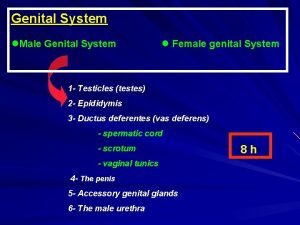
Female Genital Anatomy and Female Genital MutilationCutting Development
- Slides: 13
Female Genital Anatomy and Female Genital Mutilation/Cutting ‘Development Issues – A course for Transition Year’ Gender
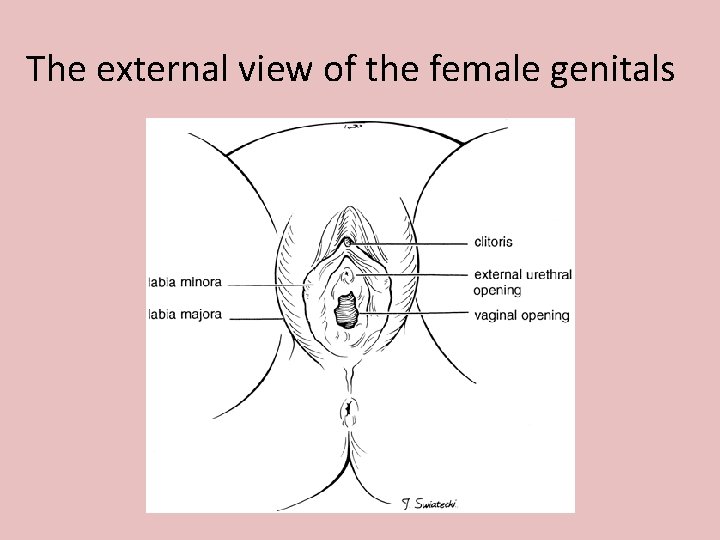
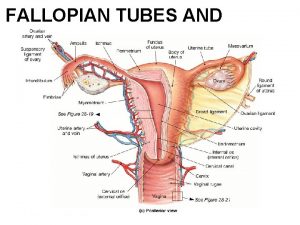
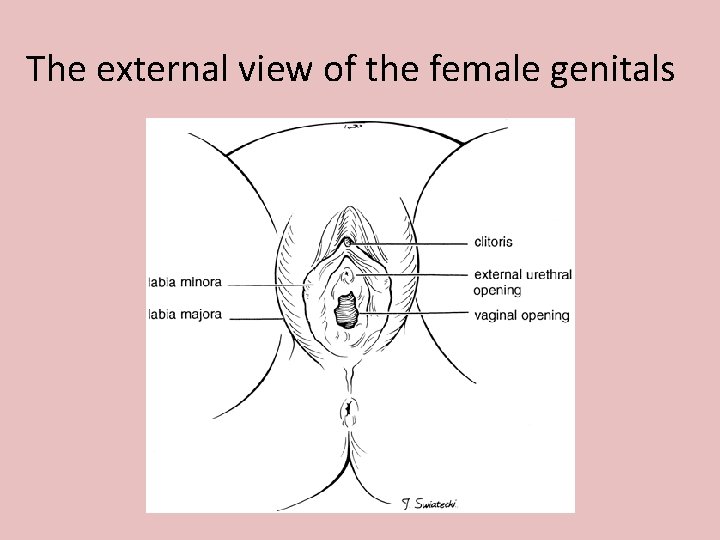
The external view of the female genitals
What is FGM/C? All procedures which involve the partial or total removal of the external genitalia or injury to the female genital organs whether for cultural or any other non-medical reasons The World Health Organisation
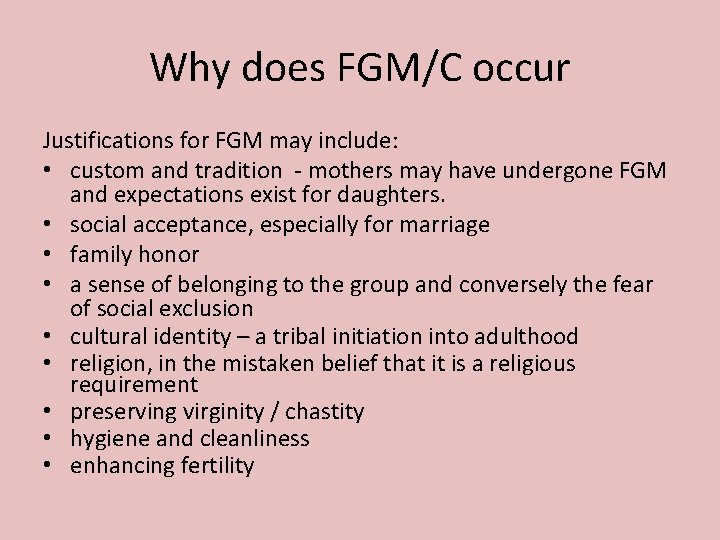
Why does FGM/C occur Justifications for FGM may include: • custom and tradition - mothers may have undergone FGM and expectations exist for daughters. • social acceptance, especially for marriage • family honor • a sense of belonging to the group and conversely the fear of social exclusion • cultural identity – a tribal initiation into adulthood • religion, in the mistaken belief that it is a religious requirement • preserving virginity / chastity • hygiene and cleanliness • enhancing fertility
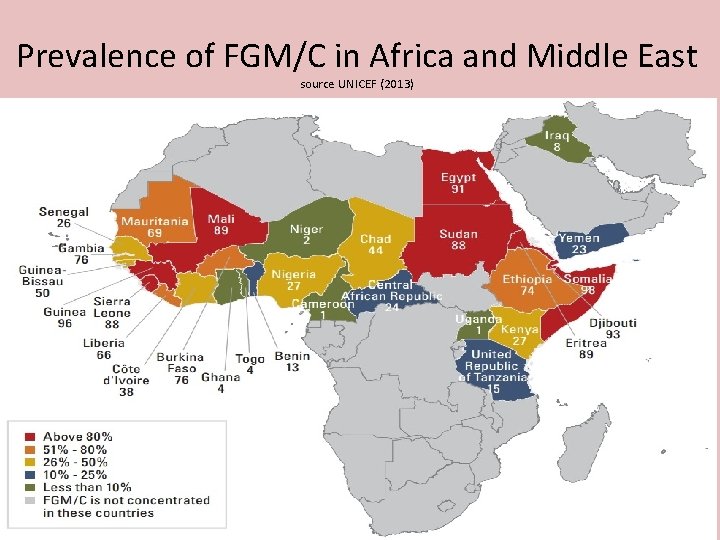
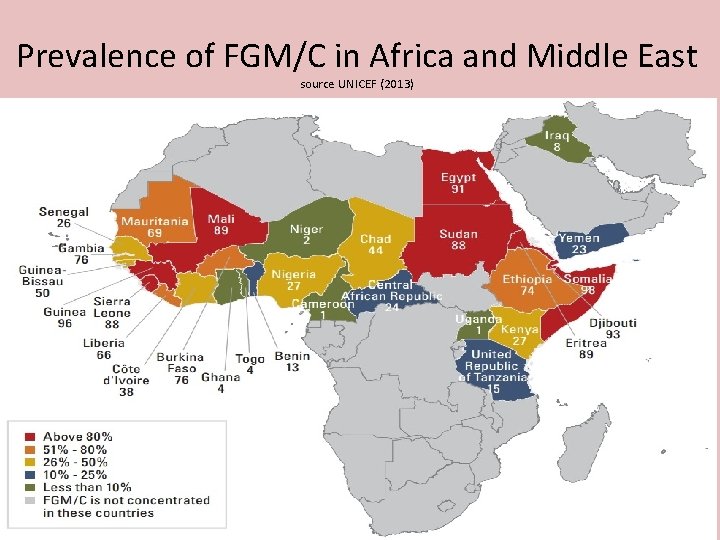
Prevalence of FGM/C in Africa and Middle East source UNICEF (2013)
Who performs FGM/C • In cultures where FGM is the custom, the operation is performed by traditional excisors, commonly elderly women in the community specially designated this task. FGM is sometimes performed by traditional birth attendance and village barbers. • Implements used are sometimes blunt razor blades or knives. • Often these are not sterilized.
Types of FGM/C • There are 4 known types of FGM/C • FGM may be performed between the age of a few days through to adolescence or young motherhood. • Six to ten years is a commonly selected age. • The procedure is often performed in poor light, without anaesthesia and using blades, knives, broken glass or non-surgical instruments that are often shared. • Girls have to be forcibly restrained. • Following more extensive forms of FGM, the legs may be tied together for many days to aid healing.
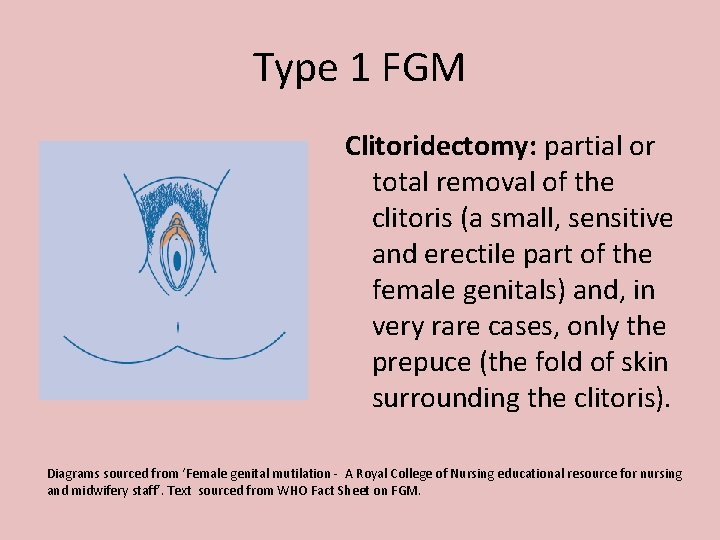
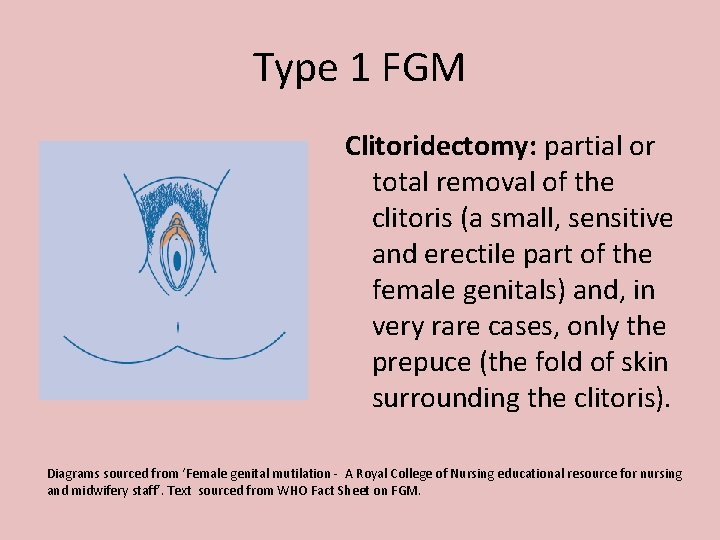
Type 1 FGM Clitoridectomy: partial or total removal of the clitoris (a small, sensitive and erectile part of the female genitals) and, in very rare cases, only the prepuce (the fold of skin surrounding the clitoris). Diagrams sourced from ‘Female genital mutilation - A Royal College of Nursing educational resource for nursing and midwifery staff’. Text sourced from WHO Fact Sheet on FGM.
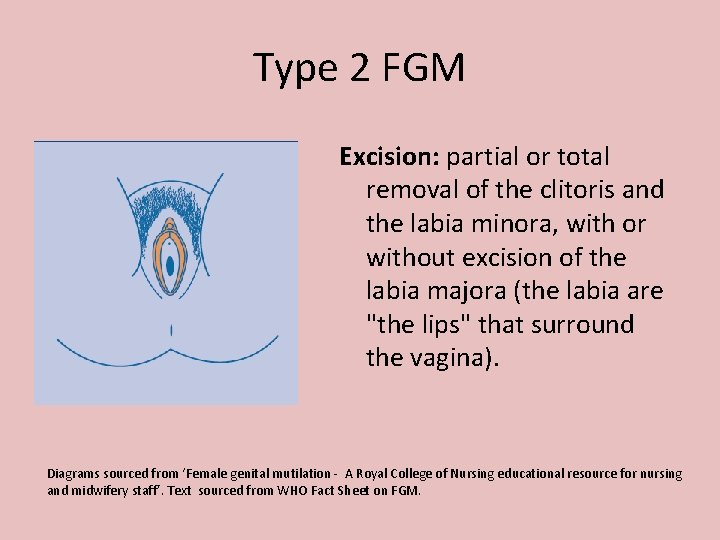
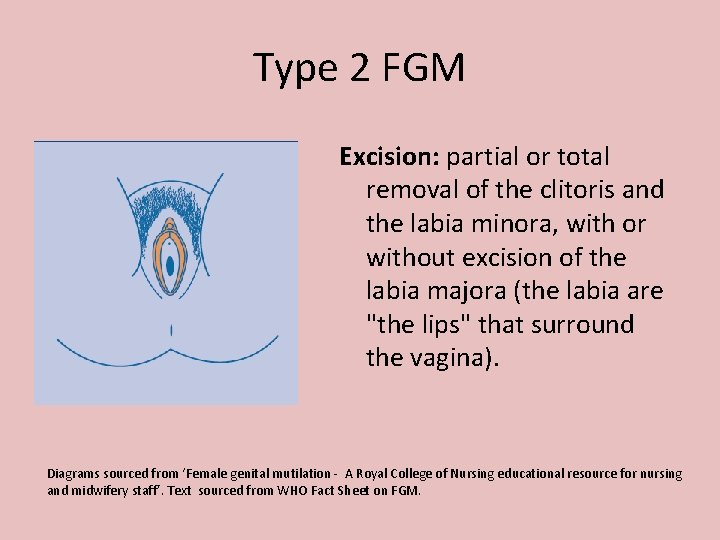
Type 2 FGM Excision: partial or total removal of the clitoris and the labia minora, with or without excision of the labia majora (the labia are "the lips" that surround the vagina). Diagrams sourced from ‘Female genital mutilation - A Royal College of Nursing educational resource for nursing and midwifery staff’. Text sourced from WHO Fact Sheet on FGM.
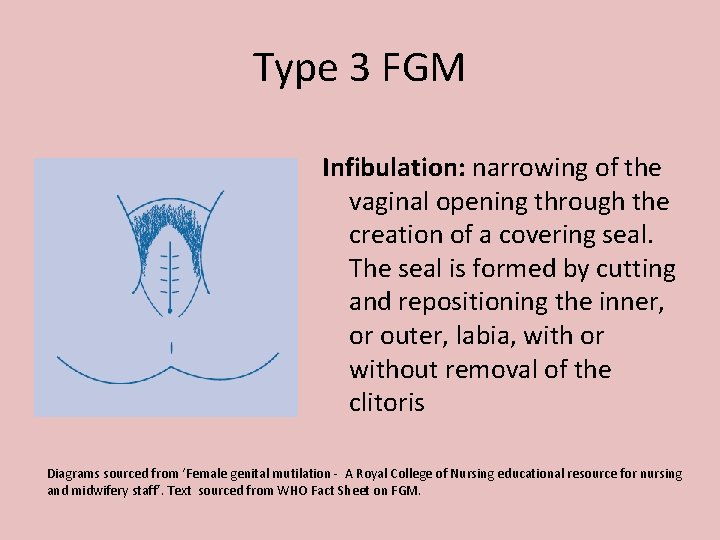
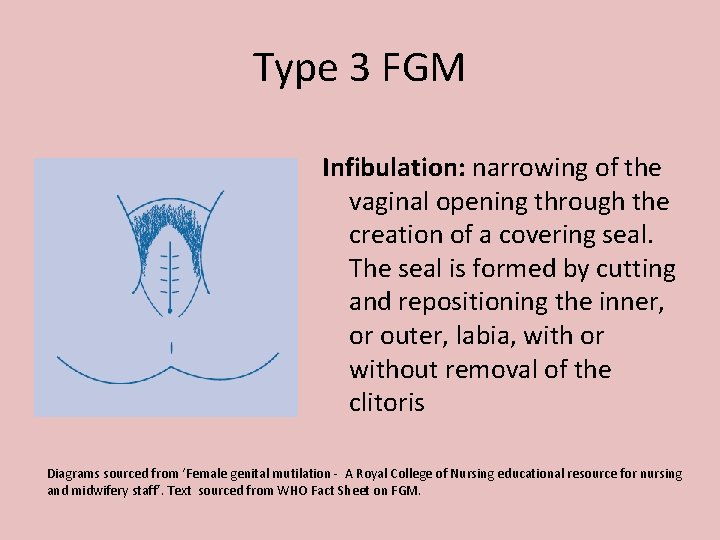
Type 3 FGM Infibulation: narrowing of the vaginal opening through the creation of a covering seal. The seal is formed by cutting and repositioning the inner, or outer, labia, with or without removal of the clitoris Diagrams sourced from ‘Female genital mutilation - A Royal College of Nursing educational resource for nursing and midwifery staff’. Text sourced from WHO Fact Sheet on FGM.
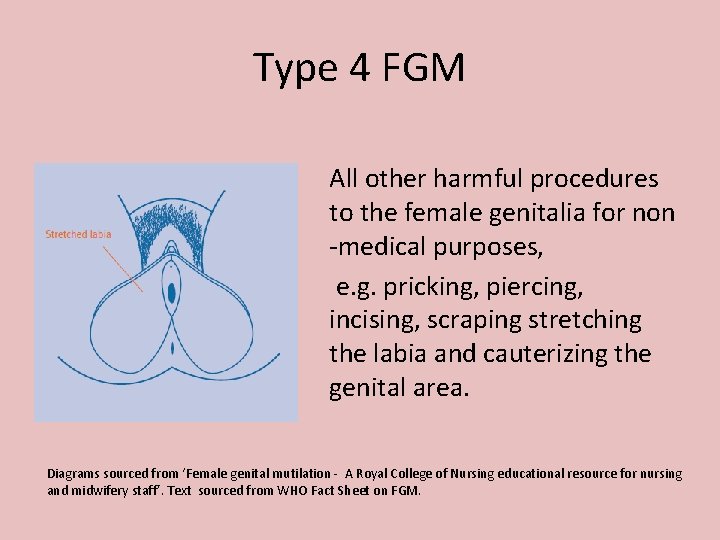
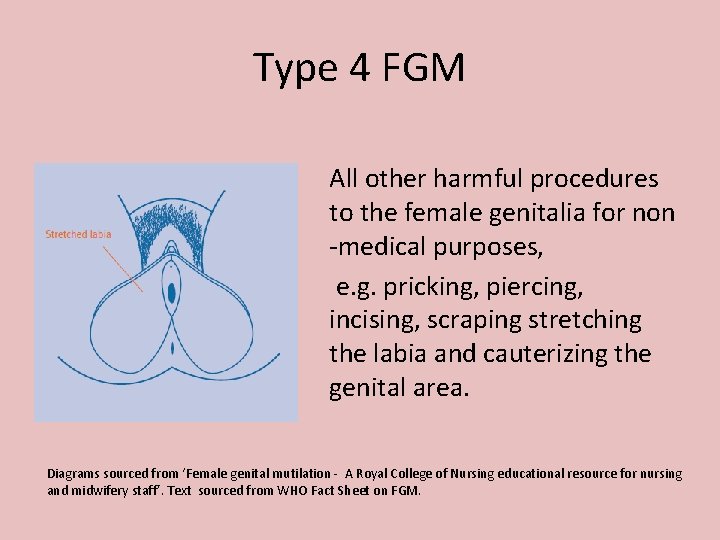
Type 4 FGM All other harmful procedures to the female genitalia for non -medical purposes, e. g. pricking, piercing, incising, scraping stretching the labia and cauterizing the genital area. Diagrams sourced from ‘Female genital mutilation - A Royal College of Nursing educational resource for nursing and midwifery staff’. Text sourced from WHO Fact Sheet on FGM.
Short term risks from procedure Severe pain, shock Hemorrhaging (sometimes to death) abscesses septicemia gangrene tetanus emotional depression, chronic anxiety risk of bacterial or HIV infection due to instruments being re-used without sterilisation • Urinary tract infections • •
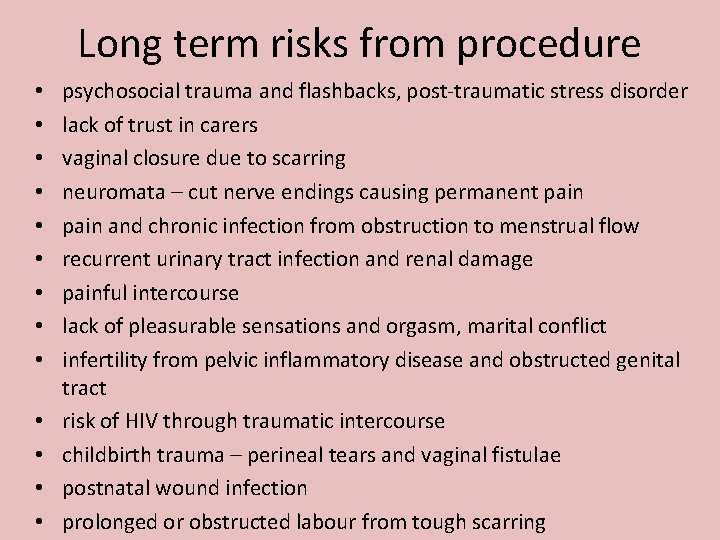
Long term risks from procedure • • • • psychosocial trauma and flashbacks, post-traumatic stress disorder lack of trust in carers vaginal closure due to scarring neuromata – cut nerve endings causing permanent pain and chronic infection from obstruction to menstrual flow recurrent urinary tract infection and renal damage painful intercourse lack of pleasurable sensations and orgasm, marital conflict infertility from pelvic inflammatory disease and obstructed genital tract risk of HIV through traumatic intercourse childbirth trauma – perineal tears and vaginal fistulae postnatal wound infection prolonged or obstructed labour from tough scarring
 Anteversion of uterus
Anteversion of uterus Female anus real
Female anus real Defence mechanism of female genital tract
Defence mechanism of female genital tract Female genital mutilation
Female genital mutilation Mutilation meaning
Mutilation meaning Internal genital organs female
Internal genital organs female What is prostate gland
What is prostate gland Gandotropin
Gandotropin Girls body part name
Girls body part name Positive deep ring occlusion test
Positive deep ring occlusion test Cow reproductive system
Cow reproductive system What kingdom is a squid in
What kingdom is a squid in Female reproductive system anatomy
Female reproductive system anatomy Structure of female
Structure of female