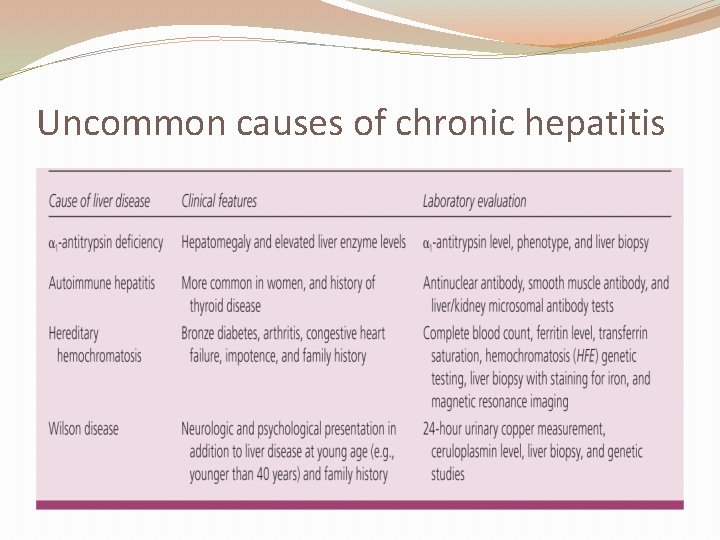
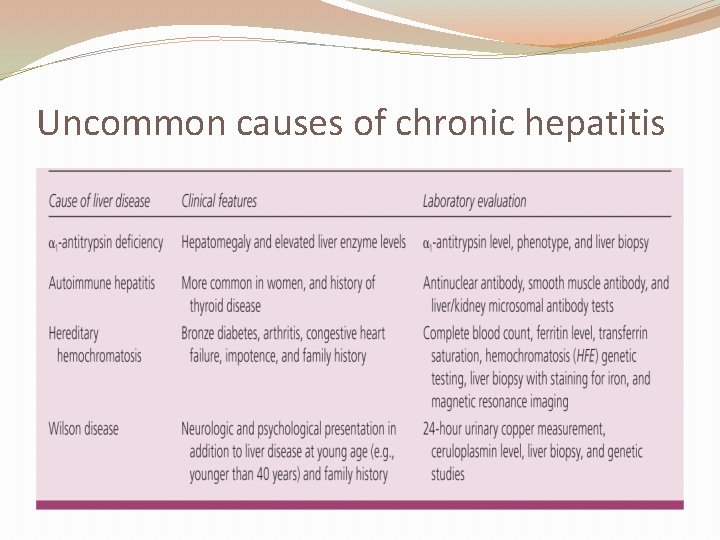
Uncommon causes of chronic hepatitis
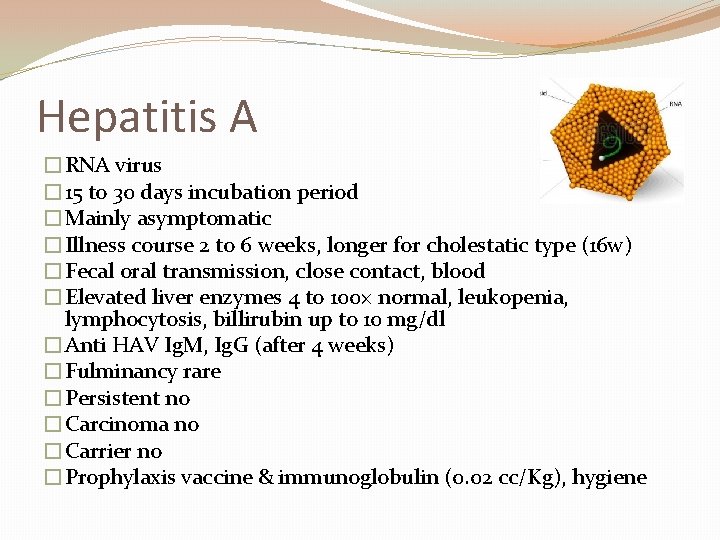
Hepatitis A �RNA virus � 15 to 30 days incubation period �Mainly asymptomatic �Illness course 2 to 6 weeks, longer for cholestatic type (16 w) �Fecal oral transmission, close contact, blood �Elevated liver enzymes 4 to 100× normal, leukopenia, lymphocytosis, billirubin up to 10 mg/dl �Anti HAV Ig. M, Ig. G (after 4 weeks) �Fulminancy rare �Persistent no �Carcinoma no �Carrier no �Prophylaxis vaccine & immunoglobulin (0. 02 cc/Kg), hygiene
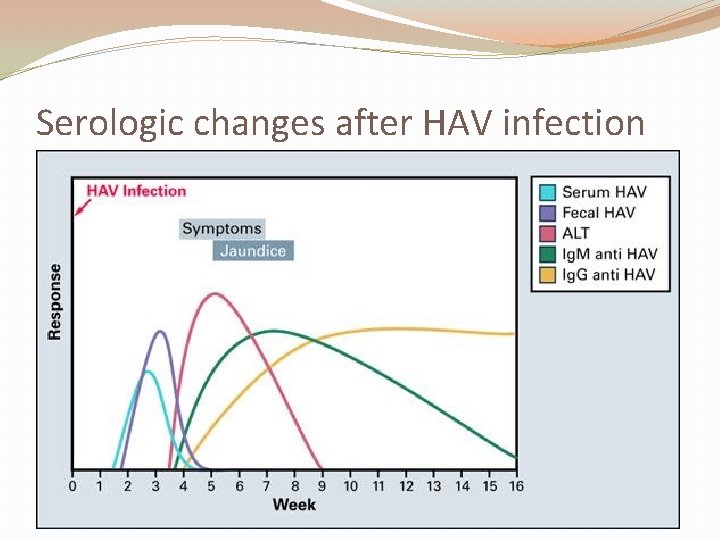
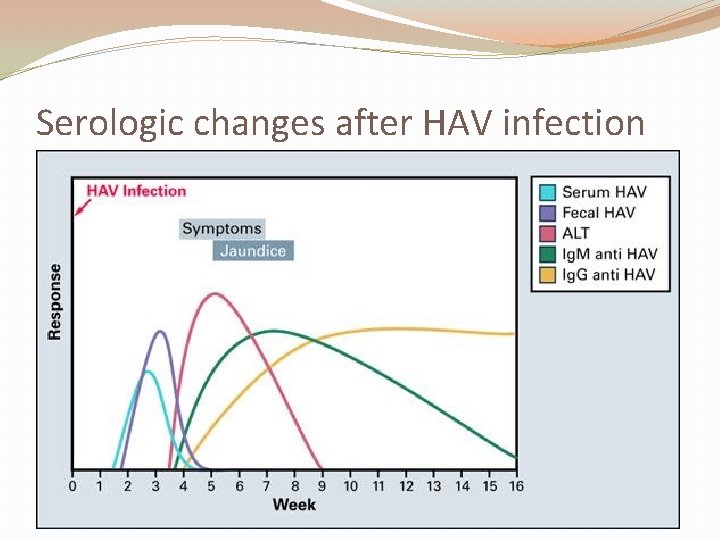
Serologic changes after HAV infection
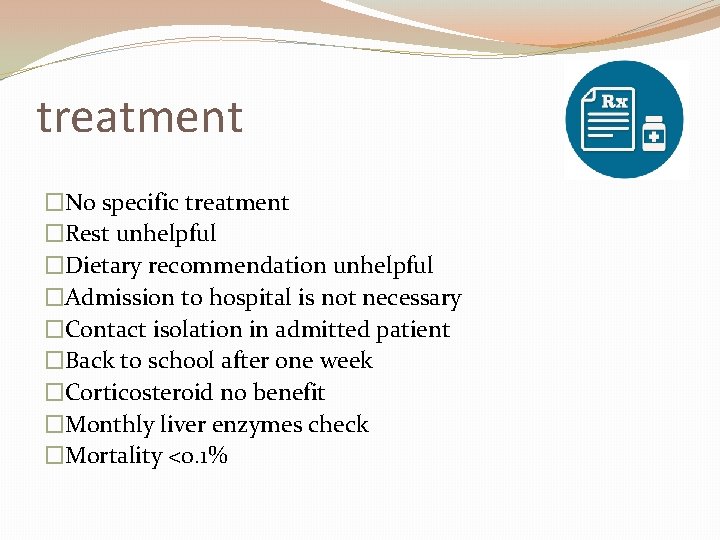
treatment �No specific treatment �Rest unhelpful �Dietary recommendation unhelpful �Admission to hospital is not necessary �Contact isolation in admitted patient �Back to school after one week �Corticosteroid no benefit �Monthly liver enzymes check �Mortality <0. 1%
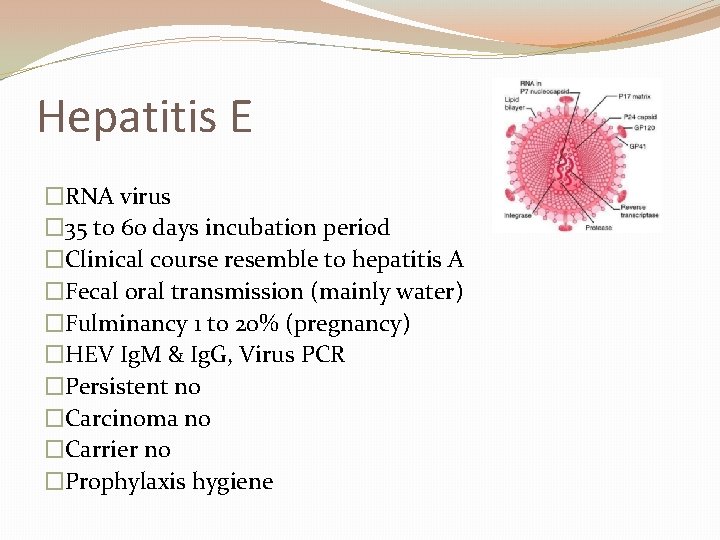
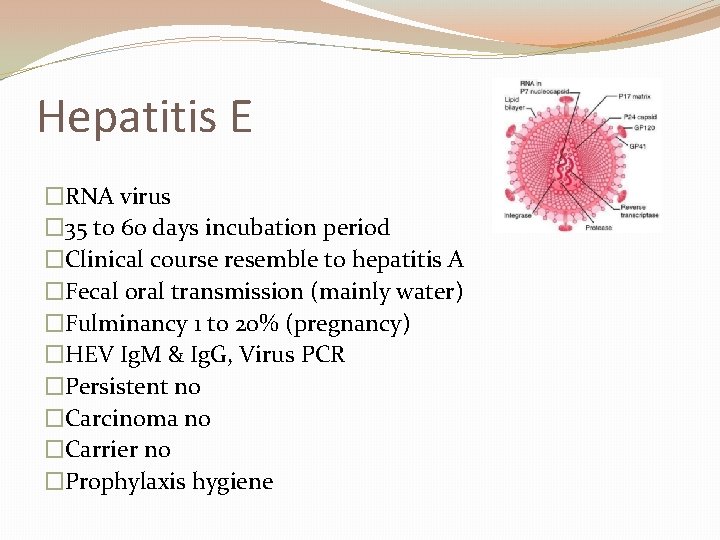
Hepatitis E �RNA virus � 35 to 60 days incubation period �Clinical course resemble to hepatitis A �Fecal oral transmission (mainly water) �Fulminancy 1 to 20% (pregnancy) �HEV Ig. M & Ig. G, Virus PCR �Persistent no �Carcinoma no �Carrier no �Prophylaxis hygiene
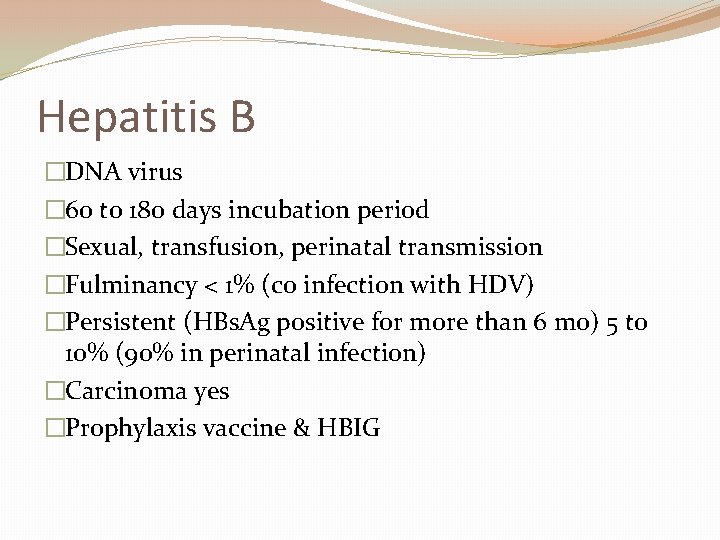
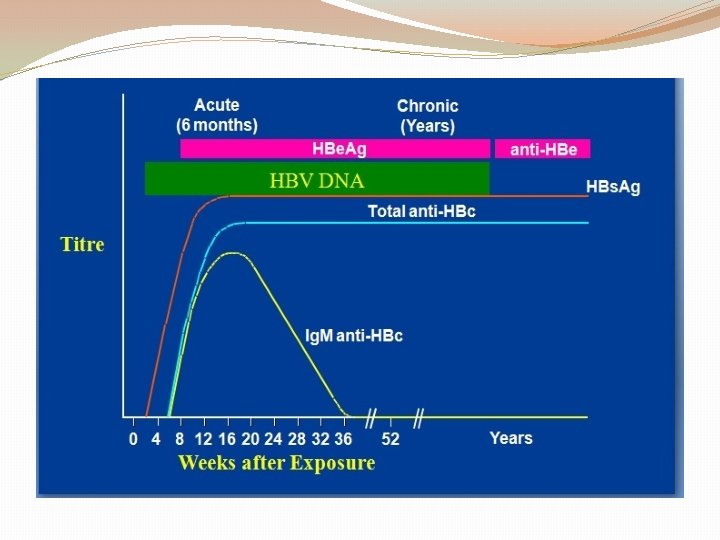
Hepatitis B �DNA virus � 60 to 180 days incubation period �Sexual, transfusion, perinatal transmission �Fulminancy < 1% (co infection with HDV) �Persistent (HBs. Ag positive for more than 6 mo) 5 to 10% (90% in perinatal infection) �Carcinoma yes �Prophylaxis vaccine & HBIG
Body fluid concentration of virus �High (blood, wound exudates, serum) �Moderate (semen, saliva, vaginal fluid) �Low or not detectable (urine, feces, breast milk, tear, sweat)
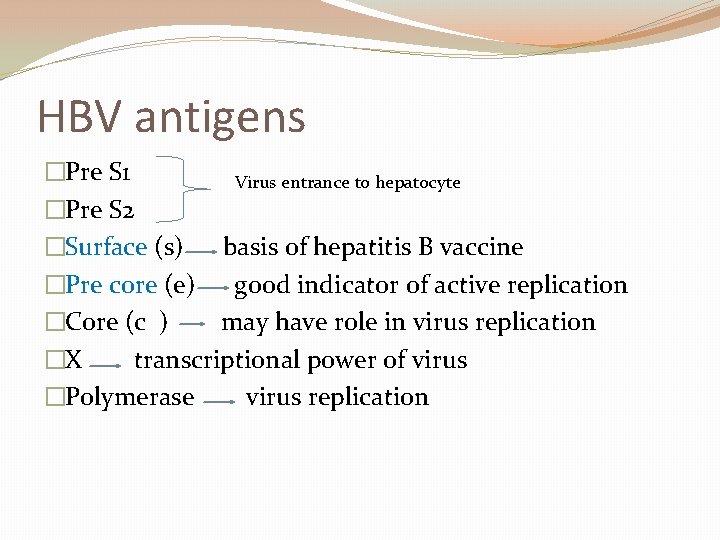
HBV antigens �Pre S 1 Virus entrance to hepatocyte �Pre S 2 �Surface (s) basis of hepatitis B vaccine �Pre core (e) good indicator of active replication �Core (c ) may have role in virus replication �X transcriptional power of virus �Polymerase virus replication
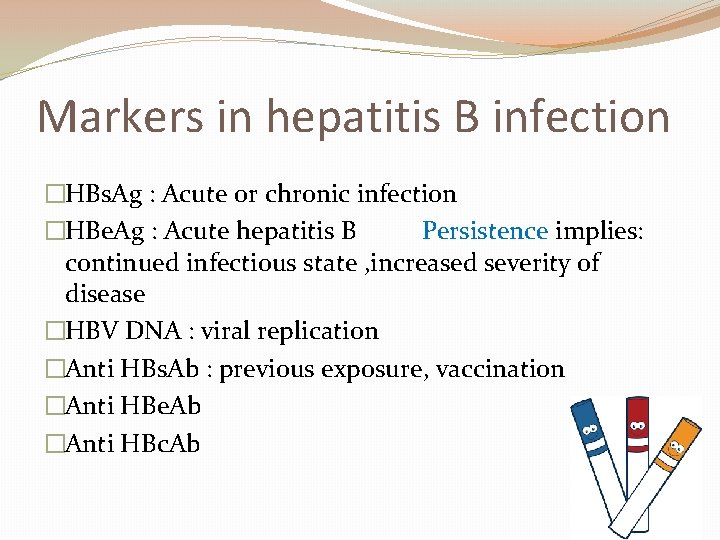
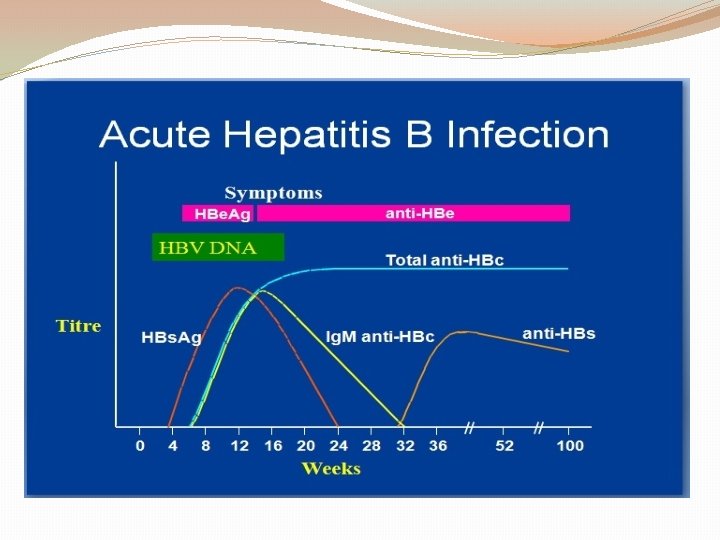
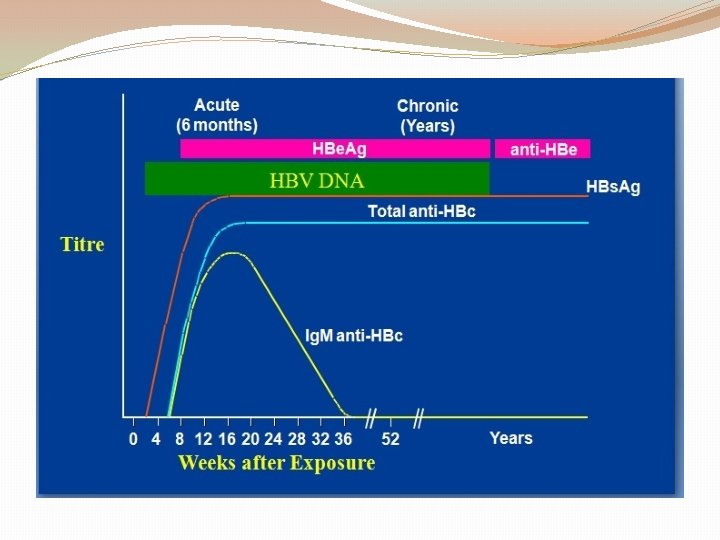
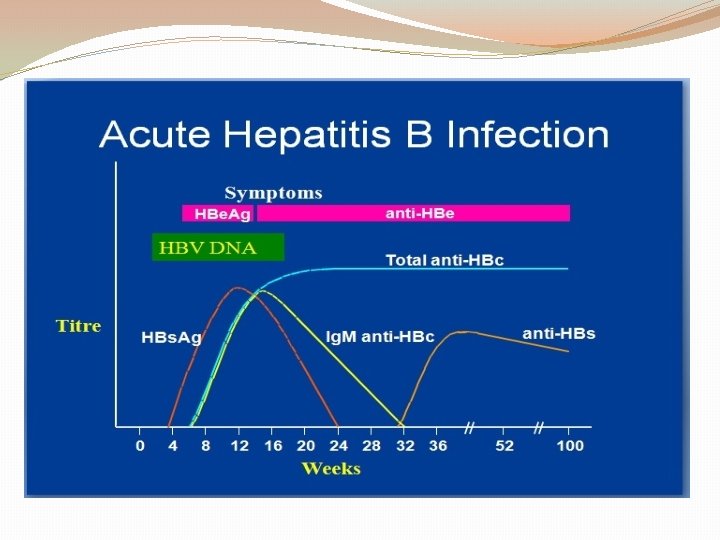
Markers in hepatitis B infection �HBs. Ag : Acute or chronic infection �HBe. Ag : Acute hepatitis B Persistence implies: continued infectious state , increased severity of disease �HBV DNA : viral replication �Anti HBs. Ab : previous exposure, vaccination �Anti HBe. Ab �Anti HBc. Ab
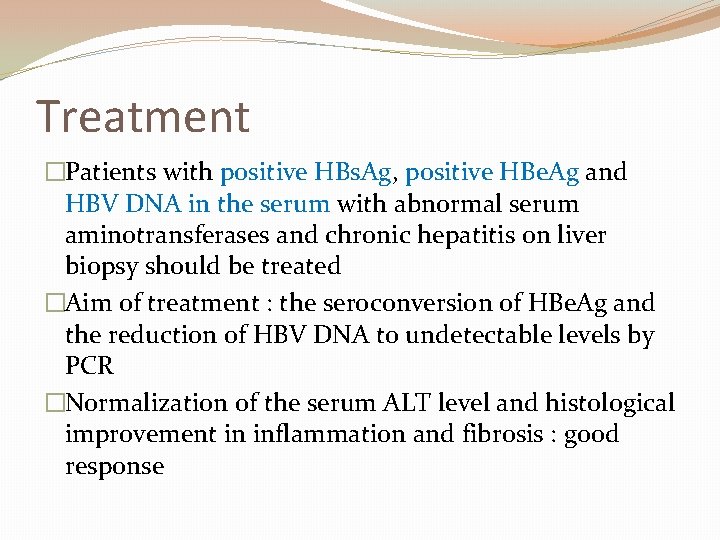
Treatment �Patients with positive HBs. Ag, positive HBe. Ag and HBV DNA in the serum with abnormal serum aminotransferases and chronic hepatitis on liver biopsy should be treated �Aim of treatment : the seroconversion of HBe. Ag and the reduction of HBV DNA to undetectable levels by PCR �Normalization of the serum ALT level and histological improvement in inflammation and fibrosis : good response
Treatment �Lamivudine 100 mg/Kg �Interferon alfa 2 b (normal LFT and decompensated liver failure) �HBIG (0. 5 cc) + vaccine Neonate of mother with positive HBs. Ag Needle stick with HBs. Ag positive patient Sex partner of newly diagnosed patient with positive HBs. Ag
Neonate of HBs. Ag + mother �HBIG 0. 5 ml Within 12 hours of birth �Hepatitis B vaccine �Vaccine at 1 and 6 mo �HBs. Ag check between 9 to 15 mo
Hepatitis D �RNA virus � 60 to 180 days incubation period �Co infection or super infection with HBV �Fulminancy (co infection) 2 to 20% �Persistent (super infection) 2 to 70% �Carcinoma no
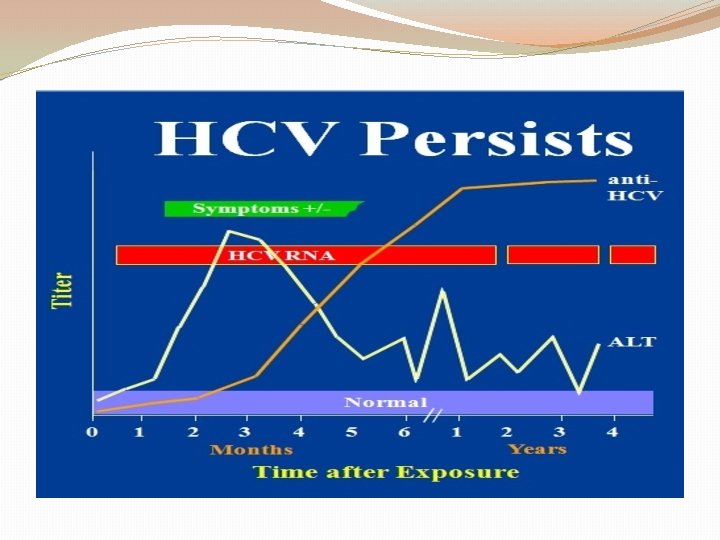
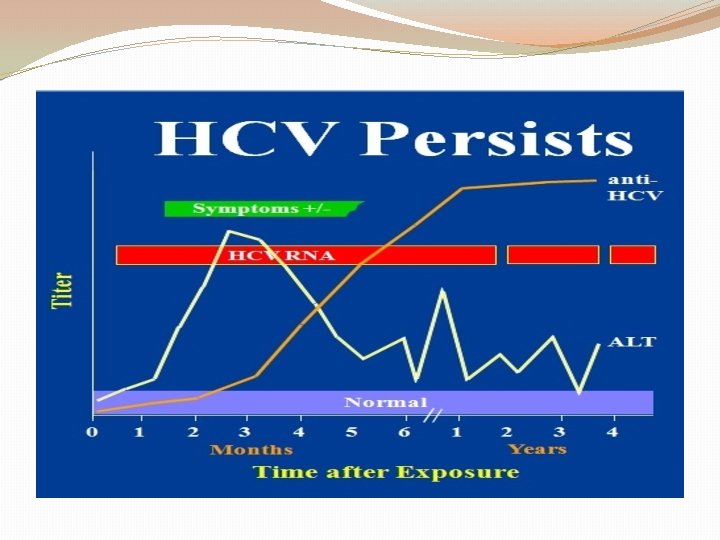
Hepatitis C �RNA virus �Incubation period of 30 to 60 days �Fulminancy rare �Persistent 85% �Carcinoma yes (7 to 15%) �Anti HCV Ig. M & Ig. G, virus PCR �Asymptomatic and accidental detection 50%

Treatment �Treat when liver biopsy is consistent with chronic hepatitis, abnormal LFT for more than 6 mo, detectable HCV RNA in serum �Treat abnormal biopsy and normal LFT �Treat cirrhosis on the base of HCV hepatitis �Uncompensated cirrhosis liver transplant �Aim of treatment : stop progression of active liver disease and prevent the development of hepatocellular carcinoma
Treatment �Ribavirin 800 to 1200 mg/Day for 6 to 12 mo + INF alfa 1 a 180 microg/w �Experience in children is not sufficient
Autoimmune hepatitis �Female predominance �Associated with other autoimmune diseases like as Coombs positive hemolytic anemia, pernicious anemia, thyroiditis �Genetically predisposed patient �Type 2 in teens, jaundice and very high level of liver enzymes with other features of autoimmune disorders, go to cirrhosis, high level of serum gamma globulins, often high PT, Anti LKM �Type 1 ANA & ASMA positive �Type 3 Anti soluble liver Ag positive ASMA: anti smooth muscle antibody LKM: liver kidney microsomal
Treatment �Prednisolone 30 mg is given daily for 2 weeks, followed by a slow reduction and then a maintenance dose of 10 -15 mg daily �Azathioprine should be added, 1 -2 mg/kg daily, as a steroid-sparing agent and in some patients as sole long-term maintenance therapy �Therapy induce remission in over 80% of cases �Treatment is lifelong in most cases

 Isfahan makamı dinle
Isfahan makamı dinle Hepatitis b markers interpretation
Hepatitis b markers interpretation Hepatitis e
Hepatitis e Window period of hepatitis b
Window period of hepatitis b Gonorrhea
Gonorrhea Is syphilis cureable
Is syphilis cureable Vacuna hepatitis b dosis
Vacuna hepatitis b dosis Dieta hepatitis
Dieta hepatitis Hepatitis c symptoms in men
Hepatitis c symptoms in men Hep b series for adults
Hep b series for adults Hepatitis c medications
Hepatitis c medications Biliary tract
Biliary tract Colestasis
Colestasis Hepatitis b
Hepatitis b Classification of chronic hepatitis
Classification of chronic hepatitis Corticoides hepatitis alcoholica
Corticoides hepatitis alcoholica Hepar facies diaphragmatica
Hepar facies diaphragmatica Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Hepatitis b panel
Hepatitis b panel Chronic hepatitis
Chronic hepatitis Hep b mode of transmission
Hep b mode of transmission Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Clinical manifestation of hepatitis
Clinical manifestation of hepatitis Chronic pancreatitis nursing care plan
Chronic pancreatitis nursing care plan Score simplificado hepatitis autoinmune
Score simplificado hepatitis autoinmune Hepatitis a
Hepatitis a Hepatitis c symptoms in men
Hepatitis c symptoms in men Hepatitis types chart
Hepatitis types chart Hgado
Hgado Hepatitis b
Hepatitis b Nursing management of liver abscess
Nursing management of liver abscess Pbc vs psc
Pbc vs psc Gail lupica
Gail lupica Ano ang pagkakaiba ng hepatitis a at b
Ano ang pagkakaiba ng hepatitis a at b Hepatitis
Hepatitis Hepatitis a treatment
Hepatitis a treatment Alcoholic hepatitis
Alcoholic hepatitis Hepatic coma diet
Hepatic coma diet Ggh providencia
Ggh providencia Klasifikasi hepatitis a
Klasifikasi hepatitis a Michael le md
Michael le md Doctors license number
Doctors license number Gbmc medical records
Gbmc medical records Hepburn osteometric board
Hepburn osteometric board Torrance memorial medical center medical records
Torrance memorial medical center medical records Cartersville medical center medical records
Cartersville medical center medical records University medical centre maribor
University medical centre maribor Liaoning medical university
Liaoning medical university Vietnam military medical university
Vietnam military medical university M.gorky donetsk national medical university
M.gorky donetsk national medical university