The 5 th Consensus Statement on Concussion Statement
- Slides: 20
The 5 th Consensus Statement on Concussion Statement (Berlin) A 15 Minute Update David W. Lawrence, MD, CCFP(SEM), Dip Sport Med, MPH (Cand)
Overview • • • Definition & Diagnosis Signs and Symptoms Sideline Evaluation Management Neuropsychological Evaluation Persistent Symptoms Residual Effects Prevention SCAT 5
Definition & Diagnosis • Traumatic brain injury • Caused either by a direct or transmitted force to the head • Rapid onset of short-lived impairment of neurological function that resolves spontaneously. • Functional disturbance rather than a structural injury – no abnormality is seen on standard structural neuroimaging studies. • Range of clinical signs and symptoms. • The clinical signs and symptoms cannot be explained by other conditions: – drug, alcohol, medications, other injuries, or other comorbidities
Signs and Symptoms • Symptoms and signs are non-specific to concussion • The suspected diagnosis of SRC can include one or more of the following clinical domains: a. Symptoms: – b. c. d. e. f. somatic, cognitive, and/or emotional symptoms Physical signs Balance impairment Behavioural changes Cognitive impairment Sleep/wake disturbance
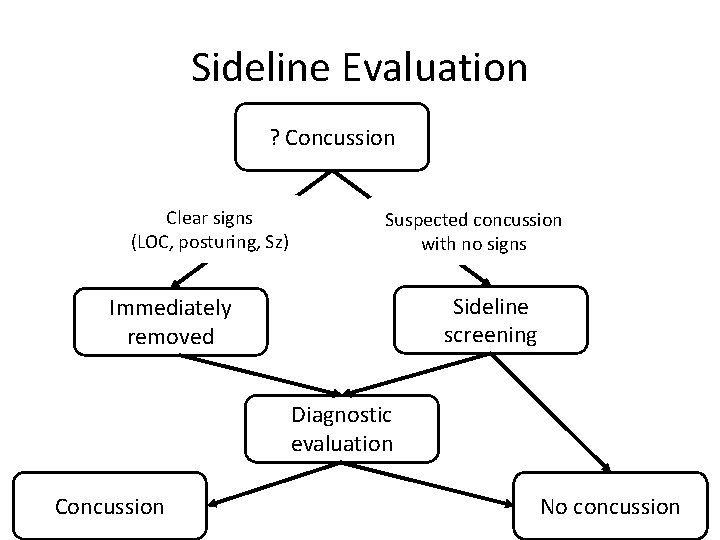
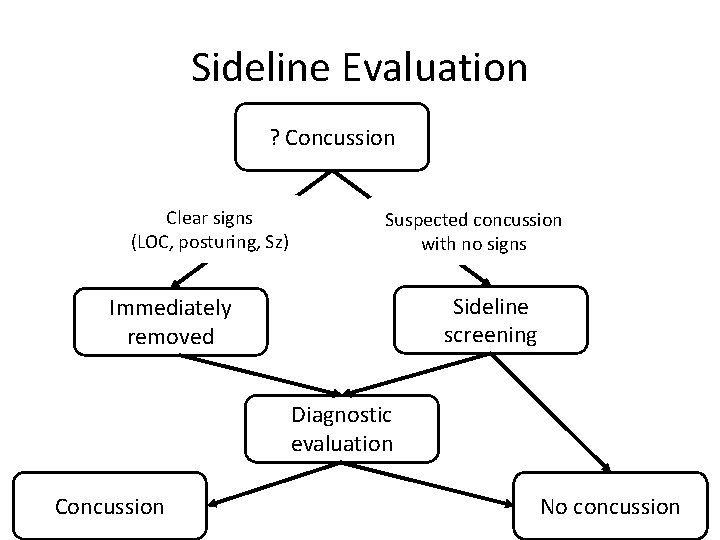
Sideline Evaluation ? Concussion Clear signs (LOC, posturing, Sz) Suspected concussion with no signs Sideline screening Immediately removed Diagnostic evaluation Concussion No concussion
Sideline evaluation • • • SCAT 5 Sideline video review Occulomotor screening Reaction time Objective assessment to exclude more serious injury is critical.
Acute Management • Concussion is suspected, the athlete should be removed from the sporting environment • Re-evaluation with consideration of neuroimaging to r/o more severe imaging
Concussion Investigations • No investigations recommended for concussion-specific management. • Biomarkers are important research tools but require further validation prior to clinical use.
Rest • Insufficient evidence to prescribing complete rest. • After a brief period of rest during the acute phase (24– 48 hours) after injury, patients can begin subsymptom threshold progression.
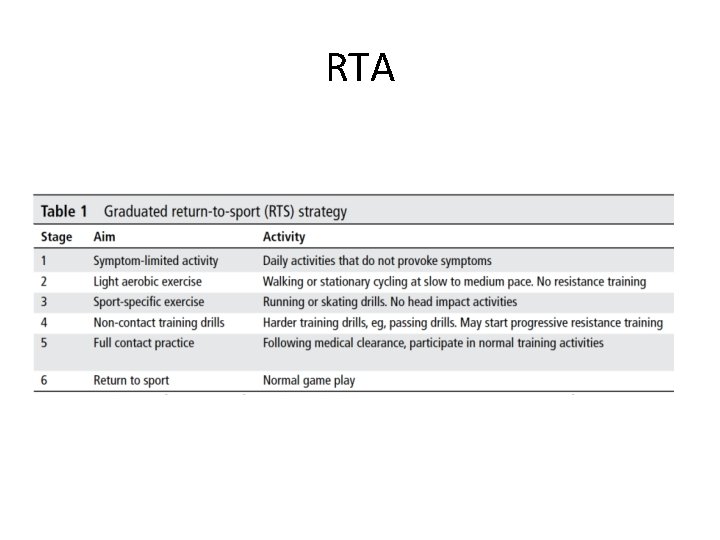
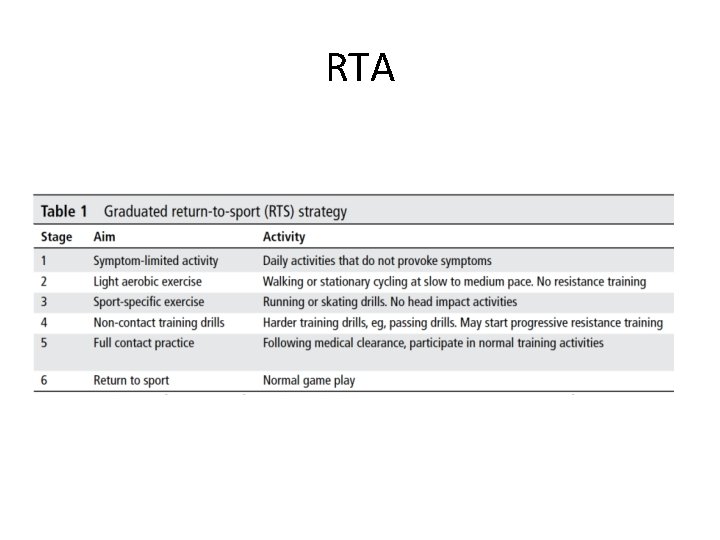
RTA
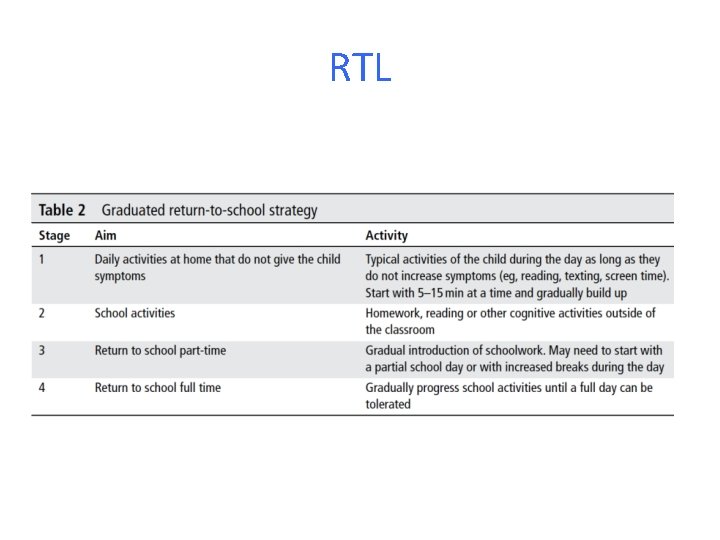
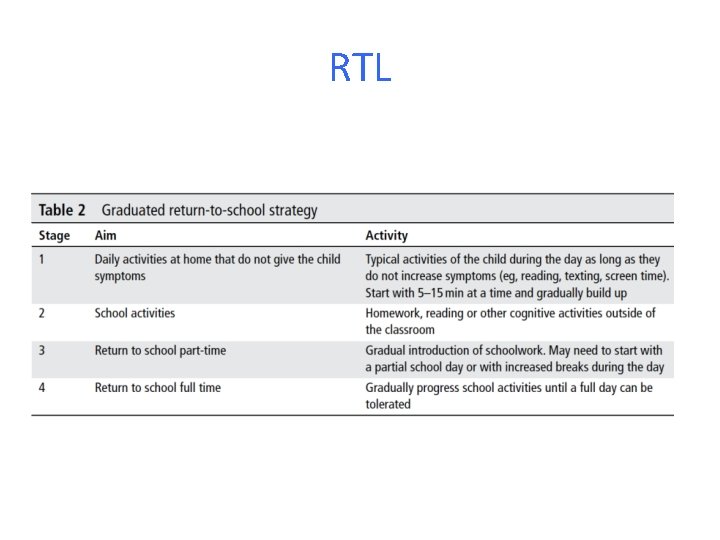
RTL
Rehabilitation • Additional multidisciplinary interventions – psychological rehabilitation – cervical rehabilitation – vestibular rehabilitation – active rehabilitation – pharmacological treatment
Neuropsychological Assessment • NP assessment has been previously described as the ‘cornerstone’ of concussion management • NP testing has clinical value and contributes significant information • NP assessment should not be the sole basis of management decisions • Post-injury NP testing is not required for all athletes • Should be performed by a trained and accredited neuropsychologist. • Brief computerised cognitive evaluation tools are not substitutes for complete NP assessment. • Baseline or pre-season NP testing not felt to be required as a mandatory aspect of every assessment.
Post-Concussion Syndrome Persistent Symptoms • Failure of normal clinical recovery – symptoms that persist beyond expected time frames (ie, >10– 14 days in adults and >4 weeks in children). • Does not reflect a single pathophysiological entity • Constellation of non-specific post-traumatic symptoms • May be linked to coexisting and/ or confounding factors • Does not necessarily reflect ongoing physiological injury to the brain
Establishing Recovery • “Difficult task”
Special Populations • Elite athletes: – no difference • Child and adolescent: – Children and adolescents should not return to sport until they have successfully returned to school. – Early introduction of symptom-limited physical activity is appropriate.
Chronic Traumatic Encephalopathy Residual Effects and Sequelae • Clinicians need to be mindful of the potential for long-term problems in the management of all athletes. • Literature on long-term consequences of exposure to recurrent head trauma is inconsistent. • There is much more to learn about the potential cause-and-effect relationships of repetitive headimpact exposure and concussions.
CTE • The potential for developing chronic traumatic encephalopathy (CTE) must be a consideration – Distinct tauopathy with an unknown incidence in athletic populations. – Cause-and-effect relationship bw CTE and concussion has not yet been demonstrated – The notion that repeated concussion or subconcussive impacts cause CTE remains unknown.
Prevention • Helmets: – Evidence is limited for an overall effect – There is sufficient evidence in skiing/snowboarding to recommend use to prevent overall head injuries • Mouth guards: – Evidence is limited for an overall effect – Meta-analysis suggests a non-significant trend towards a protective effect in collision sports • Intrinsic risk factors: – No evidence • Extrinsic risk factors (i. e. rule & policy changes) – Strong evidence
SCTA 5 • The SCAT is useful immediately after injury in differentiating concussed from non-concussed athletes • Its utility appears to decrease significantly 3– 5 days after injury. • The symptom checklist, however, does demonstrate clinical utility in tracking recovery. • Baseline testing may be useful, but is not necessary for interpreting post-injury scores.