HEALTH PLANS IN THE LIMELIGHT ONCE AGAIN Wally





- Slides: 46
HEALTH PLANS IN THE LIMELIGHT ONCE AGAIN Wally Miller Schwabe Williamson & Wyatt

ASSOCIATION HEALTH PLANS
PRE-ACA • Prior to 2014, health insurance offered to members of a bona fide association was considered large group coverage, regardless of purchased by individual, small employer group, or large employer group 3
PRE-ACA • Bona Fide Association Status: – Actively in existence for at least 5 years – Constitution and bylaws – Formed for purpose other than to purchase insurance 4
PRE-ACA • As large group coverage, association coverage was exempt from small employer community rate pooling rules • Could also cover individuals who were members of the association • Although a single policyholder, each employer was considered a sponsor of its own separate plan for ERISA purposes 5
ACA (2014) • Ceased to recognize associations as a separate market • Association coverage is either group (small or large ) or individual market • However, a "bona fide group plan" can qualify as a single plan under ERISA (MEWA) qualifying for large employer market status 6
ERISA BONA FIDE PLANS • ERISA bona fide plan status allows avoidance of: – Guaranty issue – Essential health benefits – Rating rules – Single risk pools • Bona fide status requires plan be maintained by a "group or association of employers" acting in the interest of an employer 7
ERISA BONA FIDE PLANS • Participating employers must be bound by a common economic or representation interest (the "commonality of interest standard”) • The plan must be controlled by the participating employers (rather than the association) • All participating employers must be "employers, " meaning sole proprietors are not eligible 8
COMMONALITY OF INTEREST • Generally requires that all employers: – Be within the same industry in the same geographical local – Have a history of organized coordination on matters unrelated to benefits 9
CONTROL STANDARD • Employers that actually participate in plan must have control over plan – Amendments and termination • Association itself cannot unilaterally run the show • Typically, a “Group Insurance Board” is established – Members voted in by employers 10
EMPLOYERS ONLY • Only employers can participate • Sole proprietors, partnerships and LLCs can join only if they have common-law employees 11
ERISA BONA FIDE PLANS • A bona fide group plan is a single plan for purposes of ERISA. • The plan sponsor files a single 5500 • A Form M-1 must be filed before the effective date, and then each year, with the DOL • The Oregon Insurance Division requires an opinion letter from an ERISA attorney regarding satisfaction of bona fide standards 12
PROPOSED AHP REGULATIONS 13
PROPOSED AHP REGULATIONS • One of three directives included in Trump Executive Order (10/12/17) – Expand the scope of current commonality-ofinterest; and – Promote AHP formation on basis of common geography or industry • A plan will be allowed to rely on the current DOL “subregulatory” standards, or the new AHP regulations 14
NEW COMMONALITY OF INTEREST • Employers must be: – In the same industry or profession; or – Have a principal place of business within the same state or metropolitan area • Coverage can cross state lines (subject to above) • Employers can band together for the sole purpose of purchasing insurance 15
NEW BONA FIDE STANDARDS • Must have proper organizational structure – Governing board – By-laws or equivalent • Control by participating employers – Regular nomination and election of officers 16
NONDISCRIMINATION • Cannot condition employer participation on employees’ clean bill of health • May not treat employer-members as distinct group of similarly-situated employees – Differing rates among employers must be based on HIPAA similarly-situated criteria (e. g. , geography) 17
WORKING OWNERS • Plan must restrict coverage to: – Common-law employees; and – “Working Owners” • Working owners must: – Work at least 30 hours per week (or 120 hours per month) or – Have earned income exceeding cost of coverage – Not be eligible for subsidized coverage under another plan (such as a spouse’s plan) 18
SELF-INSURED PLANS • ERISA generally provides that states can fully regulate (or even prohibit) self-insured MEWAs • However, ERISA also provides that the DOL may issue regulations exempting self -insured MEWAs from general state governance • Not doing so now, but has requested comments 19

WHO’S AGAINST, AND WHY? • Comment period ended March 6, 2018 – 720 comments • 13 Democratic States Attorneys • Various Citzens – Both claim undermines the ACA protections • Insurance companies – Unless state regulation – Don’t want self-insurance allowed 20
WHO’S FOR, AND WHY? • House Committee of Education and Workforce • Chambers of Commerce – No longer subject to same industry rule • Realtor Boards – Can offer to individual • ASPPA – But wants to be able to sell to all individual members of 501(c)(6) associations 21
SHORT-TERM POLICIES
SHORT-TERM POLICIES • Are not “excepted benefits” • Instead are expressly excluded from ACA’s definition of individual health insurance • Short-term not defined – Obama administration proposed a definition of 3 months – Proposed regulation defines it as fewer than 12 months 23
SHORT-TERM POLICIES • Can deny based on health status • Can exclude coverage for pre-existing conditions • EHB coverage not required • Annual and lifetime limits permitted • No cost-sharing limits 24
25
STAND-ALONE HEALTH REIMBURSEMENT ARRANGEMENTS (HRAs) 26
STAND-ALONE HRAs • Prior to 2014, very popular for small businesses • ACA now generally prohibits – May only have integrated HRAs • Small employers may now have a Qualified Small Employer Health Reimbursement Arrangement (“QSEHRA”) 27
QSEHRA • Available only if employer: – Had fewer than 50 FTEEs in preceding year; and – Does not offer group health coverage to any employees 28
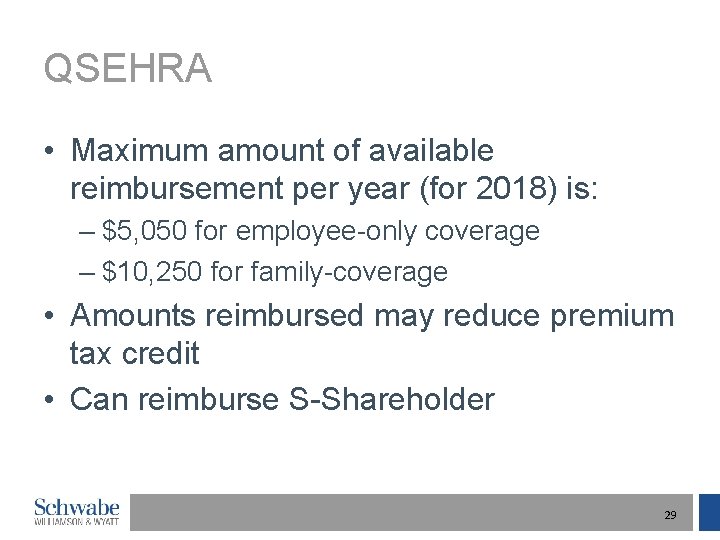
QSEHRA • Maximum amount of available reimbursement per year (for 2018) is: – $5, 050 for employee-only coverage – $10, 250 for family-coverage • Amounts reimbursed may reduce premium tax credit • Can reimburse S-Shareholder 29
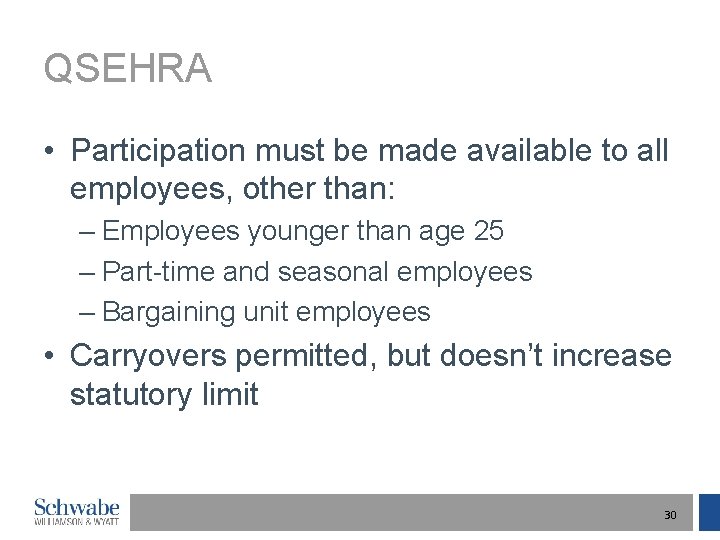
QSEHRA • Participation must be made available to all employees, other than: – Employees younger than age 25 – Part-time and seasonal employees – Bargaining unit employees • Carryovers permitted, but doesn’t increase statutory limit 30
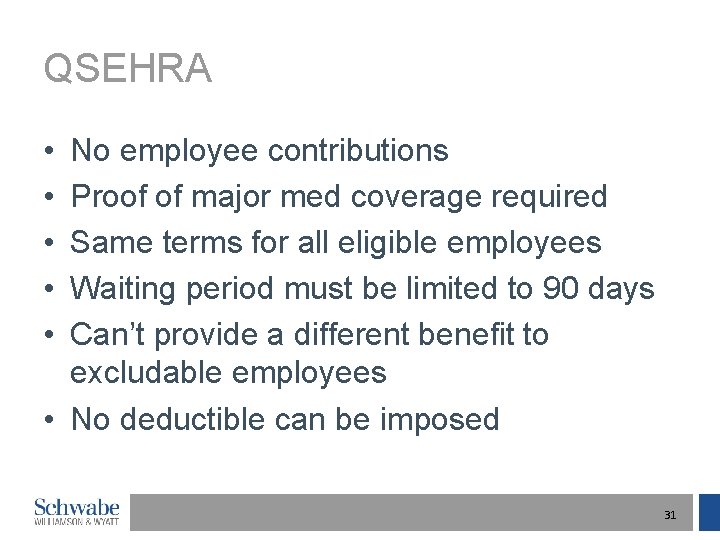
QSEHRA • • • No employee contributions Proof of major med coverage required Same terms for all eligible employees Waiting period must be limited to 90 days Can’t provide a different benefit to excludable employees • No deductible can be imposed 31
ACA ESRP EXCISE TAX

ACA ESRP EXCISE TAX • Two Play-or-Pay penalties – “A” penalty for failing to cover 95% of FTE (70% for 2015) – “B” penalty for not offering affordable MEC coverage to an FTE who receives a premium tax credit 33
ACA ESRP EXCISE TAX • IRS is sending out proposed penalty notices – Form 226 J – For 2015 – For “A” penalty only • Common error – Failing to declare eligibility for 70% threshold – Failing to declare offering of MEC to 70% of FTEs 34
ACA ESRP EXCISE TAX • 30 day response deadline (Form 14764) – Extension can be requested – Challenge requires signed statement • Check 2016 and 2017 Forms – File amended returns if errors discovered 35

STATE INITIATIVES
IDAHO • Governor issued Executive Order allowing state-based health plans with pre-ACA standards • Insurer must also offer exchange policy • Features include: – Pre-existing conditions exclusion permitted, subject to pre-ACA creditable coverage rule – Certain minimum benefits must be provided (but not all EHBs) 37
IDAHO • Features (continued) – Age 26 standard remains – $1 million annual limits – No maximum OOP limit – Full preventive coverage not required • May have non-maternity plan, if other maternity plan offered • HHS has responded, saying don't mess with the ACA – But will it enforce? 38
IOWA • ACA governs group health plans and governs health insurance insurers • An “insurer” is defined as a company subject to state law that regulates insurance 39
IOWA • Iowa passed law declaring that health coverage offered by nonprofit agricultural organization is exempt from state insurance laws – Iowa Farm Bureau • Consequently, can offer non-ACA, nonregulated insurance • Seems like a solid loophole 40
QUIZ SHOW 41

QUIZ SHOW • Wally attains age 65 on May 6, 2019. He waits a year, and on July 1, 2020, at age 66, retires and applies for Medicare. He becomes an HSA Ineligible Individual on: [ [ [ ] May 6, 2019 ] January 1, 2020 ] July 1, 2020 42
QUIZ SHOW • HMO region-specific employer has out-ofstate salesperson • Can the employer reimburse the salesperson for the premiums for an individual policy? [ [ ] Yes ] No 43
ONE PARTICIPANT HRA PLANS • The ACA market reform rules do not apply to plans with fewer than 2 participants who are active employees • Ergo, a one-participant plan is permitted • Remains subject to other ACA laws, ERISA and the IRC 44
QUIZ SHOW • Self-insured employer has employee with gigantic Rx bills • Can the employer induce the employee to waive coverage, and provide reimbursment for an individual policy? [ [ ] Yes ] No 45
QUESTIONS? 46
 Operation limelight
Operation limelight Again and again signpost picture books
Again and again signpost picture books She's like a song played again and again
She's like a song played again and again Rise and rise again until lambs become lions
Rise and rise again until lambs become lions The outsiders signposts
The outsiders signposts On sitting down to read king lear once again
On sitting down to read king lear once again I believe jesus saves
I believe jesus saves Banquero de la resistencia
Banquero de la resistencia John lasseter andre and wally b
John lasseter andre and wally b Wally was eager to prove
Wally was eager to prove Obermeyer case
Obermeyer case Sir walter wally
Sir walter wally Wally berry
Wally berry The clothes poem by mongane wally serote analysis
The clothes poem by mongane wally serote analysis Wally is a paleontologist in the future
Wally is a paleontologist in the future Wally waters
Wally waters Wally olins podręcznik brandingu
Wally olins podręcznik brandingu Wally stevens
Wally stevens Ocf formula
Ocf formula Wally gibson
Wally gibson Rph pathology
Rph pathology Wally pilot mascot
Wally pilot mascot Art schneiderman
Art schneiderman Rocky mountain health plans dualcare plus
Rocky mountain health plans dualcare plus Mental health policy, plans and programmes michelle funk
Mental health policy, plans and programmes michelle funk 215-967-4690
215-967-4690 Apple health managed care plans
Apple health managed care plans Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Tư thế worm breton
Tư thế worm breton Hát lên người ơi alleluia
Hát lên người ơi alleluia Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Phép trừ bù
Phép trừ bù độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi