ANTEPARTUM HAEMORRHAGE 11282020 APH 1 Antepartum Haemorrhage l




- Slides: 27
ANTEPARTUM HAEMORRHAGE 11/28/2020 APH 1
Antepartum Haemorrhage l vaginal blood loss >15 m. L after 20 weeks’ gestation l 5% of all pregnancies l Accounts for 20 -25% of perinatal mortality 11/28/2020 APH 2

Causes l Placenta praevia 20% l Placental abruption 30% l Others/ unknown 45% l Vasa praevia l Marginal sinus bleeding l Rupture uterus l Local 11/28/2020 causes 5% APH 3
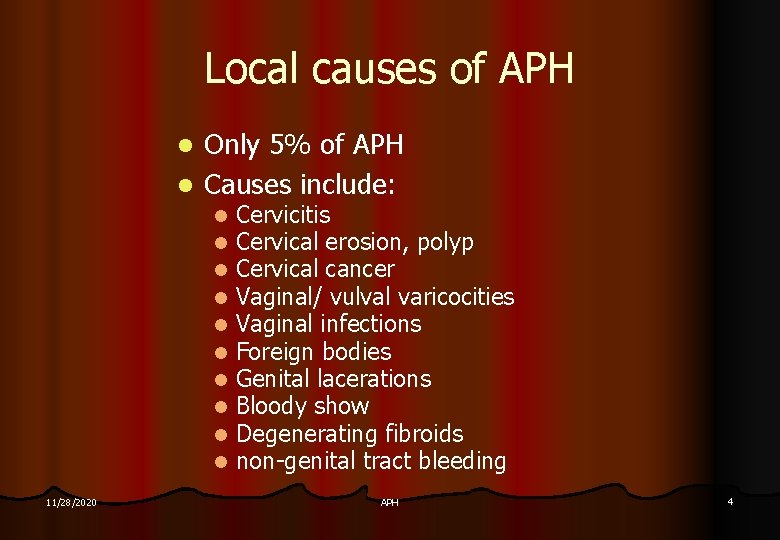
Local causes of APH Only 5% of APH l Causes include: l l l 11/28/2020 Cervicitis Cervical erosion, polyp Cervical cancer Vaginal/ vulval varicocities Vaginal infections Foreign bodies Genital lacerations Bloody show Degenerating fibroids non-genital tract bleeding APH 4
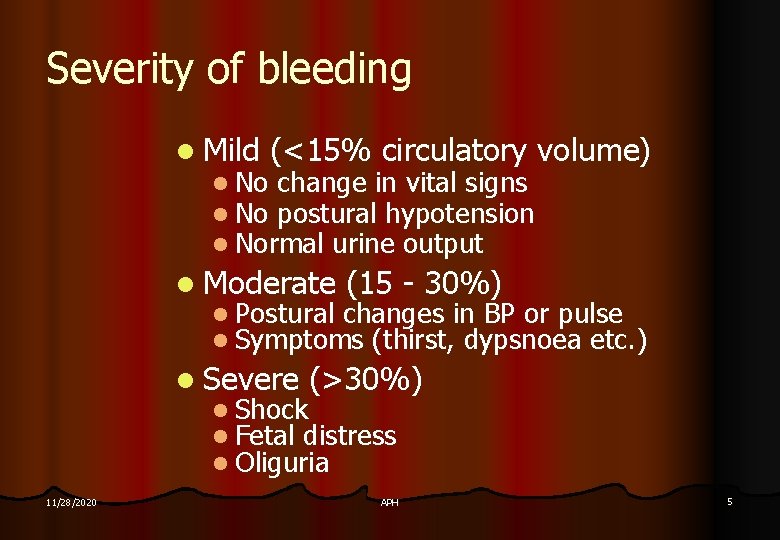
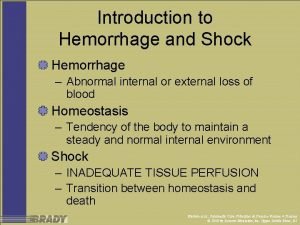
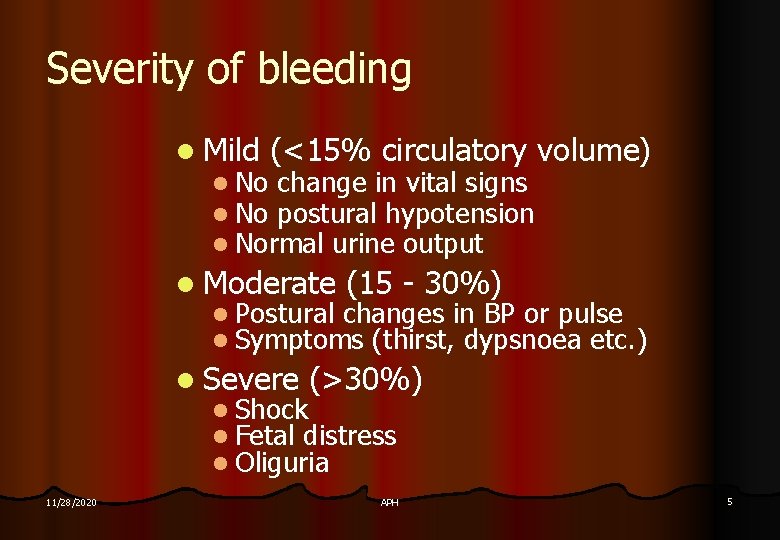
Severity of bleeding l Mild (<15% circulatory volume) l No change in vital signs l No postural hypotension l Normal urine output l Moderate (15 - 30%) l Postural changes in BP or pulse l Symptoms (thirst, dypsnoea etc. ) l Severe (>30%) l Shock l Fetal distress l Oliguria 11/28/2020 APH 5
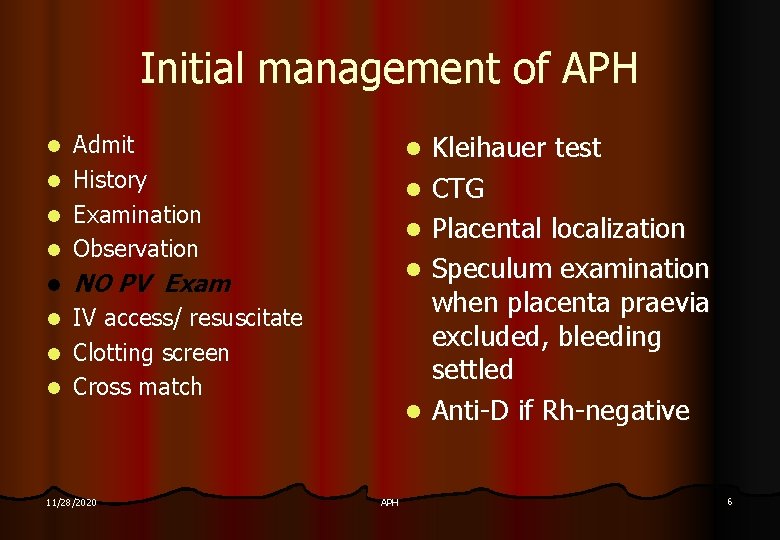
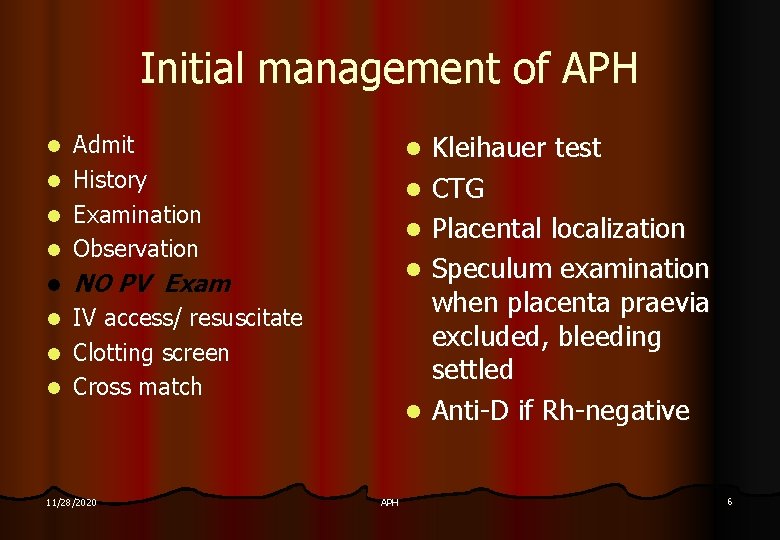
Initial management of APH Admit l History l Examination l Observation l l l NO PV Exam IV access/ resuscitate l Clotting screen l Cross match l 11/28/2020 l APH Kleihauer test CTG Placental localization Speculum examination when placenta praevia excluded, bleeding settled Anti-D if Rh-negative 6
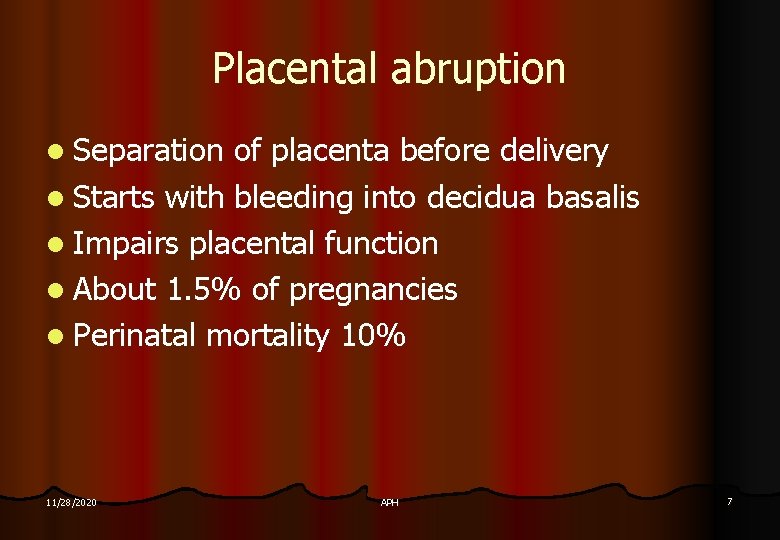
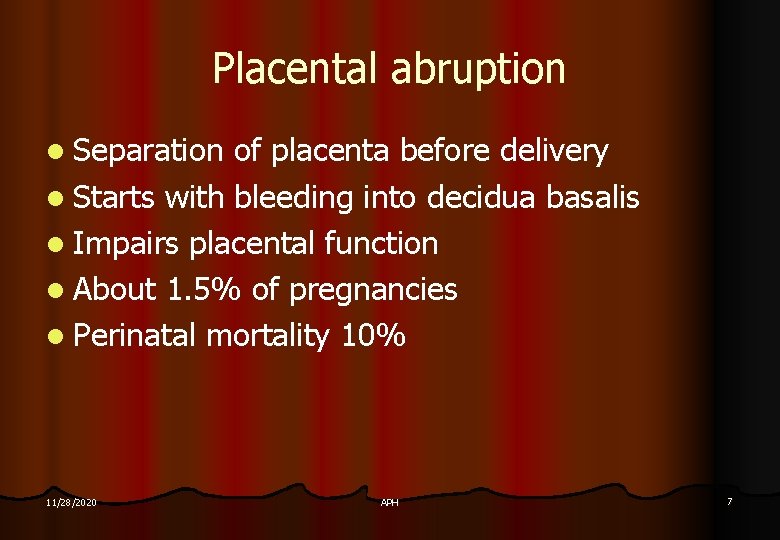
Placental abruption l Separation of placenta before delivery l Starts with bleeding into decidua basalis l Impairs placental function l About 1. 5% of pregnancies l Perinatal mortality 10% 11/28/2020 APH 7
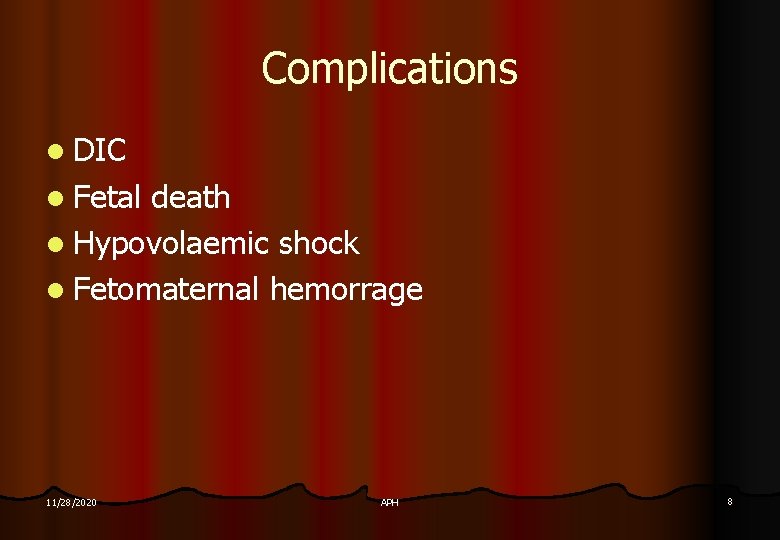
Complications l DIC l Fetal death l Hypovolaemic shock l Fetomaternal hemorrage 11/28/2020 APH 8
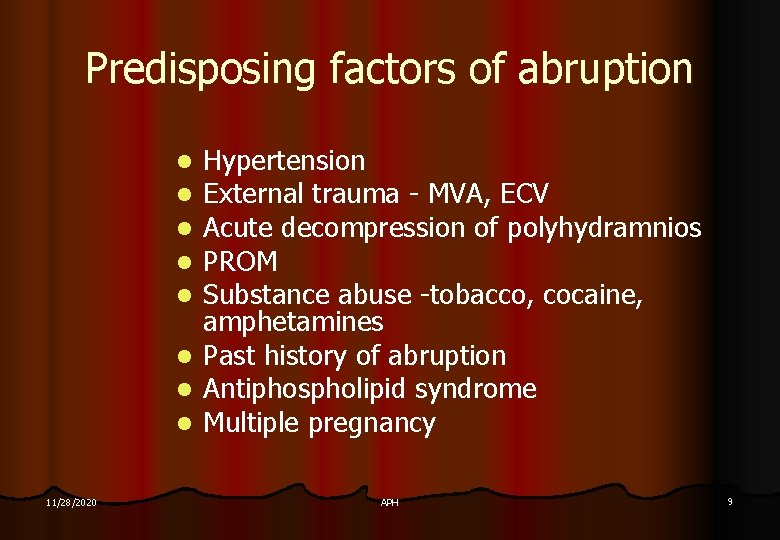
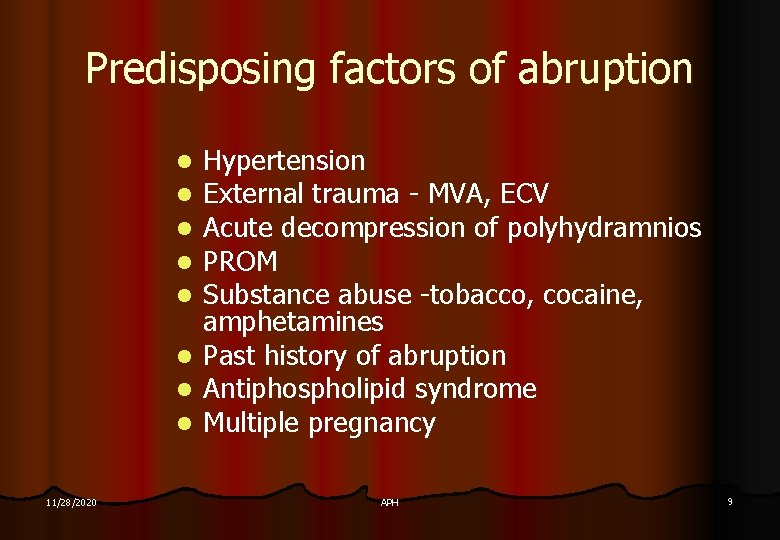
Predisposing factors of abruption l l l l 11/28/2020 Hypertension External trauma - MVA, ECV Acute decompression of polyhydramnios PROM Substance abuse -tobacco, cocaine, amphetamines Past history of abruption Antiphospholipid syndrome Multiple pregnancy APH 9
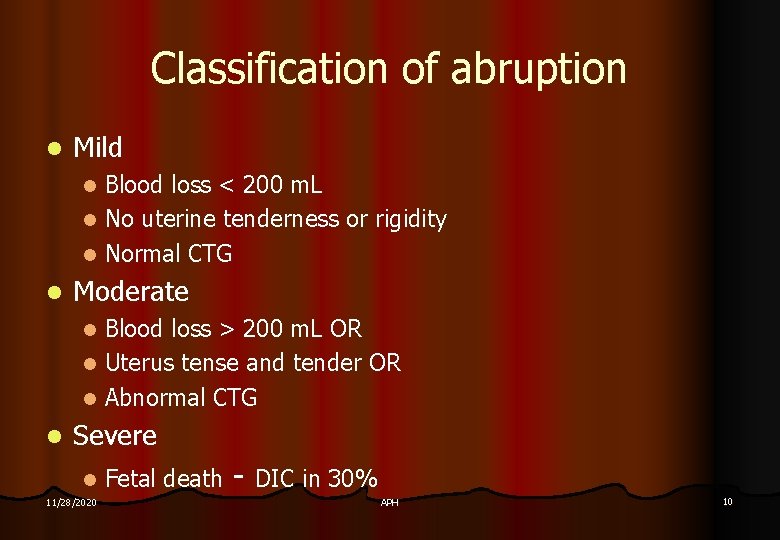
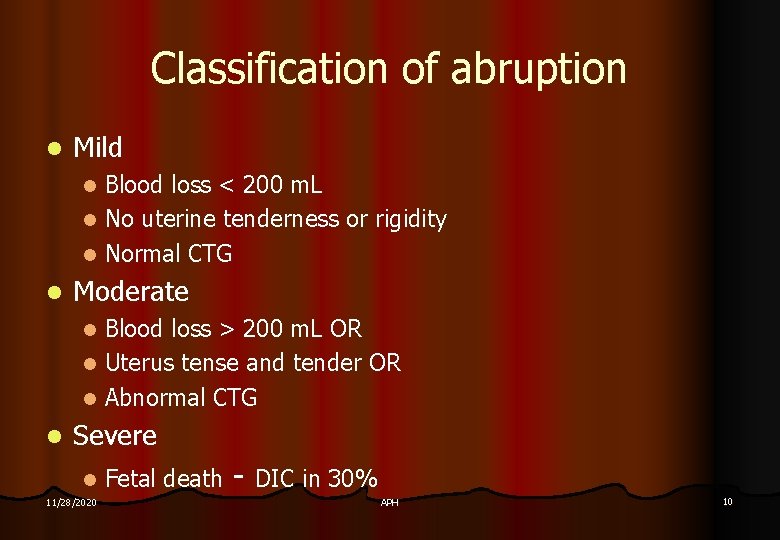
Classification of abruption l Mild Blood loss < 200 m. L l No uterine tenderness or rigidity l Normal CTG l l Moderate Blood loss > 200 m. L OR l Uterus tense and tender OR l Abnormal CTG l l Severe l 11/28/2020 Fetal death - DIC in 30% APH 10
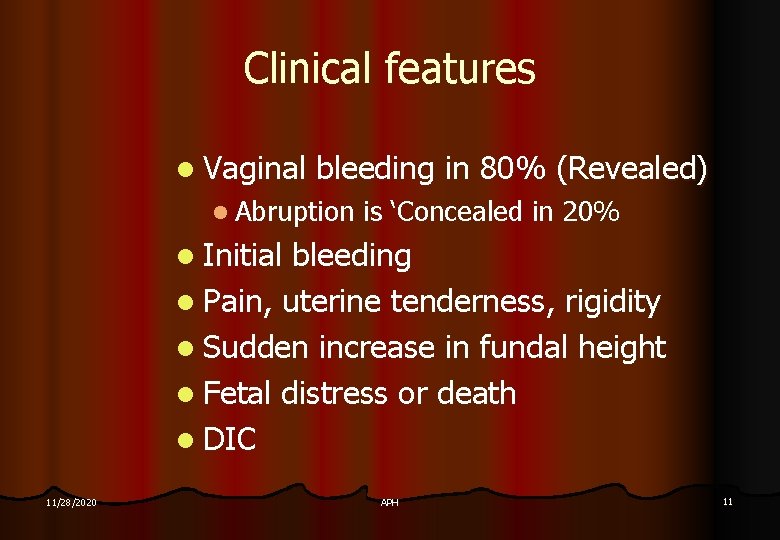
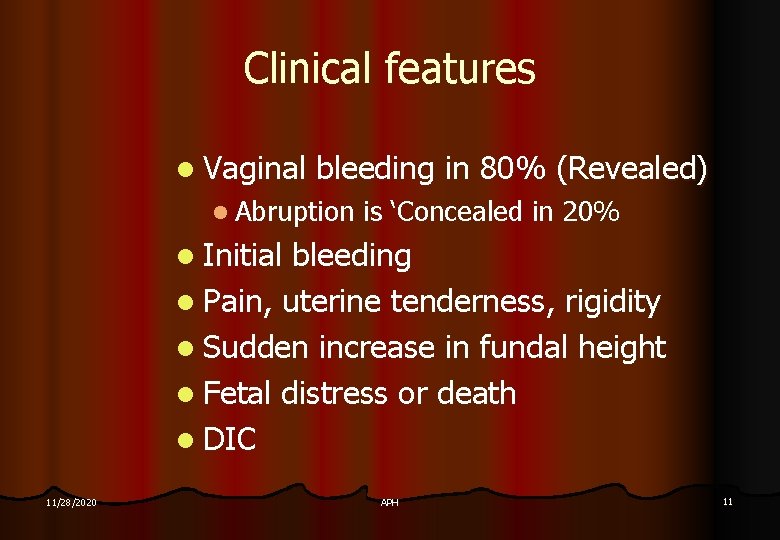
Clinical features l Vaginal bleeding in 80% (Revealed) l Abruption is ‘Concealed in 20% l Initial bleeding l Pain, uterine tenderness, rigidity l Sudden increase in fundal height l Fetal distress or death l DIC 11/28/2020 APH 11

Diagnosis l Clinical diagnosis, confirmed retrospectively by examination of placenta l Clinical features important in concealed abruption l Ultrasound unreliable l Only 11/28/2020 shows 25% of abruptions APH 12
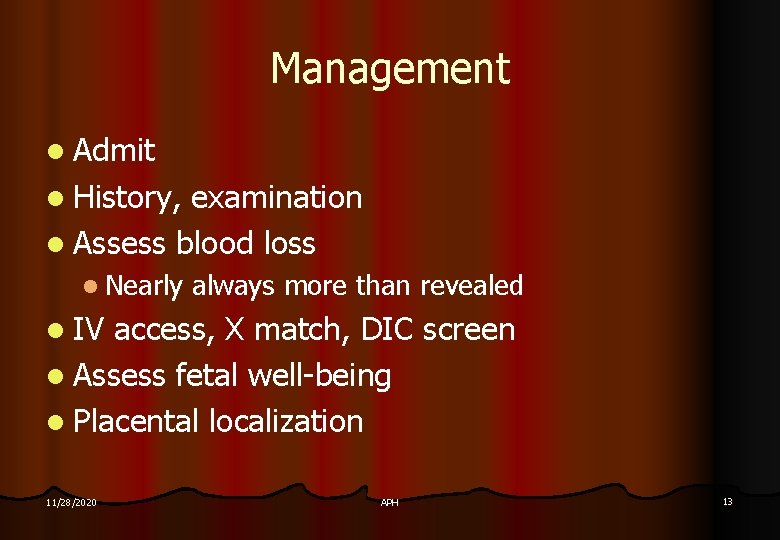
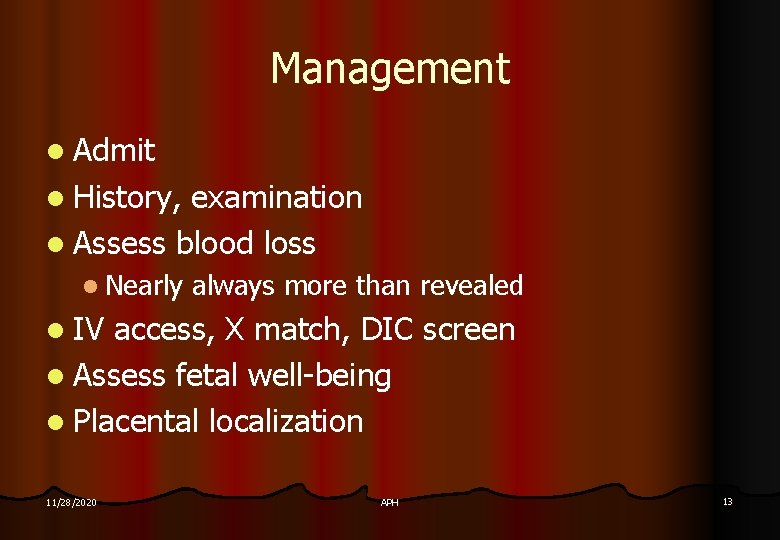
Management l Admit l History, examination l Assess blood loss l Nearly always more than revealed l IV access, X match, DIC screen l Assess fetal well-being l Placental localization 11/28/2020 APH 13
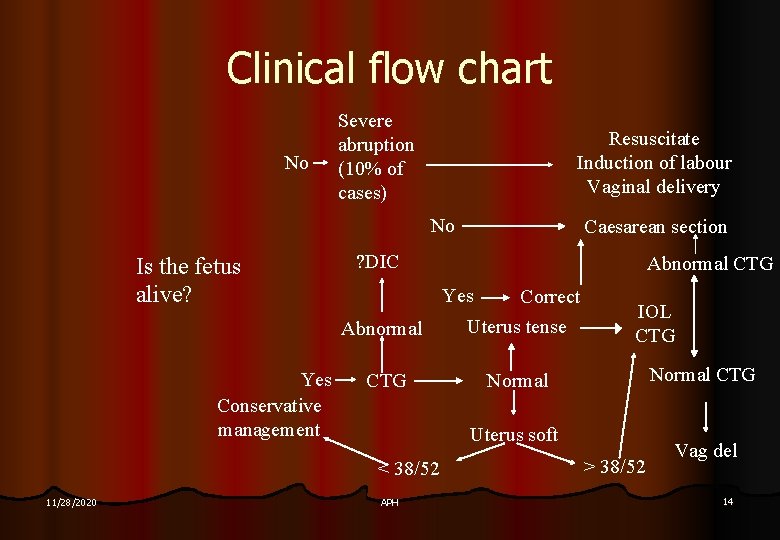
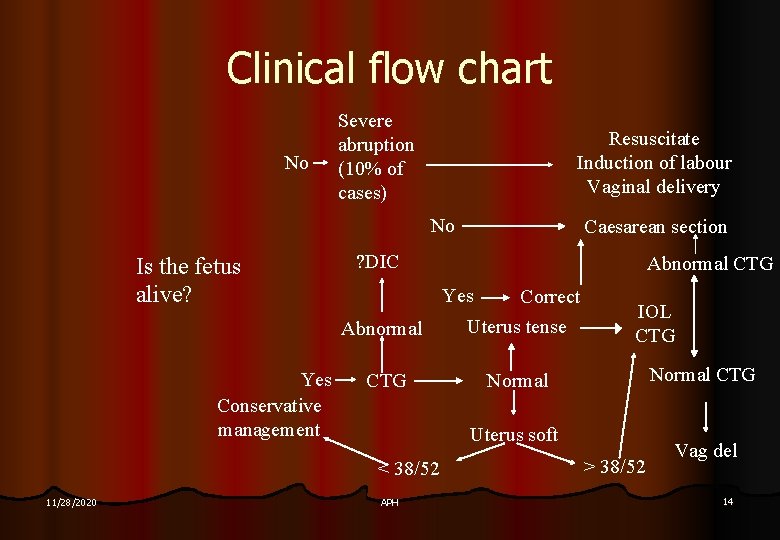
Clinical flow chart No Severe abruption (10% of cases) Resuscitate Induction of labour Vaginal delivery No Is the fetus alive? Yes Conservative management ? DIC Abnormal CTG Yes Correct Abnormal Uterus tense CTG Normal IOL CTG Normal CTG Uterus soft < 38/52 11/28/2020 Caesarean section APH > 38/52 Vag del 14
Placenta praevia l Placenta implanted on lower uterine segment l 1% of all pregnancies l Perinatal mortality rate ~ 3% l Major l At 11/28/2020 problem is preterm delivery 18 weeks, ~5% of placentas are ‘low lying’ APH 15
Classification 4 grades or degrees of placenta praevia: 1. Low-lying: edge not near internal os, but could be palpated by finger through cervix. 2. Marginal: edge of placenta reaches but does not cover os. 3. Partial: placenta partially covers internal os. 4. Total: placenta completely covers internal os. 11/28/2020 APH 16
Aetiology/ associations l Uterine surgery or instrumentation l Previous CS, D&C, myomectomy l 1 previous CS + anterior placenta praevia = 25% risk placenta accreta l. P H placenta praevia l Increasing parity and age l Multiple pregnancy 11/28/2020 APH 17

Clinical presentation l Painless Recurrent Vaginal bleeding l 1/3 < 30 weeks l 1/3 30 -35 weeks l 1/3 > 36 weeks l Usually first episode mild l Earlier is worse l Often gets worse l Abnormal presentation or lie 11/28/2020 APH 18
Diagnosis l Placental localization is by ultrasound examination l Transvaginal ultrasound better l Not always right l PPV 93%, NPV 96% l At 18 weeks, 5 -10% of placentas low lying. l Repeat 11/28/2020 scan at 32 - 34 weeks APH 19

Management l Admit l to hospital NO VAGINAL EXAMINATION l IV access l Placental localization l Conservative treatment until fetal maturity if possible 11/28/2020 APH 20
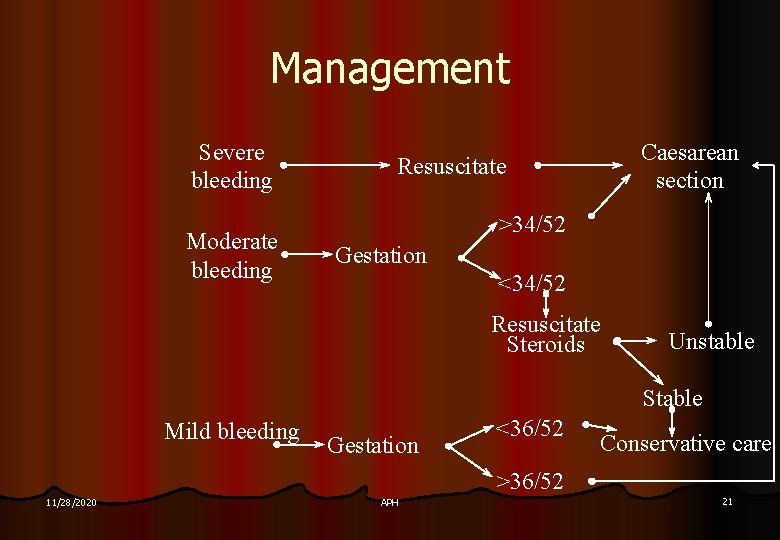
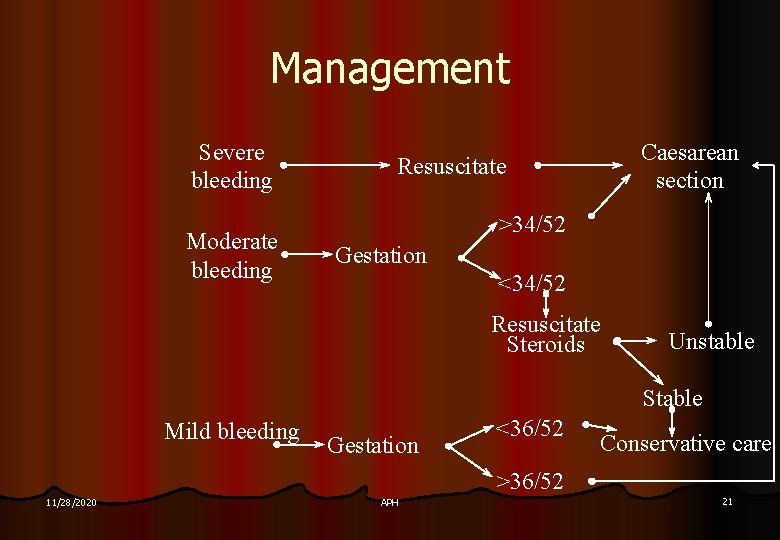
Management Severe bleeding Moderate bleeding Caesarean section Resuscitate >34/52 Gestation <34/52 Resuscitate Steroids Unstable Stable Mild bleeding Gestation <36/52 Conservative care >36/52 11/28/2020 APH 21
Delivery l Delivery is by Caesarean section l Usually LSCS, go around placenta l Beware morbidly adherent placenta l Occasionally Caesarean hysterectomy necessary 11/28/2020 APH 22
Outpatient management l Inpatient observation for 72 hours without bleeding l Stable haematocrit > 35% l Reactive CTG l Can call ambulance 24 hours/day l Rest at home, no intercourse l Patient understands complications l Weekly follow-up until delivery 11/28/2020 APH 23
Asymptomatic patients l Placenta 11/28/2020 praevia now diagnosed prior to bleeding l If no bleeding, no need to admit before 34 weeks l Admit if bleeds l Delivery still by CS at 37 -38 weeks l Uncertainty about admission between 34 and 37 weeks - admit grades 3 and 4 APH 24
Vasa Praevia l l l Vellamentous insertion of cord, bipartite or succenturriate placenta Fetal vessels in membranes over cervix May rupture at or before ROM Suspect in small APH with abnormal CTG Confirm with Apt test 11/28/2020 APH 25
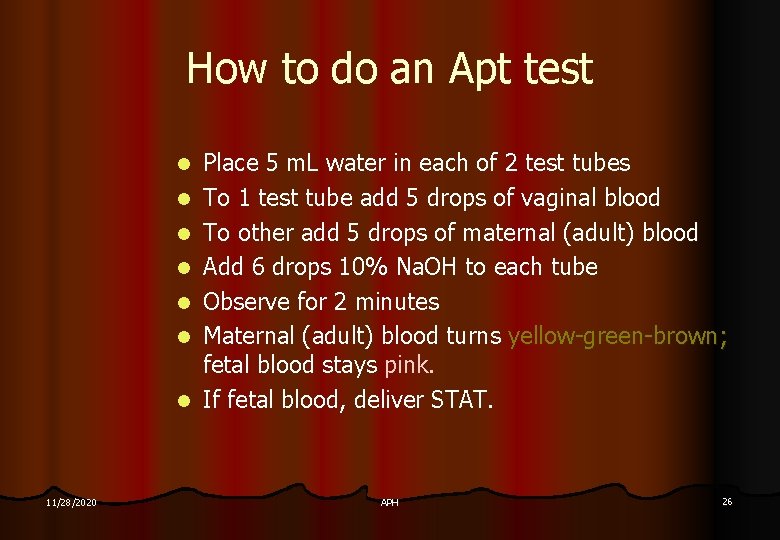
How to do an Apt test l l l l 11/28/2020 Place 5 m. L water in each of 2 test tubes To 1 test tube add 5 drops of vaginal blood To other add 5 drops of maternal (adult) blood Add 6 drops 10% Na. OH to each tube Observe for 2 minutes Maternal (adult) blood turns yellow-green-brown; fetal blood stays pink. If fetal blood, deliver STAT. APH 26
APH of uncertain origin l l l 2. 5% of all deliveries PNM 2% (3 x background rate) Initial management as for all APH Monitor fetal well-being Marginal sinus bleeding Retrospective diagnosis l Increased incidences of PROM, preterm labour l 11/28/2020 APH 27