FURCATION INVOLVEMENT Introduction The successful long term treatment


































































- Slides: 168

FURCATION INVOLVEMENT
Introduction The successful long term treatment of multirooted teeth with attachment loss into their furcations has been one of the greatest challenges to dentists. Due to the complex anatomy of the furcation, it is difficult to arrest the disease progression at this area. Early in the 20 th century, Leonard et al recommended extraction of teeth with furcation invasion. It is reported that furcation involvement occurs three times more frequently among maxillary than mandibular molars and that the incidence of distal furcation involvements is higher when compared to mesial furcation involvements in maxillary molars. (Ross et al 1980) Treatment of the furcation invasion can result in the long term retention of these teeth.
Terminology • Root complex is the portion of a tooth that is located apical to the CEJ. The root complex may be divided into two parts : the root trunk and the root cones • The root trunk represents the undivided region of the root. The height of the root trunk is defined as the distance between the CEJ and the separation line (furcation) between two root cones.
• The root cones (root) is included in the divided region of the root complex. Two or more root cones make up the furcation region of the root complex. • The root portion of a teeth may be single or multiple. • Teeth with multiple roots have a bifurcation in case of two roots or a trifurcation in case of three roots dividing the root portion into two or more extensions.


• The furcation is the area located between • • • individual root cones. Furcation entrance is the transitional area between the undivided and the divided parts of the root. Furcation fornix is the roof of the furcation. Degree of separation is the angle of seperation between two roots (cones). Divergence is the distance between two roots. Coefficient of separation is the length of the root cones in relation to the length of the root complex
• The term furcation involvement refers to the commonly occurring conditions in which the bifurcations and trifurcations of multirooted teeth are invaded by disease process. • The loss of periodontium in the interradicular area is referred to as a furcation invasion

Diagnosis • Careful probing- Naber’s Probe • Transgingival sounding- to define the anatomy • Radiograph


Differential diagnosis • Pulpal pathosis • Trauma from occlusion • Plaque associated lesion

Classification of Furcation Involvement A. Based on horizontal component Glickman (1953) Grade I involvement – incipient or early lesion. The pocket is suprabony, involving the soft tissue; there is slight bone loss in the furcation area. Radiographic change is not usual, as bone loss is minimal.

Grade II involvement – bone is destroyed on one or more aspects of the furcation, but a portion of the alveolar bone and periodontal ligaments remains intact permitting only partial penetration of the probe into the furcation. The lesion is a cul-de-sac Radiographs may or may not revel grade II furcation involvement

Grade III involvement – the interradicular bone is completely absent, but the facial and/or lingual orifice of the furcation are covered by the gingiva. The lesion is a through-and-through tunnel. Radiolucent area between roots on radiograph.
Grade IV involvement – the intraradicular bone is completely destroyed, the gingiva is apically positioned, resulting in clinically visible furcation opening.
Hamp, Nyman, Lindhe (1975) Devised a classification into three degrees based on horizontal depth to delineate the depth of Glickman’s grade II furcation involvement Degree I : horizontal loss of periodontal tissue support less than 3 mm Degree II : horizontal loss of periodontal support exceeding 3 mm but not encompassing the total width of the furcation area Degree III : horizontal through-and-through destruction of the periodontal tissue in the furcation

Lindhe (1983) Grade I (initial) –loss of interradicular bone less than or equal to one-third. Grade II (partial) – loss of interradicular bone greater than one-third but not through and through. Grade III (total) – through and through loss of interradicular bone.


Fedi (1985) • Merged Glickman’s and Hamp’s classification into one ØGrade II v. Degree I : horizontal depth < 3 mm v. Degree II : horizontal depth > 3 mm ØGrade III ØGrade IV
B. Based on vertical component Tarnow and Fletcher (1984) (depending on the distance from the bottom of the defect to the roof of the furcation) • Subgroup A- 0 -3 mm • Subgroup B- 4 -7 mm • Subgroup C- 7 mm or more. ØVertical component has more influence on the prognosis of a teeth than the horizontal component.
Eskow and Kapin (1984) • Classified vertical bone loss in thirds of the interradicular loss. Subclass A : vertical destruction to one third of total interradicular height Subclass B : reaching two thirds Subclass C: interradicular osseous destruction into or beyond the apical third.
C. Based on the presence or absence of complex anatomical features of the furcation Useful for Grade II involvement Subclassificated as • Good • Fair • Poor prognosis for regeneration
D. Descriptive classification Goldman and Cohen (1968) Grade I – incipient Grade II – cul-de-sac Grade III- through and through
Ricchetti 1982 • Proposed a linear classification that provides horizontal and vertical measurements and establishes a meaningful clinical tool to determine treatment approach
• Class I : 1 mm of horizontal measurement- the root furrow • Class II a : 1 -2 mm of horizontal invasion – earliest damage R • Will respond to pocket elimination treatment on both the buccal and lingual surface. • Tooth preparation in the form of odontoplasty to eliminate the dentinal hood over the furcation and provide a smooth surface
• Class II : 2 -4 mm of horizontal invasion R • Observe or perform odontoplasty. • Class II a : 4 -6 mm of horizontal invasion R • Observe, section or attempt regeneration
• Class III : more than 6 mm of horizontal invasion. ( Denotes furcal invasion half the distance from the buccal surface to the lingual surface) R • Too deep to resolve by odontoplasty and must be considered a candidate for periodontal regeneration , maintained as is, or hemisection.
Furcations are normally classified by including the horizontal as well as vertical component • IA, IB, IC • IIA, IIB, IIC • IIIA, IIIB, IIIC • IVA, IVB, IVC ØThese sub classifications aid in prognosis and treatment planning

Etiologic Factors Primary etiologic factor • Bacterial plaque and the inflammatory consequences. Ø It results in destruction of collagen fiber attachment of the gingiva and bone to cementum of the tooth root. (Page 1976) Ø Glickman(1950) showed that furcation invasions are a phase in the rootward extension of periodontal pockets in the region of furcations, when attachment loss progress apically on the furcal surface.
Pathogenesis • Bacterial plaque host defence system. • Results in signs of inflammation. • Increase in number of Leukocytes in gingival sulcus. • Proteases released from bacteria and neutrophils destroy collagen and other components of perivascular extracellular matrix. • Stimulates coronal cell of junctional epithelium to proliferate, as plaque extends apically, resulting in gingival pocket.
• Later lymphocytes infiltrate and the lesion is • • dominated by B cells , T cells , macrophages and neutrophils which become activated, if plaque is not removed. They secrete cytokines, produce antibody producing antibody, prosthoglandins and MMP , which are capable of altering the environment to favor collagen degradation. As disease worsens, periodontal pocket deepens, the component of extracellular matrix of the gingiva and periodontal ligament are destroyed and alveolar bone is resorbed.

Predisposing Cofactors • Trauma from occlusion ØIn absence of inflammation the lesion of trauma of occlusion does not initiate attachment loss with deepening of sulcus (Wentz 1952). ØWhen inflammation has progressed extensively, areas subjected to trauma from occlusion, show more loss of connective tissue (Lindhe 1974).
• Cervical enamel projection ØAs connective tissue does not attach to enamel a long junctional epithelium on a grade II or III CEP would extend into a furcation. ØThis long junctional epithelium is more susceptible to breakdown and rapid pocket formation in presence of active inflammation. (Barrington 1981)
• Pulpal periodontal disease ØPresence of patent accessory canals opening into the furcations of molar teeth suggests that pulpal disease could be an initiating cofactor in the development of furcation invasion (Gutmann 1978) ØIn the absence of periodontal furcation involvement, these pulpal lesions are initially pure endodontic sinus tracts draining , through the periodontal ligament and gingival sulcus (Simon 1972)

ØEarly treatment of the pulpal lesion , results in resolution of the furcation defect with regeneration of new interfurcation bone and attachment. ØIf furcation invasion progresses to a combined endodontic- periodontic defect, the prognosis for complete resolution is poor (Simon 1972). ØUsual sequence of treatment in a non-vital teeth is first endodontic treatment followed by periodontal surgery after 6 months if necessary, to allow for healing of the hard and soft tissue defects caused by endodontic lesion.

• Iatrogenic predisposing cofactors üIsolated furcation invasion caused by therapist themselves. v. Overhanging restoration v. Pin and endodontic perforation into furcations ØHarbor plaque , initiate periodontal inflammation and attachment loss. (Lang 1983)

• Root fractures involving furcations ØRapid , localized alveolar bone loss is often seen in the furcation areas in association with vertical root fracture involving the trunk of multirooted molars. (Lommel et al 1978).
Local Factors- affect rate of plaque deposition and clinical attachment loss 1. Local anatomical factors • Root trunk length • Root morphology • Local developmental anomalies 2. Dental caries , pulpal death
Contributing Factors 1. The morphology of the affected tooth 2. The position of the tooth relative to 3. 4. 5. adjacent teeth The local anatomy of any alveolar bone The configuration of any bony defect The presence and extent of other dental disease such as caries and puplal necrosis
Local anatomic factors in treatment of furcation 1. Root trunk length • It is the distance from the CEJ to the • furcation The combination of root trunk length with number and configuration of roots affects both the ease and success of therapy

• The shorter the root trunk , the less attachment loss has to be lost before the furcation is involved. Short root trunks are more accessible to maintenance procedure following therapy Facilitate some surgical procedures • Long root trunks or fused roots may not be appropriate candidates for treatment
2. Root length • Root length is directly related to the quantity of attachment supporting the tooth. • Tooth with long root trunks and short roots -majority of support lost • Tooth with long roots and short root trunk –more readily treated as sufficient attachment remains
3. Root form • Mesial root of mandibular 1 st and 2 nd • • • molars and mesiofacial root of maxillary 1 st molar - curved to the distal in the apical third. Increased potential for root perforation during endodontics or complicate postplacement. Increased incidence of vertical root fracture. Size of the mesial radicular pulp –result in removal of majority of the portion of the tooth during preperation

4. Interradicular dimension • The degree of separation of the roots – • • important factor in treatment planing. Closely approximated /fused roots – prevent adequate instrumentation Widely separated roots presents more treatment options and are more readily treated.
5. Anatomy of the furcation Rootplaning, surgical therapy (Matia et al 1986), and periodontal maintenance complicated by • Bifurcational ridges • Concavity in the dome (Everett et al 1958) • Possible accessory canals Gutmann 1978) Odontoplasty to reduce/eliminate these ridges for optimal results



6. Cervical enamel projections (CEPs) • Reported on 8. 6% - 28. 6% of molars • (Larato et al 1975, Masters et al 1964, Tal et al 1982) Affect plaque removal, complicate scaling, and may be a local factor in the development of gingivitis and periodontitis.


Classification of CEPs based on extent (Masters and Hoskins-1964) • Grade I –a definite change in cementoenamel junction level, with enamel projecting towards the furcation. • Grade II – approaches the furcation but does not make contact with it • Grade III – extends into the furcation
• Lieb et al found more grade II than grade III CEP in mandibular molars but more grade III CEP in maxillary molars • Masters and Hoskins reported that CEP were found in 29% of mandibular and 17% of maxillary molars. • Grade I projections most common (Lieb, Swan) • Buccal surface mostly affected (Lieb, Matia)
Anatomy of the bony defect • Pattern of attachment loss ØHorizontal bone loss – thin facial/lingual plates of bone ØVertical bone loss –areas with thickened bony ledges v. Complex multiwalled defects with deep interradicular vertical component may be candidates for regenerative procedure. v. Molars with advanced attachment loss on only one root – resective procedure
Other dental findings Dental and periodontal condition of adjacent teeth Combination of furcation involvement Root approximation with adjacent tooth Presence of an adequate band of attached gingiva Vestibular depth All these factors may modify the treatment

Treatment of furcation involvement Objectives 1. The elimination of the microbial plaque from the exposed surfaces of the root complex. 2. Facilitate maintenance. The establishment of an anatomy of the affected surfaces that facilitates proper selfperformed plaque control and obliterate the furcation defects as a periodontal maintenance problem. 3. Prevent further attachment loss
Factors to be considered in treatment of furcation involved molars • Tooth related factors v. Degree of furcation invlivement v. Amount of remaining periodontal support v. Probing depth v. Tooth mobility v. Endodontic conditions and root/root canal anatomy v. Available sound tooth structure v. Tooth position and occlusal antagonism

• Patient related factors v. Stragic value of the tooth in relation to the overall plan. v. Patients functional and esthetic demands v. Patients age and health conditions v. Oral hygiene capacity.
Selection of therapeutic mode • Depends on 1. 2. 3. Class of furcation involvement Extent and configuration of bone loss Other anatomic factors such as size, shape and divergence of roots; size of crown; crown-root ratio; length of root trunk.

Therapy for early furcation defect: class I Resolution of inflammation repair of periodontal tissue can be achieved by; • Conservative periodontal therapy- scaling and root planning. • Elimination of overhanging restoration, facial grooves, cervical enamel projections by odontoplasty, recontouring, or replacement.

Therapy for furcation involvement: Class II ØShallow horizontal involvement without significant vertical bone loss –good prognosis R Closed or open scaling, root planing. Localized flap operation with odontoplasty and osteoplasty; and apical positioning of flap.


Therapy for furcation involvement: Class II ØDeep isolated class II furcations üCheck occlusion for possible traumatic forces. R • Flap procedure with scaling and root planing. • Grade IV Tunnel preparation Øreduces the dome of the furcation and alters • • gingival contour to facilitate the patient’s plaque control. GTR –mandibular molars Root resection- GTR or other surgical procedure contraondicated.

Therapy for furcation involvement: Class III • Closed and open flap scaling and root planing. • Grade IV Tunnel preparation- as GTR less successful compared with grade II FI. • Root resection- when regeneration is unpredictable • Tooth extraction • Obturation of furcation defect with restorative material such as polmeric reinforced zinic oxide (Baer-Klinsberg) , resin ionomer (Anderegy)



Therapy for advanced furcation defects: Class II-IV • Tunnel preparation • Root resection • Maintenance – perform plaque control measures • Extraction

Scaling and root planning • Used for incipient lesion where no interradicular bone lesion exists and pocket is suprabony. • Helps to resolve the inflammatory lesion of the gingiva and re-establishment of normal gingival anatomy and reduce pocket depth. (Goldman 1958)
Furcation plasty –Odontoplasy and Osteoplasty • Described by Hamp, Nyman and Lindhe (1975) • It is a resective treatment modality which should lead to the elimination of the interradicular defect. Tooth substance is removed (odontoplasty) and the alveolar bone crust is remodeled (osteoplasty) at the level of the furcation entrance. Used mainly at buccal and lingual furcations.
Procedure • Reflect soft tissue flap to gain access to the interradicular • • area Removal of the inflammatory soft tissue from furcation area Removal of crown and root substance in the furcation area to reduce/eliminate the horizontal component of the defect and to widen the furcation entrance Recon touring of the alveolar bone crest in order to reduce the buccal lingual dimension of a bone defect in the furcationdefect The flap is positioned and sutured at the level of the alveolar crest in order to cover the furcation entrance with soft tissue.

Prognosis of furcation plasty • Hamp et al in a 5 year study showed that more than 85% of the furcation treated with scaling, root planing alone maintained stable conditions or showed signs of improvement.
Tunnel preparation • It is a resective procedure which can be done for Mandibular molars which have a short root trunk, a wide separation angle and long divergence between the mesial and distal roots. • Indicated for advanced grade II and grade III lesions (through and through), where resection is not possible.
• The major advantage of tunnel preparation is • • that, in general, it does not require subsequent endodontics or fixed prosthetics. Also on teeth with reduced bone support, this treatment will not lead to significantly increased mobility such as is commonly observed after resection of one or more roots. It should be pointed out that a tunnel preparation procedure does not exclude the possibility for later hemisection or root resection, if this is indicated.
• Criteria for selection of a grade III FI to tunnel 1. Tooth should be a mandibular molar for 2. 3. 4. 5. clear two way access Patient should have low caries index and demonstrate good plaque control The root trunk should be short with high furcation entrance and long roots. Roots should have good spread with wide furcal entrance Floor of the pulp chamber should not be close to the root of the furcation to allow for possible odontoplasty at the entrance.
Procedure • Reflect buccal and lingual mucosal flap and • • remove the granulation tissue. The furcation area is widened by removal of some of the interradicular bone. The alveolar bone crest is recontoured to obtain a flat outline of the bone, some of the interdental bone, mesial and distal to the tooth in the region, is also removed. Following hard tissue resection enough space is established in the furcation area to allow for access for cleaning devices. The flap is repositioned apically to the surgically established interradicular and Interproximal bone level.
Prognosis of tunnel preparation • On teeth with reduced bone support, this treatment will not lead to significantly increased mobility such as is commonly observed after resection of one or more roots. • Tunnel preparations have been associated with a poor prognosis. In particular, it has been reported that the risk of root caries development is a major concern. This corresponds to a failure rate of about 60%. (Hamp et al 1975).

• Leif B. Hellden et al (1989) showed that 11% of • • the tooth surfaces developed caries. Ravald and Hamp and Ravald et al. reported that most of the root caries developed within 2 years after treatment. The higher incidence of root surface caries development which was observed among the tunnel prepared teeth might, primarily be attributed to difficulties in achieving optimal plaque control and less to a reduced caries resistanc of the tooth surface in the furcation regions.

Root separation and resection (RSR) • Root separation/ bicuspidization/ hemisection/ tooth sectioning involves the sectioning of the root complex and the maintenance of all roots. • Root resection/amputation involves the sectioning and removal of one or two roots of a multirooted tooth. • RSR is frequently used in cases of deep degree II , degree III and degree IV furcation involving molars
Root resection • Indicated in maxillary multirooted teeth with grade II to IV furcation involvement. Hemisection • Performed on mandibular molar with buccal and lingual class II or III furcation involvement. ØFurcations that extend more than 2/3 rd the buccolingual dimension of the tooth can only be treated by maintenance or root resection
Indications and contraindications (Bassaraba 1969) Indications 1. Grade II and III lesions 2. Advanced decay 3. Severe gingival recession on a single root 4. Close root proximity with minimal interseptal bone, preventing adequate embrasure space for prosthetic restoration.
5. Inability to perform endodontic therapy 6. Endodontic failure 7. Tooth fracture 8. Extensive root caries 9. Root resorption 10. Root perforation 11. Severe vertical bone loss about one or more roots

Contraindications 1. Tooth with a poor crown-root ratio on the remaining roots 2. Inadequate bone support on roots to be retained 3. Unfavorable roof anatomy of retained tooth 4. Long tooth trunk 5. Fused roots 6. Extensive webbing between roots
7. Bell shaped crowns 8. Teeth in which endodontic treatment restoration are not possible on the remaining roots 9. Poor surgical access 10. Inability to perform oral hygiene 11. Poor form of remaining roots 12. Splinting is not possible 13. Severe vertical bone loss internally
Disadvantage • Need for additional complex restorative procedure.
Factors to be considered A. Length of the root trunk • • In patient with progressive periodontal disease a tooth with short root trunk may have early involvement of the furcation (larato 1975 , Gher and Vernino 1980). A tooth with short root trunk is a good candidate for RSR; the amount of remaining periodontal tissue support following seperation and resection is often sufficient to ensure the stability of remaining root cones. If root trunk is long , furcation involvement occurs later in the disease process and amount of periodontal tissue support will be insufficien to allow for RSR.

B. Divergence between the root cones • Root with short divergence are technically more difficult to separate than roots which are wide apart. Smaller the divergence , smaller the interradiculr space. In such cases orthodontic seperation may be considered. • The furction space may also be increased by odontoplasty performed on 1) the distal part of the mesial root and 2) mesial part of the distal root and deep finishing lines prepared for subsequent restoration.
C. Length and shape of the root cones • Shorter and smaller root cones following seperation tend to exibit increased mobility.

D. Fusion between root cones • The mesial and distal root of the furcation must be probed to 3 -5 mm to ascertain that a fusion does not exist between the root scheduled for RSR.
E. Amount of remaining support around individual roots • A localized deep attachment loss at one surface of one particular root may compromise the long term prognosis for an otherwise ideal root.
F. Stability of individual roots • Examined following root seperation. The more mobile the root cone is, the less periodontal tissue support remains

G. Access for oral hygiene devices • The site after completion of therapy must a have an anatomy which facilitated proper self-performed tooth cleaning.

Which root to remove • Mobility • State of repair of the tooth structure • Morphology of periodontal defect • Endodontics • Edentulous span • Root anatomy
Guidelines for root removal 1. Remove the roots that will eliminate the 2. 3. furcation and allow the production of a maintainable architecture on the remaining roots. Remove the roots with the greatest amount of bone and attachment loss. Remove the root that best contributes to the elimination of periodontal problems on adjacent teeth.

4. Remove the roots with the greatest 5. number of anatomic problems such as severe curvature, developmental grooves, root flutings or accessory and multiple root canals. Remove the root that least complicates future periodontal maintenance.

Maxillary premolar • Furcation often located at apical level. Thus in presence of deep furcation involvement of degree II or degree III involvement extraction is advisable.
Maxillary molar • The distobuccal root is the shortest and root • trukl is long. Thus, it has small quantity of bone support and is thus the most often removed as part of RSR (Rosenberg 1978, Ross and Thompson 1980) The mesiobuccal root has a wide buccopalatal dimension , an hour-glass cross-section and thus a large surface area. It is located centrally in the alveolar process and is properly aligned with the maxillary premolars and is in an ideal position to function as a separate unite. Thus, they are preferred to be retained when clinician is selecting between the mesiobuccal or palatal root. In case of deep attachment loss, bone loss at the distal palatal aspect of MB root , the palatal root is retained.

Mandibular molar Treatment alternatives include; 1. separating the two roots, but maintaining 2. 3. both roots (premolarization) separate and extract the mesial root separate and extract the distal root.

• The mesial root has greater surface area than the distal root. It has an hour-glass cross-section , which may make selfperformed plaque control and restorative procedure difficult. • The distal root is oval shaped and large, providing a greater mass of dentin to resist root fracture (Langer et al 1981), and is a good candidate for pin or post plaement. Also, in case of an terminal abutment for a bridge, retension of the distal root will result in a longer arch.
Sequence of treatment for RSR 1. Endodontic phase - • Need to do endodontic treatment for vital and non-vital teeth undergoing resection • Avoid root perforation • If furcation involvement identified during periodontal surgery, complete RSR along with sealing the root canal entrance. Definitive RCT may be completed in 2 weeks.

2. Provisional restoration- • Impression is taken and a provisional restoration made.

3. Resective phase • Full thickness periodontal flap elevation followed by osseous resective surgery.
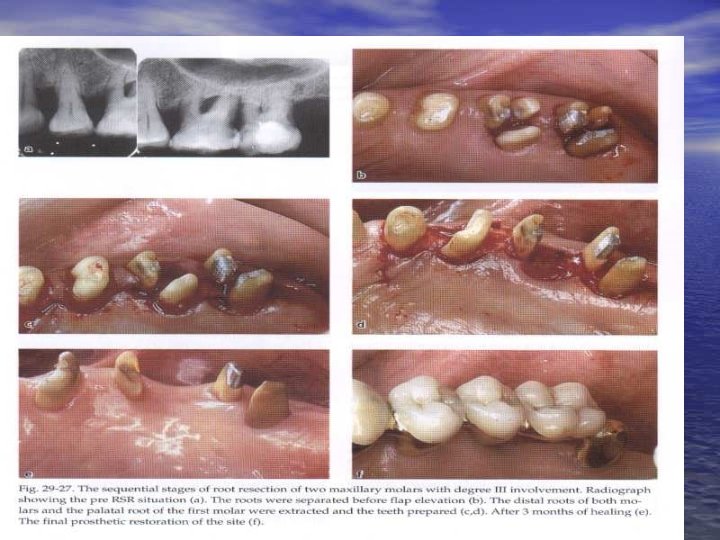
Root separation and resection- • It may be performed as part of preparation of the segment for prosthetic rehabilitation i. e. prior to periodontal surgery (Carnevale et al 1981) or along with periodontal flap surgery.
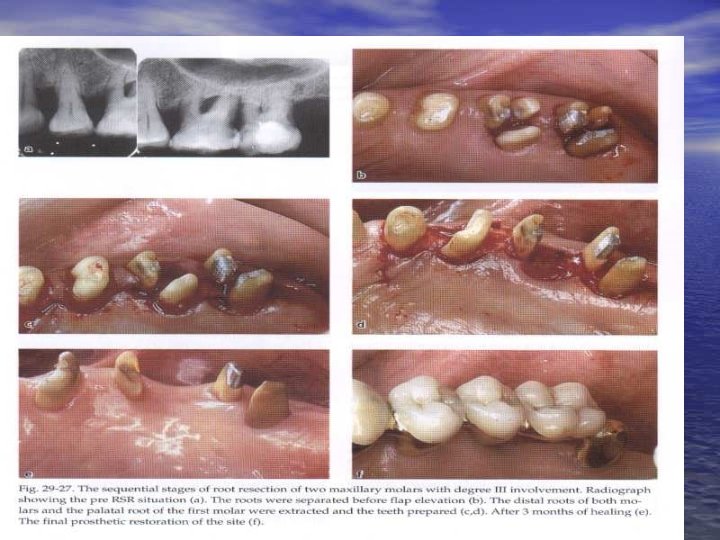
Root Resection Procedure • Elevate a full thickness flap on both facial and lingual/palatal aspect. • After debridement the resection of the root begins with the exposure of the furcation on the root to be removed • The removal of small amount of facial or palatal bone may be required to provide access for elevation and faciliate root removal

• A cut then directed from just apical to the contact point of the tooth, through the tooth , to the facial and distal orifices of the furcation. • This cut is made with a high speed surgical length fissure or cross-cut fissure carbide bur.
• If the tooth is vital a more horizontal cut through the tooth is advisable. • An oblique cut exposes a large surface area of the radicular pulp and/or dental pulp chamber, which can lead to postoperative pain and complicate the performance of endodontics.

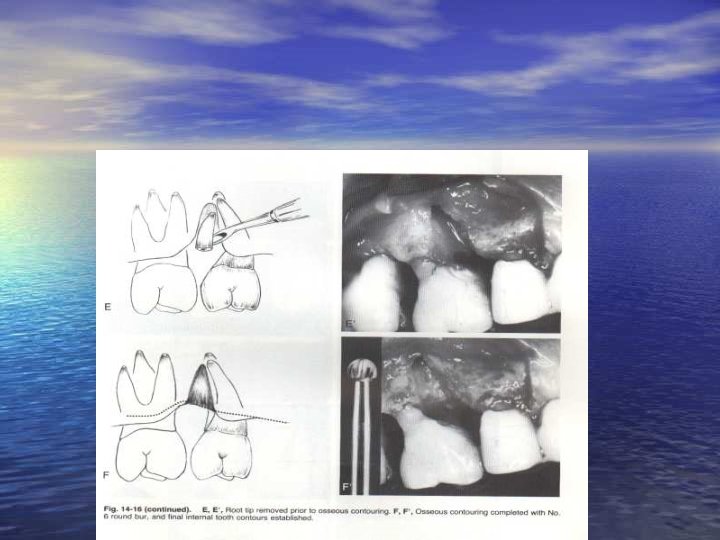
• After sectioning the root is elevated from its socket. • Care should be taken not to traumatize bone on the remaining roots or to damage an adjacent tooth. • Removal of provides visibility to the furcation aspects of the remaining roots and simplifies the debridement of the furcation with hand, rotary or ultrasonic instruments.
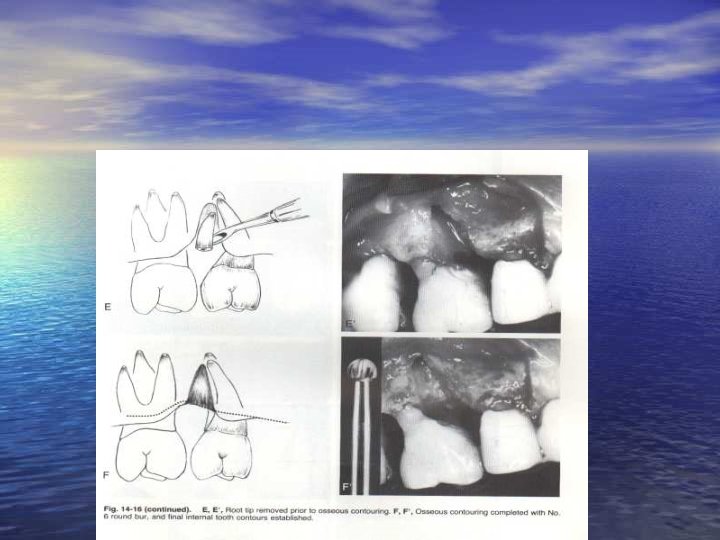
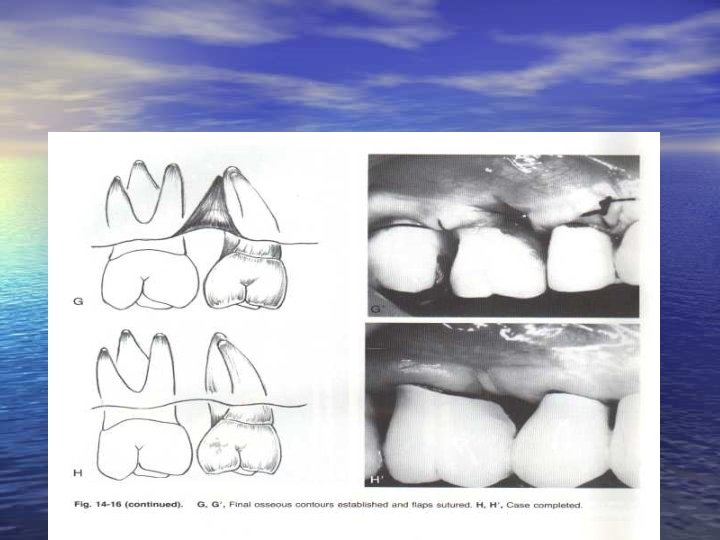
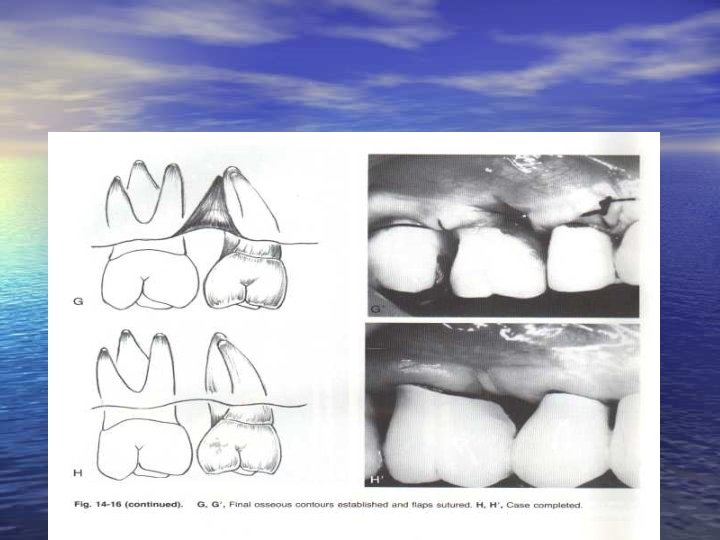
• If necessary , odontoplasty is performed to remove portions of the developmental ridges and prepare a furcation that is free of any deformity that would enhance plaque retention • Osseous surgery may also be combined with root resection if necessary. • The flaps are approximated to cover bony margin and sutured.

Hemisection • For hemisection a vertical oriented cit is made faciolingually through the buccal and lingual developmental grooves of the tooth, , through the pulp chamber , and through the furcation.
Guidelines for sectioning mandibular molars 1. 2. 3. 4. 5. 6. 7. Do not section excessively mobile teeth Try not to section heavily restored teeth Remove all overhanging tooth structure at the time of sectioning Do not be aggressive with endodontic instrumentaton Do not use internalized tooth preparation Do not construct large occlusal table Recognize the moment when it is too late to section the tooth successfully


During the prosthetic preparation it is important to avoid • exposing the interradicular bone to undue mechanical trauma • leaving behind parts of the furcation fornix • perforating the root canals • preparing the vertical surfaces of the remaining roots with sharp angles
4. Restorative phase Final prosthetic restoration • The preparation margin should be located supragingivally. The framework of the restoration must be rigid to compensate for compromised abutments • The restorative margin must be placed on sound tooth structure, including the area apical to the pulp chamber.
Common cause of failure 1. Root fracture because of a) Lack of conservative endodontic b) c) 2. 3. treatment Failure to restore teeth adequately with posts and crowns Inadequate provisional or final splinting for stablization Poor tooth selection Incomplete sectioning
4. Failure to diagnose involvement of other 5. 6. 7. furcations Failure to correct osseous deformities, resulting in residual pockets Failure to remove residual furcations Inability to maintain an adequate level of oral physiotherapy about adjacent furcations
Prognosis for RSR • Reported failures are categorized as being caused by • caries endodontic complication and periodontal disease. Failure rates for resected and restored teeth demonstrates that a high percentage of maxillary molar failures occur for periodontal reasons due to deeper concavity on the distal aspect making plaque contol difficult and that the percentage of periodontal failures is higher for maxillary than for mandibular molars. (Langer et al 1981) • Despite the concavity on the furcal aspect of the remaining mesial or distal root, (Bower)) it seems that periodontal breakdown is not the primary cause of failure of root resection in mandibular molars. (Langer et al , Carnevale et al 1984, Klavan 1975
• Keough suggested a modification of the contours • of the final restoration in order to minimize this problem; shoulders are placed on the convex surfaces immediately adjacent to the concavities to facilitate the flattening of these surfaces faciolingually. It seems, however, that this modification does not affect the actual depth of the concavity if the flat emergence profile is to be preserved. Kastenbaum suggested that the preparation should be opened or rounded into the furca and the root prominence on either side flattened. This allows the preservation of the flat emergence profile at the distal aspect of the tooth and for the flattening of the concavity to a certain extent.
• Periodontal failures was found to be less than 10%. Carneval et al reported failures of 5. 7% as being due periodontal reasons. • Retrospective longitudina studies have shown success rates ranging from 100% to 62% over 3 to 12 years. •

• Animal and short-term human studies (Tal 1989, • Tarnow et al 1986) have suggested that restorations interfering with the biologic width will result in a certain loss of periodontal attachment levels. The 2. 04 mm value of adequate biologic width need to be maintained as reported by Garguilo et al. If the biologic width of 2. 04 mm is violated on the distal surface of resected maxillary molars , loss of attachment is likely to occur.
• Carneval et al 1998 in a 10 year prospective controlled clinical trial demonstrated a 93% survival rate of root resected furcation involved teeth and a 99% survival rate of non furcation involved teeth • Svardstrom (2001) in a retrospective study demonstrated a 11% loss of resected / separated over 9. 5 years and of the tooth considered for maintenance 3. 5% were lost.
• Langer et al. reported a relatively high frequency of complications and failures, in particular root fractures. After an observation time of 5 years, the failure rate was 15. 8% and after 10 years the failure rate was 38%. • In the 5 -year follow-up study by Hamp et al. , on the other hand, no root fractures were reported and caries was only observed on 5. 7% of the root resected teeth.

Regeneration of furcation defects • Periodontal regeneration is the restoration of the tooth-supported tissues including cementum, periodontal ligament and alveolar bone over previously diseased root surface.

Regenerative procedure • Indicated in furcation defects with deep two-walled or significant three-walled components. • Mainly grade II mandibular furcation defects Techniques • Root surface conditioning • Coronally advanced flap procedure • Bone grafts with or with out membrane • Polypeptide Growth factors. • Enamel matrix protein

Wound healing in furcation defects • Melcher suggested that the type of cell • 1. 2. 3. 4. that repopulates the periodontitis affects root surface after periodontal surgery determines the nature of the attachment that will form. The cleaned root surface can be repopulated by Epithelial cells Gingival connective tissue cells Bone cells Periodontal ligment cells

• The key cells in periodontal regeneration are the periodontal ligament cells resulting in new attachment. • Root resorption rather than new attachment occurs if the detached root surface is repopulated by cells derived from bone or gingival connective tissue. • Apical migration epithelium results in long junctional epithelium.
Root conditioning • It was suggested by Stahl that demineralization of the previously periodontitis-involved root surface, exposing the collagen of the dentin, would facilitate periodontal regeneration • Agents used where citric acid, fibrinfibronectin complex, tertacyclin,

Biological concept • Acid treatment causes demineralization of the root planed dentin, hereby exposing collagen fibrils of the dentin matrix. The exposed collagen fibrils may facilitate adhesion of blood clot to the root surface and favour migration of fibroblasts and that the exposed collagen fibrils of dentin matrix may interdigitate with newly formed collagen fibrils in the adjacent healing tissues resulting in new connective tissue attachment. .
Coronally positioned flap • Can be used along with root conditioning • Provides adequate coverage of furcation defect for the formation of new attachment. • Delay apical migration of oral epithelium
Bone graft Biological concept • 1. 2. The bone graft used may Contain bone forming cells (osteogenesis), or Serve as a scaffold for bone formation (osteoconductive), or 3. The matrix of the grafting material contains inductive substances (osteoinductive) which may stimulate both the regrowth of alveolar bone and the formation of new attachment.
Bone grafts Studies of healing of furcation defect following flap surgery including bone grafts by Ellengaard, Nielsen have shown that • Only iliac bone marrow grafts resulted in consistent bone fill • Jaw bone grafts or xenografts did not actively contribute to bone formation but served as scaffold for bone growth from the interradicular bone septum and often persisted as isolated particles surrounded by a cementum like substance.

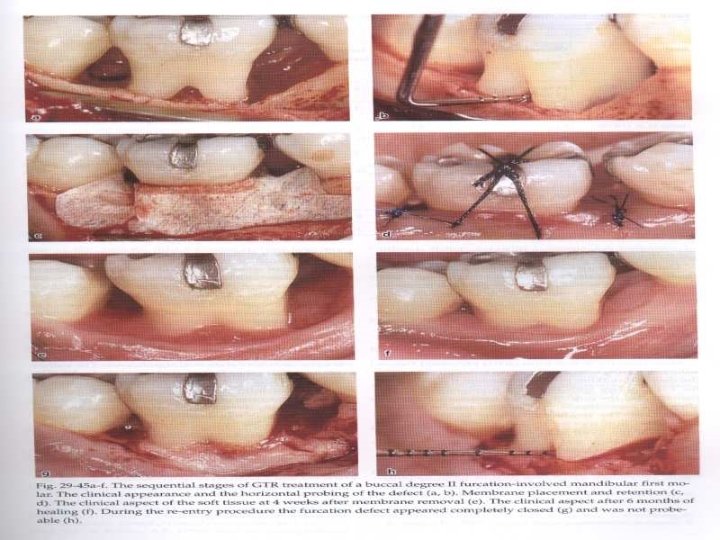
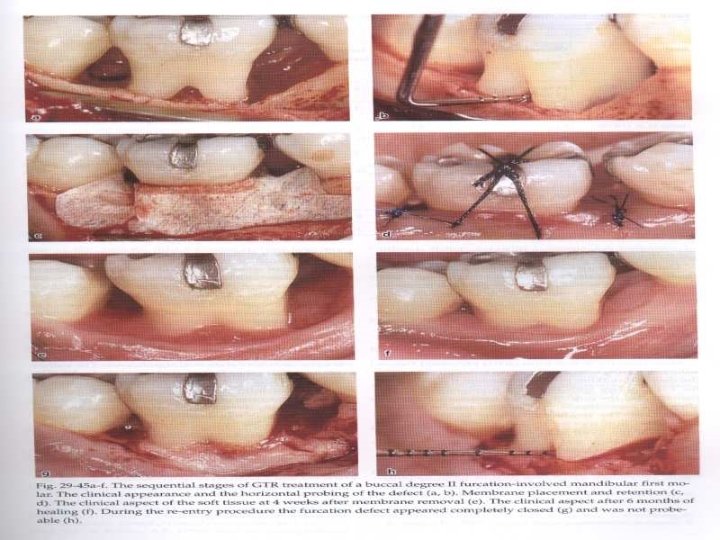
Guided tissue regeneration • It involves the placement of a physical • barrier to ensure that previously periodontitis affected root surfaces become repopulated with cells from the periodontal ligament.
Biological concept • The progenitor cells for the formation of a new connective tissue attachment to the root surface are residing in the periodontal ligament. By preventing both gingival connective tissue and gingival epithelium from contacting the root surface by using a barrier membrane, repopulation of the detached root surface with periodontal ligament cells can be ensured.
Predictability of GTR depends • On the size of the entrance of the defect (Pontoriero 1989) (>. 4 mm cross section – nocomplete healing ) • Height of the defect and complete flap coverage of the membrane during healing period (Pontriero & Lindhe 1995) (<3 mm complete healing

Polypeptide growth factors • Polypeptide growth factors are a class of natural biological • mediators which regulate key cellular events in tissue repair; i. e. , cell proliferation, chemotaxis (directed migration), differentiation, and matrix synthesis via binding to specific cell-surface receptors. Examples of GDFs found in bone, cementum, and healing wound tissues include platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), transforming growth factors (TGF-a and -b), acidic and basic fibroblast growth factors, (a- and b. FGF), epidermal growth factor (EGF), insulin-like growth factors (IGF-I and -II), cementum-derived growth factor (CGF), parathyroid hormone-related protein (PTHr. P), and bone morphogenetic proteins (BMPs 1 -12).
• Healing following injury involves a series of well orchestrated cell-cell and cellmacromolecular interactions. In the normal wound healing process, multiple growth factors act in concert to form an intricate molecular arrangement regulating the activity of cells within and adjacent to a wound
• Following acute tissue injury involving • • • subepithelial tissues, disruption of the wound vasculature leads to fibrin formation and platelet aggregation forming a cellular plug. Activated platelets at the wound margins release several growth factors such as PDGF, TGF-b 1, an epidermal growth factor (EGF)-like protein, and platelet-derived endothelial cell growth factor (PD-ECGF). In addition, the plasma exudate provides an important source of insulin-like growth factors. Cells adjacent to the injured site also are induced to release growth factors such as IGF-I, PDGF, TGF-a, and TGF-b 1 within a few hours after injury.
• Following tissue injury, neutrophils accumulate • • with subsequent migration of macrophages into the area several days later. Macrophages exert multiple effects on the wound healing microenvironment including debridement of damaged tissue and serving as another source of growth factors such as PDGF, TGF-a, and TGFb 1. In addition, bone and cementum contain large concentrations of growth factors such as IGF-I, II, TGF-b 1, and PDGF which may be released following injury. Differentiation (e. g. , osteoinductive) factors such as BMPs appear to be expressed in mature bone as well as during repair.
• The expression of various GDFs following bone and soft tissue injury (possibly during periodontal disease) may regulate the repair and/or regenerative process. • Thus, the objective for GDF administration in the treatment of chronic adult-onset periodontitis such as furcation involvement, is to enhance the normal wound healing response which may be of insufficient magnitude to promote complete regeneration of all attachment structures.
• For periodontal regeneration, the coronal re- establishment of the PDL is required together with corresponding cementum and supporting alveolar bone. Thus agents which promote PDL fibroblast (PLF) proliferation and migration as well as collagen biosynthesis would appear to be critical mediators for enhancing new periodontal ligament formation. Currently, the most wellstudied growth factors on PLF activity include PDGF-BB, TGF-b 1, b. FGF, EGF, IGF-I, CGF, and BMP-7 (osteogenic protein-1).

• These growth factors may be produced synthetically and applied along with a carrier alone or in combination with other growth factors to induce periodontal regeneration.
Enamel matrix protein • Enamel matrix proteins, mainly amelogenin, are secreted by Hertwig’s epithelial root sheath during tooth development and induce acellular cementum formation. • They are believed to favor periodontal regeneration.
Technique of application of Enamel Matrix Proteins (Mellonig) 1. 2. 3. 4. 5. 6. Raise flap for regenerative procedure Remove granulation tissue and expose underlying bone. Control bleeding within the defect. Demineralize the root surface with citric acid p. H 1. Rinse the wound with saline. Apply gel to fully cover the root surface. Close the flap with sutures to completely cover the defect.
Prognosis for regenerative procedure • Reasonably predictable outcome of GTR therapy • was demonstrated only in degree II furcation involved mandibular molars , where a clinical sot tissue closure or decreased probing depth was recorded. (Pontoriero et al 1988, Lekovic et al 1989, Cafesse et al 1996) Less favourable results have been reported when GTR therapy was used in other types of furcation defects as degree III furcation involved mandibular and maxillary molars (Pontoriero 1989, Pontooriero and Lindhe 1995) and degree IIfurcation in maxillary molars (Metzeler et al
• GTR demonstrat significant clinical improvement • • in treating degree II mandibular furcation defect. Regarding degree II maxillary furcations, the results are inconsistent, and the treatment of degree III furcation defect is unpredictable. (Becker et al 1988, Pontoriero et al 1992) Karring and Corteline (1999) demonstrated that treating degree III furcations with GTR was unpredictable. Metzler (1991) and co-workers and Mellonig and co-workers (1994) have reported limited improvement on the treatment of maxillary furcations with GTR.
• Raymond et al (2001) demonstrated equal • • clinical results in treating mandibular class II facial defect with bioglass bone replacement and expanded polytetrafluroethylene barrier membrane. Mehlbauer et al treated class IIIfurcation with coronally positioned flap and demonstrated a 66% closure when used along with polyglactic membrane and 33% closure when the mesh was not used. Kling et al (1981) demonstrated that adequate post operative coverage of through and through defects is critical for successful healing
• Bone grafts along with GTR can be used for • • treatment of mandibular degree II furcations for added benefit. Evans et al (1996) demonstrated that monotherapy with bone grafts resulted in 55% overall improvement either complete fill or partial furcation fill compared to 52% for GTR barrier and only 16% for open flap debridement in mandibular class II furcations Park et al 1995 demonstrated that combination of PDGF and GTR results in faster and complete regeneration of periodontal ligment and alveolar bone in degree III furcation defects
• Grantes treated class II defect with coronally repositioned flap with or without DFDBA , demonstrated a 67% bone fill with 43% of the defects completely filled. The results were not dramatic for class III defects. • Garrett et al treated class III furcations with citric acid root conditioning, DFBA, coronally positioned flap with or with out membrane and demonstrated a bone fill of 8 -21% of the defect
• Grantes treated class II defect with coronally repositioned flap with or without DFDBA , demonstrated a 67% bone fill with 43% of the defects completely filled. The results were not dramatic for class III defects. • Garrett et al treated class III furcations with citric acid root conditioning, DFBA, coronally positioned flap with or with out membrane and demonstrated a bone fill of 8 -21% of the defect

• Mehlbauer et al treated class III furcation with coronally positioned flap and demonstrated a 66% closure when used along with polyglactic membrane and 33% closure when the mesh was not used.
• Park et al 1995 used platelet-derived growth • factor-BB (PDGF-BB)-modulated guided tissue regenerative (GTR) therapy (P-GTR), and demonstrated that it was capable of achieving periodontal regeneration of horizontal (Class III) furcation defects with 80% bone fill compared to 14 % at 8 weeks with GTR alone Murakami et al (2003) treated class II furcation defects in beagle dog with recombinant human basic fibroblast growth factor and demonstrated significant regeneration as represented by new bone formation of 83. 3% , new trabecular bone formation of 44. 1% and new cementum formation of 97% without epithelial down growth.
• Rossa et al (2000) used b. FGF with GTR in class III furcation, and demonstrated extensive periodontal regeneration. • Kinoshita et al used BMP-2, Lynch et al used PDGF , Sigurdsson et al used BMP-2, Giannobile used OP-1, Wikesjo et al used TGF-B with varying results. • Terranova (1987) has proposed that one isolated growth fator may not be sufficient for regenerative therapy needs due to the complex nature of connective tissue involved in the process of periodontal regeneration.
• Donos et al (2003) demonstrated that enamel matrix derivative resulted in new attachment , new bone formation , acellular cementum apically and mixture of cellular and acellular cementum coronally. But in grade III furcation treatment was unpredictable. • EMD, GTR, EMD and GTR resulted in true periodontal regeneration (Donos)

The reason for limited predictability of GTR therapy in furcation involved teeth may be related to several factors • Morphology of the periodontal defect. • The anatomy of the furcation may prevent proper instrumentation. • The varying and changing location of the soft tissue margins during the early phase of healing with a possible recession of the flap margin and early exposure of the membrane and fornix of the furcation.
Predictability of GTR can be improved only if 1. The interproximal bone is located at the 2. 3. 4. level which is close to the CEJ. Debridement of the exposed root surface in furcation area is comprehensive. The membrane is properly placed and a space between tooth and material is established. Post surgical plaque maintenance every 2 -3 momths

Extraction • Advised in through and through furcation defects (class III and Class IV) and advanced attachment loss. • Patients who can not perform adequate plaque control • High caries activity. ØOsseointegrated dental implant as an alternative
Factors determining tooth extraction • Tooth mobility • Tooth position • Absence of occlusal antagonism • Degree of furcation involved • Probing depth • Amount of remaining periodontal support
Factors affecting clinical outcome • Patent factor ØProper plaque control ØSmoking • Defect factors Ø 1 st and 2 nd mandibular molars and buccal and lingual degree II furcation defects respond well to GTR. ØMaxillary molars- large avascular area, inaccessibility –poor response
• Technical factors ØFlap margin- away from the entrance of the healing defect ØPostoperative infection
summary Multirooted teeth FI present some of the biggest challenges in periodontal therapy despite a large arsenal of therapeutic techniques. Early diagnosis and treatment are critical for long term success. Guided tissue regeneration has improved the long term prognosis of many deep grade II lesions but has not always shown consistent predictability. However, GTR may well become the treatment of choice for all grade II and III FI.
As long as the pathological process is extending only a minor distance (<5 mm, Degrees I and II involvement) into the furcation area, further progress of the disease can usually be prevented by scaling and root planing provided proper oral hygiene programe is established after treatment.
• In more advanced cases (5 -6 mm; degree II involvement) the initial cause related treatment is frequently supplemented with surgery involving contouring of the interradicular bone (osteoplasty) or reduction of tooth prominence at furcation entrance by grinding (odontoplasty), in order to reduce the horizontal extension of the furcation involvement.
• In cases where the involvement extends deeper into the furcation area (>5 mm; degree II) or through and through defect (degree III involvement) has developed , tunnel preparation or root resection has been advocated as choice of treatment (Muller 1995)
 Glickman furcation classification
Glickman furcation classification Class 2 furcation
Class 2 furcation Hamp furcation classification
Hamp furcation classification Long term plan and short term plan
Long term plan and short term plan Long term memory vs short term memory
Long term memory vs short term memory Example of short term human resources
Example of short term human resources Difference between long term and short term liabilities
Difference between long term and short term liabilities Long term liabilities
Long term liabilities Good short term goals
Good short term goals Long term and short term financial planning
Long term and short term financial planning Short short short long long long short short short
Short short short long long long short short short Once upon a time there lived a little country girl
Once upon a time there lived a little country girl Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Tarnow and fletcher classification
Tarnow and fletcher classification Wall hemiseptal
Wall hemiseptal Furcation plasty procedure
Furcation plasty procedure Youth involvement
Youth involvement Personal ministry goals
Personal ministry goals Panther involvement network
Panther involvement network Seven principles of social work
Seven principles of social work Panther involvement network
Panther involvement network What is the panther involvement network (pin)
What is the panther involvement network (pin) How can employee involvement measures motivate employees
How can employee involvement measures motivate employees Gaisce.ie
Gaisce.ie Brazil ww2 involvement
Brazil ww2 involvement Community participation
Community participation What drove european involvement in asian commerce
What drove european involvement in asian commerce Father involvement in early childhood
Father involvement in early childhood Contoh kasus social judgement theory
Contoh kasus social judgement theory Epstein's six types of parent involvement
Epstein's six types of parent involvement Six types of parental involvement
Six types of parental involvement Muscular involvement continuum
Muscular involvement continuum Panther involvement network
Panther involvement network Panther involvement network
Panther involvement network Panther involvement network
Panther involvement network Classify the
Classify the Allied forces ww1
Allied forces ww1 Tarnside curve of involvement
Tarnside curve of involvement Panther involvement network
Panther involvement network Twincs
Twincs A national policy of avoiding involvement in world affairs
A national policy of avoiding involvement in world affairs Internally paced skill
Internally paced skill Term-to-term rule
Term-to-term rule Linear pattern formula
Linear pattern formula Position-to-term rule
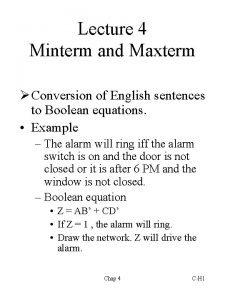
Position-to-term rule Minterms
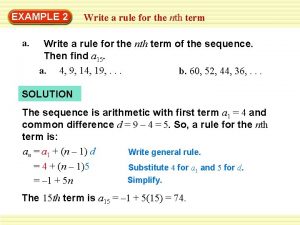
Minterms Term to term rule example
Term to term rule example Term to term rule
Term to term rule Wisconsin long term care partnership program
Wisconsin long term care partnership program Long term financing
Long term financing Goals in grade 11
Goals in grade 11 Long term scheduler
Long term scheduler Gsa long term lodging
Gsa long term lodging Manitoba teachers society long term disability
Manitoba teachers society long term disability When was the loom invented
When was the loom invented The long-term future of particle accelerators
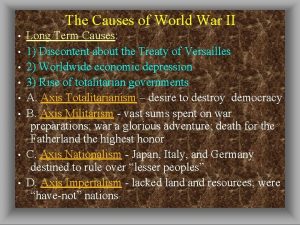
The long-term future of particle accelerators Long term causes of ww2
Long term causes of ww2 Long term causes of ww1
Long term causes of ww1 Nstu bereavement days
Nstu bereavement days Advantages of retained earnings
Advantages of retained earnings Short term finance sources
Short term finance sources Long term memory example
Long term memory example Physical activity examples
Physical activity examples Long-term incentive plan examples
Long-term incentive plan examples Persistence of learning over time
Persistence of learning over time Long term potentiation
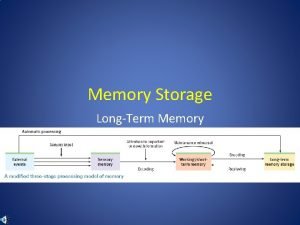
Long term potentiation Long term storage and retrieval
Long term storage and retrieval Premium on bonds payable classification
Premium on bonds payable classification Long-term notes payable
Long-term notes payable Bonds payable balance sheet
Bonds payable balance sheet Orthogonal frequency division multiplexing
Orthogonal frequency division multiplexing Long term effects of anorexia and bulimia
Long term effects of anorexia and bulimia Are lipids long term energy storage
Are lipids long term energy storage Long term debt ratio
Long term debt ratio Consequences of industrial revolution
Consequences of industrial revolution Enclosure movement industrial revolution
Enclosure movement industrial revolution Nmda ltp
Nmda ltp Long term goals examples
Long term goals examples Definition of goal setting
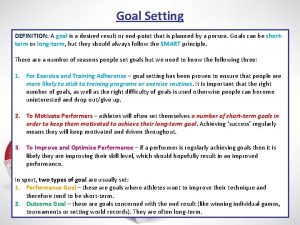
Definition of goal setting Process of memory encoding
Process of memory encoding A word slogan or symbol that distinctively
A word slogan or symbol that distinctively Euro btp futures
Euro btp futures Current portion of ltd
Current portion of ltd Current portion of long term debt
Current portion of long term debt Memory encoding
Memory encoding Sum of the years method of depreciation
Sum of the years method of depreciation Long term debt instruments
Long term debt instruments Long term debt instruments
Long term debt instruments Pdp smart goals examples
Pdp smart goals examples Long term career goals examples
Long term career goals examples Other long term assets
Other long term assets Example of encoding failure
Example of encoding failure Long term debt in balance sheet
Long term debt in balance sheet Creating long term loyalty relationships in marketing
Creating long term loyalty relationships in marketing Priority scheduling algorithm example
Priority scheduling algorithm example How to write off fixed assets
How to write off fixed assets Arizona altcs program
Arizona altcs program What is altcs
What is altcs Long term objectives and strategies
Long term objectives and strategies Long term causes french revolution
Long term causes french revolution Ltsa long term service agreement
Ltsa long term service agreement Hockey canada development model
Hockey canada development model Long-term goals for teenager
Long-term goals for teenager Long term financial planning process
Long term financial planning process Long-term debt preferred stock and common stock
Long-term debt preferred stock and common stock Ahcccs long term care
Ahcccs long term care Questions about loyalty in relationships
Questions about loyalty in relationships Evaluation of types of long term memory
Evaluation of types of long term memory Long term effects of rape
Long term effects of rape Long term financing
Long term financing Std crabs pics
Std crabs pics Long-term scheduler
Long-term scheduler Long term financial planning
Long term financial planning Manpower requirement meaning
Manpower requirement meaning Main long term & immediate causes of wwi
Main long term & immediate causes of wwi What is working capital in financial management
What is working capital in financial management Long term financial planning and growth chapter 4
Long term financial planning and growth chapter 4 Sustainable growth rate
Sustainable growth rate Chapter 10 accounting for long term liabilities
Chapter 10 accounting for long term liabilities Creating long term loyalty relationships
Creating long term loyalty relationships What is long term loans and advances
What is long term loans and advances Pull questions
Pull questions Valuation of long term securities
Valuation of long term securities Debentures advantages and disadvantages
Debentures advantages and disadvantages Long term capacity strategies
Long term capacity strategies What part of the brain stores long term memory
What part of the brain stores long term memory Wesel bayar tanpa bunga
Wesel bayar tanpa bunga Long term plan
Long term plan Short term goals
Short term goals Nhs long term plan physiotherapy
Nhs long term plan physiotherapy Memory stages model
Memory stages model Explicit memory
Explicit memory Macromolecules
Macromolecules Long term notes receivable
Long term notes receivable Shiba long term
Shiba long term Irr interpolation formula
Irr interpolation formula What were the long term causes of the great depression
What were the long term causes of the great depression Internal growth rate
Internal growth rate Tubal ligation side effects
Tubal ligation side effects Ecmwf long term forecast
Ecmwf long term forecast Tinker v des moines defendant
Tinker v des moines defendant Long term effects of exercise on skeletal system
Long term effects of exercise on skeletal system Long term securities
Long term securities Chapter 14 long term liabilities
Chapter 14 long term liabilities Long term financial planning and growth
Long term financial planning and growth Tbi long term servival after traumatic
Tbi long term servival after traumatic Ct ltc map
Ct ltc map Long term operational assets
Long term operational assets Spinning mule long term effects
Spinning mule long term effects Not so long ago people
Not so long ago people Once upon time there was a king
Once upon time there was a king Props in tinikling
Props in tinikling Once upon a time long ago and far away
Once upon a time long ago and far away Long long int c
Long long int c Greek
Greek Lông vằn lông vện mắt xanh
Lông vằn lông vện mắt xanh Once upon a long time ago
Once upon a long time ago Mình tròn thân trắng dáng hình thon thon
Mình tròn thân trắng dáng hình thon thon Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Glasgow thang điểm
Glasgow thang điểm Hát lên người ơi
Hát lên người ơi Môn thể thao bắt đầu bằng từ đua
Môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng