Congestion in Heart Failure Mihai Gheorghiade MD Professor




- Slides: 42
Congestion in Heart Failure Mihai Gheorghiade, MD Professor of Medicine Northwestern University Feinberg School of Medicine Chicago, Illinois
Congestion in HF Definitions 2
Congestion in Heart Failure (HF) Clinical congestion: symptoms (dyspnea) and signs (JVD, rales, edema) Hemodynamic or cardiopulmonary congestion: high LV filling pressures with or without clinical congestion JVD, jugular venous distention; LV, left ventricular. 3
Hemodynamic Congestion Often Does Not Translate into Signs/Symptoms of HF 4
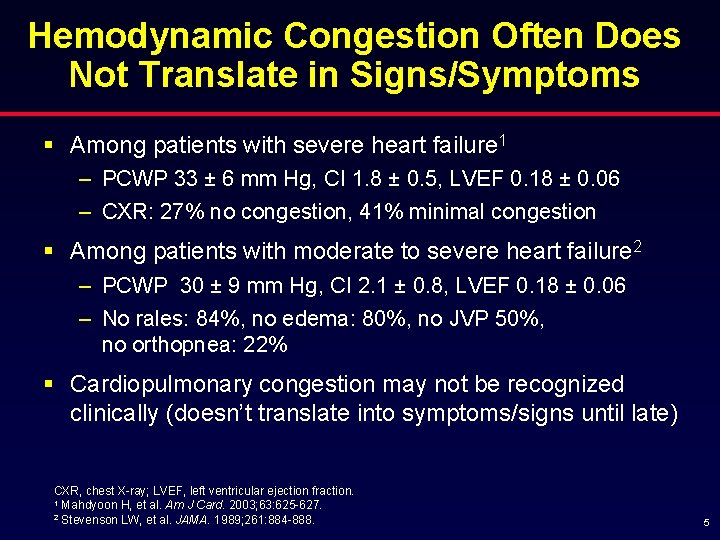
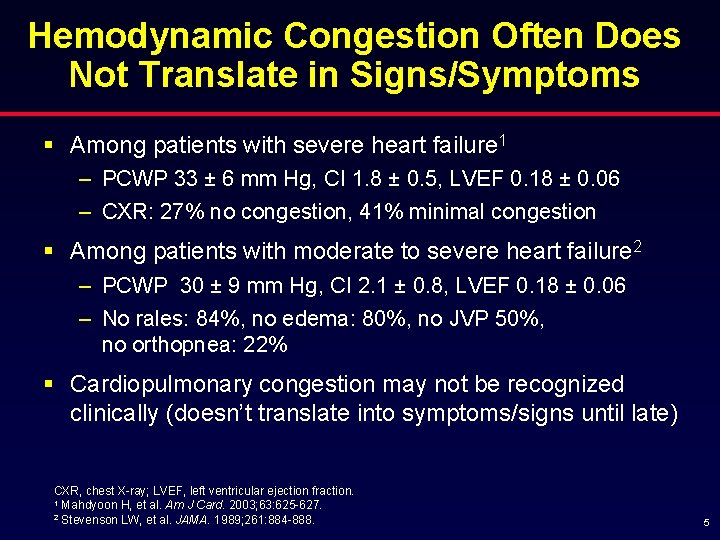
Hemodynamic Congestion Often Does Not Translate in Signs/Symptoms § Among patients with severe heart failure 1 – PCWP 33 ± 6 mm Hg, CI 1. 8 ± 0. 5, LVEF 0. 18 ± 0. 06 – CXR: 27% no congestion, 41% minimal congestion § Among patients with moderate to severe heart failure 2 – PCWP 30 ± 9 mm Hg, CI 2. 1 ± 0. 8, LVEF 0. 18 ± 0. 06 – No rales: 84%, no edema: 80%, no JVP 50%, no orthopnea: 22% § Cardiopulmonary congestion may not be recognized clinically (doesn’t translate into symptoms/signs until late) CXR, chest X-ray; LVEF, left ventricular ejection fraction. 1 Mahdyoon H, et al. Am J Card. 2003; 63: 625 -627. 2 Stevenson LW, et al. JAMA. 1989; 261: 884 -888. 5
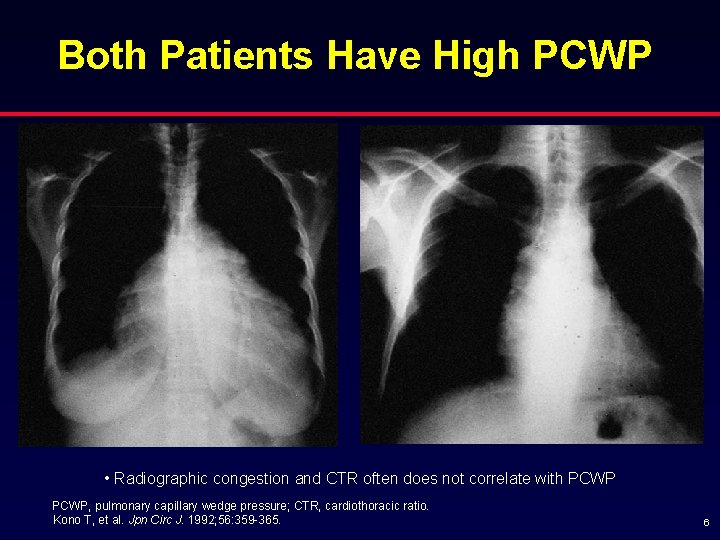
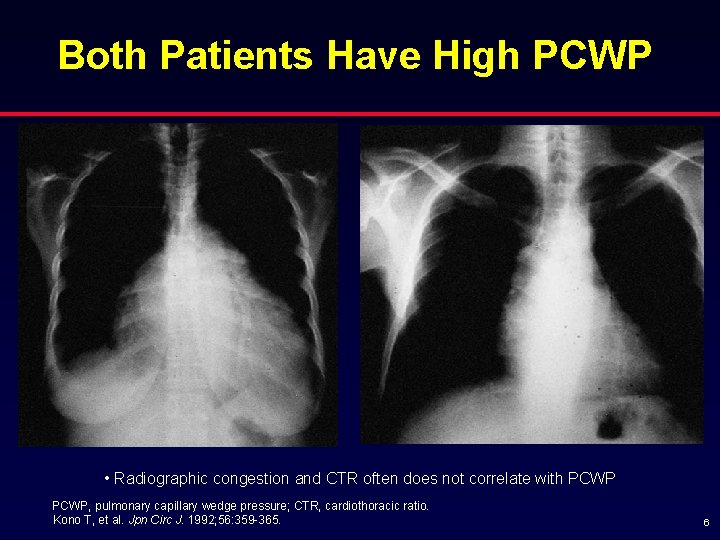
Both Patients Have High PCWP • Radiographic congestion and CTR often does not correlate with PCWP, pulmonary capillary wedge pressure; CTR, cardiothoracic ratio. Kono T, et al. Jpn Circ J. 1992; 56: 359 -365. 6
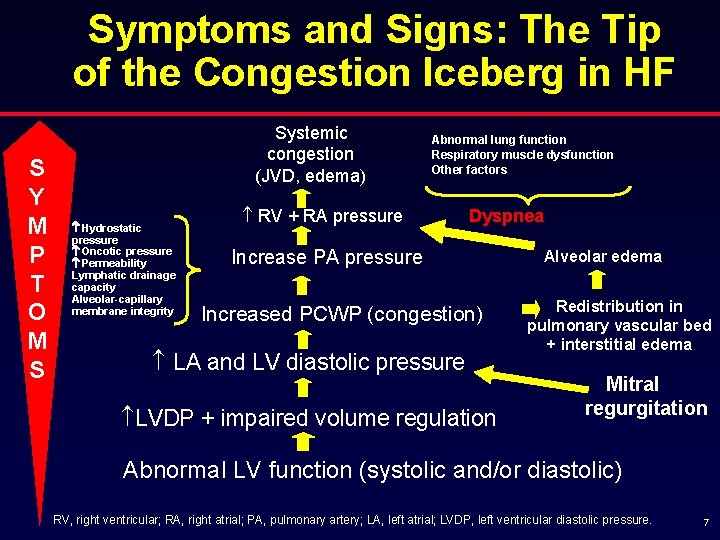
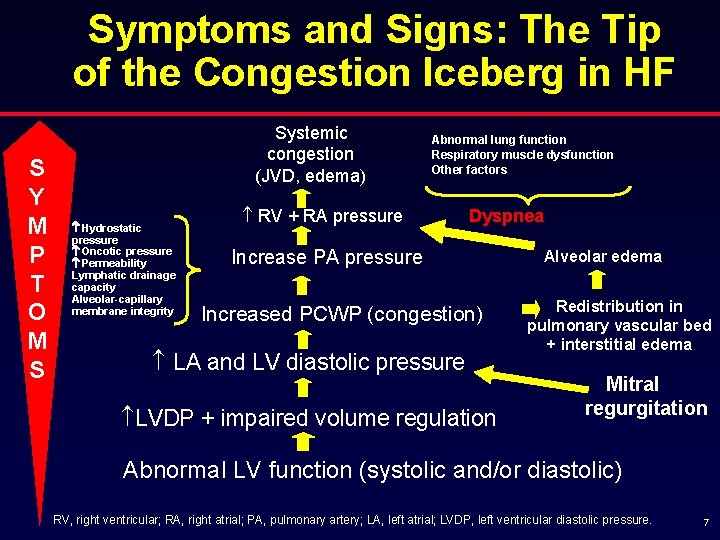
Symptoms and Signs: The Tip of the Congestion Iceberg in HF S Y M P T O M S Systemic congestion (JVD, edema) Hydrostatic pressure Oncotic pressure Permeability Lymphatic drainage capacity Alveolar-capillary membrane integrity Abnormal lung function Respiratory muscle dysfunction Other factors RV + RA pressure Dyspnea Increase PA pressure Increased PCWP (congestion) LA and LV diastolic pressure LVDP + impaired volume regulation Alveolar edema Redistribution in pulmonary vascular bed + interstitial edema Mitral regurgitation Abnormal LV function (systolic and/or diastolic) RV, right ventricular; RA, right atrial; PA, pulmonary artery; LA, left atrial; LVDP, left ventricular diastolic pressure. 7
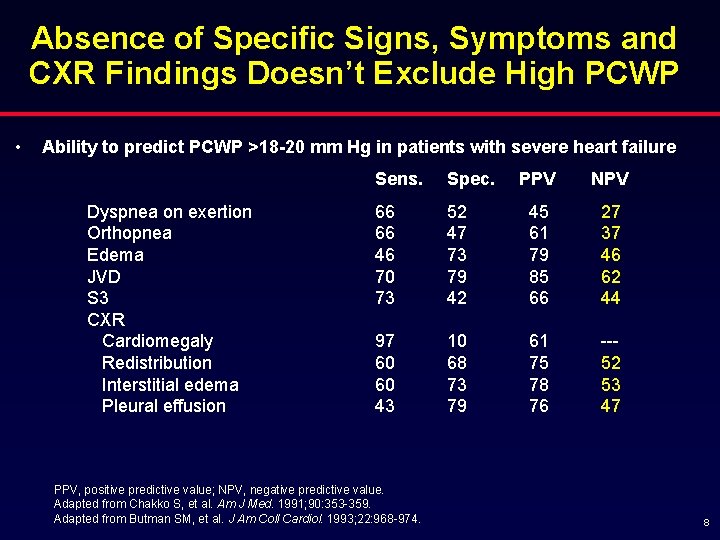
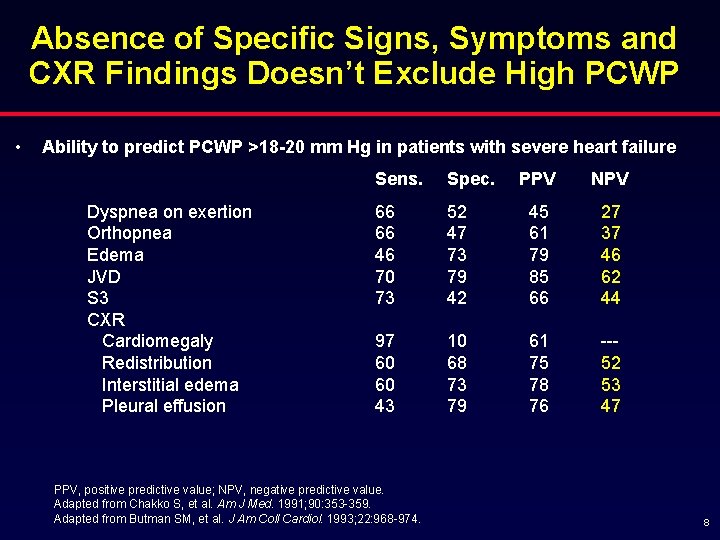
Absence of Specific Signs, Symptoms and CXR Findings Doesn’t Exclude High PCWP • Ability to predict PCWP >18 -20 mm Hg in patients with severe heart failure Dyspnea on exertion Orthopnea Edema JVD S 3 CXR Cardiomegaly Redistribution Interstitial edema Pleural effusion Sens. Spec. 66 66 46 70 73 97 60 60 43 PPV, positive predictive value; NPV, negative predictive value. Adapted from Chakko S, et al. Am J Med. 1991; 90: 353 -359. Adapted from Butman SM, et al. J Am Coll Cardiol. 1993; 22: 968 -974. PPV NPV 52 47 73 79 42 45 61 79 85 66 27 37 46 62 44 10 68 73 79 61 75 78 76 --52 53 47 8
Importance of Recognizing Congestion Early § Identifying hemodynamic congestion early will lead to early treatment, and prevent hospitalizations and possibly progression of heart failure 9

Congestion Is the Main Reason for Heart Failure Hospital Admissions and Readmissions 10
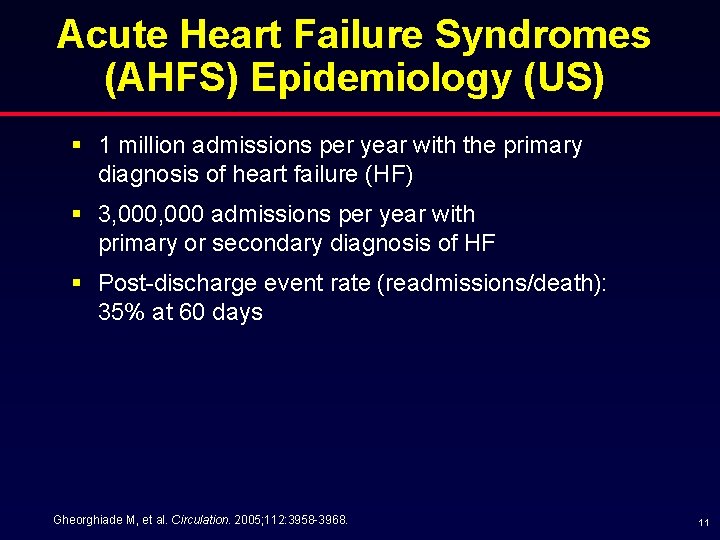
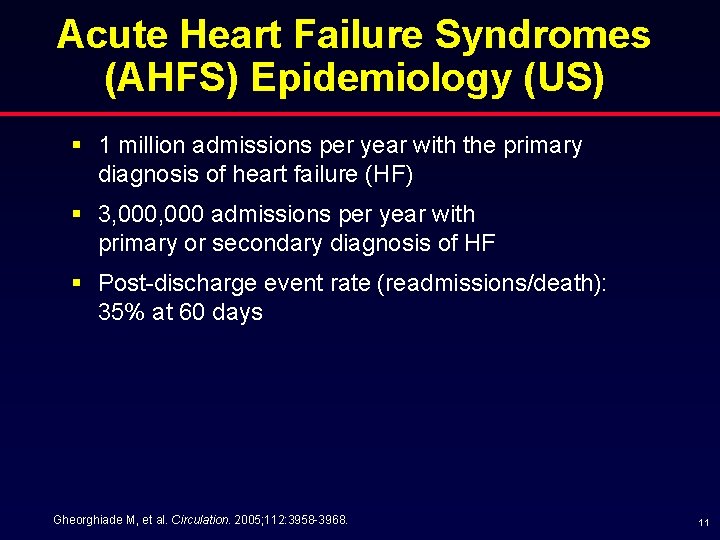
Acute Heart Failure Syndromes (AHFS) Epidemiology (US) § 1 million admissions per year with the primary diagnosis of heart failure (HF) § 3, 000 admissions per year with primary or secondary diagnosis of HF § Post-discharge event rate (readmissions/death): 35% at 60 days Gheorghiade M, et al. Circulation. 2005; 112: 3958 -3968. 11

AHFS: Hospitalizations § Worsening chronic HF (80%) § Acute de novo heart failure (diagnosed for the first time) (15%) § Advanced/end-stage/refractory HF (5%) Gheorghiade M, et al. Circulation. 2005; 112: 3958 -3968. 12
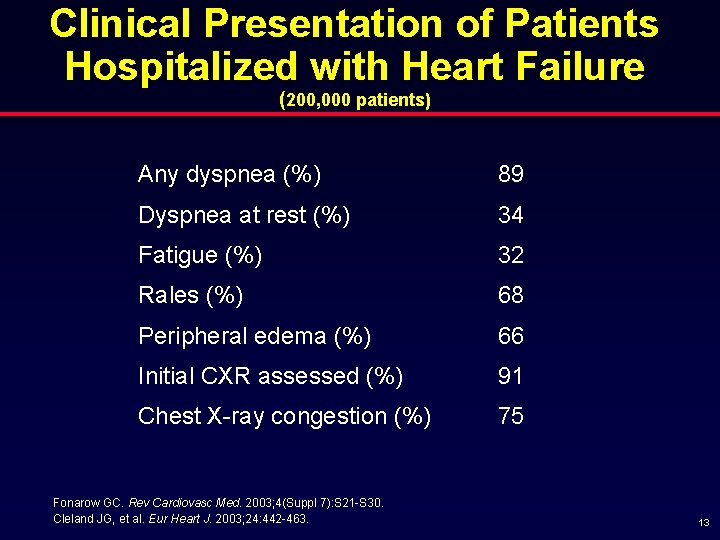
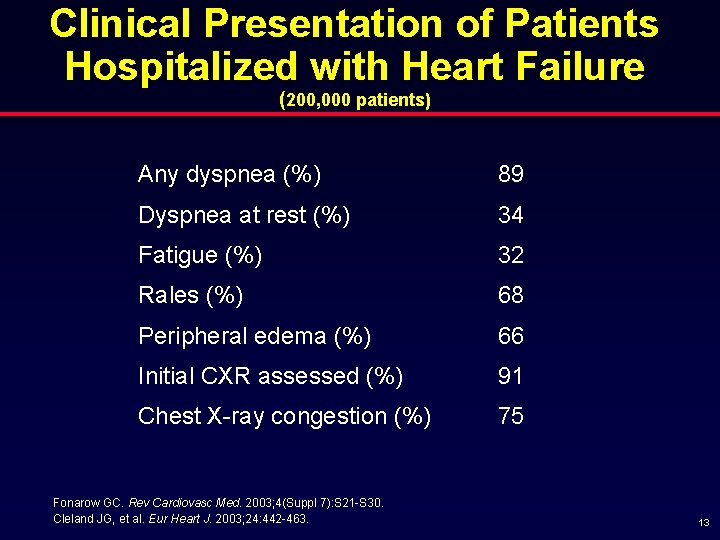
Clinical Presentation of Patients Hospitalized with Heart Failure (200, 000 patients) Any dyspnea (%) 89 Dyspnea at rest (%) 34 Fatigue (%) 32 Rales (%) 68 Peripheral edema (%) 66 Initial CXR assessed (%) 91 Chest X-ray congestion (%) 75 Fonarow GC. Rev Cardiovasc Med. 2003; 4(Suppl 7): S 21 -S 30. Cleland JG, et al. Eur Heart J. 2003; 24: 442 -463. 13
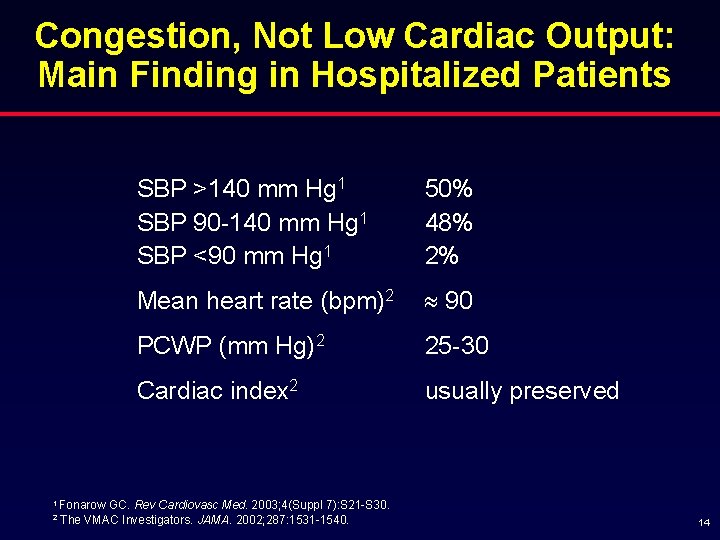
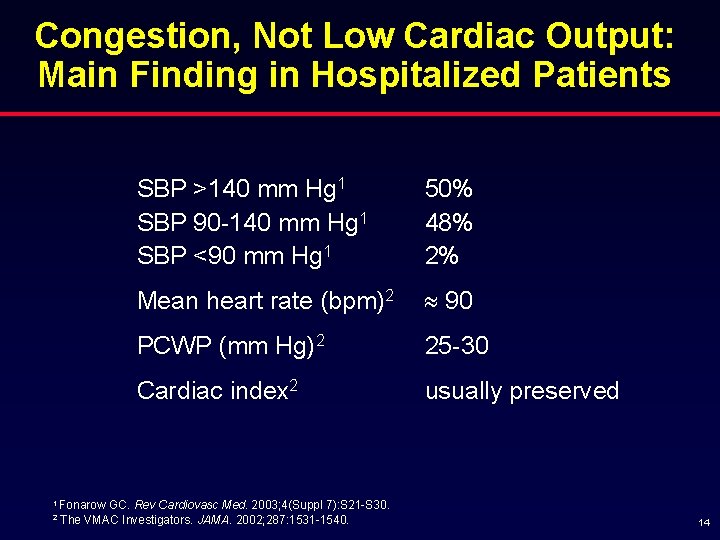
Congestion, Not Low Cardiac Output: Main Finding in Hospitalized Patients SBP >140 mm Hg 1 SBP 90 -140 mm Hg 1 SBP <90 mm Hg 1 50% 48% 2% Mean heart rate (bpm)2 90 PCWP (mm Hg)2 25 -30 Cardiac index 2 usually preserved 1 Fonarow 2 GC. Rev Cardiovasc Med. 2003; 4(Suppl 7): S 21 -S 30. The VMAC Investigators. JAMA. 2002; 287: 1531 -1540. 14
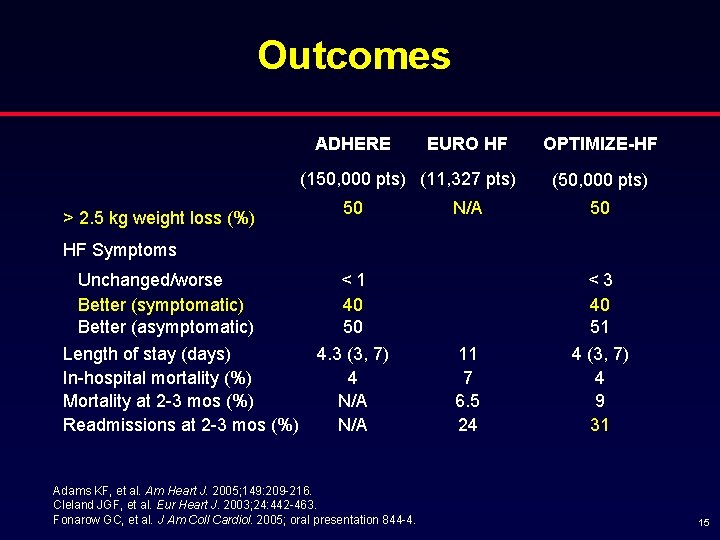
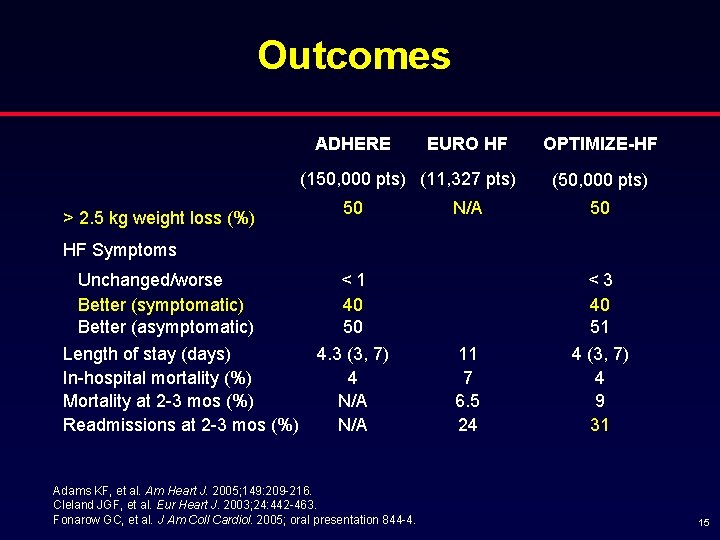
Outcomes ADHERE EURO HF (150, 000 pts) (11, 327 pts) > 2. 5 kg weight loss (%) 50 N/A OPTIMIZE-HF (50, 000 pts) 50 HF Symptoms Unchanged/worse Better (symptomatic) Better (asymptomatic) Length of stay (days) In-hospital mortality (%) Mortality at 2 -3 mos (%) Readmissions at 2 -3 mos (%) <1 40 50 4. 3 (3, 7) 4 N/A Adams KF, et al. Am Heart J. 2005; 149: 209 -216. Cleland JGF, et al. Eur Heart J. 2003; 24: 442 -463. Fonarow GC, et al. J Am Coll Cardiol. 2005; oral presentation 844 -4. <3 40 51 11 7 6. 5 24 4 (3, 7) 4 9 31 15
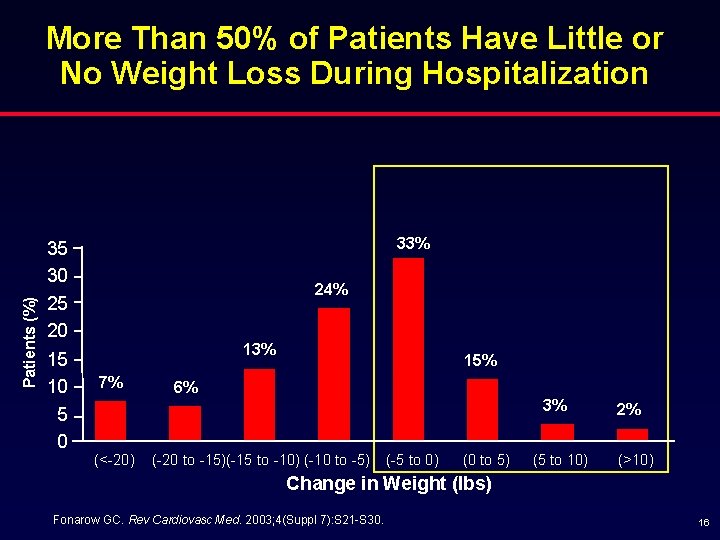
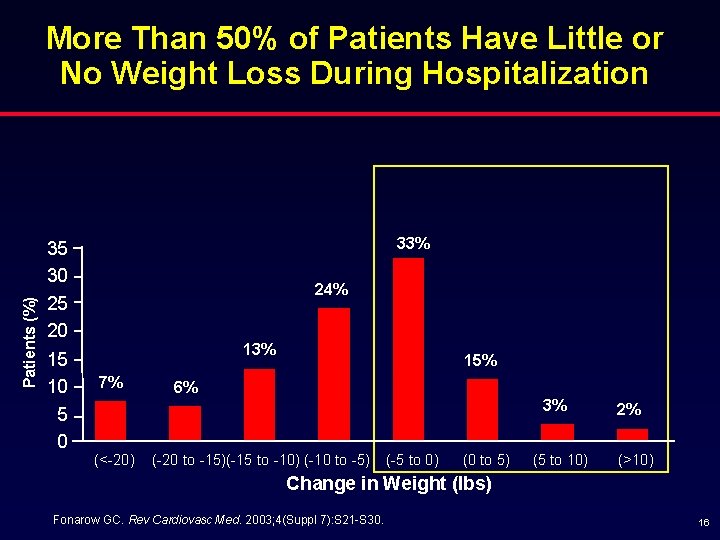
Patients (%) More Than 50% of Patients Have Little or No Weight Loss During Hospitalization 35 30 25 20 15 10 5 0 33% 24% 13% 7% (<-20) 15% 6% 3% (-20 to -15)(-15 to -10) (-10 to -5) (-5 to 0) (0 to 5) (5 to 10) 2% (>10) Change in Weight (lbs) Fonarow GC. Rev Cardiovasc Med. 2003; 4(Suppl 7): S 21 -S 30. 16
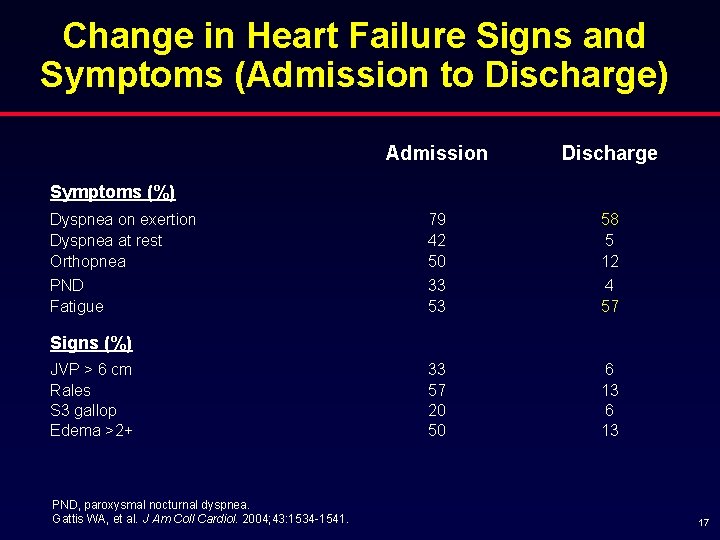
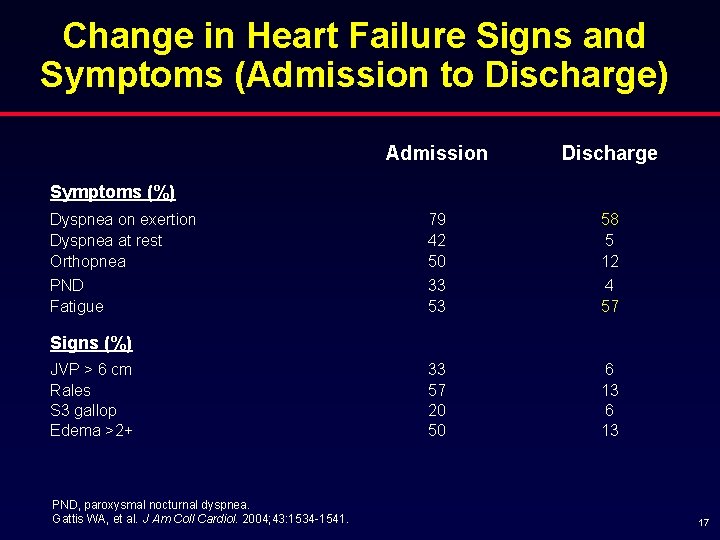
Change in Heart Failure Signs and Symptoms (Admission to Discharge) Admission Discharge 79 42 50 33 53 58 5 12 4 57 33 57 20 50 6 13 Symptoms (%) Dyspnea on exertion Dyspnea at rest Orthopnea PND Fatigue Signs (%) JVP > 6 cm Rales S 3 gallop Edema >2+ PND, paroxysmal nocturnal dyspnea. Gattis WA, et al. J Am Coll Cardiol. 2004; 43: 1534 -1541. 17
Hospitalizations for Heart Failure § Clinical congestion is the primary reason for HF admissions § Low cardiac output and associated signs/symptoms are uncommon § Suboptimal weight reduction during hospitalization § Although appearing improved clinically, many patients are discharged with signs and symptoms (related to hemodynamic congestion that is not being identified clinically) 18
Congestion and Prognosis in Heart Failure 19
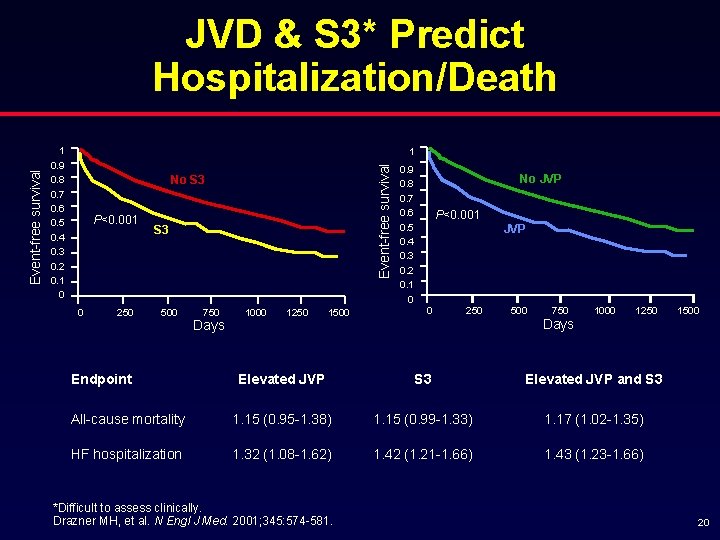
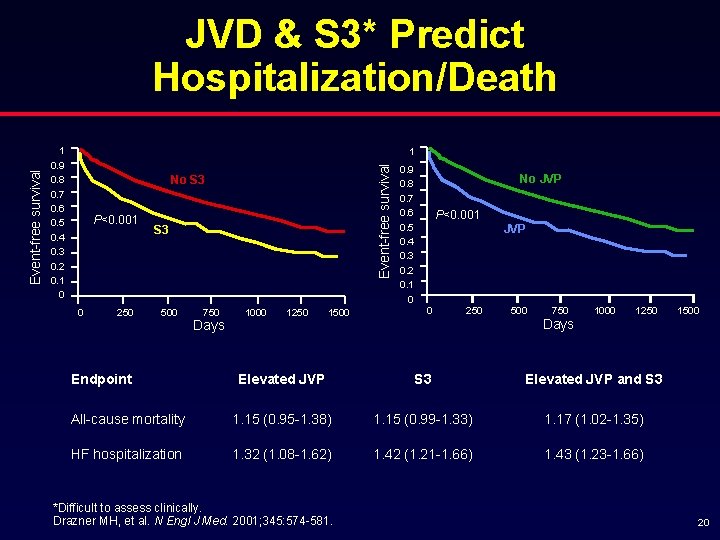
1 0. 9 0. 8 0. 7 0. 6 0. 5 0. 4 0. 3 0. 2 0. 1 0 1 Event-free survival JVD & S 3* Predict Hospitalization/Death No S 3 P<0. 001 0 250 S 3 500 Endpoint 750 Days 1000 1250 1500 0. 9 0. 8 0. 7 0. 6 0. 5 0. 4 0. 3 0. 2 0. 1 0 No JVP P<0. 001 JVP 0 250 500 750 Days 1000 1250 Elevated JVP S 3 Elevated JVP and S 3 All-cause mortality 1. 15 (0. 95 -1. 38) 1. 15 (0. 99 -1. 33) 1. 17 (1. 02 -1. 35) HF hospitalization 1. 32 (1. 08 -1. 62) 1. 42 (1. 21 -1. 66) 1. 43 (1. 23 -1. 66) *Difficult to assess clinically. Drazner MH, et al. N Engl J Med. 2001; 345: 574 -581. 1500 20

High PCWP at Hospital Discharge Is Associated with Higher Long-Term Mortality 60 60 Mortality (%) 50 50 PCWP >16 mm. Hg N=199 40 40 P=0. 001 30 20 30 10 10 0 0 6 12 18 Time (months) Fonarow GC, et al. Circulation. 1994; 90: I-488. P=NS 20 PCWP ≤ 16 mm. Hg N=257 0 CI >2. 6 L/min/m 2 N=236 24 0 6 CI ≤ 2. 6 L/min/m 2 N=220 12 18 Time (months) 24 21
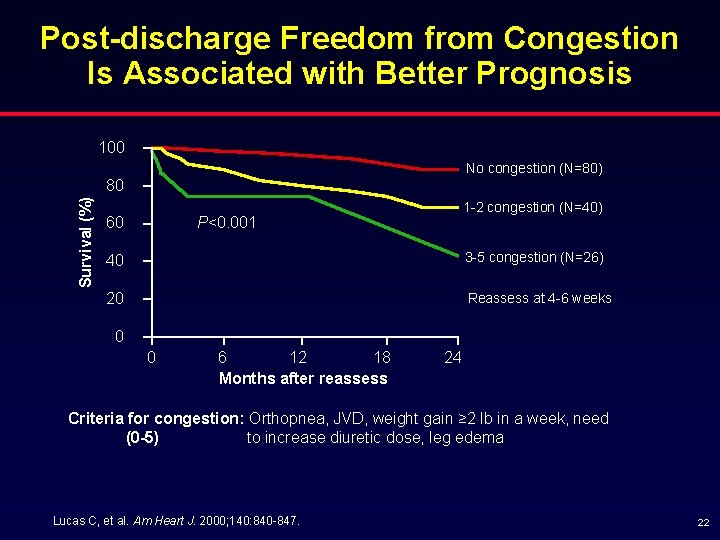
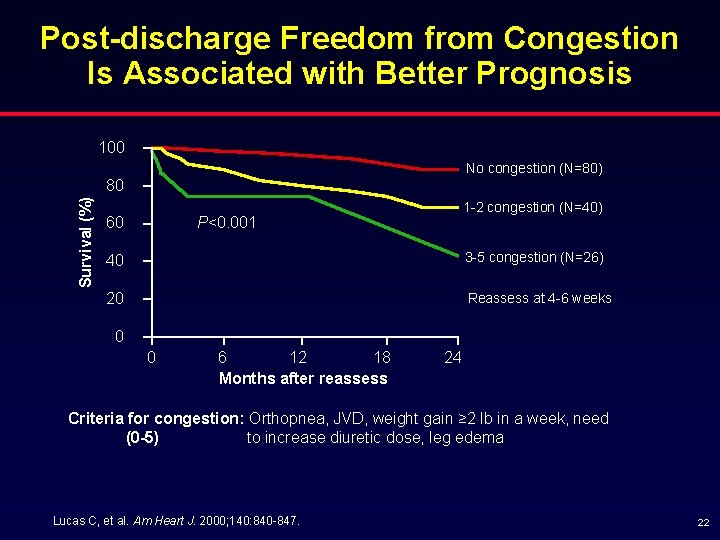
Post-discharge Freedom from Congestion Is Associated with Better Prognosis 100 No congestion (N=80) Survival (%) 80 60 1 -2 congestion (N=40) P<0. 001 40 3 -5 congestion (N=26) 20 Reassess at 4 -6 weeks 0 0 6 12 18 Months after reassess 24 Criteria for congestion: Orthopnea, JVD, weight gain ≥ 2 lb in a week, need (0 -5) to increase diuretic dose, leg edema Lucas C, et al. Am Heart J. 2000; 140: 840 -847. 22
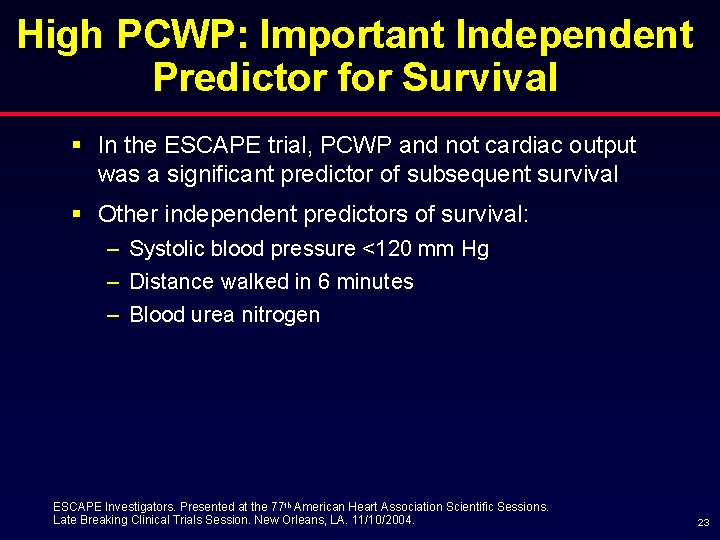
High PCWP: Important Independent Predictor for Survival § In the ESCAPE trial, PCWP and not cardiac output was a significant predictor of subsequent survival § Other independent predictors of survival: – Systolic blood pressure <120 mm Hg – Distance walked in 6 minutes – Blood urea nitrogen ESCAPE Investigators. Presented at the 77 th American Heart Association Scientific Sessions. Late Breaking Clinical Trials Session. New Orleans, LA. 11/10/2004. 23

Pathophysiology of Congestion Way congestion develops? What are the consequences? 24
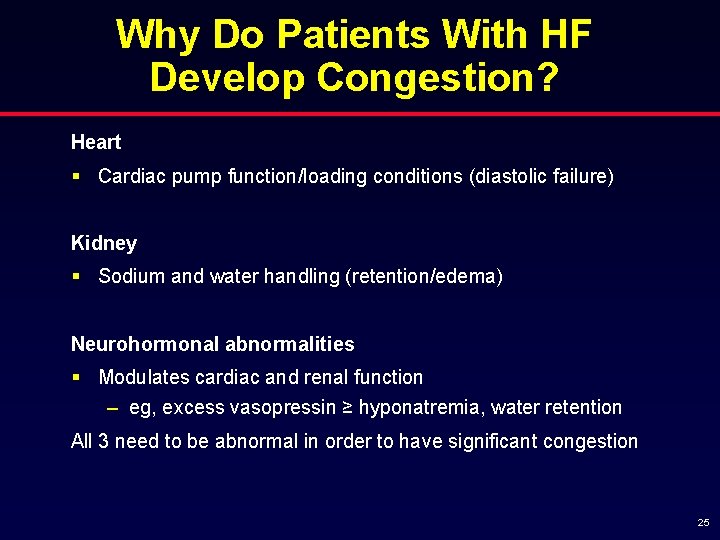
Why Do Patients With HF Develop Congestion? Heart § Cardiac pump function/loading conditions (diastolic failure) Kidney § Sodium and water handling (retention/edema) Neurohormonal abnormalities § Modulates cardiac and renal function – eg, excess vasopressin ≥ hyponatremia, water retention All 3 need to be abnormal in order to have significant congestion 25
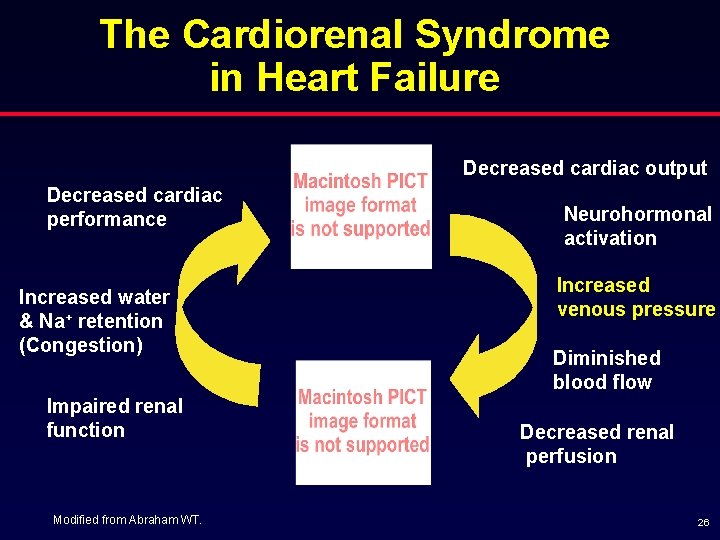
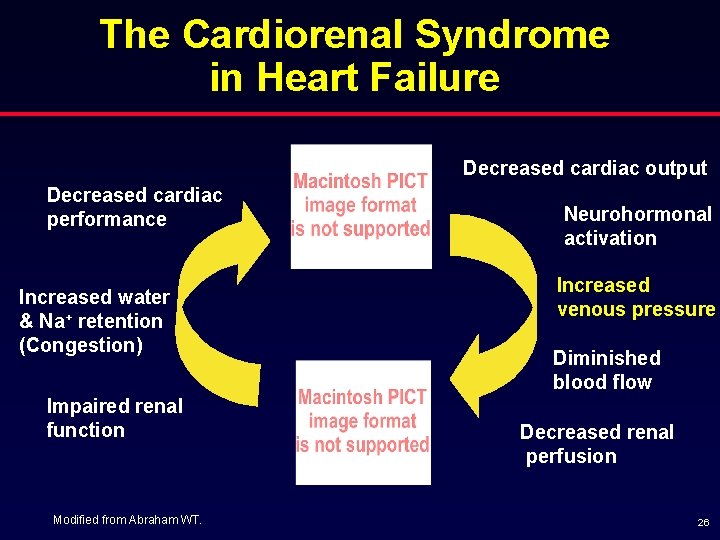
The Cardiorenal Syndrome in Heart Failure Decreased cardiac output Decreased cardiac performance Increased water & Na+ retention (Congestion) Impaired renal function Modified from Abraham WT. Neurohormonal activation Increased venous pressure Diminished blood flow Decreased renal perfusion 26
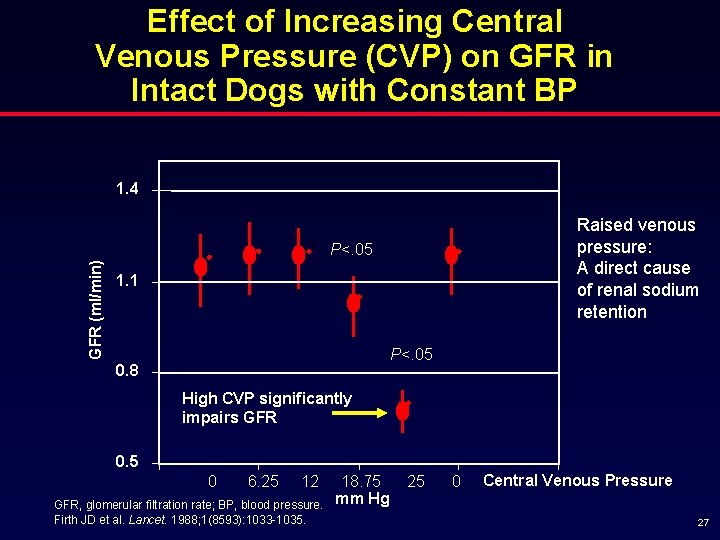
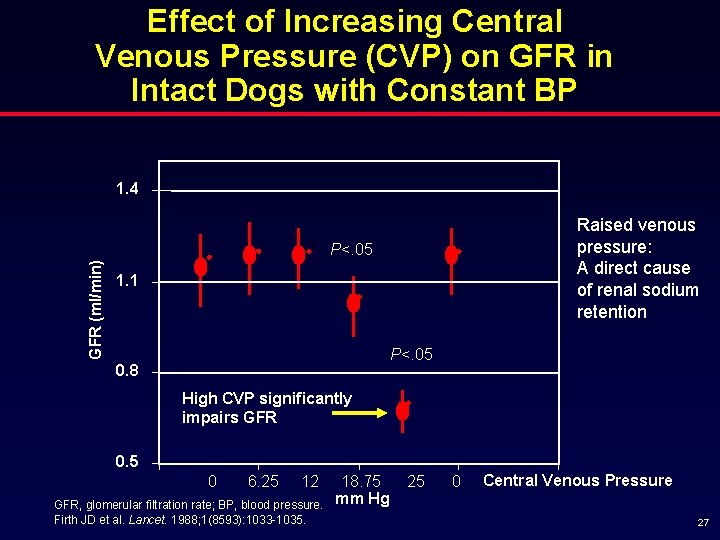
Effect of Increasing Central Venous Pressure (CVP) on GFR in Intact Dogs with Constant BP 1. 4 Raised venous pressure: A direct cause of renal sodium retention GFR (ml/min) P<. 05 1. 1 P<. 05 0. 8 High CVP significantly impairs GFR 0. 5 0 0 6. 25 2 12 GFR, glomerular filtration rate; BP, blood pressure. Firth JD et al. Lancet. 1988; 1(8593): 1033 -1035. 18. 75 4 Hg mm 25 0 6 Central Venous Pressure 8 27
Congestion May Contribute to the Progression of Heart Failure in Patients Admitted With HF 28
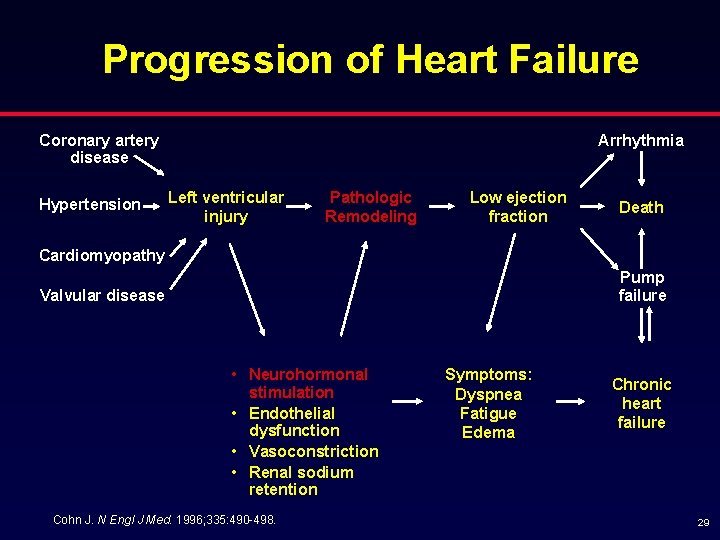
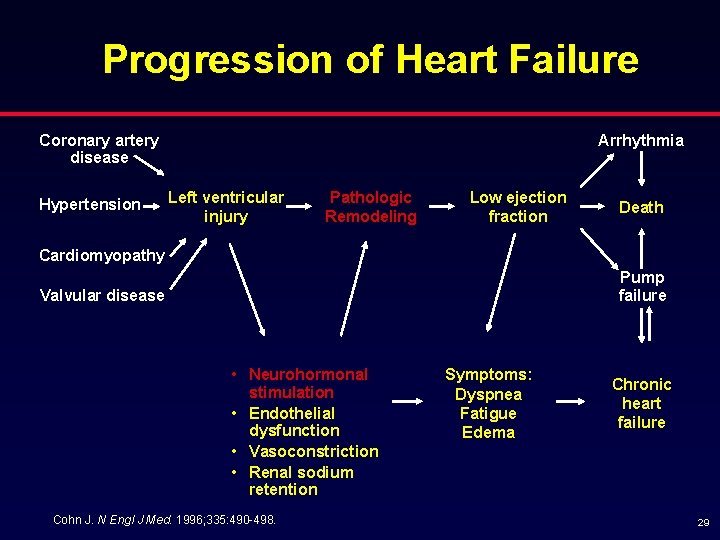
Progression of Heart Failure Coronary artery disease Hypertension Arrhythmia Left ventricular injury Pathologic Remodeling Low ejection fraction Death Cardiomyopathy Pump failure Valvular disease • Neurohormonal stimulation • Endothelial dysfunction • Vasoconstriction • Renal sodium retention Cohn J. N Engl J Med. 1996; 335: 490 -498. Symptoms: Dyspnea Fatigue Edema Chronic heart failure 29
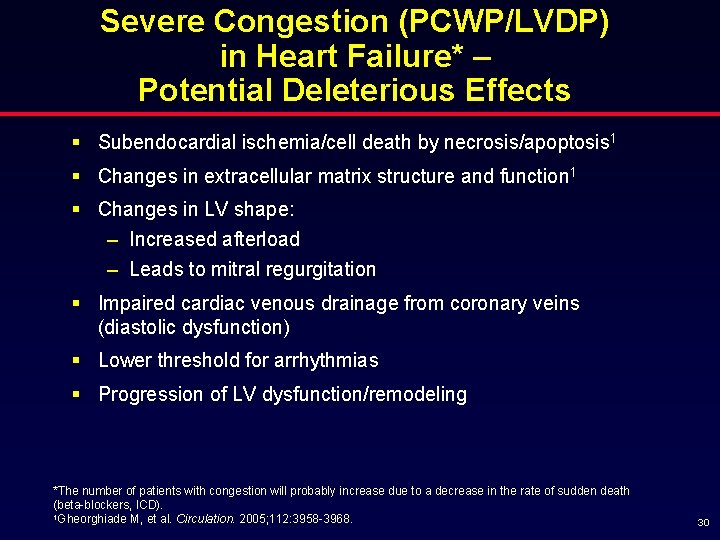
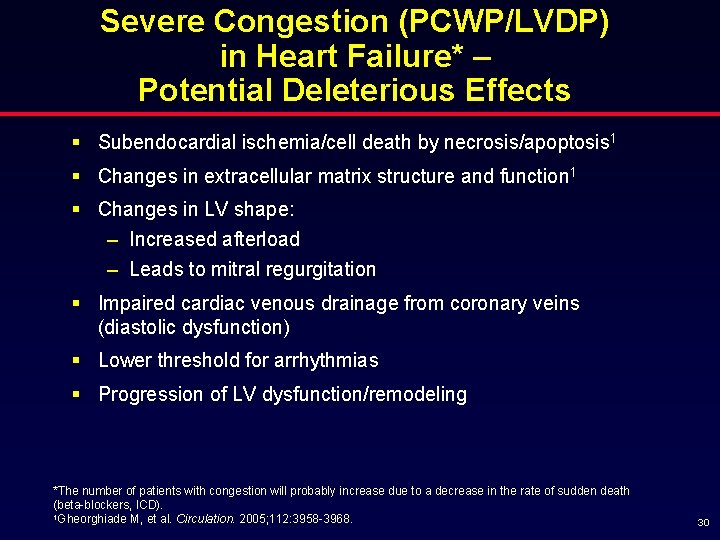
Severe Congestion (PCWP/LVDP) in Heart Failure* – Potential Deleterious Effects § Subendocardial ischemia/cell death by necrosis/apoptosis 1 § Changes in extracellular matrix structure and function 1 § Changes in LV shape: – Increased afterload – Leads to mitral regurgitation § Impaired cardiac venous drainage from coronary veins (diastolic dysfunction) § Lower threshold for arrhythmias § Progression of LV dysfunction/remodeling *The number of patients with congestion will probably increase due to a decrease in the rate of sudden death (beta-blockers, ICD). 1 Gheorghiade M, et al. Circulation. 2005; 112: 3958 -3968. 30
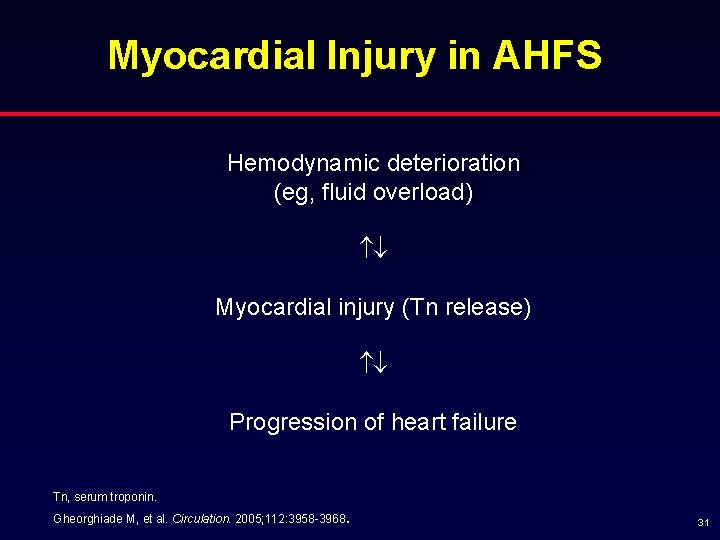
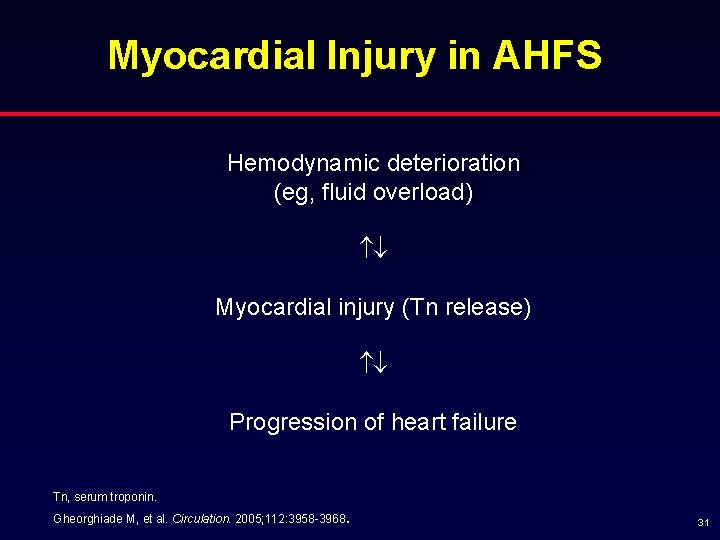
Myocardial Injury in AHFS Hemodynamic deterioration (eg, fluid overload) Myocardial injury (Tn release) Progression of heart failure Tn, serum troponin. . Gheorghiade M, et al. Circulation. 2005; 112: 3958 -3968 31
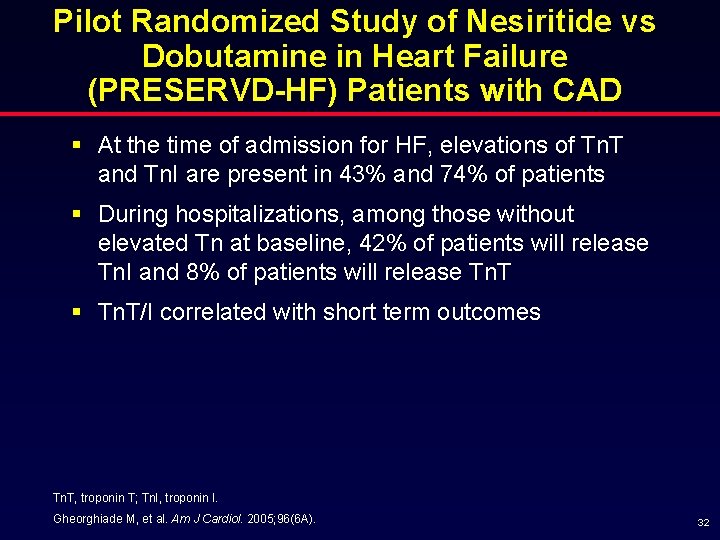
Pilot Randomized Study of Nesiritide vs Dobutamine in Heart Failure (PRESERVD-HF) Patients with CAD § At the time of admission for HF, elevations of Tn. T and Tn. I are present in 43% and 74% of patients § During hospitalizations, among those without elevated Tn at baseline, 42% of patients will release Tn. I and 8% of patients will release Tn. T § Tn. T/I correlated with short term outcomes Tn. T, troponin T; Tn. I, troponin I. Gheorghiade M, et al. Am J Cardiol. 2005; 96(6 A). 32
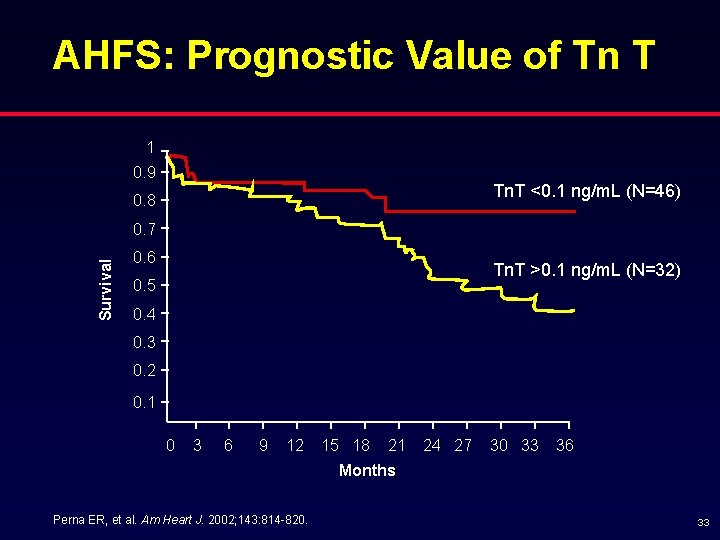
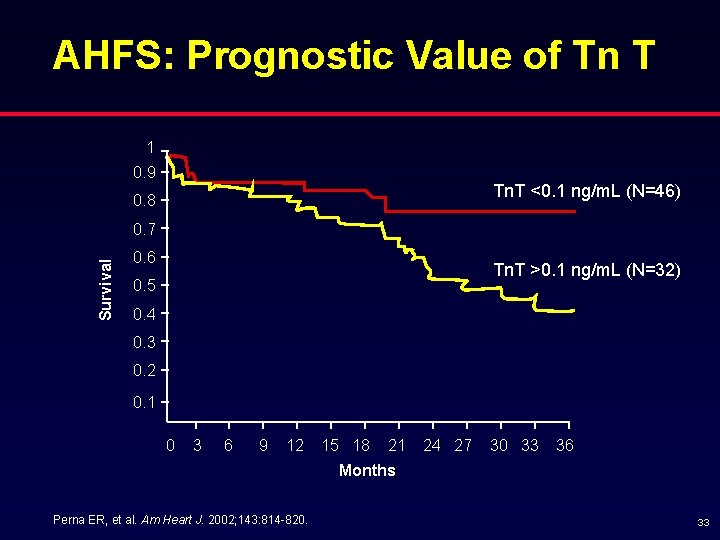
AHFS: Prognostic Value of Tn T 1 0. 9 Tn. T <0. 1 ng/m. L (N=46) 0. 8 Survival 0. 7 0. 6 Tn. T >0. 1 ng/m. L (N=32) 0. 5 0. 4 0. 3 0. 2 0. 1 0 3 6 9 12 15 18 21 24 27 30 33 36 Months Perna ER, et al. Am Heart J. 2002; 143: 814 -820. 33
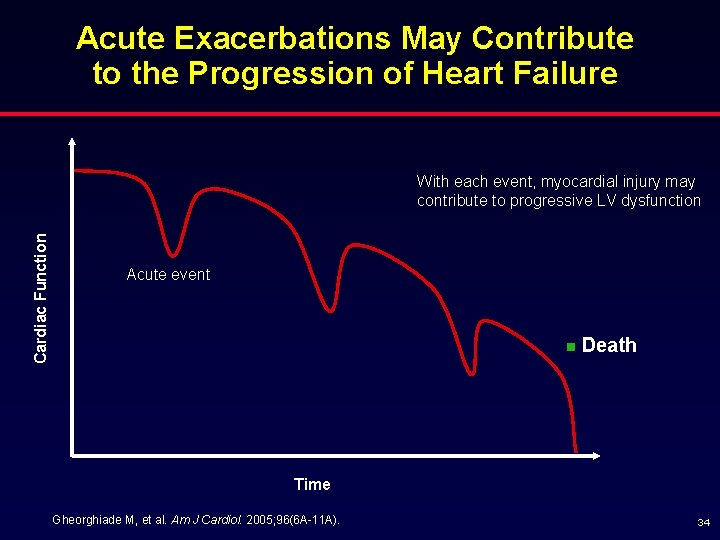
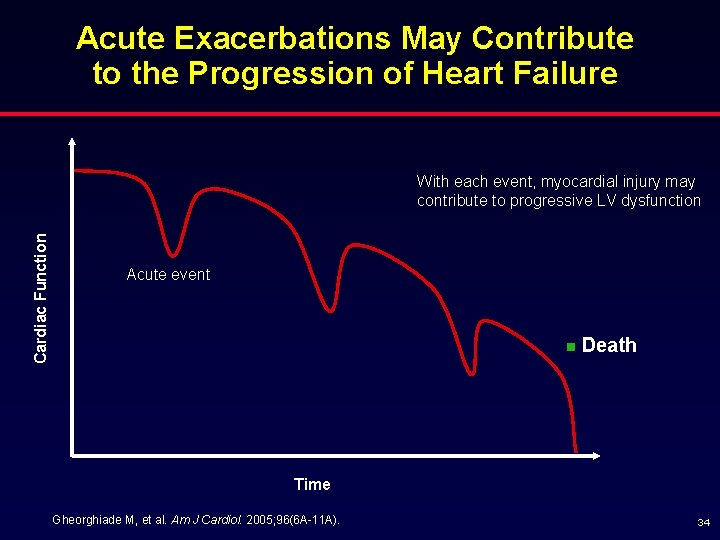
Acute Exacerbations May Contribute to the Progression of Heart Failure Cardiac Function With each event, myocardial injury may contribute to progressive LV dysfunction Acute event n Death Time Gheorghiade M, et al. Am J Cardiol. 2005; 96(6 A-11 A). 34
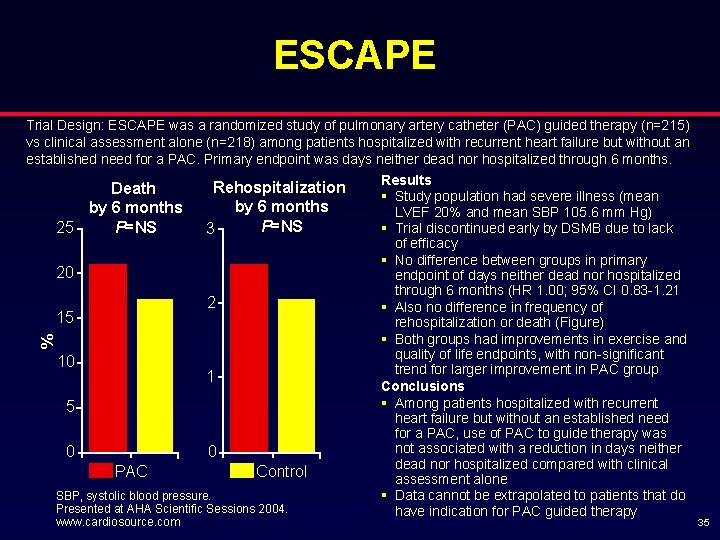
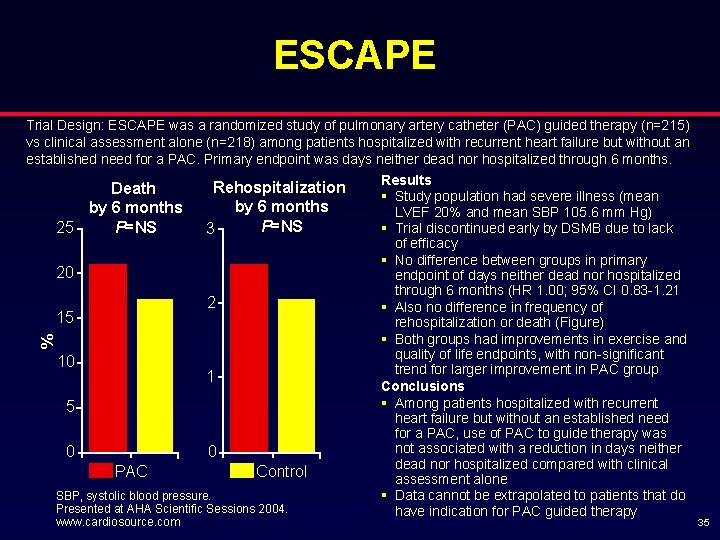
ESCAPE % Trial Design: ESCAPE was a randomized study of pulmonary artery catheter (PAC) guided therapy (n=215) vs clinical assessment alone (n=218) among patients hospitalized with recurrent heart failure but without an established need for a PAC. Primary endpoint was days neither dead nor hospitalized through 6 months. Results Rehospitalization Death § Study population had severe illness (mean by 6 months LVEF 20% and mean SBP 105. 6 mm Hg) P=NS § Trial discontinued early by DSMB due to lack 25 3 of efficacy § No difference between groups in primary 20 endpoint of days neither dead nor hospitalized through 6 months (HR 1. 00; 95% CI 0. 83 -1. 21 2 § Also no difference in frequency of 15 rehospitalization or death (Figure) § Both groups had improvements in exercise and quality of life endpoints, with non-significant 10 trend for larger improvement in PAC group 1 Conclusions § Among patients hospitalized with recurrent 5 heart failure but without an established need for a PAC, use of PAC to guide therapy was not associated with a reduction in days neither 0 0 dead nor hospitalized compared with clinical PAC Control assessment alone SBP, systolic blood pressure. § Data cannot be extrapolated to patients that do Presented at AHA Scientific Sessions 2004. have indication for PAC guided therapy www. cardiosource. com 35
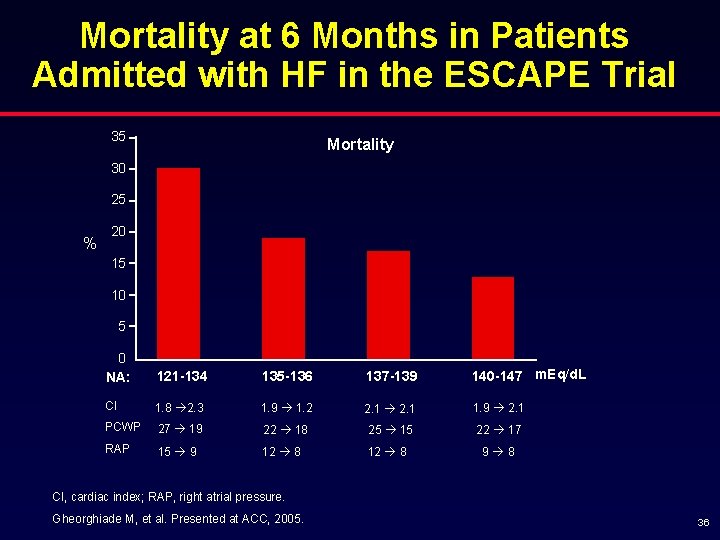
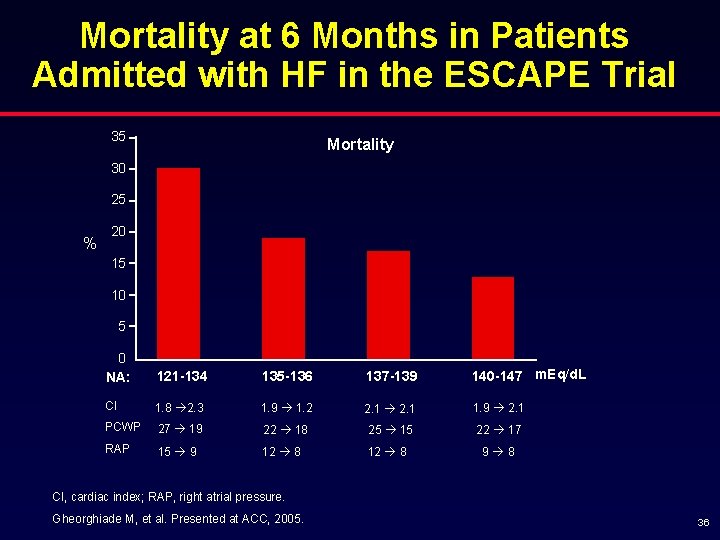
Mortality at 6 Months in Patients Admitted with HF in the ESCAPE Trial 35 Mortality 30 25 % 20 15 10 5 0 NA: 121 -134 135 -136 137 -139 140 -147 m. Eq/d. L CI 1. 8 2. 3 1. 9 1. 2 2. 1 1. 9 2. 1 PCWP 27 19 22 18 25 15 22 17 RAP 15 9 12 8 9 8 CI, cardiac index; RAP, right atrial pressure. Gheorghiade M, et al. Presented at ACC, 2005. 36
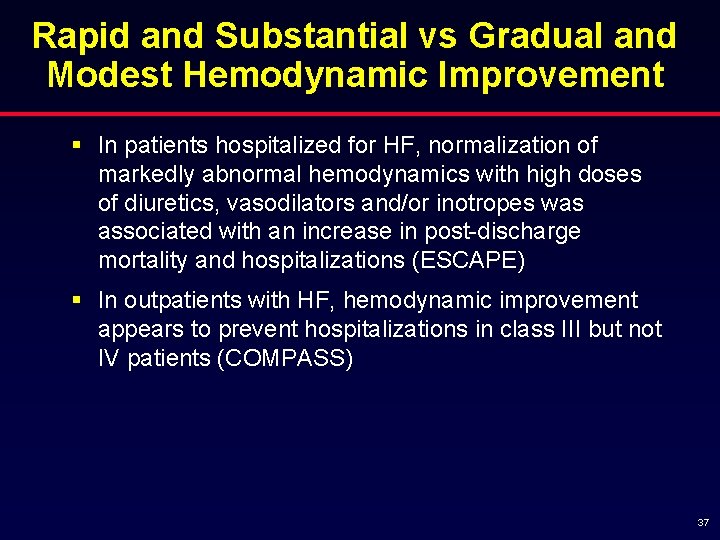
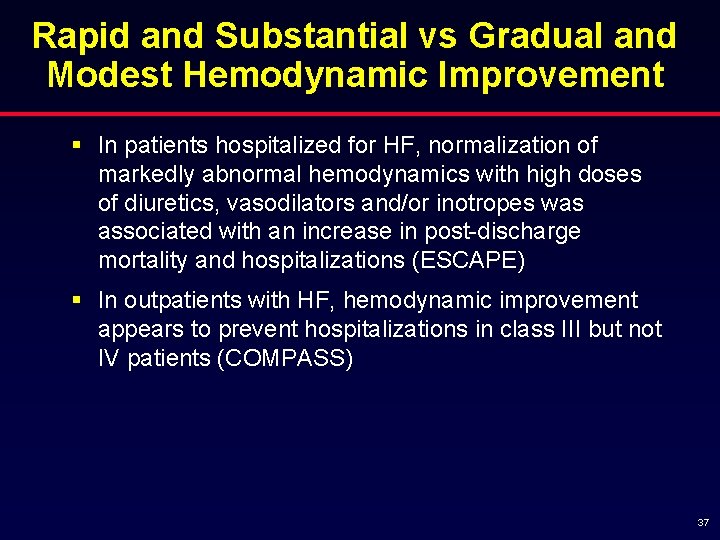
Rapid and Substantial vs Gradual and Modest Hemodynamic Improvement § In patients hospitalized for HF, normalization of markedly abnormal hemodynamics with high doses of diuretics, vasodilators and/or inotropes was associated with an increase in post-discharge mortality and hospitalizations (ESCAPE) § In outpatients with HF, hemodynamic improvement appears to prevent hospitalizations in class III but not IV patients (COMPASS) 37
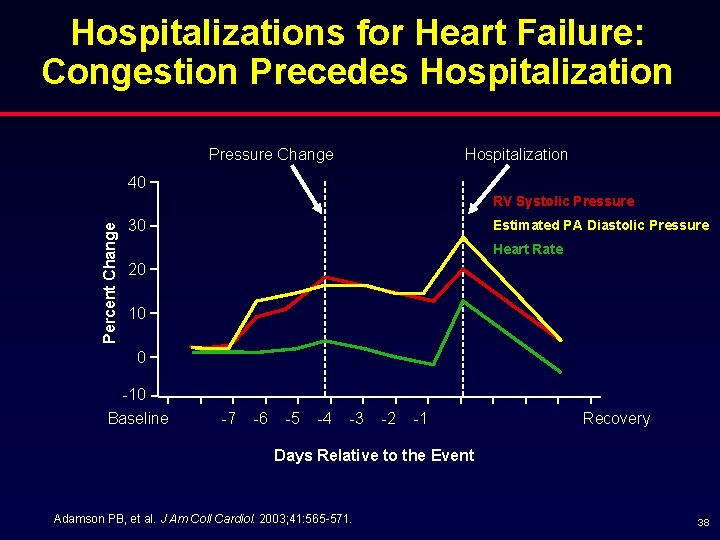
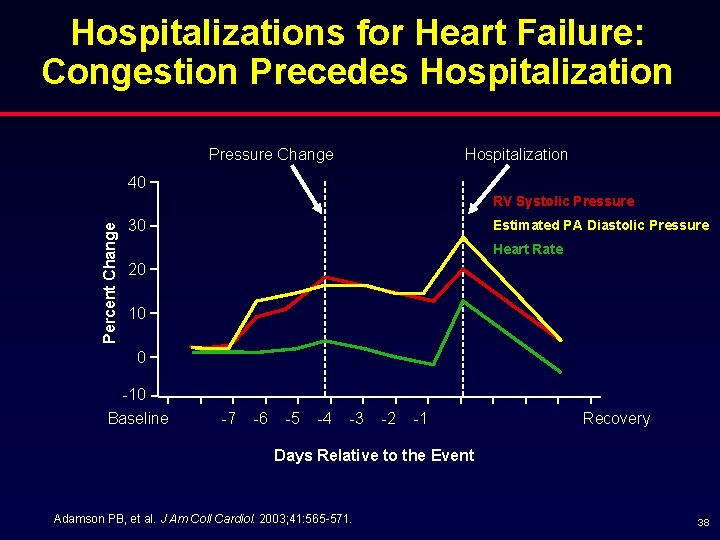
Hospitalizations for Heart Failure: Congestion Precedes Hospitalization Pressure Change Hospitalization 40 Percent Change RV Systolic Pressure Estimated PA Diastolic Pressure 30 Heart Rate 20 10 0 -10 Baseline -7 -6 -5 -4 -3 -2 -1 Recovery Days Relative to the Event Adamson PB, et al. J Am Coll Cardiol. 2003; 41: 565 -571. 38
Congestion in HF: Conclusions § Congestion is an important predictor of mortality and morbidity § Congestion is the primary cause of HF hospital admissions and predicts readmissions § Hemodynamic congestion is often difficult to recognize, delaying appropriate interventions § Clinical congestion often lags behind hemodynamic congestion § Congestion may contribute to the progression of HF 39
Hemodynamic Congestion § Hemodynamic or cardiopulmonary congestion (elevated PCWP) starts days or weeks prior to hospitalization § May occur in the absence of signs (rales, JVD, edema) or symptoms of clinical congestion § Early treatment of hemodynamic congestion may prevent hospitalization and progression of heart failure § Improved methods of monitoring hemodynamic congestion may improve clinical management and outcomes 40
Why Prevent Hospitalizations*? § Prevent possible myocardial injury (progression of HF) § Once the patient is hospitalized, we're forced to use interventions (eg, inotropic agents) that may cause myocardial injury § High post-discharge mortality and hospitalizations § Cost *The most important predictor of prognosis. Gheorghiade M, et al. Circulation. 2005; 112: 3958 -3968. 41
ACC/AHA HF Performance Measures: Outpatient § Initial laboratory tests § Left ventricular systolic function assessment § Weight measurement § Blood pressure measurement § Assessment of clinical symptoms of congestion § Assessment of clinical signs of congestion § Assessment of activity level § Patient education § Beta-blocker therapy in patients with HF and LVSD § ACEI or ARB in patients with HF and LVSD § Warfarin therapy in patients with atrial fibrillation ACC/AHA, American College of Cardiology/American Heart Association; ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker. Bonow RO, et al. J Amer Coll Cardiol. 2005; 46: 1144 -1178. 42
 Mihai gheorghiade
Mihai gheorghiade Circumciliary congestion and conjunctival congestion
Circumciliary congestion and conjunctival congestion Non conducted pac ecg
Non conducted pac ecg Supparerk vision center
Supparerk vision center Cup and cone fracture
Cup and cone fracture Promotion from associate professor to professor
Promotion from associate professor to professor Heart failure complications
Heart failure complications Compensatory mechanisms of heart failure
Compensatory mechanisms of heart failure Keith rn heart failure case study
Keith rn heart failure case study Causes of cardiomegaly in child
Causes of cardiomegaly in child Pvkov
Pvkov Chapter 24 heart failure drugs
Chapter 24 heart failure drugs Right sided heart failure
Right sided heart failure Forrester classification heart failure
Forrester classification heart failure Donkey analogy heart failure
Donkey analogy heart failure Nursing assessment for congestive heart failure
Nursing assessment for congestive heart failure Vetsulin dosage chart for dogs
Vetsulin dosage chart for dogs Congestive heart failure zones for management
Congestive heart failure zones for management Heart failure
Heart failure Heart failure definition
Heart failure definition Acute vs chronic heart failure
Acute vs chronic heart failure Congestive heart failure symtoms
Congestive heart failure symtoms Nursing assessment for congestive heart failure
Nursing assessment for congestive heart failure Diabetes and heart failure
Diabetes and heart failure Lmnop heart failure
Lmnop heart failure Heart failure definition
Heart failure definition Right vs left-sided heart failure chart
Right vs left-sided heart failure chart Acute pulmonary congestion histology
Acute pulmonary congestion histology Spleen congestion
Spleen congestion Conclusion of traffic congestion
Conclusion of traffic congestion General principles of congestion control
General principles of congestion control Essential oils for pelvic congestion syndrome
Essential oils for pelvic congestion syndrome Congestion control in network layer
Congestion control in network layer Network congestion causes
Network congestion causes Traffic throttling and load shedding
Traffic throttling and load shedding Estasis de leche
Estasis de leche Congestion control in virtual circuit
Congestion control in virtual circuit In2140
In2140 Circumcorneal congestion
Circumcorneal congestion Principles of congestion control
Principles of congestion control What is choke packet
What is choke packet Traffic congestion essay
Traffic congestion essay Congestion prevention policies
Congestion prevention policies