EPIDEMIOLOGY OF NOSOCOMIAL INFECTIONS NCIs PART1 Dr A










- Slides: 42
EPIDEMIOLOGY OF NOSOCOMIAL INFECTIONS (NCIs) PART-1 Dr. A. K. AVASARALA MBBS, M. D. PROFESSOR & HEAD DEPT OF COMMUNITY MEDICINE & EPIDEMIOLOGY PRATHIMA INSTITUTE OF MEDICAL SCIENCES, KARIMNAGAR, A. P. . INDIA: +91505417 avasarala@yahoo. com
DEFINITION • Nosocomial infection is an infection that is not present or incubating when a patient is admitted to a hospital
LEARNING OBJECTIVES LEARNER SHOULD LEARN 1. PUBLIC HEALTH IMPACT OF HOSPITAL ACQUIRED INFECTIONS. 2. EPIDEMIOLOGY, PREVENTION, SURVEILLANCE AND CONTROL STRATEGIES 3. INDIAN SITUATION OF THE PROBLEM
PERFORMANCE OBJECTIVES LEARNER SHOULD BE ABLE TO 1. Estimate the extent and nature of nosocomial infections in his hospital 2. Identify the changes in the incidence of nosocomial infections and the pathogens that cause them. 3. Provide his hospital with comparative data on nosocomial infection rates. 4. Develop efficient and effective data collection, management and analysis methods for his hospital. 5. Conduct collaborative research studies on nosocomial infections in his hospital.
TYPES BY ORIGIN 1. Endogenous: Caused by the organisms that are present as part of normal flora of the patient 2. Exogenous: caused by organisms acquiring by exposure to hospital personnel, medical devices or hospital environment

TYPES OF NCI BY SITE • Urinary tract infections (UTI) • Surgical wound infections (SWI) • Lower respiratory infections (LRI) • Blood stream infections (BSI)
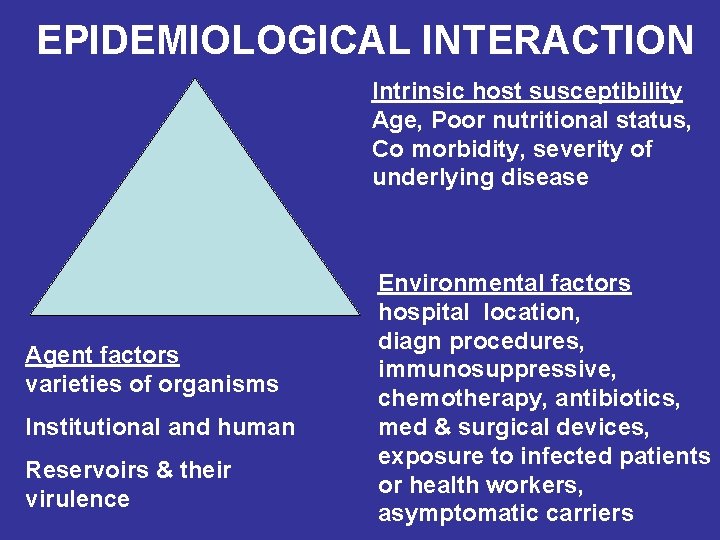
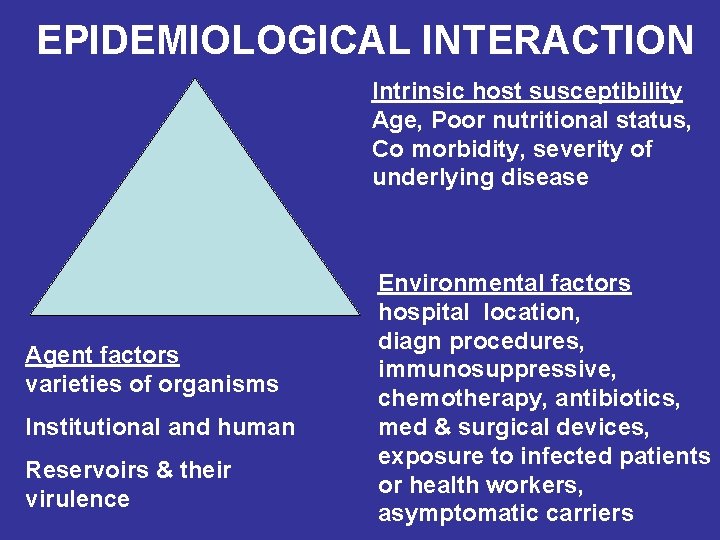
EPIDEMIOLOGICAL INTERACTION Intrinsic host susceptibility Age, Poor nutritional status, Co morbidity, severity of underlying disease Agent factors varieties of organisms Institutional and human Reservoirs & their virulence Environmental factors hospital location, diagn procedures, immunosuppressive, chemotherapy, antibiotics, med & surgical devices, exposure to infected patients or health workers, asymptomatic carriers
DISEASE BURDEN • 5 -10% in developed countries • 10 -30% IN DEVELOPING COUNTRIES • Rates vary between countries, within the country, within the districts and sometimes even within the hospital itself, due to 1) complex mix of the patients 2) aggressive treatment 3) local practices

INDIAN SCENARIO

HOSPITAL INFECTION SOCIETY (HIS), INDIA • Ten to 30 per cent of patients admitted to hospitals and nursing homes in India, acquire nosocomial infection as against an impressive five per cent in the West, according to member of HIS, Rita Dutta – Mumbai.
HINDUJA, HOSPITAL Dr F D Dastur, Director, Medical education, P D Hinduja, Hospital: “nosocomial control programme is at a nascent stage in Indian hospitals, with some yet to establish a central sterilization and supply department (CSSD) and appoint an infection control nurse”
ASIAN HEART INSTITUTE (AHI) Dr Vijay D Silva, director, critical care, Asian Heart Institute (AHI): “Suggestions to strengthen the infection control programme is turned down by the management of most hospitals as spending on infection control does not generate revenue. ”
INCIDENCE • Average Incidence - 5% to 10%, but maybe up to 28% in ICU • Urinary Tract Infection - usually catheter related -28% • Surgical Site Infection or wound infection -19% • Pneumonia -17% • Blood Stream infection - 7% to 16%
INCIDENCE • Depends upon • Average level of patient risk depends upon intrinsic host factors and extrinsic environment factors • Sensitivity &specificity of surveillance programmes

AGE RANKS OF NCIs Ranks in infants Ranks in children Ranks in adults 1) SKIN 2) LRI 3) BSI 4) UTI 5) SWI 1) UTI 2) LRI 3) SWI 4) BSI
PEDIATRIC INFECTIONS • Epidemiology is Unique • Rates of infection by site and pathogen differ from those reported in adults • Pathogen distribution is also different – S. aureus in children and E. Coli in adults • Pediatric viral URI&LRI far exceeds that caused by bacterial ones.
CONSEQUENCES OF NOSOCOMIAL INFECTIONS 1. Prolongation of hospital stay: Varies by site, greatest with pneumonias and wound infections 2. Additional morbidity 3. Mortality increases - in order - LRI, BSI, UTI 4. Long-term physical &neurological consequences 5. Direct patient costs increased. Escalation of the cost of care
ECONOMICS OF NCIS • Extra cost of NCI consequences • Bed, • Intensive care unit stay, • Hematological, biochemical, microbiological and radiological tests, • Antibiotics & other drugs, • Extra surgical procedures • Working hours
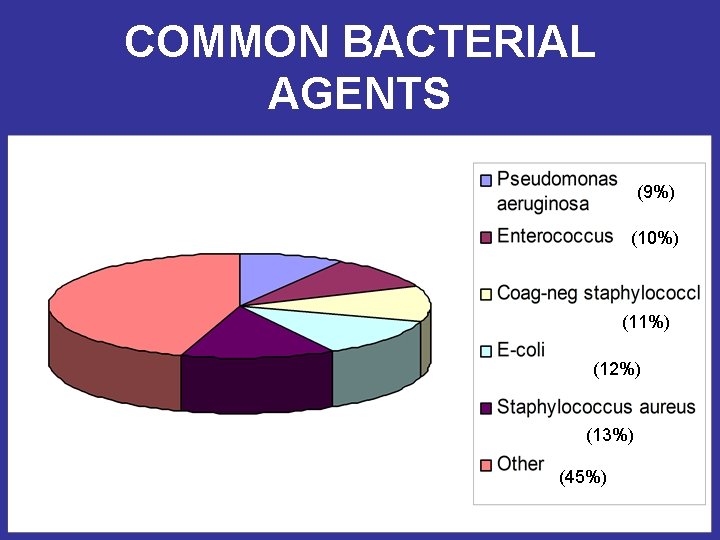
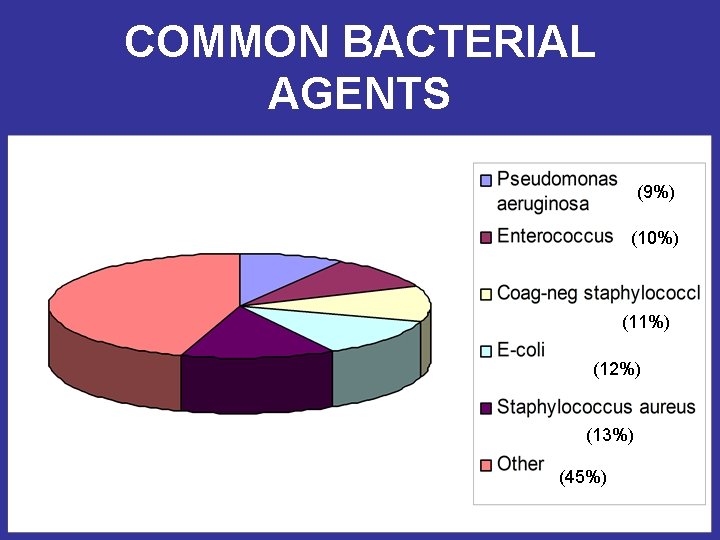
COMMON BACTERIAL AGENTS (9%) (10%) (11%) (12%) (13%) (45%)
KASTURBA MEDICAL COLLEGE, MANGALORE • Drug resistance was more common with • • • MRSA nosocomial strains. All MRSA strains were resistant to penicillin and sensitive (73. 8 percent), ciprofloxacin (78. 6 percent) gentamicin (84. 7 percent) and trimethoprim-sulphamethoxazole (95. 7 percent). Bhat KG; Bhat MV Department of Microbiology, Kasturba Medical College, Light House Hill Road, Mangalore 575001, India Prevalence of nosocomial infections due to methicillin resistant staphylococcus aureus in Mangalore, India Biomedicine. 1997; 17(1): 17 -20

CHRISTIAN MEDICAL COLLEGE, VELLORE • Says Dr J Kang, professor of microbiology at CMC: “ While MRSA is the troublemaker in most cases, at Vellore nosocomial infection due to MRSA is only five per cent because of genotyping. ”
FUNGI • Due to increased antibiotic use &host susceptibility • Candida species– most common, causing BSI (38% mortality) • Changing bacterial & fungal spectrum in the hospital reflects the increased use, particularly of the newer antibiotics • Development of resistance (MRSA, VRE, MDRTB) • Overcrowding & understaffing of nursing units increased the rates of infections (MRSA colonization)
VIRUSES • • • CMV, HERPES SIMPLEX V-Z VIRUSES HEPATITIS VIRUSES- A, B , C HIV INFLUENZA, PARA INFLUENZA, R. S. VIRUS, ROTAVIRUS
EPIDEMIOLOGY OF VIRAL INFECTIONS • Mostly affects Resp & Gastrointestinal tracts (90%) whereas bacterial infections attack these systems to about 15% only. • Pediatric viral URI & LRI far exceeds that caused by bacterial ones.
PLACE DISTRIBUTION ICU RISK • • PROLONGED ICU STAY MECHANICAL VENTILATION TRAUMA URINARY CATHETER, VASCULAR CATHETER • STRESS ULCER PROPHYLAXIS
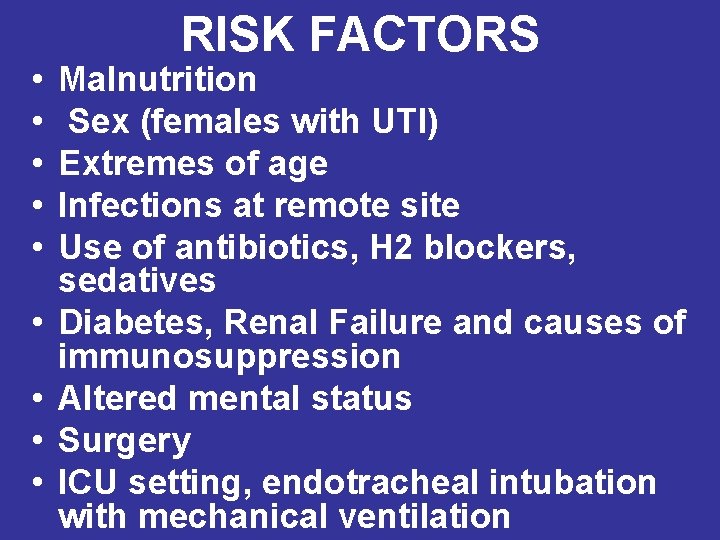
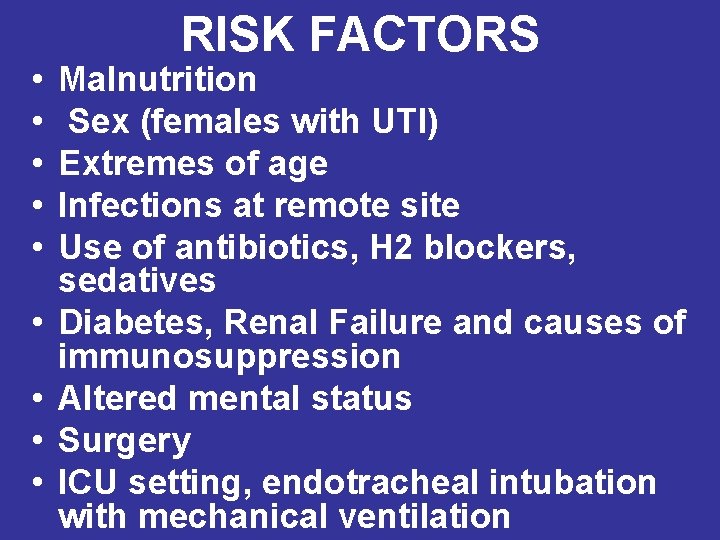
• • • RISK FACTORS Malnutrition Sex (females with UTI) Extremes of age Infections at remote site Use of antibiotics, H 2 blockers, sedatives Diabetes, Renal Failure and causes of immunosuppression Altered mental status Surgery ICU setting, endotracheal intubation with mechanical ventilation

MODES OF TRANSMISSION • BY CONTACT • 1) Direct - between Patients and between patient care personnel 2) Indirect - contaminated inanimate objects in environment (Endoscopes etc) 3) Droplet infections by large aerosols THRO COMMON VEHICE like Food, Blood & blood products, Diagnostic reagents, Medications AIRBORNE e. g. legionellosis, aspergillosis VECTORBORNE – by flies • • •
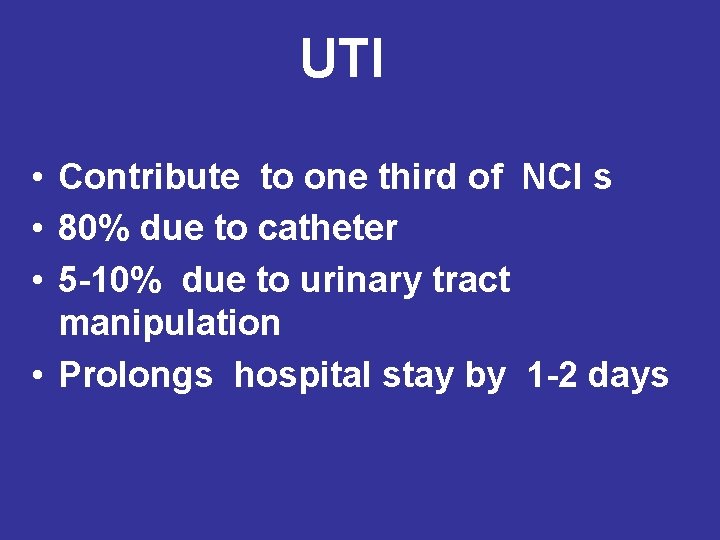
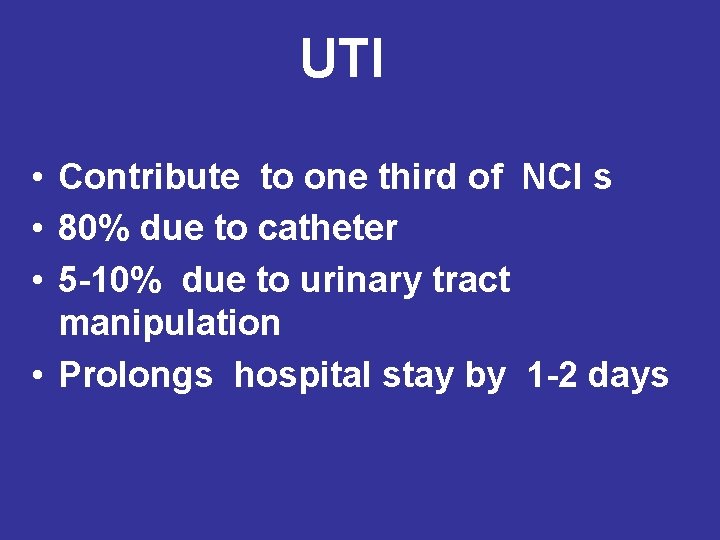
UTI • Contribute to one third of NCI s • 80% due to catheter • 5 -10% due to urinary tract manipulation • Prolongs hospital stay by 1 -2 days
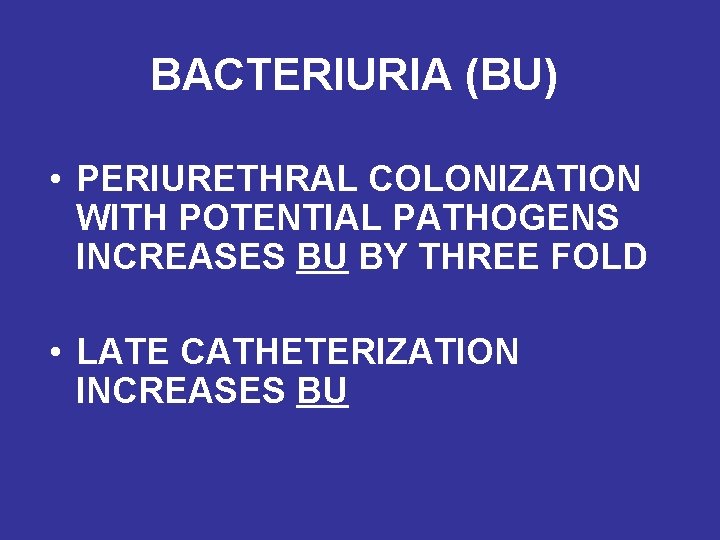
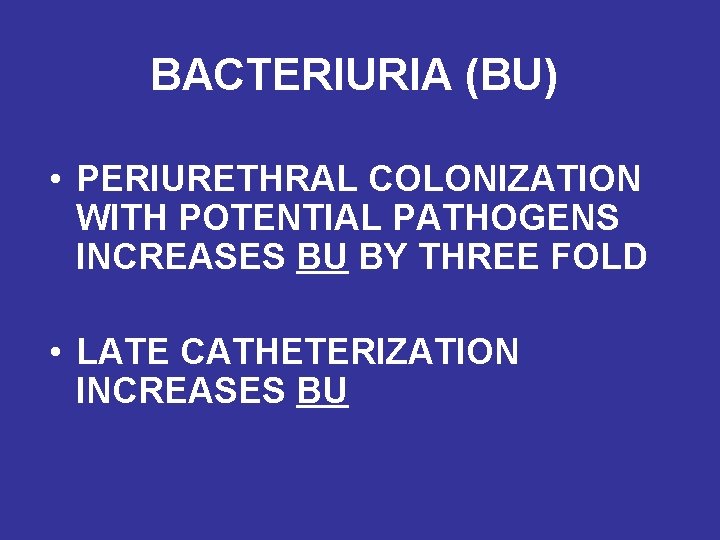
BACTERIURIA (BU) • PERIURETHRAL COLONIZATION WITH POTENTIAL PATHOGENS INCREASES BU BY THREE FOLD • LATE CATHETERIZATION INCREASES BU
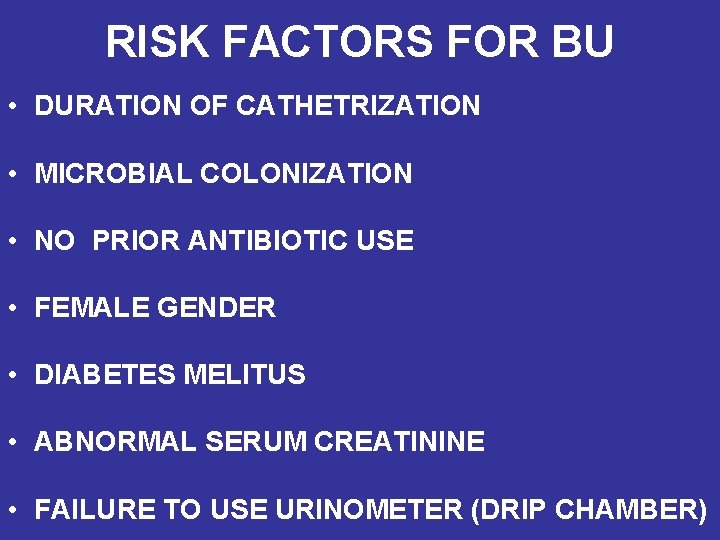
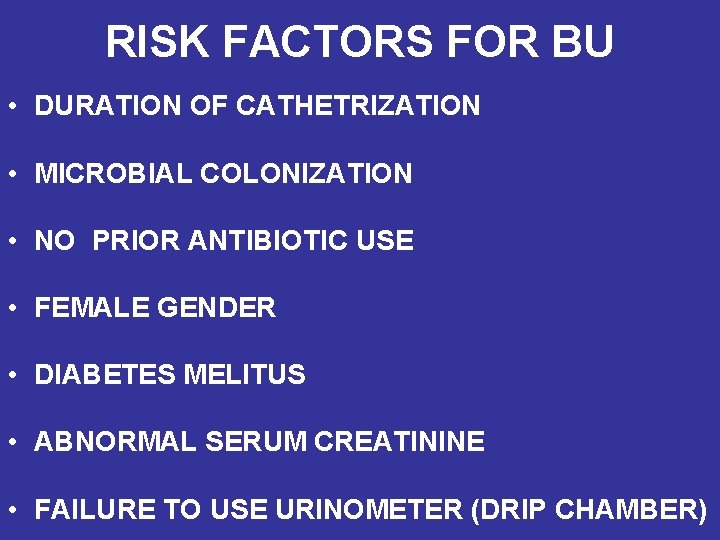
RISK FACTORS FOR BU • DURATION OF CATHETRIZATION • MICROBIAL COLONIZATION • NO PRIOR ANTIBIOTIC USE • FEMALE GENDER • DIABETES MELITUS • ABNORMAL SERUM CREATININE • FAILURE TO USE URINOMETER (DRIP CHAMBER)
CATHETER & UTI • Presence of catheter leads to increased incidence of Bacteriuria • Short term catheter use (urinary outpu measurement, surgery ) increase BU by 15% Long term catheter use (retention, obstruction, incontinence) increases BU by 90%

CATHETER USE COMPLICATIONS • MORE SEEN IN MEN (BACTEREMIA DUE TO UTI 15%) • SHORT TERM USE - EVERS, SYMPTOMATIC UTI, BACTEREMIA • LONG TERM CATHETER USE - ABOVE + CATHETER OBSTRUCTION, URINARY STONES, PERIURINARY INFECTIONS, RENAL FAILURE, BLADDER CANCER
SURGICAL WOUND INFECTIONS (SWI) Incidence varies from 1. 5 to 13 per 100 operations. • It can be classified as • Superficial incisional SWI • Deep incisional SWI and • Organ/Space SWI.

EPIDEMIOLOGY OF SWI • HOST FACTORS OLD AGE • OBESITY • CURRENT INFECTION AT ANOTHER SITE • PROLONGED POST OPERATIVE HOSPITALIZATION •
SOURCES OF INFECTION • • • DIRECT INOCULATION FROM PATIENT’S FLORA CONTAMINATED HOST TISSUES HANDS OF SURGEONS AIRBORNE TRANSMISSION POST- OPERATIVE DRAINS/CATHETERS
LOWER RESPIRATORY INFECTIONS (LRI) MOSTLY SEEN IN ICU RISK FACTORS • • • TRACHEOSTOMY, ENDOTRACHEAL INTUBATION, VENTILATOR, CONTAMINATED AEROSOLS, BAD EQIPPMENT, CONDENSATE IN VENTILATOR TUBING, ANTIBIOTICS, SURGERY, OLD AGE , COPD, IMMUNO SUPPRESSION

LOGISTIC REGRESSION OF CONTRIBUTING FACTORS • TIME FROM ADMISSION TO PNEUMONIA +++++++ • PROLONGED HOSPITAL STAY +++++ • NASOGASTRIC INTUBATION +++ • AGE ++ • PRIOR USE OF MECHANICAL VENTILATORS++ • POST TRACHEOSTOMY STATUS++ • IMMUNOSSUPPRESSION OR LEUKOPENIA++ • NEOPLASTIC DISEASE +
COHORT STUDY • ON PNEUMONIA PATIENTS WITH VENTILATORS • ATTRIBUTABLE RISK 27% • DEATH RISK 2% • LRI IS DIRECTLY RELATED TO THE LENGTH OF STAY
RISK FACTORS FOR DIARRHEAS • • • BY CLOSTRIDIUM DIFFICILE OLD AGE SEVERE UNDERLYING DISEASE HOSPITALISATION FOR >1 WEEK LONG STAY IN ICU PRIOR ANTIBIOTICS
BLOOD STREAM INFECTIONS (BSI) • PRIMARY = ISOLATION OF BACTERIAL BLOOD PATHOGEN IN THE ABSENCE OF INFECTION AT ANOTHER SITE • SECONDARY = WHEN BACTERIA ARE ISOLATED FROM THE BLOOD DURING AN INFECTION WITH THE SAME ORGANISM AT ANOTHER SITE i. e. UTI, SWI OR LRI
BACTEREMIA (BSI) BSI ARE INCREASING PRIMARILY DUE TO INCREASE IN INFECTIONS WITH GM+VE BACTERIA & FUNGI MOST COMMON IN NEONATES IN HIGH RISK NURSERIES MORTALITY RATE FOR NOSOCOMIAL BACTEREMIA IS HIGHER THAN FOR COMMUNITY ACQUIRED BACTEREMIA

SOURCES OF BSI • IV CATHETERS, INTRINSIC IV FLUID CONTAMINATION • MULTIDOSE PARENTERAL MEDICATION VIALS • VASCULAR CATHETER RELATED INFECTIONS, CONTAMINATED ANTISEPTICS, CONTAMINATED HANDS OF HEALTH CARE WORKERS • AUTOINFECTION FOLLOWING HEMATOGENOUS SEEDLING - RISK INCREASES WITH LONGER DURATION >72 HOURS
 Salmonella life cycle
Salmonella life cycle Beth has a nosocomial infection. how did she get it?
Beth has a nosocomial infection. how did she get it? Vitamins part1
Vitamins part1 Ncis
Ncis Ncis
Ncis Ncis
Ncis Ncis
Ncis Ncis
Ncis Opportunistic infections
Opportunistic infections Acute gingival infections
Acute gingival infections Understanding the mirai botnet
Understanding the mirai botnet Bone and joint infections
Bone and joint infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Methotrexate yeast infection
Methotrexate yeast infection Cryptosporidiose
Cryptosporidiose Storch infections
Storch infections Genital infections
Genital infections Opportunistic infections
Opportunistic infections Bacterial vaginosis
Bacterial vaginosis Storch infections
Storch infections Genital infections
Genital infections Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Postpartum infections
Postpartum infections Distribution in epidemiology
Distribution in epidemiology Defination of epidemiology
Defination of epidemiology How to calculate incidence rate example
How to calculate incidence rate example Difference between descriptive and analytical epidemiology
Difference between descriptive and analytical epidemiology Celiac beri beri
Celiac beri beri Define epidemiology
Define epidemiology Gordon epidemiology
Gordon epidemiology Field epidemiology ppt
Field epidemiology ppt Rambo critical appraisal tool
Rambo critical appraisal tool How to calculate prevalence
How to calculate prevalence Epidemiology definition
Epidemiology definition Epidemiology of malaria
Epidemiology of malaria Effect modification epidemiology
Effect modification epidemiology Concept of epidemiology
Concept of epidemiology Bibliography of epidemiology
Bibliography of epidemiology Perbedaan or dan rr
Perbedaan or dan rr Epidemiology made easy
Epidemiology made easy Prevalensi adalah
Prevalensi adalah Epidemiology kept simple
Epidemiology kept simple Bhisma murti
Bhisma murti