SYSTEMIC LUPUS ERYTHEMATOSUS OUTLINE Definition Epidemiology Pathophysiology Classification





- Slides: 45
SYSTEMIC LUPUS ERYTHEMATOSUS
OUTLINE • • Definition Epidemiology Pathophysiology Classification and diagnosis Clinical Features Lupus related syndromes Treatment Prognosis
DEFINITION • Inflammatory autoimmune disorder affecting multiple organ systems characterized by the production of autoantibodies directed against cell nuclei”
EPIDEMIOLOGY • Prevalence influenced by age, gender, race, and genetics • • • Prevalence: 1: 2000 Peak incidence 14 -45 years Black > White (1: 250 vs. 1: 1000) Female predominance 10: 1 HLA DR 3 association, Family History • Severity is equal in male and female
Etiology • Genetic (HLA DR 3 association) • Abnormal immune response • Environmental • UV • Viruses • Hormones (Estrogen)
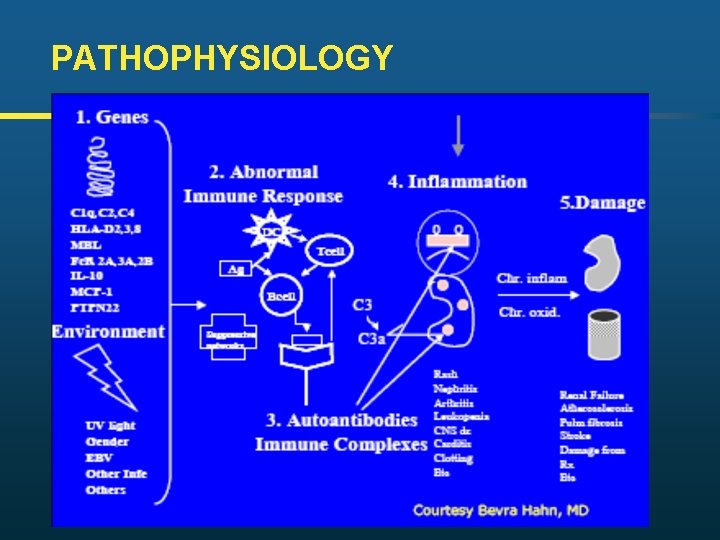
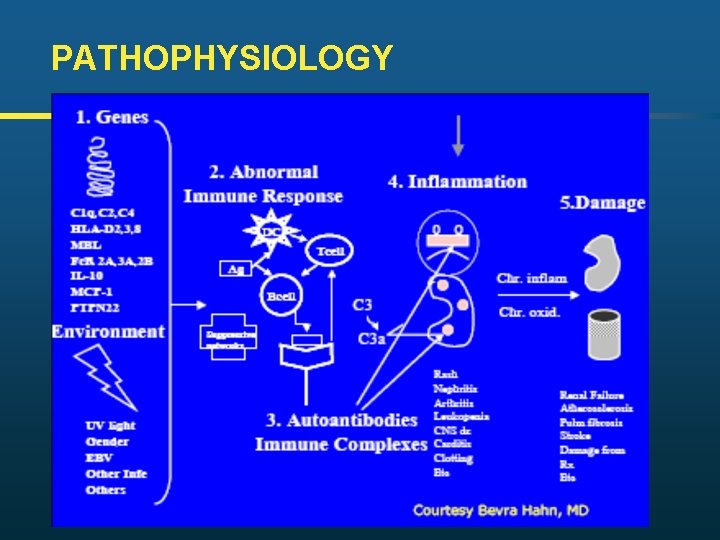
PATHOPHYSIOLOGY
CLINICAL FEATURES: Mucocutaneous • • Malar Rash (butterfly erythema) Discoid rash Photosensitive rash Subacute cutaneous LE Livedo reticularis Alopecia Raynaud’s • • Vasculitic ulceration Oral ulceration Nasal septal perforation Nailfold capillary changes
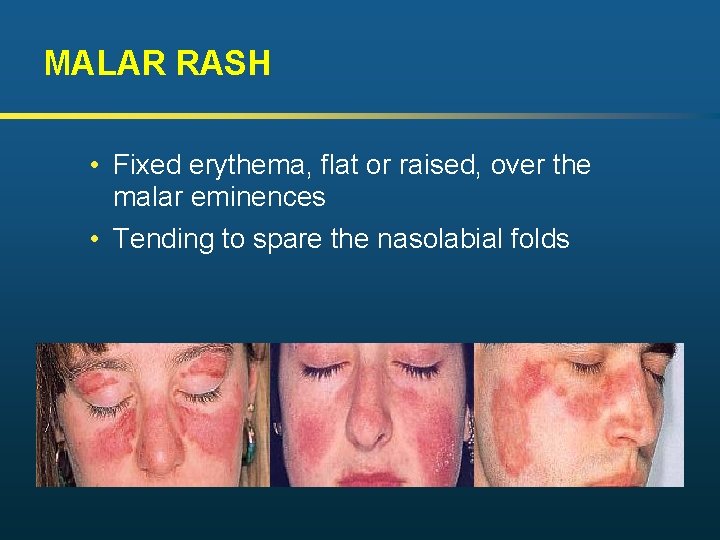
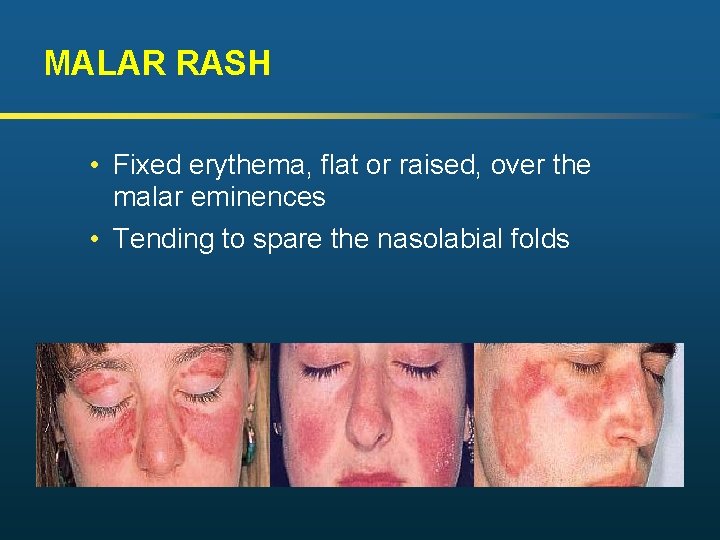
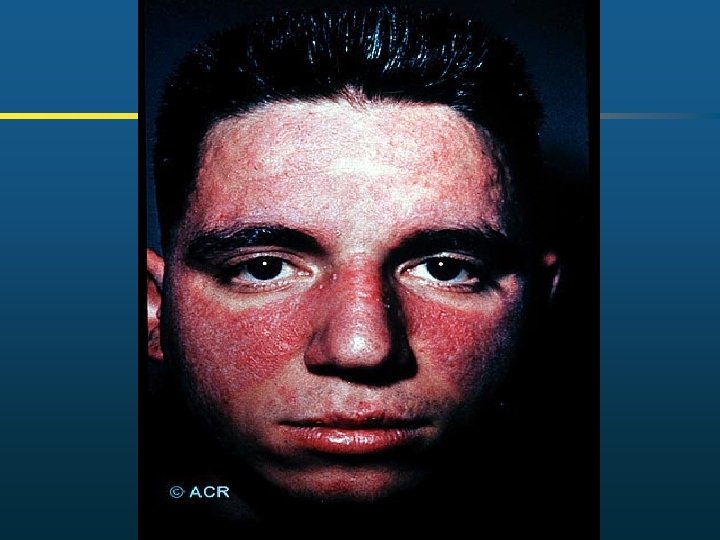
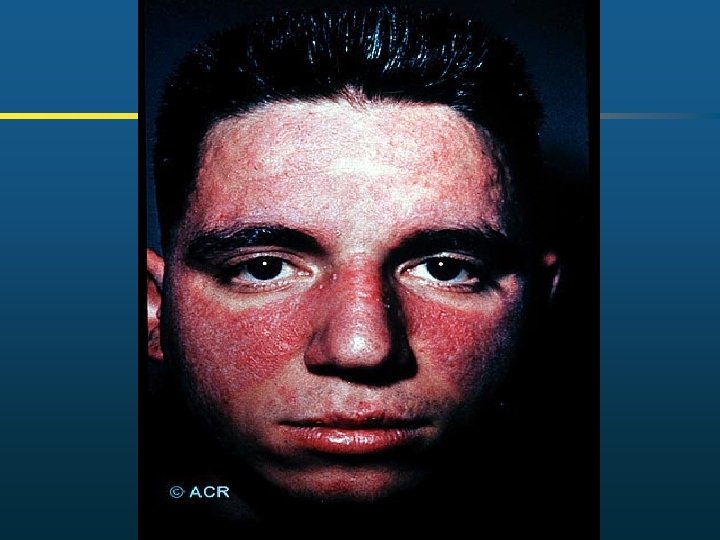
MALAR RASH • Fixed erythema, flat or raised, over the malar eminences • Tending to spare the nasolabial folds

DISCOID RASH • Erythematous raised patches with adherent keratotic scaling and follicular plugging; • Atrophic scarring may occur in older lesions
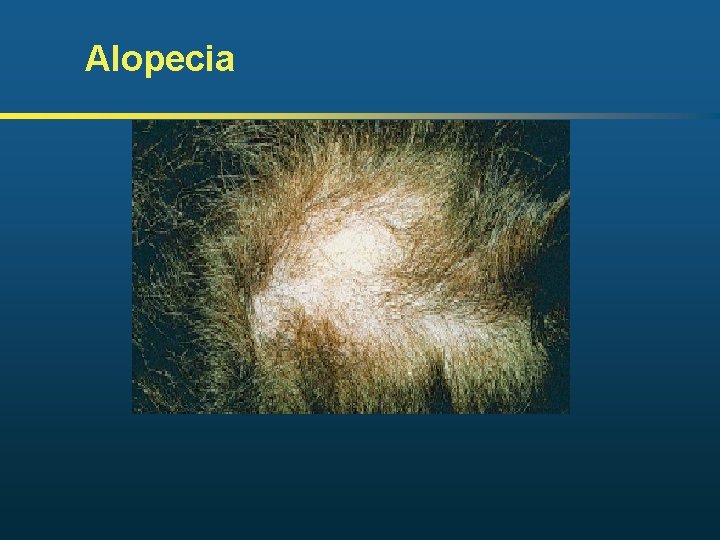
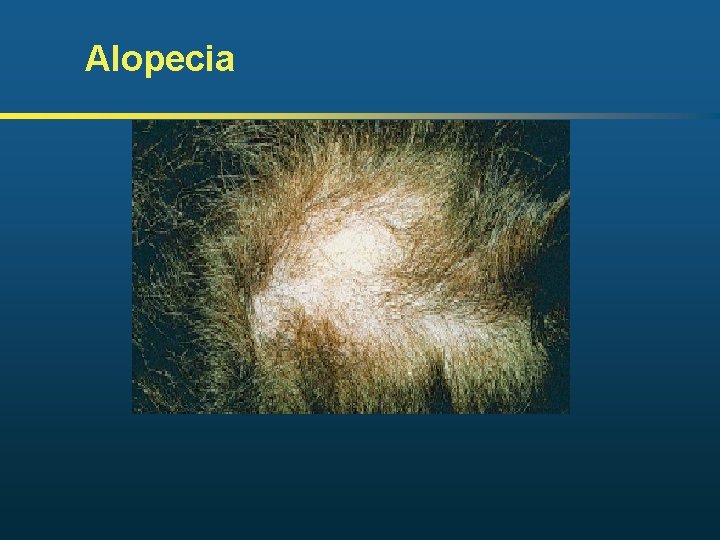
Alopecia
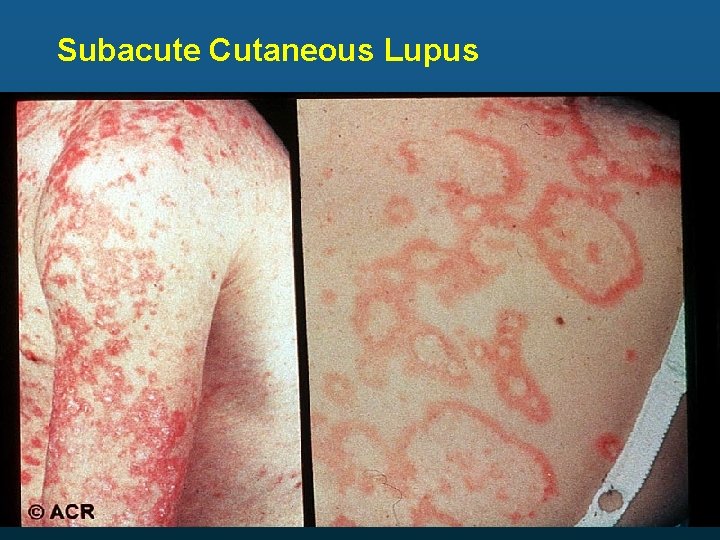
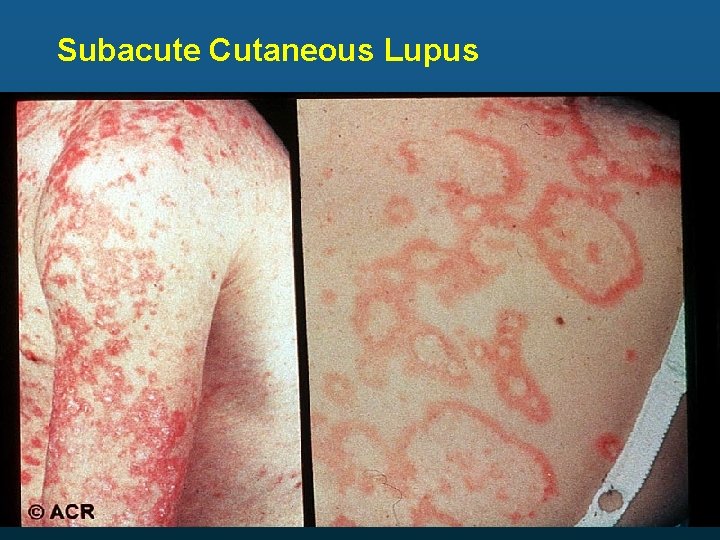
Subacute Cutaneous Lupus


Acute Cutaneous: Malar Rash Note Sparing of Nasolabial Folds Chronic Cutaneous: Discoid Note Scarring, Hyperpigmentation

Follicular Plugging ACR Livedo Reticularis
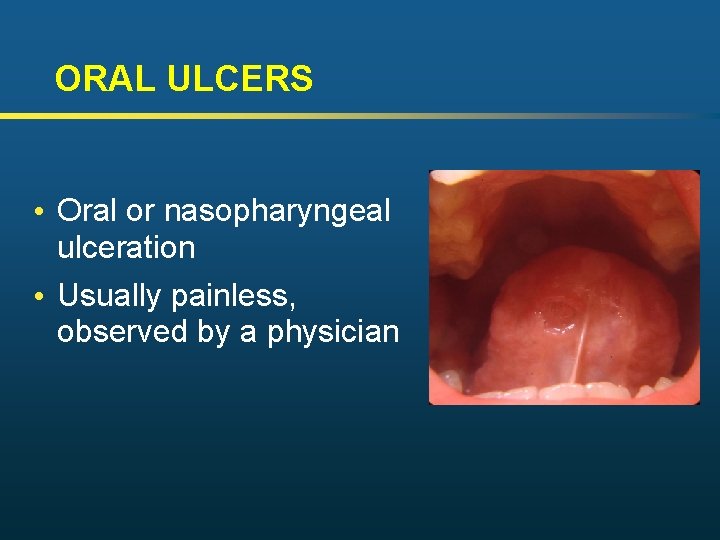
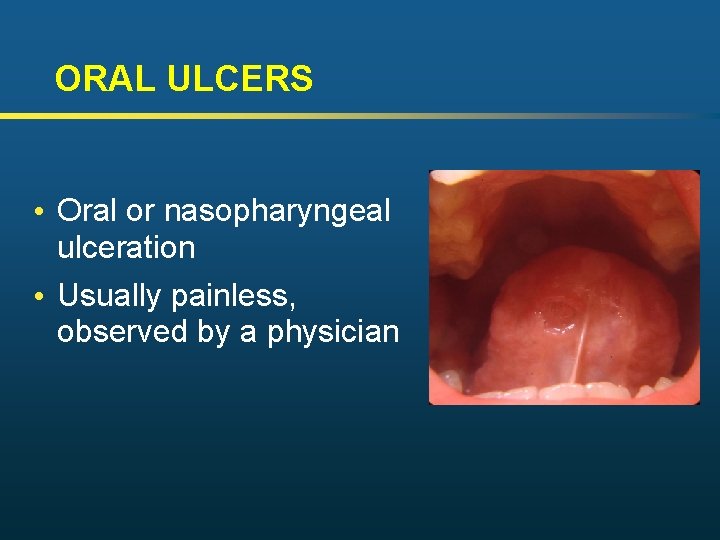
ORAL ULCERS • Oral or nasopharyngeal ulceration • Usually painless, observed by a physician
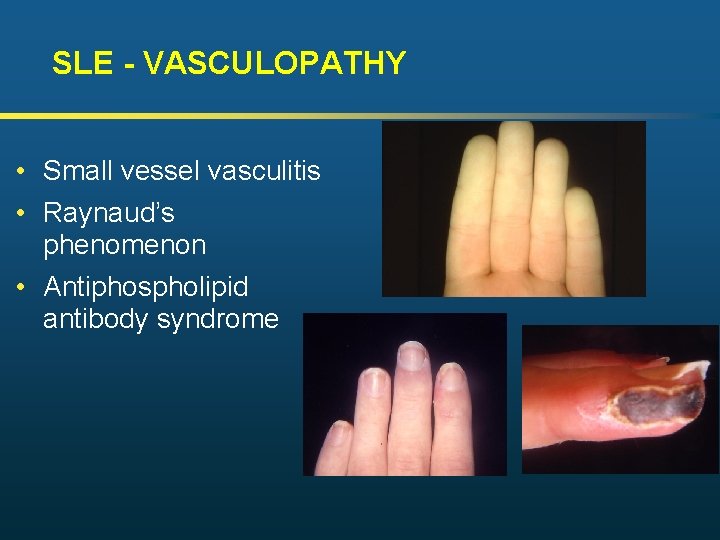
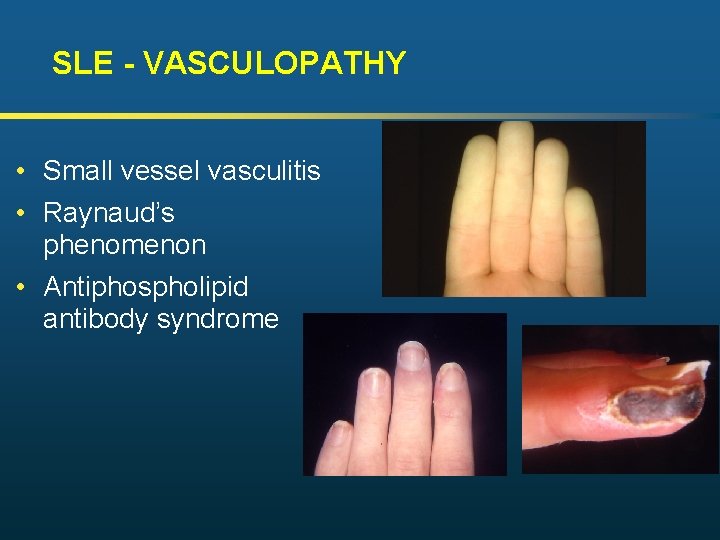
SLE - VASCULOPATHY • Small vessel vasculitis • Raynaud’s phenomenon • Antiphospholipid antibody syndrome
CLINICAL FEATURES: Musculoskeletal • Arthritis is NONEROSIVE, transient, symmetrical, affecting small joints, seldom deforming, less severe than RA • Most common presenting feature of SLE

Jaccoud’s Arthopathy: Nonerosive, Reducible Deformities
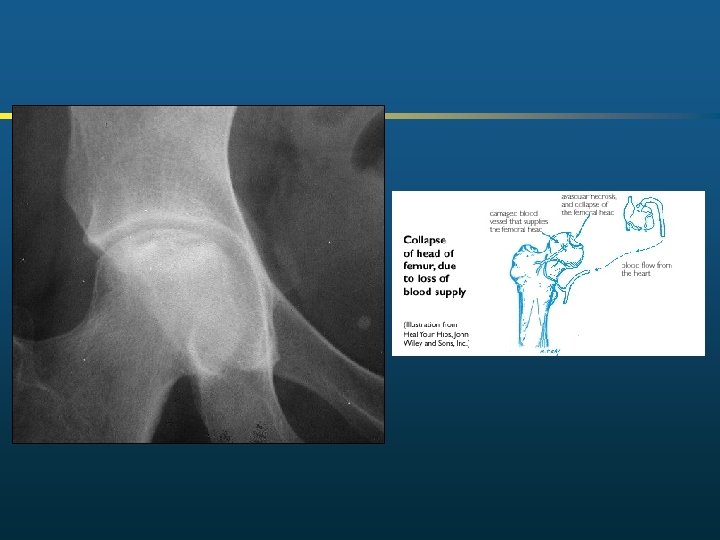
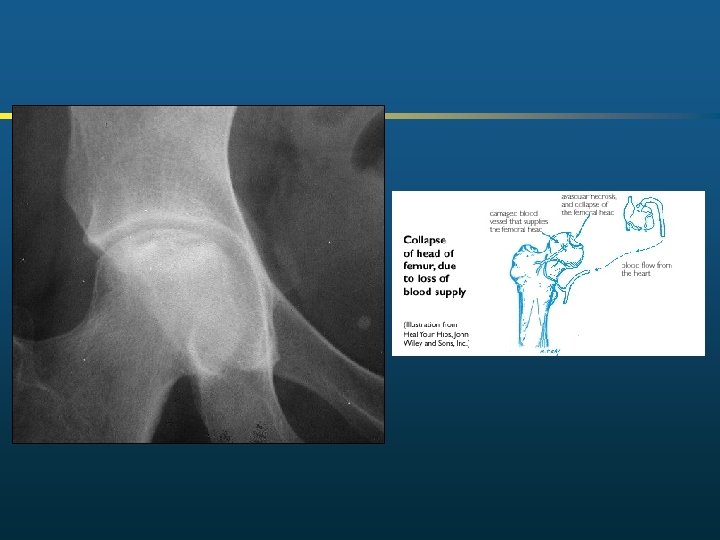
CLINICAL FEATURES: Musculoskeletal • Synovitis-90% patients, often the earliest sign • Osteoporosis • From SLE itself and therapy (usually steroids) • Osteonecrosis (avascular necrosis) • Can occur with & without history of steroid therapy
CLINICAL FEATURES: Ocular • • • Conjunctivitis Photophobia Monocular blindness-transient or permanent Blurred vision Cotton-Wool spots on retina-degeneration nerves fibers due to occlusion retinal blood vessels
CLINICAL FEATURES: PLEUROPULMONAR • • • Pleuritis/Pleural effusion Infiltrates/ Discoid Atelectasis Acute lupus pneumonitis Pulmonary hemorrhage “Shrinking lung” - diaphragm dysfunction Restrictive lung disease
CLINICAL FEATURES: Cardiac • • • Pericarditis –in majority of patients Libman Sacks endocarditis Cardiac failure Cardiac Arrythmias-common Valvular heart disease Coronary Artery Disease
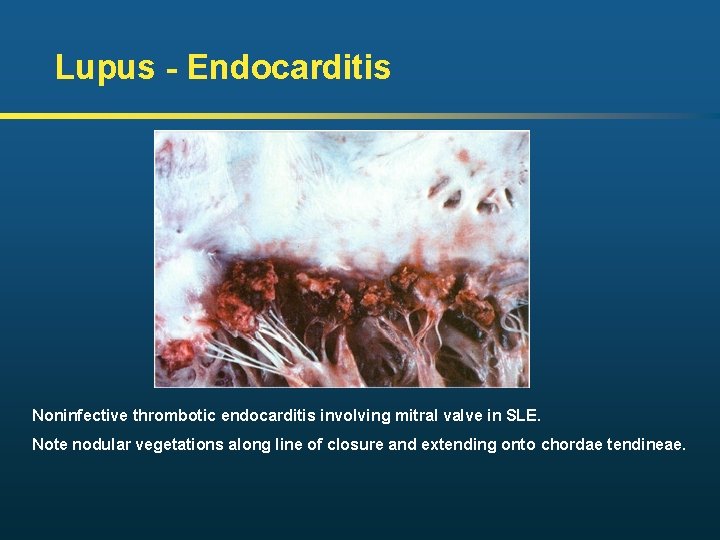
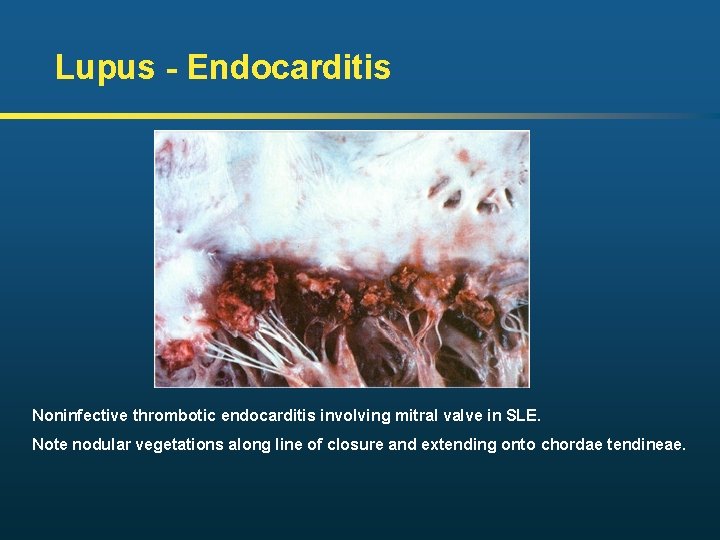
Lupus - Endocarditis Noninfective thrombotic endocarditis involving mitral valve in SLE. Note nodular vegetations along line of closure and extending onto chordae tendineae.
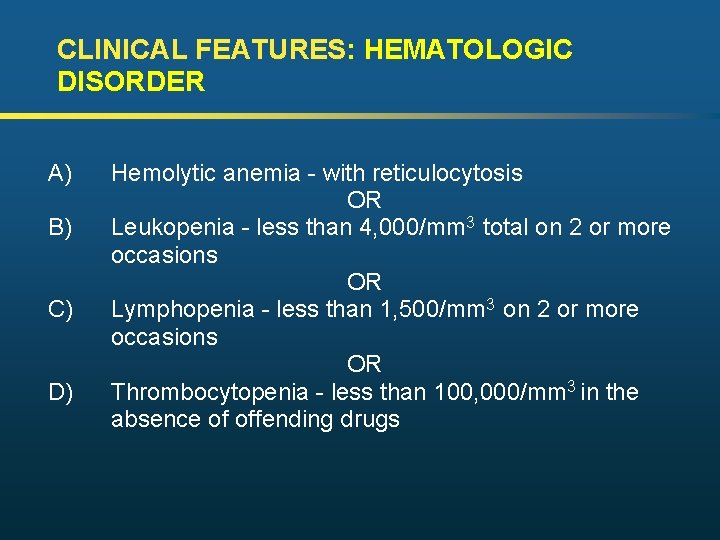
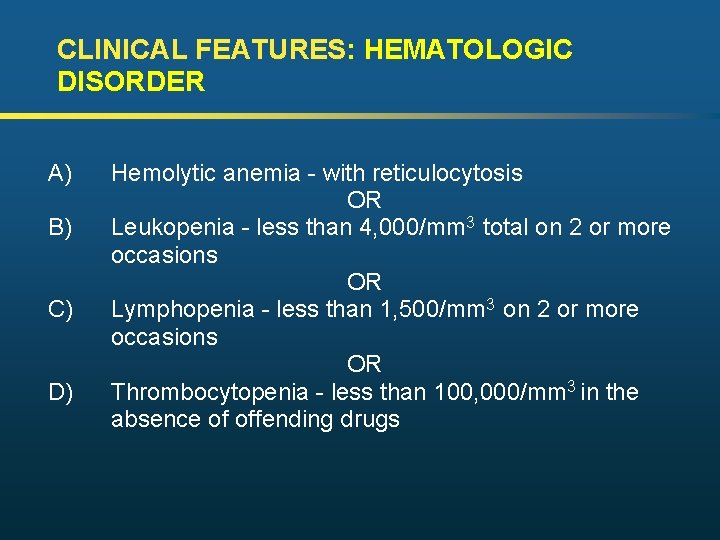
CLINICAL FEATURES: HEMATOLOGIC DISORDER A) B) C) D) Hemolytic anemia - with reticulocytosis OR Leukopenia - less than 4, 000/mm 3 total on 2 or more occasions OR Lymphopenia - less than 1, 500/mm 3 on 2 or more occasions OR Thrombocytopenia - less than 100, 000/mm 3 in the absence of offending drugs
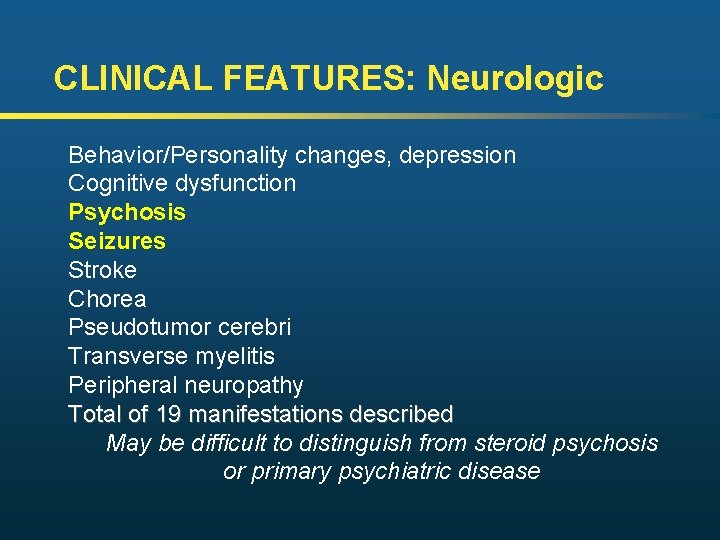
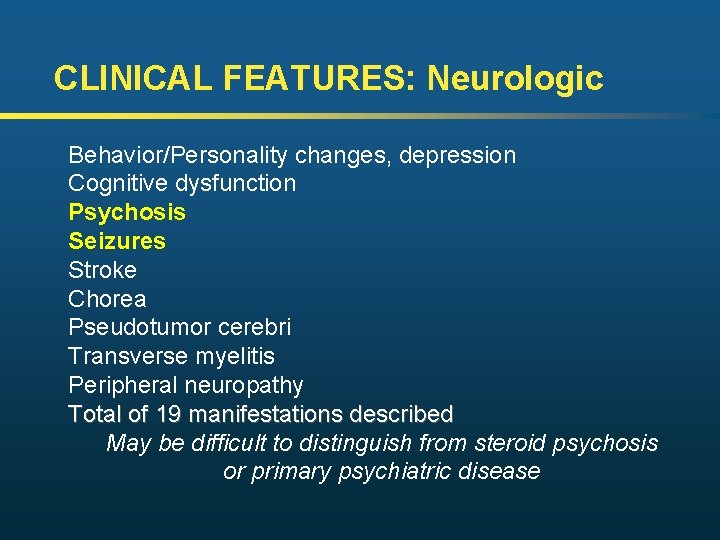
CLINICAL FEATURES: Neurologic Behavior/Personality changes, depression Cognitive dysfunction Psychosis Seizures Stroke Chorea Pseudotumor cerebri Transverse myelitis Peripheral neuropathy Total of 19 manifestations described May be difficult to distinguish from steroid psychosis or primary psychiatric disease
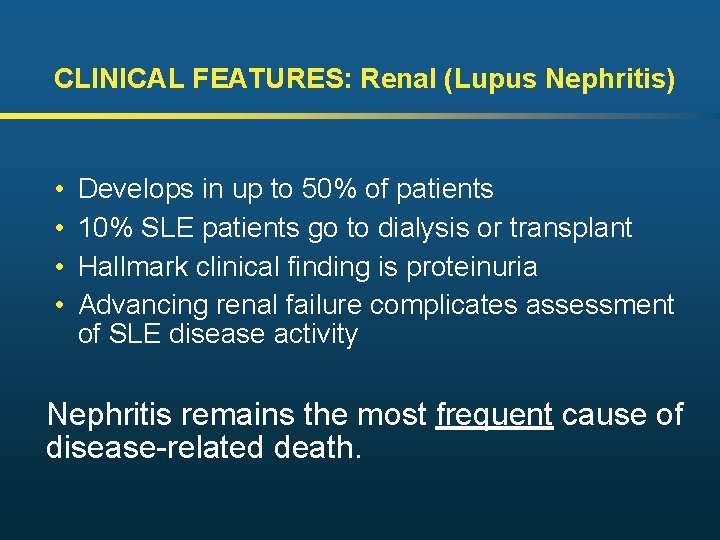
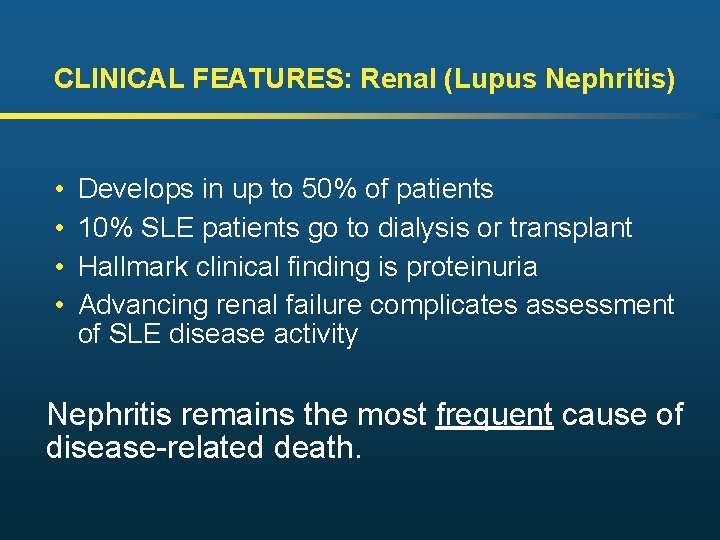
CLINICAL FEATURES: Renal (Lupus Nephritis) • • Develops in up to 50% of patients 10% SLE patients go to dialysis or transplant Hallmark clinical finding is proteinuria Advancing renal failure complicates assessment of SLE disease activity Nephritis remains the most frequent cause of disease-related death.
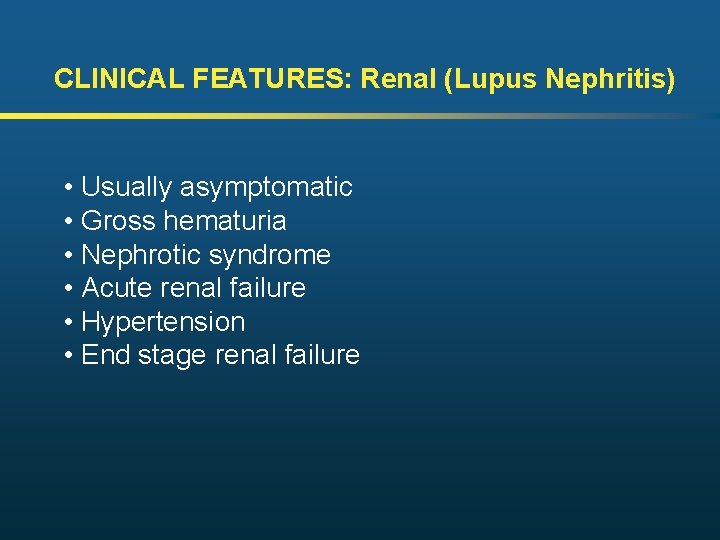
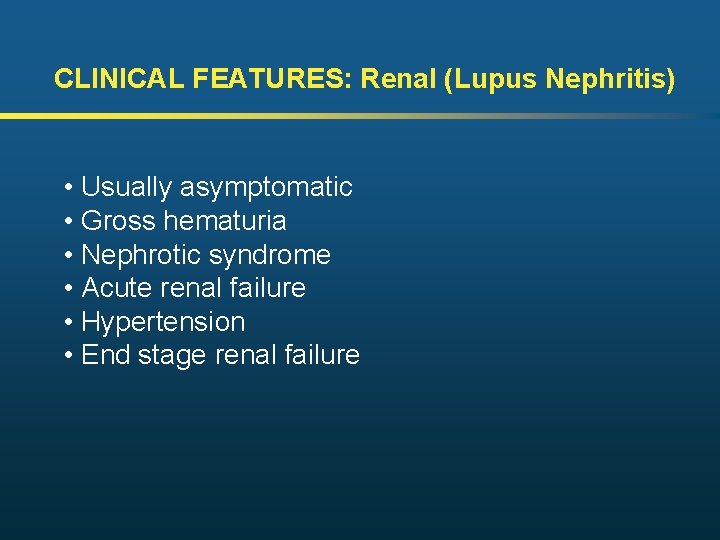
CLINICAL FEATURES: Renal (Lupus Nephritis) • Usually asymptomatic • Gross hematuria • Nephrotic syndrome • Acute renal failure • Hypertension • End stage renal failure
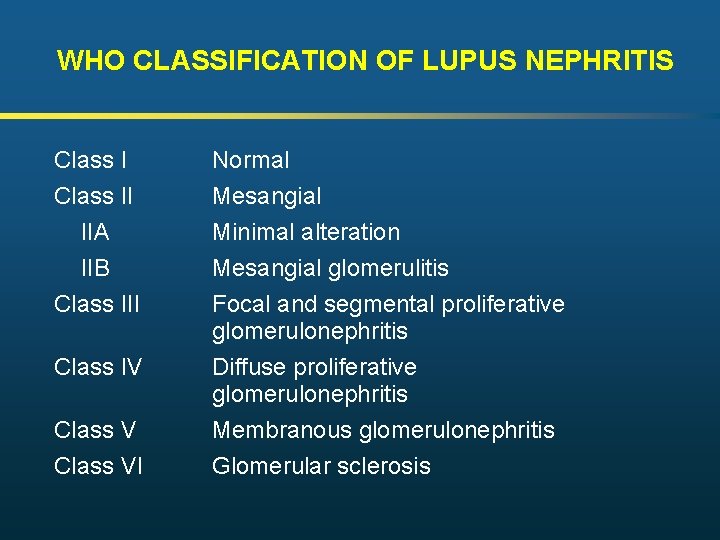
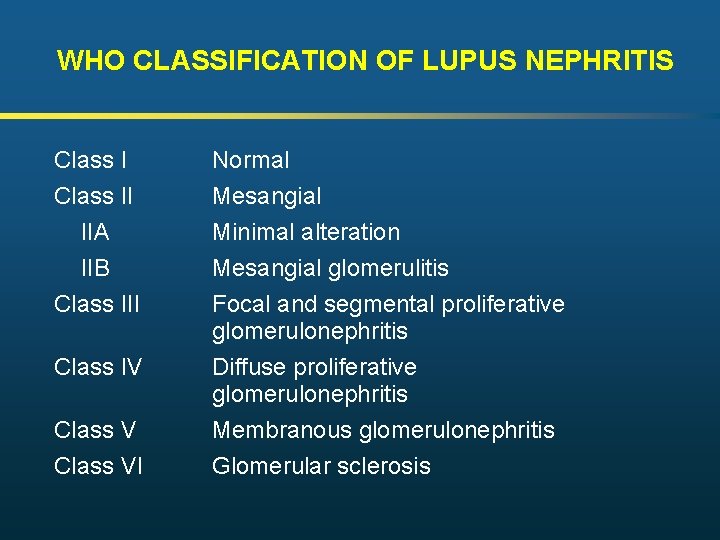
WHO CLASSIFICATION OF LUPUS NEPHRITIS Class I Normal Class II IIA IIB Class III Mesangial Minimal alteration Mesangial glomerulitis Focal and segmental proliferative glomerulonephritis Diffuse proliferative glomerulonephritis Membranous glomerulonephritis Glomerular sclerosis Class IV Class VI
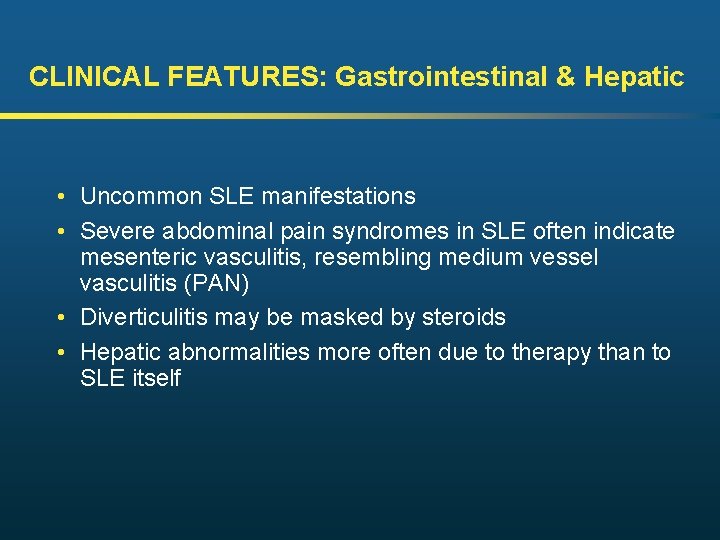
CLINICAL FEATURES: Gastrointestinal & Hepatic • Uncommon SLE manifestations • Severe abdominal pain syndromes in SLE often indicate mesenteric vasculitis, resembling medium vessel vasculitis (PAN) • Diverticulitis may be masked by steroids • Hepatic abnormalities more often due to therapy than to SLE itself
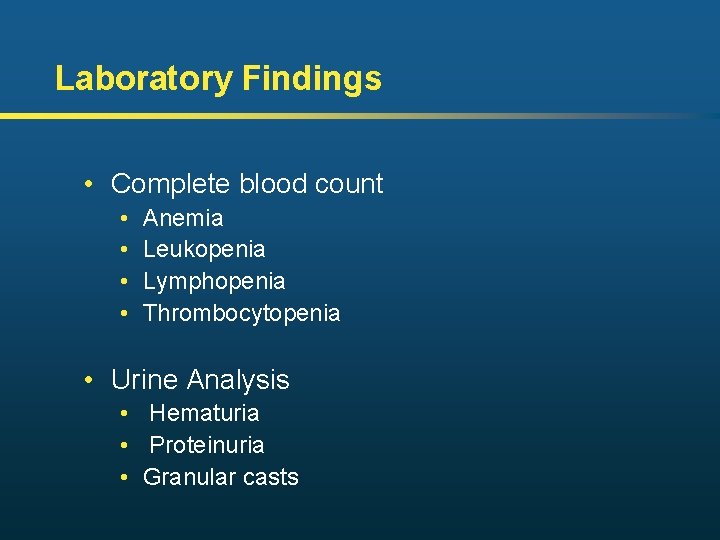
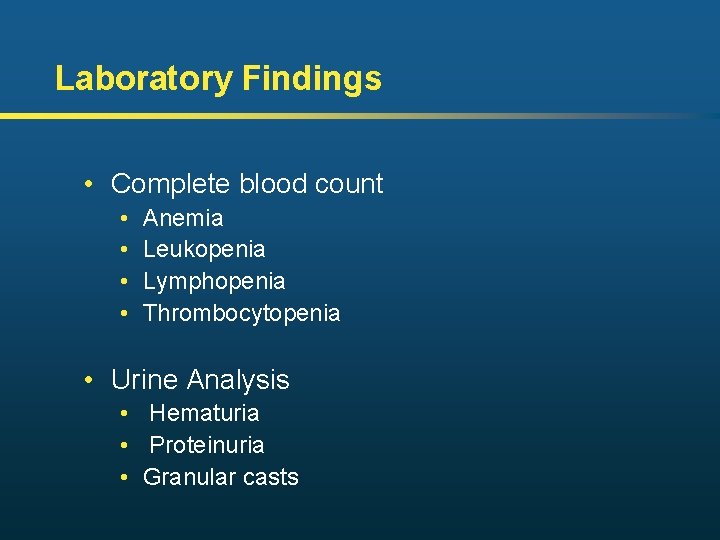
Laboratory Findings • Complete blood count • • Anemia Leukopenia Lymphopenia Thrombocytopenia • Urine Analysis • Hematuria • Proteinuria • Granular casts
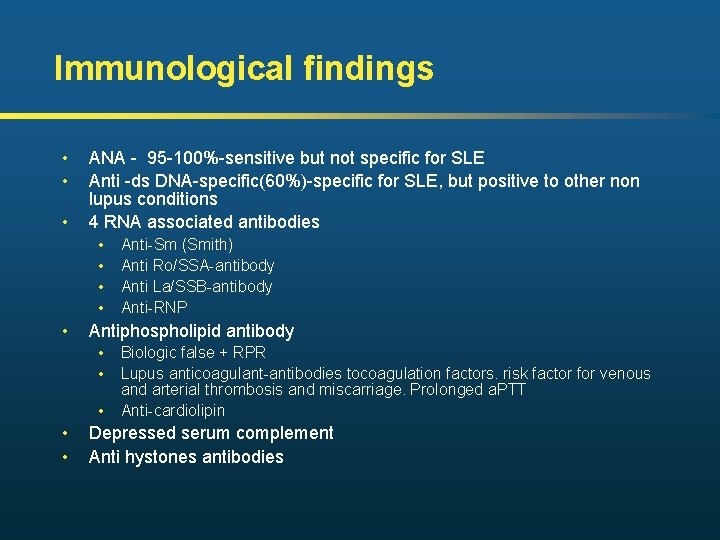
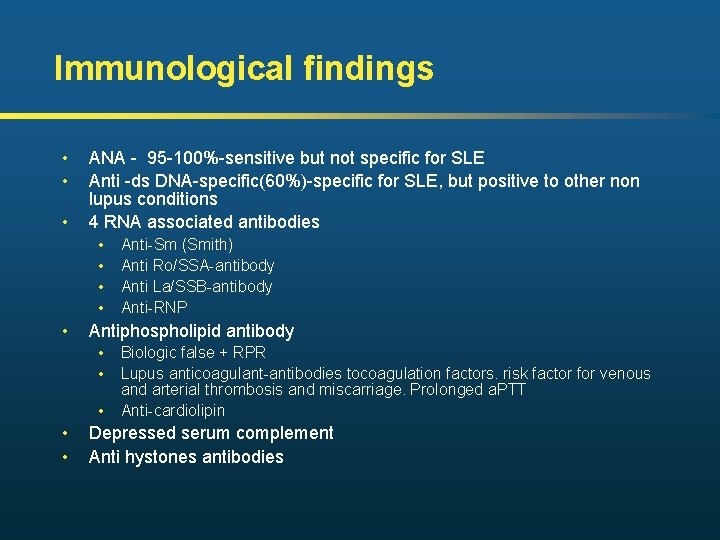
Immunological findings • • • ANA - 95 -100%-sensitive but not specific for SLE Anti -ds DNA-specific(60%)-specific for SLE, but positive to other non lupus conditions 4 RNA associated antibodies • • • Antiphospholipid antibody • • • Anti-Sm (Smith) Anti Ro/SSA-antibody Anti La/SSB-antibody Anti-RNP Biologic false + RPR Lupus anticoagulant-antibodies tocoagulation factors. risk factor for venous and arterial thrombosis and miscarriage. Prolonged a. PTT Anti-cardiolipin Depressed serum complement Anti hystones antibodies
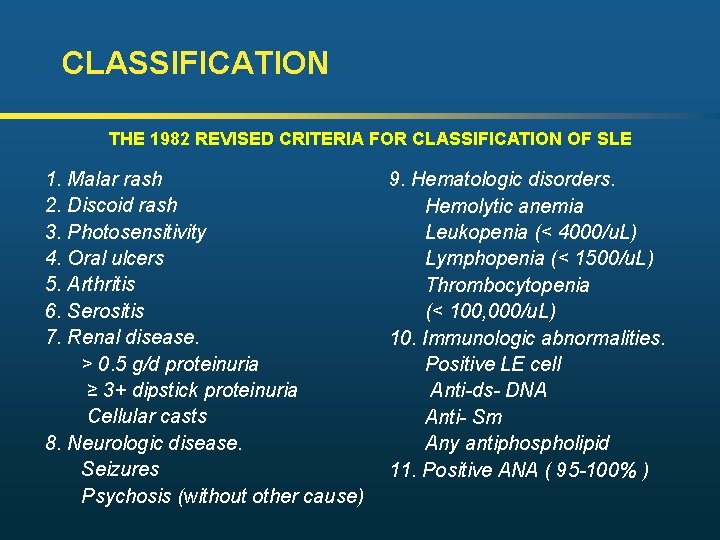
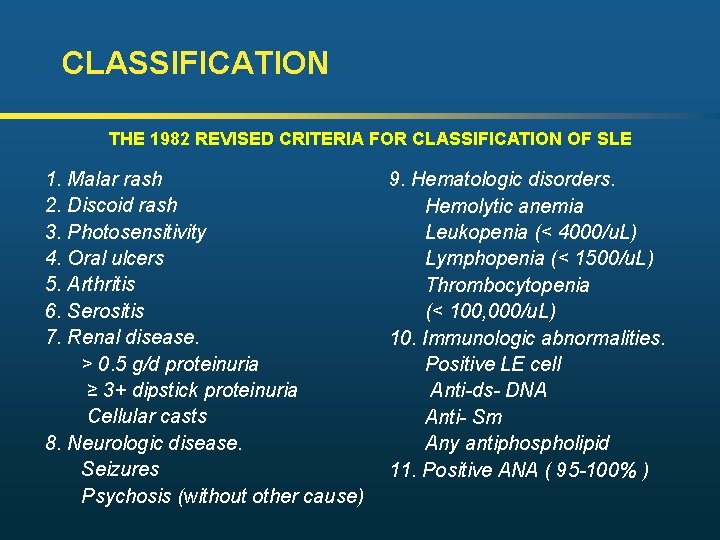
CLASSIFICATION THE 1982 REVISED CRITERIA FOR CLASSIFICATION OF SLE 1. Malar rash 2. Discoid rash 3. Photosensitivity 4. Oral ulcers 5. Arthritis 6. Serositis 7. Renal disease. > 0. 5 g/d proteinuria ≥ 3+ dipstick proteinuria Cellular casts 8. Neurologic disease. Seizures Psychosis (without other cause) 9. Hematologic disorders. Hemolytic anemia Leukopenia (< 4000/u. L) Lymphopenia (< 1500/u. L) Thrombocytopenia (< 100, 000/u. L) 10. Immunologic abnormalities. Positive LE cell Anti-ds- DNA Anti- Sm Any antiphospholipid 11. Positive ANA ( 95 -100% )
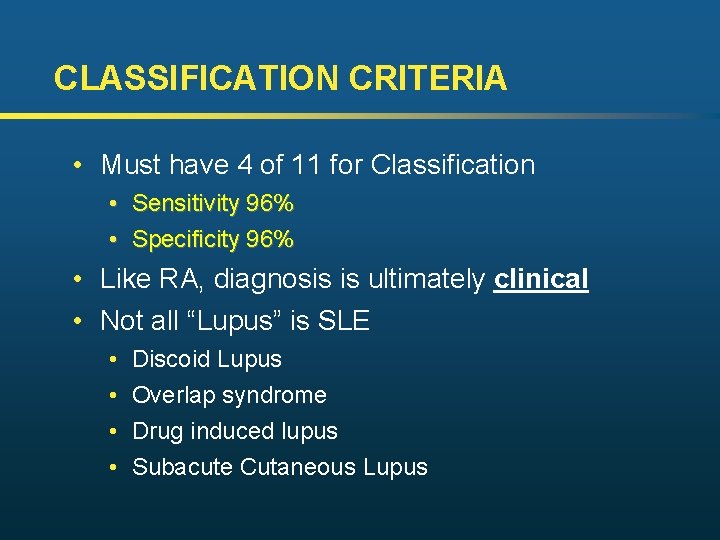
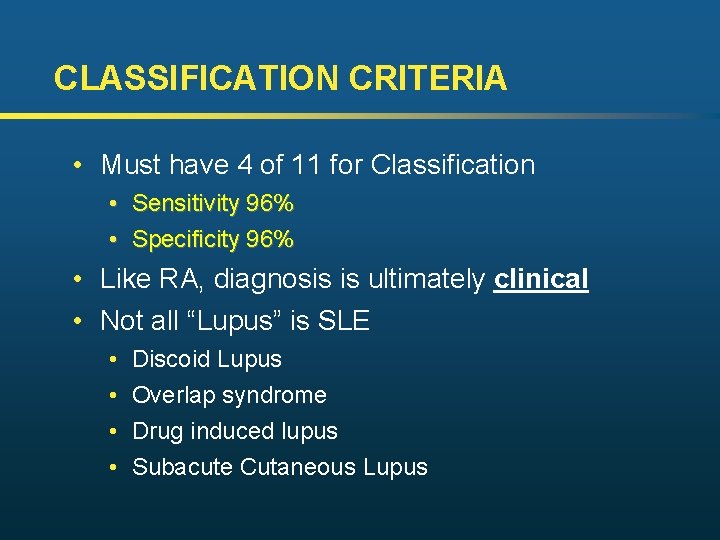
CLASSIFICATION CRITERIA • Must have 4 of 11 for Classification • • Sensitivity 96% Specificity 96% • Like RA, diagnosis is ultimately clinical • Not all “Lupus” is SLE • • Discoid Lupus Overlap syndrome Drug induced lupus Subacute Cutaneous Lupus
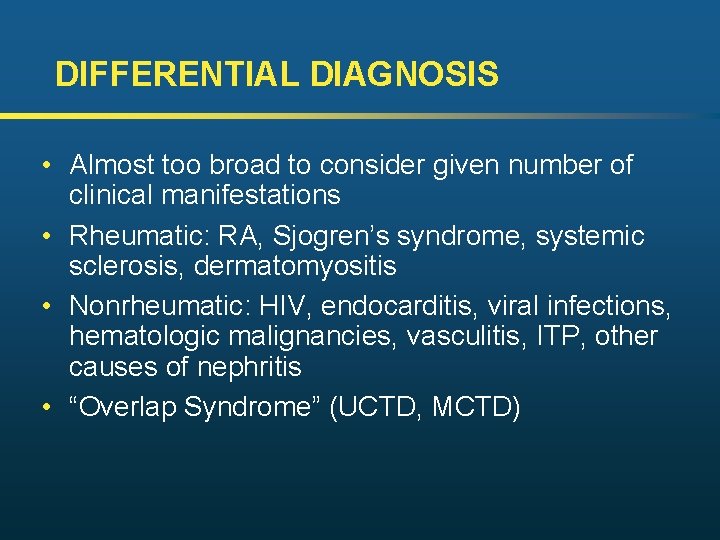
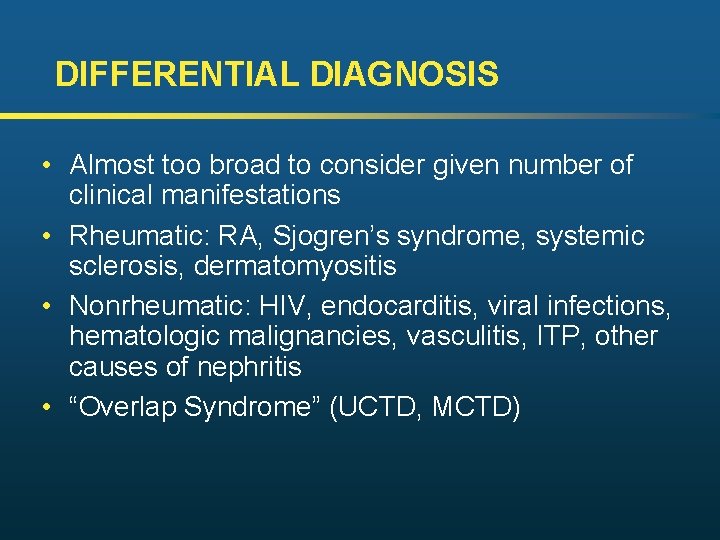
DIFFERENTIAL DIAGNOSIS • Almost too broad to consider given number of clinical manifestations • Rheumatic: RA, Sjogren’s syndrome, systemic sclerosis, dermatomyositis • Nonrheumatic: HIV, endocarditis, viral infections, hematologic malignancies, vasculitis, ITP, other causes of nephritis • “Overlap Syndrome” (UCTD, MCTD)
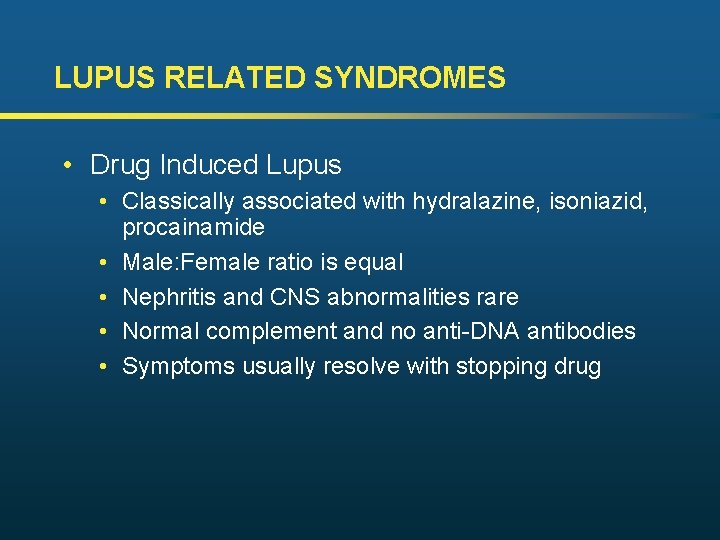
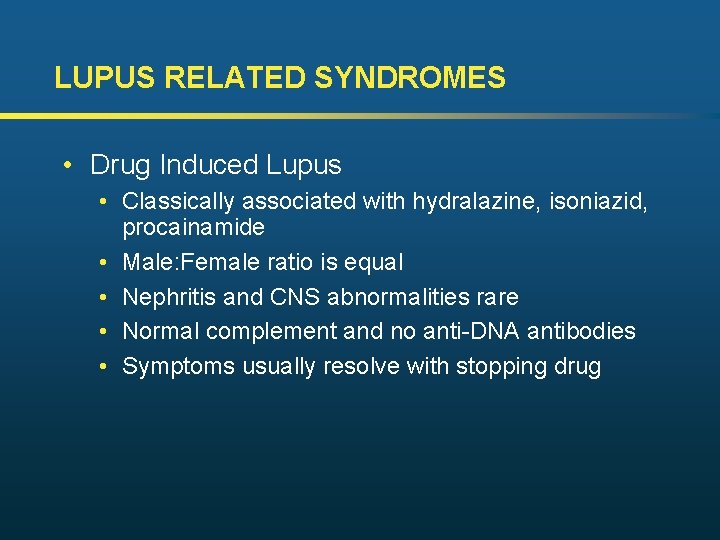
LUPUS RELATED SYNDROMES • Drug Induced Lupus • Classically associated with hydralazine, isoniazid, procainamide • Male: Female ratio is equal • Nephritis and CNS abnormalities rare • Normal complement and no anti-DNA antibodies • Symptoms usually resolve with stopping drug
LUPUS RELATED SYNDROMES • Antiphospholipid Syndrome (APS) • Hypercoagulability with recurrent thrombosis of either venous or arterial circulation • Thrombocytopenia-common • Pregnancy complication-miscarriage in first trimester • Lifelong anticoagulation warfarin is currently recommended for patients with serious complications due to common recurrence of thrombosis • Antiphospholipid Antibodies • Primary when present without other SLE feature. • Secondary when usual SLE features present
LUPUS RELATED SYNDROMES Raynaud’s Syndrome: -Not part of the diagnostic criteria for SLE - Does NOT warrant ANA if no other clinical evidence to suggest autoimmune disease
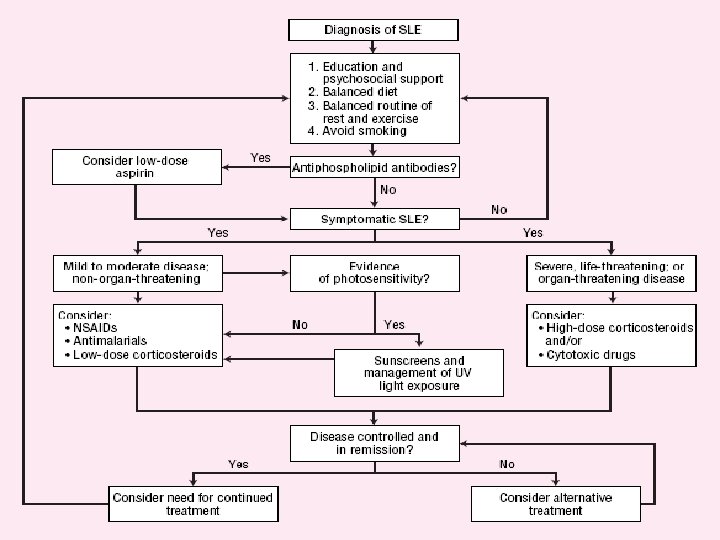
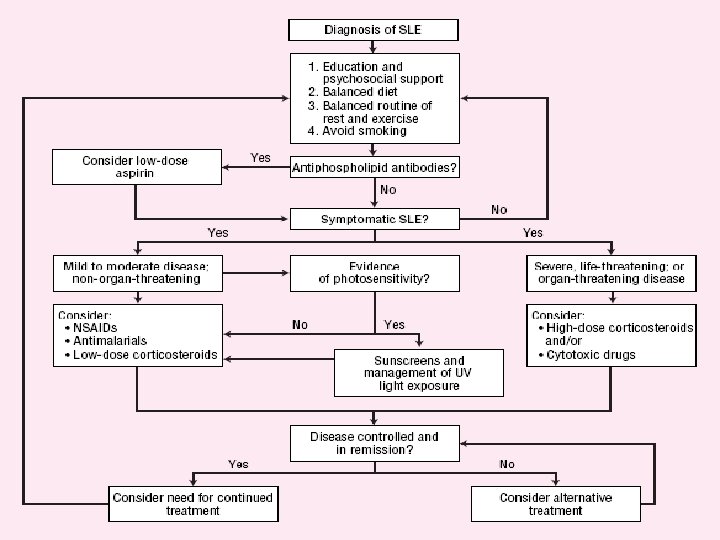
SLE – treatment I. • Mild cases (mild skin or joint involvement): NSAID, local treatment, hydroxy-chloroquin • Cases of intermediate severity (serositis, cytopenia, marked skin or joint involvement): corticosteroid (12 -64 mg methylprednisolon), azathioprin, methotrexat
SLE – treatment II. • Severe, life-threatening organ involvements (carditis, nephritis, systemic vasculitis, cerebral manifestations): high-dose intravenous corticosteroid + iv. cyclophosphamide + in some cases: plasmapheresis or iv. immunoglobulin, or, instead of cyclophosphamide: mycophenolate mofetil (not registered in the EU) • Some cases of nephritis (especially membranous), myositis, thrombocytopenia: cyclosporine
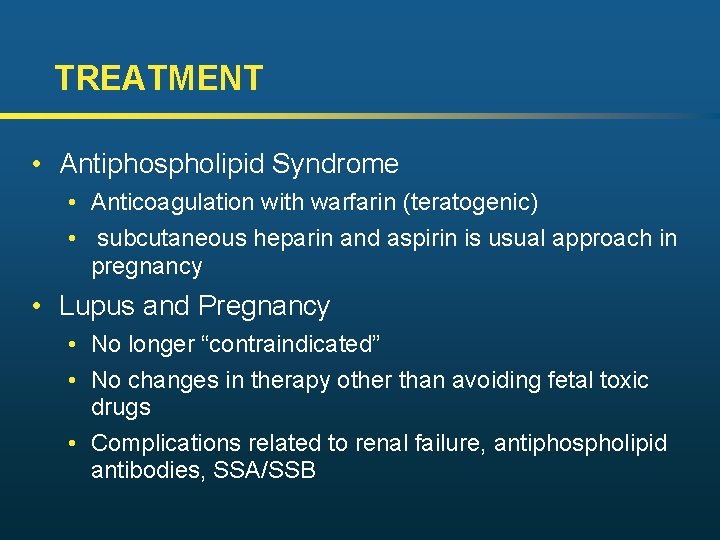
TREATMENT • Antiphospholipid Syndrome • Anticoagulation with warfarin (teratogenic) • subcutaneous heparin and aspirin is usual approach in pregnancy • Lupus and Pregnancy • No longer “contraindicated” • No changes in therapy other than avoiding fetal toxic drugs • Complications related to renal failure, antiphospholipid antibodies, SSA/SSB
TREATMENT • ESR, CRP probably useful as general markers of disease activity • Complement and anti-DNA antibodies may correlate to disease activity but often impractical turnaround time from lab • Patient history
PROGNOSIS • Unpredictable course • 10 year survival rates exceed 85% • Most SLE patients die from infection, probably related to therapy which suppresses immune system • Recommend smoking cessation, yearly flu shots, pneumovax q 5 years, and preventive cancer screening recommendations