Health Assessment Definition of Health History health history


- Slides: 30
= Health Assessment
Definition of Health History health history defined as the systematic collection of subjective data which stated with client, and objective data which observed by the nurse or midwife.
Phases of taking health history It takes two phases: - The interview phase The recording phase
Guidelines for Taking health History Establish private, comfortable, and quiet environment. Allow the client to state problems and expectations for the interview. Provide the client with an orientation to the structure, purposes, and expectations of the history. Communicate and allow priorities with the client. Listen more than you talk. Observe non verbal communications e. g. "body language, voice tone, and appearance".
review information before starting interview. Clarify& rationalize the client condition. Avoid questions that can be answered as yes or no Record the health history as soon as possible after the interview.
n n n Types of Assessment • Initial comprehensive assessment • Ongoing or partial assessment • Focused or problem-oriented assessment • Emergency assessment • Time-lapsed assessment
Types of Health History A complete health history : This is taken on initial visits to health care facilities. partial : An interval health history used to collect information in visits following the one in which an initial data base is collected. A problem- focused health history used to collect data about a specific problem system or region.
n n Sources of Data • Primary source: – data directly gathered from the client using interview and physical examination.
n n n Sources of Data • Secondary source: – data gathered from client’s family members, significant others, client’s medical records/chart, other members of health team, and related care literature/journals
Components of Health History 1 -Biographical Data: This includes Full name Address and telephone numbers (client's permanent contact of client) Birth date and birth place. Sex Religion and race. Marital status. Social security number. Occupation (usual and present) Source of referral. Usual source of healthcare. Source and reliability of information. Date of interview.
2 - Chief Complaint: “Reason For Hospitalization”. The following are examples of adequately stated chief complaints: Chest pain for 3 days. Swollen ankles for 2 weeks. Fever and headache for 24 hours.
3 -History of present illness Gathering information relevant to the chief complaint, and the Onset of client's problem, .
Component of Present Illness Introduction: "client's summary and usual health". Investigation of symptoms: "onset, date, gradual or sudden, duration, precipitating factors, frequency, location, quality, and alleviating or aggravating factors". Relevant family information. Disability system "affected the client's total life".
4 - Past Health History: The purpose of the past history is to identify all major past health problems of the client. This includes. Childhood illness e. g. history of rheumatic fever. History of accidents and disabling injuries regard less he was hospitalized or not.
Past Health History. Cont… History of hospitalization includes time of admission and date of it with admitting diagnosis and the follow up care. History of operations "how and why this done" History of immunizations and allergies. Physical examinations and diagnostic tests.
5 -Family History The purpose of the family history is to learn about the general health of the client's blood relatives, spouse, and children and to identify any illness of environmental genetic, or familiar nature that might have implications for the client's current or future health problems and needs or to their solution.
Family History. Cont… Family history of communicable diseases. Heredity factors Strong family history of certain problems. Health of family members "maternal, parents, siblings, aunts, uncles, spouse and children". Cause of death of the family members
6 -Environmental History: purpose "to gather information about surroundings of the client", including physical, psychological, social environment, and presence of hazards, pollutants and safety measures. "
7 - Current Health Information Allergies: environmental, ingestion, drug, other. Habits "alcohol, tobacco, drug, caffeine" Medications taken regularly "by doctor or self prescription Exercise patterns. Sleep patterns. The pattern of sedentary and active activities in the client's Usual routine is explored. A weekly pattern of activity is recorded. The client's sleep pattern is explored and usual daily routine is recorded.
8 - Psychosocial History: Which includes : How client and his family cope with disease or stress, and how they responses to illness and health. The nurse or midwife can assess if there is psychological or social problem and if it affects general health of the client.
9 - Review of Systems (ROS) This includes a collection of data about the past and the present of each of the client systems. This review of the client’s physical, sociologic, and psychological health status may identify hidden problems and provides an opportunity to indicate client strength
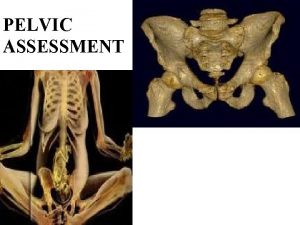
Physical Systems Which includes assessment of: - General review of skin, hair, head, face, eyes, ears, noise, sinuses, mouth, throat, neck nodes and breasts. Assessment of respiratory and cardiovascular system. Assessment of gastrointestinal system. Assessment of urinary system. Assessment of genital system. Assessment of extremities and musculoskeletal system. Assessment of endocrine system. Assessment of heamatoboitic system. Assessment of social system. Assessment of psychological system.
11 - Assessment of Interpersonal Factors. This includes : - Ethnic and cultural background Life style e. g. rest and sleep pattern Self concept perception of strength Sexuality developmental level and concerns Stress response copping pattern, support system.
Subjective Data: Describe your illness or current health problem. How has this affected your normal daily activities? How do you feel your current daily activities have affected your Health What do you feel caused your illness? How do you feel your illness should be treated?
Pain Assessment Describe any pain you have now. What brings it on? What relieves it? When does it occur? How often? How long does it last? What else do you feel when you have this pain? Rate your pain on a scale of 1 to 10, with 10 being the most severe Pain. How has your pain affected your activities of daily living?
Exam of the Skin n n Examine the patient in good lighting Inspect and palpate skin for the following: • Color • Texture • Turgor • Moisture
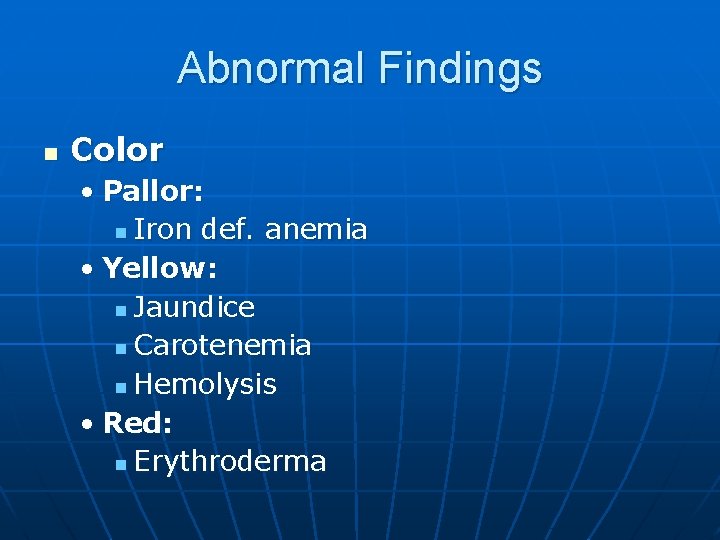
Abnormal Findings n Color • Pallor: n Iron def. anemia • Yellow: n Jaundice n Carotenemia n Hemolysis • Red: n Erythroderma

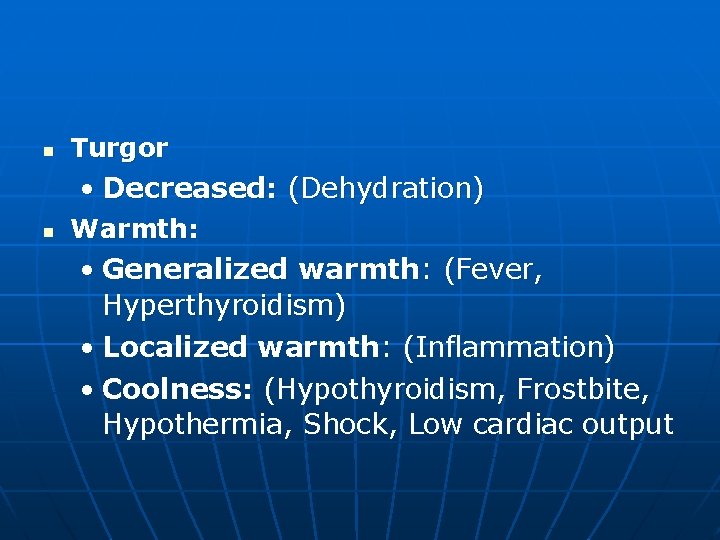
n Texture • Soft: (Thyrotoxicosis) • Tight: (Scleroderma) • Rough: (Hypothyroidism) n Moisture • Dry: (Vitamin A def, Myxedema) • Oily: (Acne)
n Turgor • Decreased: (Dehydration) n Warmth: • Generalized warmth: (Fever, Hyperthyroidism) • Localized warmth: (Inflammation) • Coolness: (Hypothyroidism, Frostbite, Hypothermia, Shock, Low cardiac output

 Biographical data in health history
Biographical data in health history Portfolio assessment matches assessment to teaching
Portfolio assessment matches assessment to teaching Define dynamic assessment
Define dynamic assessment Portfolio assessment matches assessment to teaching
Portfolio assessment matches assessment to teaching Chapter 32 assessment world history
Chapter 32 assessment world history Floral design tools assessment
Floral design tools assessment Chapter 17 section 2 world history
Chapter 17 section 2 world history Brief history of assessment
Brief history of assessment Chapter 19 assessment world history
Chapter 19 assessment world history Chapter 9 assessment world history
Chapter 9 assessment world history Chapter 15 assessment world history
Chapter 15 assessment world history Chapter 12 assessment world history
Chapter 12 assessment world history Assessment skills
Assessment skills Subjective health assessment
Subjective health assessment Kapan pelaksanaan rapid health assessment dilakukan
Kapan pelaksanaan rapid health assessment dilakukan Occupational health and safety assessment series
Occupational health and safety assessment series Agility health
Agility health Ohio state health assessment
Ohio state health assessment Health and safety risk assessment template
Health and safety risk assessment template Chapter 5 glencoe health answers
Chapter 5 glencoe health answers Population health risk assessment and management
Population health risk assessment and management Component of health assessment
Component of health assessment Pamela schwartz kaiser
Pamela schwartz kaiser Htai bobigny
Htai bobigny Health technology assessment in india
Health technology assessment in india Whats a focus group
Whats a focus group Integrative health and wellness assessment ihwa
Integrative health and wellness assessment ihwa Health needs assessment
Health needs assessment Gereedschapskoffer action
Gereedschapskoffer action Terminal assessment
Terminal assessment Also history physical
Also history physical