Cognitive Disorders theme Fahad Alosaimi MD Psychiatry Psychosomatic








- Slides: 63

Cognitive Disorders theme Fahad Alosaimi MD Psychiatry & Psychosomatic medicine Consultant Assistant professer KSU
Case study Abdullah is a 72 -year-old male. He was brought to the Emergency Department by his son for vomiting, new onset urinary incontinence, confusion, and incoherent speech for the past 2 days. The patient was disoriented and could see people climbing trees outside the window. He had difficulty sustaining attention, and his level of consciousness waxed and waned. He had been talking about his deceased wife. Patient was also trying to pull out his intravenous access line. Past history included diabetes mellitus, hyperlipidemia, osteoarthritis, and stroke.
Case study On examination, the patient was drowsy and falling asleep while practitioners were talking to him. Patient was not cooperative with the physical examination and with a formal mental status examination. Limited examination of the abdomen indicated that it was flat and soft with normal bowel sounds. The patient moves all 4 limbs and plantar is bilateral flexor. Laboratory test results revealed elevated BUN and creatinine levels, and the urine analysis was positive for urinary tract infection. CT scan of the head showed cortical atrophy plus an old infarct. The patient's family physician had recently prescribed Tylenol with codeine for the patient's severe knee pain 5 days earlier.
A- Analysis of symptoms, MSE and psychopathology especially perception; differential diagnosis discussion (including drug intoxication and withdrawal): Analyze the symptoms (presented and expected) in this case and signs, including mood, thoughts, cognition, perception and physical aspects Discuss other elements related to the case includes possible etiological reasons Discuss the initial possible diagnosis of this case and different types of such clinical presentation
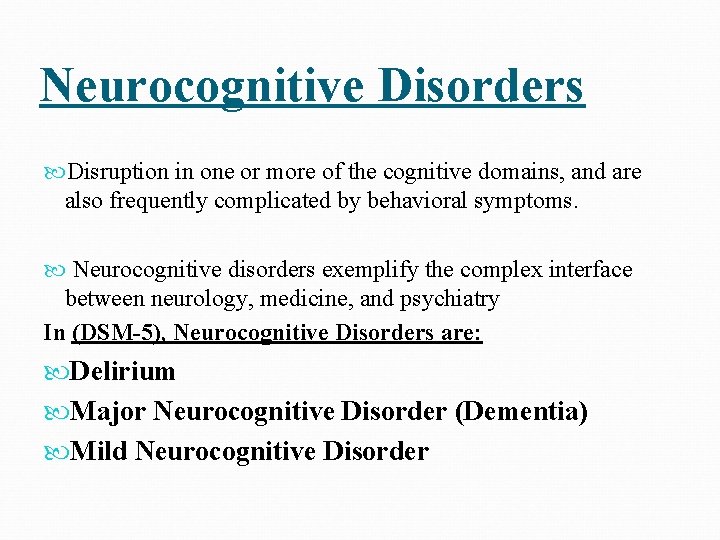
Neurocognitive Disorders Disruption in one or more of the cognitive domains, and are also frequently complicated by behavioral symptoms. Neurocognitive disorders exemplify the complex interface between neurology, medicine, and psychiatry In (DSM-5), Neurocognitive Disorders are: Delirium Major Neurocognitive Disorder (Dementia) Mild Neurocognitive Disorder
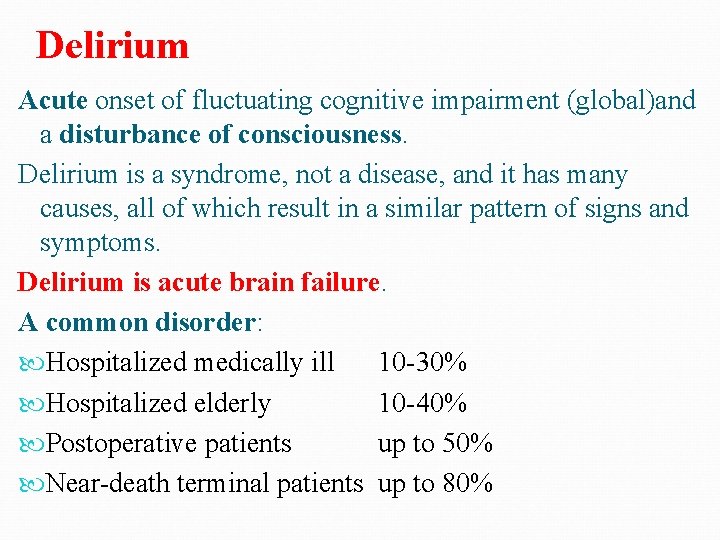
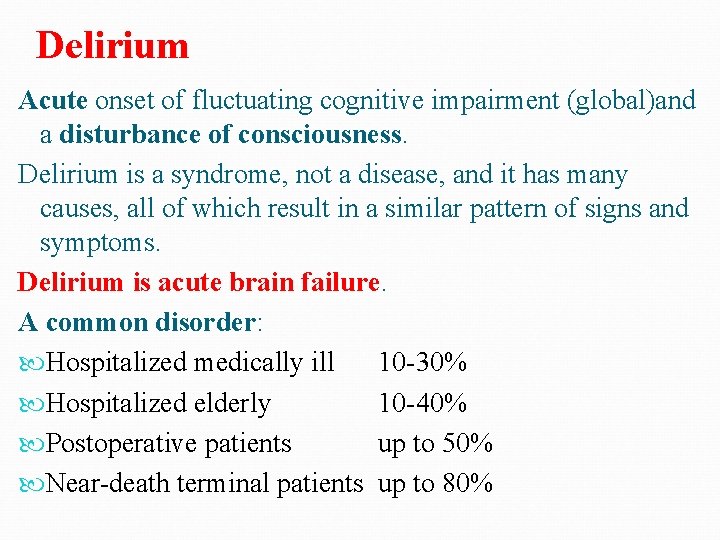
Delirium Acute onset of fluctuating cognitive impairment (global)and a disturbance of consciousness. Delirium is a syndrome, not a disease, and it has many causes, all of which result in a similar pattern of signs and symptoms. Delirium is acute brain failure. A common disorder: Hospitalized medically ill 10 -30% Hospitalized elderly 10 -40% Postoperative patients up to 50% Near-death terminal patients up to 80%
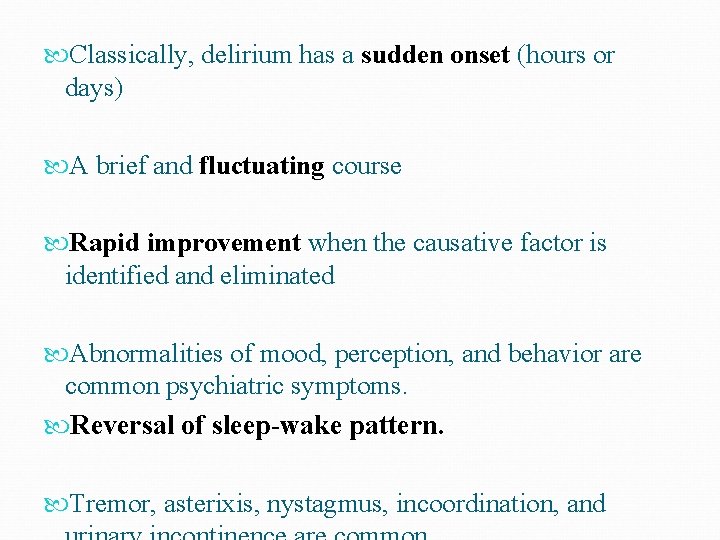
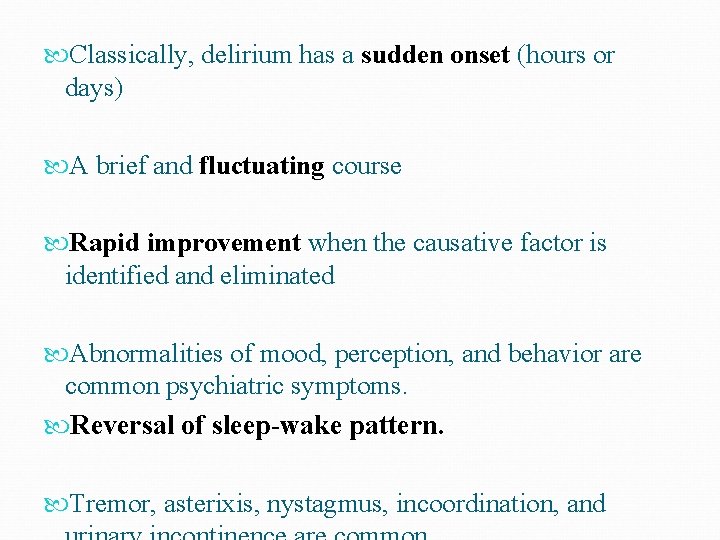
Classically, delirium has a sudden onset (hours or days) A brief and fluctuating course Rapid improvement when the causative factor is identified and eliminated Abnormalities of mood, perception, and behavior are common psychiatric symptoms. Reversal of sleep-wake pattern. Tremor, asterixis, nystagmus, incoordination, and

Delirium has bad prognosis May progress to stupor, coma, seizures or death, particularly if untreated. Increased risk for postoperative complications, longer postoperative recuperation, longer hospital stays, long -term disability. Elderly patients 22 -76% chance of dying during that hospitalization Several studies suggest that up to 25% of all patients with delirium die within 6 months
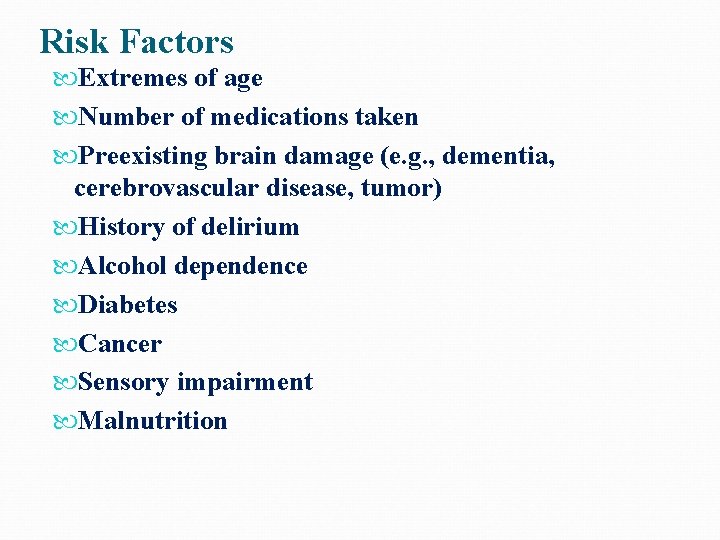
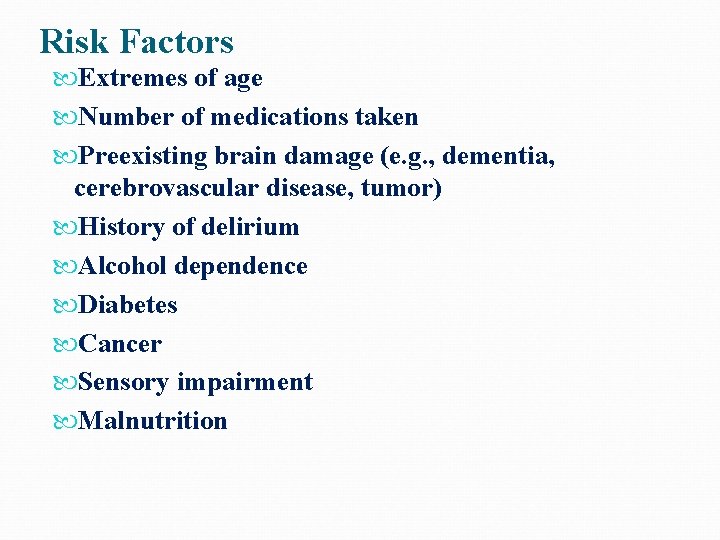
Risk Factors Extremes of age Number of medications taken Preexisting brain damage (e. g. , dementia, cerebrovascular disease, tumor) History of delirium Alcohol dependence Diabetes Cancer Sensory impairment Malnutrition
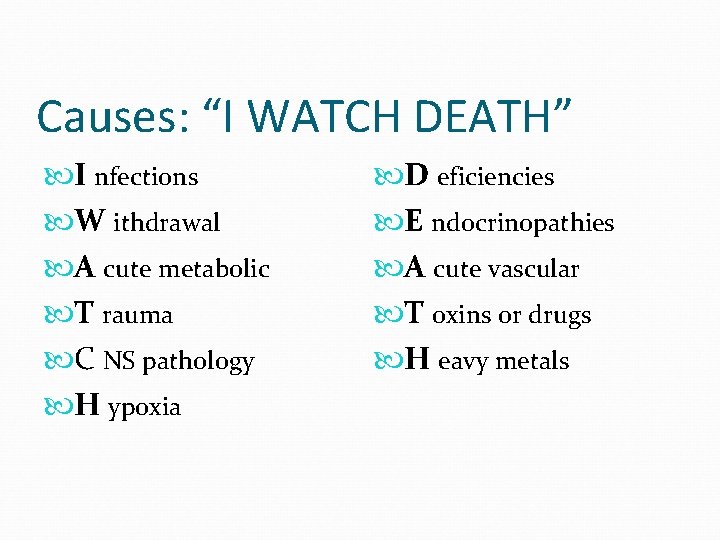
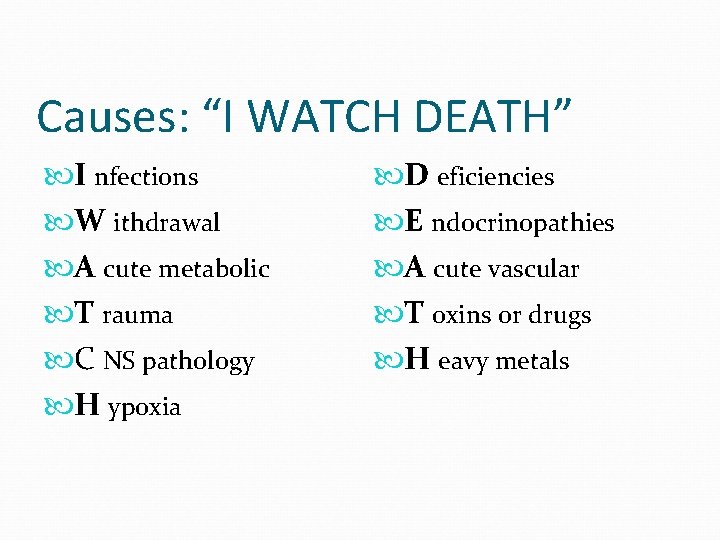
Causes: “I WATCH DEATH” I nfections W ithdrawal A cute metabolic T rauma C NS pathology H ypoxia D eficiencies E ndocrinopathies A cute vascular T oxins or drugs H eavy metals
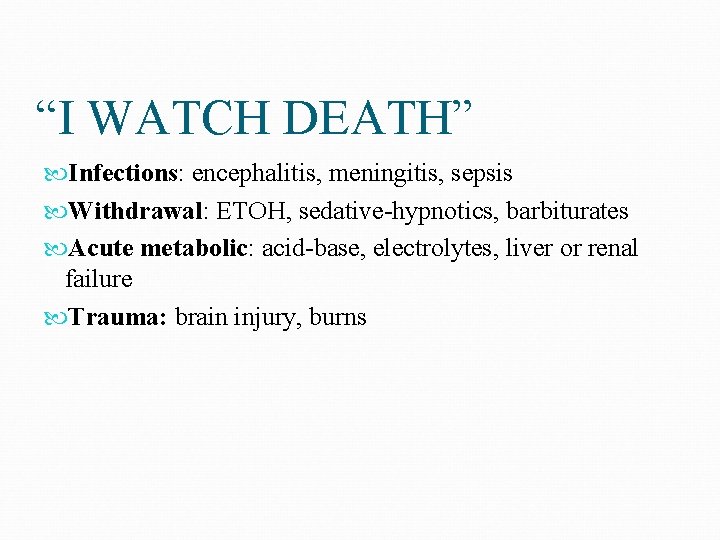
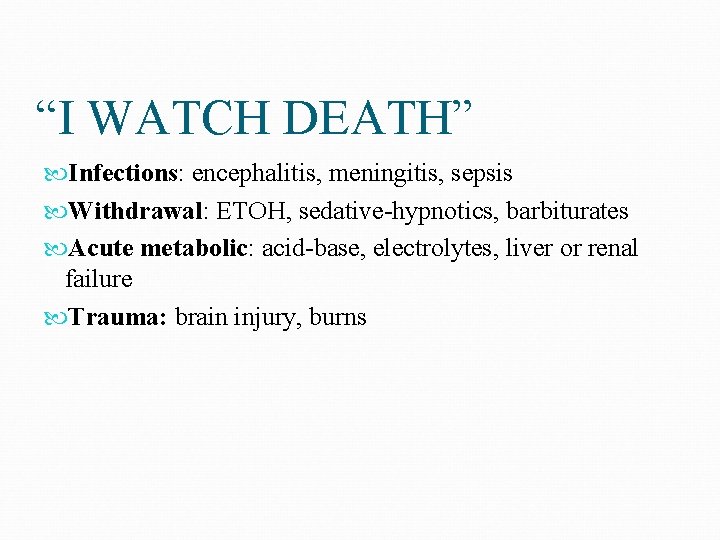
“I WATCH DEATH” Infections: encephalitis, meningitis, sepsis Withdrawal: ETOH, sedative-hypnotics, barbiturates Acute metabolic: acid-base, electrolytes, liver or renal failure Trauma: brain injury, burns
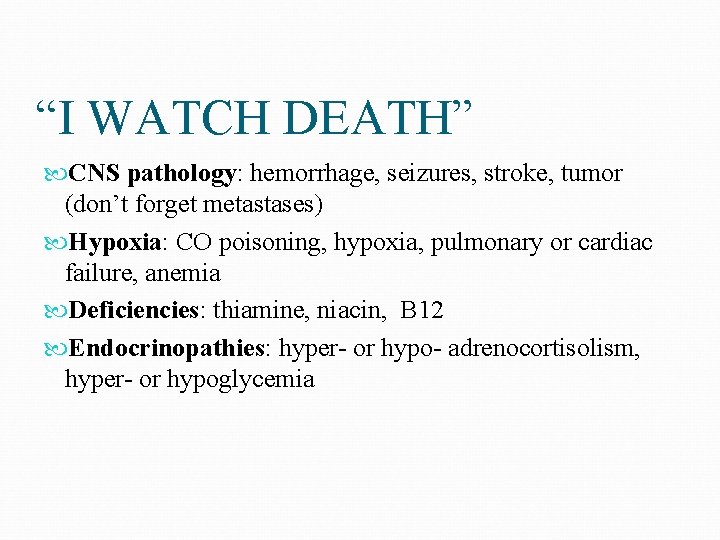
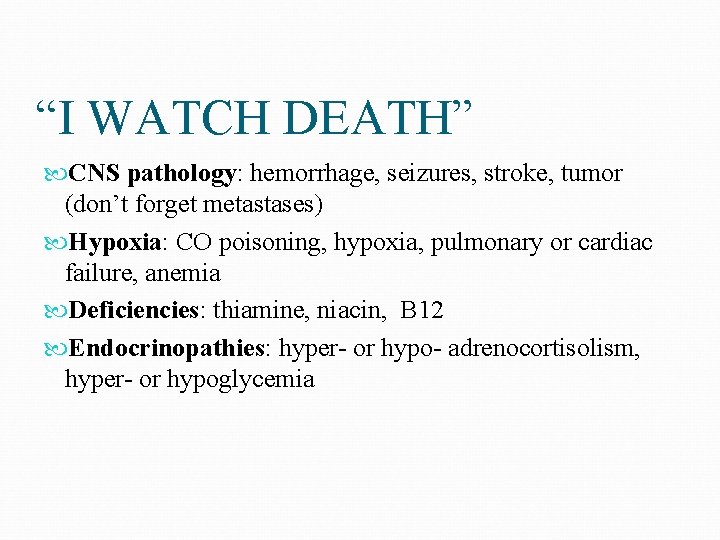
“I WATCH DEATH” CNS pathology: hemorrhage, seizures, stroke, tumor (don’t forget metastases) Hypoxia: CO poisoning, hypoxia, pulmonary or cardiac failure, anemia Deficiencies: thiamine, niacin, B 12 Endocrinopathies: hyper- or hypo- adrenocortisolism, hyper- or hypoglycemia
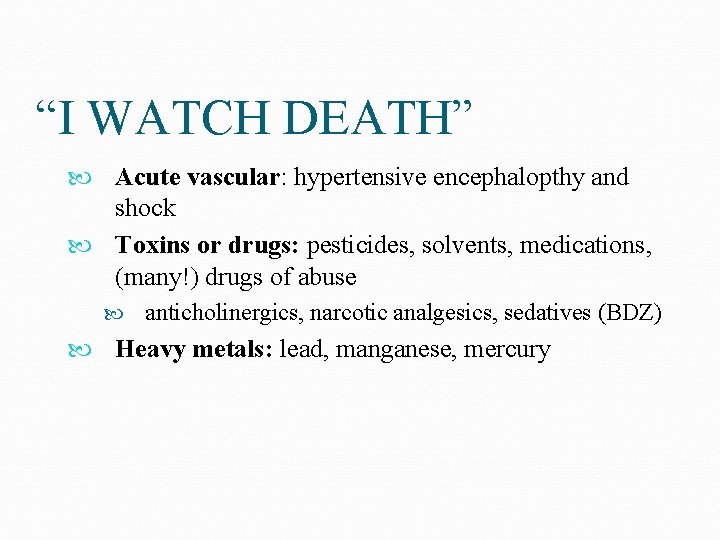
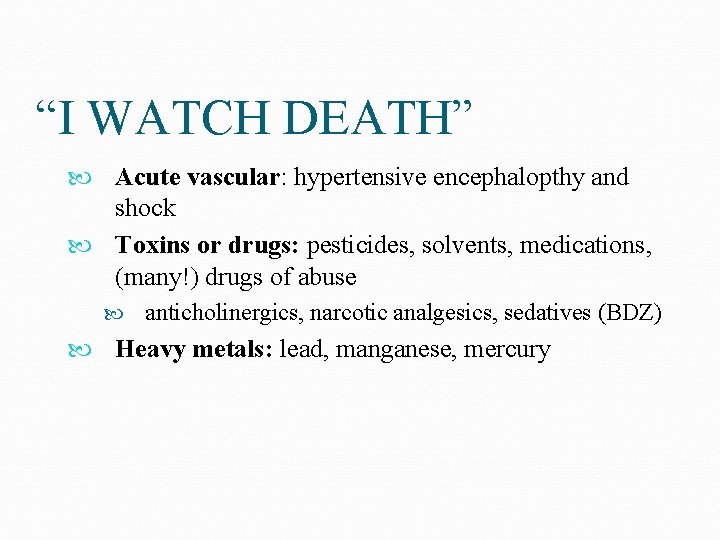
“I WATCH DEATH” Acute vascular: hypertensive encephalopthy and shock Toxins or drugs: pesticides, solvents, medications, (many!) drugs of abuse anticholinergics, narcotic analgesics, sedatives (BDZ) Heavy metals: lead, manganese, mercury
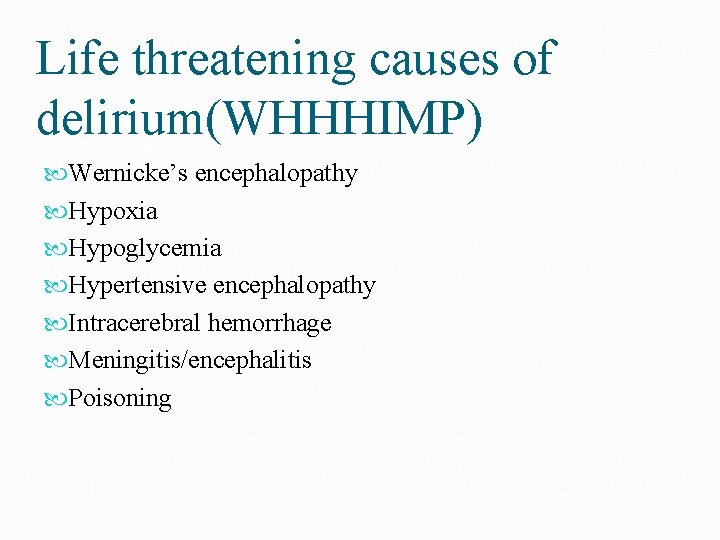
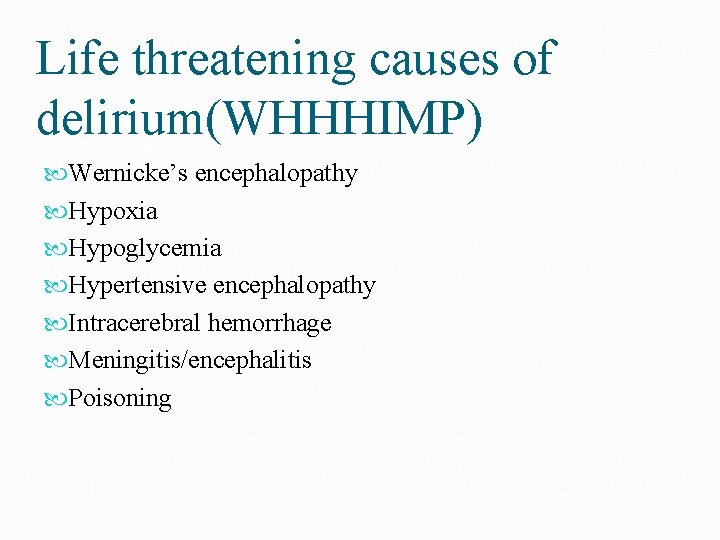
Life threatening causes of delirium(WHHHIMP) Wernicke’s encephalopathy Hypoxia Hypoglycemia Hypertensive encephalopathy Intracerebral hemorrhage Meningitis/encephalitis Poisoning
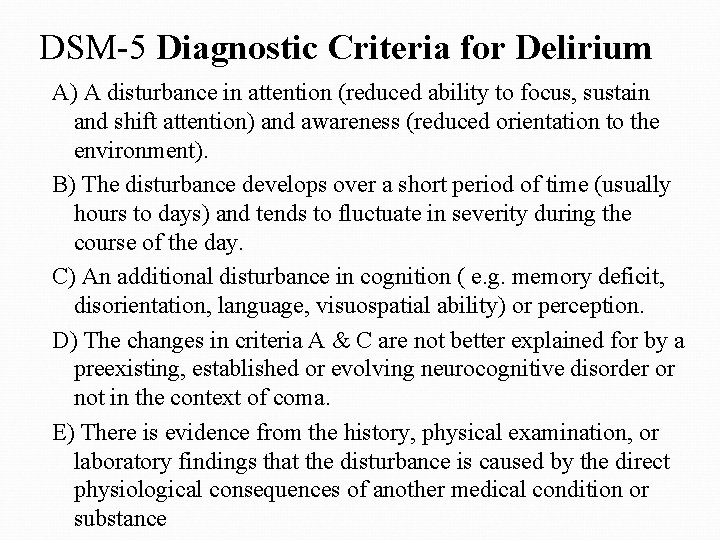
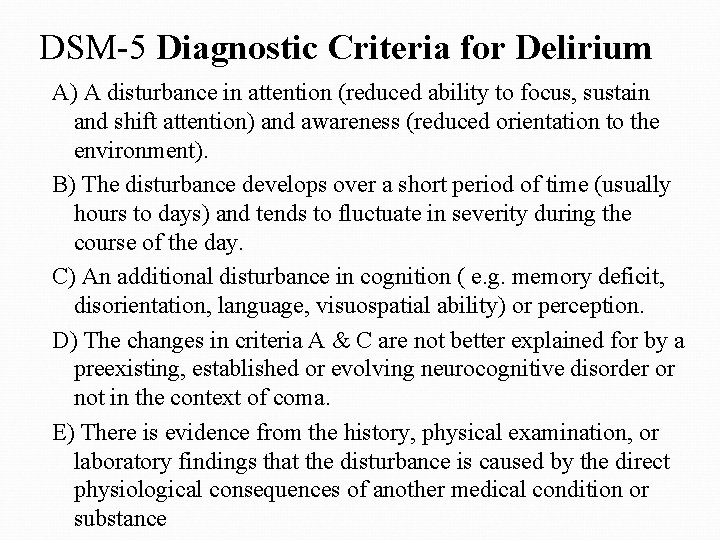
DSM-5 Diagnostic Criteria for Delirium A) A disturbance in attention (reduced ability to focus, sustain and shift attention) and awareness (reduced orientation to the environment). B) The disturbance develops over a short period of time (usually hours to days) and tends to fluctuate in severity during the course of the day. C) An additional disturbance in cognition ( e. g. memory deficit, disorientation, language, visuospatial ability) or perception. D) The changes in criteria A & C are not better explained for by a preexisting, established or evolving neurocognitive disorder or not in the context of coma. E) There is evidence from the history, physical examination, or laboratory findings that the disturbance is caused by the direct physiological consequences of another medical condition or substance
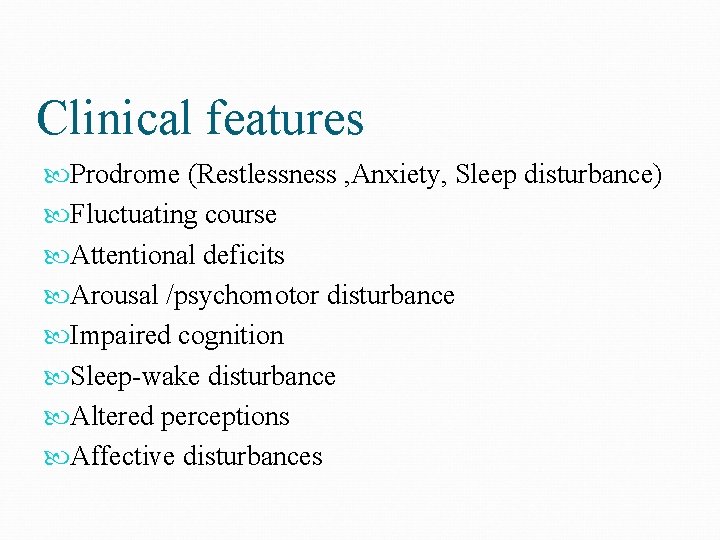
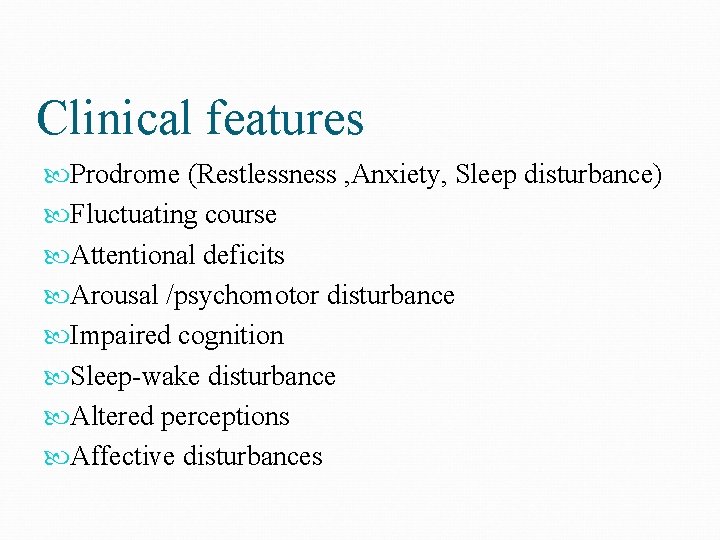
Clinical features Prodrome (Restlessness , Anxiety, Sleep disturbance) Fluctuating course Attentional deficits Arousal /psychomotor disturbance Impaired cognition Sleep-wake disturbance Altered perceptions Affective disturbances

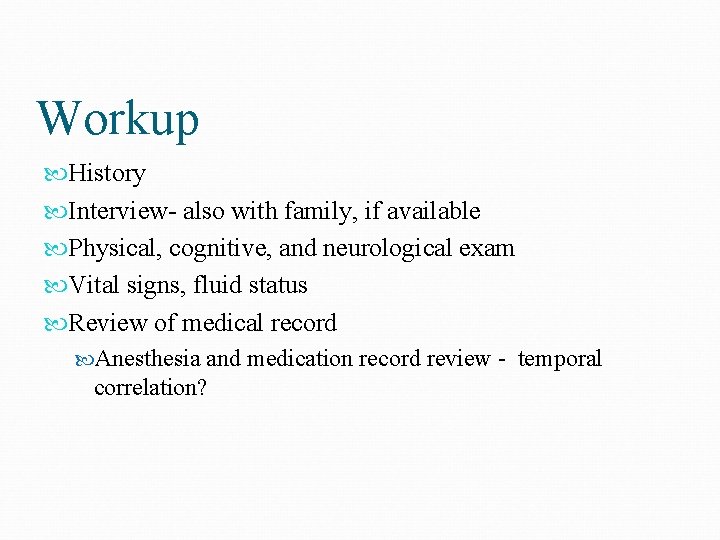
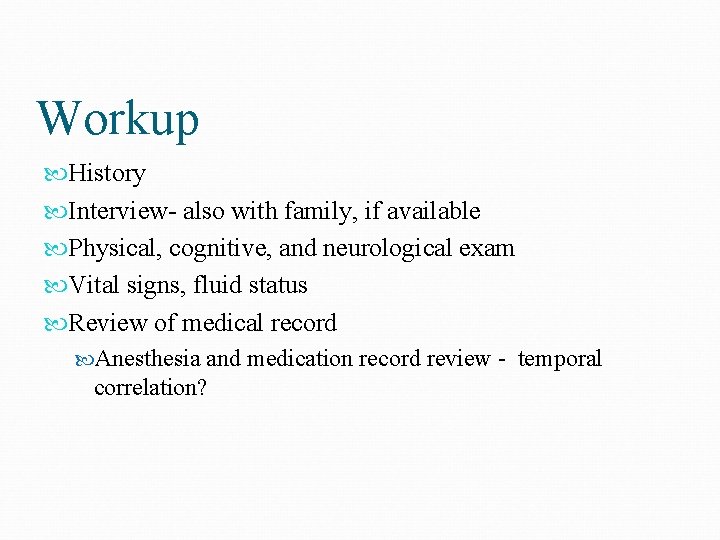
Workup History Interview- also with family, if available Physical, cognitive, and neurological exam Vital signs, fluid status Review of medical record Anesthesia and medication record review - temporal correlation?
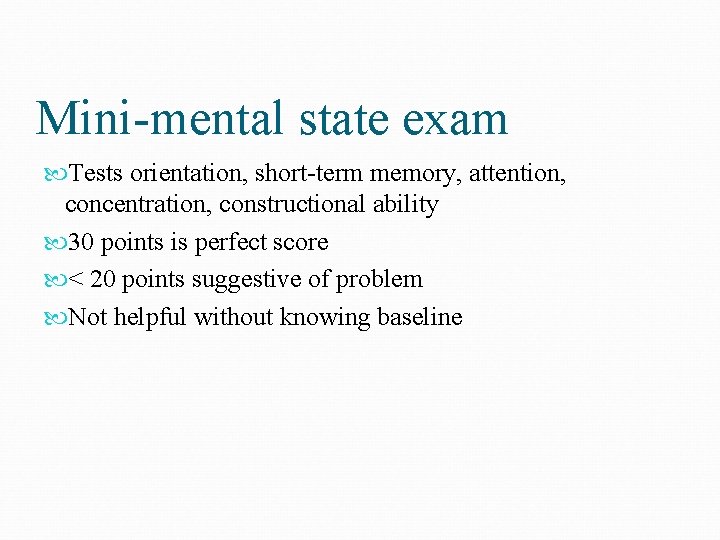
Mini-mental state exam Tests orientation, short-term memory, attention, concentration, constructional ability 30 points is perfect score < 20 points suggestive of problem Not helpful without knowing baseline
Workup Electrolytes CBC EKG CXR EEG- not usually necessary
Workup Arterial blood gas or Oxygen saturation Urinalysis +/- Culture and sensitivity Urine drug screen Blood alcohol Serum drug levels (digoxin, theophylline, phenobarbital, cyclosporin, lithium, etc)
Workup Arterial blood gas or Oxygen saturation Urinalysis +/- Culture and sensitivity Urine drug screen Blood alcohol Serum drug levels (digoxin, theophylline, phenobarbital, cyclosporin, lithium, etc)
Workup Consider: - Heavy metals - Lupus workup - Urinary porphyrins
Differential Diagnosis Major Neurocognitive Disorder (Dementia) Mild Neurocognitive Disorder Depression Schizophrenia
Management Identify and treat the underlying etiology Increase observation and monitoring – vital signs, fluid intake and output, oxygenation, safety Discontinue or minimize dosing of nonessential medications Coordinate with other physicians and providers
Management Monitor and assure safety of patient and staff: - suicidality and violence potential - fall & wandering risk - need for a sitter - remove potentially dangerous items from the environment - restrain ONLY when other means not effective (it may worsen delirium).
Management Assess individual and family psychosocial characteristics Establish and maintain an alliance with the family and other clinicians Educate the family – temporary and part of a medical condition – not “crazy” Provide post-delirium education and processing for patient
Treatment The primary goal is to treat the underlying cause The other important goal of treatment is to provide physical, sensory, and environmental support

Management Pharmacologic management ( the primary treatment of delirium) : - Low doses of high potency antipsychotics (i. e. haloperidol) po, im or iv - Atypical antipsychotics (risperidone, olanzapine, quetiapine, aripiprazol). *Rarely, some antipsychotics are associated with torsade de pointes arrhythmia by lengthening the QT interval; avoid or monitor this by ECG monitoring.
Summary Delirium is common and is often a harbinger of death - especially in vulnerable populations It is a sudden change in mental status, with a fluctuating course, marked by decreased attention It is caused by underlying medical problems, drug intoxication/withdrawal, or a combination Recognizing delirium and searching for the cause can save the patient’s life
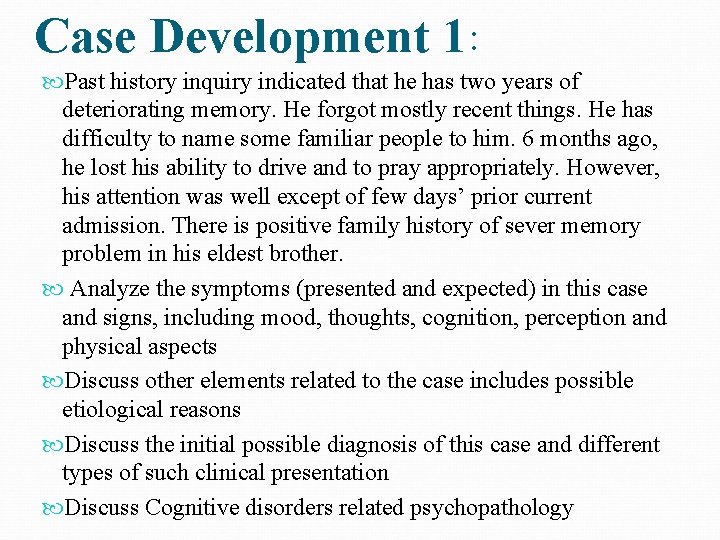
Case Development 1: Past history inquiry indicated that he has two years of deteriorating memory. He forgot mostly recent things. He has difficulty to name some familiar people to him. 6 months ago, he lost his ability to drive and to pray appropriately. However, his attention was well except of few days’ prior current admission. There is positive family history of sever memory problem in his eldest brother. Analyze the symptoms (presented and expected) in this case and signs, including mood, thoughts, cognition, perception and physical aspects Discuss other elements related to the case includes possible etiological reasons Discuss the initial possible diagnosis of this case and different types of such clinical presentation Discuss Cognitive disorders related psychopathology
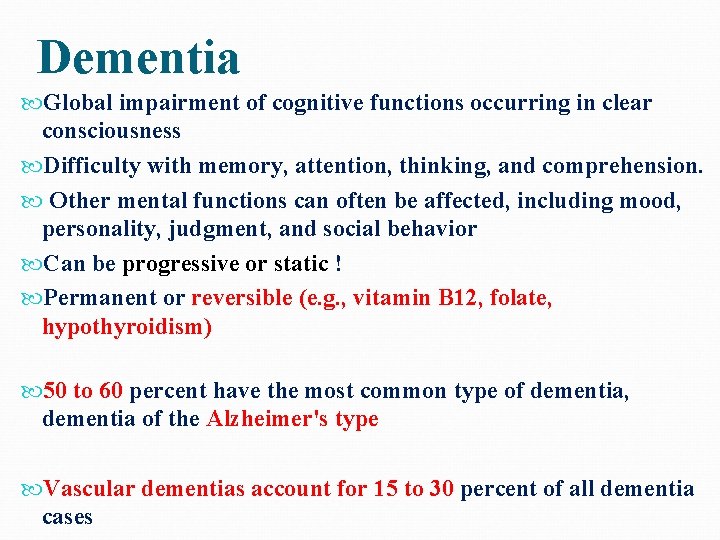
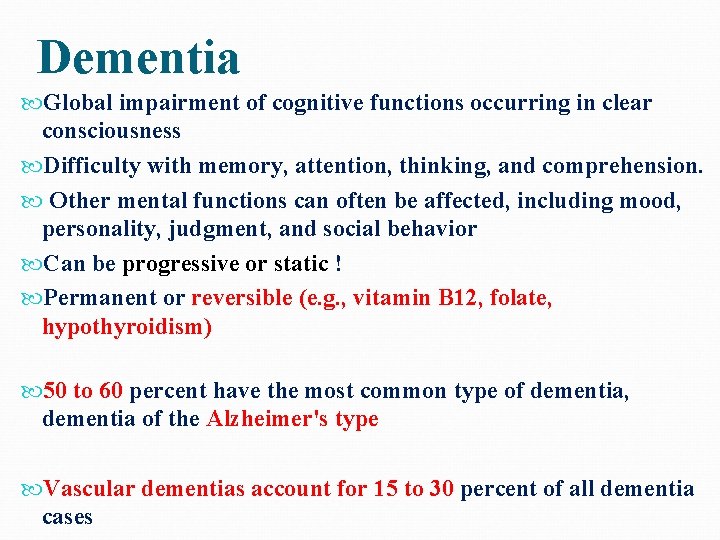
Dementia Global impairment of cognitive functions occurring in clear consciousness Difficulty with memory, attention, thinking, and comprehension. Other mental functions can often be affected, including mood, personality, judgment, and social behavior Can be progressive or static ! Permanent or reversible (e. g. , vitamin B 12, folate, hypothyroidism) 50 to 60 percent have the most common type of dementia, dementia of the Alzheimer's type Vascular dementias account for 15 to 30 percent of all dementia cases
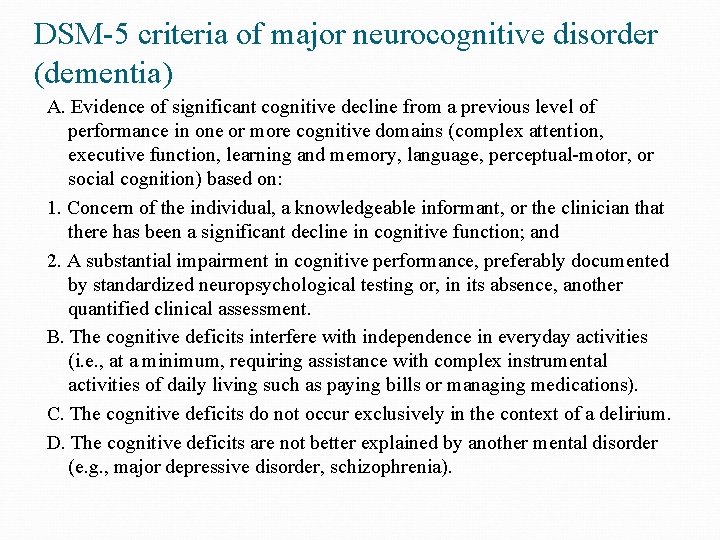
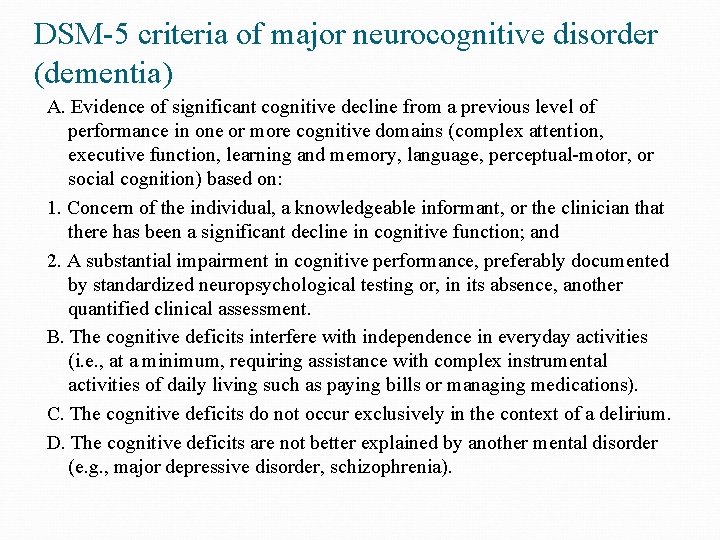
DSM-5 criteria of major neurocognitive disorder (dementia) A. Evidence of significant cognitive decline from a previous level of performance in one or more cognitive domains (complex attention, executive function, learning and memory, language, perceptual-motor, or social cognition) based on: 1. Concern of the individual, a knowledgeable informant, or the clinician that there has been a significant decline in cognitive function; and 2. A substantial impairment in cognitive performance, preferably documented by standardized neuropsychological testing or, in its absence, another quantified clinical assessment. B. The cognitive deficits interfere with independence in everyday activities (i. e. , at a minimum, requiring assistance with complex instrumental activities of daily living such as paying bills or managing medications). C. The cognitive deficits do not occur exclusively in the context of a delirium. D. The cognitive deficits are not better explained by another mental disorder (e. g. , major depressive disorder, schizophrenia).
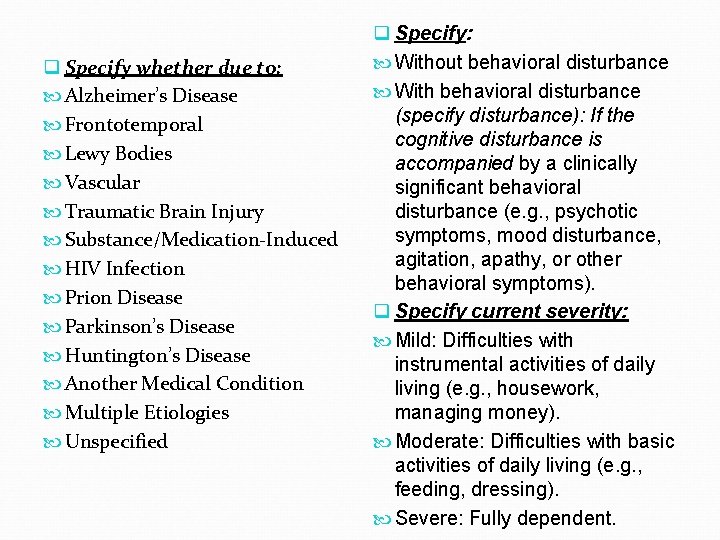
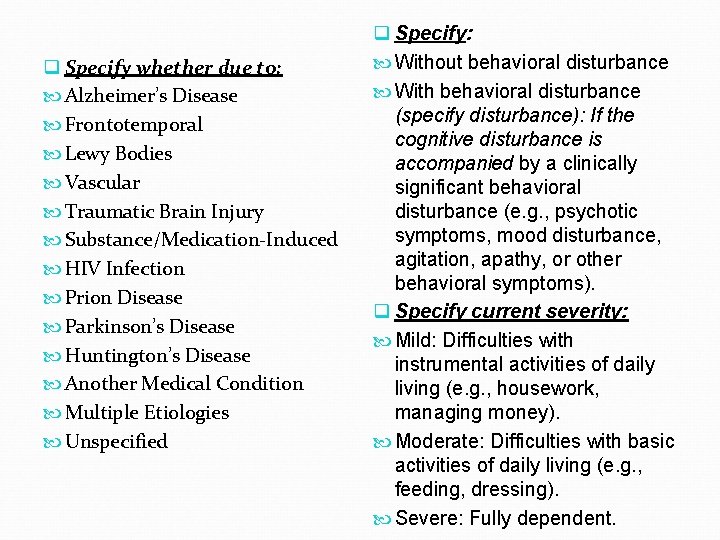
q Specify whether due to: Alzheimer’s Disease Frontotemporal Lewy Bodies Vascular Traumatic Brain Injury Substance/Medication-Induced HIV Infection Prion Disease Parkinson’s Disease Huntington’s Disease Another Medical Condition Multiple Etiologies Unspecified q Specify: Without behavioral disturbance With behavioral disturbance (specify disturbance): If the cognitive disturbance is accompanied by a clinically significant behavioral disturbance (e. g. , psychotic symptoms, mood disturbance, agitation, apathy, or other behavioral symptoms). q Specify current severity: Mild: Difficulties with instrumental activities of daily living (e. g. , housework, managing money). Moderate: Difficulties with basic activities of daily living (e. g. , feeding, dressing). Severe: Fully dependent.
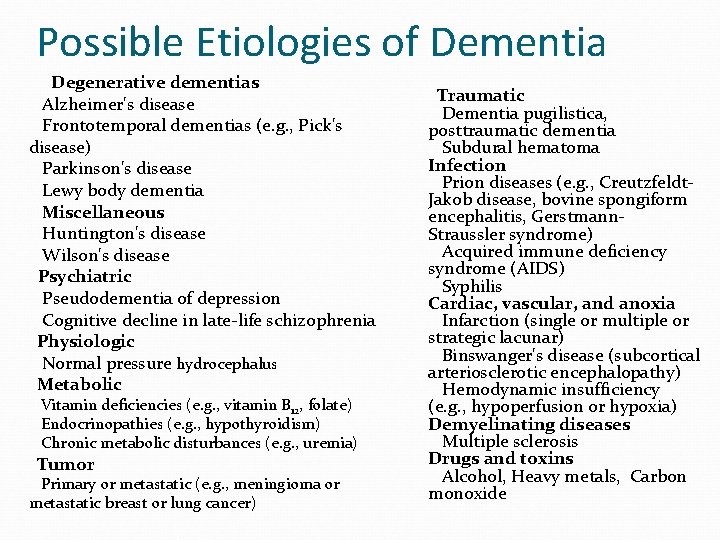
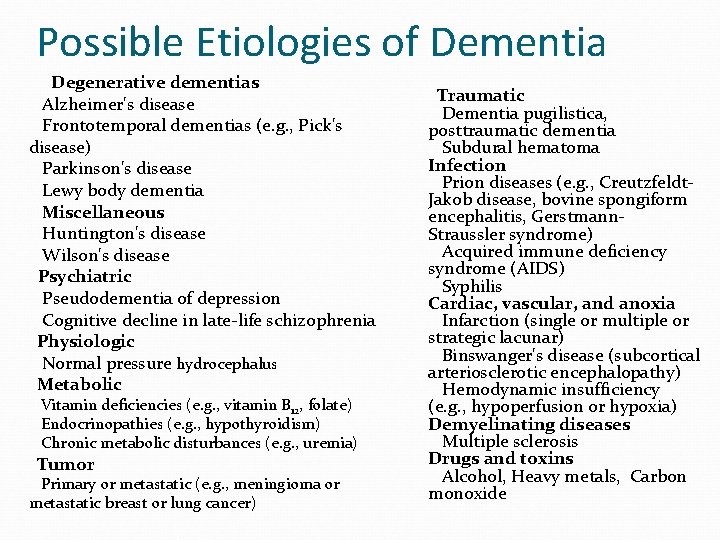
Possible Etiologies of Dementia Degenerative dementias Alzheimer's disease Frontotemporal dementias (e. g. , Pick's disease) Parkinson's disease Lewy body dementia Miscellaneous Huntington's disease Wilson's disease Psychiatric Pseudodementia of depression Cognitive decline in late-life schizophrenia Physiologic Normal pressure hydrocephalus Metabolic Vitamin deficiencies (e. g. , vitamin B 12, folate) Endocrinopathies (e. g. , hypothyroidism) Chronic metabolic disturbances (e. g. , uremia) Tumor Primary or metastatic (e. g. , meningioma or metastatic breast or lung cancer) Traumatic Dementia pugilistica, posttraumatic dementia Subdural hematoma Infection Prion diseases (e. g. , Creutzfeldt. Jakob disease, bovine spongiform encephalitis, Gerstmann. Straussler syndrome) Acquired immune deficiency syndrome (AIDS) Syphilis Cardiac, vascular, and anoxia Infarction (single or multiple or strategic lacunar) Binswanger's disease (subcortical arteriosclerotic encephalopathy) Hemodynamic insufficiency (e. g. , hypoperfusion or hypoxia) Demyelinating diseases Multiple sclerosis Drugs and toxins Alcohol, Heavy metals, Carbon monoxide
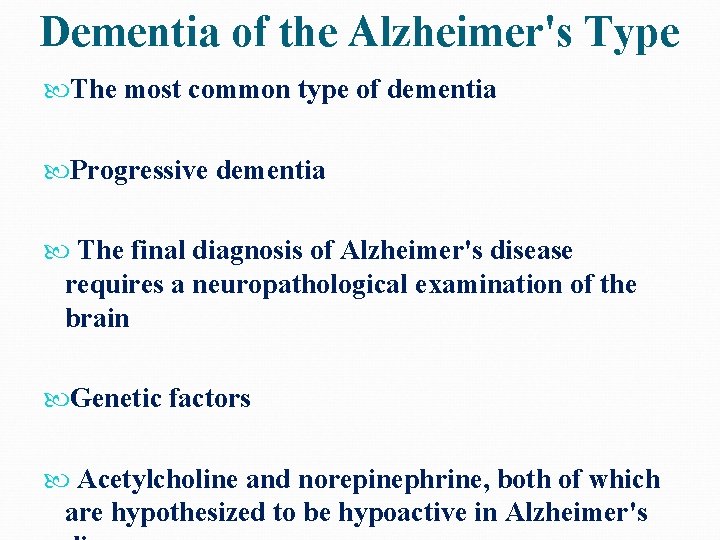
Dementia of the Alzheimer's Type The most common type of dementia Progressive dementia The final diagnosis of Alzheimer's disease requires a neuropathological examination of the brain Genetic factors Acetylcholine and norepinephrine, both of which are hypothesized to be hypoactive in Alzheimer's
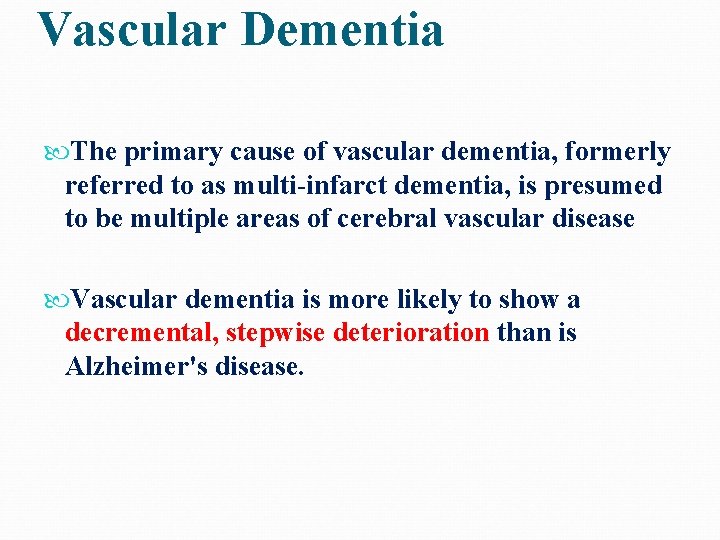
Vascular Dementia The primary cause of vascular dementia, formerly referred to as multi-infarct dementia, is presumed to be multiple areas of cerebral vascular disease Vascular dementia is more likely to show a decremental, stepwise deterioration than is Alzheimer's disease.
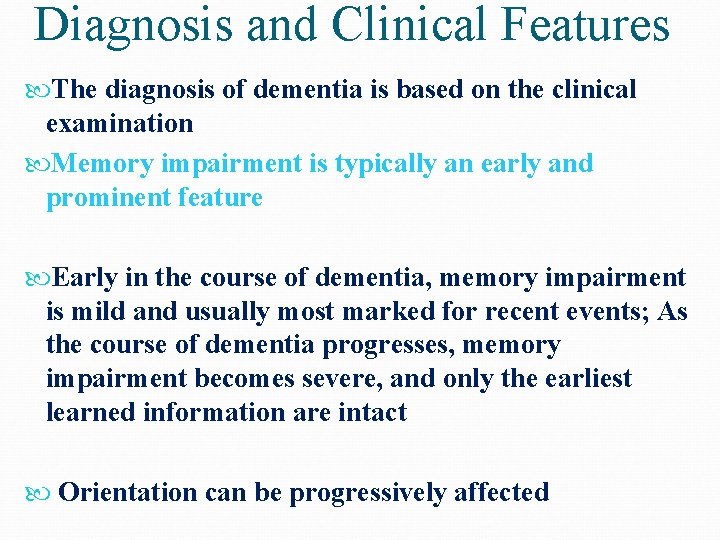
Diagnosis and Clinical Features The diagnosis of dementia is based on the clinical examination Memory impairment is typically an early and prominent feature Early in the course of dementia, memory impairment is mild and usually most marked for recent events; As the course of dementia progresses, memory impairment becomes severe, and only the earliest learned information are intact Orientation can be progressively affected
Personality change, intellectual impairment, forgetfulness, social withdrawal, anger and lability of emotions are common Hallucinations…………. 20 to 30 percent Delusions……………… 30 to 40 percent Physical aggression and other forms of violence are common in demented patients who also have psychotic symptoms. Depression and anxiety symptoms Pathological laughter or crying
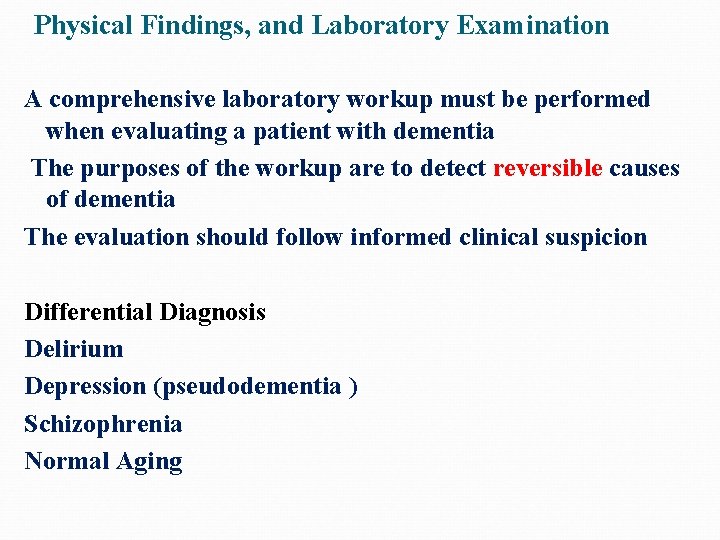
Physical Findings, and Laboratory Examination A comprehensive laboratory workup must be performed when evaluating a patient with dementia The purposes of the workup are to detect reversible causes of dementia The evaluation should follow informed clinical suspicion Differential Diagnosis Delirium Depression (pseudodementia ) Schizophrenia Normal Aging

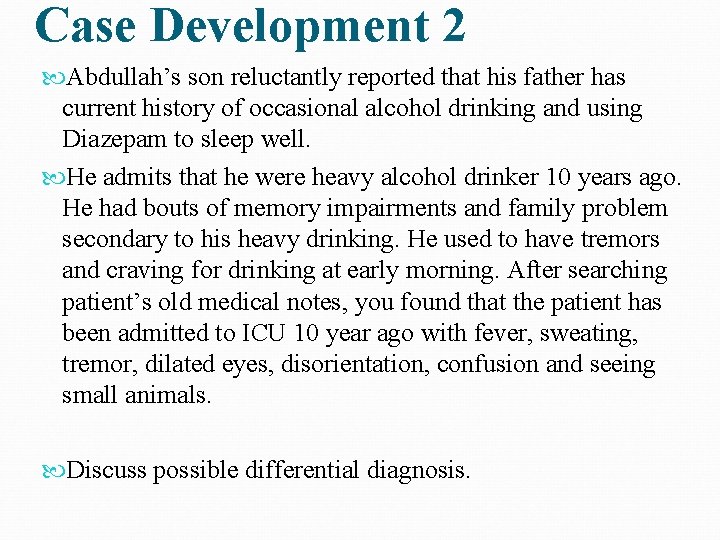
Case Development 2 Abdullah’s son reluctantly reported that his father has current history of occasional alcohol drinking and using Diazepam to sleep well. He admits that he were heavy alcohol drinker 10 years ago. He had bouts of memory impairments and family problem secondary to his heavy drinking. He used to have tremors and craving for drinking at early morning. After searching patient’s old medical notes, you found that the patient has been admitted to ICU 10 year ago with fever, sweating, tremor, dilated eyes, disorientation, confusion and seeing small animals. Discuss possible differential diagnosis.

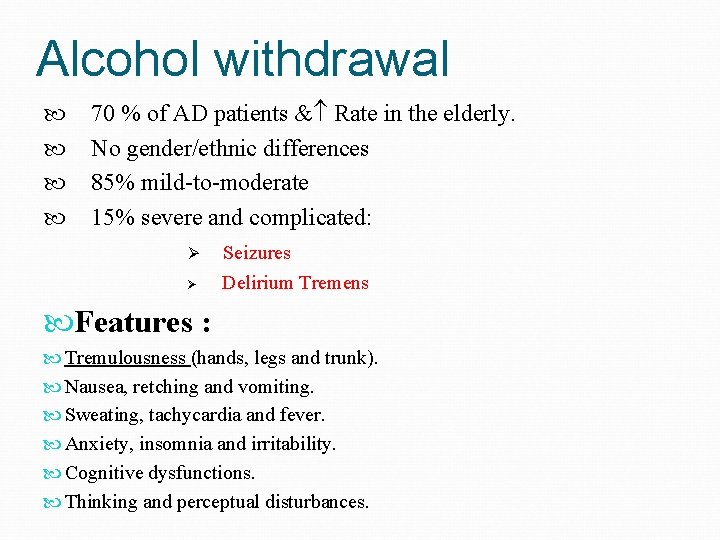
Alcohol withdrawal 70 % of AD patients & Rate in the elderly. No gender/ethnic differences 85% mild-to-moderate 15% severe and complicated: Ø Ø Seizures Delirium Tremens Features : Tremulousness (hands, legs and trunk). Nausea, retching and vomiting. Sweating, tachycardia and fever. Anxiety, insomnia and irritability. Cognitive dysfunctions. Thinking and perceptual disturbances.
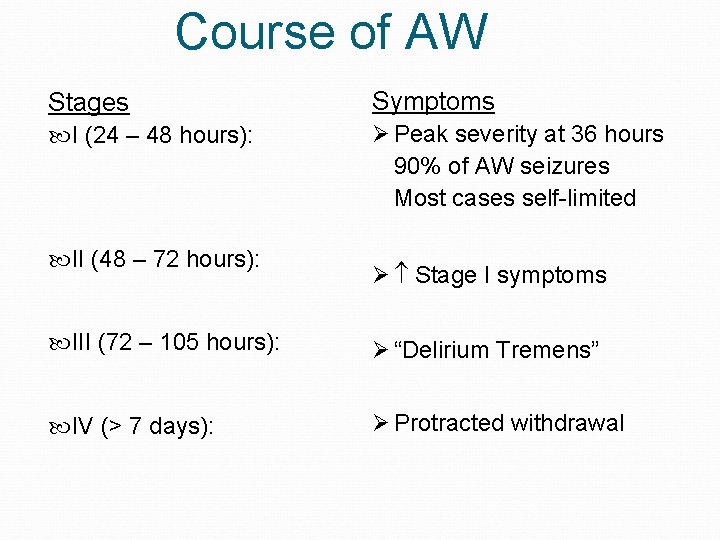
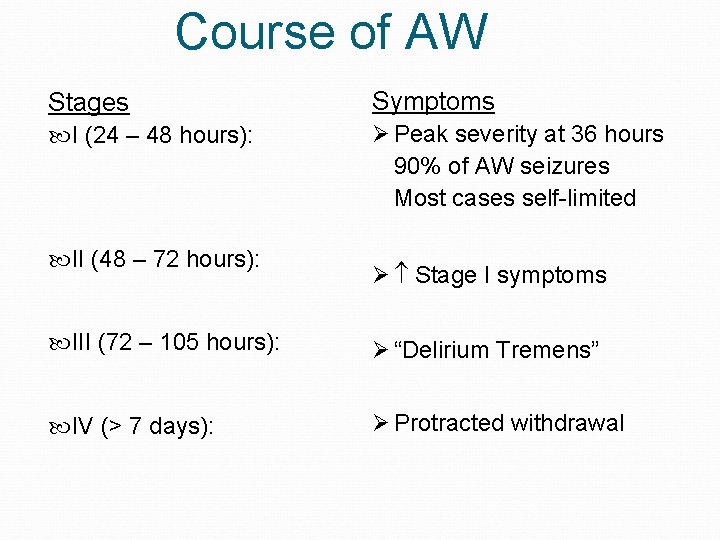
Course of AW Stages Symptoms I (24 – 48 hours): Ø Peak severity at 36 hours 90% of AW seizures Most cases self-limited II (48 – 72 hours): Ø Stage I symptoms III (72 – 105 hours): Ø “Delirium Tremens” IV (> 7 days): Ø Protracted withdrawal
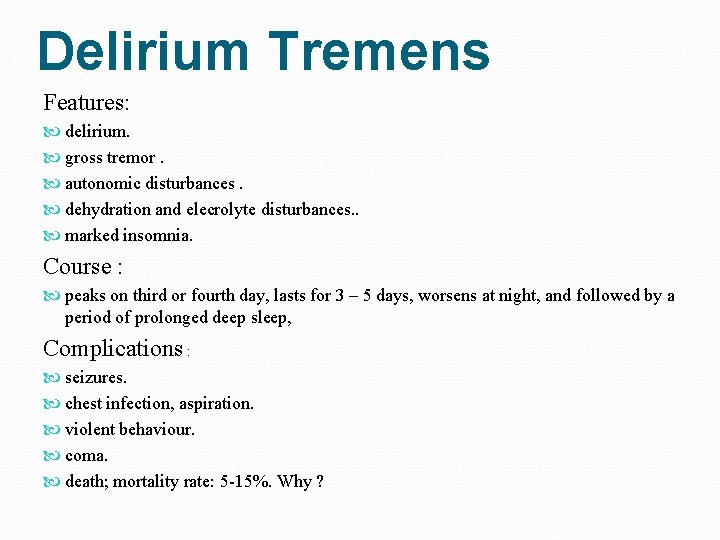
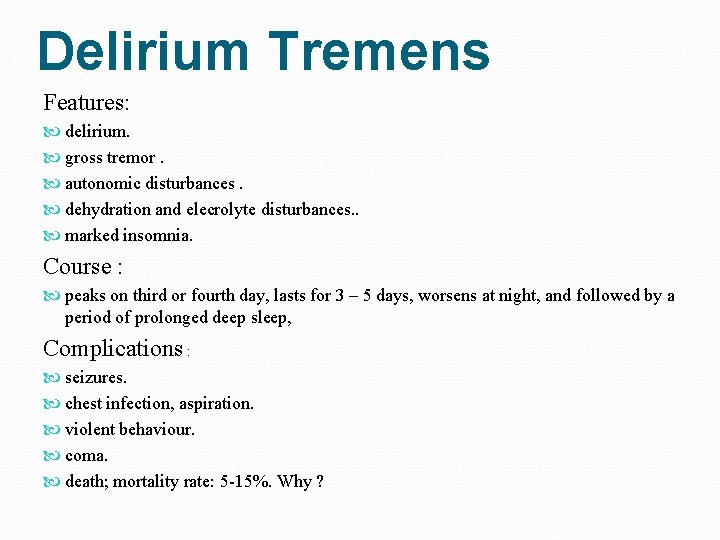
Delirium Tremens Features: delirium. gross tremor. autonomic disturbances. dehydration and elecrolyte disturbances. . marked insomnia. Course : peaks on third or fourth day, lasts for 3 – 5 days, worsens at night, and followed by a period of prolonged deep sleep, Complications : seizures. chest infection, aspiration. violent behaviour. coma. death; mortality rate: 5 -15%. Why ?
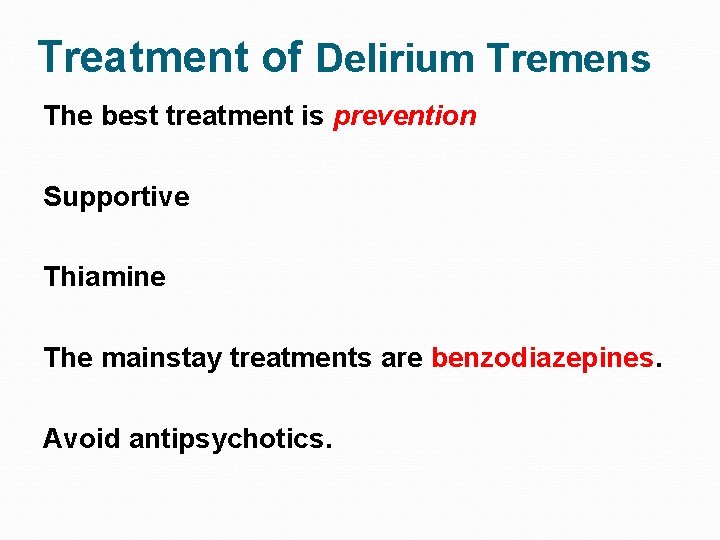
Treatment of Delirium Tremens The best treatment is prevention Supportive Thiamine The mainstay treatments are benzodiazepines. Avoid antipsychotics.
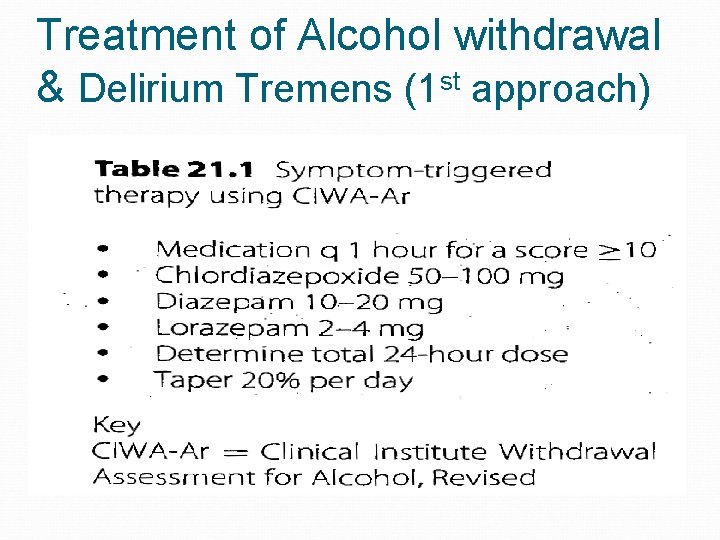
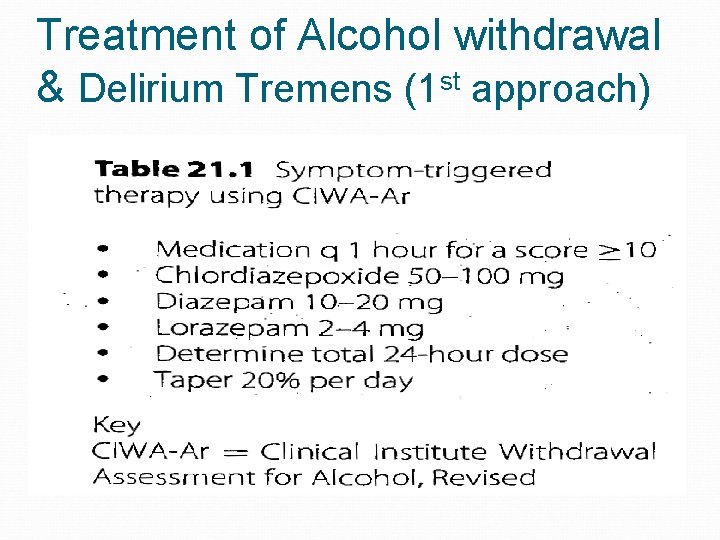
Treatment of Alcohol withdrawal & Delirium Tremens (1 st approach)
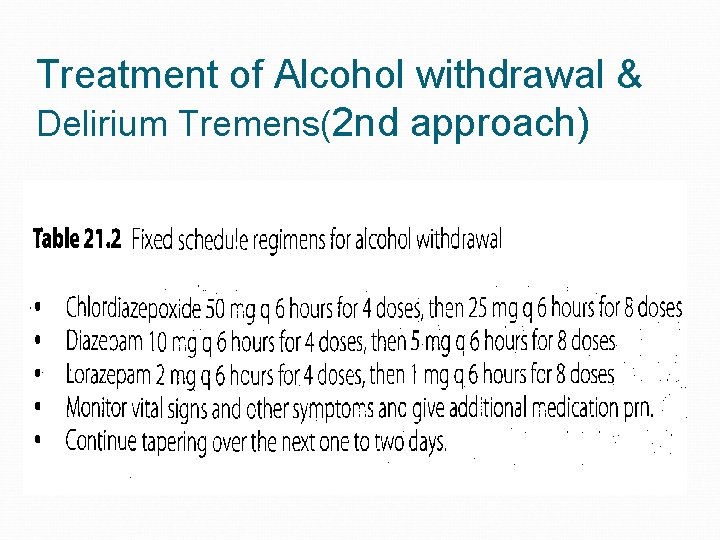
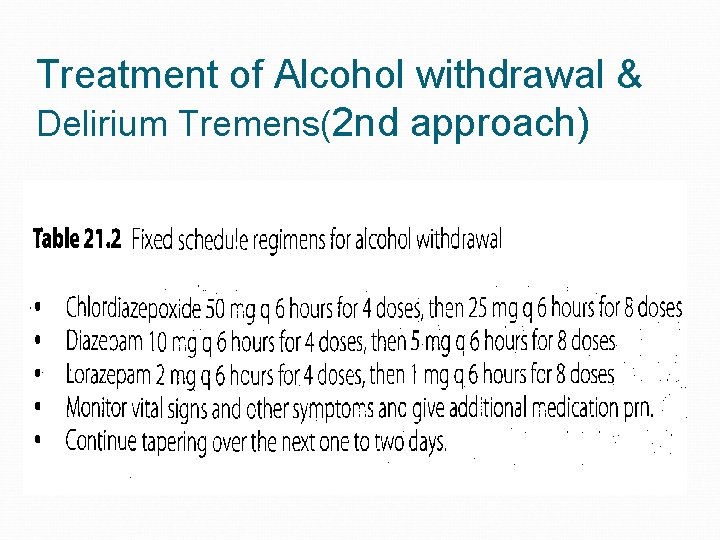
Treatment of Alcohol withdrawal & Delirium Tremens(2 nd approach)
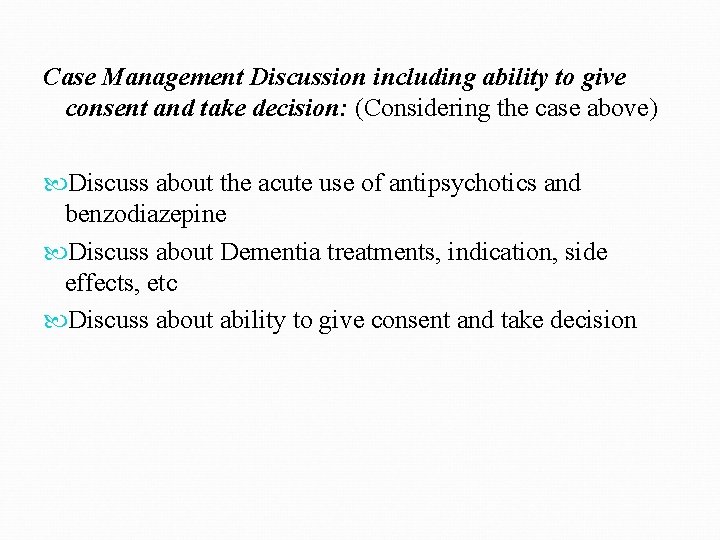
Case Management Discussion including ability to give consent and take decision: (Considering the case above) Discuss about the acute use of antipsychotics and benzodiazepine Discuss about Dementia treatments, indication, side effects, etc Discuss about ability to give consent and take decision
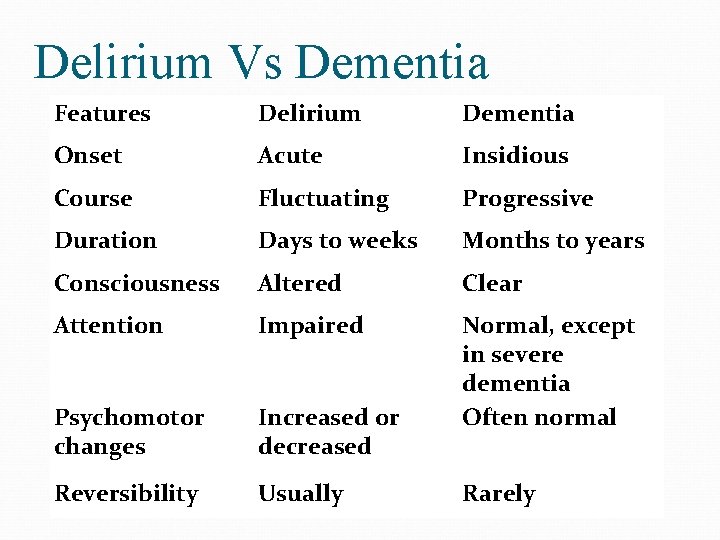
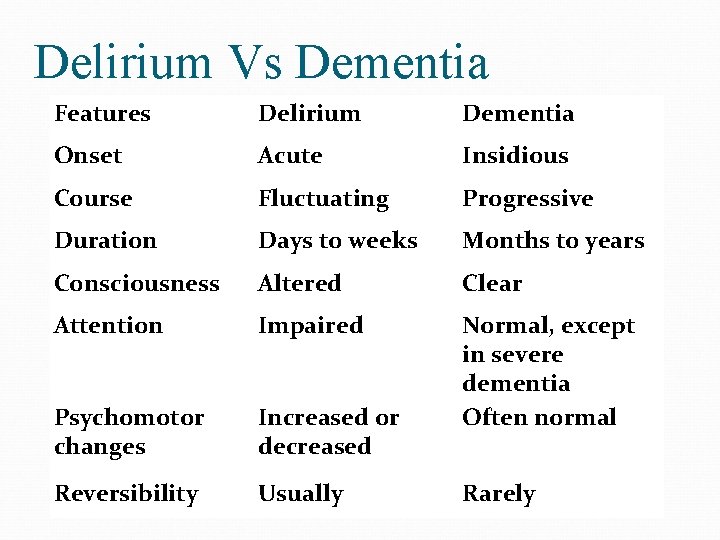
Delirium Vs Dementia Features Delirium Dementia Onset Acute Insidious Course Fluctuating Progressive Duration Days to weeks Months to years Consciousness Altered Clear Attention Impaired Psychomotor changes Increased or decreased Normal, except in severe dementia Often normal Reversibility Usually Rarely
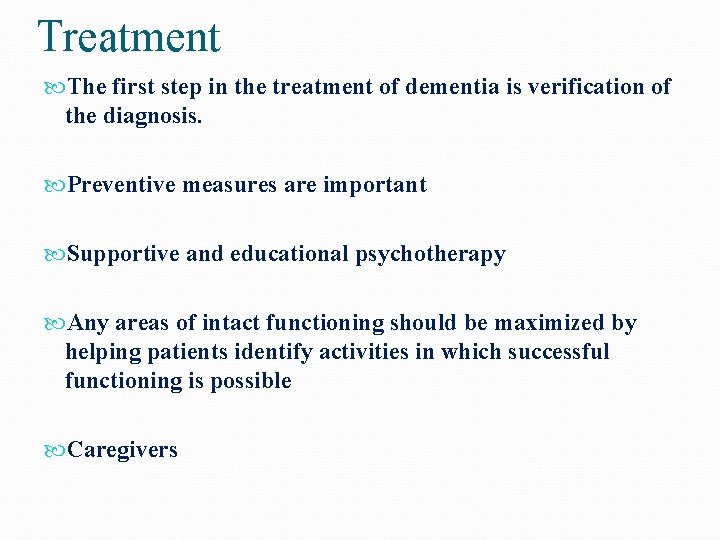
Treatment The first step in the treatment of dementia is verification of the diagnosis. Preventive measures are important Supportive and educational psychotherapy Any areas of intact functioning should be maximized by helping patients identify activities in which successful functioning is possible Caregivers
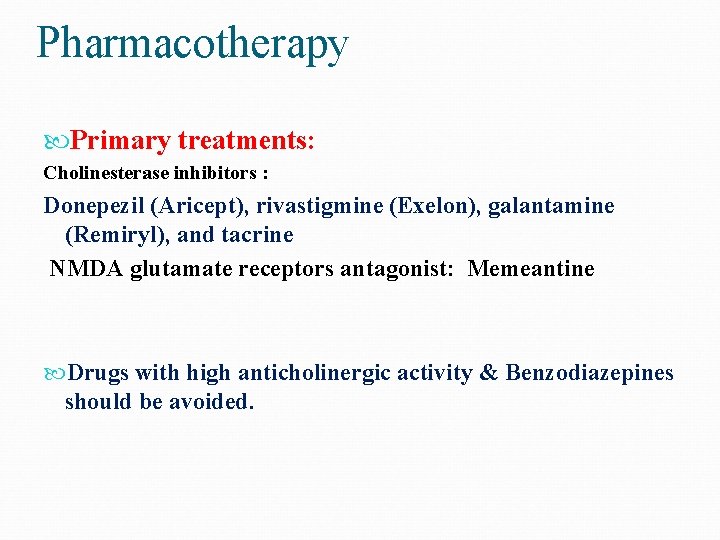
Pharmacotherapy Primary treatments: Cholinesterase inhibitors : Donepezil (Aricept), rivastigmine (Exelon), galantamine (Remiryl), and tacrine NMDA glutamate receptors antagonist: Memeantine Drugs with high anticholinergic activity & Benzodiazepines should be avoided.
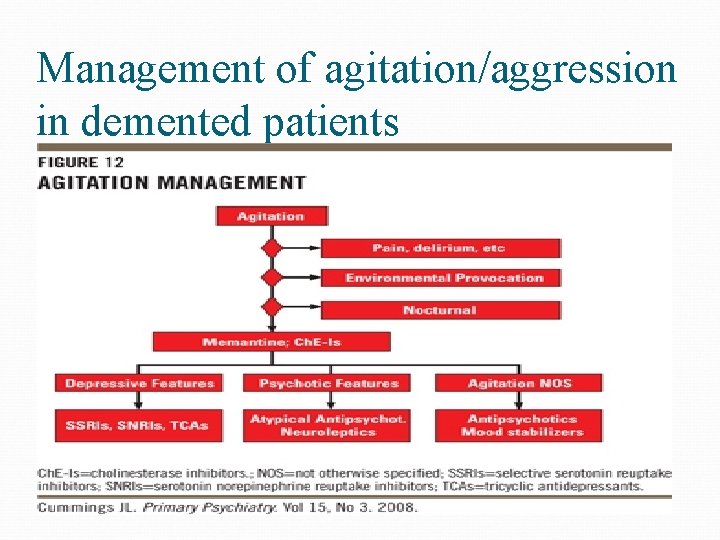
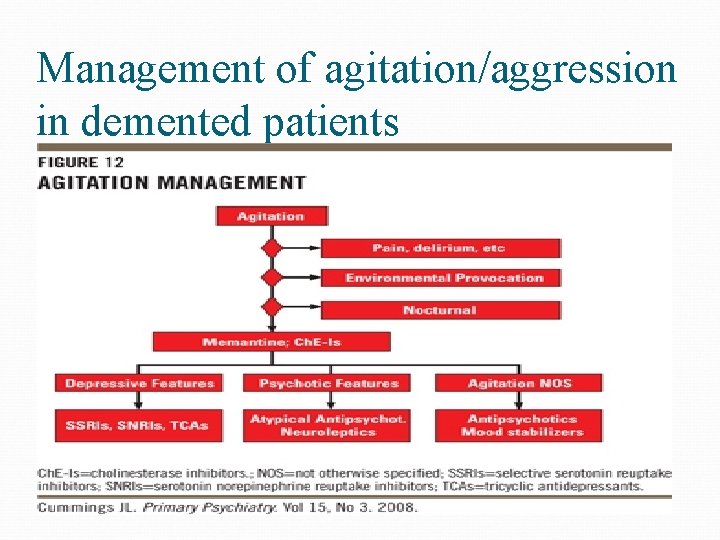
Management of agitation/aggression in demented patients
Capacity vs. Competency Clinical vs. Legal term that denotes the ability to make rational and reasonably well informed decisions by a particular patient (vs. person) in their treatment and/ or life decision/s Capacity is a clinical determination that addresses the integrity of mental functions. Competency is a legal determination that addresses societal interest in restricting a person’s right to make decisions or do acts because of incapacity.
Valid Informed Consent Permission voluntary given by a competent person without any elements of force, deceit, coercion after explanation and disclosure of 1. Purpose and details of procedure or treatment 2. Risks, Benefits and available alternative treatment/s 3. The right to withdrawal consent verbally or in written forms at anytime
Exceptions Life threatening situation Patient who waive their rights to disclose and consent (do not want to be informed) Instances where “ disclosure’ may be harmful to the patient “ Therapeutic privileges”
Rules of capacity Being mentally ill doesn’t in itself imply a loss of capacity or competency. Having Capacity or being Competent should be presumed until proven otherwise.
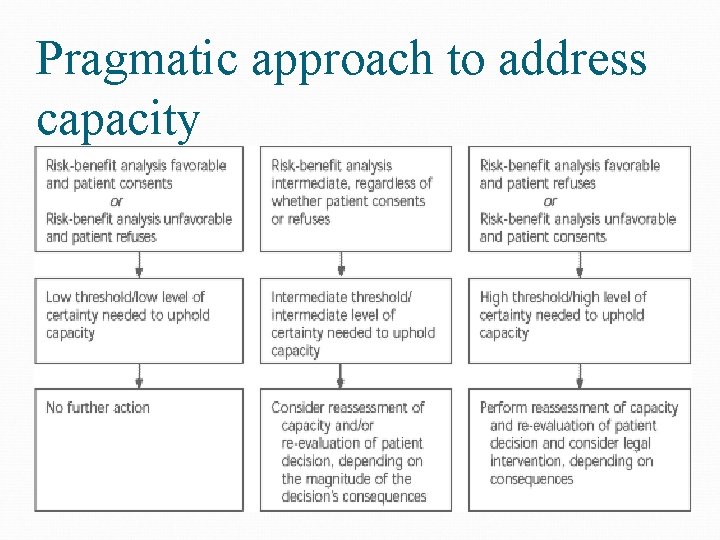
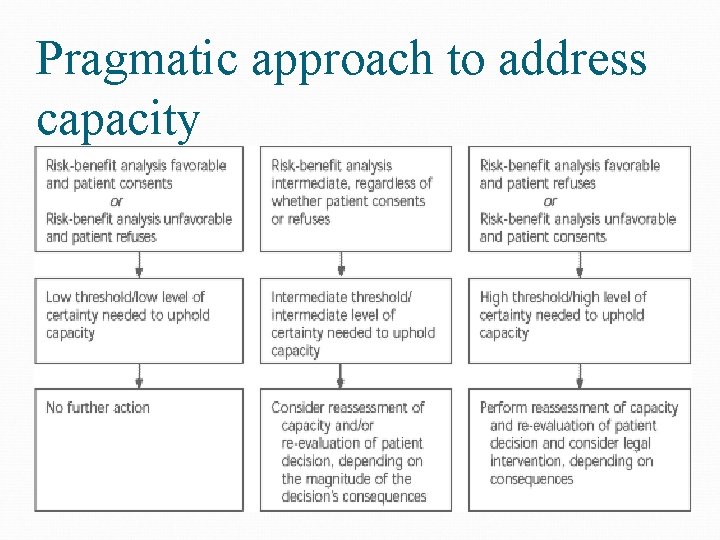
Pragmatic approach to address capacity
Steps in Mental Capacity Assessment A. General perspective or specific (Psychiatric hospitalization, ECT) Find out the best language of communication Determine if patient has adequate information on which to base a decision MMSE: attention, concentration, memory Inform the patient about the nature of the disorder, AND the risk and benefit of the PROPOSED treatment, and of ALTERNATIVE treatments or of NO treatment B. Repeat information number of times and in different ways. Let the patient paraphrase or restate the understanding. Evaluate nature of questions that patient asks regarding treatment plan Periodical Reassessment of capacity ( if any change in clinical conditions or, mental status such as in delirium or any modifications in treatment plan) C. If patient has “severe deficit” in understanding information- No Capacity to make informed consent or make decision Arrange a process for “ a substitute decision maker”


 Fahad alosaimi
Fahad alosaimi Psychosomatic
Psychosomatic Fahad subhi mohammed
Fahad subhi mohammed Cognitive and non cognitive religious language
Cognitive and non cognitive religious language European psychiatry
European psychiatry Pediprn
Pediprn Addiction expert witness
Addiction expert witness Who is this
Who is this Asclepiades father of psychiatry
Asclepiades father of psychiatry Psychiatry in ethiopia
Psychiatry in ethiopia Radical psychiatry sociology
Radical psychiatry sociology Community geriatric psychiatry
Community geriatric psychiatry Site:slidetodoc.com
Site:slidetodoc.com What is forensic psychiatry
What is forensic psychiatry Jamaica hospital psychiatry residency
Jamaica hospital psychiatry residency Psychiatric assessment
Psychiatric assessment Core psychiatry
Core psychiatry Obgyn shelf percentiles
Obgyn shelf percentiles Gipsofia
Gipsofia What is criminal psychology definition
What is criminal psychology definition Geriatric psychiatry definition
Geriatric psychiatry definition National network of child psychiatry access programs
National network of child psychiatry access programs What is the theme for theme for english b
What is the theme for theme for english b Theme or genre
Theme or genre What is the difference between theme and universal theme?
What is the difference between theme and universal theme? Example of universal theme
Example of universal theme Nursing management of sleep disorders
Nursing management of sleep disorders Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Seborrheic keratoses
Seborrheic keratoses York eating disorders service
York eating disorders service Types of somatic disorder
Types of somatic disorder Tromboemboly
Tromboemboly Chapter 18 psychological disorders review worksheet
Chapter 18 psychological disorders review worksheet Eczema icd 10
Eczema icd 10 Bipolar
Bipolar Chromosome deletion definition
Chromosome deletion definition Paraphilic
Paraphilic Assistive technology for emotional and behavioral disorders
Assistive technology for emotional and behavioral disorders The assistant chapter 40
The assistant chapter 40 Eating disorders in uae
Eating disorders in uae Bipolar and other related disorders
Bipolar and other related disorders Looney tunes speech impediments
Looney tunes speech impediments Chapter 12 schizophrenia spectrum disorders
Chapter 12 schizophrenia spectrum disorders The uk national disorders
The uk national disorders Gross
Gross Neurocognitive disorder
Neurocognitive disorder Sleep disorders
Sleep disorders Dominant gene disorders
Dominant gene disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 10 nail disorders and diseases
Chapter 10 nail disorders and diseases Mood disorders dsm 5
Mood disorders dsm 5 Cluster c
Cluster c Thought broadcasting
Thought broadcasting Behavior disorders
Behavior disorders Avoidant personality disorder
Avoidant personality disorder Type c personality disorder
Type c personality disorder Communication disorders (dsm-5 ppt)
Communication disorders (dsm-5 ppt) Nursing care of male patients with genitourinary disorders
Nursing care of male patients with genitourinary disorders Neurosis vs psychosis
Neurosis vs psychosis Bandl's ring
Bandl's ring Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Sample dsm-5 diagnosis format
Sample dsm-5 diagnosis format Physiological disorders and their care
Physiological disorders and their care Anxiety disorders def
Anxiety disorders def