The New Advanced Cardiac Life Support Guidelines Implementing

- Slides: 52
The New Advanced Cardiac Life Support Guidelines: Implementing with Precision and Quality! Robert W. Neumar, MD, Ph. D University of Michigan Medical School
Presenter Disclosure Information Robert W. Neumar, MD, Ph. D The New Advanced Cardiac Life Support Guidelines: Implementing with Precision and Quality! FINANCIAL DISCLOSURE: § Research Support: NIH and Physio. Control UNLABELED/UNAPPROVED USES DISCLOSURE: § Use of devices for post-cardiac arrest hypothermic targeted temperature management is not approved by FDA
http: //ECCGuidelines. heart. org
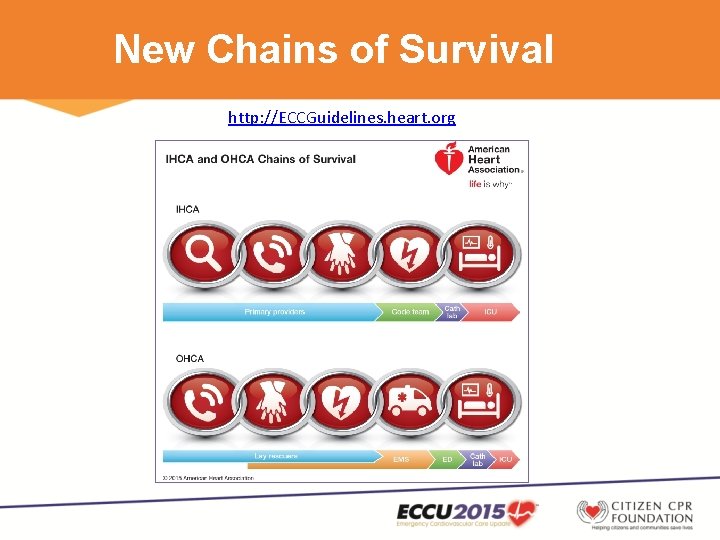
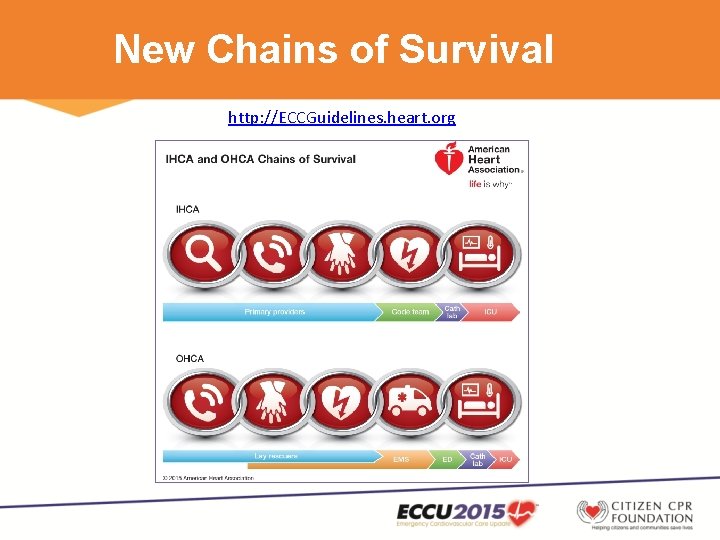
New Chains of Survival http: //ECCGuidelines. heart. org
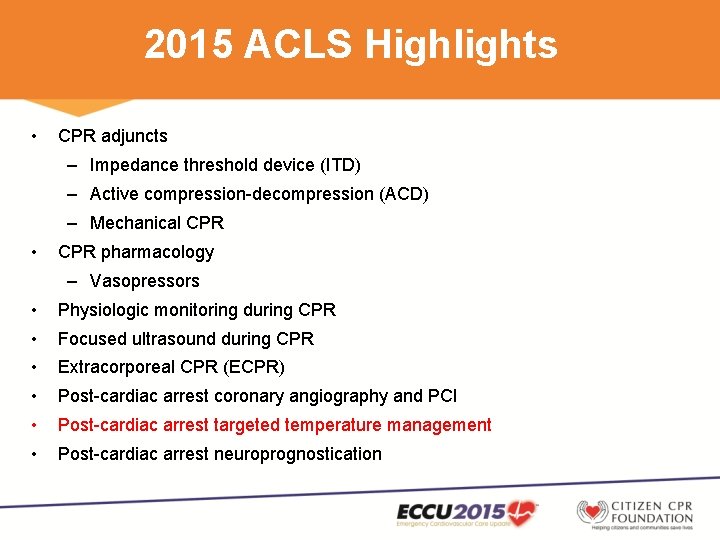
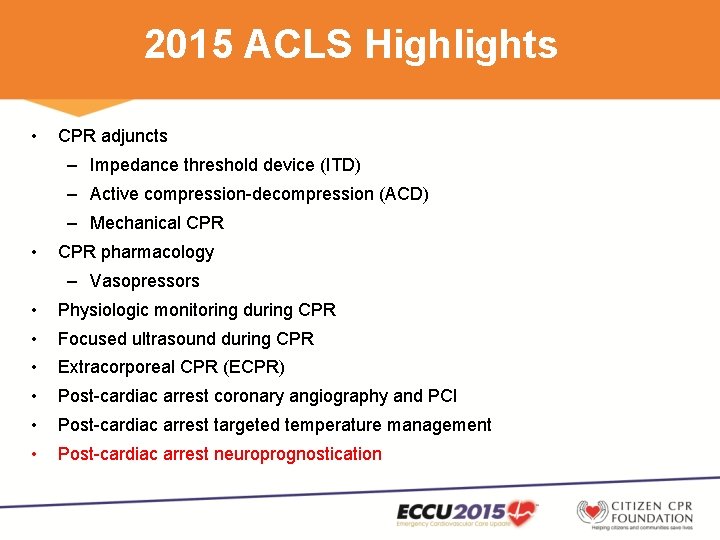
2015 ACLS Highlights • CPR adjuncts – Impedance threshold device (ITD) – Active compression-decompression (ACD) – Mechanical CPR • CPR pharmacology – Vasopressors • Physiologic monitoring during CPR • Focused ultrasound during CPR • Extracorporeal CPR (ECPR) • Post-cardiac arrest coronary angiography and PCI • Post-cardiac arrest targeted temperature management • Post-cardiac arrest neuroprognostication
2015 ACLS Highlights • CPR adjuncts – Impedance threshold device (ITD) – Active compression-decompression (ACD) – Mechanical CPR • CPR pharmacology – Vasopressors • Physiologic monitoring during CPR • Focused ultrasound during CPR • Extracorporeal CPR (ECPR) • Post-cardiac arrest coronary angiography and PCI • Post-cardiac arrest targeted temperature management • Post-cardiac arrest neuroprognostication
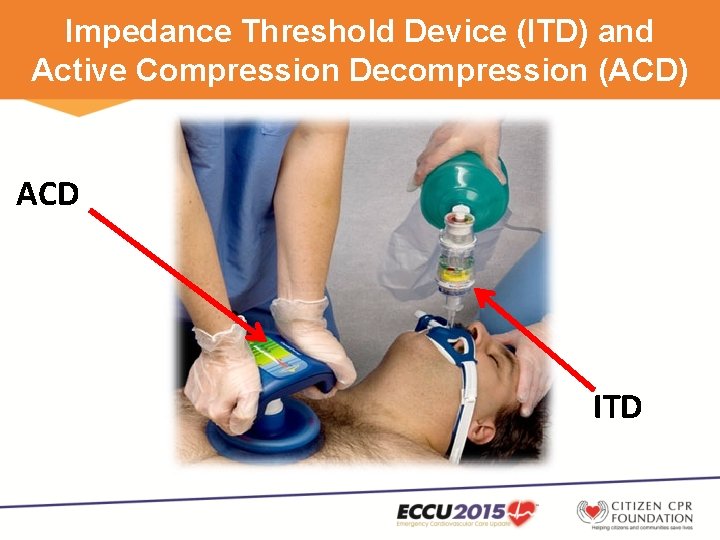
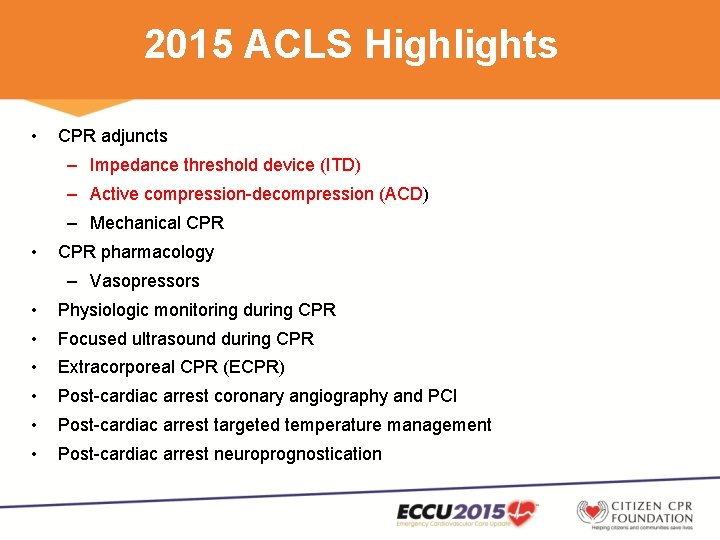
Impedance Threshold Device (ITD) and Active Compression Decompression (ACD) ACD ITD
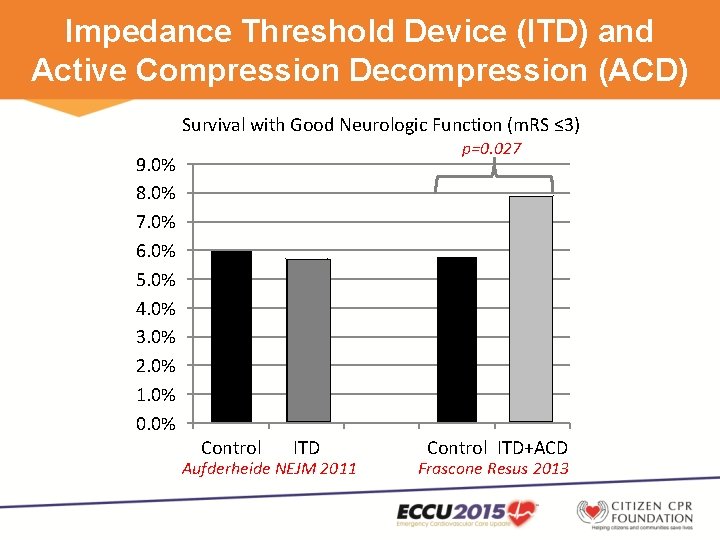
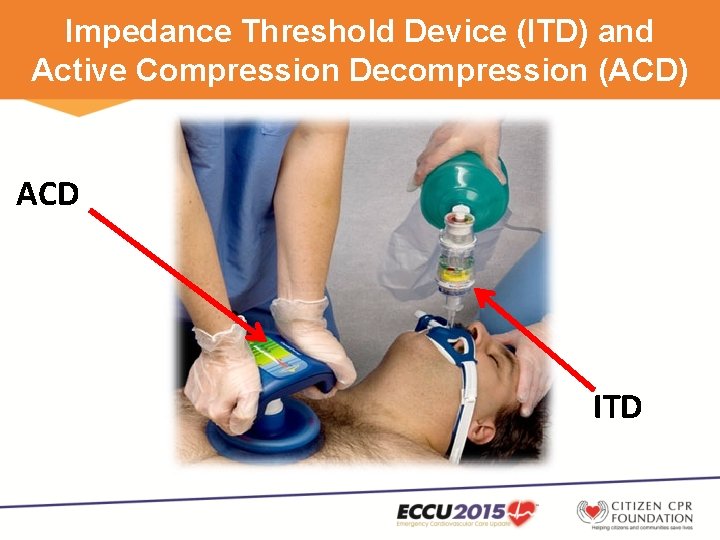
Impedance Threshold Device (ITD) and Active Compression Decompression (ACD) Survival with Good Neurologic Function (m. RS ≤ 3) p=0. 027 9. 0% 8. 0% 7. 0% 6. 0% 5. 0% 4. 0% 3. 0% 2. 0% 1. 0% 0. 0% Control ITD Aufderheide NEJM 2011 Control ITD+ACD Frascone Resus 2013
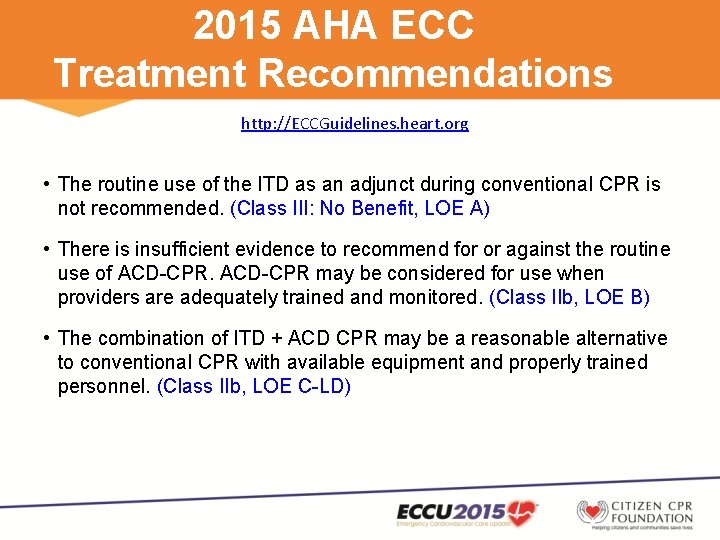
2015 AHA ECC Treatment Recommendations http: //ECCGuidelines. heart. org • The routine use of the ITD as an adjunct during conventional CPR is not recommended. (Class III: No Benefit, LOE A) • There is insufficient evidence to recommend for or against the routine use of ACD-CPR may be considered for use when providers are adequately trained and monitored. (Class IIb, LOE B) • The combination of ITD + ACD CPR may be a reasonable alternative to conventional CPR with available equipment and properly trained personnel. (Class IIb, LOE C-LD)
2015 ACLS Highlights • CPR adjuncts – Impedance threshold device (ITD) – Active compression-decompression (ACD) – Mechanical CPR • CPR pharmacology – Vasopressors • Physiologic monitoring during CPR • Focused ultrasound during CPR • Extracorporeal CPR (ECPR) • Post-cardiac arrest coronary angiography and PCI • Post-cardiac arrest targeted temperature management • Post-cardiac arrest neuroprognostication

Mechanical CPR Load Distributing Band Mechanical Piston
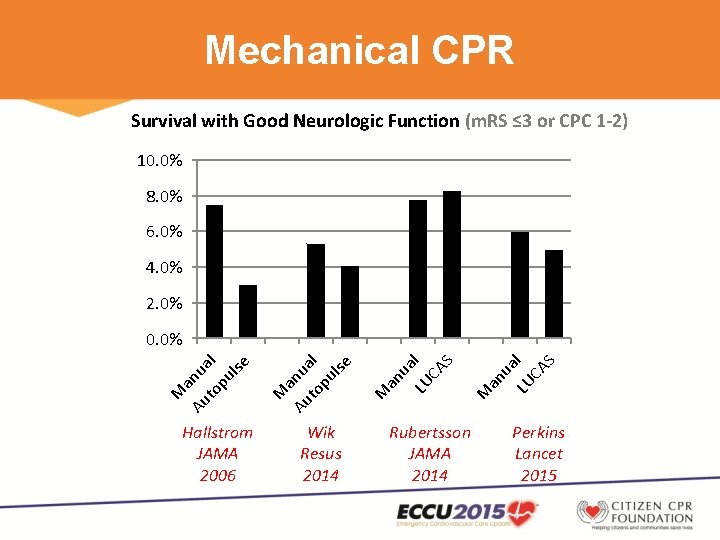
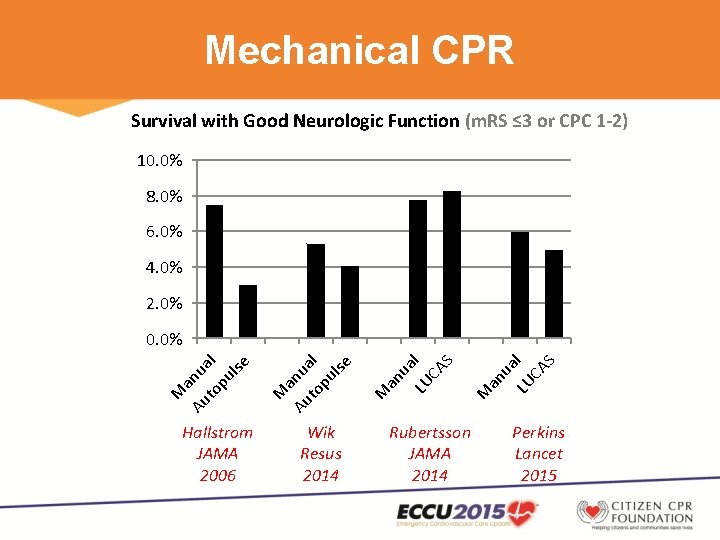
Mechanical CPR Survival with Good Neurologic Function (m. RS ≤ 3 or CPC 1 -2) 10. 0% 8. 0% 6. 0% 4. 0% 2. 0% Hallstrom JAMA 2006 Wik Resus 2014 LU l CA S M an ua LU l CA S ua an M a Au nu to al pu lse M M a Au nu to al pu lse 0. 0% Rubertsson JAMA 2014 Perkins Lancet 2015
2015 AHA ECC Treatment Recommendations http: //ECCGuidelines. heart. org • Manual chest compressions remain the standard of care for the treatment of cardiac arrest, but mechanical piston and load distributing band devices may be a reasonable alternative for use by properly trained personnel. (Class IIb, LOE B-R) • The use of mechanical piston or load distributing band devices may be considered in specific settings where the delivery of high-quality manual compressions may be challenging or dangerous for the provider (eg, limited rescuers available, prolonged CPR, during hypothermic cardiac arrest, in a moving ambulance, in the angiography suite, during preparation for extracorporeal CPR [ECPR]), provided that rescuers strictly limit interruptions in CPR during deployment and removal of the devices. (Class IIb, LOE C-EO)
2015 ACLS Highlights • CPR adjuncts – Impedance threshold device (ITD) – Active compression-decompression (ACD) – Mechanical CPR • CPR pharmacology – Vasopressors • Physiologic monitoring during CPR • Focused ultrasound during CPR • Extracorporeal CPR (ECPR) • Post-cardiac arrest coronary angiography and PCI • Post-cardiac arrest targeted temperature management • Post-cardiac arrest neuroprognostication
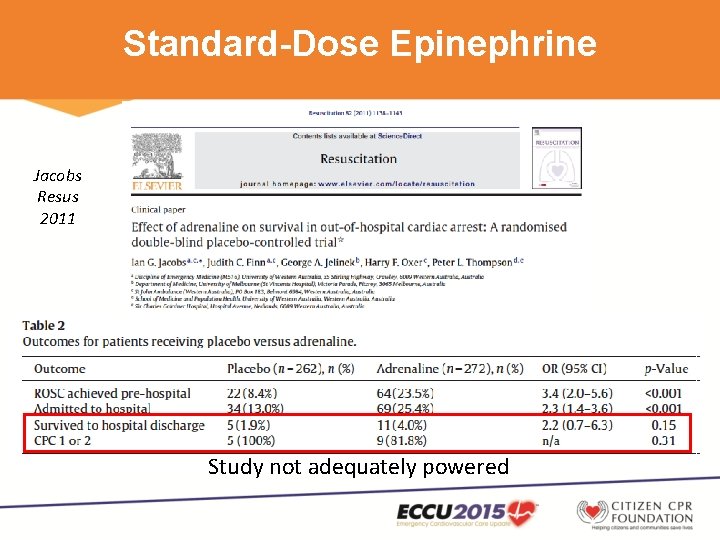
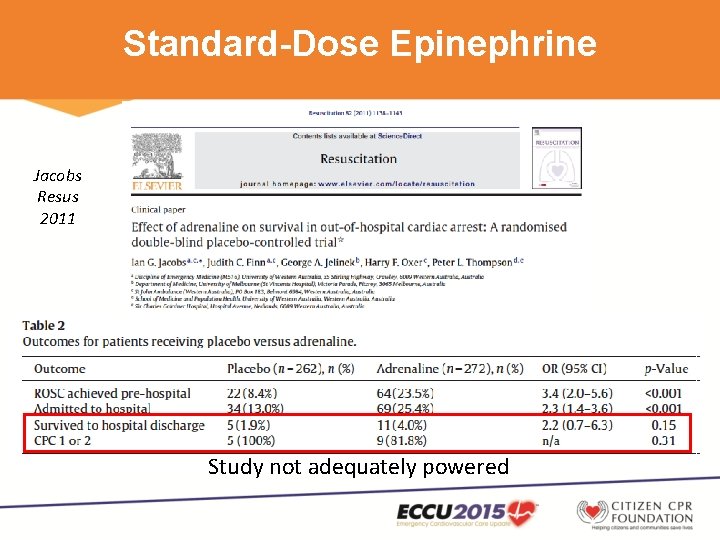
Standard-Dose Epinephrine Jacobs Resus 2011 Study not adequately powered
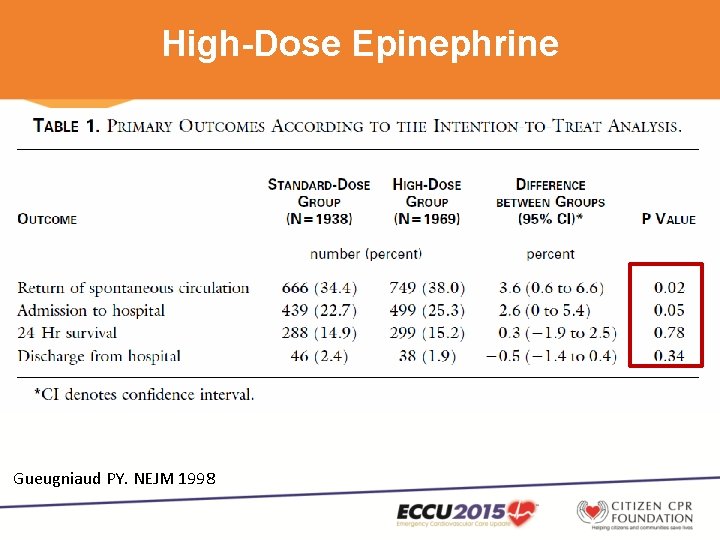
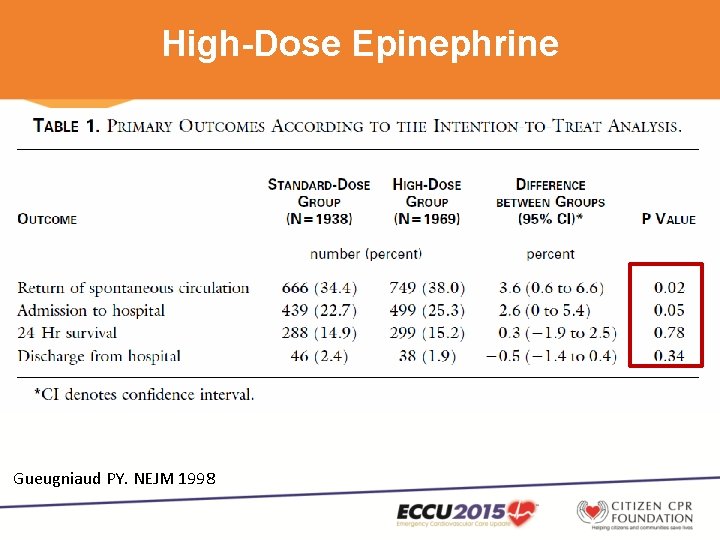
High-Dose Epinephrine Gueugniaud PY. NEJM 1998
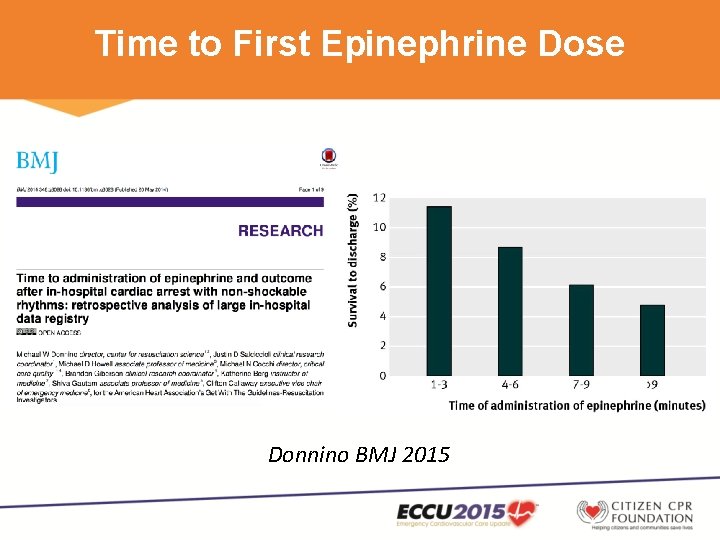
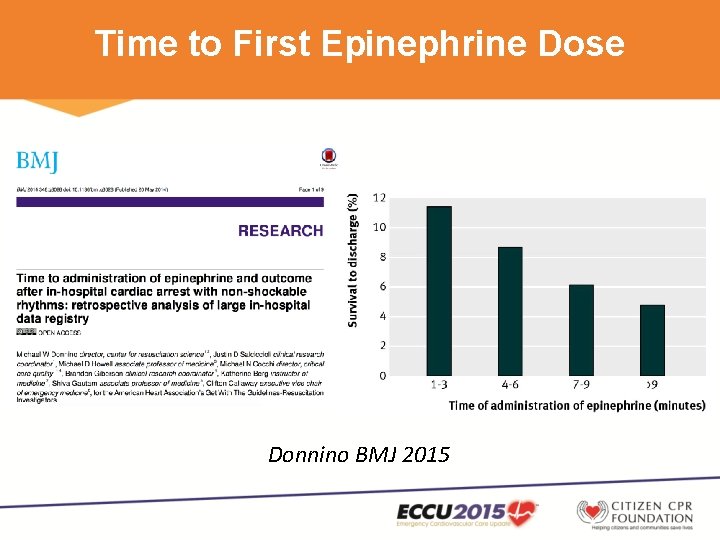
Time to First Epinephrine Dose Donnino BMJ 2015
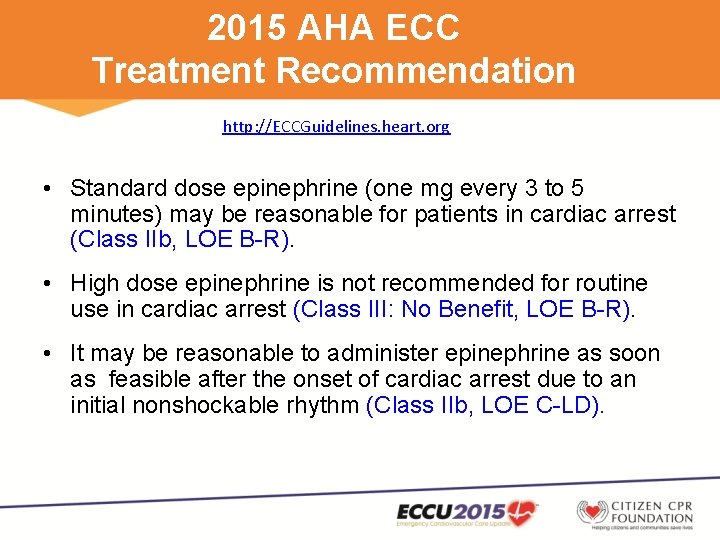
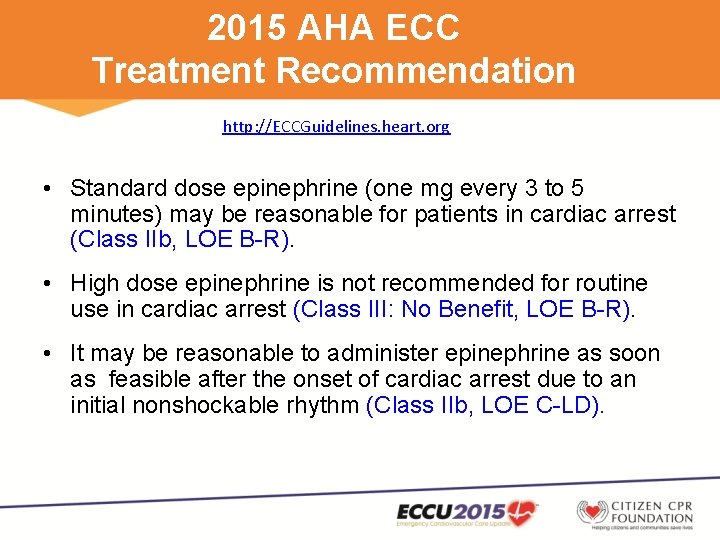
2015 AHA ECC Treatment Recommendation http: //ECCGuidelines. heart. org • Standard dose epinephrine (one mg every 3 to 5 minutes) may be reasonable for patients in cardiac arrest (Class IIb, LOE B-R). • High dose epinephrine is not recommended for routine use in cardiac arrest (Class III: No Benefit, LOE B-R). • It may be reasonable to administer epinephrine as soon as feasible after the onset of cardiac arrest due to an initial nonshockable rhythm (Class IIb, LOE C-LD).
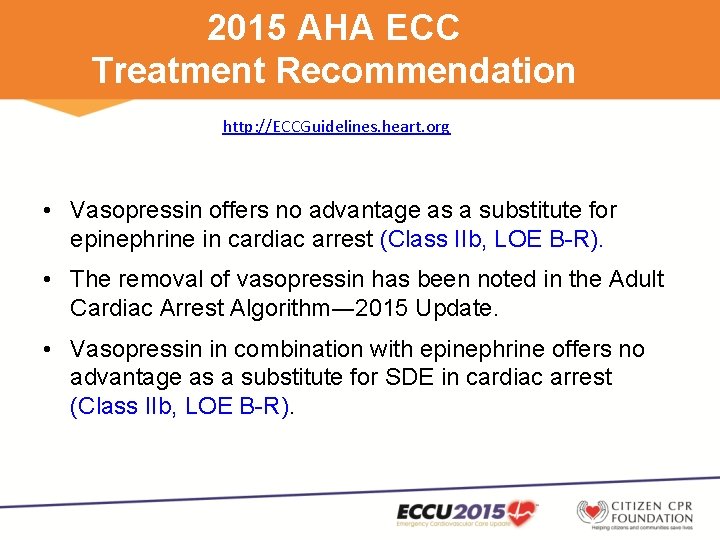
2015 AHA ECC Treatment Recommendation http: //ECCGuidelines. heart. org • Vasopressin offers no advantage as a substitute for epinephrine in cardiac arrest (Class IIb, LOE B-R). • The removal of vasopressin has been noted in the Adult Cardiac Arrest Algorithm― 2015 Update. • Vasopressin in combination with epinephrine offers no advantage as a substitute for SDE in cardiac arrest (Class IIb, LOE B-R).
2015 ACLS Highlights • CPR adjuncts – Impedance threshold device (ITD) – Active compression-decompression (ACD) – Mechanical CPR • CPR pharmacology – Vasopressors • Physiologic monitoring during CPR • Focused ultrasound during CPR • Extracorporeal CPR (ECPR) • Post-cardiac arrest coronary angiography and PCI • Post-cardiac arrest targeted temperature management • Post-cardiac arrest neuroprognostication
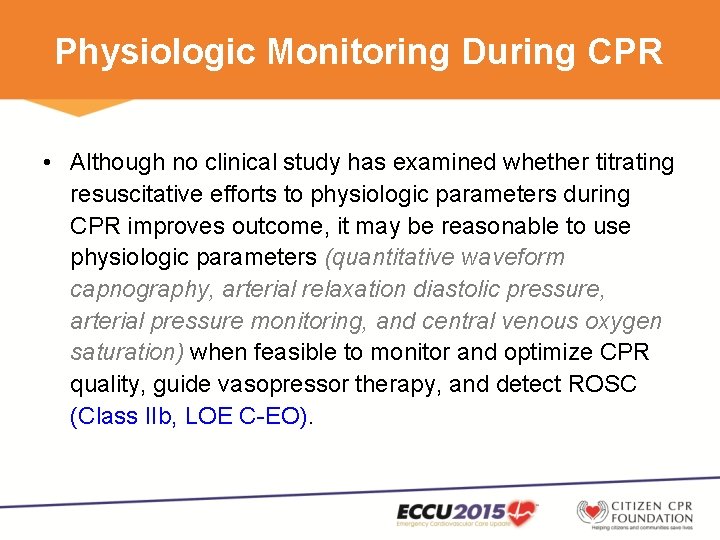
Physiologic Monitoring During CPR • Although no clinical study has examined whether titrating resuscitative efforts to physiologic parameters during CPR improves outcome, it may be reasonable to use physiologic parameters (quantitative waveform capnography, arterial relaxation diastolic pressure, arterial pressure monitoring, and central venous oxygen saturation) when feasible to monitor and optimize CPR quality, guide vasopressor therapy, and detect ROSC (Class IIb, LOE C-EO).
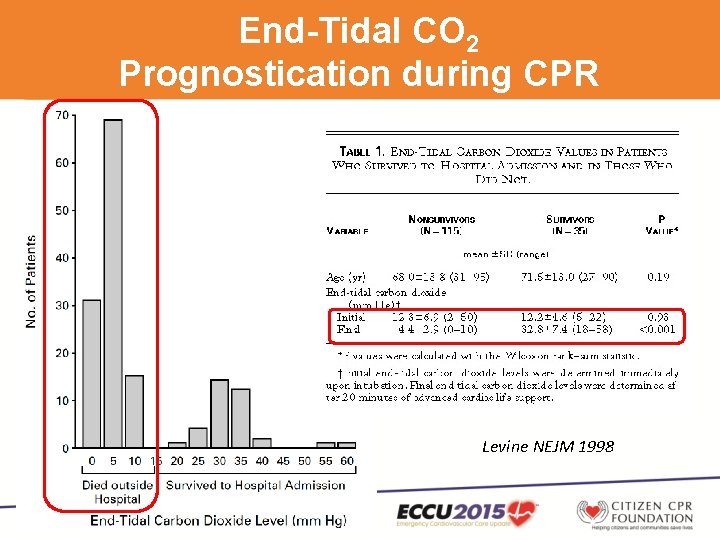
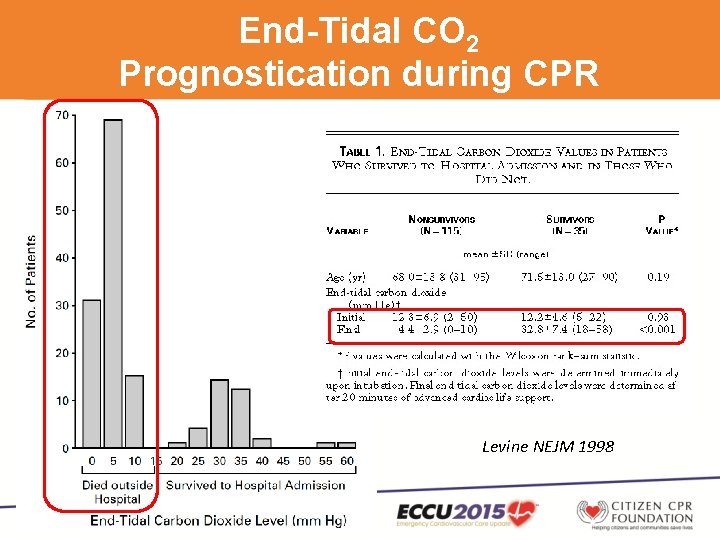
End-Tidal CO 2 Prognostication during CPR Levine NEJM 1998
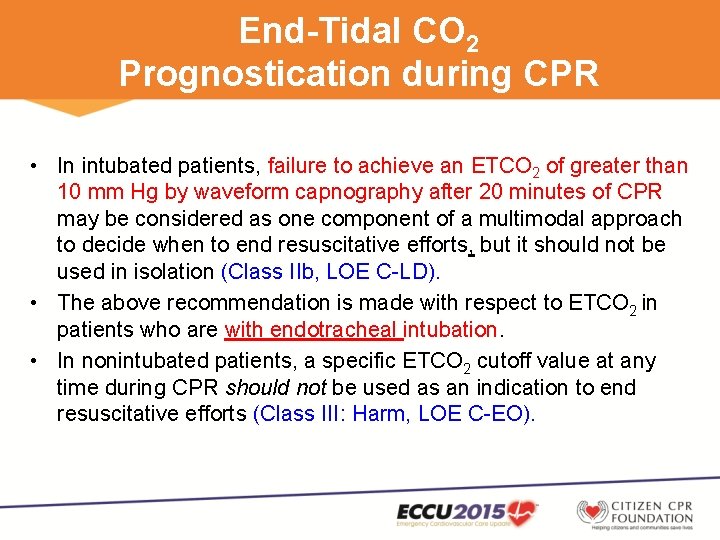
End-Tidal CO 2 Prognostication during CPR • In intubated patients, failure to achieve an ETCO 2 of greater than 10 mm Hg by waveform capnography after 20 minutes of CPR may be considered as one component of a multimodal approach to decide when to end resuscitative efforts, but it should not be used in isolation (Class IIb, LOE C-LD). • The above recommendation is made with respect to ETCO 2 in patients who are with endotracheal intubation. • In nonintubated patients, a specific ETCO 2 cutoff value at any time during CPR should not be used as an indication to end resuscitative efforts (Class III: Harm, LOE C-EO).
2015 ACLS Highlights • CPR adjuncts – Impedance threshold device (ITD) – Active compression-decompression (ACD) – Mechanical CPR • CPR pharmacology – Vasopressors • Physiologic monitoring during CPR • Focused ultrasound during CPR • Extracorporeal CPR (ECPR) • Post-cardiac arrest coronary angiography and PCI • Post-cardiac arrest targeted temperature management • Post-cardiac arrest neuroprognostication
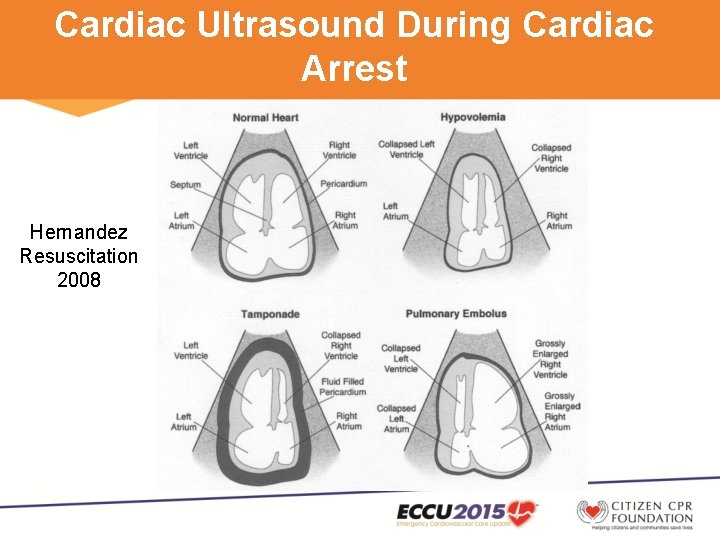
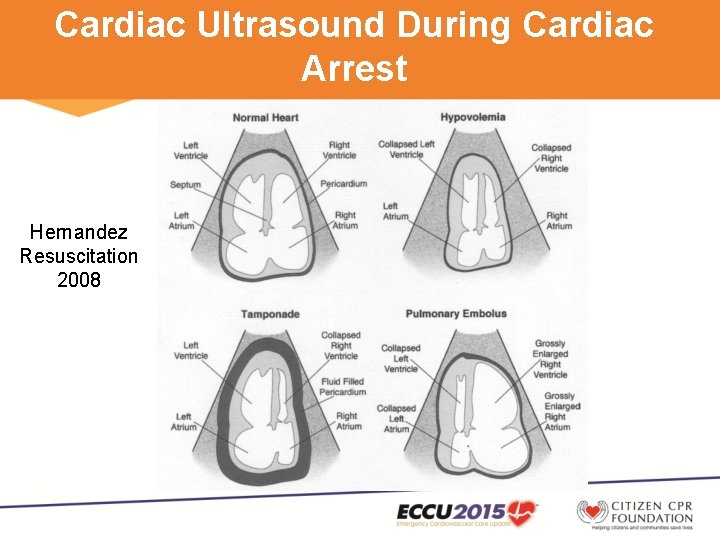
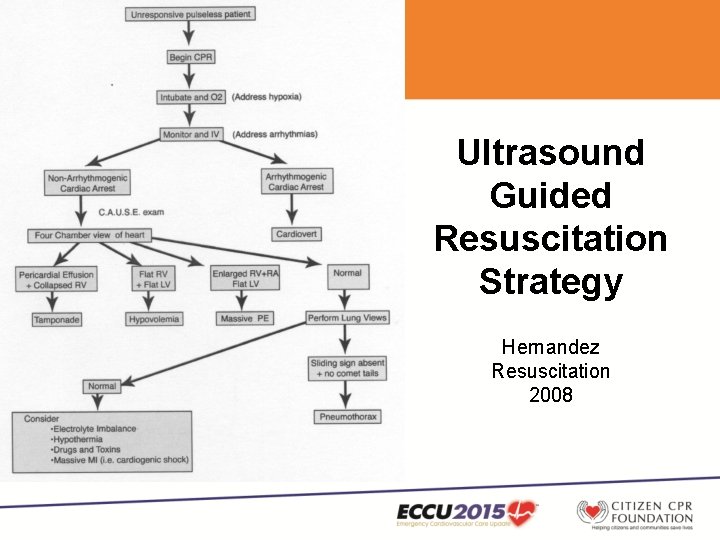
Cardiac Ultrasound During Cardiac Arrest Hernandez Resuscitation 2008
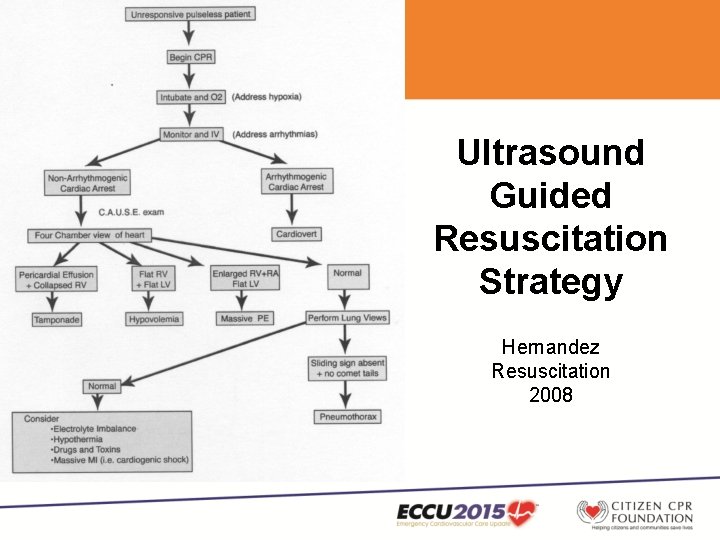
Ultrasound Guided Resuscitation Strategy Hernandez Resuscitation 2008
2015 AHA ECC Treatment Recommendation http: //ECCGuidelines. heart. org • Ultrasound (cardiac or noncardiac) may be considered during the management of cardiac arrest, although its usefulness has not been well established (Class IIb, LOE C-EO). • If a qualified sonographer is present and use of ultrasound does not interfere with the standard cardiac arrest treatment protocol, then ultrasound may be considered as an adjunct to standard patient evaluation (Class IIb, LOE C-EO).
2015 ACLS Highlights • CPR adjuncts – Impedance threshold device (ITD) – Active compression-decompression (ACD) – Mechanical CPR • CPR pharmacology – Vasopressors • Physiologic monitoring during CPR • Focused ultrasound during CPR • Extracorporeal CPR (ECPR) • Post-cardiac arrest coronary angiography and PCI • Post-cardiac arrest targeted temperature management • Post-cardiac arrest neuroprognostication
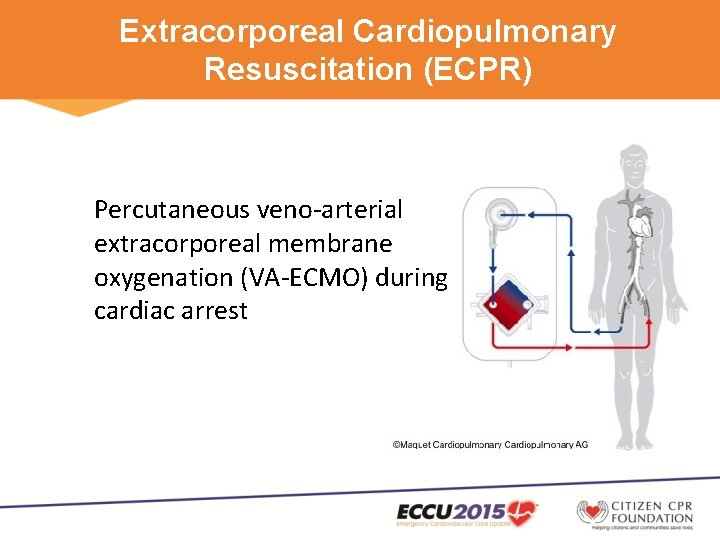
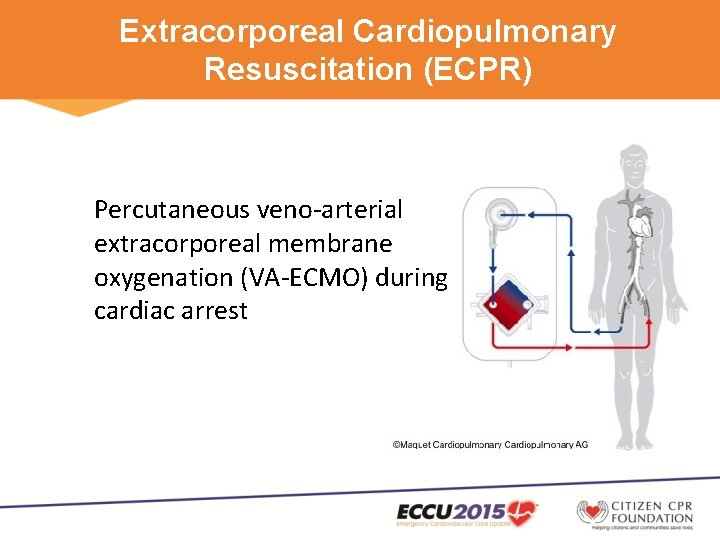
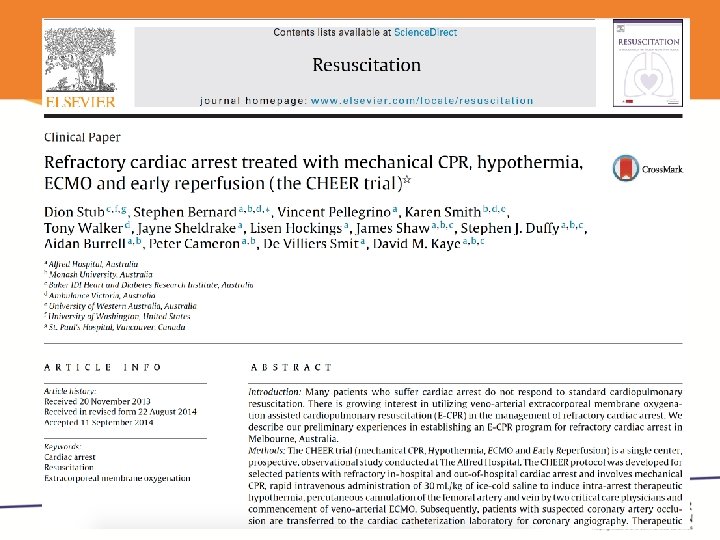
Extracorporeal Cardiopulmonary Resuscitation (ECPR) Percutaneous veno-arterial extracorporeal membrane oxygenation (VA-ECMO) during cardiac arrest
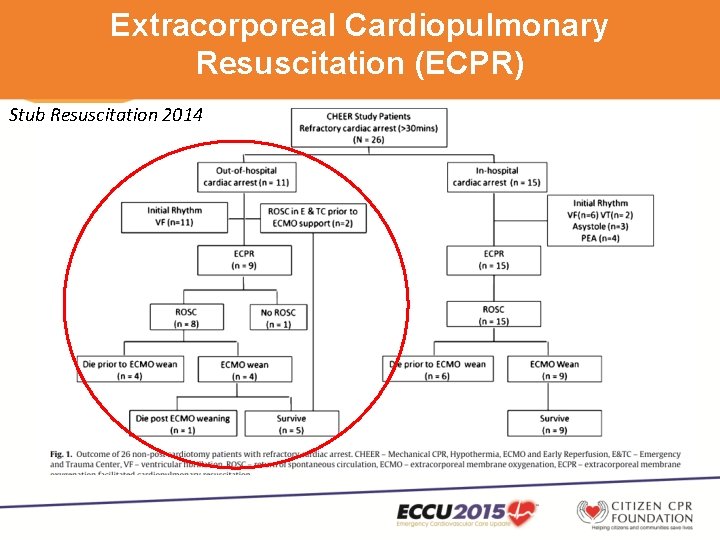
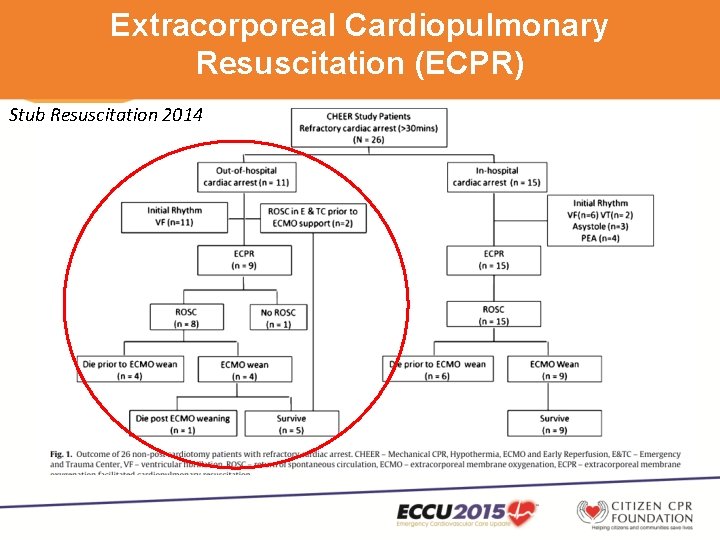
Extracorporeal Cardiopulmonary Resuscitation (ECPR) Stub Resuscitation 2014
2015 AHA ECC Treatment Recommendation http: //ECCGuidelines. heart. org • There is insufficient evidence to recommend the routine use of ECPR for patients with cardiac arrest. • In settings where it can be rapidly implemented, ECPR may be considered for select patients for whom the suspected etiology of the cardiac arrest is potentially reversible during a limited period of mechanical cardiorespiratory support. (Class IIb, LOE C-LD)
2015 ACLS Highlights • CPR adjuncts – Impedance threshold device (ITD) – Active compression-decompression (ACD) – Mechanical CPR • CPR pharmacology – Vasopressors • Physiologic monitoring during CPR • Focused ultrasound during CPR • Extracorporeal CPR (ECPR) • Post-cardiac arrest coronary angiography and PCI • Post-cardiac arrest targeted temperature management • Post-cardiac arrest neuroprognostication
2015 AHA ECC Treatment Recommendation http: //ECCGuidelines. heart. org • Coronary angiography should be performed emergently (rather than later in the hospital stay or not at all) for OHCA patients with suspected cardiac etiology of arrest and ST elevation on ECG (Class I, LOE B-NR). • Consistent with all other STEMI care • Neurological outcomes are unknowable at time of decision • Many observational studies showing high rates of good outcome after PCI, and association of successful PCI with better outcomes
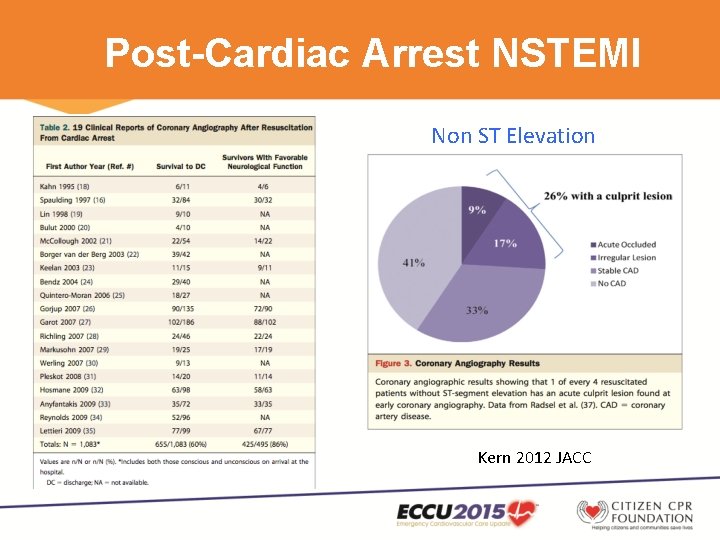
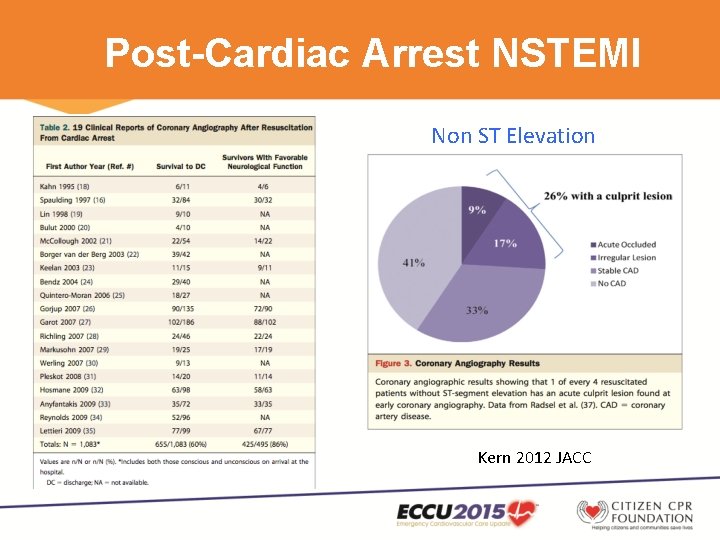
Post-Cardiac Arrest NSTEMI Non ST Elevation Kern 2012 JACC
Post-Cardiac Arrest NSTEMI Dumas, Cardiovasc Interv, 2010
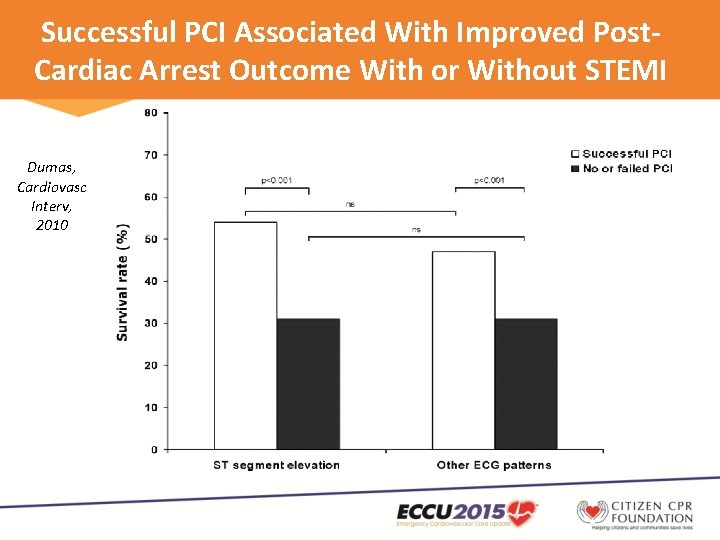
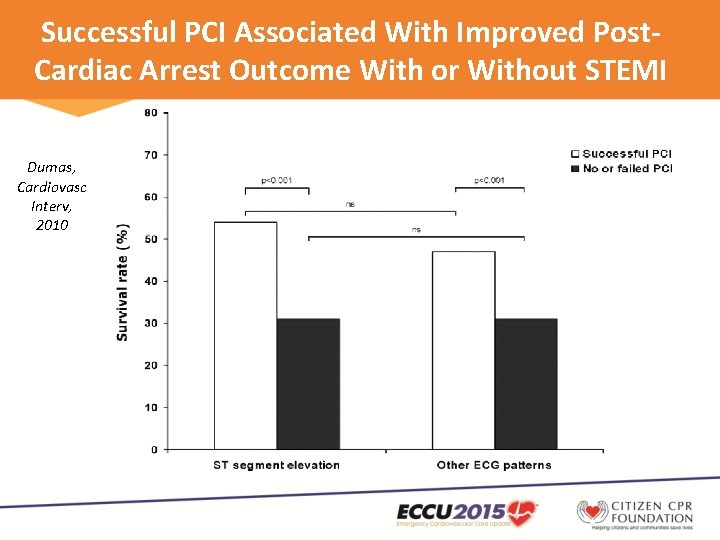
Successful PCI Associated With Improved Post. Cardiac Arrest Outcome With or Without STEMI Dumas, Cardiovasc Interv, 2010
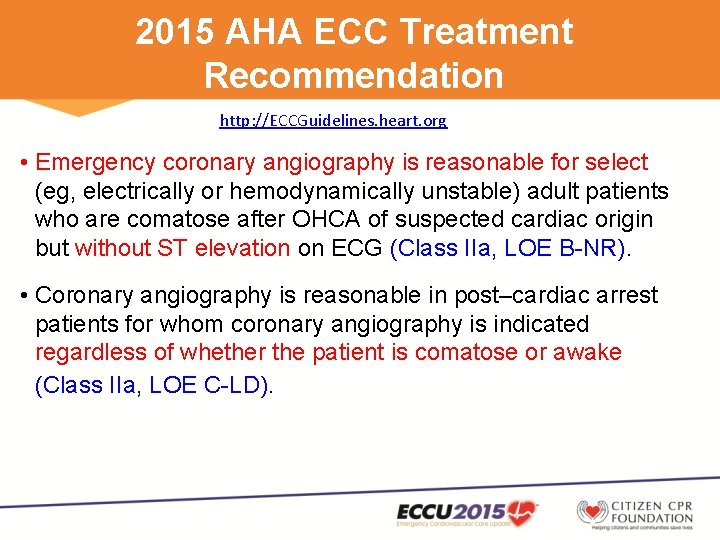
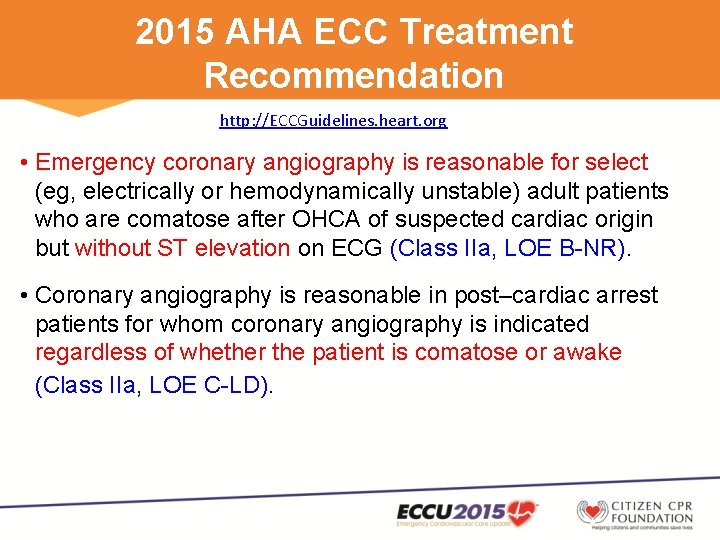
2015 AHA ECC Treatment Recommendation http: //ECCGuidelines. heart. org • Emergency coronary angiography is reasonable for select (eg, electrically or hemodynamically unstable) adult patients who are comatose after OHCA of suspected cardiac origin but without ST elevation on ECG (Class IIa, LOE B-NR). • Coronary angiography is reasonable in post–cardiac arrest patients for whom coronary angiography is indicated regardless of whether the patient is comatose or awake (Class IIa, LOE C-LD).
2015 ACLS Highlights • CPR adjuncts – Impedance threshold device (ITD) – Active compression-decompression (ACD) – Mechanical CPR • CPR pharmacology – Vasopressors • Physiologic monitoring during CPR • Focused ultrasound during CPR • Extracorporeal CPR (ECPR) • Post-cardiac arrest coronary angiography and PCI • Post-cardiac arrest targeted temperature management • Post-cardiac arrest neuroprognostication
Optimizing Therapeutic Hypothermia • How cold? • How soon? • How long? • Rewarming rate?
Optimizing Therapeutic Hypothermia • How cold? • How soon? • How long? • Rewarming rate?
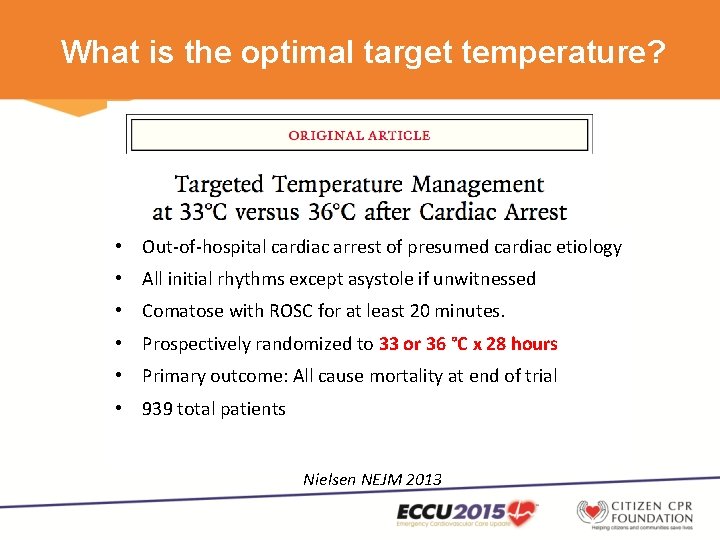
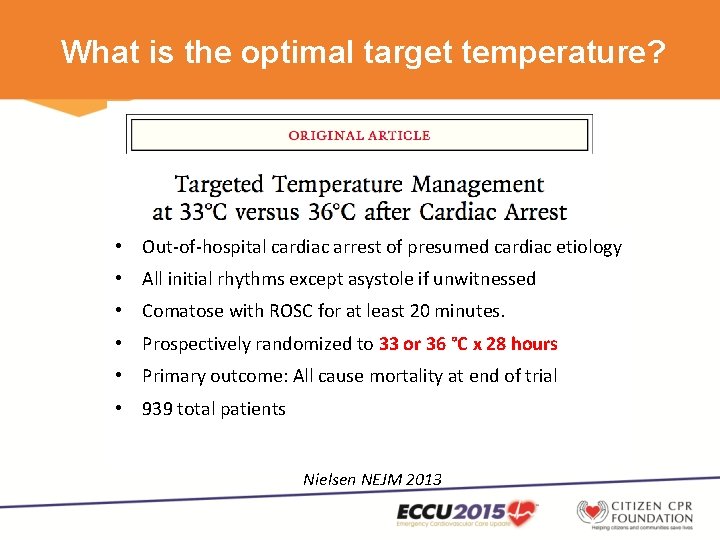
What is the optimal target temperature? • Out-of-hospital cardiac arrest of presumed cardiac etiology • All initial rhythms except asystole if unwitnessed • Comatose with ROSC for at least 20 minutes. • Prospectively randomized to 33 or 36 °C x 28 hours • Primary outcome: All cause mortality at end of trial • 939 total patients Nielsen NEJM 2013
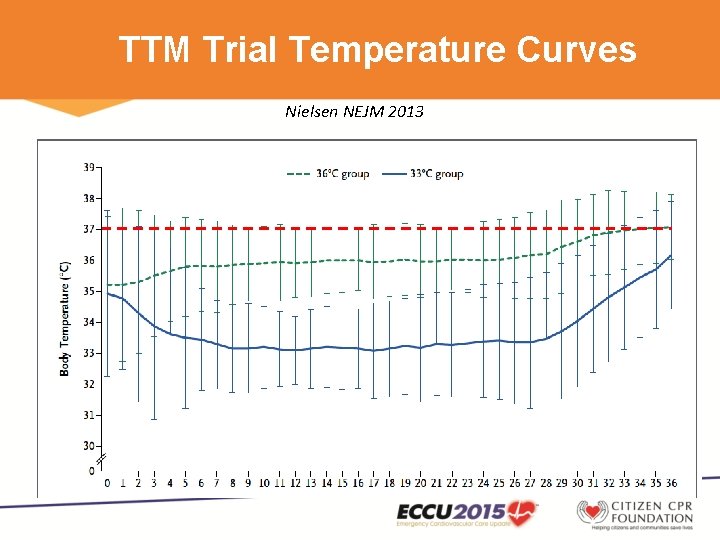
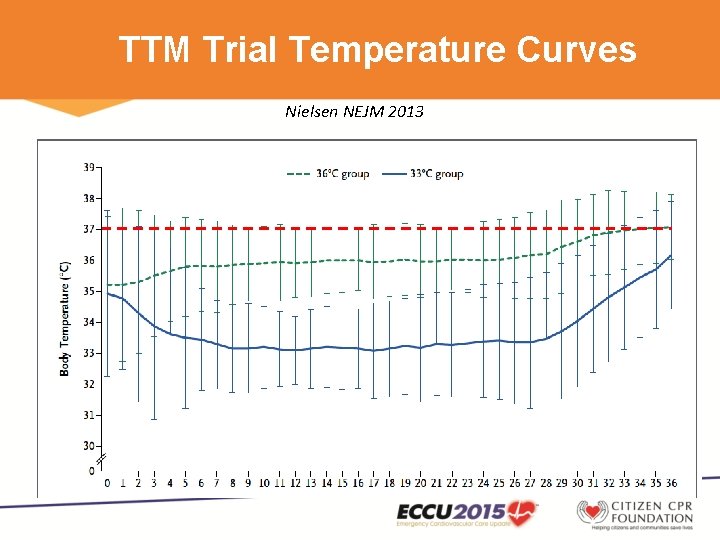
TTM Trial Temperature Curves Nielsen NEJM 2013
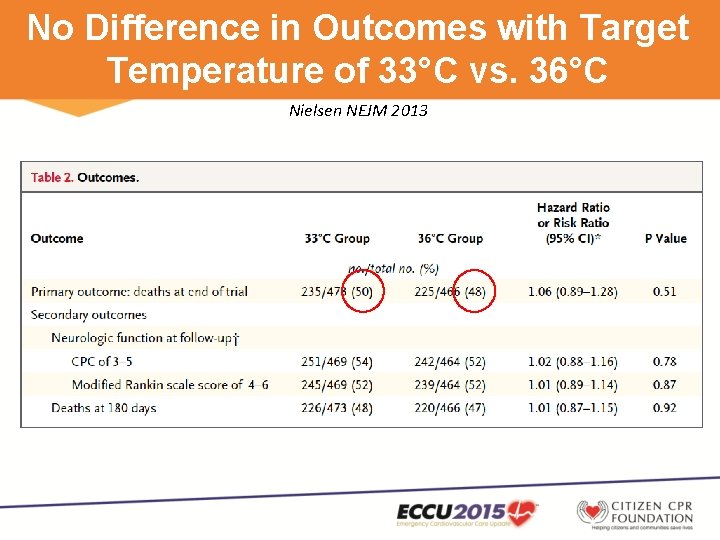
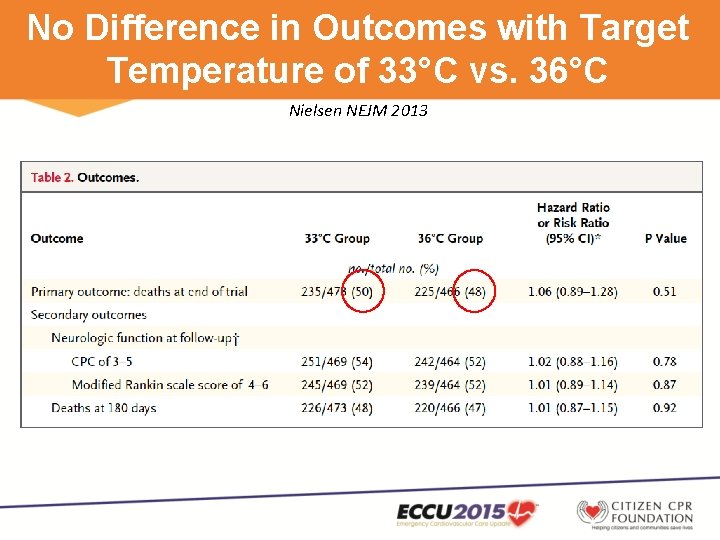
No Difference in Outcomes with Target Temperature of 33°C vs. 36°C Nielsen NEJM 2013
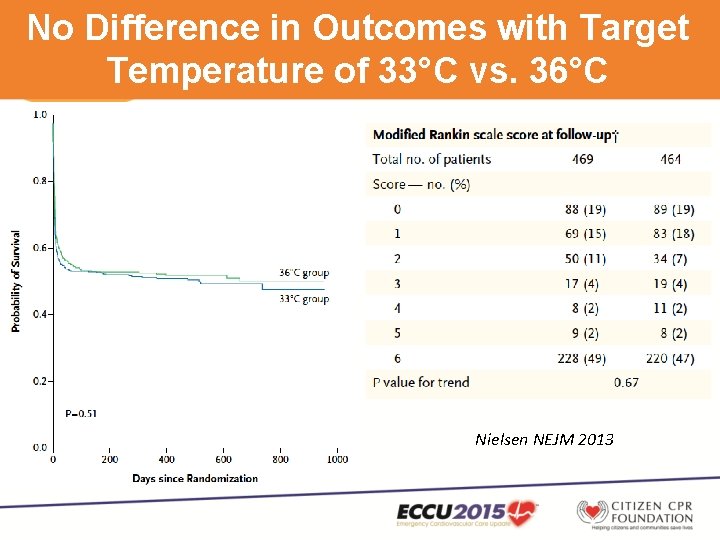
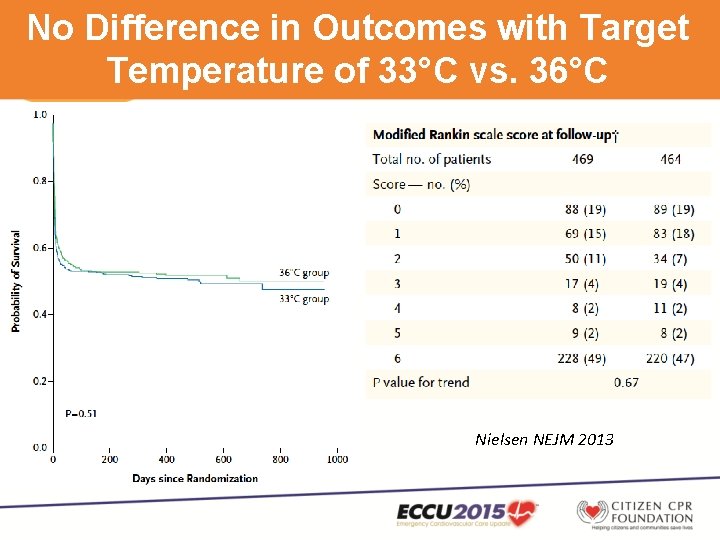
No Difference in Outcomes with Target Temperature of 33°C vs. 36°C Nielsen NEJM 2013
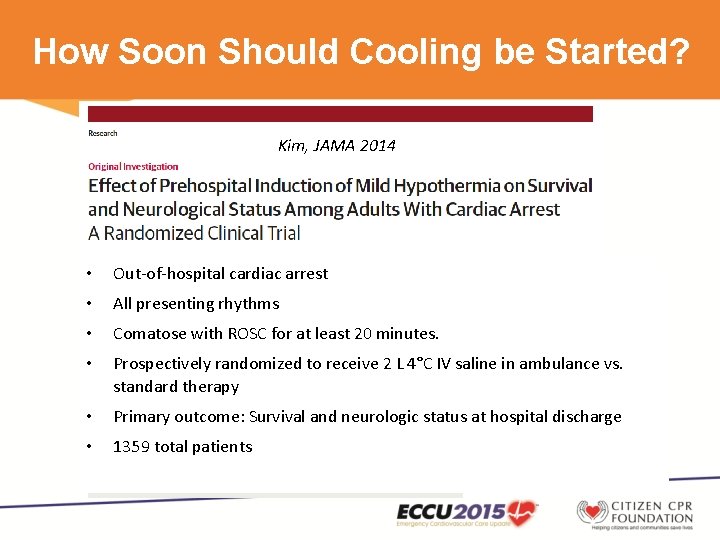
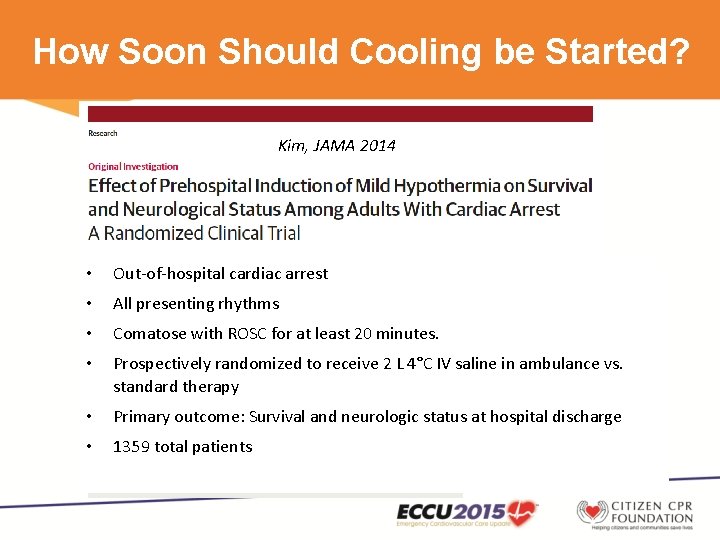
How Soon Should Cooling be Started? Kim, JAMA 2014 • Out-of-hospital cardiac arrest • All presenting rhythms • Comatose with ROSC for at least 20 minutes. • Prospectively randomized to receive 2 L 4°C IV saline in ambulance vs. standard therapy • Primary outcome: Survival and neurologic status at hospital discharge • 1359 total patients
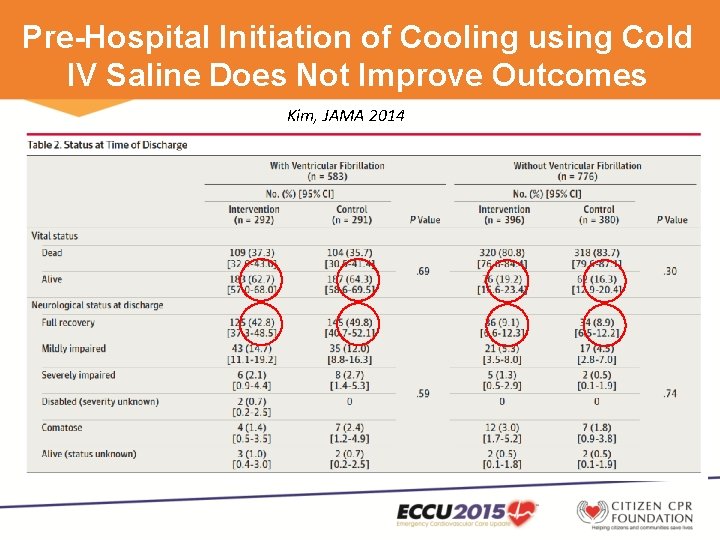
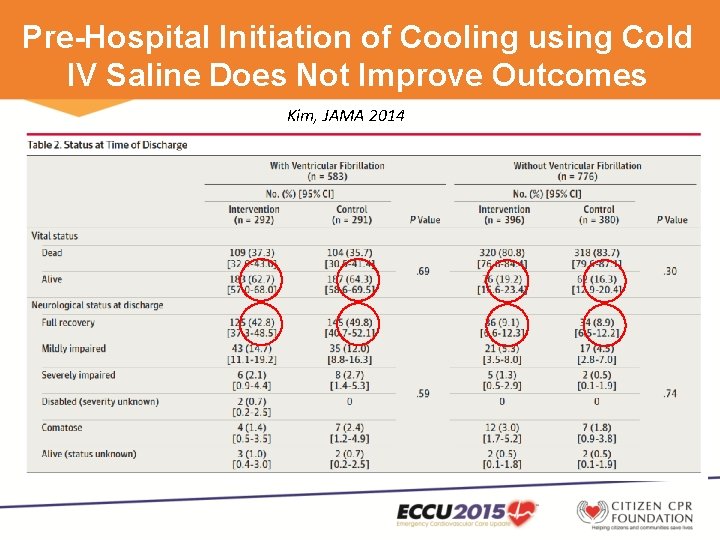
Pre-Hospital Initiation of Cooling using Cold IV Saline Does Not Improve Outcomes Kim, JAMA 2014
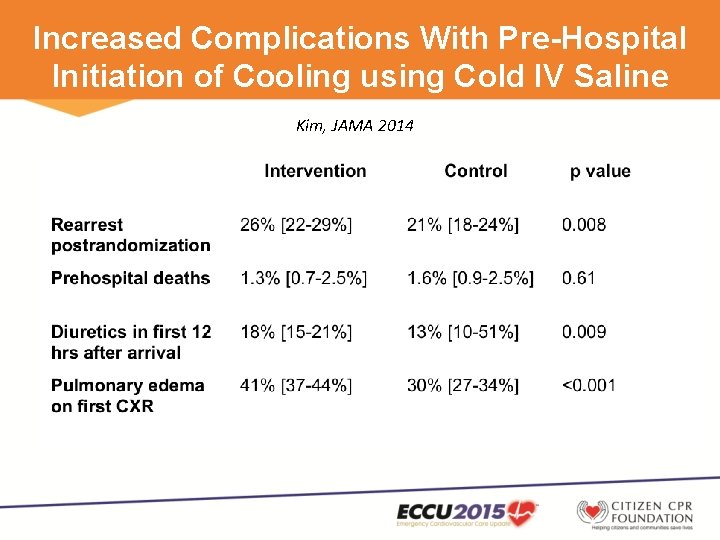
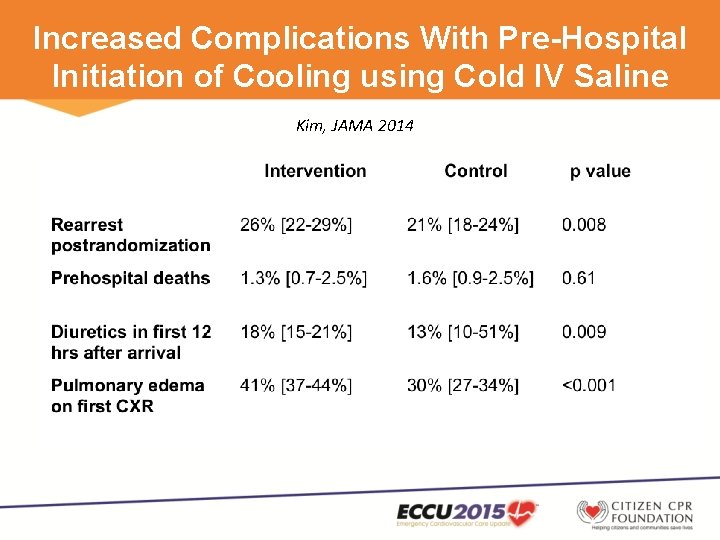
Increased Complications With Pre-Hospital Initiation of Cooling using Cold IV Saline Kim, JAMA 2014
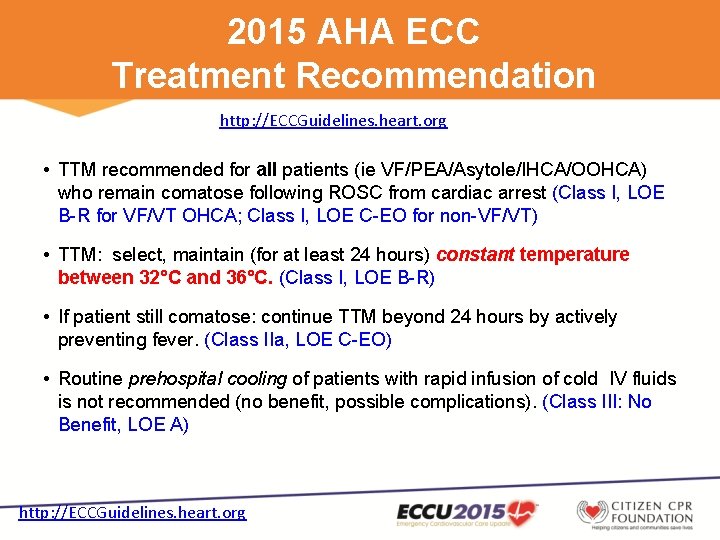
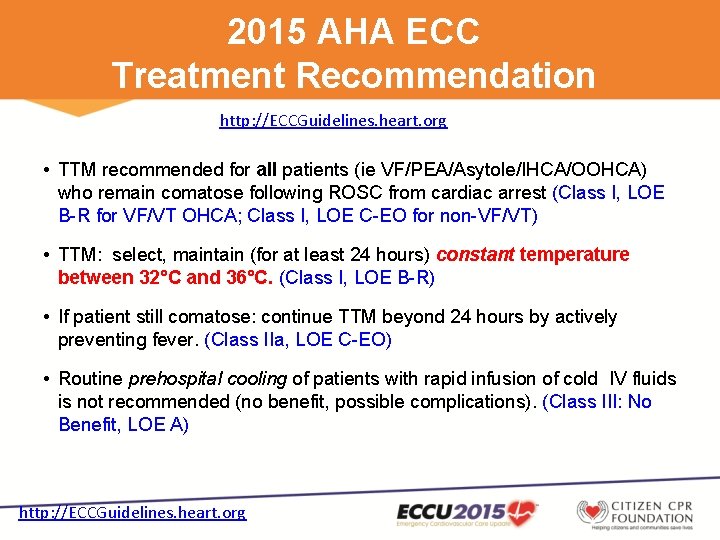
2015 AHA ECC Treatment Recommendation http: //ECCGuidelines. heart. org • TTM recommended for all patients (ie VF/PEA/Asytole/IHCA/OOHCA) who remain comatose following ROSC from cardiac arrest (Class I, LOE B-R for VF/VT OHCA; Class I, LOE C-EO for non-VF/VT) • TTM: select, maintain (for at least 24 hours) constant temperature between 32°C and 36°C. (Class I, LOE B-R) • If patient still comatose: continue TTM beyond 24 hours by actively preventing fever. (Class IIa, LOE C-EO) • Routine prehospital cooling of patients with rapid infusion of cold IV fluids is not recommended (no benefit, possible complications). (Class III: No Benefit, LOE A) http: //ECCGuidelines. heart. org
2015 ACLS Highlights • CPR adjuncts – Impedance threshold device (ITD) – Active compression-decompression (ACD) – Mechanical CPR • CPR pharmacology – Vasopressors • Physiologic monitoring during CPR • Focused ultrasound during CPR • Extracorporeal CPR (ECPR) • Post-cardiac arrest coronary angiography and PCI • Post-cardiac arrest targeted temperature management • Post-cardiac arrest neuroprognostication
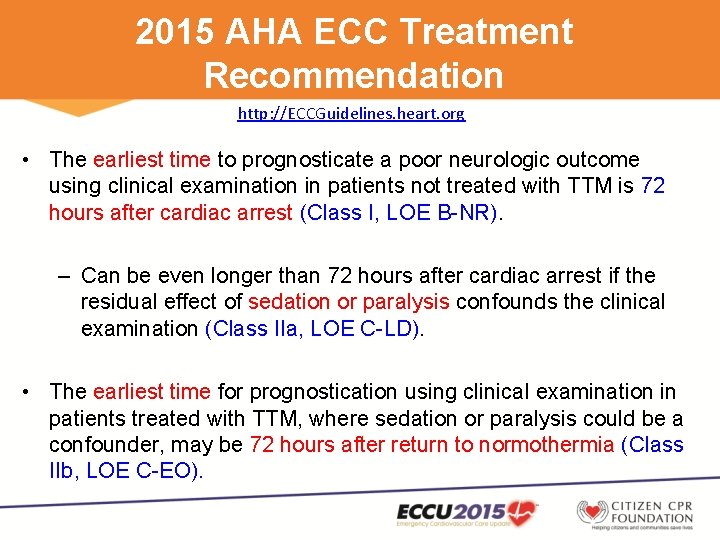
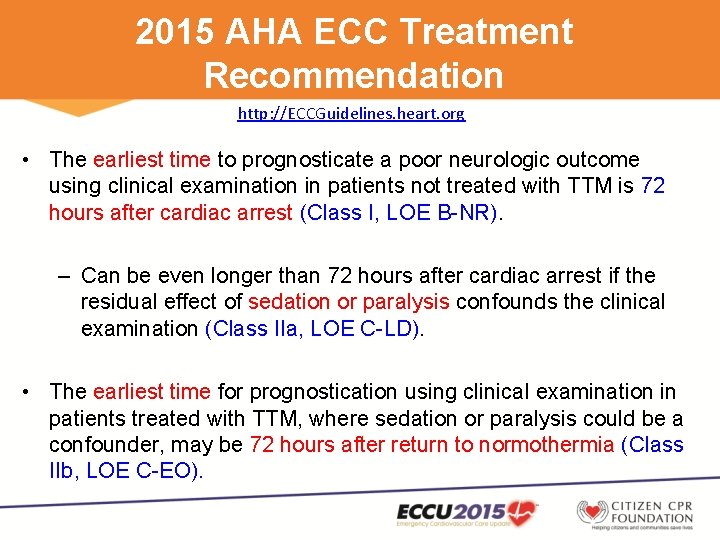
2015 AHA ECC Treatment Recommendation http: //ECCGuidelines. heart. org • The earliest time to prognosticate a poor neurologic outcome using clinical examination in patients not treated with TTM is 72 hours after cardiac arrest (Class I, LOE B-NR). – Can be even longer than 72 hours after cardiac arrest if the residual effect of sedation or paralysis confounds the clinical examination (Class IIa, LOE C-LD). • The earliest time for prognostication using clinical examination in patients treated with TTM, where sedation or paralysis could be a confounder, may be 72 hours after return to normothermia (Class IIb, LOE C-EO).
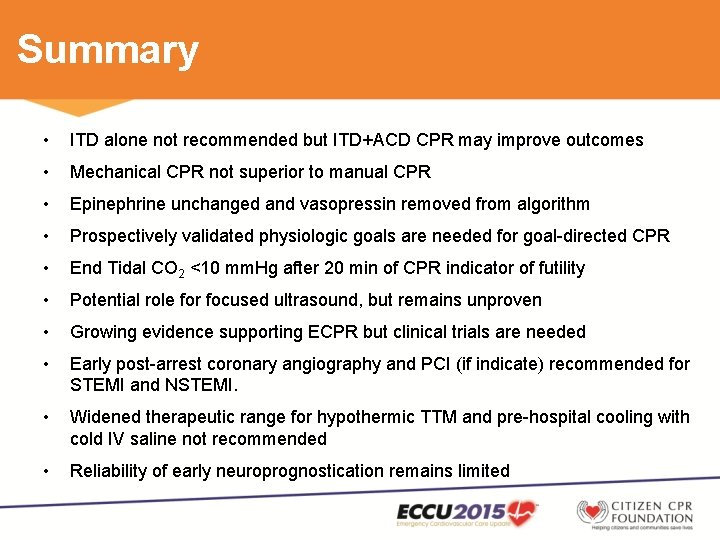
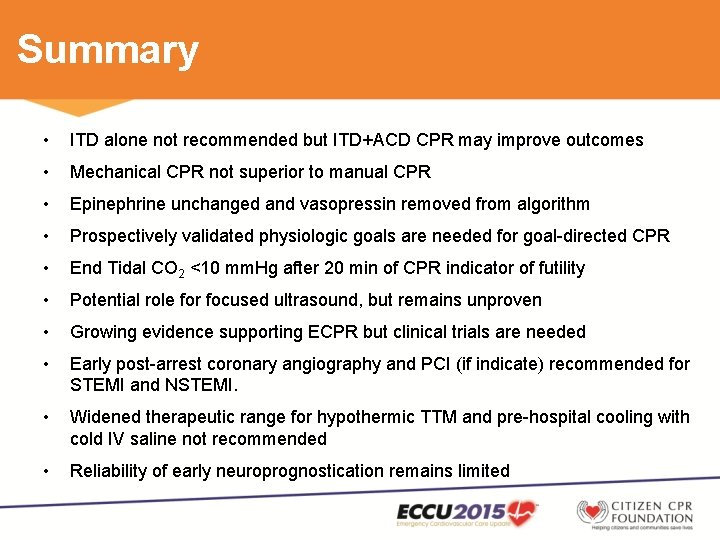
Summary • ITD alone not recommended but ITD+ACD CPR may improve outcomes • Mechanical CPR not superior to manual CPR • Epinephrine unchanged and vasopressin removed from algorithm • Prospectively validated physiologic goals are needed for goal-directed CPR • End Tidal CO 2 <10 mm. Hg after 20 min of CPR indicator of futility • Potential role for focused ultrasound, but remains unproven • Growing evidence supporting ECPR but clinical trials are needed • Early post-arrest coronary angiography and PCI (if indicate) recommended for STEMI and NSTEMI. • Widened therapeutic range for hypothermic TTM and pre-hospital cooling with cold IV saline not recommended • Reliability of early neuroprognostication remains limited