Patient Safety Community of Practice South East Toronto








- Slides: 18

Patient Safety Community of Practice South East Toronto Family Health Team Experience 1
Strategy 1. Foster formal Incident Analysis through Patient Safety Rounds via Informal Reporting 2. Parallel Development of Proactive Accreditation 3. Parallel Formalization of the Reporting of Incidents 4. Expansion of Faculty Capacity for Incident Analysis 2
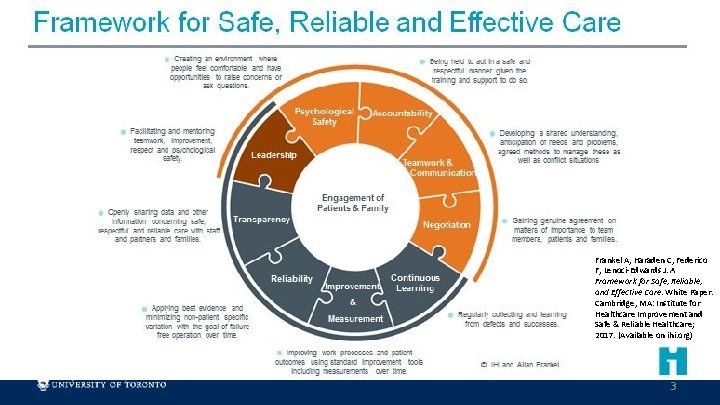
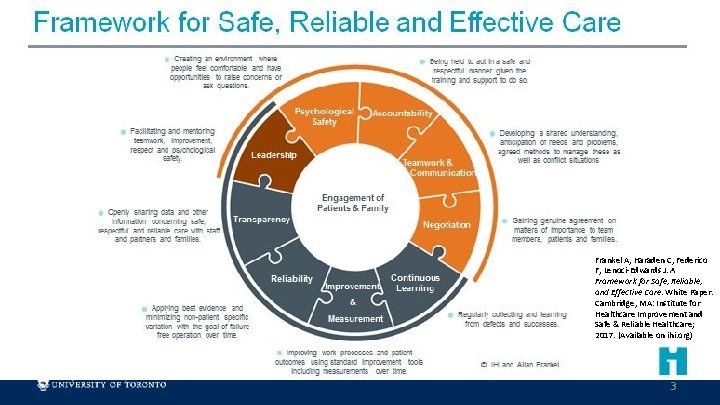
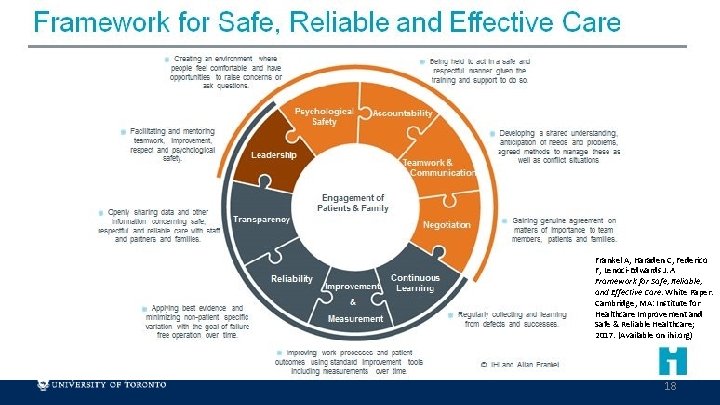
Frankel A, Haraden C, Federico F, Lenoci-Edwards J. A Framework for Safe, Reliable, and Effective Care. White Paper. Cambridge, MA: Institute for Healthcare Improvement and Safe & Reliable Healthcare; 2017. (Available on ihi. org) 3

Patient Safety Rounds • Informal Reporting of incidents through friends/colleagues through the discussion of cases • Physical environment facilitates discussions • The presence of an underlying and open culture of safety amongst providers • Support from Leadership 4
Patient Safety Rounds • Means of formalizing mental exercises when individuals review their practice after an incident • Allow for greater organizational impact with the potential for process change and communication. 5

Patient Safety Rounds • 2 Organization-Wide Rounds where discussion re: Incident Safety Analysis occurred via OTN through 2 sites • Multiple providers including ED, Nursing, Nurse Practitioners, Dietitians, Pharmacist, Social Workers, Clinical Care Coordinator, Physicians • Well attended by staff • Not as well attended by residents • Reach out to improve resident attendance moving forward 6

Patient Safety Rounds • 2 smaller, more informal rounds occurring with a subset of staff and then presented in different forums as a communiqué • FHO meetings • Board of Directors meetings 7
Patient Safety Rounds • Medical emergencies in the office: 2 incidents of anaphylaxis • Review of Policy of Ward Stock of Medications • Adherence to Check Box review of inventory of emergency medications, expiry dates, functionality of AED on site • Training of staff in BLS and ACLS in coordinated format • Development of Case Studies led by faculty for emergency preparedness 8
Patient Safety Rounds • Incident Involving the Reporting of Critical Results • Process for reporting of after-hours critical results to ordering staff • The development of a process for the reporting of critical results verbally • Introduction of clinical tools in the Electronic Medical Record 9
Patient Safety Rounds • Incident involving transitions in care in the Residency Practice • Static supervisors as patient transition from one resident to another • Greater orientation to generate patient lists for residents when they enter residency 10

Migration to Accreditation System • Accreditation-type environment in a community based academic practice: • A work in progress with review of reprocessed items and best practice as per Public Health Ontario 11
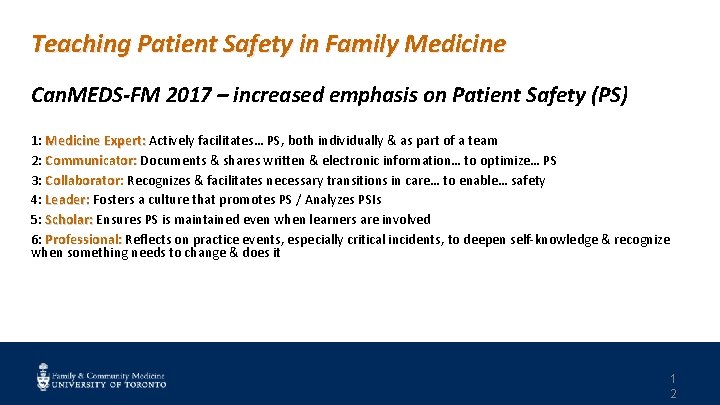
Teaching Patient Safety in Family Medicine Can. MEDS-FM 2017 – increased emphasis on Patient Safety (PS) 1: Medicine Expert: Actively facilitates… PS, both individually & as part of a team Expert: 2: Communicator: Documents & shares written & electronic information… to optimize… PS Communicator: 3: Collaborator: Recognizes & facilitates necessary transitions in care… to enable… safety Collaborator: 4: Leader: Fosters a culture that promotes PS / Analyzes PSIs Leader: 5: Scholar: Ensures PS is maintained even when learners are involved Scholar: 6: Professional: Reflects on practice events, especially critical incidents, to deepen self-knowledge & recognize Professional: when something needs to change & does it 1 2
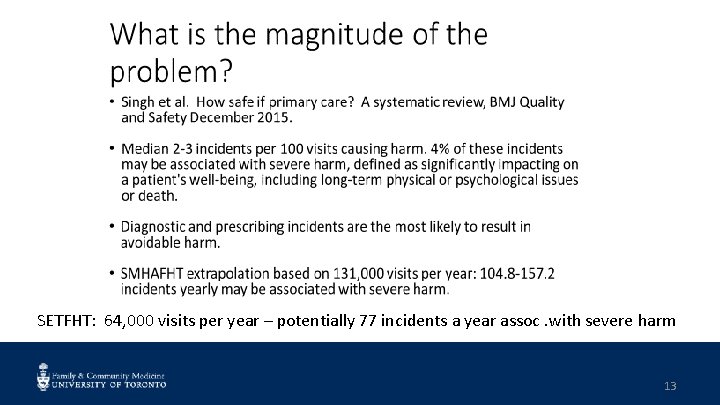
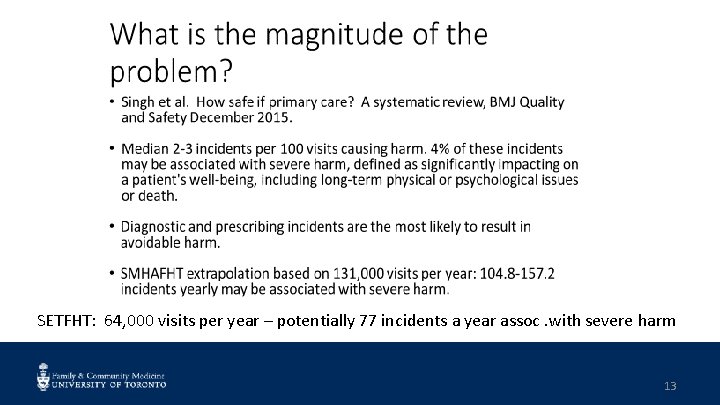
SETFHT: 64, 000 visits per year – potentially 77 incidents a year assoc. with severe harm 13

14

What are common incidents in primary care? COMMON THEME INTERSECTS WITH Communication Missed or Delayed Diagnosis Vaccinations Medication Management Pediatric Dosing Errors Administrative process Provider knowledge & skills CPSI 2010 Patient Safety in Primary Care 1 5
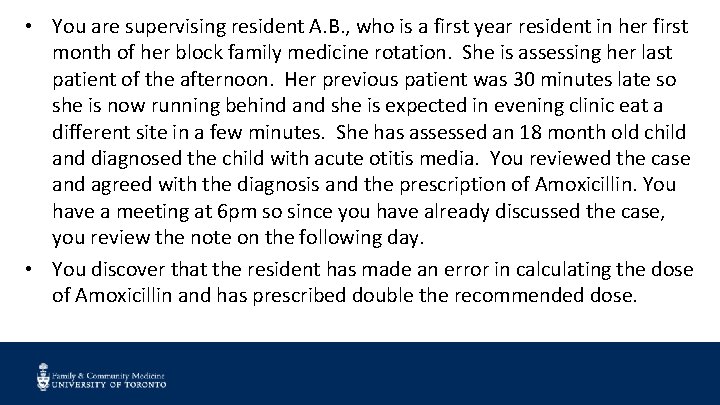
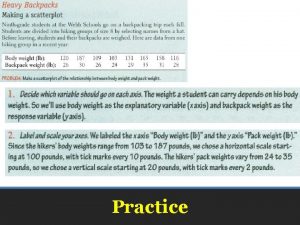
• You are supervising resident A. B. , who is a first year resident in her first month of her block family medicine rotation. She is assessing her last patient of the afternoon. Her previous patient was 30 minutes late so she is now running behind and she is expected in evening clinic eat a different site in a few minutes. She has assessed an 18 month old child and diagnosed the child with acute otitis media. You reviewed the case and agreed with the diagnosis and the prescription of Amoxicillin. You have a meeting at 6 pm so since you have already discussed the case, you review the note on the following day. • You discover that the resident has made an error in calculating the dose of Amoxicillin and has prescribed double the recommended dose.

1. What issues does this case raise? 2. What steps do you need to take, and in what order? 3. How could you use the incident analysis tool in this situation? 4. How would you discuss your own role as supervisor in the incident? 17
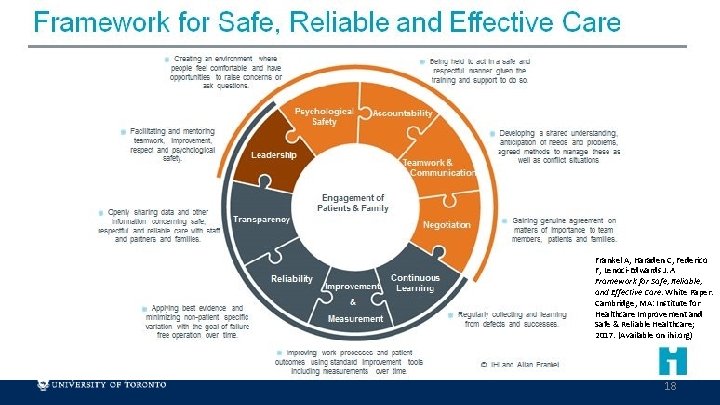
Frankel A, Haraden C, Federico F, Lenoci-Edwards J. A Framework for Safe, Reliable, and Effective Care. White Paper. Cambridge, MA: Institute for Healthcare Improvement and Safe & Reliable Healthcare; 2017. (Available on ihi. org) 18
 South east toronto family health team
South east toronto family health team Horizontal movement of air
Horizontal movement of air Mid east toronto
Mid east toronto Patient 2 patient
Patient 2 patient North american
North american East is east and west is west
East is east and west is west Southeast region capitals and abbreviations
Southeast region capitals and abbreviations Orthopaedic treatment south east london
Orthopaedic treatment south east london Maps.google.comps
Maps.google.comps The meeting of longitude and latitude lines
The meeting of longitude and latitude lines Jppso southeast
Jppso southeast 50 nifty united states
50 nifty united states Fifty united states
Fifty united states Southeast asian ministers of education
Southeast asian ministers of education North south east west leadership styles
North south east west leadership styles South east regional hospital
South east regional hospital North east south west
North east south west South east strategic partnership for migration
South east strategic partnership for migration North, south east west leadership styles
North, south east west leadership styles