Chemical Pathology 1 Silvia Muttoni silvia muttoni 1nhs



- Slides: 53
Chemical Pathology 1 Silvia Muttoni silvia. muttoni 1@nhs. net
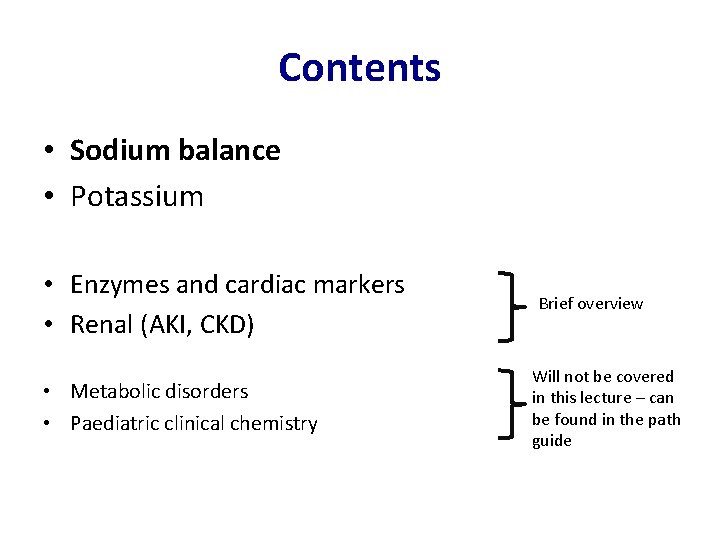
Contents • Sodium balance • Potassium • Enzymes and cardiac markers • Renal (AKI, CKD) • Metabolic disorders • Paediatric clinical chemistry Brief overview Will not be covered in this lecture – can be found in the path guide
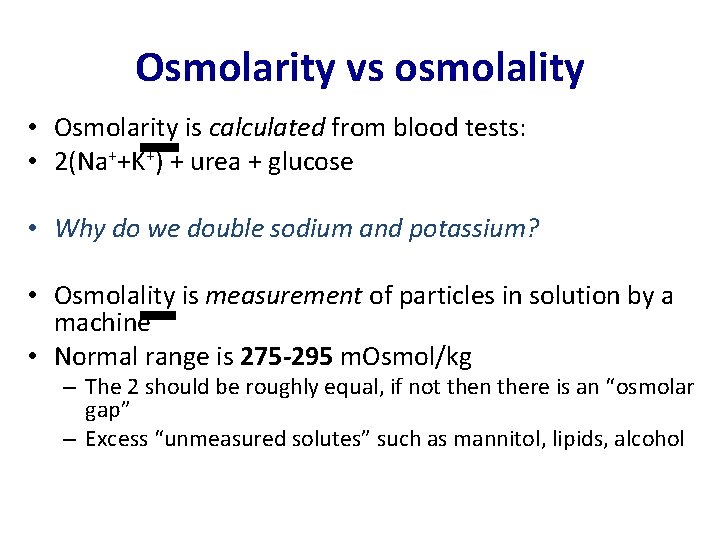
Osmolarity vs osmolality • Osmolarity is calculated from blood tests: • 2(Na++K+) + urea + glucose • Why do we double sodium and potassium? • Osmolality is measurement of particles in solution by a machine • Normal range is 275 -295 m. Osmol/kg – The 2 should be roughly equal, if not then there is an “osmolar gap” – Excess “unmeasured solutes” such as mannitol, lipids, alcohol
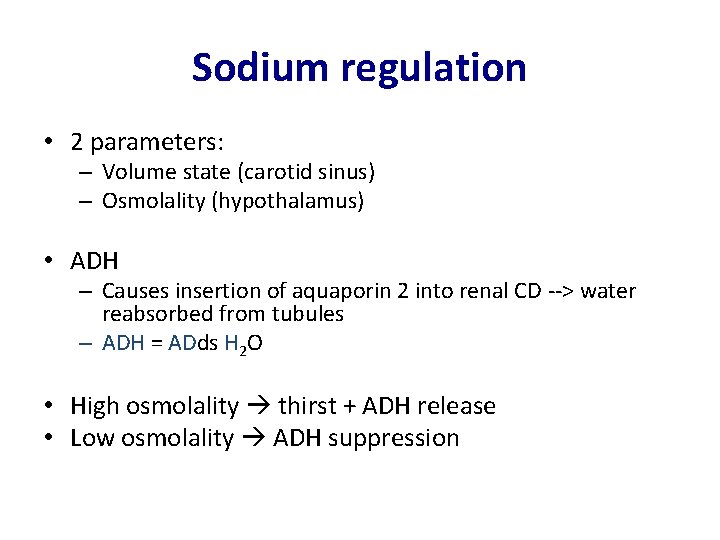
Sodium regulation • 2 parameters: – Volume state (carotid sinus) – Osmolality (hypothalamus) • ADH – Causes insertion of aquaporin 2 into renal CD --> water reabsorbed from tubules – ADH = ADds H 2 O • High osmolality thirst + ADH release • Low osmolality ADH suppression
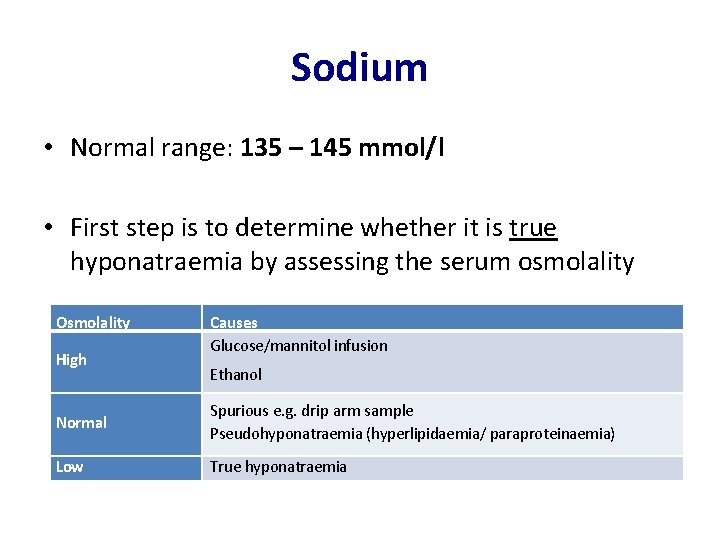
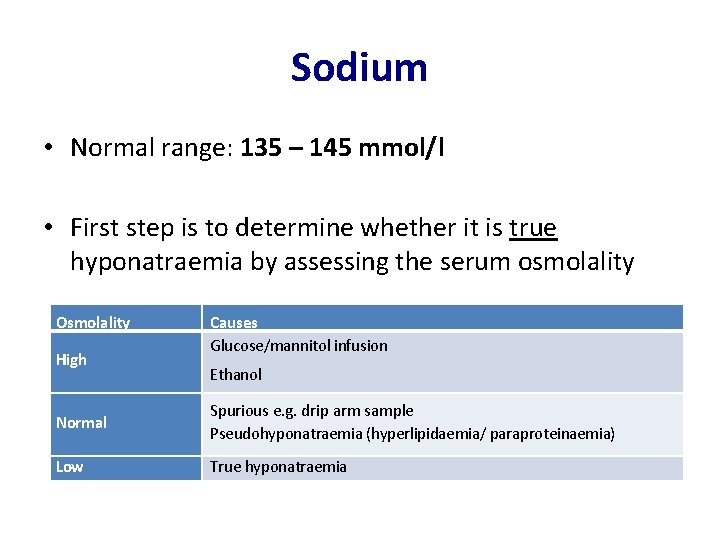
Sodium • Normal range: 135 – 145 mmol/l • First step is to determine whether it is true hyponatraemia by assessing the serum osmolality Osmolality High Causes Glucose/mannitol infusion Ethanol Normal Spurious e. g. drip arm sample Pseudohyponatraemia (hyperlipidaemia/ paraproteinaemia) Low True hyponatraemia

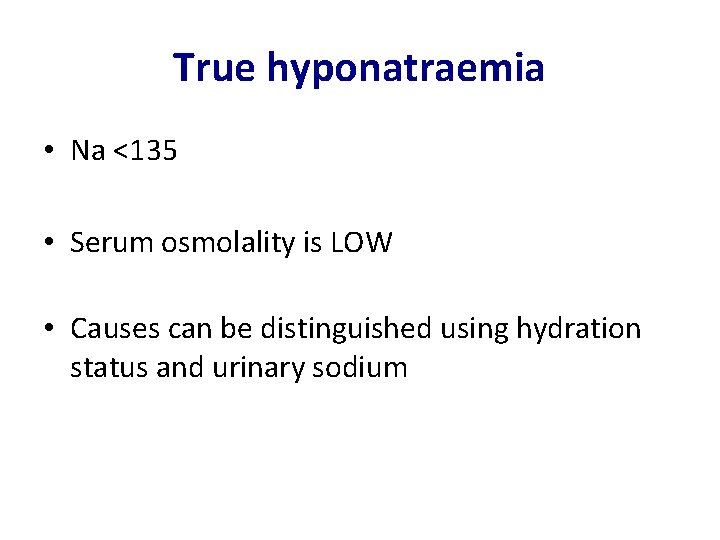
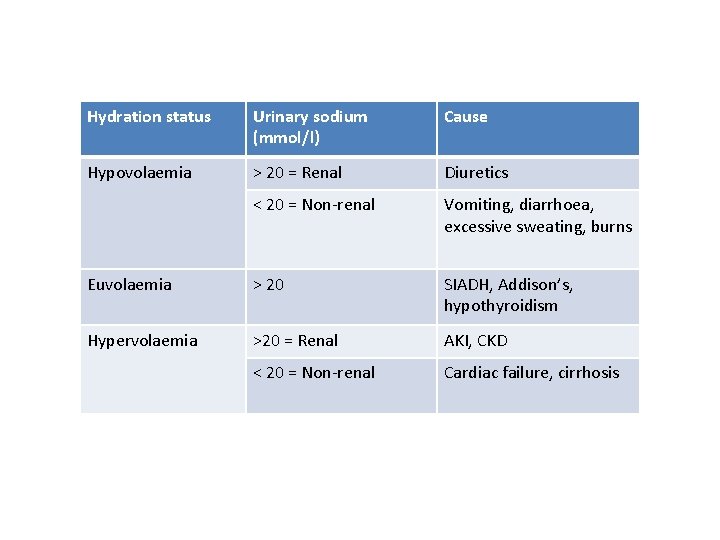
True hyponatraemia • Na <135 • Serum osmolality is LOW • Causes can be distinguished using hydration status and urinary sodium

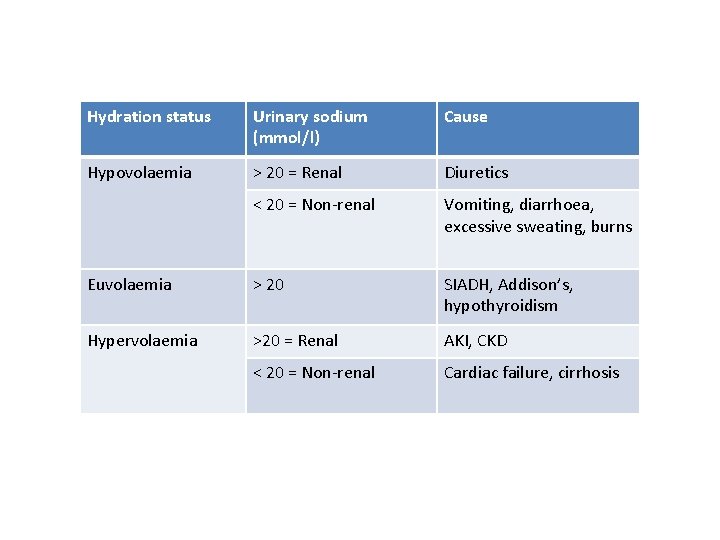
Hydration status Urinary sodium (mmol/l) Cause Hypovolaemia > 20 = Renal Diuretics < 20 = Non-renal Vomiting, diarrhoea, excessive sweating, burns Euvolaemia > 20 SIADH, Addison’s, hypothyroidism Hypervolaemia >20 = Renal AKI, CKD < 20 = Non-renal Cardiac failure, cirrhosis
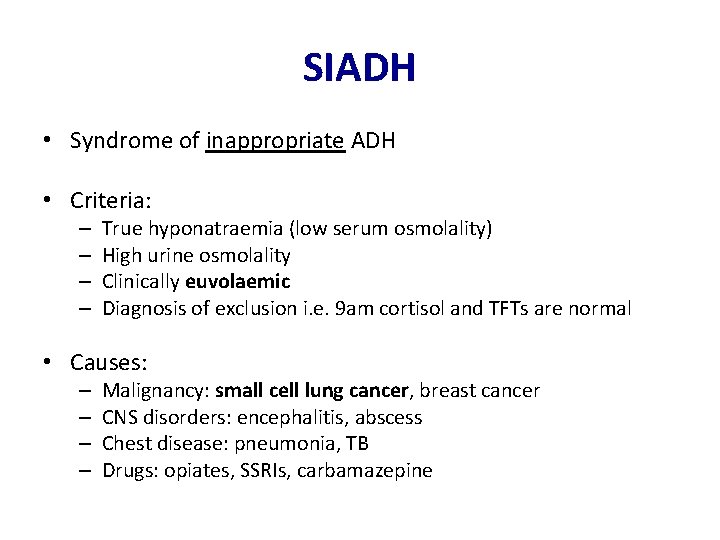
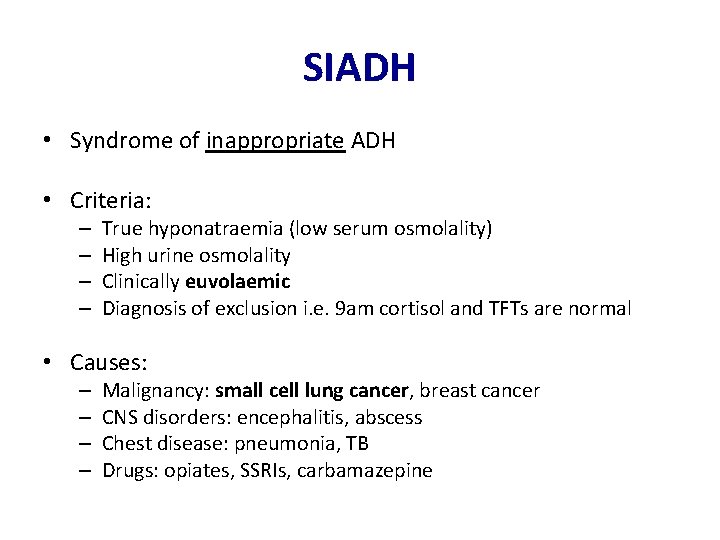
SIADH • Syndrome of inappropriate ADH • Criteria: – – True hyponatraemia (low serum osmolality) High urine osmolality Clinically euvolaemic Diagnosis of exclusion i. e. 9 am cortisol and TFTs are normal • Causes: – – Malignancy: small cell lung cancer, breast cancer CNS disorders: encephalitis, abscess Chest disease: pneumonia, TB Drugs: opiates, SSRIs, carbamazepine
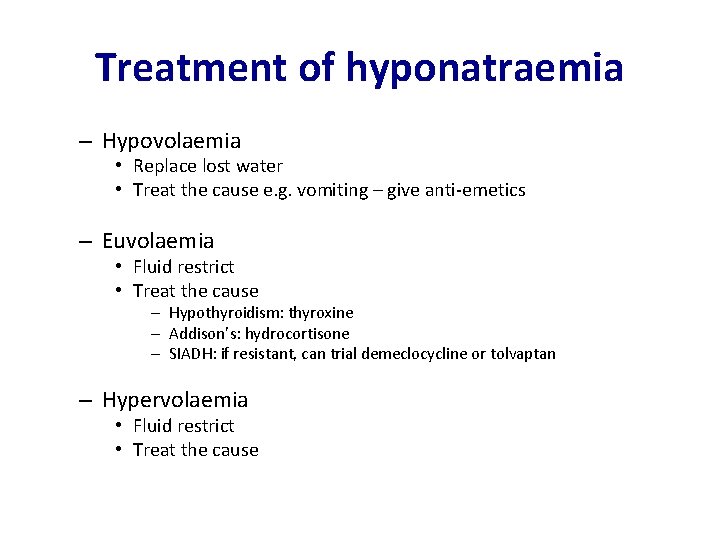
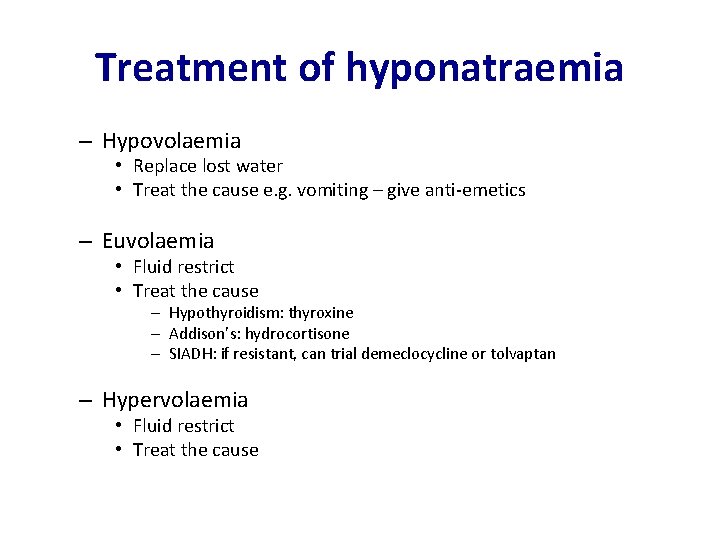
Treatment of hyponatraemia – Hypovolaemia • Replace lost water • Treat the cause e. g. vomiting – give anti-emetics – Euvolaemia • Fluid restrict • Treat the cause – Hypothyroidism: thyroxine – Addison’s: hydrocortisone – SIADH: if resistant, can trial demeclocycline or tolvaptan – Hypervolaemia • Fluid restrict • Treat the cause
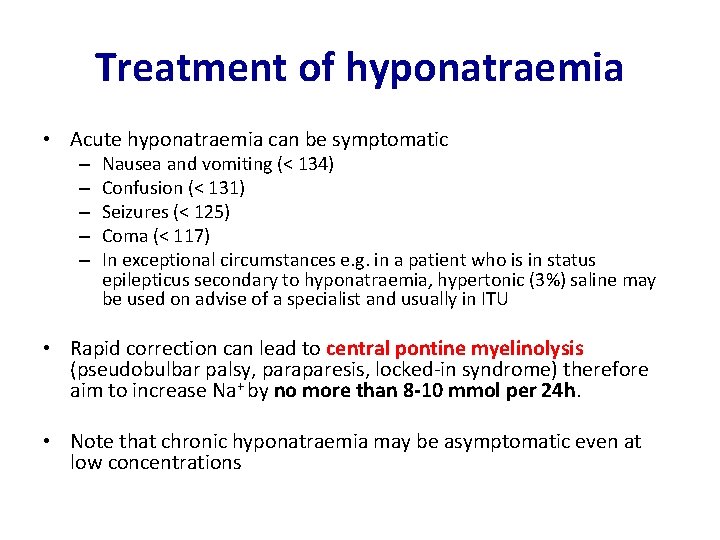
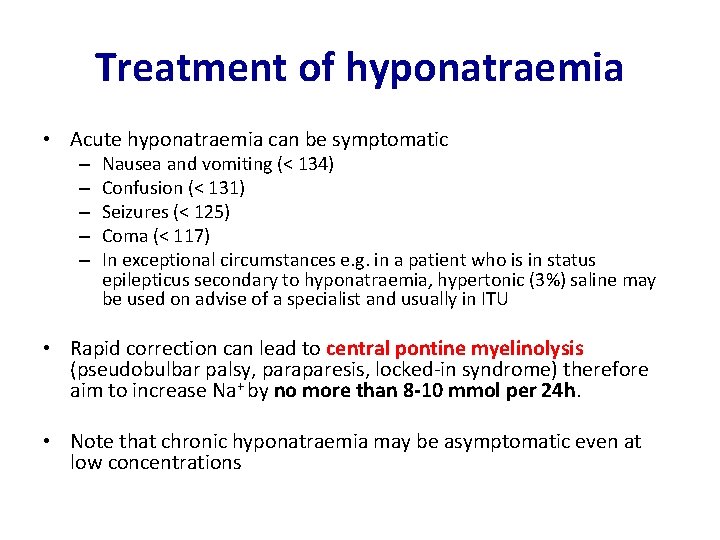
Treatment of hyponatraemia • Acute hyponatraemia can be symptomatic – – – Nausea and vomiting (< 134) Confusion (< 131) Seizures (< 125) Coma (< 117) In exceptional circumstances e. g. in a patient who is in status epilepticus secondary to hyponatraemia, hypertonic (3%) saline may be used on advise of a specialist and usually in ITU • Rapid correction can lead to central pontine myelinolysis (pseudobulbar palsy, paraparesis, locked-in syndrome) therefore aim to increase Na+ by no more than 8 -10 mmol per 24 h. • Note that chronic hyponatraemia may be asymptomatic even at low concentrations
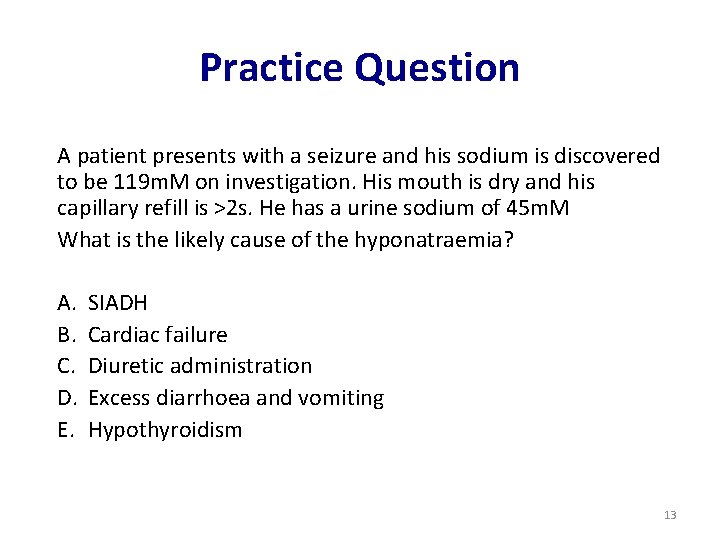
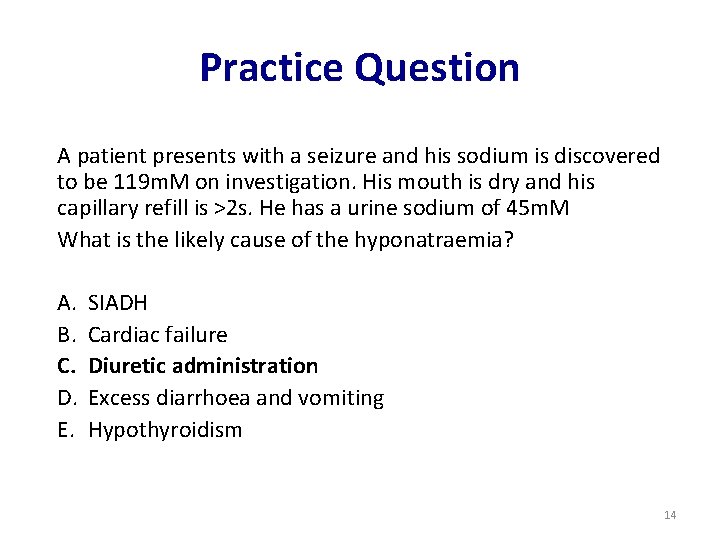
Practice Question A patient presents with a seizure and his sodium is discovered to be 119 m. M on investigation. His mouth is dry and his capillary refill is >2 s. He has a urine sodium of 45 m. M What is the likely cause of the hyponatraemia? A. B. C. D. E. SIADH Cardiac failure Diuretic administration Excess diarrhoea and vomiting Hypothyroidism 13
Practice Question A patient presents with a seizure and his sodium is discovered to be 119 m. M on investigation. His mouth is dry and his capillary refill is >2 s. He has a urine sodium of 45 m. M What is the likely cause of the hyponatraemia? A. B. C. D. E. SIADH Cardiac failure Diuretic administration Excess diarrhoea and vomiting Hypothyroidism 14
Practice Question VSA – type 1. A patient with severe hyponatraemia is thought to have SIADH. What would you expect his urine sodium to be? 15
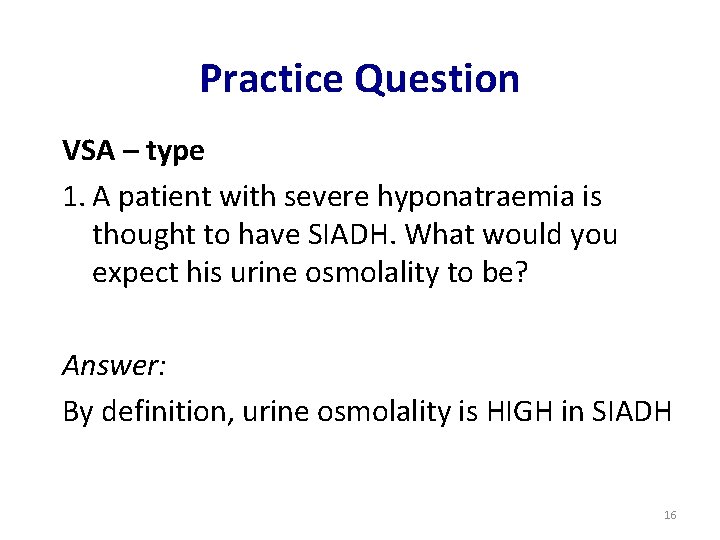
Practice Question VSA – type 1. A patient with severe hyponatraemia is thought to have SIADH. What would you expect his urine osmolality to be? Answer: By definition, urine osmolality is HIGH in SIADH 16
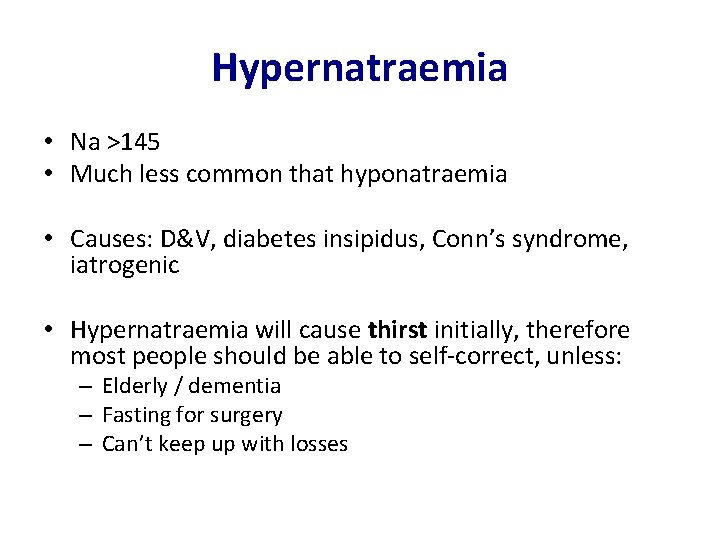
Hypernatraemia • Na >145 • Much less common that hyponatraemia • Causes: D&V, diabetes insipidus, Conn’s syndrome, iatrogenic • Hypernatraemia will cause thirst initially, therefore most people should be able to self-correct, unless: – Elderly / dementia – Fasting for surgery – Can’t keep up with losses
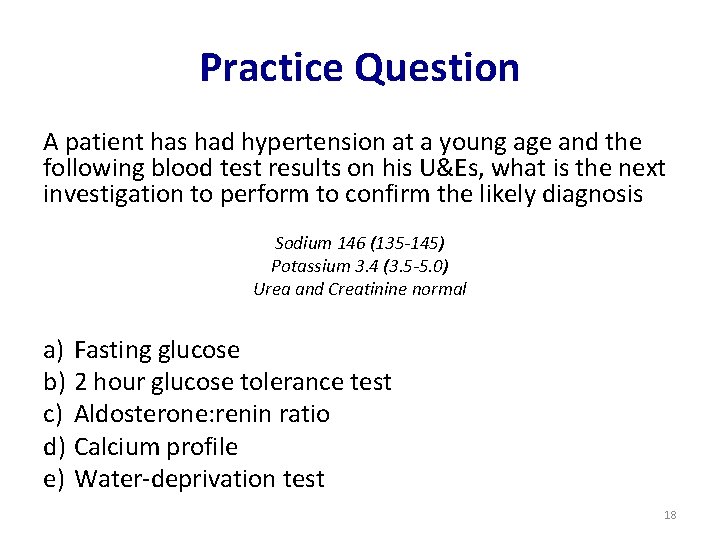
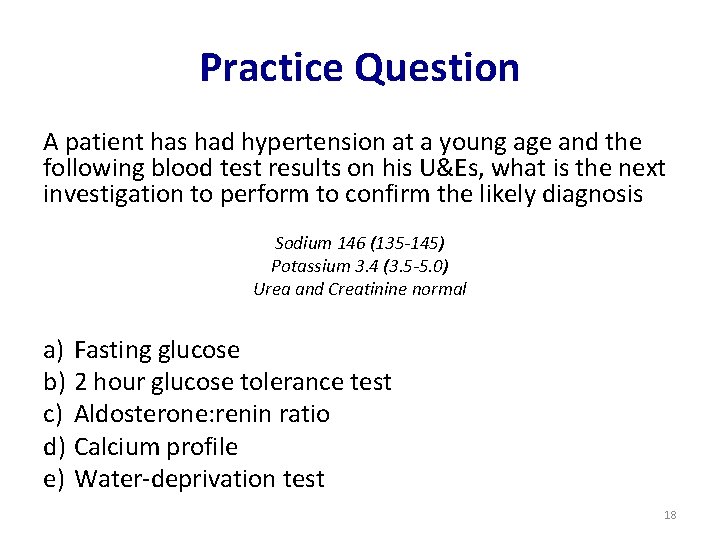
Practice Question A patient has had hypertension at a young age and the following blood test results on his U&Es, what is the next investigation to perform to confirm the likely diagnosis Sodium 146 (135 -145) Potassium 3. 4 (3. 5 -5. 0) Urea and Creatinine normal a) Fasting glucose b) 2 hour glucose tolerance test c) Aldosterone: renin ratio d) Calcium profile e) Water-deprivation test 18
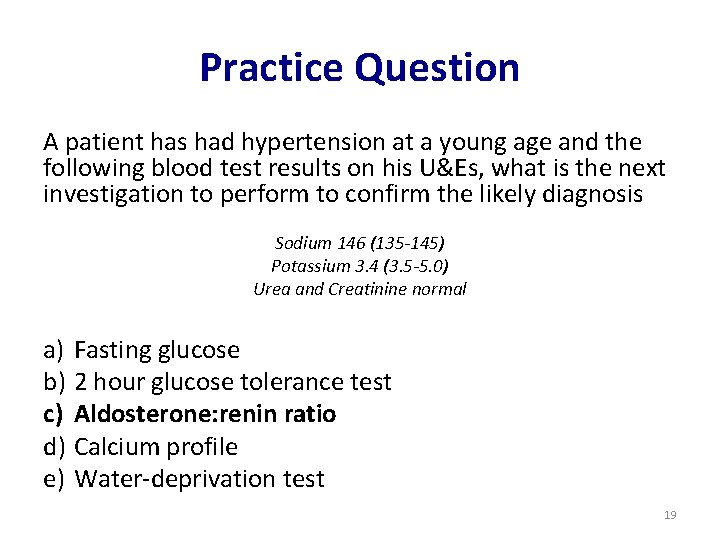
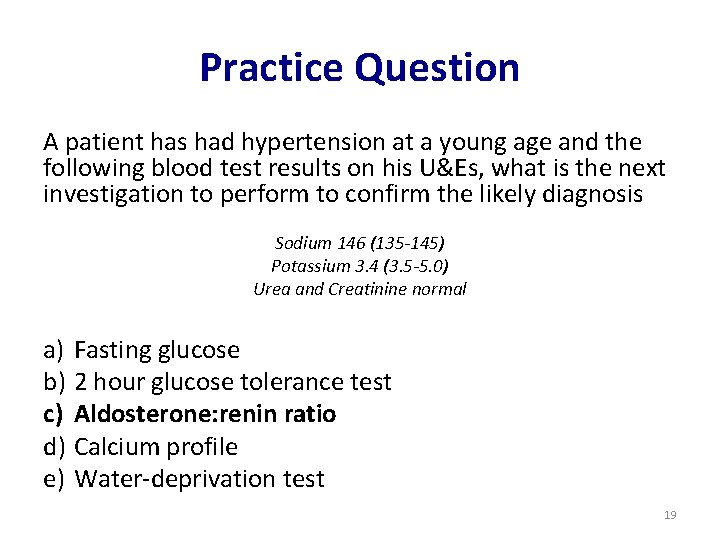
Practice Question A patient has had hypertension at a young age and the following blood test results on his U&Es, what is the next investigation to perform to confirm the likely diagnosis Sodium 146 (135 -145) Potassium 3. 4 (3. 5 -5. 0) Urea and Creatinine normal a) Fasting glucose b) 2 hour glucose tolerance test c) Aldosterone: renin ratio d) Calcium profile e) Water-deprivation test 19
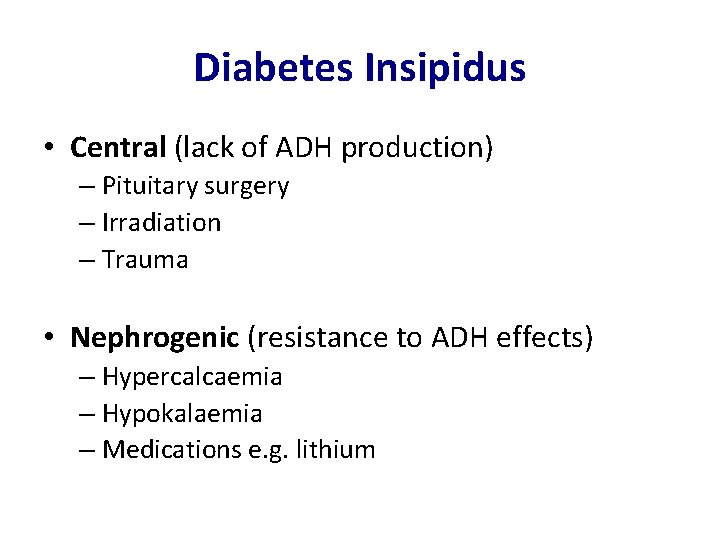
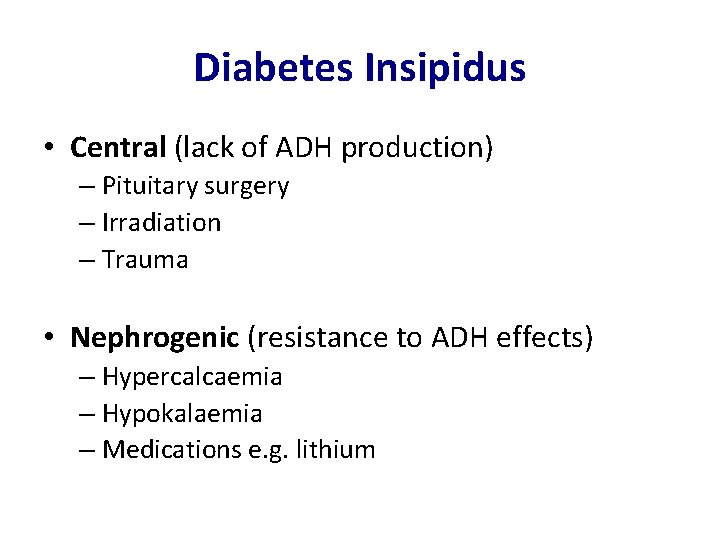
Diabetes Insipidus • Central (lack of ADH production) – Pituitary surgery – Irradiation – Trauma • Nephrogenic (resistance to ADH effects) – Hypercalcaemia – Hypokalaemia – Medications e. g. lithium
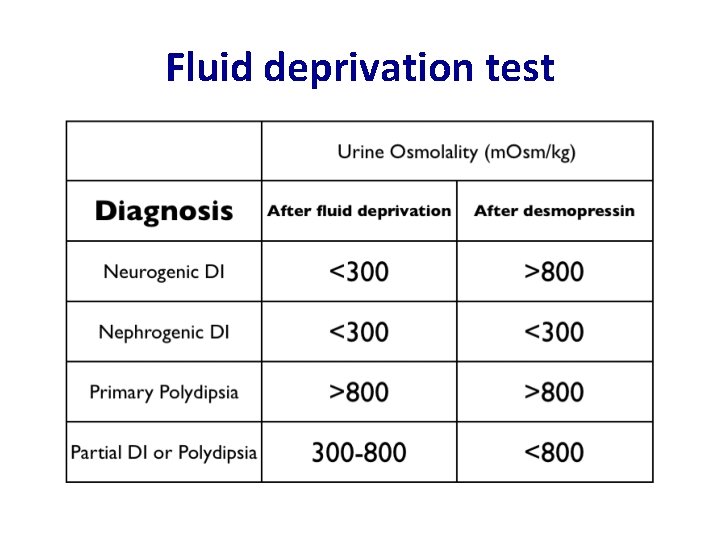
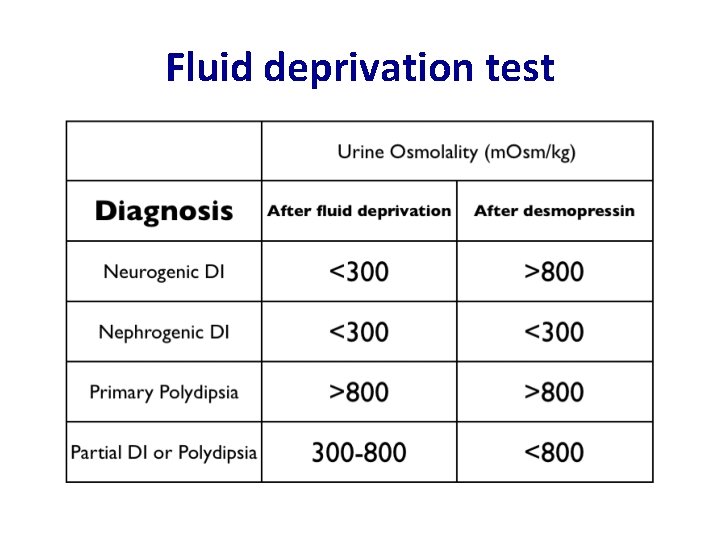
Fluid deprivation test
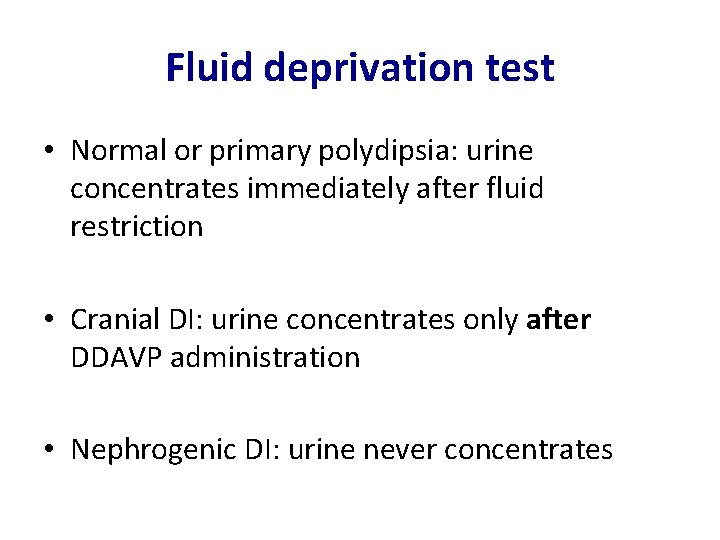
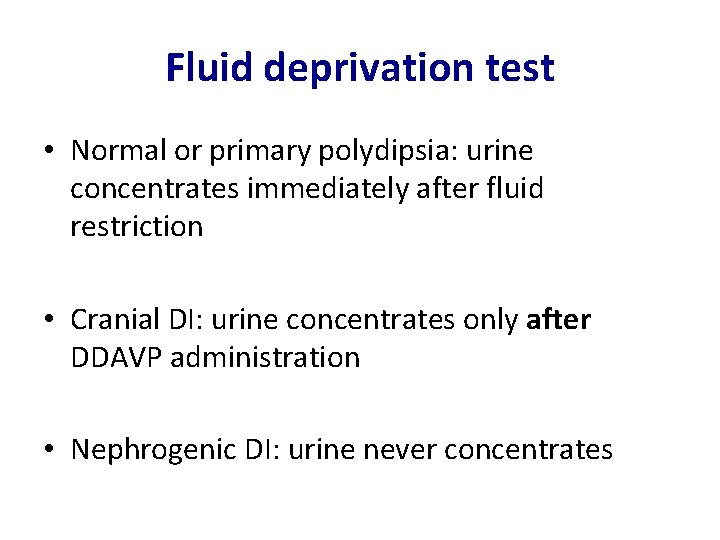
Fluid deprivation test • Normal or primary polydipsia: urine concentrates immediately after fluid restriction • Cranial DI: urine concentrates only after DDAVP administration • Nephrogenic DI: urine never concentrates
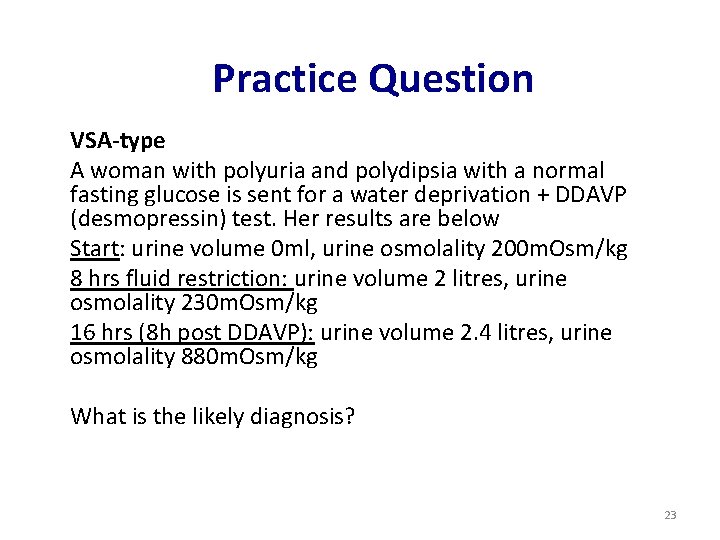
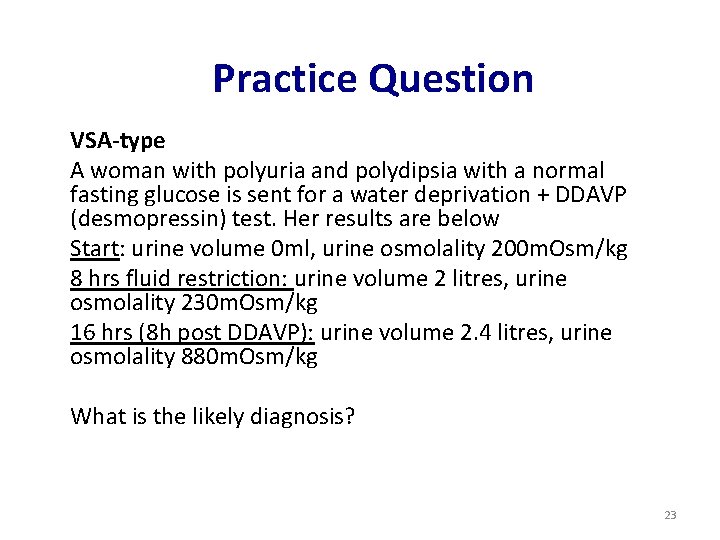
Practice Question VSA-type A woman with polyuria and polydipsia with a normal fasting glucose is sent for a water deprivation + DDAVP (desmopressin) test. Her results are below Start: urine volume 0 ml, urine osmolality 200 m. Osm/kg 8 hrs fluid restriction: urine volume 2 litres, urine osmolality 230 m. Osm/kg 16 hrs (8 h post DDAVP): urine volume 2. 4 litres, urine osmolality 880 m. Osm/kg What is the likely diagnosis? 23
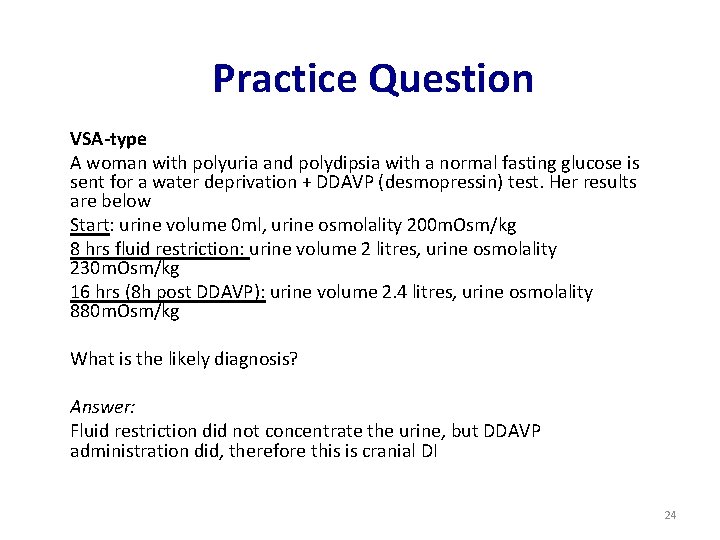
Practice Question VSA-type A woman with polyuria and polydipsia with a normal fasting glucose is sent for a water deprivation + DDAVP (desmopressin) test. Her results are below Start: urine volume 0 ml, urine osmolality 200 m. Osm/kg 8 hrs fluid restriction: urine volume 2 litres, urine osmolality 230 m. Osm/kg 16 hrs (8 h post DDAVP): urine volume 2. 4 litres, urine osmolality 880 m. Osm/kg What is the likely diagnosis? Answer: Fluid restriction did not concentrate the urine, but DDAVP administration did, therefore this is cranial DI 24
Contents • Sodium balance • Potassium • Enzymes and cardiac markers • Renal (AKI, CKD) • Metabolic disorders • Paediatric clinical chemistry Brief overview Will not be covered in this lecture – can be found in the path guide
Potassium • Normal range 3. 5 – 5. 5 mmol/l
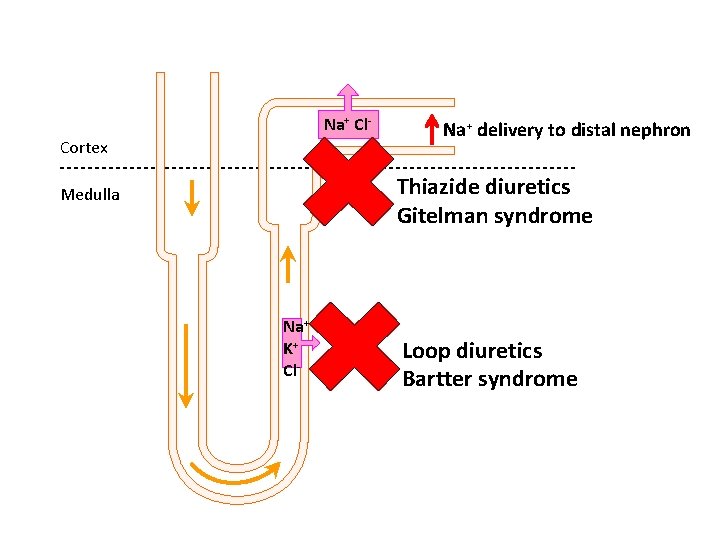
Hypokalaemia • Potassium < 3. 5 m. M • Causes: – GIT losses: vomiting, diarrhoea – Redistribution into cells, insulin, salbutamol, alkalosis – Renal losses: Conn’s, loop diuretics (and Barter’s syndrome), thiazide diuretics (and Gitelman syndrome), renal tubular acidosis – Very poor dietary intake
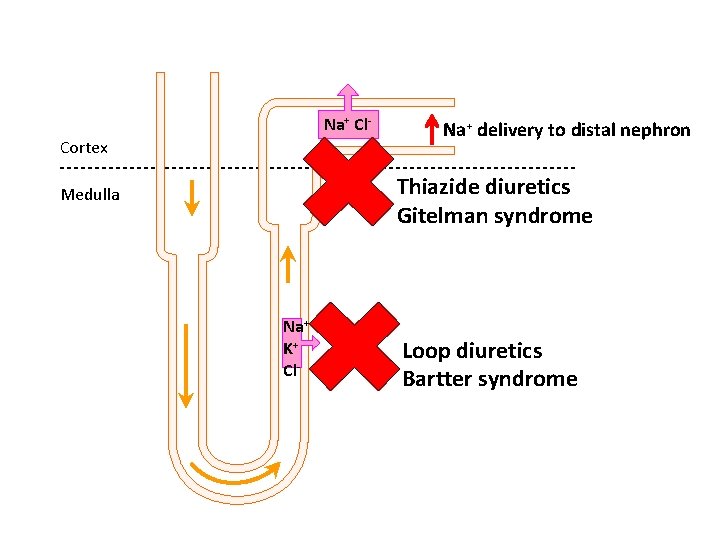
Na+ Cl. Cortex Na+ delivery to distal nephron Thiazide diuretics Gitelman syndrome Medulla Na+ K+ Cl- Loop diuretics Bartter syndrome
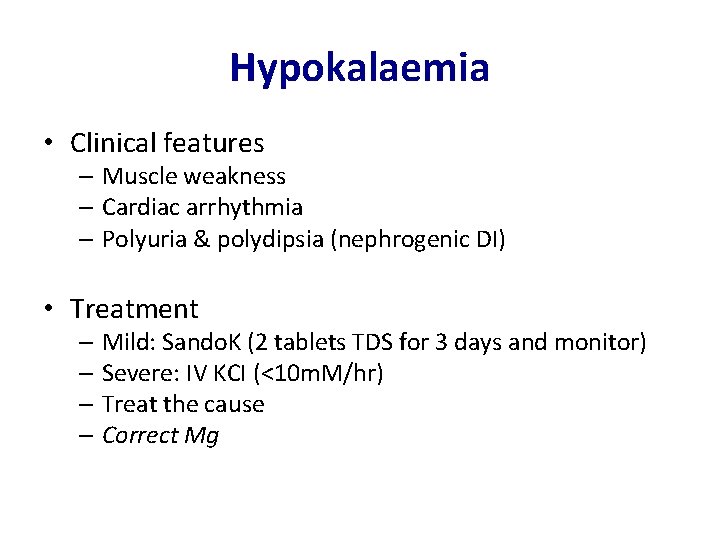
Hypokalaemia • Clinical features – Muscle weakness – Cardiac arrhythmia – Polyuria & polydipsia (nephrogenic DI) • Treatment – Mild: Sando. K (2 tablets TDS for 3 days and monitor) – Severe: IV KCI (<10 m. M/hr) – Treat the cause – Correct Mg
Practice Question Which of the following drugs is most likely to contribute to hypokalaemia in a patient? a) Spironolactone b) Digoxin c) Lithium d) Frusemide e) Ramipril 30
Practice Question Which of the following drugs is most likely to contribute to hypokalaemia in a patient? a) Spironolactone b) Digoxin c) Lithium d) Frusemide e) Ramipril 31
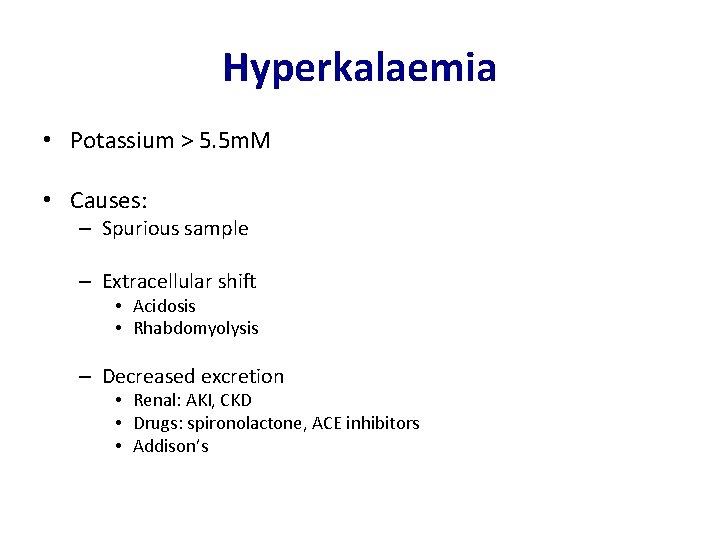
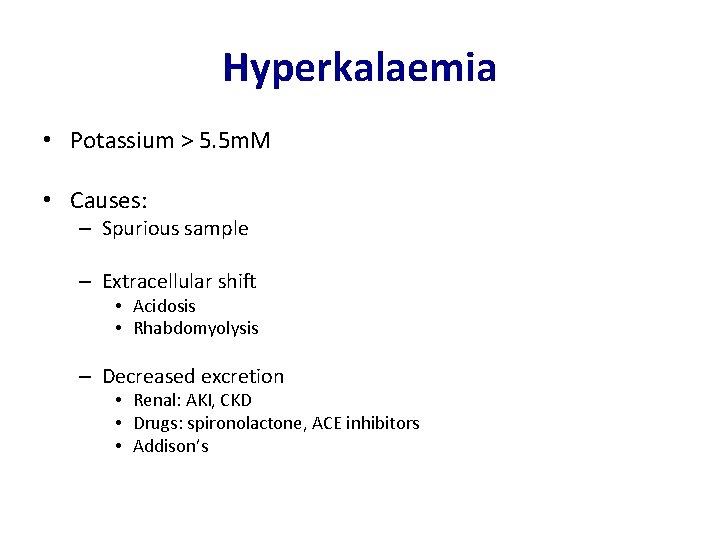
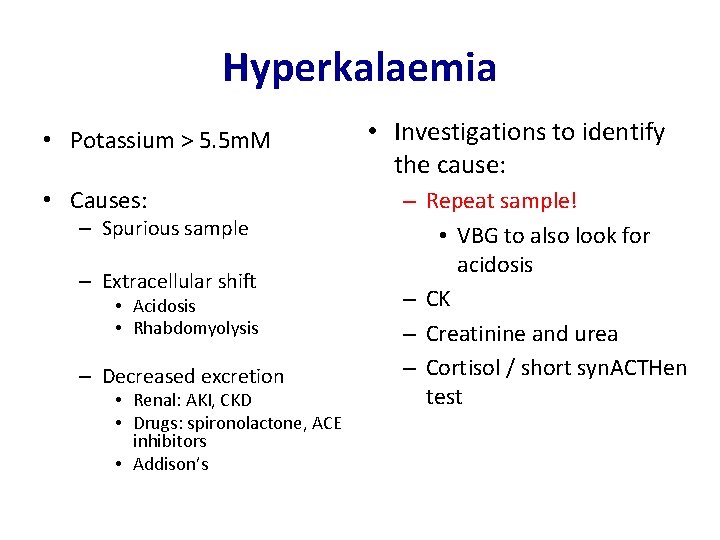
Hyperkalaemia • Potassium > 5. 5 m. M • Causes: – Spurious sample – Extracellular shift • Acidosis • Rhabdomyolysis – Decreased excretion • Renal: AKI, CKD • Drugs: spironolactone, ACE inhibitors • Addison’s
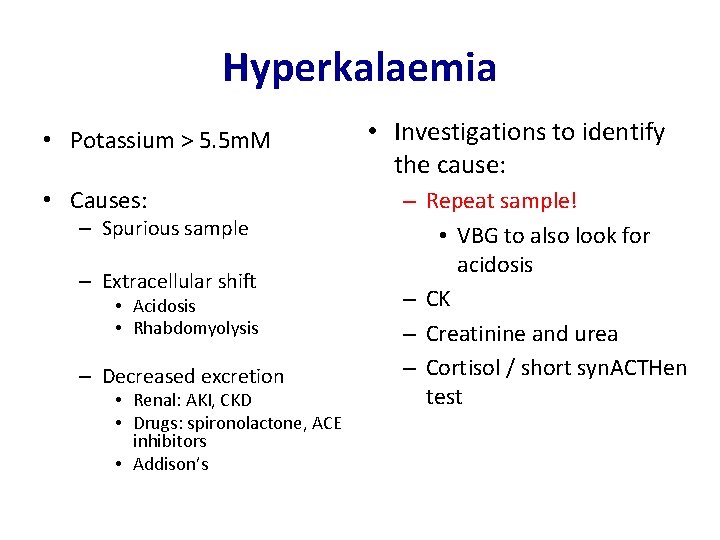
Hyperkalaemia • Potassium > 5. 5 m. M • Causes: – Spurious sample – Extracellular shift • Acidosis • Rhabdomyolysis – Decreased excretion • Renal: AKI, CKD • Drugs: spironolactone, ACE inhibitors • Addison’s • Investigations to identify the cause: – Repeat sample! • VBG to also look for acidosis – CK – Creatinine and urea – Cortisol / short syn. ACTHen test
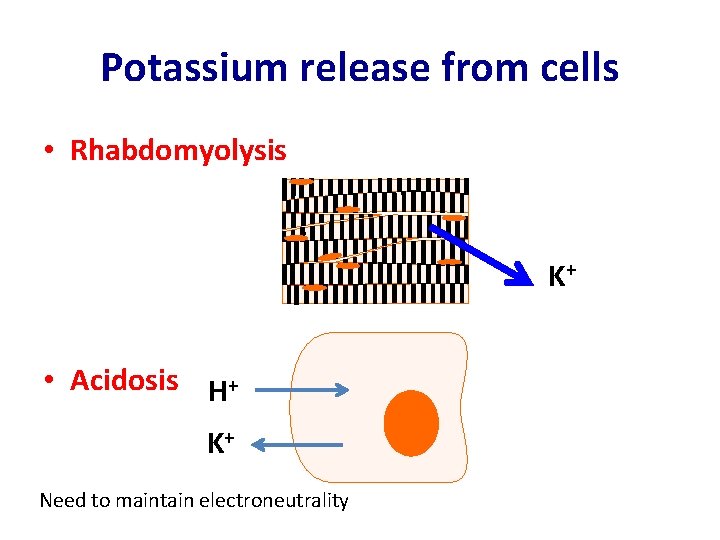
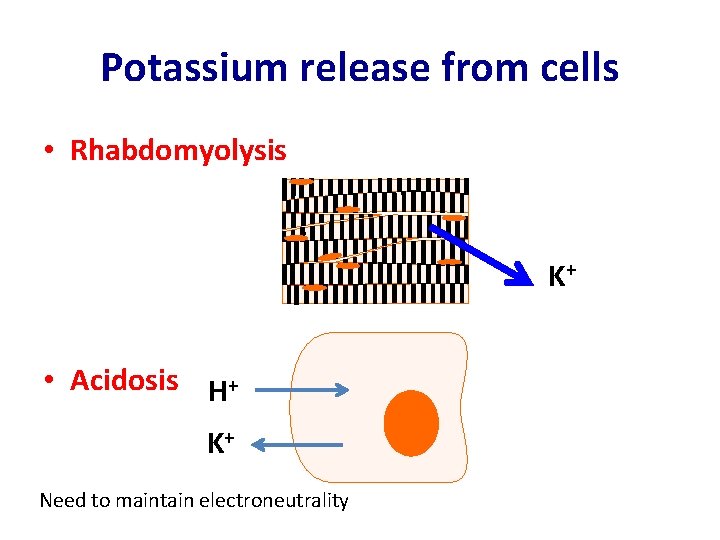
Potassium release from cells • Rhabdomyolysis K+ • Acidosis H+ K+ Need to maintain electroneutrality
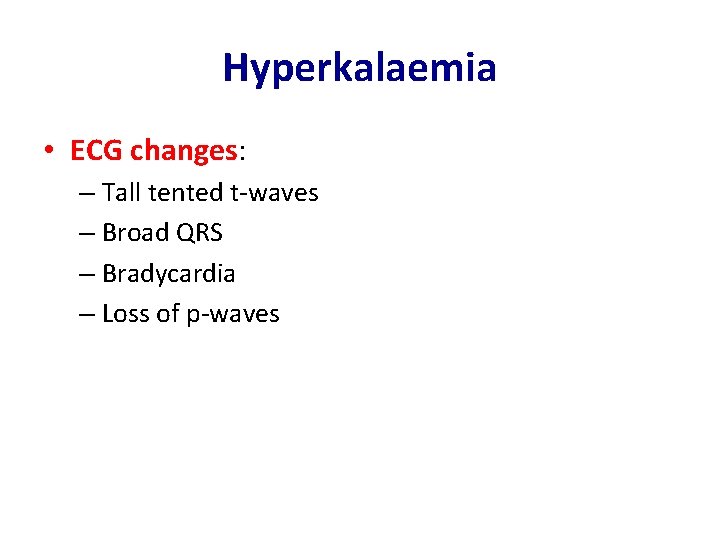
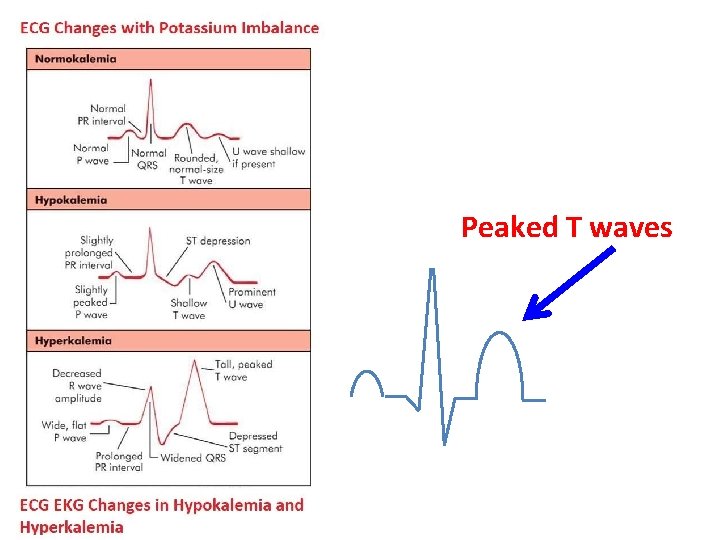
Hyperkalaemia • ECG changes: – Tall tented t-waves – Broad QRS – Bradycardia – Loss of p-waves
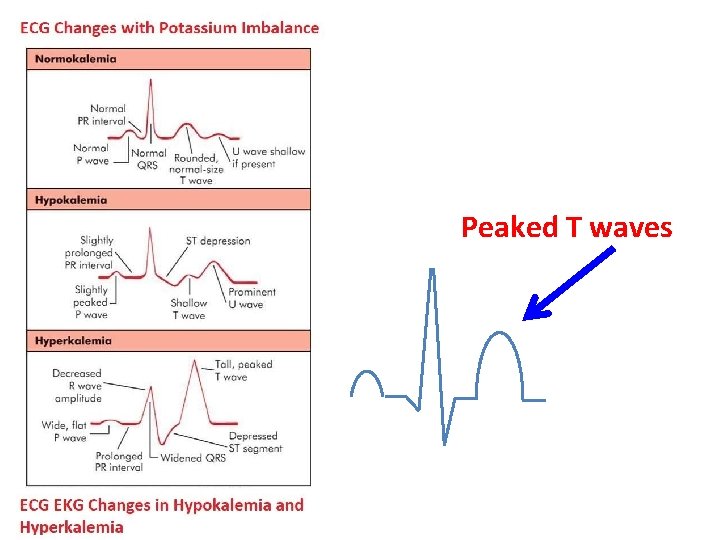
Peaked T waves
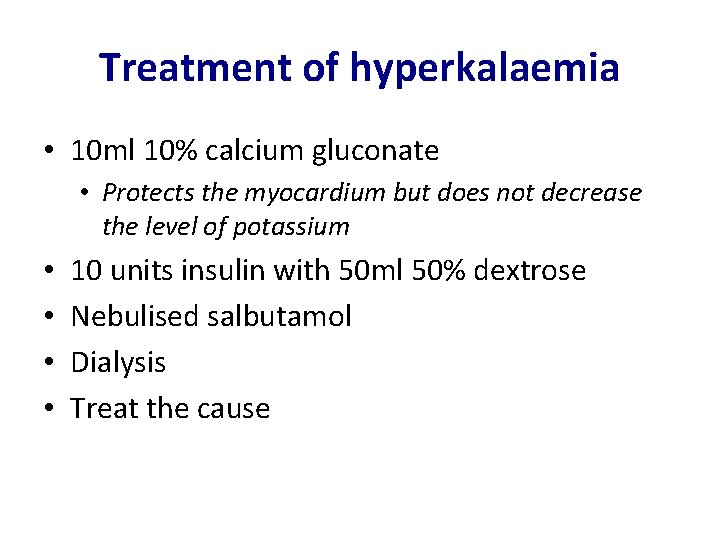
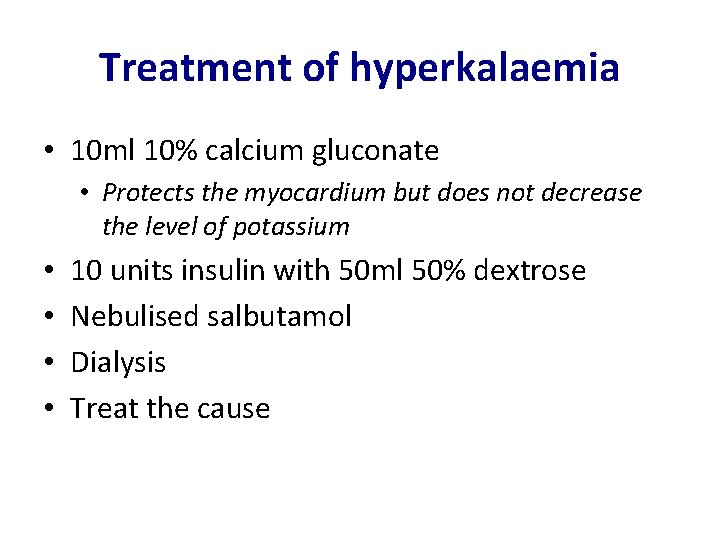
Treatment of hyperkalaemia • 10 ml 10% calcium gluconate • Protects the myocardium but does not decrease the level of potassium • • 10 units insulin with 50 ml 50% dextrose Nebulised salbutamol Dialysis Treat the cause
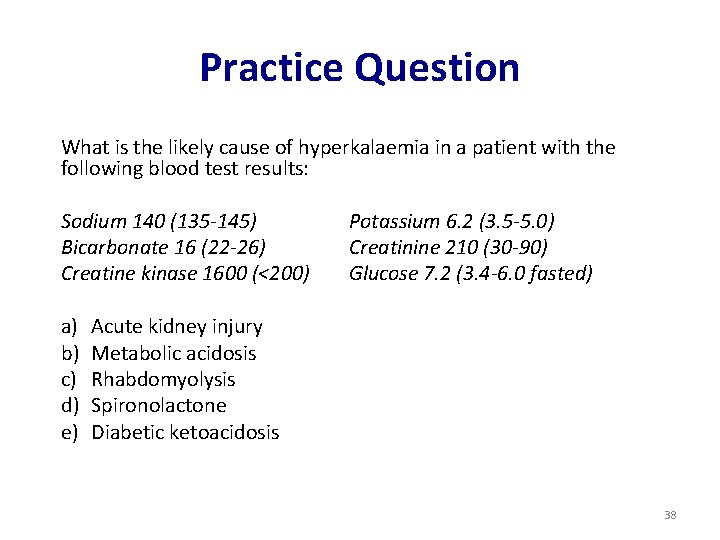
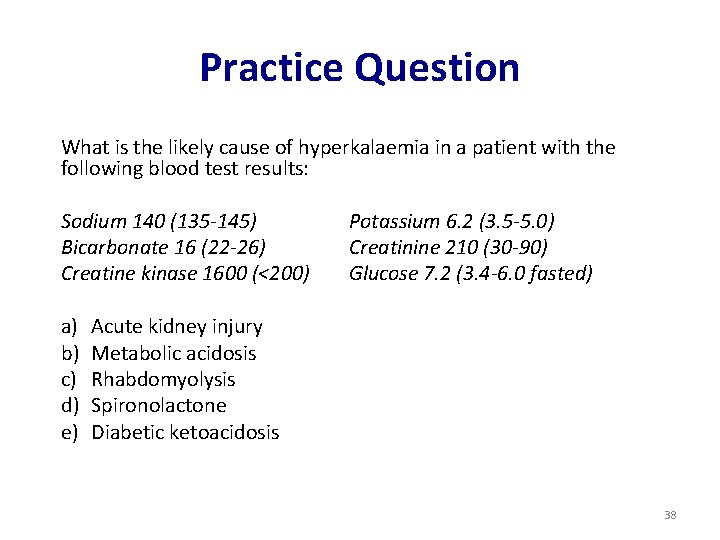
Practice Question What is the likely cause of hyperkalaemia in a patient with the following blood test results: Sodium 140 (135 -145) Bicarbonate 16 (22 -26) Creatine kinase 1600 (<200) a) b) c) d) e) Potassium 6. 2 (3. 5 -5. 0) Creatinine 210 (30 -90) Glucose 7. 2 (3. 4 -6. 0 fasted) Acute kidney injury Metabolic acidosis Rhabdomyolysis Spironolactone Diabetic ketoacidosis 38
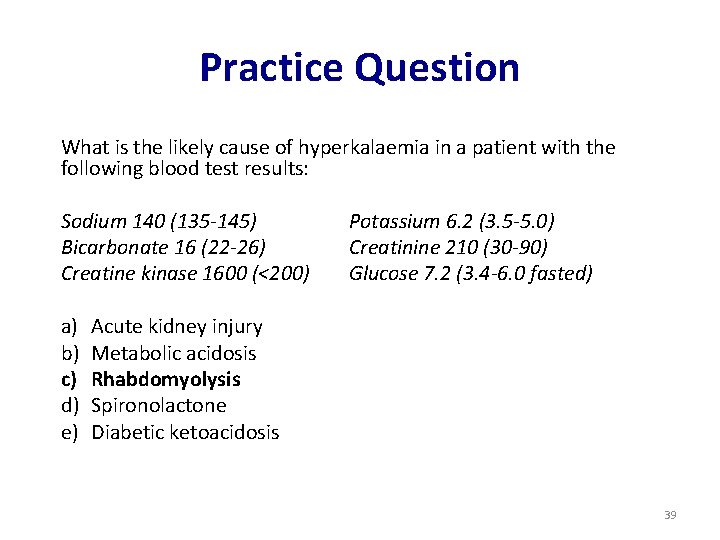
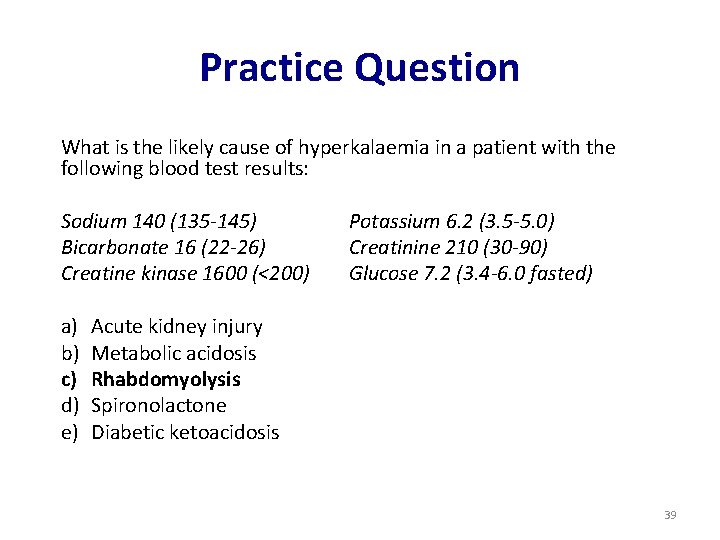
Practice Question What is the likely cause of hyperkalaemia in a patient with the following blood test results: Sodium 140 (135 -145) Bicarbonate 16 (22 -26) Creatine kinase 1600 (<200) a) b) c) d) e) Potassium 6. 2 (3. 5 -5. 0) Creatinine 210 (30 -90) Glucose 7. 2 (3. 4 -6. 0 fasted) Acute kidney injury Metabolic acidosis Rhabdomyolysis Spironolactone Diabetic ketoacidosis 39
Contents • Sodium balance • Potassium • Enzymes and cardiac markers • Renal (AKI, CKD) • Metabolic disorders • Paediatric clinical chemistry Brief overview Will not be covered in this lecture – can be found in the path guide
Enzymes and cardiac markers • • • Amylase CK Troponin ALP BNP
Amylase • Typically raised in acute abdominal pathology • Very high serum levels (usually >10 x ULN) in acute pancreatitis
CK • Creatine Kinase • Marker of muscle damage • Causes: – Physiological: Afro-Carribean, body-builders – Pathological: Duchenne Muscular Dystrophy (>10 x ULN), statin related myopathy, rhabdomyolysis
Troponin • Myocardial injury biomarker • Serial measurements particularly useful • Measure at 6 h, then at 12 h after onset of chest pain (remains elevated for 3 -10 days) • In clinical practice, often measured at 2 h intervals
ALP • Alkaline phosphatase • Present in high concentrations in liver, bone, intestine and placenta • To differentiate liver from bone ALP you can measure another organ-specific enzyme e. g. GGT • Causes: – Physiological: pregnancy – Pathological: • >5 x ULN: bone (e. g. Paget’s – isolated rise), liver (cholestasis – will also have raised GGT) • <5 x ULN: bone (tumours, fractures), liver (hepatitis)
BNP • Brain natriuretic peptide • Released from ventricles in the heart in response to ventricular stretch • Levels <100 are highly specific for excluding heart failure • Levels >400 highly sensitive for heart failure
Contents • Sodium balance • Potassium • Enzymes and cardiac markers • Renal (AKI, CKD) • Metabolic disorders • Paediatric clinical chemistry Brief overview Will not be covered in this lecture – can be found in the path guide
Acute kidney injury • Considered a medical emergency • Causes: – Pre-renal: usually hypovolaemia • Treatment: volume replacement – Renal: vascular, glomerular, tubular, interstitial • Treat the cause – Post-renal: usually obstruction e. g. BPH, ureteric stone • Treatment: relieve the obstruction
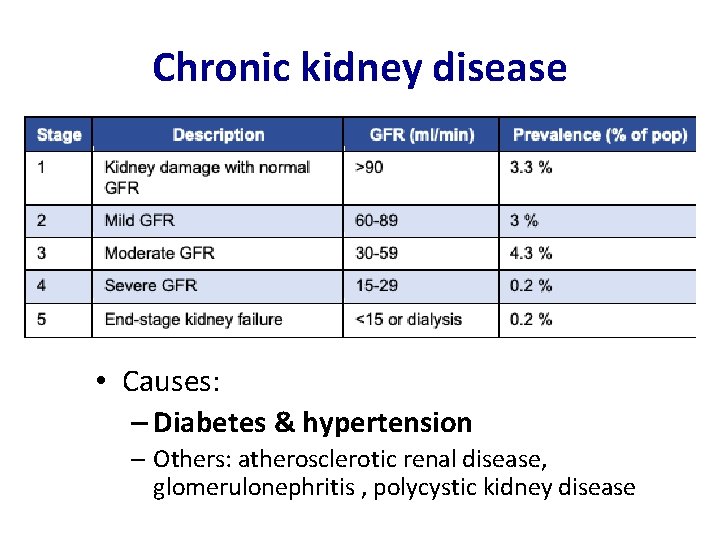
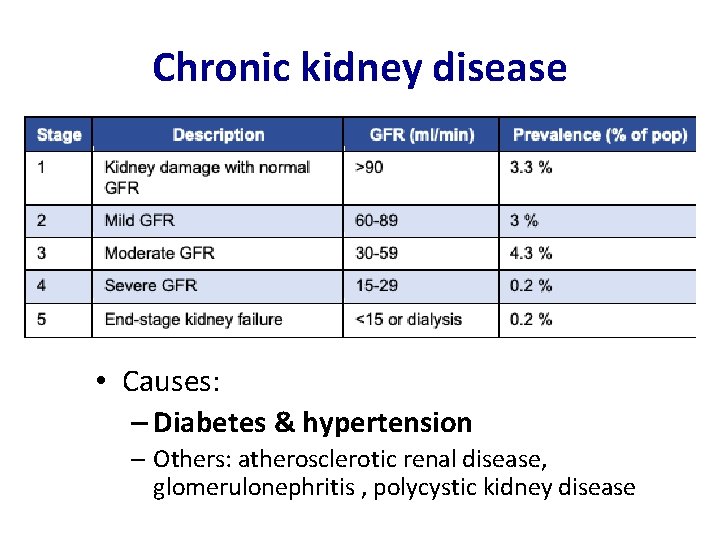
Chronic kidney disease • Causes: – Diabetes & hypertension – Others: atherosclerotic renal disease, glomerulonephritis , polycystic kidney disease
Chronic kidney disease • Complications are related to the primary functions of the kidney • Progressive failure of homeostatic function – Acidosis • Progressive failure of hormonal function – Anaemia (loss of EPO synthesis) – Renal Bone Disease (secondary hyperparathyroidism due to low Vit D) • Progressive failure to maintain water balance – Fluid overload • Progressive failure to maintain electrolyte balance – Hyperkalaemia • Cardiovascular disease – Vascular calcification and subsequent atherosclerosis (biggest mortality in CKD) • Uraemia and Death
Indications for dialysis • Remember your vowels: A E I O • • • U Acidosis (metabolic) Electrolytes (refractory hyperkalaemia) Ingested toxins Overload (pulmonary oedema) Uraemia (symptomatic)
Renal replacement therapy • Dialysis – Haemodialysis • Via central line or AV fistulae (requires surgery to create) • Usually done 3 x/week in hospital – Peritoneal dialysis • Done via a Tenckoff catheter – uses peritoneum as the dialysis membrane • Can be done at home • Increased risk of infections • Renal transplant – The only definitive cure – Requires life long immunosuppression

Thank you for listening! Any questions? Feedback link: https: //forms. gle/P 3 X 31 X 9 WEUxgawb 36
 Ayling sanjaya
Ayling sanjaya Empirical formula pogil
Empirical formula pogil Are kc and kp equal
Are kc and kp equal Section 2 classifying chemical reactions worksheet answers
Section 2 classifying chemical reactions worksheet answers Section 1 chemical changes
Section 1 chemical changes Section 2 reinforcement classifying chemical reactions
Section 2 reinforcement classifying chemical reactions Love chemical formula
Love chemical formula Prostate pathology
Prostate pathology Marcroft grains pathology
Marcroft grains pathology Plant pathology
Plant pathology Quad tendon ultrasound
Quad tendon ultrasound Pathology branches
Pathology branches Echinococcus granulosus sketchy
Echinococcus granulosus sketchy American board of pathology moc
American board of pathology moc Types of fungicides
Types of fungicides Crenation
Crenation Tennis racket appearance in oral pathology
Tennis racket appearance in oral pathology Pathology of rheumatoid arthritis
Pathology of rheumatoid arthritis Clinical pathology accreditation
Clinical pathology accreditation Oral medicine
Oral medicine Rph pathology
Rph pathology Aschoff bodies diagram
Aschoff bodies diagram Data-centric pathology
Data-centric pathology Vesiculography
Vesiculography Musculoskeletal
Musculoskeletal Snomed codes pathology
Snomed codes pathology Clavulonate
Clavulonate Granulation tissue
Granulation tissue Staphyl/o medical term
Staphyl/o medical term Plant pathology
Plant pathology Systemic pathology questions and answers pdf
Systemic pathology questions and answers pdf Monomorphic adenoma salivary gland
Monomorphic adenoma salivary gland Plant pathology
Plant pathology Anisofilia
Anisofilia Destructive pathology
Destructive pathology Functional pathology definition
Functional pathology definition Oral pathology
Oral pathology Clinical pathology accreditation
Clinical pathology accreditation Concomitant
Concomitant Thyroid pathology
Thyroid pathology Job market for pathologists
Job market for pathologists Albugo eye
Albugo eye Interlocking pathology
Interlocking pathology Body fluid
Body fluid Cardiac asthma vs bronchial asthma
Cardiac asthma vs bronchial asthma Ajkd atlas
Ajkd atlas Female reproductive system pathology
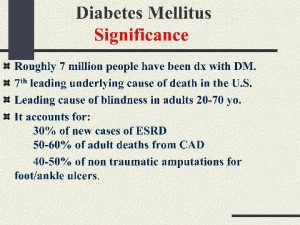
Female reproductive system pathology Dm pathology
Dm pathology Cert 3 in pathology collection
Cert 3 in pathology collection Congestion intestinal
Congestion intestinal Oral pathology
Oral pathology Where does fraser health cover
Where does fraser health cover Penis small
Penis small Pyelonephritis
Pyelonephritis