Chapter 33 Shock and Multisystem Organ Dysfunction Syndrome
![Management • Optimize cardiac output and preload (left ventricular enddiastolic pressure [LVEDP]) of 14 Management • Optimize cardiac output and preload (left ventricular enddiastolic pressure [LVEDP]) of 14](https://slidetodoc.com/presentation_image_h2/4744aad139151fb9152d3d8f0832e4bb/image-15.jpg)
- Slides: 33
Chapter 33 Shock and Multisystem Organ Dysfunction Syndrome Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Shock • Hypoperfusion, hypercoagulability, and activation of the inflammatory response • In hypoperfused states, the lack of sufficient oxygen causes the cells to convert to anaerobic metabolism. • If oxygen continues to be insufficient to meet cellular demands for energy, cell death ensues. • As more cells die, tissues and organs become progressively dysfunctional and eventually end-organ failure ensues. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Three Stages of Shock • Stage 1. The body activates compensatory mechanisms in an effort to maintain circulatory volume, blood pressure, and cardiac output. – Normal vital signs and cerebral perfusion, and the shock state often goes unrecognized. • Stage 2. Compensatory mechanisms begin to fail, metabolic and circulatory derangements become more pronounced, and the inflammatory and immune responses may become fully activated. – Signs of dysfunction in one or more organs may become apparent. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Three Stages of Shock (cont. ) • Stage 3. In the final, irreversible stage, cellular and tissue injury are so severe that the patient’s life is not sustainable even if metabolic, circulatory, and inflammatory derangements are corrected. – Full-blown multisystem organ dysfunction syndrome (MODS) may become evident. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • Compensatory mechanisms in response to shock states result in which of the following? – A. Decreased urine output – B. Vasodilation of blood vessels – C. Decreased heart rate – D. Decreased cardiac output Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer • A. Decreased urine output • Rationale: In response to decreased venous return or decreased renal blood flow, compensatory mechanisms are initiated to maintain cardiovascular function and maintain blood volume. To maintain blood volume, the renin-angiotensin-aldosterone system is initiated for the kidneys to retain sodium and water. The net result is decreased urine output. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Hypovolemic Shock • Result of inadequate circulating blood volume, caused by sudden blood loss, severe dehydration, or injuries that cause significant fluid shifts from the intravascular space to the interstitial space (e. g. , burns) Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
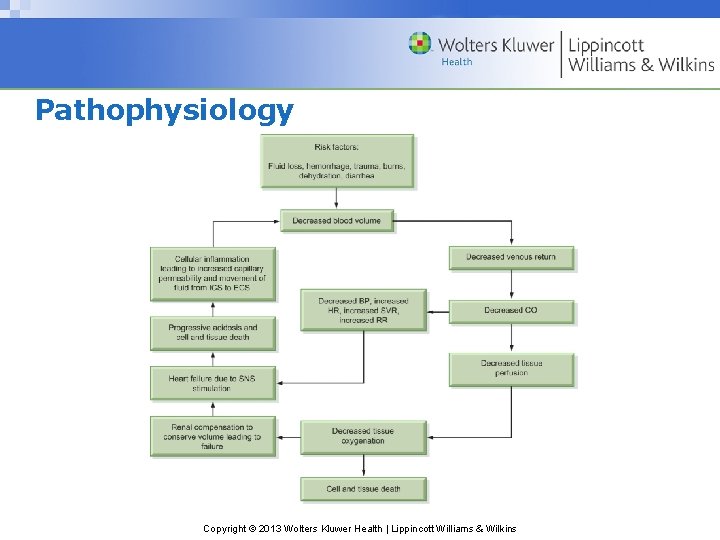
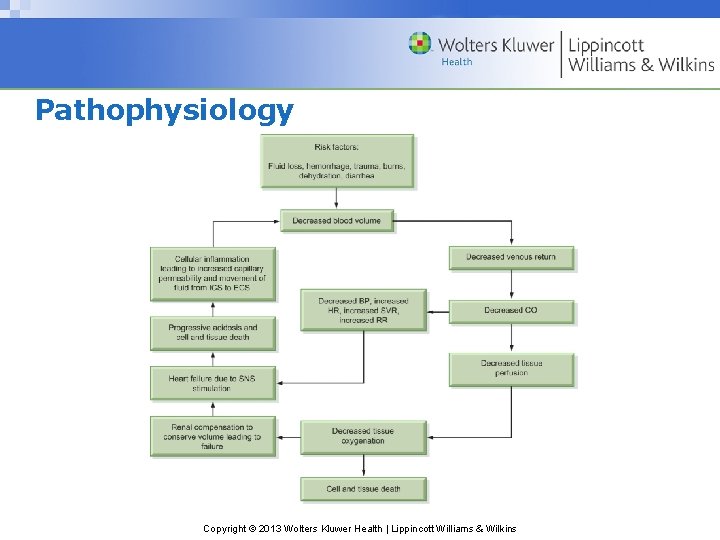
Pathophysiology Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Assessment • History • Monitor vital signs. – Tachycardia, hypotension • Monitor respiratory status. • Use of nonsteroidal anti-inflammatory agents (NSAIDs), which can cause upper gastrointestinal bleeding • Clinical findings are related to the severity and acuity of volume loss. • Serum lactate, arterial p. H, serial hemoglobin, and hematocrit and coagulation Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Management • Volume administration • Large-bore 16 -gauge or larger for rapid infusion • Fluids are warmed during infusion to limit the negative effects of hypothermia. • Isotonic crystalloid solutions • Blood products and other colloid solutions if blood loss is the primary cause Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • Which of the following is not a common pathophysiological manifestation seen in patients with hypovolemic shock? – A. Altered mentation – B. Rapid and deep respirations – C. Cool and clammy skin – D. Bradycardia Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer • D. Bradycardia • Rationale: Patients with hypovolemic shock have signs and symptoms caused by poor organ perfusion. This includes tachycardia due to activation of the sympathetic nervous system; altered mentation, ranging from lethargy to unresponsiveness; rapid and deep respirations, which gradually become labored and shallow as the patient’s condition deteriorates; and cool, clammy skin. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Cardiogenic Shock • Loss of ventricular contractility decreases stroke volume and cardiac output. • Neuroendocrine compensatory mechanisms are activated. • Increasing preload through retention of sodium and water • Increasing afterload (systemic vascular resistance) through vasoconstriction • These compensatory mechanisms further impair cardiac output, exacerbating the problem. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Assessment • Develops within a few hours after the onset of myocardial infarction symptoms • Close monitoring for progressive hemodynamic compromise and clinical deterioration • Systolic blood pressure <90 mm Hg • Mean arterial pressure (MAP) <70 mm Hg • Cardiac index <2. 2 L/minute/m 2 • Pulmonary artery occlusion pressure (PAOP) >18 mm Hg Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
![Management Optimize cardiac output and preload left ventricular enddiastolic pressure LVEDP of 14 Management • Optimize cardiac output and preload (left ventricular enddiastolic pressure [LVEDP]) of 14](https://slidetodoc.com/presentation_image_h2/4744aad139151fb9152d3d8f0832e4bb/image-15.jpg)
Management • Optimize cardiac output and preload (left ventricular enddiastolic pressure [LVEDP]) of 14 to 18 mm Hg. • Pharmacological agents to increase contractility • Antidysrhythmic agents, cardioversion, or pacing can help to restore a stable heart rhythm and enhance cardiac output. • Potassium, calcium, and magnesium replacement Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Management (cont. ) • Decreasing left ventricular workload • Pharmacotherapy: vasodilators may be administered to reduce SVR and LVEDP. • Intra-aortic balloon pump (IABP) or left ventricular assist device • Mechanical ventilation may be necessary to improve oxygen delivery to the tissues. • Scheduling physical care to ensure periods of rest Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Distributive Shock • The mechanism underlying all distributive shock states is vasodilation that causes decreased venous return. • Distributive shock states include – Neurogenic shock – Anaphylactic shock – Septic shock • In neurogenic shock, vasodilation results from a loss of sympathetic innervation to the blood vessels. • In anaphylactic shock and septic shock, vasodilation results from the presence of vasodilating substances in the blood. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Neurogenic Shock • Neurogenic shock results from loss or disruption of sympathetic tone most often due to severe cervical or upper thoracic spinal cord injury. – Signs and symptoms include hypotension, severe bradycardia, and warm, dry skin. – Volume resuscitation – Vasoconstrictors may be used. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Anaphylactic Shock • Anaphylaxis is an allergic reaction that evokes a lifethreatening hypersensitivity response. • Ig. E-mediated anaphylaxis occurs as a result of the immune response to a specific antigen after being exposed and forming antibodies. • Non-Ig. E responses (anaphylactoid reactions) occur without the presence of Ig. E antibodies and can occur the first time the person is exposed to the antigen. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Anaphylactic Shock (cont. ) • WBCs secrete chemical mediators causing systemic vasodilation. • Increased capillary permeability • Bronchoconstriction, coronary vasoconstriction, and urticaria • Arterial vasodilation causes maldistribution of blood volume to tissues, and venous dilation decreases preload, thus decreasing cardiac output. • Increased capillary permeability • Death due to circulatory collapse or extreme bronchoconstriction can occur within minutes or hours. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Clinical Manifestations of Anaphylaxis • Generalized erythema • Stridor • Urticaria/pruritus • Laryngeal edema • Anxiety and restlessness • Bronchoconstriction with stridor • Dyspnea/wheezing • Chest tightness • Hypotension • Angioedema Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Assessment • History of allergies is used to avoid known allergens and is the best way to prevent anaphylactic shock. • Anaphylactic shock may occur without any known predisposing factors. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Management • Remove the offending antigen. • Reverse effects of chemical mediators. • Restore adequate tissue perfusion. • Oxygen • Subcutaneous or IV antihistamine • Epinephrine • Corticosteroids, bronchodilators • Mechanical ventilation is required. • Vasoconstrictors and positive inotropic agents Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • What is the initial therapy of choice for the treatment of anaphylactic shock? – A. Epinephrine – B. Rapid infusion of normal saline – C. Dobutamine – D. Norepinephrine Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer • A. Epinephrine • Rationale: Epinephrine is given to reverse the vasodilation and bronchoconstriction. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Septic Shock • Complex interactions among invading microorganisms and the immune system, the inflammatory system, and the coagulation system • Proinflammatory cytokines are released. • Activation of the immune response, complement system, and coagulation system • Increased vascular permeability • To balance the proinflammatory response, antiinflammatory cytokines are released causing an “out of control” inflammatory response. • Cardiovascular, pulmonary, and hematologic alterations Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Sepsis • The systemic response to known infection, manifested by two or more of the following conditions as a result of infection: – Temperature greater than 100. 4°F (38°C) or less than 96. 8°F (36°C) – Heart rate greater than 90 beats/minute – Respiratory rate greater than 20 breaths/minute or arterial carbon dioxide tension Pa. CO 2 less than 32 mm Hg – White blood cell (WBC) count greater than 12, 000 cells/mm 3 or less than 4, 000 cells/mm 3 OR more than 10% immature (band) forms Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Assessment • Early signs of changes in mental status, an increased respiratory rate, and either hyper- or hypothermia • Lab studies • Cultures, (CBC), SMA-7, ABGs, lactate level, end-tidal carbon dioxide monitoring • Pulmonary artery catheterization with mixed venous oxygen (Sv. O 2) monitoring • CT, chest and abdominal x-rays Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Management • Identify and treat the cause. • Volume repletion • Mechanical ventilation • Maintain adequate cardiac output. • Correct coagulopathies • Nutritional support Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Multiorgan System Failure (MODS) • The pathophysiology of similar to sepsis and SIRS • Endothelial injury, inflammatory mediators, disturbed hemostasis, and microcirculatory failure • Tissue hypoxia caused by microvascular thromboses contributes to MODS. • Typically, the first organs to manifest signs of dysfunction are the lungs and kidneys. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Assessment and Management • Identifying SIRS and signs and symptoms of organ failure • Multiple scoring systems exist to determine the extent of MODS, including the Sepsis-Related Organ Failure Assessment (SOFA) • Treatment is supportive and directed at specific organ systems. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • Which of the following classifications best describes septic shock? – A. Hypovolemic shock – B. Cardiogenic shock – C. Vasodilatory shock – D. Anaphylactic shock Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer • C. Vasodilatory shock • Rationale: Widespread vasodilation and maldistribution of blood flow associated with septic shock result in decreased venous return to the heart, resulting in a shock state. Hypovolemic shock is caused by dehydration or hemorrhage. Cardiogenic shock occurs when the heart fails to function as a pump as a result of myocardial infarction, abnormal heart rate or rhythm, or impaired diastolic filling. Anaphylactic shock occurs as a result of an antibody-antigen reaction. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins