Diagnosis and Staging Jo Anne Zujewski MD Head





- Slides: 45
Diagnosis and Staging Jo. Anne Zujewski, MD Head, Breast Cancer Therapeutics Clinical Investigations Branch Cancer Therapy Evaluation Program Division of Cancer Diagnostics and Treatment May 2011
NEJM, November 23, 2000
Early Detections reduces the risk of dying from breast cancer.
Cancer Diagnosis: Defining the Cancer • The first step in designing the treatment plan is carefully defining the cancer – Clinical examination – Radiology tests – Pathology tests – Blood tests

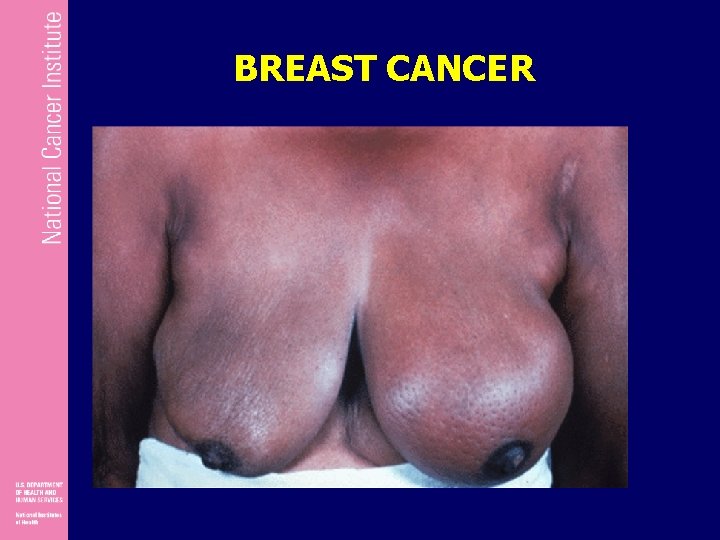
Breast Cancer Signs and Symptoms • • None Lump or mass Pain in breast Tenderness Thickening Firmness Nipple discharge • • Skin redness Asymmetry Enlargement Nipple retraction Dimpling Mass in axilla (armpit) Warmth


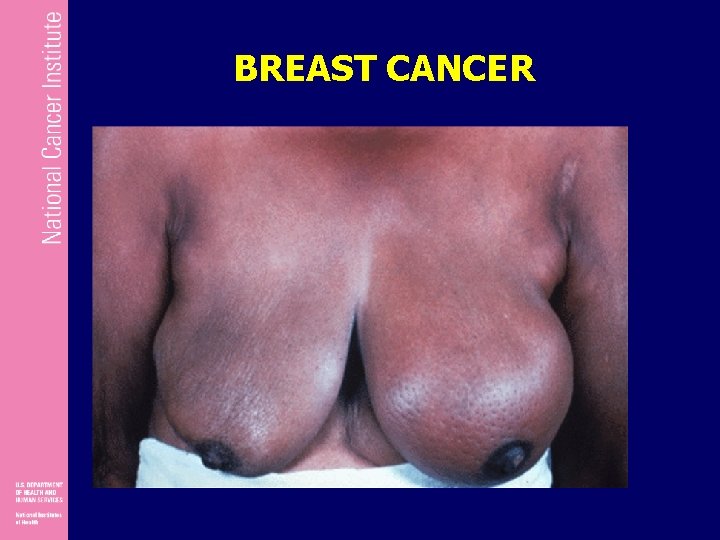
BREAST CANCER

Defining the Cancer: Radiology • Radiologic imaging can help determine the location and spread of the cancer – Local extent – Regional lymph nodes – Distant spread (metastases)
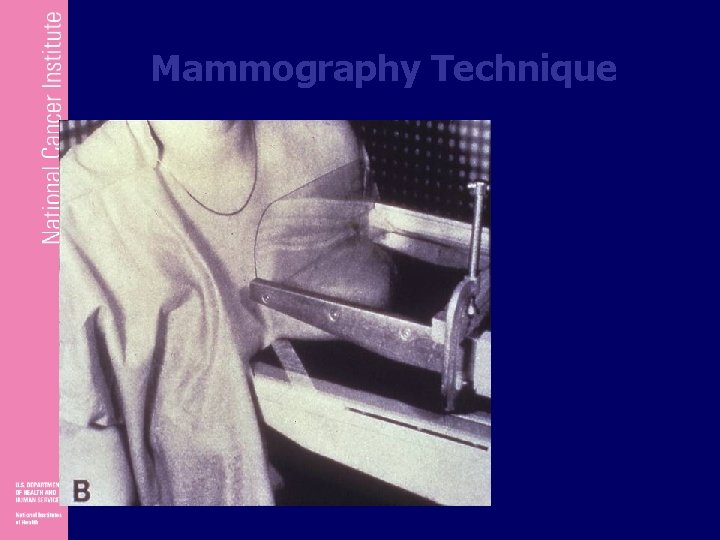
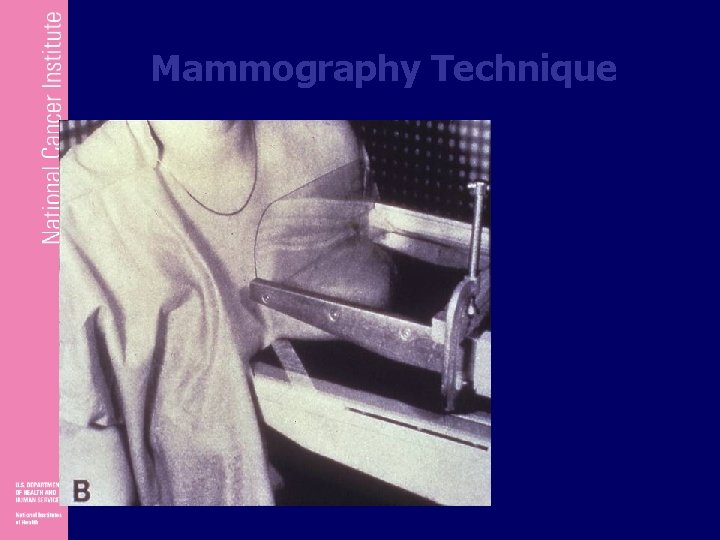
Mammography Technique
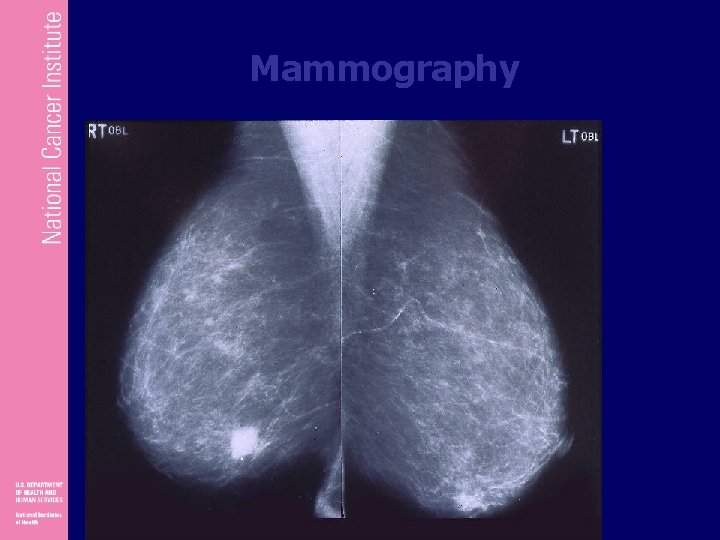
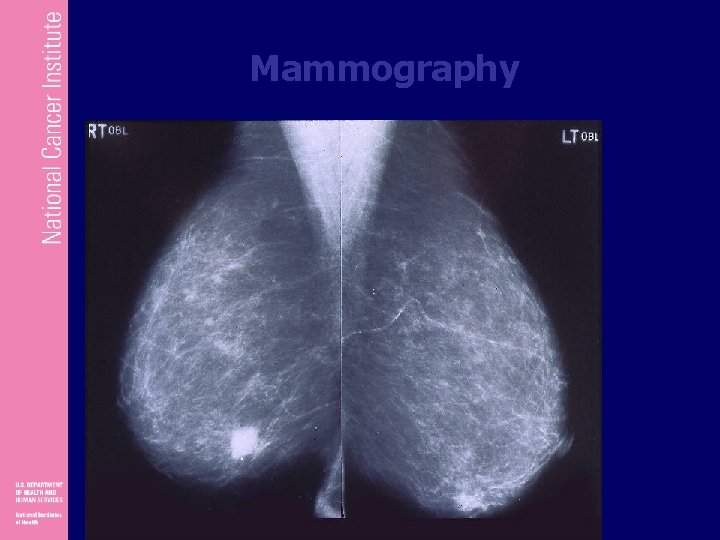
Mammography
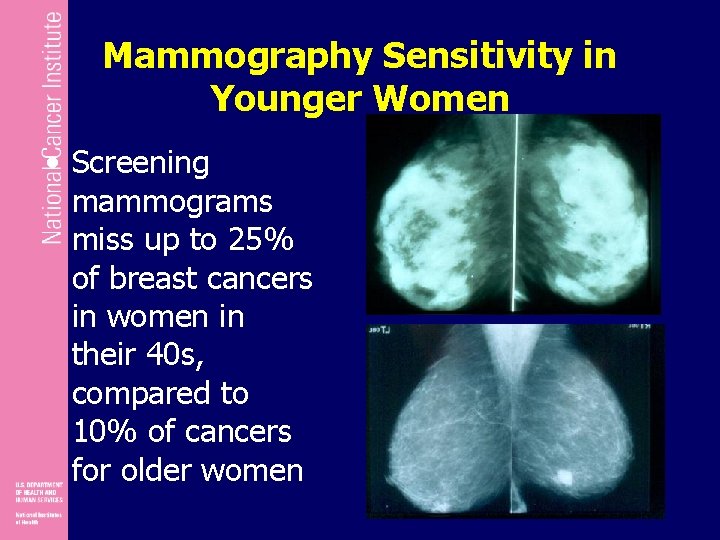
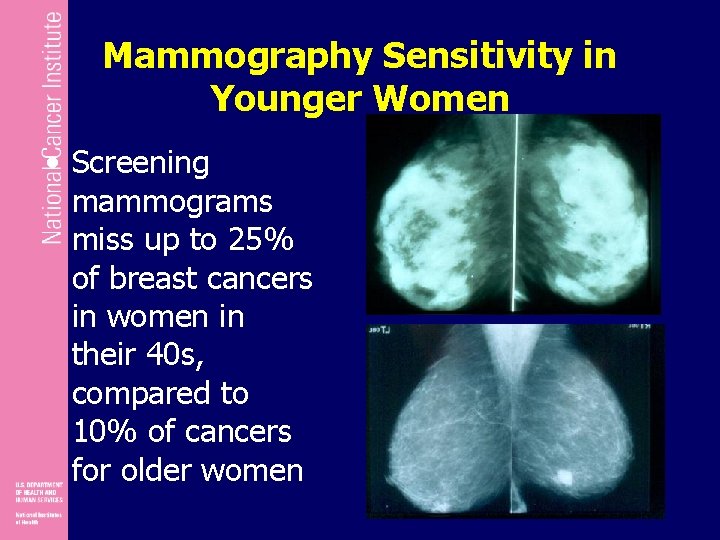
Mammography Sensitivity in Younger Women • Screening mammograms miss up to 25% of breast cancers in women in their 40 s, compared to 10% of cancers for older women
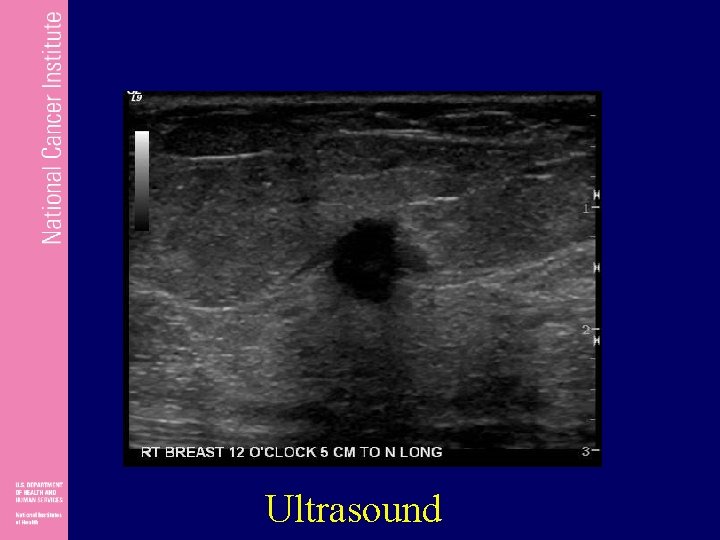
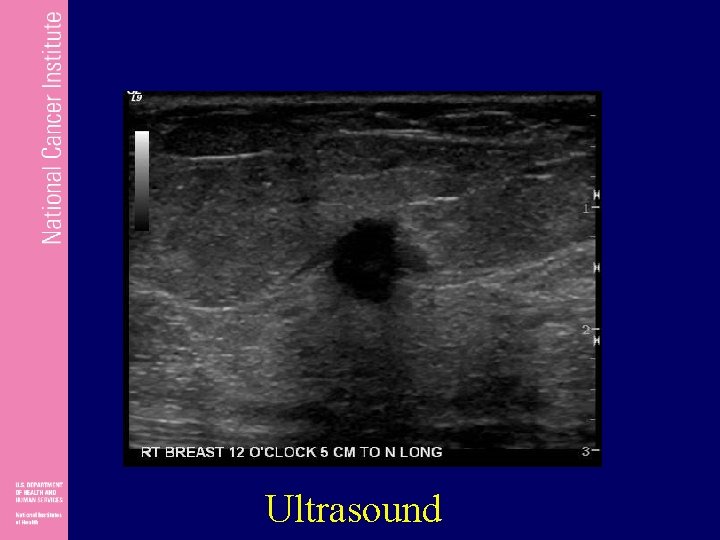
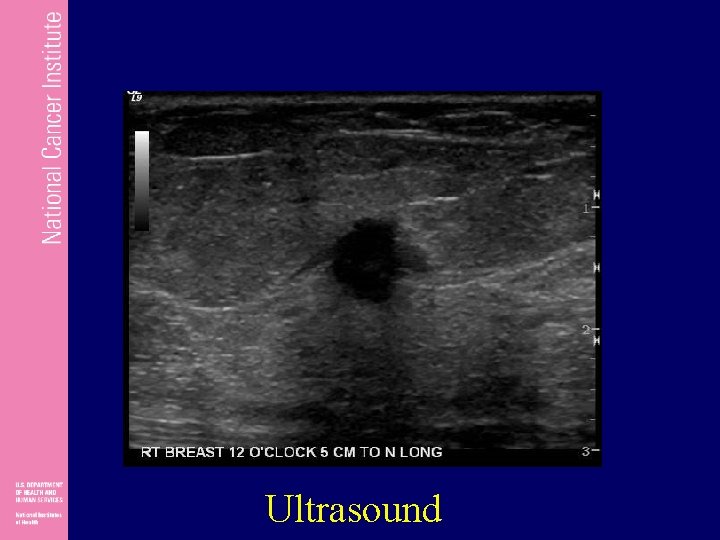
Ultrasound
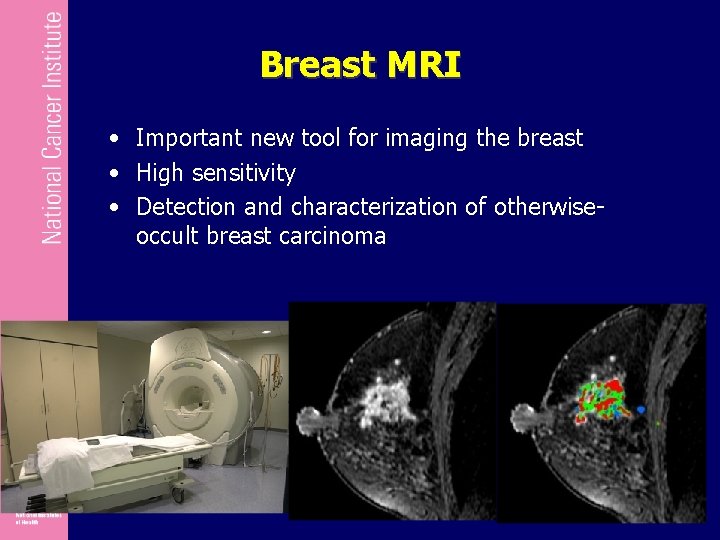
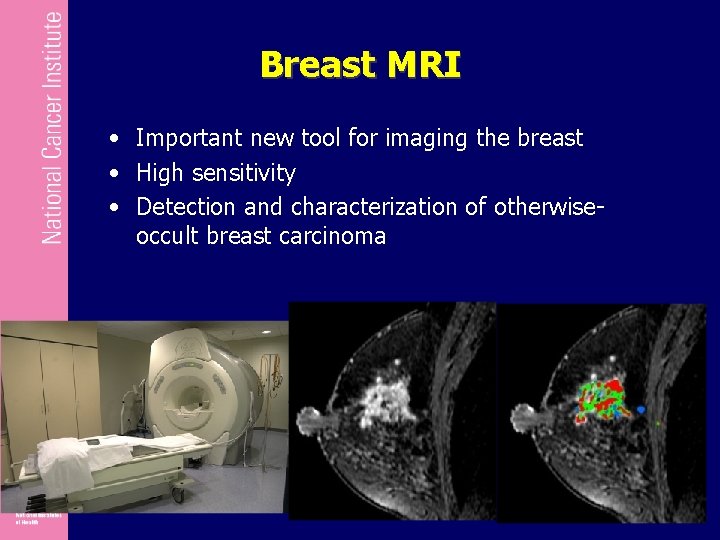
Breast MRI • Important new tool for imaging the breast • High sensitivity • Detection and characterization of otherwiseoccult breast carcinoma
Breast Cancer Diagnosis • Any breast change or lump needs to be evaluated • Breast cancer needs to be diagnosed by biopsy – Fine needle aspiration – Core needle biopsy – Surgical biopsy
Mammotone & Minimally Invasive Breast Biopsy (MIBB) The Mammotone and MIBB are different from the core needle biopsy in that a needle is inserted once and multiple specimens are removed through contiguous sampling. Core needle biopsies require the needle to be inserted multiple times. Both the Mammotone and MIBB biopsy utilize a vacuum system. A probe is inserted and samples of tissue are collected in a chamber. Tissue samples are removed by action of a gentle vacuum.
Advantages of Needle Biopsies • • • Simple procedure – does not require surgery Accurate Quick – only takes a few minutes Not painful Inexpensive Quick results
Disadvantages of Needle Biopsies • Entire lump is not removed • Open biopsy may be necessary For Fine Needle Only: • Specialist needed to read results • In situ cancer not distinguishable from invasive cancer
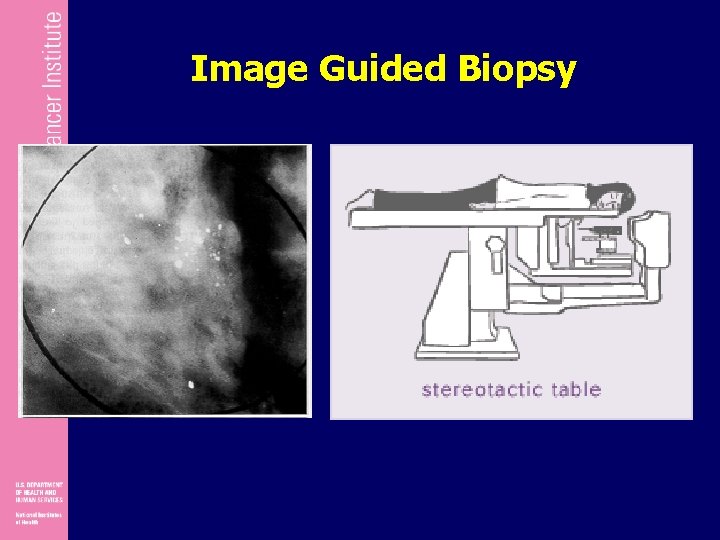
Image Guided Biopsy in Clinical Practice • • Allows treatment planning Better cosmesis Can mark site with clip Less costly • Needs specialized equipment • May still require confirmatory pathology in minority of cases
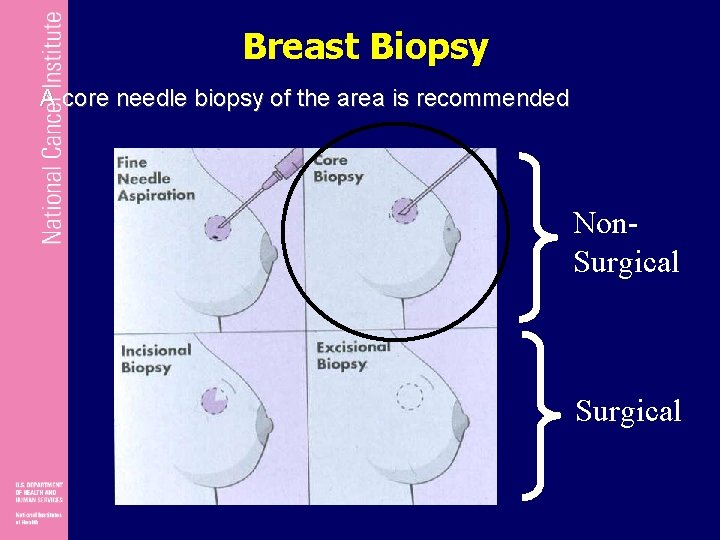
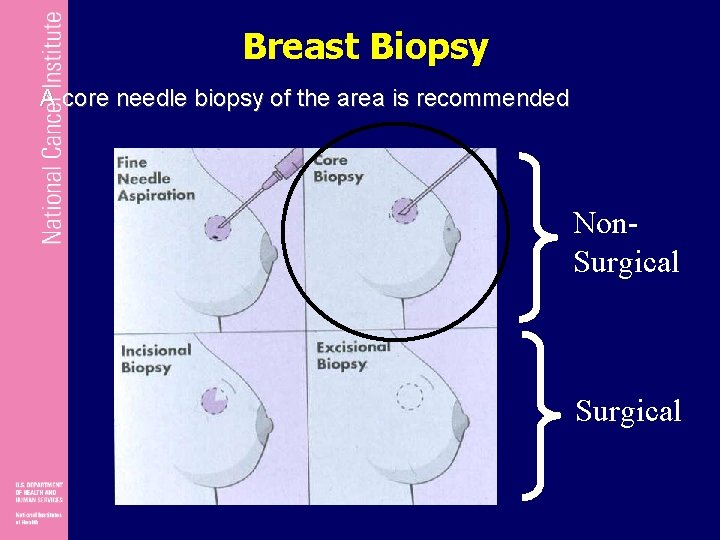
Breast Biopsy A core needle biopsy of the area is recommended Non. Surgical
Ultrasound-Guided Breast Biopsy
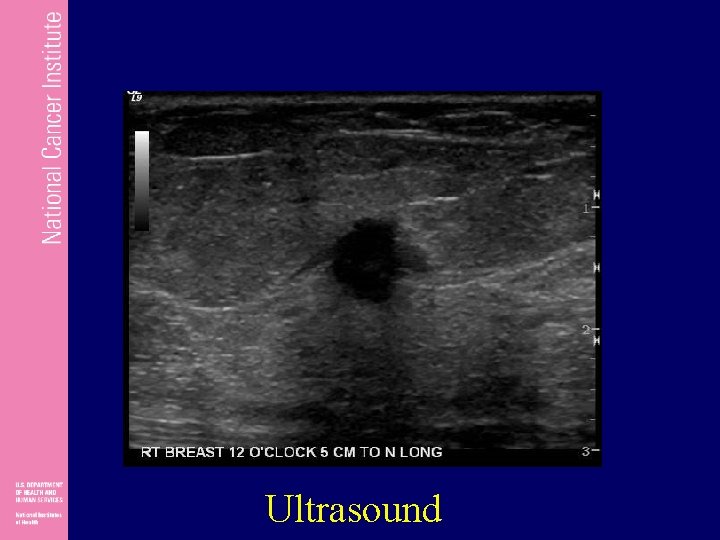
Ultrasound
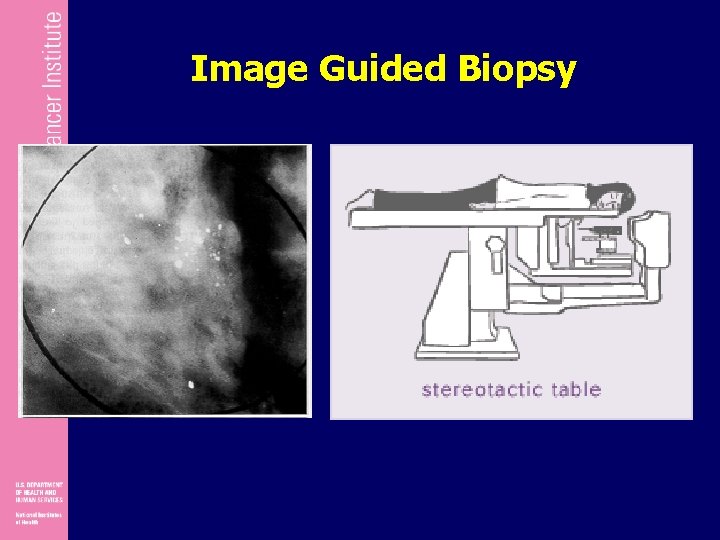
Image Guided Biopsy
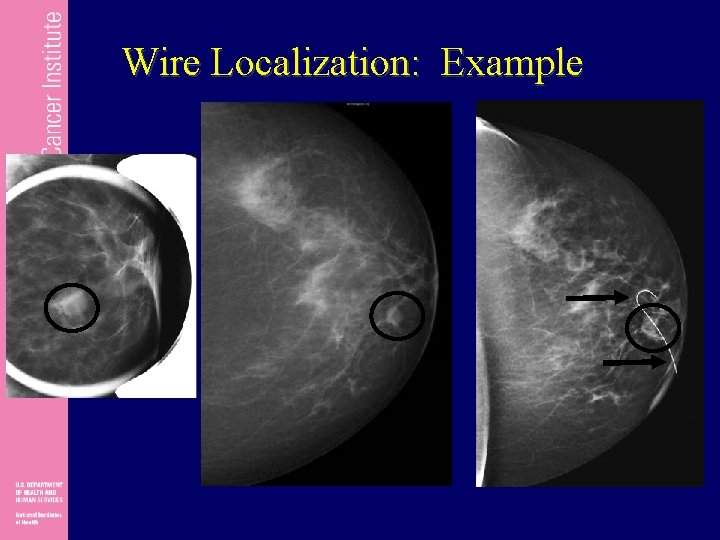
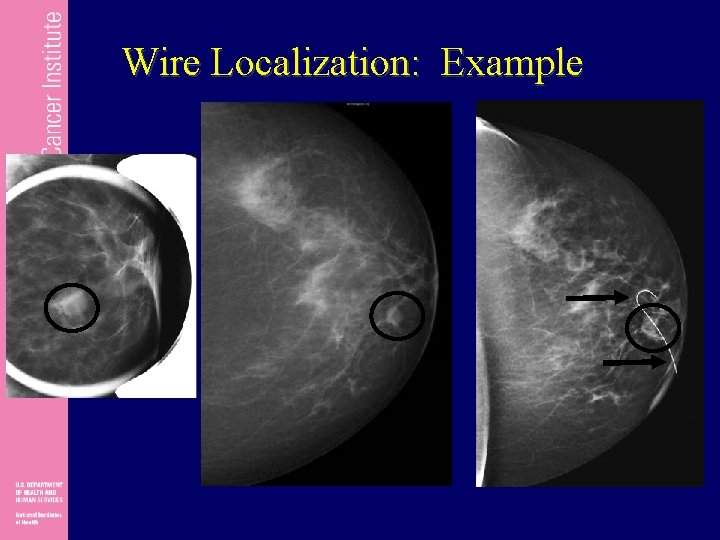
Wire Localization: Example
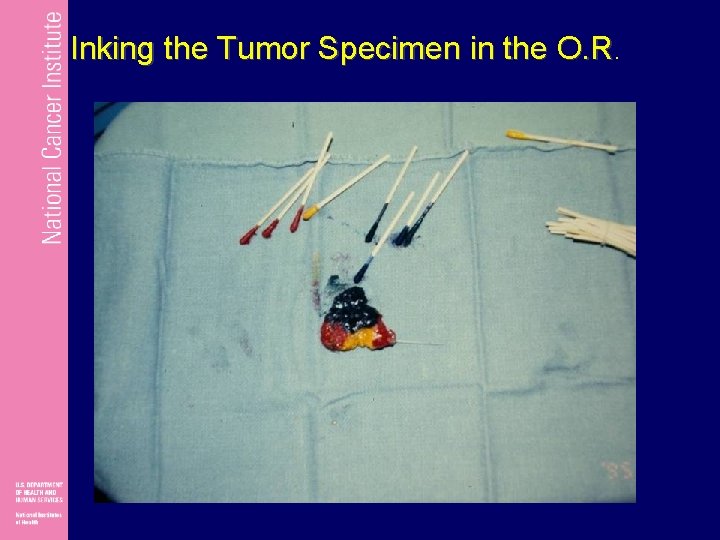
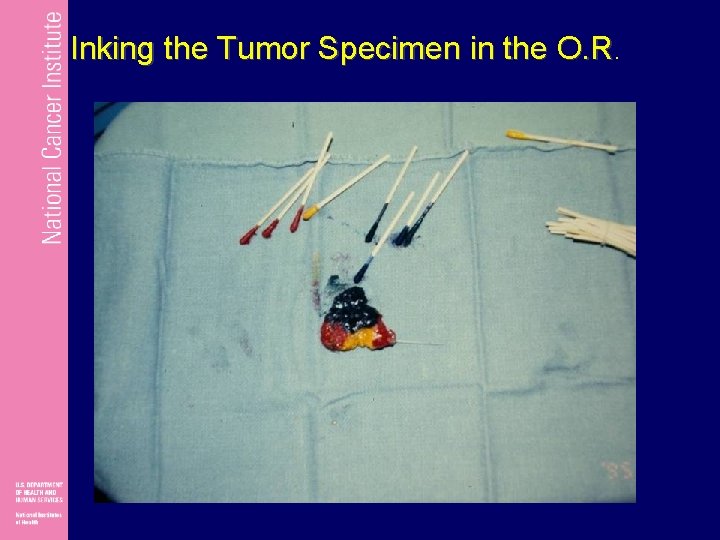
Inking the Tumor Specimen in the O. R.
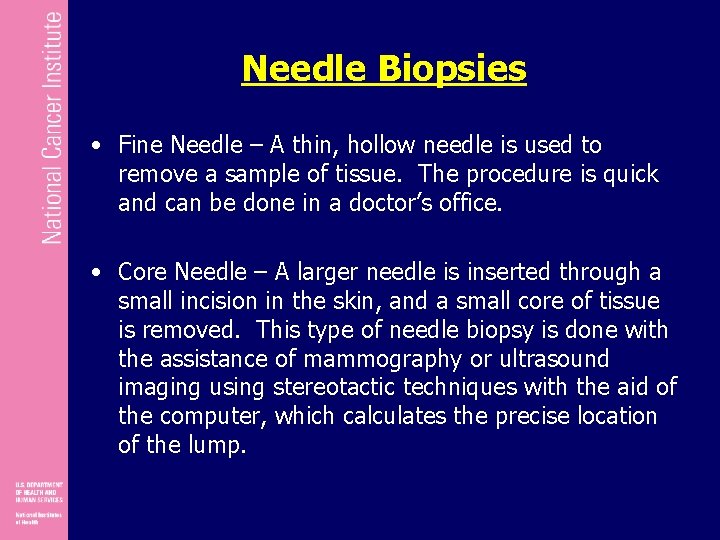
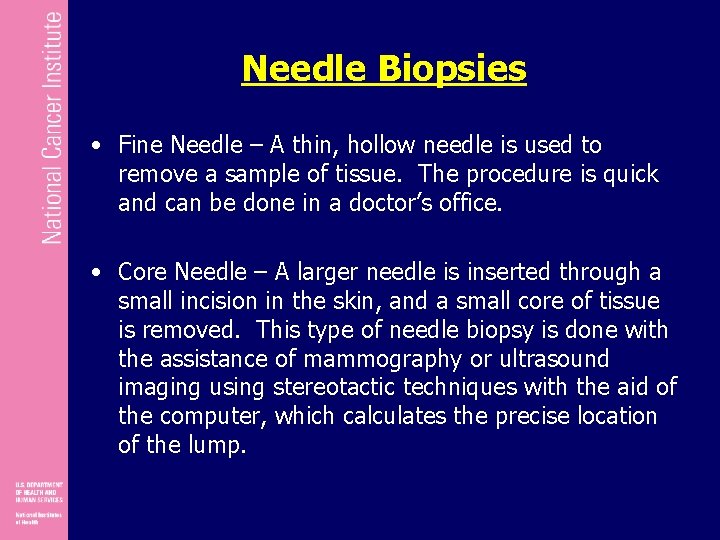
Needle Biopsies • Fine Needle – A thin, hollow needle is used to remove a sample of tissue. The procedure is quick and can be done in a doctor’s office. • Core Needle – A larger needle is inserted through a small incision in the skin, and a small core of tissue is removed. This type of needle biopsy is done with the assistance of mammography or ultrasound imaging using stereotactic techniques with the aid of the computer, which calculates the precise location of the lump.
Incisional Biopsy • A surgical procedure where only a portion of a tumor is removed • Generally reserved for lumps that are larger • Performed under local anesthesia in a hospital or outpatient clinic
Excisional Biopsy • A surgical procedure that removes the entire suspected area plus some surrounding normal tissue. • Standard procedure for lumps that are smaller than an inch or so in diameter • Similar to a lumpectomy • Performed under local anesthetic or general anesthesia in a hospital or outpatient clinic
Advantages of Open Biopsies • Quick – takes only one hour • More accurate than a needle biopsy • Larger samples provide information for treatment plan Excisional Only: • Removes entire lump • May be the only surgical treatment needed
Disadvantages of Open Biopsies • Surgical procedure • Expensive • Side effects such as infection or blood collection under the skin Excisional Only: • Removing tissue can change the look and feel of the breast
Cancer is diagnosed in 1 of 5 breast biopsies
Staging

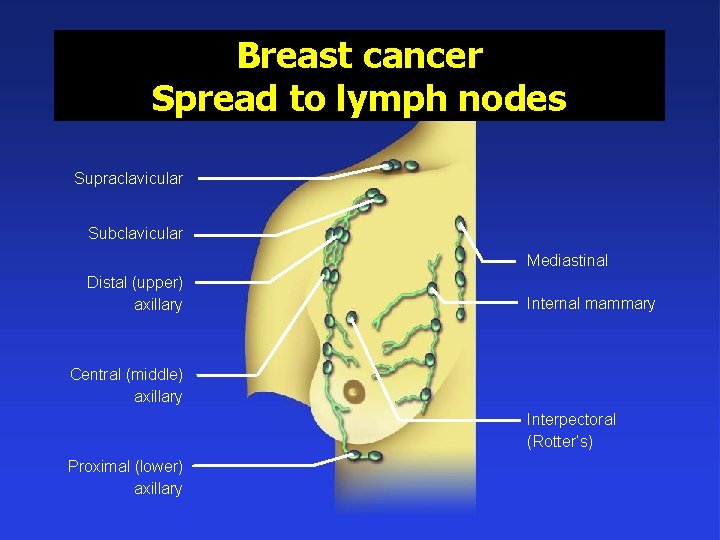
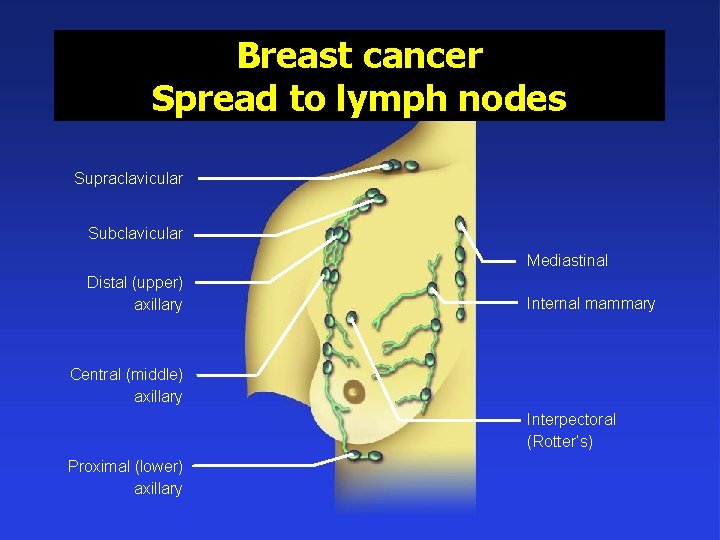
Breast cancer Spread to lymph nodes Supraclavicular Subclavicular Mediastinal Distal (upper) axillary Internal mammary Central (middle) axillary Interpectoral (Rotter’s) Proximal (lower) axillary
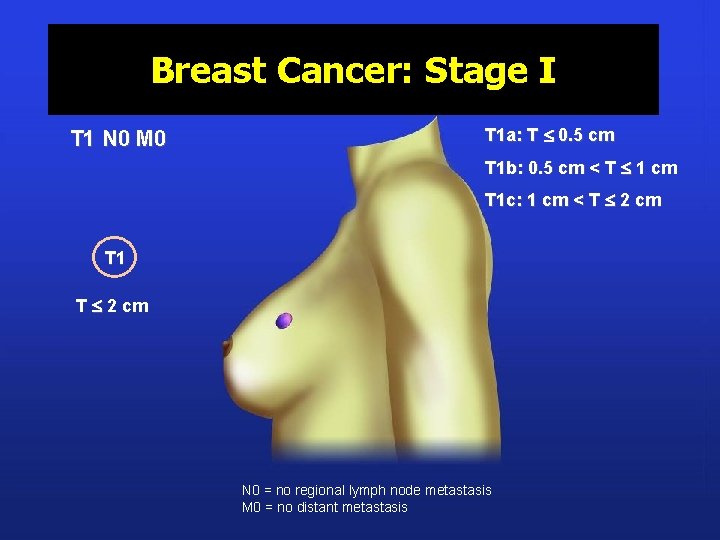
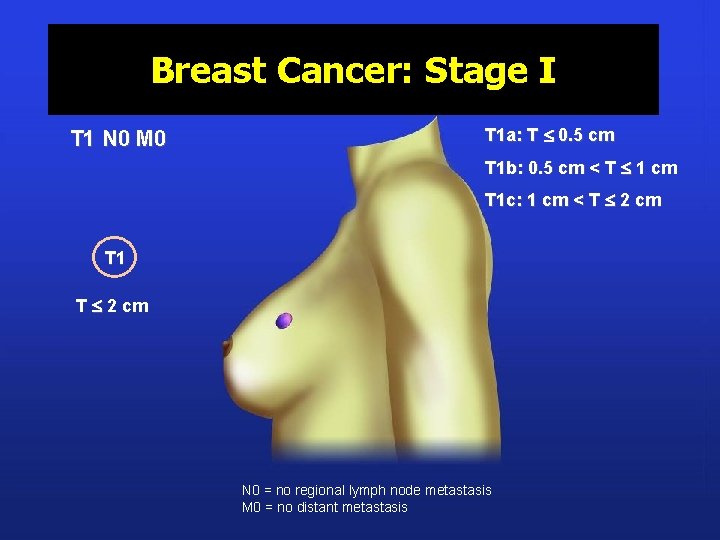
Breast Cancer: Stage I T 1 N 0 M 0 T 1 a: T 0. 5 cm T 1 b: 0. 5 cm < T 1 cm T 1 c: 1 cm < T 2 cm T 1 T 2 cm N 0 = no regional lymph node metastasis M 0 = no distant metastasis
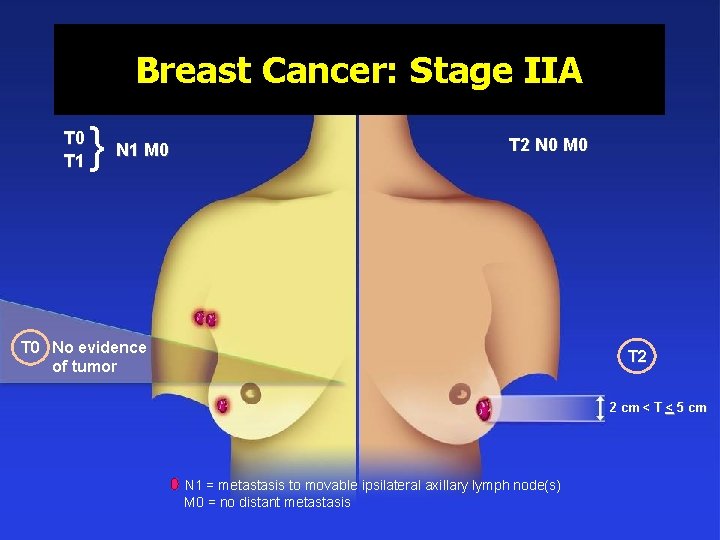
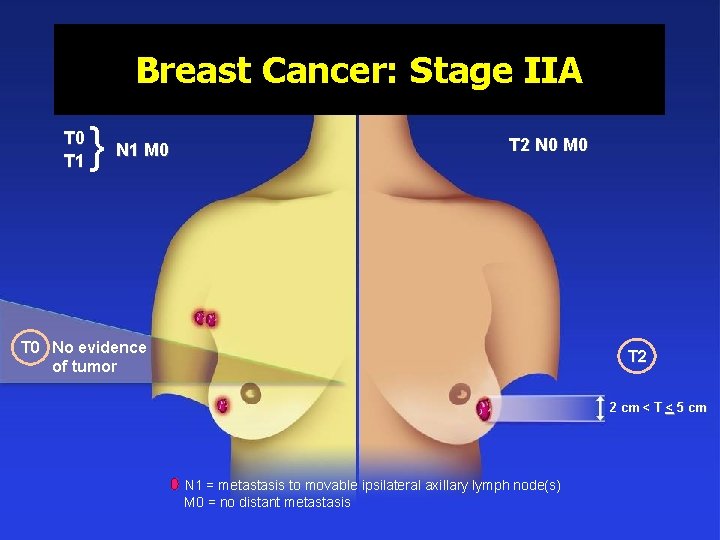
Breast Cancer: Stage IIA T 0 T 1 } N 1 M 0 T 2 N 0 M 0 T 0 No evidence of tumor T 2 2 cm < T < 5 cm N 1 = metastasis to movable ipsilateral axillary lymph node(s) M 0 = no distant metastasis
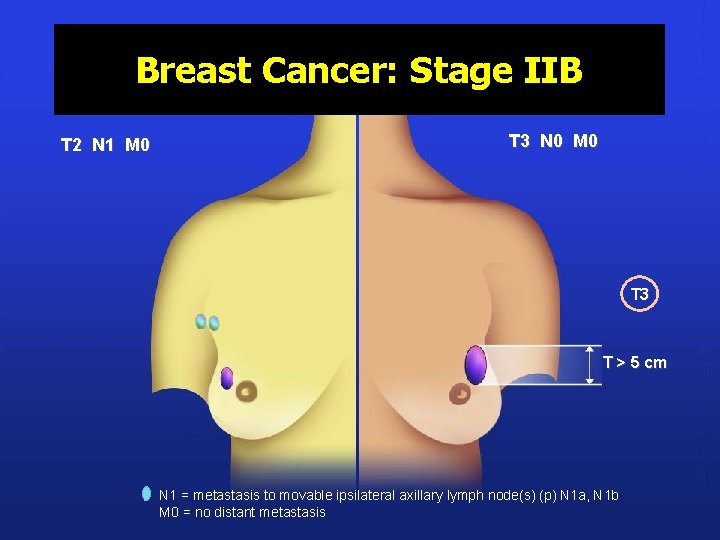
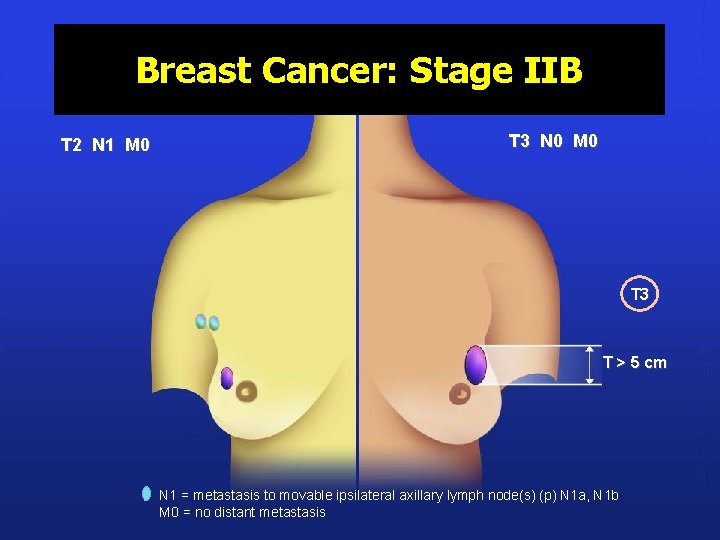
Breast Cancer: Stage IIB T 2 N 1 M 0 T 3 N 0 M 0 T 3 T > 5 cm N 1 = metastasis to movable ipsilateral axillary lymph node(s) (p) N 1 a, N 1 b M 0 = no distant metastasis
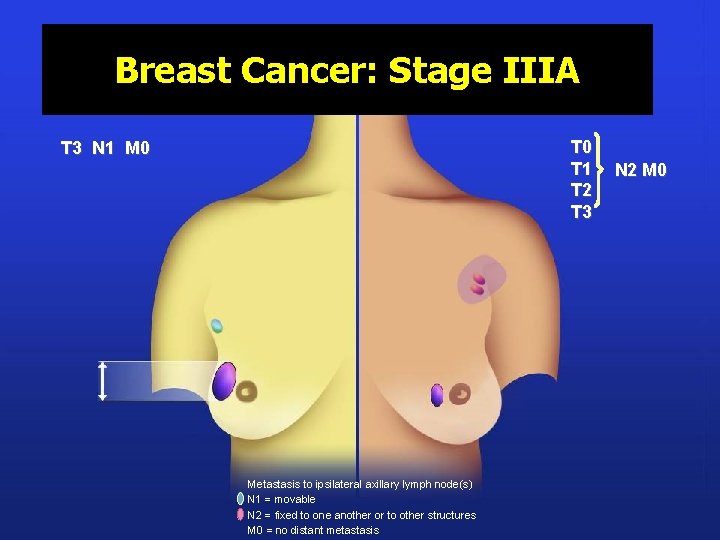
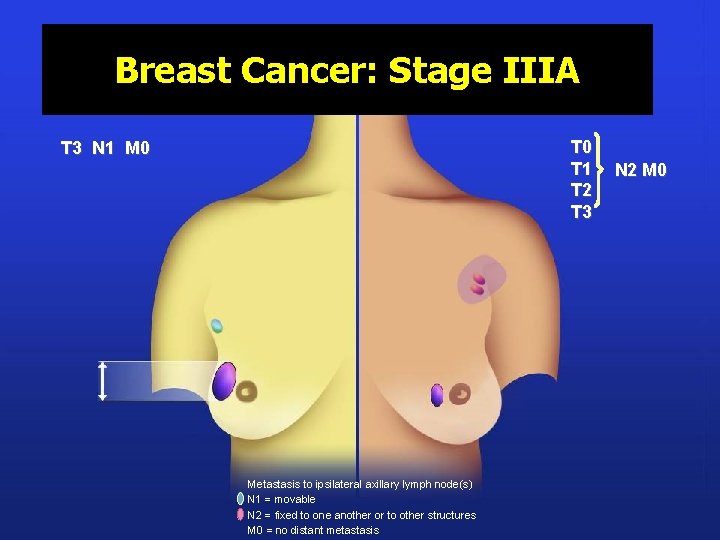
Breast Cancer: Stage IIIA T 0 T 1 T 2 T 3 N 1 M 0 Metastasis to ipsilateral axillary lymph node(s) N 1 = movable N 2 = fixed to one another or to other structures M 0 = no distant metastasis N 2 M 0
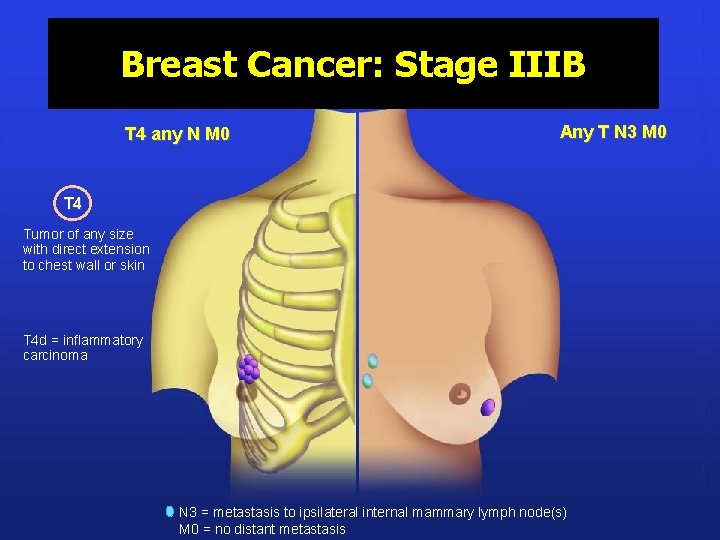
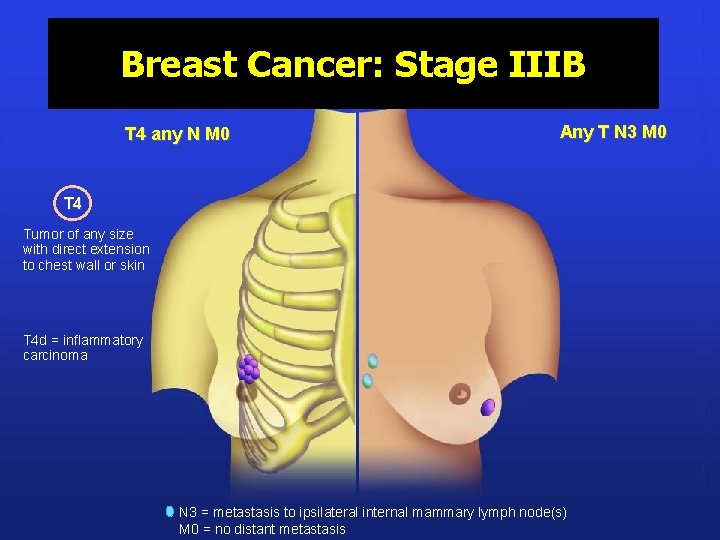
Breast Cancer: Stage IIIB T 4 any N M 0 Any T N 3 M 0 T 4 Tumor of any size with direct extension to chest wall or skin T 4 d = inflammatory carcinoma N 3 = metastasis to ipsilateral internal mammary lymph node(s) M 0 = no distant metastasis
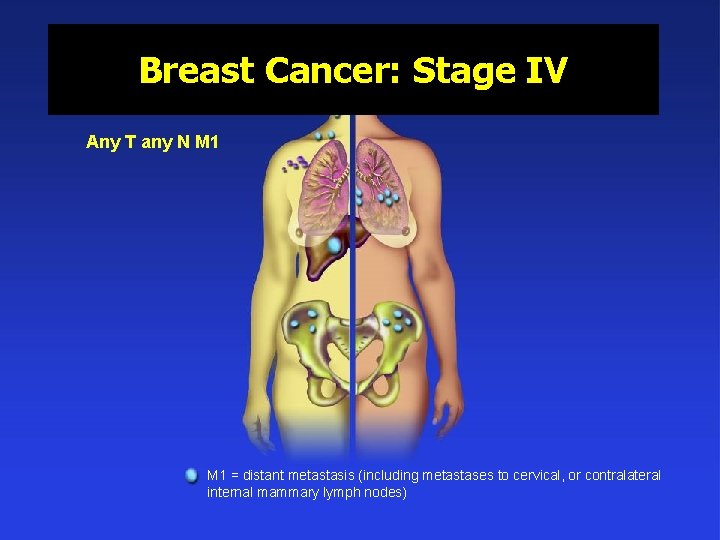
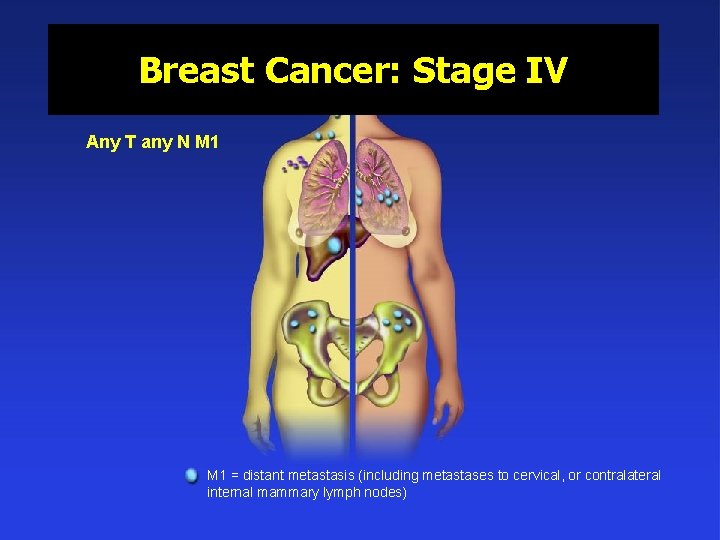
Breast Cancer: Stage IV Any T any N M 1 = distant metastasis (including metastases to cervical, or contralateral internal mammary lymph nodes)
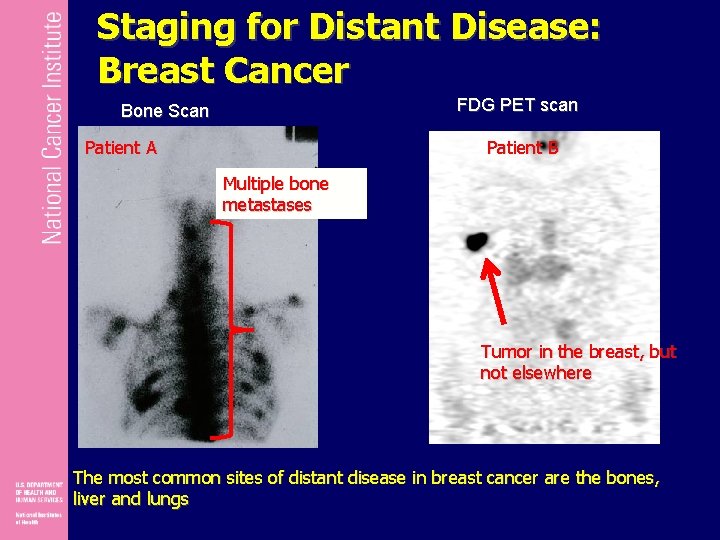
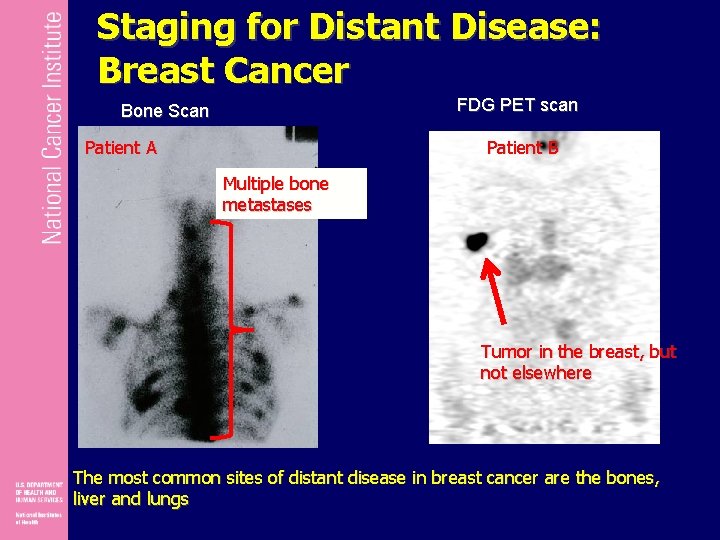
Staging for Distant Disease: Breast Cancer FDG PET scan Bone Scan Patient A Patient B Multiple bone metastases Tumor in the breast, but not elsewhere The most common sites of distant disease in breast cancer are the bones, liver and lungs
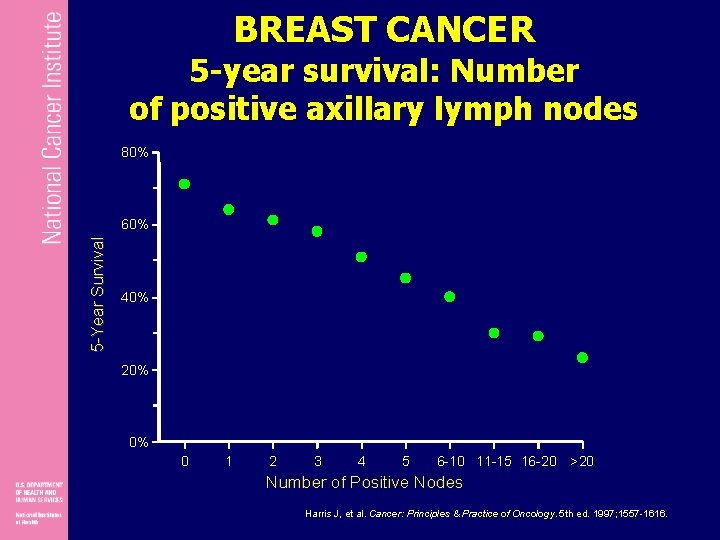
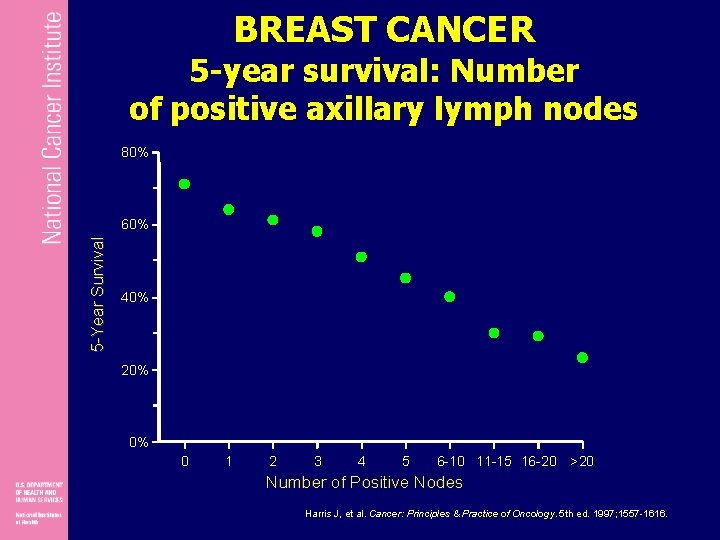
BREAST CANCER 5 -year survival: Number of positive axillary lymph nodes 80% 5 -Year Survival 60% 40% 20% 0% 0 1 2 3 4 5 6 -10 11 -15 16 -20 >20 Number of Positive Nodes Harris J, et al. Cancer: Principles & Practice of Oncology. 5 th ed. 1997; 1557 -1616.
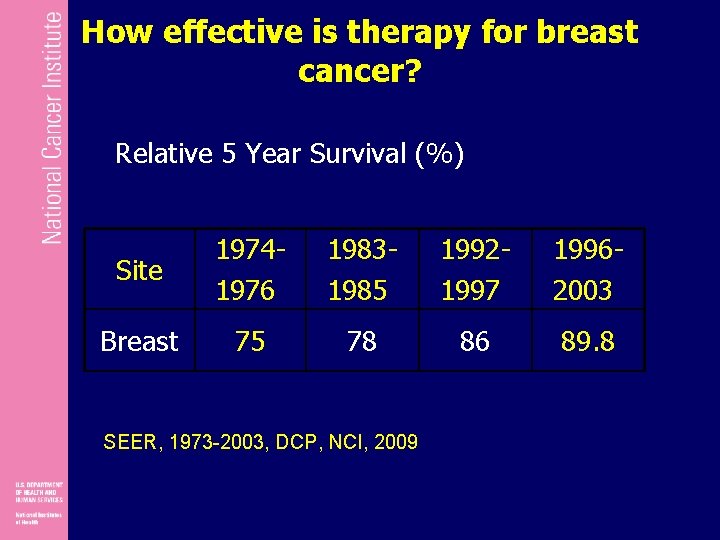
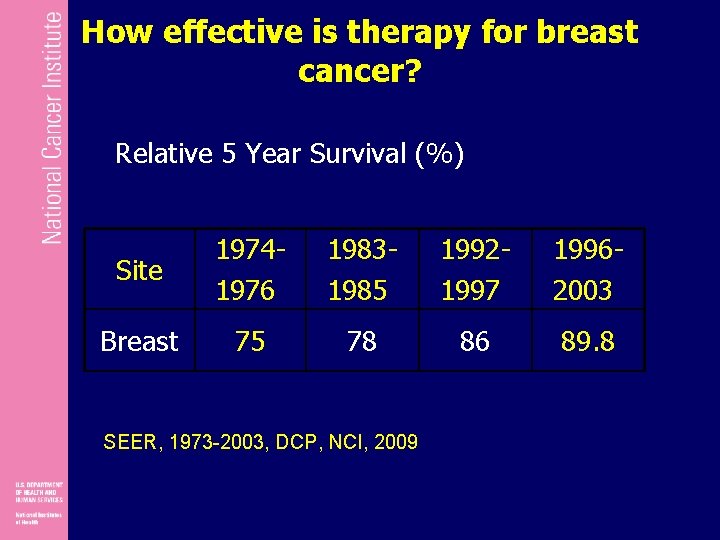
How effective is therapy for breast cancer? Relative 5 Year Survival (%) Site 19741976 19831985 19921997 19962003 Breast 75 78 86 89. 8 SEER, 1973 -2003, DCP, NCI, 2009
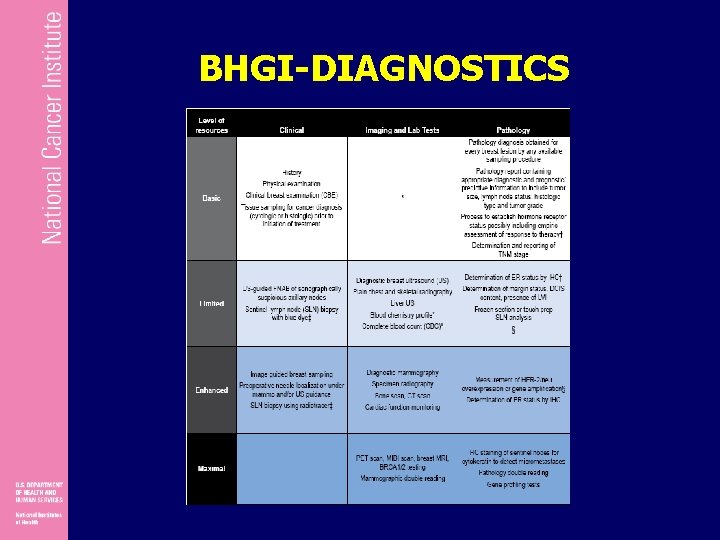
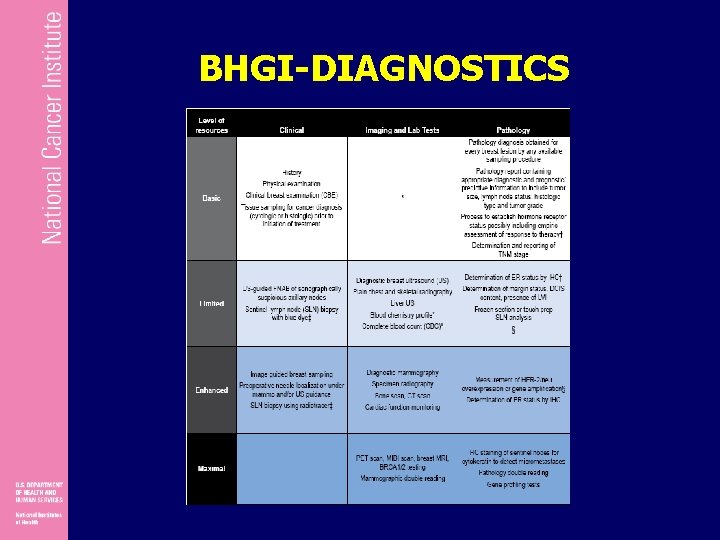
BHGI-DIAGNOSTICS
 Nursing diagnosis
Nursing diagnosis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Types of nursing diagnosis
Types of nursing diagnosis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Dividing head chart
Dividing head chart Flooded suction pump
Flooded suction pump The attacking firm goes head-to-head with its competitor.
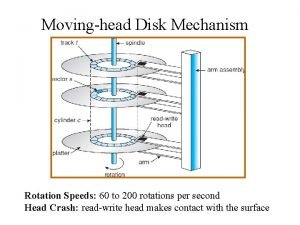
The attacking firm goes head-to-head with its competitor. Disk
Disk Head body head body gif
Head body head body gif What is tonic syllable
What is tonic syllable Patientsite.com
Patientsite.com What is tone unit
What is tone unit The head of moving head disk with 100 tracks
The head of moving head disk with 100 tracks Traverse stage cons
Traverse stage cons What is staging
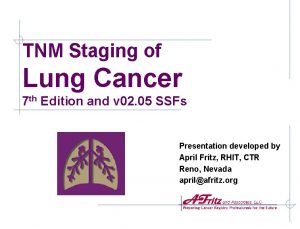
What is staging Tnm stage lung cancer
Tnm stage lung cancer Tnm staging lung
Tnm staging lung Different theatre stages
Different theatre stages Edmonton stage obesity
Edmonton stage obesity Position control definition
Position control definition Zarobki dyspozytora
Zarobki dyspozytora Tanner stages male
Tanner stages male Laila
Laila Varicose vein staging
Varicose vein staging Edmonton obesity staging system
Edmonton obesity staging system Tnm breast cancer staging
Tnm breast cancer staging Ann arbor staging system
Ann arbor staging system Perminaye
Perminaye Glottic cancer staging
Glottic cancer staging Olga olgim staging system
Olga olgim staging system Sarnat staging
Sarnat staging Iap slides
Iap slides Hodgkin's lymphoma classification
Hodgkin's lymphoma classification Primary cutaneous gamma/delta t-cell lymphoma
Primary cutaneous gamma/delta t-cell lymphoma Lugano classification
Lugano classification Amenorrhea symptoms
Amenorrhea symptoms Tanner staging male
Tanner staging male Data warehouse staging area
Data warehouse staging area Data warehouse components
Data warehouse components Chirurgia bariatrica
Chirurgia bariatrica Ajcc breast cancer staging 8th edition poster
Ajcc breast cancer staging 8th edition poster Ajcc staging breast
Ajcc staging breast Emaco regimen
Emaco regimen Stage right stage left
Stage right stage left