Acute Renal Failure Aniruddha Palya MD MPH Learning










- Slides: 53
Acute Renal Failure Aniruddha Palya MD, MPH
Learning Objectives • • • Define renal failure Understand the impact of acute renal failure Describe the categories of acute renal failure (ARF) Recognize the clinical manifestations of ARF. Discuss the assessment and diagnostic findings associated with ARF. • Describe the medical management of a patient with ARF. • Discuss the nursing interventions designed to meet specific goals associated with ARF. 2
Acute Kidney Injury Glomerular filtration rate (GFR) = rate of transfer of protein free plasma filtrate (ultrafiltration) across the walls of the glomerular capillaries. In its most severe form AKI is referred to as acute renal failure.
Incidence of ARF (any ARF) • • • 1 -2% of all hospital admissions 20 -30% of Post-operative cases 10 -25% of ICU admissions 20 -30% of Acute sepsis Up to 40% in Hematologic malignancy The kidney fails when other organs fail. . . Lanore, Crit Care Med 1991; Nolan, J Am Soc Neph 1998; Shusterman, Am J Med 1987; others
Impact of ARF • ARF (any) increases hospital mortality x 5 Levy et al, JAMA 1996 • ARF needing RRT carries 45 -65% mortality somewhat better survival over last 5 -10 yr Nolan et al, J Am Soc Neph 1998 • ARF in “critically ill” - 27% 6 mo survival Adj-life-yr cost: $274 K/yr in worst cases $ 62 K/yr in best cases • AKI has a higher rate of death globally than prostate cancer, breast cancer, heart failure and diabetes combined Hamel et al, Ann Int Med 1996
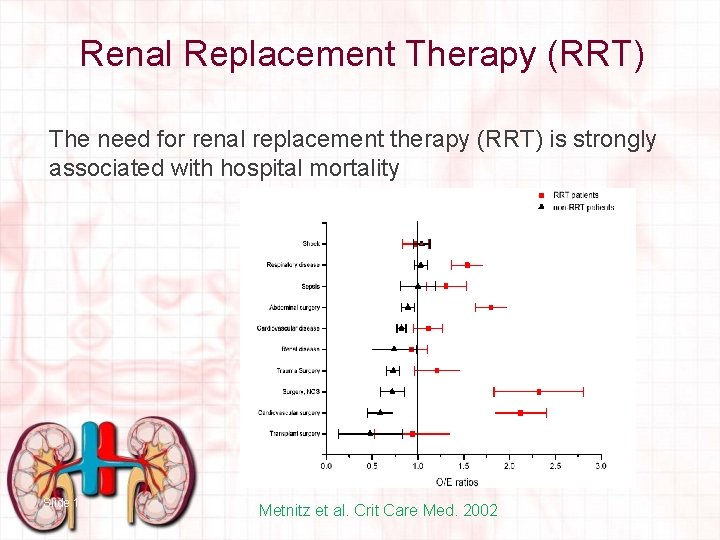
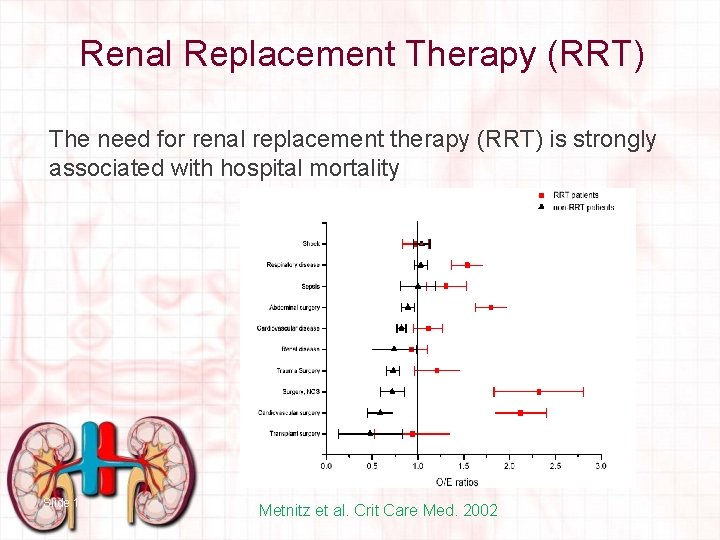
Presence of AKI is Strongly Associated with Hospital Mortality Slide 6
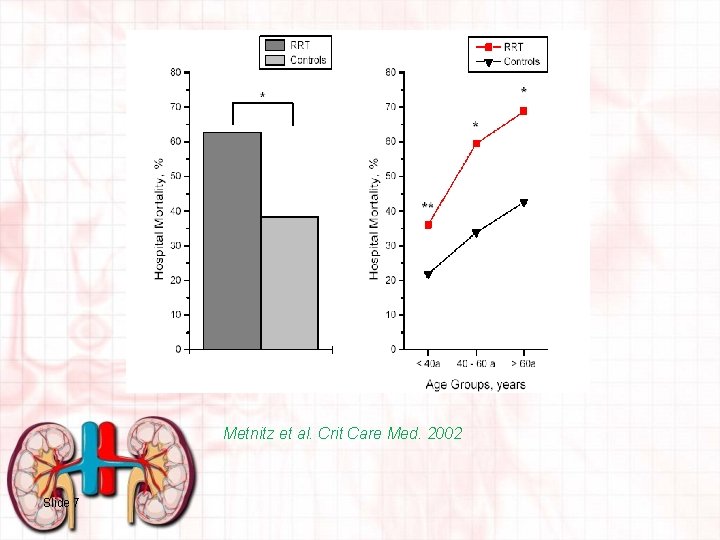
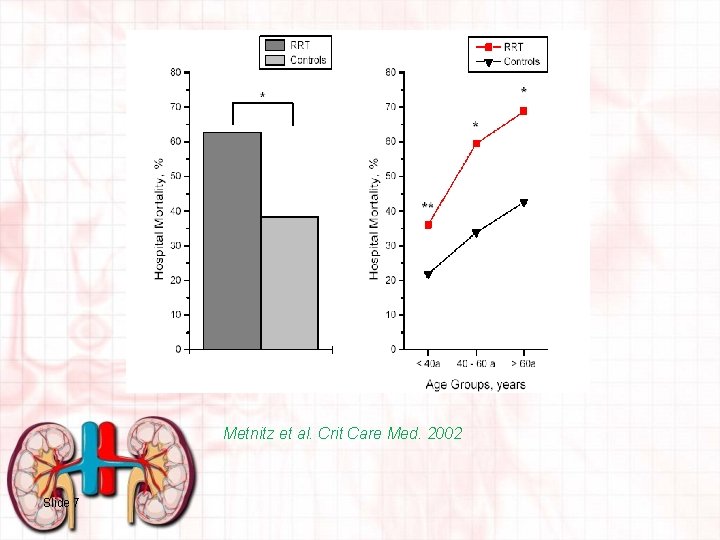
Metnitz et al. Crit Care Med. 2002 Slide 7
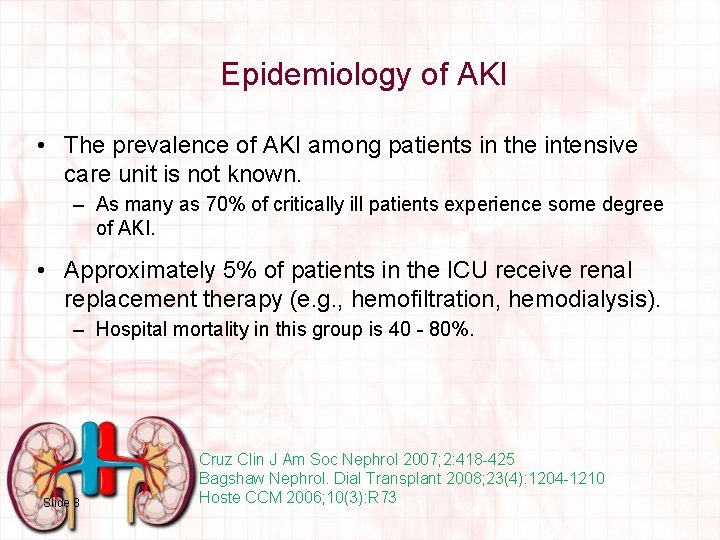
Epidemiology of AKI • The prevalence of AKI among patients in the intensive care unit is not known. – As many as 70% of critically ill patients experience some degree of AKI. • Approximately 5% of patients in the ICU receive renal replacement therapy (e. g. , hemofiltration, hemodialysis). – Hospital mortality in this group is 40 - 80%. Slide 8 Cruz Clin J Am Soc Nephrol 2007; 2: 418 -425 Bagshaw Nephrol. Dial Transplant 2008; 23(4): 1204 -1210 Hoste CCM 2006; 10(3): R 73
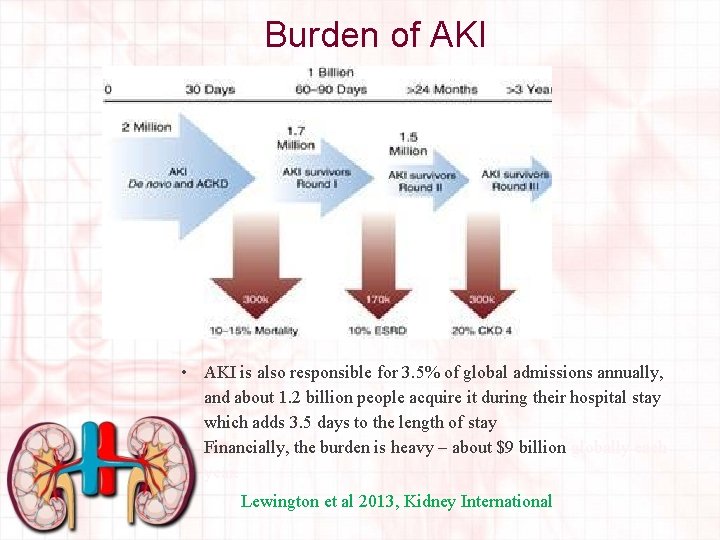
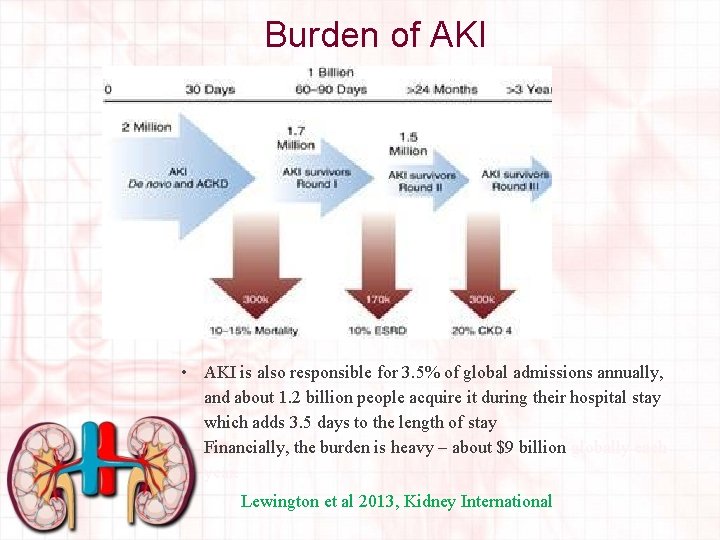
Burden of AKI • AKI is also responsible for 3. 5% of global admissions annually, and about 1. 2 billion people acquire it during their hospital stay which adds 3. 5 days to the length of stay • Financially, the burden is heavy – about $9 billion globally each year. Lewington et al 2013, Kidney International
Renal Replacement Therapy (RRT) The need for renal replacement therapy (RRT) is strongly associated with hospital mortality Slide 10 Metnitz et al. Crit Care Med. 2002
Defining Acute Kidney Injury • Acute Dialysis Quality Initiative (ADQI) called RIFLE Criteria (2002) • Acute Kidney Injury Network (AKIN, 2004)
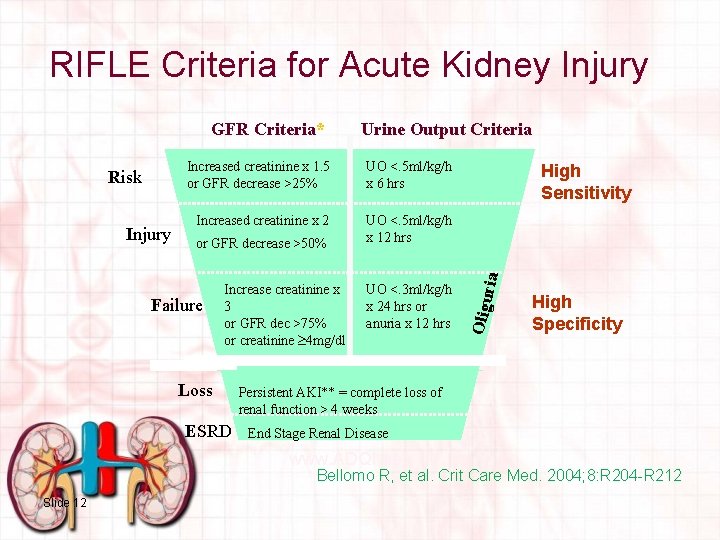
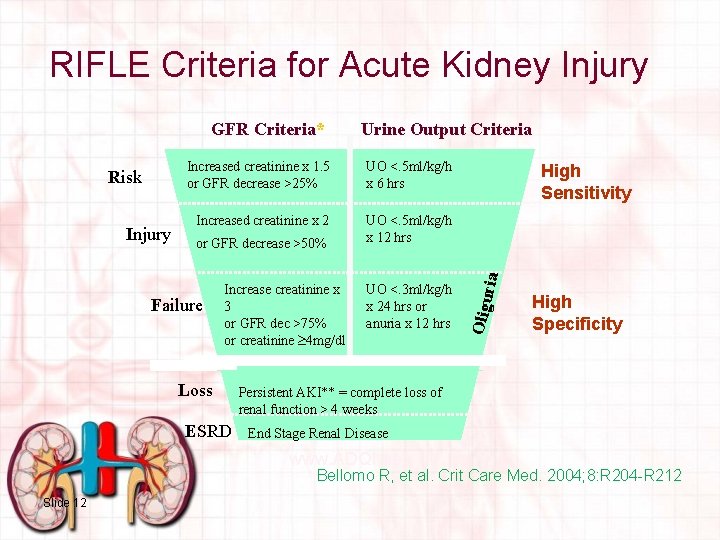
RIFLE Criteria for Acute Kidney Injury Increased creatinine x 1. 5 or GFR decrease >25% UO <. 5 ml/kg/h x 6 hrs Increased creatinine x 2 UO <. 5 ml/kg/h x 12 hrs or GFR decrease >50% Failure Increase creatinine x 3 or GFR dec >75% or creatinine 4 mg/dl UO <. 3 ml/kg/h x 24 hrs or anuria x 12 hrs High Sensitivity ria Risk Urine Output Criteria Oligu GFR Criteria* High Specificity (Acute rise of 0. 5 mg/dl) Loss ESRD Persistent AKI** = complete loss of renal function > 4 weeks End Stage Renal Disease www. ADQI. net Bellomo R, et al. Crit Care Med. 2004; 8: R 204 -R 212 Slide 12
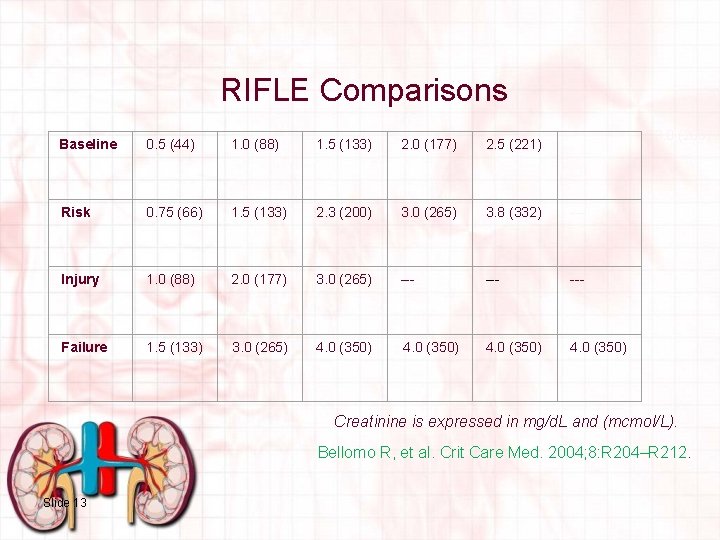
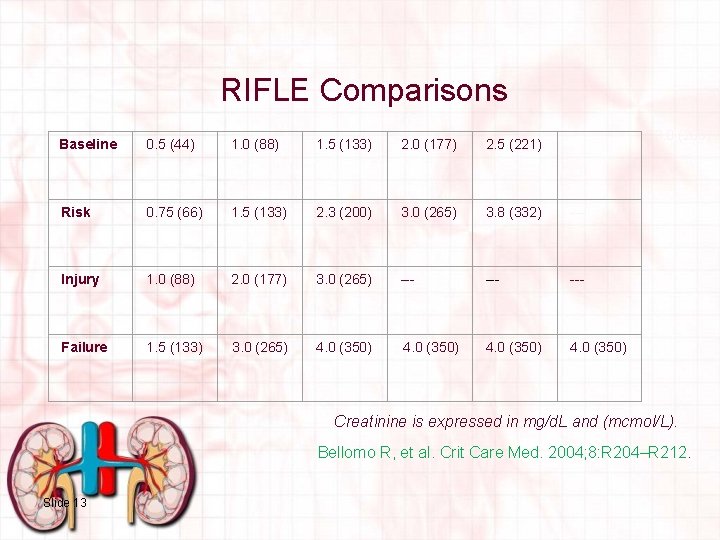
RIFLE Comparisons 3. 0 (265) Baseline 0. 5 (44) 1. 0 (88) 1. 5 (133) 2. 0 (177) 2. 5 (221) Risk 0. 75 (66) 1. 5 (133) 2. 3 (200) 3. 0 (265) 3. 8 (332) --- Injury 1. 0 (88) 2. 0 (177) 3. 0 (265) --- --- Failure 1. 5 (133) 3. 0 (265) 4. 0 (350) Creatinine is expressed in mg/d. L and (mcmol/L). Bellomo R, et al. Crit Care Med. 2004; 8: R 204–R 212. Slide 13
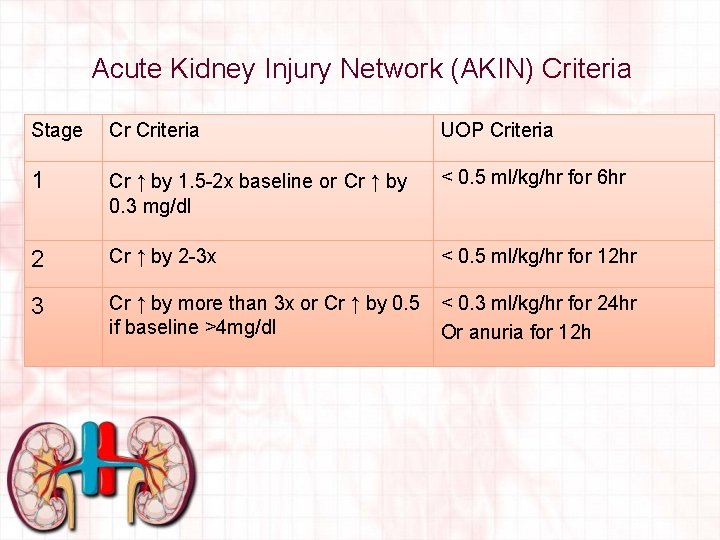
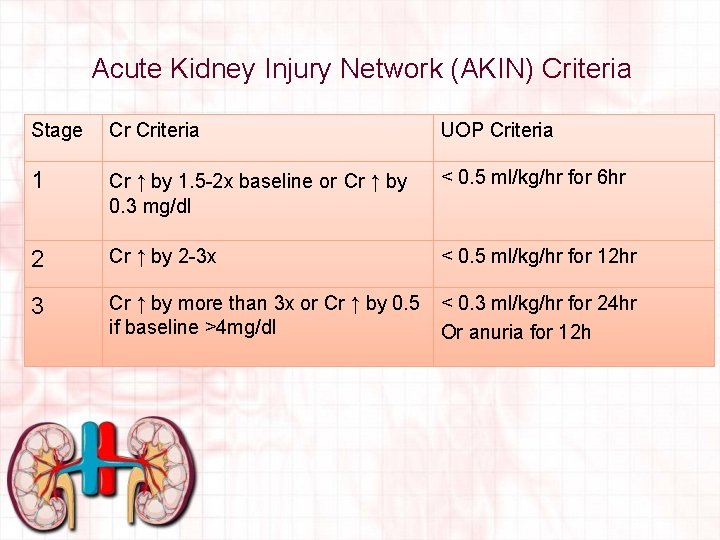
Acute Kidney Injury Network (AKIN) Criteria Stage Cr Criteria UOP Criteria 1 Cr ↑ by 1. 5 -2 x baseline or Cr ↑ by 0. 3 mg/dl < 0. 5 ml/kg/hr for 6 hr 2 Cr ↑ by 2 -3 x < 0. 5 ml/kg/hr for 12 hr 3 Cr ↑ by more than 3 x or Cr ↑ by 0. 5 if baseline >4 mg/dl < 0. 3 ml/kg/hr for 24 hr Or anuria for 12 h
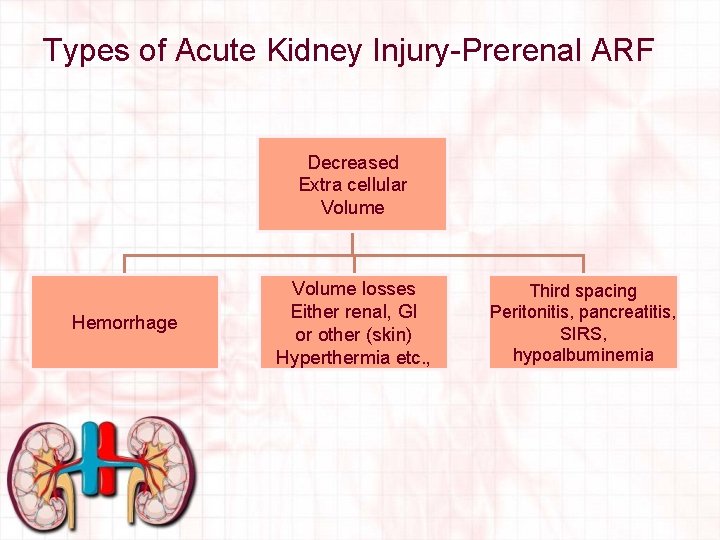
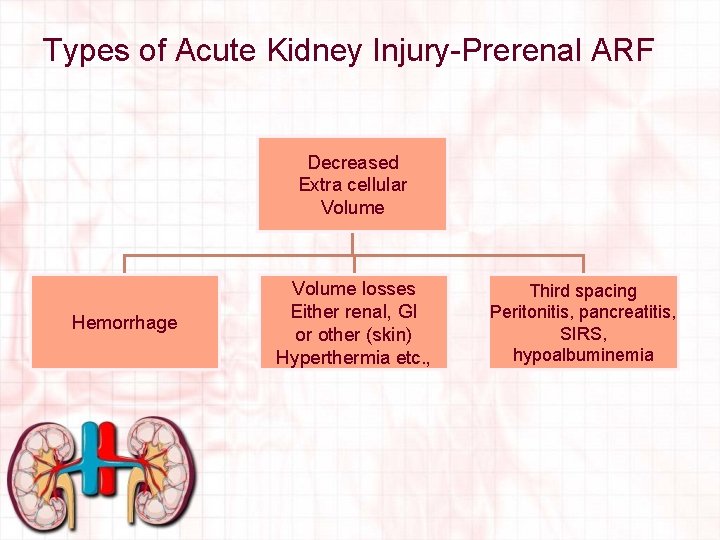
Types of Acute Kidney Injury-Prerenal ARF Decreased Extra cellular Volume Hemorrhage Volume losses Either renal, GI or other (skin) Hyperthermia etc. , Third spacing Peritonitis, pancreatitis, SIRS, hypoalbuminemia
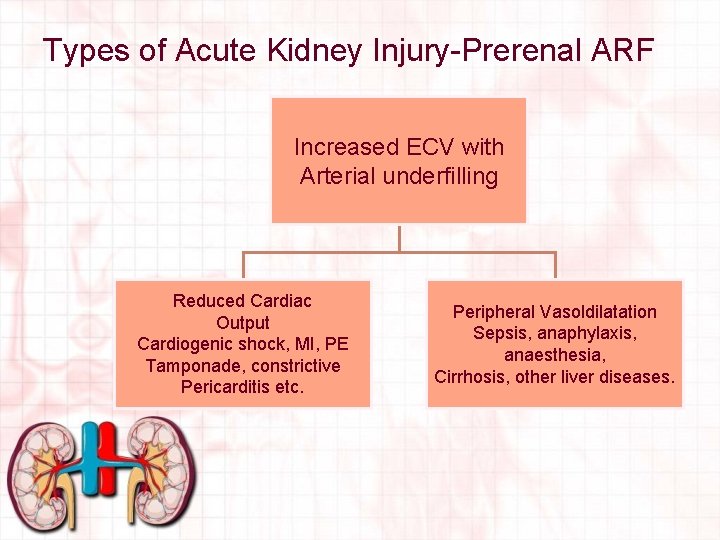
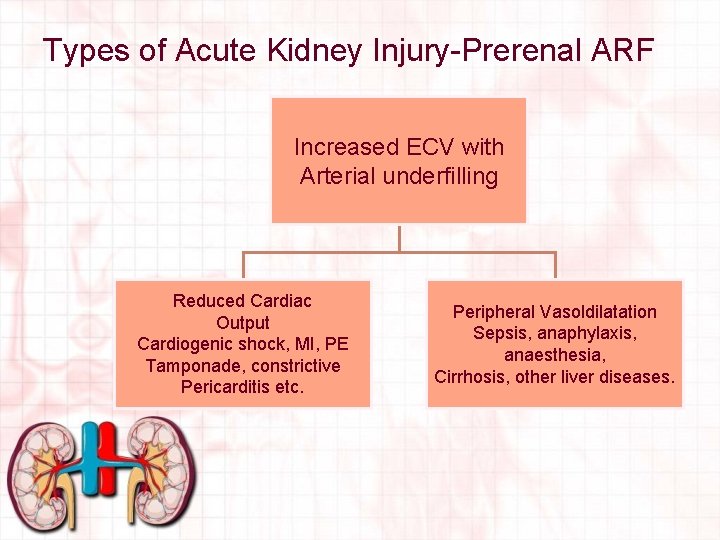
Types of Acute Kidney Injury-Prerenal ARF Increased ECV with Arterial underfilling Reduced Cardiac Output Cardiogenic shock, MI, PE Tamponade, constrictive Pericarditis etc. Peripheral Vasoldilatation Sepsis, anaphylaxis, anaesthesia, Cirrhosis, other liver diseases.
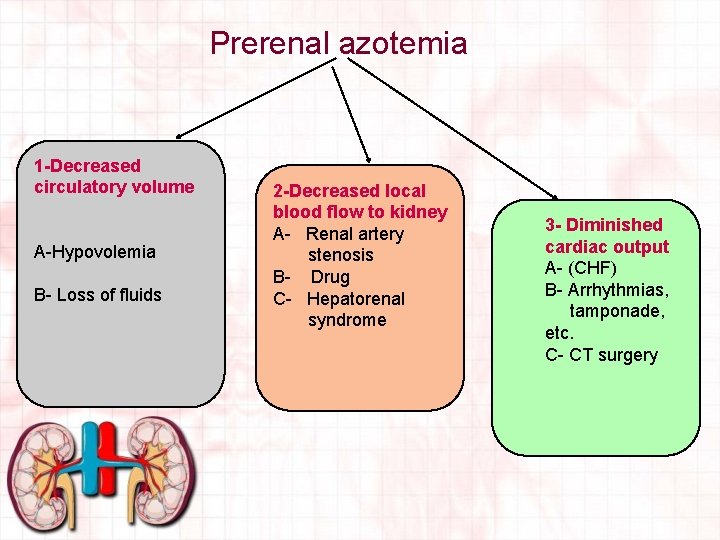
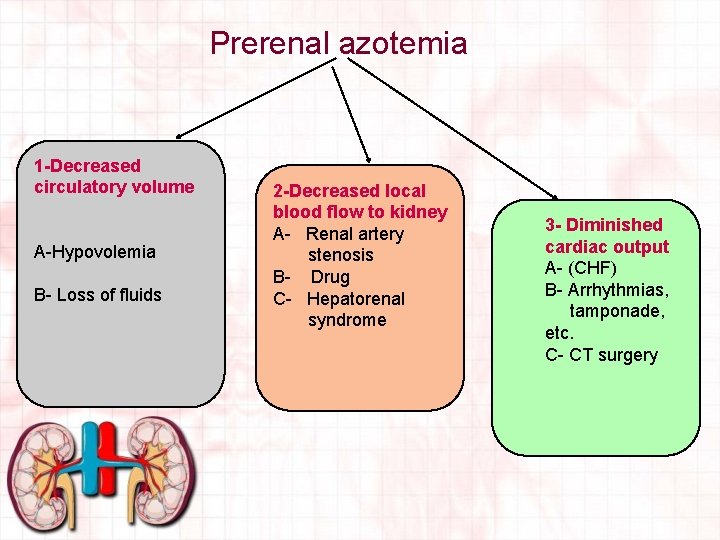
Prerenal azotemia 1 -Decreased circulatory volume A-Hypovolemia B- Loss of fluids 2 -Decreased local blood flow to kidney A- Renal artery stenosis B- Drug C- Hepatorenal syndrome 3 - Diminished cardiac output A- (CHF) B- Arrhythmias, tamponade, etc. C- CT surgery
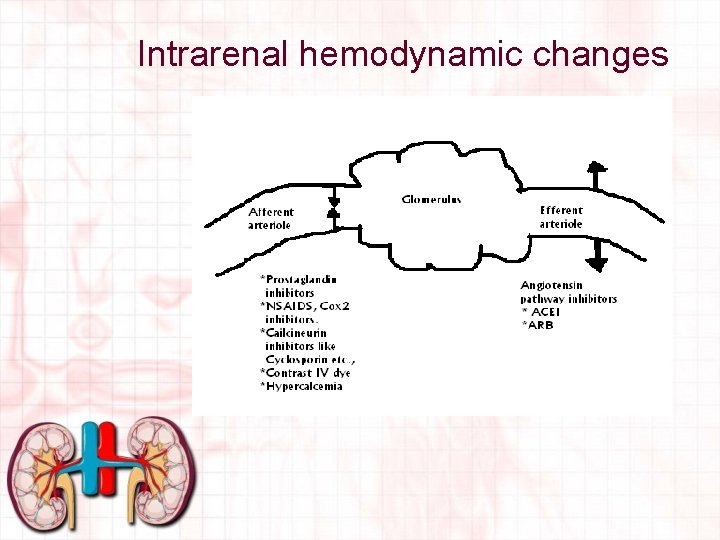
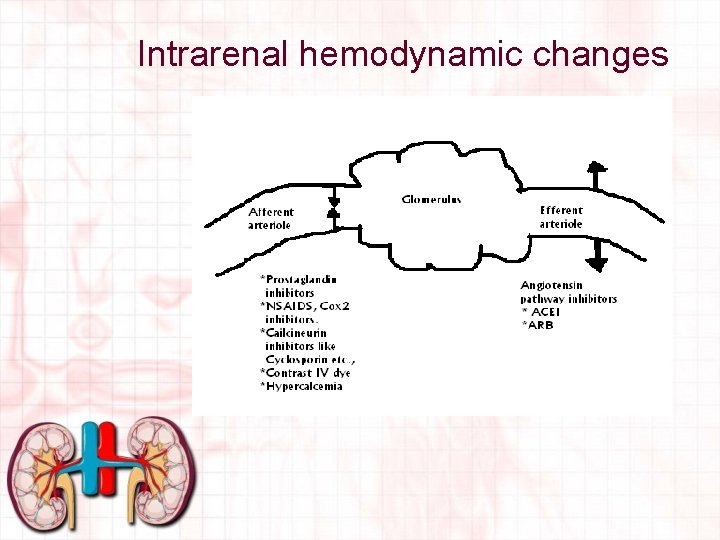
Intrarenal hemodynamic changes
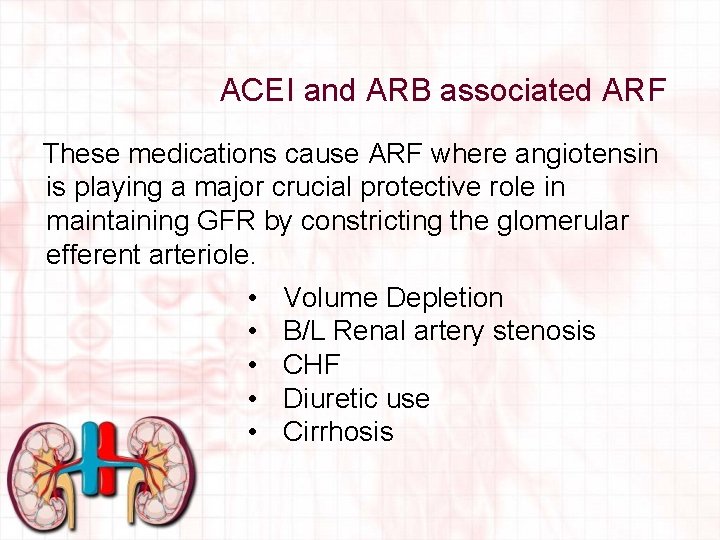
ACEI and ARB associated ARF These medications cause ARF where angiotensin is playing a major crucial protective role in maintaining GFR by constricting the glomerular efferent arteriole. • • • Volume Depletion B/L Renal artery stenosis CHF Diuretic use Cirrhosis
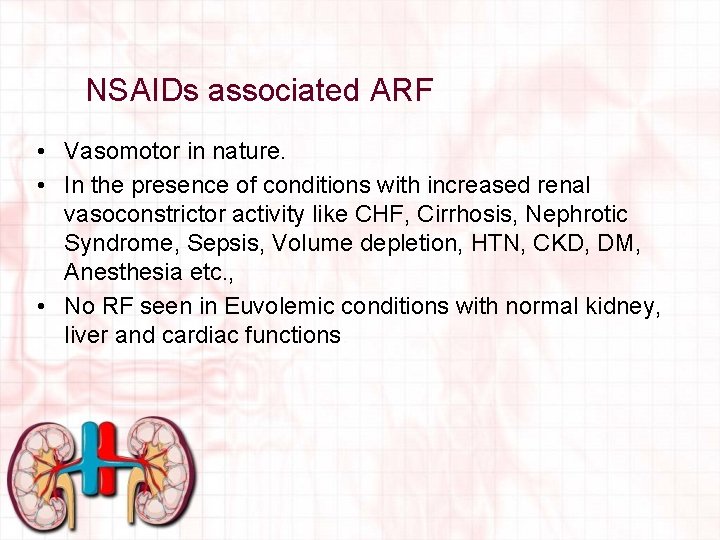
NSAIDs associated ARF • Vasomotor in nature. • In the presence of conditions with increased renal vasoconstrictor activity like CHF, Cirrhosis, Nephrotic Syndrome, Sepsis, Volume depletion, HTN, CKD, DM, Anesthesia etc. , • No RF seen in Euvolemic conditions with normal kidney, liver and cardiac functions.
Hepatorenal syndrome (HRS) is defined as the occurrence of renal failure in a patient with advanced liver disease in the absence of an identifiable cause of renal failure DIAGNOSIS OF EXCLUSION
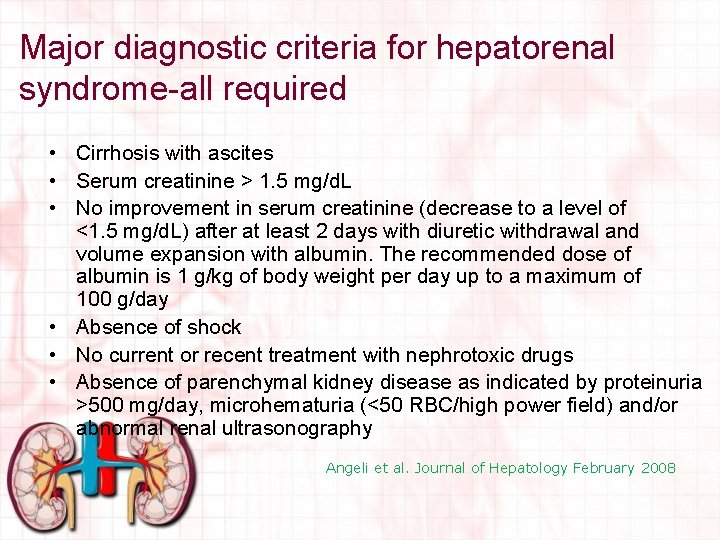
Major diagnostic criteria for hepatorenal syndrome-all required • Cirrhosis with ascites • Serum creatinine > 1. 5 mg/d. L • No improvement in serum creatinine (decrease to a level of <1. 5 mg/d. L) after at least 2 days with diuretic withdrawal and volume expansion with albumin. The recommended dose of albumin is 1 g/kg of body weight per day up to a maximum of 100 g/day • Absence of shock • No current or recent treatment with nephrotoxic drugs • Absence of parenchymal kidney disease as indicated by proteinuria >500 mg/day, microhematuria (<50 RBC/high power field) and/or abnormal renal ultrasonography Angeli et al. Journal of Hepatology February 2008
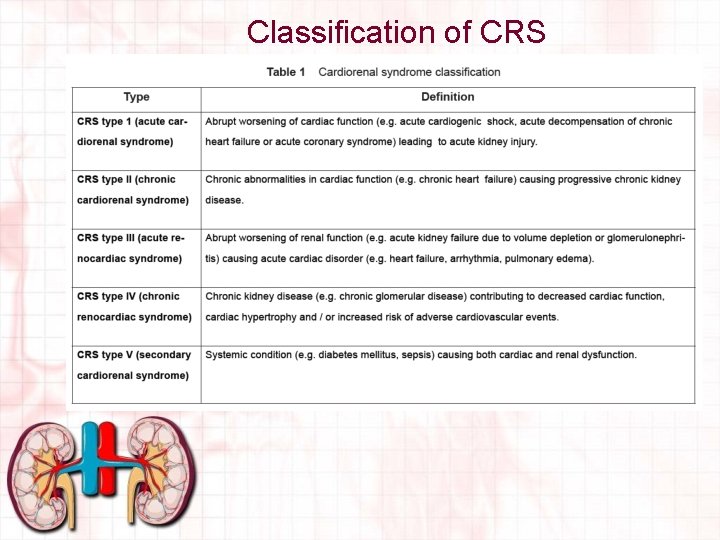
Cardiorenal syndrome “Disorders of the heart and kidneys whereby acute or chronic dysfunction in one organ may induce acute or chronic dysfunction of the other”
Acute Kidney Injury in CHF Ø Ø Acute kidney injury complicates 1/3 of total admissions for CHF (Forman et al, 2004, JACC) AKI is associated with a three fold increase in length of stay (Wencker, 2007) Higher likelihood for hospital readmission, and a 22% higher mortality rate (Fonarow et al, 2005 JAMA) Reduction in outcomes noted with small increases in serum creatinine as little as 0. 33 mg/dl, regardless of its presence at admission or its development during the course of heart failure treatment (Damman, 2007 and Gottlieb 2000)
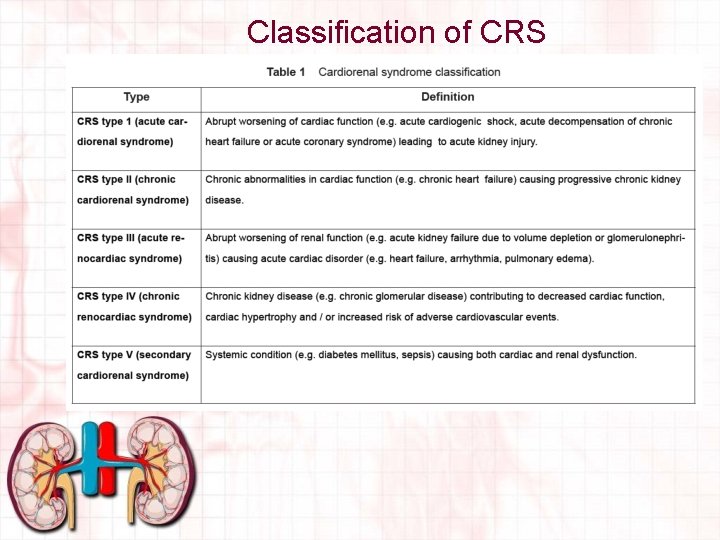
Classification of CRS
Intrarenal ARF • • Tubular Glomerular Interstitial Vascular
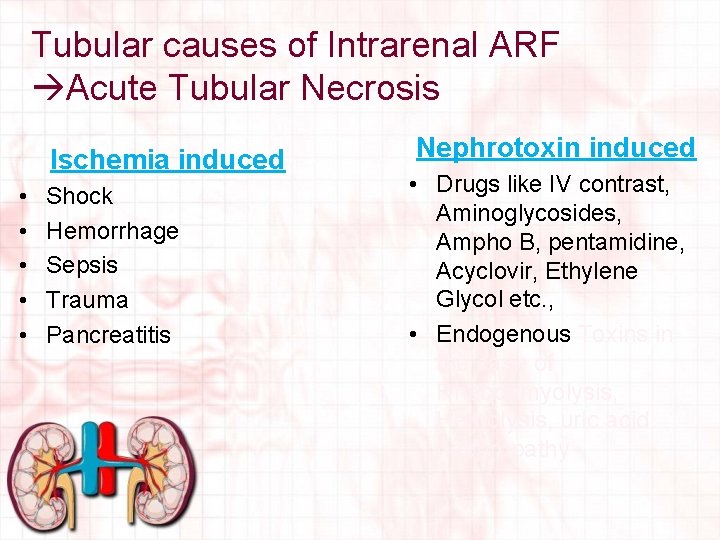
Tubular causes of Intrarenal ARF Acute Tubular Necrosis Ischemia induced • • • Shock Hemorrhage Sepsis Trauma Pancreatitis Nephrotoxin induced • Drugs like IV contrast, Aminoglycosides, Ampho B, pentamidine, Acyclovir, Ethylene Glycol etc. , • Endogenous Toxins in the case of Rhabdomyolysis, Hemolysis, uric acid nephropathy
Clinical course of Acute Tubular Necrosis (ATN) I- Initiating phase – Begins with an initial insult and lasts until cell injury occurs – Lasts from hours to days – Clinical manifestations in this phase include reduced urine output and worsening serum Creatinine II- Maintenance phase – Characterized by a stabilization of GFR at a very low level – Typically lasts 1 -2 weeks – Oliguria <400 ml/24 hrs or <20 ml/hr or Anuria <50 ml/24 hrs may be seen
Clinical course of tubular Necrosis (ATN) III- Recovery phase – characterized by regeneration of tubular epithelial cells – lasts from months – Renal functions return to its normality – abnormal diuresis sometimes occurs, causing salt and water loss and volume depletion
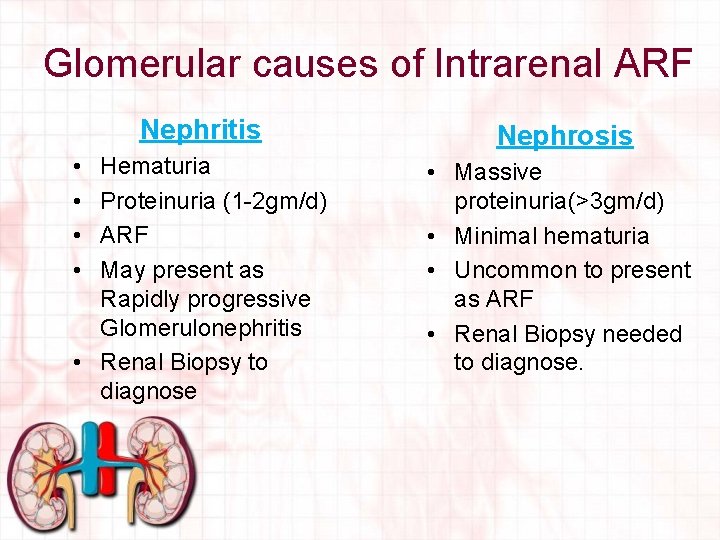
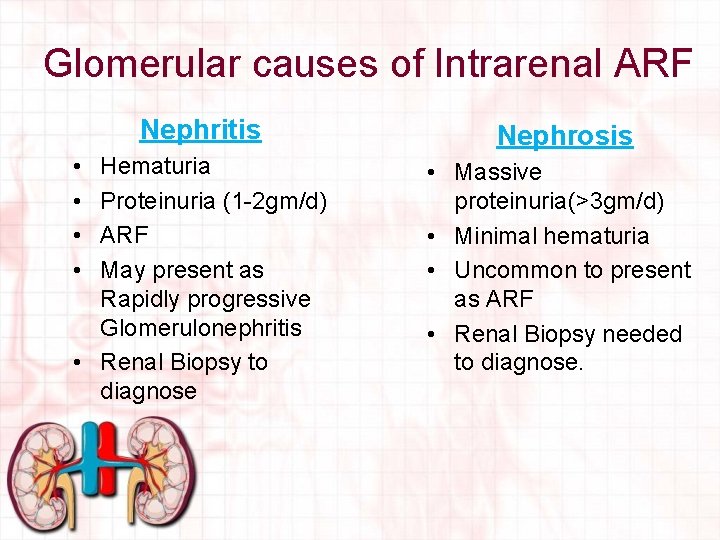
Glomerular causes of Intrarenal ARF Nephritis Nephrosis Hematuria Proteinuria (1 -2 gm/d) ARF May present as Rapidly progressive Glomerulonephritis • Renal Biopsy to diagnose • Massive proteinuria(>3 gm/d) • Minimal hematuria • Uncommon to present as ARF • Renal Biopsy needed to diagnose. • •
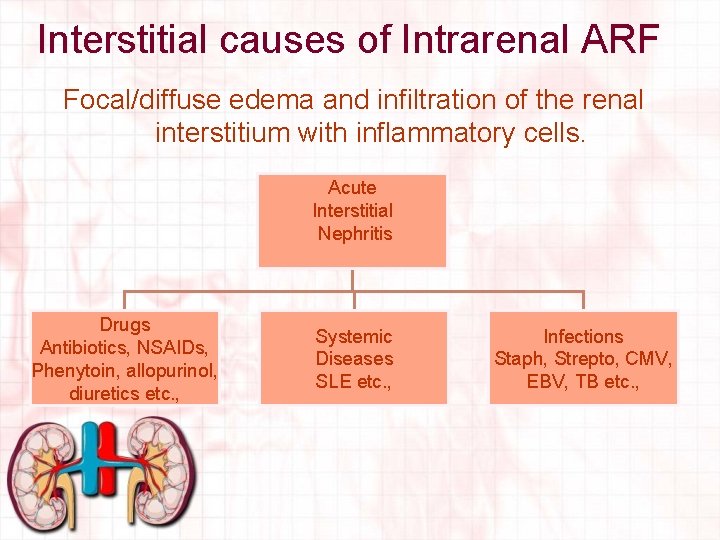
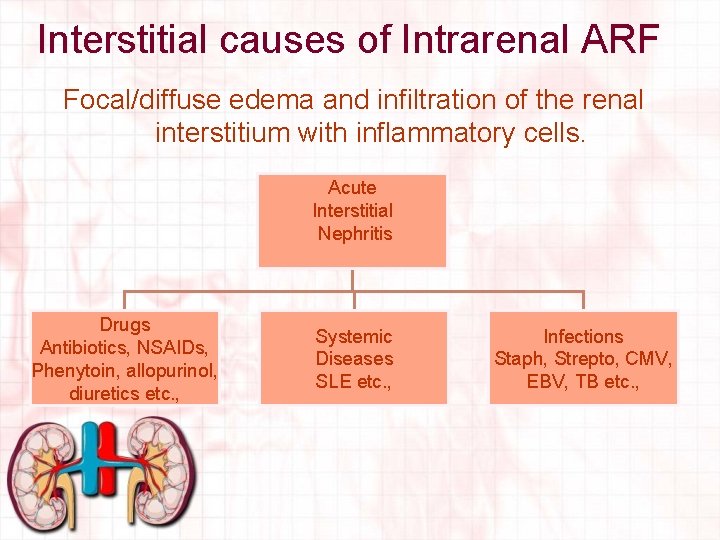
Interstitial causes of Intrarenal ARF Focal/diffuse edema and infiltration of the renal interstitium with inflammatory cells. Acute Interstitial Nephritis Drugs Antibiotics, NSAIDs, Phenytoin, allopurinol, diuretics etc. , Systemic Diseases SLE etc. , Infections Staph, Strepto, CMV, EBV, TB etc. ,
Vascular causes of Intrarenal ARF • Large and Medium size vessels Renal artery thrombosis or emboli Renal vein thrombosis Polyarterial nodosa • Small vessel disease Atheroembolic phenomenon Microangiopathies like TTP, HUS, HELLP and malignant HTN.
Post renal Failure • • • Kidney stone (usually UVJ) Ureteropelvic junction (UPJ) or UVJ obstruction Bladder: as neurogenic bladder or fungus ball Urethra: posterior urethral valve; foreign body Iatrogenic: obstructed Foley; narcotics
Diagnosis and Assessment of ARF Clinical history • Frequently reveals recent hypotension, sepsis, muscle necrosis, or volume depletion, as well as exposure to nephrotoxic agents • Patients with rhabdomyolysis present with severe muscle pains and generalized soreness • Check for symptoms of primary renal disease - UTI, gross hematuria, flank pain, Hx of strept infection, drug exposure ( aminoglycosides or narcotics) for bladder dysfunction
Assessment of ARF During physical exam Look for secondary causes – Causes of decreased effective circulatory volume - CHF, ascites, edema, sepsis – Signs of systemic illness - (vasculitis, SLE): rash, arthritis, purpura – Signs of obstructive uropathy: enlarged kidneys or bladder CHECK FOLEY.
Assessment of ARF • UA: – – High specific gravity = dehydration RBCs = UTI, urolithiasis WBCs, bacteria = UTI Casts: RBC (glomerulonephritis), WBC (pyelonephritis), and epithelial cells and granular casts (ischemic damage) • Electrolytes to assess for metabolic d/o • Urine Na, Creatinine • ECG to look for peaked T waves, indicates Hyperkalemia
Assessment for ARF • • • BUN, Cr; CBC with platelets. Urine Analysis: hematuria, myoglobinuria, proteinuria, RBC casts, eosinophils Urine indices (U-osm, U-CR, U-Na ) Renal Ultra Sound (with Doppler flow to rule out renal vein thrombosis) Anti-DNA, ANA, renal biopsy
Role of Nurses in management • The nurse plays a pivotal role in the assessment of the patient’s volume status to determine if he/she is hypovolaemic or hypervolaemic








Nursing Considerations • • Make sure the dressing remains intact Do not push or pull on the catheter Do not disconnect any of the catheters Always transport the patient and bags/catheters as one piece • Never inject anything into catheter 03/05/2011 47

Acute Renal Failure • Nursing interventions 03/05/2011 – Monitor I/O, including all body fluids – Monitor lab results – Watch hyperkalemia symptoms: malaise, anorexia, or muscle weakness, EKG changes – watch for hyperglycemia or hypoglycemia if receiving TPN or insulin infusions – – – Maintain nutrition Safety measures Mouth care Daily weights Assess for signs of heart failure – Skin integrity problems 49
Nursing Management of ARF • Monitoring fluid and electrolyte balance. The nurse: – monitors the patient’s serum electrolyte levels and physical indicators of fluid and electrolyte imbalances. – carefully screens parenteral fluids, all oral intake, and all medications to ensure that hidden sources of potassium are not inadvertently administered or consumed. – monitors the patient closely for signs and symptoms of hyperkalemia (Slide 12). – monitors fluid status by paying careful attention to fluid intake, urine output, apparent edema, distention of the jugular veins, breath sounds, and increasing difficulty in breathing. – maintains accurate daily weight, and intake and output record. – reports to physician indicators of deteriorating fluid and electrolyte status, and prepares for emergency treatment. 50
Nursing Management of ARF (Continued…) • Reducing metabolic rate. The nurse: – should reduce the patient’s metabolic rate to reduce catabolism and the subsequent release of potassium and accumulation of waste products (urea and creatinine). – may keep the patient on bed rest to reduce exertion and the metabolic rate during the most acute stage of ARF. – should prevent or promptly treat fever and infection to decrease the metabolic rate and catabolism. 51
Nursing Management of ARF (Continued…) • Promoting pulmonary function. The nurse: – assist the patient to turn, cough, and take deep breaths frequently to prevent atelectasis and respiratory tract infection. • Preventing infection. The nurse: – strictly observes aseptic technique when caring for the patient to minimise the risk of infection and increased metabolism. – avoids, when possible, inserting an indwelling urinary catheter as it is a high risk for urinary tract infection (UTI). 52
