Diseases of the respiratory tract Dr Gyrgy Fekete


















- Slides: 41
Diseases of the respiratory tract Dr. György Fekete www. gyer 2. sote. hu
Pediatric pulmonary diseases Ø 50% of deaths under age of 1 yr Ø 20% of all hospitalisations under age of 15 yrs Ø 7% of children: chronic disorder of the lower respiratory system
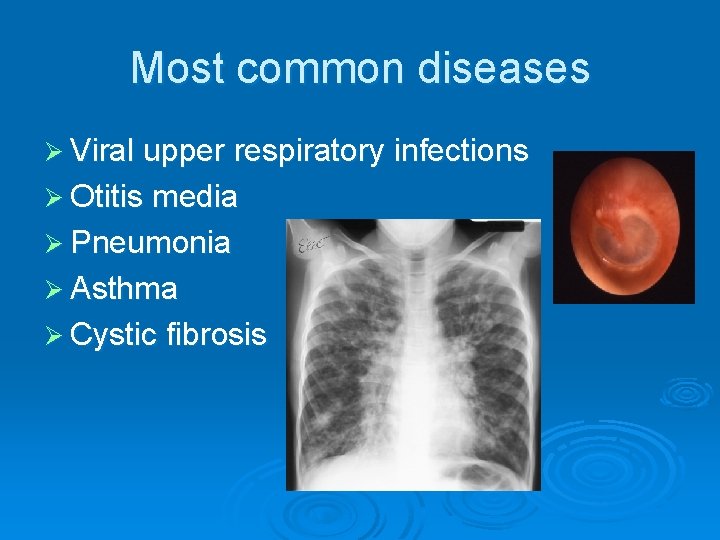
Most common diseases Ø Viral upper respiratory infections Ø Otitis media Ø Pneumonia Ø Asthma Ø Cystic fibrosis
Symptoms Ø Dyspnea, tachypnea, hyperpnea Ø Cough Ø Chest pain Ø Rales(crackles), rhonchi Ø Wheezing Ø Retractions Ø Fever
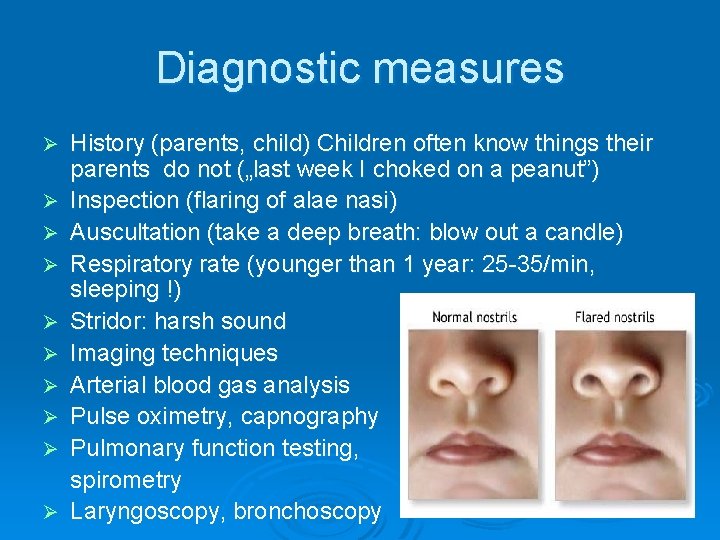
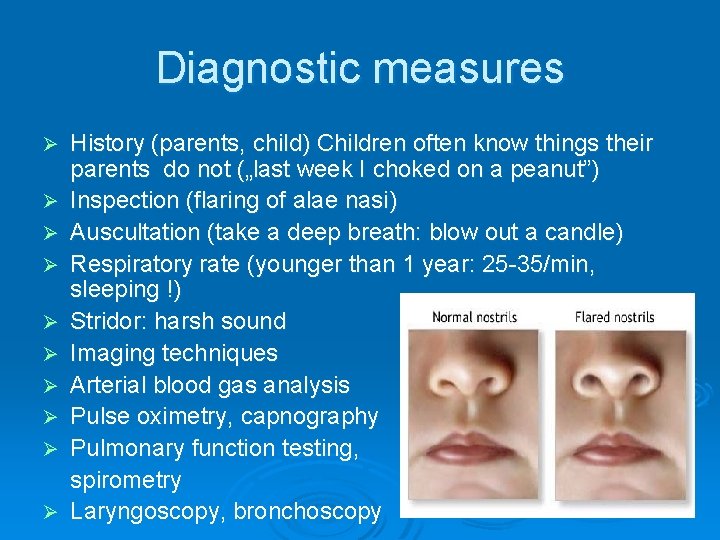
Diagnostic measures Ø Ø Ø Ø Ø History (parents, child) Children often know things their parents do not („last week I choked on a peanut”) Inspection (flaring of alae nasi) Auscultation (take a deep breath: blow out a candle) Respiratory rate (younger than 1 year: 25 -35/min, sleeping !) Stridor: harsh sound Imaging techniques Arterial blood gas analysis Pulse oximetry, capnography Pulmonary function testing, spirometry Laryngoscopy, bronchoscopy
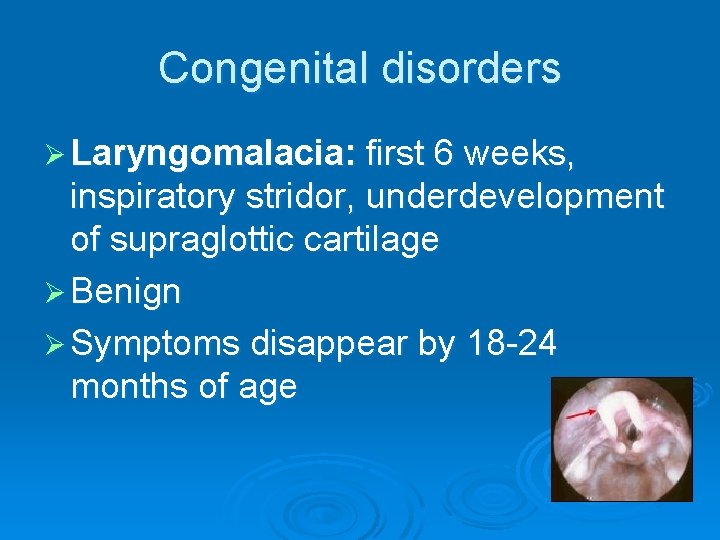
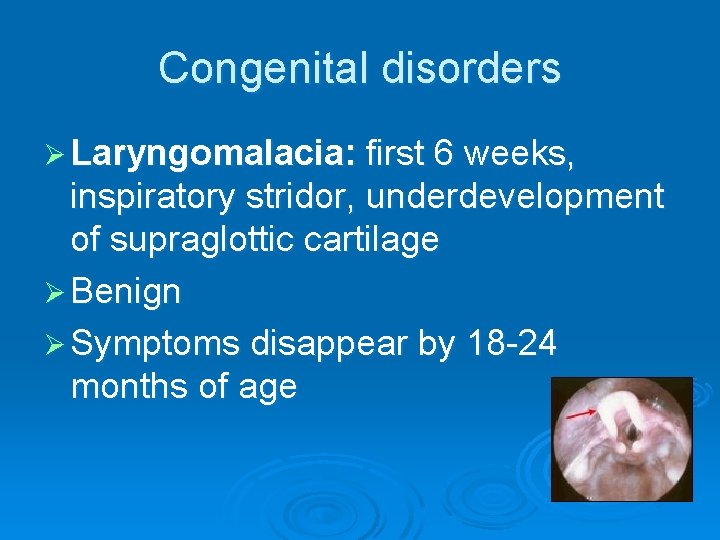
Congenital disorders Ø Laryngomalacia: first 6 weeks, inspiratory stridor, underdevelopment of supraglottic cartilage Ø Benign Ø Symptoms disappear by 18 -24 months of age
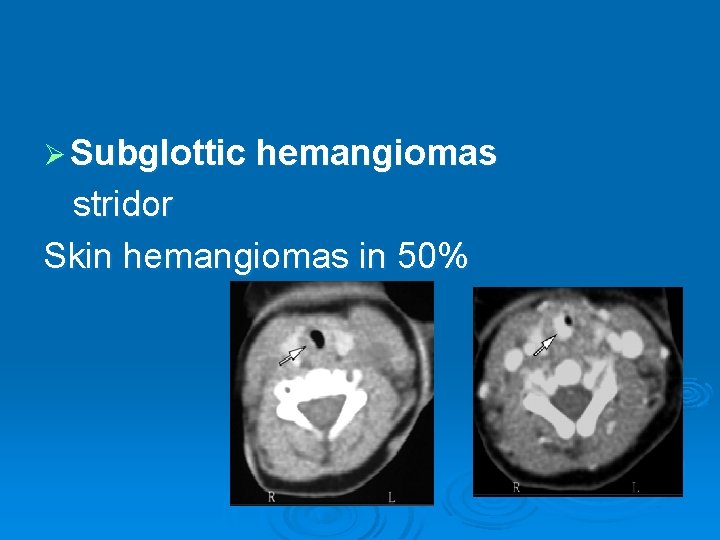
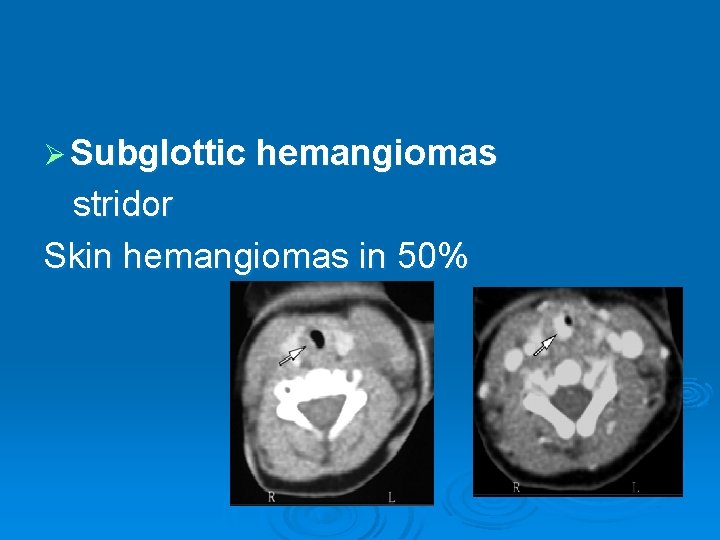
Ø Subglottic hemangiomas stridor Skin hemangiomas in 50%
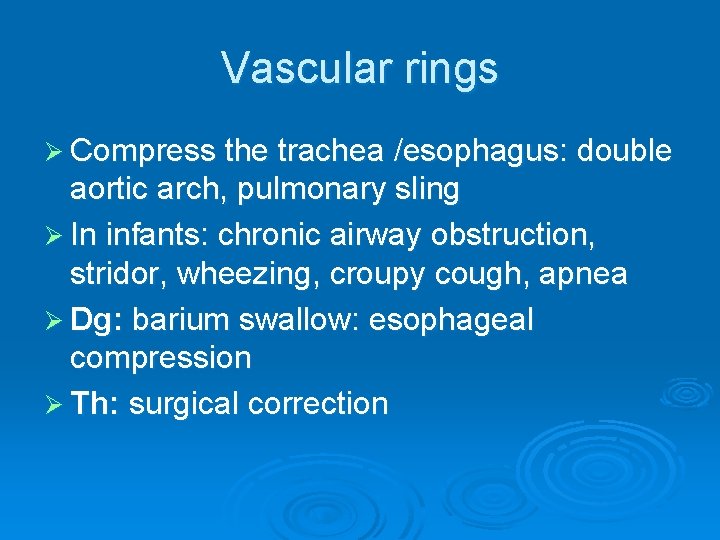
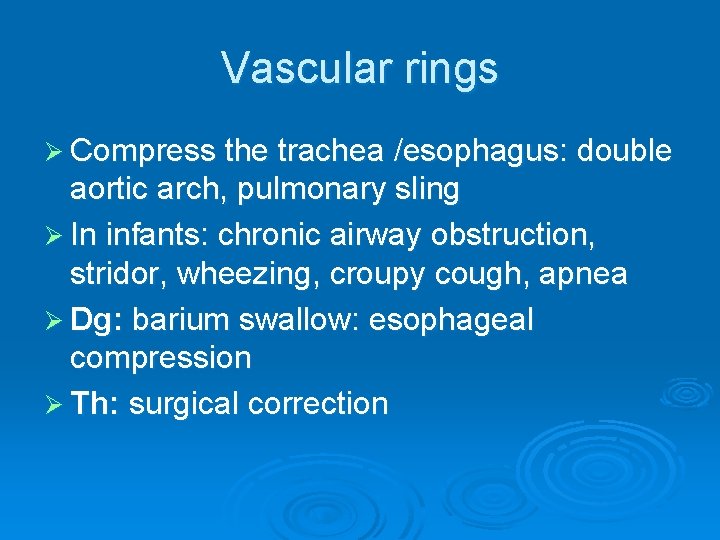
Vascular rings Ø Compress the trachea /esophagus: double aortic arch, pulmonary sling Ø In infants: chronic airway obstruction, stridor, wheezing, croupy cough, apnea Ø Dg: barium swallow: esophageal compression Ø Th: surgical correction


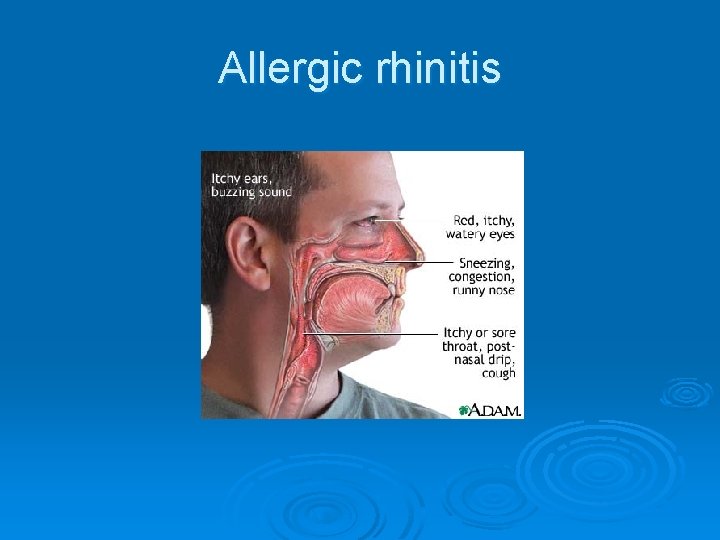
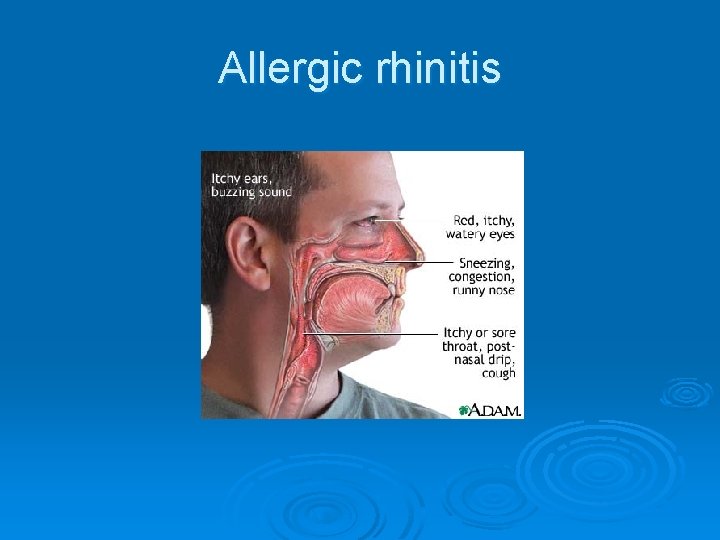
Allergic rhinitis
Allergic rhinitis Ø Most prevalent chronic condition: 5 -40% in children Ø Recurrent sneezing, nasal congestion, nasal discharge Ø Rubbing the nose with the palm of the hand („allergic salute”)
Allergic rhinitis
Croup syndrome Ø Upper airway obstruction Ø Viral croup: parainfluenza, RSV, adenovirus Ø Mycoplasma pneumoniae Ø Barking cough, stridor, suprasternal, intercostal, subcostal retractions, cyanosis Ø Th: hospitalization, oral hydration, nebulized racemic epinephrine (2. 25% sol. ), oral dexamethasone (0. 15 mg/kg), inhaled budenoside
Epiglottitis Emergency! 2 -7 yrs Ø Haemophilus influenzae type B (vaccination) Ø Sudden onset of high fever Ø Dysphagia, muffled voice, cyanosis, stridor, inspir. retractions Ø Progression to total airway obstruction Ø Th: endotracheal intubation, ceftriaxone iv. Ø Manipulate as little as possible! Ø



Foreign body aspiration, upper respiratory tract Ø 6 mo. – 4 yrs (small toys, peanuts) Ø Acute onset of cyanosis, choking, stridor (partial obstruction), inability to caugh or vocalize / aphonia / (complete obstruction) Ø Loss of consciousness, seizures, cardiopulmonary arrest Ø Th: emergency intubation, tracheostomy

Foreign body aspiration, lower respiratory tract Sudden onset of caugh, wheezing, later chronic cough, recurrent pneumonia Ø Bronchiectasis, lung abscess Ø Physical finding: asymmetric breath sounds, localized wheezing Ø Dg. : inspiratory and forced expiratory chest Xray : mediastinal shift away from the affected side (Holzknecht sign) Ø Complete obstruction: atelectasis Ø Th: bronchoscopy Ø
Bronchitis Ø Acute: nonproductive caugh, low fever Ø Physical symptom: diffuse rhonchi Ø Viral infection Ø Chronic: non-infectious causes: asthma, sinusitis, cystic fibrosis, respiratory tract anomalies, foreign bodies, recurrent aspiration
Asthma Ø Risk factors: atopic dermatitis, smoking in the family Ø Shedding of airway epithelium, edema, mucus plug formation, mast cell activation Ø Sensitisation to inhalant allergens: perennial aeroallergens, dust mites, cockroaches, animals
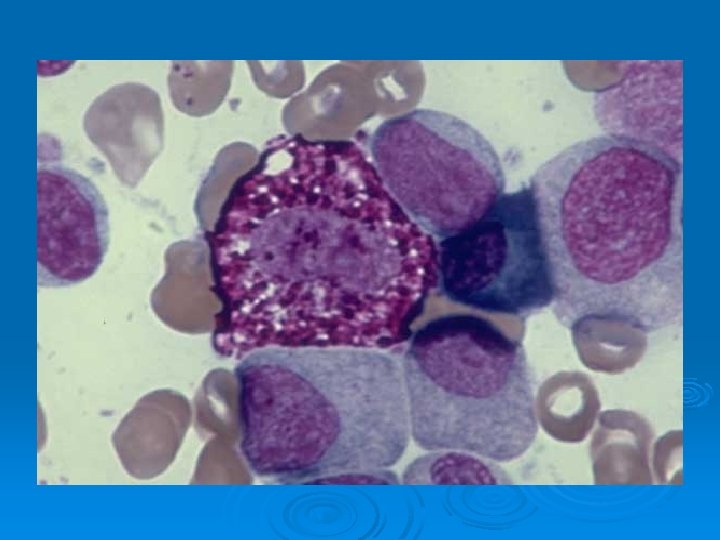
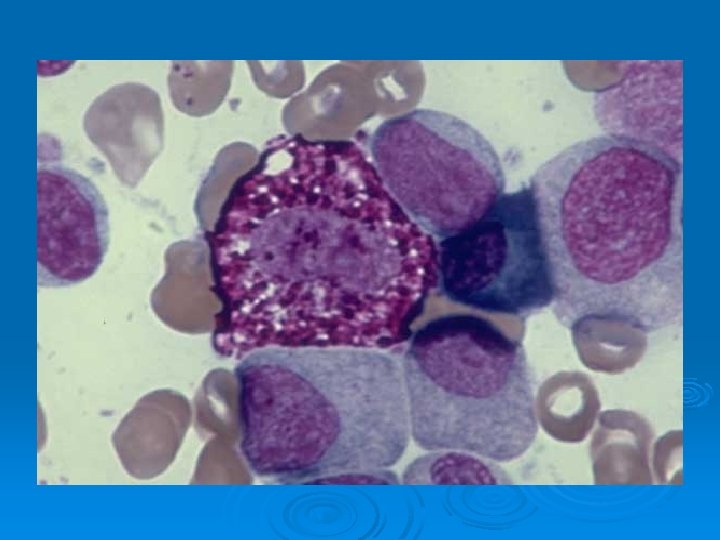
Mast cell, Normal marrow One mast cell partially degranulated (vacuolated areas), 1 plasma cell, 1 blast (top right center) 4 neutrophilic myelocytes, 2 band neutrophils, 1 smudge cell. Normal marrow - 100 X





Asthma Ø Wheezing, caugh, dyspnea, exercise intolerance, recurrent bronchitis and pneumonia, prolongation of the expiratory phase Ø Flaring of nostrils, intercostal- suprasternal retractions Ø Hypoxia: cyanosis of the lips, nail beds, tachycardia, agitation

Asthma Ø X-ray: hyperinflation , atelectasis Ø Serum Ig. E elevated, RIA for specific allergens Ø Skin tests Ø Pulmonary function tests (FEV 1, PEFR)

Asthma treatment Stepwise approach, assessment of clinical symptoms Ø Inhaled corticosteroids Ø Long-acting inhaled beta-2 agonists Ø Rescue: systemic corticosteroids Ø Bronchodilators Ø Leukotriene receptor antagonists and modifiers (Montelukast, zileuton) Ø Anti-inflammatory drugs Ø


Ø Nebulizers are used to treat asthma, Chronic Obstructive Pulmonary Disease (COPD), and other conditions where inhaled medicines are indicated. Nebulizers deliver a stream of medicated air to the lungs over a period of time.

Bronchopulmonary dysplasia (BPD) Ø Acute respiratory distress, first week of life Ø 30% of infants with birth-weight of less than 1000 grams Ø Chronic lung disease, inflammatory mediators, infection, lung development, barotrauma Ø Oxygen requirement for more than 28 days, positive pressure ventilation, CPAP, gestational age
Bacterial pneumonia Risks: aspiration, immunodeficiency, tracheoesophageal fistula, cleft palate, CF, congestive heart failure, splenectomia, etc. Ø Fever, cough, dyspnea, meningismus, abdominal pain, otitis media, Ø Laboratory findings: elevated WBC, CRP Ø Chest X-ray Ø Age-specific bacteria Ø Complications: empyema, sepsis, abscesses Ø


Mediastinal masses Ø Cough, wheezing, symptoms of infection, hemoptysis, dysphagia, pressure on the recurrent laryngeal nerve: hoarseness, vena cava superior syndrome Ø Cystic hygromas, vascular or neurogenic tumors, thymic masses, lymphomas, teratomas, esophageal lesions, mediastinal abscess
 Gyrgy
Gyrgy Phokomelien
Phokomelien Olivospinal tract vs tectospinal tract
Olivospinal tract vs tectospinal tract Difference between pyramidal and extrapyramidal tract
Difference between pyramidal and extrapyramidal tract Capnia medical term
Capnia medical term Global alliance against chronic respiratory diseases
Global alliance against chronic respiratory diseases Laynx
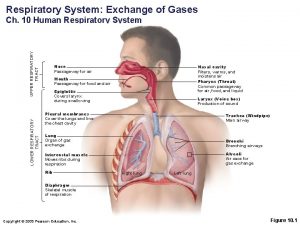
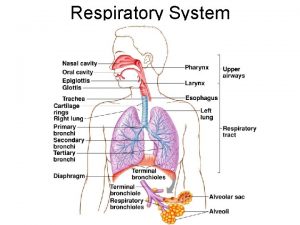
Laynx Upper and lower respiratory system
Upper and lower respiratory system Respiratory zone
Respiratory zone Upper respiratory tract
Upper respiratory tract Classification of upper respiratory tract infection
Classification of upper respiratory tract infection Anatomy of the upper respiratory tract
Anatomy of the upper respiratory tract Lrti
Lrti Trachea and windpipe
Trachea and windpipe Hrpangina
Hrpangina Normal flora of respiratory tract
Normal flora of respiratory tract Classification of pneumonia
Classification of pneumonia Upper rti
Upper rti Conducting zone and respiratory zone
Conducting zone and respiratory zone Dr fekete erika
Dr fekete erika Tvedse
Tvedse Wolf hirschhorn syndrom lebenserwartung
Wolf hirschhorn syndrom lebenserwartung Alexandra fekete
Alexandra fekete Dr fekete rita
Dr fekete rita Ii. anund svéd király
Ii. anund svéd király Fekete árpád
Fekete árpád Fekete csilla
Fekete csilla Ede de bedezodoroztad magad
Ede de bedezodoroztad magad Dr fekete rita
Dr fekete rita Fekete zab lovaknak
Fekete zab lovaknak Paul fekete
Paul fekete Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Phối cảnh
Phối cảnh Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Slidetodoc
Slidetodoc Sơ đồ cơ thể người
Sơ đồ cơ thể người Thế nào là số nguyên tố
Thế nào là số nguyên tố đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Thang điểm glasgow
Thang điểm glasgow