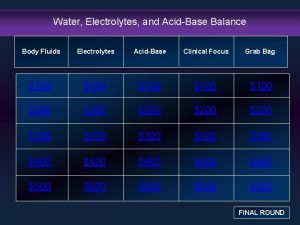
FLUIDS ELECTROLYTES NCLIN 411 Seminar April 21 2014





- Slides: 31
FLUIDS & ELECTROLYTES NCLIN 411 Seminar April 21, 2014 Instructor: Musetta C Fu

FLUID BALANCE REGULATION Antidiuretic hormone (ADH) secreted by posterior pituitary gland ADH = H 2 O retention Aldosterone (Na+ regulation) secreted by Adrenal Cortex aldosterone = Na H 2 O Sodium concentration Where Na goes, water follows
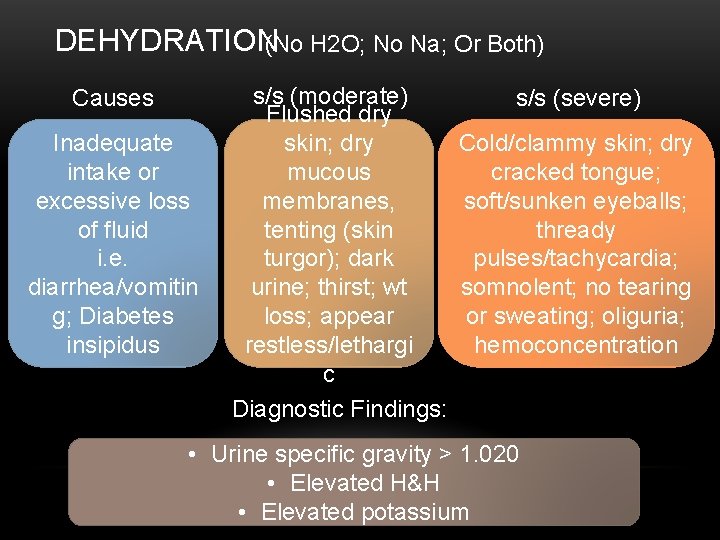
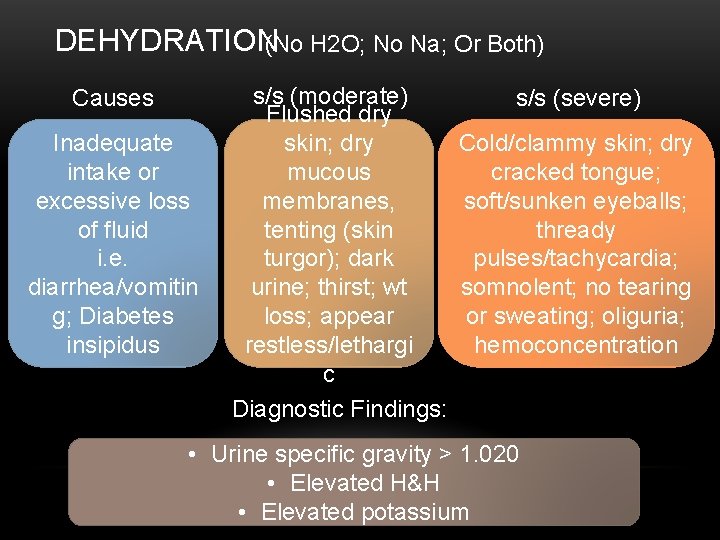
DEHYDRATION(No H 2 O; No Na; Or Both) Causes Inadequate intake or excessive loss of fluid i. e. diarrhea/vomitin g; Diabetes insipidus s/s (moderate) Flushed dry skin; dry mucous membranes, tenting (skin turgor); dark urine; thirst; wt loss; appear restless/lethargi c Diagnostic Findings: s/s (severe) Cold/clammy skin; dry cracked tongue; soft/sunken eyeballs; thready pulses/tachycardia; somnolent; no tearing or sweating; oliguria; hemoconcentration • Urine specific gravity > 1. 020 • Elevated H&H • Elevated potassium
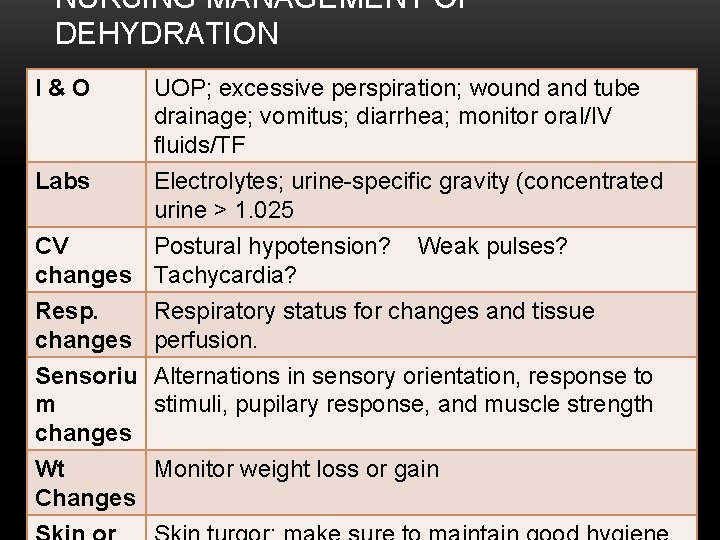
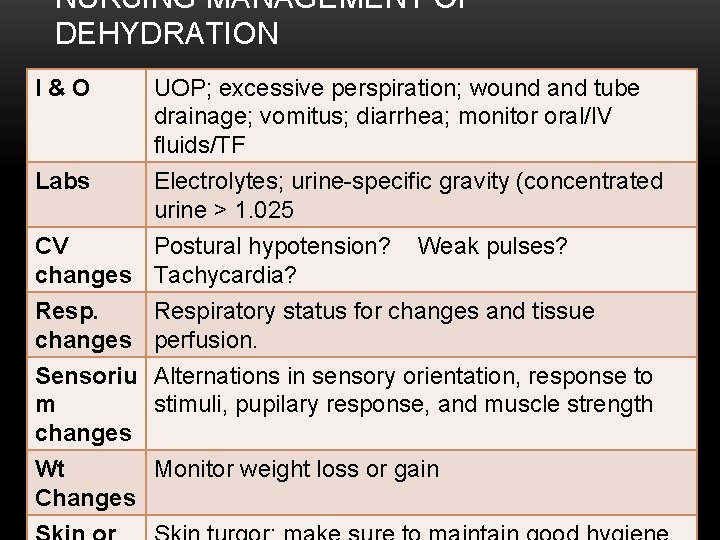
NURSING MANAGEMENT OF DEHYDRATION I&O Labs UOP; excessive perspiration; wound and tube drainage; vomitus; diarrhea; monitor oral/IV fluids/TF Electrolytes; urine-specific gravity (concentrated urine > 1. 025 CV Postural hypotension? changes Tachycardia? Resp. changes Sensoriu m changes Wt Changes Weak pulses? Respiratory status for changes and tissue perfusion. Alternations in sensory orientation, response to stimuli, pupilary response, and muscle strength Monitor weight loss or gain
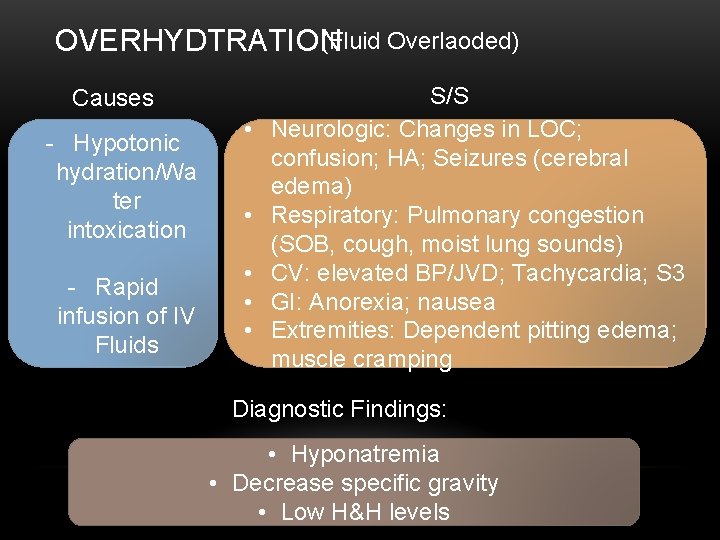
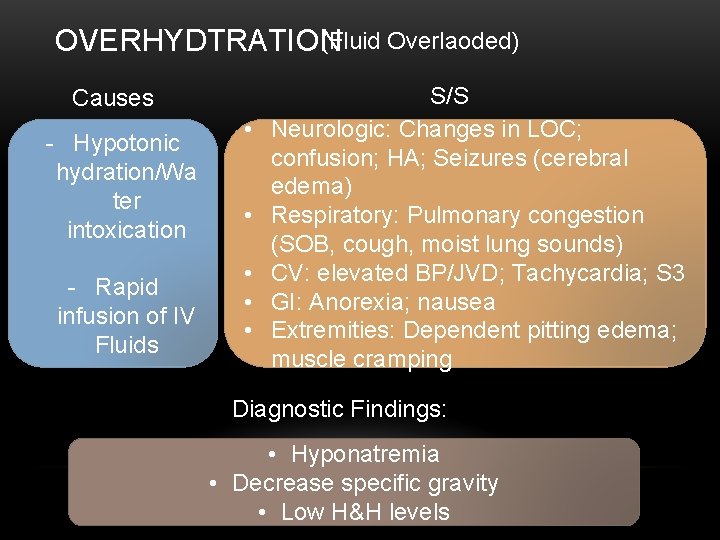
(Fluid Overlaoded) OVERHYDTRATION Causes - Hypotonic hydration/Wa ter intoxication - Rapid infusion of IV Fluids • • • S/S Neurologic: Changes in LOC; confusion; HA; Seizures (cerebral edema) Respiratory: Pulmonary congestion (SOB, cough, moist lung sounds) CV: elevated BP/JVD; Tachycardia; S 3 GI: Anorexia; nausea Extremities: Dependent pitting edema; muscle cramping Diagnostic Findings: • Hyponatremia • Decrease specific gravity • Low H&H levels
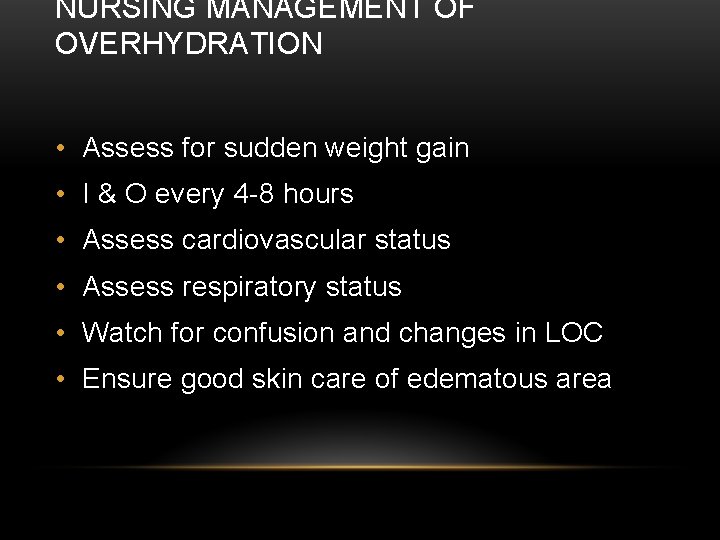
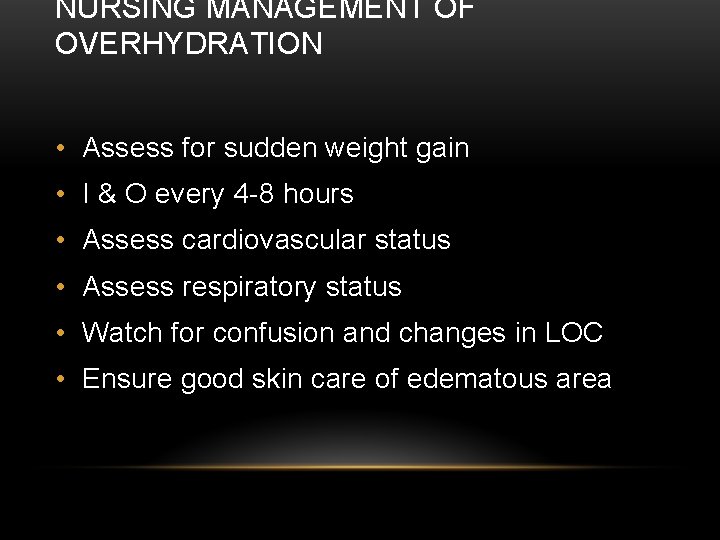
NURSING MANAGEMENT OF OVERHYDRATION • Assess for sudden weight gain • I & O every 4 -8 hours • Assess cardiovascular status • Assess respiratory status • Watch for confusion and changes in LOC • Ensure good skin care of edematous area
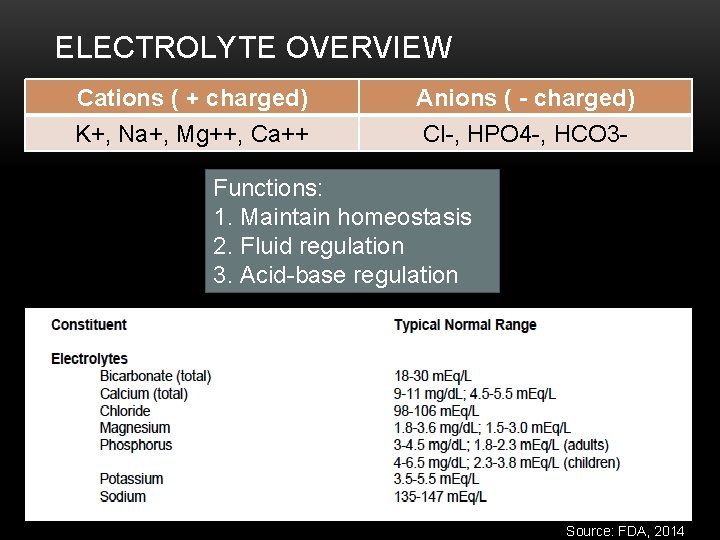
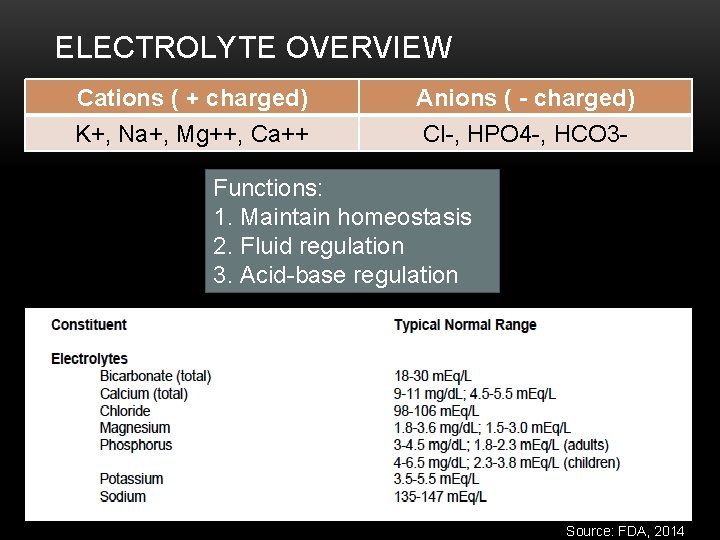
ELECTROLYTE OVERVIEW Cations ( + charged) K+, Na+, Mg++, Ca++ Anions ( - charged) Cl-, HPO 4 -, HCO 3 - Functions: 1. Maintain homeostasis 2. Fluid regulation 3. Acid-base regulation Source: FDA, 2014
SODIUM • Regulates osmolality • Helps maintain BP by balancing the volume of water in the body • Works with other electrolytes to promote the transmission of nerve impulses to muscles and tissues • Helps maintain acid-base balance
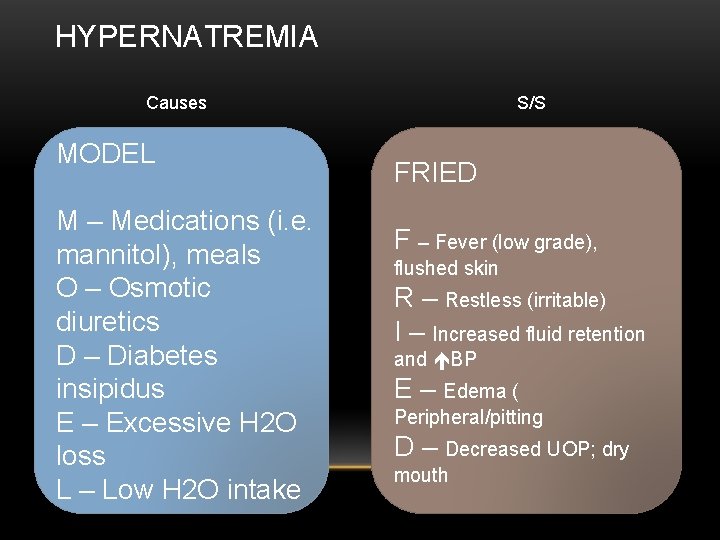
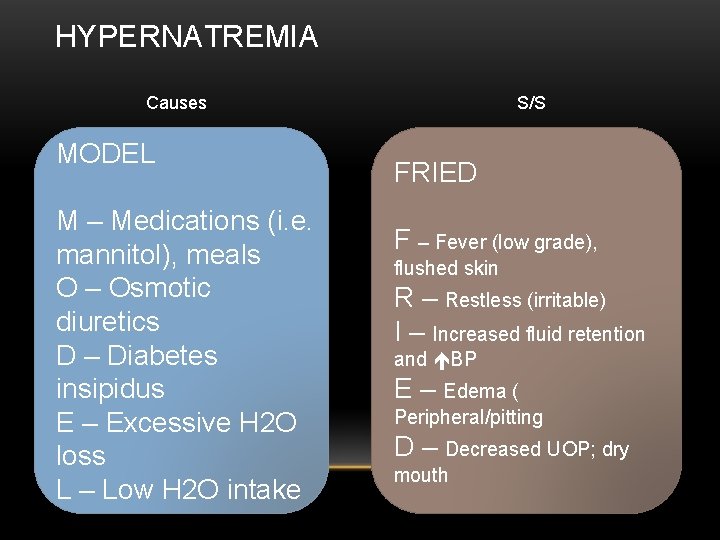
HYPERNATREMIA Causes MODEL M – Medications (i. e. mannitol), meals O – Osmotic diuretics D – Diabetes insipidus E – Excessive H 2 O loss L – Low H 2 O intake S/S FRIED F – Fever (low grade), flushed skin R – Restless (irritable) I – Increased fluid retention and BP E – Edema ( Peripheral/pitting D – Decreased UOP; dry mouth
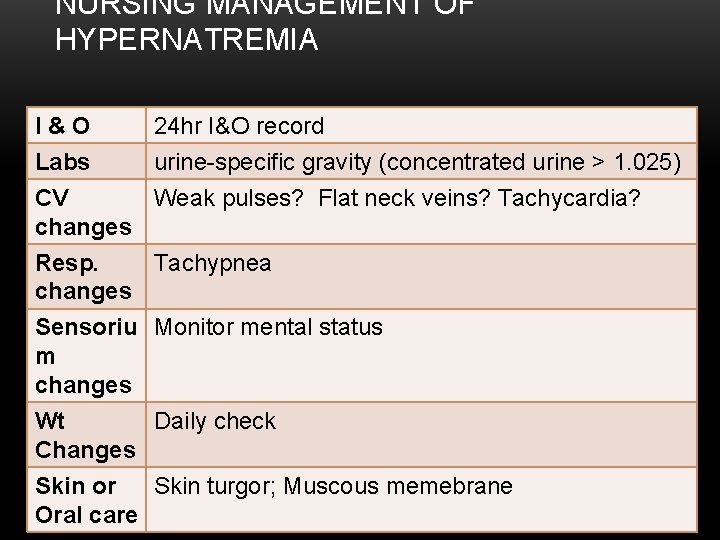
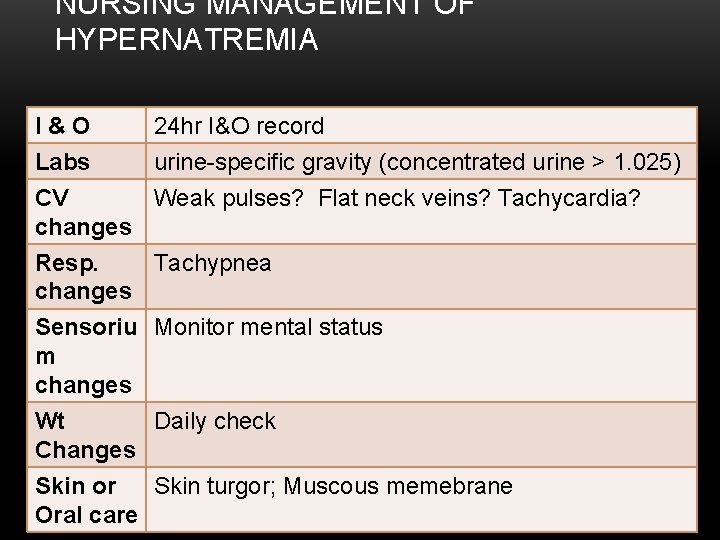
NURSING MANAGEMENT OF HYPERNATREMIA I&O 24 hr I&O record Labs urine-specific gravity (concentrated urine > 1. 025) CV Weak pulses? Flat neck veins? Tachycardia? changes Resp. Tachypnea changes Sensoriu Monitor mental status m changes Wt Daily check Changes Skin or Skin turgor; Muscous memebrane Oral care
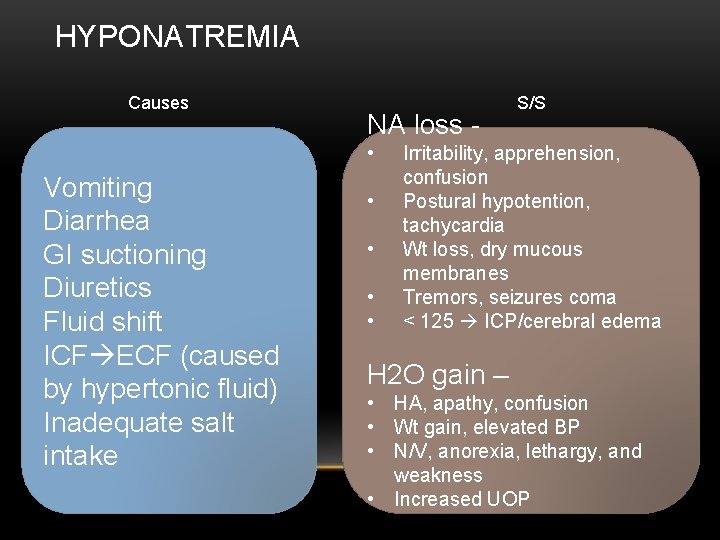
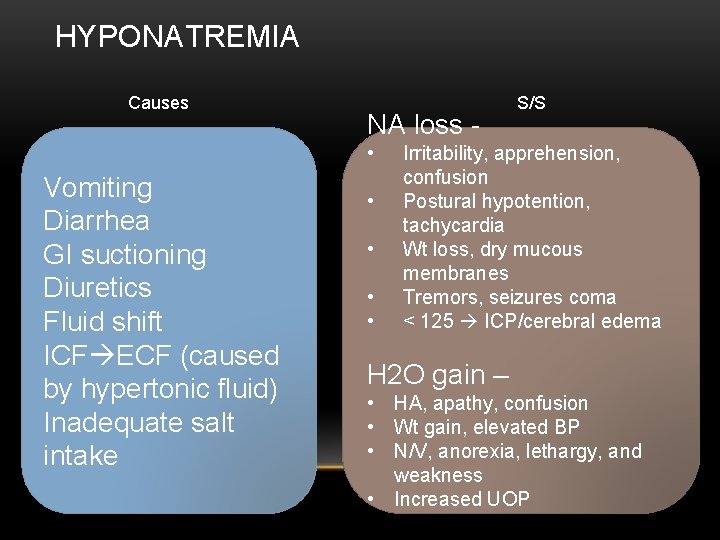
HYPONATREMIA Causes NA loss • Vomiting Diarrhea GI suctioning Diuretics Fluid shift ICF ECF (caused by hypertonic fluid) Inadequate salt intake • • S/S Irritability, apprehension, confusion Postural hypotention, tachycardia Wt loss, dry mucous membranes Tremors, seizures coma < 125 ICP/cerebral edema H 2 O gain – • HA, apathy, confusion • Wt gain, elevated BP • N/V, anorexia, lethargy, and weakness • Increased UOP

NURSING MANAGEMENT OF HYPONATREMIA I&O 24 hr I&O record Labs urine-specific gravity (concentrated urine < 1. 010) CV Check for bounding pulses or bulging neck veins changes Resp. Check for respiratory changes (fluid overloaded) changes Sensoriu Monitor mental status for cerebral edema m changes Wt Daily check Changes Skin or Pitting edema with fluid excess Oral care
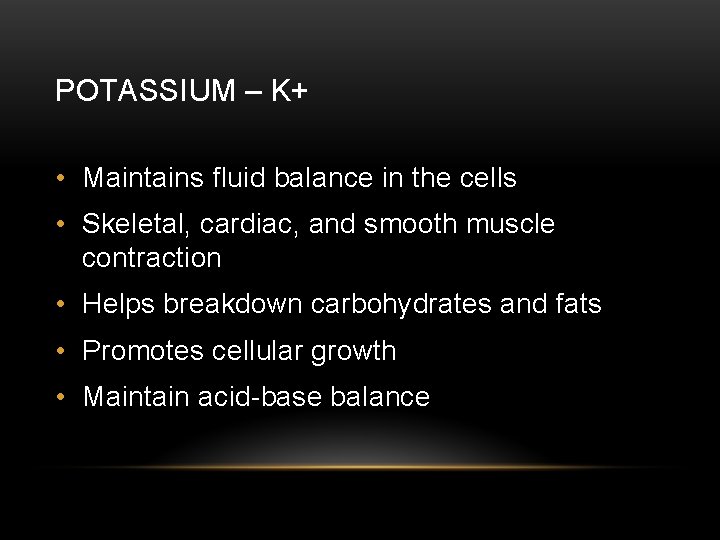
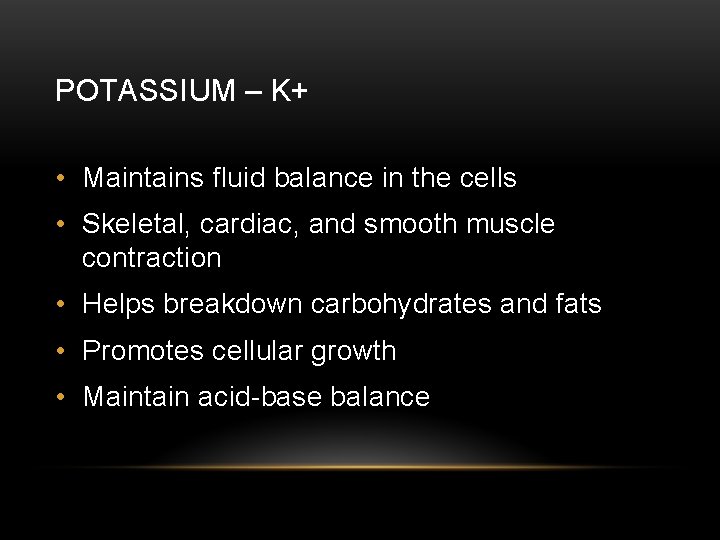
POTASSIUM – K+ • Maintains fluid balance in the cells • Skeletal, cardiac, and smooth muscle contraction • Helps breakdown carbohydrates and fats • Promotes cellular growth • Maintain acid-base balance
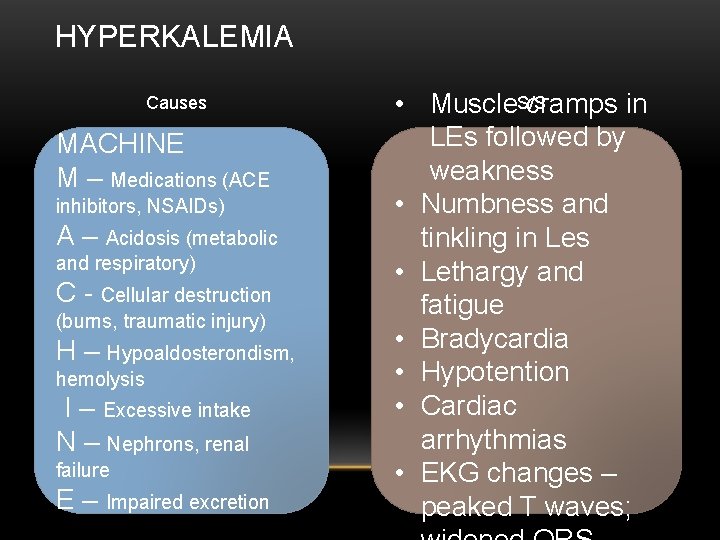
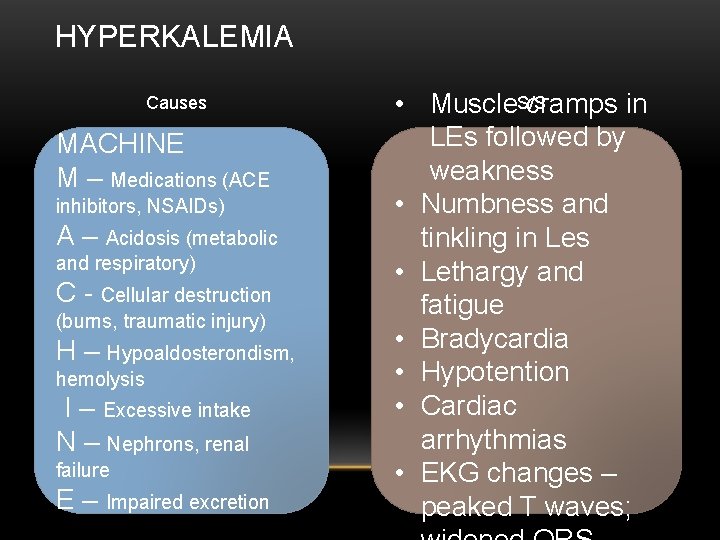
HYPERKALEMIA Causes MACHINE M – Medications (ACE inhibitors, NSAIDs) A – Acidosis (metabolic and respiratory) C - Cellular destruction (burns, traumatic injury) H – Hypoaldosterondism, hemolysis I – Excessive intake N – Nephrons, renal failure E – Impaired excretion • Muscle. S/S cramps in LEs followed by weakness • Numbness and tinkling in Les • Lethargy and fatigue • Bradycardia • Hypotention • Cardiac arrhythmias • EKG changes – peaked T waves;
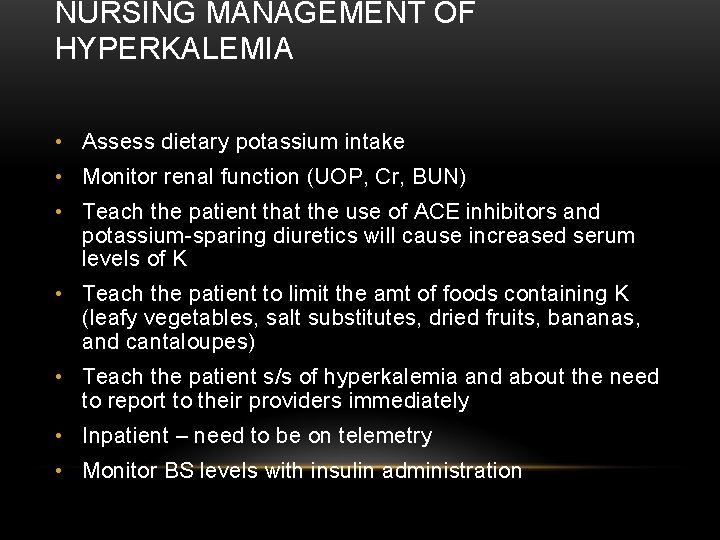
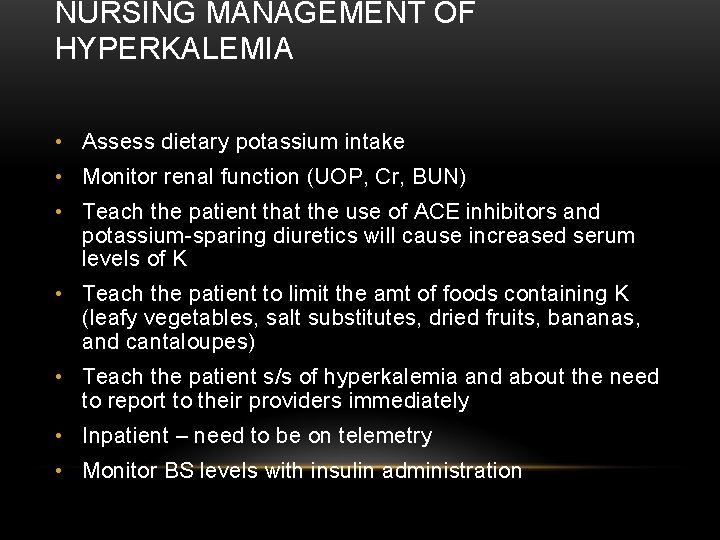
NURSING MANAGEMENT OF HYPERKALEMIA • Assess dietary potassium intake • Monitor renal function (UOP, Cr, BUN) • Teach the patient that the use of ACE inhibitors and potassium-sparing diuretics will cause increased serum levels of K • Teach the patient to limit the amt of foods containing K (leafy vegetables, salt substitutes, dried fruits, bananas, and cantaloupes) • Teach the patient s/s of hyperkalemia and about the need to report to their providers immediately • Inpatient – need to be on telemetry • Monitor BS levels with insulin administration
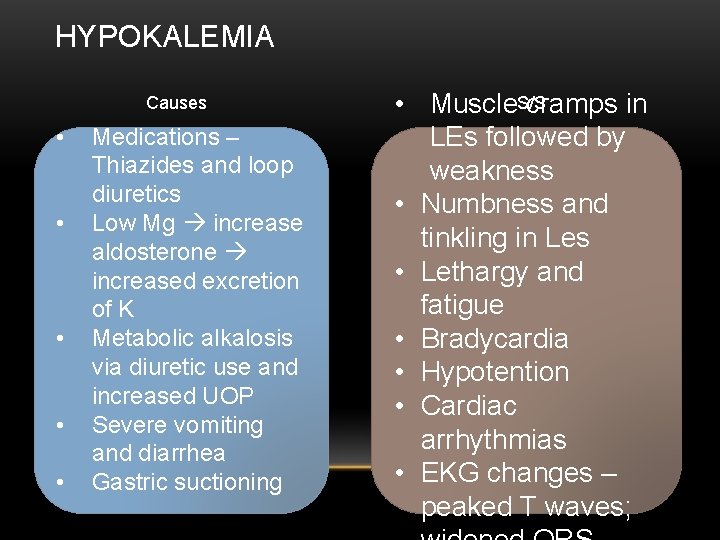
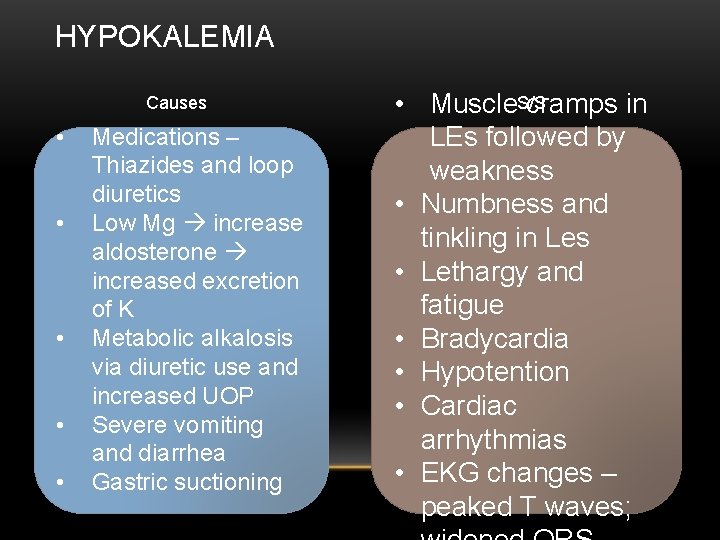
HYPOKALEMIA Causes • • • Medications – Thiazides and loop diuretics Low Mg increase aldosterone increased excretion of K Metabolic alkalosis via diuretic use and increased UOP Severe vomiting and diarrhea Gastric suctioning • Muscle. S/S cramps in LEs followed by weakness • Numbness and tinkling in Les • Lethargy and fatigue • Bradycardia • Hypotention • Cardiac arrhythmias • EKG changes – peaked T waves;
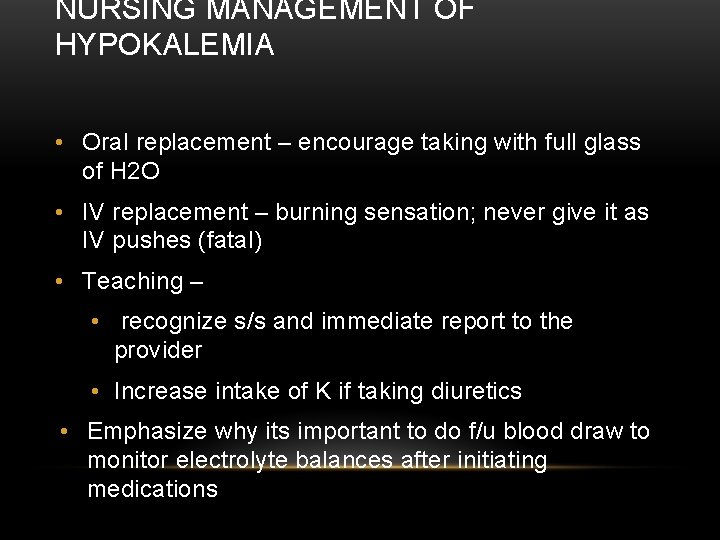
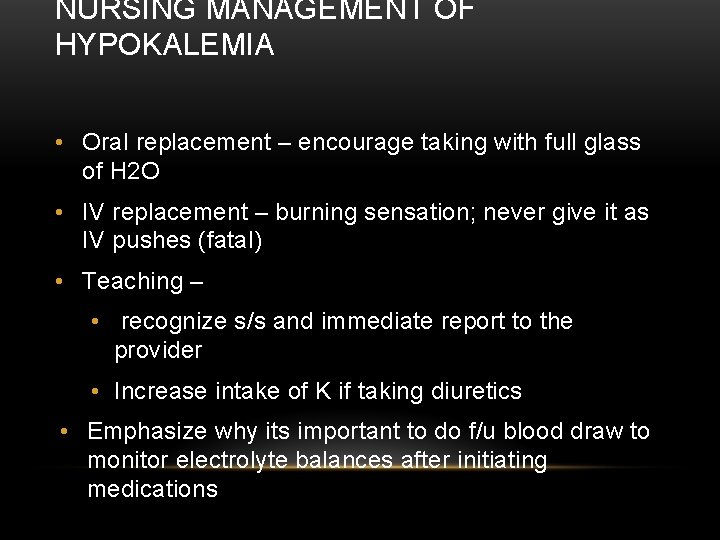
NURSING MANAGEMENT OF HYPOKALEMIA • Oral replacement – encourage taking with full glass of H 2 O • IV replacement – burning sensation; never give it as IV pushes (fatal) • Teaching – • recognize s/s and immediate report to the provider • Increase intake of K if taking diuretics • Emphasize why its important to do f/u blood draw to monitor electrolyte balances after initiating medications
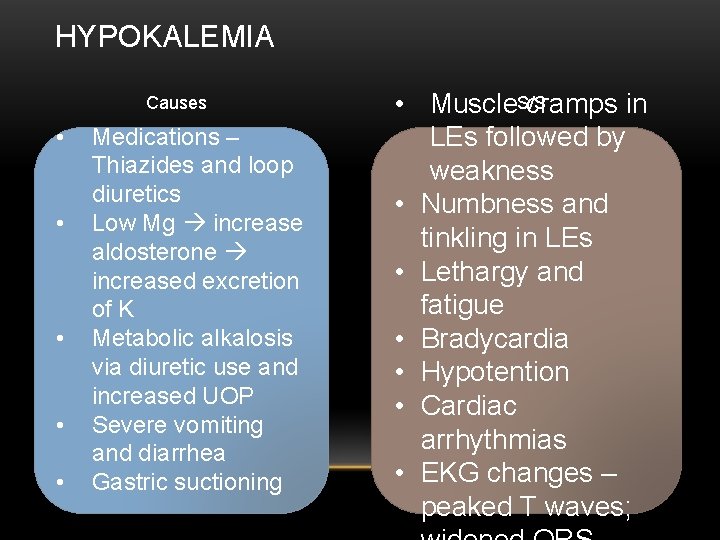
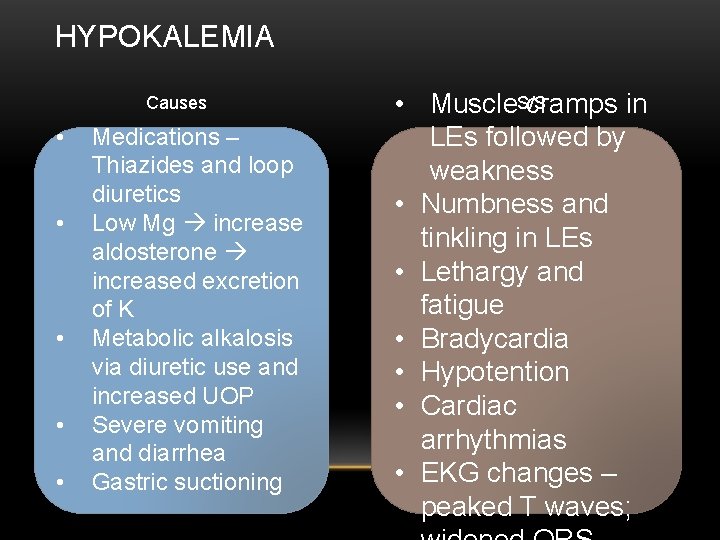
HYPOKALEMIA Causes • • • Medications – Thiazides and loop diuretics Low Mg increase aldosterone increased excretion of K Metabolic alkalosis via diuretic use and increased UOP Severe vomiting and diarrhea Gastric suctioning • Muscle. S/S cramps in LEs followed by weakness • Numbness and tinkling in LEs • Lethargy and fatigue • Bradycardia • Hypotention • Cardiac arrhythmias • EKG changes – peaked T waves;
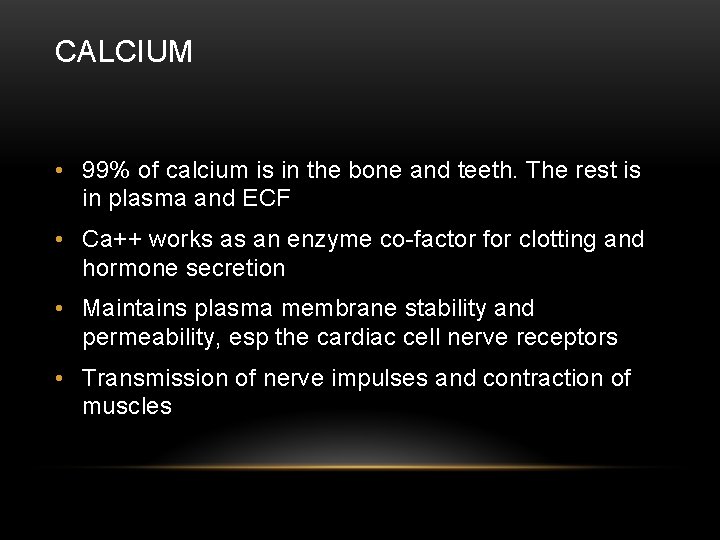
CALCIUM • 99% of calcium is in the bone and teeth. The rest is in plasma and ECF • Ca++ works as an enzyme co-factor for clotting and hormone secretion • Maintains plasma membrane stability and permeability, esp the cardiac cell nerve receptors • Transmission of nerve impulses and contraction of muscles
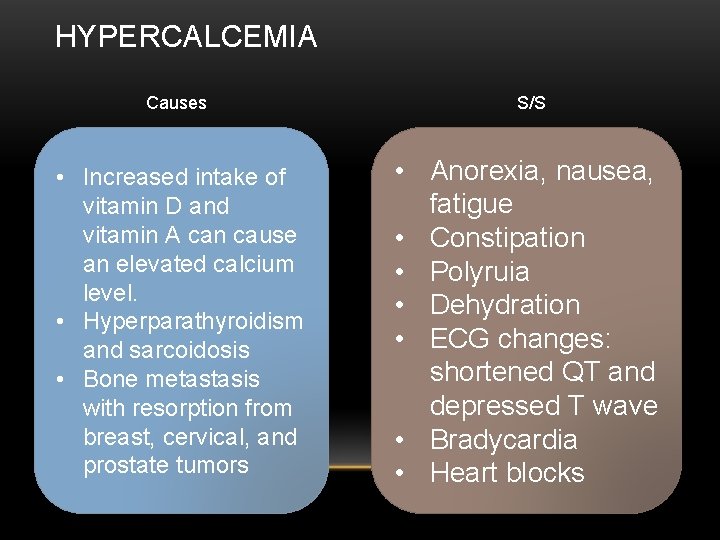
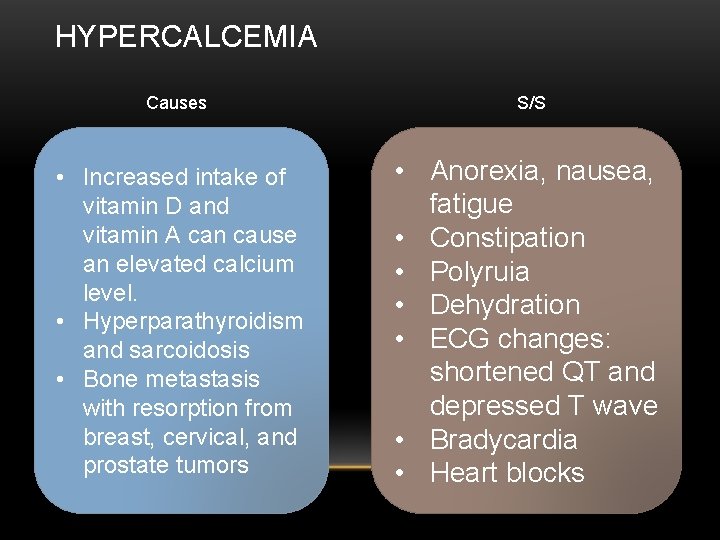
HYPERCALCEMIA Causes S/S • Increased intake of vitamin D and vitamin A can cause an elevated calcium level. • Hyperparathyroidism and sarcoidosis • Bone metastasis with resorption from breast, cervical, and prostate tumors • Anorexia, nausea, fatigue • Constipation • Polyruia • Dehydration • ECG changes: shortened QT and depressed T wave • Bradycardia • Heart blocks

NURSING MANAGEMENT OF HYPERCALCEMIA • Encourage oral intake of fluids to 3 -4 L/day • Risk for injury (following institute safety precautions) • Be aware of altered gait and weakness • Assess neurologic status/LOC often ( per protocol) • Monitor for arrhythmias • Teach to limit intake of foods high in calcium • Avoid vitamin preparations that contain vitamin D

HYPOCALCEMIA Causes • Vitamin D deficiency • Inadequate of Ca++ intake • Increased intake of phosphorus (antacids) • Administration of a large amount of stored blood products • Removal of parathyroid glad • Excessive loss of calcium with the used of diuretics S/S • Tetany • Positive Chvostek’s Sign • Hyperreflexia • Laryngnospasm • Arrhythmia (V Fib, prolonged QT) • Decrease cardiac contraction and decreased BP • Hypomagnesemia
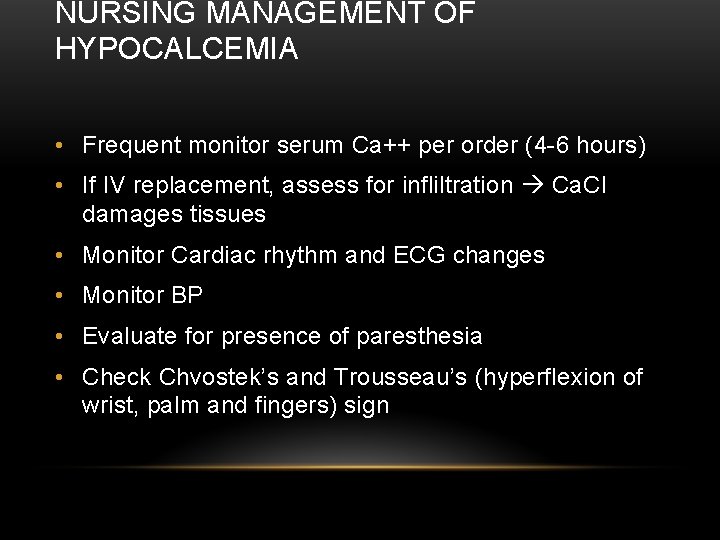
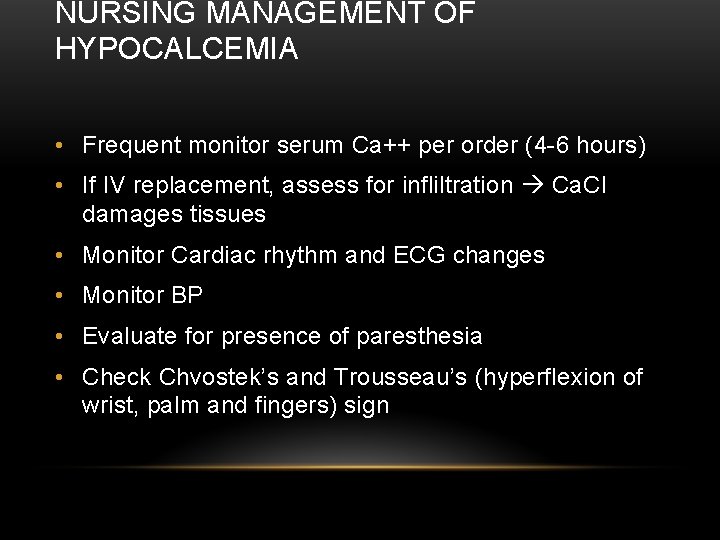
NURSING MANAGEMENT OF HYPOCALCEMIA • Frequent monitor serum Ca++ per order (4 -6 hours) • If IV replacement, assess for infliltration Ca. Cl damages tissues • Monitor Cardiac rhythm and ECG changes • Monitor BP • Evaluate for presence of paresthesia • Check Chvostek’s and Trousseau’s (hyperflexion of wrist, palm and fingers) sign
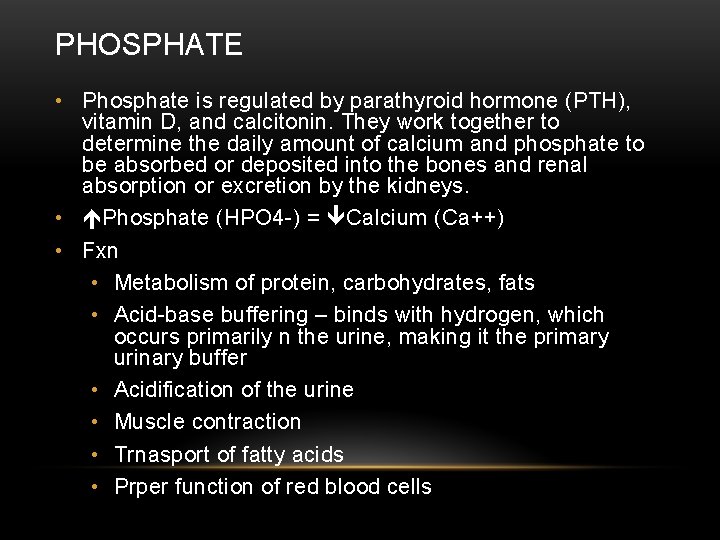
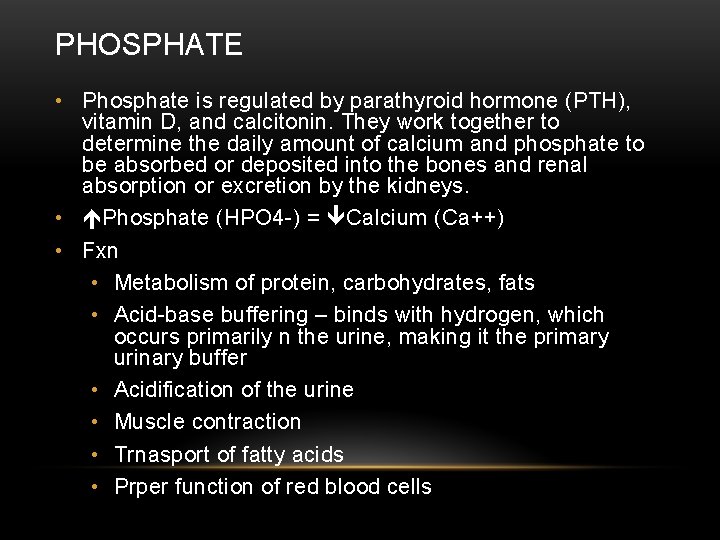
PHOSPHATE • Phosphate is regulated by parathyroid hormone (PTH), vitamin D, and calcitonin. They work together to determine the daily amount of calcium and phosphate to be absorbed or deposited into the bones and renal absorption or excretion by the kidneys. • Phosphate (HPO 4 -) = Calcium (Ca++) • Fxn • Metabolism of protein, carbohydrates, fats • Acid-base buffering – binds with hydrogen, which occurs primarily n the urine, making it the primary urinary buffer • Acidification of the urine • Muscle contraction • Trnasport of fatty acids • Prper function of red blood cells
HYPERPHOSPHATEMIA & HYPHOSPHATEMIA • Reciprocal relationship to calcium • Refer to information of Ca++
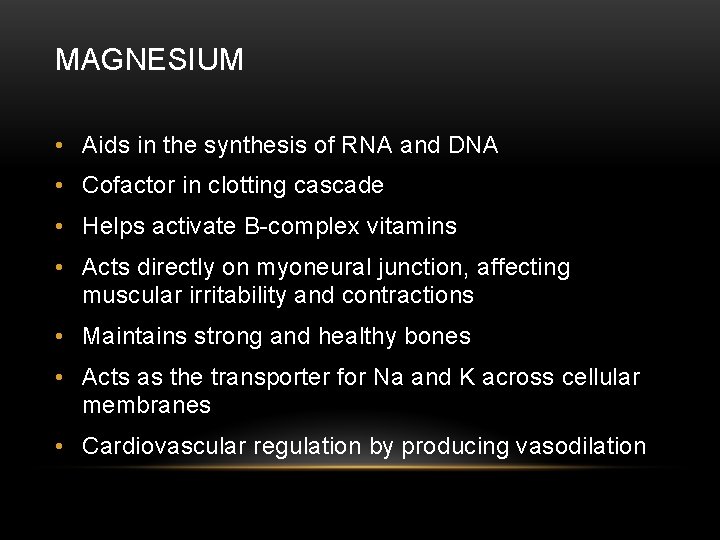
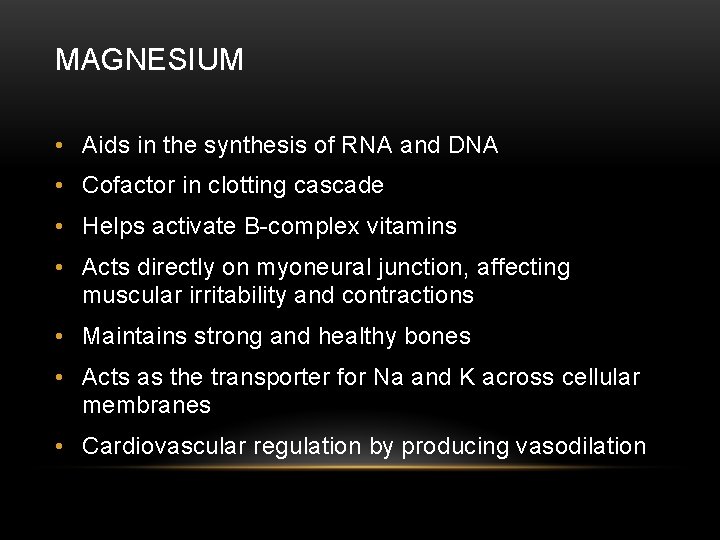
MAGNESIUM • Aids in the synthesis of RNA and DNA • Cofactor in clotting cascade • Helps activate B-complex vitamins • Acts directly on myoneural junction, affecting muscular irritability and contractions • Maintains strong and healthy bones • Acts as the transporter for Na and K across cellular membranes • Cardiovascular regulation by producing vasodilation
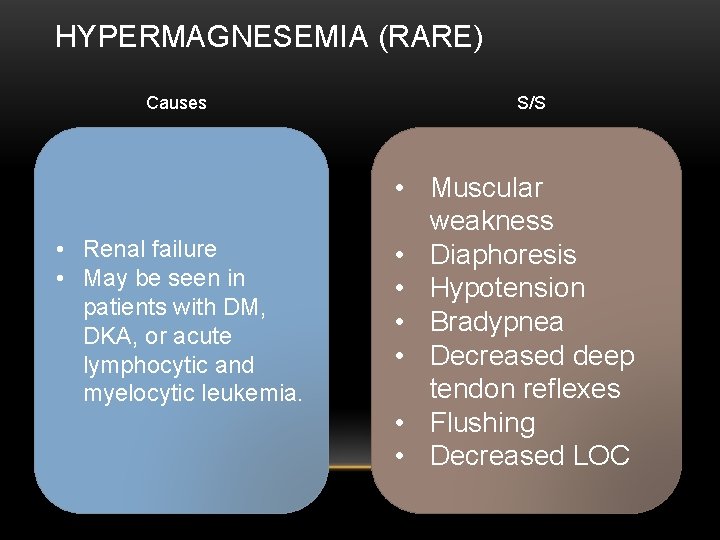
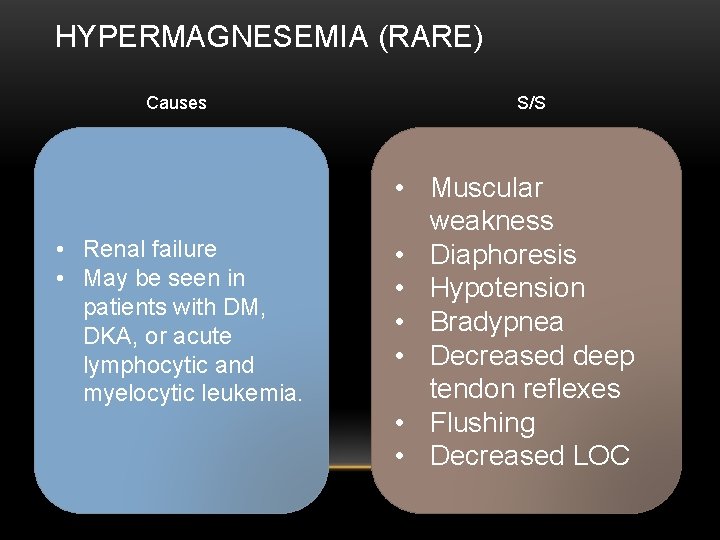
HYPERMAGNESEMIA (RARE) Causes • Renal failure • May be seen in patients with DM, DKA, or acute lymphocytic and myelocytic leukemia. S/S • Muscular weakness • Diaphoresis • Hypotension • Bradypnea • Decreased deep tendon reflexes • Flushing • Decreased LOC
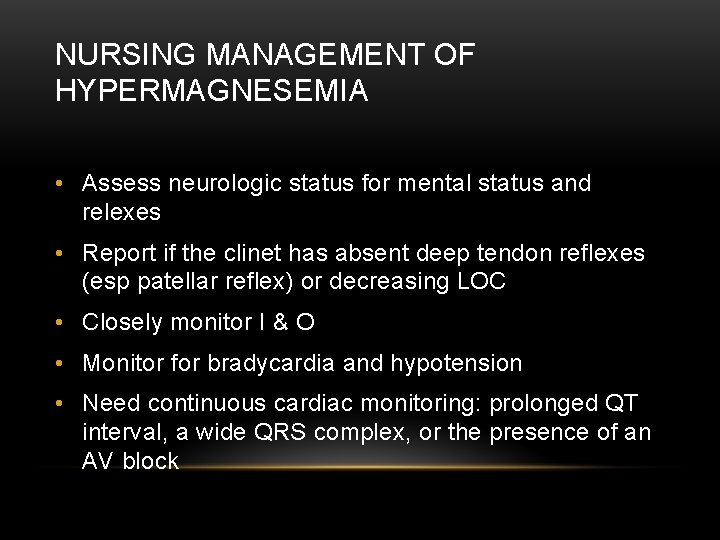
NURSING MANAGEMENT OF HYPERMAGNESEMIA • Assess neurologic status for mental status and relexes • Report if the clinet has absent deep tendon reflexes (esp patellar reflex) or decreasing LOC • Closely monitor I & O • Monitor for bradycardia and hypotension • Need continuous cardiac monitoring: prolonged QT interval, a wide QRS complex, or the presence of an AV block
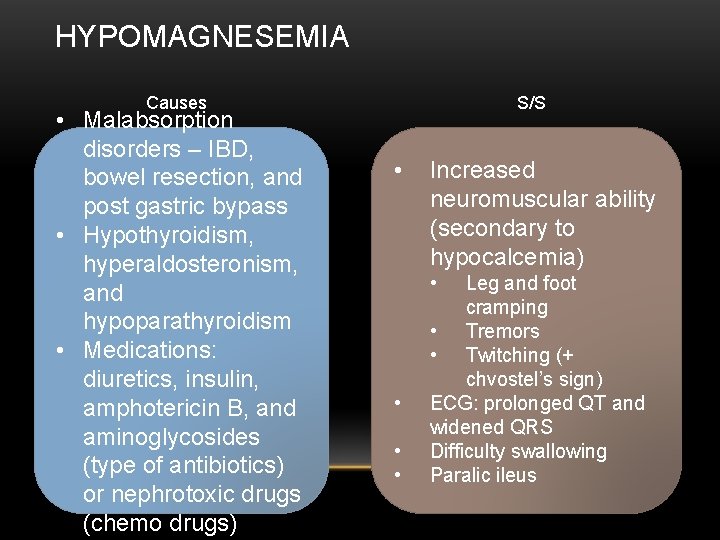
HYPOMAGNESEMIA Causes • Malabsorption disorders – IBD, bowel resection, and post gastric bypass • Hypothyroidism, hyperaldosteronism, and hypoparathyroidism • Medications: diuretics, insulin, amphotericin B, and aminoglycosides (type of antibiotics) or nephrotoxic drugs (chemo drugs) S/S • Increased neuromuscular ability (secondary to hypocalcemia) • • Leg and foot cramping • Tremors • Twitching (+ chvostel’s sign) ECG: prolonged QT and widened QRS Difficulty swallowing Paralic ileus
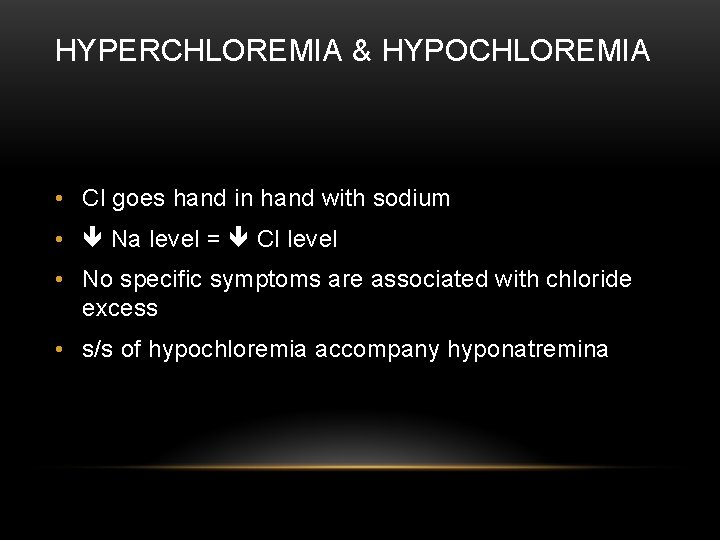
HYPERCHLOREMIA & HYPOCHLOREMIA • Cl goes hand in hand with sodium • Na level = Cl level • No specific symptoms are associated with chloride excess • s/s of hypochloremia accompany hyponatremina

TAKE HOME CASE STUDY
 Chapter 18 fluids and electrolytes
Chapter 18 fluids and electrolytes Tropolar
Tropolar Normal values of potassium
Normal values of potassium Major intra and extracellular electrolytes
Major intra and extracellular electrolytes How does electrolytes affect the chemical equilibria
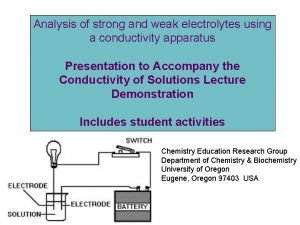
How does electrolytes affect the chemical equilibria Strong vs weak electrolytes
Strong vs weak electrolytes Effect of electrolytes on colloidal dispersion
Effect of electrolytes on colloidal dispersion Strong vs weak electrolytes
Strong vs weak electrolytes Weak electrolyte examples
Weak electrolyte examples Electrolytes and nonelectrolytes
Electrolytes and nonelectrolytes Vacid definition
Vacid definition Congenital adrenal hyperplasia electrolytes
Congenital adrenal hyperplasia electrolytes What is colloidal state
What is colloidal state Strong vs weak electrolytes
Strong vs weak electrolytes рефидинг синдром
рефидинг синдром 24 hydrate
24 hydrate Weak electrolytes
Weak electrolytes Rome mnemonic for acid base balance
Rome mnemonic for acid base balance Vapor pressure lowering
Vapor pressure lowering Hhs symptoms
Hhs symptoms Medicare enteral qualification checklist
Medicare enteral qualification checklist Rule 411
Rule 411 411 database
411 database Opwekking 411 tekst
Opwekking 411 tekst Comp 411
Comp 411 Csce 411
Csce 411 Unc comp 411
Unc comp 411 Uic cs 411
Uic cs 411 Ist 411
Ist 411 Cpsc 411
Cpsc 411 Mgt 411
Mgt 411 Csce 411
Csce 411