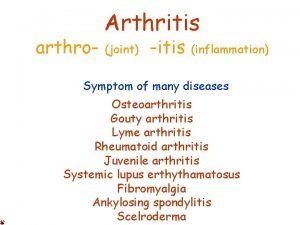
Definition Arthroplasty Arthro Plasty Arthro Joint Plasty Molding
























- Slides: 61

Definition • Arthroplasty = Arthro + Plasty – Arthro = Joint – Plasty = Molding, grafting, or formation of a specified part • E. g. Rhinoplasty, Mammoplasty
Definition • Arthroplasty = surgical reconstruction or replacement of a joint • THA = Total hip arthroplasty • THR = Total hip replacement
Type of Hip arthroplasty • Total hip arthroplasty • Hemiarthroplasty – Bipolar Hemiarthroplasty – Unipolar Hemiarthroplasty • Hip resurfacing • Revision THA

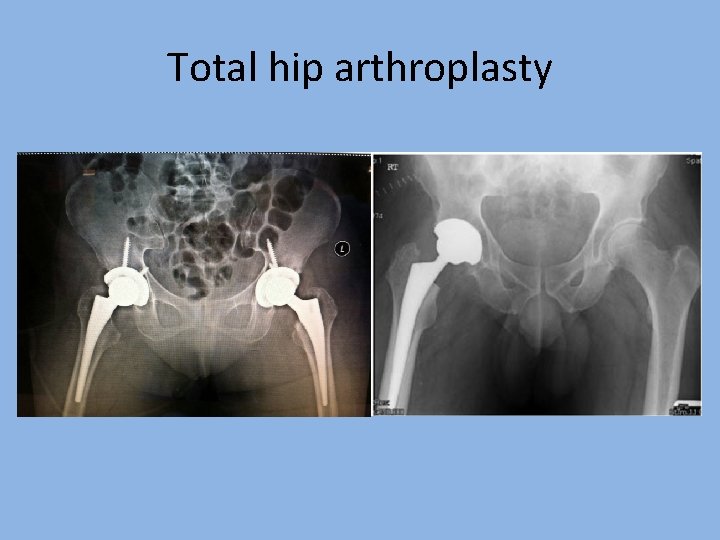
Total hip arthroplasty

Total hip arthroplasty

Total hip arthroplasty
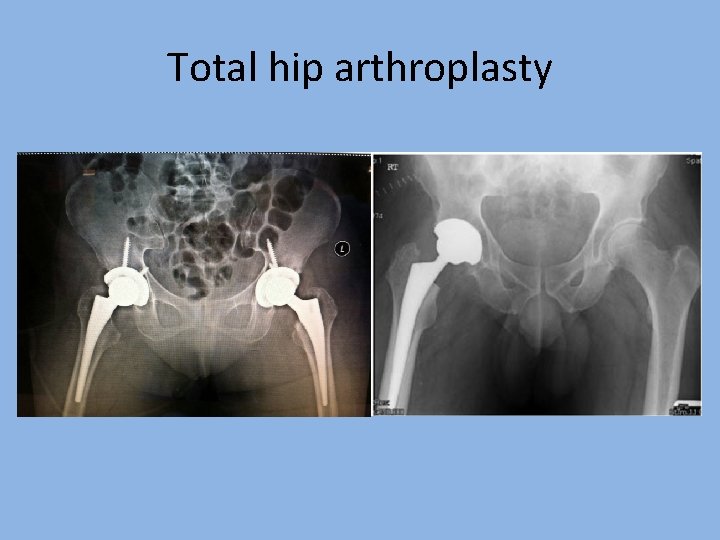
Total hip arthroplasty
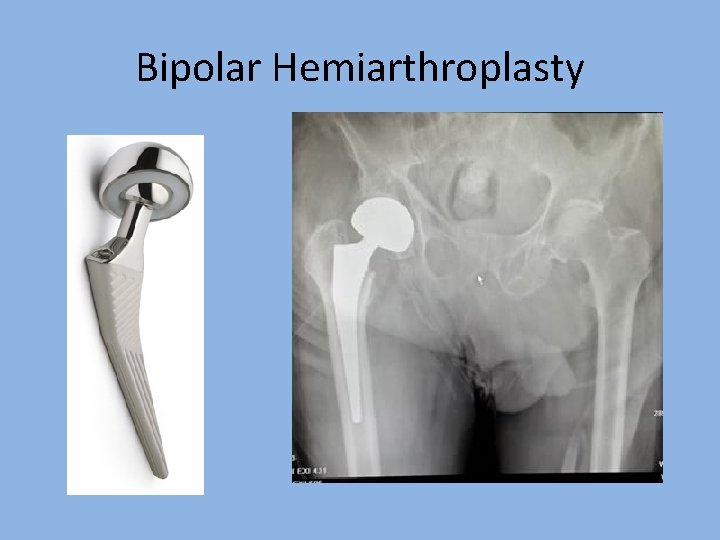
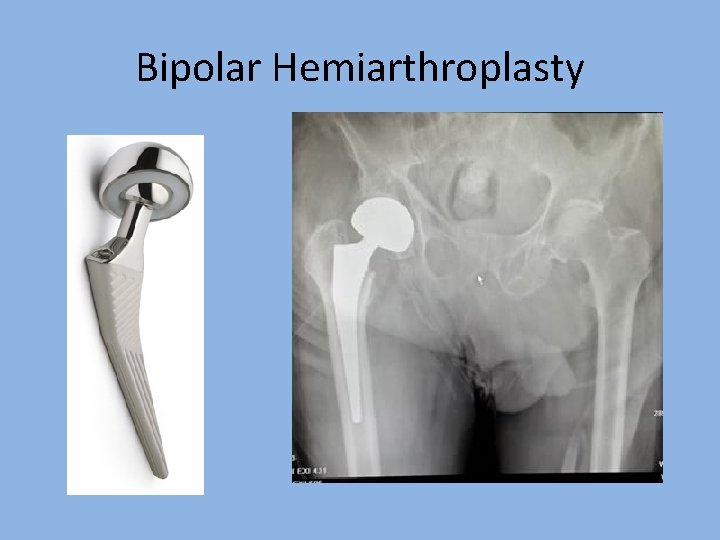
Bipolar Hemiarthroplasty
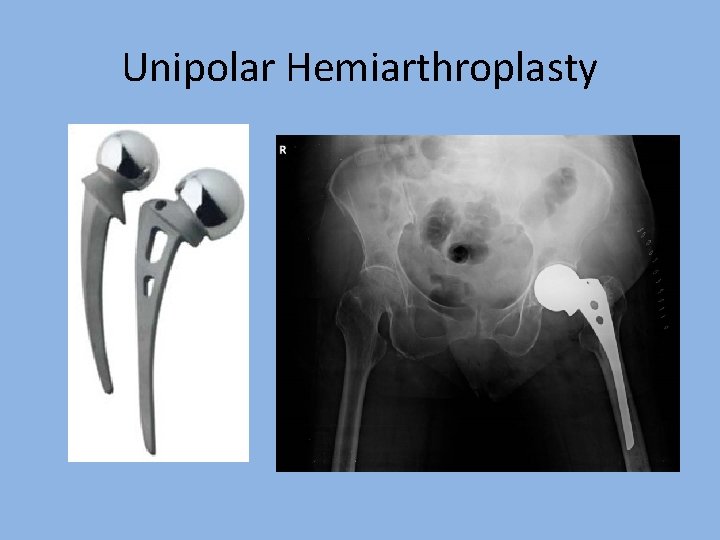
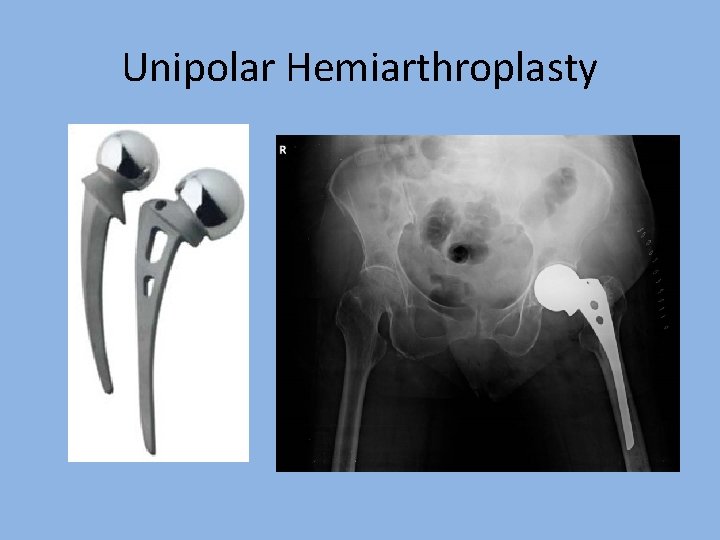
Unipolar Hemiarthroplasty

Hip resurfacing
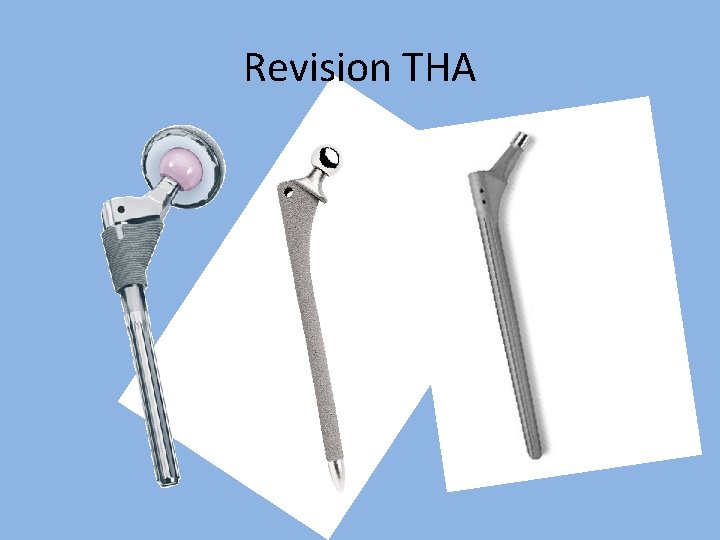
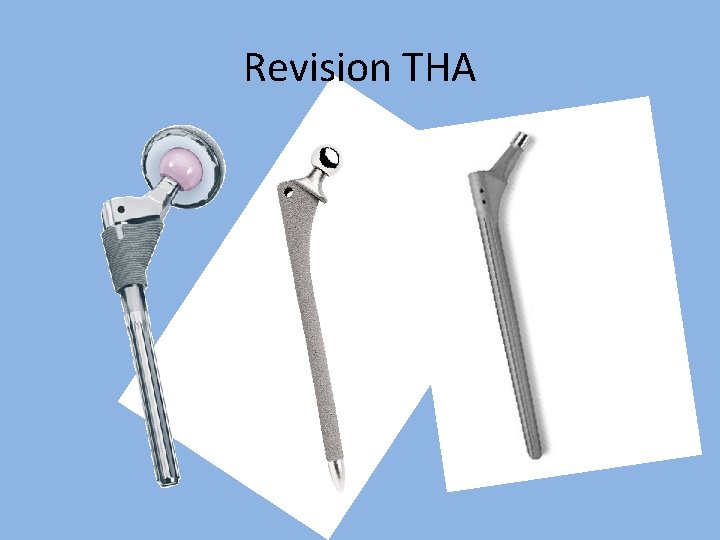
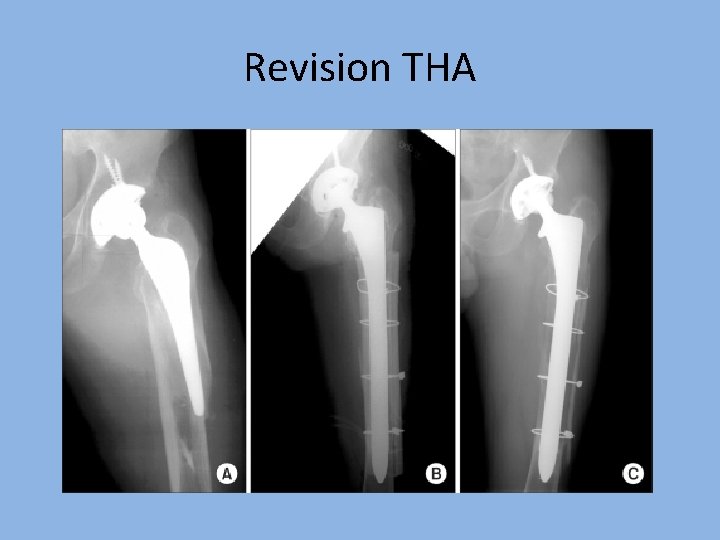
Revision THA
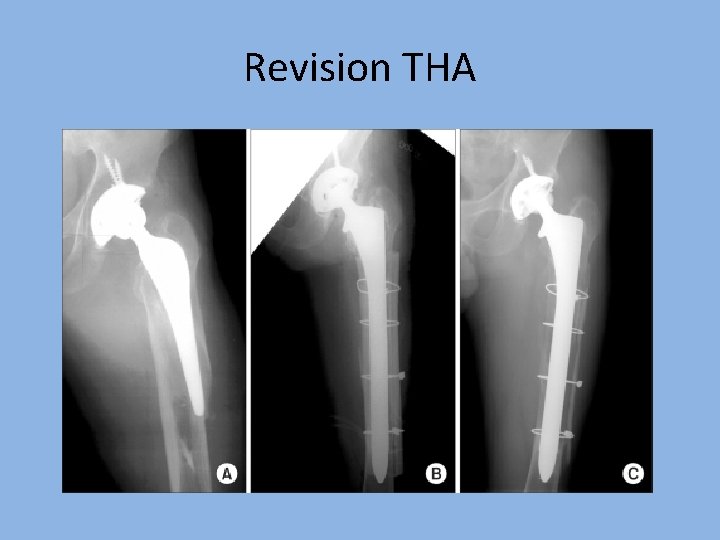
Revision THA

Why do we have to do a hip arthroplasty?
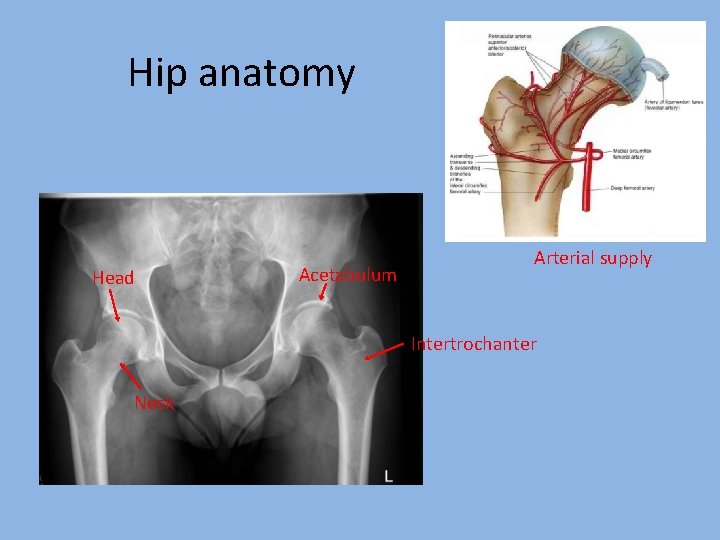
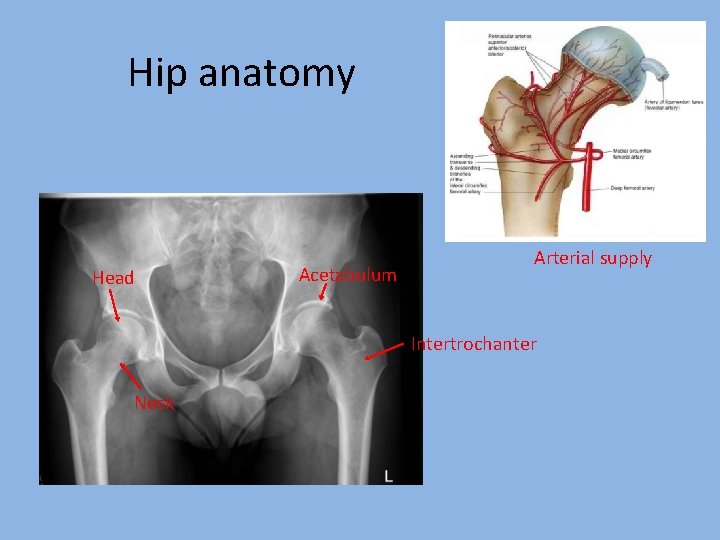
Hip anatomy Head Acetabulum Arterial supply Intertrochanter Neck
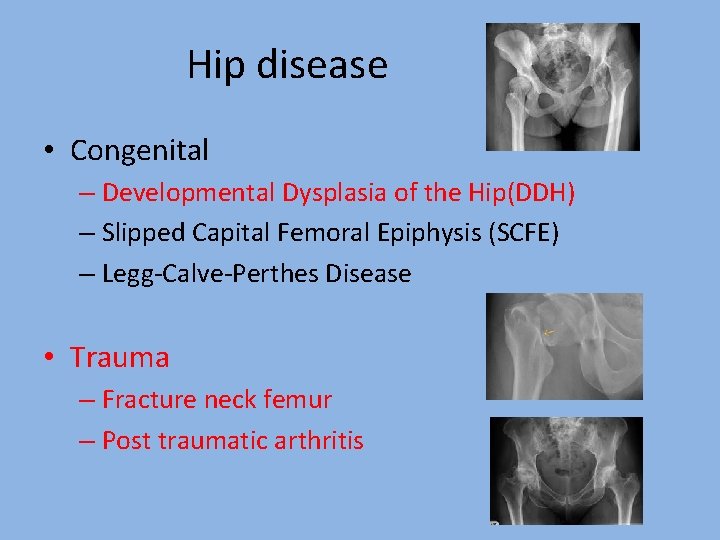
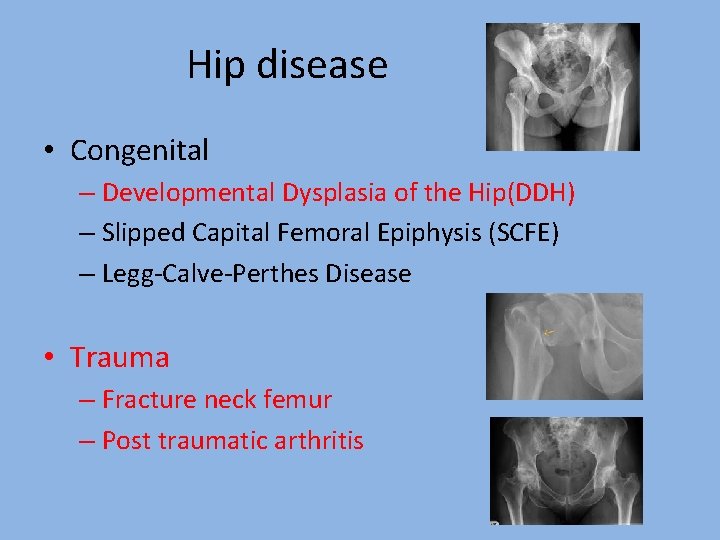
Hip disease • Congenital – Developmental Dysplasia of the Hip(DDH) – Slipped Capital Femoral Epiphysis (SCFE) – Legg-Calve-Perthes Disease • Trauma – Fracture neck femur – Post traumatic arthritis
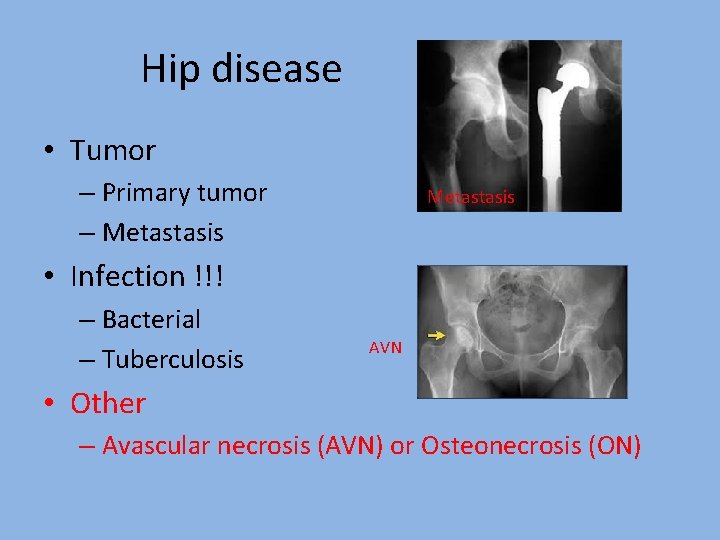
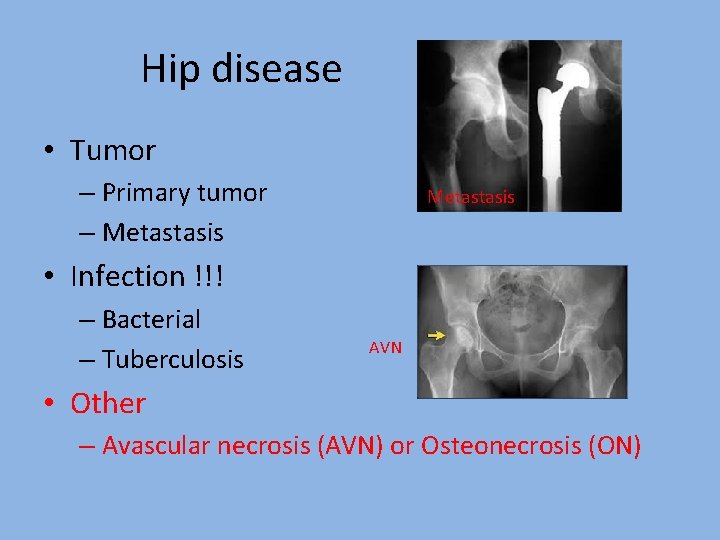
Hip disease • Tumor – Primary tumor – Metastasis • Infection !!! – Bacterial – Tuberculosis AVN • Other – Avascular necrosis (AVN) or Osteonecrosis (ON)
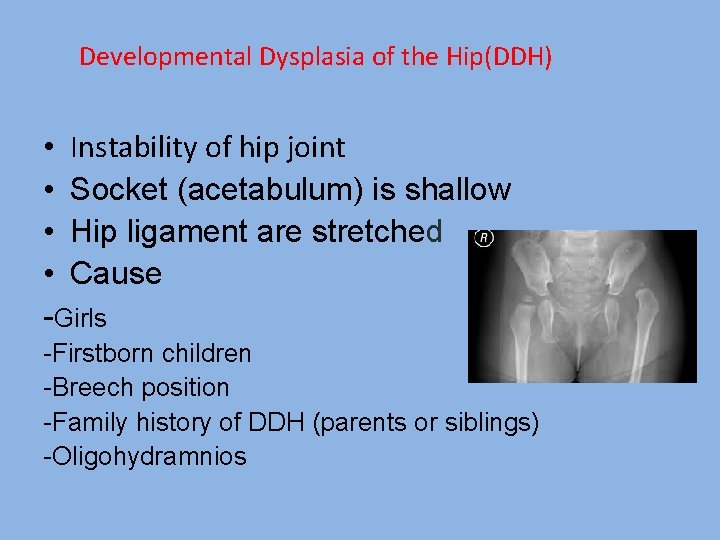
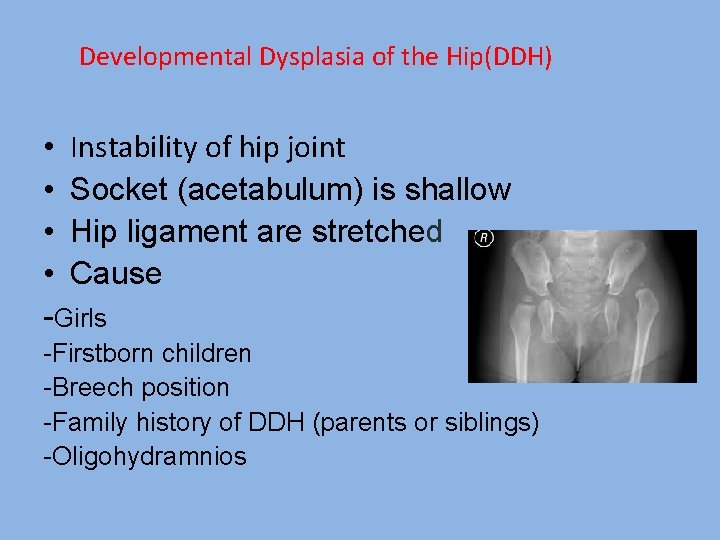
Developmental Dysplasia of the Hip(DDH) • Instability of hip joint • Socket (acetabulum) is shallow • Hip ligament are stretched • Cause -Girls -Firstborn children -Breech position -Family history of DDH (parents or siblings) -Oligohydramnios

Developmental Dysplasia of the Hip(DDH) • Symptoms -Legs of different lengths -Limping, waddling gait • Treatment -Pavlik harness (1 -2 M)=<6 M -Closed reduction and spica casting=6 M-2 Yrs -Open surgery=Failure close reduction, >2 Yrs • Complications -osteoarthritis by early adulthood
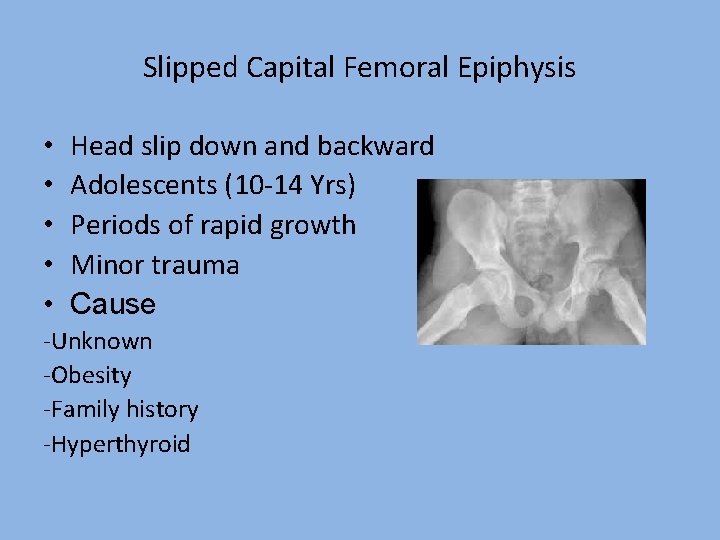
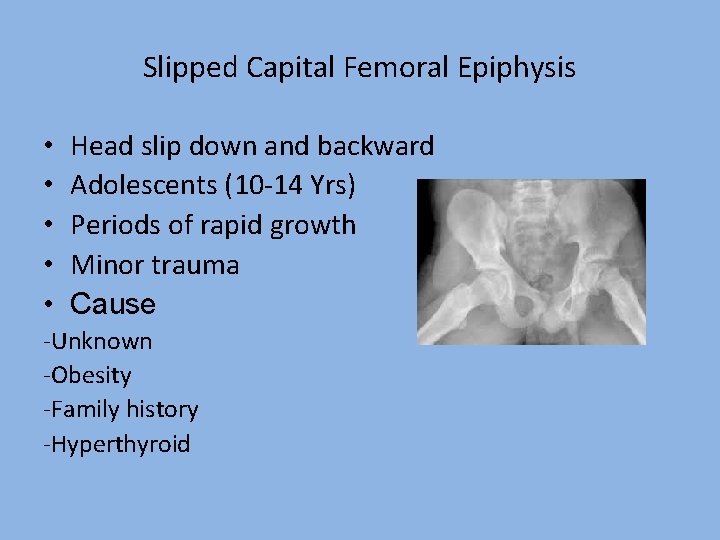
Slipped Capital Femoral Epiphysis • • • Head slip down and backward Adolescents (10 -14 Yrs) Periods of rapid growth Minor trauma Cause -Unknown -Obesity -Family history -Hyperthyroid

Slipped Capital Femoral Epiphysis • Symptoms -intermittent pain in hip-Stable -Inability to walk, Outward &Shorted leg-Unstable • Treatment -Surgery-Screw fixation • Complications -Avascular necrosis -Chondrolysis
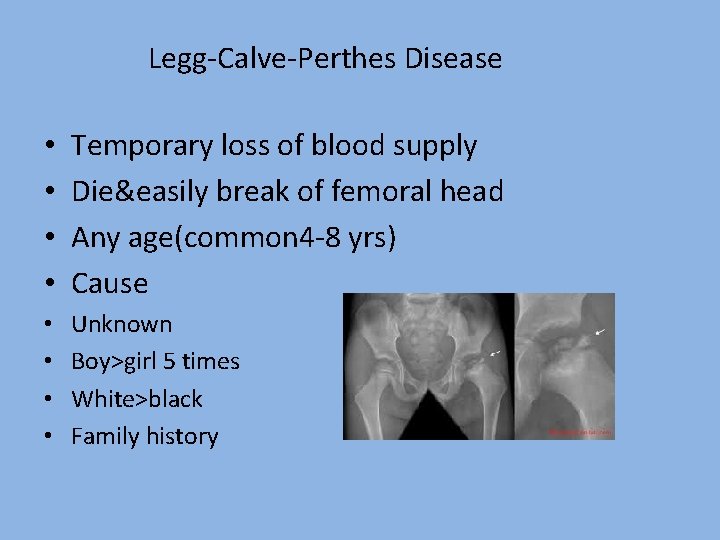
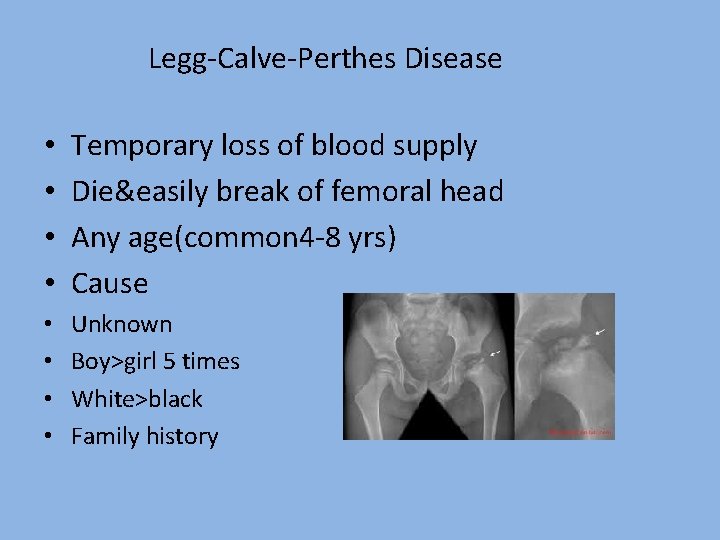
Legg-Calve-Perthes Disease • • Temporary loss of blood supply Die&easily break of femoral head Any age(common 4 -8 yrs) Cause • • Unknown Boy>girl 5 times White>black Family history

Legg-Calve-Perthes Disease • Symptoms -Pain or stiffness in the hip -Limping gait • Treatment -Physical therapy, Traction, Cast=<6 yrs -Surgery= > 6 yrs • Complications -Osteoarthritis in adulthood(Rx >6 Yrs)

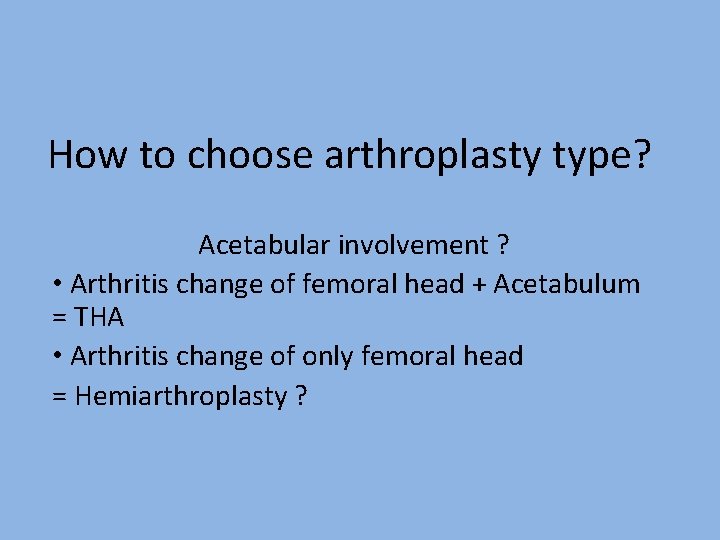
How to choose arthroplasty type? Acetabular involvement ? • Arthritis change of femoral head + Acetabulum = THA • Arthritis change of only femoral head = Hemiarthroplasty ?
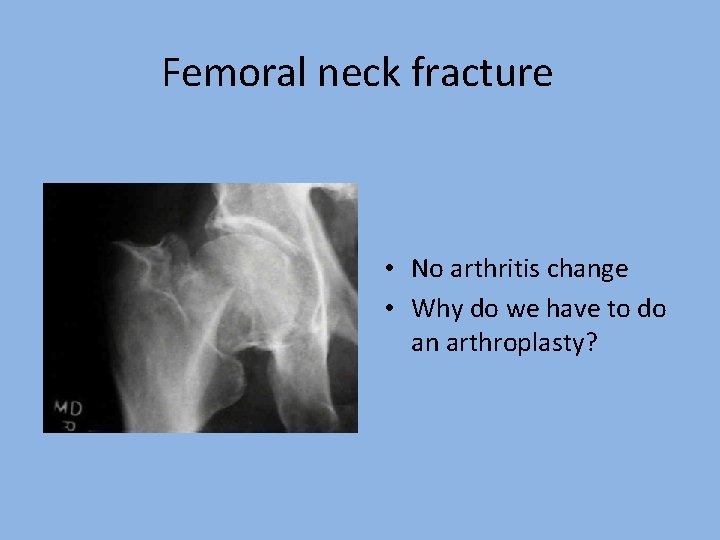
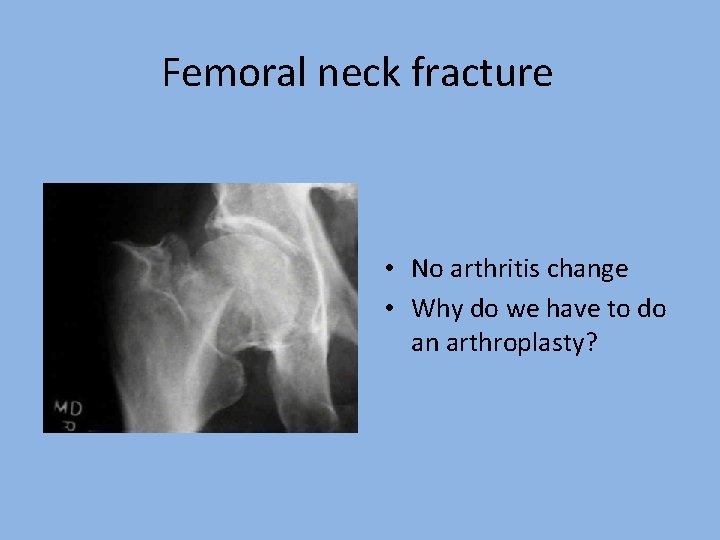
Femoral neck fracture • No arthritis change • Why do we have to do an arthroplasty?
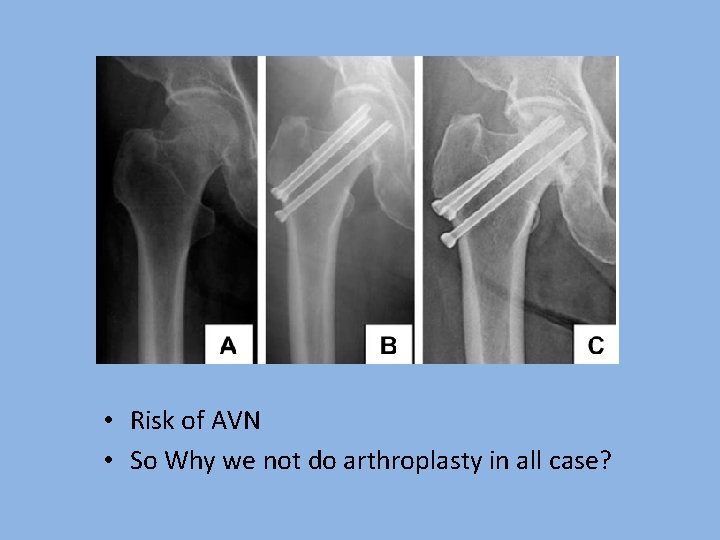
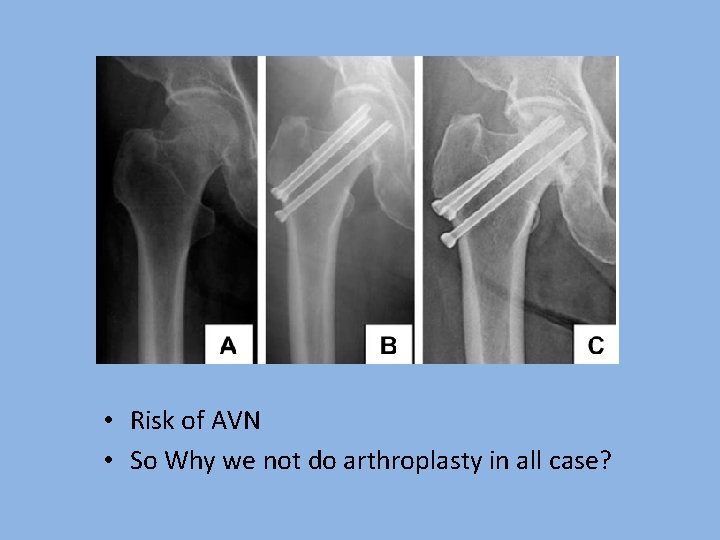
• Risk of AVN • So Why we not do arthroplasty in all case?
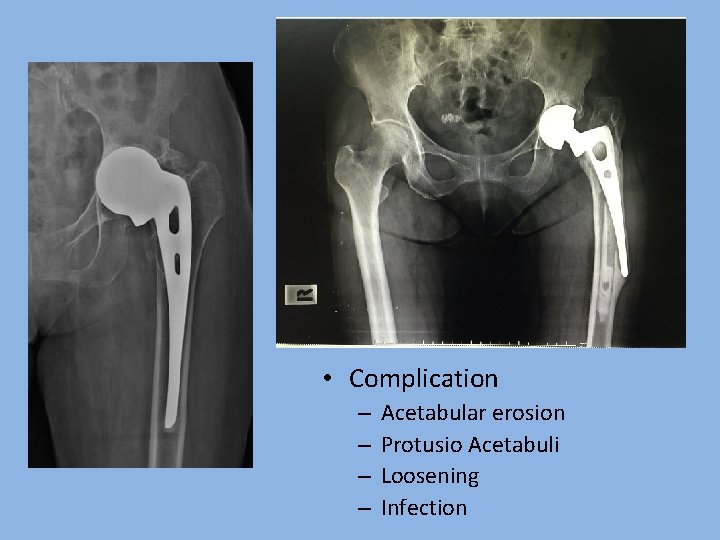
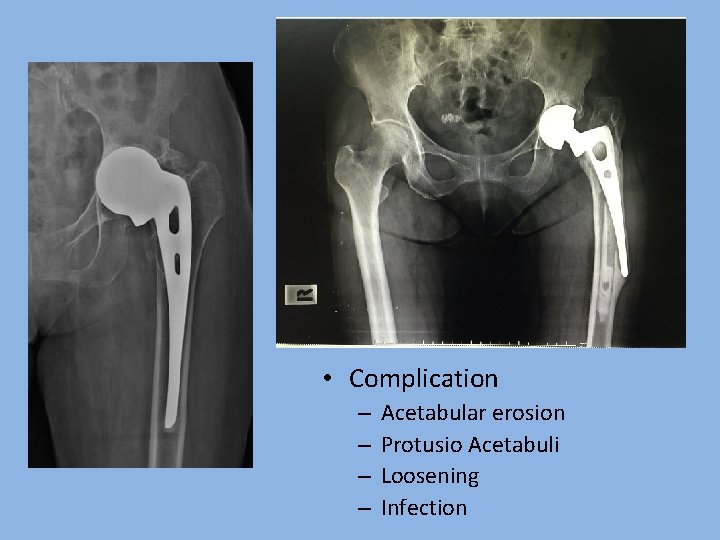
• Complication – – Acetabular erosion Protusio Acetabuli Loosening Infection
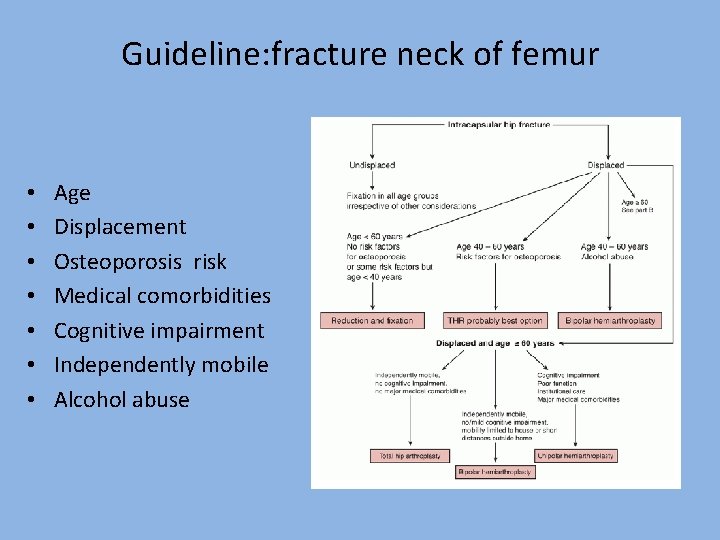
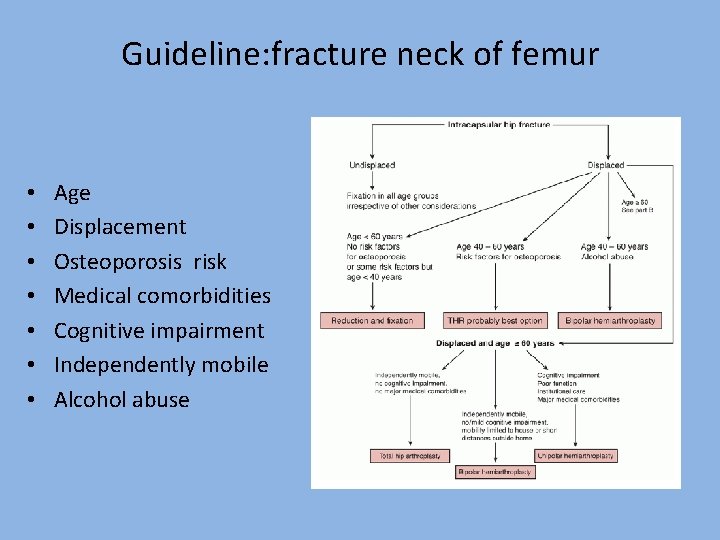
Guideline: fracture neck of femur • • Age Displacement Osteoporosis risk Medical comorbidities Cognitive impairment Independently mobile Alcohol abuse

How do we choose Bipolar or Unipolar?
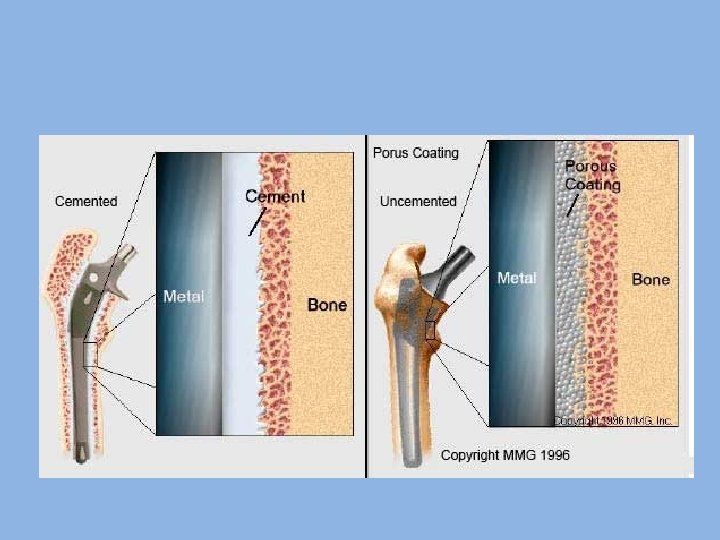
Type of prosthesis fixation • Cemented • Cementless • Hybrid – Cementless acetabulum – Cemented femoral stem
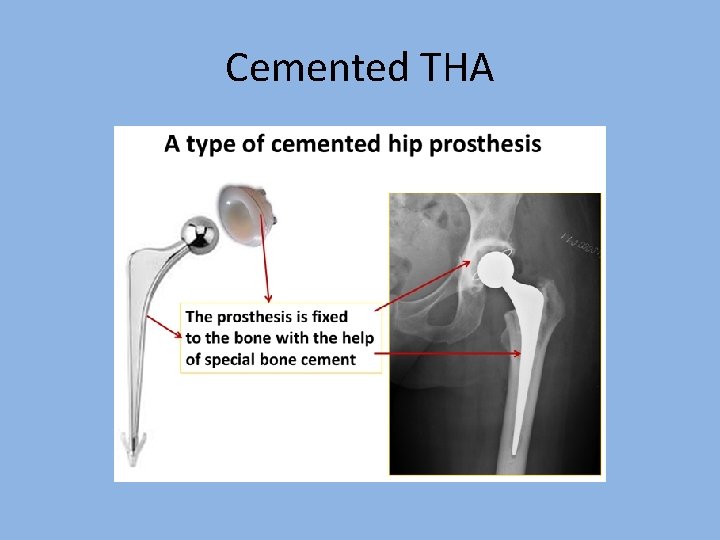
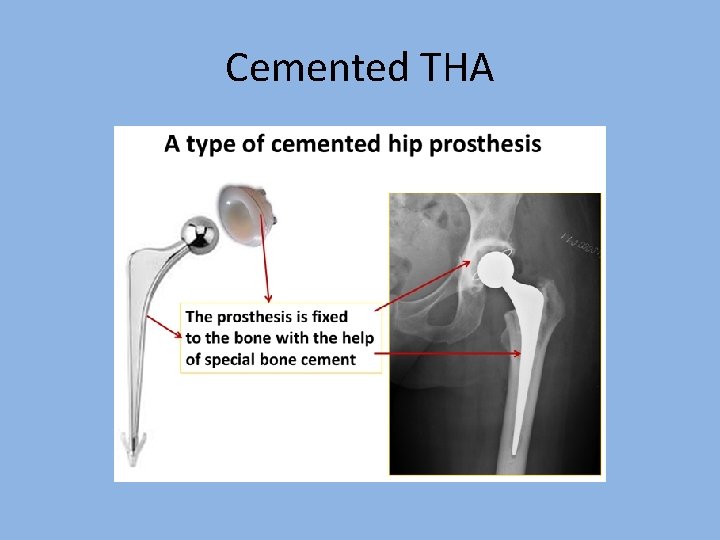
Cemented THA

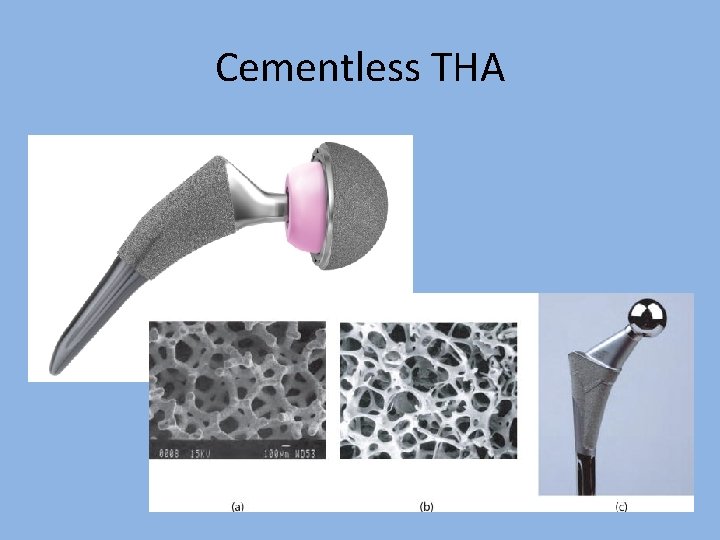
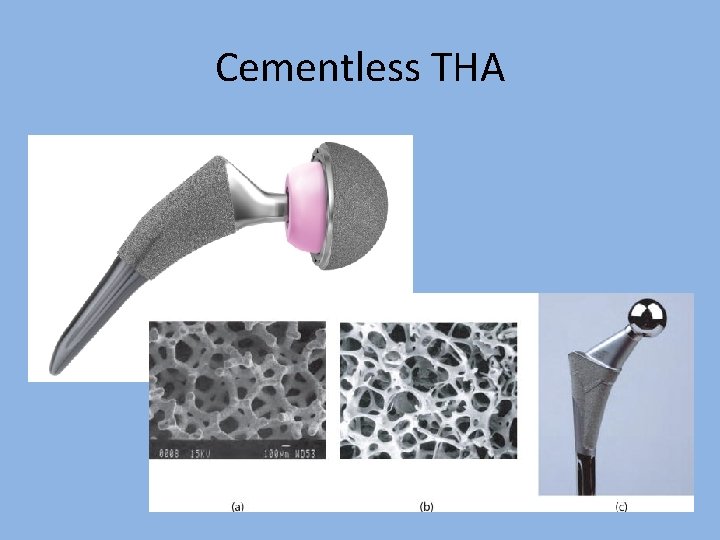
Cementless THA
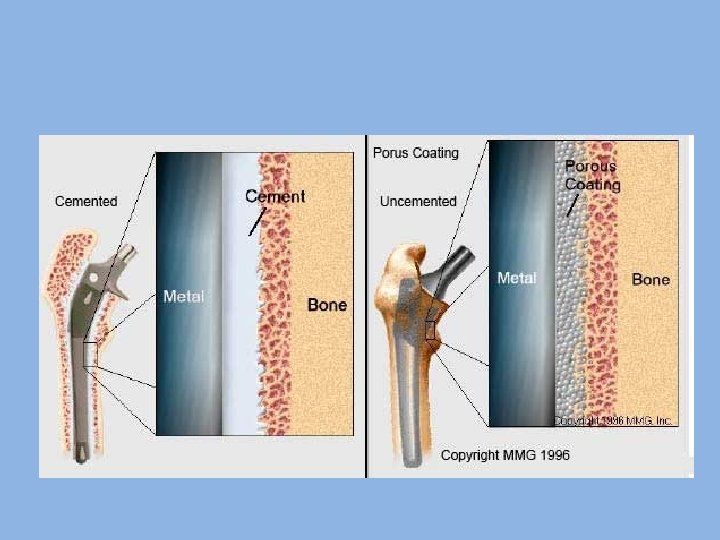
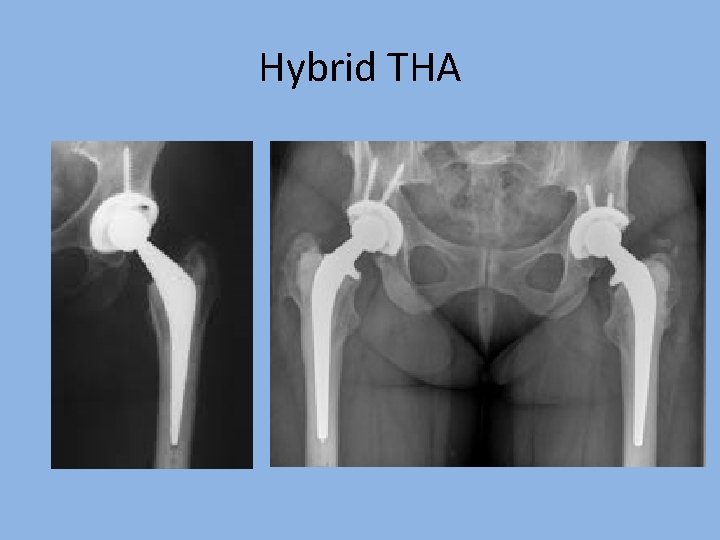
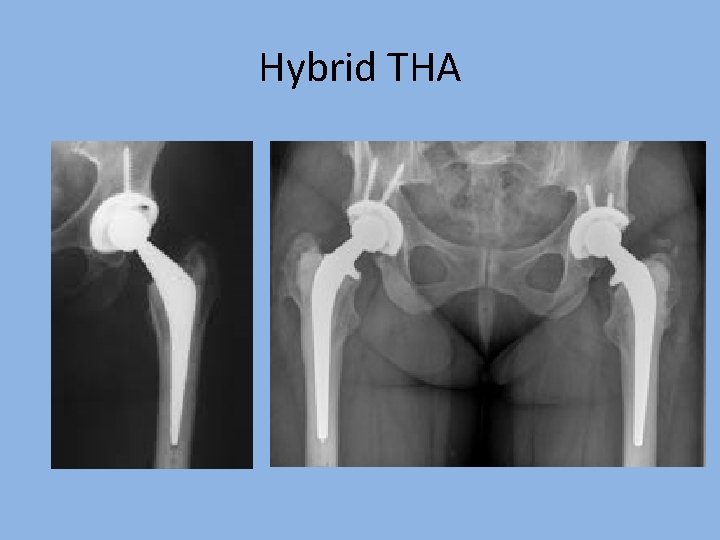
Hybrid THA
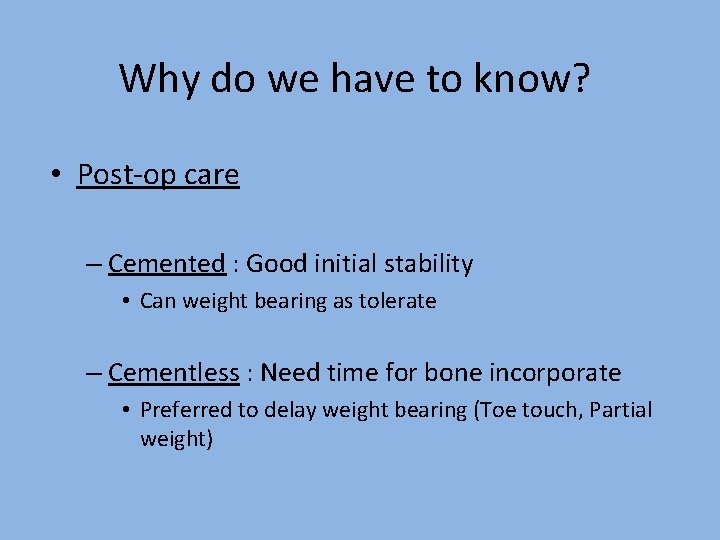
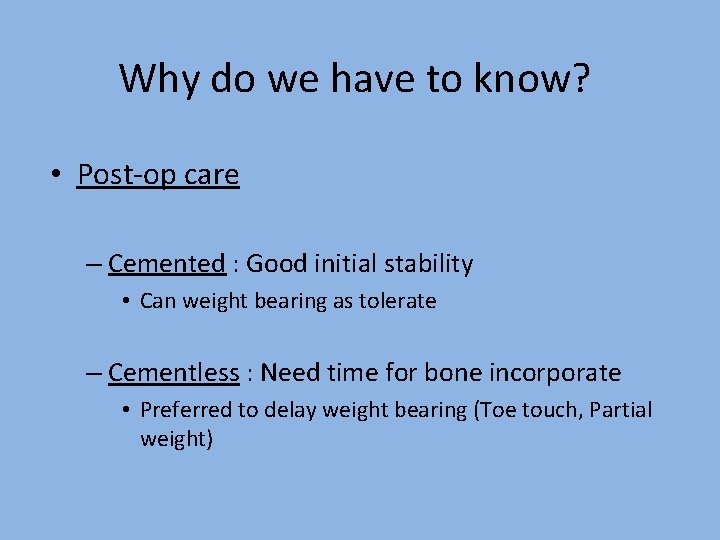
Why do we have to know? • Post-op care – Cemented : Good initial stability • Can weight bearing as tolerate – Cementless : Need time for bone incorporate • Preferred to delay weight bearing (Toe touch, Partial weight)
Why not we all do cemented?

Result of Cemented Cup • Clohisy JC matched-pair study of primary THA • 45 all-polyethylene & 45 cementless • Follow up 9 -12 years • Cemented 1 revision from loosening 31% were radiographically loose • Cemenless cup : No radiographic looseing. Clohisy JC, Harris WH. Matched-pair analysis of cemented and cementless acetabular reconstruction in primary total hip arthroplasty. J Arthroplasty. 2001 Sep; 16(6): 697 -705.

Result of cemented cup • Hartofilakidis compared • 50 cemented all-polyethylene & 51 cementless cup • Follow-up 10 year • revision rate for aseptic loosening - 28% for the cemented cup -12% for the cementless cup Hartofilakidis G. A comparison of the outcome of cemented all-polyethylene and cementless metal-backed acetabular sockets in primary total hip arthroplasty. J Arthroplasty. 2009 Feb; 24)2: (217 -25.
So nowadays Cemented THA are not routinely done How about Cemented stem?

Results of cemented stem • First generation cementing technique Stauffer RN, J Bone Joint Surg(Am), 1982, 983 -90 – Aseptic loosening of femoral component in 231 hips • 24% for 5 yrs • 29. 9% for 10 yrs

Contemporary cementing technique Link R. Technique in orthopaedics 1991; 34 -9 • • Distal plug, distal centralizer Manual mixing cement (60 beats per minute) Retrograde insertion Pressurization

Results • Contemporary cementing technique Williams HD. J Bonr Joint Surg(Br). 2002; 324 -34 • Exeter university stem • 325 hips, means 8. 9 yrs follow up • Revision from aseptic loosening of femoral component - 0%
Results • Contemporary cementing technique Yate PJ. J Bone Joint Surg(Br), 2008; 16 -22 – – – 191 hips Collarless polished double-taper design Means F/U 11. 08 yrs Revision from aseptic loosening femoral component -0% Subsidence • 1 st year subsidence 0. 8 mm • Total subsidence 1. 95 mm • Overall subsidence 0. 18 mm/yrs
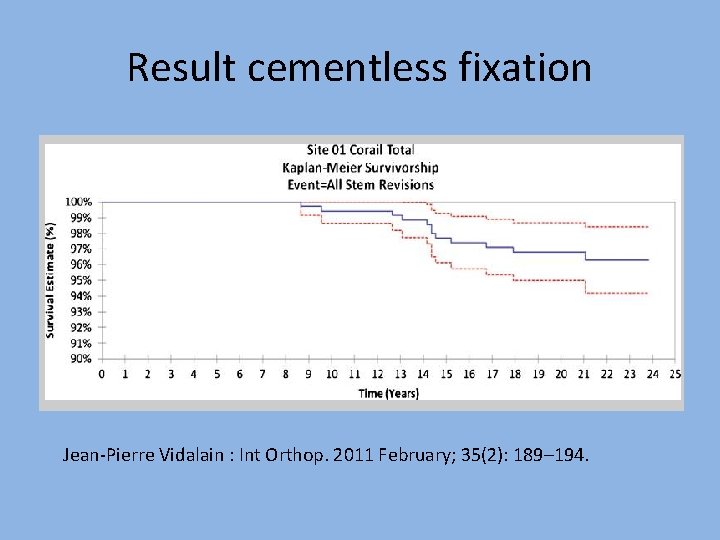
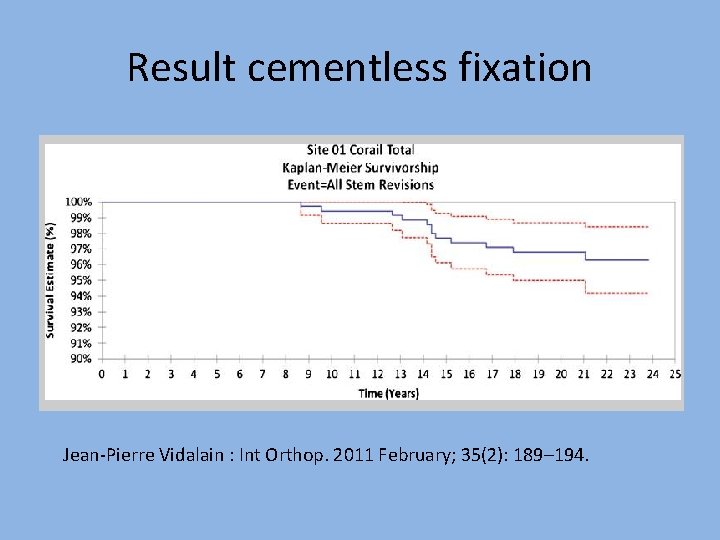
Result cementless fixation Jean-Pierre Vidalain : Int Orthop. 2011 February; 35(2): 189– 194.
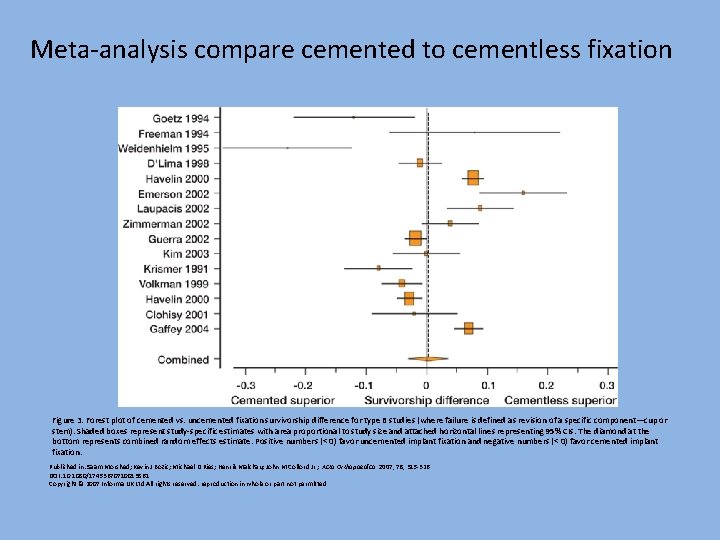
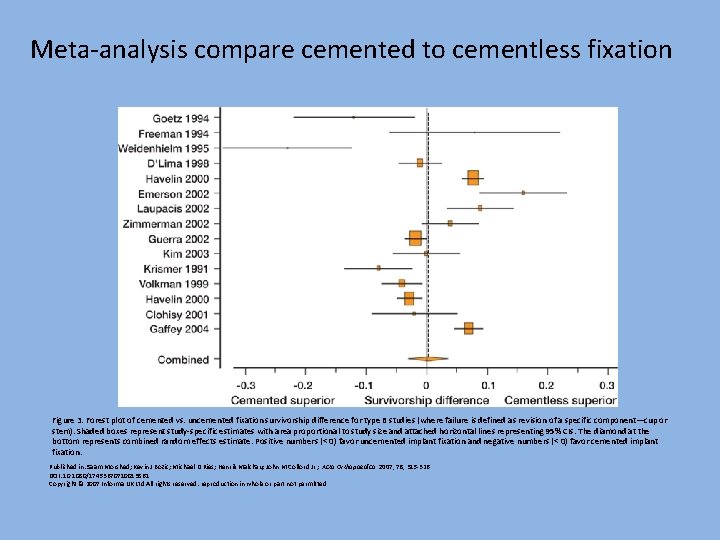
Meta-analysis compare cemented to cementless fixation Figure 3. Forest plot of cemented vs. uncemented fixation survivorship difference for type B studies (where failure is defined as revision of a specific component—cup or stem). Shaded boxes represent study-specific estimates with area proportional to study size and attached horizontal lines representing 95% CIs. The diamond at the bottom represents combined random effects estimate. Positive numbers (< 0) favor uncemented implant fixation and negative numbers (< 0) favor cemented implant fixation. Published in: Saam Morshed; Kevin J Bozic; Michael D Ries; Henrik Malchau; John M Colford Jr. ; Acta Orthopaedica 2007, 78, 315 -326. DOI: 10. 1080/17453670710013861 Copyright © 2007 Informa UK Ltd All rights reserved: reproduction in whole or part not permitted

So not much different How can we choose Cementless THA or Hybrid?

How can we choose Cementless THA or Hybrid?
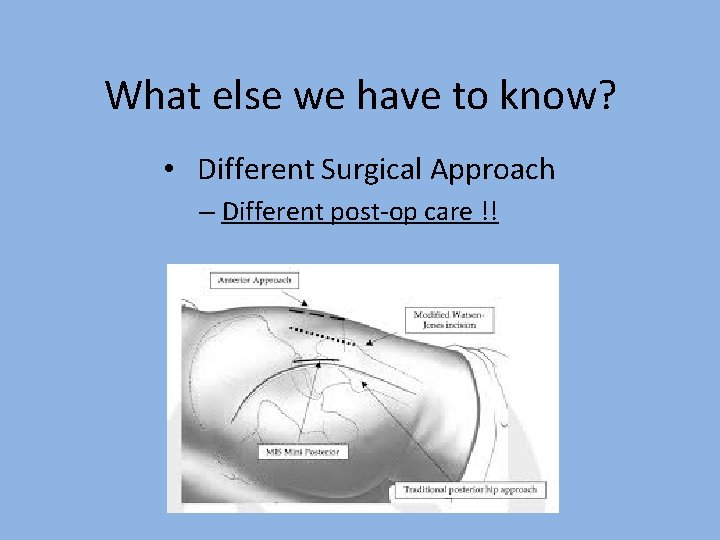
What else we have to know? • Different Surgical Approach – Different post-op care !!
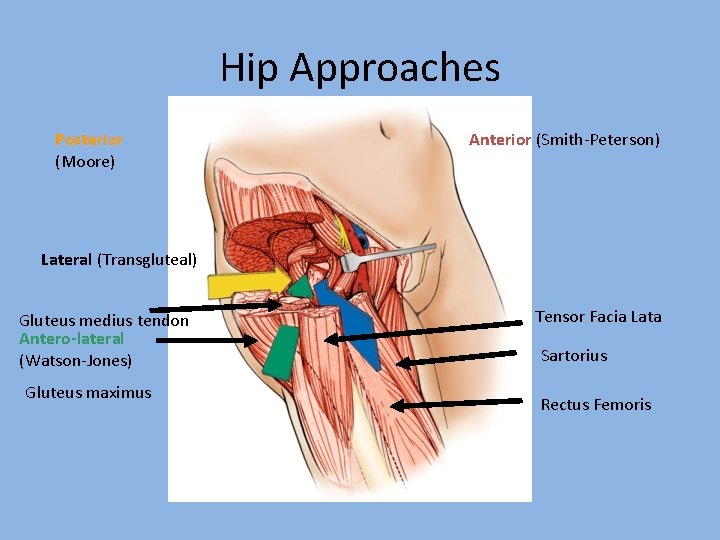
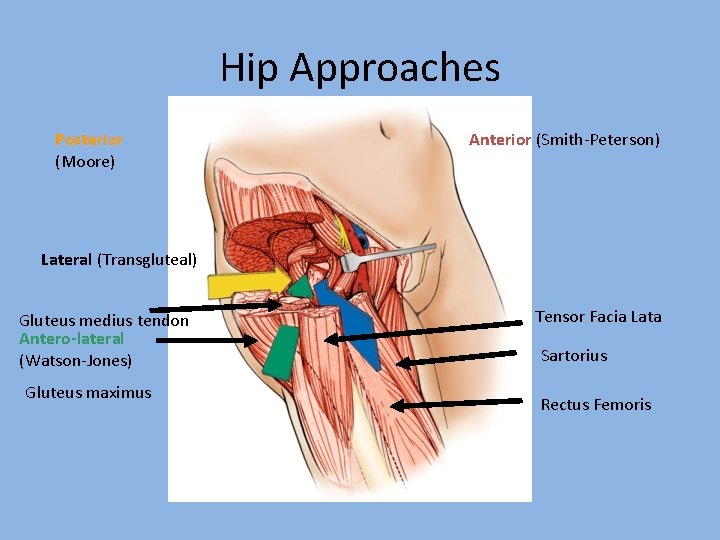
Hip Approaches Posterior (Moore) Anterior (Smith-Peterson) Lateral (Transgluteal) Gluteus medius tendon Antero-lateral (Watson-Jones) Gluteus maximus Tensor Facia Lata Sartorius Rectus Femoris

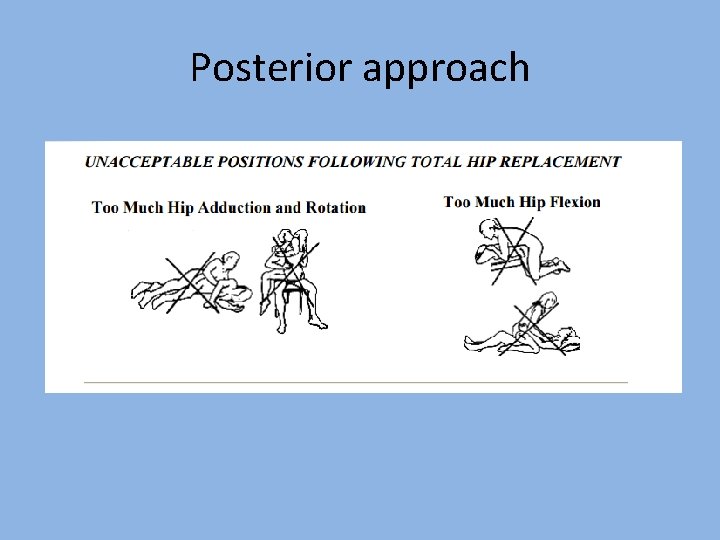
Posterior approach • • Moore approach Most popular High risk of dislocation Post-op education is important*

Posterior approach • Precautions for the first 6 weeks – – – Should not bend your hip beyond 90° Should not bring your legs or knees together Use a pillow between your legs in bed Do not rotate your operative leg inward Use a reacher to pick objects off the floor ไมถก ถกตอง
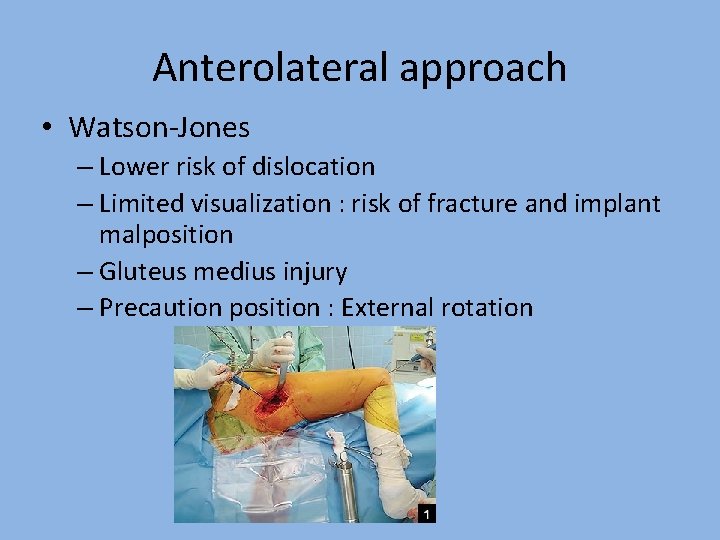
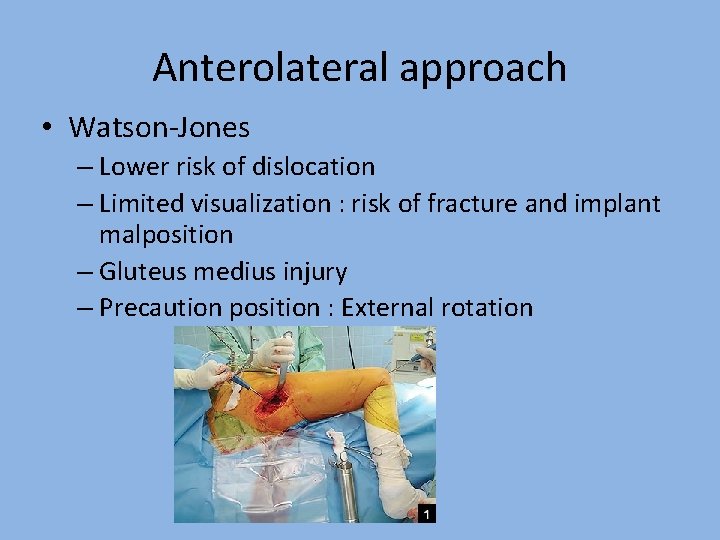
Anterolateral approach • Watson-Jones – Lower risk of dislocation – Limited visualization : risk of fracture and implant malposition – Gluteus medius injury – Precaution position : External rotation
Anterior approach • • Smith-Peterson Trendy Intermuscular-Internervous plain Low risk of dislocation
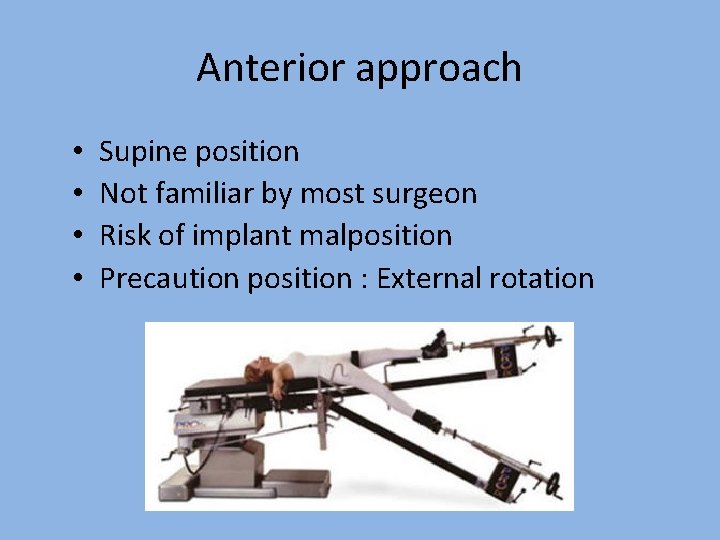
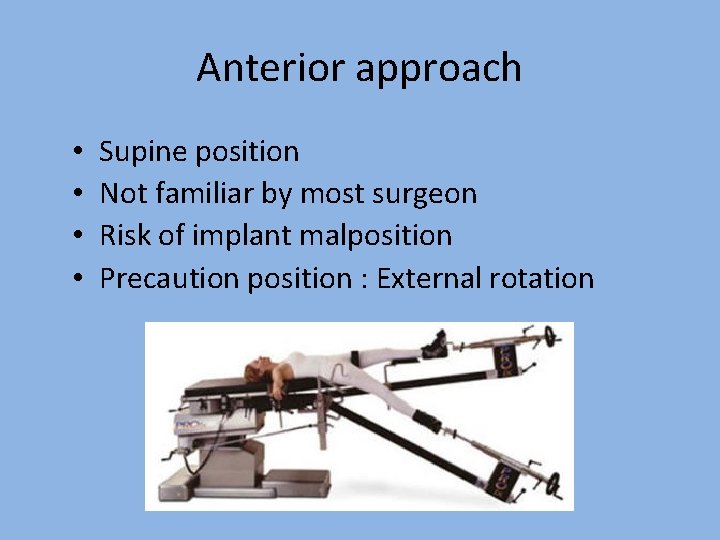
Anterior approach • • Supine position Not familiar by most surgeon Risk of implant malposition Precaution position : External rotation
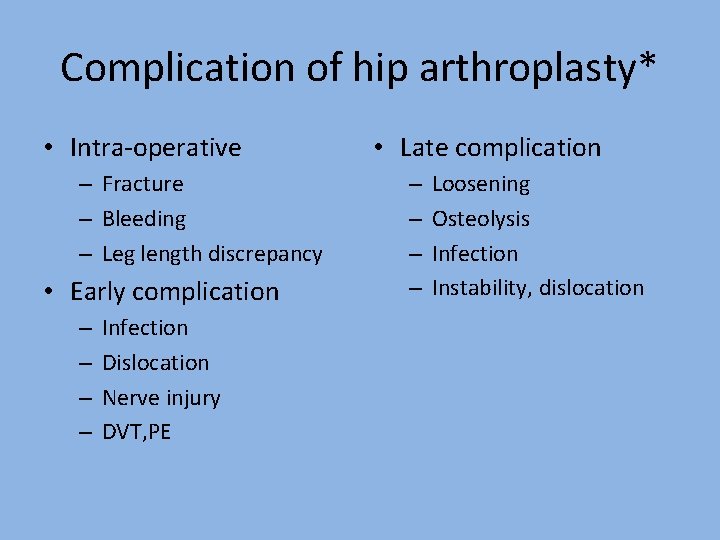
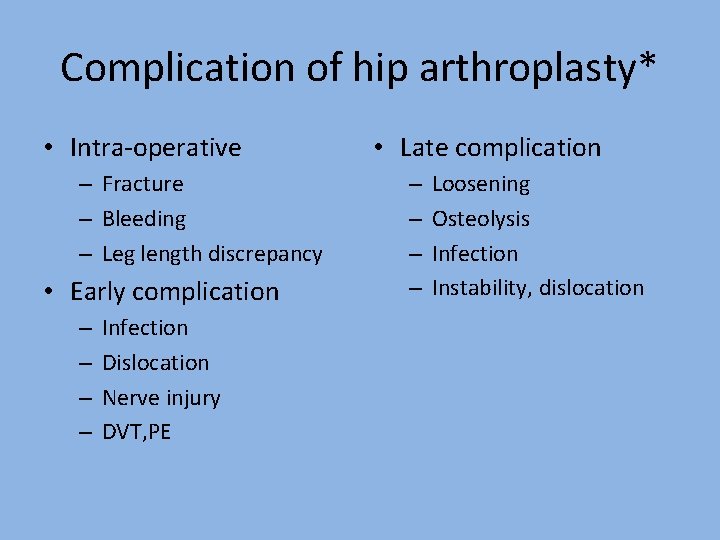
Complication of hip arthroplasty* • Intra-operative – Fracture – Bleeding – Leg length discrepancy • Early complication – – Infection Dislocation Nerve injury DVT, PE • Late complication – – Loosening Osteolysis Infection Instability, dislocation

Posterior approach
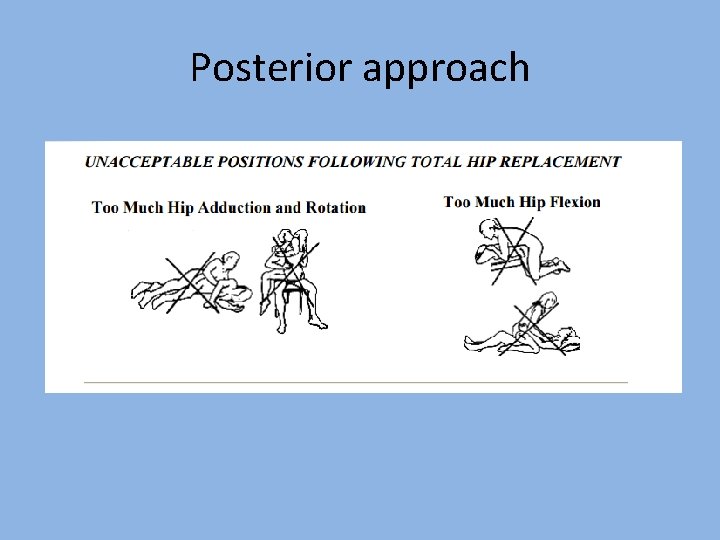
Posterior approach


Thank you
 Arthroplasty practitioner
Arthroplasty practitioner Occupational therapy intervention plan for hip arthroplasty
Occupational therapy intervention plan for hip arthroplasty Arthropoda insecta
Arthropoda insecta Arthros means
Arthros means Longtoptumor
Longtoptumor Tunnel prep
Tunnel prep Furcation plasty procedure
Furcation plasty procedure Plasty artinya
Plasty artinya Plasty a syntetické vlákna
Plasty a syntetické vlákna Plasty
Plasty Liten mb71
Liten mb71 Plasty
Plasty Mosaic plasty
Mosaic plasty Neuroplasty meaning
Neuroplasty meaning Cephalohematoma vs caput succedaneum
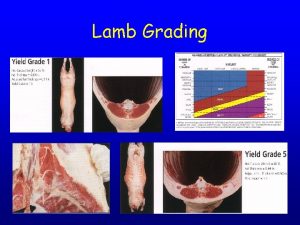
Cephalohematoma vs caput succedaneum Lamb grading
Lamb grading Costotransverse ligament
Costotransverse ligament Which joint is permanent type
Which joint is permanent type Joint venture account is a
Joint venture account is a Lamb carcass grading
Lamb carcass grading Plane joint
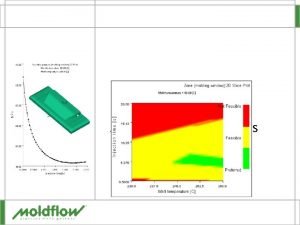
Plane joint Injection molding indiana
Injection molding indiana Light resin transfer molding
Light resin transfer molding Disadvantages of structural foam molding
Disadvantages of structural foam molding Phenolic molding compound
Phenolic molding compound Molding personality meaning
Molding personality meaning Cold slug in injection molding
Cold slug in injection molding Extrusion molding process
Extrusion molding process Erp software for plastic injection molding
Erp software for plastic injection molding Rotational molding design guidelines
Rotational molding design guidelines Black spots of plastic injection molded parts
Black spots of plastic injection molded parts Molding defect
Molding defect Indirect tooling
Indirect tooling Injection machine
Injection machine Husky injection molding investor relations
Husky injection molding investor relations Rotational molding speed ratio
Rotational molding speed ratio Injection molding
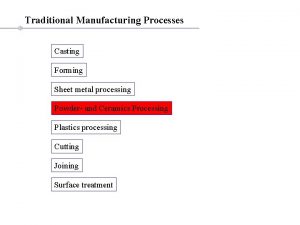
Injection molding Sand casting sand types
Sand casting sand types Advantages of injection stretch blow moulding
Advantages of injection stretch blow moulding Outsert molding
Outsert molding Cold slug well injection molding
Cold slug well injection molding Diaphragms pronunciation
Diaphragms pronunciation Distolingual molding
Distolingual molding Stretch blow molding training
Stretch blow molding training Fetal skull
Fetal skull Molding of fetal skull
Molding of fetal skull Injection molding
Injection molding Greek word for plastic
Greek word for plastic Suppository semi solid
Suppository semi solid Rotational molding advantages and disadvantages
Rotational molding advantages and disadvantages Reinforced reaction injection molding
Reinforced reaction injection molding Blow molding process steps
Blow molding process steps Injection molding
Injection molding Aim injection molding
Aim injection molding Blow moulding advantages
Blow moulding advantages How to calculate projected area injection molding
How to calculate projected area injection molding Multi colour injection moulding
Multi colour injection moulding Cocoa butter is example of which base
Cocoa butter is example of which base Evaluation of suppositories
Evaluation of suppositories Types of bases in suppositories
Types of bases in suppositories Microcellular injection molding
Microcellular injection molding Resin casting small metal parts
Resin casting small metal parts