Consensus Statement on Concussion in Sport The 5


- Slides: 32
Consensus Statement on Concussion in Sport: The 5 th international conference Berlin October 2016 (review) Dr. Pete Biglin, DO
th 5 International Conference- 2016 • Reflects the current state of knowledge on concussion (previous meetings 2001, 2004, 2008, 2012, 2016) • The document will be modified as new knowledge develops • Treatment of (SRC-Sports Related Concussion) remain in the realm of clinical judgment • Systematic review of literature provided
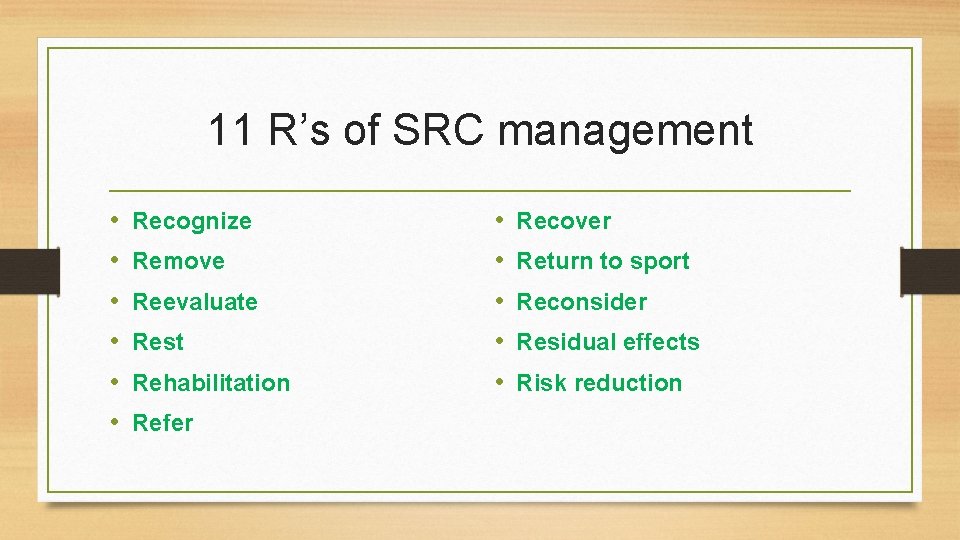
11 R’s of SRC management • • • Recognize Remove Reevaluate Rest Rehabilitation Refer • • • Recover Return to sport Reconsider Residual effects Risk reduction
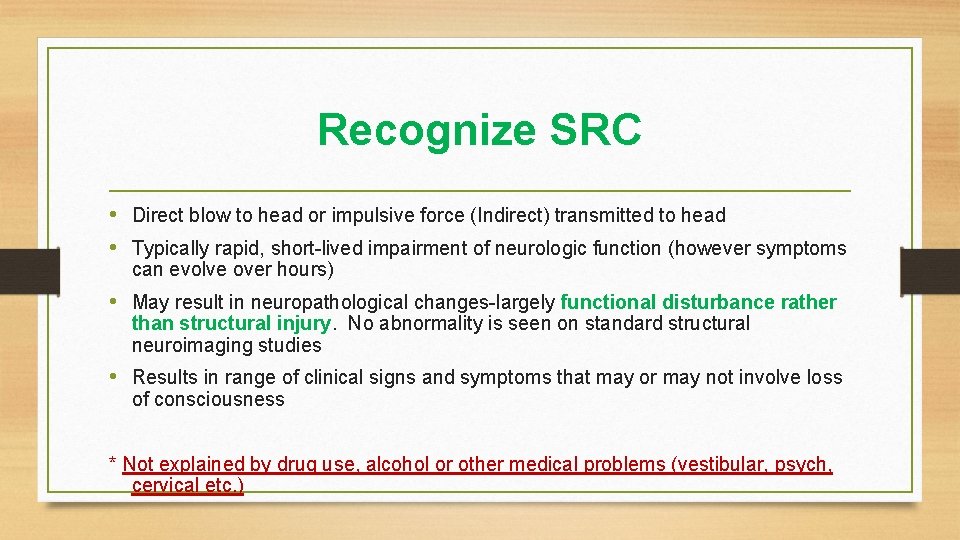
Recognize SRC • Direct blow to head or impulsive force (Indirect) transmitted to head • Typically rapid, short-lived impairment of neurologic function (however symptoms can evolve over hours) • May result in neuropathological changes-largely functional disturbance rather than structural injury. No abnormality is seen on standard structural neuroimaging studies • Results in range of clinical signs and symptoms that may or may not involve loss of consciousness * Not explained by drug use, alcohol or other medical problems (vestibular, psych, cervical etc. )
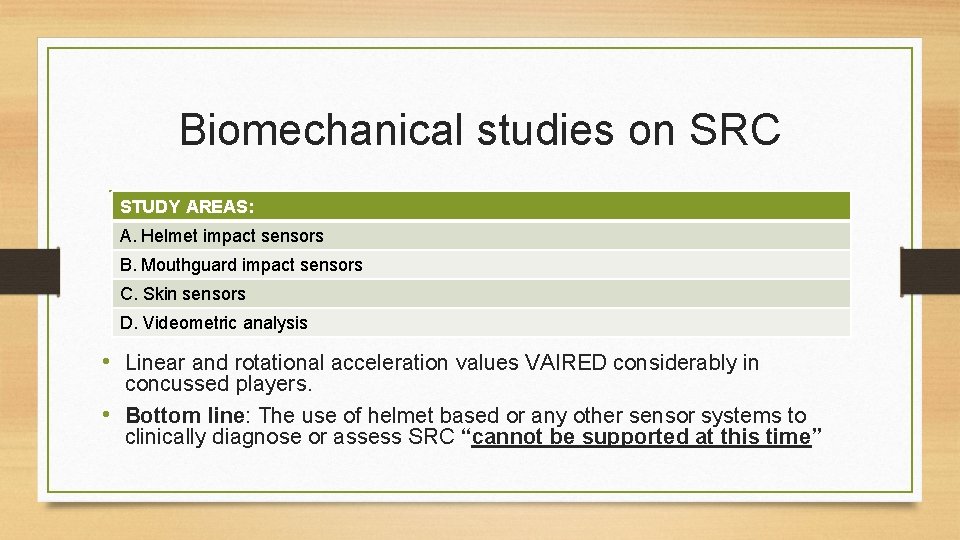
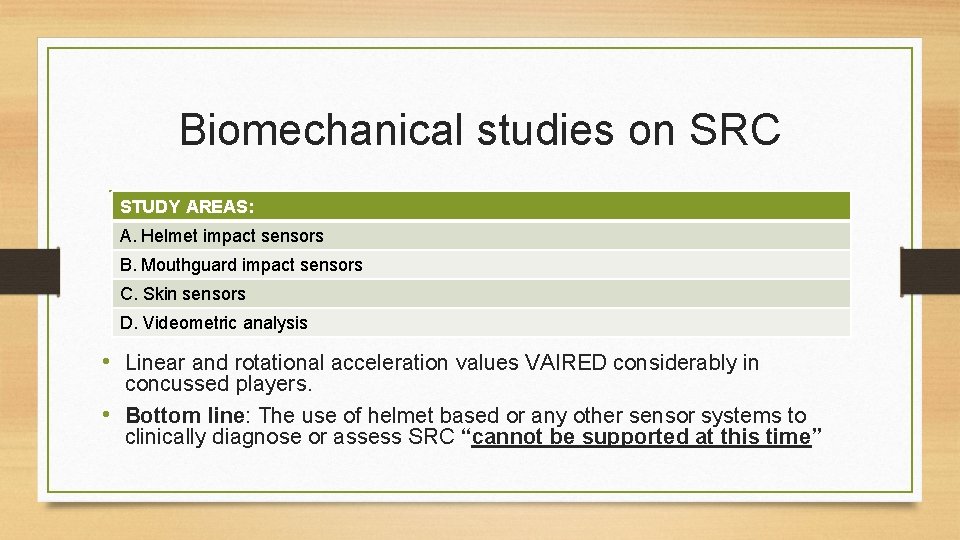
Biomechanical studies on SRC STUDY AREAS: A. Helmet impact sensors B. Mouthguard impact sensors C. Skin sensors D. Videometric analysis • Linear and rotational acceleration values VAIRED considerably in concussed players. • Bottom line: The use of helmet based or any other sensor systems to clinically diagnose or assess SRC “cannot be supported at this time”
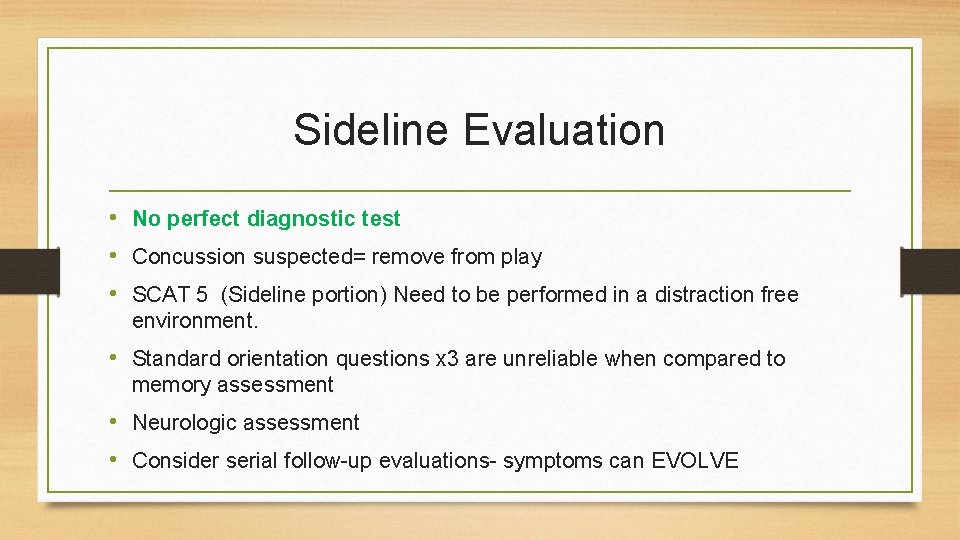
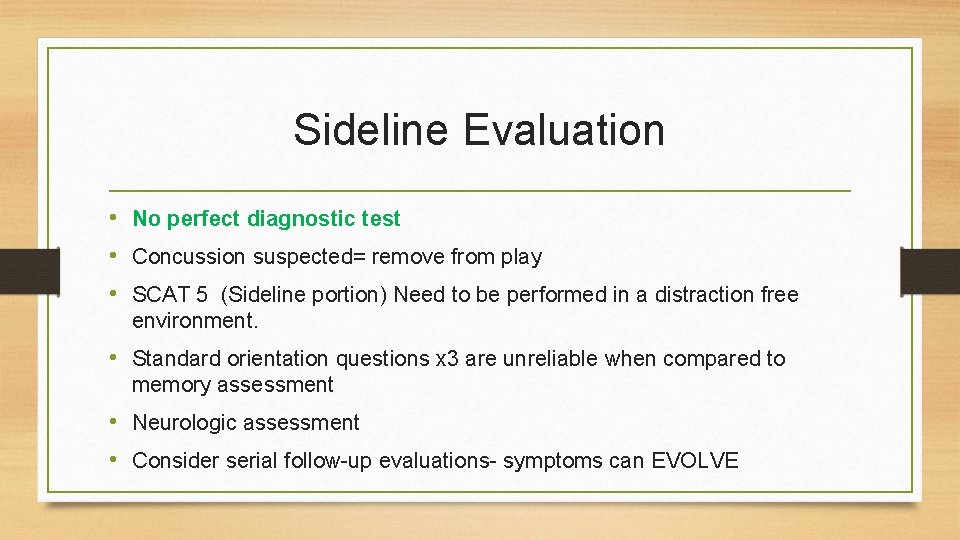
Sideline Evaluation • No perfect diagnostic test • Concussion suspected= remove from play • SCAT 5 (Sideline portion) Need to be performed in a distraction free environment. • Standard orientation questions x 3 are unreliable when compared to memory assessment • Neurologic assessment • Consider serial follow-up evaluations- symptoms can EVOLVE
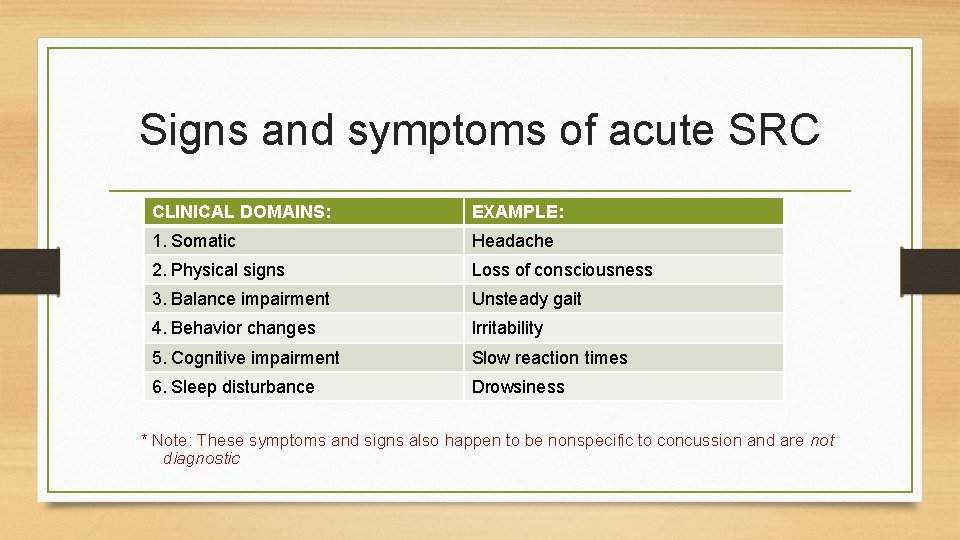
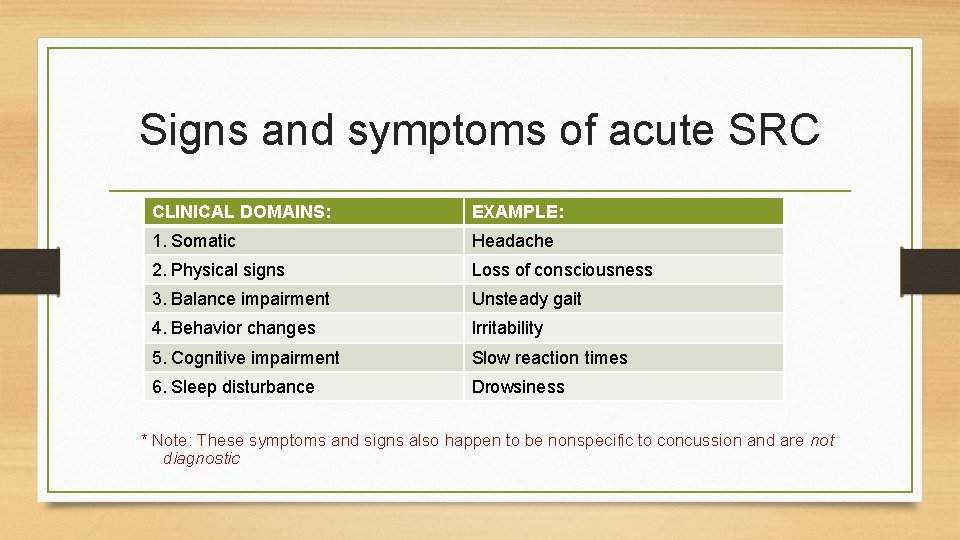
Signs and symptoms of acute SRC CLINICAL DOMAINS: EXAMPLE: 1. Somatic Headache 2. Physical signs Loss of consciousness 3. Balance impairment Unsteady gait 4. Behavior changes Irritability 5. Cognitive impairment Slow reaction times 6. Sleep disturbance Drowsiness * Note: These symptoms and signs also happen to be nonspecific to concussion and are not diagnostic
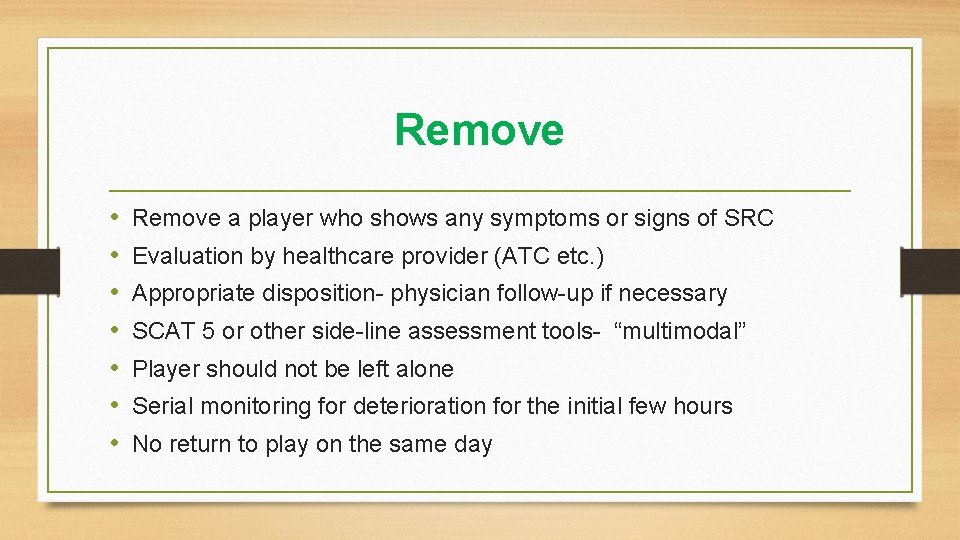
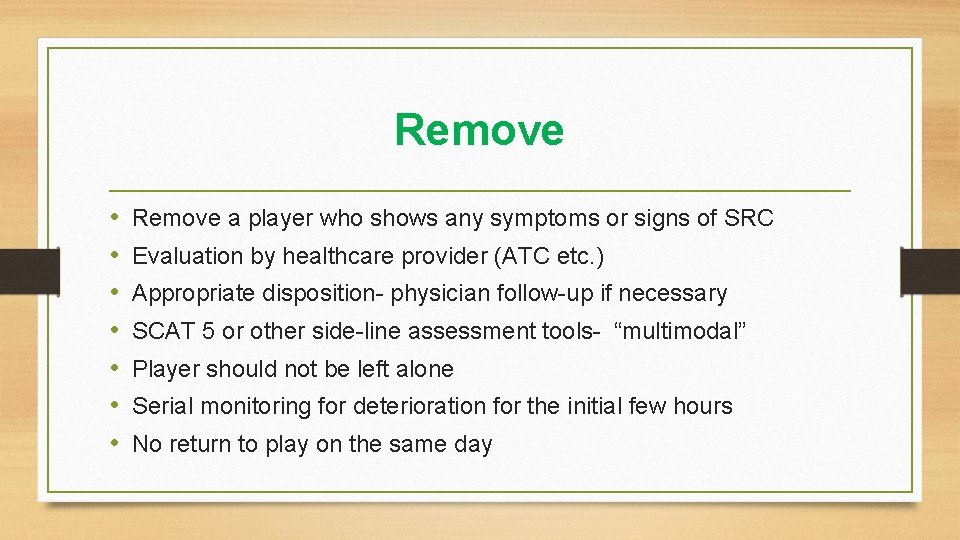
Remove • • Remove a player who shows any symptoms or signs of SRC Evaluation by healthcare provider (ATC etc. ) Appropriate disposition- physician follow-up if necessary SCAT 5 or other side-line assessment tools- “multimodal” Player should not be left alone Serial monitoring for deterioration for the initial few hours No return to play on the same day
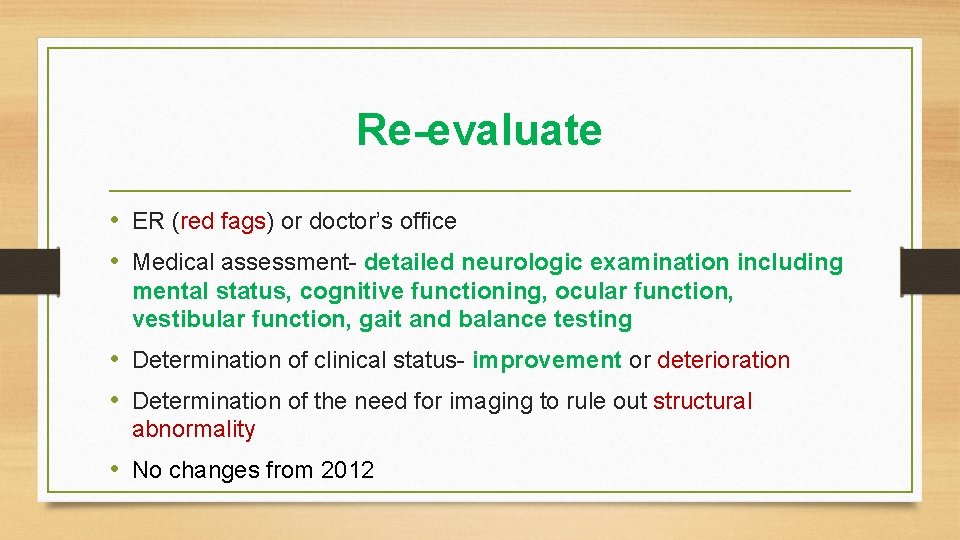
Re-evaluate • ER (red fags) or doctor’s office • Medical assessment- detailed neurologic examination including mental status, cognitive functioning, ocular function, vestibular function, gait and balance testing • Determination of clinical status- improvement or deterioration • Determination of the need for imaging to rule out structural abnormality • No changes from 2012
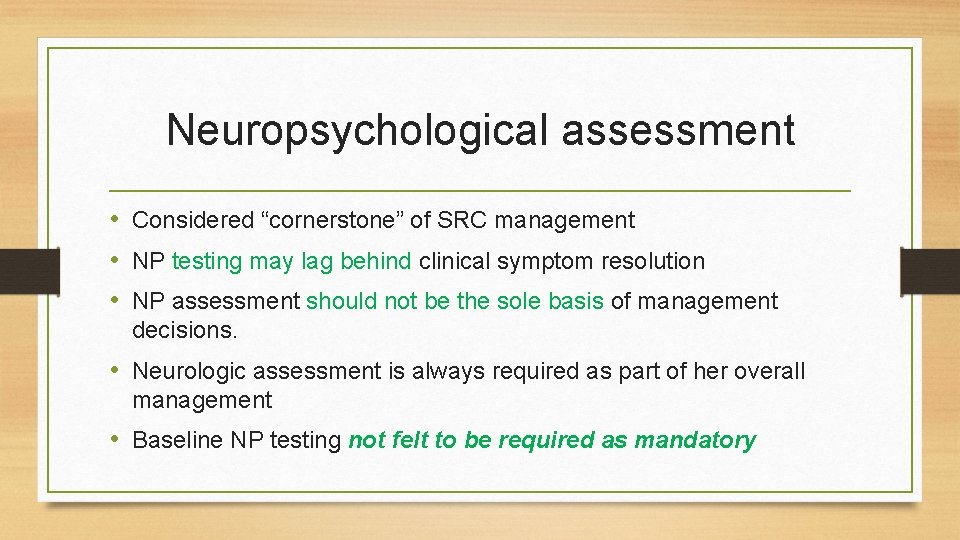
Neuropsychological assessment • Considered “cornerstone” of SRC management • NP testing may lag behind clinical symptom resolution • NP assessment should not be the sole basis of management decisions. • Neurologic assessment is always required as part of her overall management • Baseline NP testing not felt to be required as mandatory
Concussion Investigations • Advanced neuroimaging • Selective fluid biomarkers–blood, saliva and CSF along with genetic biomarkers for TBI are rapidly expanding in studies but they have limited application in clinical management at this time. • Expanding the broader TBI literature-there is growing interest role of genetics in predicting injury * All require further validation with future studies
Rest • • “Relative” Rest until symptom-free Prescribed rest most widely used intervention in SRC Rest is both cognitive and physical Rest should be brief in the acute phase 24 -48 hours. *Patient’s are then encouraged to become gradually and progressively more active while staying below their cognitive and physical symptom exacerbation thresholds- i. e. activity level should not bring on or worsened her symptoms (new)
Rehabilitation • Treat coexisting injuries- for example cervical strain • Psychological and vestibular rehabilitation are supported in the data • Closely monitored subject threshold submaximal exercise have some benefit in facilitating recovery • Pharmacologic treatment • School accommodations
Refer • Persistent symptoms : are greater than 10 -14 days in adults and greater than 4 weeks and children. However, these do not necessarily reflect ongoing physiologic injury to the brain. • Refer: Neuropsychologists, Neurology, Physical Therapy etc. • Currently limited evidence to support use of medications for concussive symptoms
Recovery • Clinical recovery is defined functionally as a return to normal activities, encompassing resolution of post concussive related symptoms and a return to clinically normal balance and cognitive function. • There is growing literature that a “sizable minority” of youth/high school and collegiate athletes may take much longer than 10 days to clinically recover.
Recovery -continued • Neural biological recovery may extend beyond clinical recovery in some athletes. Means that athletes may be exposed to additional risk by returning to play while there is ongoing brain dysfunction. • There is also a growing body of literature indicating psychological factors play significant role in symptom recovery and contribute to the risk of persistent symptoms in some cases
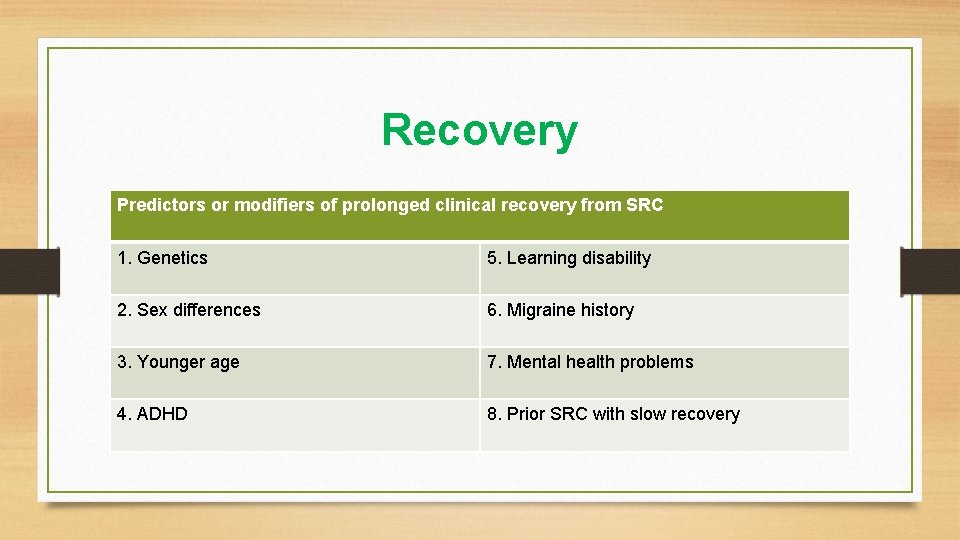
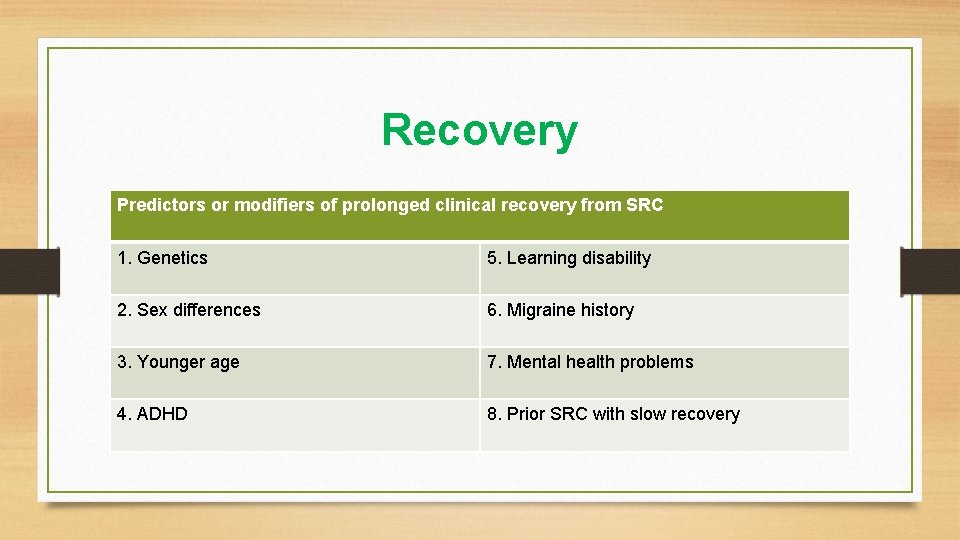
Recovery Predictors or modifiers of prolonged clinical recovery from SRC 1. Genetics 5. Learning disability 2. Sex differences 6. Migraine history 3. Younger age 7. Mental health problems 4. ADHD 8. Prior SRC with slow recovery
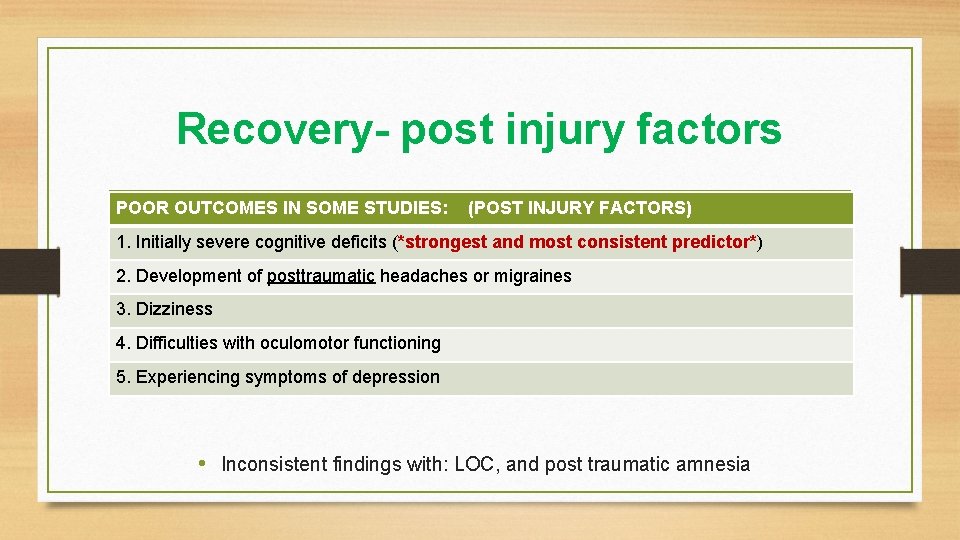
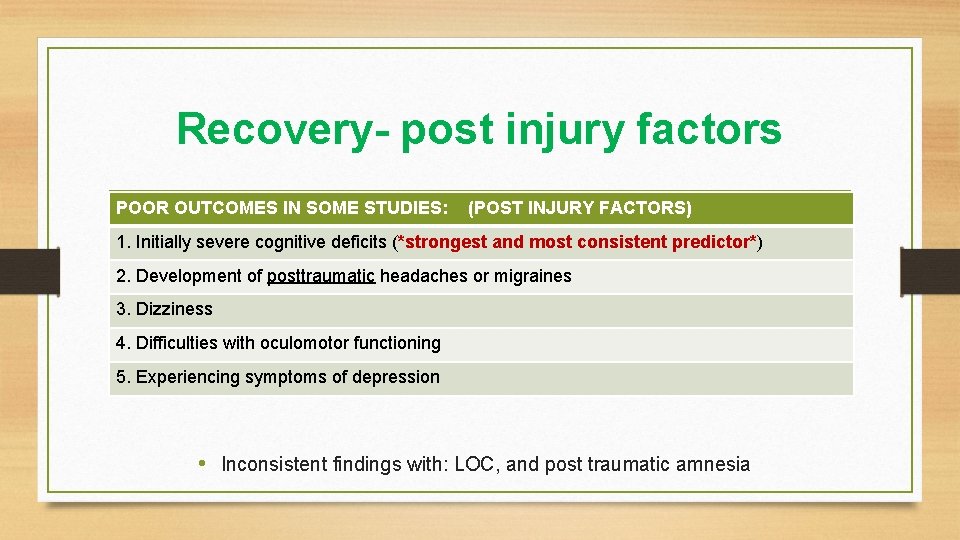
Recovery- post injury factors POOR OUTCOMES IN SOME STUDIES: (POST INJURY FACTORS) 1. Initially severe cognitive deficits (*strongest and most consistent predictor*) 2. Development of posttraumatic headaches or migraines 3. Dizziness 4. Difficulties with oculomotor functioning 5. Experiencing symptoms of depression • Inconsistent findings with: LOC, and post traumatic amnesia
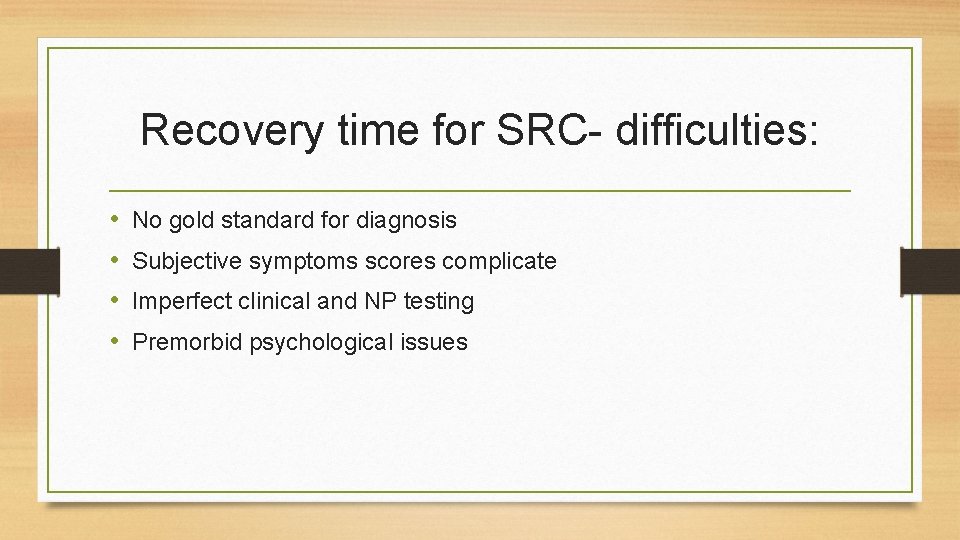
Recovery time for SRC- difficulties: • • No gold standard for diagnosis Subjective symptoms scores complicate Imperfect clinical and NP testing Premorbid psychological issues
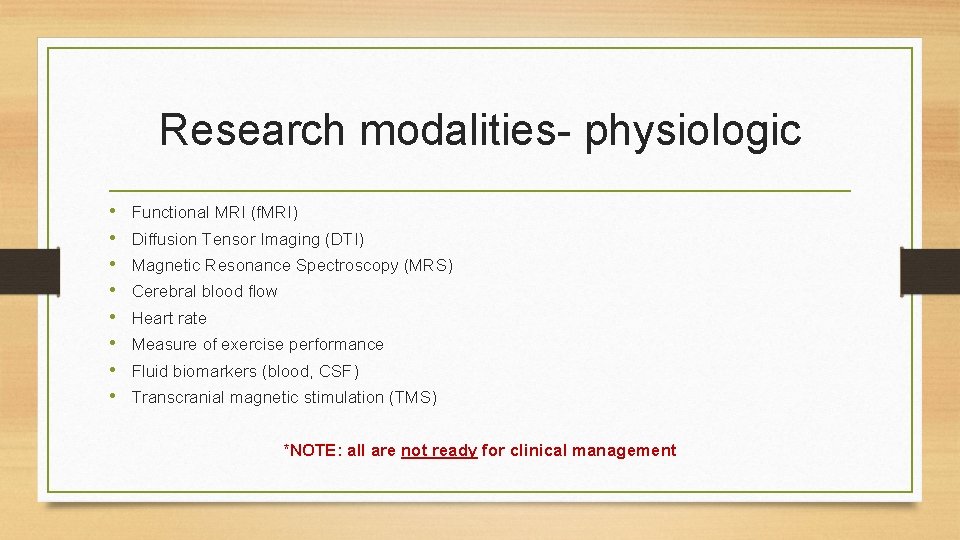
Research modalities- physiologic • • Functional MRI (f. MRI) Diffusion Tensor Imaging (DTI) Magnetic Resonance Spectroscopy (MRS) Cerebral blood flow Heart rate Measure of exercise performance Fluid biomarkers (blood, CSF) Transcranial magnetic stimulation (TMS) *NOTE: all are not ready for clinical management

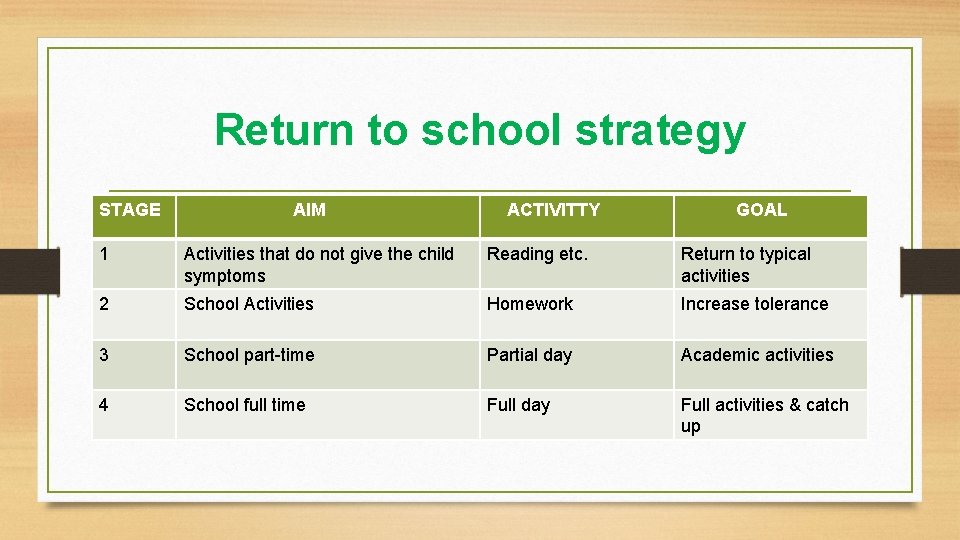
Return to Sport/school • Stepwise rehabilitation strategies modified from previous versions to improve clarity • Return to play “strategy” stages 1 through 6 The word “protocol” has been removed. Management needs to be individualized. Generally each step should take 24 hours so that athletes would take a minimum of one week to proceed through the full rehabilitation protocol once they are asymptomatic at rest. • Return to school “strategy” stages 1 through 4

Return to Sport Strategy STAGE ACTIVITY 1 ADLs that do not promote symptoms (goal reintroduce school) 2 Light aerobic exercise 3 Sport specific exercise- drills 4 Non-contact drills- progressive resistance 5 Full contact practice 6 Return to sport- game play
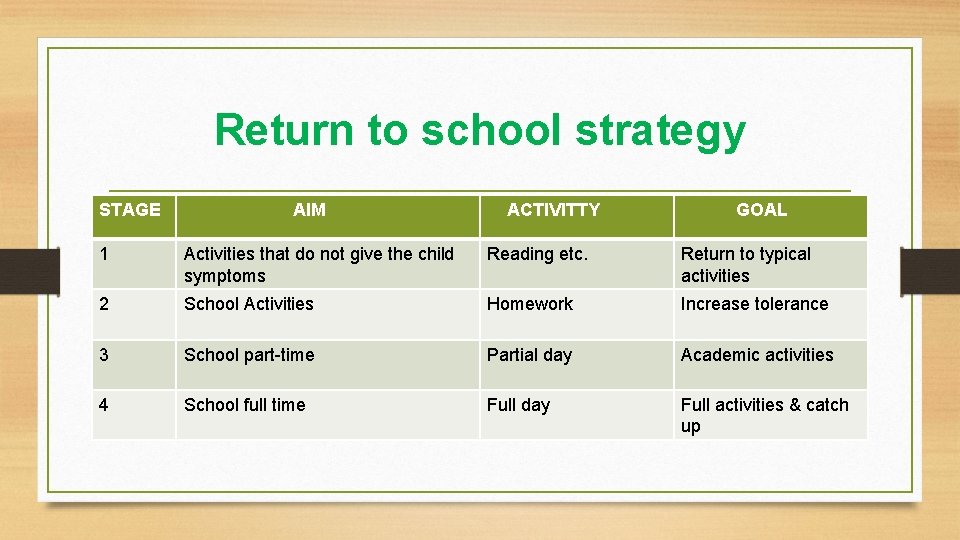
Return to school strategy STAGE AIM ACTIVITTY GOAL 1 Activities that do not give the child symptoms Reading etc. Return to typical activities 2 School Activities Homework Increase tolerance 3 School part-time Partial day Academic activities 4 School full time Full day Full activities & catch up
Reconsider- special populations • Elite versus non-elite athletes should be managed using the same management principals • The literature does not adequately address the question of age groups in which children with SRC should be managed differently from adults. • Schools are encouraged to have an SRC policy • Children/adolescence should not return to sport until they have successfully returned to school (priority)
Risk Reduction • Role of pre-participation physical (SRC evaluation) • Goal is to identify high risk athletes- possible opportunity to educate athlete • • Previous length of recovery from SRC, not just the # of concussions Recall from coaches or teammates is not reliable Associated injuries to the neck and head may have missed coexistent SRC Seek details regarding protective equipment used at the time of SRC
Prevention studies • Evidence for helmets reducing risk of SRC is limited many sports because of the mandatory nature of helmet regulations. • There is sufficient evidence in terms of head injury in skiing and snowboarding mandate helmet use in skiing and snow boarding. to support strong recommendations to • Evidence for mouth guard use in preventing SRC is mixed but met a analysis suggest a non-significant trend towards a protective affect in collision sports. More rigorous case controlled designs are required to further evaluate this finding • Disallowing body checking under age 13 in hockey- strong evidence
PEE-WEE Hockey Brain: Strong evidence for rule changes
Prevention studies–continued • Evidence for SRC risk reduction in the following areas: • Fair play rules in ice hockey- do not lead to SRC risk reduction • American football tackle technique training- do not lead to SRC risk reduction • Soccer rule enforcement of red cards for high elbows during heading dual in is based on evidence supporting a reduced risk of head contact. • Limiting contact practices in football shows promising results • Vision training in collegiate football also showing promising results
Knowledge Translation • Target audiences benefit from specific learning strategies- parents coaches, referees, administrators, health professionals and athletes • Fair play and respect for opponents are ethical values that should be encouraged & taught in all sports
Conclusion • Authors indicated the importance of differentiation between SRC and m. TBI for detailed phenotypic data in sports, versus other types of trauma such as motor vehicle crashes(m. TBI). • “Science of concussion is incomplete and therefore management and return to play decisions like largely in the realm of clinical judgment on an individualized basis”