T Cymes Stage 3 student doctor University of
- Slides: 13
T. Cymes Stage 3 student doctor University of Cambridge Paediatrics Respiratory system
Plan �Examination tips differences from adults red flags �Asthma �Bronchiolitis �Pneumonia �Cystic fibrosis �Other diseases
Examination – how to survive �Get to their level! �Let young children play with your stethoscope Great toy! Lets them get used to it �Let parents undress the child only when needed �Start with least invasive examination �Show on parents, toy etc �Auscultate early �Save percussion until the end ▪ Start on arm or knee – they get used to it!
Examination – difference from adults �Position Infants – lying on couch Toddler – on parent's lap Pre-school – while at play �Initial impression important ? unwell child �Look for dysmorphic features �Percussion can be omitted Little information in infants
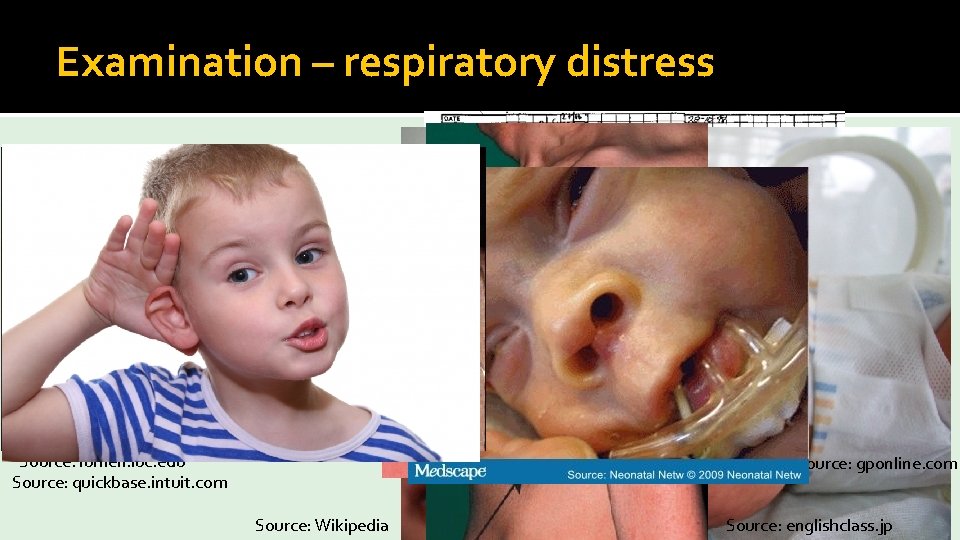
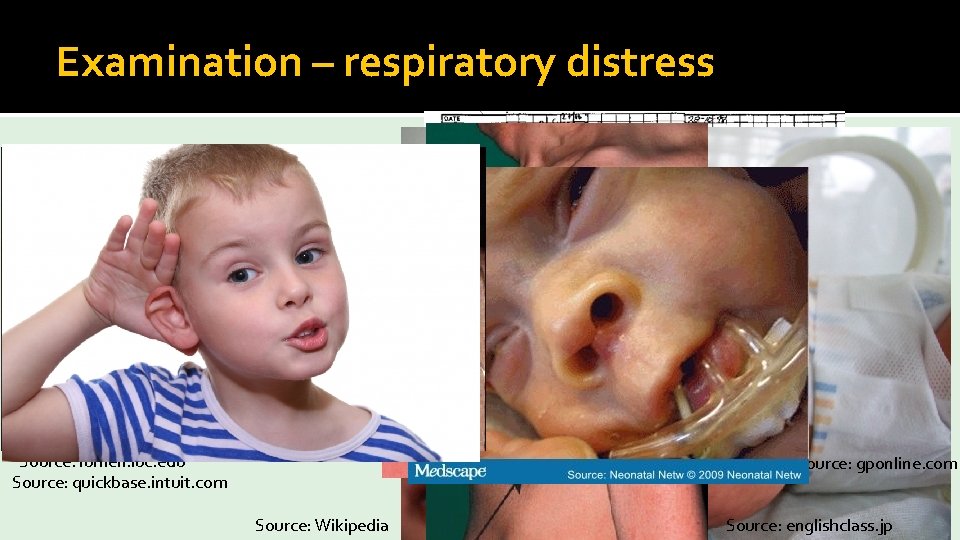
Examination – respiratory distress � Tachypnoea / tachycardia � Accessory muscles � Intercostal recessions � Wheeze � Harrison’s sulcus � Stridor � Cyanosis � Grunting � Nasal flaring � Silent chest Source: lumen. luc. edu Source: quickbase. intuit. com Source: gponline. com Source: Wikipedia Source: BMJ Source: englishclass. jp
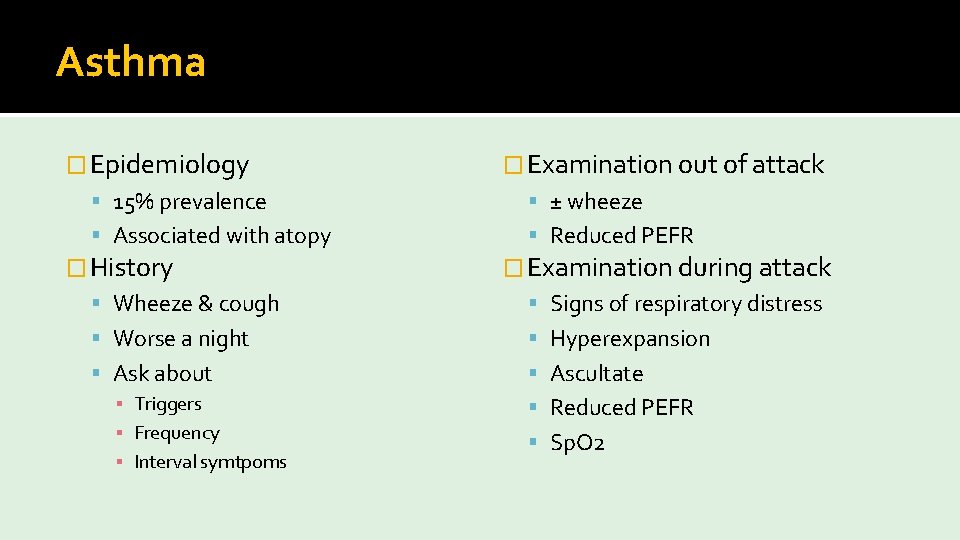
Asthma � Epidemiology � Examination out of attack 15% prevalence ± wheeze Associated with atopy Reduced PEFR � History � Examination during attack Wheeze & cough Signs of respiratory distress Worse a night Hyperexpansion Ask about Ascultate ▪ Triggers ▪ Frequency ▪ Interval symtpoms Reduced PEFR Sp. O 2
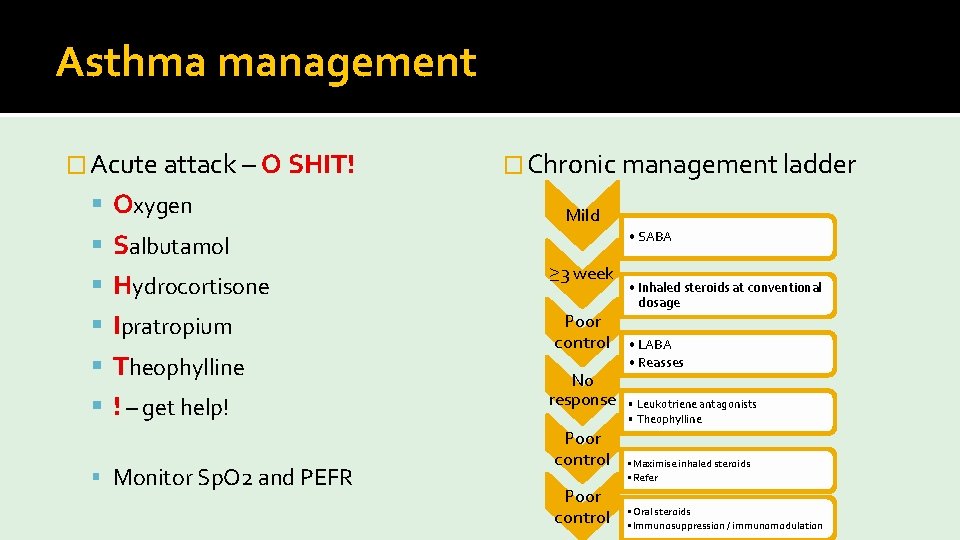
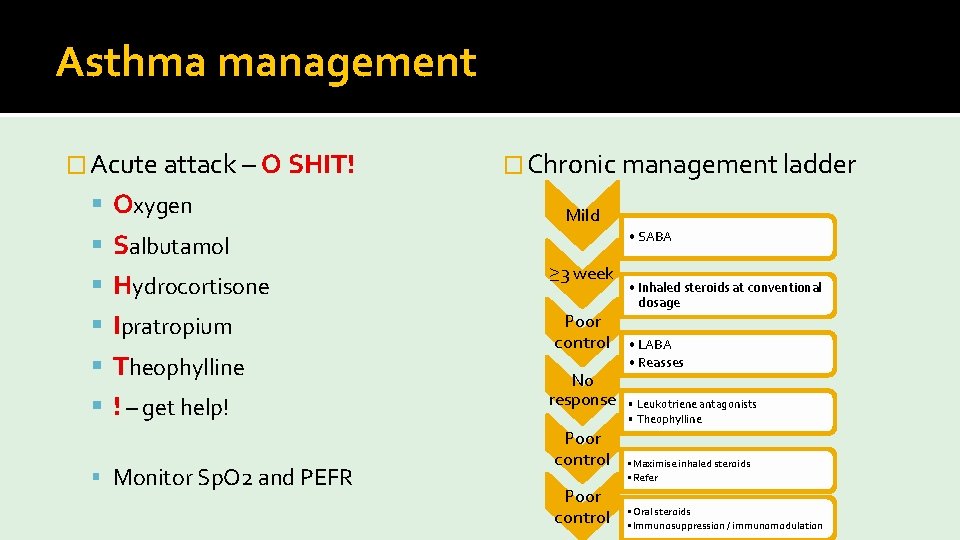
Asthma management � Acute attack – O SHIT! Oxygen � Chronic management ladder Mild Salbutamol • SABA Hydrocortisone ≥ 3 week Ipratropium Poor control Theophylline ! – get help! Monitor Sp. O 2 and PEFR No response Poor control • Inhaled steroids at conventional dosage • LABA • Reasses • Leukotriene antagonists • Theophylline • Maximise inhaled steroids • Refer • Oral steroids • Immunosuppression / immunomodulation
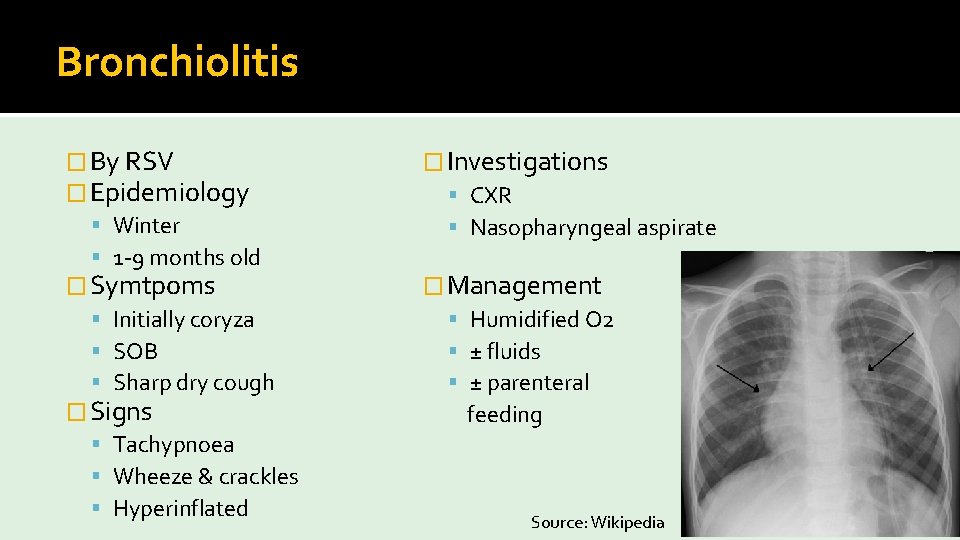
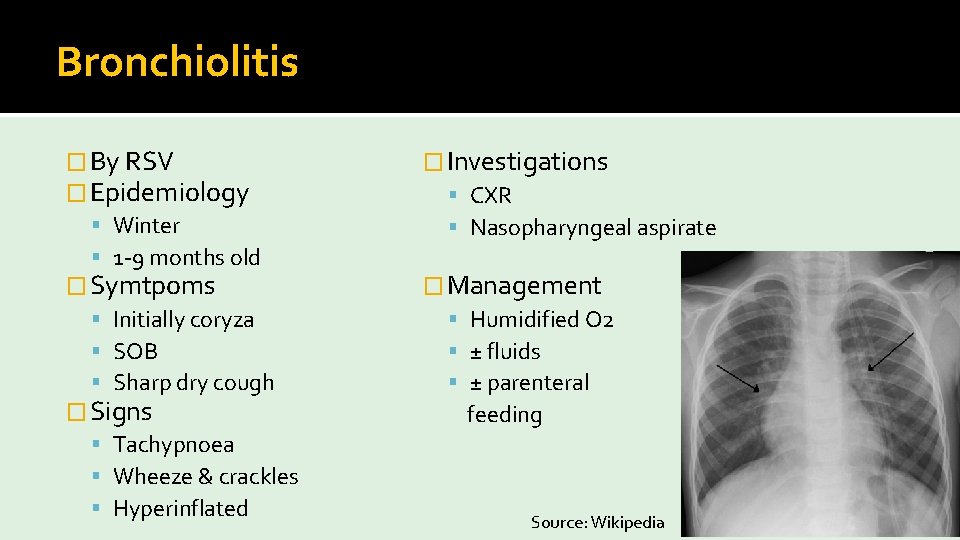
Bronchiolitis � By RSV � Epidemiology Winter 1 -9 months old � Symtpoms Initially coryza SOB Sharp dry cough � Signs Tachypnoea Wheeze & crackles Hyperinflated � Investigations CXR Nasopharyngeal aspirate � Management Humidified O 2 ± fluids ± parenteral feeding Source: Wikipedia
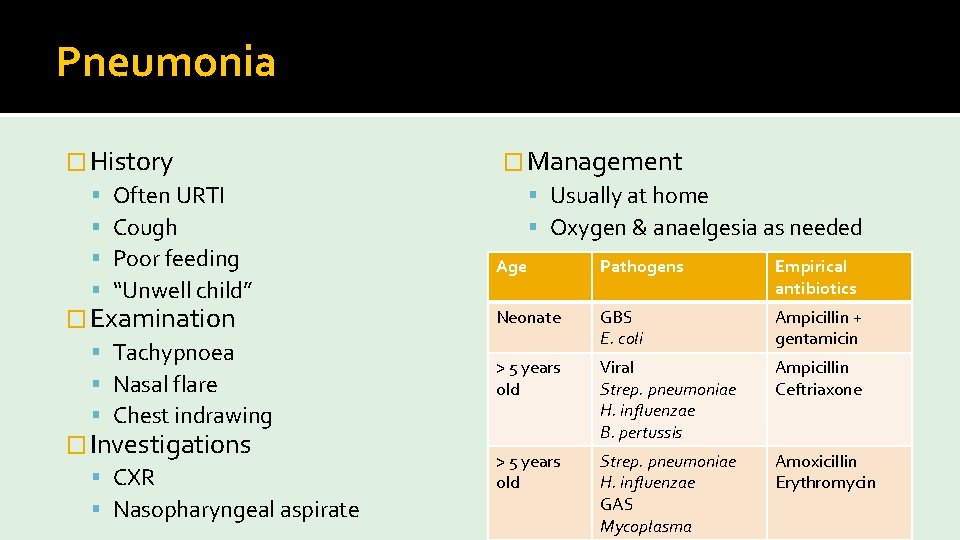
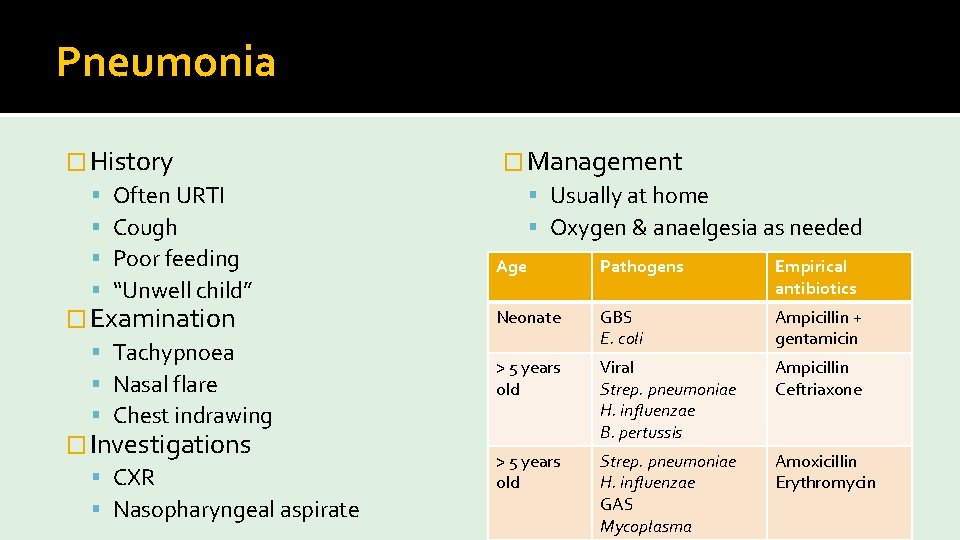
Pneumonia � History Often URTI Cough Poor feeding “Unwell child” � Examination Tachypnoea Nasal flare Chest indrawing � Investigations CXR Nasopharyngeal aspirate � Management Usually at home Oxygen & anaelgesia as needed Age Pathogens Empirical antibiotics Neonate GBS E. coli Ampicillin + gentamicin > 5 years old Viral Strep. pneumoniae H. influenzae B. pertussis Ampicillin Ceftriaxone > 5 years old Strep. pneumoniae H. influenzae GAS Mycoplasma Amoxicillin Erythromycin
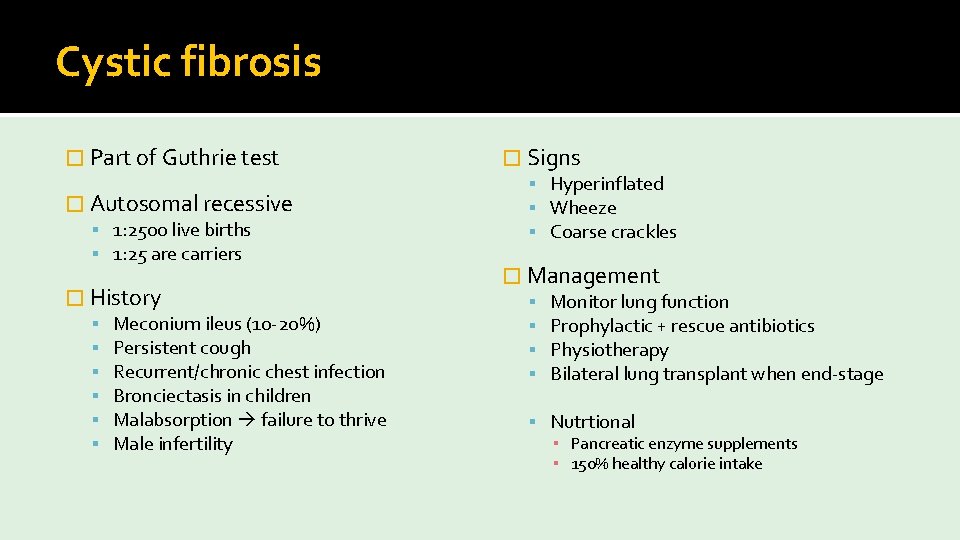
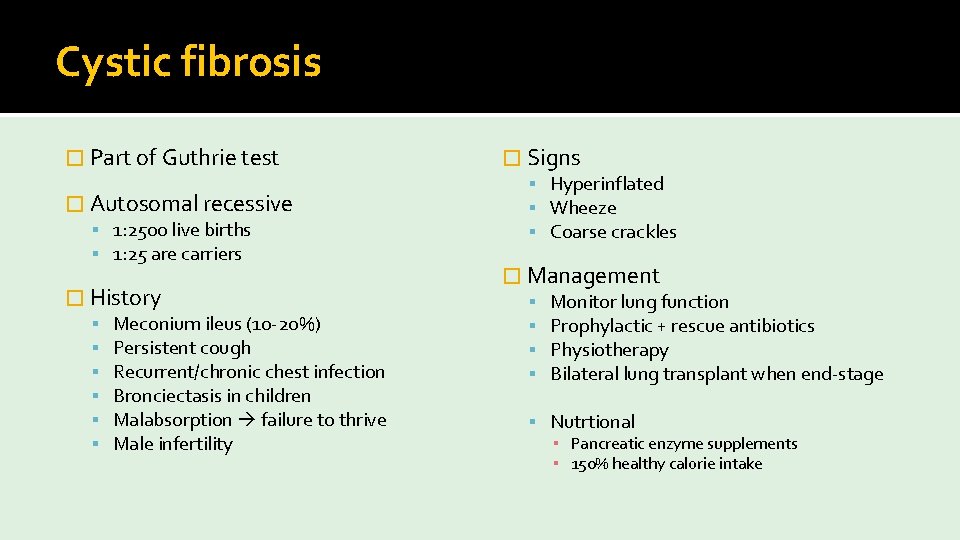
Cystic fibrosis � Part of Guthrie test � Autosomal recessive 1: 2500 live births 1: 25 are carriers � History Meconium ileus (10 -20%) Persistent cough Recurrent/chronic chest infection Bronciectasis in children Malabsorption failure to thrive Male infertility � Signs Hyperinflated Wheeze Coarse crackles � Management Monitor lung function Prophylactic + rescue antibiotics Physiotherapy Bilateral lung transplant when end-stage Nutrtional ▪ Pancreatic enzyme supplements ▪ 150% healthy calorie intake
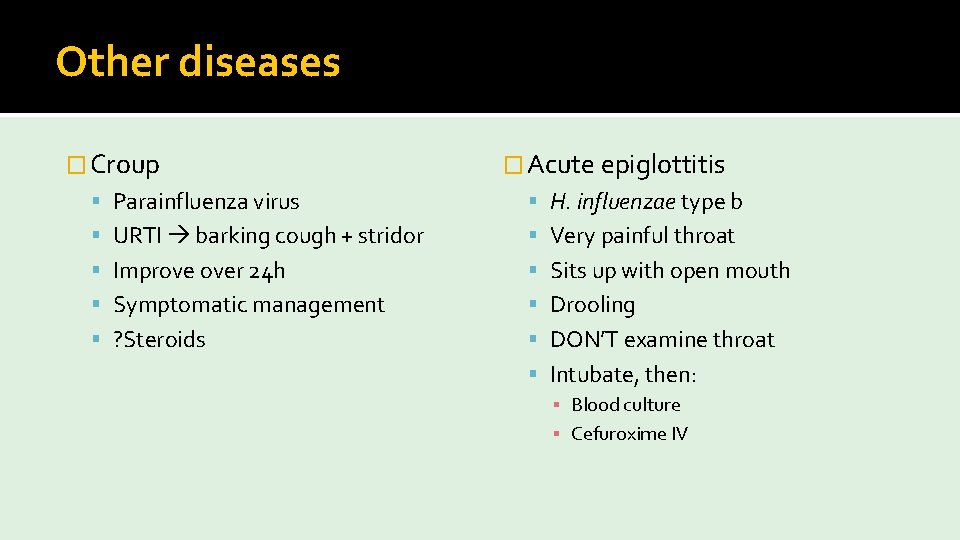
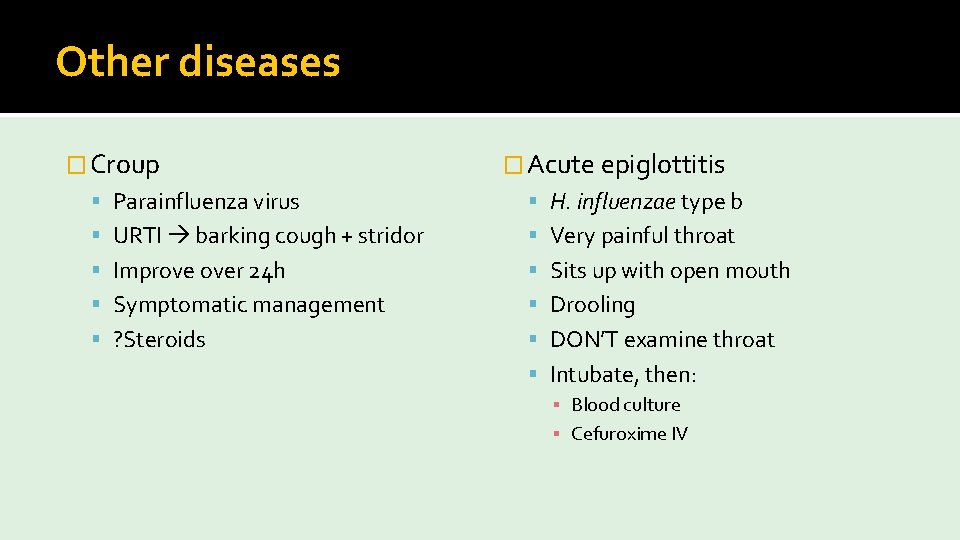
Other diseases � Croup � Acute epiglottitis Parainfluenza virus H. influenzae type b URTI barking cough + stridor Very painful throat Improve over 24 h Sits up with open mouth Symptomatic management Drooling ? Steroids DON’T examine throat Intubate, then: ▪ Blood culture ▪ Cefuroxime IV
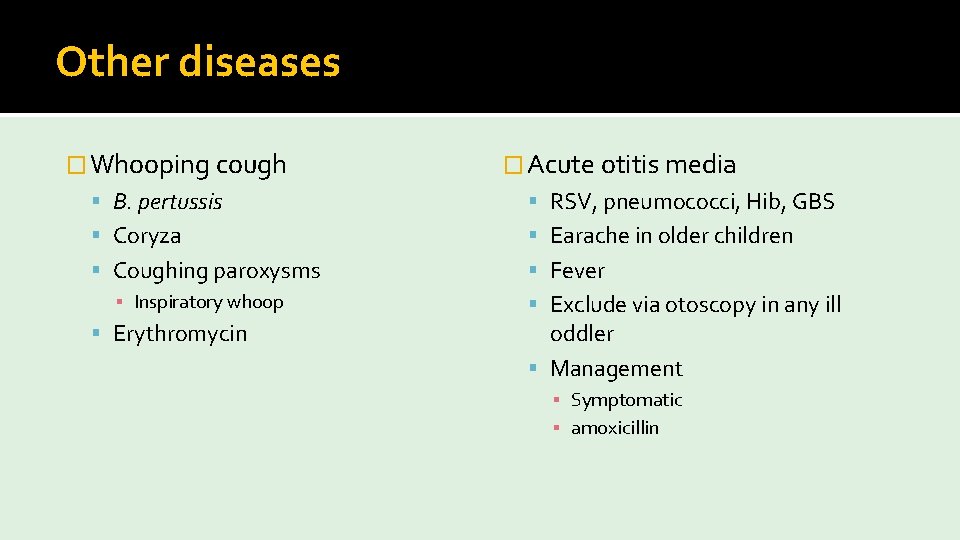
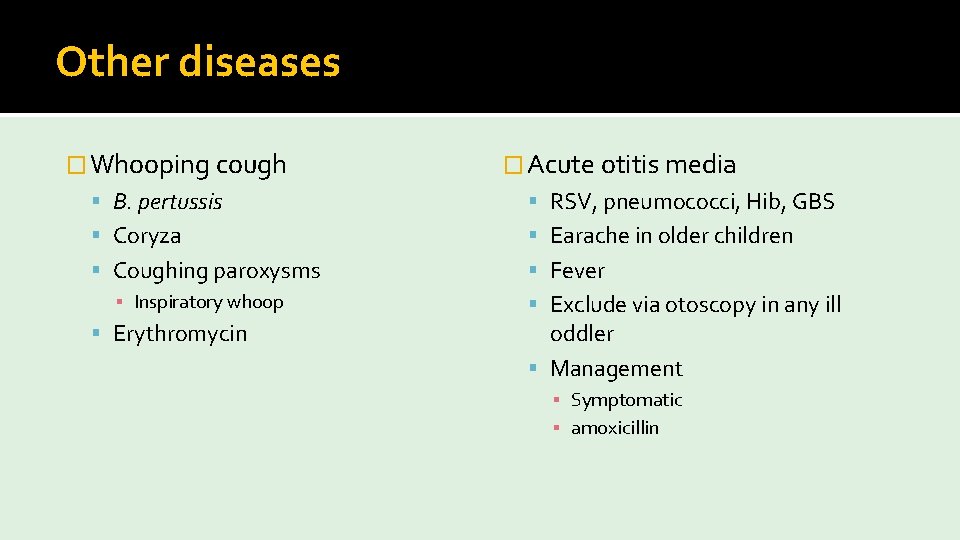
Other diseases � Whooping cough � Acute otitis media B. pertussis RSV, pneumococci, Hib, GBS Coryza Earache in older children Coughing paroxysms Fever ▪ Inspiratory whoop Erythromycin Exclude via otoscopy in any ill oddler Management ▪ Symptomatic ▪ amoxicillin
Thank you!
 Doctor doctor google drive
Doctor doctor google drive Dr suman jana
Dr suman jana Dr ash stamford university
Dr ash stamford university Phase one denial
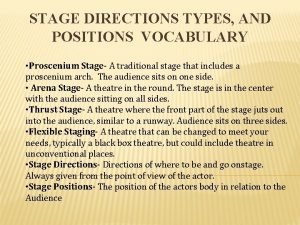
Phase one denial Upstage right
Upstage right Arena
Arena What is two stage tendering
What is two stage tendering Downstage and upstage
Downstage and upstage House left vs stage left
House left vs stage left Were you at the beach last weekend
Were you at the beach last weekend What did you do over the weekend
What did you do over the weekend Uheaa contact
Uheaa contact Class maths student student1 class student string name
Class maths student student1 class student string name National student clearinghouse student tracker
National student clearinghouse student tracker