Chapter 13 Neurodevelopmental and Neurocognitive Disorders Outline Introduction

- Slides: 98

Chapter 13 Neurodevelopmental and Neurocognitive Disorders
Outline • Introduction • Neurodevelopmental Disorders – ADHD – Specific Learning Disorder – Autism Spectrum Disorders – Intellectual Disability • Neurocognitive Disorders – Delirium – Major and Minor Neurocognitive Disorders
Focus Questions o What are the defining features of ADHD? o What is a specific learning disorder? o What are the major features of autism spectrum disorders? o How is intellectual disability defined? o What are the defining features of neurocognitive disorders? o What are some of the causes of neurocognitive disorders?
Nature of Developmental Psychopathology: An Overview • Normal vs. abnormal development – Consider age and environment of child • Developmental psychopathology – Study of how disorders arise and change with time – Disruption of early skills can affect later development
Neurodevelopmental Disorders • Diagnosed first in infancy, childhood, or adolescence • Include the following: – Attention deficit hyperactivity disorder (ADHD) – Specific learning disorder – Autism spectrum disorder – Intellectual Disability – Communication and Motor Disorders
Communication and Motor Disorders, Part 1 • Childhood Onset Fluency Disorder – Speech difficulty that may include repeated syllabus (stuttering), pauses or substituting words that are easier to pronounce • Language Disorder – Limited speech in all situations; understanding of speech is normal and problem may self-correct
Communication and Motor Disorders, Part 2 • Social (Pragmatic) Communication Disorder – Difficulty with social aspects of communication (e. g. , dominating conversations, switching topics excessively), but lacks other features of autism spectrum disorder (e. g. , restrictive behaviors and interests) • Tourette’s Disorder – Involuntary motor movements and/or vocalizations, which may include obscenities
Attention Deficit Hyperactivity Disorder (ADHD), Part 1 • Nature of ADHD – Central features – inattention, overactivity, and impulsivity – Associated with numerous impairments • Behavioral • Cognitive • Social and academic problems
Attention Deficit Hyperactivity Disorder (ADHD), Part 2 • DSM-5 symptom types – Predominantly inattentive presentation – Predominantly hyperactive/impulsive presentation – Combined presentation
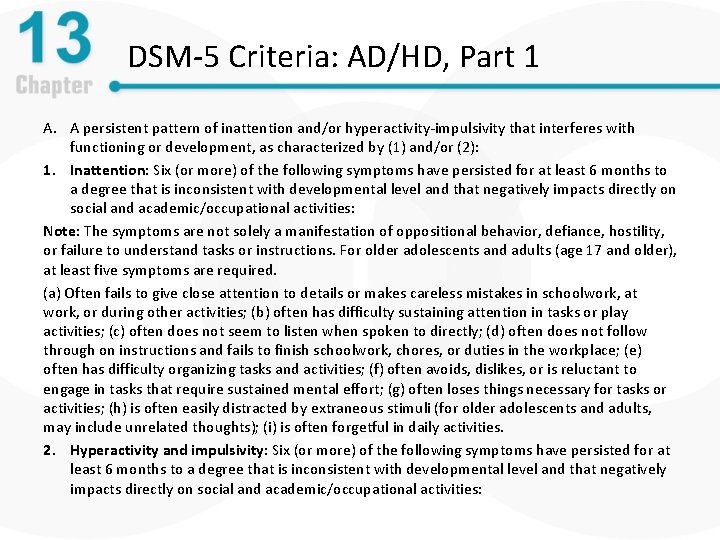
DSM-5 Criteria: AD/HD, Part 1 A. A persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development, as characterized by (1) and/or (2): 1. Inattention: Six (or more) of the following symptoms have persisted for at least 6 months to a degree that is inconsistent with developmental level and that negatively impacts directly on social and academic/occupational activities: Note: The symptoms are not solely a manifestation of oppositional behavior, defiance, hostility, or failure to understand tasks or instructions. For older adolescents and adults (age 17 and older), at least five symptoms are required. (a) Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or during other activities; (b) often has difficulty sustaining attention in tasks or play activities; (c) often does not seem to listen when spoken to directly; (d) often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace; (e) often has difficulty organizing tasks and activities; (f) often avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort; (g) often loses things necessary for tasks or activities; (h) is often easily distracted by extraneous stimuli (for older adolescents and adults, may include unrelated thoughts); (i) is often forgetful in daily activities. 2. Hyperactivity and impulsivity: Six (or more) of the following symptoms have persisted for at least 6 months to a degree that is inconsistent with developmental level and that negatively impacts directly on social and academic/occupational activities:
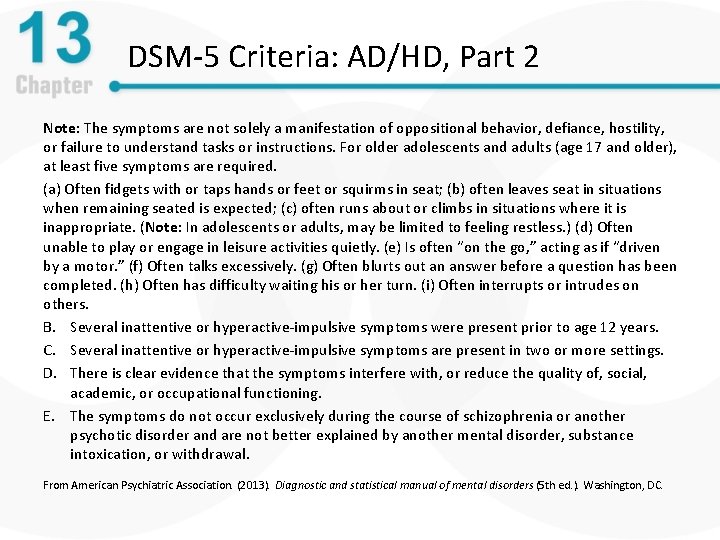
DSM-5 Criteria: AD/HD, Part 2 Note: The symptoms are not solely a manifestation of oppositional behavior, defiance, hostility, or failure to understand tasks or instructions. For older adolescents and adults (age 17 and older), at least five symptoms are required. (a) Often fidgets with or taps hands or feet or squirms in seat; (b) often leaves seat in situations when remaining seated is expected; (c) often runs about or climbs in situations where it is inappropriate. (Note: In adolescents or adults, may be limited to feeling restless. ) (d) Often unable to play or engage in leisure activities quietly. (e) Is often “on the go, ” acting as if “driven by a motor. ” (f) Often talks excessively. (g) Often blurts out an answer before a question has been completed. (h) Often has difficulty waiting his or her turn. (i) Often interrupts or intrudes on others. B. Several inattentive or hyperactive-impulsive symptoms were present prior to age 12 years. C. Several inattentive or hyperactive-impulsive symptoms are present in two or more settings. D. There is clear evidence that the symptoms interfere with, or reduce the quality of, social, academic, or occupational functioning. E. The symptoms do not occur exclusively during the course of schizophrenia or another psychotic disorder and are not better explained by another mental disorder, substance intoxication, or withdrawal. From American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5 th ed. ). Washington, DC.
ADHD: Facts and Statistics • Prevalence – Occurs in approximately 5% of school-aged children – Symptoms are usually present around age three or four – Children with ADHD have similar problems as adults • Gender differences: Boys outnumber girls 3: 1 • Cultural factors – ADHD most commonly diagnosed in the United States, although prevalence appears fairly constant worldwide
The Causes of ADHD: Biological Contributions, Part 1 • Genetic contributions – ADHD seems to run in families – DAT 1 – dopamine transporter gene has been implicated • Some ADHD drugs work by inhibiting DAT 1
The Causes of ADHD: Biological Contributions, Part 2 • Neurobiological correlates of ADHD – Smaller brain volume – Inactivity of the frontal cortex and basal ganglia – Abnormal frontal lobe development and functioning
The Causes of ADHD: Biological Contributions, Part 3 • The role of toxins – Food additives (e. g. , dyes, pesticides) may play very small role in hyperactive/impulsive behavior among children – Maternal smoking increases risk
The Causes of ADHD: Psychosocial Contributions • Psychosocial factors – ADHD children are often viewed negatively by others > Frequent negative feedback from peers and adults • Peer rejection and resulting social isolation • Such factors foster low self-esteem
Biological Treatment of ADHD, Part 1 • Goal of biological treatments – To reduce impulsivity and hyperactivity and to improve attention • Stimulant medications – Currently prescribed for approximately 4 million American children – Low doses of stimulants improve focusing abilities – Examples include Ritalin, Dexedrine, Adderall – Problem: May increase risk for later substance abuse
Biological Treatment of ADHD, Part 2 • Other medications with more limited efficacy – Imipramine and clonidine (antihypertensive) • Genes affect individuals’ response to meds – Some trial and error is necessary • Effects of medications – Improve compliance, decrease negative behaviors – Do not affect learning/academics directly – Benefits are not lasting following discontinuation
Behavioral and Combined Treatment of ADHD • Behavioral treatment – Reinforcement programs • To increase appropriate behaviors • Decrease inappropriate behaviors – May also involve parent training • Combined bio-psycho-social treatments – Often recommended – May be superior to medication or behavioral treatments alone, but more research is needed
Specific Learning Disorders: An Overview • Scope of learning disorders – Academic problems in reading, mathematics, and/or writing – Performance substantially below expected levels based on age and/or demonstrated capacity – Problems persist for 6+ months despite targeted intervention
Specific Learning Disorder: Types, Part 1 • With impairment in reading, may include: – Word reading accuracy – Reading rate or fluency – Reading comprehension • With impairment in written expression, may include: – Spelling accuracy – Grammar punctuation and accuracy – Clarity/organization of written expression
Specific Learning Disorder: Types, Part 2 • With impairment in mathematics, may include: – Number sense – Memorization of arithmetic facts – Accurate or fluent calculation – Accurate math reasoning
DSM-5 Criteria: Specific Learning Disorder, Part 1 A. Difficulty learning and using academic skills, as indicated by the presence of at least one of the following symptoms that have persisted for at least 6 months, despite the provision of interventions that target those difficulties: (1) Inaccurate or slow and effortful word reading; (2) difficulty understanding the meaning of what is read; (3) difficulties with spelling; (4) difficulties with written expression; (5) difficulties mastering number sense, number facts, or calculation; (6) difficulties with mathematical reasoning (e. g. , has severe difficulty applying mathematical concepts, facts, or procedures to solve quantitative problems) B. The affected academic skills are substantially and quantifiably below those expected for the individual’s chronological age and cause significant interference with academic or occupational performance, or with activities of daily living, as confirmed by individually administered standardized achievement measures and comprehensive clinical assessment. For individuals age 17 years and older, a documented history of impairing learning difficulties may be substituted for the standardized assessment.
DSM-5 Criteria: Specific Learning Disorder, Part 2 C. The learning difficulties begin during school-age years but may not become fully manifest until the demands for those affected academic skills exceed the individual’s limited capacities (e. g. , as in timed tests, reading, or writing lengthy complex reports for a tight deadline, excessively heavy academic loads). D. The learning difficulties are not better accounted for by intellectual disabilities, uncorrected visual or auditory acuity, other mental or neurological disorders, psychosocial adversity, lack of proficiency in the language of academic instruction, or inadequate educational instruction. Note: The four diagnostic criteria are to be met based on clinical synthesis of the individual’s history (developmental, medical, family, educational), school reports, and psycho-educational assessment. From American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5 th ed. ). Washington, DC.
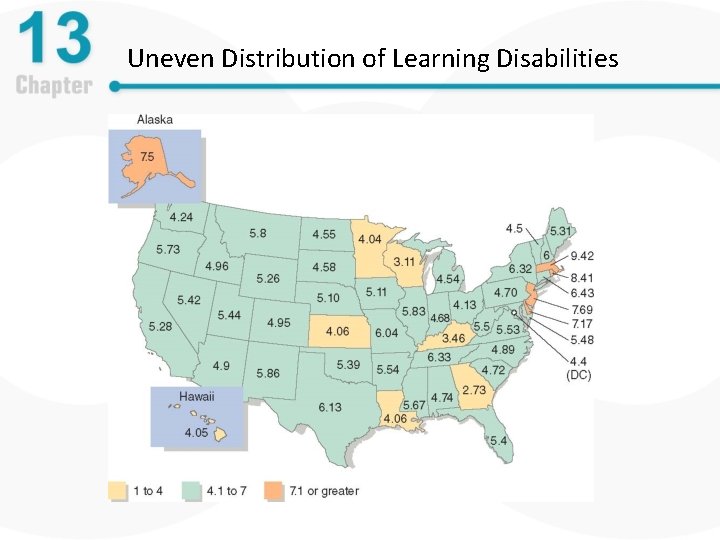
Specific Learning Disorder: Statistics • Prevalence of learning disorders – Six million children have been diagnosed in the United States – Highest rate of diagnosis in wealthier regions, but children with low SES more likely to have difficulties – Reading difficulties most common, affect 4 -10% of the general population – School experience tends to be generally negative
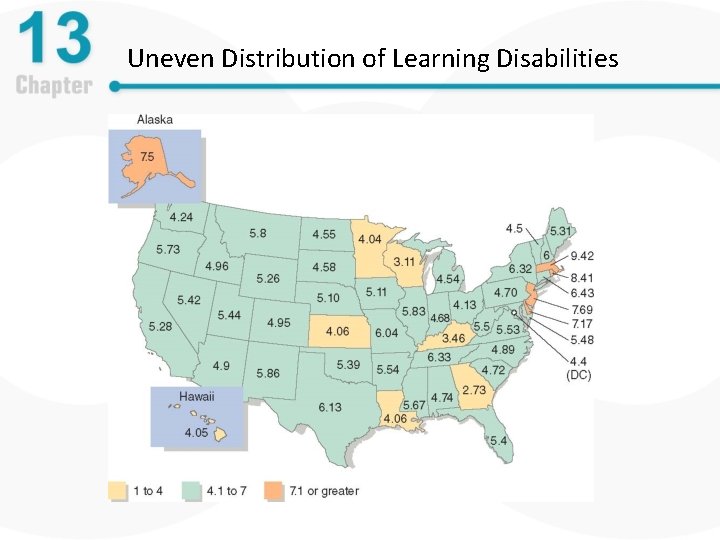
Uneven Distribution of Learning Disabilities
Biological and Psychosocial Causes of Specific Learning Disorder • Genetic and neurobiological contributions – Learning disorders run in families, but specific difficulties are not inherited – Evidence for subtle neurological difficulties is mounting (e. g. , decreased functioning of areas responsible for word recognition) – Overall, contributions are unclear • Psychosocial contributions are likely important
Treatment of Specific Learning Disorder • Requires intense educational interventions – Remediation of basic processing problems – Improvement of cognitive skills – Targeting skills to compensate for problem areas • Data support behavioral educational interventions
Autism Spectrum Disorder, Part 1 • Problems occur in language, socialization, and cognition • Pervasive – problems span many life areas • Two main areas of impairment: – Communication and social interaction • 25% don’t acquire effective speech – Restricted, repetitive patterns of behavior, interests, or activities • Need to maintain “sameness” - high level of consistency in activities or experience
Autism Spectrum Disorder, Part 2 • Label is new to DSM-5 • Encompasses several disorders previously classified as “pervasive developmental disorders”, • Including: – Autistic disorder – Asperger’s disorder – Childhood disintegrative disorder – Rett syndrome
DSM-5 Criteria: Autism Spectrum Disorder, Part 1 A. Persistent deficits in social communication and social interaction across multiple contexts, as manifested by the following, currently or by history: (1) Deficits in social–emotional reciprocity, ranging, for example, from abnormal social approach and failure of normal backand-forth conversation, to reduced sharing of interests, emotions, and affect, to failure to initiate or respond to social interactions. (2)Deficits in nonverbal communicative behaviors used for social interaction, ranging, for example, from poorly integrated verbal and nonverbal communication, to abnormalities in eye contact and body language or deficits in understanding and use of gestures, to a total lack of facial expressions and nonverbal communication. (3) Deficits in developing, maintaining, and understanding relationships, ranging, for example, from difficulties adjusting behavior to suit various social contexts, to difficulties in sharing imaginative play and in making friends, to absence of interest in peers. B. Restricted, repetitive patterns of behavior, interests, or activities, as manifested by at least two of the following, currently or by history: (1) stereotyped or repetitive motor movements, use of objects or, speech; (2) insistence on sameness, inflexible adherence to routines, or ritualized patterns of verbal or nonverbal behavior; (3) highly restricted, fixated interests that are abnormal in intensity or focus; (4) hyper- or hyporeactivity to sensory input or unusual interest in sensory aspects of the environment
DSM-5 Criteria: Autism Spectrum Disorder, Part 2 C. D. E. Symptoms must be present in the early developmental period, but they may not become fully manifest until social demands exceed limited capacities, or they may be masked by learned strategies in later life. Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning. The disturbances are not better explained by intellectual disability (intellectual developmental disorder) or global developmental delay. Intellectual disability and autism spectrum disorder frequently co-occur; to make comorbid diagnoses of autism spectrum disorder and intellectual disability, social communication should be below that expected for general developmental level. From American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5 th ed. ). Washington, DC.
Autism Spectrum Disorder: Prevalence • 1 in 50 school-aged children meet criteria • More commonly diagnosed in males • IQ interaction – 38% show intellectual disabilities • Occurs worldwide
Psychological and Social Dimensions • Historical views – Failed parenting • Perfectionistic, cold, and aloof • High socioeconomic status • Higher IQs – Lack of self-awareness – Behavioral correlates • Echolalia (immediate, delayed, mitigated) • Self-injury
Biological Dimensions, Part 1 • Significant genetic component – Familial component: If have one child with autism, the chance of having a second child with autism is 20% (100 x greater risk than general population) • Numerous genes on several chromosomes involved • Oxytocin receptor genes – Bonding and social memory • Older parents associated with increased risk
Biological Dimensions, Part 2 • Neurobiological influences – Amygdala • Larger size at birth = higher anxiety, fear • Elevated cortisol • Neuronal damage in the amygdala results from high stress, which may affect processing of social situations – Oxytocin • Lower levels
Causes of Autism Spectrum Disorder: Biological • Neurobiological influences – Vaccinations do NOT increase the risk of autism • Mercury in some vaccinations was rumored to increase autism risk • Large scale studies do NOT support this • High rates of vaccinations do NOT increase risk for autism in the community at large • Health risk of not vaccinating is substantial
Treatment of Autism Spectrum Disorder, Parts 1 • Psychosocial treatments – Behavioral approaches • • • Skill building Reduce problem behaviors Communication and language training Increase socialization Naturalistic teaching strategies – Early intervention is critical – may “normalize” the functioning of the developing brain
Treatment of Autism Spectrum Disorder, Part 2 • Biological treatments – Medical intervention has had little positive impact on core dysfunction – Some drugs decrease agitation • Tranquilizers • SSRIs • Indicators of good prognosis – High IQ, good language ability
Treatment of Autism Spectrum Disorder • Integrated treatments – Preferred model: Multidimensional, comprehensive focus • Children offered special education at school focusing on communication • Judicious use of medication in some cases • Families given support too – When older, focus on integrating into the community while maximizing independence
Intellectual Disability, Part 1 • Overview – Below-average intellectual and adaptive functioning – First evident in childhood – Range of impairment varies greatly – Previously called mental retardation
Intellectual Disability, Part 2 • IQ typically below 70 -75 – Previously distinguished different levels of severity; IQ may be as low as under 20 • Previously diagnosed on DSM-IV Axis II – Reserved for conditions that 1) are chronic and pervasive and 2) are likely to influence the presentation of other mental disorders
Intellectual Disability, Part 3 • DSM-5 identifies difficulties in three domains – Conceptual (e. g. , skill deficits in areas such as language, reasoning, knowledge, and memory) – Social (e. g. , problems with social judgment and the ability to make and retain friendships) – Practical (e. g. , difficulties managing personal care or job responsibilities) • Devalued by society
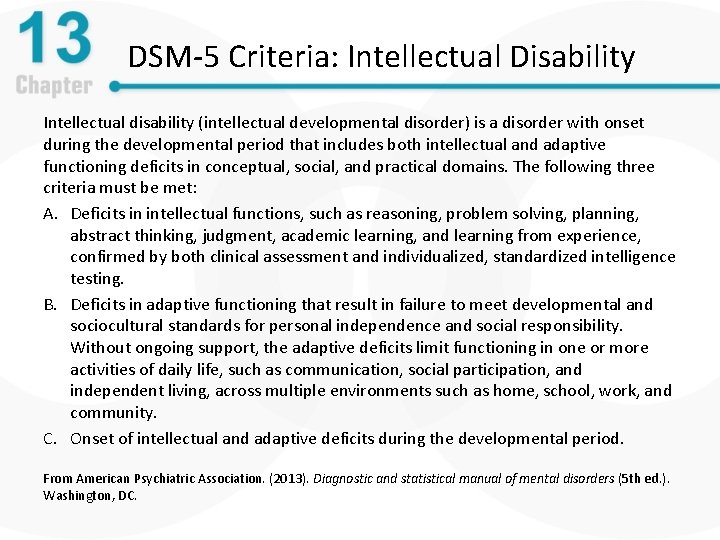
DSM-5 Criteria: Intellectual Disability Intellectual disability (intellectual developmental disorder) is a disorder with onset during the developmental period that includes both intellectual and adaptive functioning deficits in conceptual, social, and practical domains. The following three criteria must be met: A. Deficits in intellectual functions, such as reasoning, problem solving, planning, abstract thinking, judgment, academic learning, and learning from experience, confirmed by both clinical assessment and individualized, standardized intelligence testing. B. Deficits in adaptive functioning that result in failure to meet developmental and sociocultural standards for personal independence and social responsibility. Without ongoing support, the adaptive deficits limit functioning in one or more activities of daily life, such as communication, social participation, and independent living, across multiple environments such as home, school, work, and community. C. Onset of intellectual and adaptive deficits during the developmental period. From American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5 th ed. ). Washington, DC.
Other Classification Systems for Intellectual Disability • American Association of Intellectual and Developmental Disabilities (AAIDD) – Based on assistance required • • Intermittent Limited Extensive Pervasive – Keeps the emphasis on what assistance is needed
Intellectual Disability: Statistics • Prevalence = 2% of general population – 9 in 10 people with ID have mild impairment (IQ 50 -70) • Chronic course • Highly variable individual prognosis – Independence is possible for many individuals with mild impairment when provided with appropriate resources (e. g. , skills training)
Causes of Intellectual Disability, Part 1 • Hundreds of known causes – Environmental (e. g. , neglect) – Prenatal – Perinatal (e. g. , problems with delivery) – Postnatal
Causes of Intellectual Disability, Part 2 • Examples – Fetal alcohol syndrome – Exposure to other illness in the womb – Lack of oxygen (anoxia) during birth – Malnutrition – Head injuries – Childhood abuse
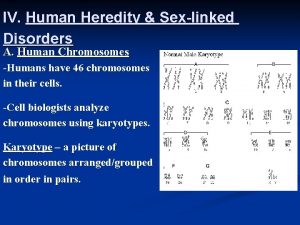
Causes of Intellectual Disability, Part 3 • Genetic influences – Chromosomal disorders (e. g. , Down Syndrome) – Multiple genetic mutations – Single genes can be responsible • Dominant genes less often responsible for ID (because people with ID are less likely to have children) • Recessive genes more often responsible • Most cases of ID have no identified etiology
Causes of Intellectual Disability, Part 4 • Genetic influences – De novo disorders – Lesch-Nyham syndrome • Intellectual disability, symptoms of cerebral palsy, selfinjurious behavior • Recessive allele on the X chromosome > only affects males (females have an additional X chromosome to balance)
Causes of Intellectual Disability, Part 5 • Phenylketonuria (PKU) – Cannot break down phenylalanine, which is found in some foods – Results in ID when the individual eats phenylalanine – Now, test at birth can detect PKU > diets without phenylalanine actually prevent development of intellectual disability and other problems
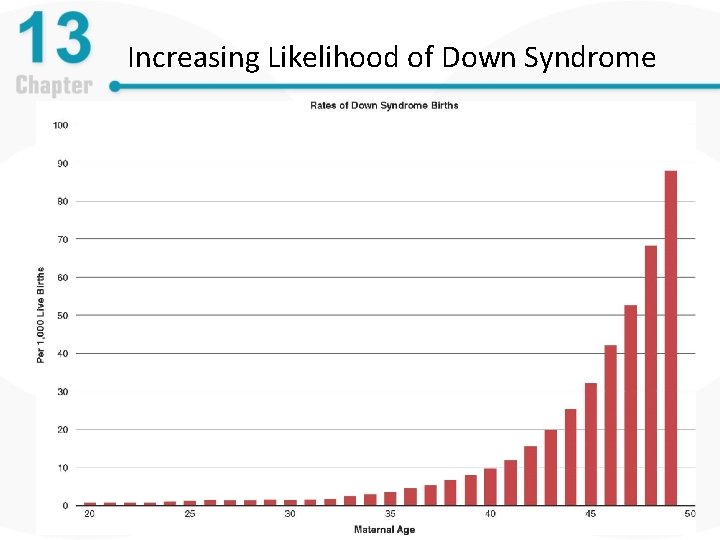
Causes of Intellectual Disability, Part 6 • Chromosomal influences – Down syndrome • Most common chromosomal cause of intellectual disability • Extra 21 st chromosome (Trisomy 21) • Distinctive physical symptoms
Causes of Intellectual Disability, Part 7 • Down syndrome – Higher risk with advanced maternal age – Detectable with some prenatal tests • • • Amniocentesis Chorionic villus sampling (CVS) Mother’s blood tests Tests do not indicate severity of impairment 1 in 4 mothers elects to terminate the pregnancy
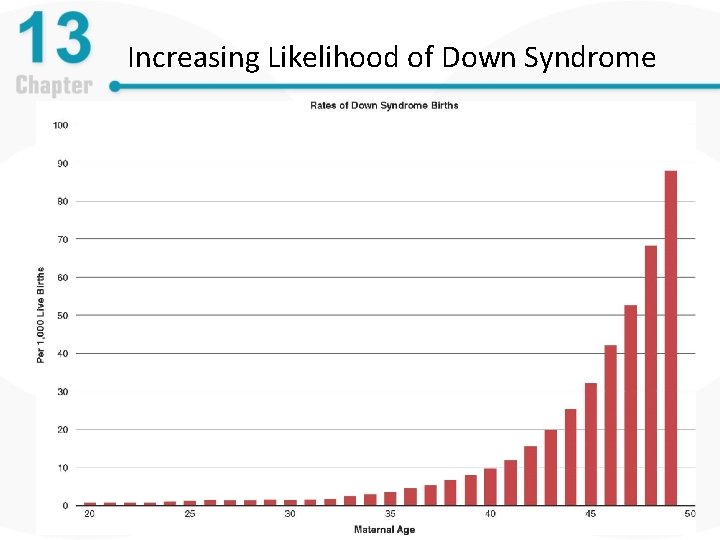
Increasing Likelihood of Down Syndrome
Causes of Intellectual Disability, Part 8 • Fragile X syndrome – Symptoms • • • Learning disabilities Hyperactivity Short attention spans Gaze avoidance Perseverative speech – Gender differences • Primarily affects males • Women with Fragile X have mild symptoms
Causes of Intellectual Disability, Part 9 • Cultural-familial intellectual disability: Refers to intellectual disability influenced by social environmental factors, such as: – Abuse – Neglect – Social deprivation • These factors likely interact with existing biological factors
Treatment of Intellectual Disability, Part 1 – Severe ID: Treatment similar to that for autism spectrum disorder – Mild ID: Treatment similar to that for learning disorders – Goals are similar across severity; level of assistance differs – Behavioral interventions teach: • Basic skills (e. g. , dressing, hygiene) • Social skills • Practical skills (e. g. , paying bills)
Treatment of Intellectual Disability, Part 2 • Common goals – Participate in community life – Benefit from education – hold a job or other productive pursuits (e. g. , volunteering) – Build meaningful relationships
Prevention of Neurodevelopmental Disorders • Efforts are still in early stages • Early interventions for at-risk children – Head Start Program: Educational, medical (e. g. , nutritional) and social support • Future directions: Genetic screening – Detection and correction – Prenatal gene therapy
Summary of Neurodevelopmental Disorders • This category encompasses a wide range of disorders with varying severity • May be caused by genetic or environmental factors or have indeterminate cause • Treatment focuses on mitigating functional impairment
Neurocognitive Disorders: An Overview, Part 1 • Affect learning, memory, and consciousness • Most develop later in life • Three classes of cognitive disorders – Delirium – temporary confusion and disorientation – Major or mild neurocognitive disorder – marked by broad cognitive deterioration – Amnestic disorders – memory dysfunctions
Neurocognitive Disorders: An Overview, Part 2 • Shifting DSM perspectives – From “organic” mental disorders to “cognitive” disorders – Broad impairments in cognitive functioning – Profound changes in behavior and personality
Delirium: An Overview, Part 1 • Nature of delirium – Central features – impaired consciousness and cognition – Develops rapidly over several hours or days – Appear confused, disoriented, and inattentive – Marked memory and language deficits
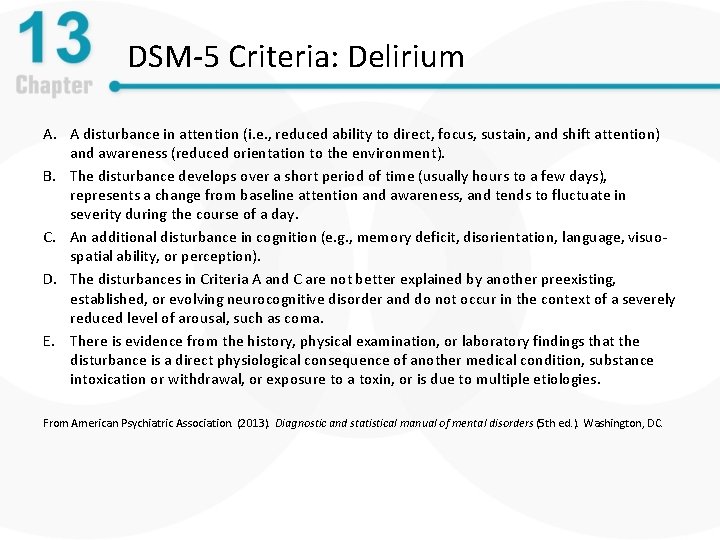
DSM-5 Criteria: Delirium A. A disturbance in attention (i. e. , reduced ability to direct, focus, sustain, and shift attention) and awareness (reduced orientation to the environment). B. The disturbance develops over a short period of time (usually hours to a few days), represents a change from baseline attention and awareness, and tends to fluctuate in severity during the course of a day. C. An additional disturbance in cognition (e. g. , memory deficit, disorientation, language, visuospatial ability, or perception). D. The disturbances in Criteria A and C are not better explained by another preexisting, established, or evolving neurocognitive disorder and do not occur in the context of a severely reduced level of arousal, such as coma. E. There is evidence from the history, physical examination, or laboratory findings that the disturbance is a direct physiological consequence of another medical condition, substance intoxication or withdrawal, or exposure to a toxin, or is due to multiple etiologies. From American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5 th ed. ). Washington, DC.
Delirium: An Overview, Part 2 • Facts and statistics – Affects up 20% of adults in acute care facilities (e. g. , ER) – More prevalent in certain populations, including: • Older adults • Those undergoing medical procedures • AIDS patients and cancer patients – Full recovery often occurs within several weeks
Medical Conditions Related to Delirium • Medical conditions – Dementia (50% of cases involve temporary delirium) – Drug intoxication, poisons, withdrawal from drugs – Infections – Head injury and several forms of brain trauma – Sleep deprivation, immobility, and excessive stress
Treatment and Prevention of Delirium • Treatment – Attention to precipitating medical problems – Psychosocial interventions • Reassurance/comfort, coping strategies, inclusion of patients in treatment decisions • Prevention – Address proper medical care for illnesses, proper use and adherence to therapeutic drugs
Major and Mild Neurocognitive Disorders, Part 1 • Nature of dementia – Gradual deterioration of brain functioning – Deterioration in judgment and memory – Deterioration in language / advanced cognitive processes – Has many causes and may be irreversible
Major and Mild Neurocognitive Disorders, Part 2 • Major neurocognitive disorder: The new DSM-5 term for dementia • Mild neurocognitive disorder: New DSM-5 classification for early stages of cognitive decline – Individual is able to function independently with some accommodations (e. g. , reminders/lists)
Major Neurocognitive Disorder • DSM-5 criteria – One or more cognitive deficits that represent a decrease from previous functioning – Substantiated by clinical assessment – Interfere with daily independent activities
DSM-5 Criteria: Major Neurocognitive Disorder A. Evidence of significant cognitive decline from a previous level of performance in one or more cognitive domains (complex attention, executive function, learning and memory, language, perceptual-motor, or social cognition) based on: (1) concern of the individual, a knowledgeable informant, or the clinician that there has been a significant decline in cognitive function; and (2) a substantial impairment in cognitive performance, preferably documented by standardized neuropsychological testing or, in its absence, another quantified clinical assessment. B. The cognitive deficits interfere with independence in everyday activities. C. The cognitive deficits do not occur exclusively in the context of a delirium. D. The cognitive deficits are not better explained by another mental disorder. Specify whether due to: Alzheimer’s disease, Frontotemporal lobar degeneration, Lewy body disease, Vascular disease, Traumatic brain injury, Substance/medication use, HIV infection, Prion disease, Parkinson’s disease, Huntington’s disease, Another medical condition, Multiple etiologies, Unspecified From American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5 th ed. ). Washington, DC.
DSM-5 Criteria: Mild Neurocognitive Disorder A. Evidence of modest cognitive decline from a previous level of performance in one or more cognitive domains (complex attention, executive function, learning and memory, language, perceptual motor, or social cognition) based on: (1) concern of the individual, a knowledgeable informant, or the clinician that there has been a mild decline in cognitive function; and (2) a modest impairment in cognitive performance, preferably documented by standardized neuropsychological testing or, in its absence, another quantified clinical assessment. B. The cognitive deficits do not interfere with capacity for independence in everyday activities. C. The cognitive deficits do not occur exclusively in the context of a delirium. D. The cognitive deficits are not better explained by another mental disorder. Specify whether due to: Alzheimer’s disease, Frontotemporal lobar degeneration, Lewy body disease, Vascular disease, Traumatic brain injury, Substance/medication use, HIV infection, Prion disease, Parkinson’s disease, Huntington’s disease, Another medical condition, Multiple etiologies, Unspecified From American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5 th ed. ). Washington, DC.
Major Neurocognitive Disorder, Part 1 • Initial stages – Memory and visuospatial skills impairments – Facial agnosia – inability to recognize familiar faces – Other symptoms • Delusions, apathy, depression, agitation, aggression
Major Neurocognitive Disorder, Part 2 • Later stages – Cognitive functioning continues to deteriorate – Total support is needed to carry out day-to-day activities – Increased risk for early death due to inactivity and onset of other illnesses
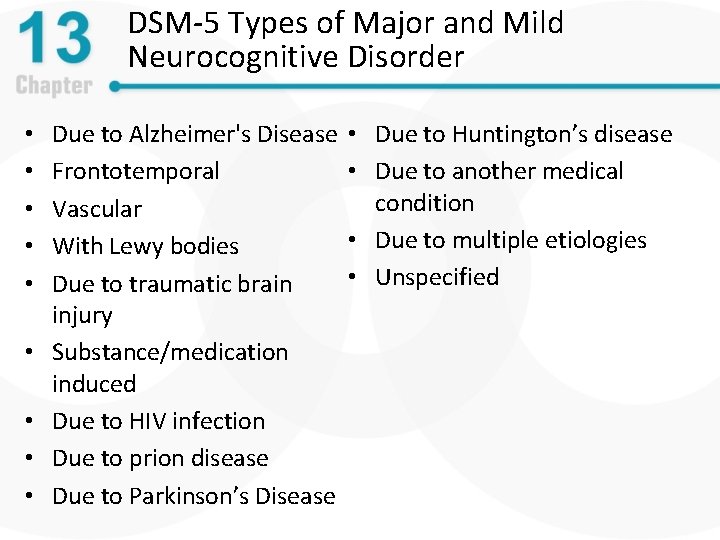
DSM-5 Types of Major and Mild Neurocognitive Disorder • • • Due to Alzheimer's Disease Frontotemporal Vascular With Lewy bodies Due to traumatic brain injury Substance/medication induced Due to HIV infection Due to prion disease Due to Parkinson’s Disease • Due to Huntington’s disease • Due to another medical condition • Due to multiple etiologies • Unspecified
Neurocognitive Disorder Due to Alzheimer’s Disease • Accounts for nearly half of neurocognitive disorders • Clinical Features – Typically develop gradually and steadily – Memory, orientation, judgment, and reasoning deficits – Additional symptoms may include • Agitation, confusion, or combativeness • Depression and/or anxiety
Alzheimer’s Disorder: Extent of Deficits • Range of cognitive deficits – Aphasia – difficulty with language – Apraxia – impaired motor functioning – Agnosia – failure to recognize objects – Difficulties with • Planning, Organizing • Sequencing • Abstracting information – Negative impact on social and occupational functioning
Alzheimer’s Disease: Some Facts and Statistics, Part 1 • Nature and progression of the disease – Deterioration is slow during the early and later stages – Deterioration is rapid during middle stages – Average survival time is about eight years – Onset usually occurs in the 60 s or 70 s
Alzheimer’s Disease: Some Facts and Statistics, Part 2 • Prevalence of Alzheimer’s disease – Greater prevalence in low-education groups • Thought to reflect protective effects of high education (delays the onset of some symptoms) • Better-educated people will eventually decline more rapidly – Women at slightly higher risk – Prevalence rates were thought to be low in some ethnic groups • Likely a reflection of education and who seeks care, not reflective of a true difference
Amnesia • Previously diagnosed as amnestic disorder • Now considered a type of neurocognitive disorder • Presentation – Circumscribed loss of memory – Inability to learn new information or recall previous information – No loss of other high-level cognitive functions
Vascular Neurocognitive Disorder, Part 1 – Caused by blockage or damage to blood vessels – Second leading cause of neurocognitive disorder after Alzheimer’s disease – Onset is often sudden (e. g. , stroke) – Patterns of impairment are variable – Most require formal care in later stages
Vascular Neurocognitive Disorder, Part 2 • Features – Cognitive disturbances – identical to dementia – Obvious neurological signs of brain tissue damage – Prevalence 1. 5% in people 70 -75 and 15% for people over 80 – Risk slightly higher in men
Other Causes of Neurocognitive Disorder, Part 1 • Head trauma – accidents are leading cause – Memory loss is the most common symptom – May be found in athletes who experience repeated blows to the head (e. g. , football players)
Other Causes of Neurocognitive Disorder, Part 2 • Parkinson’s disease – degenerative brain disorder – Affects about one out of 1, 000 people worldwide – Motor problems – central feature of this disorder • Caused by damage to dopamine pathways – 75% survival rate for 10 years
Other Causes of Neurocognitive Disorder, Part 3 • HIV-1 – In some, causes neurological impairments and dementia – Cognitive slowness, impaired attention, and forgetfulness – Apathy and social withdrawal
Other Causes of Dementia: Huntington’s Disease • Genetic autosomal dominant disorder • Manifests initially as chorea, usually later in life • Somewhere between 20 -80% display neurocognitive disorder • Dementia follows a subcortical pattern
Other Causes of Neurocognitive Disorder, Part 4 • Pick’s disease – Rare neurological condition – Produces a cortical dementia like Alzheimer’s – Also occurs later in life (around 40 s or 50 s) – Little is known about what causes this disease
Other Causes of Neurocognitive Disorder, Part 5 • Prion disease: Disorder of proteins in the brain that reproduce and cause damage • Example: Creutzfeldt-Jakob disease – Affects one out of 1, 000 persons – Linked to mad cow disease
Other Causes of Neurocognitive Disorder, Part 6 • Substance-induced – Results from prolonged drug use, especially in combination with poor diet – Several drugs can lead to symptoms of dementia – Resulting brain damage endures beyond actual state of intoxication – Symptoms similar to Alzheimer’s – Deficits may include • Aphasia, apraxia, agnosia • Disturbed executive functioning
Causes of Neurocognitive Disorder: The Example of Alzheimer’s Disease, Part 1 • Current neurobiological findings – Neurofibrillary tangles – Amyloid plaques – Brains of Alzheimer’s patients tend to atrophy
Causes of Neurocognitive Disorder: The Example of Alzheimer’s Disease, Part 2 • Deterministic genes – Rare genes that inevitably lead to Alzheimer’s • Beta-amyloid precursor gene • Presenilin-1 and Presenilin-2 genes • Susceptibility genes – Make it more likely but not certain to develop Alzheimer’s – Example: Apo. E 4 gene. Future research will focus on inhibiting this gene
Causes of Dementia: The Example of Alzheimer’s Disease • Current neurobiological findings – Multiple genes are involved in Alzheimer’s disease – Include genes on chromosomes 21, 19, 14, 12 – Chromosome 14 • Associated with early onset Alzheimer’s – Chromosome 19 • Associated with late onset Alzheimer’s
The Contributions of Psychosocial Factors in Neurocognitive Disorders • Psychosocial factors – Do not cause dementia directly – May influence onset and course – Lifestyle factors – drug use, diet, exercise, stress – Cultural factors • Risk for certain conditions vary by ethnicity and class – Psychosocial factors • Educational attainment, coping skills, social support
Medical Treatment of Neurocognitive Disorders – When possible, treat primary cause • Few exist for most types of neurocognitive disorders (e. g. , Huntington’s disease) • Most treatments attempt to slow progression of deterioration, but cannot stop it – Future directions • Glial cell-derived neurotrophic factor, stem cells: may slow deterioration – Some drugs target cognitive deficits • Long-term effects not well demonstrated • Also need to target anxiety, depression
Psychosocial Treatment of Neurocognitive Disorders • Psychosocial treatments – aims – To enhance lives of patients and their families – To teach compensatory skills – To use memory enhancement devices, if needed – Caregivers also under great deal of stress, may need their own services (e. g. , mental health treatment)
Prevention of Neurocognitive Disorders • Reducing risk in older adults – Use of anti-inflammatory medications – Control blood pressure, don’t smoke and lead active social life • Other targets of prevention efforts – Increasing safety behaviors to reduce head trauma – Reducing exposure to neurotoxins and use of drugs
Summary of Neurocognitive Disorders, Part 1 • Cognitive disorders span a range of deficits – Affect attention, memory, language, and motor behavior – Causes include • • Aging Medical conditions Drug use Environmental factors
Summary of Neurocognitive Disorders, Part 2 • Most result in progressive deterioration of functioning • Few treatments exist to reverse damage and deficits
 Neurocognitive disorder
Neurocognitive disorder Chapter 11 childhood and neurodevelopmental disorders
Chapter 11 childhood and neurodevelopmental disorders Communication disorders (dsm-5 ppt)
Communication disorders (dsm-5 ppt) Neurodevelopmental disorders
Neurodevelopmental disorders Neurocognitive disorder
Neurocognitive disorder Mild neurocognitive disorder
Mild neurocognitive disorder Reflex inhibiting patterns
Reflex inhibiting patterns Neurodevelopmental therapy principles
Neurodevelopmental therapy principles Remiryl
Remiryl Major neurocognitive disorder criteria
Major neurocognitive disorder criteria Paragraph sandwich example
Paragraph sandwich example Define a primary skin lesion and list three types
Define a primary skin lesion and list three types Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Chapter 46 digestive and endocrine disorders
Chapter 46 digestive and endocrine disorders Somatic symptom disorder
Somatic symptom disorder Chapter 29 endocrine and metabolic disorders
Chapter 29 endocrine and metabolic disorders Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Chapter 18 eating and feeding disorders
Chapter 18 eating and feeding disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Chapter 15 anxiety and obsessive-compulsive disorders
Chapter 15 anxiety and obsessive-compulsive disorders Elsevier
Elsevier Plicatured nail treatment
Plicatured nail treatment Milady chapter 10
Milady chapter 10 Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases Chapter 47 urinary and reproductive disorders
Chapter 47 urinary and reproductive disorders Extreme harmful eating behaviors
Extreme harmful eating behaviors 10 diseases of lymphatic system
10 diseases of lymphatic system Medical model psychology
Medical model psychology Concept mapping chapter 11 genetic disorders
Concept mapping chapter 11 genetic disorders Chapter 18 psychological disorders
Chapter 18 psychological disorders Chapter 14 psychological disorders
Chapter 14 psychological disorders Chapter 14 depressive disorders
Chapter 14 depressive disorders Glencoe health chapter 5 review answers
Glencoe health chapter 5 review answers Chapter 5 mental and emotional problems
Chapter 5 mental and emotional problems Chapter 14 psychological disorders
Chapter 14 psychological disorders Ap psychology chapter 15 psychological disorders
Ap psychology chapter 15 psychological disorders Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders Chapter 17 somatic symptom disorders
Chapter 17 somatic symptom disorders Chapter 12 schizophrenia spectrum disorders
Chapter 12 schizophrenia spectrum disorders Chapter 12 schizophrenia spectrum disorders
Chapter 12 schizophrenia spectrum disorders Conclusion paragraph outline
Conclusion paragraph outline In a formal outline, what should roman numerals represent?
In a formal outline, what should roman numerals represent? Software engineering 1 course outline
Software engineering 1 course outline Unit 14 physiological disorders
Unit 14 physiological disorders Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders Emotional disturbance assistive technology
Emotional disturbance assistive technology Puberty and autism spectrum disorders
Puberty and autism spectrum disorders Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders Neurotic stress-related and somatoform disorders
Neurotic stress-related and somatoform disorders Physical disorders and health psychology
Physical disorders and health psychology Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders Little albert
Little albert Cengage
Cengage Physiological disorders and their care
Physiological disorders and their care Neurotic personality disorder
Neurotic personality disorder Mcqs on protein metabolism
Mcqs on protein metabolism Hypothalamus eating disorders
Hypothalamus eating disorders Difference between mendelian and chromosomal disorders
Difference between mendelian and chromosomal disorders Unit 14 health and social care level 3
Unit 14 health and social care level 3 Flinders model
Flinders model Somatization disorder
Somatization disorder Egodystone
Egodystone Types of sensory disorders
Types of sensory disorders Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Section 4-1 mental disorders answers
Section 4-1 mental disorders answers What are the 10 personality disorders
What are the 10 personality disorders Cluster b
Cluster b Avoidant personality traits
Avoidant personality traits Personality disorders dsm 5
Personality disorders dsm 5 Psychological disorders characterized by inflexible
Psychological disorders characterized by inflexible Cluster b
Cluster b Cluster b
Cluster b Examples of personality disorders
Examples of personality disorders York eating disorder unit
York eating disorder unit Immunoproliferative disorders examples
Immunoproliferative disorders examples Mood disorders
Mood disorders Orotic aciduria
Orotic aciduria Purine disorders
Purine disorders Down klinefelter turner
Down klinefelter turner Sex linked disorders
Sex linked disorders Unit 14 physiological disorders assignment 1
Unit 14 physiological disorders assignment 1 Autism authorization ctc
Autism authorization ctc Gross features
Gross features Slidetodoc.com
Slidetodoc.com Jamal gross
Jamal gross Edema heart
Edema heart Edema robbins
Edema robbins Difference between hyperemia and congestion
Difference between hyperemia and congestion Neurobehavioral disorders list
Neurobehavioral disorders list Hemodynamic disorders
Hemodynamic disorders Causes of paraphilic disorders
Causes of paraphilic disorders Eating disorders in uae
Eating disorders in uae Acupuncture for eating disorders
Acupuncture for eating disorders Dissociative disorders
Dissociative disorders What is detachment disorder
What is detachment disorder Dsm v sexual disorders
Dsm v sexual disorders