Antepartum Fetal Health Assessment Associate Professor Dr Atiwut
























- Slides: 67
Antepartum Fetal Health Assessment Associate Professor Dr Atiwut Kamudhamas Department of Obstetrics and Gynecology Faculty of Medicine Thammasat University
Definition Fetal health assessment during the viable period before true labor pain
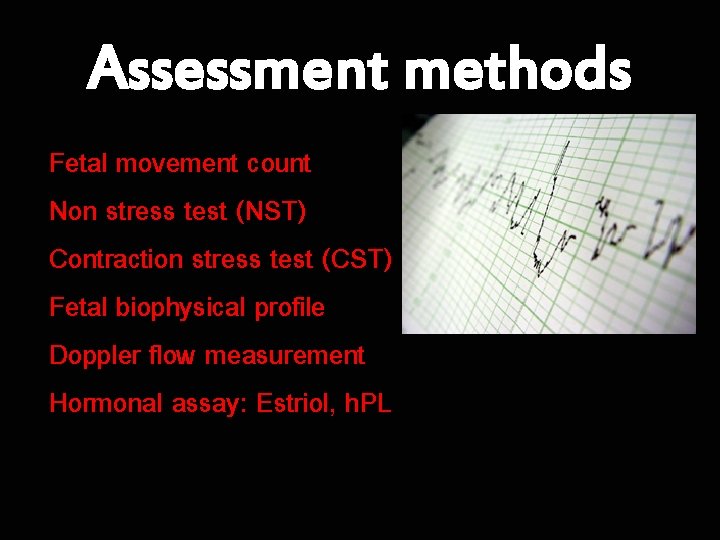
Assessment methods Fetal movement count Non stress test (NST) Contraction stress test (CST) Fetal biophysical profile Doppler flow measurement Hormonal assay: Estriol, h. PL

Fetal movement count
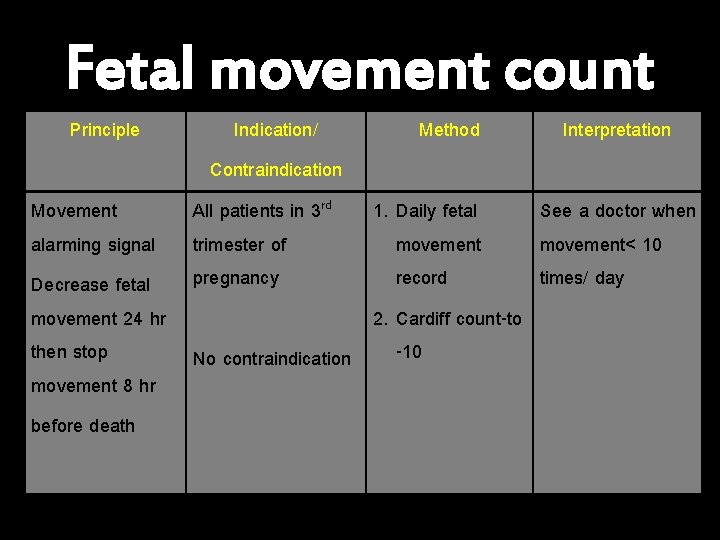
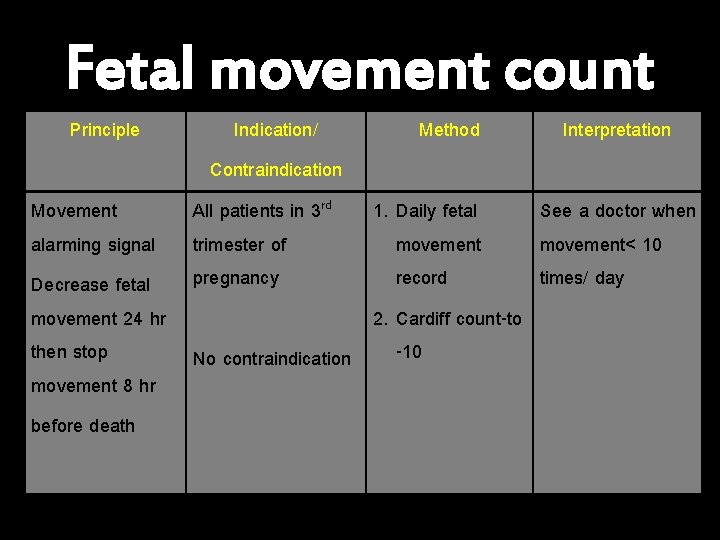
Fetal movement count Principle Indication/ Contraindication All patients in 3 rd trimester of pregnancy Method Interpretation Movement 1. Daily fetal See a doctor when alarming signal movement< 10 record times/ day Decrease fetal movement 24 hr 2. Cardiff count-to then stop -10 No contraindication movement 8 hr before death


Fetal behavioral states – – State 1 F : quiet sleep State 2 F : active sleep (rapid eye movement) State 3 F : quiet awake State 4 F : active awake (FHR acceleration + vigorous body movement + REM)


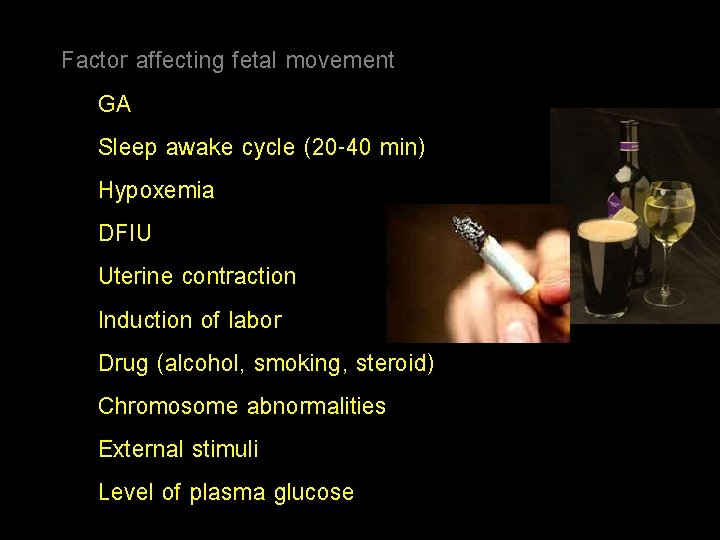
Factor affecting fetal movement GA Sleep awake cycle (20 -40 min) Hypoxemia DFIU Uterine contraction Induction of labor Drug (alcohol, smoking, steroid) Chromosome abnormalities External stimuli Level of plasma glucose



Factor affecting perception of movement Placental site Amniotic fluid volume GA Obesity Anxiety
Management NST
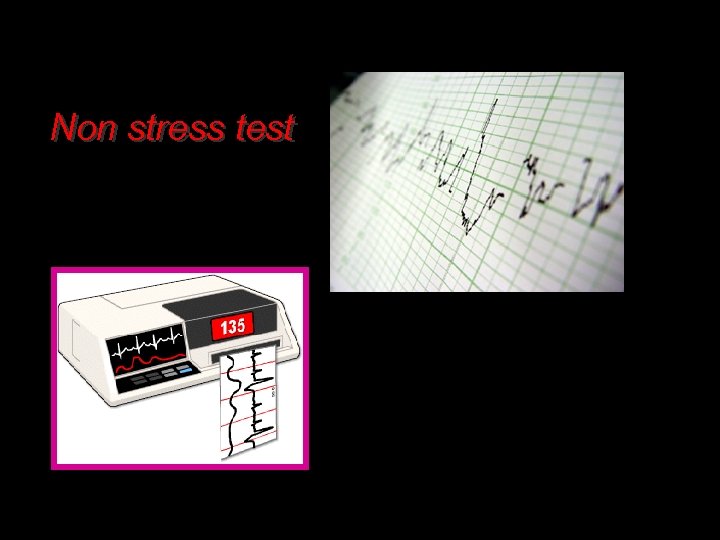
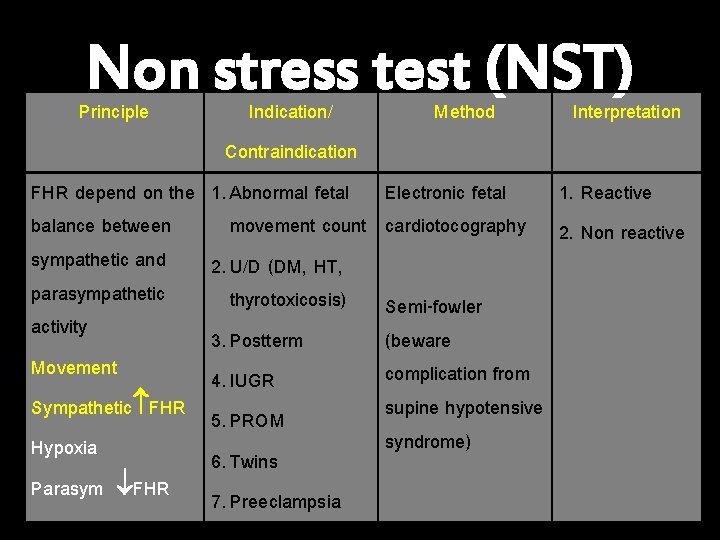
Non stress test
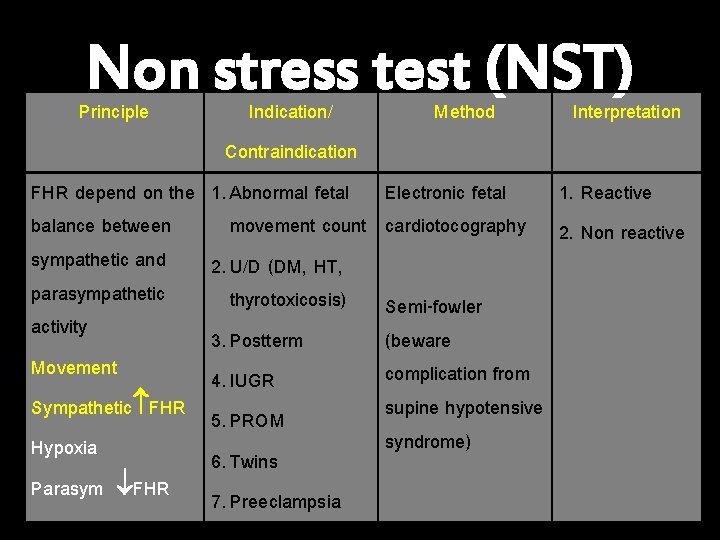
Non stress test (NST) Principle Indication/ Method Interpretation Contraindication FHR depend on the 1. Abnormal fetal balance between movement count sympathetic and 2. U/D (DM, HT, parasympathetic thyrotoxicosis) activity 3. Postterm Movement 4. IUGR Sympathetic FHR 5. PROM Hypoxia 6. Twins Parasym FHR 7. Preeclampsia Electronic fetal cardiotocography Semi-fowler (beware complication from supine hypotensive syndrome) 1. Reactive 2. Non reactive

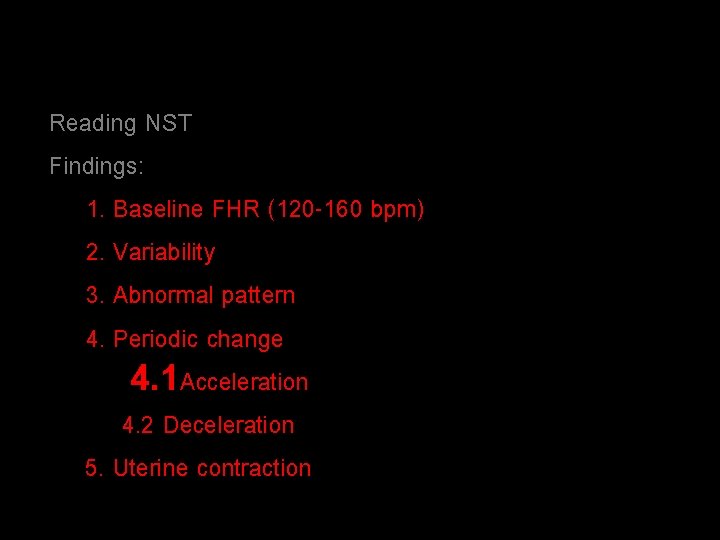
Reading NST Findings: 1. Baseline FHR (120 -160 bpm) 2. Variability 3. Abnormal pattern 4. Periodic change 4. 1 Acceleration 4. 2 Deceleration 5. Uterine contraction
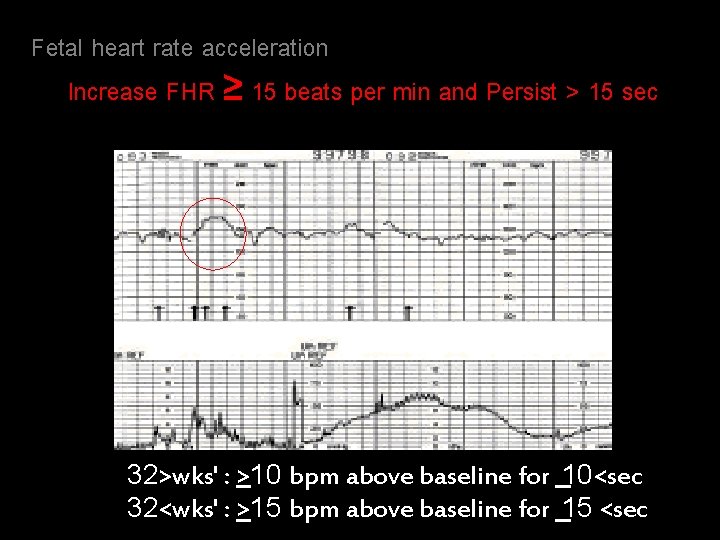
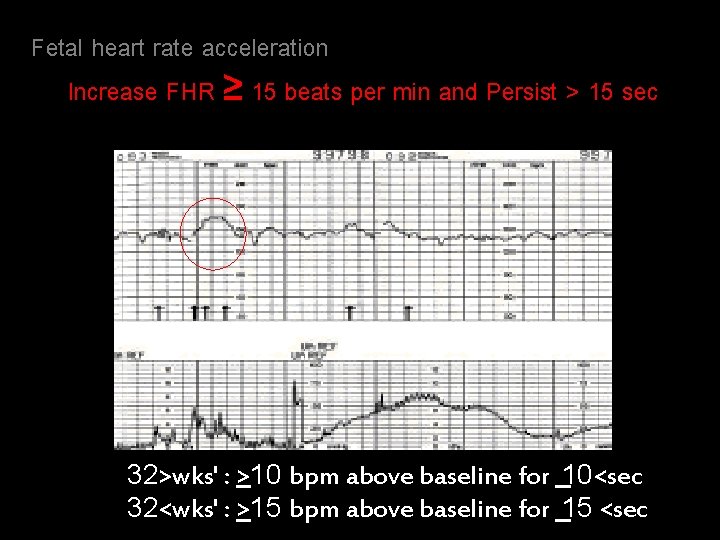
Fetal heart rate acceleration Increase FHR ≥ 15 beats per min and Persist > 15 sec 32>wks' : >10 bpm above baseline for 10<sec 32<wks' : >15 bpm above baseline for 15 <sec

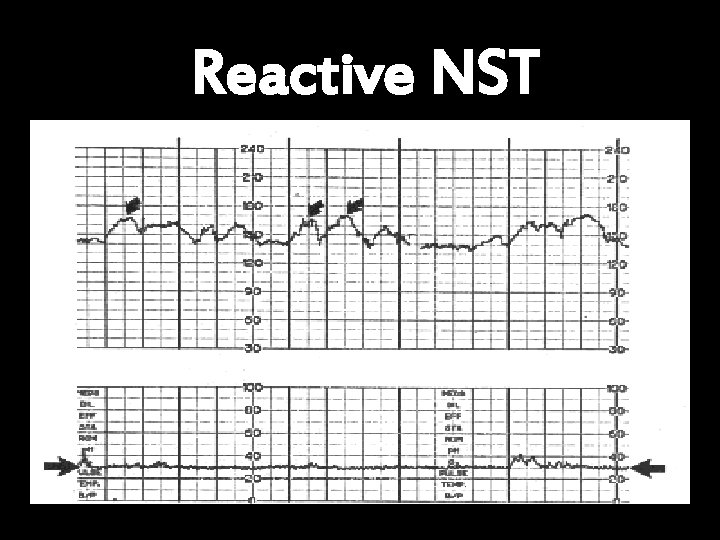
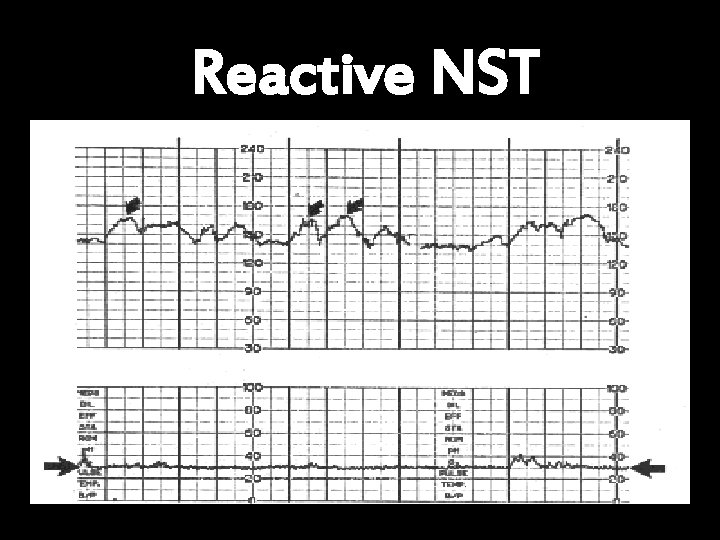
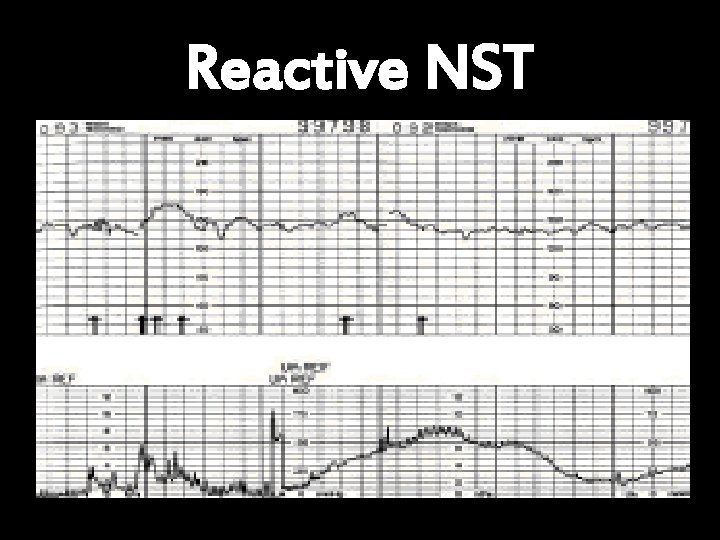
Reactive NST

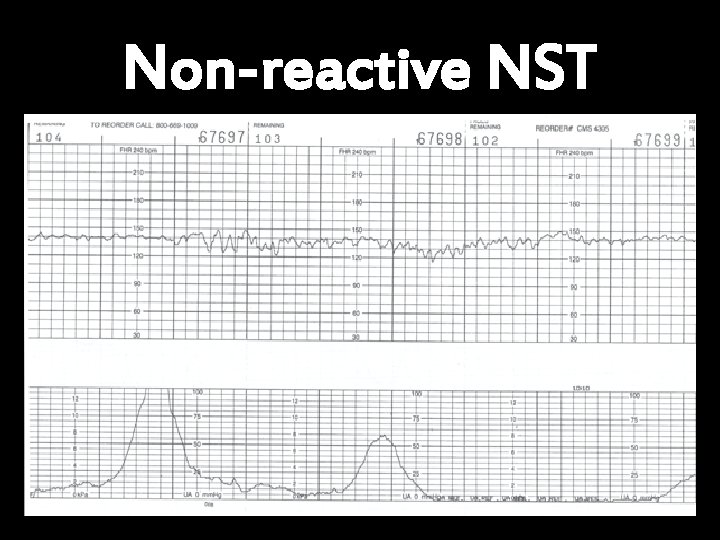
Non-reactive NST
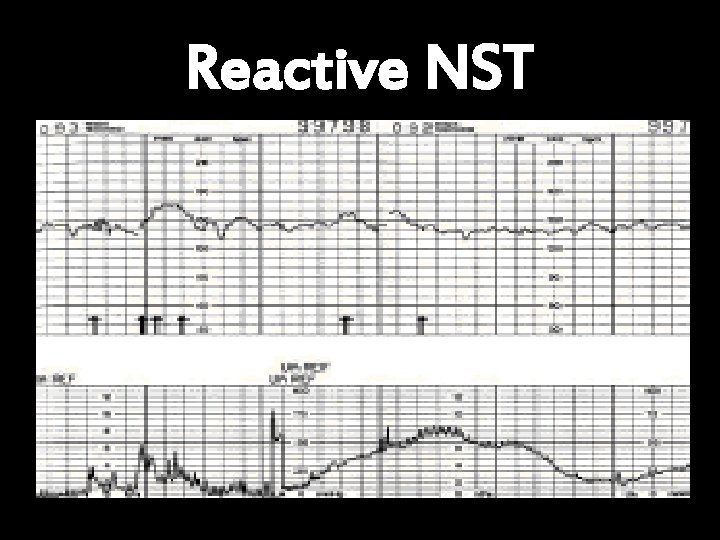
Reactive NST

Non-reactive NST with spontaneus deceleration
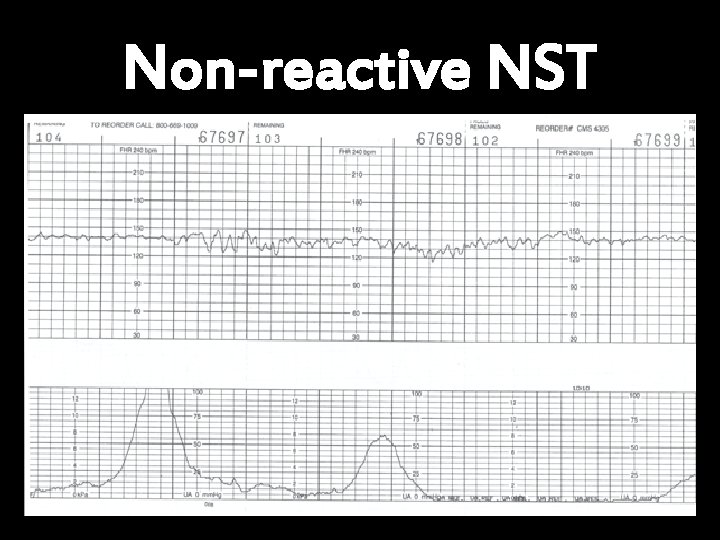
Non-reactive NST
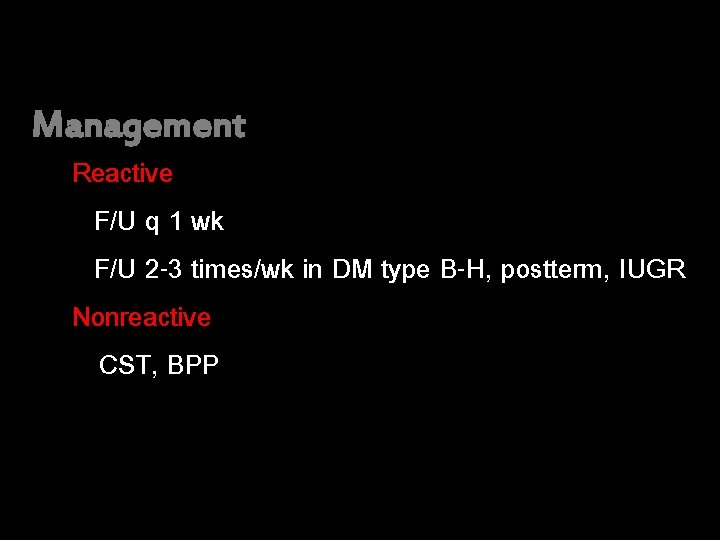
Management Reactive F/U q 1 wk F/U 2 -3 times/wk in DM type B-H, postterm, IUGR Nonreactive CST, BPP
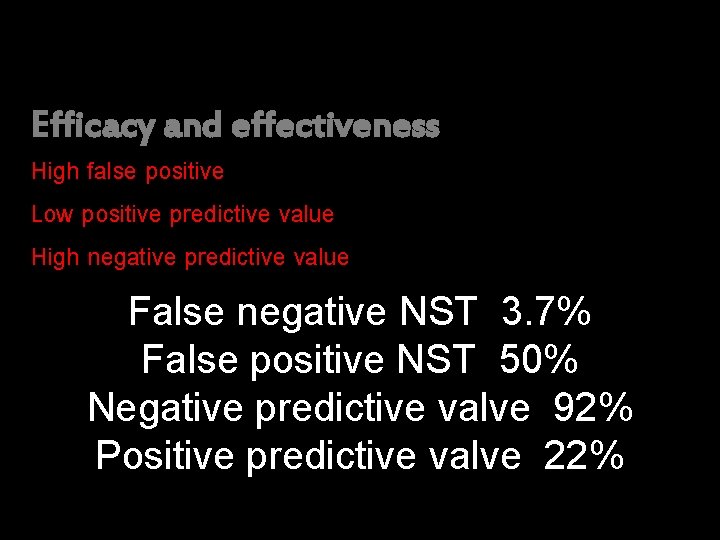
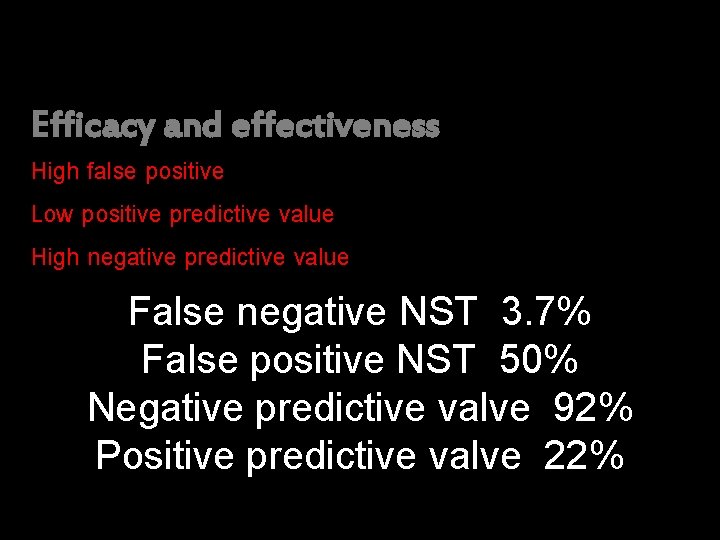
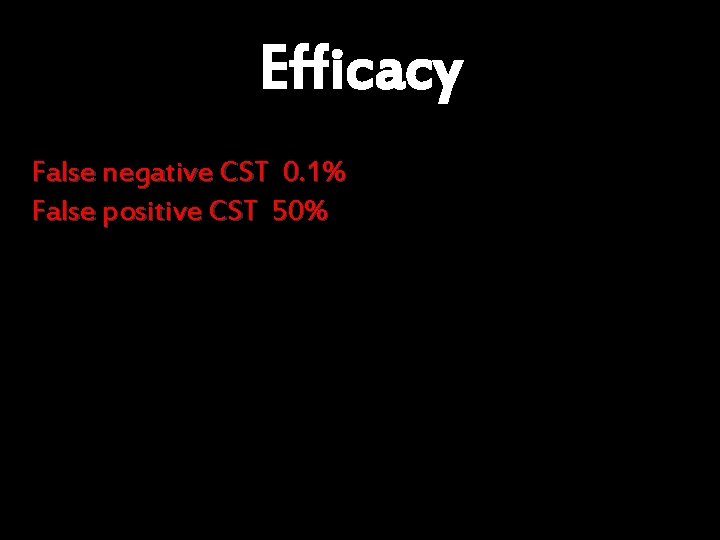
Efficacy and effectiveness High false positive Low positive predictive value High negative predictive value False negative NST 3. 7% False positive NST 50% Negative predictive valve 92% Positive predictive valve 22%
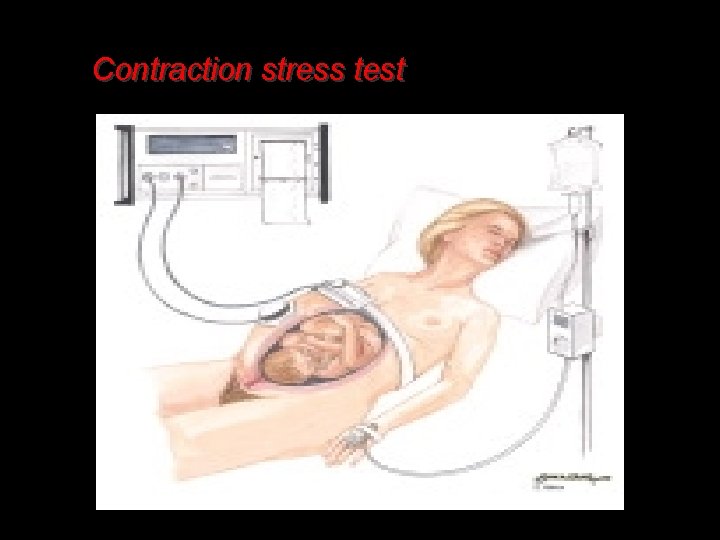
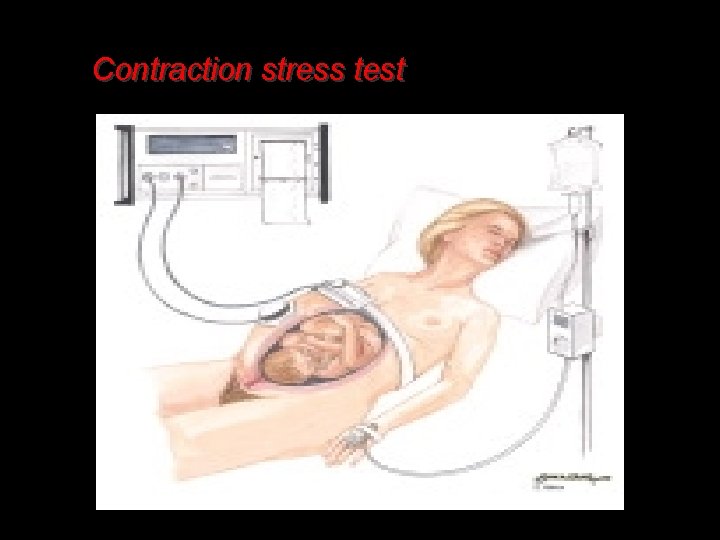
Contraction stress test

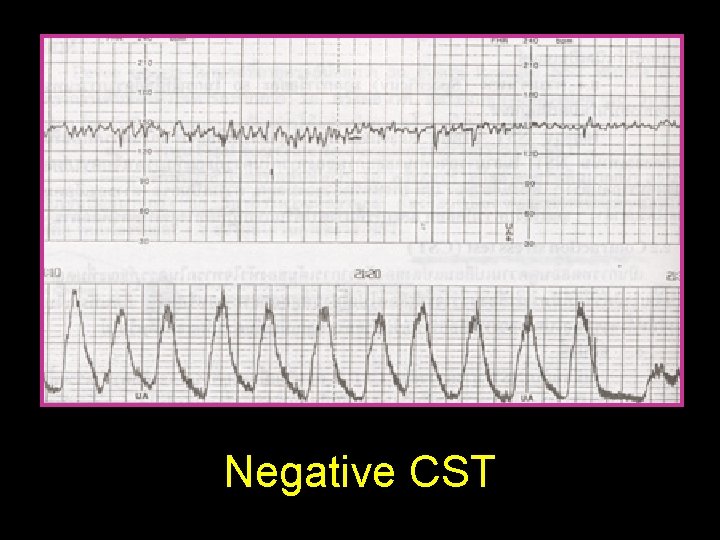
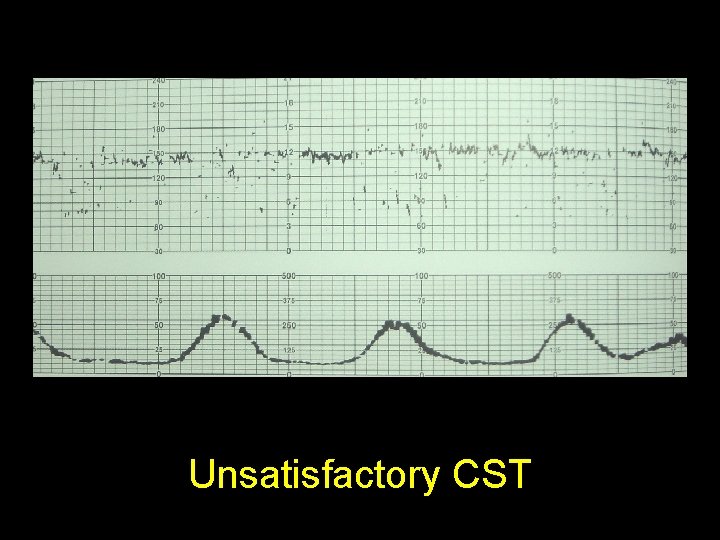
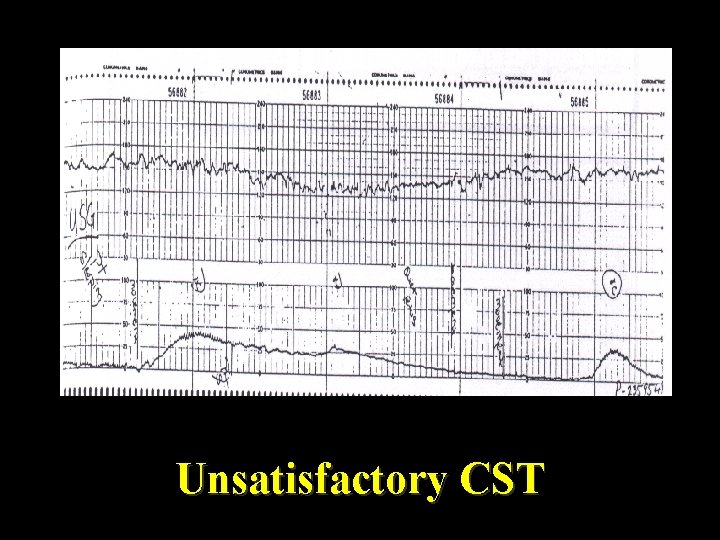
Contraction stress test (CST) Principle Uterine contraction hypoxemia FHR Indication/ Method Contraindication Nonreactive NST 1. OCT 2. Nipple Contraindication stimulation test (See next slide) Interpretation 1. Negative 2. Positive 3. Suspicious 4. Hyperstimulation 5. Unsatisfactory
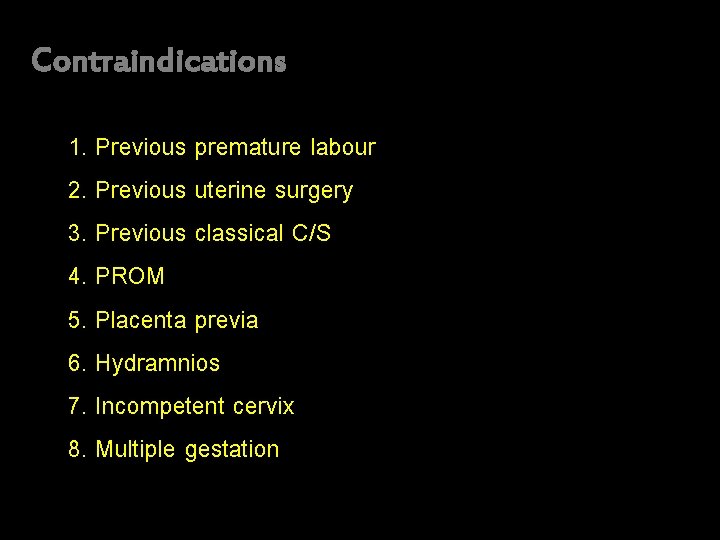
Contraindications 1. Previous premature labour 2. Previous uterine surgery 3. Previous classical C/S 4. PROM 5. Placenta previa 6. Hydramnios 7. Incompetent cervix 8. Multiple gestation
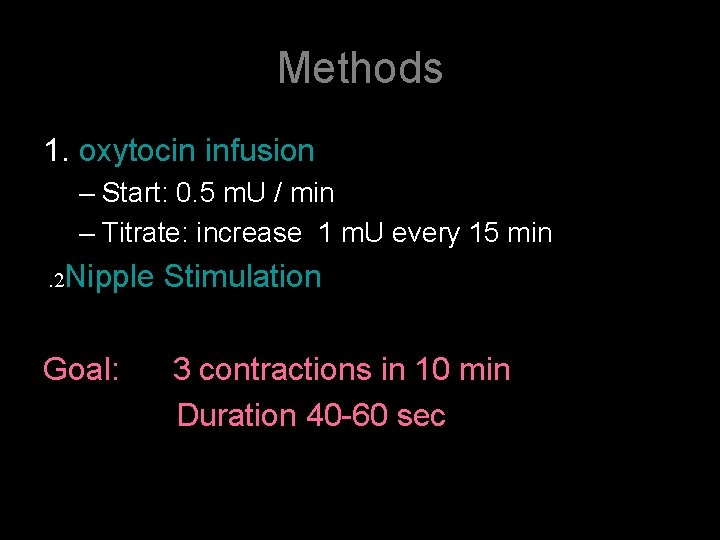
Methods 1. oxytocin infusion – Start: 0. 5 m. U / min – Titrate: increase 1 m. U every 15 min . 2 Nipple Stimulation Goal: 3 contractions in 10 min Duration 40 -60 sec

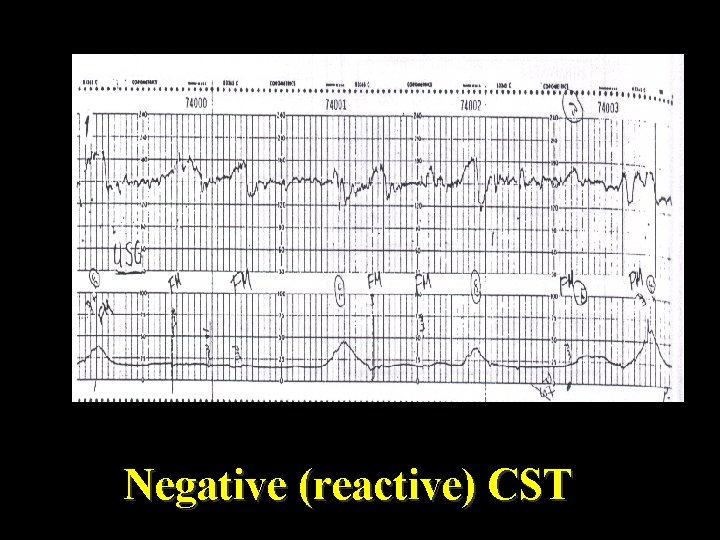
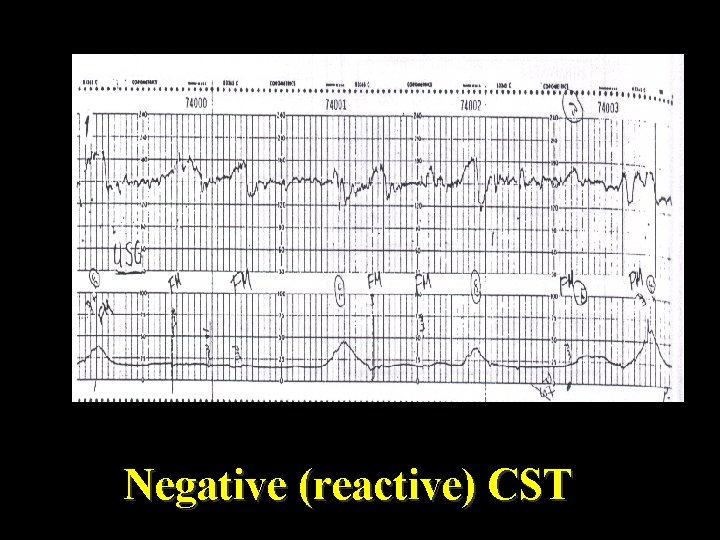
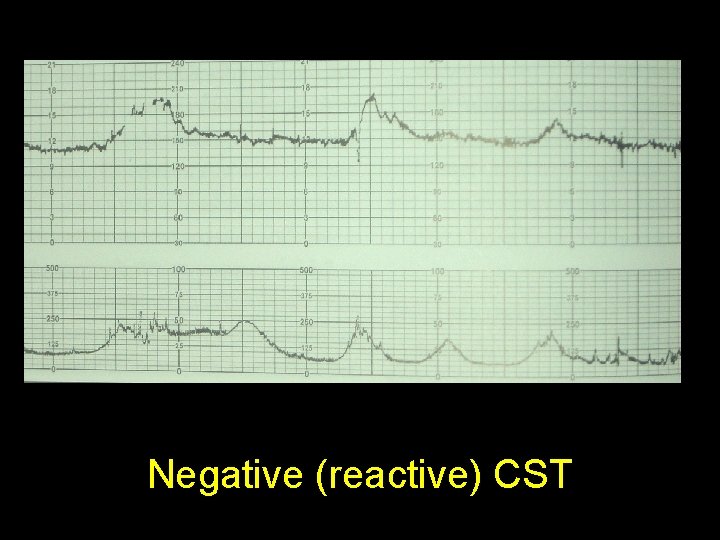
Negative (reactive) CST
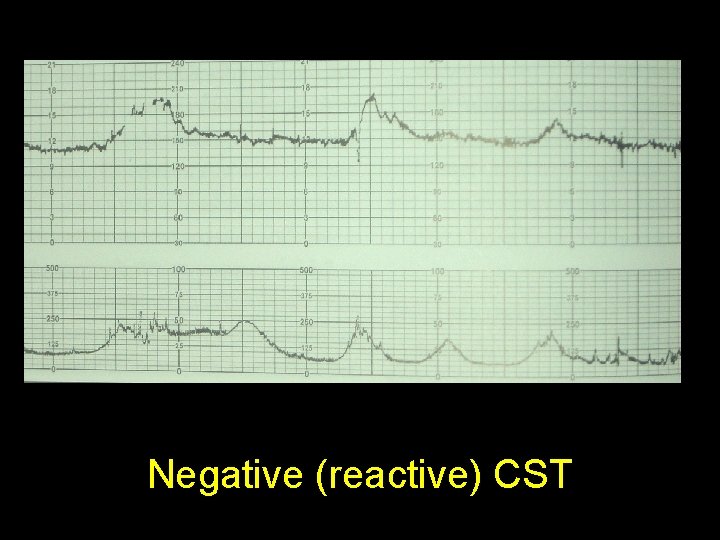
Negative (reactive) CST
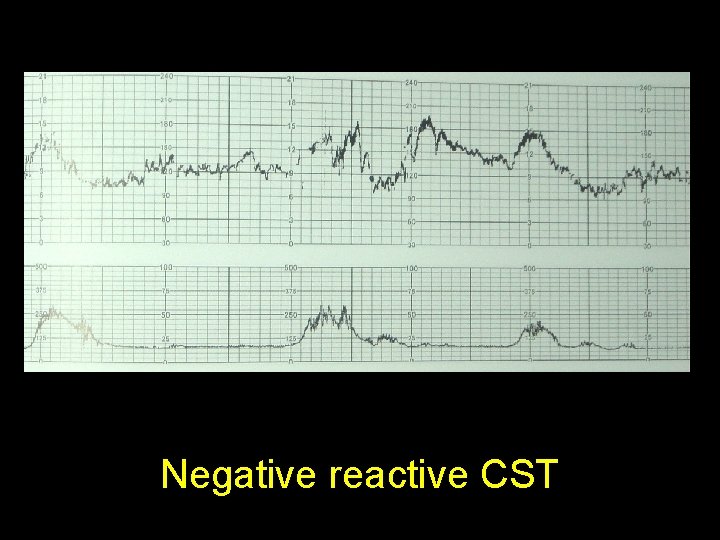
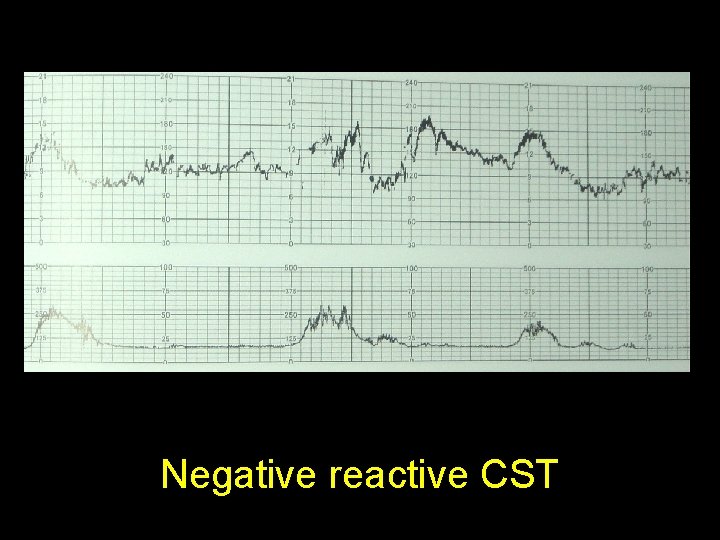
Negative reactive CST
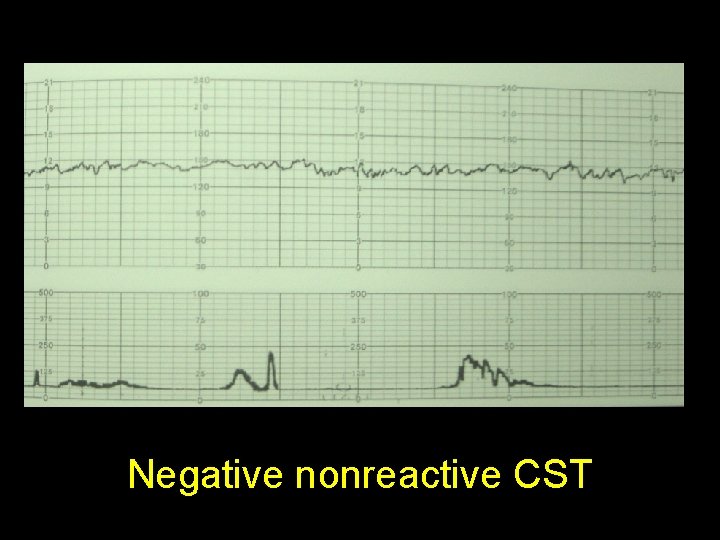
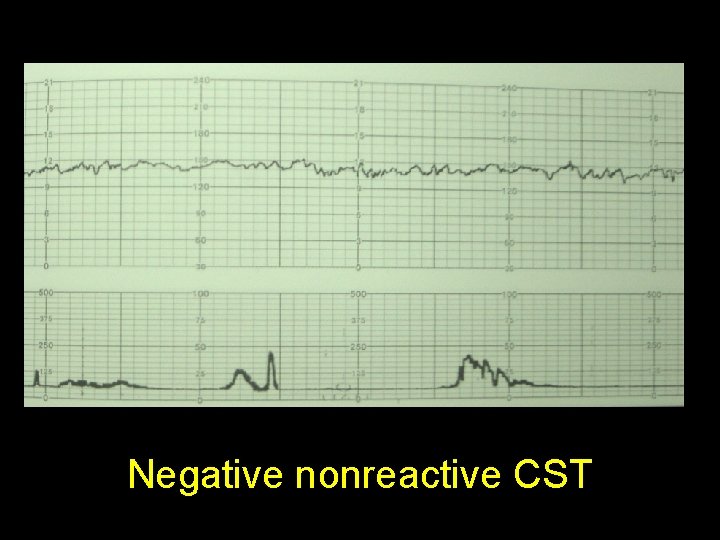
Negative nonreactive CST
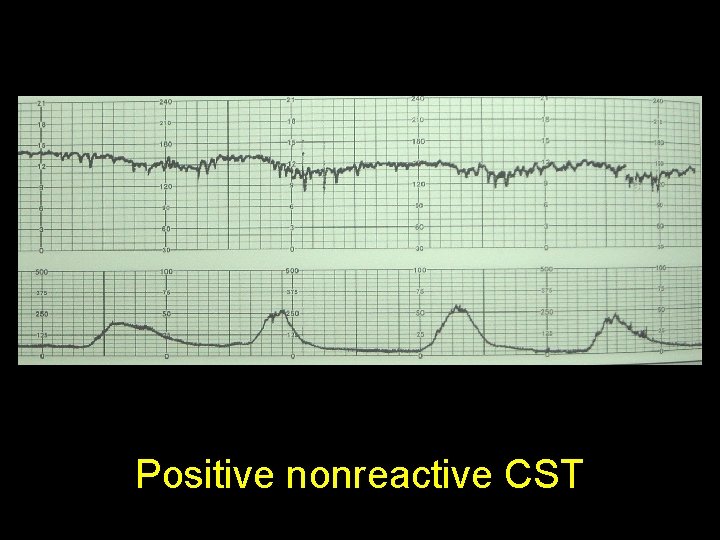
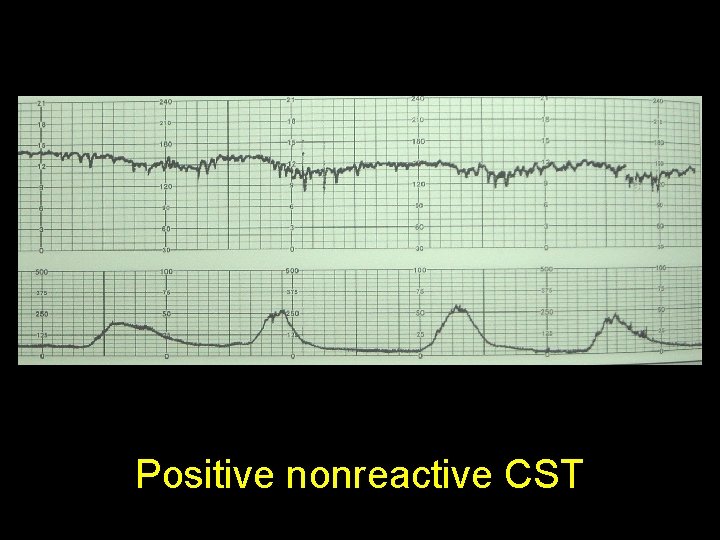
Positive nonreactive CST
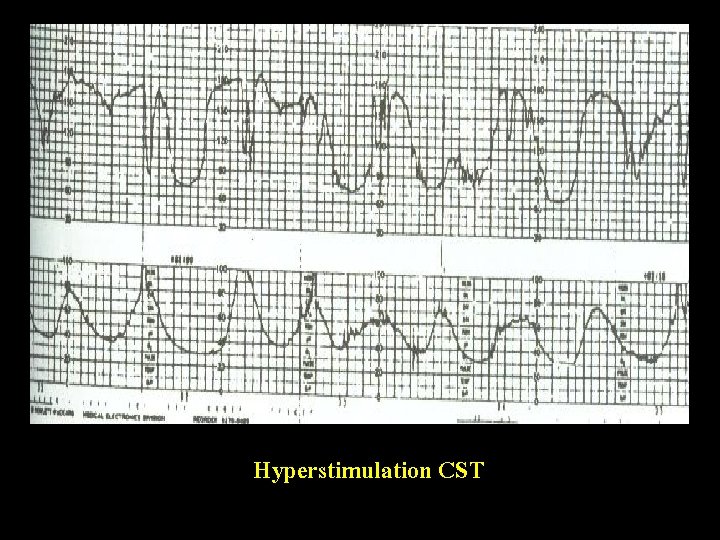
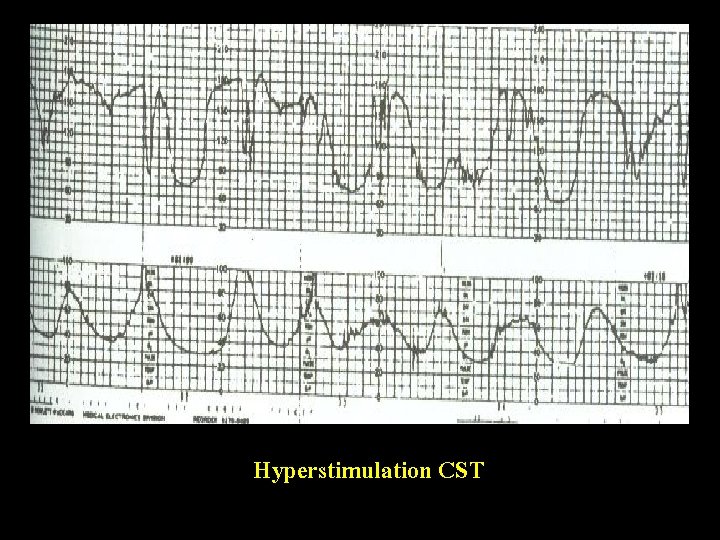
Hyperstimulation CST
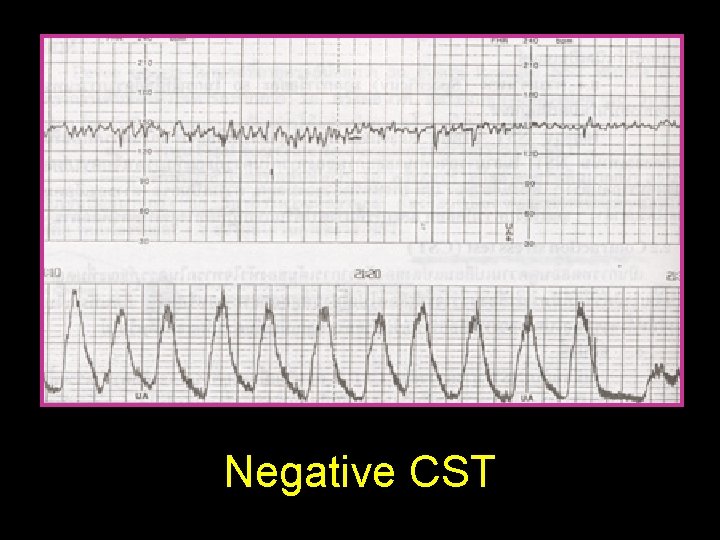
Negative CST
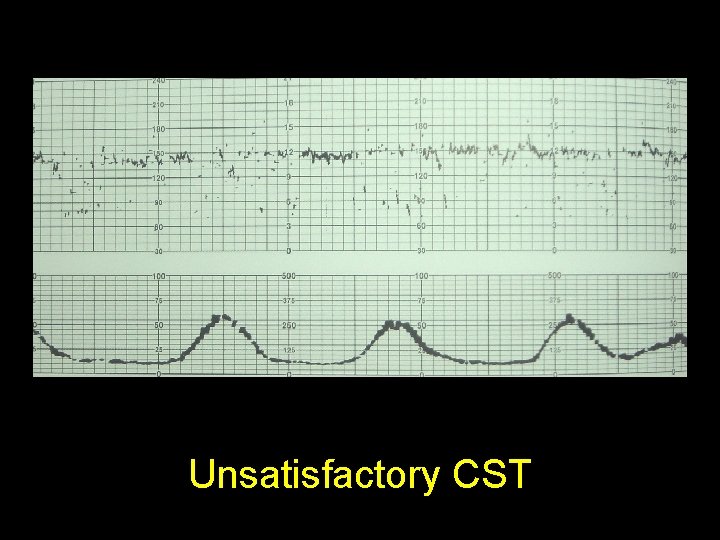
Unsatisfactory CST
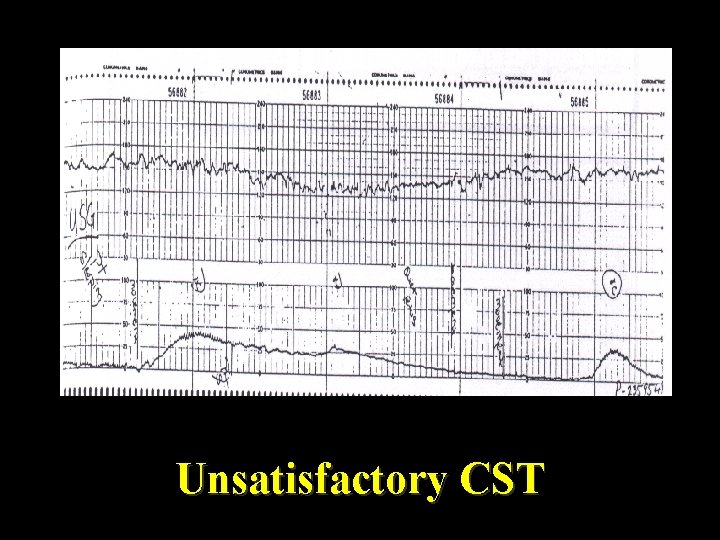
Unsatisfactory CST

Efficacy False negative CST 0. 1% False positive CST 50%
Fetal biophysical profile (BPP)
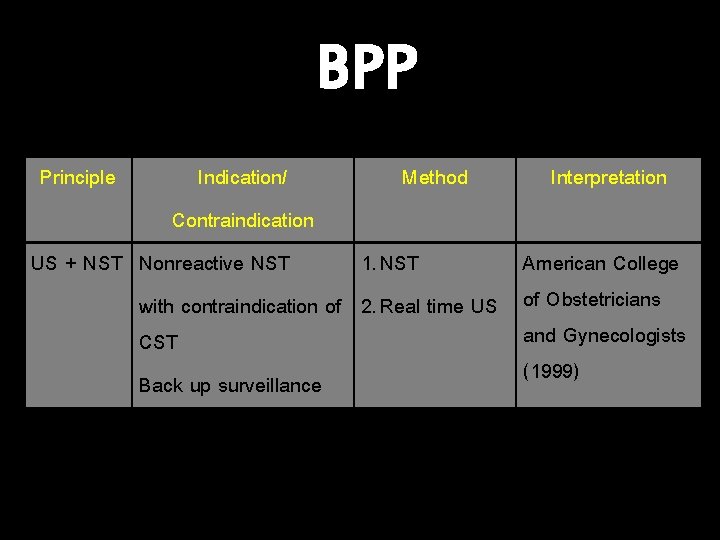
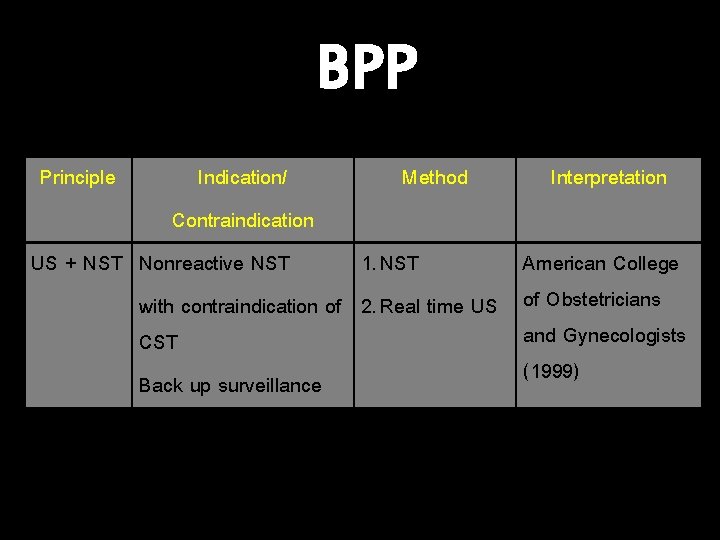
BPP Principle Indication/ Method Contraindication US + NST Nonreactive NST 1. NST with contraindication of 2. Real time US CST Back up surveillance Interpretation American College of Obstetricians and Gynecologists (1999)

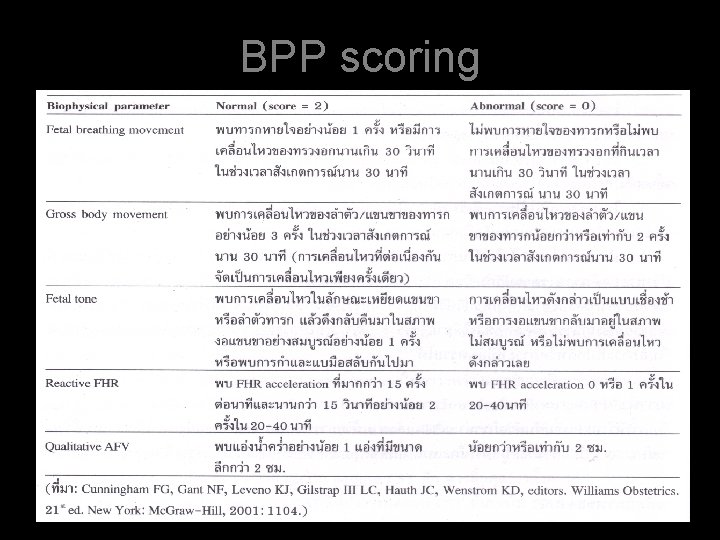
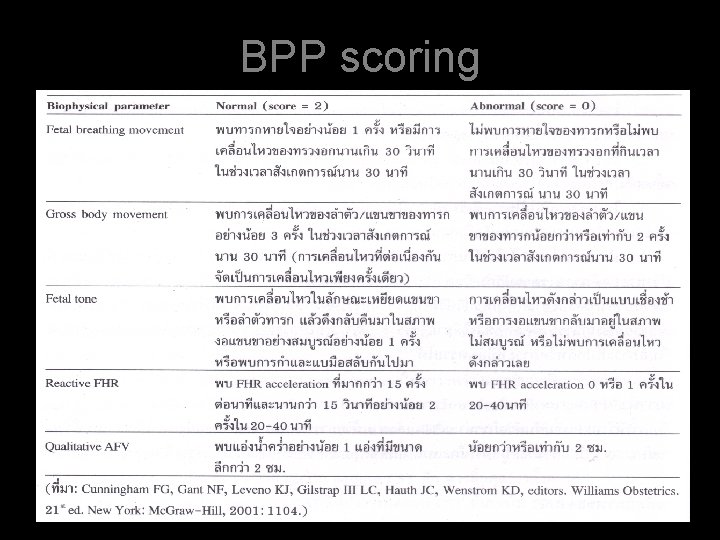
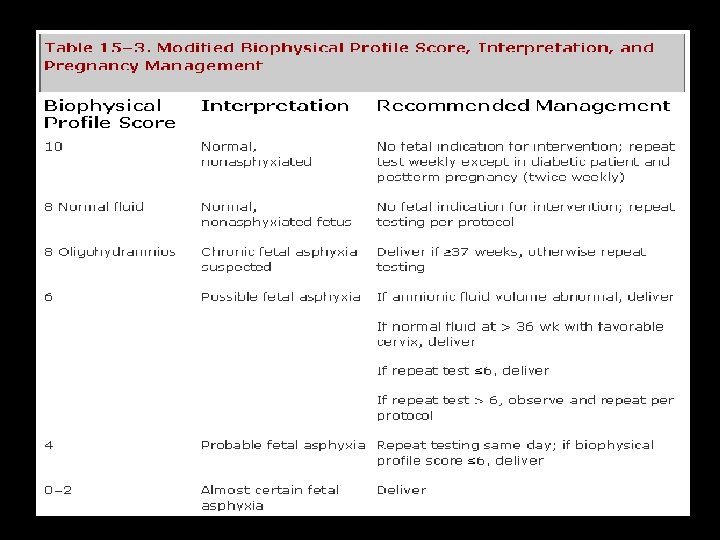
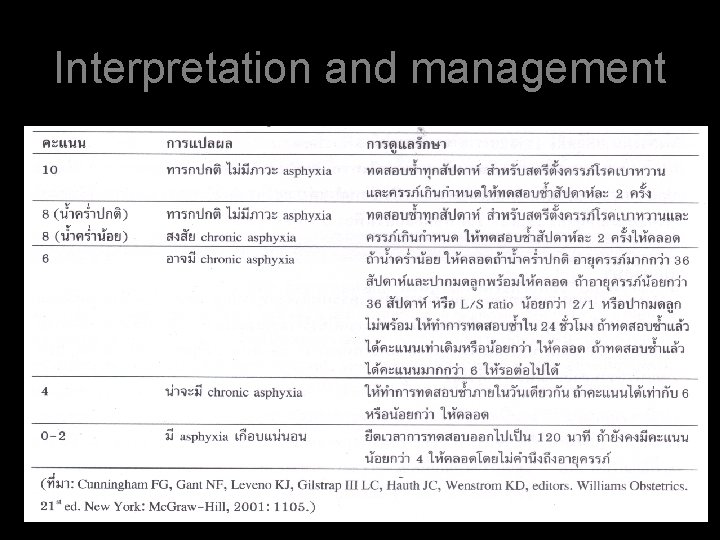
BPP scoring
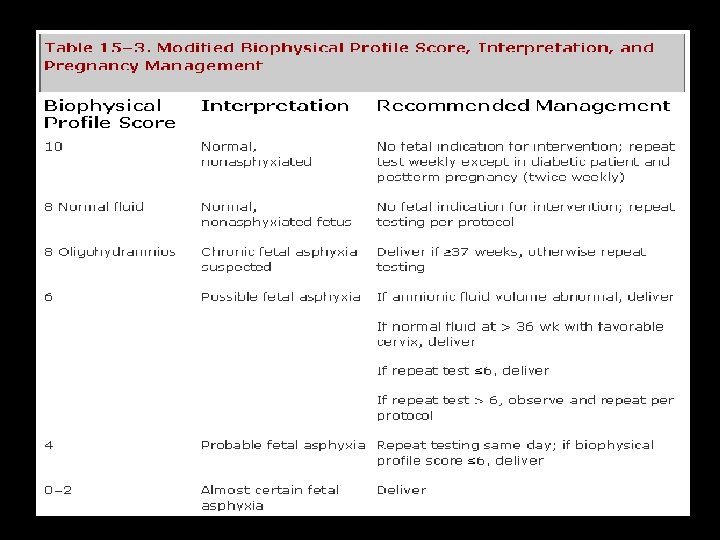
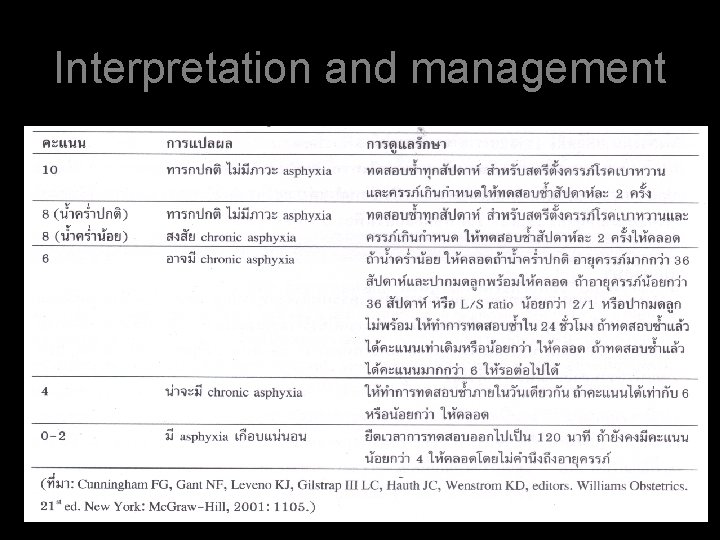
Interpretation and management


Efficacy • False negative BPP 0. 007% • False positive BPP 1%
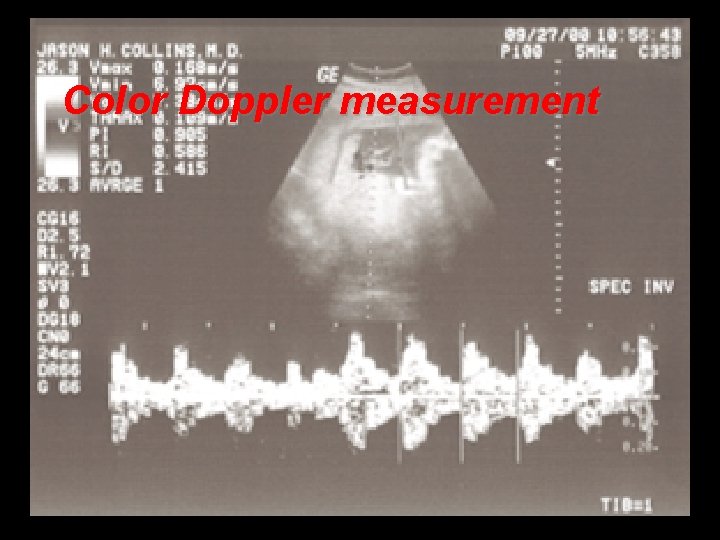
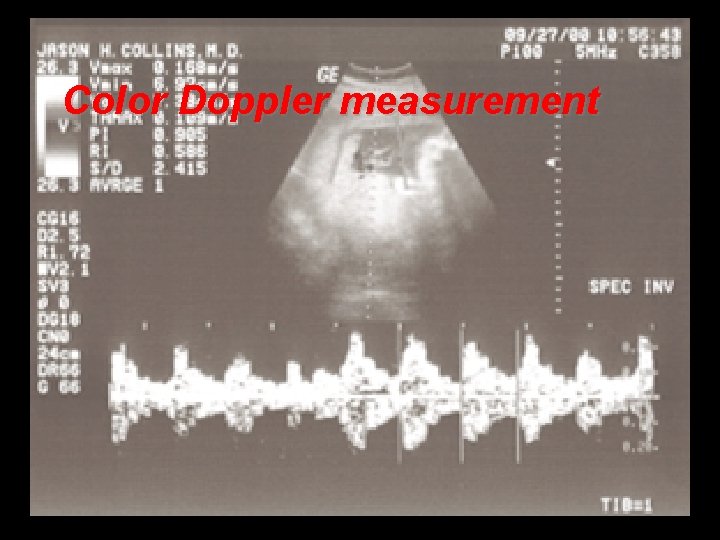
Color Doppler measurement

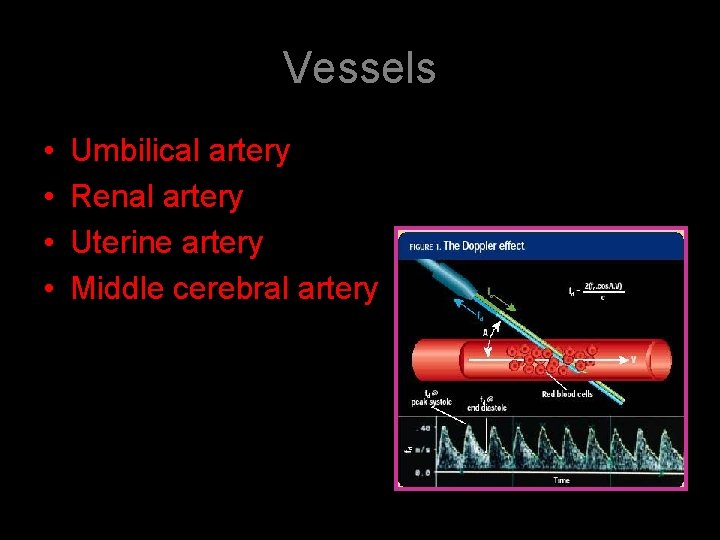
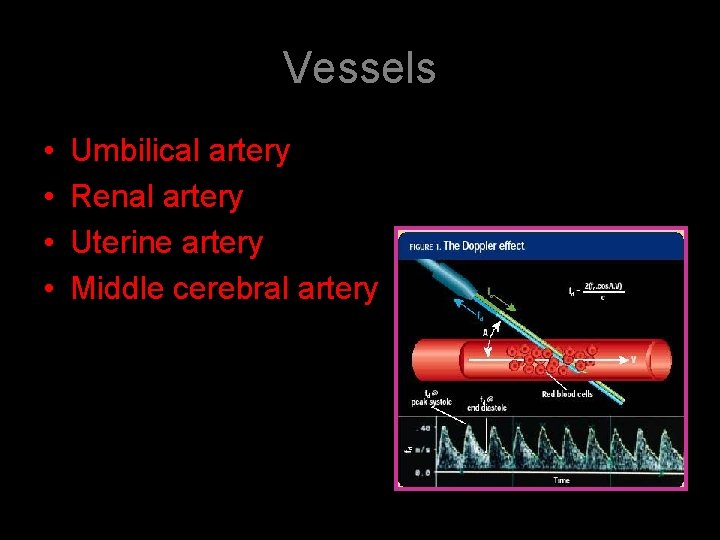
Vessels • • Umbilical artery Renal artery Uterine artery Middle cerebral artery
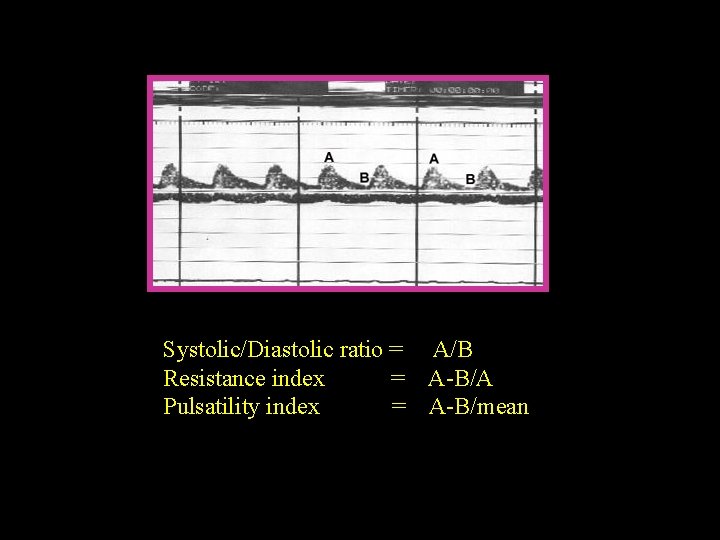
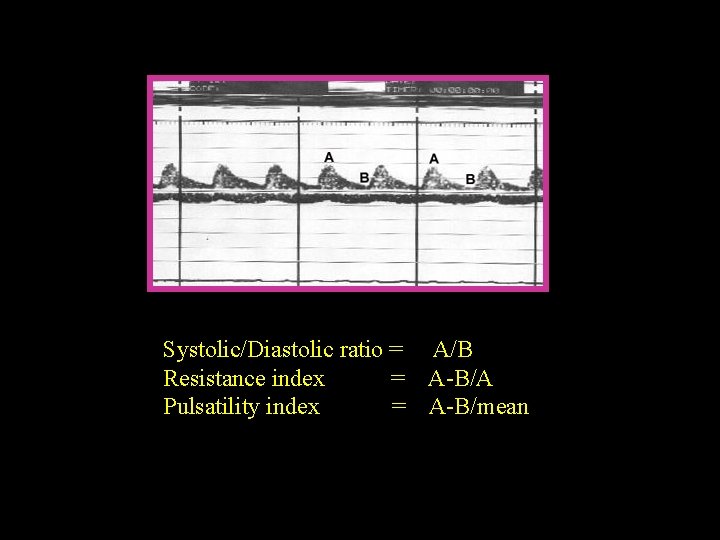
Systolic/Diastolic ratio = A/B Resistance index = A-B/A Pulsatility index = A-B/mean
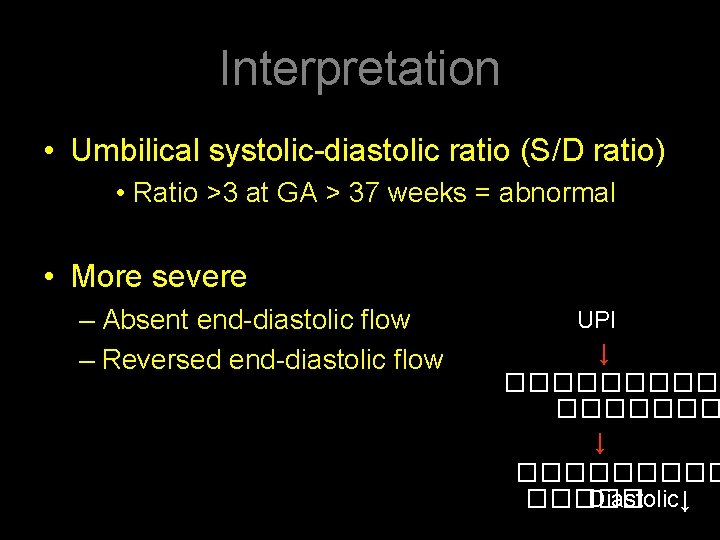
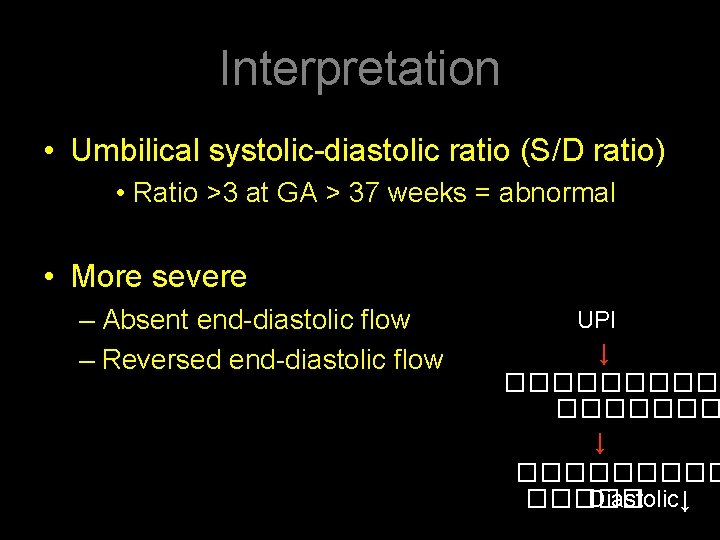
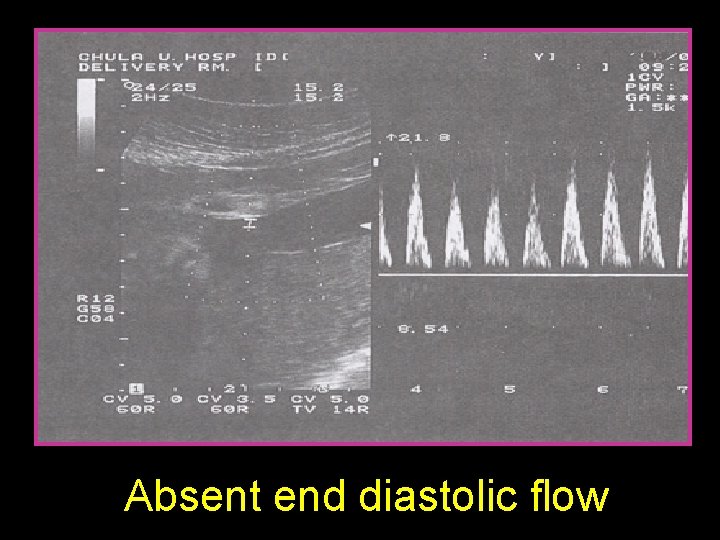
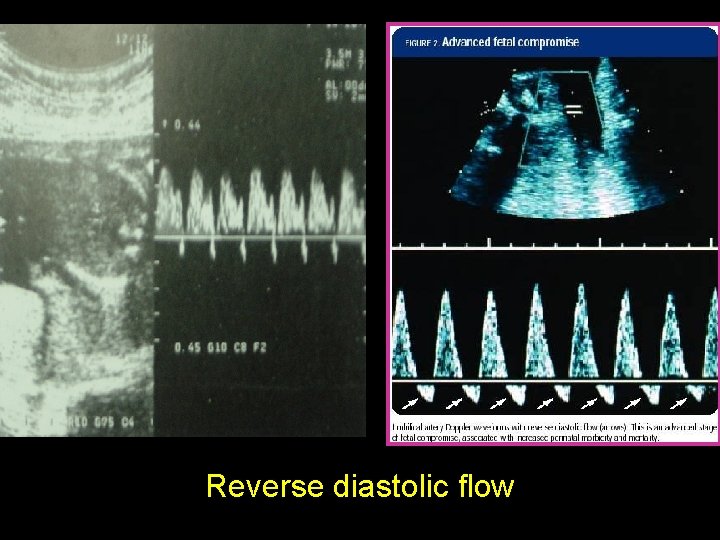
Interpretation • Umbilical systolic-diastolic ratio (S/D ratio) • Ratio >3 at GA > 37 weeks = abnormal • More severe – Absent end-diastolic flow – Reversed end-diastolic flow UPI ↓ ������� ↓ ����� Diastolic↓


Normal
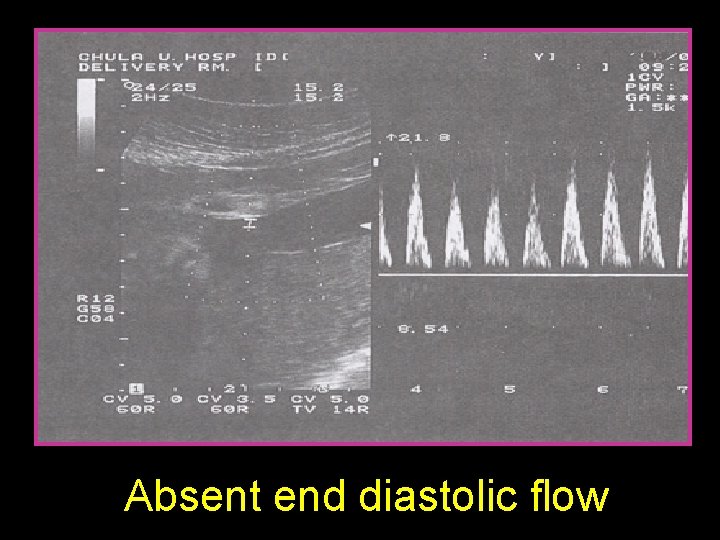
Absent end diastolic flow
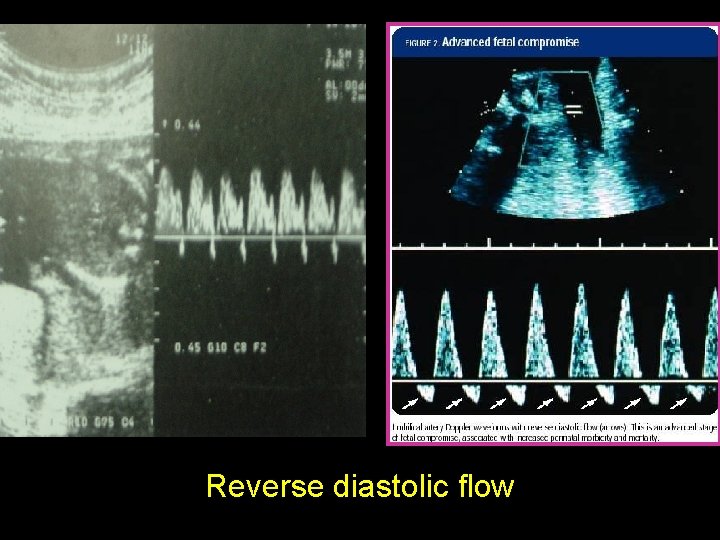
Reverse diastolic flow
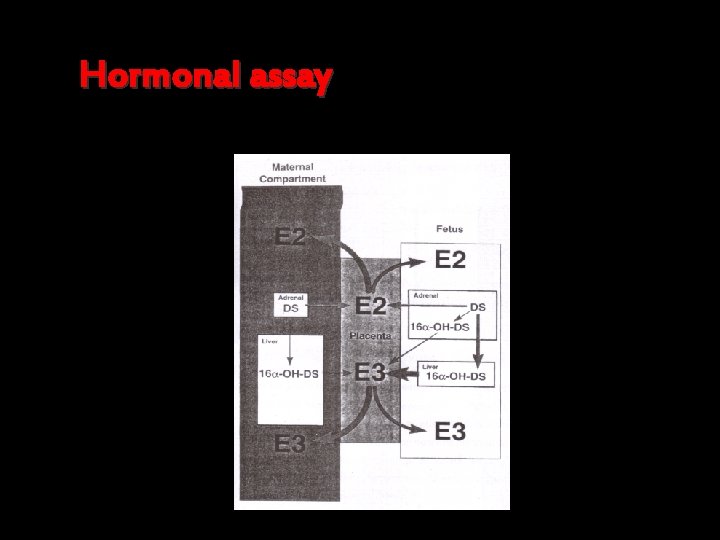
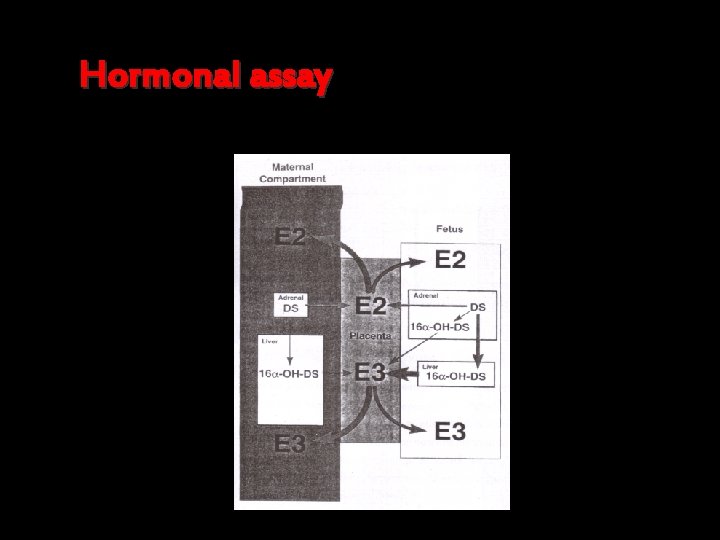
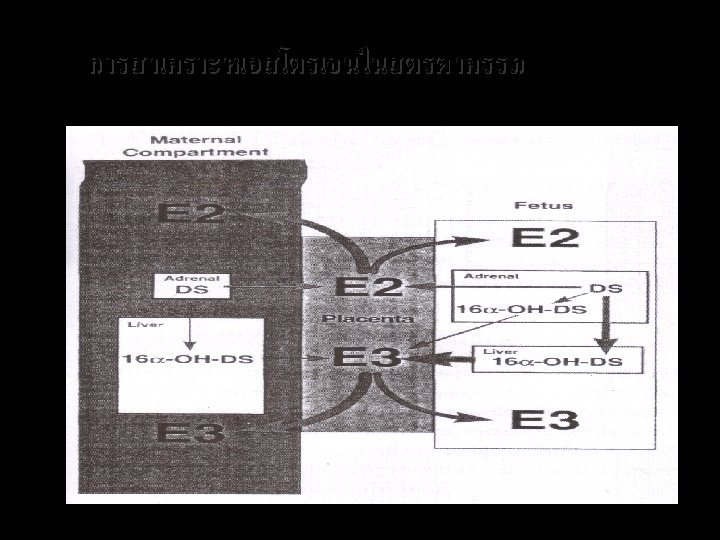
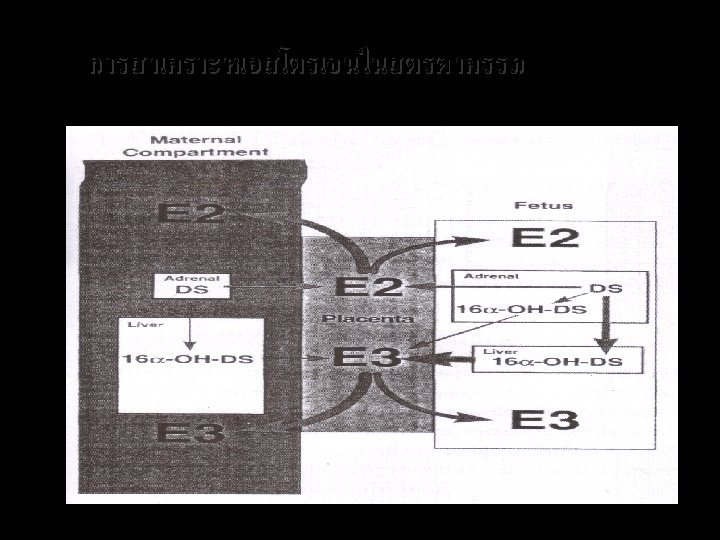
Hormonal assay



End of the session Thank you for your attention
 Promotion from assistant to associate professor
Promotion from assistant to associate professor Antipartum
Antipartum Klasifikasi perdarahan antepartum
Klasifikasi perdarahan antepartum Mbcs membership
Mbcs membership Tecniche associate al pensiero computazionale
Tecniche associate al pensiero computazionale The pyramid at chichen itza is most closely associate with
The pyramid at chichen itza is most closely associate with Lone star college nursing score sheet
Lone star college nursing score sheet Incose certification
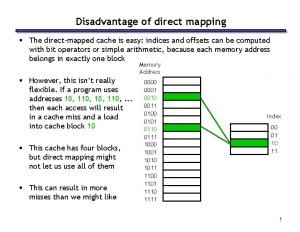
Incose certification Direct mapping advantages and disadvantages
Direct mapping advantages and disadvantages Home institution declaration cern
Home institution declaration cern Associate's degree in the netherlands
Associate's degree in the netherlands Berstoff gearbox repair
Berstoff gearbox repair Jeannie watkins
Jeannie watkins Rcog cpd portfolio
Rcog cpd portfolio Kosten tio hbo
Kosten tio hbo Associate director meaning
Associate director meaning Harper college
Harper college Iter project associate
Iter project associate Michelin aad program
Michelin aad program Los angeles harbor college catalog
Los angeles harbor college catalog Involves scrutinizing any information that you read or hear
Involves scrutinizing any information that you read or hear Delta chi flag
Delta chi flag Associate degree rmit
Associate degree rmit Adobe certified associate visual design specialist
Adobe certified associate visual design specialist Cincinnati state associate degrees
Cincinnati state associate degrees Safety associate
Safety associate Associate warden
Associate warden Customer kpi
Customer kpi Imeche associate membership
Imeche associate membership To associate
To associate Hea associate fellowship
Hea associate fellowship Associate consultant in capgemini
Associate consultant in capgemini Associate program
Associate program Associate consultant in capgemini
Associate consultant in capgemini Mhp associate partner gehalt
Mhp associate partner gehalt Ruckus certified partner
Ruckus certified partner Doctrine of ultra vires
Doctrine of ultra vires Marine corps league red blazer
Marine corps league red blazer Cipd professional discussion
Cipd professional discussion Name something you associate with superman
Name something you associate with superman Child development teacher permit
Child development teacher permit Documentation portfolio example
Documentation portfolio example Define dynamic assessment
Define dynamic assessment Portfolio assessment matches assessment to teaching
Portfolio assessment matches assessment to teaching Purpose of health assessment
Purpose of health assessment Health assessment
Health assessment Tim rapid health assessment adalah
Tim rapid health assessment adalah Occupational health and safety assessment series
Occupational health and safety assessment series Agility health
Agility health Ohio state health assessment
Ohio state health assessment Health and safety risk assessment template
Health and safety risk assessment template Chapter 5 lesson 2 mental disorders
Chapter 5 lesson 2 mental disorders Population health risk assessment and management
Population health risk assessment and management Component of health assessment
Component of health assessment Pamela schwartz kaiser
Pamela schwartz kaiser Hospital based health technology assessment
Hospital based health technology assessment Health technology assessment in india
Health technology assessment in india Key informant interview questions community assessment
Key informant interview questions community assessment Integrative health and wellness assessment ihwa
Integrative health and wellness assessment ihwa Health needs assessment
Health needs assessment Action gereedschapskoffer
Action gereedschapskoffer Methods of health assessment
Methods of health assessment Health assessment definition
Health assessment definition Wwe
Wwe Obito fetal grados de maceracion
Obito fetal grados de maceracion Primer plano de hodge
Primer plano de hodge Sindrome alcoholico fetal chile
Sindrome alcoholico fetal chile Circulação fetal
Circulação fetal