Psychotic disorders theme FAHAD ALOSAIMI MD psychiatry and







- Slides: 50
Psychotic disorders theme FAHAD ALOSAIMI MD psychiatry and psychosomatic medicine consultant Associate professor KSU, Riyadh
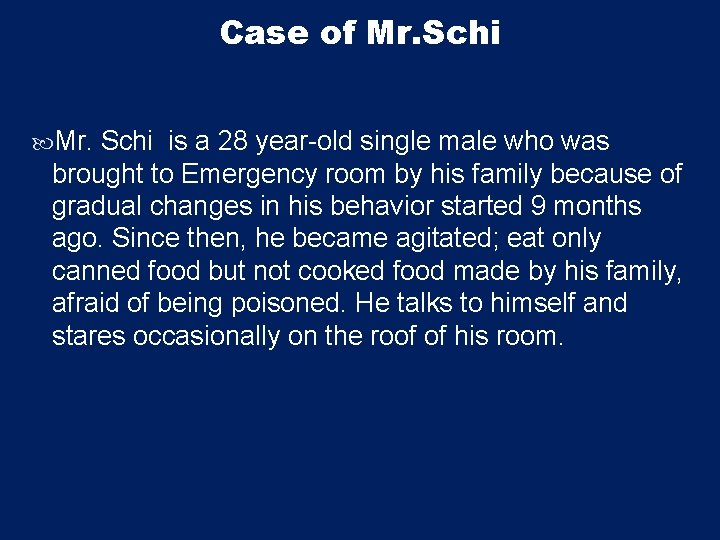
Case of Mr. Schi is a 28 year-old single male who was brought to Emergency room by his family because of gradual changes in his behavior started 9 months ago. Since then, he became agitated; eat only canned food but not cooked food made by his family, afraid of being poisoned. He talks to himself and stares occasionally on the roof of his room.
Case of Mr. Schi He had two brief psychiatric hospitalizations in last 3 years that were precipitated by anger at his neighbor and voices commenting about his behavior. His personal history indicated that he was a healthy child, but his parents report that he was a bed wetter and seemed slower to develop than his brothers and sisters.
Analyze the symptoms & signs, both presented and expected in this case including mood, thoughts, cognition, perception and physical aspects. Discuss possible etiological reasons Discuss differential diagnosis
Schizophrenia - It is not a single disease but a group of disorders with heterogeneous etiologies. - Found in all societies and countries with equal prevalence & incidence worldwide. - A life prevalence of 0. 6 – 1. 9 % - Annual incidence of 0. 5 – 5. 0 per 10, 000 - Peak age of onset are 10 -25 years for ♂ & 25 -35 years for ♀
http: //image. slidesharecdn. com/schizophrenia 1 -090716160801 -phpapp 02/95/schizophrenia 1 -5 -728. jpg? cb=1247760507
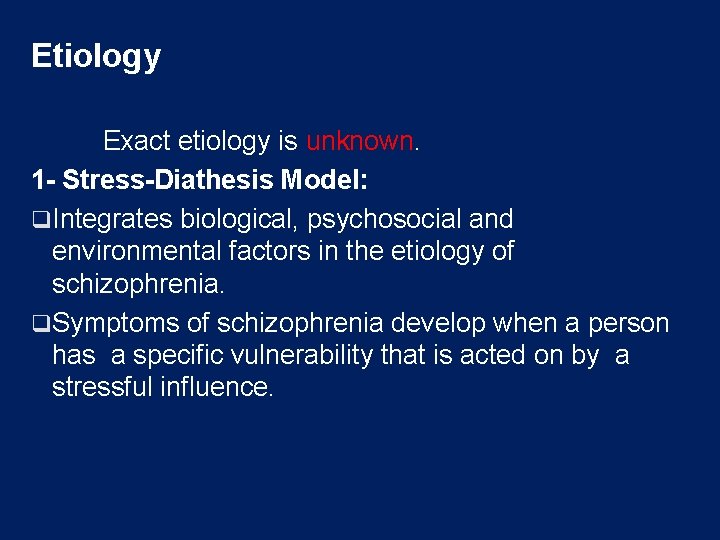
Etiology Exact etiology is unknown. 1 - Stress-Diathesis Model: q. Integrates biological, psychosocial and environmental factors in the etiology of schizophrenia. q. Symptoms of schizophrenia develop when a person has a specific vulnerability that is acted on by a stressful influence.
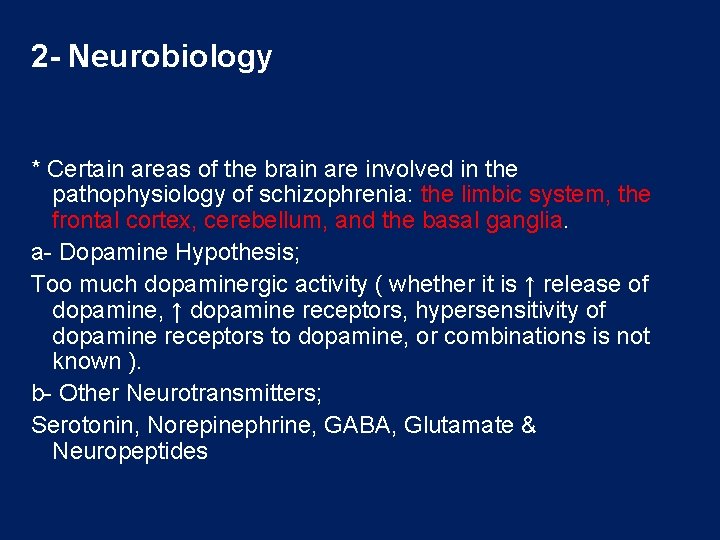
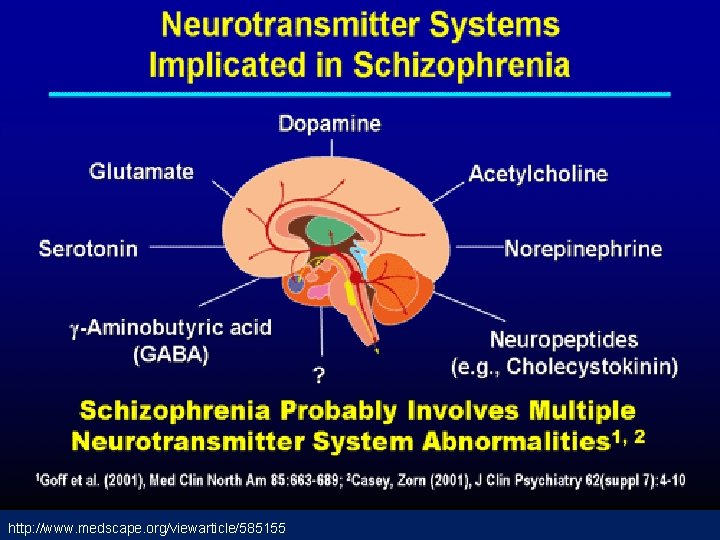
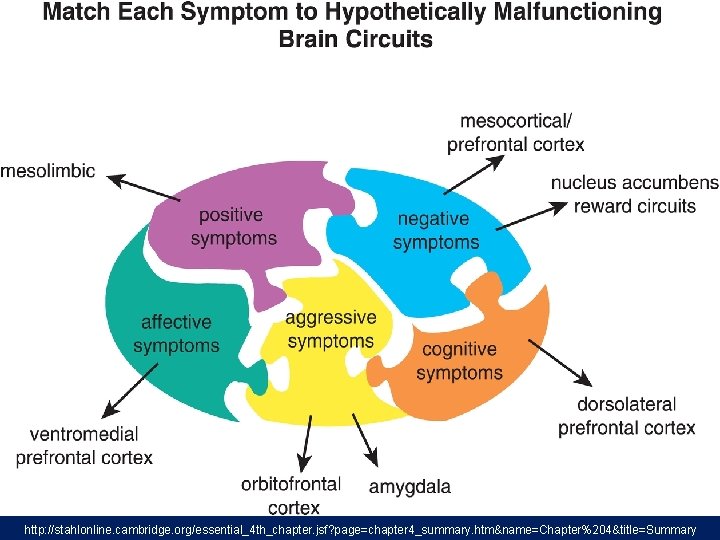
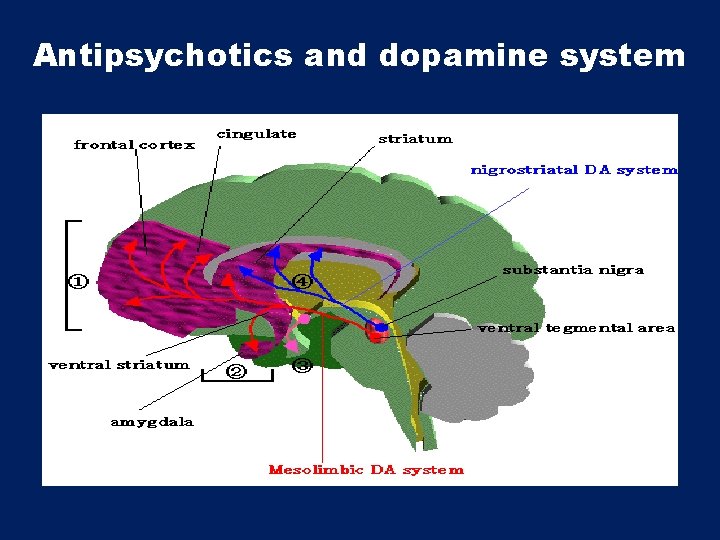
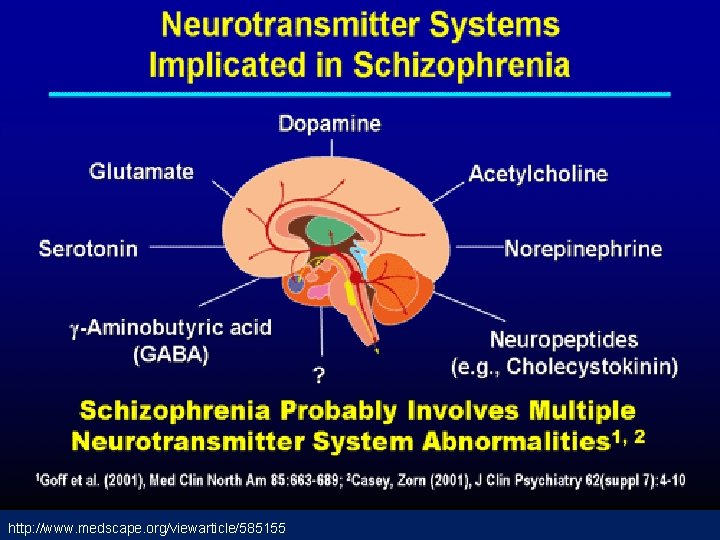
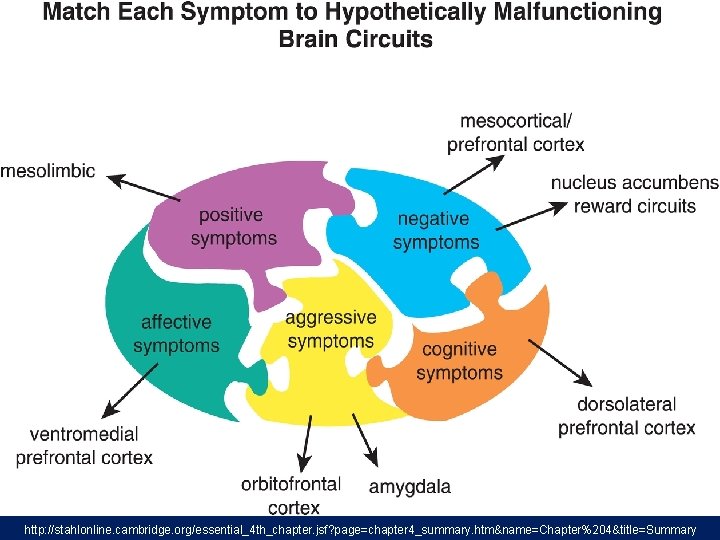
2 - Neurobiology * Certain areas of the brain are involved in the pathophysiology of schizophrenia: the limbic system, the frontal cortex, cerebellum, and the basal ganglia. a- Dopamine Hypothesis; Too much dopaminergic activity ( whether it is ↑ release of dopamine, ↑ dopamine receptors, hypersensitivity of dopamine receptors to dopamine, or combinations is not known ). b- Other Neurotransmitters; Serotonin, Norepinephrine, GABA, Glutamate & Neuropeptides
http: //www. medscape. org/viewarticle/585155


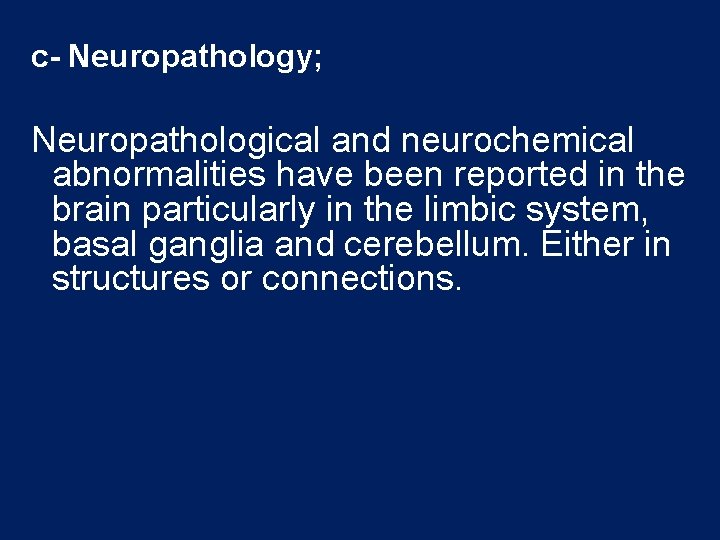
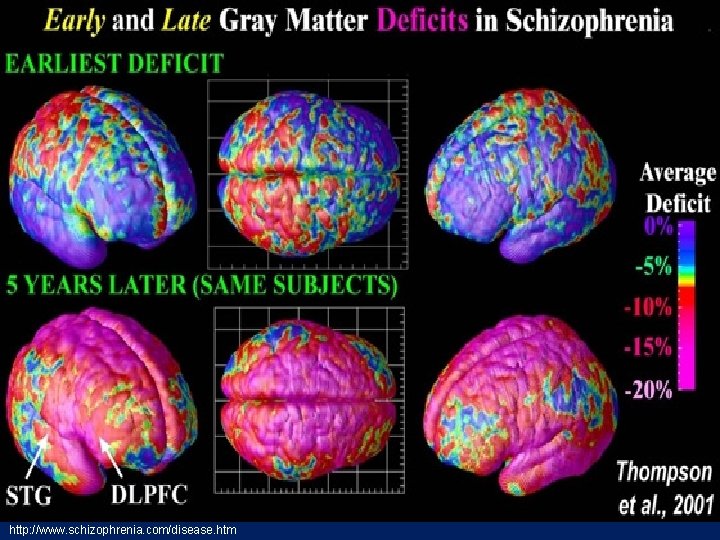
c- Neuropathology; Neuropathological and neurochemical abnormalities have been reported in the brain particularly in the limbic system, basal ganglia and cerebellum. Either in structures or connections.
http: //stahlonline. cambridge. org/essential_4 th_chapter. jsf? page=chapter 4_summary. htm&name=Chapter%204&title=Summary
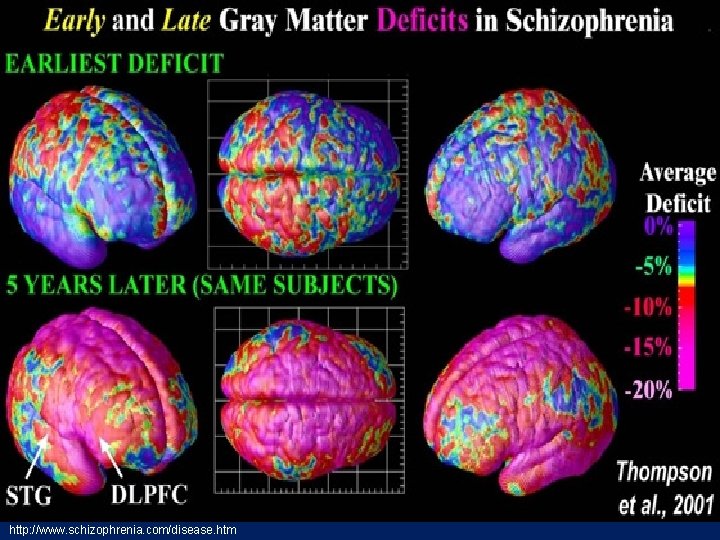
http: //www. schizophrenia. com/disease. htm
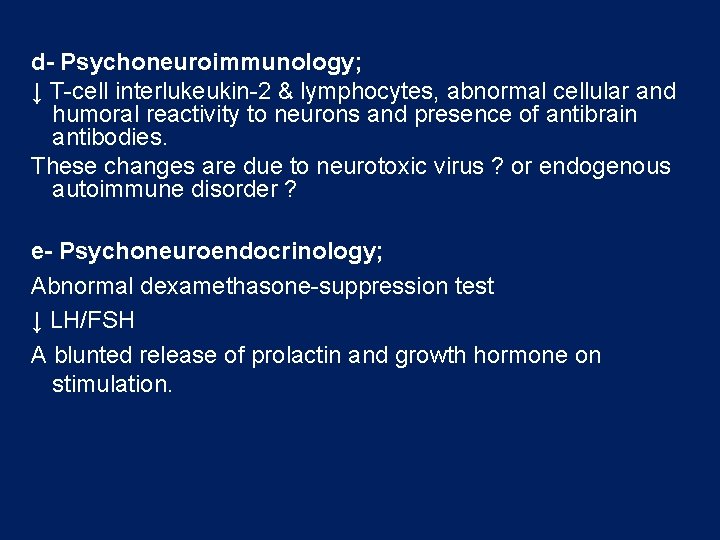
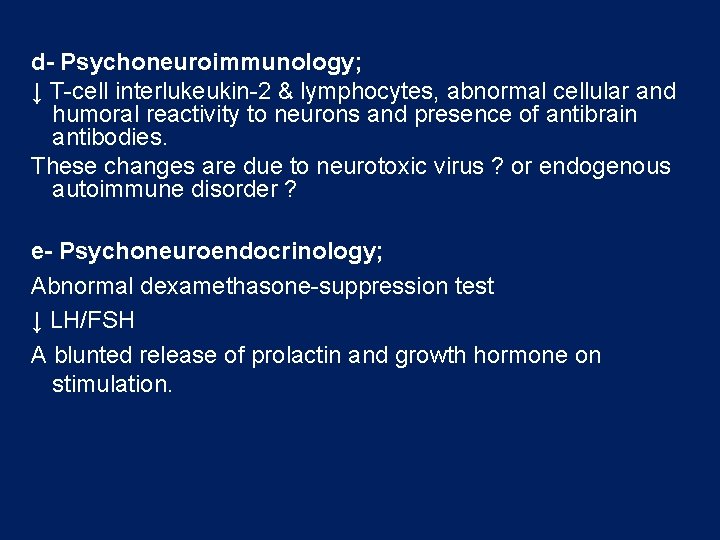
d- Psychoneuroimmunology; ↓ T-cell interlukeukin-2 & lymphocytes, abnormal cellular and humoral reactivity to neurons and presence of antibrain antibodies. These changes are due to neurotoxic virus ? or endogenous autoimmune disorder ? e- Psychoneuroendocrinology; Abnormal dexamethasone-suppression test ↓ LH/FSH A blunted release of prolactin and growth hormone on stimulation.
3 - Genetic Factors - A wide range of genetic studies strongly suggest a genetic component to the inheritance of schizophrenia that outweights the environmental influence. - These include: family studies, twin studies and chromosomal studies.

4 - Psychosocial Factors: q. In family dynamics studies, no well-controlled evidence indicates specific family pattern plays a causative role in the development of schizophrenia. q. High Expressed Emotion family : increase risk of relapse.
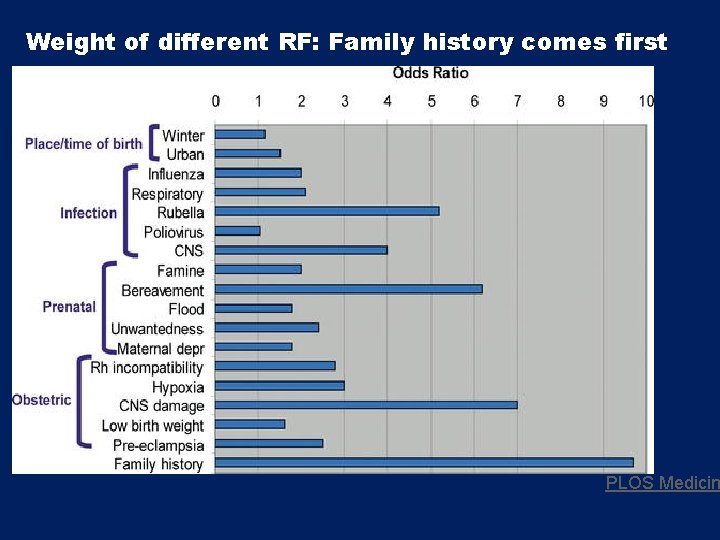
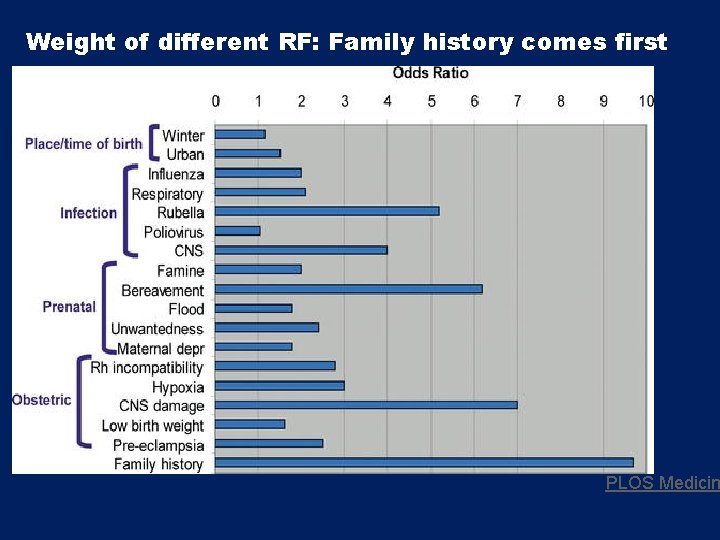
Weight of different RF: Family history comes first PLOS Medicin
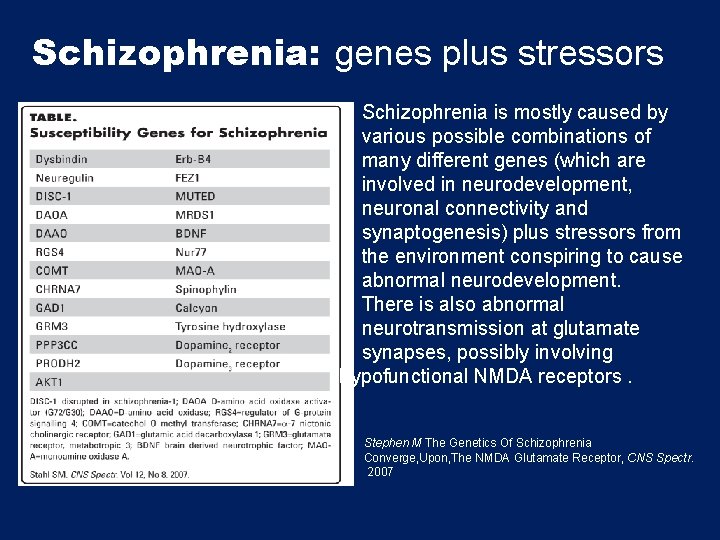
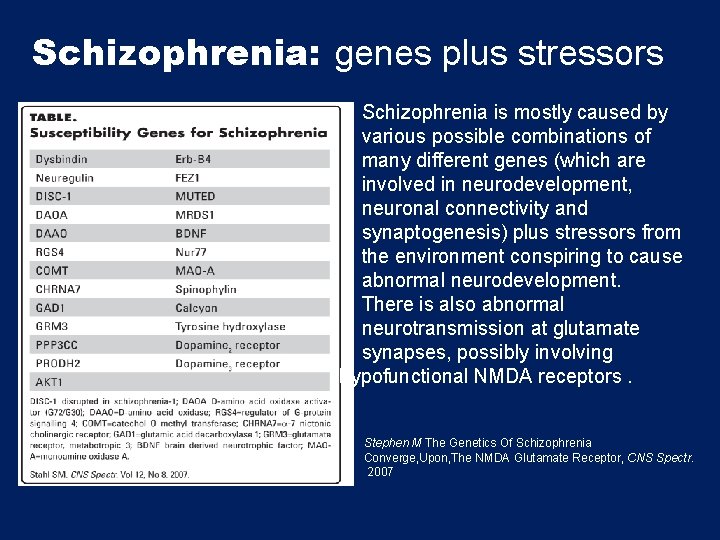
Schizophrenia: genes plus stressors Schizophrenia is mostly caused by various possible combinations of many different genes (which are involved in neurodevelopment, neuronal connectivity and synaptogenesis) plus stressors from the environment conspiring to cause abnormal neurodevelopment. There is also abnormal neurotransmission at glutamate synapses, possibly involving hypofunctional NMDA receptors. Stephen M The Genetics Of Schizophrenia Converge, Upon, The NMDA Glutamate Receptor, CNS Spectr. 2007
Diagnosis # DSM-5 Diagnostic Criteria for Schizophrenia: A- ≥ two characteristic symptoms for one month, at least one of them is (1), (2) or (3) 1 - Delusions 2 - Hallucinations 3 - Disorganized speech (frequent derailment or incoherence) 4 - Grossly disorganized or catatonic behavior 5 - Negative symptoms ( diminished emotional expression or lack of drive (avolition))
B- Social, Occupation or self-care dysfunction C- Duration of at least 6 months of disturbance (include at least one month of active symptoms that meet Criterion A; in addition of periods of prodromal and residual symptoms). D- Schizoaffective & mood disorder exclusion E- The disturbance is not due to Substance or another medical condition. F- If there is history of autism spectrum disorder or a communication disorder of childhood onset, schizophrenia diagnosis is made only if delusion or hallucinations plus other criteria are present.
Clinical Features q. No single clinical sign or symptom is pathognomonic for schizophrenia q. Patient's history & mental status examination are essential for diagnosis. q Premorbid history includes schizoid or schizotypal personalities, few friends & exclusion of social activities. q Prodromal features include obsessive compulsive behaviors , attenuated positive psychotic features.
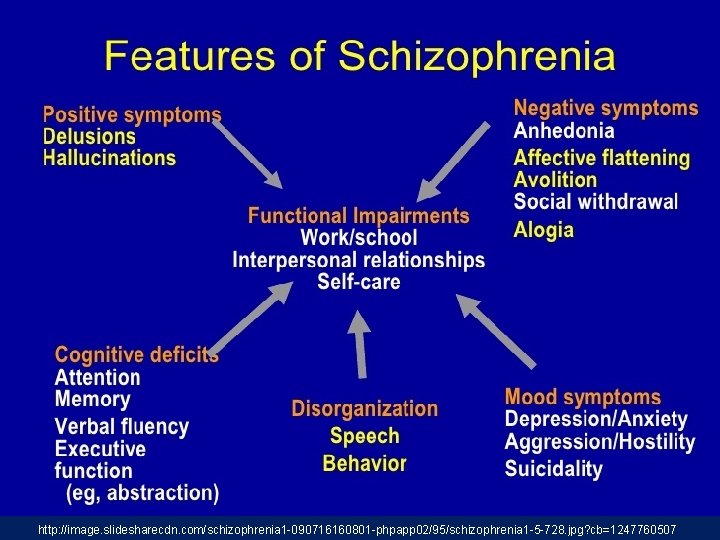
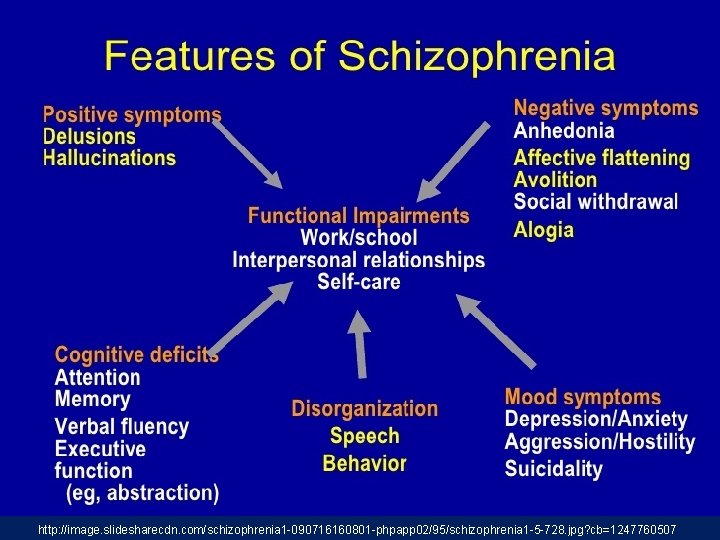
- Picture of schizophrenia includes positive and negative symptoms. - Positive symptoms like: delusions & hallucinations. - Negative symptoms like: affective flattening or blunting, poverty of speech, poor grooming, lack of motivation, and social withdrawal.
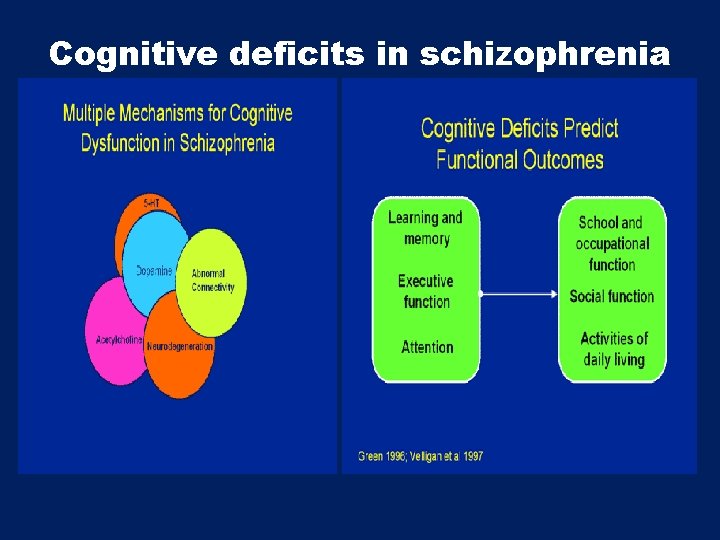
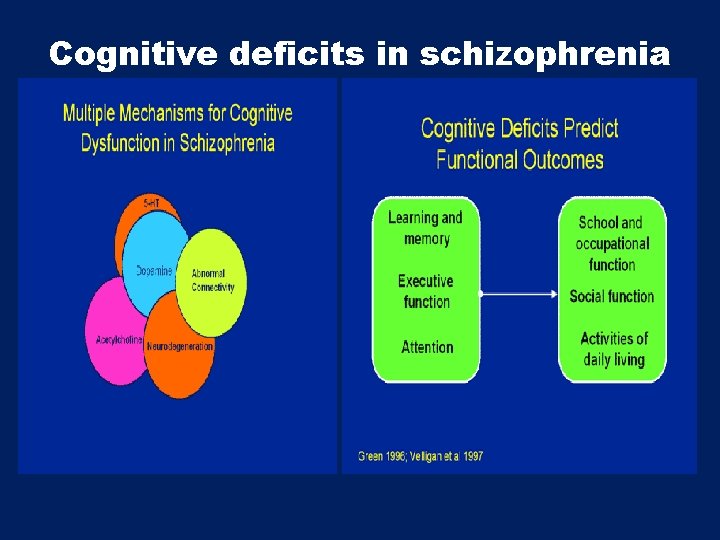
Cognitive deficits in schizophrenia
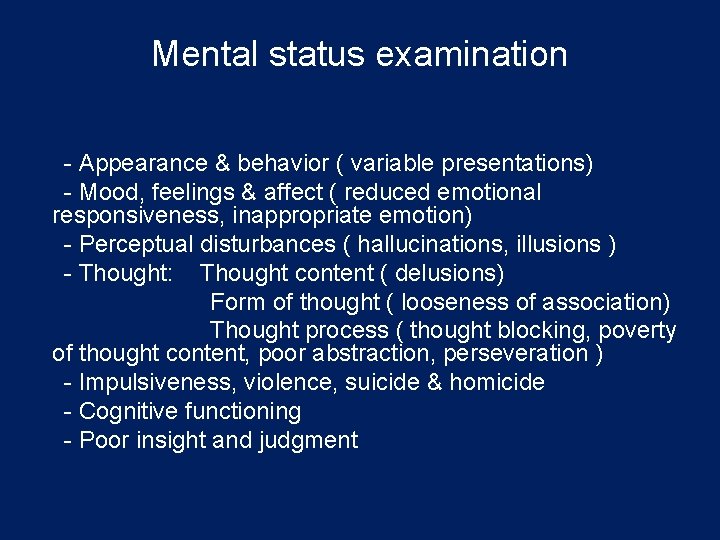
Mental status examination - Appearance & behavior ( variable presentations) - Mood, feelings & affect ( reduced emotional responsiveness, inappropriate emotion) - Perceptual disturbances ( hallucinations, illusions ) - Thought: Thought content ( delusions) Form of thought ( looseness of association) Thought process ( thought blocking, poverty of thought content, poor abstraction, perseveration ) - Impulsiveness, violence, suicide & homicide - Cognitive functioning - Poor insight and judgment
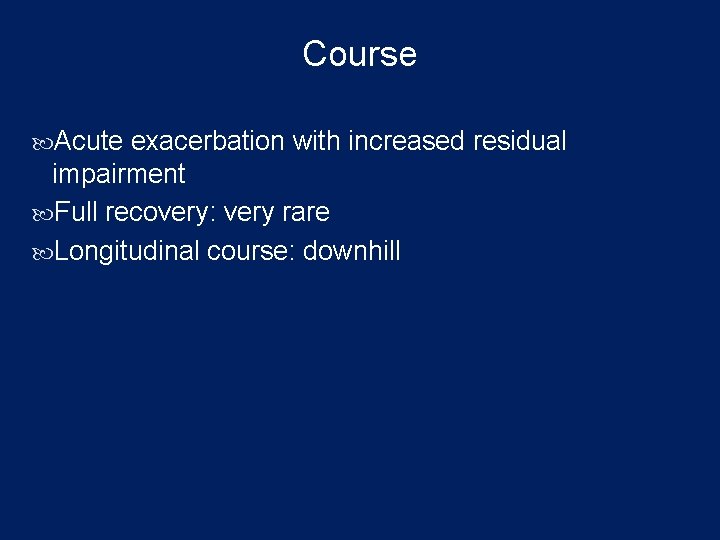
Course Acute exacerbation with increased residual impairment Full recovery: very rare Longitudinal course: downhill

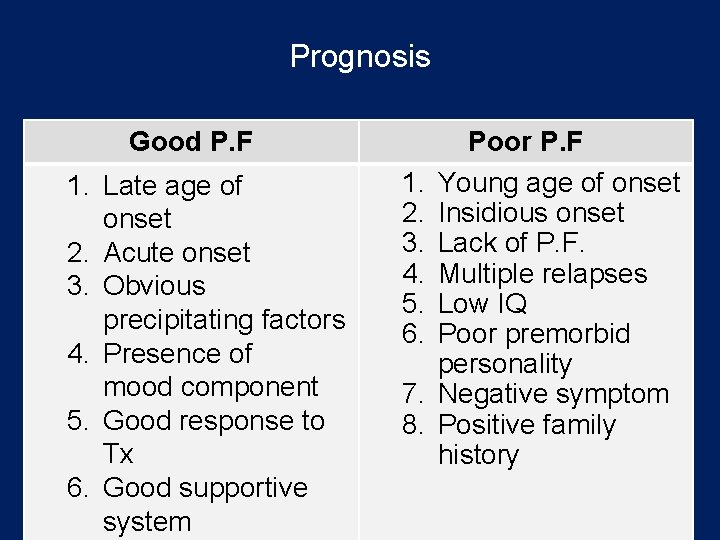
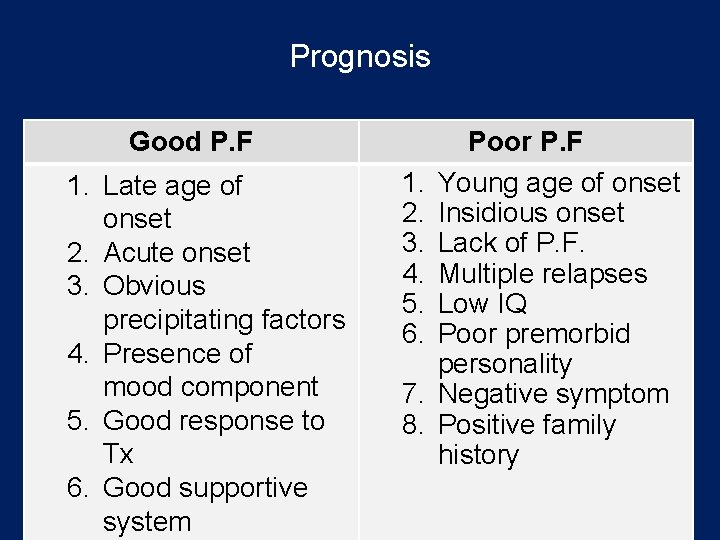
Prognosis Good P. F 1. Late age of onset 2. Acute onset 3. Obvious precipitating factors 4. Presence of mood component 5. Good response to Tx 6. Good supportive system 1. 2. 3. 4. 5. 6. 7. 8. Poor P. F Young age of onset Insidious onset Lack of P. F. Multiple relapses Low IQ Poor premorbid personality Negative symptom Positive family history
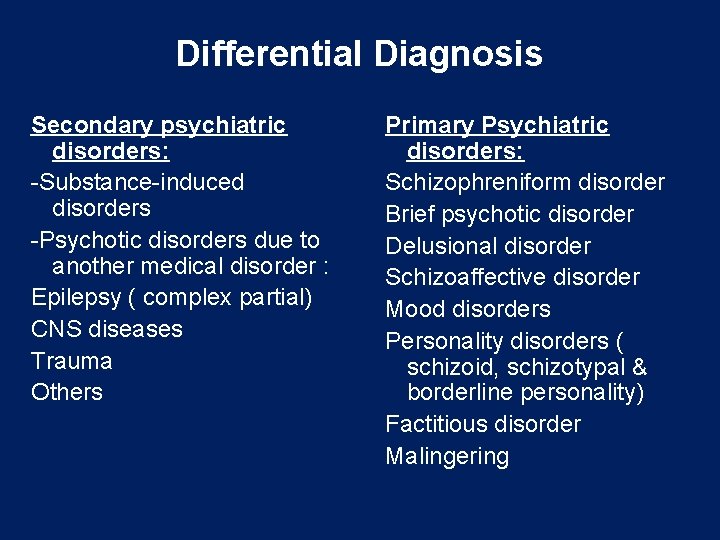
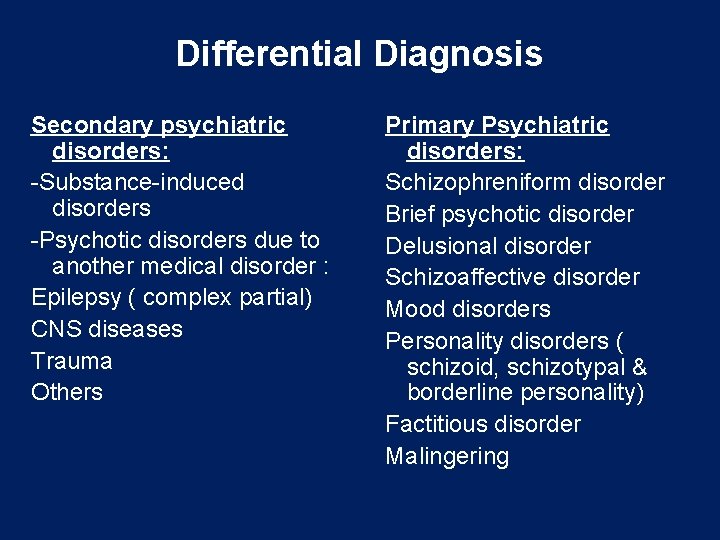
Differential Diagnosis Secondary psychiatric disorders: -Substance-induced disorders -Psychotic disorders due to another medical disorder : Epilepsy ( complex partial) CNS diseases Trauma Others Primary Psychiatric disorders: Schizophreniform disorder Brief psychotic disorder Delusional disorder Schizoaffective disorder Mood disorders Personality disorders ( schizoid, schizotypal & borderline personality) Factitious disorder Malingering
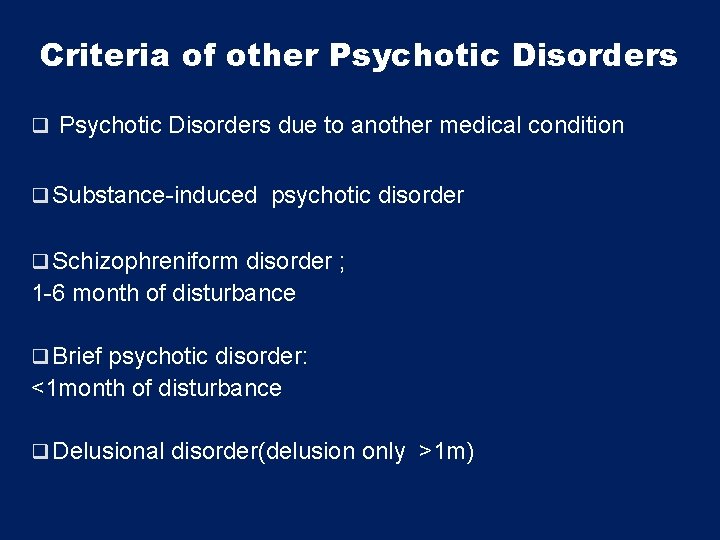
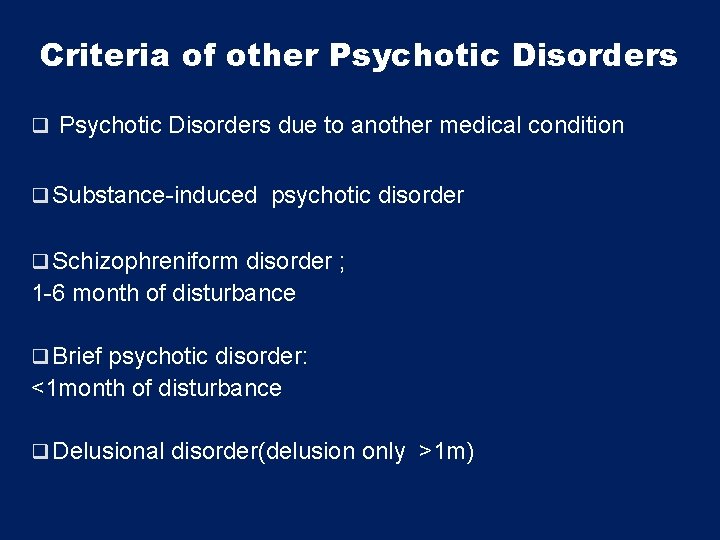
Criteria of other Psychotic Disorders q Psychotic Disorders due to another medical condition q Substance-induced psychotic disorder q Schizophreniform disorder ; 1 -6 month of disturbance q Brief psychotic disorder: <1 month of disturbance q Delusional disorder(delusion only >1 m)
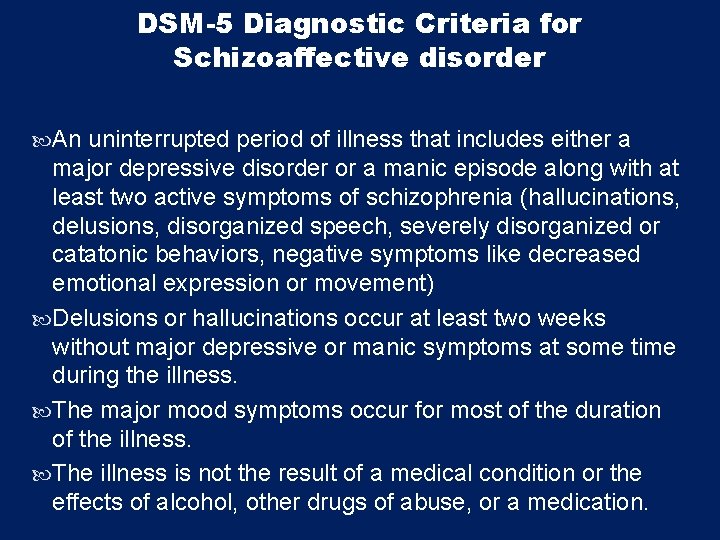
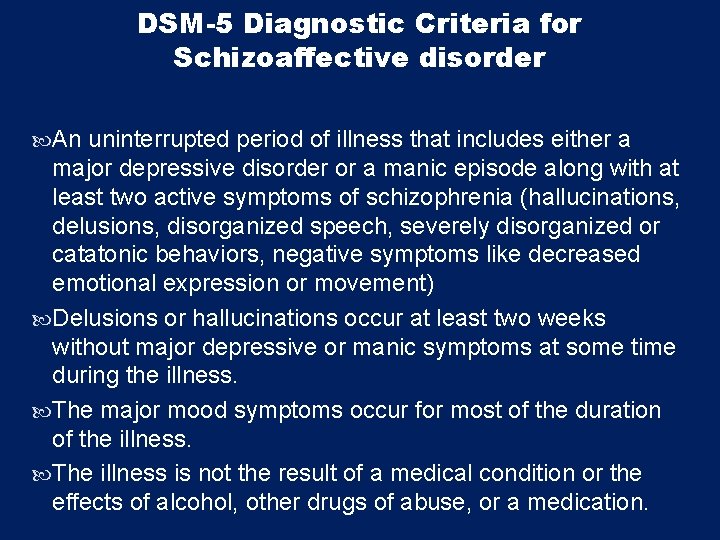
DSM-5 Diagnostic Criteria for Schizoaffective disorder An uninterrupted period of illness that includes either a major depressive disorder or a manic episode along with at least two active symptoms of schizophrenia (hallucinations, delusions, disorganized speech, severely disorganized or catatonic behaviors, negative symptoms like decreased emotional expression or movement) Delusions or hallucinations occur at least two weeks without major depressive or manic symptoms at some time during the illness. The major mood symptoms occur for most of the duration of the illness. The illness is not the result of a medical condition or the effects of alcohol, other drugs of abuse, or a medication.
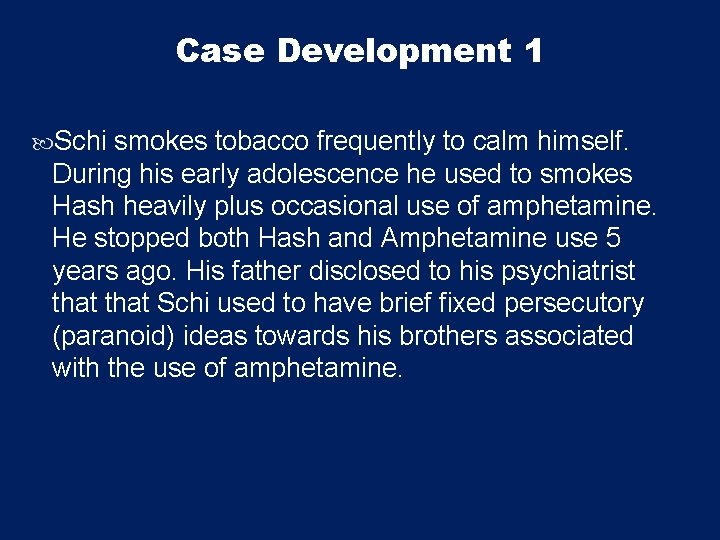
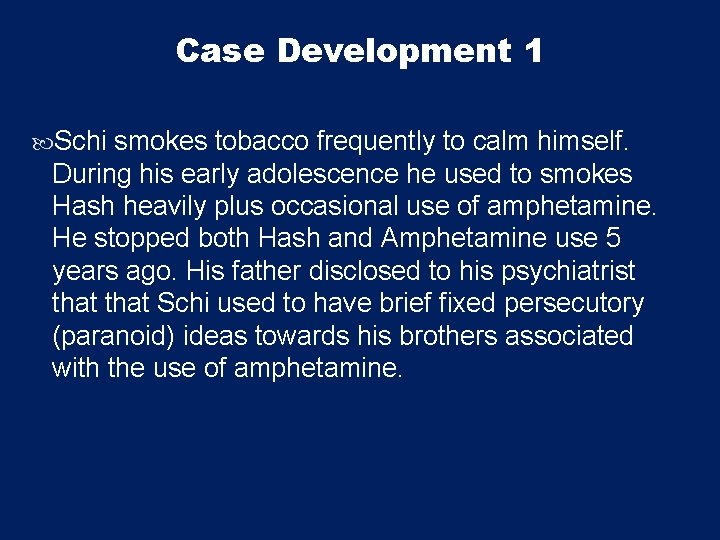
Case Development 1 Schi smokes tobacco frequently to calm himself. During his early adolescence he used to smokes Hash heavily plus occasional use of amphetamine. He stopped both Hash and Amphetamine use 5 years ago. His father disclosed to his psychiatrist that Schi used to have brief fixed persecutory (paranoid) ideas towards his brothers associated with the use of amphetamine.
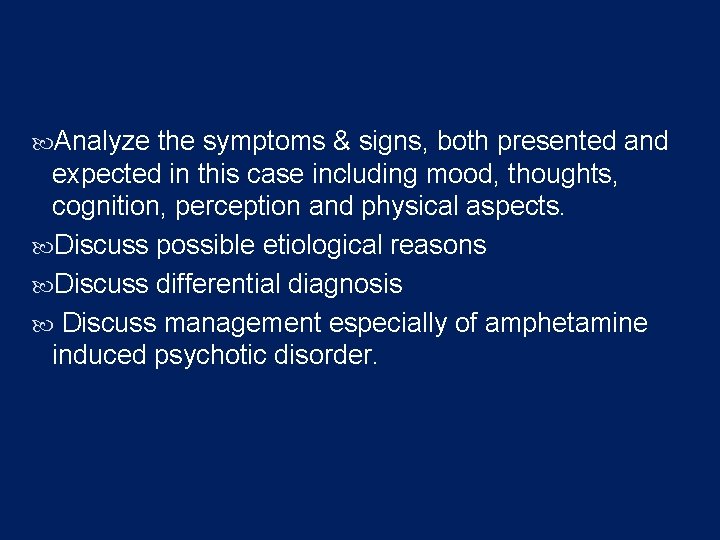
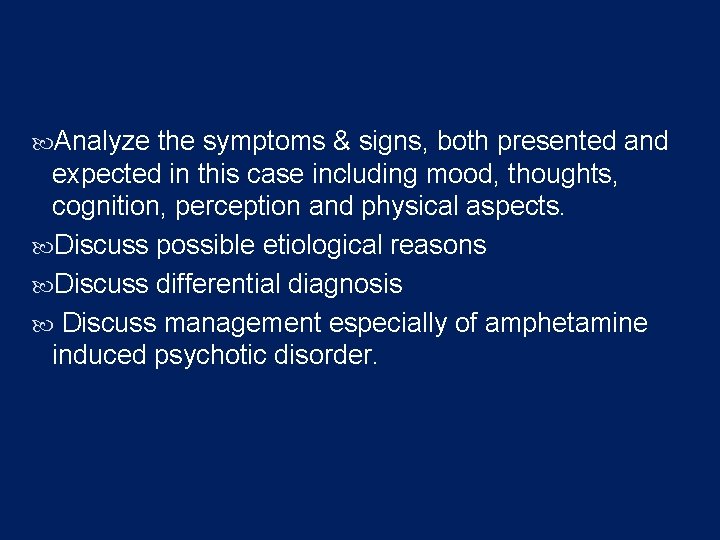
Analyze the symptoms & signs, both presented and expected in this case including mood, thoughts, cognition, perception and physical aspects. Discuss possible etiological reasons Discuss differential diagnosis Discuss management especially of amphetamine induced psychotic disorder.
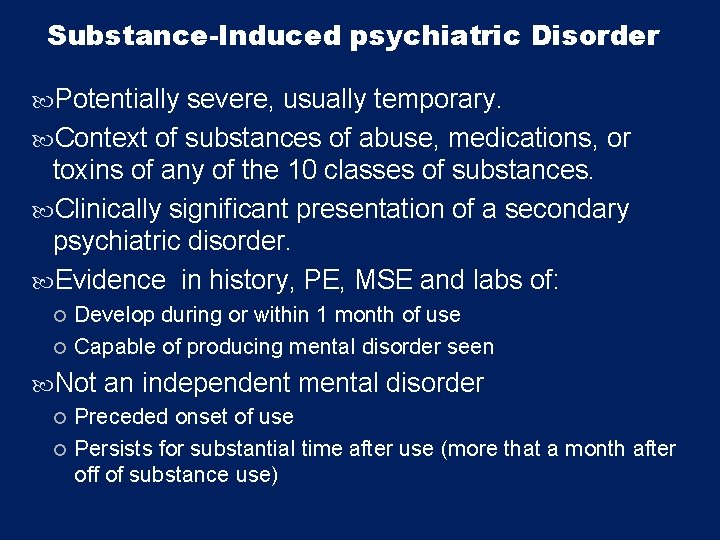
Substance-Induced psychiatric Disorder Potentially severe, usually temporary. Context of substances of abuse, medications, or toxins of any of the 10 classes of substances. Clinically significant presentation of a secondary psychiatric disorder. Evidence in history, PE, MSE and labs of: Develop during or within 1 month of use Capable of producing mental disorder seen Not an independent mental disorder Preceded onset of use Persists for substantial time after use (more that a month after off of substance use)
Case Development 2 He sees a psychiatrist for 15 minutes every two months but sometimes misses his appointment. His parents support him financially and he has a social worker whom he sees often. Schi was treated with Haloperidol which gave him muscle cramps especially in his neck, he was then treated with Olanzapine and gained 10 kg and developed Diabetes Mellitus. During his illness course, the patient’s family became less supportive to him & he became less compliant on his treatments. His psychiatrist would like to switch him to long acting injectable antipsychotic treatment but Schi is afraid of injections and isn't sure that he needs medication.
Considering this case: Discuss management of schizophrenia. Discuss the types of antipsychotics, indication, side effects, etc Discuss the role of psychotherapy, the role of family and other social approaches Discuss in detail Extrapyramidal side effect and Neuroleptic malignant syndrome(NMS)
Treatment What are the indications for hospitalization? Diagnostic purpose Patient & other's safety Initiating or stabilizing medications Establishing an effective association between patient & community supportive systems

Biological therapies q Antipsychotic medications are the mainstay of the treatment of schizophrenia. q Generally, they are remarkably safe. q Two major classes: -Dopamine receptor antagonists ( haloperidol, chlorpromazine ) -Serotonin-dopamine receptor antagonists ( Risperidone, clozapine, olanzapine ). q Depot forms of antipsychotics eg. Risperidone Consta is indicated for poorly compliant patients. q - Electroconvulsive therapy (ECT) for catatonic or poorly responding patients to medications

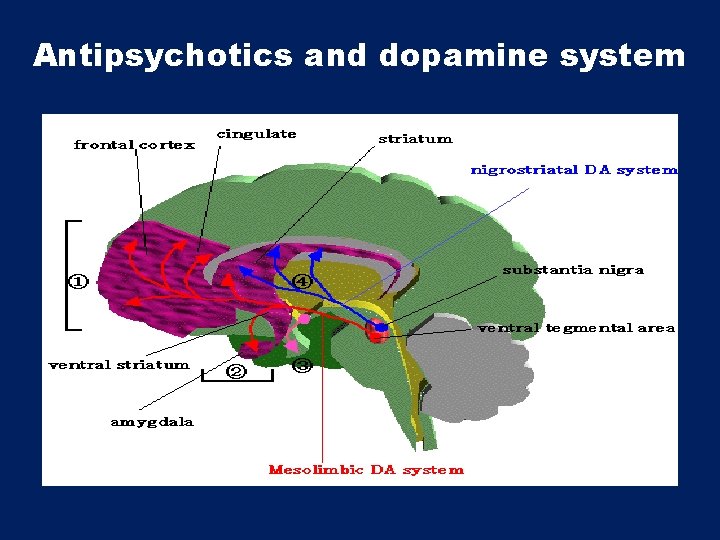
Antipsychotics and dopamine system
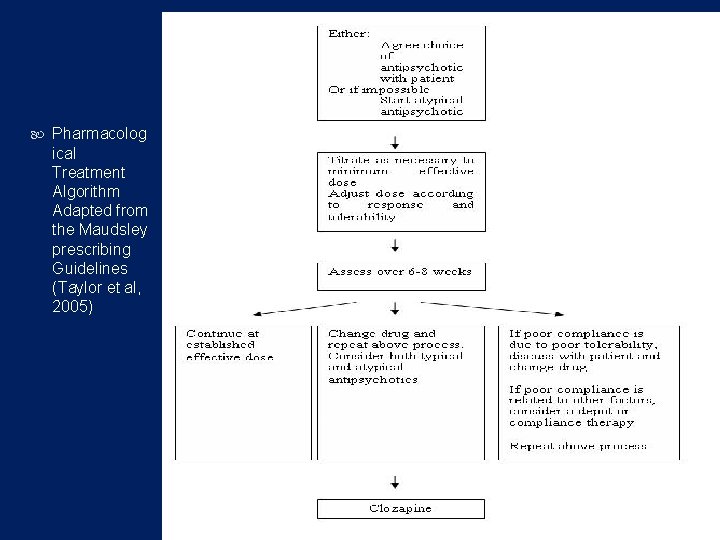
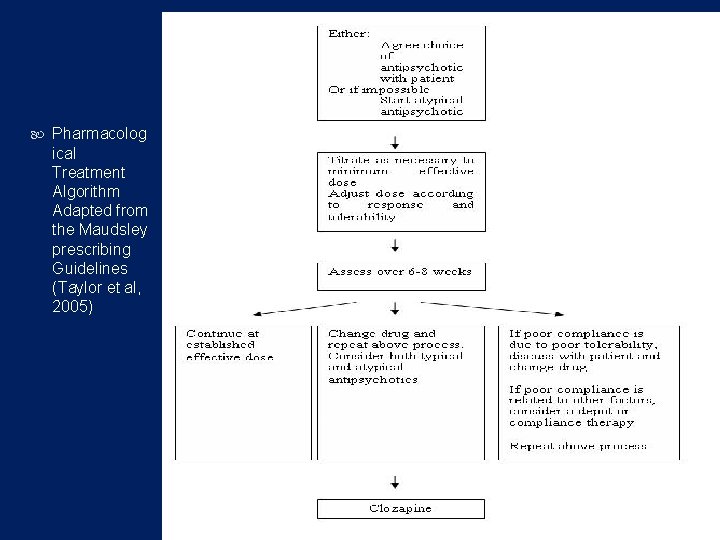
Pharmacolog ical Treatment Algorithm Adapted from the Maudsley prescribing Guidelines (Taylor et al, 2005)
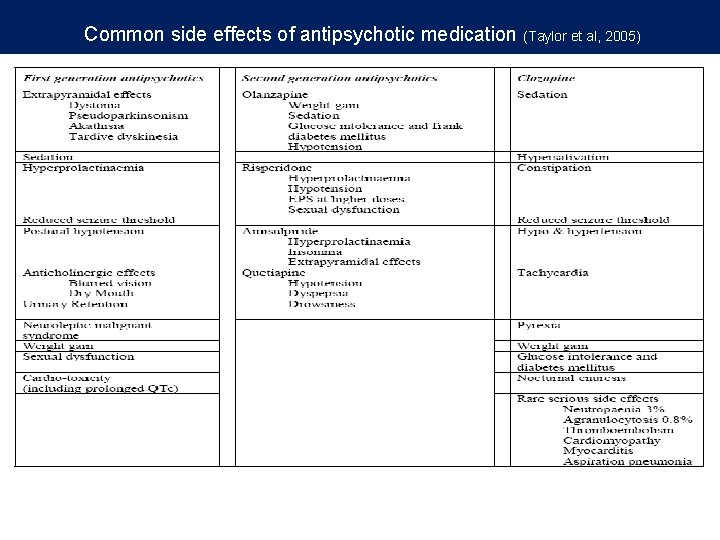
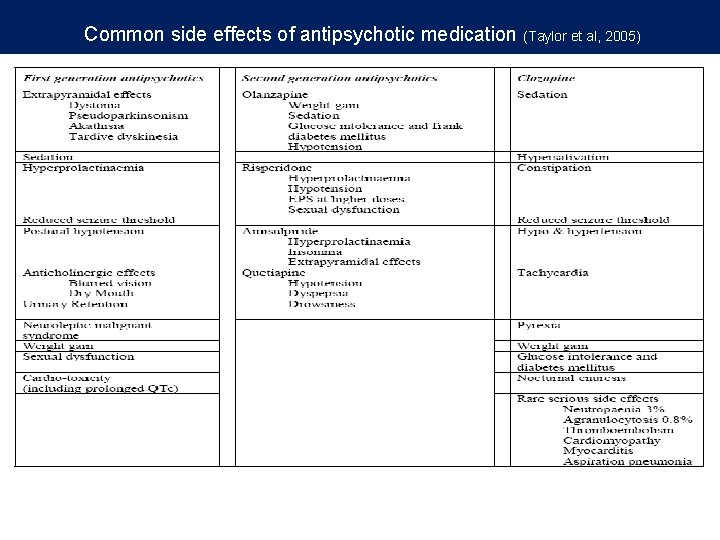
Common side effects of antipsychotic medication (Taylor et al, 2005)
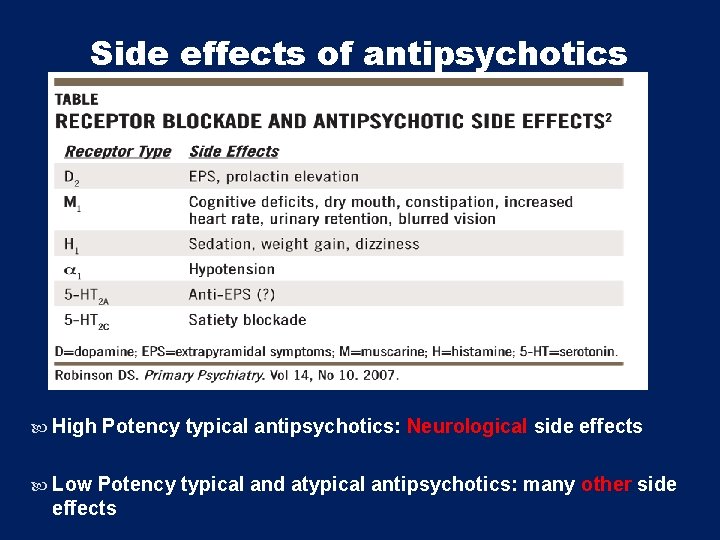
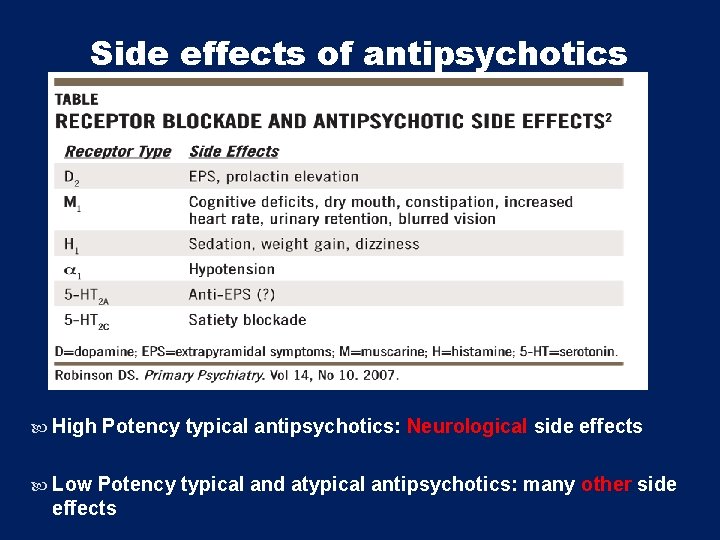
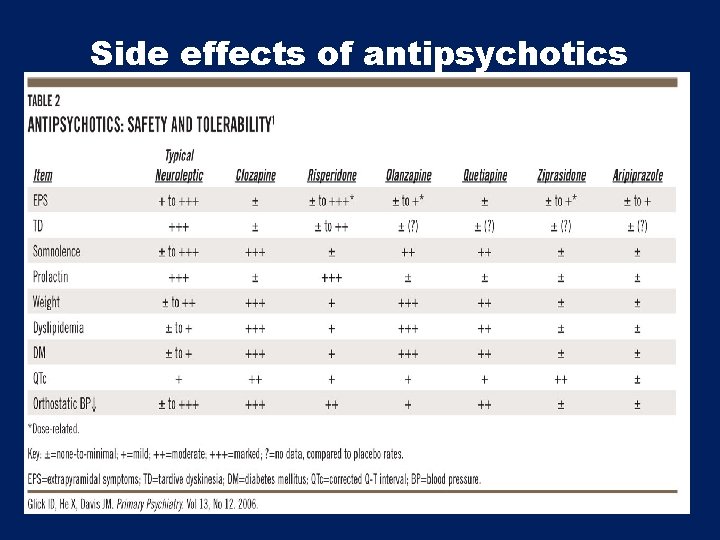
Side effects of antipsychotics High Potency typical antipsychotics: Neurological side effects Low Potency typical and atypical antipsychotics: many other side effects
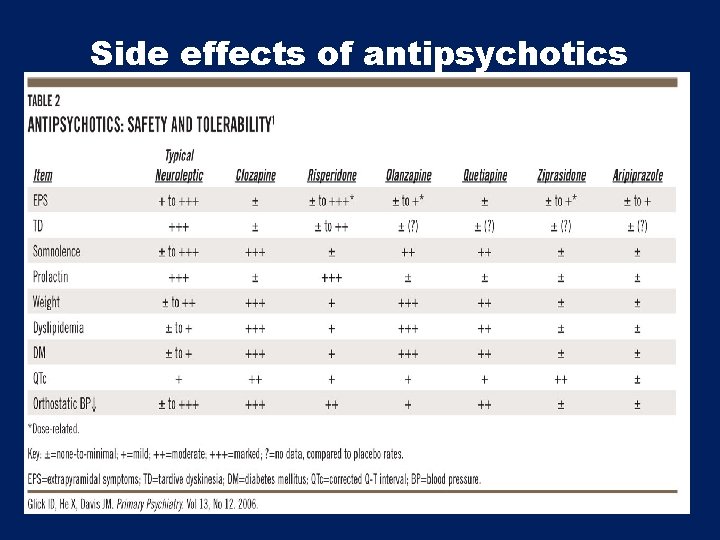
Side effects of antipsychotics
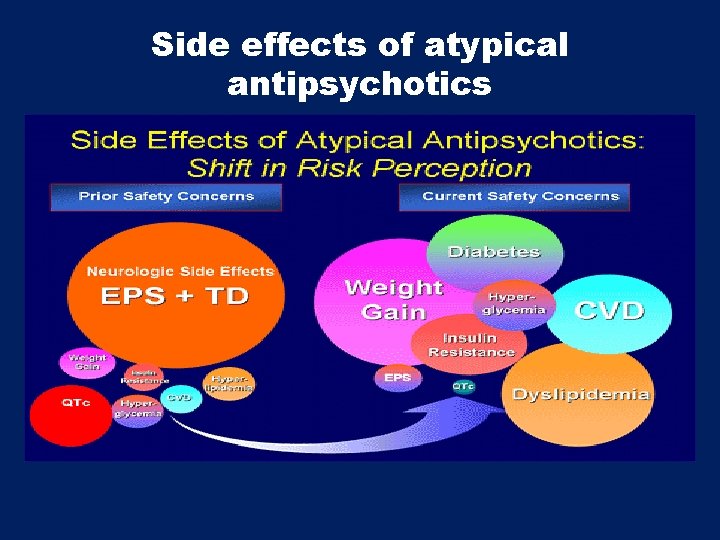
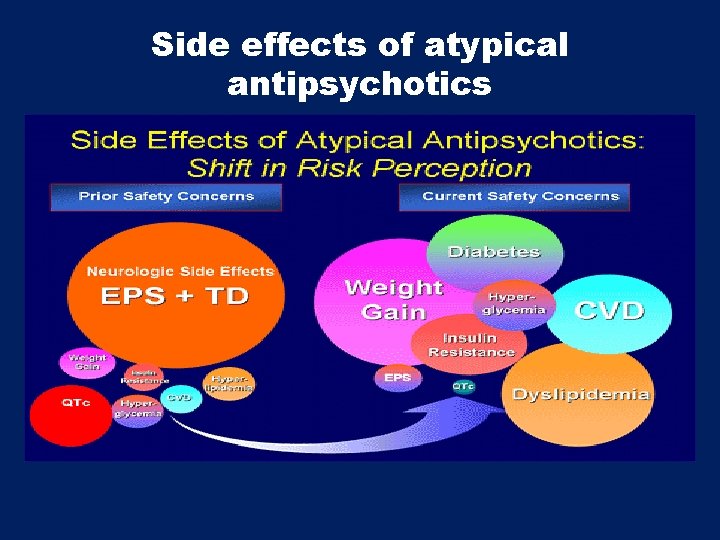
Side effects of atypical antipsychotics
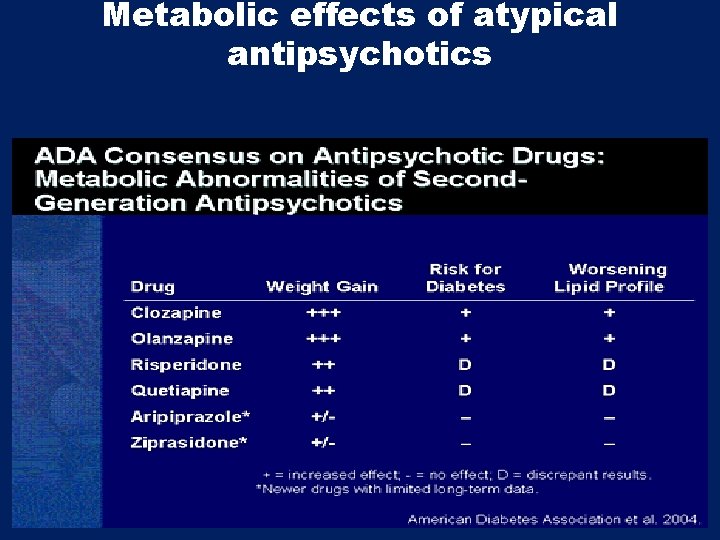
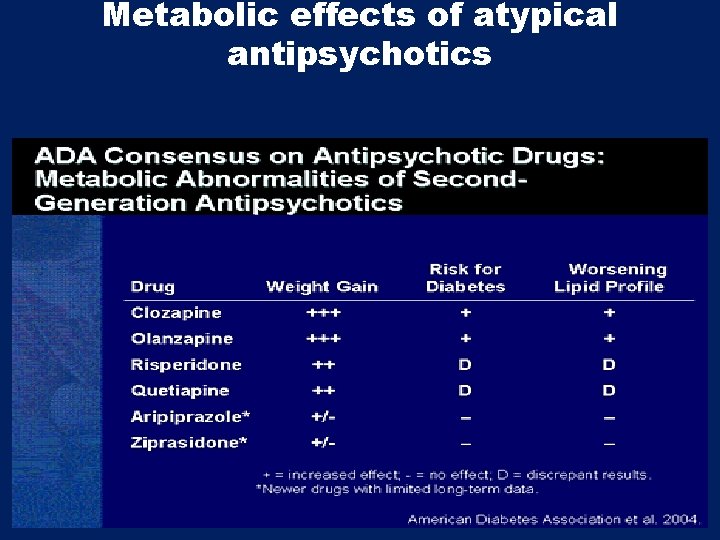
Metabolic effects of atypical antipsychotics
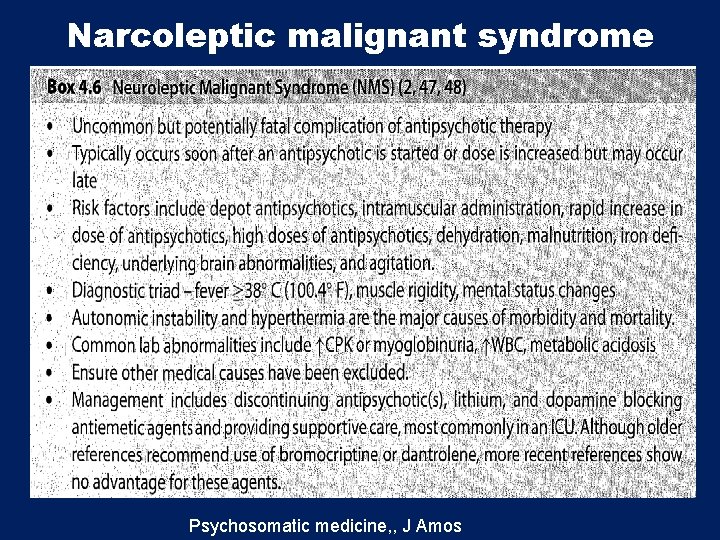
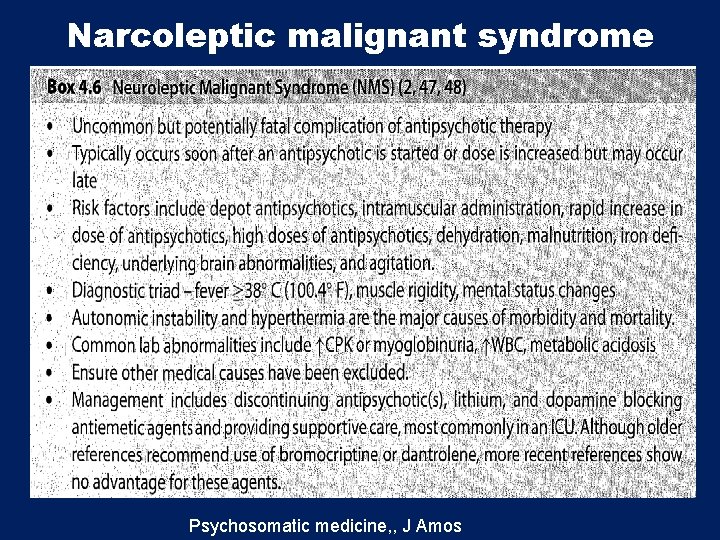
Narcoleptic malignant syndrome Psychosomatic medicine, , J Amos
Psychosocial therapies Social skills training Family oriented therapies Group therapy Individual psychotherapy Assertive community treatment Vocational therapy

Thank you
 Neurosis vs psychosis
Neurosis vs psychosis Looseness of association
Looseness of association Fahad subhi mohammed
Fahad subhi mohammed Neuroses
Neuroses Psychopath causes
Psychopath causes Dsm 5 vs dsm 4
Dsm 5 vs dsm 4 Types of delusions
Types of delusions Radical psychiatry sociology
Radical psychiatry sociology Mse assessment
Mse assessment Geriatric psychiatry definition
Geriatric psychiatry definition Who is this
Who is this Site:slidetodoc.com
Site:slidetodoc.com Pediatrics shelf exam percentiles
Pediatrics shelf exam percentiles Cécile hanon
Cécile hanon Psychiatry in ethiopia
Psychiatry in ethiopia Jamaica hospital psychiatry
Jamaica hospital psychiatry Criminal psychology meaning
Criminal psychology meaning Addiction medicine expert witness
Addiction medicine expert witness National network of child psychiatry access programs
National network of child psychiatry access programs Community geriatric psychiatry
Community geriatric psychiatry Core psychiatry
Core psychiatry National network of child psychiatry access programs
National network of child psychiatry access programs Asclepiades father of psychiatry
Asclepiades father of psychiatry Mutilomania
Mutilomania Global initiative on psychiatry
Global initiative on psychiatry Difference of genre and theme
Difference of genre and theme What is the difference between theme and universal theme?
What is the difference between theme and universal theme? Theme for english b summary
Theme for english b summary Theme vs universal theme
Theme vs universal theme Health and social care level 3 unit 14
Health and social care level 3 unit 14 Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders Assistive technology for behavior
Assistive technology for behavior Puberty and autism spectrum disorders
Puberty and autism spectrum disorders Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders What is neurosis disorder
What is neurosis disorder Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases Physical disorders and health psychology
Physical disorders and health psychology Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Chapter 46 digestive and endocrine disorders
Chapter 46 digestive and endocrine disorders Somatic symptom disorder
Somatic symptom disorder Chapter 29 endocrine and metabolic disorders
Chapter 29 endocrine and metabolic disorders Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders Chapter 18 eating and feeding disorders
Chapter 18 eating and feeding disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Chapter 15 anxiety and obsessive-compulsive disorders
Chapter 15 anxiety and obsessive-compulsive disorders Chapter 11 childhood and neurodevelopmental disorders
Chapter 11 childhood and neurodevelopmental disorders Nail diseases and disorders milady
Nail diseases and disorders milady Little albert
Little albert