Contents o o o o Definition Classification Pathophysiology










- Slides: 57
Contents o o o o Definition & Classification Pathophysiology Clinical Presentation Risk Stratification Medical therapy Treatment Strategies & Intervention Prinzmetal Variant Angina
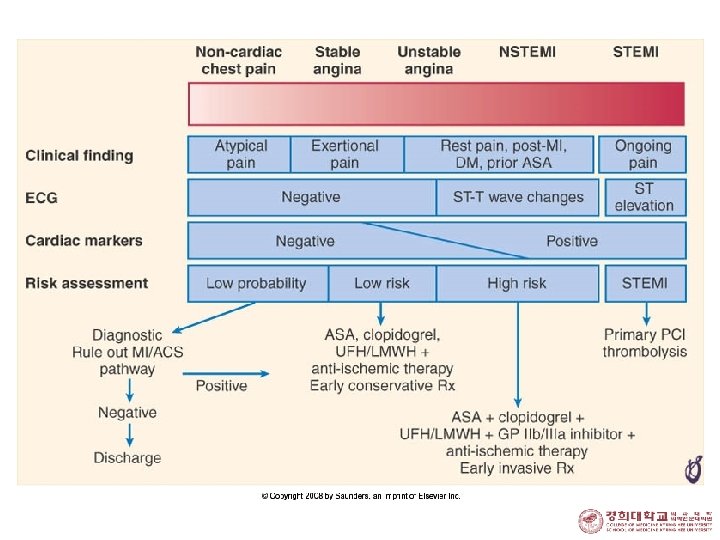
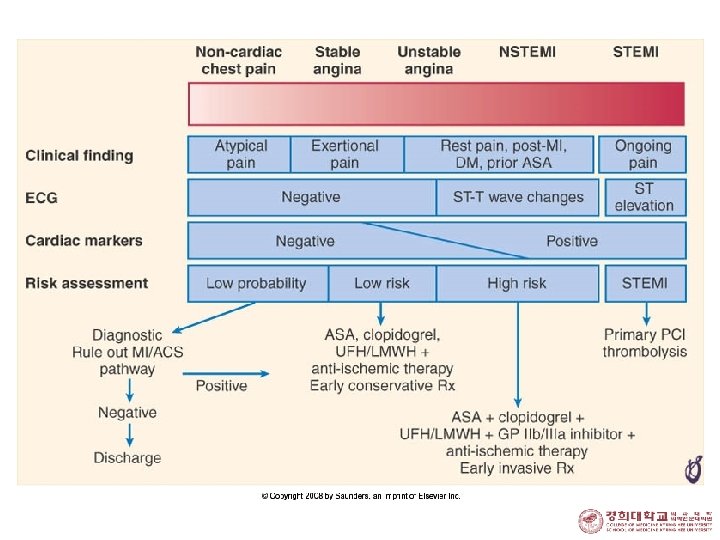
Definition o UA n angina pectoris or equivalent ischemic discomfort with at least one of three 1. at rest (or with minimal exertion) usually lasting > 20 min 2. severe and of new onset: , within the prior 4 to 6 weeks) 3. with a crescendo pattern: distinctly more severe, prolonged, or frequent o NSTEMI n the clinical features of UA develops evidence of myocardial necrosis, as reflected in elevated cardiac biomarkers.
Acute Coronary Syndrome o Rapid progression of coronary obstruction by intravascular thrombus 1. STEMI 2. Unstable angina pectoris NSTE-ACS 3. NSTEMI 4. Sudden cardiac death 5. Complications of PCIs
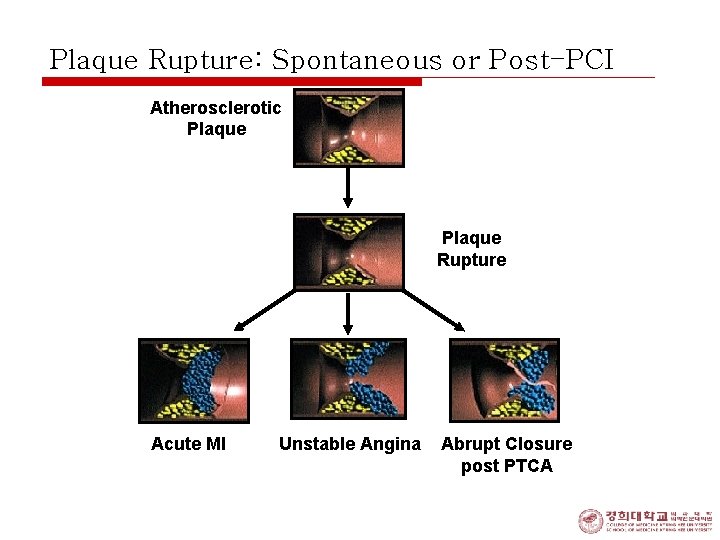
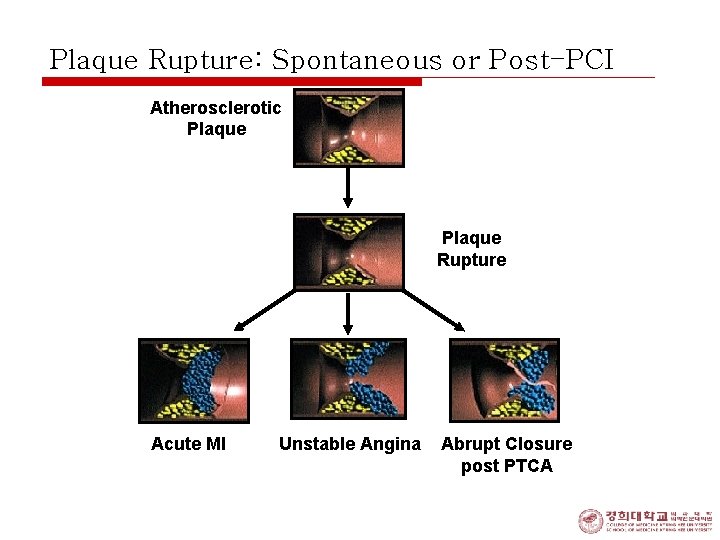
Plaque Rupture: Spontaneous or Post-PCI Atherosclerotic Plaque Rupture Acute MI Unstable Angina Abrupt Closure post PTCA
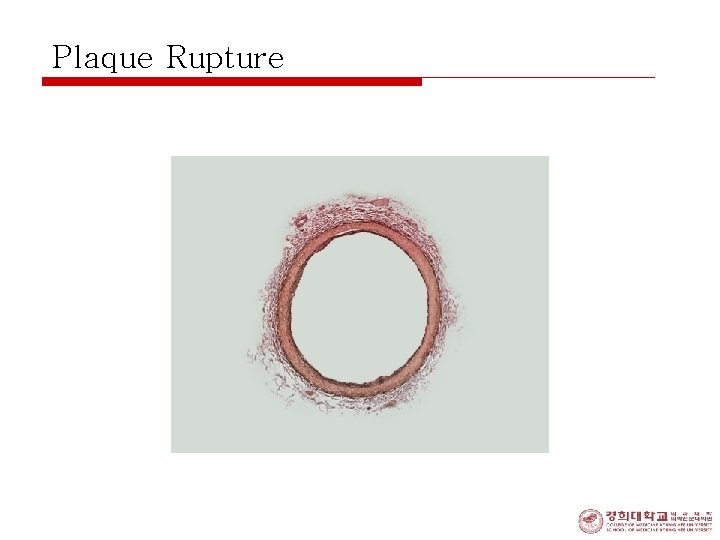
Plaque Rupture
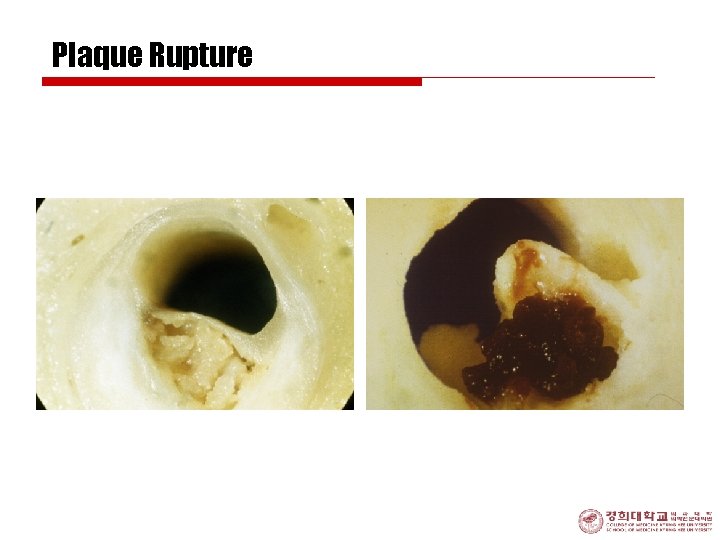
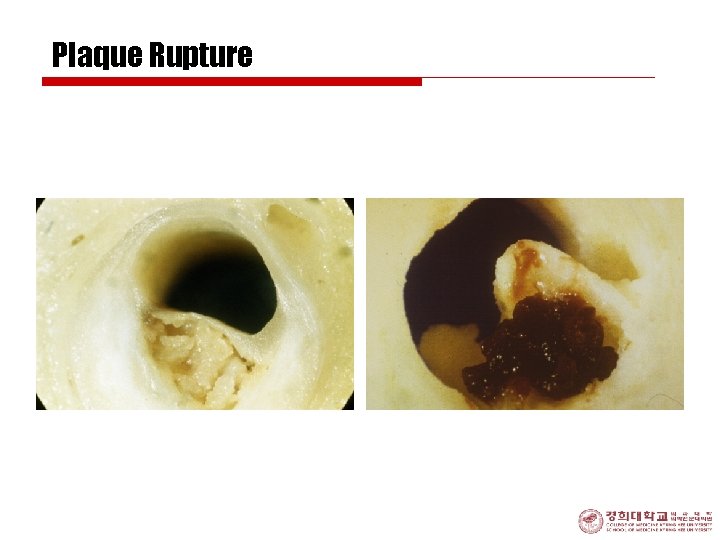
Plaque Rupture
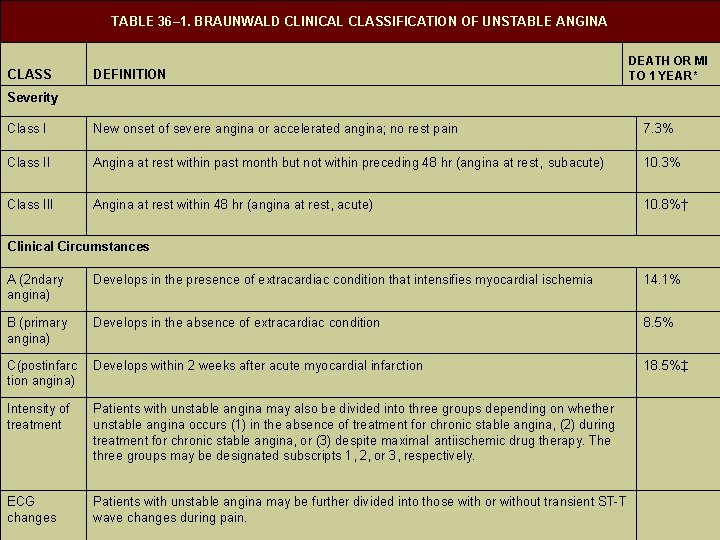
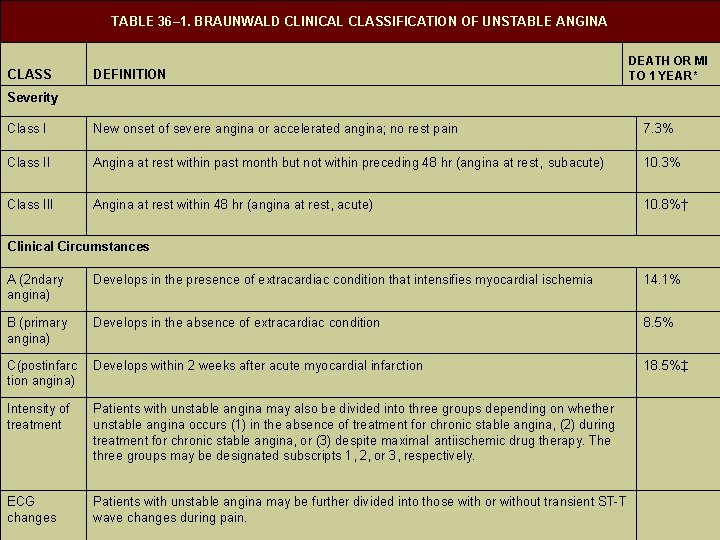
TABLE 36– 1. BRAUNWALD CLINICAL CLASSIFICATION OF UNSTABLE ANGINA CLASS DEFINITION DEATH OR MI TO 1 YEAR* Severity Class I New onset of severe angina or accelerated angina; no rest pain 7. 3% Class II Angina at rest within past month but not within preceding 48 hr (angina at rest, subacute) 10. 3% Class III Angina at rest within 48 hr (angina at rest, acute) 10. 8%† Clinical Circumstances A (2 ndary angina) Develops in the presence of extracardiac condition that intensifies myocardial ischemia 14. 1% B (primary angina) Develops in the absence of extracardiac condition 8. 5% C(postinfarc tion angina) Develops within 2 weeks after acute myocardial infarction 18. 5%‡ Intensity of treatment Patients with unstable angina may also be divided into three groups depending on whether unstable angina occurs (1) in the absence of treatment for chronic stable angina, (2) during treatment for chronic stable angina, or (3) despite maximal antiischemic drug therapy. The three groups may be designated subscripts 1, 2, or 3, respectively. ECG changes Patients with unstable angina may be further divided into those with or without transient ST-T wave changes during pain.

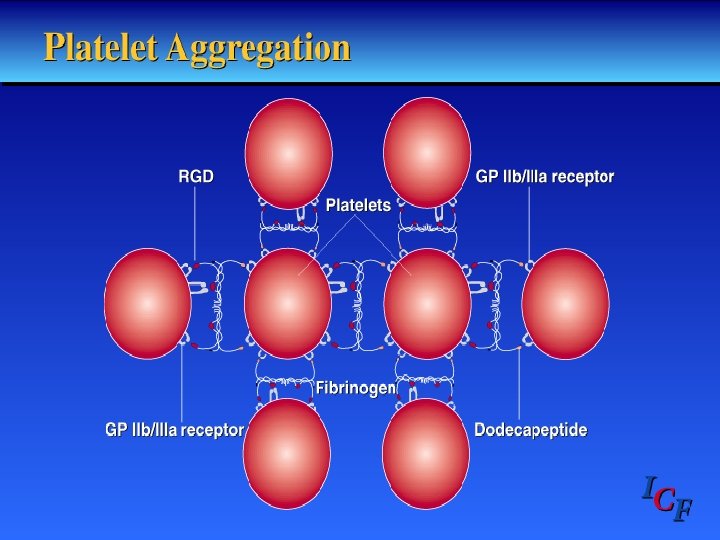
Pathophysiology 1. 2. 3. 4. 5. Thrombosis Paltelet Activation an Aggregation Coronary Vasoconstriction Progressive Mechanical obstruction Secondary Unstable Angina
Mechanisms § Abrupt decrease in myocardial oxygen delivery: 1. Plaque rupture or erosion with non-occlusive thrombus 2. Dynamic obstruction: by 1. Spasm of epicardial artery in Prinzmetal angina 3. Progressive mechanical obstruction § § Rapidly advancing atherosclerosis Restenosis following PCI 4. Secondary UA § increased myocardial oxygen demands and/or decreased supply(tachycardia, anemia)



Clinical Presentation o o History & Clinical Exam ECG Cardiac Markers for Dx. of NSTEMI CAG and IVUS
History Clinical Exam o Chest pain n Substernal, epigastrium radiate to neck, left shoulder and arm n Anginal Equivalent: dyspnea, epigastric discomfort o Unremarkable exam o Extensive Cardiac Ischemia n n n Diaphoresis Pale cool skin Sinus tachycardia 3 rd or 4 th Heart sound Basilar rale Rarely, hypotension
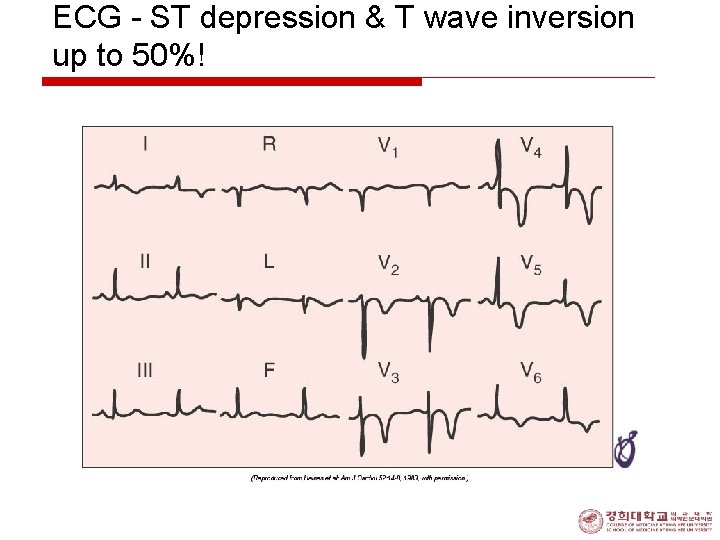
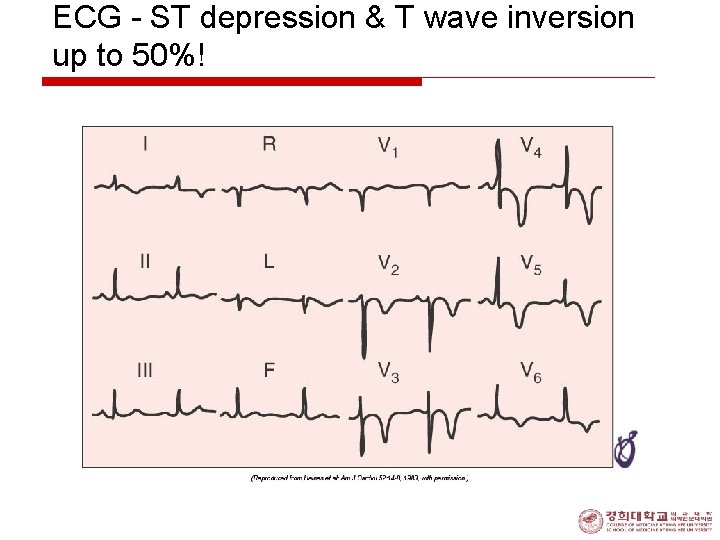
ECG - ST depression & T wave inversion up to 50%!
Cardiac Necrosis Markers for Dx. Of NSTEMI o Elevation of CK-MB, Troponin T or I n Indicate NSTEMI o With use of Troponin n Greater % of pts. are classified as NSTEMI o False positive Troponin elevation n CHF, Myocarditis n Worse prognosis than negative troponin

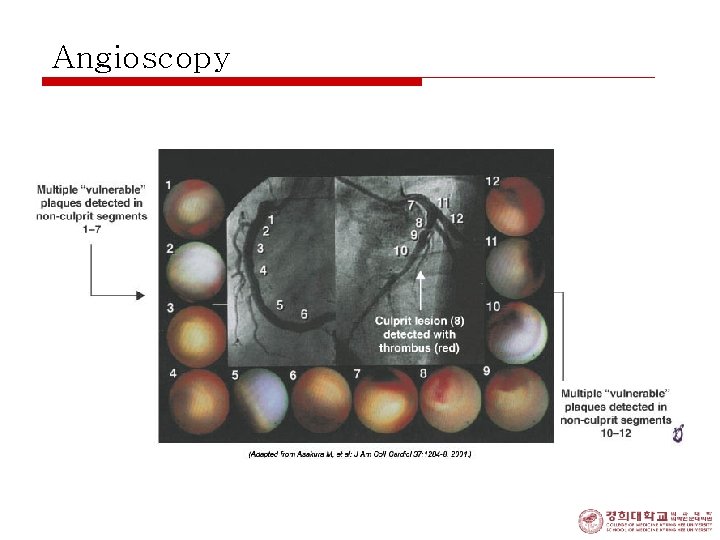
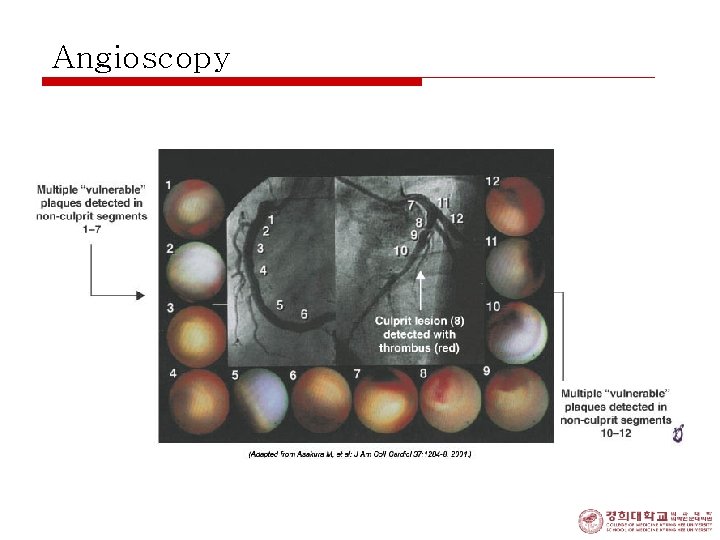
Angioscopy
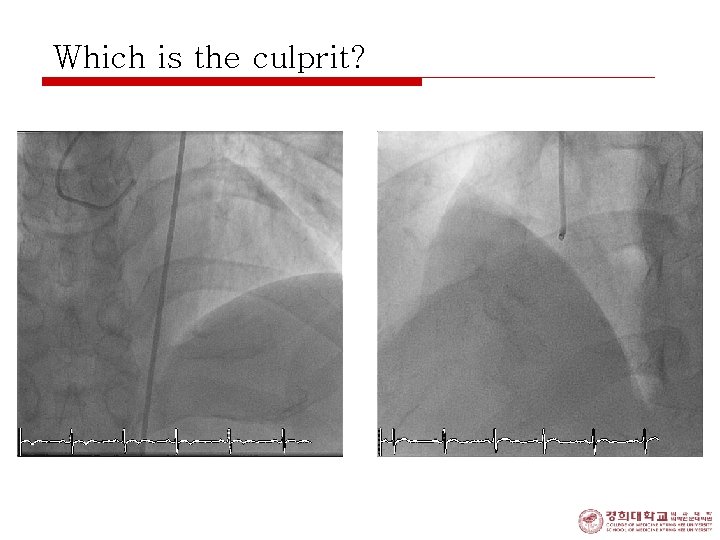
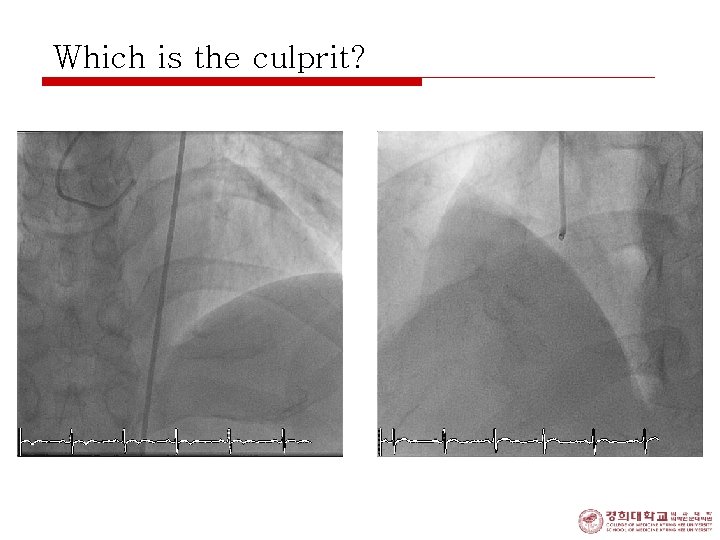
Which is the culprit?
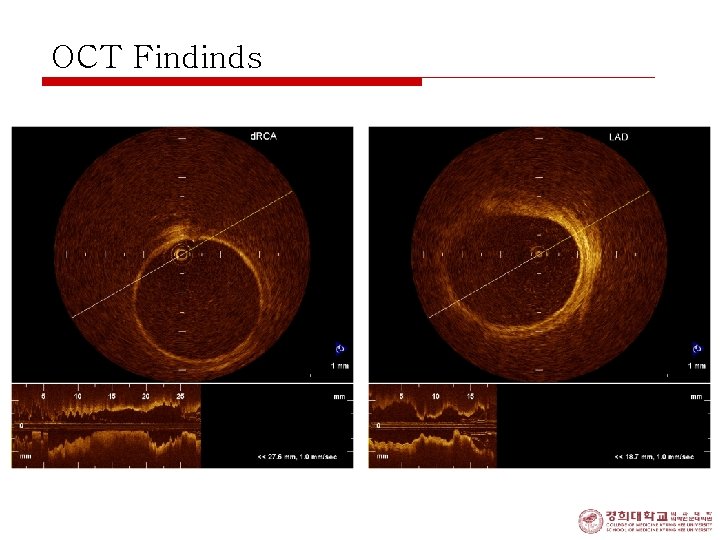
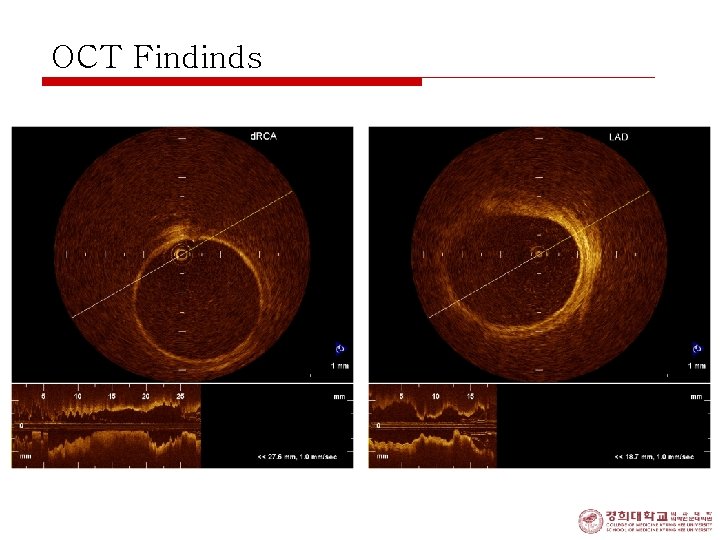
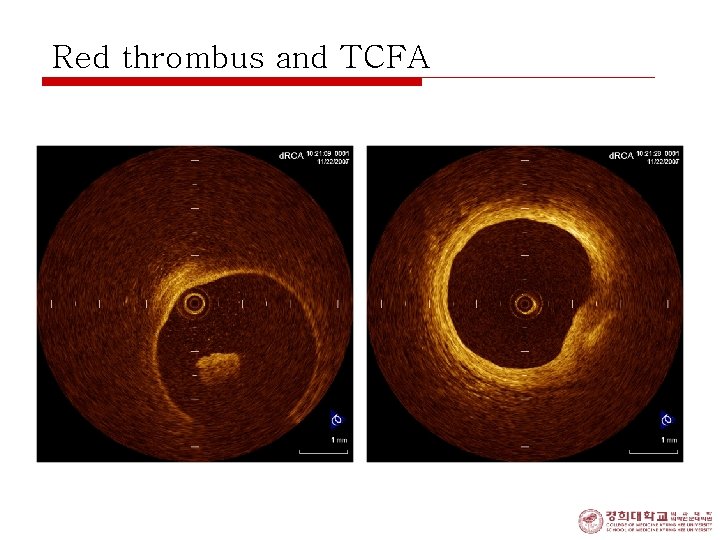
OCT Findinds
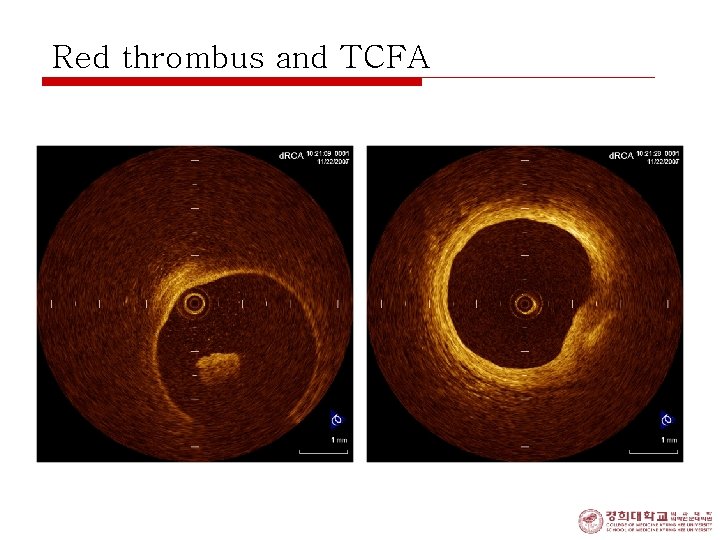
Red thrombus and TCFA

Check the thickness! 200 um
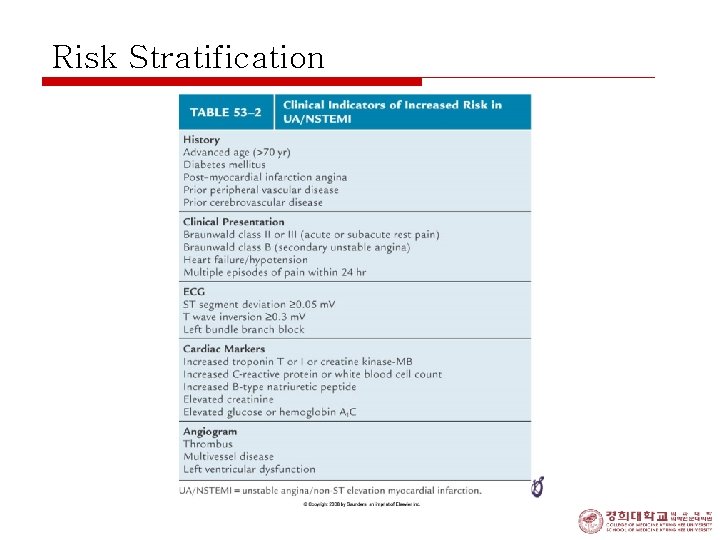
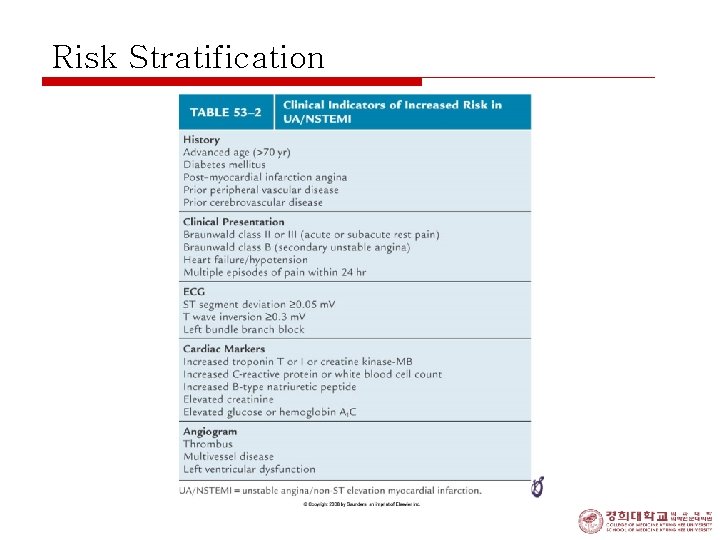
Risk Stratification
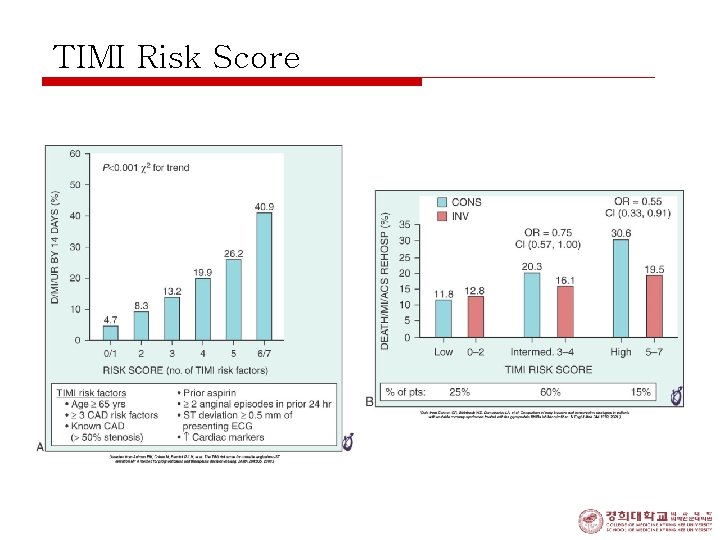
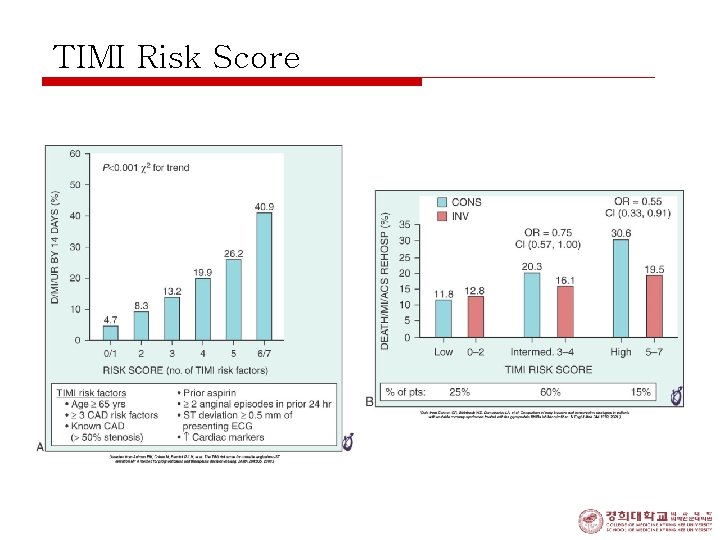
TIMI Risk Score
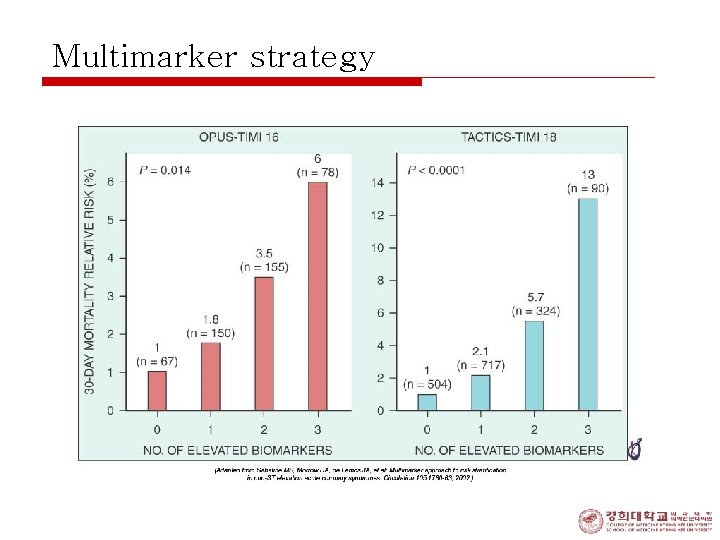
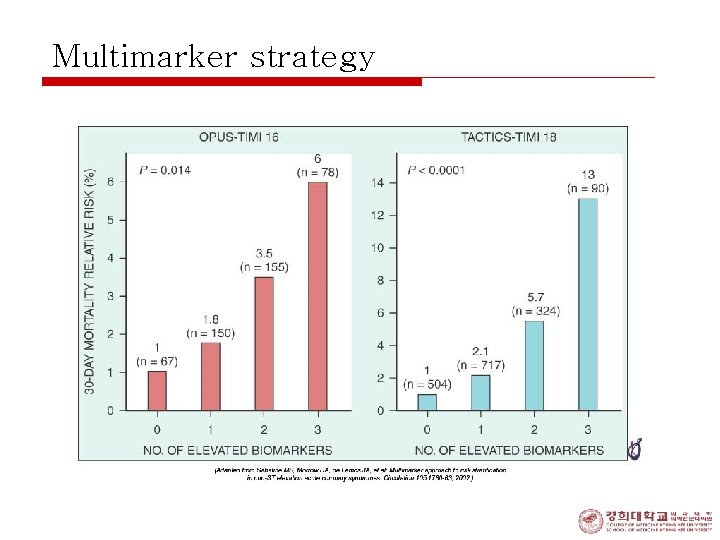
Multimarker strategy
Treatment (I) o Risk stratification; divided into 3 groups o high, intermediate, and low risk of death or nonfatal MI in short term n interventions; 1. to control pain 2. to reduce myocardial oxygen demand 3. to increase myocardial oxygen supply
Treatment (II) o High risk group: 1. 2. 3. 4. 5. 6. 7. prolonged (>20 min) rest angina recurrent angina cardiac failure; depressed LV function new systolic murmur hypotension wide spread ≥ 1 mm of ST segment change positive markers (troponin I or T)
Treatment (III) 1. General managements: 1) admitted, rest, sedated, and reassured 2) vigorously treated those intensify ischemia o tachycardia, hypertension, DM, cardiomegaly, heart failure, arrhythmias, thyrotoxicosis, and febrile illness 3) R/O MI 4) ECG monitoring
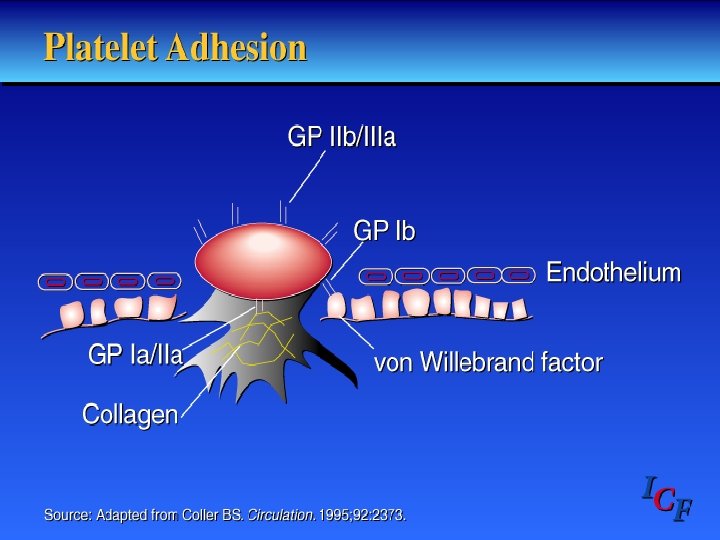
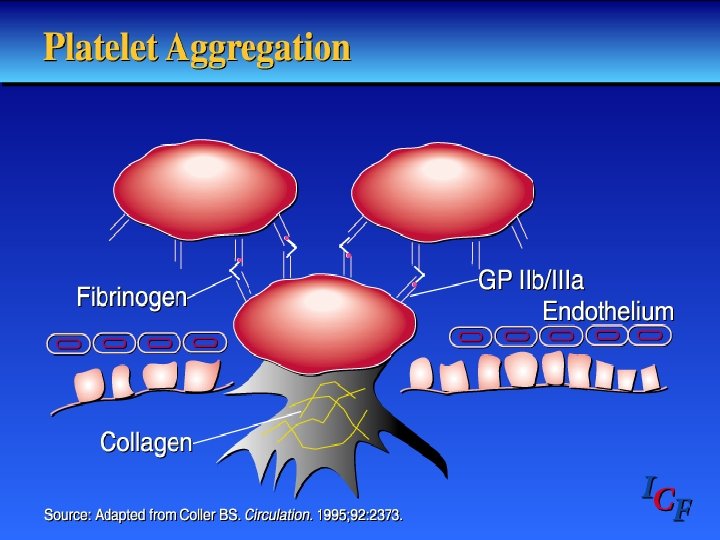
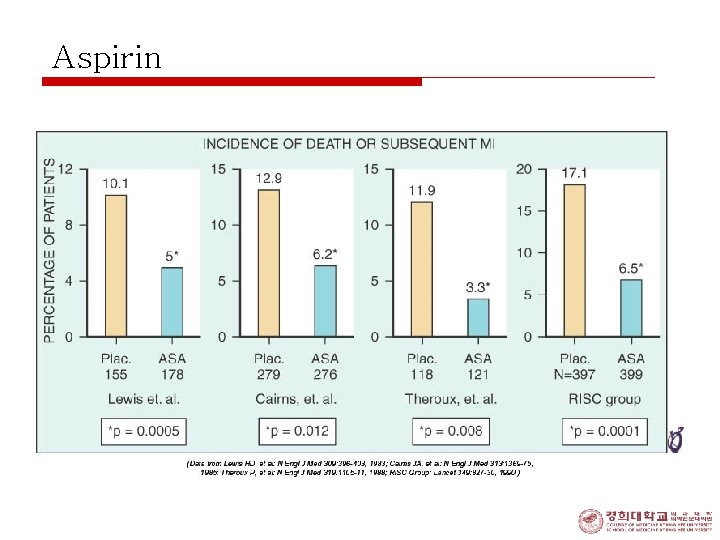
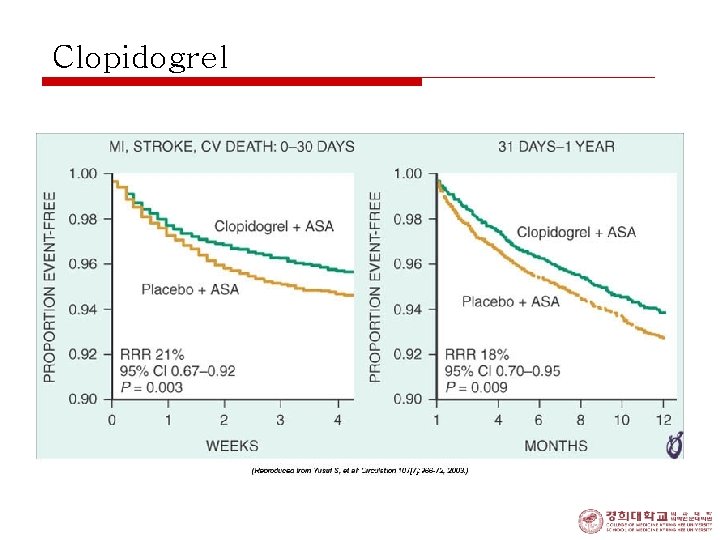
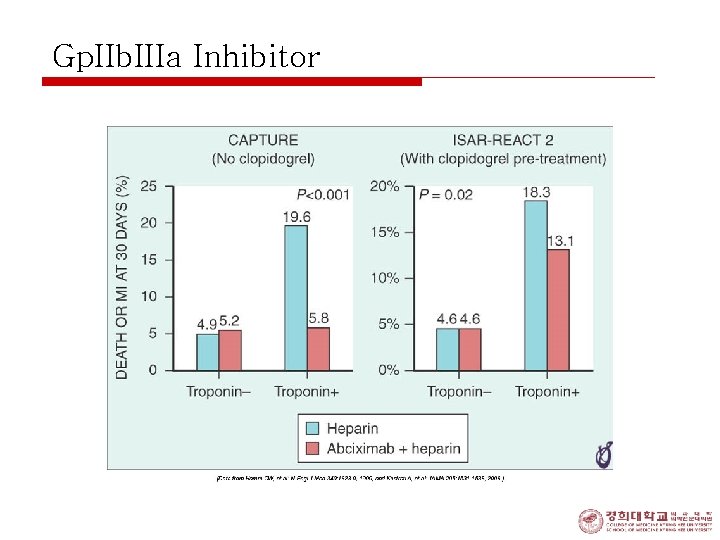
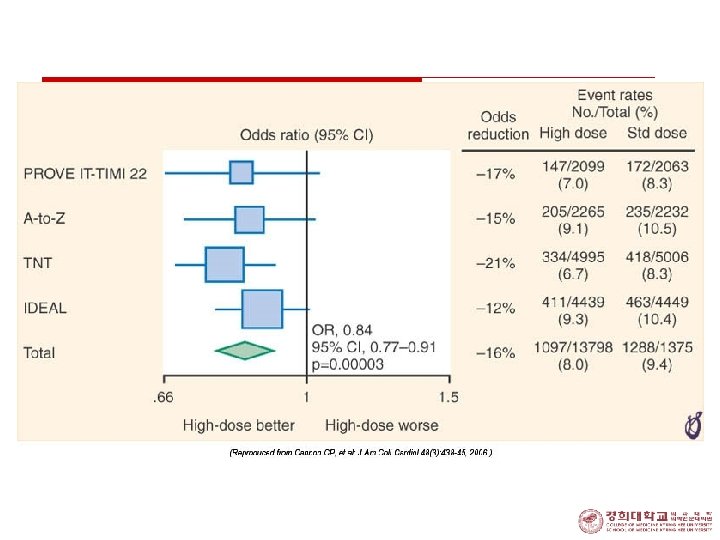
Treatment (IV) - Antithrombotic therapy: n Oral antiplatelet agents: o oral aspirin 162 -325 mg/day followed by 75162 mg/day or o clopidogrel loading 300 mg followed by 75 mg/day n i. v. Antiplatelet Tx. o Gp IIb/IIIa receptor blocker; high-risk group n Abciximab n Epifibatide n Tirofiban
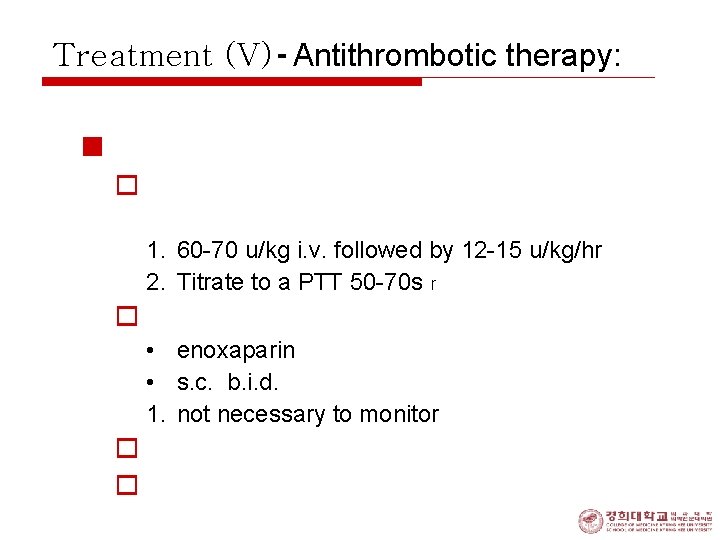
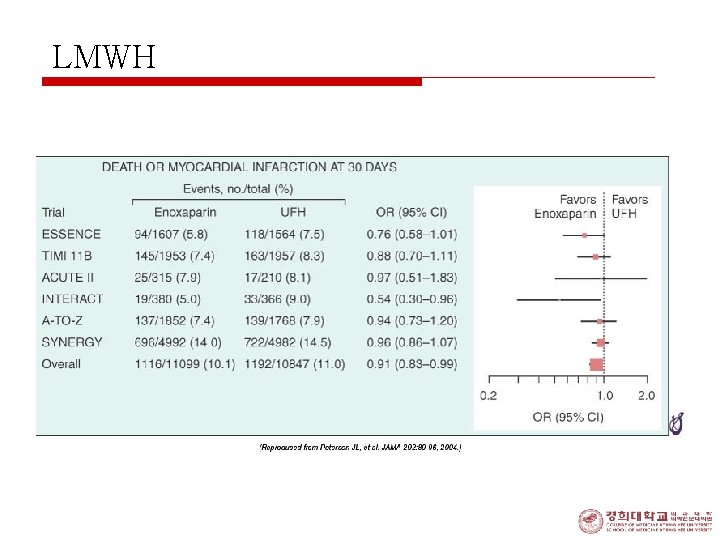
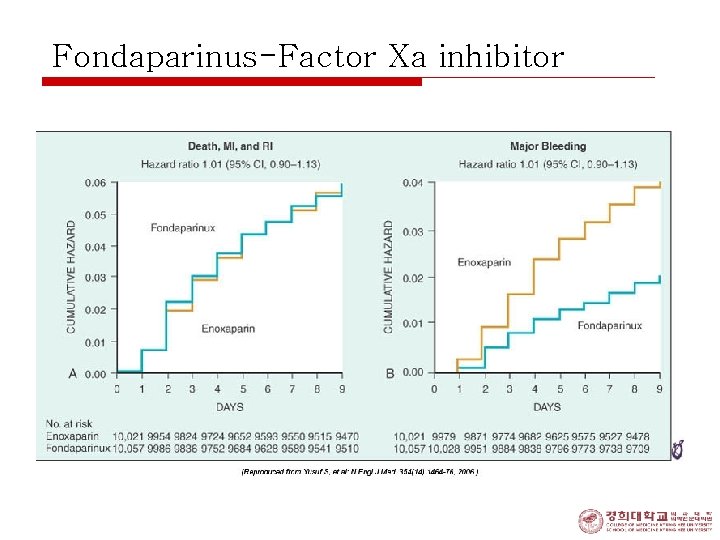
Treatment (V) - Antithrombotic therapy: n Heparins: . o heparin; conventonal, unfractionated (UFH) 1. 60 -70 u/kg i. v. followed by 12 -15 u/kg/hr 2. Titrate to a PTT 50 -70 s r o low-molecular weight heparin(LMWH) • enoxaparin • s. c. b. i. d. 1. not necessary to monitor o Fondaparinux o Bivlirudin
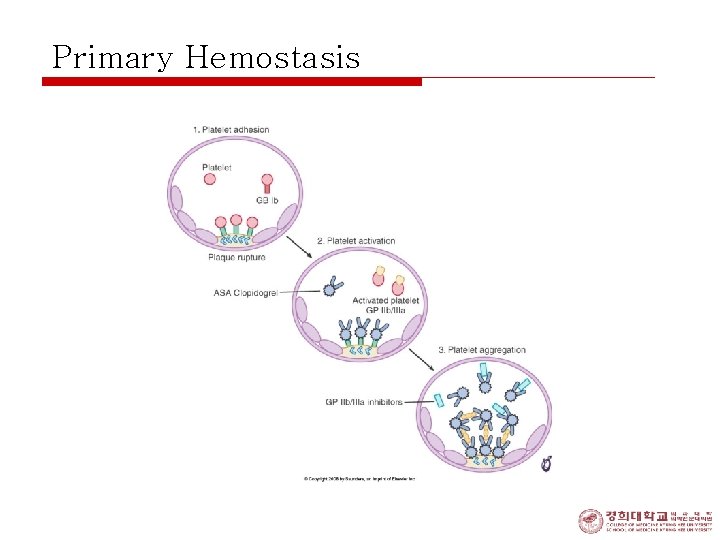
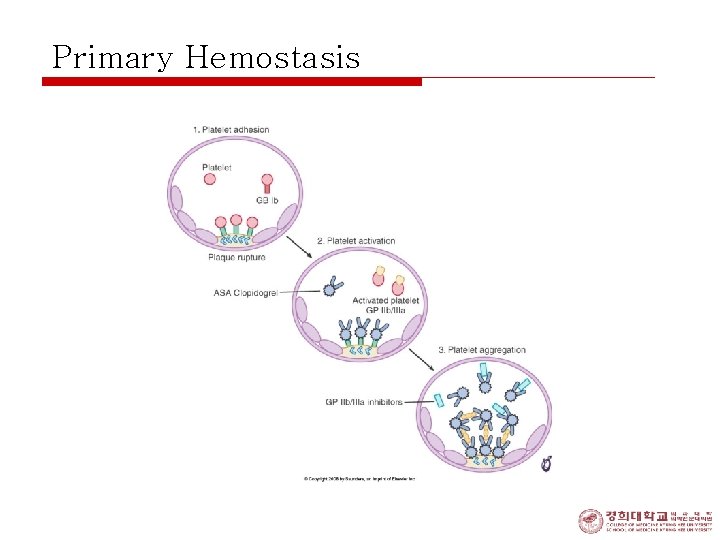
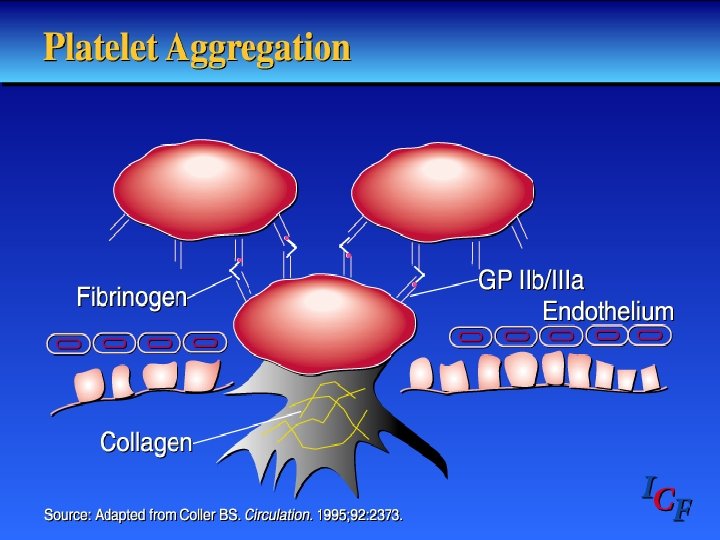
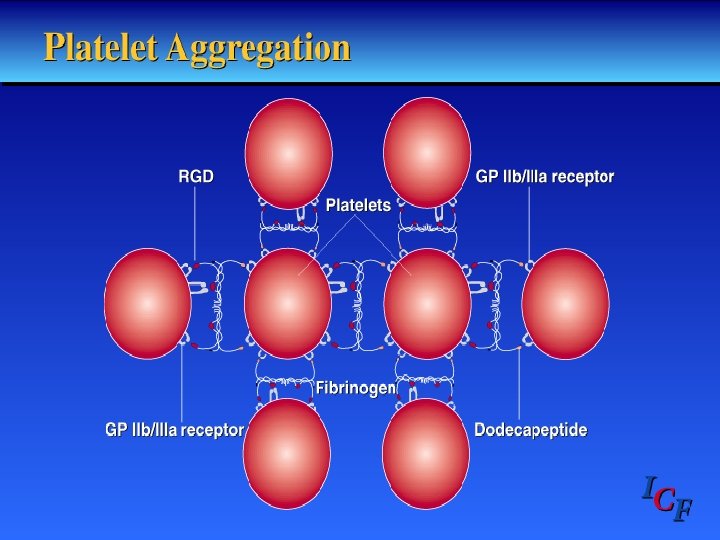
Primary Hemostasis
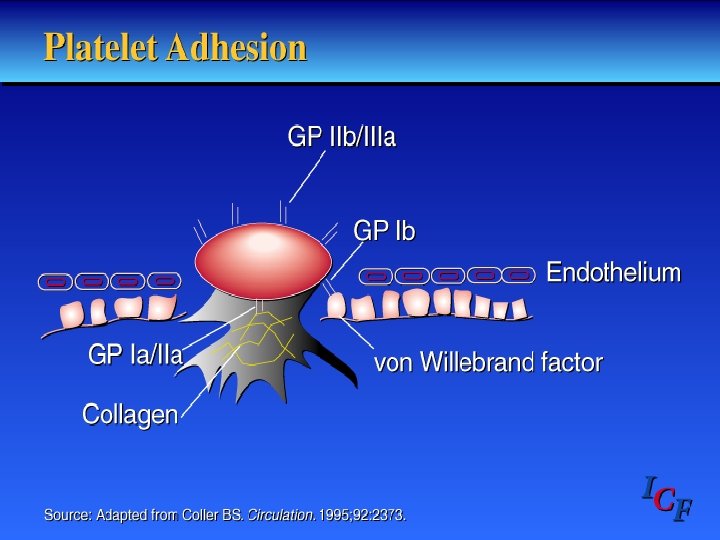


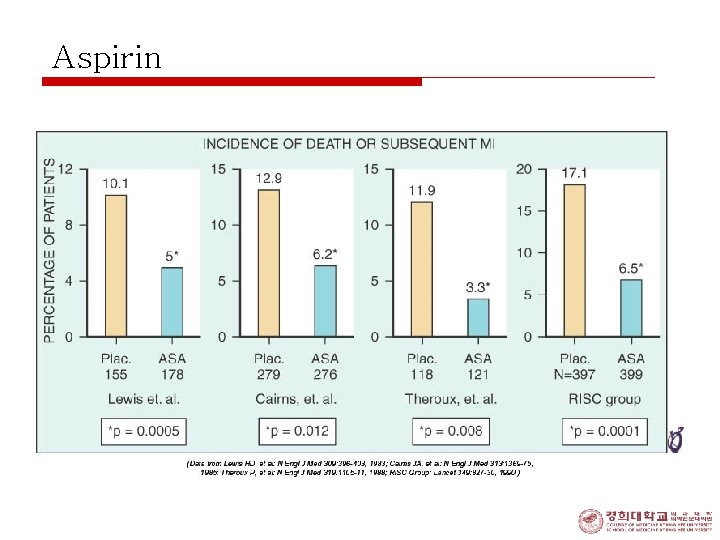
Aspirin
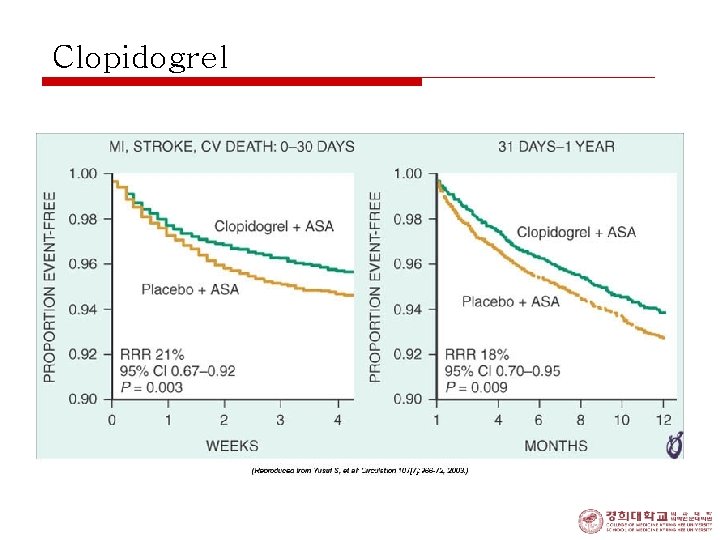
Clopidogrel
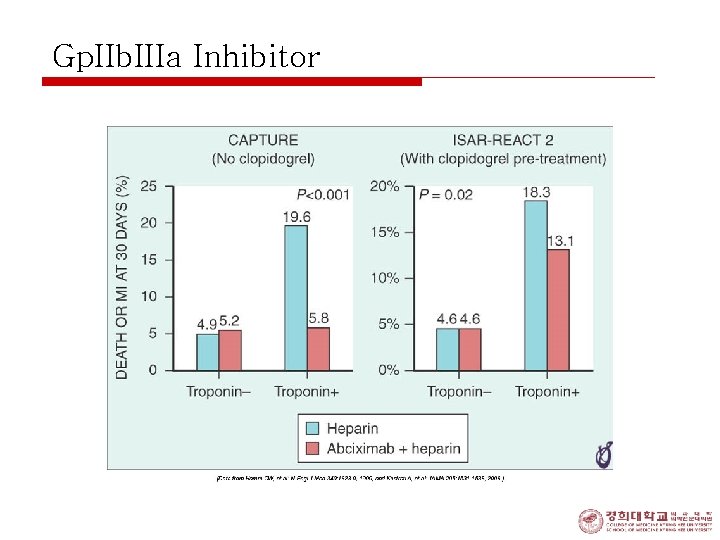
Gp. IIb. IIIa Inhibitor
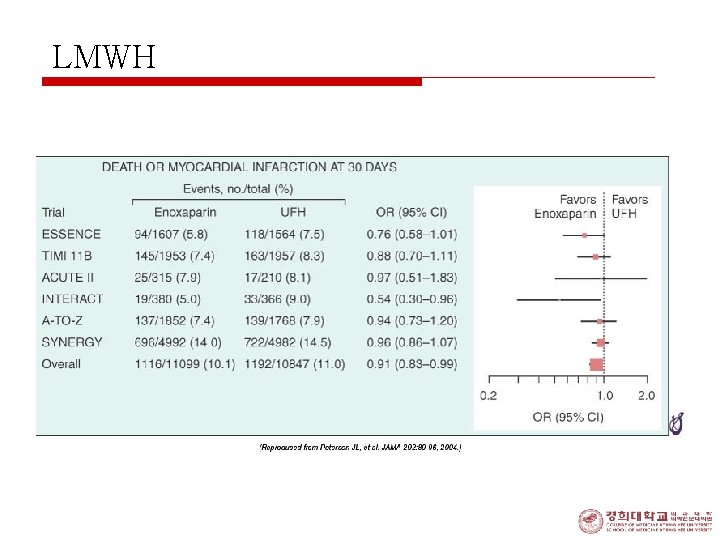
LMWH
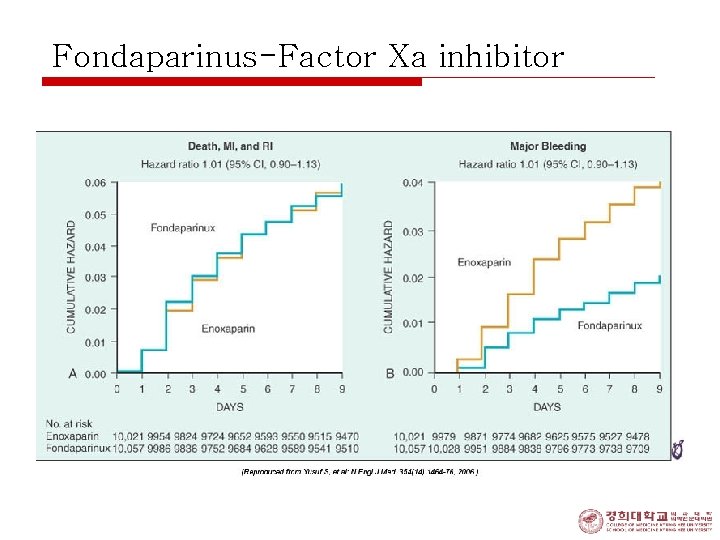
Fondaparinus-Factor Xa inhibitor


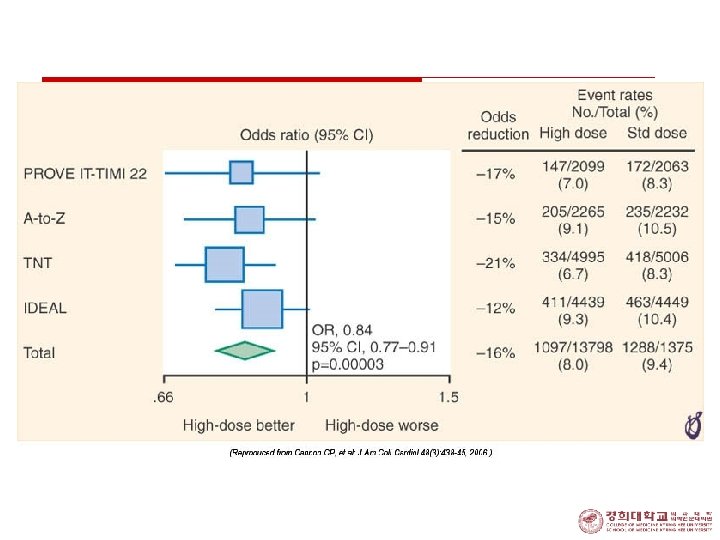
Treatment (VI) 3. Antiischemic therapy 1) beta blocker; should be administered • target of 50 to 60 beats/min 2) IV nitroglycerin; quite effective • • Increments to level at chest pain is abolished Sublingual NIG; needed for symptom relief 3) Calcium antagonist; with caution o Short acting nifedipine; never be used o Might increase the risk of MI
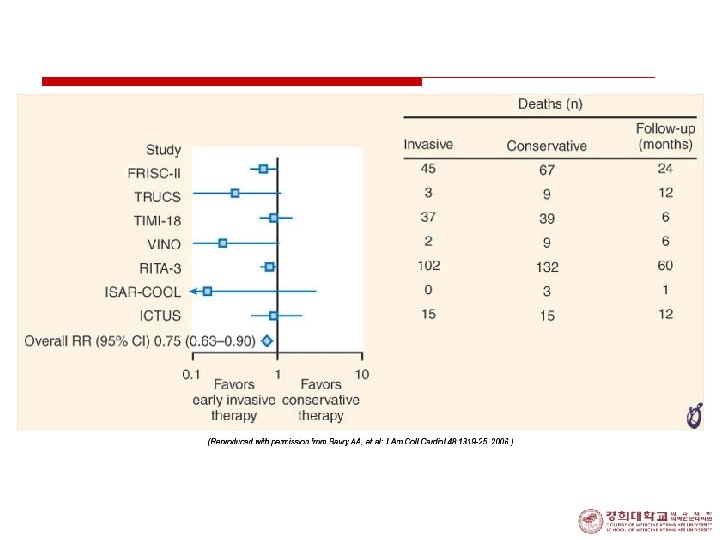
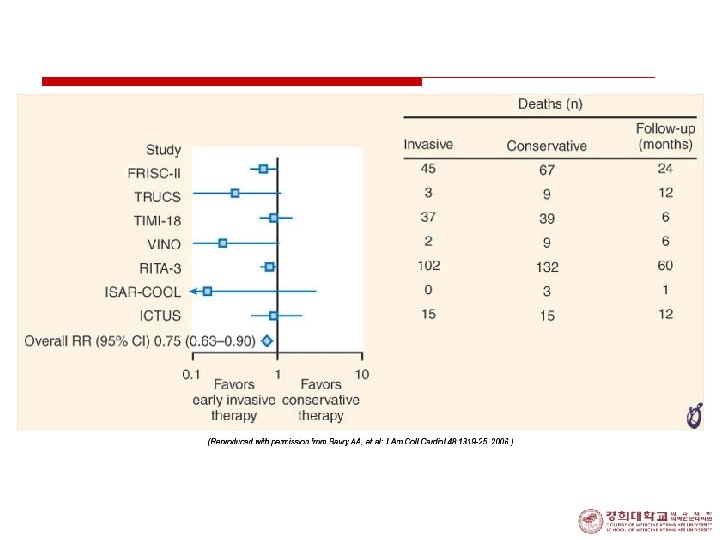
Treatment (VI) 4. Class I Indication for Invasive Strategy 1. Recurrent angina at rest/low-level activity despite Rx. 2. Elevated Tn. I or Tn. T 3. New ST depression 4. Rec. angina/ischemia with CHF sx, rales, MR 5. Positive stress test 6. EF < 0. 40 7. Decreased BP 8. Sustained VT 9. PCI < 6 mo, prior CABG
Prinzmetal’s (Variant) Angina o uncommon form of unstable angina o recurrent, prolonged attacks caused by episodic focal spasm of epicardial artery o in ¾; mild or mederately severe fixed obstruction within 1 cm of spasm o often in smoker and in younger patients
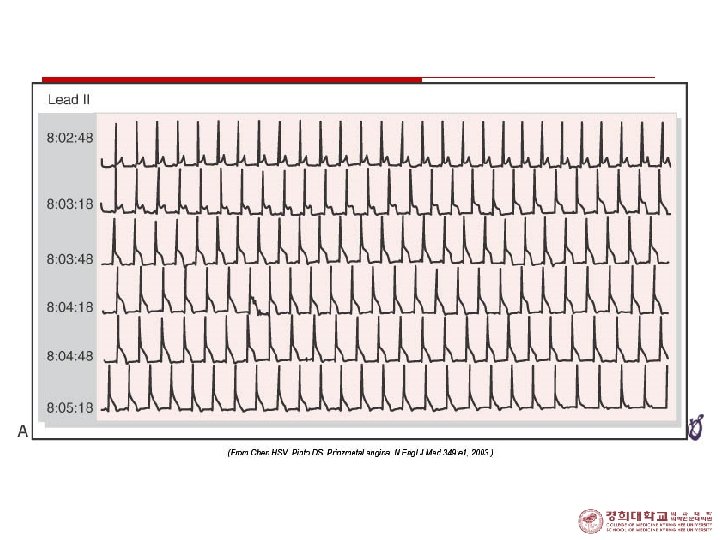
Prinzmetal’s (Variant) Angina o Raynaud’s phenomenon, migraine in some patients o usually occurs at rest, sometimes awaken from sleep, associated with transient, multileads ST elevation o ECG n episodic ST segment elevation with pain n Asymptomatic ST segment elevation n Transient conduction disturbance
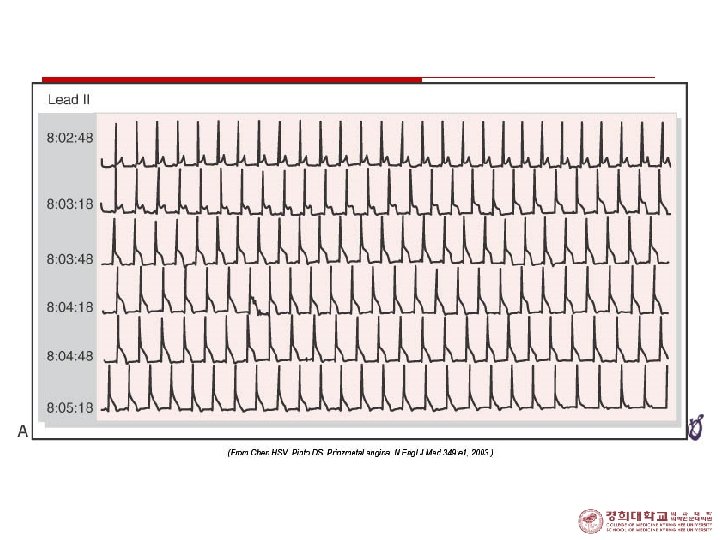
Prinzmetal’s(Variant) Angina o Confirm Diagnosis; • detecting transient spasm by provocative stimulus (i. c. ACH or ergonovine, hyperventilation) on CAG o Long-term survival; excellent n survival at 5 years is excellent (~90 to 95%) o Complications; • disabling pain, MI, VT, AV block, syncope, rarely sudden death
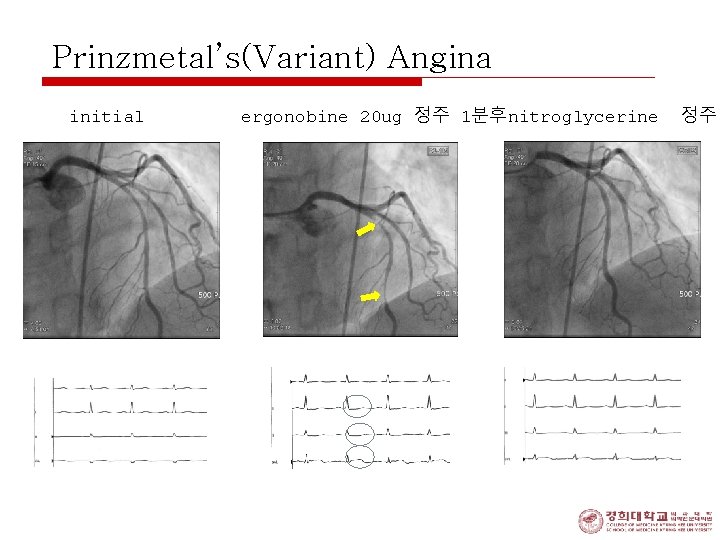
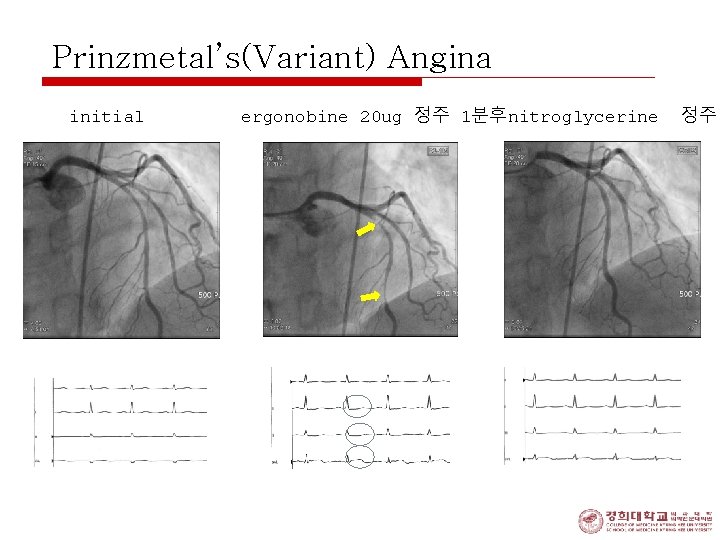
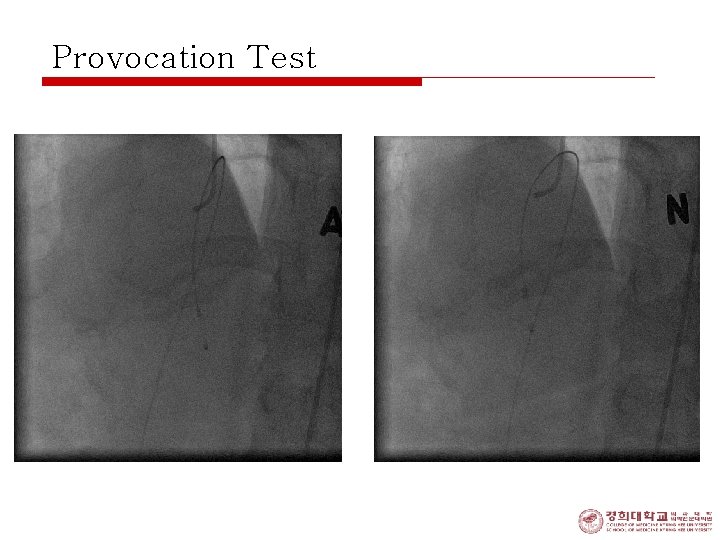
Prinzmetal’s(Variant) Angina initial ergonobine 20 ug 정주 1분후nitroglycerine 정주
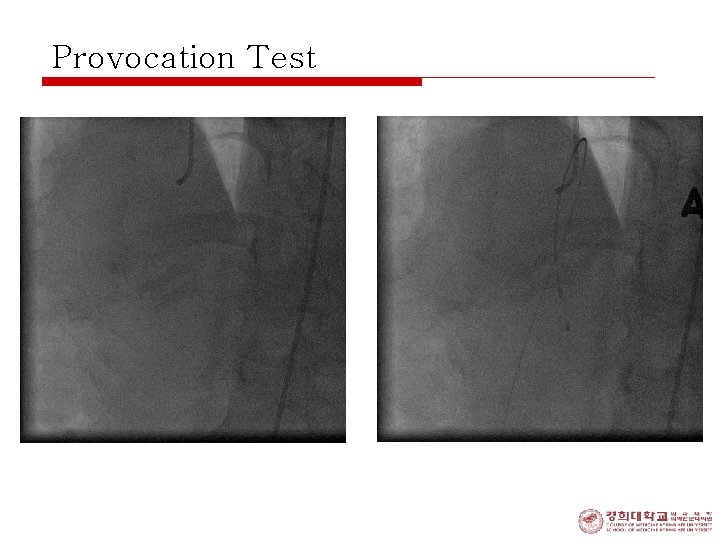
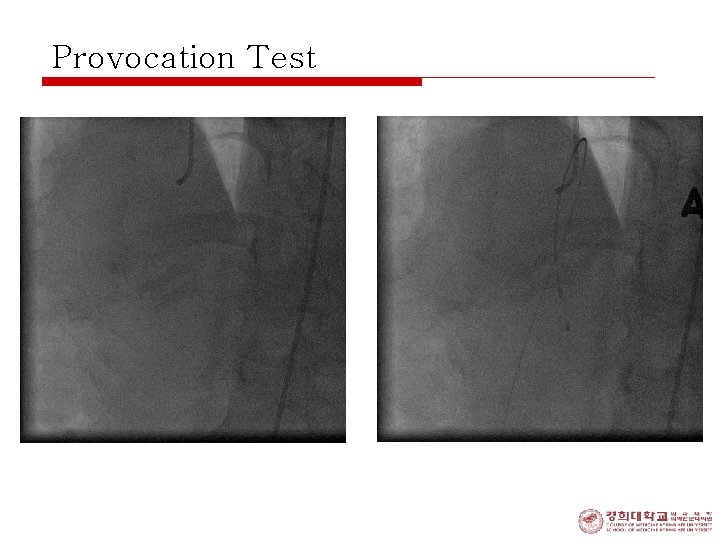
Provocation Test
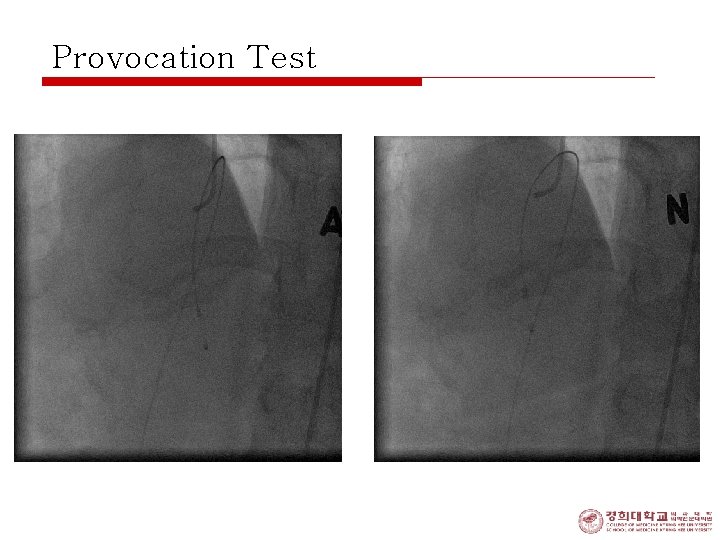
Provocation Test
Prinzmetal’s(Variant) Angina o Treatment; • in acute attack: multiple doses of sublingual NIG, i. v. NIG, short-acting nifedipine • in chronic state: long-acting nitrates and calcium antagonists, little value of beta blocker • revascularization; : helpful in severe discrete obstructive lesion