Asthma Management Update Lisa Musso ARNP MN CPNP

- Slides: 45
Asthma Management Update Lisa Musso, ARNP, MN, CPNP Division of Pediatric Pulmonary Medicine Children’s Hospital and Regional Medical Center
Asthma Management Update Objectives: Upon completion of this session, participants will be able to: Describe three changes that asthma causes in the airway Identify two types of medicine used to treat asthma List three typical asthma triggers and ways of minimizing their effect
Asthma Management Update Overview: Airway Changes in Asthma How is Asthma Managed - Medications, Trigger Management Asthma Management Plan - Working with the Parent and Health Care Provider Triggers Trigger Management
What is Asthma? Definition of Asthma: Lung disease characterized by; reversible airway obstruction l airway inflammation l increased airway responsiveness l
Pathophysiology Airway Changes: Physiologic response inflammation l bronchoconstriction l hypersecretion of mucus l All lead to airway plugging, hyperinflation and atelectasis. l
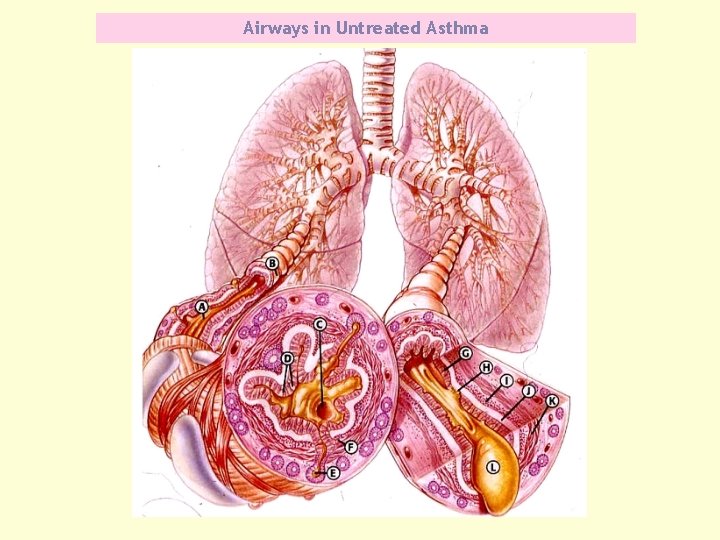
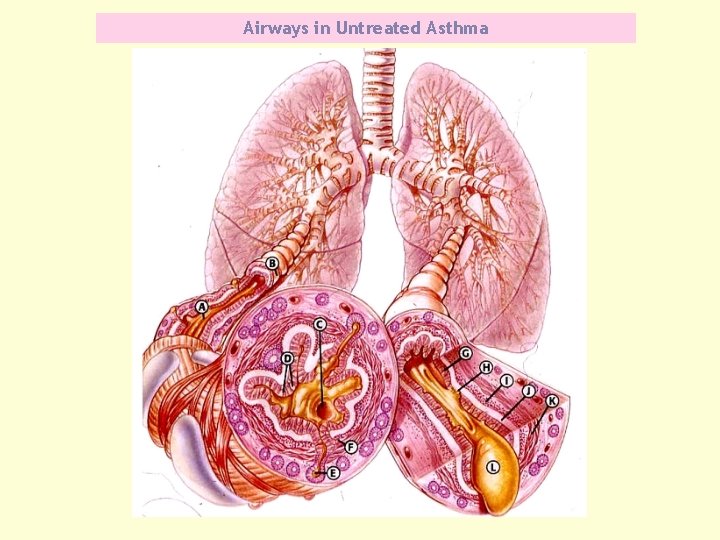
Airways in Untreated Asthma
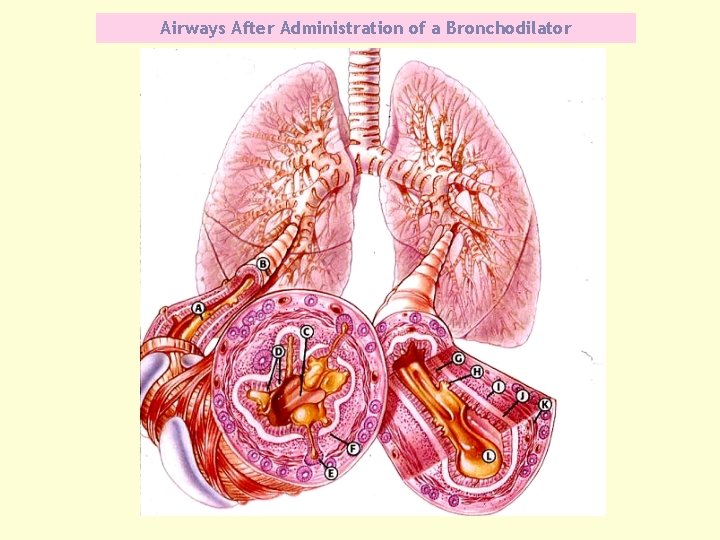
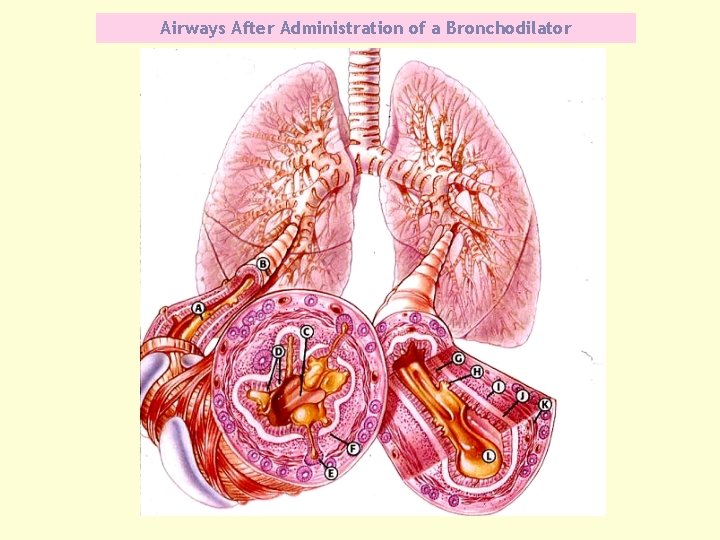
Airways After Administration of a Bronchodilator
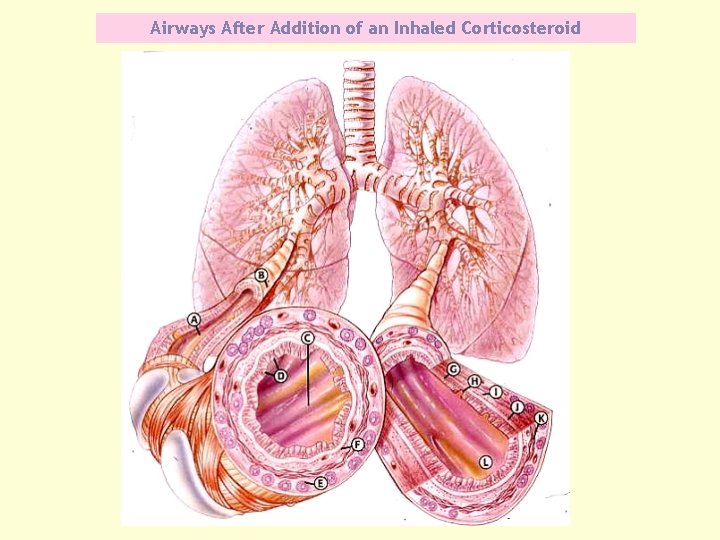
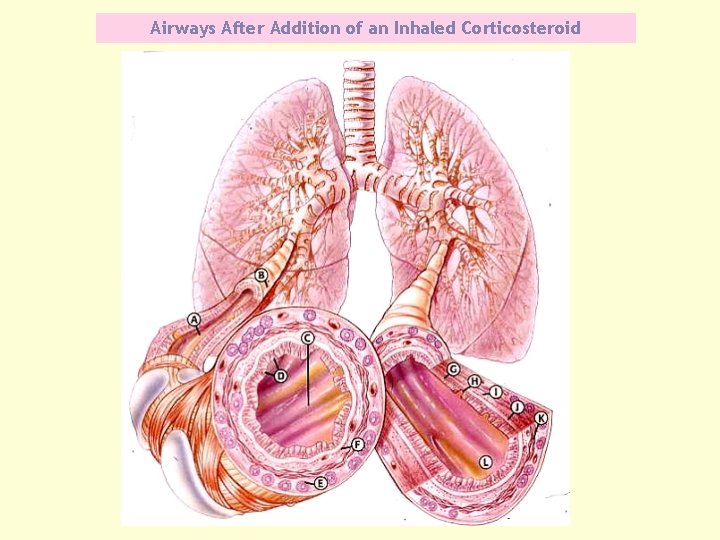
Airways After Addition of an Inhaled Corticosteroid
Asthma Severity Mild Intermittent days with symptoms: < 2/week l nights with symptoms: < 2/month l FEV 1 or PEF: > 80% l
Asthma Severity Mild Persistent days with symptoms: >2/week l nights with symptoms: 3 - 4/month l FEV 1 or PEF: > 80% l
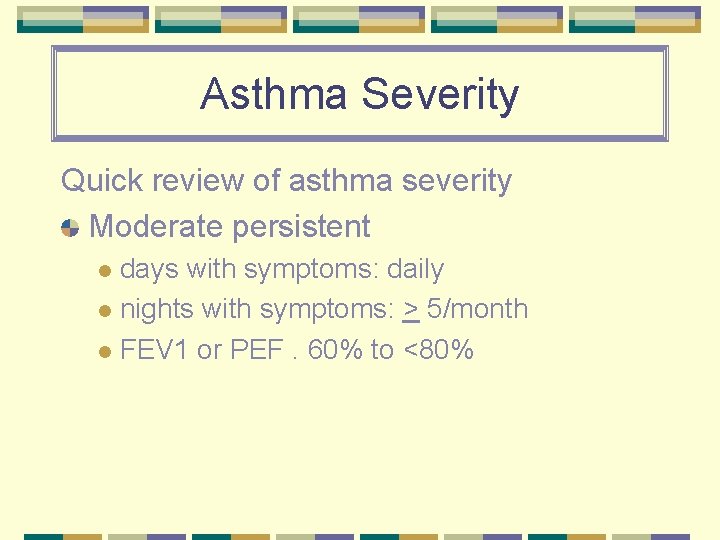
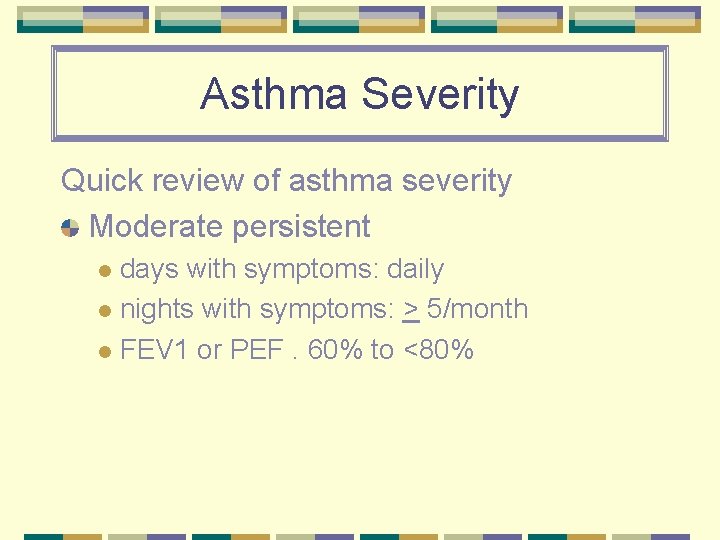
Asthma Severity Quick review of asthma severity Moderate persistent days with symptoms: daily l nights with symptoms: > 5/month l FEV 1 or PEF. 60% to <80% l
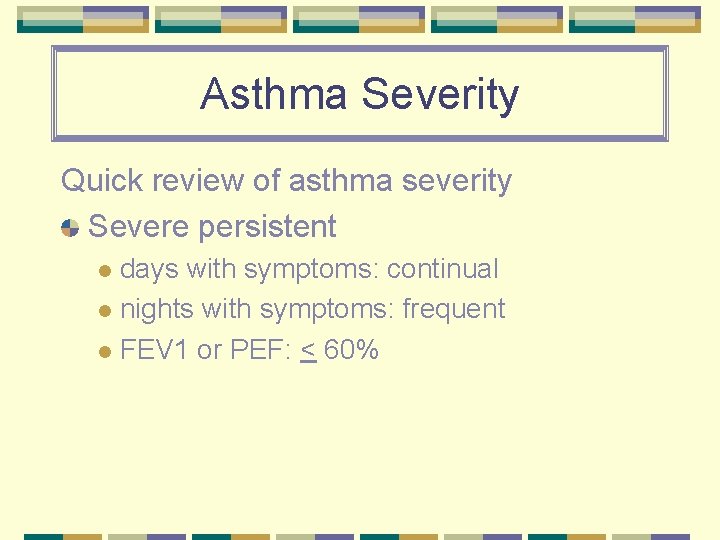
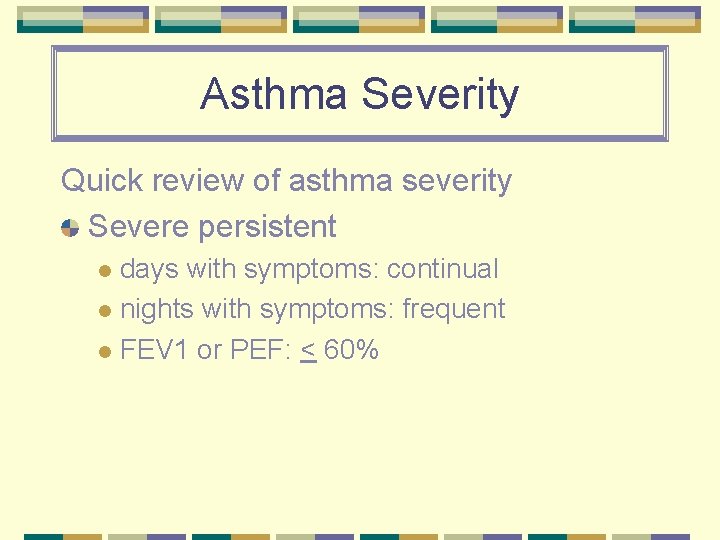
Asthma Severity Quick review of asthma severity Severe persistent days with symptoms: continual l nights with symptoms: frequent l FEV 1 or PEF: < 60% l
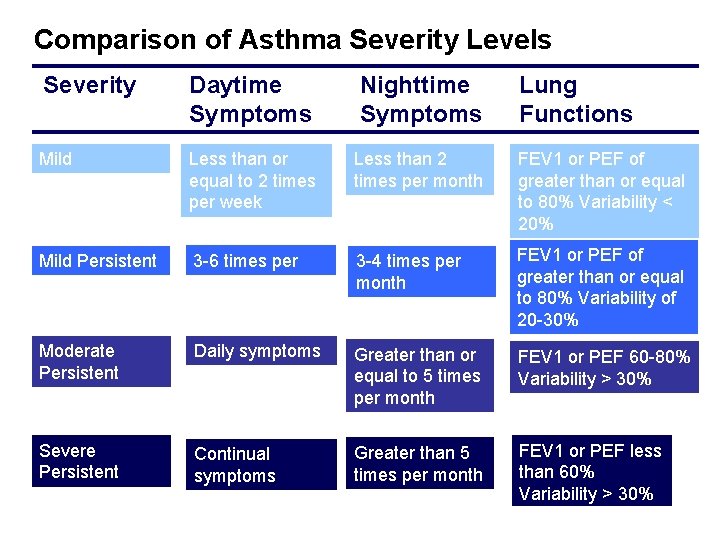
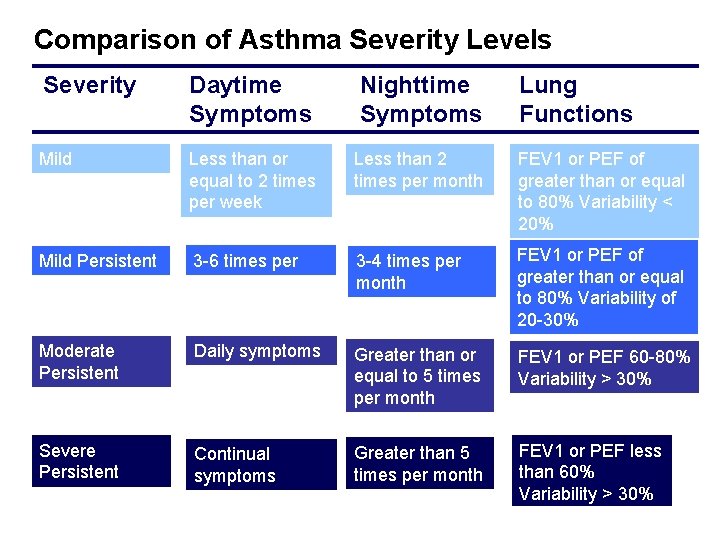
Comparison of Asthma Severity Levels Severity Daytime Symptoms Nighttime Symptoms Lung Functions Mild Intermittent Less than or equal to 2 times per week Less than 2 times per month FEV 1 or PEF of greater than or equal to 80% Variability < 20% Mild Persistent 3 -6 times per week 3 -4 times per month FEV 1 or PEF of greater than or equal to 80% Variability of 20 -30% Moderate Persistent Daily symptoms Greater than or equal to 5 times per month FEV 1 or PEF 60 -80% Variability > 30% Severe Persistent Continual symptoms Greater than 5 times per month FEV 1 or PEF less than 60% Variability > 30%
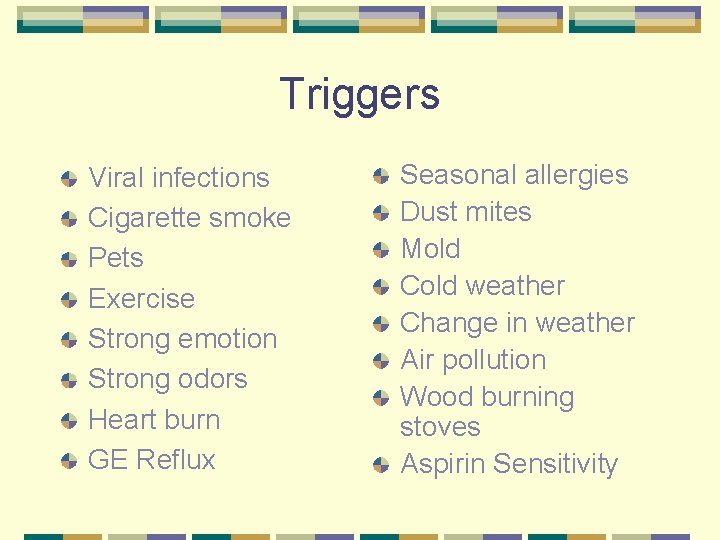
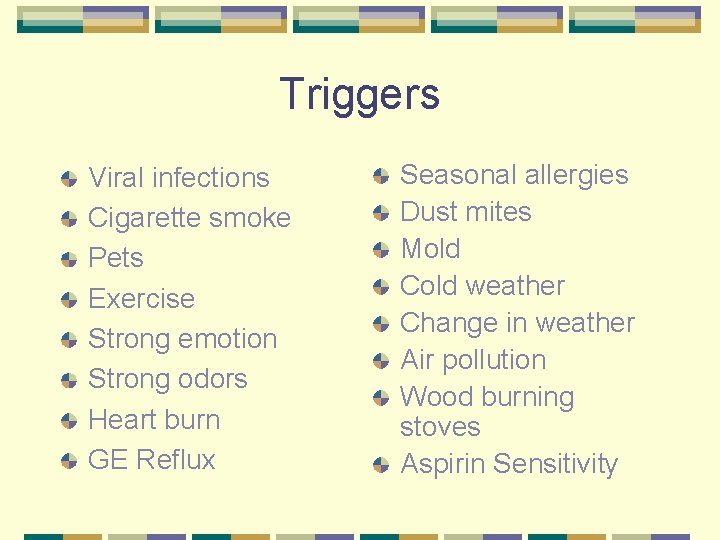
Triggers Viral infections Cigarette smoke Pets Exercise Strong emotion Strong odors Heart burn GE Reflux Seasonal allergies Dust mites Mold Cold weather Change in weather Air pollution Wood burning stoves Aspirin Sensitivity
Infections Upper Respiratory infections Viral or bacterial “colds” ear aches sinus “flu”
Smoke Active smoking Passive smoking Inside/outside home Inside/outside car
Animals Furry, hairy l Shedding Cats l Dogs l Birds l Rabbits, hamsters, guinea pigs, rats l
To Run and Play Exercise How much is too much l Recess l Gym l Team Sports l
To laugh or cry Laughing Crying Stress Anger Anxious Scared
Things that Smell Perfume/cologne Incense Wood burning stoves Paint Cleaning products Hair products Foods
Allergens dust mites animal dander molds, mildew, fungi pollens—grass, trees, weeds cockroaches
Cold or Warm Air – Weather Changes Cold air versus warm air To exercise or not Weather changes
Prevention Strategies
Infections Prevention l l l l Good hand washing Use of tissues Cleaning of school areas Cleaning of toys Sharing of school supplies, equipment, toys Staying at home Completion of course of medication if given
Tobacco Smoke Controlling environmental tobacco smoke: smoke-free child care environment smoke-free vehicle quit smoking smoke outside wearing “smoking jacket”
Animal Dander Controlling animal dander: keep cats, dogs, and other furry animals out of children’s area replace w/non furred or feathered animals
Molds Controlling molds, mildews and fungi: locate and remove mold growth check walls, floors, window molding, ceiling, under carpet don’t lay carpet on cement prevent growth w/ good ventilation
Roaches Controlling cockroaches: restrict where food is eaten clean up after food preparation do not leave out pet food overnight cover trash bins don’t store paper products/ bottles at floor level repair cracks, holes in foundation, plumbing, walls fix leaky faucets
Pollens Controlling pollen exposure: minimize outdoor activity on high pollen days close windows and doors on high pollen days run air conditioning allergy medicine as directed by parent/provider
Allergy Controlling dust mites: cover mattresses and pillows minimize stuffed animals remove upholstered furniture vacuum frequently w/children absent maintain humidity @ about 40% filters over heating ducts washable rugs instead of carpets
Air Pollution Controlling exposure to air pollution/ozone: Minimize outside activity on high pollution days avoid ozone-generating air cleaners
Odors---the good and the bad Controlling exposure to fumes/sprays/strong odors: avoid aerosol sprays avoid strong “clean” smelling sprays avoid perfumes, after shave, candles, potpourri, incense clean with weak bleach solution and let air dry (see handout)

Exercise Dealing with exercise-induced asthma: pre-treat as directed by parent/ provider Cover mouth and nose warm up before strenuous exercise rest periods minimize outdoor activity if high level of triggers are present
Triggers Drop in peak flow cough wheeze cold symptoms chest tightness difficulty breathing Fast breathing shortness of breath restlessness poor appetite headache dark circles
Medications Controller l l l l Cromolyn sodium Nedocromil sodium Inhaled Corticosteroids Leukotriene modifiers Long acting Beta 2 Sustained released theophylline Nebulized steroids Rescue l l Short acting Beta 2 Oral steroids (short burst)
Gadgets and Gizmos Nebulizers metered dose inhaler (MDI) spacer /spacer with mask diskhaler Aerolizers Turbohaler dry powder inhaler tablets liquids
Peak Flow Meters What do they really tell you? If asthma is worsening l If asthma is better or worse l If medications is helping l Are you really having an asthma attack l
Peak Flow Meters Who should use one? Moderate to severe asthmatics l Poor perceivers of severity of symptoms l Newly diagnosed l History of severe exacerbations l Exercised Induced Asthmatics l
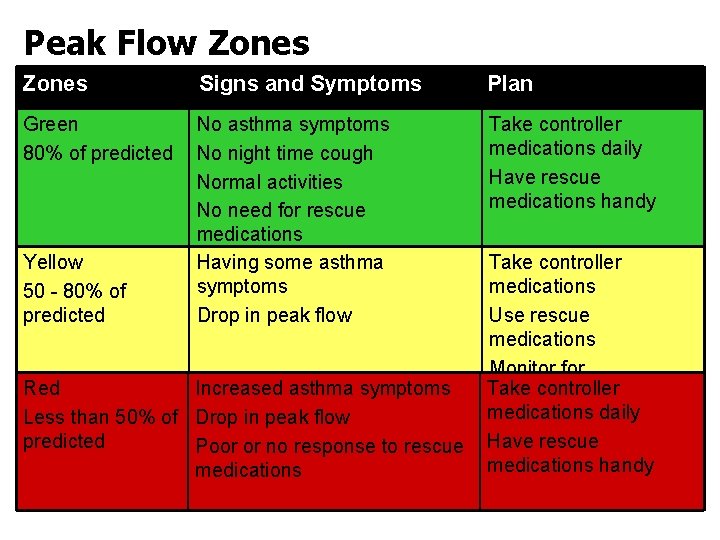
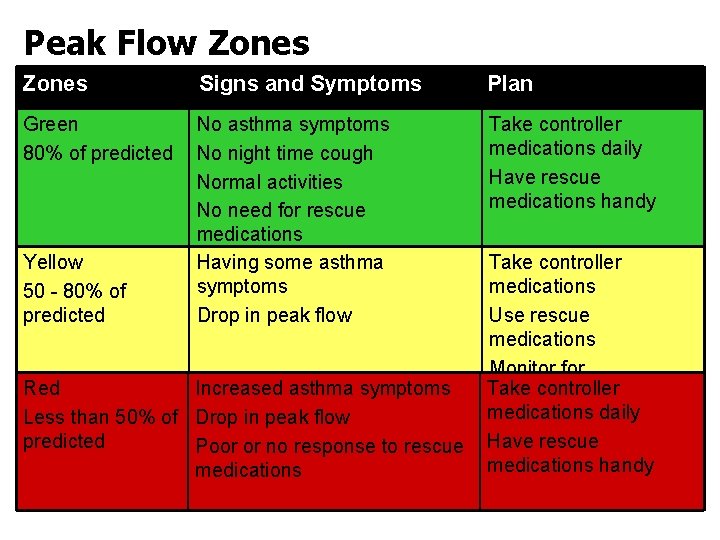
Peak Flow Zones Signs and Symptoms Plan Green 80% of predicted No asthma symptoms No night time cough Normal activities No need for rescue medications Having some asthma symptoms Drop in peak flow Take controller medications daily Have rescue medications handy Yellow 50 - 80% of predicted Red Increased asthma symptoms Less than 50% of Drop in peak flow predicted Poor or no response to rescue medications Take controller medications Use rescue medications Monitor for Take controller improvement medications daily Have rescue medications handy
Asthma Management Plans Definition: l an written educational tool or plan which describes daily management and how to handle asthma episodes/excerbations
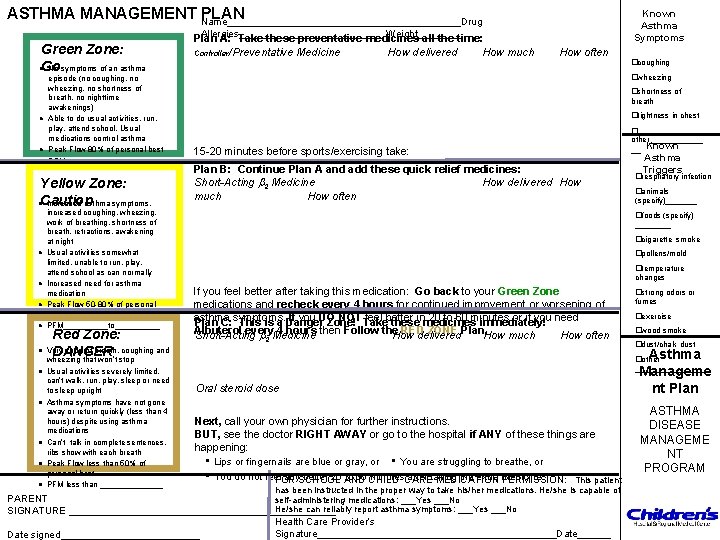
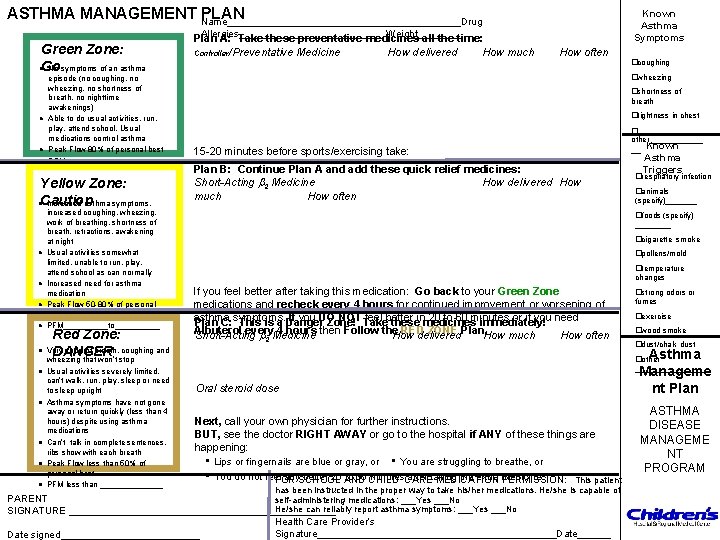
ASTHMA MANAGEMENT Name_____________________Drug PLAN Known Asthma Symptoms Allergies_____________ Weight____ Green Zone: Go No symptoms of an asthma Plan A: Take these preventative medicines all the time: Controller/Preventative Medicine How delivered How much How often �coughing l l episode (no coughing, no wheezing, no shortness of breath, no nighttime awakenings) Able to do usual activities, run, play, attend school. Usual medications control asthma Peak Flow 80% of personal best PFM____to____ Yellow Zone: Caution Increased asthma symptoms, l l l l l increased coughing, wheezing, work of breathing, shortness of breath, retractions, awakening at night Usual activities somewhat limited, unable to run, play, attend school as can normally Increased need for asthma medication Peak Flow 50 -80% of personal best PFM_____to_____ Red Zone: Very short of breath, coughing and DANGER wheezing that won’t stop Usual activities severely limited, can’t walk, run, play, sleep or need to sleep upright Asthma symptoms have not gone away or return quickly (less than 4 hours) despite using asthma medications Can’t talk in complete sentences, ribs show with each breath Peak Flow less than 50% of personal best PFM less than _______ �wheezing �shortness of breath �tightness in chest 15 -20 minutes before sports/exercising take: Plan B: Continue Plan A and add these quick relief medicines: Short-Acting 2 Medicine How delivered How much How often Asthma Triggers �respiratory infection �animals (specify)_______ �foods (specify) ____ �cigarette smoke �pollens/mold �temperature changes If you feel better after taking this medication: Go back to your Green Zone medications and recheck every 4 hours for continued improvement or worsening of asthma If you DO NOT Take feel better 20 to 60 minutes or if you need Plan C: symptoms. This is a Danger Zone! theseinmedicines immediately! Albuterol every 4 hours then Follow the RED ZONE Plan. Short-Acting Medicine How delivered How much How often 2 �strong odors or fumes �exercise �wood smoke �dust/chalk dust Asthma Manageme nt Plan �other ________ Oral steroid dose Next, call your own physician for further instructions. BUT, see the doctor RIGHT AWAY or go to the hospital if ANY of these things are happening: • Lips or fingernails are blue or gray, or • You are struggling to breathe, or • You do not feel any. SCHOOL better 20 AND to 30 CHILD minutes. CARE after taking the extra medicine. FOR MEDICATION PERMISSION: This patient has been instructed in the proper way to take his/her medications. He/she is capable of PARENT self-administering medications: ___Yes ___No He/she can reliably report asthma symptoms: ___Yes ___No SIGNATURE ________________________ l � other______ __ Known Date signed_____________ Health Care Provider’s Signature______________________Date______ ASTHMA DISEASE MANAGEME NT PROGRAM
What does this mean in real life? No coughing No difficulty breathing No waking at night Normal activities No acute episodes that require PCP visit, ER or hospitalization No absences from school or work Normal ( or near normal) lung function
Summary Asthma is a chronic disease It is controllable, some exacerbations sometimes can be prevented Different medications treat the different phases of asthma Asthma Management Plans really do help School Nurses do a great job!
Questions
References Helpful Web Resources http: //www. ginasthma. com l http: //www. guidelines. gov l http: //nhlbi. nih. gov l http: //lungusa. org l
 Lisa musso
Lisa musso Cardiac asthma vs bronchial asthma
Cardiac asthma vs bronchial asthma Saas cpnp
Saas cpnp Eu cosmetic product notification portal (cpnp)
Eu cosmetic product notification portal (cpnp) Alternative of log based recovery
Alternative of log based recovery Guido musso
Guido musso Andrea musso
Andrea musso Leonardo musso mannheim
Leonardo musso mannheim Musso logo
Musso logo Viral induced wheeze vs asthma
Viral induced wheeze vs asthma Asthma vs copd spirometry
Asthma vs copd spirometry Non atopic asthma
Non atopic asthma Asthma treatment
Asthma treatment Asthma diagnosis criteria
Asthma diagnosis criteria Asthma classification chart
Asthma classification chart Icd 10 code for allergic reaction to peanuts
Icd 10 code for allergic reaction to peanuts 4x4x4 asthma method 26 puffs
4x4x4 asthma method 26 puffs Asthma gold
Asthma gold Gina
Gina Allen becker
Allen becker Copd vs asthma
Copd vs asthma Asthma at night treatment
Asthma at night treatment Cough varient asthma
Cough varient asthma Mild moderate severe asthma exacerbation
Mild moderate severe asthma exacerbation Cause of asthma
Cause of asthma Pef in asthma
Pef in asthma Asthma types
Asthma types Asthma index
Asthma index Asthma index
Asthma index Asthma step up therapy
Asthma step up therapy Pathophysiology definition
Pathophysiology definition 3392chest
3392chest Asthma stages
Asthma stages Berotec nebs
Berotec nebs What is life
What is life Asthma attack
Asthma attack Specific objectives of asthma
Specific objectives of asthma Co2 narcosis
Co2 narcosis Asthma pathophysiology
Asthma pathophysiology Monday dyspnea
Monday dyspnea Specific objectives of asthma
Specific objectives of asthma Non atopic asthma
Non atopic asthma Oshit asthma
Oshit asthma Subjective data for asthma
Subjective data for asthma Pediatric asthma care near santa rosa
Pediatric asthma care near santa rosa Bendopnea definition
Bendopnea definition