Organ Pathology Female Genital System II Pathology of












































- Slides: 44

Organ Pathology Female Genital System - II Pathology of ovaries, tubes, breast, pregnancy Jaroslava Dušková Inst. Pathol. , 1 st Med. Faculty, Charles Univ. Prague

Diseases of the Fallopian Tubes v inborn – malformations: – aplasia (Müllerian duct disorders) v bilateral incl. uterus & vagina v unilateral incl. kidney – partial atresia v acquired

Diseases of the Fallopian Tubes v inborn v acquired – non neoplastic : atrophy, infection – pyosalpinx, hydrosalpinx, tbc salpingitis, synechiae – salpingitis isthmica nodosa – pseudotumours – cysts, ectopic pregnancy, – neoplastic: adenocarcinoma

Diseases of the Fallopian Tubes & Ovaries v PID – pelvic inflammatory disease (chronic salpingooophoritis) v tubar sterility

Diseases of the Ovaries v inborn v acquired – non-neoplastic – pseudotumours – neoplastic v benign v BORDERLINE v malignant (cont. )

Diseases of the Ovaries v inborn – malformations: – aplasia (incl. kidney, uterus & vagina), – hypoplasia/dysplasia (e. g. in adrenogenital syndrome – pseudohermafroditismus femininus, Turner sy (45 X 0, or 45 X 0/46 XX) v acquired (cont. )

Diseases of the Ovaries v inborn v acquired – non-neoplastic atrophy - involution, inflammation – PID, actinomycosis, tbc v – pseudotumours – neoplastic v benign v BORDERLINE

Diseases of the Ovaries v v inborn acquired – non-neoplastic – pseudotumours stromal hyperplasia v CYSTS v – neoplastic v benign v BORDERLINE v malignant (cont. )

Ovary - cysts v follicle v luteal v inclusion v endometrial („chocolate“) v. POLYCYSTIC OVARIES (Stein- Leventhal syndrome) – obesity – hirsutism – infertility – oligo- or amenorrhea

Diseases of the Ovaries v inborn v acquired – pseudotumours (stromal hyperplasia, dif. dg. –TUMOURS CYSTS)

TUMOURS of the Ovary 119 (!) coded nosology units ICD-O Classification groups v. Surface epithelial stromal Sex cord stromal v Germ cell v v Mixed germ cell sex cord-stromal Tumour of the rete ovarii Miscelaneous, tumour like lesions v Lymphomas & leukemias v v v Secondary v tumours of the ovary Peritoneal tumours

Ovary malignant neoplasms v Czech Rep. 1323 new cases 2002 v Czech Rep. 25, 3/ 100 000 women v Europe 20, 6/ 100 000 women v World 15, 1/ 100 000 women

TUMOURS of the Ovary Surface epithelial stromal tumours v v v v 30% of fem. gen. neoplasms middle & old age risk factors: longer HRT, obesity protective factors: high parity, oral contraceptives precursors: inclusion cyts, endometriosis lack of early warning symptoms 70% dg. at a late stage – ca peritonitis mean 5 -year survival in Europe 32% (!!!)

TUMOURS of the Ovary Surface epithelial stromal tumours - macroscopy v v v small to more than 20 cm two thirds bilateral solid & cystic with intracystic papillae confluent papillae, softer borderline necroses & haemorrhage susp. malignancy

TUMOURS of the Ovary stromal tumours Surface epithelial - microscopy v serous - endosalpigeoma v mucinous – endocervicoma v mixed v endometrioid (coinciding with endometrial ca) v Brenner tumour ------------v papillary cystadenoma v papillary borderline v papillary cystadenocarcinomas

TUMOURS of the Ovary 119 (!) coded nosology units ICD-O Classification groups v. Surface epithelial stromal Sex cord stromal v Germ cell v v Mixed germ cell sex cord-stromal Tumour of the rete ovarii Miscelaneous, tumour like lesions v Lymphomas & leukemias v v v Secondary v tumours of the ovary Peritoneal tumours

TUMOURS of the Ovary Sex cord stromal tumours v Granulosa-stromal cell tumours v Thecoma-fibroma group v Sertoli- Leydig cell group v Others…. .

TUMOURS of the Ovary Sex cord stromal tumours Granulosa-stromal cell tumours v manifesting mostly as a solid or cystic mass or with steroid hormones production E/A effects – adult – juvenile – bleeding disorders, virilisation, – isosexual precoccious puberty

TUMOURS of the Ovary 119 (!) coded nosology units ICD-O Classification groups v. Surface v epithelial stromal Sex cord stromal v Germ cell v Mixed germ cell sex cord-stromal Tumour of the rete ovarii Miscelaneous, tumour like lesions v Lymphomas & leukemias v v v Secondary v tumours of the ovary Peritoneal tumours

TUMOURS of the Ovary Germ cell Tumours –dysgerminoma (= seminoma ovarii) – embryonal carcinoma – teratoma (mature, immature) – yolc sac tumour – choriocarcinoma

Embryonal carcinoma v composed of primitive anaplastic-appearing epithelial cells v pure rare, mostly in combined germ cell tumours v peak incidence 30 years v swelling, 2/3 patients with metastases at diagnosis v macro : tan/gray, necroses, hemorrhages v micro: solid, tubular, PLAP, CK +

Mesoblastoma vitellinum- yolc sac tumour –endodermal sinus tumour v 80% of prepubertal germ cell tumours v in postpubertal as admixture v painless mass, serum AFP elevated v macro: gray/tan nonencapsulated v micro: many variants – microcystic, solid, festoon-like, hepatoid, spindle cell… v AFP+, alpha 1 -Antitrypsin

Choriocarcinoma (non gestational) v rare v admixture in many germ cell tumours v malignant v children & young adults v presents with bleeding and precoccious pseudopuberty v ß-HCG + morphologicall identical with gestational ch.

Teratomas Def. : Tumours (benign, borderline or malignant) composed of two or more different cell lines that are NOT normally present in the place of tumour origin

Teratoma v coetaneous – differentiated -cystic v embryonal – nondifferentiated solid

TUMOURS of the Ovary Secondary tumours of the ovary v metastatic v - advanced stage poor prognosis v Krukenberg tumour – metastatic signet ring cell ca originating mostly in the stomach or colon

Diseases of the Breast v inborn – malformations: – amastia, polymastia (mamma accessoria), aberant mammary tissue, polythelia v acquired

Diseases of the Breast v v inborn acquired – degenerations: amyloid, mastitis: acute puerperal, chronic – Pseudotumours (& precanceroses) : fibrocystic disease, lipophagic granuloma, silicon granuloma, suture granuloma…. – TUMOURS

Fibrocystic Breast Disease Def: dyshormonal changes of the breast tissue with variably increased risk of breast cancer according to the type of epithelial proliferation

Fibrocystic Breast Disease - symptoms v palpable lump v fluctuating cysts v (pain)

Fibrocystic Breast Disease - morphology v fibrosis v cysts v epithelial hyperplasia – ductal, lobular – adenosis : simple, florid, sclerosing, microglandular – usual, atypical – papillary

Tumours of the Breast WHO 2003 75 ICD-O coded nosology units v epithelial v myoepithelial v mesenchymal v fibroepithelial v tumours of the nipple v malignant lymphoma v metastatic tumours v tumours of the male breast

Tumours of the Breast symptoms v early stage – asymptomatic – mammography – (microcalciffication) v palpable lump v nipple discharge v breast configuration change v ulceration v metastases

Benign epithelial tumours vintraductal papilloma - central - peripheral vtubular adenoma

Breast cancer – high risk v age more than 50 v developed countries USA, Europe v positive family history v atypical hyperplasia v BRCA 1 gen (40 -50%), BRCA 2 gen, + other ca (bowel, ovary, prostate, stomach, pankreas. . )

Breast cancer – increased risk vmenarche prior 11 & menopause after 55 yrs vnuliparity late first delivery 30 -35 let vhigher socioeconomic group vobesity vradiation

Breast cancer – increased risk vetanol voral abuse contraceptives uncertain v. HRT following 10 -15 yrs administration

Ductal ca in situ DCIS TDLU, seldom larger ducts v precursor of invasive ca v microcalcification on mammography 85% of cases detected with imaging techniques v screening introduction incidence from 2, 4/ 100 000 to 15, 8/ 100 000

Ductal ca in situ DCIS Histopathology vsolid, papillary, cribriform, comedo v cytology (grading) G 1 -3

Lobular carcinoma in situ LCIS v v 85% multicentric, 30% bilateral precursor of invasive ca Histopathology: v preserved lobular architecture, TDLU involvement, small monomorphous cells, regular nuclei

Breast cancer -prognosis v typing v grading v staging v hormonal receptors (ER & PRimmunohistochemistry) v c-erb. B-2 receptoru (immunohistochemistry, FISH) v proliferation activity (immunohistochemistry Ki-67 index) v angioinvasion

Mixed Tumours Def. : Tumours (benign or malignant) composed of two or more different cell lines that are normally present in the place of tumour origin

Fibroadenoma vyoung vfirm age (30 yr) circumscribed, painles vmostly up to 30 mm vsolitary vstromal & epithelial component

Phyllodes tumor vmiddle age (50 yrs) vmostly benign, recurrences vpainless, up to 50 mm vmore cellular stromal component
 Female genitalia labeled
Female genitalia labeled Tubi seminiferi drepti
Tubi seminiferi drepti Cervical ectropion
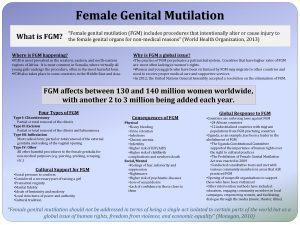
Cervical ectropion Female genital mutilation
Female genital mutilation Anteversion of uterus
Anteversion of uterus Female genital
Female genital Function of fallopian tube
Function of fallopian tube Female reproductive system pathology
Female reproductive system pathology Female reproductive system pathology
Female reproductive system pathology Female reproductive system pathology
Female reproductive system pathology Hysterosalpingoophorectomy
Hysterosalpingoophorectomy Uterine seal
Uterine seal Female reproductive system pathology
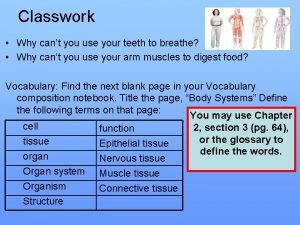
Female reproductive system pathology Cell tissue organ organ system organism
Cell tissue organ organ system organism Cell to tissue to organ to organ system to organism
Cell to tissue to organ to organ system to organism Organ and organ system
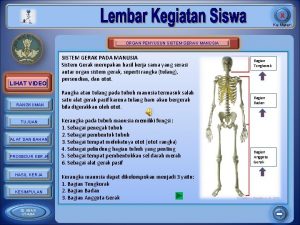
Organ and organ system Organ penyusun sistem gerak adalah ….
Organ penyusun sistem gerak adalah …. Tractus respiratorius
Tractus respiratorius Organ penyusun sistem koordinasi
Organ penyusun sistem koordinasi Similarities between male and female reproductive system
Similarities between male and female reproductive system Body parts name female
Body parts name female Pearson
Pearson Female sex organ
Female sex organ Ovarian ligament
Ovarian ligament Genital parasite
Genital parasite Male genital variation
Male genital variation Genital hijyen
Genital hijyen Fijacion en la etapa anal
Fijacion en la etapa anal Cestodes
Cestodes Genital hijyen nedir
Genital hijyen nedir Genital hijyen nedir
Genital hijyen nedir Historia natural del herpes simple
Historia natural del herpes simple Hsv-2 oral transmission rates
Hsv-2 oral transmission rates Nido sin usar
Nido sin usar Shark belongs to which phylum
Shark belongs to which phylum Appareil génital souris femelle
Appareil génital souris femelle Appareil génital souris femelle
Appareil génital souris femelle Patricia castillo anal
Patricia castillo anal Etapa incorporativa
Etapa incorporativa External genital
External genital Taenia saginata
Taenia saginata External genital
External genital Function of reproductive system
Function of reproductive system Structura testiculului
Structura testiculului Sigmund freud's psychosexual development
Sigmund freud's psychosexual development