Health Access Team United Way Kennewick O C
- Slides: 38
Health Access Team United Way, Kennewick O C T O B E 6 R , 2017
Presentation Outline • Program Update • Defining, Stratifying and Identifying the High Cost Population • The Area Deprivation Index (ADI) • P 4 P Metric Achievement Value Calculation • Performance Gap Analysis: Number Needed to Treat 2
Program Update
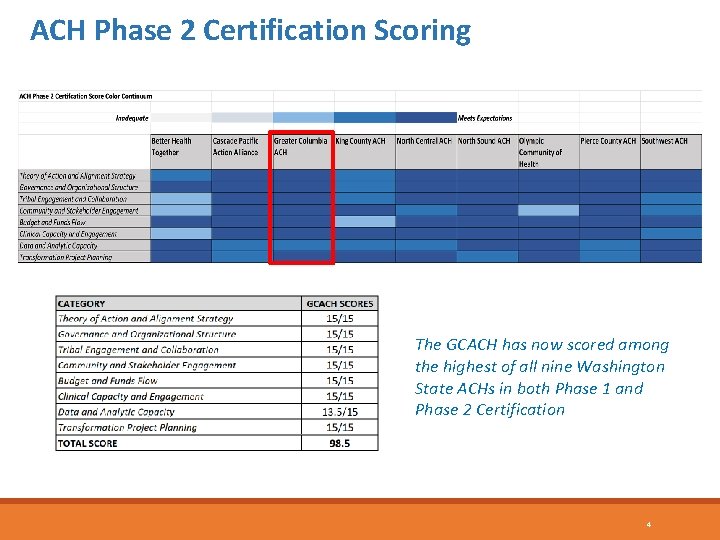
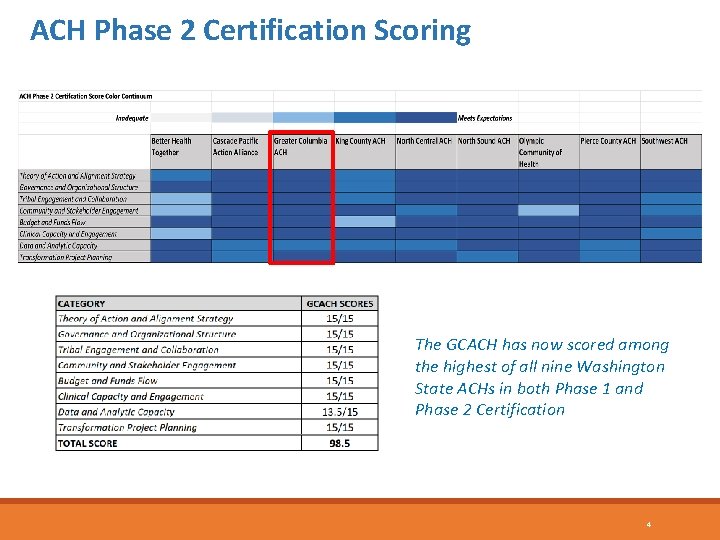
ACH Phase 2 Certification Scoring The GCACH has now scored among the highest of all nine Washington State ACHs in both Phase 1 and Phase 2 Certification 4
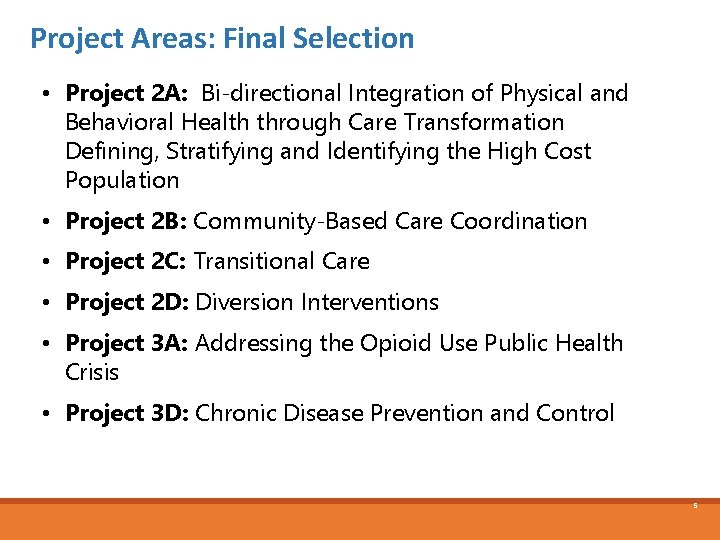
Project Areas: Final Selection • Project 2 A: Bi-directional Integration of Physical and Behavioral Health through Care Transformation Defining, Stratifying and Identifying the High Cost Population • Project 2 B: Community-Based Care Coordination • Project 2 C: Transitional Care • Project 2 D: Diversion Interventions • Project 3 A: Addressing the Opioid Use Public Health Crisis • Project 3 D: Chronic Disease Prevention and Control 5
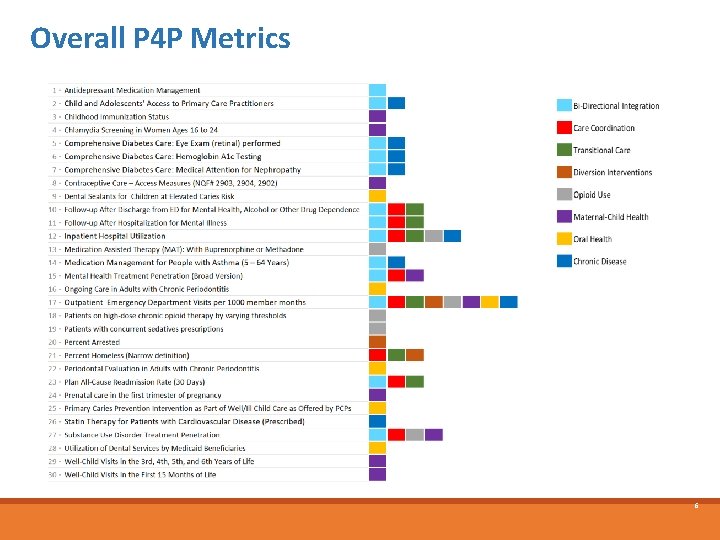
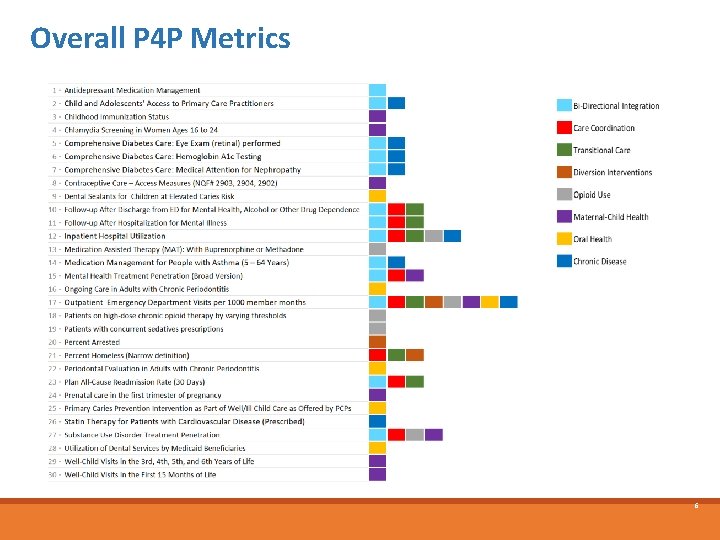
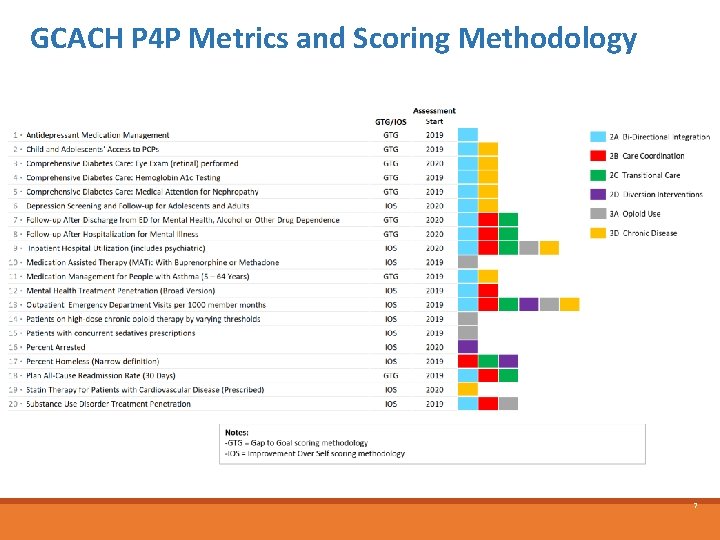
Overall P 4 P Metrics 6
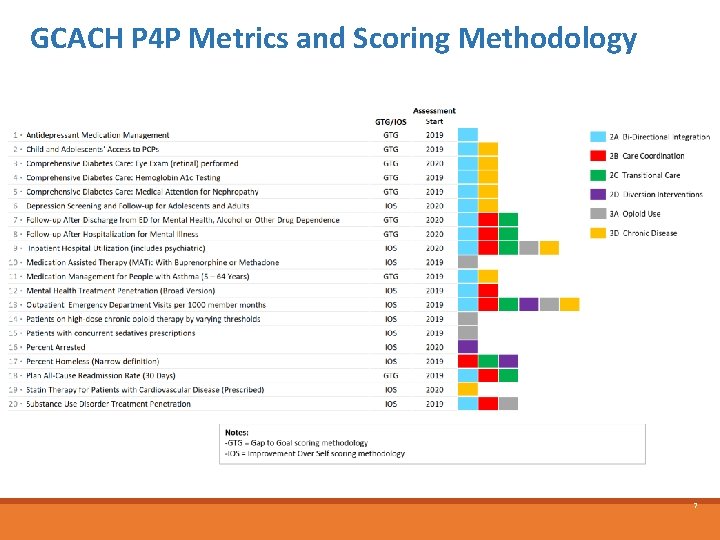
GCACH P 4 P Metrics and Scoring Methodology 7
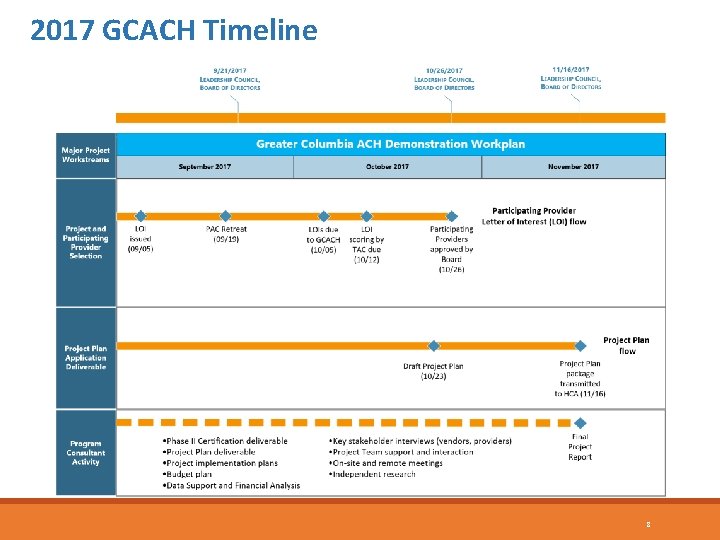
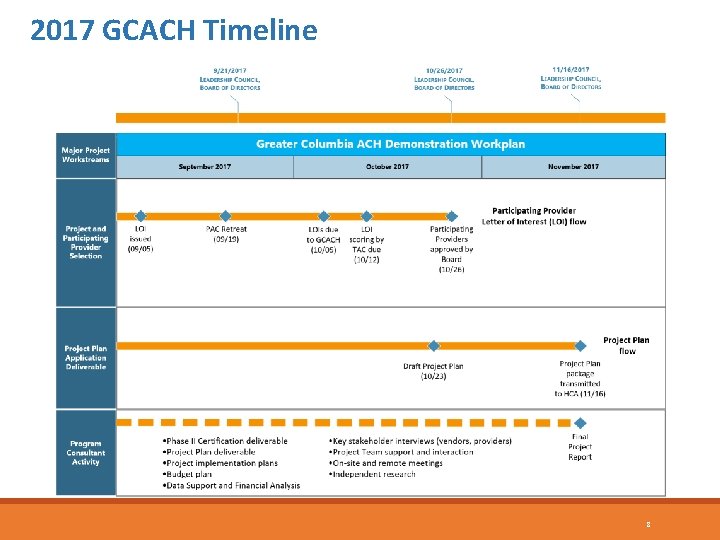
2017 GCACH Timeline 8
Defining, Stratifying and Identifying the High Cost Population
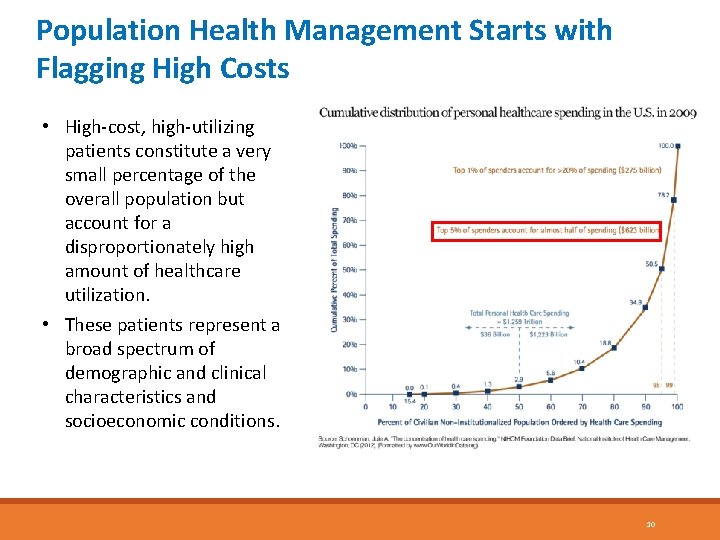
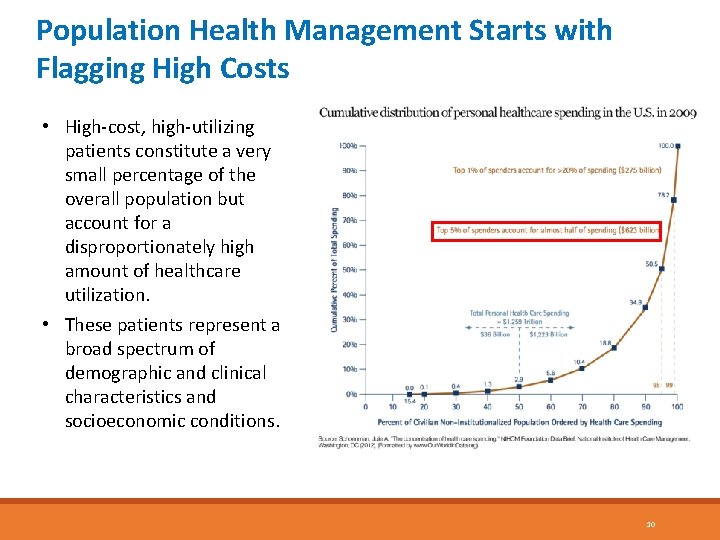
Population Health Management Starts with Flagging High Costs • High-cost, high-utilizing patients constitute a very small percentage of the overall population but account for a disproportionately high amount of healthcare utilization. • These patients represent a broad spectrum of demographic and clinical characteristics and socioeconomic conditions. 10
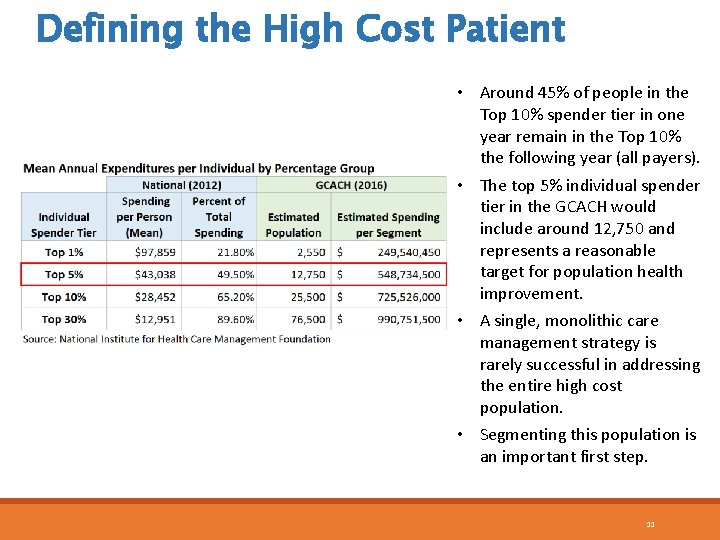
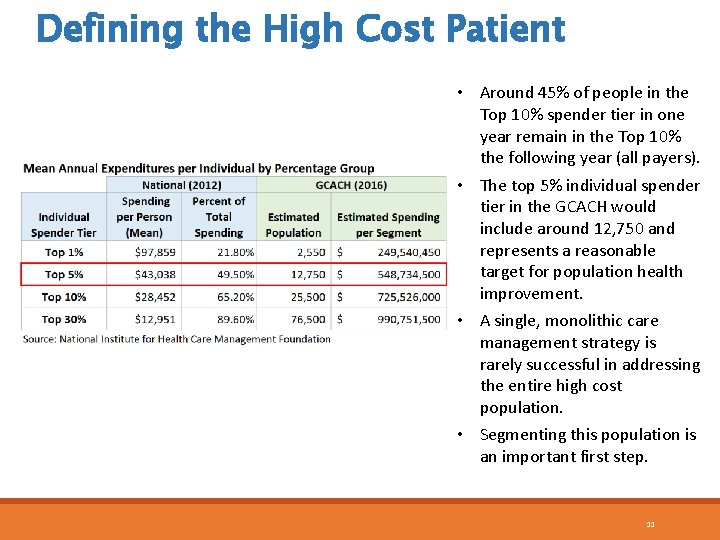
Defining the High Cost Patient • Around 45% of people in the Top 10% spender tier in one year remain in the Top 10% the following year (all payers). • The top 5% individual spender tier in the GCACH would include around 12, 750 and represents a reasonable target for population health improvement. • A single, monolithic care management strategy is rarely successful in addressing the entire high cost population. • Segmenting this population is an important first step. 11
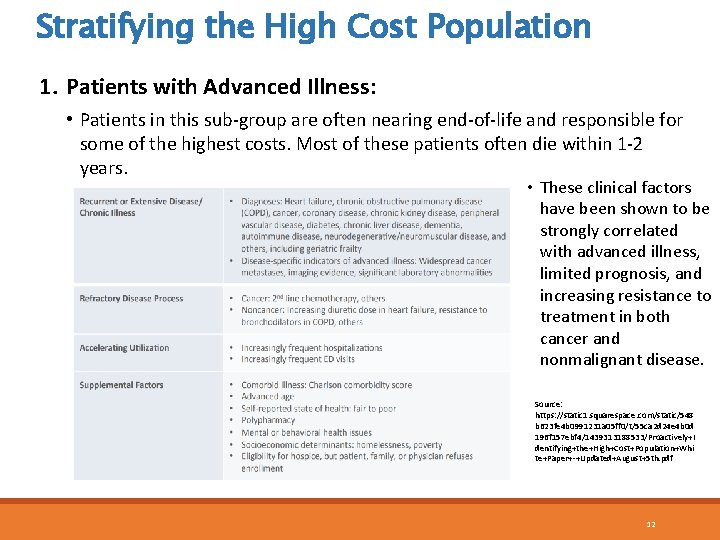
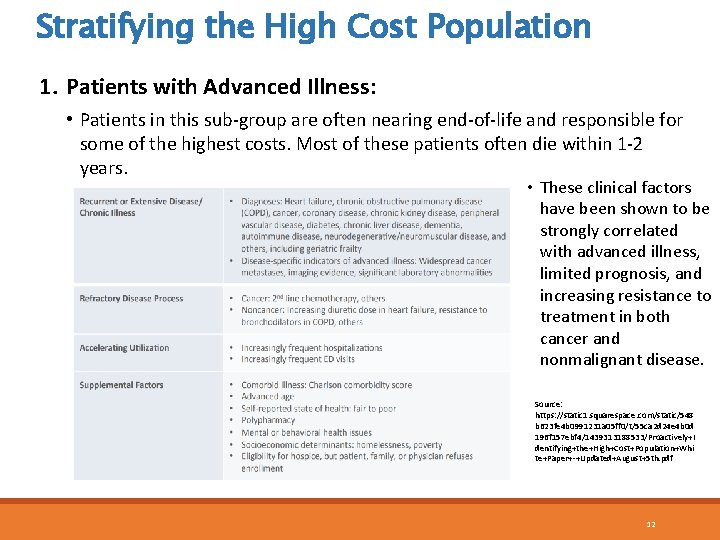
Stratifying the High Cost Population 1. Patients with Advanced Illness: • Patients in this sub-group are often nearing end-of-life and responsible for some of the highest costs. Most of these patients often die within 1 -2 years. • These clinical factors have been shown to be strongly correlated with advanced illness, limited prognosis, and increasing resistance to treatment in both cancer and nonmalignant disease. Source: https: //static 1. squarespace. com/static/548 b 623 fe 4 b 0991231 a 05 ff 0/t/55 ca 2 d 24 e 4 b 0 d 196 f 157 ebf 4/1439313188533/Proactively+I dentifying+the+High+Cost+Population+Whi te+Paper+-+Updated+August+5 th. pdf 12
Stratifying the High Cost Population 1. Patients with Advanced Illness: • Application of this criteria for patient selection will identify a large fraction of subgroup 1 patients with advanced illness. Targeted patients could be used by providers to determine referral to care management. • Opportunities to provide home and community-based services can cut down on unnecessary hospitalizations. • Care management involving informed choice and other support can optimize the use of hospice and other palliative care services to redirect end-of-life care from hospital to home and community. • Not only is this in the best interest of the patient, recognizing that most patients would prefer not to die in the hospital, but the potential for savings from such strategies is high. Source: https: //static 1. squarespace. com/static/548 b 623 fe 4 b 0991231 a 05 ff 0/t/55 ca 2 d 24 e 4 b 0 d 196 f 157 ebf 4/1439313188533/Proactively+Identifying+the+High+Cost+Population+W hite+Paper+-+Updated+August+5 th. pdf 13
Stratifying the High Cost Population 2. Patients with Persistent High Spending Patterns: • Patients within this sub-group have high-spending utilization that can carry over to subsequent years. • Characterized by multiple chronic conditions. • Many face psychological and social barriers to care. • Many are good candidates for care management and social support services. • Concentration of spending is particularly significant in Medicaid, where 60% of patients in the Top 10% Spender Tier in any given year remain in that tier the following year. Source: https: //static 1. squarespace. com/static/548 b 623 fe 4 b 0991231 a 05 ff 0/t/55 ca 2 d 24 e 4 b 0 d 196 f 157 ebf 4/1439313188533/Proactively+Identifying+the+High+Cost+Population+W hite+Paper+-+Updated+August+5 th. pdf 14
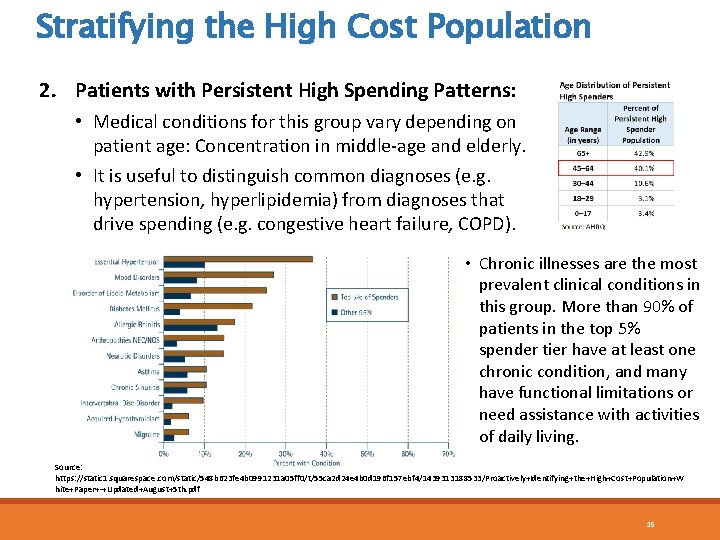
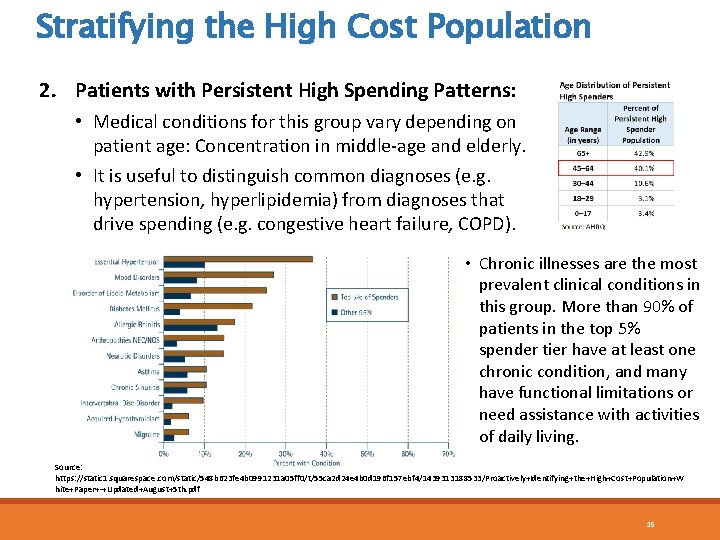
Stratifying the High Cost Population 2. Patients with Persistent High Spending Patterns: • Medical conditions for this group vary depending on patient age: Concentration in middle-age and elderly. • It is useful to distinguish common diagnoses (e. g. hypertension, hyperlipidemia) from diagnoses that drive spending (e. g. congestive heart failure, COPD). • Chronic illnesses are the most prevalent clinical conditions in this group. More than 90% of patients in the top 5% spender tier have at least one chronic condition, and many have functional limitations or need assistance with activities of daily living. Source: https: //static 1. squarespace. com/static/548 b 623 fe 4 b 0991231 a 05 ff 0/t/55 ca 2 d 24 e 4 b 0 d 196 f 157 ebf 4/1439313188533/Proactively+Identifying+the+High+Cost+Population+W hite+Paper+-+Updated+August+5 th. pdf 15
Stratifying the High Cost Population 2. Patients with Persistent High Spending Patterns: • Complex patients with low patient activation—as measured by the Patient Activation Measure (PAM)—are at particular risk due to the inability to perform adequate self-care to manage their condition. • Serious mental health and substance use diagnoses are also among the most significant drivers of cost. • Per capita costs are double or triple for Medicaid patients with a co-morbid mental health diagnosis or with evidence of substance abuse. • These diagnoses are especially prevalent in Medicaid high cost populations and care management programs need to address these underlying drivers of utilization Source: https: //static 1. squarespace. com/static/548 b 623 fe 4 b 0991231 a 05 ff 0/t/55 ca 2 d 24 e 4 b 0 d 196 f 157 ebf 4/1439313188533/Proactively+Identifying+the+High+Cost+Population+W hite+Paper+-+Updated+August+5 th. pdf 16
Stratifying the High Cost Population 3. Patients with Episodic High Spending: • Patients in this last sub-group have increased costs due to a sudden event, but costs decrease as the condition resolves. • These acute temporary spenders tend to be younger with good or excellent self-reported health status. • Difficult to target proactively because cost spikes are usually not predictable. High-cost continuation is also less likely in subsequent years. • There may be educational opportunities for this sub-group through our work. Source: https: //static 1. squarespace. com/static/548 b 623 fe 4 b 0991231 a 05 ff 0/t/55 ca 2 d 24 e 4 b 0 d 196 f 157 ebf 4/1439313188533/Proactively+Identifying+the+High+Cost+Population+W hite+Paper+-+Updated+August+5 th. pdf 17
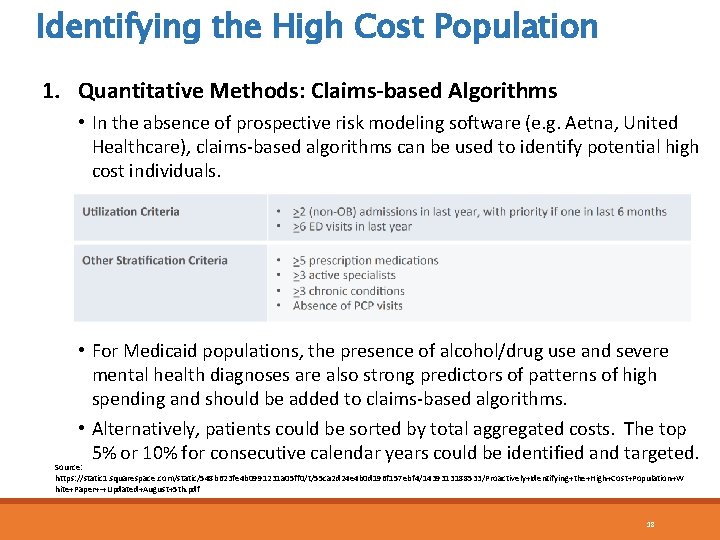
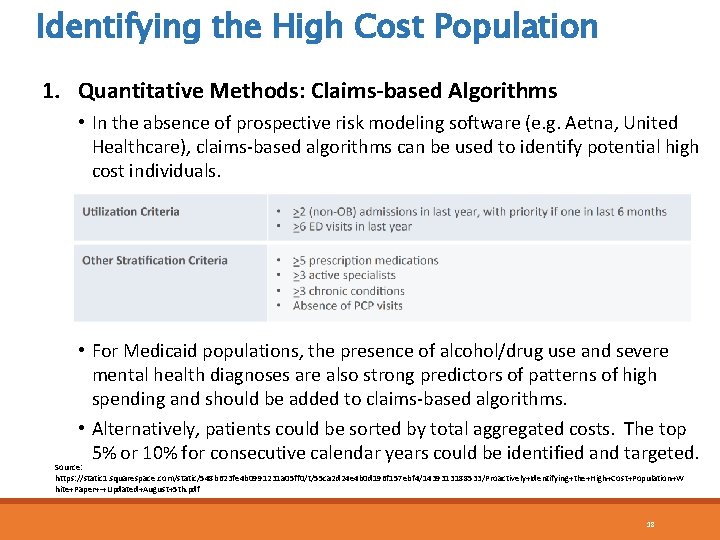
Identifying the High Cost Population 1. Quantitative Methods: Claims-based Algorithms • In the absence of prospective risk modeling software (e. g. Aetna, United Healthcare), claims-based algorithms can be used to identify potential high cost individuals. • For Medicaid populations, the presence of alcohol/drug use and severe mental health diagnoses are also strong predictors of patterns of high spending and should be added to claims-based algorithms. • Alternatively, patients could be sorted by total aggregated costs. The top 5% or 10% for consecutive calendar years could be identified and targeted. Source: https: //static 1. squarespace. com/static/548 b 623 fe 4 b 0991231 a 05 ff 0/t/55 ca 2 d 24 e 4 b 0 d 196 f 157 ebf 4/1439313188533/Proactively+Identifying+the+High+Cost+Population+W hite+Paper+-+Updated+August+5 th. pdf 18
Identifying the High Cost Population 1. Quantitative Methods: Claims-based Algorithms Drawbacks to using claims-based algorithms: • Sensitivity: These algorithms miss about half of potential enrollees. The remainder of enrollees would need to be referred through utilization or case management. • Limited Clinical Data: Many good metrics of illness progression and mortality are not routinely gathered in the traditional medical record (e. g. , functional status). • Time Delay: Collection, aggregation, and reporting of insurance claims take time. When they finally become available to individuals, illnesses may have progressed significantly and preventable utilization or death may have already occurred. Source: https: //static 1. squarespace. com/static/548 b 623 fe 4 b 0991231 a 05 ff 0/t/55 ca 2 d 24 e 4 b 0 d 196 f 157 ebf 4/1439313188533/Proactively+Identifying+the+High+Cost+Population+W hite+Paper+-+Updated+August+5 th. pdf 19
Identifying the High Cost Population 2. Qualitative Methods • Factors not captured in claims or EHR data can be the best predictors of advanced illness or persistent spending. Patient-based self-reporting and engagement can be useful for targeting: • Patients with Advanced Illness: Vulnerable Elders Survey (VES-13), indications of active functional and/or nutritional decline (Karnovsky performance status, ADLs, involuntary weight loss, reduced intake, cachexia, etc. ) and more. • Patients with Persistent High Spending: PHQ-2 or PHQ-9, Veterans RAND 12 (VR-12), Patient Activation Measure (PAM), homelessness, physician referral and more (e. g. ADI). Source: https: //static 1. squarespace. com/static/548 b 623 fe 4 b 0991231 a 05 ff 0/t/55 ca 2 d 24 e 4 b 0 d 196 f 157 ebf 4/1439313188533/Proactively+Identifying+the+High+Cost+Population+W hite+Paper+-+Updated+August+5 th. pdf 20
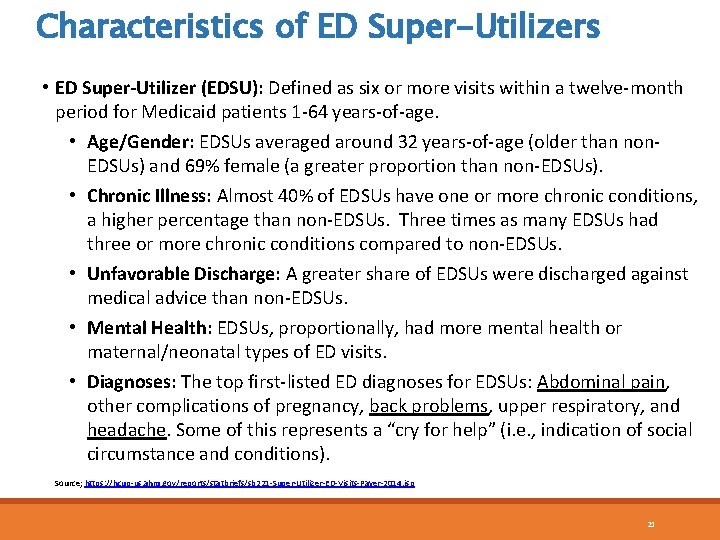
Characteristics of ED Super-Utilizers • ED Super-Utilizer (EDSU): Defined as six or more visits within a twelve-month period for Medicaid patients 1 -64 years-of-age. • Age/Gender: EDSUs averaged around 32 years-of-age (older than non. EDSUs) and 69% female (a greater proportion than non-EDSUs). • Chronic Illness: Almost 40% of EDSUs have one or more chronic conditions, a higher percentage than non-EDSUs. Three times as many EDSUs had three or more chronic conditions compared to non-EDSUs. • Unfavorable Discharge: A greater share of EDSUs were discharged against medical advice than non-EDSUs. • Mental Health: EDSUs, proportionally, had more mental health or maternal/neonatal types of ED visits. • Diagnoses: The top first-listed ED diagnoses for EDSUs: Abdominal pain, other complications of pregnancy, back problems, upper respiratory, and headache. Some of this represents a “cry for help” (i. e. , indication of social circumstance and conditions). Source; https: //hcup-us. ahrq. gov/reports/statbriefs/sb 221 -Super-Utilizer-ED-Visits-Payer-2014. jsp 21
The Area Deprivation Index (ADI)
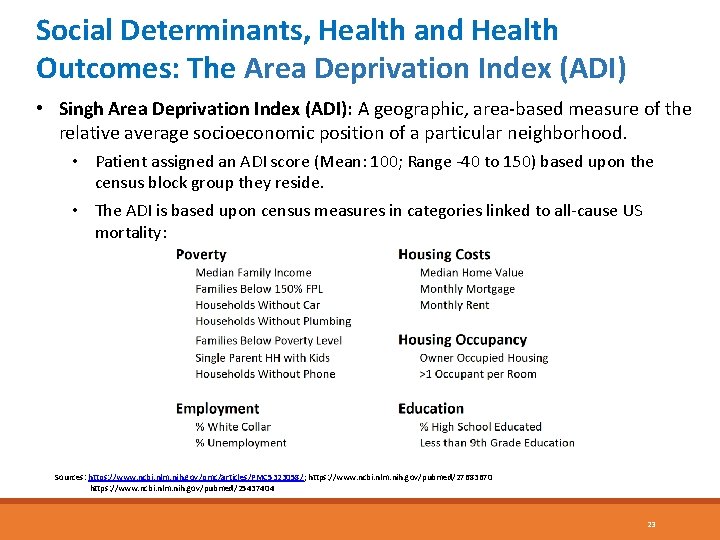
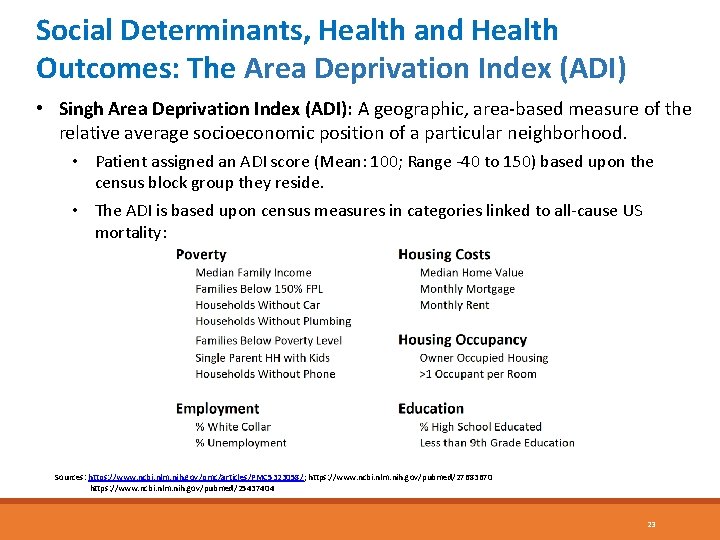
Social Determinants, Health and Health Outcomes: The Area Deprivation Index (ADI) • Singh Area Deprivation Index (ADI): A geographic, area-based measure of the relative average socioeconomic position of a particular neighborhood. • Patient assigned an ADI score (Mean: 100; Range -40 to 150) based upon the census block group they reside. • The ADI is based upon census measures in categories linked to all-cause US mortality: Sources: https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 5323058/; https: //www. ncbi. nlm. nih. gov/pubmed/27683670 https: //www. ncbi. nlm. nih. gov/pubmed/25437404 23
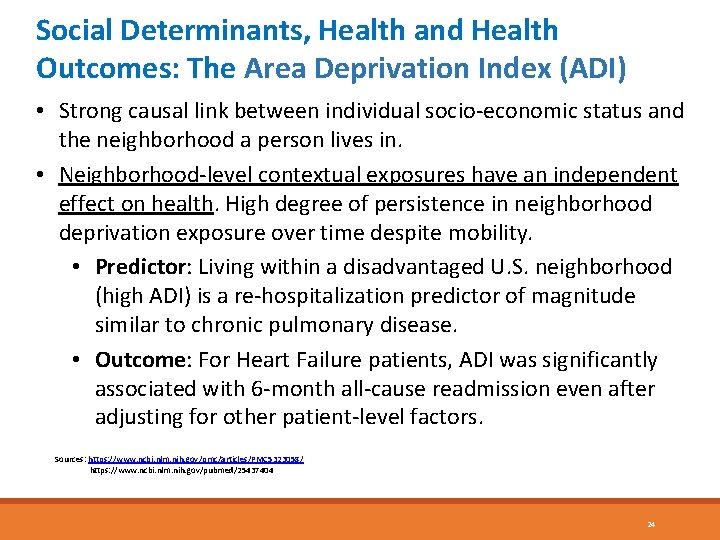
Social Determinants, Health and Health Outcomes: The Area Deprivation Index (ADI) • Strong causal link between individual socio-economic status and the neighborhood a person lives in. • Neighborhood-level contextual exposures have an independent effect on health. High degree of persistence in neighborhood deprivation exposure over time despite mobility. • Predictor: Living within a disadvantaged U. S. neighborhood (high ADI) is a re-hospitalization predictor of magnitude similar to chronic pulmonary disease. • Outcome: For Heart Failure patients, ADI was significantly associated with 6 -month all-cause readmission even after adjusting for other patient-level factors. Sources: https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 5323058/ https: //www. ncbi. nlm. nih. gov/pubmed/25437404 24
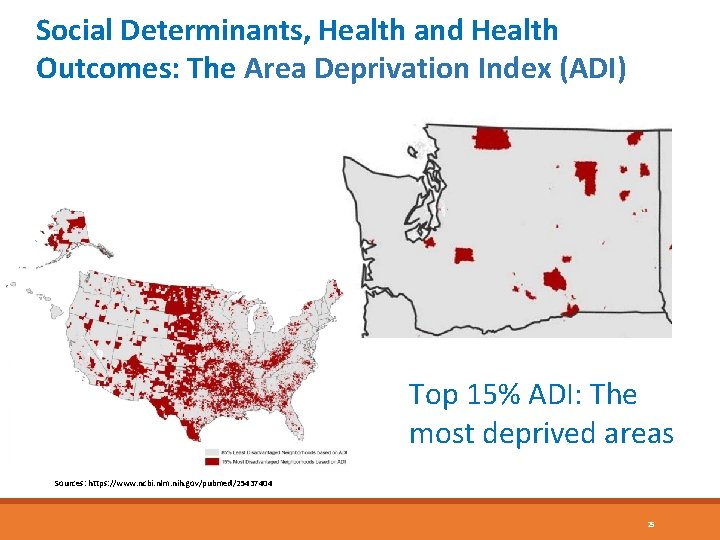
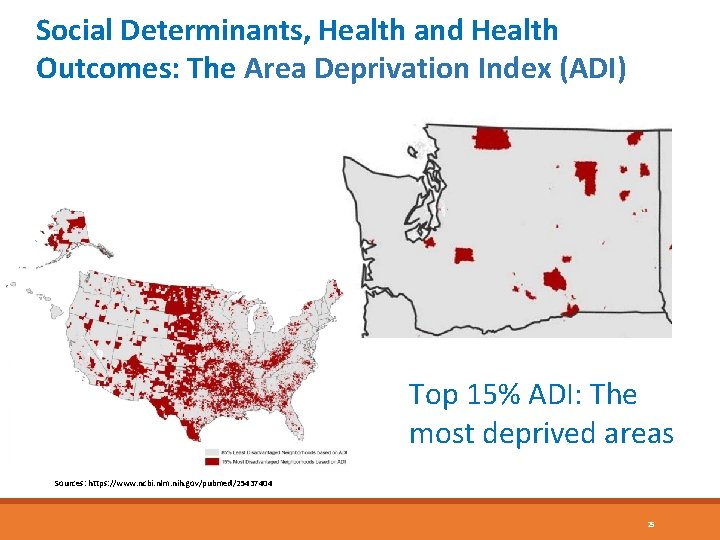
Social Determinants, Health and Health Outcomes: The Area Deprivation Index (ADI) Top 15% ADI: The most deprived areas Sources: https: //www. ncbi. nlm. nih. gov/pubmed/25437404 25
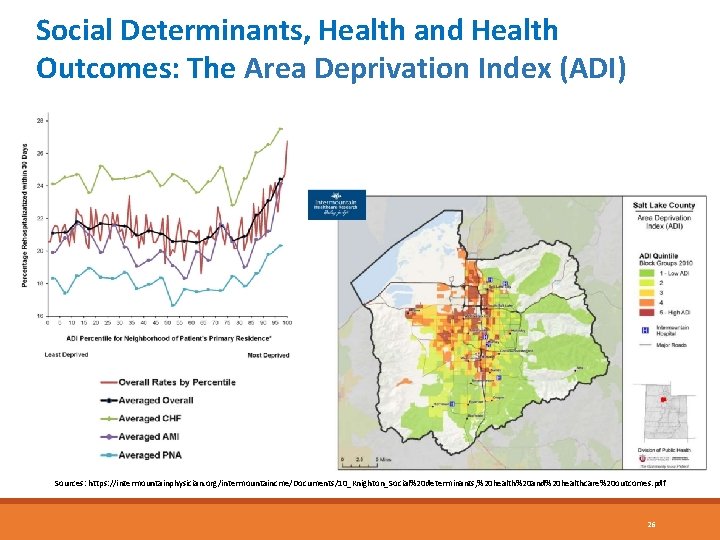
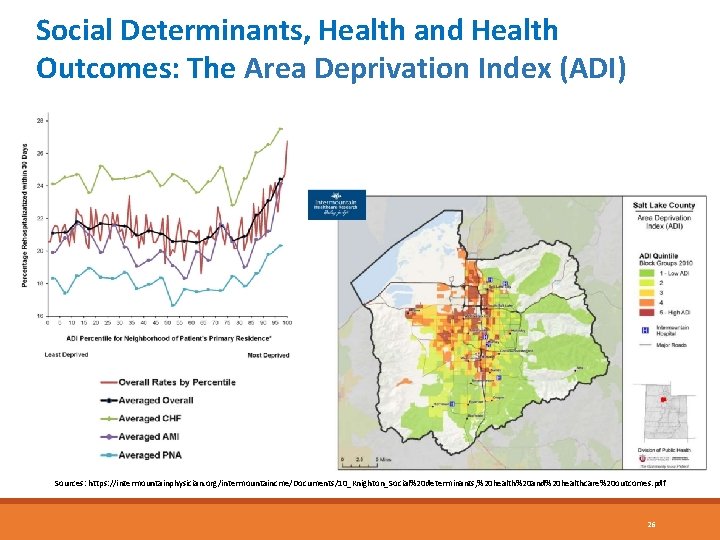
Social Determinants, Health and Health Outcomes: The Area Deprivation Index (ADI) Sources: https: //intermountainphysician. org/intermountaincme/Documents/10_Knighton_Social%20 determinants, %20 health%20 and%20 healthcare%20 outcomes. pdf 26
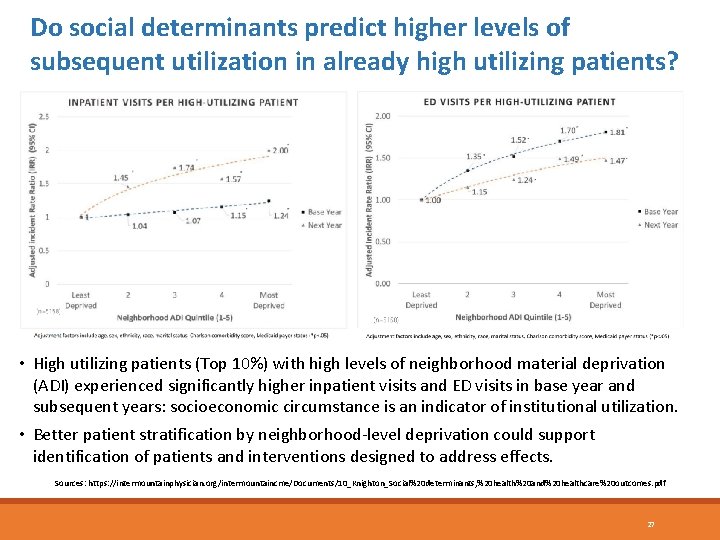
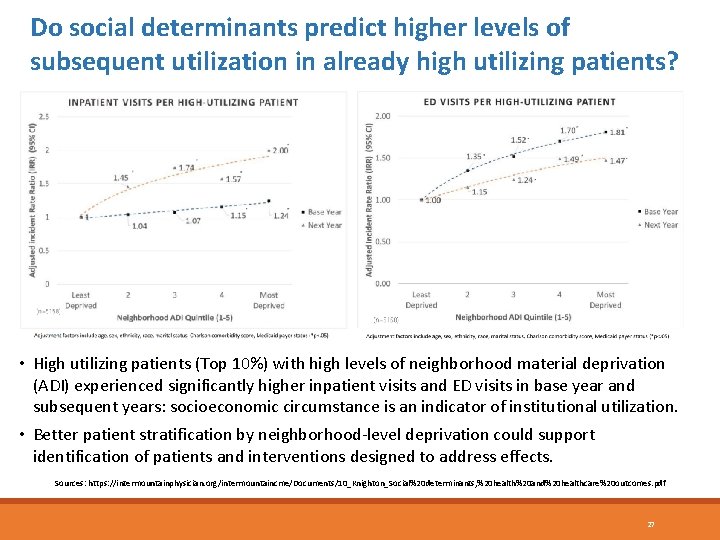
Do social determinants predict higher levels of subsequent utilization in already high utilizing patients? • High utilizing patients (Top 10%) with high levels of neighborhood material deprivation (ADI) experienced significantly higher inpatient visits and ED visits in base year and subsequent years: socioeconomic circumstance is an indicator of institutional utilization. • Better patient stratification by neighborhood-level deprivation could support identification of patients and interventions designed to address effects. Sources: https: //intermountainphysician. org/intermountaincme/Documents/10_Knighton_Social%20 determinants, %20 health%20 and%20 healthcare%20 outcomes. pdf 27
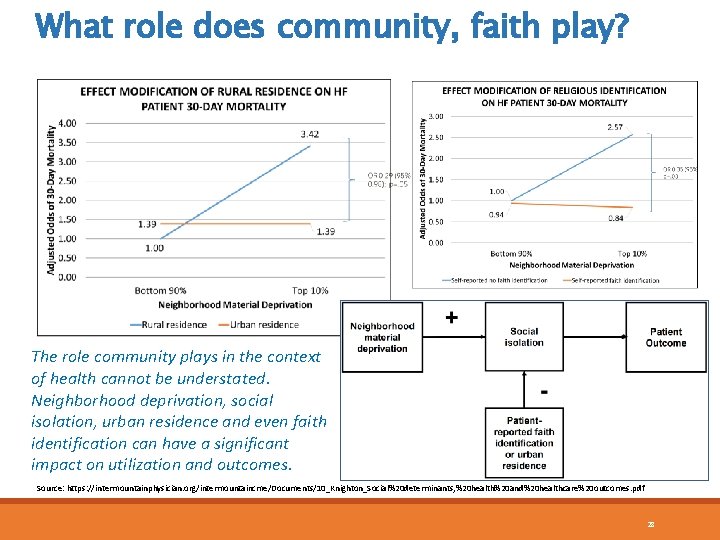
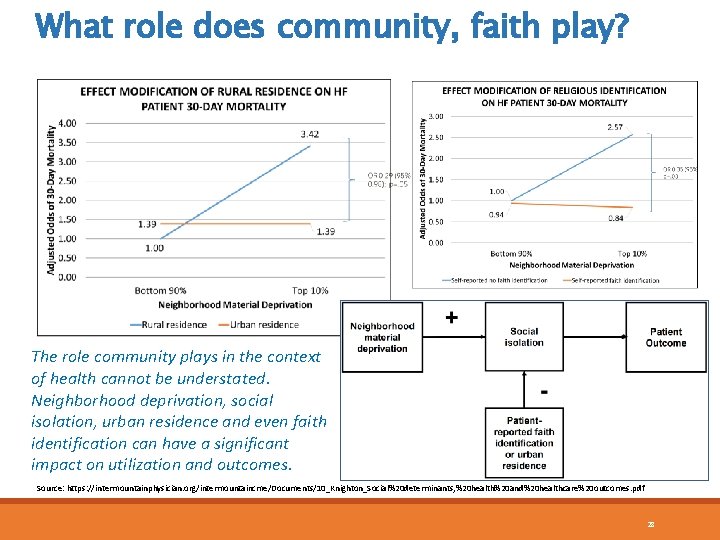
What role does community, faith play? The role community plays in the context of health cannot be understated. Neighborhood deprivation, social isolation, urban residence and even faith identification can have a significant impact on utilization and outcomes. Source: https: //intermountainphysician. org/intermountaincme/Documents/10_Knighton_Social%20 determinants, %20 health%20 and%20 healthcare%20 outcomes. pdf 28
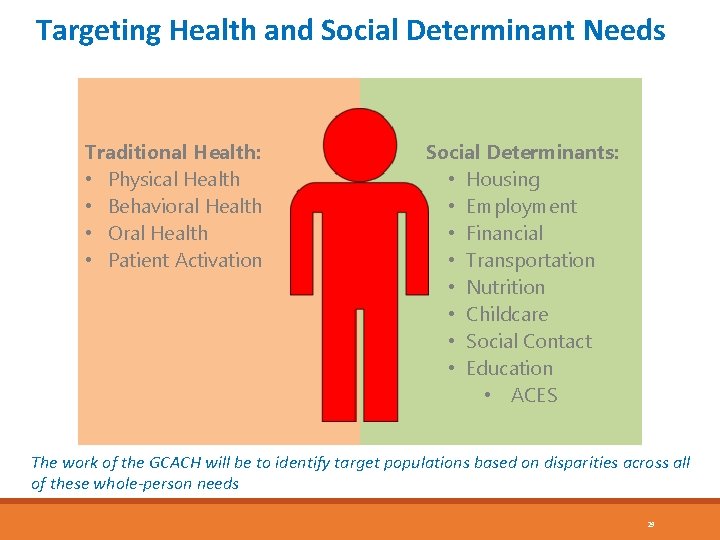
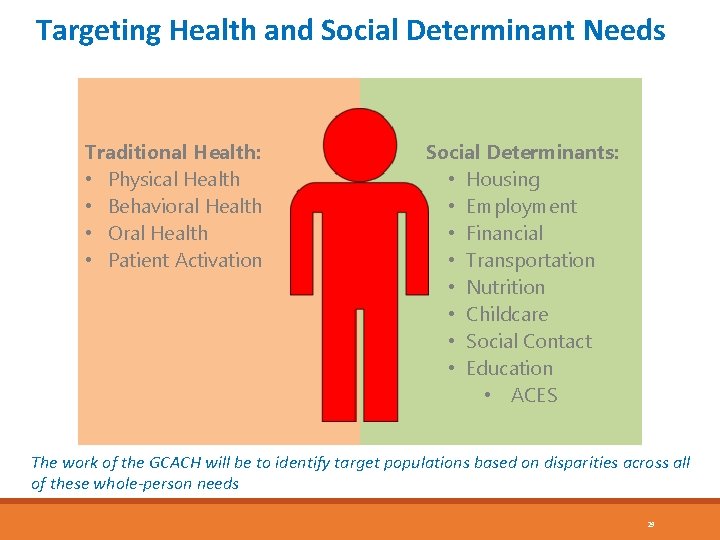
Targeting Health and Social Determinant Needs Traditional Health: • Physical Health • Behavioral Health • Oral Health • Patient Activation Social Determinants: • Housing • Employment • Financial • Transportation • Nutrition • Childcare • Social Contact • Education • ACES The work of the GCACH will be to identify target populations based on disparities across all of these whole-person needs 29
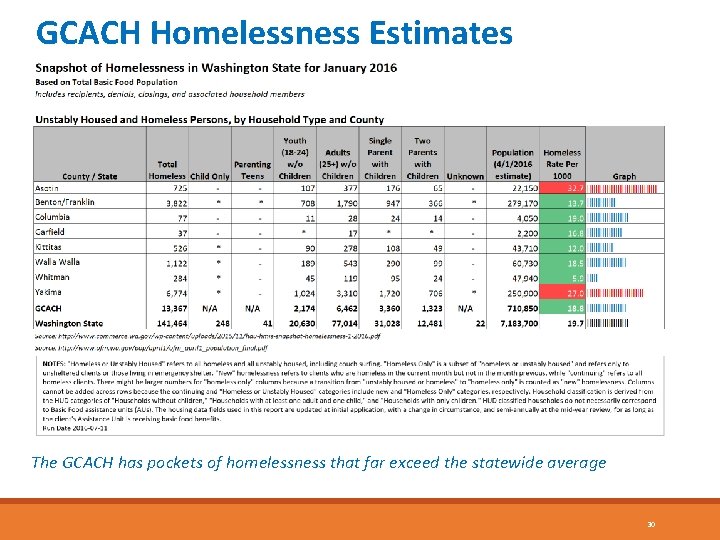
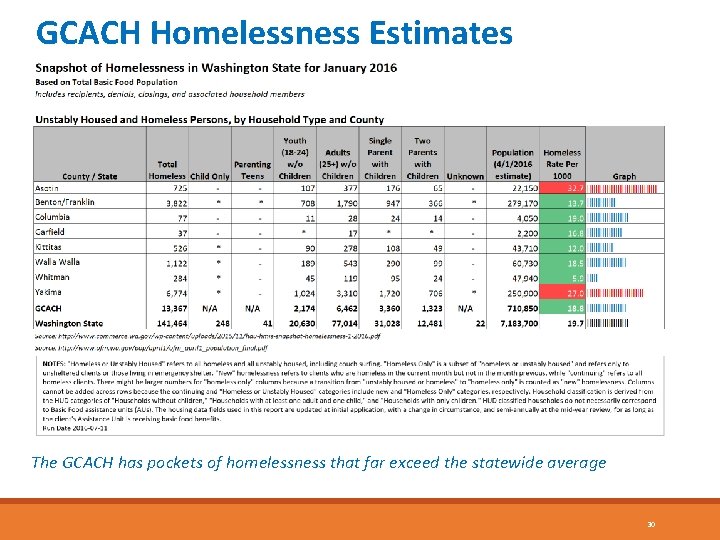
GCACH Homelessness Estimates The GCACH has pockets of homelessness that far exceed the statewide average 30
P 4 P Metric Achievement Value Calculation
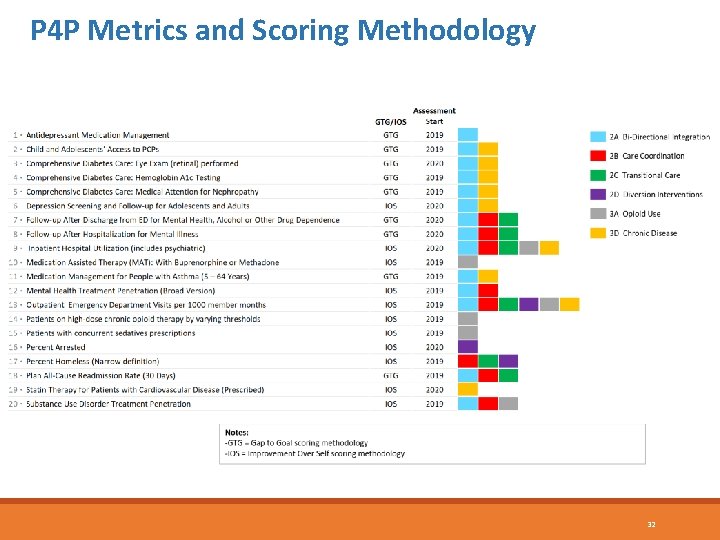
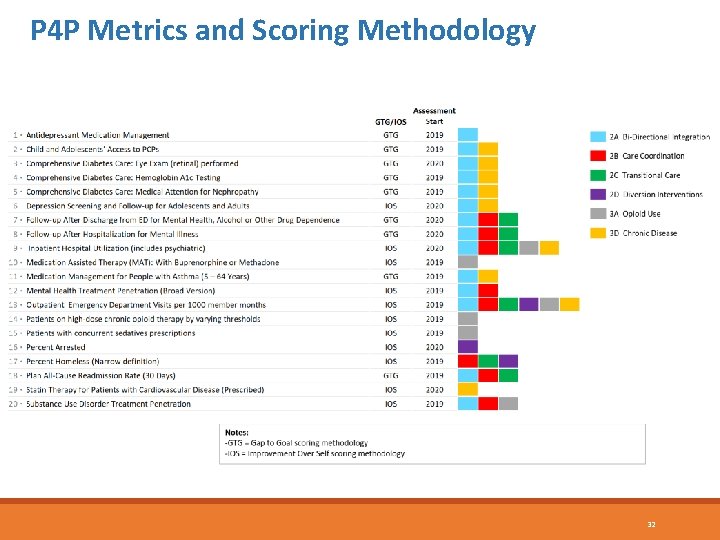
P 4 P Metrics and Scoring Methodology 32
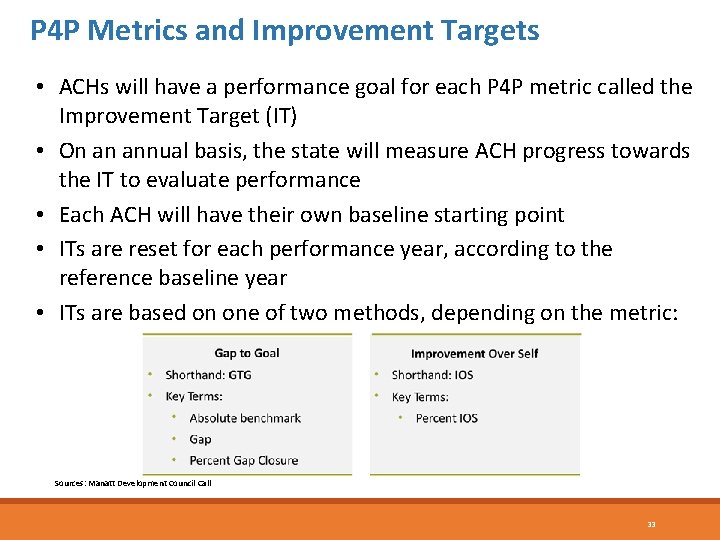
P 4 P Metrics and Improvement Targets • ACHs will have a performance goal for each P 4 P metric called the Improvement Target (IT) • On an annual basis, the state will measure ACH progress towards the IT to evaluate performance • Each ACH will have their own baseline starting point • ITs are reset for each performance year, according to the reference baseline year • ITs are based on one of two methods, depending on the metric: Sources: Manatt Development Council Call 33
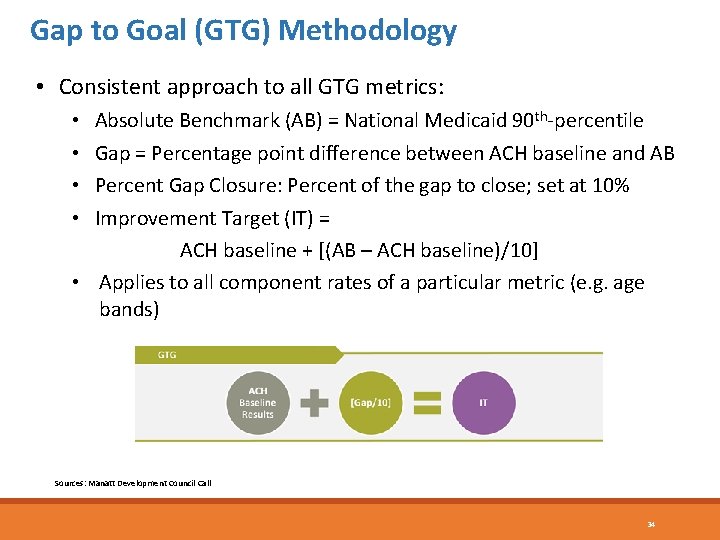
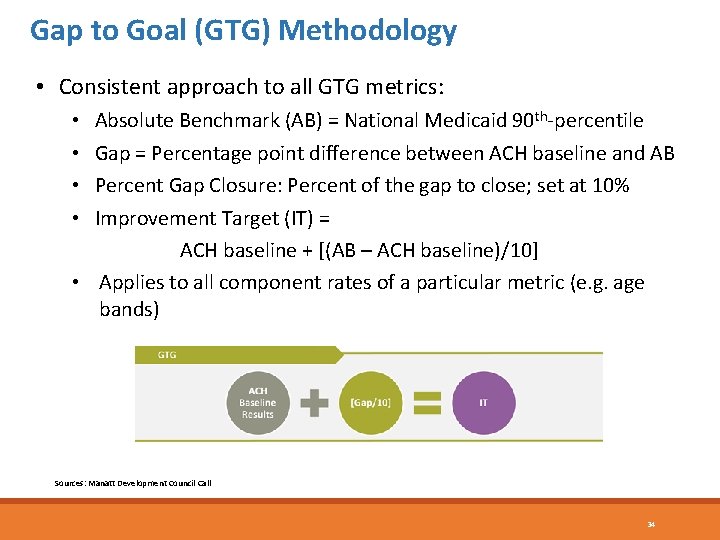
Gap to Goal (GTG) Methodology • Consistent approach to all GTG metrics: Absolute Benchmark (AB) = National Medicaid 90 th-percentile Gap = Percentage point difference between ACH baseline and AB Percent Gap Closure: Percent of the gap to close; set at 10% Improvement Target (IT) = ACH baseline + [(AB – ACH baseline)/10] • Applies to all component rates of a particular metric (e. g. age bands) • • Sources: Manatt Development Council Call 34
Gap to Goal (GTG) Example • Example: Absolute benchmark = 69. 4% ACH baseline performance = 50. 0% Gap = (69. 4% - 50. 0%) = 19. 4% percentage points Percent gap closure = 10% of 19. 4% percentage points = 1. 94% percentage points • Improvement Target (IT) = 50. 0% + 1. 94% = 51. 94% • • Sources: Manatt Development Council Call 35
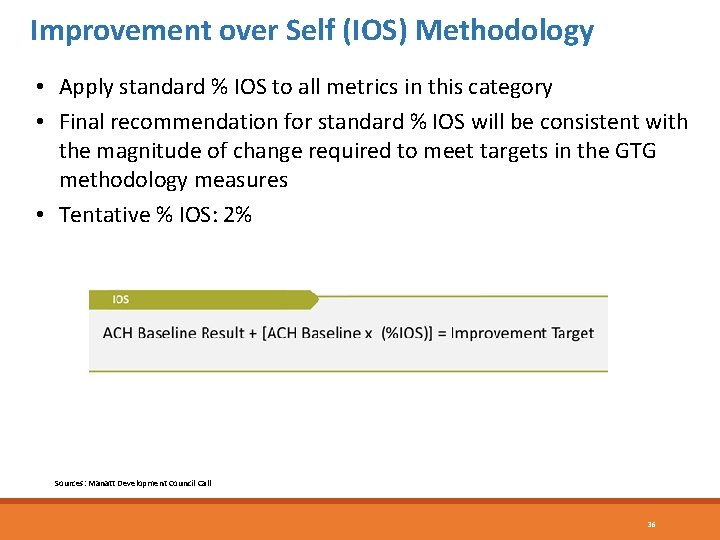
Improvement over Self (IOS) Methodology • Apply standard % IOS to all metrics in this category • Final recommendation for standard % IOS will be consistent with the magnitude of change required to meet targets in the GTG methodology measures • Tentative % IOS: 2% Sources: Manatt Development Council Call 36
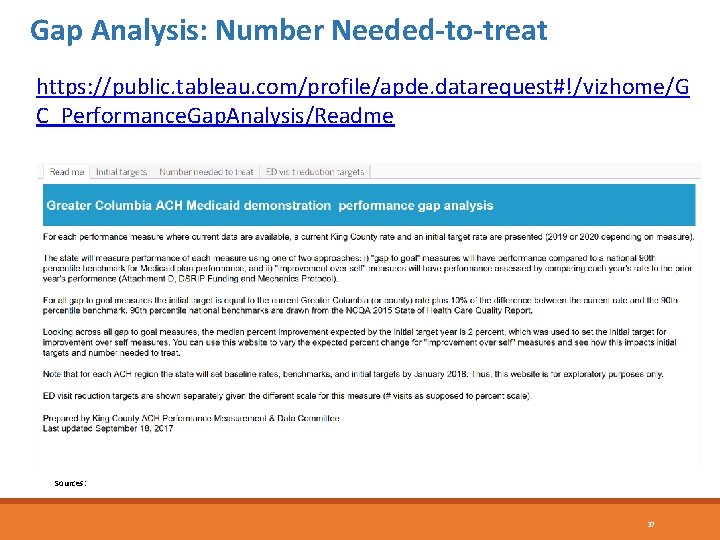
Gap Analysis: Number Needed-to-treat https: //public. tableau. com/profile/apde. datarequest#!/vizhome/G C_Performance. Gap. Analysis/Readme Sources: 37
Questions?
 Adi
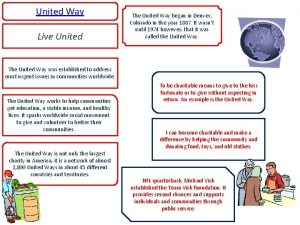
Adi United way centre county
United way centre county United way social innovation accelerator
United way social innovation accelerator United way pledge form
United way pledge form United way helpline
United way helpline United way of washington county md
United way of washington county md Trace industries hopkinsville ky
Trace industries hopkinsville ky United way of dane county
United way of dane county Team spirit becomes team infatuation
Team spirit becomes team infatuation Team spirit becomes team infatuation
Team spirit becomes team infatuation The white team cheers for the blue team, just like
The white team cheers for the blue team, just like Terminal access controller access control system
Terminal access controller access control system Terminal access controller access-control system
Terminal access controller access-control system Personification examples for computer
Personification examples for computer Marginal frequency
Marginal frequency Perbedaan one way dan two way anova
Perbedaan one way dan two way anova Explain threaded binary tree
Explain threaded binary tree Beda one way anova dan two way anova
Beda one way anova dan two way anova One-way anova hypothesis testing
One-way anova hypothesis testing One way anova vs two way anova
One way anova vs two way anova Contoh soal anova two way
Contoh soal anova two way The old way and the new way
The old way and the new way Bottle of rum to fill my tum
Bottle of rum to fill my tum Walk this way talk this way
Walk this way talk this way Toronto western family health team
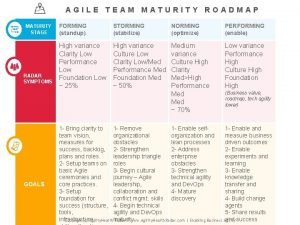
Toronto western family health team Team radar retro
Team radar retro Radar
Radar Team health check
Team health check Health team relations
Health team relations Marathon health clinic
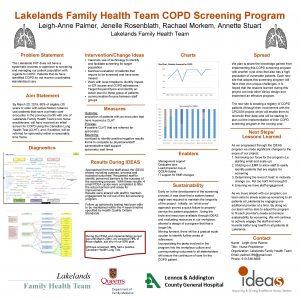
Marathon health clinic Lakelands family health team
Lakelands family health team Chapter 8 communication and the nurse patient relationship
Chapter 8 communication and the nurse patient relationship Function of health team
Function of health team Dr david makary
Dr david makary Setfht
Setfht Unit c health care systems
Unit c health care systems Health access network
Health access network Myhealthaccess network
Myhealthaccess network Flake advert
Flake advert