Transradial Access for CTO Patient Selection Techniques Ramon



- Slides: 60
Transradial Access for CTO: Patient Selection & Techniques Ramon Quesada, M. D. , FACP, FACC, FSCAI Medical Director, Interventional Cardiology, Cardiac Research & Outcomes Baptist Cardiac & Vascular Institute Clinical Associate Professor of Medicine Herbert Wertheim College of Medicine at Florida International University
Ramon Quesada, MD I have no real or apparent conflicts of interest to report.
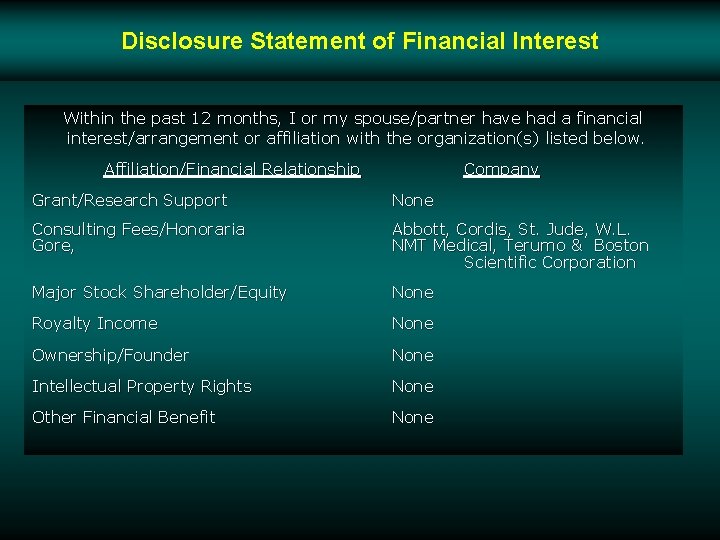
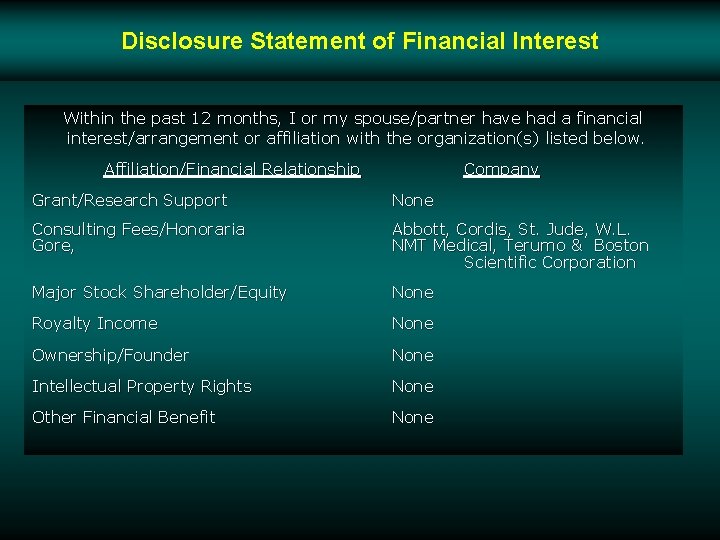
Disclosure Statement of Financial Interest Within the past 12 months, I or my spouse/partner have had a financial interest/arrangement or affiliation with the organization(s) listed below. Affiliation/Financial Relationship Company Grant/Research Support None Consulting Fees/Honoraria Gore, Abbott, Cordis, St. Jude, W. L. NMT Medical, Terumo & Boston Scientific Corporation Major Stock Shareholder/Equity None Royalty Income None Ownership/Founder None Intellectual Property Rights None Other Financial Benefit None
Why Radial? The Advantages v Decreased incidence of major entry-site complications v Easier vascular access and hemostasis for obese patients v Decreased time to ambulation v Decreased post-procedural cost v Improved patient movement
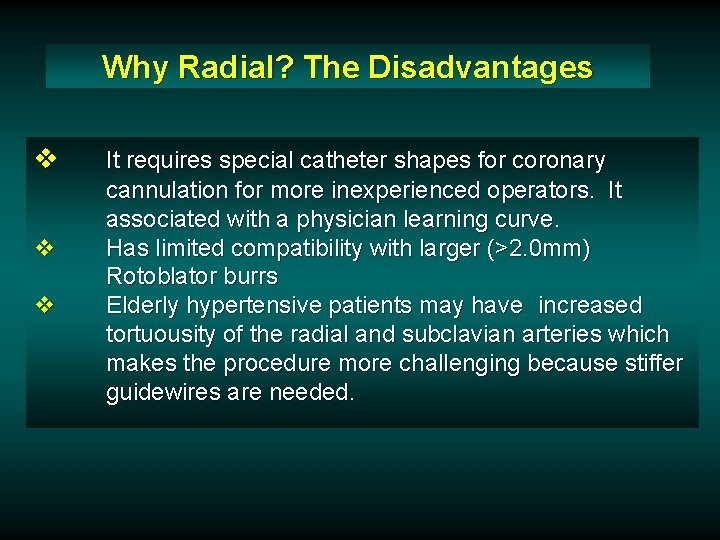
Why Radial? The Disadvantages v v v It requires special catheter shapes for coronary cannulation for more inexperienced operators. It associated with a physician learning curve. Has limited compatibility with larger (>2. 0 mm) Rotoblator burrs Elderly hypertensive patients may have increased tortuousity of the radial and subclavian arteries which makes the procedure more challenging because stiffer guidewires are needed.
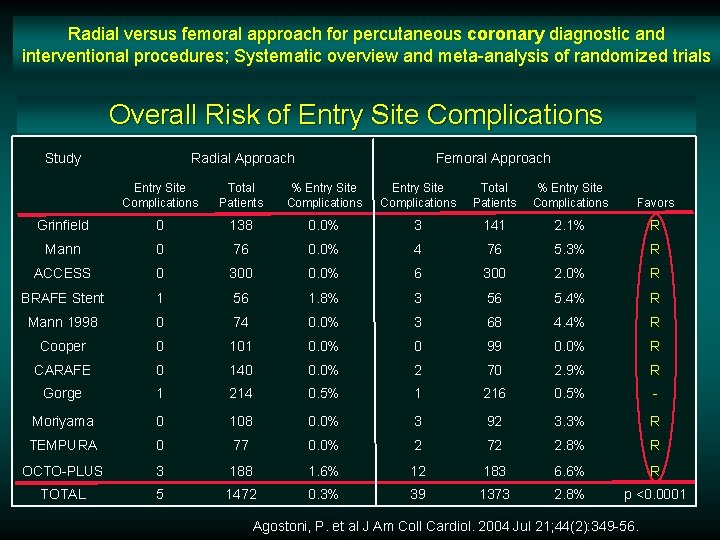
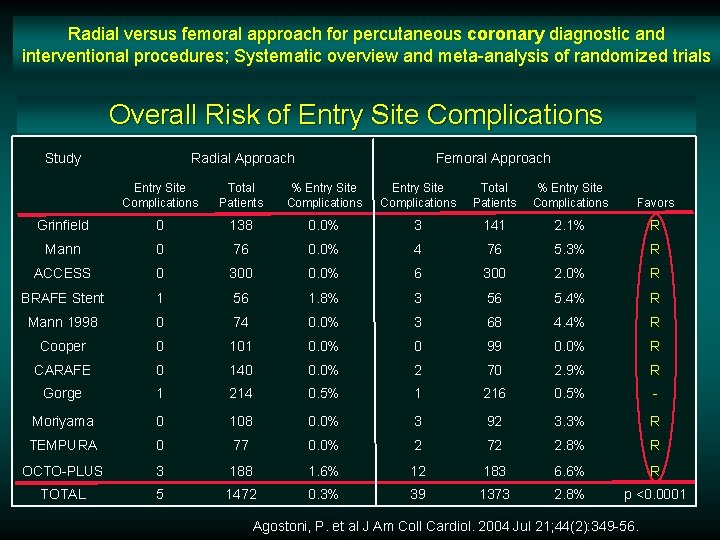
Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures; Systematic overview and meta-analysis of randomized trials Overall Risk of Entry Site Complications Study Radial Approach Femoral Approach Entry Site Complications Total Patients % Entry Site Complications Favors Grinfield 0 138 0. 0% 3 141 2. 1% R Mann 0 76 0. 0% 4 76 5. 3% R ACCESS 0 300 0. 0% 6 300 2. 0% R BRAFE Stent 1 56 1. 8% 3 56 5. 4% R Mann 1998 0 74 0. 0% 3 68 4. 4% R Cooper 0 101 0. 0% 0 99 0. 0% R CARAFE 0 140 0. 0% 2 70 2. 9% R Gorge 1 214 0. 5% 1 216 0. 5% - Moriyama 0 108 0. 0% 3 92 3. 3% R TEMPURA 0 77 0. 0% 2 72 2. 8% R OCTO-PLUS 3 188 1. 6% 12 183 6. 6% R TOTAL 5 1472 0. 3% 39 1373 2. 8% p <0. 0001 Agostoni, P. et al J Am Coll Cardiol. 2004 Jul 21; 44(2): 349 -56.
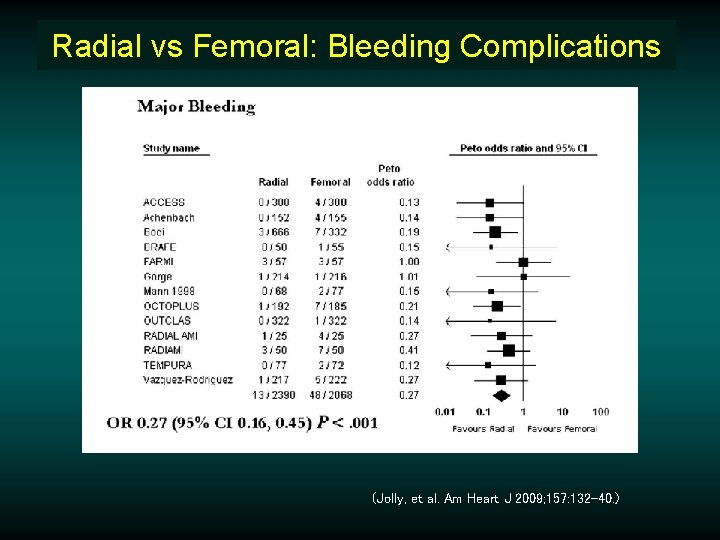
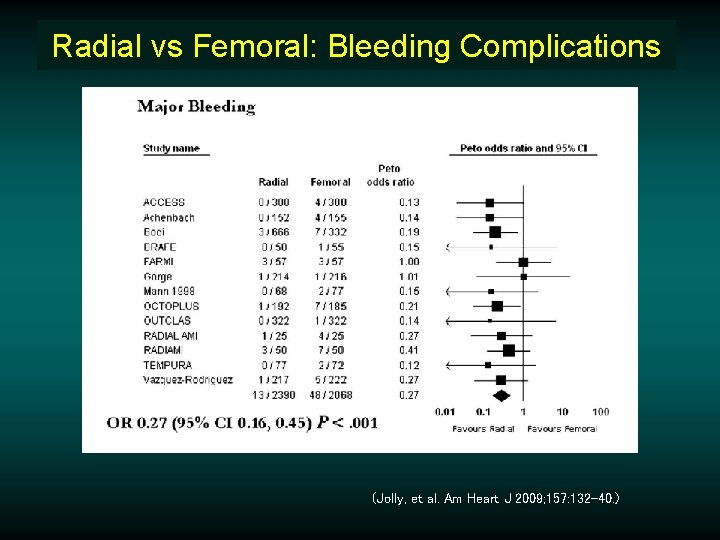
Radial vs Femoral: Bleeding Complications (Jolly, et al. Am Heart J 2009; 157: 132 -40. )
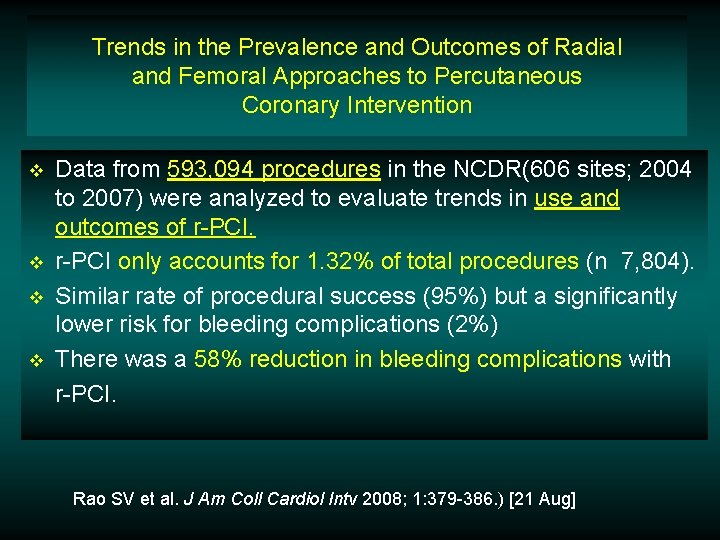
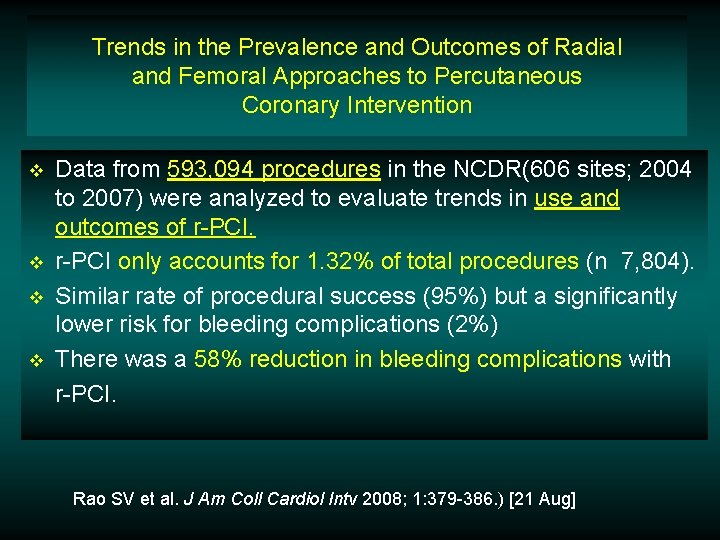
Trends in the Prevalence and Outcomes of Radial and Femoral Approaches to Percutaneous Coronary Intervention v v Data from 593, 094 procedures in the NCDR(606 sites; 2004 to 2007) were analyzed to evaluate trends in use and outcomes of r-PCI only accounts for 1. 32% of total procedures (n 7, 804). Similar rate of procedural success (95%) but a significantly lower risk for bleeding complications (2%) There was a 58% reduction in bleeding complications with r-PCI. Rao SV et al. J Am Coll Cardiol Intv 2008; 1: 379 -386. ) [21 Aug]
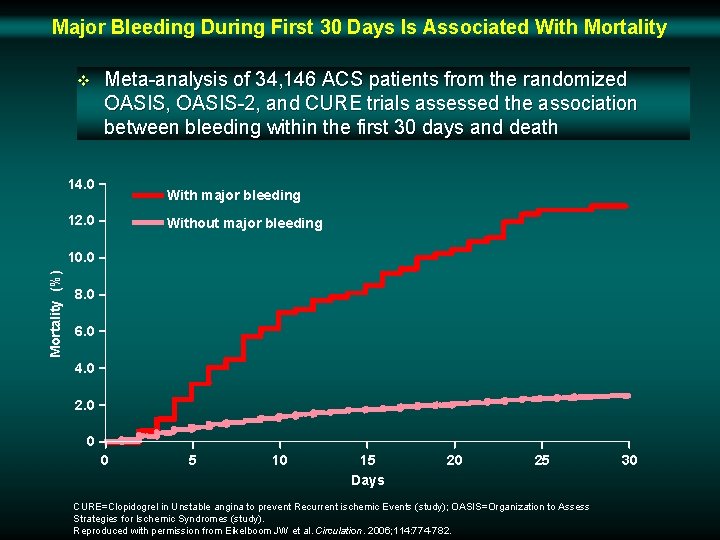
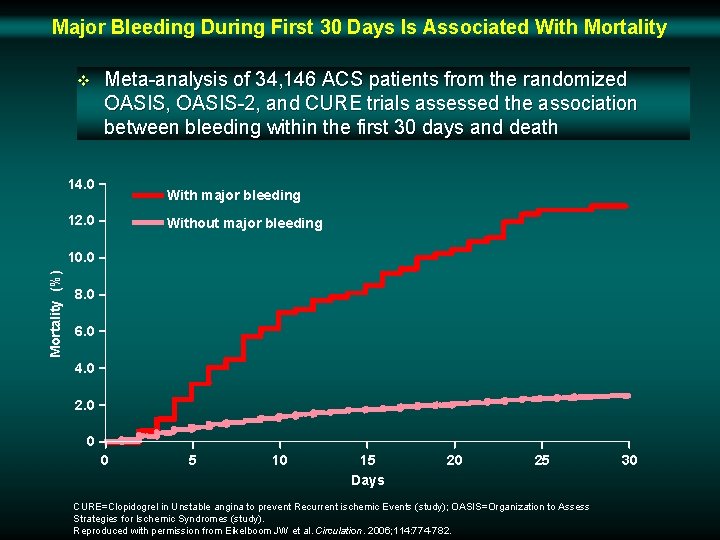
Major Bleeding During First 30 Days Is Associated With Mortality v Meta-analysis of 34, 146 ACS patients from the randomized OASIS, OASIS-2, and CURE trials assessed the association between bleeding within the first 30 days and death 14. 0 With major bleeding 12. 0 Without major bleeding Mortality (%) 10. 0 8. 0 6. 0 4. 0 2. 0 0 0 5 10 15 Days 20 25 CURE=Clopidogrel in Unstable angina to prevent Recurrent ischemic Events (study); OASIS=Organization to Assess Strategies for Ischemic Syndromes (study). Reproduced with permission from Eikelboom JW et al. Circulation. 2006; 114: 774 -782. 30
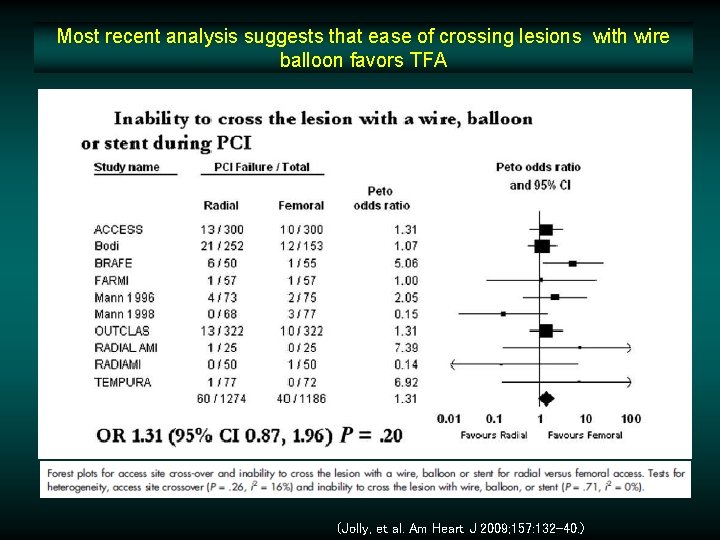
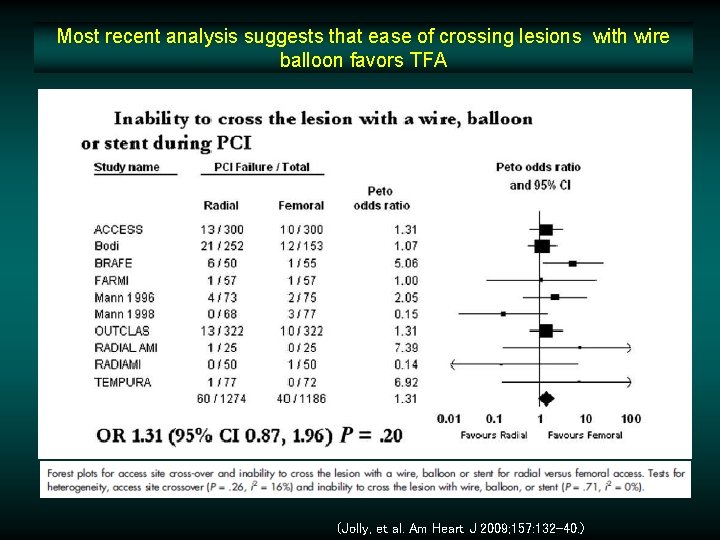
Most recent analysis suggests that ease of crossing lesions with wire balloon favors TFA (Jolly, et al. Am Heart J 2009; 157: 132 -40. )
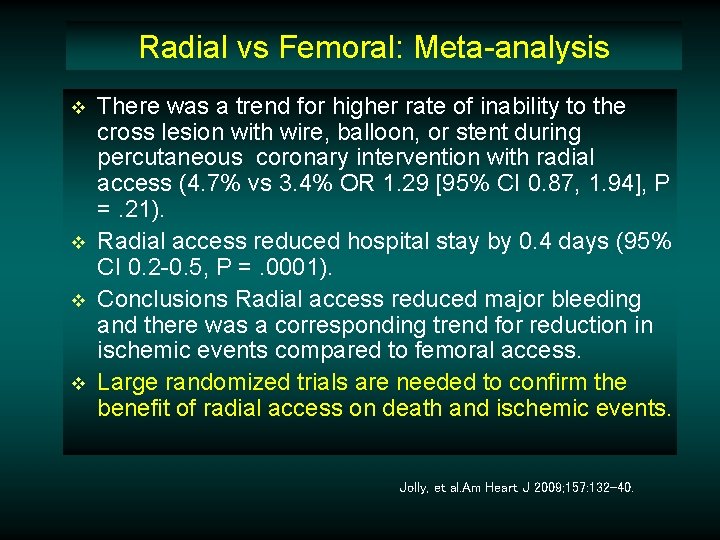
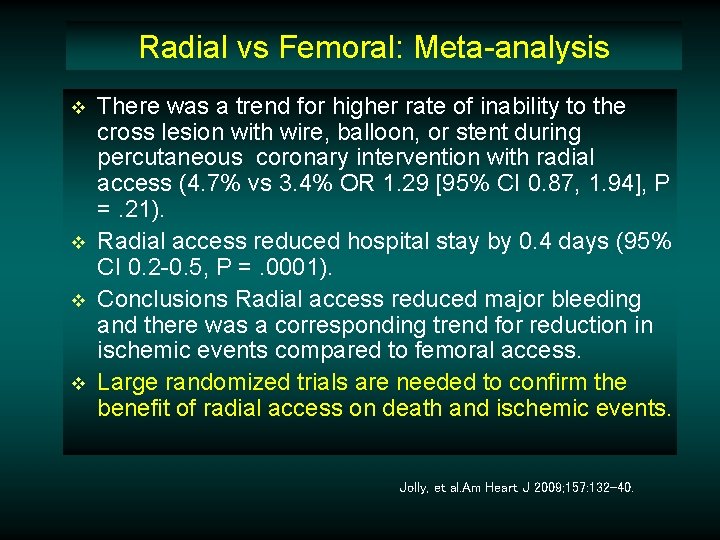
Radial vs Femoral: Meta-analysis v v There was a trend for higher rate of inability to the cross lesion with wire, balloon, or stent during percutaneous coronary intervention with radial access (4. 7% vs 3. 4% OR 1. 29 [95% CI 0. 87, 1. 94], P =. 21). Radial access reduced hospital stay by 0. 4 days (95% CI 0. 2 -0. 5, P =. 0001). Conclusions Radial access reduced major bleeding and there was a corresponding trend for reduction in ischemic events compared to femoral access. Large randomized trials are needed to confirm the benefit of radial access on death and ischemic events. Jolly, et al. Am Heart J 2009; 157: 132 -40.
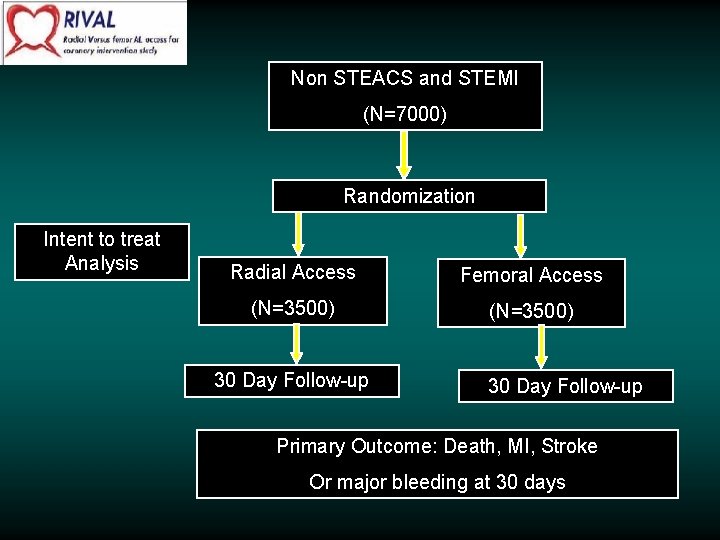
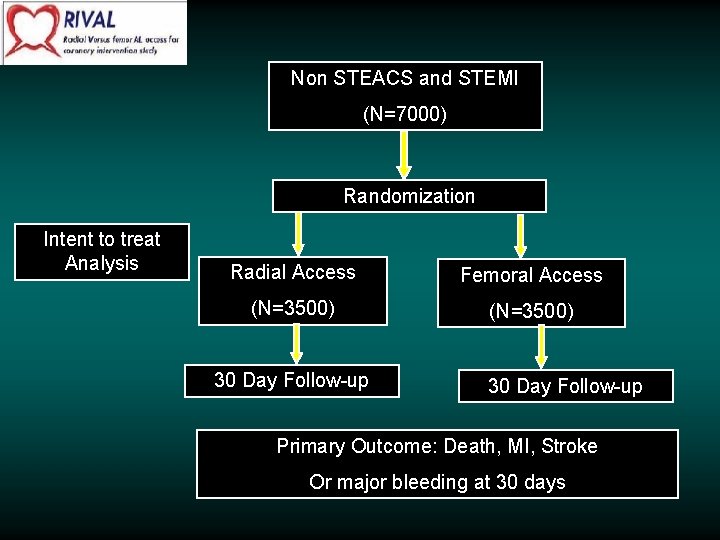
Non STEACS and STEMI (N=7000) Randomization Intent to treat Analysis Radial Access Femoral Access (N=3500) 30 Day Follow-up Primary Outcome: Death, MI, Stroke Or major bleeding at 30 days
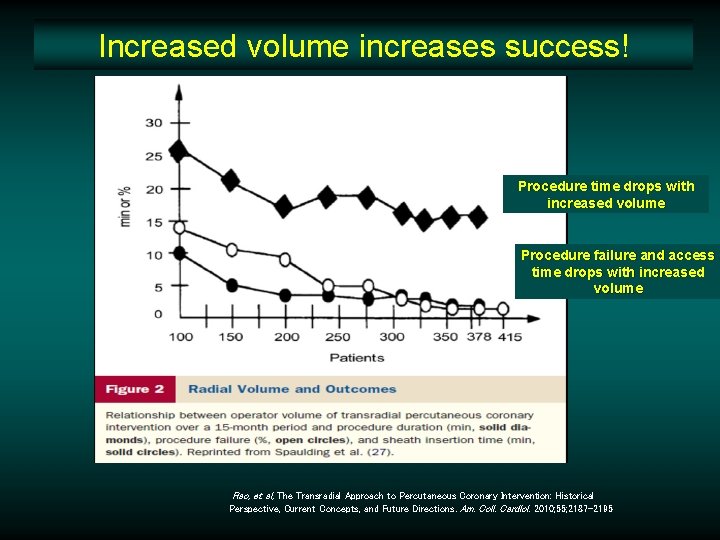
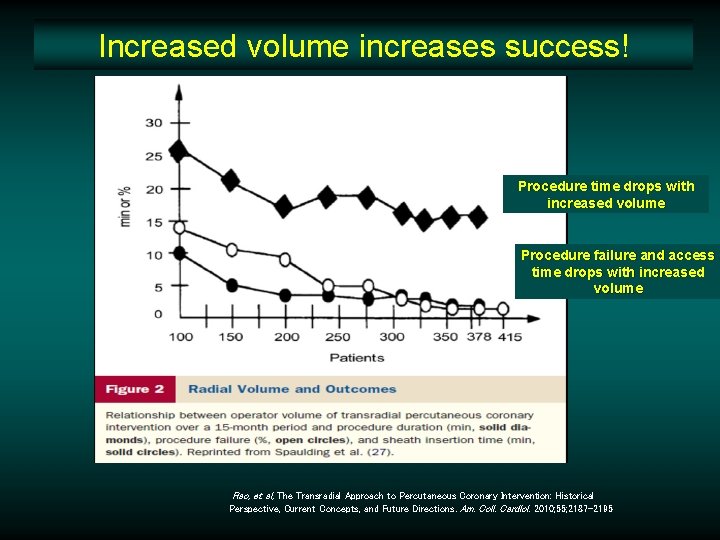
Increased volume increases success! Procedure time drops with increased volume Procedure failure and access time drops with increased volume Rao, et al, The Transradial Approach to Percutaneous Coronary Intervention: Historical Perspective, Current Concepts, and Future Directions. Am. Coll. Cardiol. 2010; 55; 2187 -2195
Ideal Candidates for Transradial Access v 90% of the population who have dual circulation to the hand v Obese individuals who are at increased risk of complications from transfemoral access v Individuals with severe peripheral vascular disease
Contraindications? There is only one contraindication -- an abnormal Allen test.
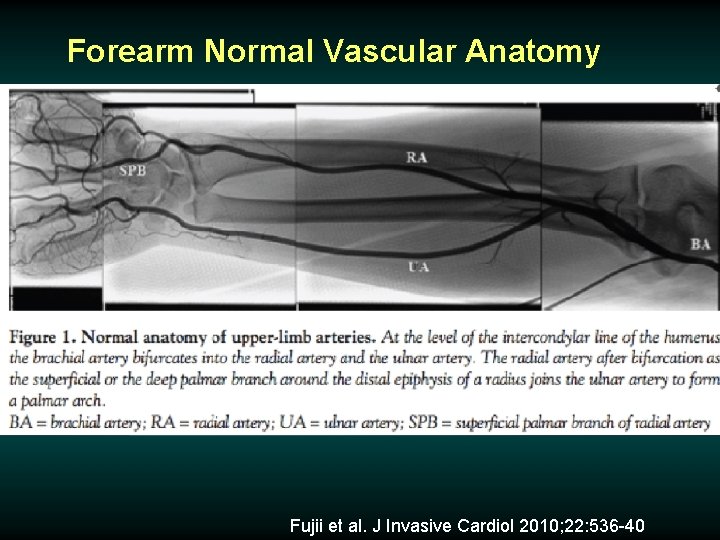
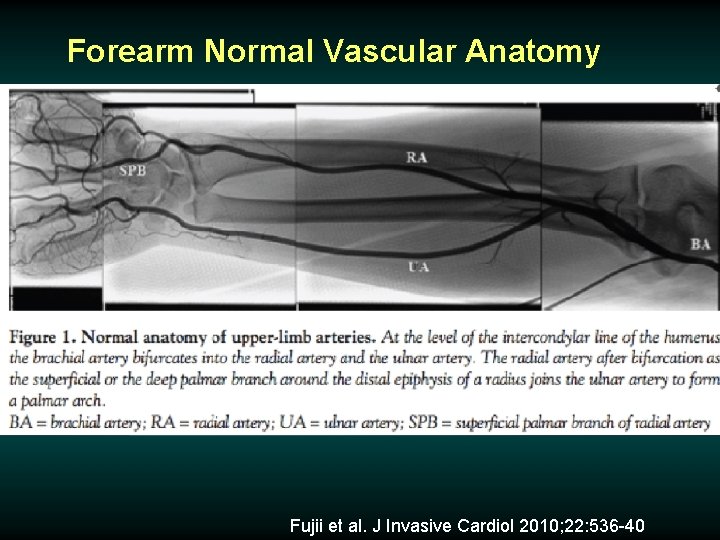
Forearm Normal Vascular Anatomy Fujii et al. J Invasive Cardiol 2010; 22: 536 -40
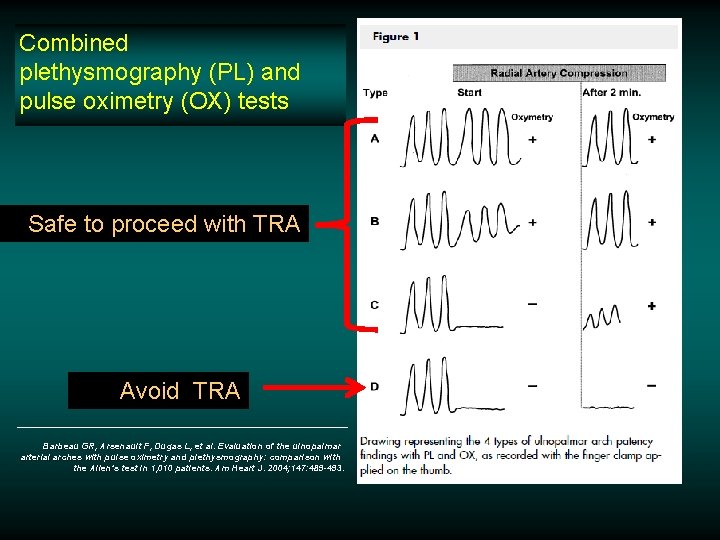
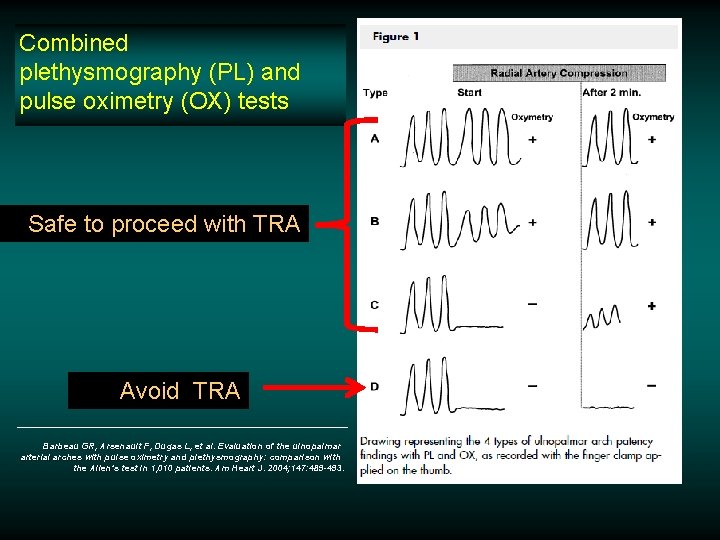
Combined plethysmography (PL) and pulse oximetry (OX) tests Safe to proceed with TRA Avoid TRA Barbeau GR, Arsenault F, Dugas L, et al. Evaluation of the ulnopalmar arterial arches with pulse oximetry and plethysmography: comparison with the Allen’s test in 1, 010 patients. Am Heart J. 2004; 147: 489 -493.
TRA for Complex Subgroups v v v Elderly Patients (Octogenarians) Acute Myocardial Infarction Bifurcations Other Complex (B 2 -C) Lesions Chronic Total Occlusions
TRA for Complex Subgroups v v v Elderly Patients (Octogenarians) Acute Myocardial Infarction Bifurcations Other Complex (B 2 -C) Lesions Chronic Total Occlusions
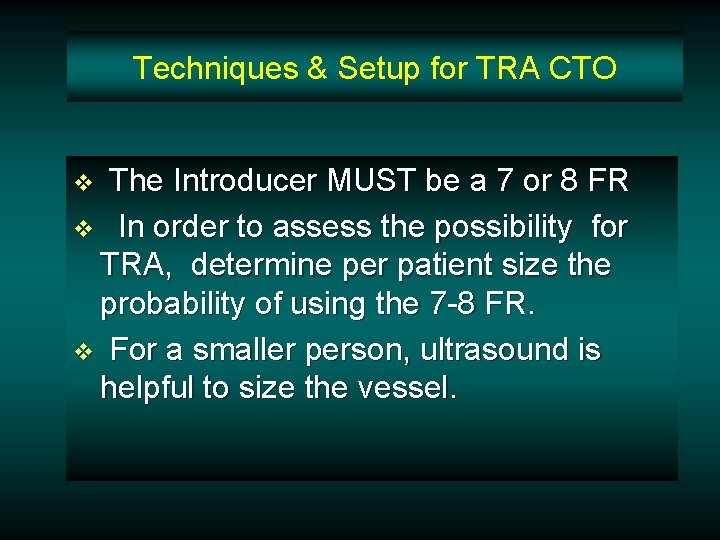
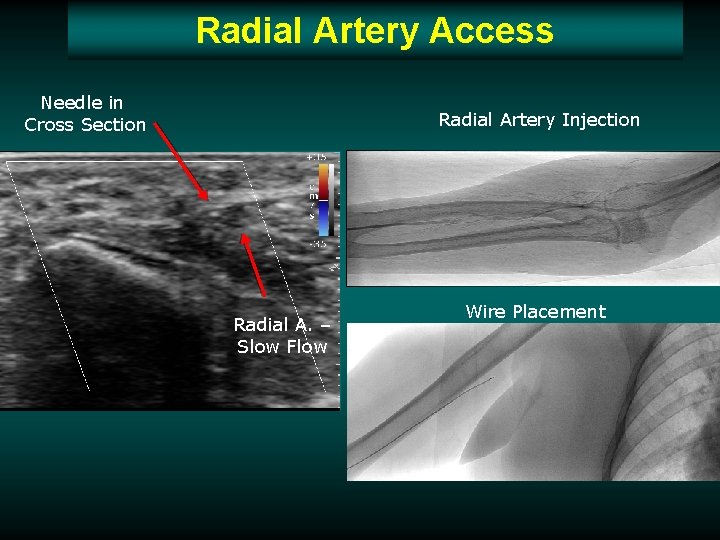
Techniques & Setup for TRA CTO The Introducer MUST be a 7 or 8 FR v In order to assess the possibility for TRA, determine per patient size the probability of using the 7 -8 FR. v For a smaller person, ultrasound is helpful to size the vessel. v
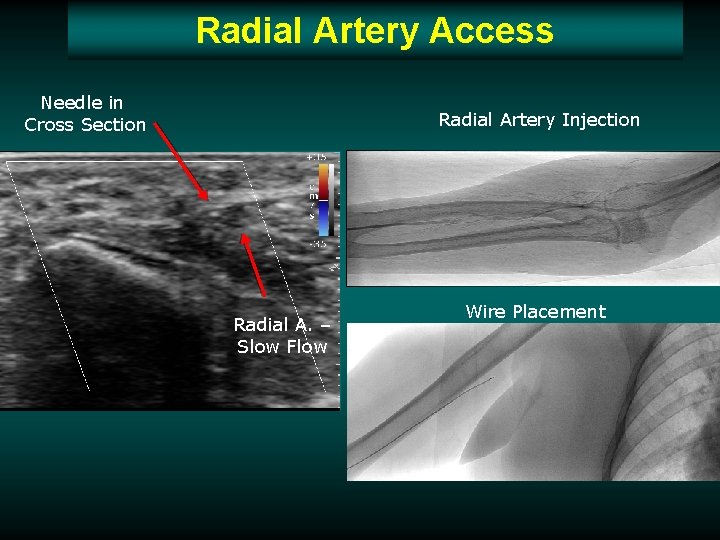
Radial Artery Access Needle in Cross Section Radial Artery Injection Radial A. – Slow Flow Wire Placement
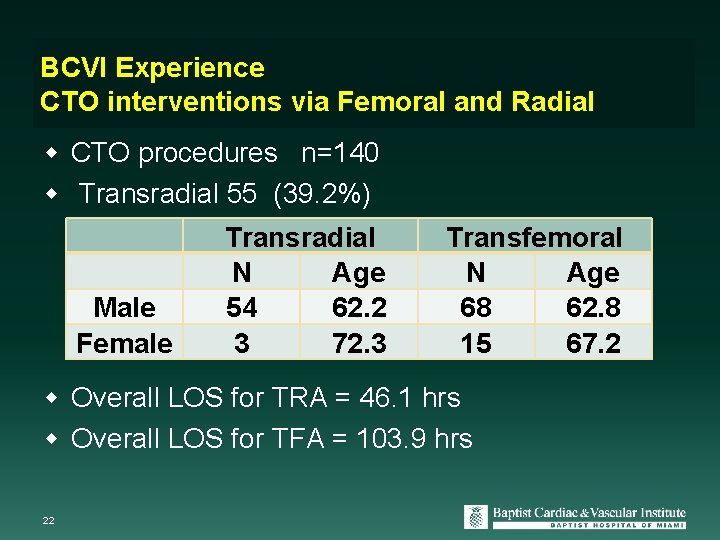
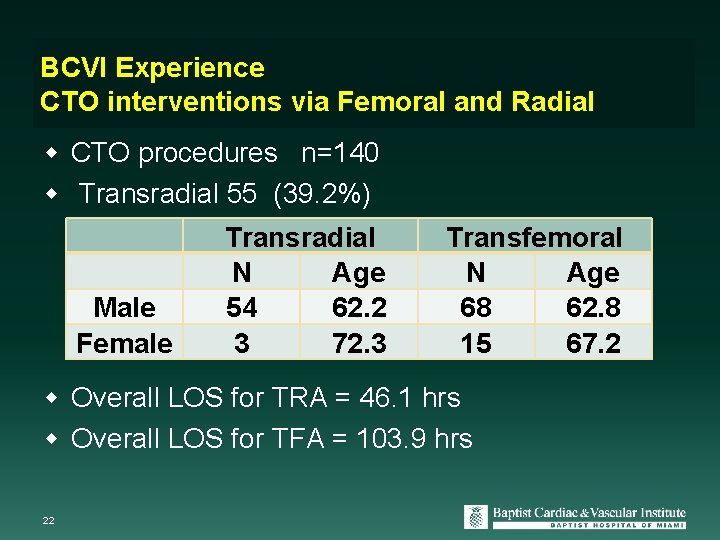
BCVI Experience CTO interventions via Femoral and Radial CTO procedures n=140 Transradial 55 (39. 2%) Male Female Transradial N Age 54 62. 2 3 72. 3 Transfemoral N Age 68 62. 8 15 67. 2 Overall LOS for TRA = 46. 1 hrs Overall LOS for TFA = 103. 9 hrs 22
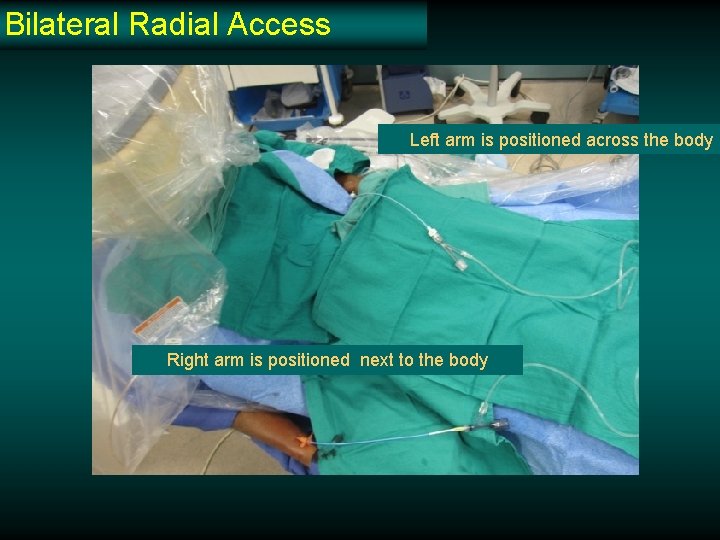
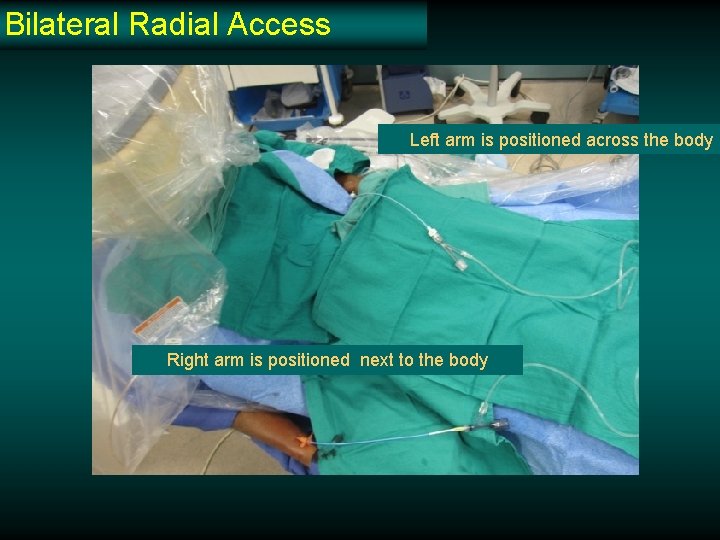
Bilateral Radial Access Left arm is positioned across the body Right arm is positioned next to the body
Are the Right and Left Radial Arteries Equal in Ease of Access?
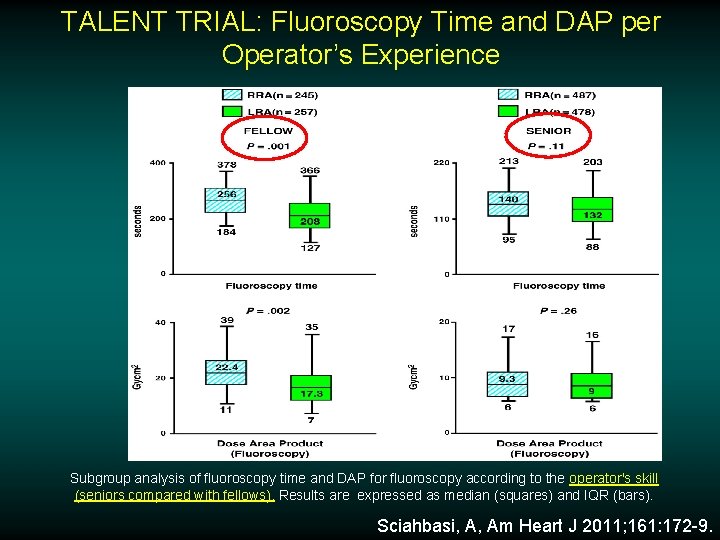
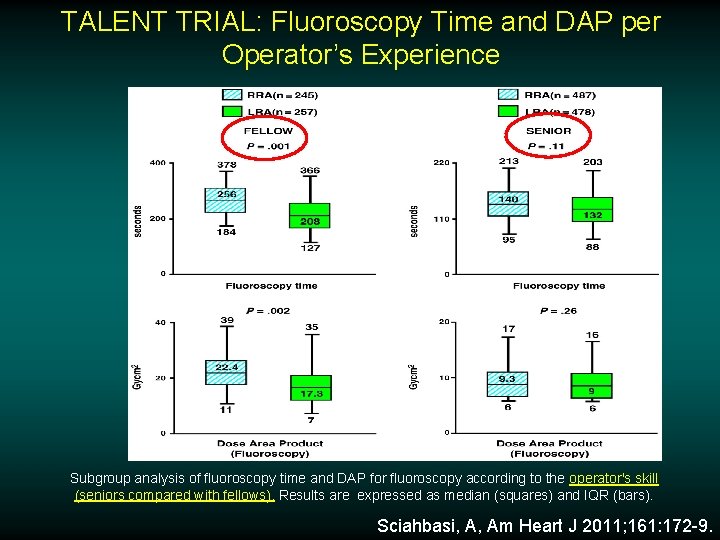
TALENT TRIAL: Fluoroscopy Time and DAP per Operator’s Experience Subgroup analysis of fluoroscopy time and DAP for fluoroscopy according to the operator's skill (seniors compared with fellows). Results are expressed as median (squares) and IQR (bars). Sciahbasi, A, Am Heart J 2011; 161: 172 -9.
How I Ensure TRA CTO success Patient selection Select guide catheter Apply CTO techniques
Patient Selection v Remember that you must be able to cannulate the coronaries with proper guide support so it is imperative that you SEE the arch
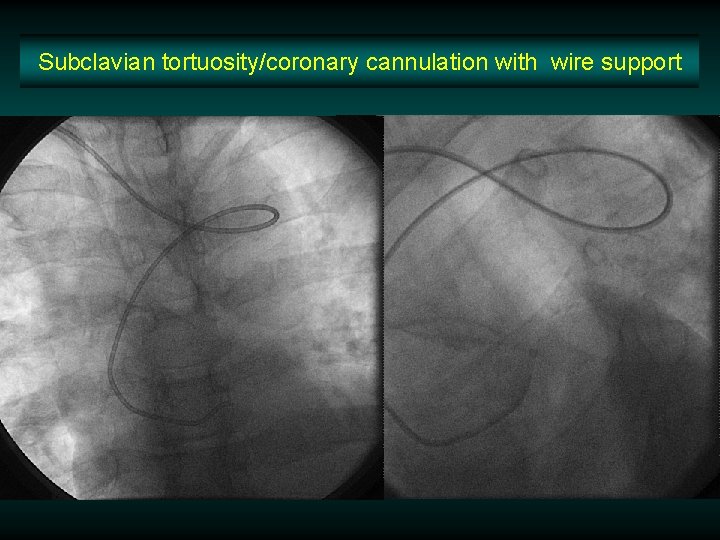
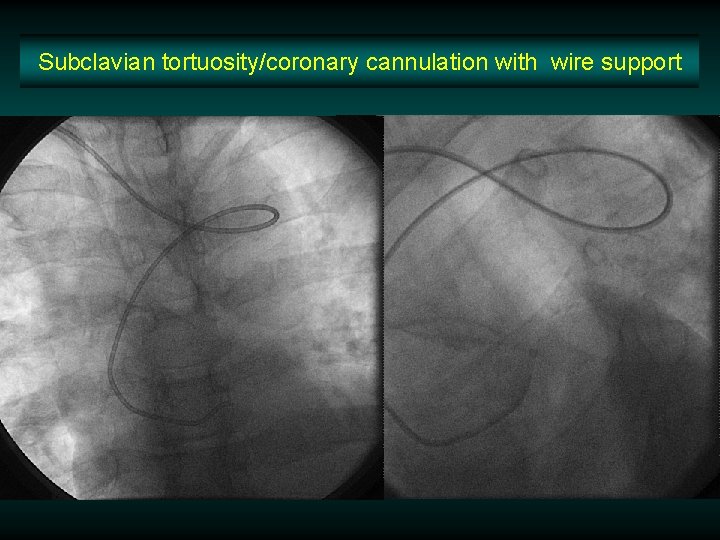
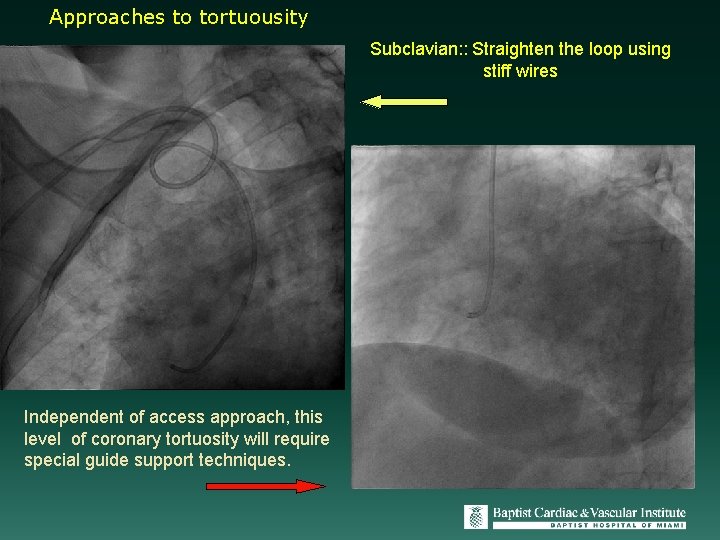
Subclavian tortuosity/coronary cannulation with wire support
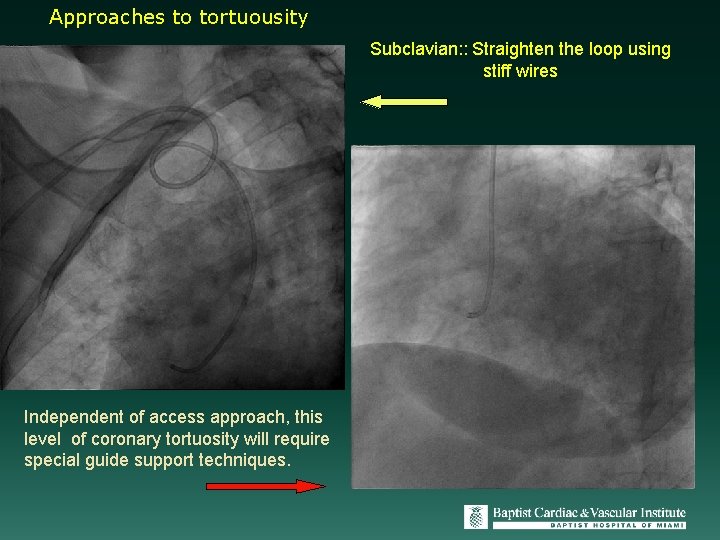
Approaches to tortuousity Subclavian: : Straighten the loop using stiff wires Independent of access approach, this level of coronary tortuosity will require special guide support techniques.
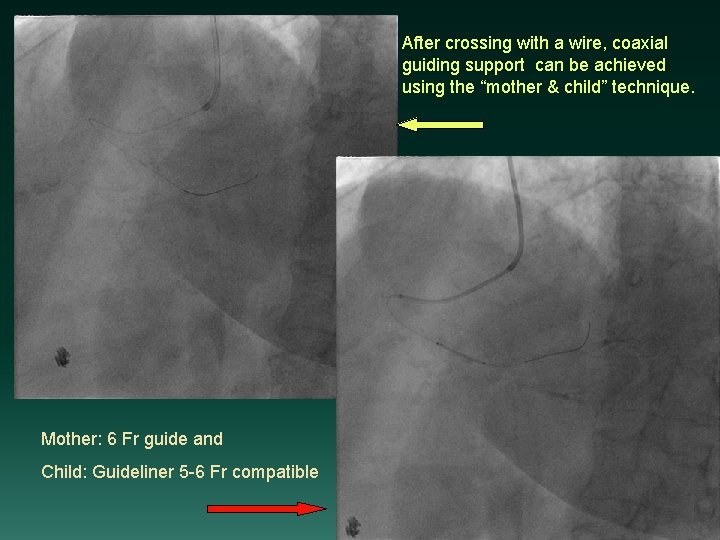
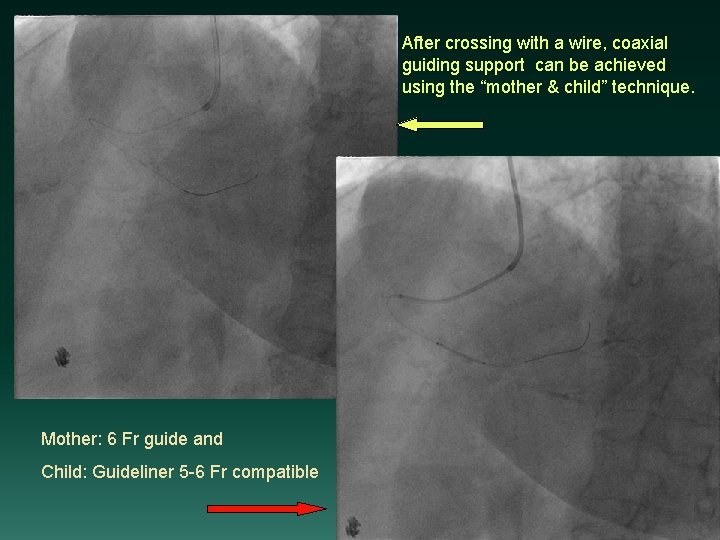
After crossing with a wire, coaxial guiding support can be achieved using the “mother & child” technique. Mother: 6 Fr guide and Child: Guideliner 5 -6 Fr compatible
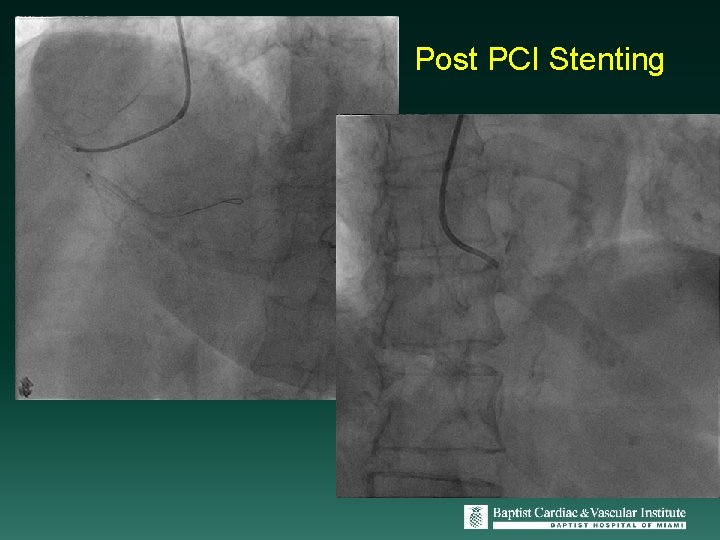
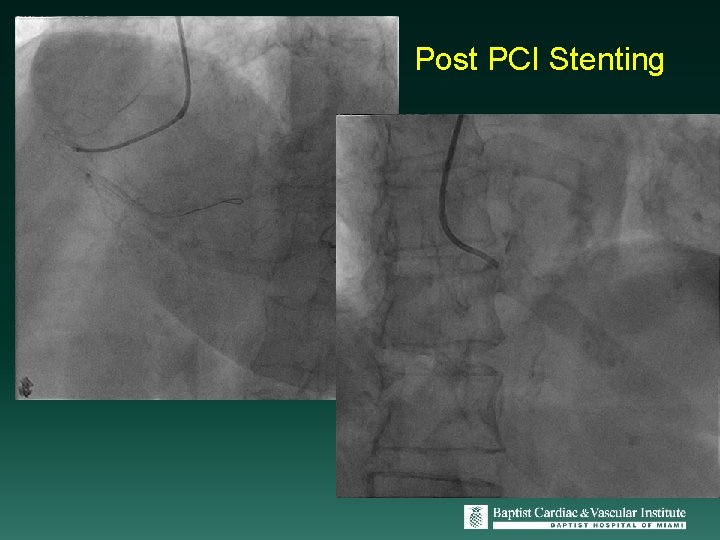
Post PCI Stenting
Select Guide Catheter v Selection of the best guide catheter is essential and should be chosen based on anatomic characteristics of the patient – a 7 or 8 FR to ensure adequate support and backup. v I favor XB for LCA and LAs for RCA

Can you apply all the CTO techniques via the transradial approach?
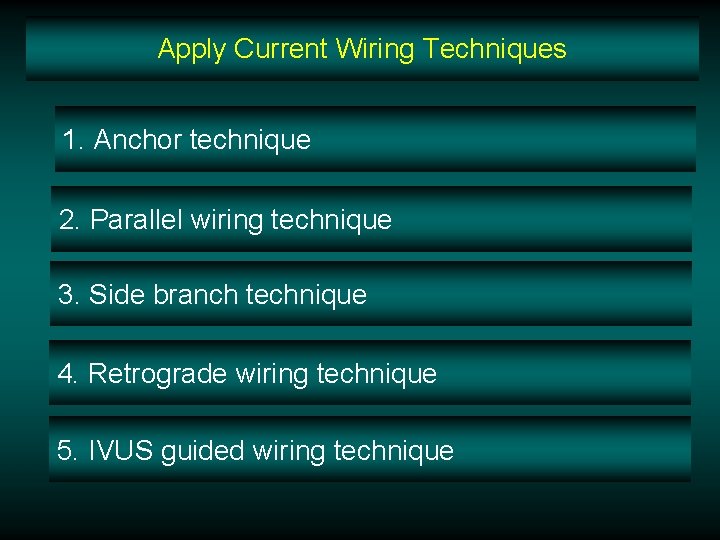
Apply Current Wiring Techniques 1. Anchor technique 2. Parallel wiring technique 3. Side branch technique 4. Retrograde wiring technique 5. IVUS guided wiring technique
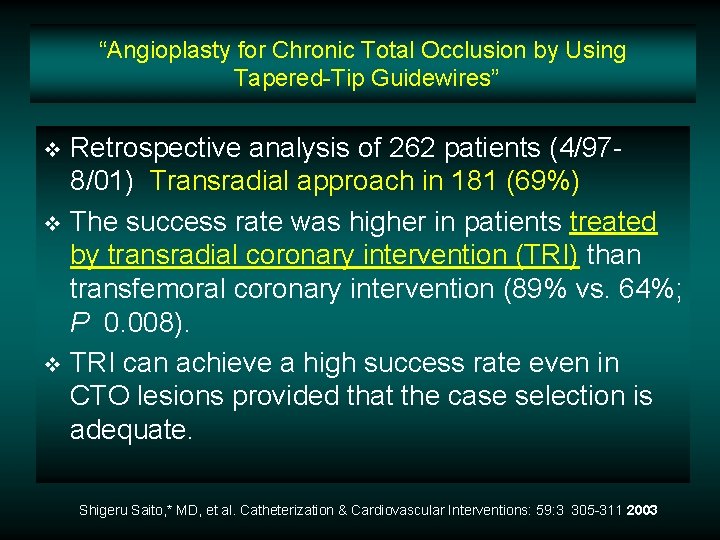
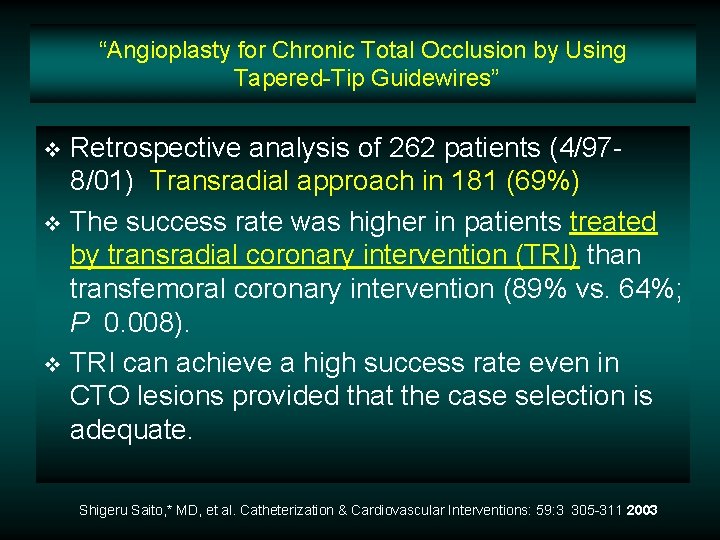
“Angioplasty for Chronic Total Occlusion by Using Tapered-Tip Guidewires” Retrospective analysis of 262 patients (4/978/01) Transradial approach in 181 (69%) v The success rate was higher in patients treated by transradial coronary intervention (TRI) than transfemoral coronary intervention (89% vs. 64%; P 0. 008). v TRI can achieve a high success rate even in CTO lesions provided that the case selection is adequate. v Shigeru Saito, * MD, et al. Catheterization & Cardiovascular Interventions: 59: 3 305 -311 2003
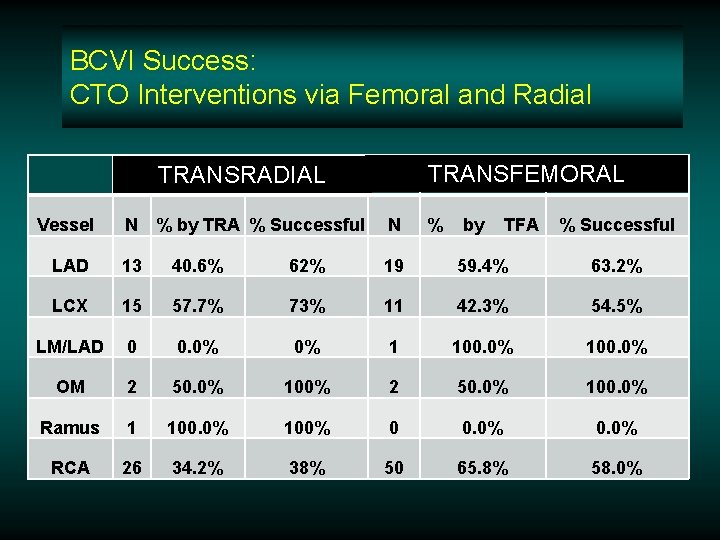
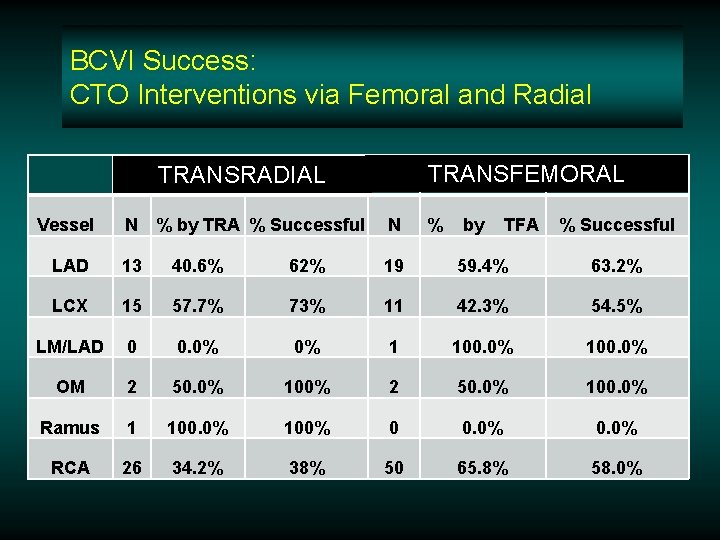
BCVI Success: CTO Interventions via Femoral and Radial TRANSFEMORAL TRANSRADIAL Vessel N % by TRA % Successful N % by TFA % Successful LAD 13 40. 6% 62% 19 59. 4% 63. 2% LCX 15 57. 7% 73% 11 42. 3% 54. 5% LM/LAD 0 0. 0% 0% 1 100. 0% OM 2 50. 0% 100% 2 50. 0% 100. 0% Ramus 1 100. 0% 100% 0 0. 0% RCA 26 34. 2% 38% 50 65. 8% 58. 0%
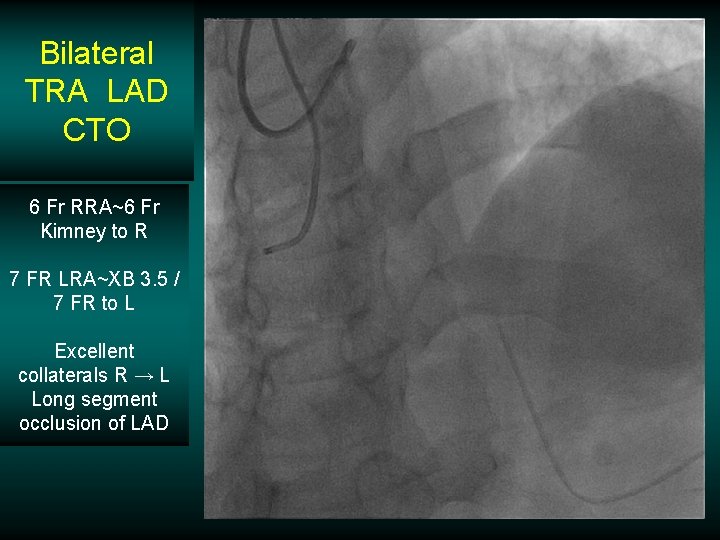
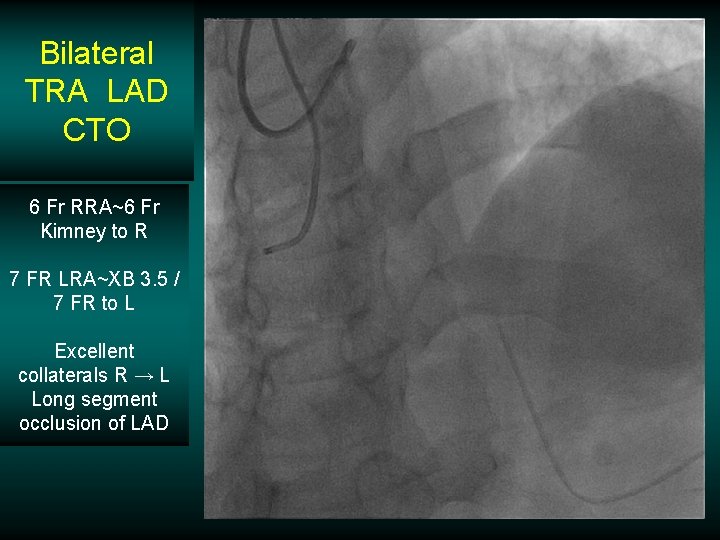
Bilateral TRA LAD CTO 6 Fr RRA~6 Fr Kimney to R 7 FR LRA~XB 3. 5 / 7 FR to L Excellent collaterals R → L Long segment occlusion of LAD
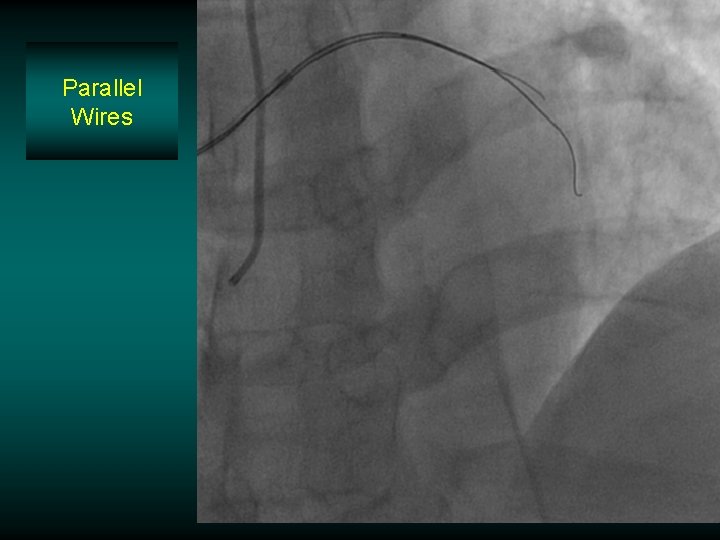
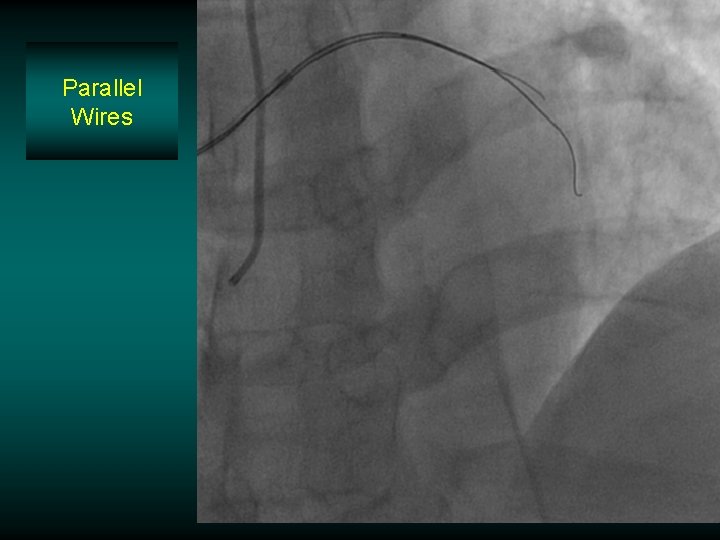
Parallel Wires
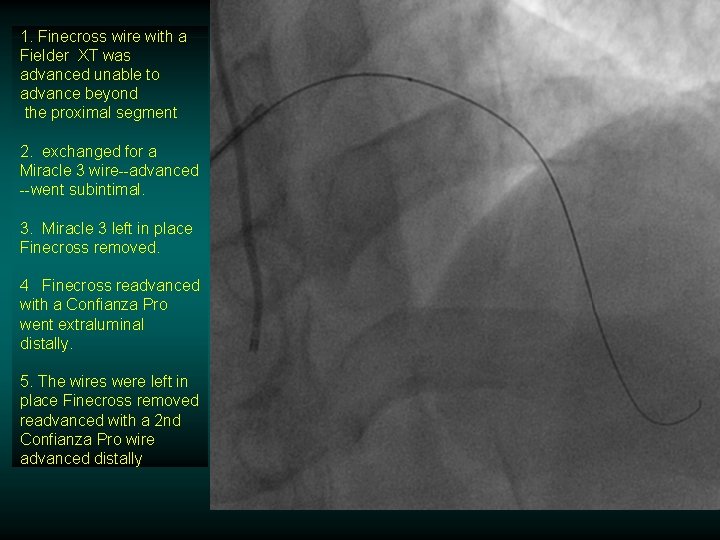
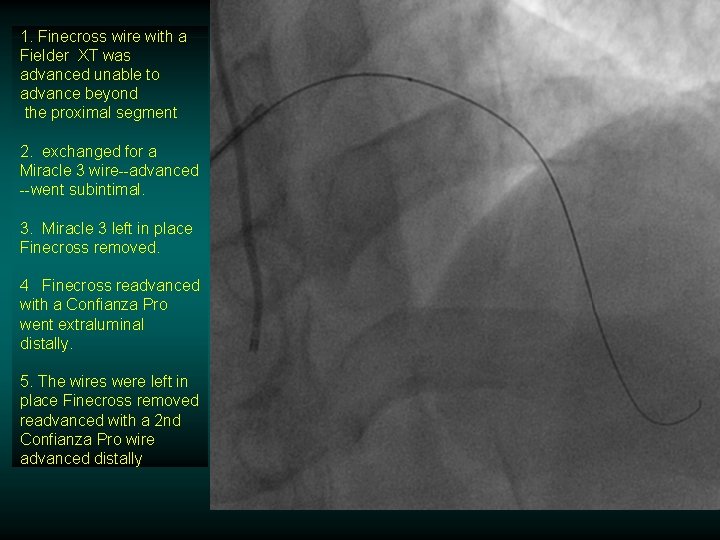
1. Finecross wire with a Fielder XT was advanced unable to advance beyond the proximal segment 2. exchanged for a Miracle 3 wire--advanced --went subintimal. 3. Miracle 3 left in place Finecross removed. 4 Finecross readvanced with a Confianza Pro went extraluminal distally. 5. The wires were left in place Finecross removed readvanced with a 2 nd Confianza Pro wire advanced distally
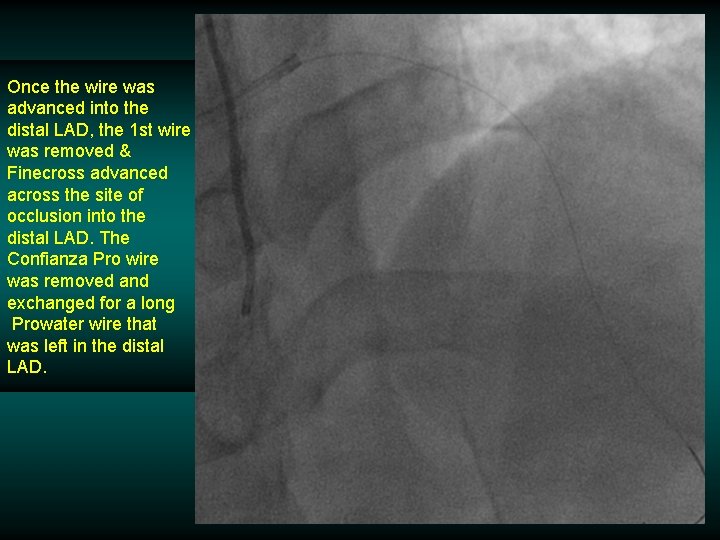
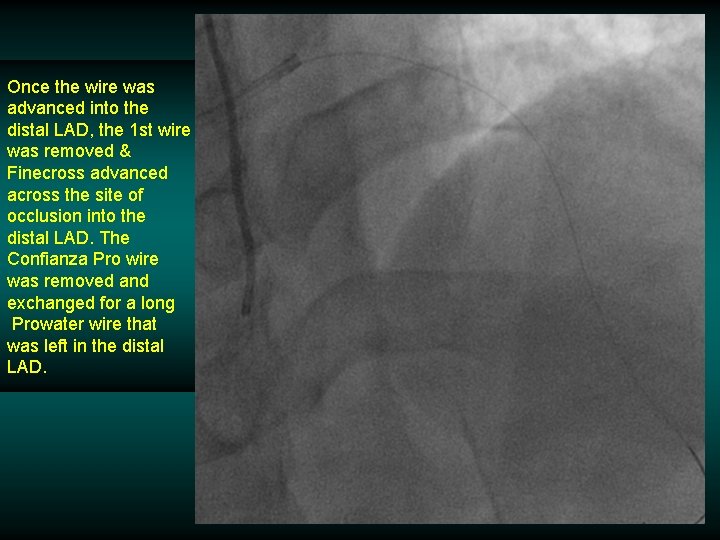
Once the wire was advanced into the distal LAD, the 1 st wire was removed & Finecross advanced across the site of occlusion into the distal LAD. The Confianza Pro wire was removed and exchanged for a long Prowater wire that was left in the distal LAD.
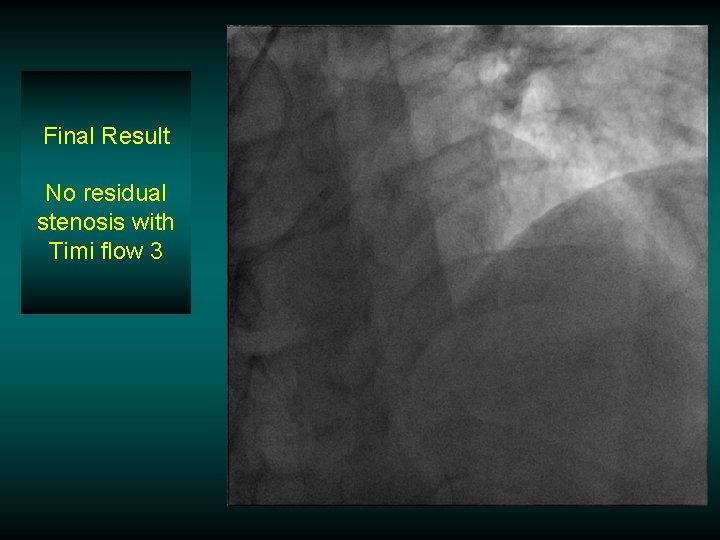
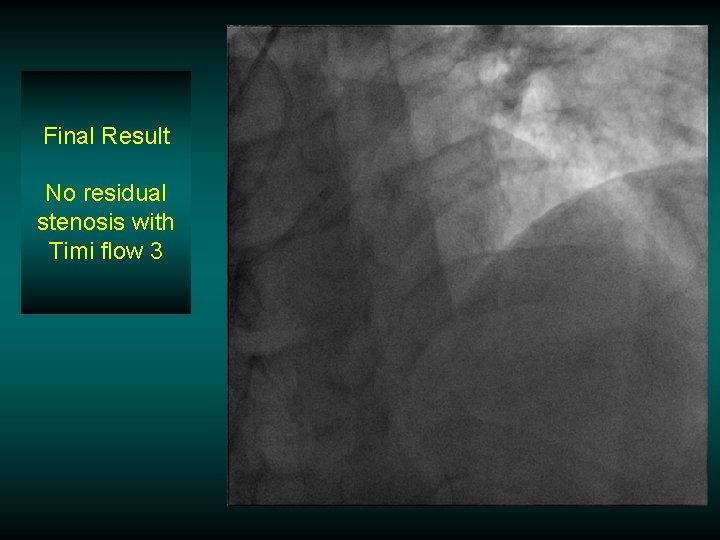
Final Result No residual stenosis with Timi flow 3
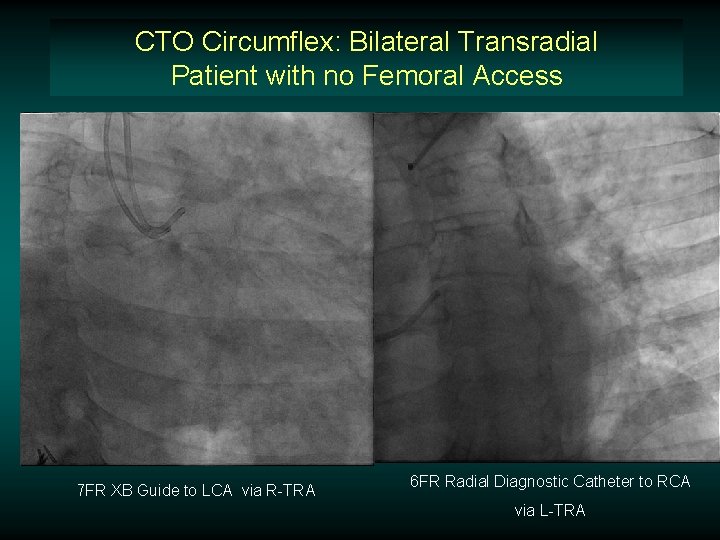
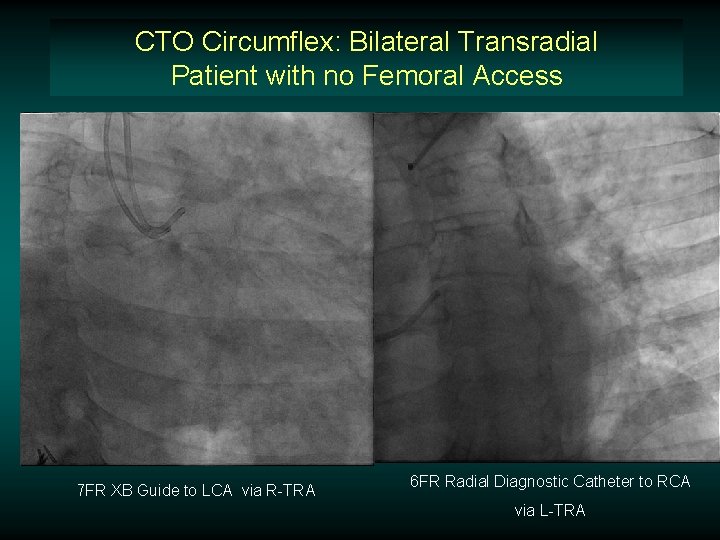
CTO Circumflex: Bilateral Transradial Patient with no Femoral Access 7 FR XB Guide to LCA via R-TRA 6 FR Radial Diagnostic Catheter to RCA via L-TRA
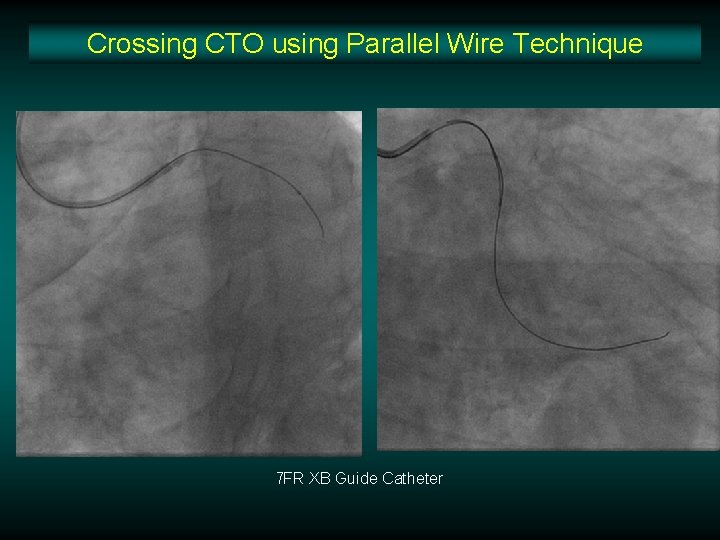
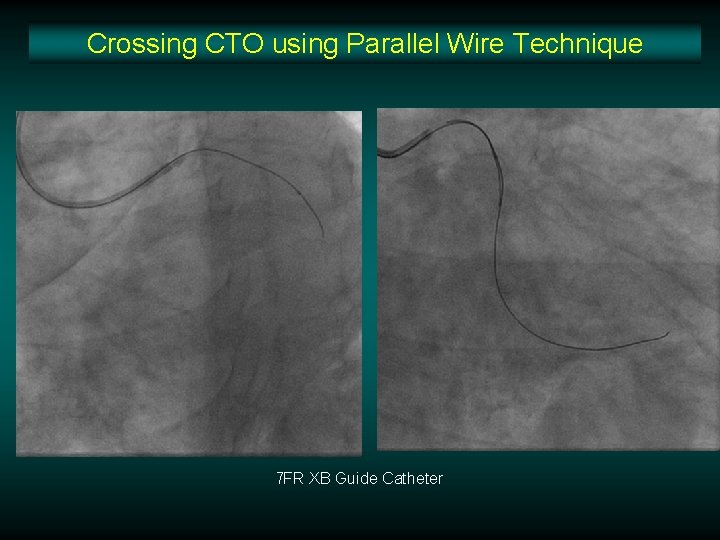
Crossing CTO using Parallel Wire Technique 7 FR XB Guide Catheter
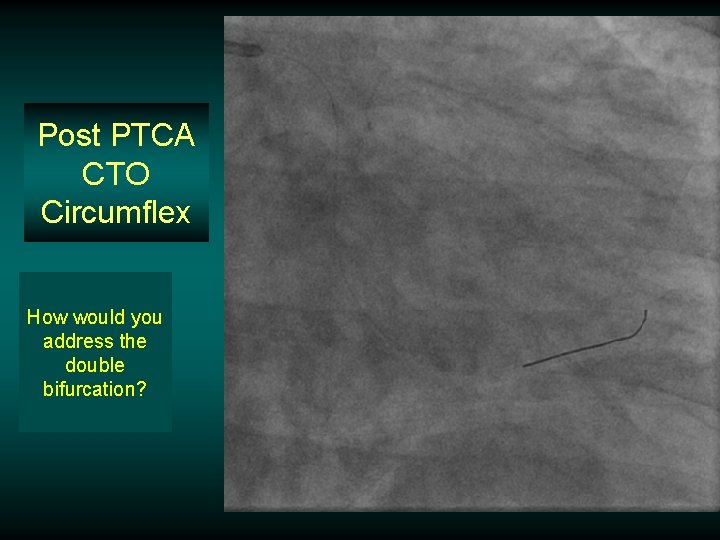
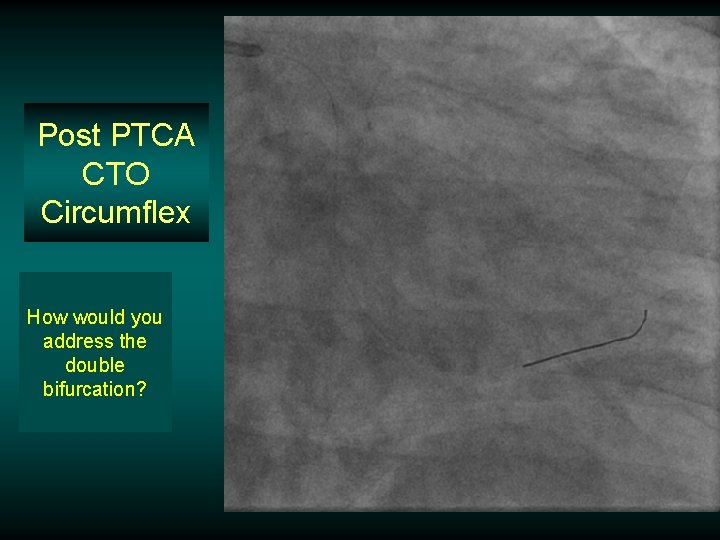
Post PTCA CTO Circumflex How would you address the double bifurcation?
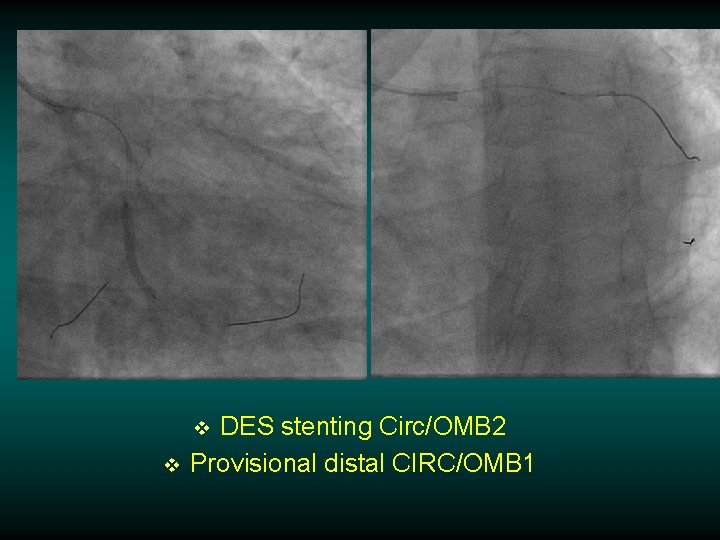
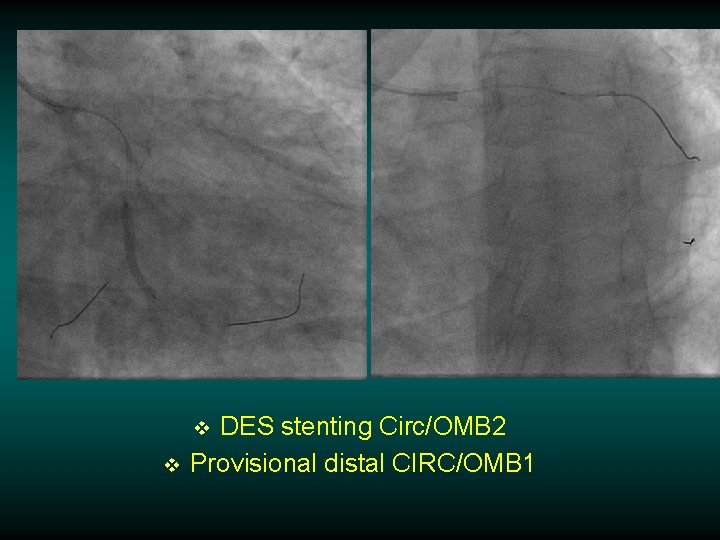
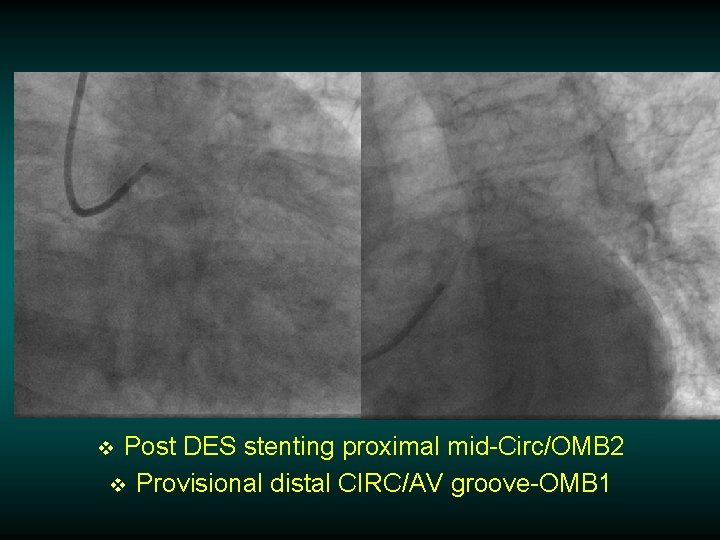
DES stenting Circ/OMB 2 Provisional distal CIRC/OMB 1 v v
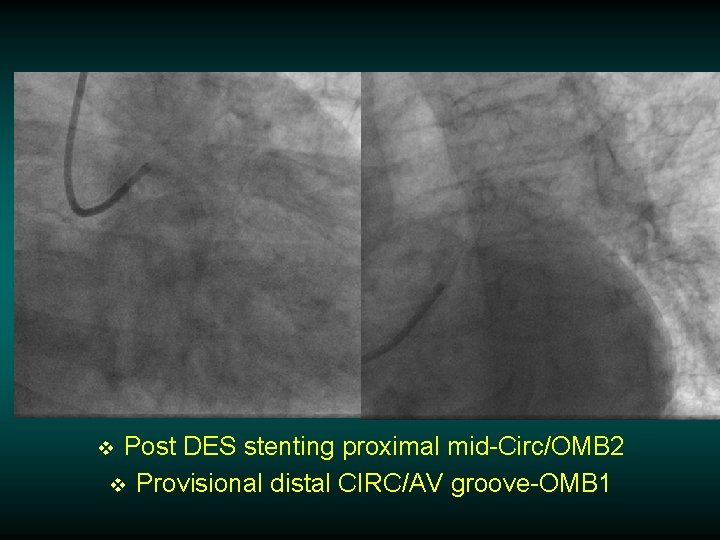
Post DES stenting proximal mid-Circ/OMB 2 v Provisional distal CIRC/AV groove-OMB 1 v
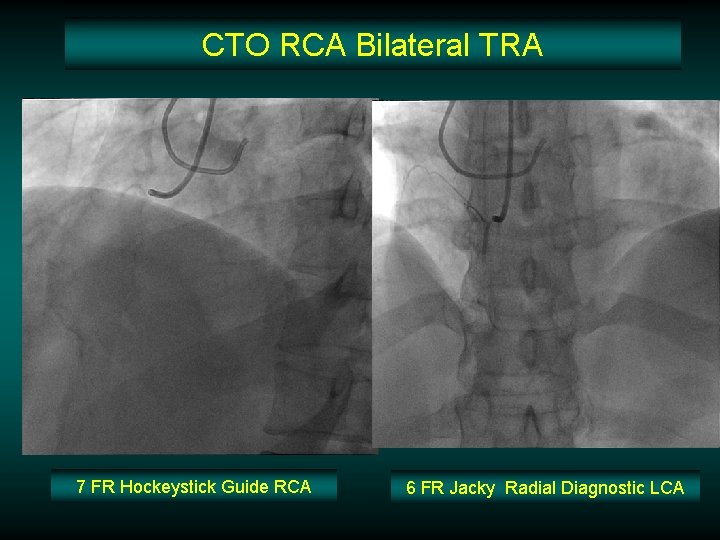
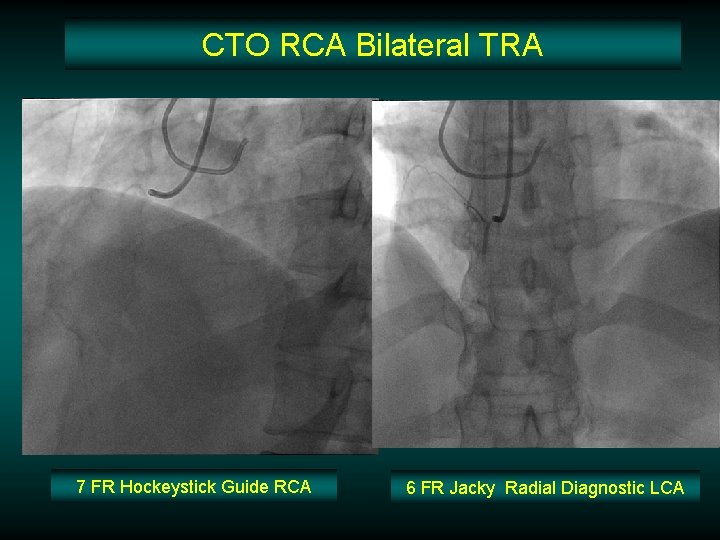
CTO RCA Bilateral TRA 7 FR Hockeystick Guide RCA 6 FR Jacky Radial Diagnostic LCA
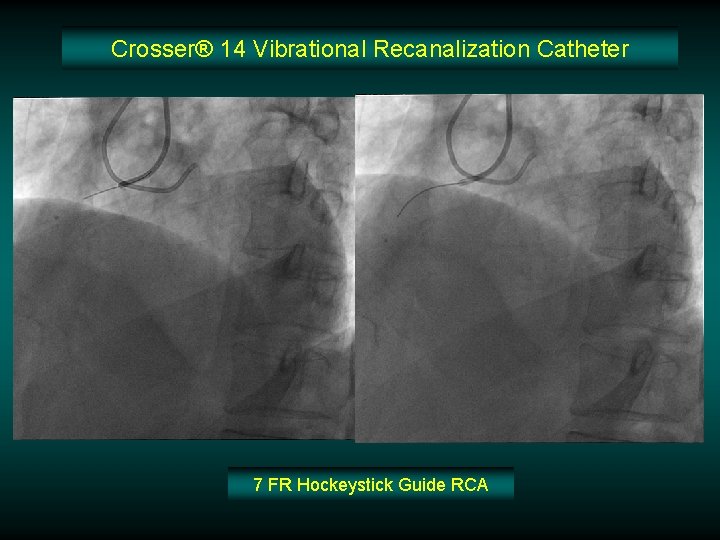
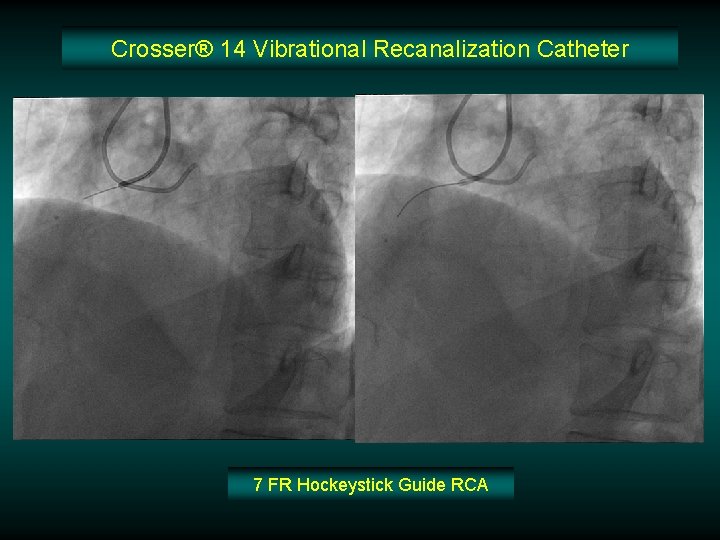
Crosser® 14 Vibrational Recanalization Catheter 7 FR Hockeystick Guide RCA
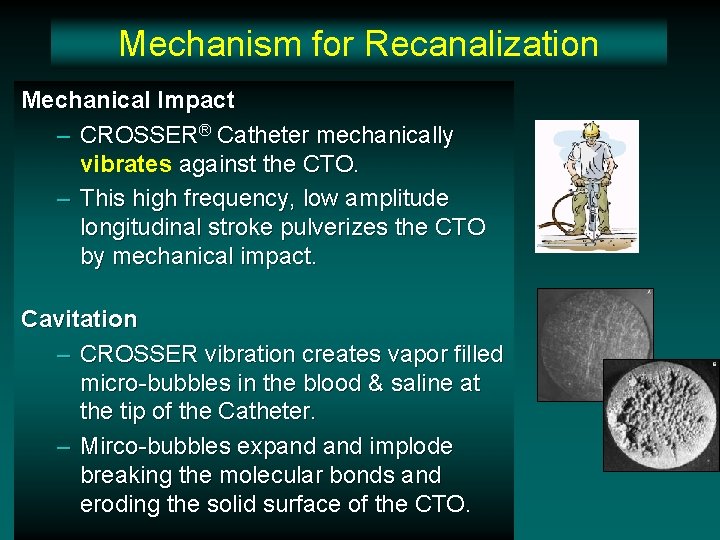
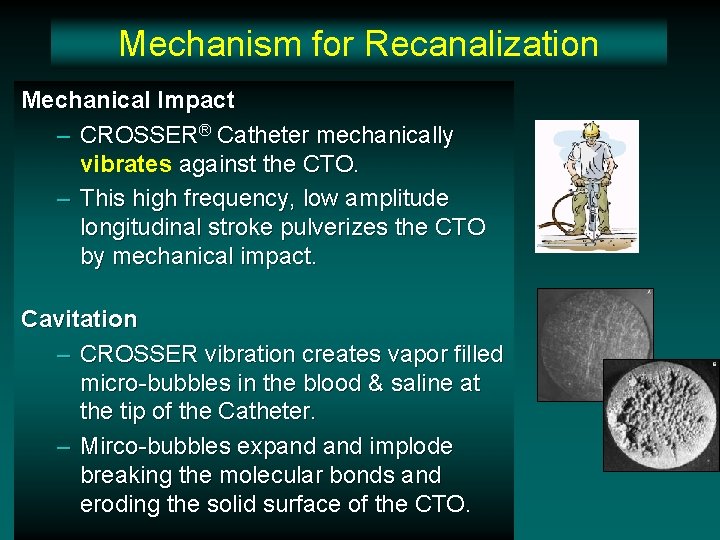
Mechanism for Recanalization Mechanical Impact – CROSSER® Catheter mechanically vibrates against the CTO. – This high frequency, low amplitude longitudinal stroke pulverizes the CTO by mechanical impact. Cavitation – CROSSER vibration creates vapor filled micro-bubbles in the blood & saline at the tip of the Catheter. – Mirco-bubbles expand implode breaking the molecular bonds and eroding the solid surface of the CTO.
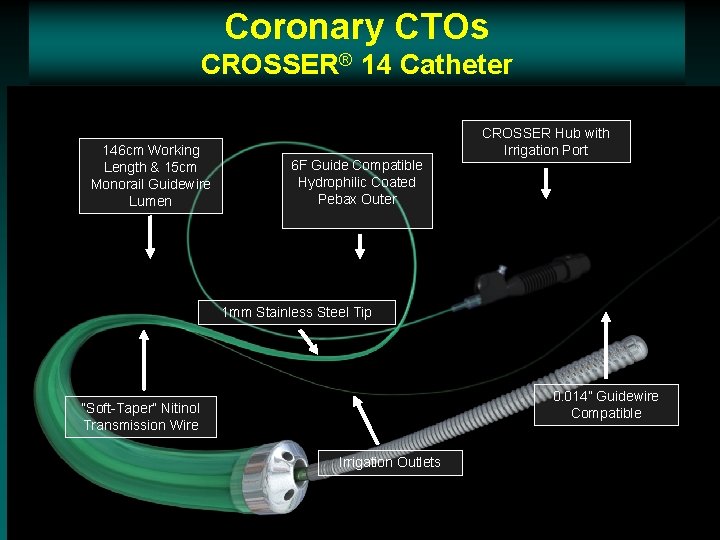
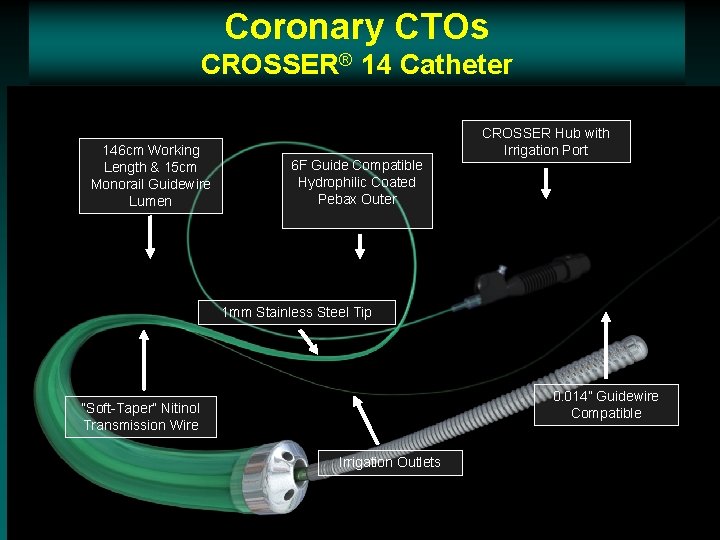
Coronary CTOs CROSSER® 14 Catheter 146 cm Working Length & 15 cm Monorail Guidewire Lumen CROSSER Hub with Irrigation Port 6 F Guide Compatible Hydrophilic Coated Pebax Outer 1 mm Stainless Steel Tip 0. 014” Guidewire Compatible “Soft-Taper” Nitinol Transmission Wire Irrigation Outlets 50
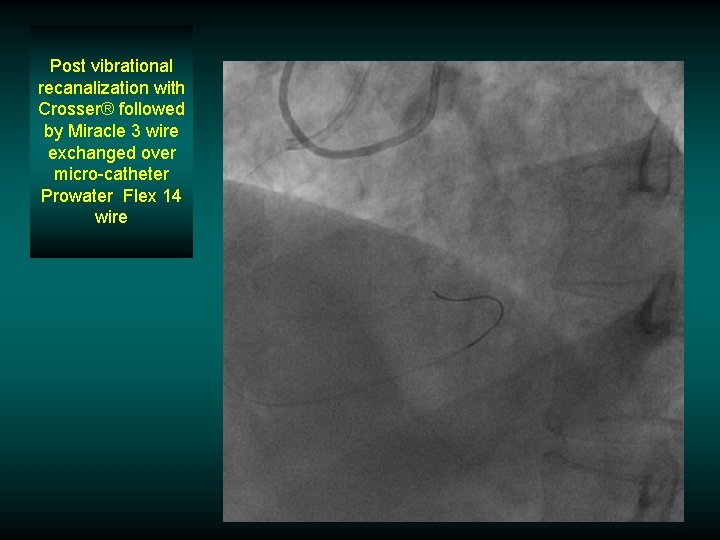
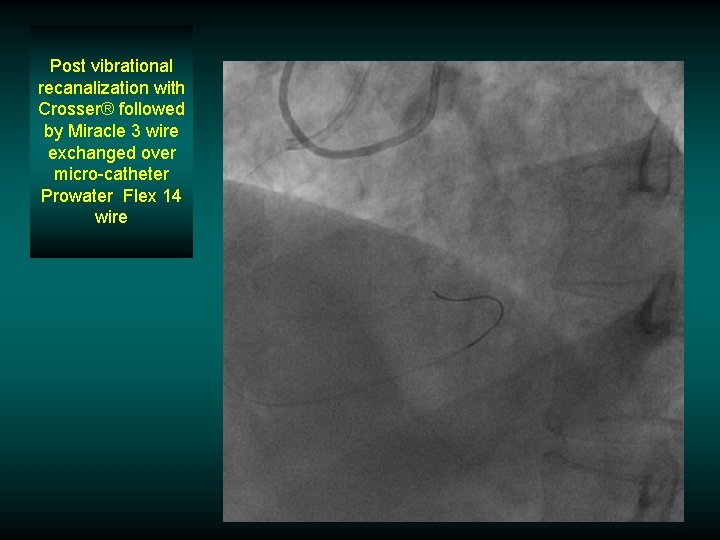
Post vibrational recanalization with Crosser® followed by Miracle 3 wire exchanged over micro-catheter Prowater Flex 14 wire
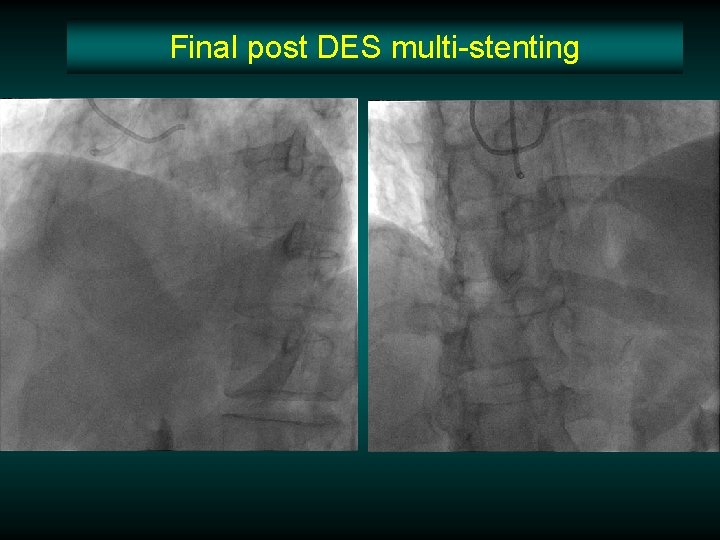
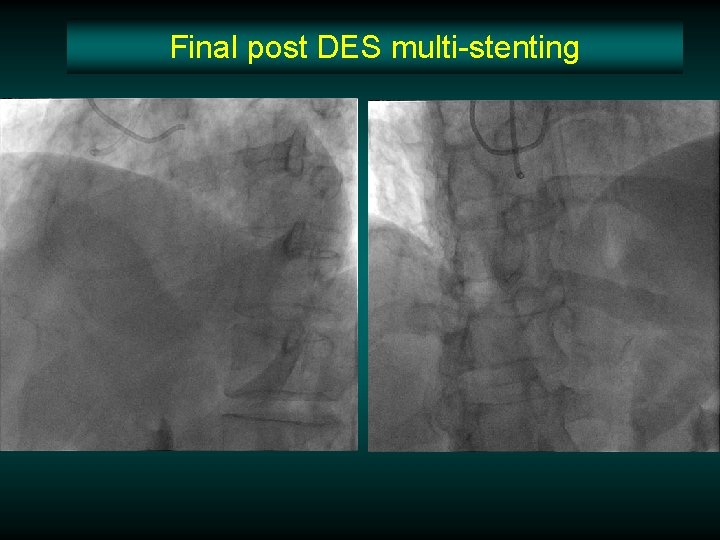
Final post DES multi-stenting
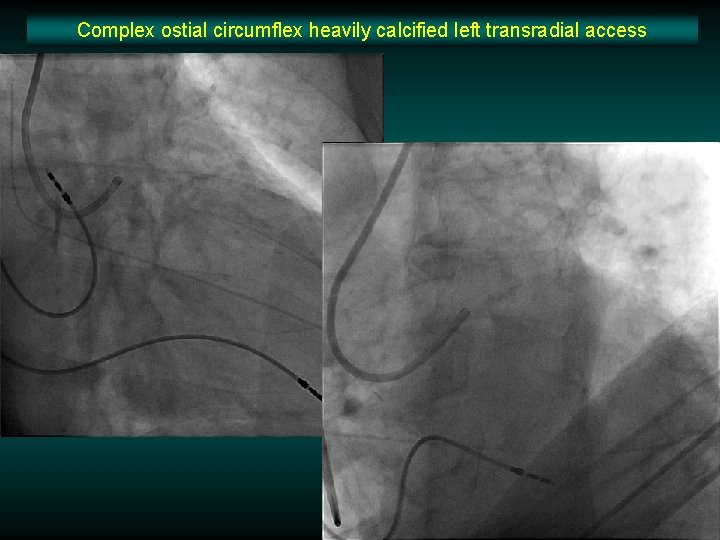
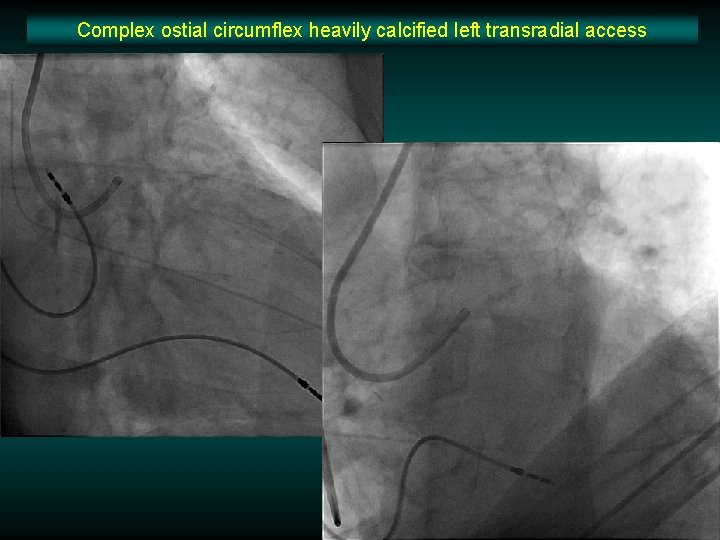
Complex ostial circumflex heavily calcified left transradial access
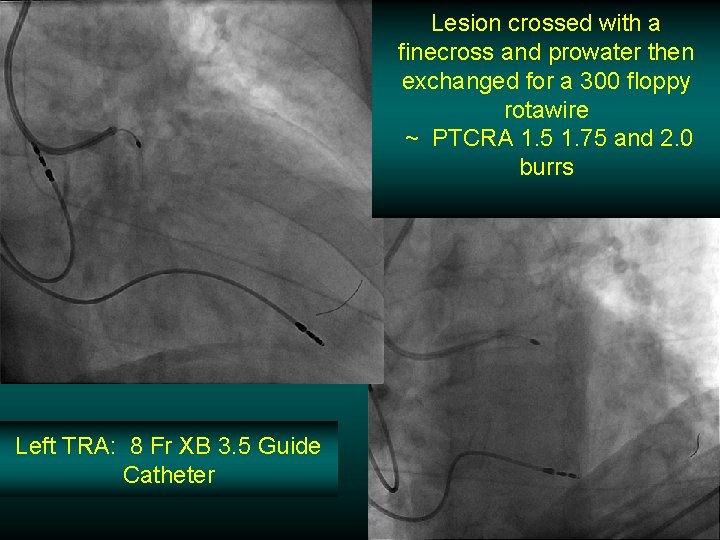
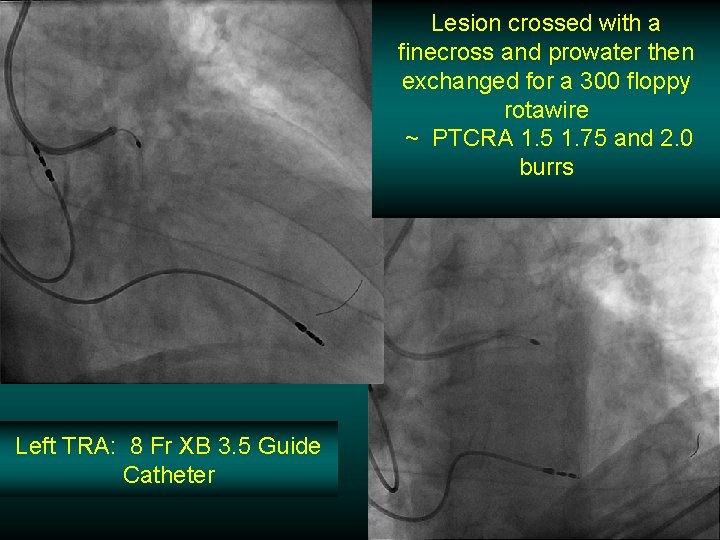
Lesion crossed with a finecross and prowater then exchanged for a 300 floppy rotawire ~ PTCRA 1. 5 1. 75 and 2. 0 burrs Left TRA: 8 Fr XB 3. 5 Guide Catheter
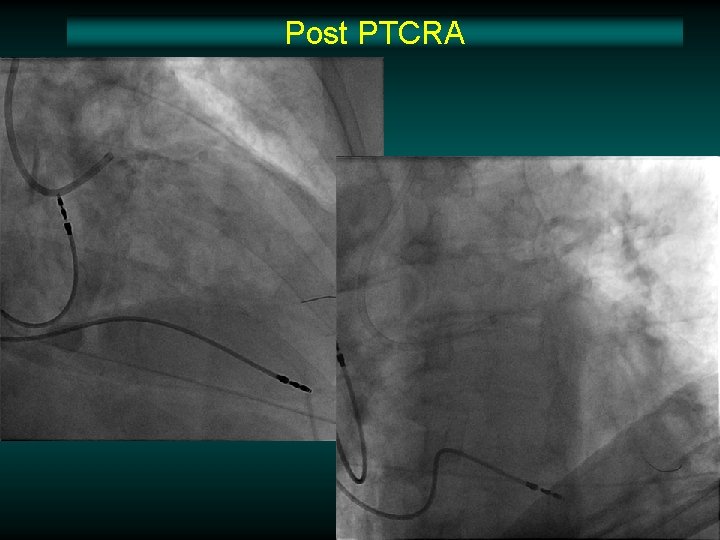
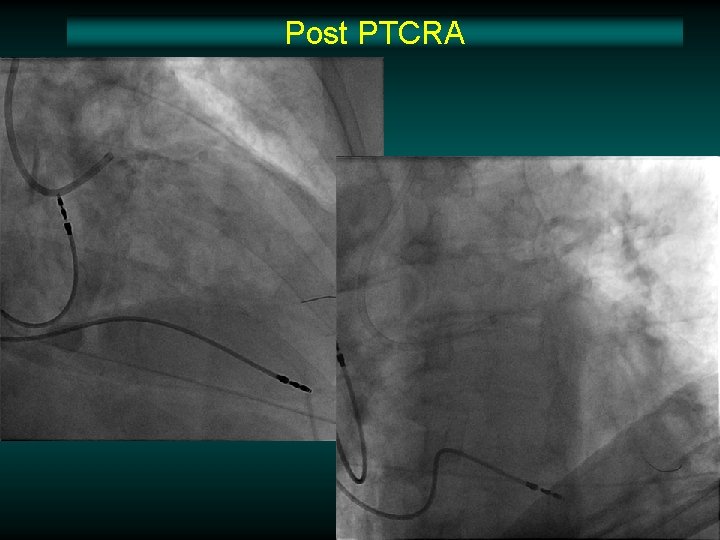
Post PTCRA
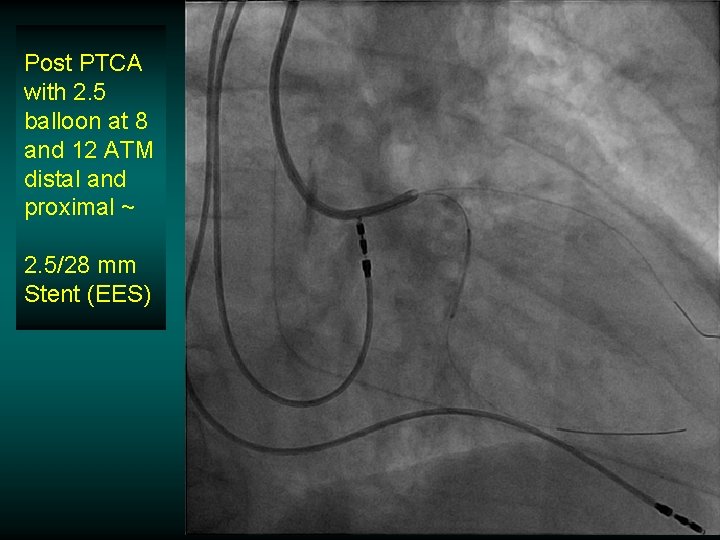
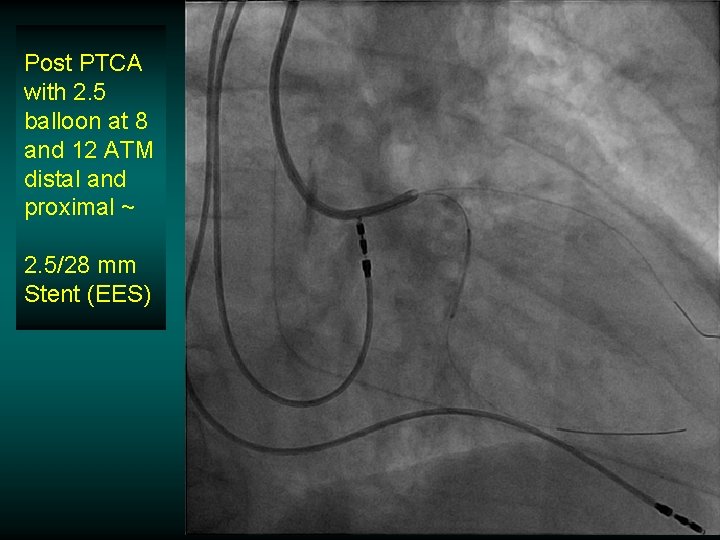
Post PTCA with 2. 5 balloon at 8 and 12 ATM distal and proximal ~ 2. 5/28 mm Stent (EES)

Overlapping stents ostial to distal CIRC 3. 0/28 mm (EES) Post dilatation 3. 5 nc balloon @ 20 ATM
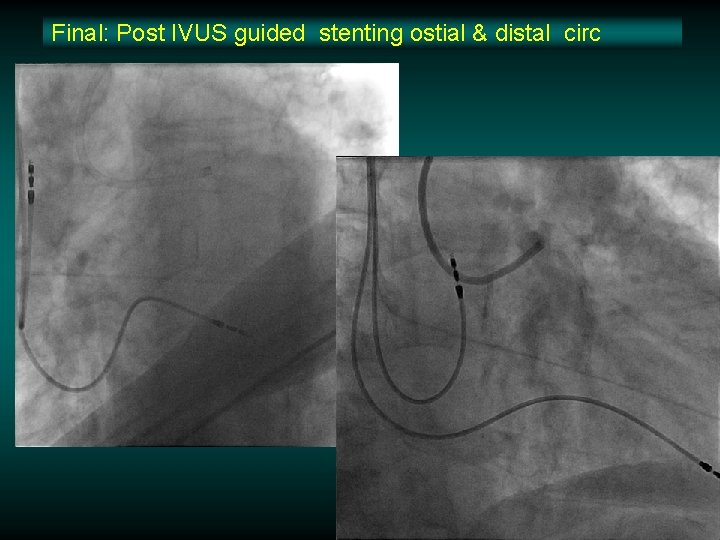
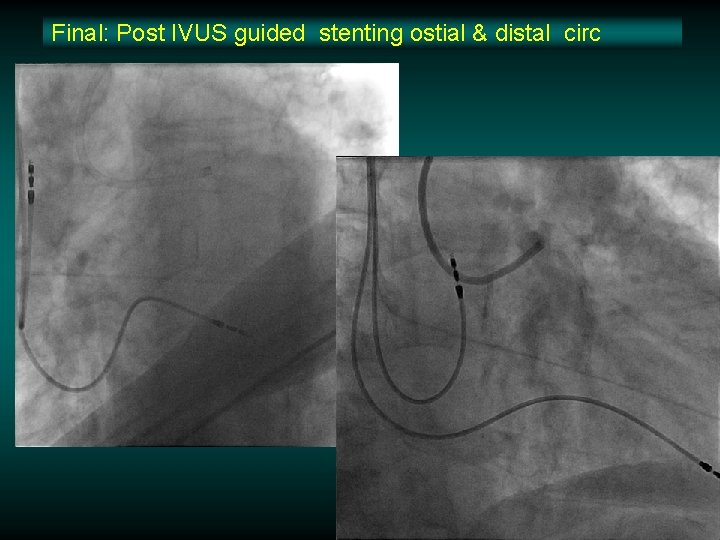
Final: Post IVUS guided stenting ostial & distal circ
Why Radial? The Advantages v Decreased incidence of major entry-site complications v Easier vascular access and hemostasis for obese patients v Decreased time to ambulation v Decreased post-procedural cost v Improved patient movement

Thank You! 60