sinusitis Scope of Sinusitis Affects 30 35 million












- Slides: 43
sinusitis
Scope of Sinusitis • Affects 30 -35 million persons/year • 25 million office visits/year • Direct annual cost $2. 4 billion and increasing • Added surgical costs: $1 billion • Third most common diagnosis for which antibiotics are prescribed 2
Development of Sinuses • Maxillary and ethmoid sinuses present at birth • Frontal sinus developed by age 5 or 6 • Sphenoid sinus last to develop, 8 -10 3
Normal Sinus • Sinus health depends on: – Mucous secretion of normal viscosity, volume, and composition, – normal mucociliary flow to prevent mucous stasis and subsequent infection; – and open sinus ostia to allow adequate drainage and aeration. 4
Physiologic Importance of Sinuses • Provide mucus to upper airways – Lubrication – Vehicle for trapping viruses, bacteria, foreign material for removal • Give characteristics to voice • Lessen skull weight • Involved with olfaction 5
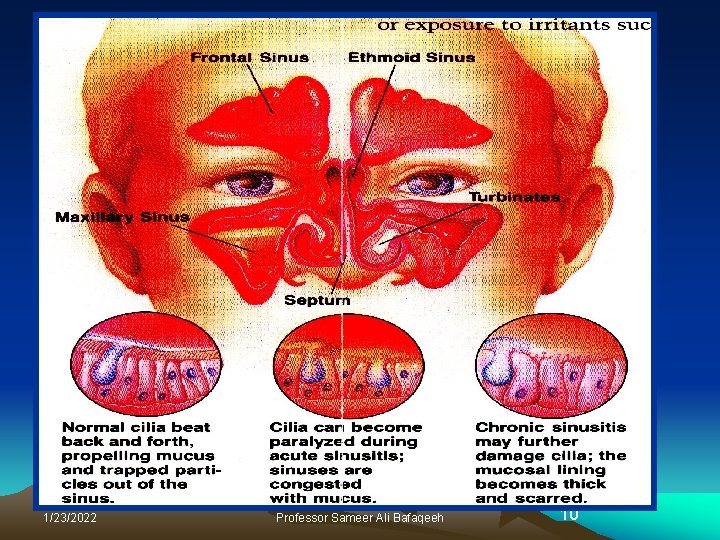
ANATOMY • Septum • Nasal Turbinates – Concha Bullosa – Middle Turbinate • Sinuses: Maxillary, Ethmoid (anterior and posterior), Frontal and Sphenoid – Osteomeatal Complex – Nasofrontal recess – Uncinate process (hiatus semilunaris)
ANATOMY (continued) • Ciliated pseudostratified columnar epithelium – Two layers of mucus • Thick “basement” layer • Thin less viscous layer that the cilia moves to the ostia – Mucosal Changes After Surgery and Long Term Disease • Neuroreceptors for smell (olfactory nerve) and airflow (located in the inferior and middle turbinates


1/23/2022 Professor Sameer Ali Bafaqeeh 10
Acute Rhinosinusitis (Viral) • Common Symptoms: Nasal discharge, nasal congestion, facial pressure, cough, fever, muscle aches, joint pains, sore throat with hoarseness. • Etiology, rhinovirus, influenza, parainflu, adenovirus, ent erovirus, RSV, …. . • Symptoms resolve in 10 -14 days • Common in fall, winter and spring. • Treatment: Symptomatic
Acute Bacterial Sinusitis • Causative agents are usually the normal inhabitants of the respiratory tract. • Common agents: Streptococcus pneumoniae Nontypeable Haemophilus Influenzae Moraxella Catarrhalis
SIGNS AND SYMPTOMS • Pain and/or pressure – frontal, maxillary, upper teeth, retro-orbital, crown of the head • temporal, parietal and occipital headaches are not generally associated with sinusitis • children under the age of 12 who complain of headaches and, without prompting from a parent, points to the top of their head, anterior face, eye, or posterior skull most likely have sphenoid sinusitis until otherwise documented by CT or MRI scan • Fever
SIGNS AND SYMPTOMS • Nasal congestion and/or drainage – Rhinorrhea • postnasal drainage • purulent • color does not determine infection • Obstruction – Deviated septum – Hypertrophy of turbinate(s) – Polyps
ACUTE SINUSITIS • Less than one month duration • Purulent drainage, fever, significant sinus pain and pressure • Isolated acute infection without recurrent “sinus symptoms” – Most commonly secondary to upper respiratory viral infection or other inflammatory condition • perennial allergic rhinitis with inflammation • obstruction of the ostia/drainage passages of the sinuses • primarily neutrophilic inflammation with a small amount of eosinophils
Diagnosis • Based on clinical signs and symptoms • Physical Exam: Palpate over the sinuses, look for structural abnormalities like DNS. • X-ray sinuses: not usually needed but may show cloudiness and air fluid levels • Limited coronal CT are more sensitive to inflammatory changes and bone destruction
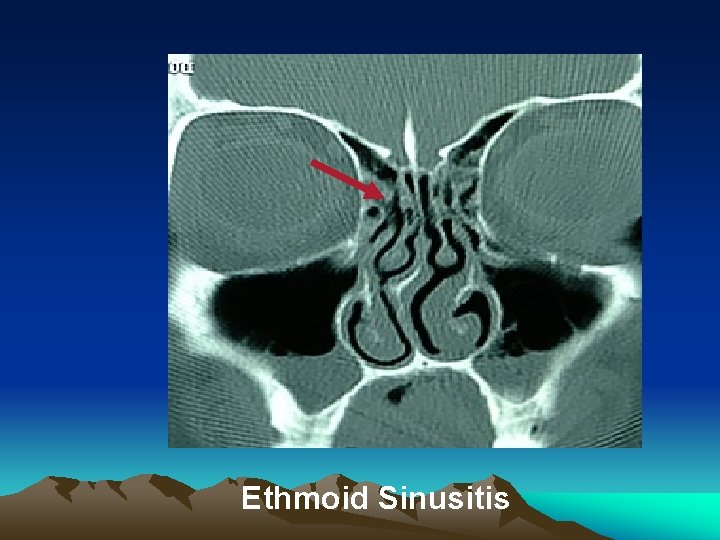
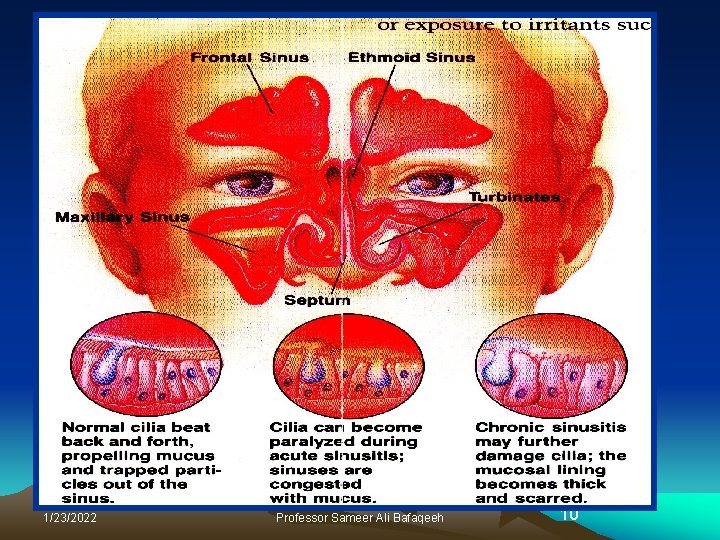
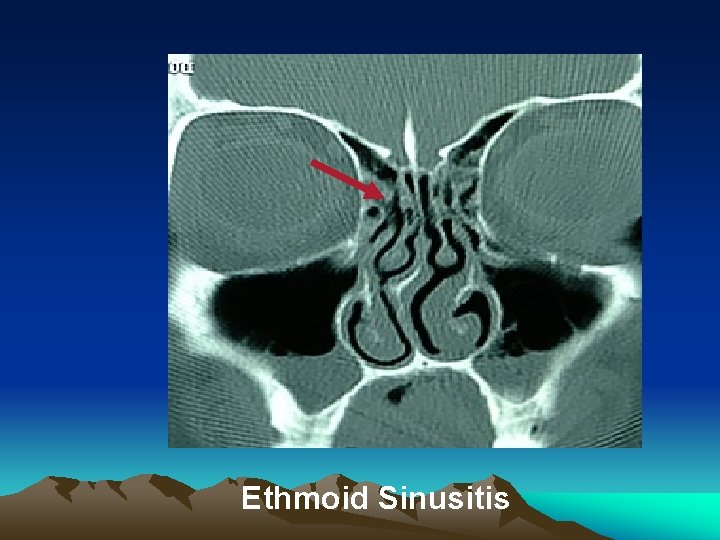
Ethmoid Sinusitis
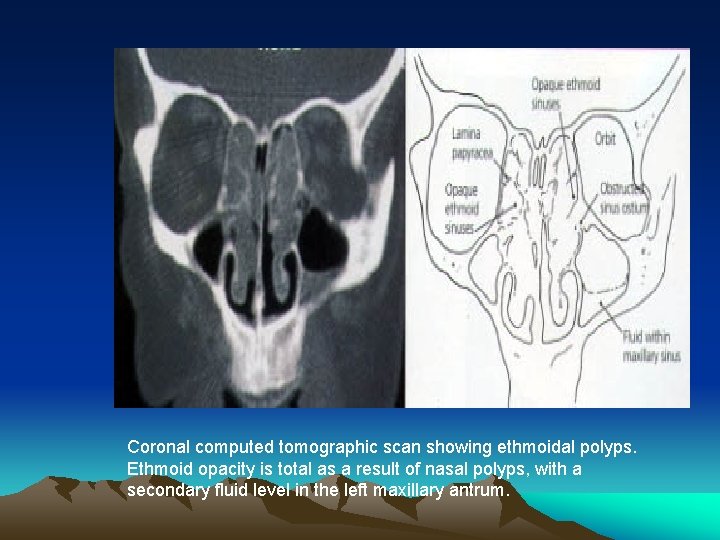
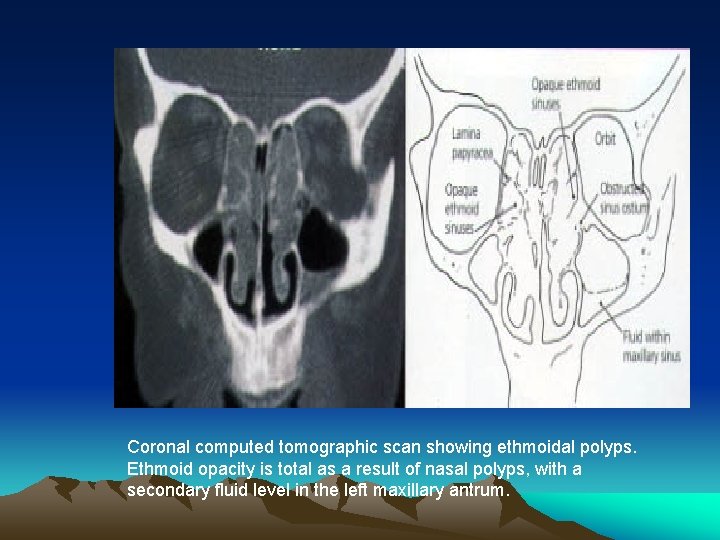
Coronal computed tomographic scan showing ethmoidal polyps. Ethmoid opacity is total as a result of nasal polyps, with a secondary fluid level in the left maxillary antrum.
Treatment • About 2/3 rd of patients will improve without treatment in 2 weeks. • Antibiotics: Reserved for patients who have symptoms for more than 10 days or who experience worsening symptoms. • OTC decongestant nasal sprays should be discouraged for use more than 5 days • Supportive therapy: Humidification, analgesics, antihistaminics
Antibiotics a) Amoxicillin (500 mg TID) OR b) TMP/SMX ( one DS for 10 days). c) Alternative antibiotics: High dose amoxi/clavunate, Flouroquinolones, macrolides, cefixime, cefuroxime, . .
CHRONIC SINUSITIS • Greater than three months duration – multiple treatments or infections within one year – multiple year history of recurrent infections or episodes of sinus pain and pressure – symptoms that coincide with changes in altitude or weather – chronic nasal congestion and drainage
CHRONIC RHINOSINUSITIS (CRS) WITHOUT POLYPS • Neutrophilic inflammation associated with obstruction and inflammation of sinus ostia
CHRONIC RHINOSINUSITIS (CRS) WITH POLYPS • Associated with eosiniphilic inflammation with some association with interleukin 4 and 5 and Ig. E mediated response • No difference in the composition of the mucin between systemic atopic patients versus nonatopic patients • Patients with genetic mucociliary transport diseases such as cystic fibrosis or, patients who have significant acquired changes of the mucosa following surgery may also have neutrophilic inflammation

ALLERGIC FUNGAL SINUSITIS (AFRS) • Non-invasive – local fungal hyphae in the mucin – allergic response to the fungus – polyps with thick grey to brownish “greasy” mucin drainage
ALLERGIC FUNGAL SINUSITIS (AFRS) • Invasive – Microscopic invasion of fungus in the mucosa – Necrotic black tissue with nonpainful debridement is an emergent life threatening fungal infection – mucomycosis


NONALLERGIC RHINITIS • May be caused by drugs such as: – – – Beta blockers Methyldopa related Reserpine Oral contraceptives Nasal sprays (OTC) Decongestants
NONALLERGIC RHINITIS • May also be caused by certain conditions such as: – – – Pregnancy Hypothyroidism Temperature related Recumbency rhinitis End-stage vascular atony (Chronic allergic/inflammatory) – Paradoxical nasal obstruction (Nasal cycle) – Non-airflow rhinitis (Adenoid hypertrophy, choanal atresia)
TREATMENT • • • Nasal and oral steroids Antibiotics Nasal saline irrigation Ponaris emollient Oral decongestants and antihistamines – Conservative use • Biofilm formation • Surgery
NON-SURGICAL TREATMENT • Acute sinusitis – – Antibiotics – ten days to three weeks Nasal steroids – six to eight weeks Nasal saline irrigations – six to eight weeks Mucocilia may take up to four to six weeks to resume normal function – CT scan of sinuses if indicated – Optional: • Nasal spray decongestants – three days only • Short course of oral steroids – Surgery if indicated
NON-SURGICAL TREATMENT • Chronic or recurrent sinusitis without polyps – Nasal steroids – long-term treatment – Nasal saline irrigation – long-term treatment – Antibiotics with acute intermittent sinus infections up to six weeks – CT scan sinuses – Otolaryngologist evaluation – Surgery
NON-SURGICAL TREATMENT • Chronic rhinosinusitis with polyps – – Otolaryngologist evaluation Nasal steroids – long-term treatment Nasal saline irrigation – long-term treatment Antibiotics with acute intermittent sinus infections up to six weeks – Allergy testing – Surgery
NON-SURGICAL TREATMENT • Allergic Fungal Sinusitis (AFRS) – Nasal steroids – long-term treatment – Nasal saline irrigation – long-term treatment – Amphotericin B, mucopricin, steroid or gentamycin irrigations – Most common organism – Aspergillus fumigates – Antibiotics with acute intermittent sinus infections up to six weeks – CT scan sinuses – Surgery
SURGICAL TREATMENT • Image guided endoscopic sinus surgery • Balloon sinuplasty






