Children and Young Peoples Mental Health Training 2020







- Slides: 106
Children and Young People’s Mental Health Training © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online

Welcome Please take a few minutes to complete the anonymous pre-course questionnaire by visiting www. wecantalk. online/pre Open a web browser and type the full address or click ‘Training’ on the We Can Talk website and scroll down to the link near the bottom. You must complete the pre- and post-course questionnaires to receive your certificate! © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online

Welcome Housekeeping © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Welcome Introductions © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Background Healthcare workers often report that they feel they lack the knowledge, skills and confidence to support young people with mental health problems. This training has been developed directly in response to the views, experiences and needs of young people and staff working in acute hospital settings. We Can Talk was developed with funding from Health Education England at Barts Health NHS Trust and works with hospitals across England in collaboration with the Common Room, Healthy Teen Minds and the Child Outcomes Research Consortium (CORC). It has been developed by a partnership between young people and adults with lived experience of mental health difficulties, acute hospital staff and mental health professionals. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Training overview The aims of today are to: • Recognise the role that hospital staff are already playing in supporting children and young people’s mental health • Develop an understanding of common mental health difficulties • Explore the different scenarios where you support children and young people who may be experiencing mental health difficulties • Understand the experiences of children and young people • Explore and understand how to communicate effectively with children and young people with mental health difficulties • Explore and understand key approaches to supporting children and young people © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Things to keep in mind • Mental health can be an emotive topic. If you need to take time out please do so. • We want to learn from experience, but please try not to use names or personal details. • Today is focused on building on your existing skills and experience, learning together, sharing practice, ideas and experiences. • Sometimes, the best way to learn is to share and reflect on examples where things haven’t gone so well. Please be respectful if people do share examples. • Don’t worry if you’re not sure the correct terminology to use about mental health. It’s better to say something than stay quiet. • It’s important to explore, discuss and debate, but try to challenge the idea not the person. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Your Role How do you support and care for children and young people who present to hospital in general? Thinking about your job role: • What do you see as your main responsibilities towards children and young people? • What do you practically do to care for young people? • What support do you provide to meet their needs? • Write your ideas down on the flipchart paper. Try to be as specific as you can and focus on all presentations (not just mental health). © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Your Role How do you support and care for children and young people who present to hospital in general? • When we ask children and young people who come to hospital for their mental health what made their experience a good one – they write the same list you have just written… • They tell us that a good experience is receiving care as usual • We don’t have to be mental health experts, we just need to show the care and compassion that we give to all patients. • But we know from talking to hospital staff that it feels different. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
© 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Your Role Now think about the times when you have supported children and young people with mental health difficulties in your role or service • • Describe some of the common situations where you support children and young people with mental health difficulties. What do you currently do to support them? Then think about you and your colleagues in these situations… • • • What do you find difficult, challenging or feel uncertain about? What are these experiences like for you? How do you feel in these situations? © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Your Role Supporting children and young people with mental health difficulties in your role or service What are the skills needed? a) A person who knows how to engage with children and young people, helps them feel safe and cared for, involves them in decisions about their care and encourages them to want to stay. b) Someone who has never worked with children or young people, doesn’t engage them or show interest in their care and might only have experience of working with adults with chronic mental illness in forensic settings. In child and adolescent inpatient mental health hospitals much of the direct care is provided by Healthcare Support Assistants (HCAs), without formal mental health training, who know how to engage and communicate with children and young people © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: RMNs • RMNs are Registered Nurses in Mental Health • Most RMNs work with adults and as a result they might not have received much or any undergraduate or post-graduate training on children and young people’s mental health • There are currently huge vacancies for RMNs within the Child and Adolescent Mental Health Service (CAMHS) system resulting in most RMNs with any experience of working with children and young people being ‘snapped up’ by these services • As a result, agency RMNs with little or no experience are routinely used to ‘special’ or ‘one-to-one’ in hospital resulting in poor experiences of care reported by children, young people and hospital staff • Only those with environment/service specific training in restraint, that includes managing challenging children and young people, should restrain (DHSC, 2017) including agency staff (DHSC, 2014) © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
© 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding mental wellbeing, mental health and mental health difficulties © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Mental health Does anyone not have physical health? When do we notice our physical health more? • • Lows – illness, exhaustion, stress, etc Highs – physical achievement, great sleep, etc Does anyone not have mental health? What mental health challenges will we all encounter? • Bereavement, stress, relationship breakup, financial? What mental health ‘highs’ might we encounter? • Births, marriages, achievement, annual leave? © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Mental health • Maintaining a good level of physical health does not mean we never get unwell. • Having a good level of mental health is not about having the ‘best life ever” but being able to get through the lows and experience the highs. • Mental health is something we can all relate to because we all experience our own mental health. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
“Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity. ” World Health Organization (WHO) © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
“Mental health is defined as a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community. ” World Health Organization (WHO) © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Mental Health Overview © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
“ 83% of people will experience a mental health problem in their lifetime” (American Psychological Association, 2016) © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
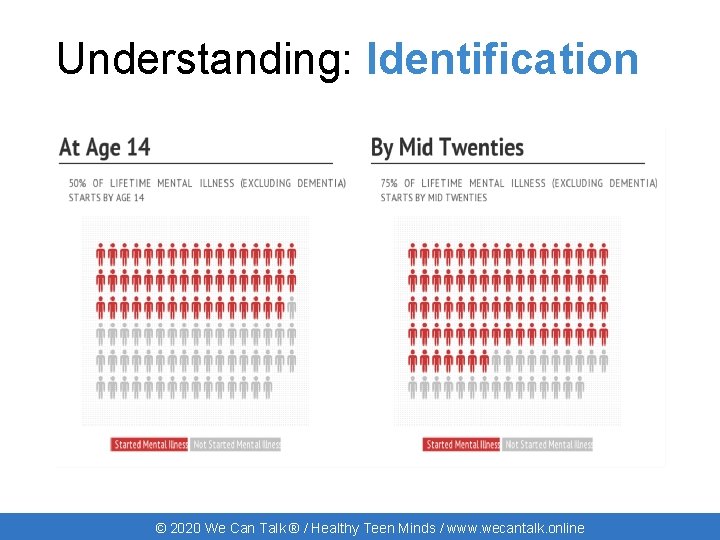
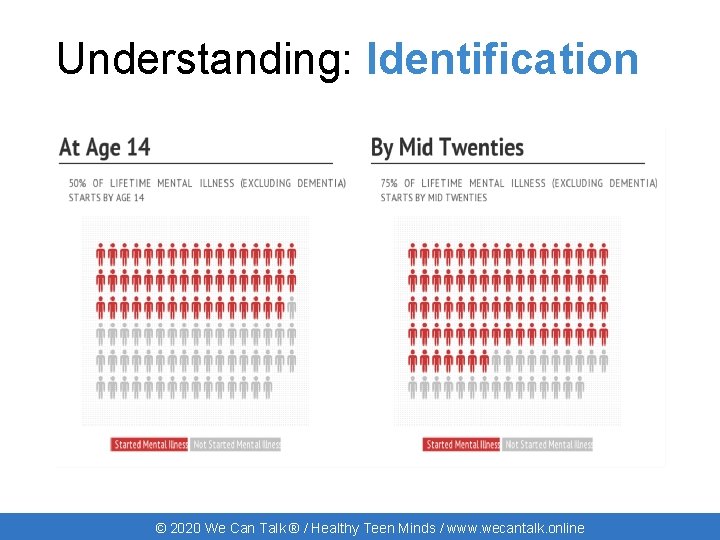
Understanding: Identification © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Identification 50% of chronic mental illness in adults starts before the age of 14 and 75% before the age of 25 (Link). Early identification in mental health has the same benefits of early identification in physical health. It can: • • Prevent illness Lead to better outcomes Allow for more treatment options Cost less to health services Spending on early intervention services for children and young people dropped by 49% (£ 3. 7 billion to £ 1. 9 billion) between 2010/11 and 2017/18. (The Children's Society, 2019). © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
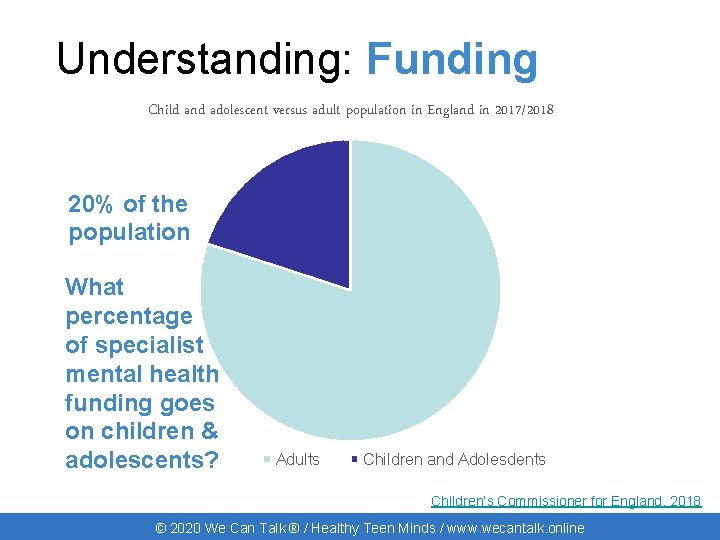
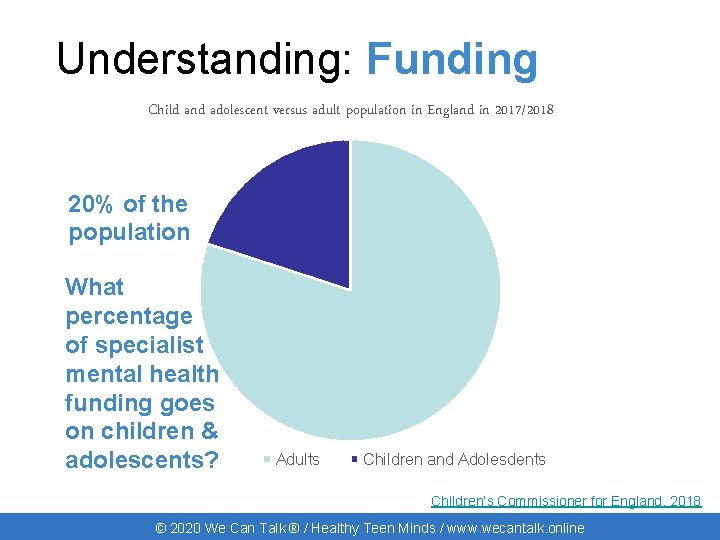
Understanding: Funding Child and adolescent versus adult population in England in 2017/2018 20% of the population What percentage of specialist mental health funding goes on children & adolescents? Adults Children and Adolesdents Children’s Commissioner for England, 2018 © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
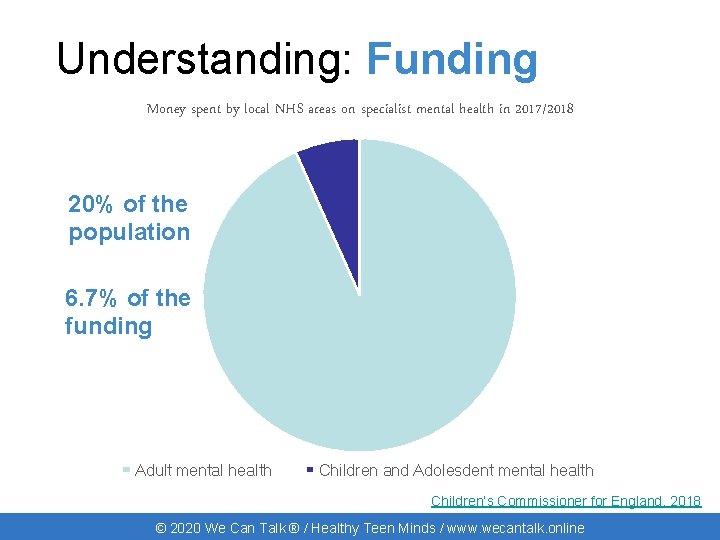
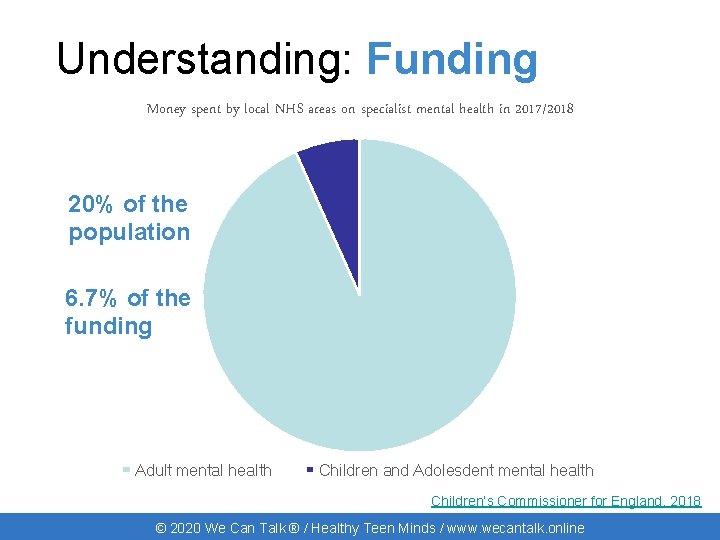
Understanding: Funding Money spent by local NHS areas on specialist mental health in 2017/2018 20% of the population 6. 7% of the funding Adult mental health Children and Adolesdent mental health Children’s Commissioner for England, 2018 © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
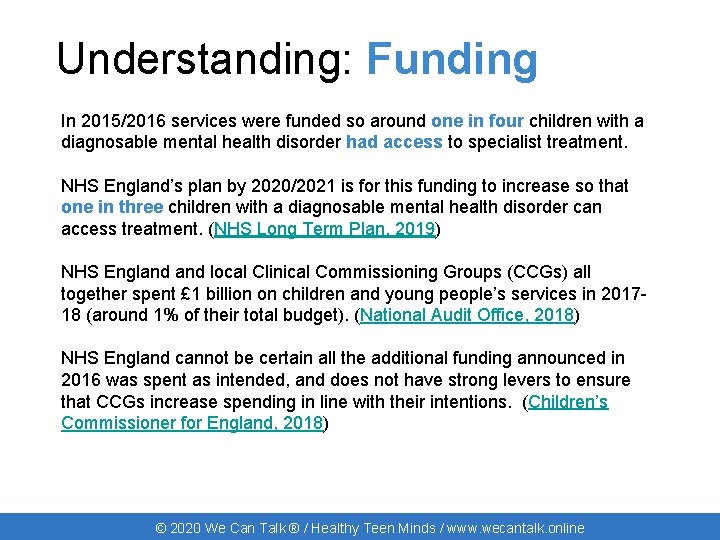
Understanding: Funding In 2015/2016 services were funded so around one in four children with a diagnosable mental health disorder had access to specialist treatment. NHS England’s plan by 2020/2021 is for this funding to increase so that one in three children with a diagnosable mental health disorder can access treatment. (NHS Long Term Plan, 2019) NHS England local Clinical Commissioning Groups (CCGs) all together spent £ 1 billion on children and young people’s services in 201718 (around 1% of their total budget). (National Audit Office, 2018) NHS England cannot be certain all the additional funding announced in 2016 was spent as intended, and does not have strong levers to ensure that CCGs increase spending in line with their intentions. (Children’s Commissioner for England, 2018) © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Defining: Depression © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Defining: Depression When we get “stuck” feeling down © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
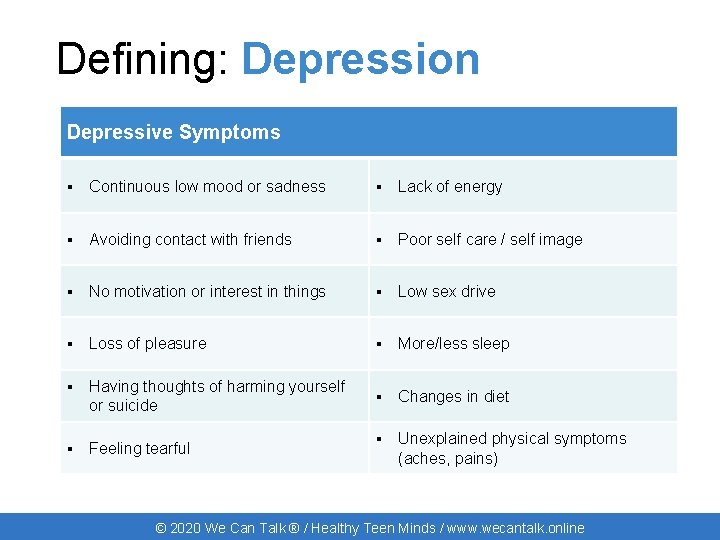
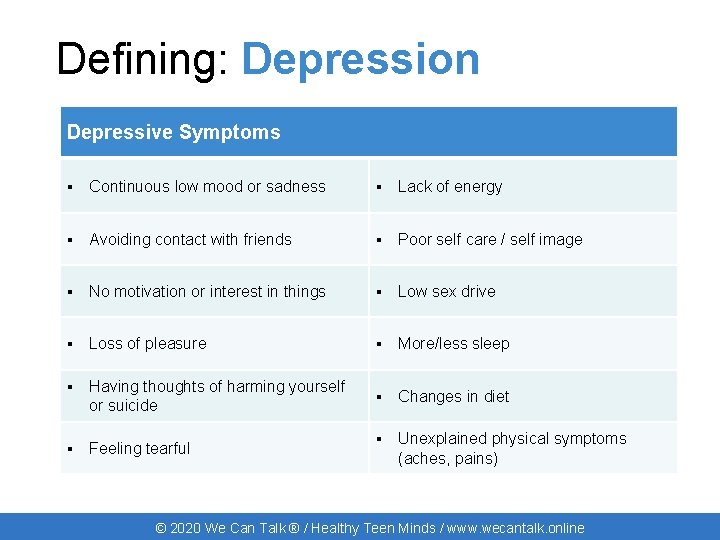
Defining: Depression Depressive Symptoms ▪ Continuous low mood or sadness ▪ Lack of energy ▪ Avoiding contact with friends ▪ Poor self care / self image ▪ No motivation or interest in things ▪ Low sex drive ▪ Loss of pleasure ▪ More/less sleep ▪ Having thoughts of harming yourself or suicide ▪ Changes in diet ▪ Feeling tearful ▪ Unexplained physical symptoms (aches, pains) © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Defining: Depression • Many people use the word ‘depression’ or ‘depressed’ to describe their mood when they’re not talking about a ‘clinical depression’ • It is normal for everyone to experience periods of sadness or low mood following trauma or other negative life events • Symptoms tick lists can give us some ideas but understanding the impact of their mood on the child or young person is key © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Defining: Anxiety © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Defining: Anxiety When our worries get in the way of our life © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
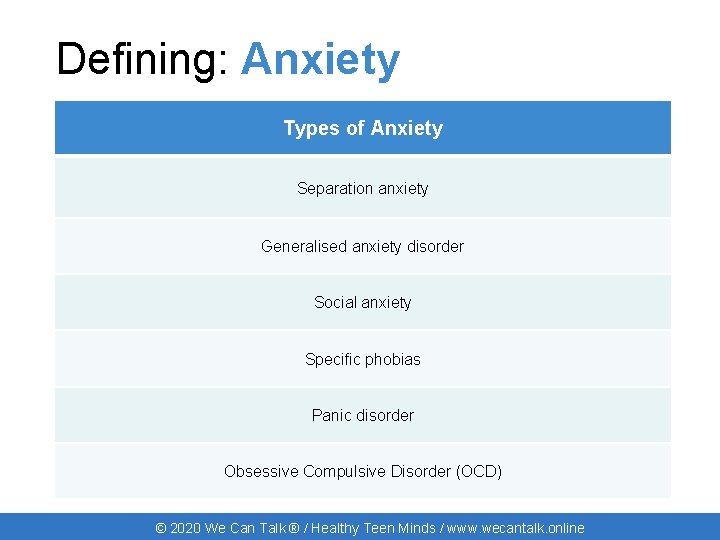
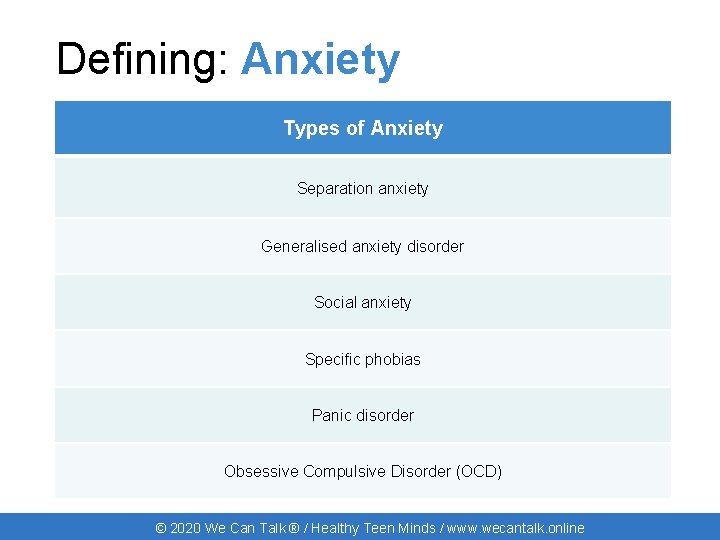
Defining: Anxiety Types of Anxiety Separation anxiety Generalised anxiety disorder Social anxiety Specific phobias Panic disorder Obsessive Compulsive Disorder (OCD) © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
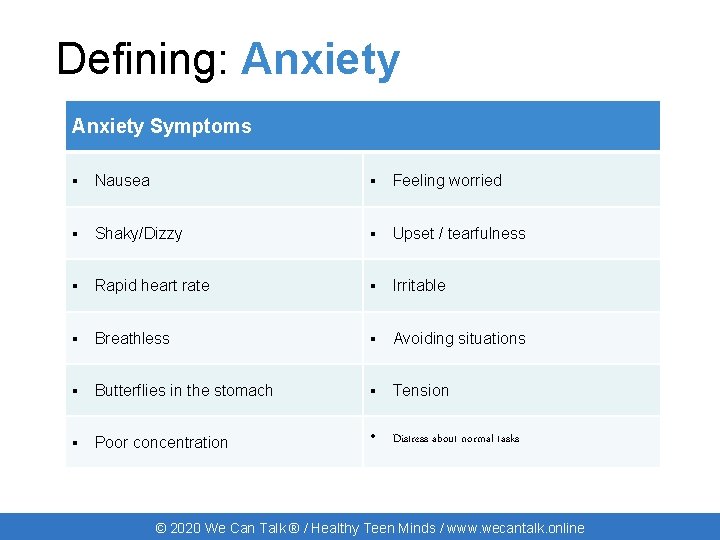
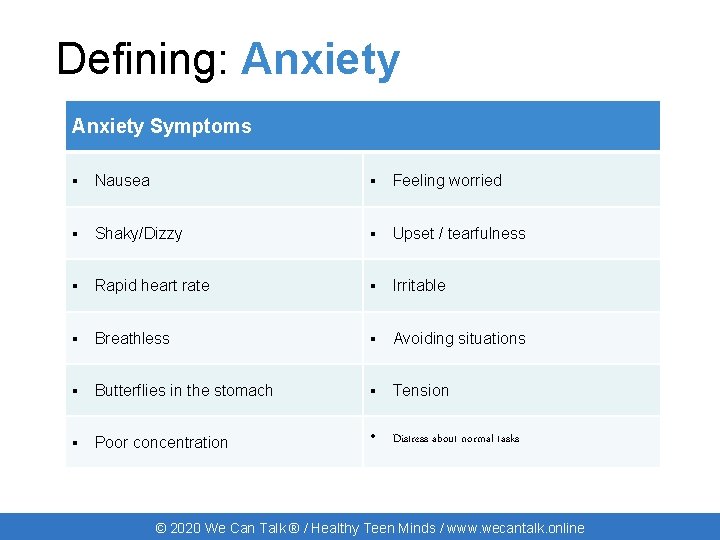
Defining: Anxiety Symptoms ▪ Nausea ▪ Feeling worried ▪ Shaky/Dizzy ▪ Upset / tearfulness ▪ Rapid heart rate ▪ Irritable ▪ Breathless ▪ Avoiding situations ▪ Butterflies in the stomach ▪ Tension ▪ Poor concentration • Distress about normal tasks © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
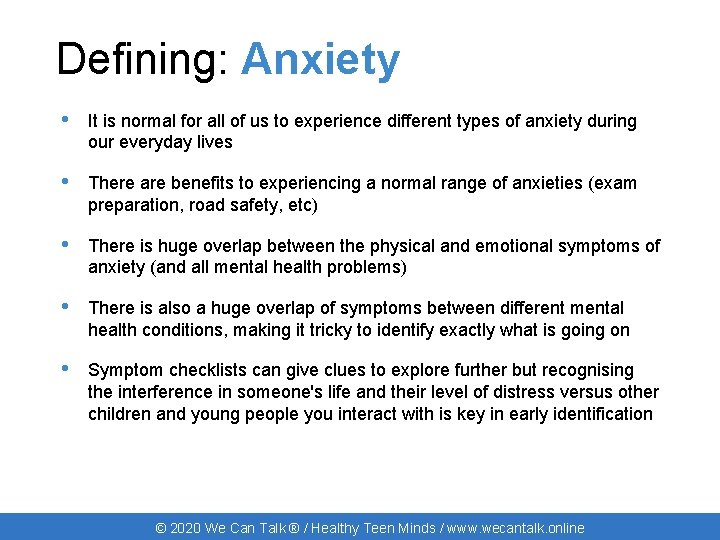
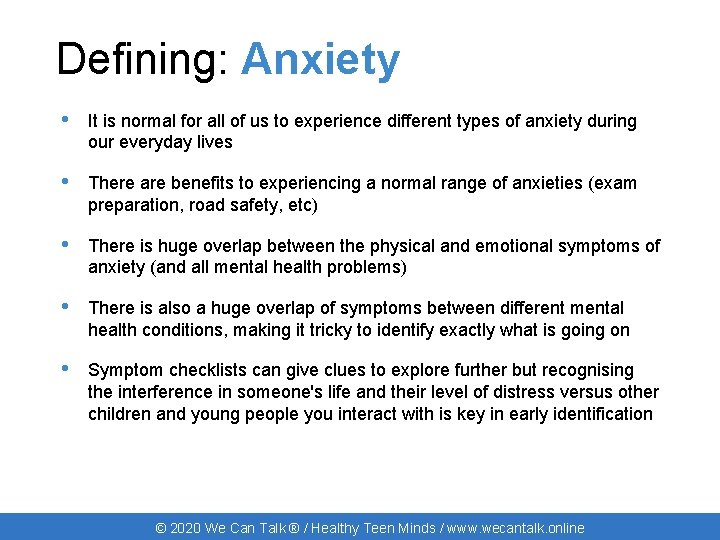
Defining: Anxiety • It is normal for all of us to experience different types of anxiety during our everyday lives • There are benefits to experiencing a normal range of anxieties (exam preparation, road safety, etc) • There is huge overlap between the physical and emotional symptoms of anxiety (and all mental health problems) • There is also a huge overlap of symptoms between different mental health conditions, making it tricky to identify exactly what is going on • Symptom checklists can give clues to explore further but recognising the interference in someone's life and their level of distress versus other children and young people you interact with is key in early identification © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Defining: Bipolar Disorder © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Defining: Bipolar Disorder Swings between extremes of depression and mania © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
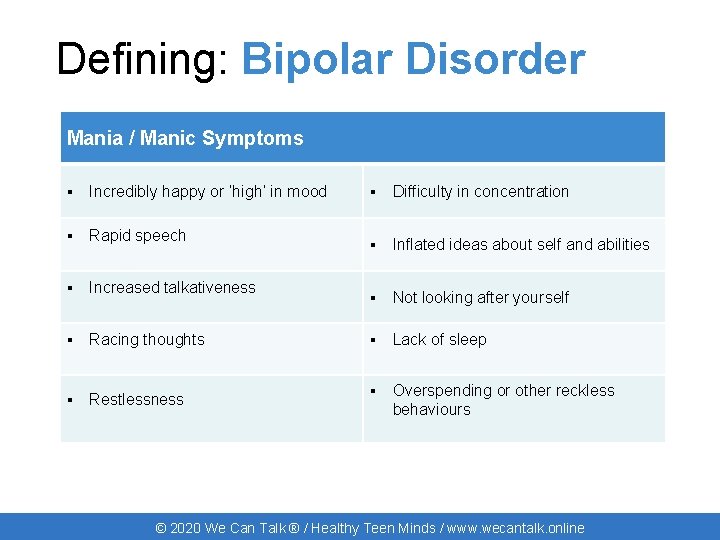
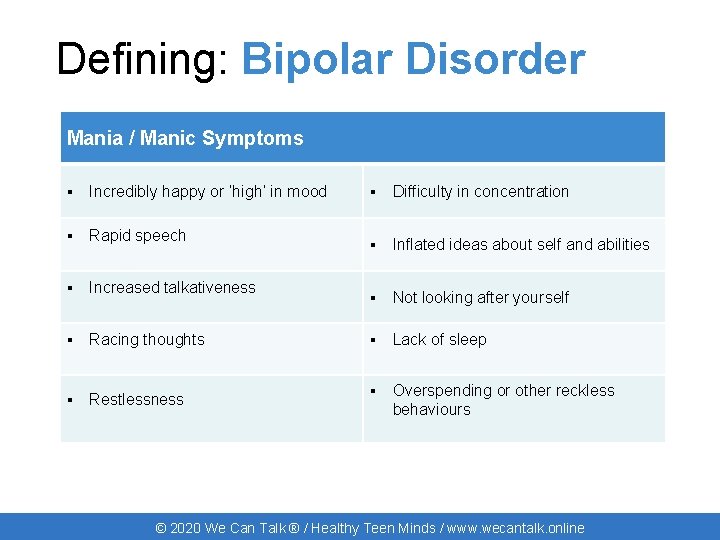
Defining: Bipolar Disorder Mania / Manic Symptoms ▪ Incredibly happy or ‘high’ in mood ▪ Rapid speech ▪ Increased talkativeness ▪ Racing thoughts ▪ Restlessness ▪ Difficulty in concentration ▪ Inflated ideas about self and abilities ▪ Not looking after yourself ▪ Lack of sleep ▪ Overspending or other reckless behaviours © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
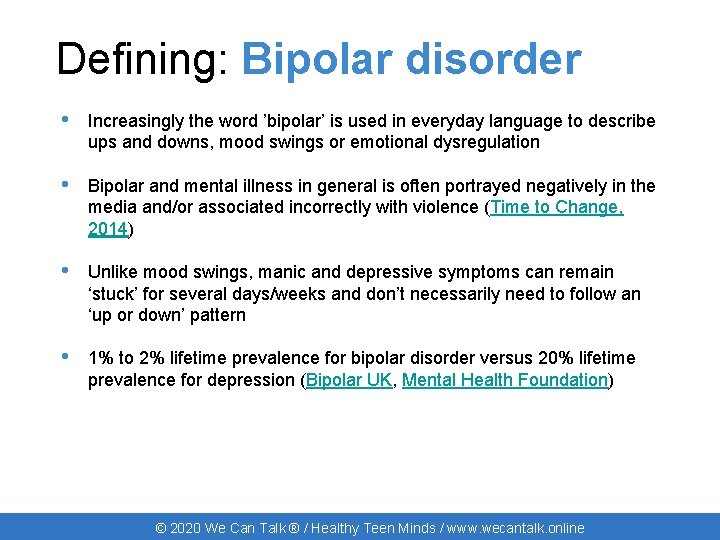
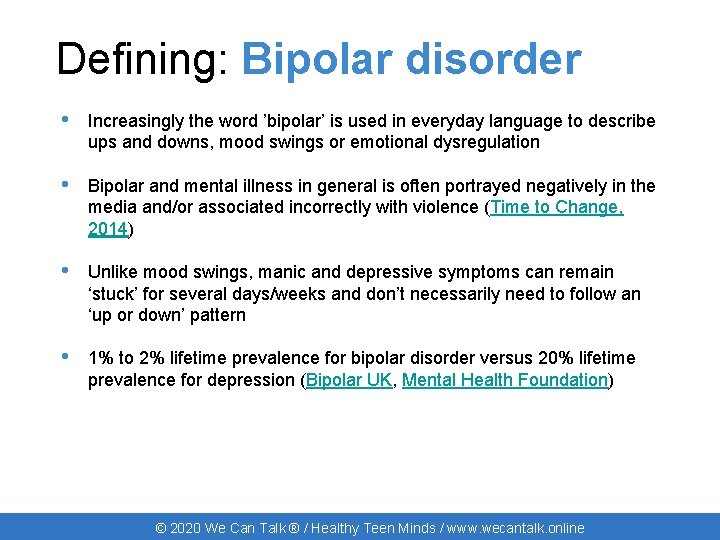
Defining: Bipolar disorder • Increasingly the word ’bipolar’ is used in everyday language to describe ups and downs, mood swings or emotional dysregulation • Bipolar and mental illness in general is often portrayed negatively in the media and/or associated incorrectly with violence (Time to Change, 2014) • Unlike mood swings, manic and depressive symptoms can remain ‘stuck’ for several days/weeks and don’t necessarily need to follow an ‘up or down’ pattern • 1% to 2% lifetime prevalence for bipolar disorder versus 20% lifetime prevalence for depression (Bipolar UK, Mental Health Foundation) © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Defining: Psychosis © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Defining: Psychosis An altered state of how we think, feel, see and act © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
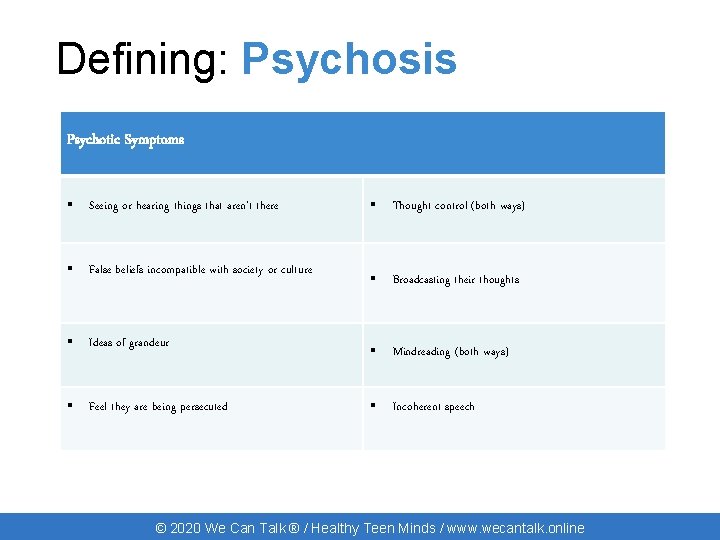
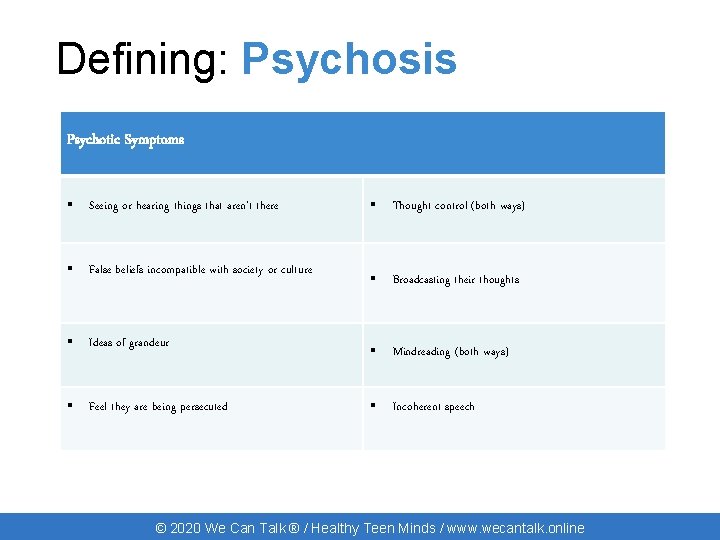
Defining: Psychosis Psychotic Symptoms ▪ Seeing or hearing things that aren’t there ▪ Thought control (both ways) ▪ False beliefs incompatible with society or culture ▪ Broadcasting their thoughts ▪ Ideas of grandeur ▪ Mindreading (both ways) ▪ Feel they are being persecuted ▪ Incoherent speech © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
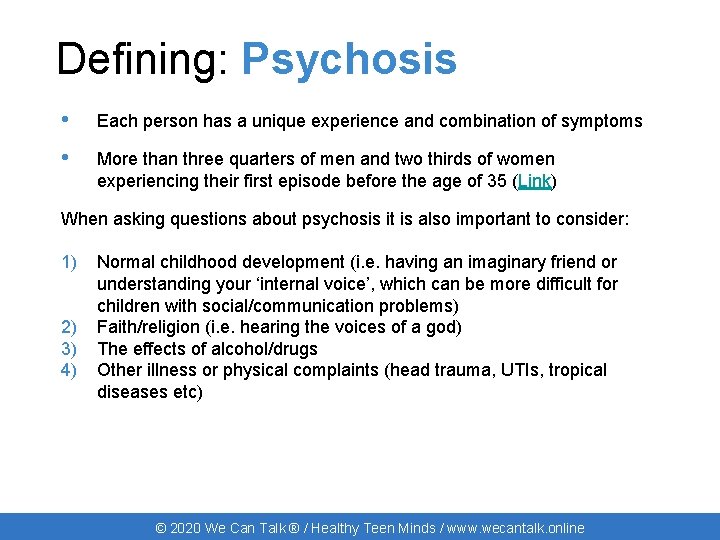
Defining: Psychosis • Each person has a unique experience and combination of symptoms • More than three quarters of men and two thirds of women experiencing their first episode before the age of 35 (Link) When asking questions about psychosis it is also important to consider: 1) 2) 3) 4) Normal childhood development (i. e. having an imaginary friend or understanding your ‘internal voice’, which can be more difficult for children with social/communication problems) Faith/religion (i. e. hearing the voices of a god) The effects of alcohol/drugs Other illness or physical complaints (head trauma, UTIs, tropical diseases etc) © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Supporting: Psychosis When we speak to young people who have experienced psychosis they tell us it’s most help for staff to: • Acknowledge the experience, connect with emotions • Don’t pretend you’re experiencing their reality • Validate their distress without colluding or backing up their abnormal experiences • Don’t assume they won’t be able to make any decisions about their care • Young people say they remember people who made them feel safe or who were nice, even when they can’t remember what the person said or did. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Defining: Medically unexplained symptoms © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Defining: Medically unexplained symptoms Physical symptoms we don’t understand © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
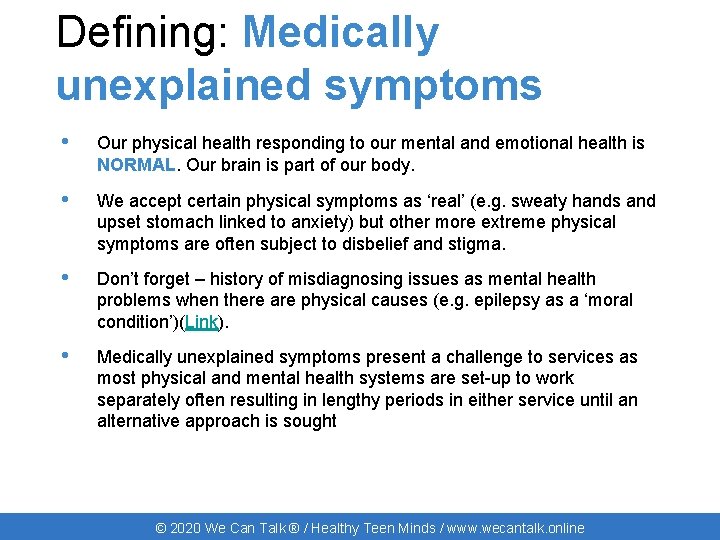
Defining: Medically unexplained symptoms • Our physical health responding to our mental and emotional health is NORMAL. Our brain is part of our body. • We accept certain physical symptoms as ‘real’ (e. g. sweaty hands and upset stomach linked to anxiety) but other more extreme physical symptoms are often subject to disbelief and stigma. • Don’t forget – history of misdiagnosing issues as mental health problems when there are physical causes (e. g. epilepsy as a ‘moral condition’)(Link). • Medically unexplained symptoms present a challenge to services as most physical and mental health systems are set-up to work separately often resulting in lengthy periods in either service until an alternative approach is sought © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
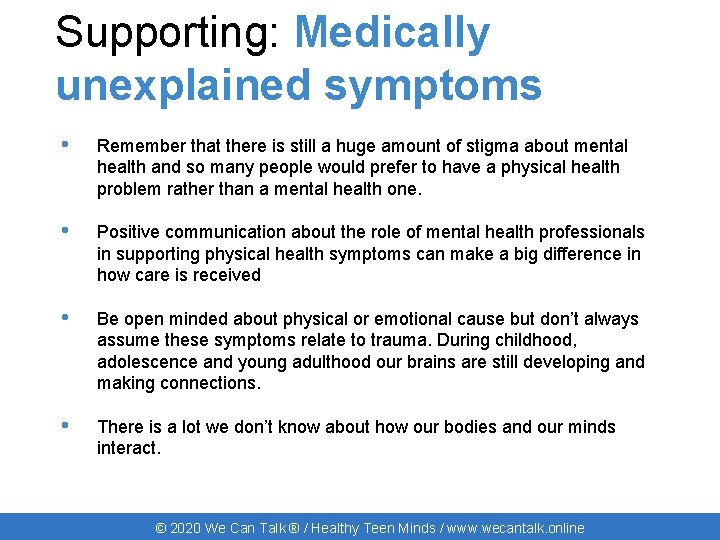
Supporting: Medically unexplained symptoms • Remember that there is still a huge amount of stigma about mental health and so many people would prefer to have a physical health problem rather than a mental health one. • Positive communication about the role of mental health professionals in supporting physical health symptoms can make a big difference in how care is received • Be open minded about physical or emotional cause but don’t always assume these symptoms relate to trauma. During childhood, adolescence and young adulthood our brains are still developing and making connections. • There is a lot we don’t know about how our bodies and our minds interact. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Defining: Eating Disorders © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
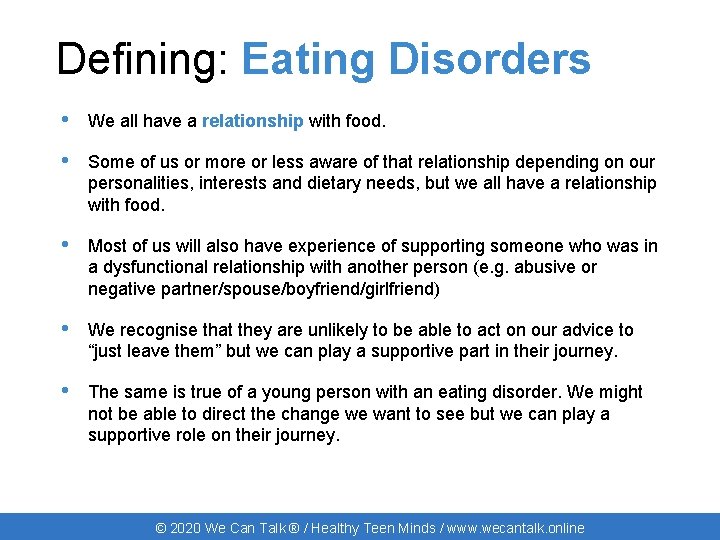
Defining: Eating Disorders • We all have a relationship with food. • Some of us or more or less aware of that relationship depending on our personalities, interests and dietary needs, but we all have a relationship with food. • Most of us will also have experience of supporting someone who was in a dysfunctional relationship with another person (e. g. abusive or negative partner/spouse/boyfriend/girlfriend) • We recognise that they are unlikely to be able to act on our advice to “just leave them” but we can play a supportive part in their journey. • The same is true of a young person with an eating disorder. We might not be able to direct the change we want to see but we can play a supportive role on their journey. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Defining: Eating Disorders Dysfunctional relationship with food © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
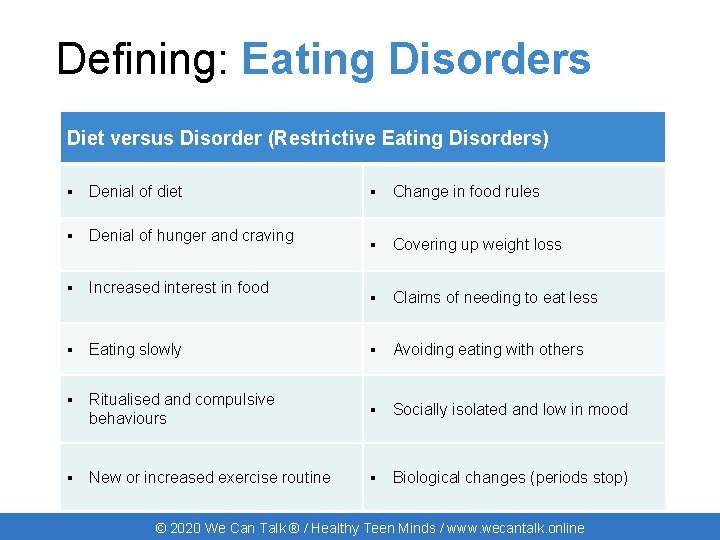
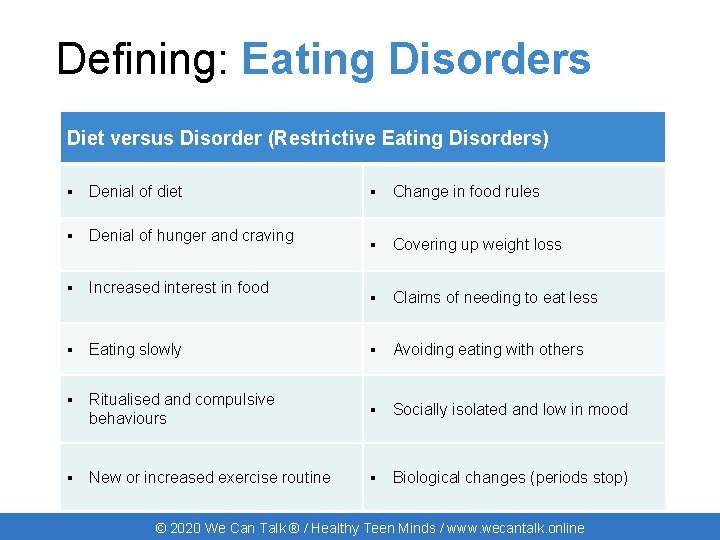
Defining: Eating Disorders Diet versus Disorder (Restrictive Eating Disorders) ▪ Denial of diet ▪ Change in food rules ▪ Denial of hunger and craving ▪ Covering up weight loss ▪ Increased interest in food ▪ Claims of needing to eat less ▪ Eating slowly ▪ Avoiding eating with others ▪ Ritualised and compulsive behaviours ▪ Socially isolated and low in mood ▪ New or increased exercise routine ▪ Biological changes (periods stop) © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
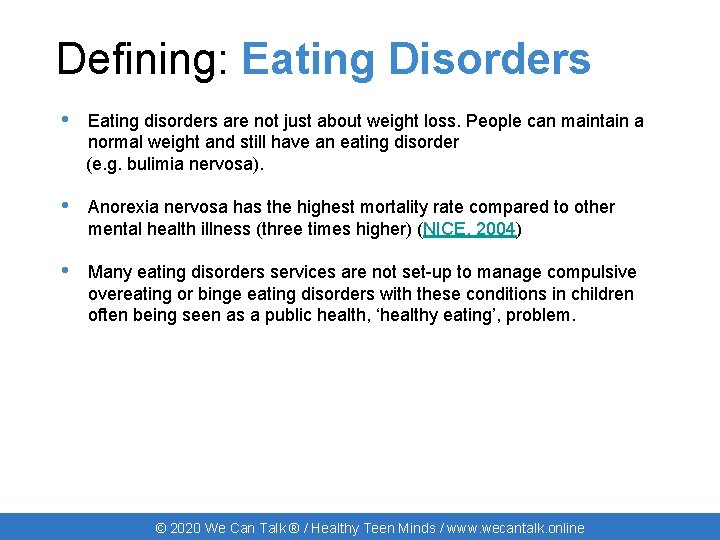
Defining: Eating Disorders • Eating disorders are not just about weight loss. People can maintain a normal weight and still have an eating disorder (e. g. bulimia nervosa). • Anorexia nervosa has the highest mortality rate compared to other mental health illness (three times higher) (NICE, 2004) • Many eating disorders services are not set-up to manage compulsive overeating or binge eating disorders with these conditions in children often being seen as a public health, ‘healthy eating’, problem. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Mental illness • Mental illness is not a tick box exercise (although often mental health services are fixated on tick boxes!) • Mental heath is still a young field, with few answers about what works / doesn’t work or what causes people to become unwell • Supporting the individual and responding to how they are feeling and acting is essential to providing high quality care. • There is a myth about violence and mental health. People with mental health problems are FIVE times more likely to be a victim of assault (rising to TEN times more likely for women with mental health problems) (Mind, 2013). • We hear from talking to hospital staff, however, that they remember these incidents more because they felt out of their depth in managing the situation (e. g. versus the child who kicks out when having a canular). © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Mental illness All people with the same diagnosis will appear, act, feel and respond differently to you. It might be helpful to consider the following when there is a question of the presence of mental illness: • • • Impact on every day functioning Rapid deterioration (in any area) Disengagement Significant change in behaviour Risk to self/others Bizarre behaviours/beliefs/statements © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding behaviour and communication © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
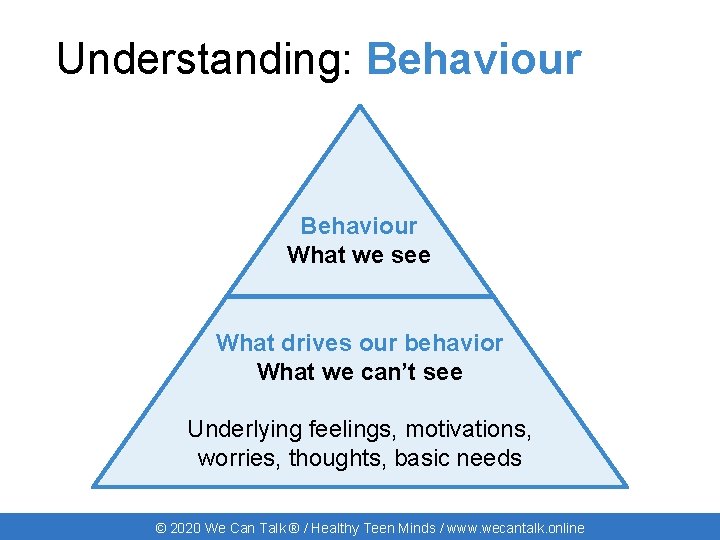
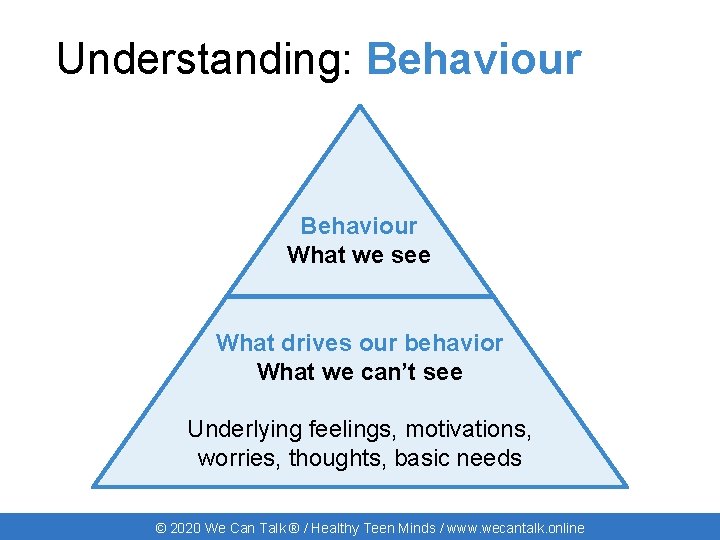
Understanding: Behaviour What we see What drives our behavior What we can’t see Underlying feelings, motivations, worries, thoughts, basic needs © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Behaviour Choose one behaviour you find difficult when supporting young people with mental health difficulties in your clinical practice Think about the young person: • What do you see or notice? How does the young person act? What do they do? • Try to imagine how the young person might be feeling - what might some of their underlying feelings and worries be? • What are their core needs in this situation? © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Behaviour Choose one behaviour you find difficult when supporting young people with mental health difficulties in your clinical practice Now think about what this is like for you: • What are some of your underlying feelings and worries? • How might you be acting? What might the young person see or notice? • What are your needs in this situation? © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Behaviour • Regardless of which mental health difficulty a young person is experiencing, they have core needs like all patients; their behaviour is not just a product of their mental health issue • Behaviour is a form of communication – we need to try and understand what they are trying to express • Young people are individuals – 10 young people with the same mental health difficulty will all have different underlying feelings, worries, wants. This is why it is important to understand respond to underlying feelings, core needs, rather than the visible behaviours (or assumptions about behaviour) • All children and young people have the same core needs - which is exactly what healthcare workers are skilled and experienced at supporting. You don’t have to be an expert in mental health to help. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
PHEW © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
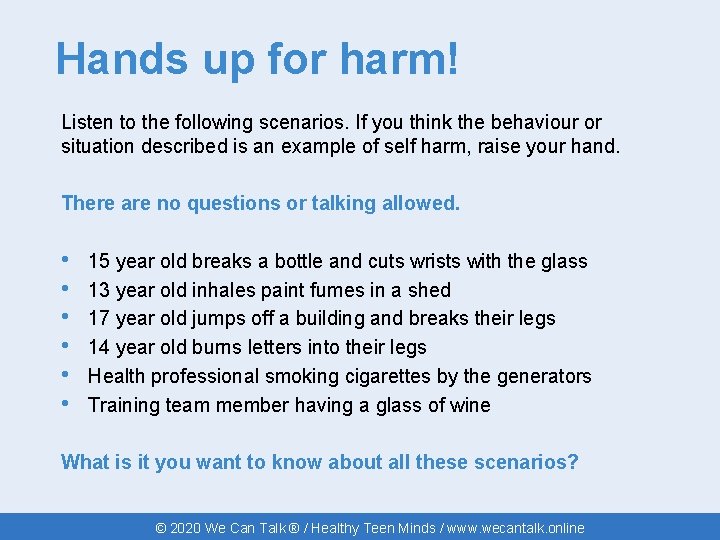
Hands up for harm! Listen to the following scenarios. If you think the behaviour or situation described is an example of self harm, raise your hand. There are no questions or talking allowed. • • • 15 year old breaks a bottle and cuts wrists with the glass 13 year old inhales paint fumes in a shed 17 year old jumps off a building and breaks their legs 14 year old burns letters into their legs Health professional smoking cigarettes by the generators Training team member having a glass of wine What is it you want to know about all these scenarios? © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Self Harm Are these the only types of self harm? • Cutting • Burning / scalding • Head banging • Breaking bones • Punching body • Inserting/swallowing objects/poisons • Throwing self against something © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Self Harm What about? • Smoking • Tattooing • Risk Taking Behaviours • Body Piercing • Eating Disorders • Alcohol use • Drug Use © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Defining: Self Harm • We all do things that are harmful in some way. There is a difference between ”things that are harmful” and self harm. • Intention is more important than the act or “amount”/severity of visible harm. Seek to clarify self harm versus suicidal act. • The children and young people most at risk to themselves may be those who describe their mood in the least risky way. • Challenge the use of the word “deliberate” or dismissive terms like “superficial” or “attention seeking”. • Young people may self harm as a way to “seek attention” or to “seek care” or “seek support” from professionals / parents / carers because they aren’t able to access it via any other route. • There all sorts of reasons why young people self harm (e. g. to feel something, to cope with difficult feelings, for a sense of control). © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Experience © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Experience Why do children and young people come to hospital in mental health crisis? • Hospital isn’t the first choice for young people experiencing mental health difficulties. • They need professional care to stay safe, just like those attending with physical needs. • When forced to seek medical care, they do so with feelings of shame and unworthiness. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Experience Hearing children and young people’s voices “I will not go up there anymore, mainly because I feel like such a time waster, and I hate all the questions they ask you … I just want to get back home, hide under the duvet and die of shame … I've ended up with numerous infections however from not getting wounds treated. ” “I can understand their frustration at having to stitch someone up knowing that there is a possibility of them returning the next day with a new injury or after re-opening the stitches … They are only human and have bad days just like anyone else. ” © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Experience Positive and negative experience of mental health support in acute hospitals Staff attitudes/behaviours have more impact on young people’s experience and are more important than a lack of knowledge around mental health. Negative experiences mean young people are less able to cope when they leave hospital and encourages young people to abscond when attending due to their mental health. CAMHS don’t always get this right either, and the same goes for nonhealthcare organisations such as schools struggling to support young people in mental health difficulty. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Experience Hearing children and young people’s voices “The last time I had a blood transfusion the consultant said that I wasting blood that was meant for patients after they'd had operations or accident victims. He asked whether I was proud of what I'd done…” “…they have concentrated on medically patching me up and getting me out. Never have I been asked any questions regarding whether this is the first time I have self-harmed or if I was to do it again or how I intend to deal with it. ” © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Experience Positive and negative experience of mental health support in acute hospitals Children and young people have a better experience if involved in decision making and if staff explain the reasons for/the goals of assessment They like being given a chance to talk about their problems Children and young people who self harm say that it is a better experience when they can talk through what led up to the event. The most positive encounters are where young people receive ‘treatment as usual’: non-discriminatory care, delivered with kindness and empathy, not just focusing on the physical aspects (if applicable). © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Experience Hearing children and young people’s voices “I allowed a student nurse to observe and she was really kind asked me why I self-harm because she said she didn't really understand it, and it was really nice … to be able to actually help someone learn about it. ” “He. . . took great pains to suture very neatly – when I commented on this he said “I don't want it to leave any scars” to which I replied that I am covered in them. He said “not on my watch”. ” “The nurse consultant who assessed me was very easy to talk to. She explained everything clearly in a non-threatening way. It felt like a friendly chat. She was great!” © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Experience Summary Whilst there may be many perceived challenges to supporting children and young people with mental health difficulties, it is the small things that make the biggest difference: • • • Care Compassion Empathy Validation Reassurance Time to talk All things that healthcare workers are highly skilled and experienced in doing. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: Experience Summary g n u o y d n e a n n o e e r • Care d m l i o h s • Compassion c t o r n s e a d w • Empathy mb e t ! t ’ e s p n i s r m o • Validation e c e d n s R d e l r d • Reassurance op a n a w e t k c w • Timep to talk e a f r y e n p a All things that healthcare workers aree highly skilled and experienced in doing. c a r b m e Whilst there may be many perceived challenges to supporting children and young people with mental health difficulties, it is the small things that make the biggest difference: © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online

Communication © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online

Support: Communication Having a go! © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
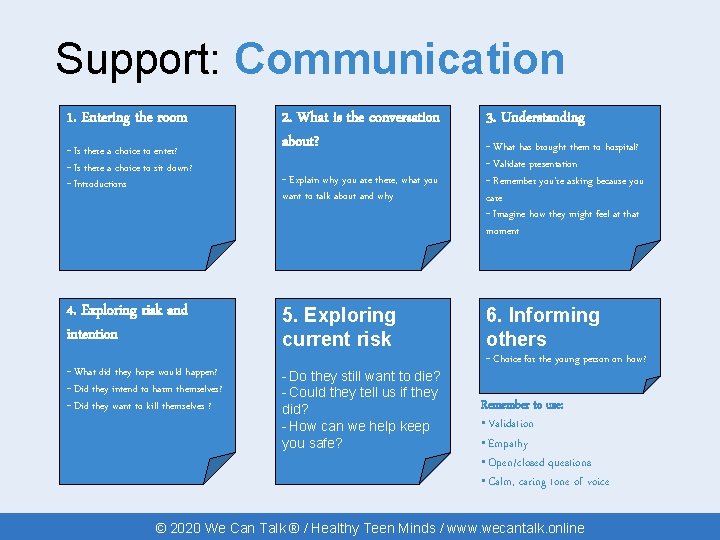
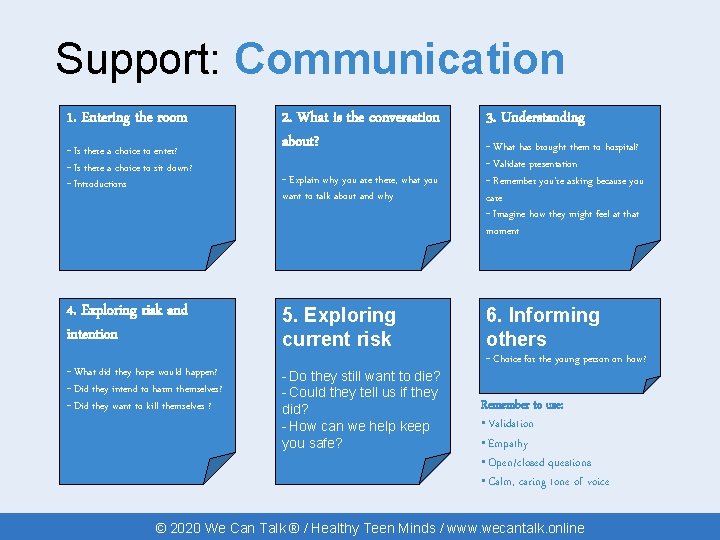
Support: Communication 1. Entering the room 2. What is the conversation about? 3. Understanding - Explain why you are there, what you want to talk about and why - What has brought them to hospital? - Validate presentation - Remember you’re asking because you care - Imagine how they might feel at that moment 4. Exploring risk and intention 5. Exploring current risk 6. Informing others - What did they hope would happen? - Did they intend to harm themselves? - Did they want to kill themselves ? - Do they still want to die? - Could they tell us if they did? - How can we help keep you safe? - Is there a choice to enter? - Is there a choice to sit down? - Introductions - Choice for the young person on how? Remember to use: • Validation • Empathy • Open/closed questions • Calm, caring tone of voice © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
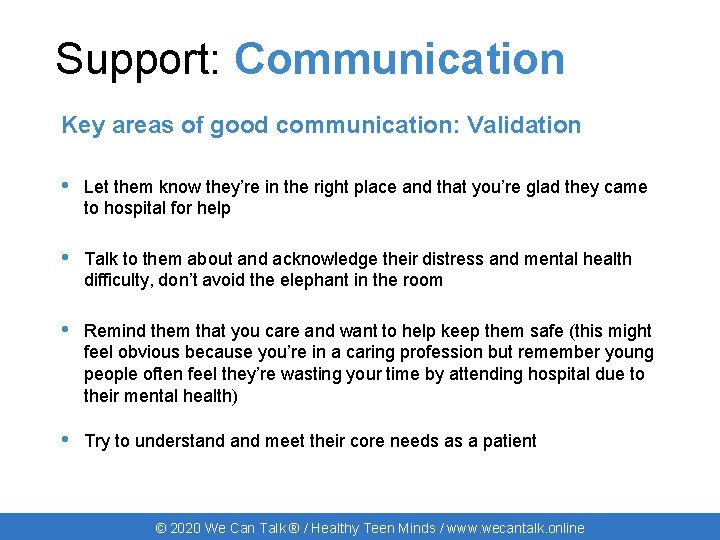
Support: Communication Key areas of good communication: Validation • Let them know they’re in the right place and that you’re glad they came to hospital for help • Talk to them about and acknowledge their distress and mental health difficulty, don’t avoid the elephant in the room • Remind them that you care and want to help keep them safe (this might feel obvious because you’re in a caring profession but remember young people often feel they’re wasting your time by attending hospital due to their mental health) • Try to understand meet their core needs as a patient © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
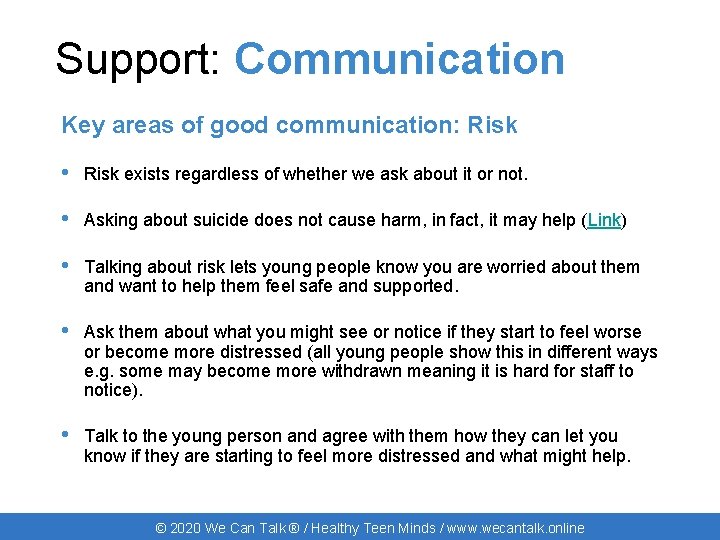
Support: Communication Key areas of good communication: Risk • Risk exists regardless of whether we ask about it or not. • Asking about suicide does not cause harm, in fact, it may help (Link) • Talking about risk lets young people know you are worried about them and want to help them feel safe and supported. • Ask them about what you might see or notice if they start to feel worse or become more distressed (all young people show this in different ways e. g. some may become more withdrawn meaning it is hard for staff to notice). • Talk to the young person and agree with them how they can let you know if they are starting to feel more distressed and what might help. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
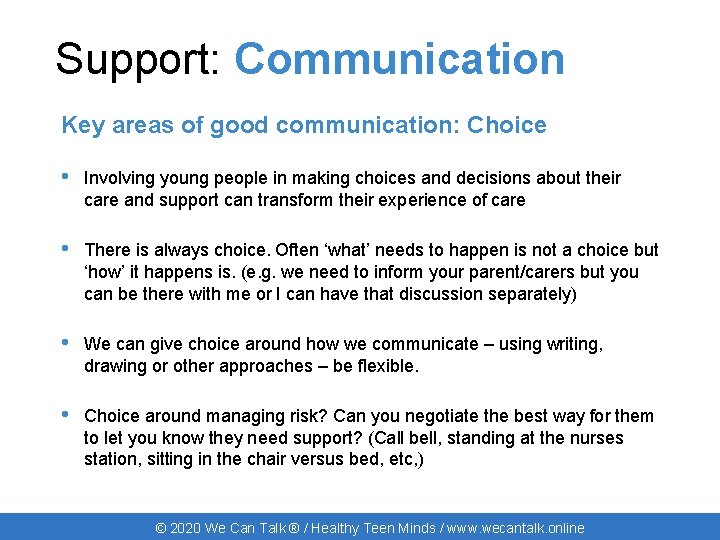
Support: Communication Key areas of good communication: Choice • Involving young people in making choices and decisions about their care and support can transform their experience of care • There is always choice. Often ‘what’ needs to happen is not a choice but ‘how’ it happens is. (e. g. we need to inform your parent/carers but you can be there with me or I can have that discussion separately) • We can give choice around how we communicate – using writing, drawing or other approaches – be flexible. • Choice around managing risk? Can you negotiate the best way for them to let you know they need support? (Call bell, standing at the nurses station, sitting in the chair versus bed, etc, ) © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Support: Communication Summary of key messages and further resources • Communication is highly valued by young people. Conversations make them feel heard, seen and valued. This alone can dramatically change their experience. • Saying something is better than saying nothing • Intention is more important than getting it perfect • Approaching these conversations with the right attitude is more important to children and young people than the right expertise. • The wecantalk. online website has a download of ’Top Tips’ on how to communicate with young people about their mental health and Mefirst. org. uk has a host of resources to support communication with CYP in healthcare © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online

© 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Support © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Support: Practical CATASTROPHE © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Support: Practical Distraction and relaxation • Paper and pens are valuable tools! • Listen to music • Board games, cards • Breathing exercises (You. Tube!) • Progressive muscle relaxation • Mindfulness (Mindful Eating) • Consider strategies specific to your clinical team or environment © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Support: Mental Health Risk and Protective Factors © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Support: Mental Health Risk factors Too many to list but some specific factors you may encounter • Learning disabilities • Physical illness • Poverty • Low self-esteem • Chronic health problems What others do you encounter? © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Support: Mental Health Protective factors • Supportive relationships • Pathways to raise problems • Good communication and problem solving skills • Faith or spirituality • Ability to reflect • Sense of community • Good housing • Opportunities for valued social roles • Strong self identity © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Support: Mental Health Protective factors Relationships are the most important factor in young people’s experience in hospital. As with all patients, their time and contact with you can make a significant impact. It’s the small things that make the biggest difference to someone’s experience. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Support: Mental Health Promoting protective factors Draw two large faces on your giant paper (one happy and one sad) What potential risk factors might young people experience during their stay with us? What could we do in our clinical environments to promote positive mental well-being? Try and be as specific as you can about things you could do in your clinical environments (realistically!). © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: CAMHS Child and Adolescent Mental Health Services (CAMHS) Work with children and young people from 0 -18* *some areas up to 25 Work with families, parents, carers & other professionals © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
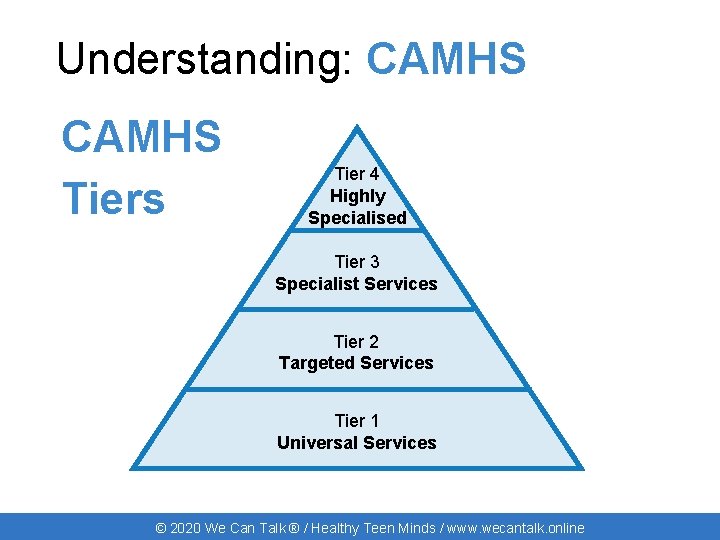
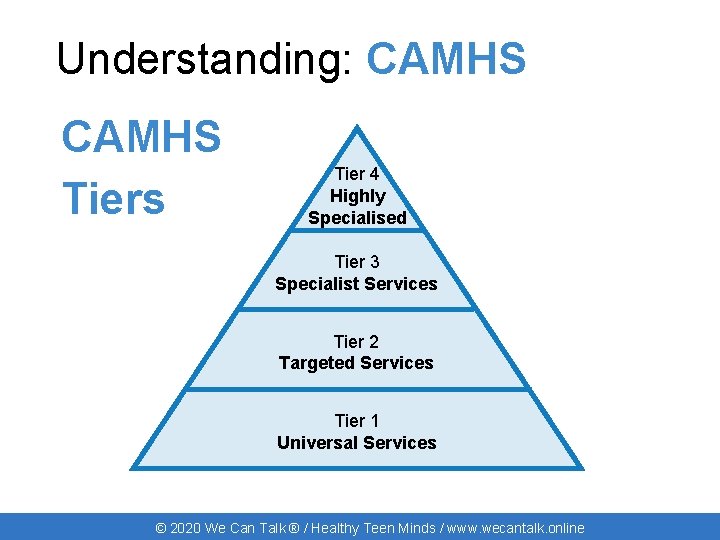
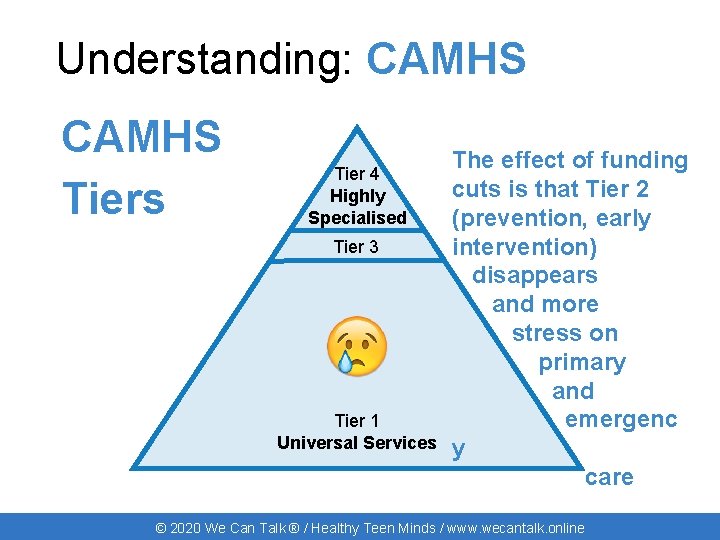
Understanding: CAMHS Tiers Tier 4 Highly Specialised Tier 3 Specialist Services Tier 2 Targeted Services Tier 1 Universal Services © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
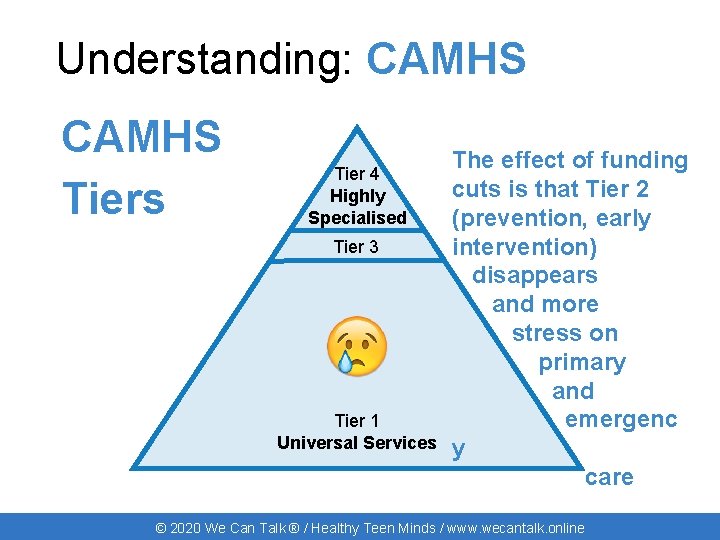
Understanding: CAMHS Tiers Tier 4 Highly Specialised Tier 3 Tier 1 Universal Services The effect of funding cuts is that Tier 2 (prevention, early intervention) disappears and more stress on primary and emergenc y care © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: CAMHS Referral Routes • Self-Referral • GP • School • Social Care Team • A&E / Urgent Care / Paediatric or Adult Wards © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: CAMHS Referrals include: • What is the problem? • Why is the referral happening now? • What does the child/carer want? • What do you think they/you need? • What is making the problem worse? • What is helping manage the problem? • What risks are involved to the young person/carer? © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: CAMHS (Better) Referrals include: • Current situation (location / on-going physical treatment? ) • Relevant historical factors • Timescales • Risks • Professional details of those involved © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Understanding: CAMHS Who are CAMHS? • Child Psychiatrists • Mental Health Nurses • Family Therapists • Child Psychotherapists • Psychologists • Maybe… Art/Drama/Other Therapists/Counsellors/OTs, Physio, ? ? • Different professional backgrounds • Different clinical approaches • One size does not fit all © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Final thoughts What one thing will you take away from today? © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online

Support: Online www. Mind. Ed. org. uk www. youngminds. org. uk www. mefirst. org. uk www. rcpsych. ac. uk www. wecantalk. online © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Support: Online Follow us online (not all the way home) Facebook. com/We. Can. Talk. CYPMH Twitter @We. Can. Talk. CYPMH #We. Can. Talk © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online

Goodbye Before you leave, please complete the anonymous posttraining questionnaire at www. wecantalk. online/post Open a web browser and type the full address or click ‘Training’ on the We Can Talk website and scroll down to the link near the bottom. Please click done and show us the screen with an elephant on a gold star and we’ll give your certificate! © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Children and Young People’s Mental Health Training © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Principles The We Can Talk Principles are a young people and staff accessible version of the educational framework that the training is based on. They outline the key areas that all staff should feel confident and capable in addressing with children and young people after attending the training 1) We Can Talk and listen about your emotional and mental health needs in a clear and non-judgmental way 2) We Can Talk about how we will look after your physical and emotional needs while in hospital 3) We Can Talk about how to help manage the challenges of being in hospital by using distraction and relaxation techniques 4) We Can Talk about your problems and we can try to find the right person to help © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Principles 5) We Can Talk about how to keep you safe while you are staying with us in hospital 6) We Can Talk or we can communicate in another way that might work better for you, by writing, drawing, using signs and pictures etc. We’re flexible. 7) We Can Talk about self harm and other big issues that might be worrying you 8) We Can Talk in private and will always talk with you about information that needs to be shared. 9) We Can Talk about difficult or awkward subjects in a way that is not as difficult or awkward as either of us thought it would be 10) We Can Talk to you and your parents / carers about helpful places to access additional support or information around your mental health © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
References Recommendations for A&E nurses from “A clash of cultures: A&E and mental health” J. J. Crowley, Accident and Emergency Nursing (2000) 8, 2– 8. Attitudes towards clinical services among people who self-harm: systematic review” T. L. Taylor, K. Hawton, S. Fortune, N. Kapur, The British Journal of Psychiatry (2009), 194 (2) 104 -110. Needs and fears of young people presenting at Accident and Emergency department following an act of self-harm: Secondary analysis of qualitative data C. Owens, L. Hansford, S. Sharkey, T. Ford, The British Journal of Psychiatry (2016), 208 (3): 286– 291. Guidelines for self-harm National Institute for Clinical Excellence (2015) Further quotes from the young volunteers of “The Mentality Project”, Off The Record (Bristol). Thanks to Newham CAMHS Participation Group for their ideas and suggestions. © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
Project Team For more information about We Can Talk please visit www. wecantalk. online, speak to your local Project Lead or e-mail the team at info@wecantalk. online. Robin Barker National Director robin@healthyteenminds. com Karen Whitelaw Director of Engagement karen@healthyteenminds. com Martha Reilly Project Coordinator Martha. Reilly@annafreud. org © 2020 We Can Talk ® / Healthy Teen Minds / www. wecantalk. online
 Mental health and mental illness chapter 20
Mental health and mental illness chapter 20 Children's mental health
Children's mental health Green paper children's mental health
Green paper children's mental health Mental health jeopardy game
Mental health jeopardy game Golden thread clinical documentation
Golden thread clinical documentation We can talk mental health training
We can talk mental health training Peer respite centers
Peer respite centers Unit 10 caring for children and young people
Unit 10 caring for children and young people Working with young children chapter 1
Working with young children chapter 1 Tscyc screening form
Tscyc screening form Phonemic awareness in young children
Phonemic awareness in young children Hampshire early years moodle
Hampshire early years moodle Alcohol consumption causes blood vessels to contract
Alcohol consumption causes blood vessels to contract Working together to safeguard children’ 2018 summary
Working together to safeguard children’ 2018 summary Lesson 1 the peoples of north america and mesoamerica
Lesson 1 the peoples of north america and mesoamerica Many territories and peoples controlled by one government
Many territories and peoples controlled by one government The peoples of north america and mesoamerica
The peoples of north america and mesoamerica Chapter 3 lesson 3 expressing emotions in healthful ways
Chapter 3 lesson 3 expressing emotions in healthful ways Mental health and older adults
Mental health and older adults Lemhwa report to congress
Lemhwa report to congress Mental health and older adults
Mental health and older adults Mental health and citizenship
Mental health and citizenship Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Chapter 3 achieving mental and emotional health answer key
Chapter 3 achieving mental and emotional health answer key Psychology, mental health and distress
Psychology, mental health and distress Mental health policy, plans and programmes michelle funk
Mental health policy, plans and programmes michelle funk Glencoe health chapter 5 review answers
Glencoe health chapter 5 review answers Chapter 5 lesson 2 mental disorders
Chapter 5 lesson 2 mental disorders Achieving mental and emotional health
Achieving mental and emotional health Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 15 achieving mental and emotional health answer key
Chapter 15 achieving mental and emotional health answer key Achieving mental and emotional health
Achieving mental and emotional health Photoshop mind map
Photoshop mind map Whooley questions nice
Whooley questions nice Chapter 3 mental and emotional health
Chapter 3 mental and emotional health Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 15 achieving mental and emotional health
Chapter 15 achieving mental and emotional health Education and training act 2020 summary
Education and training act 2020 summary Arab social structure
Arab social structure Seven habits paradigm
Seven habits paradigm John calvin peoples
John calvin peoples Latin american people win independence
Latin american people win independence Let me see your hands clap
Let me see your hands clap Latin american peoples win independence
Latin american peoples win independence World council of indigenous peoples
World council of indigenous peoples Populism in america apush
Populism in america apush Chapter 11 pastoral peoples on the global stage
Chapter 11 pastoral peoples on the global stage Respect other people's time and bandwidth
Respect other people's time and bandwidth Peoples palace qmul
Peoples palace qmul Ten commandments of netiquette
Ten commandments of netiquette Farzana and jamil are from kustia
Farzana and jamil are from kustia Latin american peoples win independence
Latin american peoples win independence Peoples speke
Peoples speke Peoples business
Peoples business 8 habits stephen covey
8 habits stephen covey Aboriginal representation in film
Aboriginal representation in film Joel shaul
Joel shaul Chapter 11 pastoral peoples on the global stage
Chapter 11 pastoral peoples on the global stage John lennon imagine paroles
John lennon imagine paroles Peoples home equity inc
Peoples home equity inc Que países conforman la gran colombia
Que países conforman la gran colombia Nomadic peoples who herded domesticated animals
Nomadic peoples who herded domesticated animals Latin american peoples win independence
Latin american peoples win independence The narratives that vanquished peoples
The narratives that vanquished peoples Latin american peoples win independence
Latin american peoples win independence Child rights act 2005 images
Child rights act 2005 images National programmes related to nutrition
National programmes related to nutrition National children's digital health collaborative
National children's digital health collaborative Health and social care component 3
Health and social care component 3 Ccu frankston
Ccu frankston Lenawee county cmh
Lenawee county cmh Van buren community mental health
Van buren community mental health Together for mental health
Together for mental health 2007 mental health act
2007 mental health act 3 sides of the health triangle
3 sides of the health triangle Titles for mental health presentations
Titles for mental health presentations Mental health committee
Mental health committee Public mental health
Public mental health Psychiatric nursing meaning
Psychiatric nursing meaning Pes in nursing process
Pes in nursing process Mental health programme
Mental health programme Objectives of national mental health programme
Objectives of national mental health programme Benefits of phr
Benefits of phr 2016494500
2016494500 Mental health toolbox talk construction
Mental health toolbox talk construction Mental health equity
Mental health equity Mental health ordinance
Mental health ordinance Axis 1-5 mental health
Axis 1-5 mental health Learning outcomes definition
Learning outcomes definition Examples of mental health
Examples of mental health Objective for mental health awareness
Objective for mental health awareness Poem on mental health awareness day
Poem on mental health awareness day Health and wellness trivia
Health and wellness trivia Billy corgan mental health
Billy corgan mental health Mental health america of san diego county
Mental health america of san diego county Individual service plan
Individual service plan How sport affects health
How sport affects health Osar
Osar Influence of culture on mental health
Influence of culture on mental health Bexar county mental health services
Bexar county mental health services Thomas snyder mental health
Thomas snyder mental health Example of emotional health
Example of emotional health Mental health equity
Mental health equity