Shedding Light on Mitochondrial Function In Vivo From


- Slides: 62
Shedding Light on Mitochondrial Function In Vivo: From Experimental animals to clinical Applications The Mina & Everard Goodman Faculty of Life-Sciences and The Leslie & Susan Gonda Multidisciplinary Brain Research Center Bar-Ilan University, Ramat-Gan, 52900, Israel Email: mayevskya@gmail. com ESCTAIC 23 rd Congress 2012 Timisoara, Romania October 4 th 2012
Bar Ilan University Ramat Gan ISRAEL
Short History –Monitoring of Mitochondrial function and Tissue Energy Metabolism. “There is no instance in which it can be proven that an organ increases its activity under physiological conditions, without also increasing in its call for oxygen, and- in no organ excited by any form of stimulation can it be shown that positive work is done without the blood supply having to respond to a call for oxygen”. Barcroft J. The Respiratory Function of the Blood. Cambridge Univ. Press, Cambridge, 1914

Major artery A Large Artery D NADH Mitochondrial NADH (Fluorometry) Art Systemic Hemoglobin Oxygenation ( Pulse Oximeter) eri ole O 2 O 2 + NADH Ac. C o. A NAD TCA Pyruvate H 2 O O 2 HOS P X O ETC- Capillary O 2 O 2 Microcirculatory Hemoglobin Oxygenation (Tissue Oximeter) B Hb. O 2 CO 2 H+ O 2 ATP ADP+Pi 2 O 2 O 2 O 2 Glucose Glycolysis Microvascular Arterioles & capillaries Lactate Venule Tissue Blood Flow (Laser Doppler Flowmetry) C
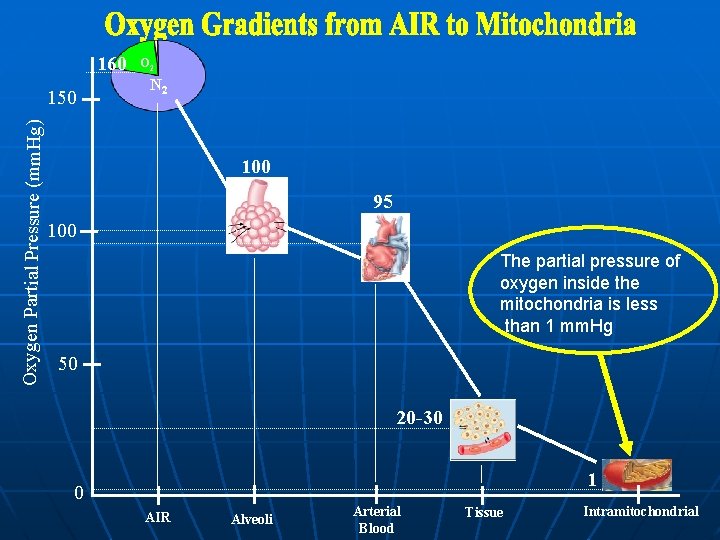
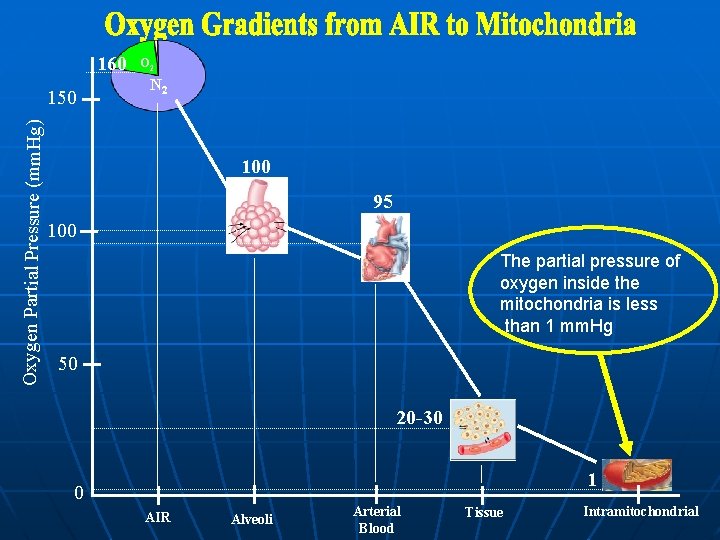
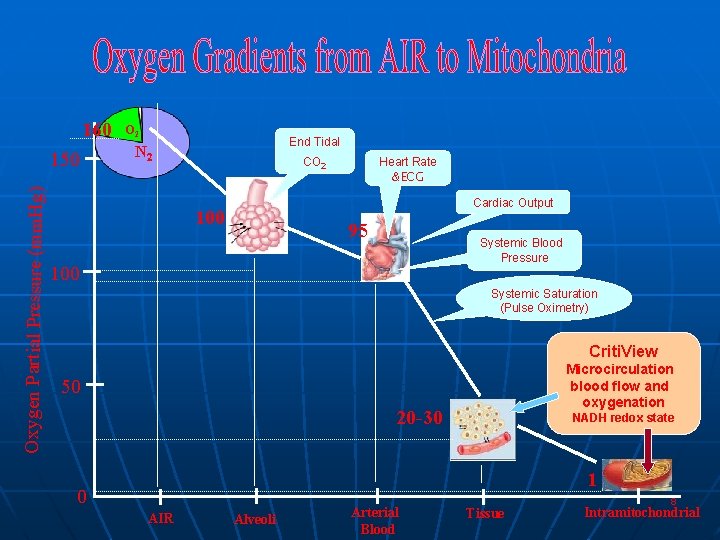
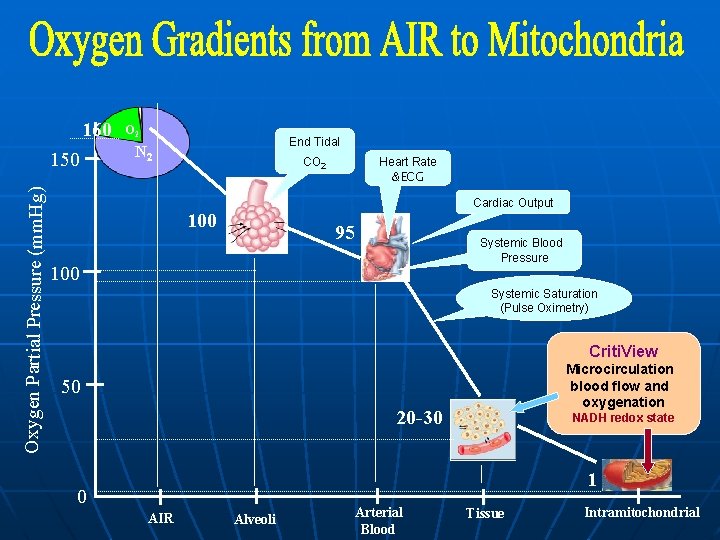
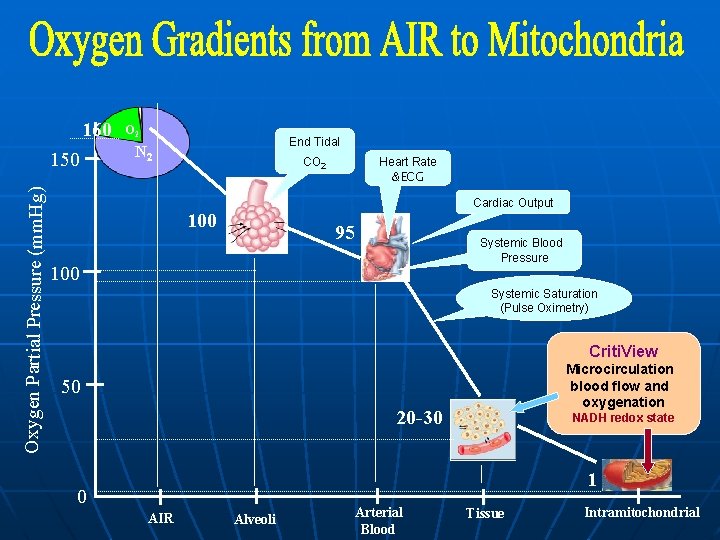
160 Oxygen Partial Pressure (mm. Hg) 150 O 2 N 2 100 95 100 The partial pressure of oxygen inside the mitochondria is less than 1 mm. Hg 50 20 -30 1 0 AIR Alveoli Arterial Blood Tissue Intramitochondrial
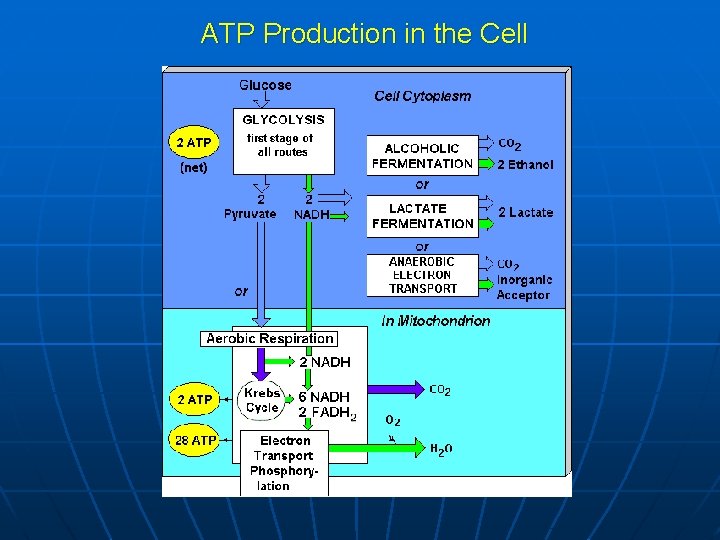
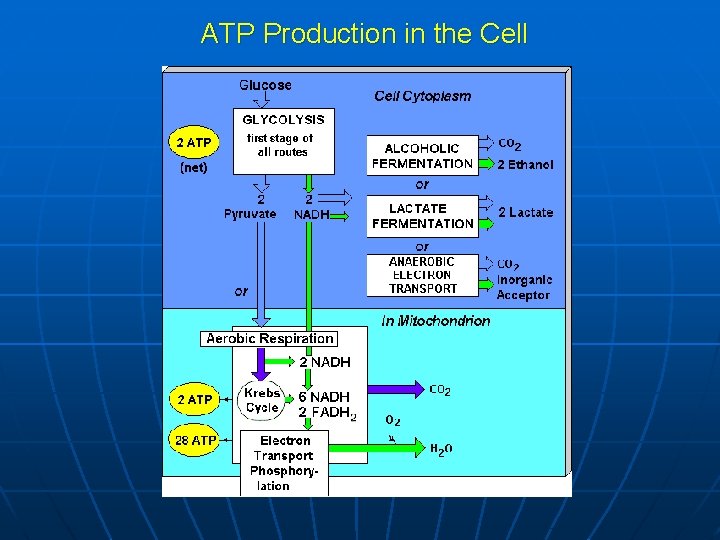
ATP Production in the Cell
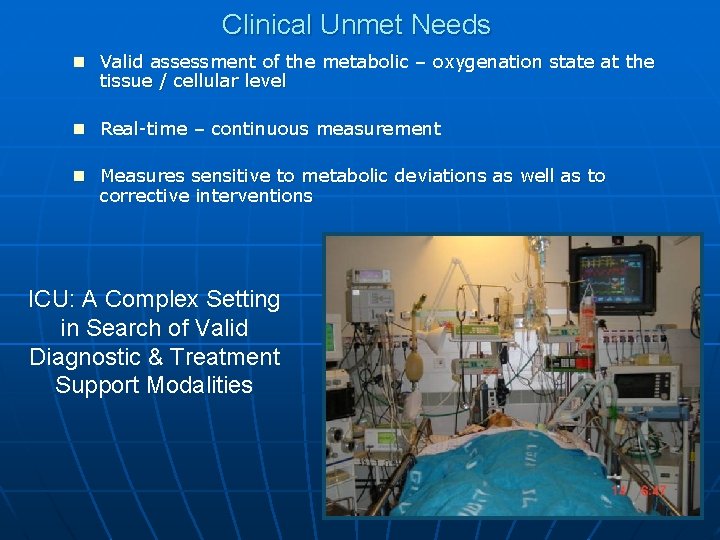
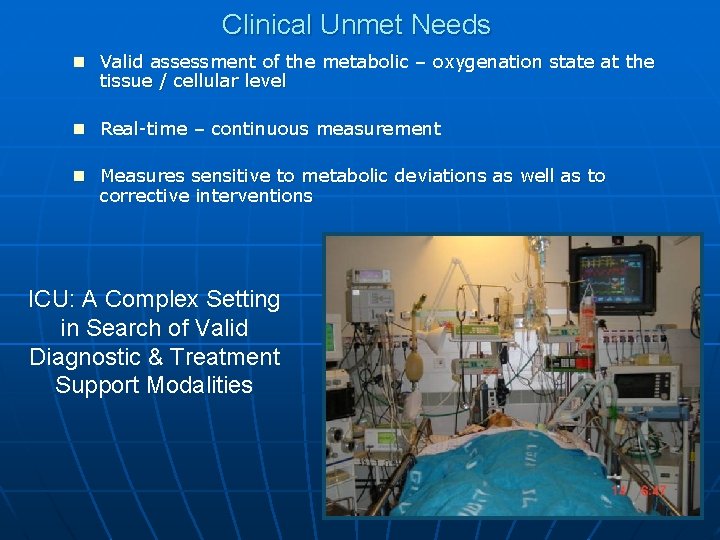
Clinical Unmet Needs n Valid assessment of the metabolic – oxygenation state at the tissue / cellular level n Real-time – continuous measurement n Measures sensitive to metabolic deviations as well as to corrective interventions ICU: A Complex Setting in Search of Valid Diagnostic & Treatment Support Modalities
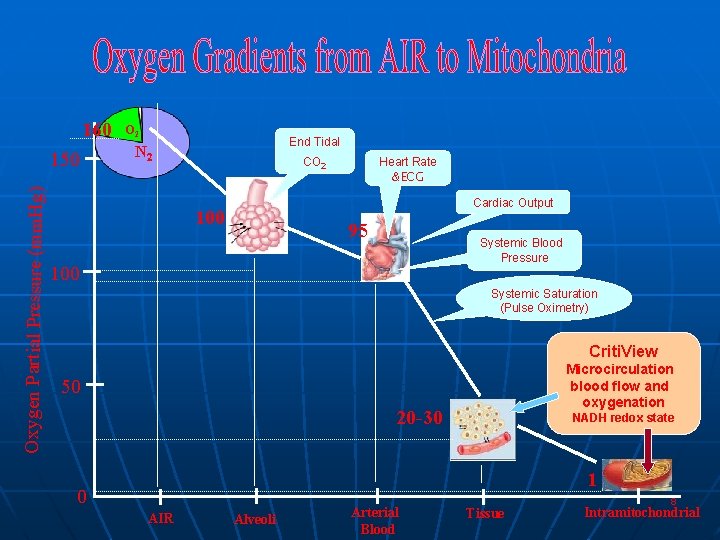
160 Oxygen Partial Pressure (mm. Hg) 150 O 2 End Tidal N 2 CO 2 Heart Rate &ECG Cardiac Output 100 95 Systemic Blood Pressure 100 Systemic Saturation (Pulse Oximetry) Criti. View Microcirculation blood flow and oxygenation 50 20 -30 NADH redox state 1 0 AIR Alveoli Arterial Blood Tissue 8 Intramitochondrial
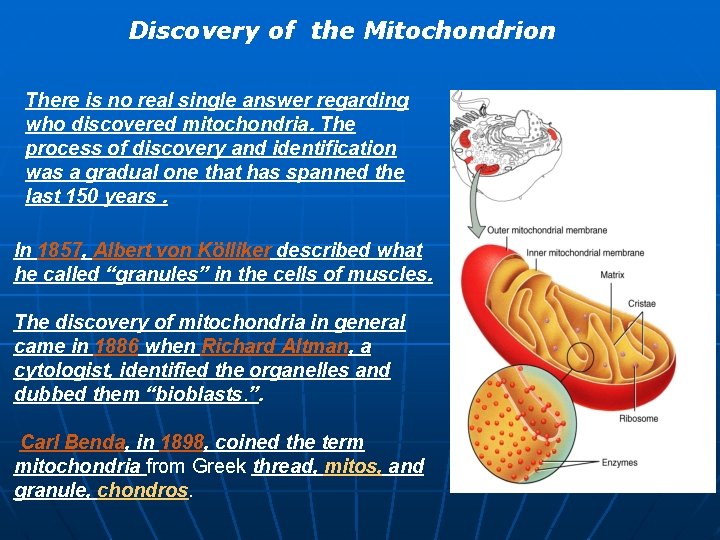
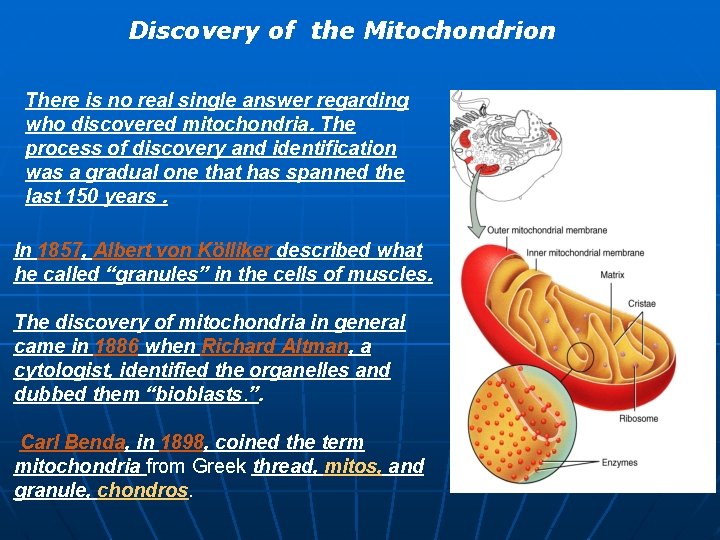
Discovery of the Mitochondrion There is no real single answer regarding who discovered mitochondria. The process of discovery and identification was a gradual one that has spanned the last 150 years. In 1857, Albert von Kölliker described what he called “granules” in the cells of muscles. The discovery of mitochondria in general came in 1886 when Richard Altman, a cytologist, identified the organelles and dubbed them “bioblasts. ”. Carl Benda, in 1898, coined the term mitochondria from Greek thread, mitos, and granule, chondros.
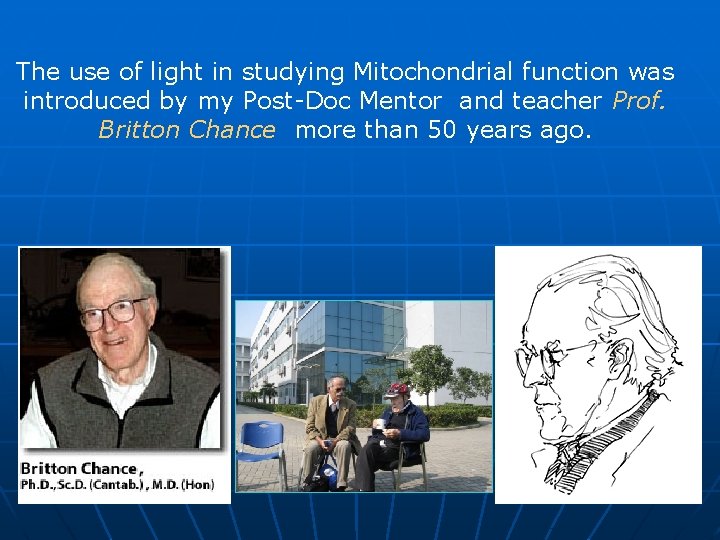
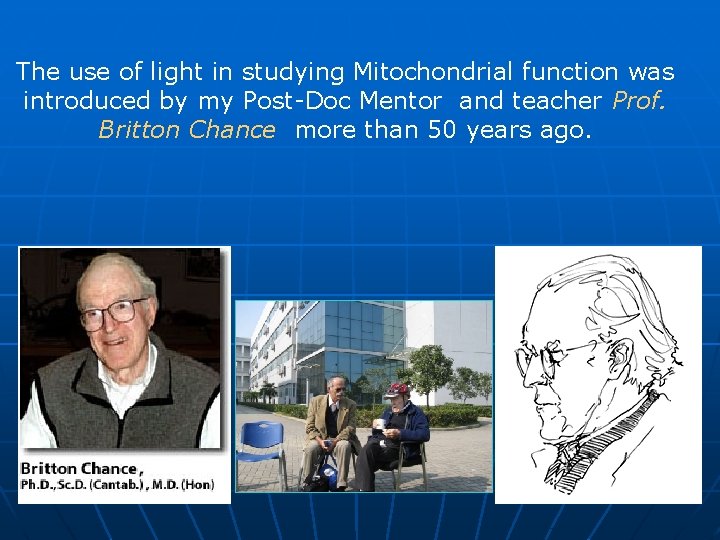
The use of light in studying Mitochondrial function was introduced by my Post-Doc Mentor and teacher Prof. Britton Chance more than 50 years ago.
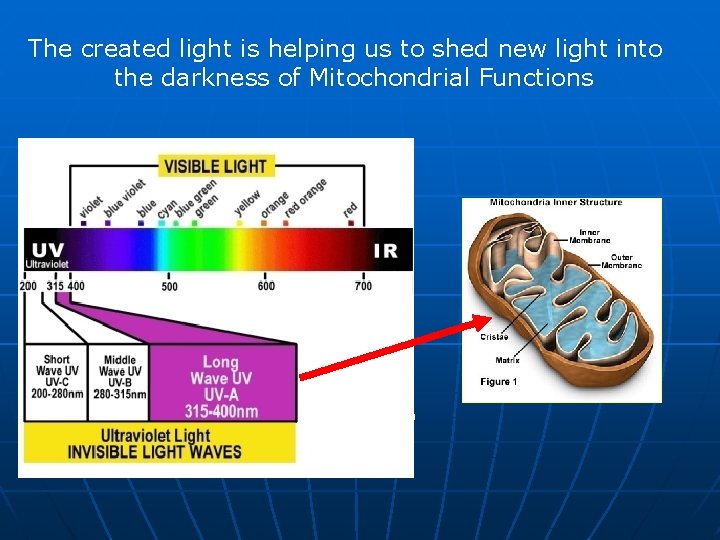
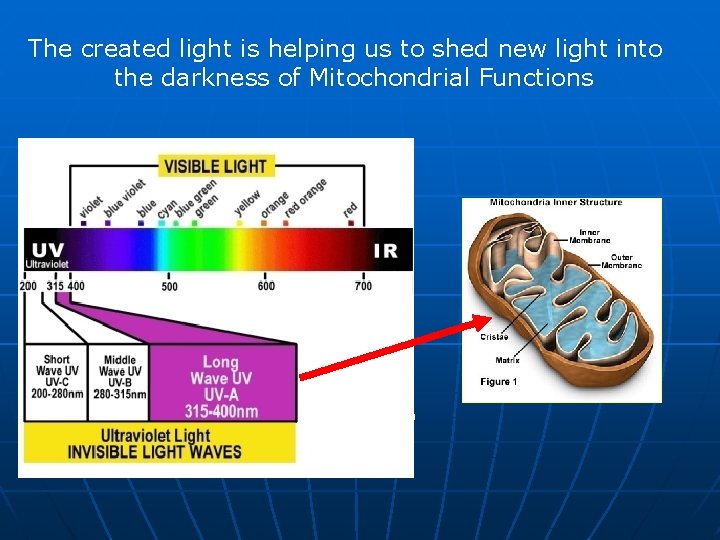
The created light is helping us to shed new light into the darkness of Mitochondrial Functions
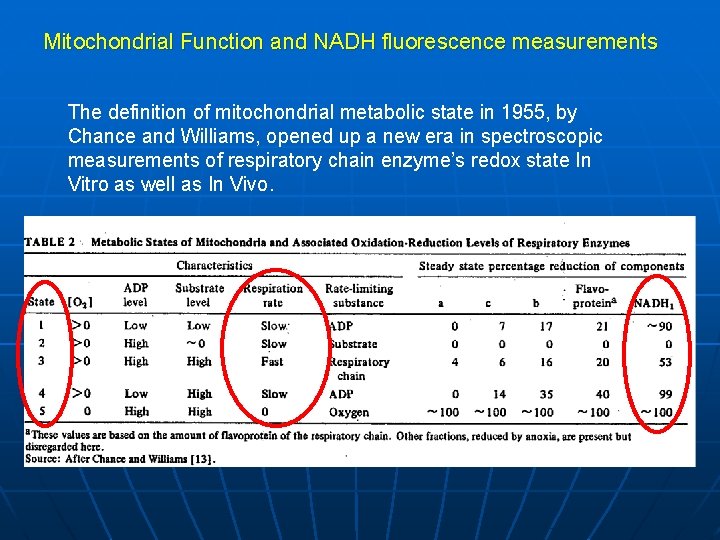
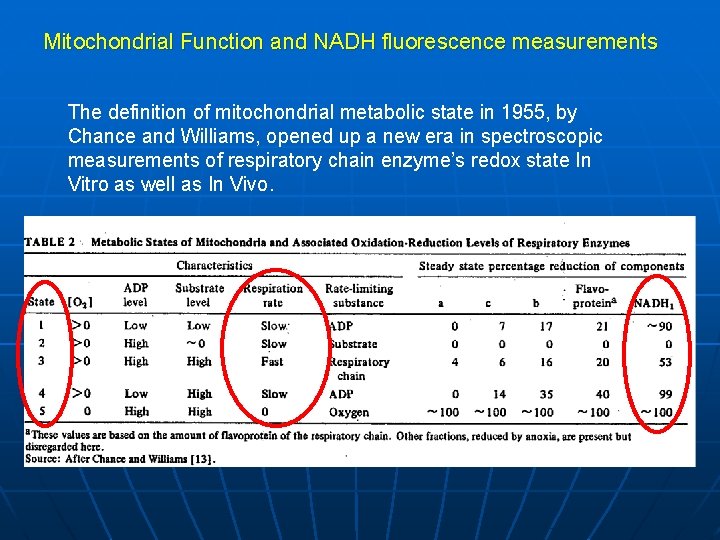
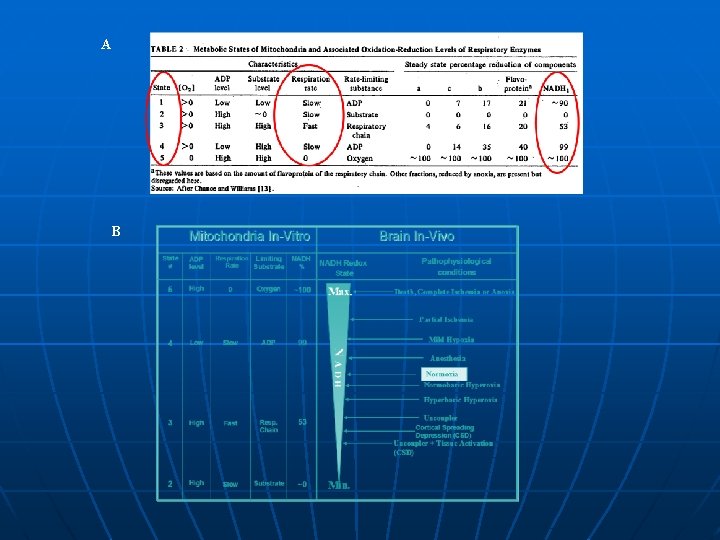
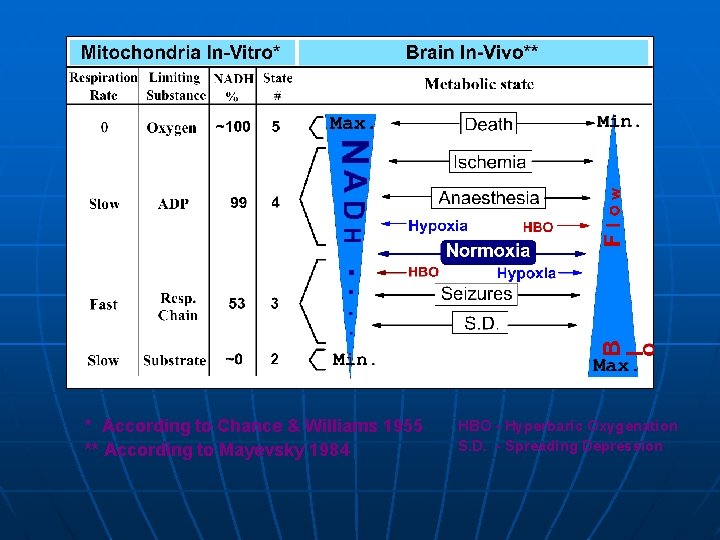
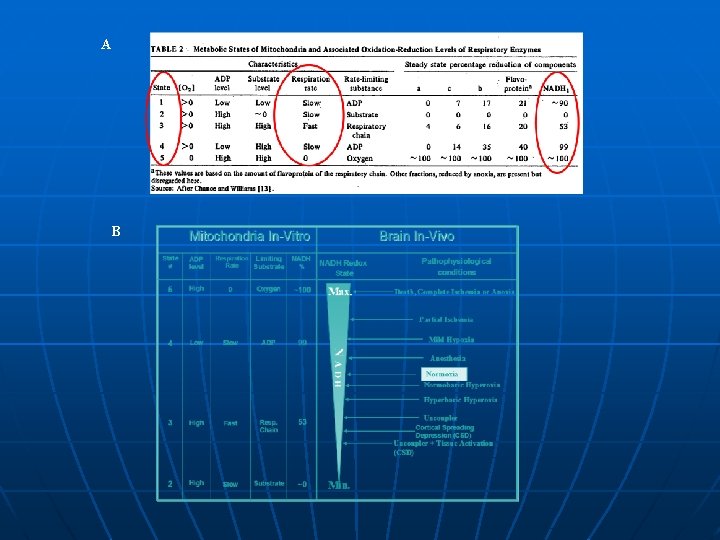
Mitochondrial Function and NADH fluorescence measurements The definition of mitochondrial metabolic state in 1955, by Chance and Williams, opened up a new era in spectroscopic measurements of respiratory chain enzyme’s redox state In Vitro as well as In Vivo.
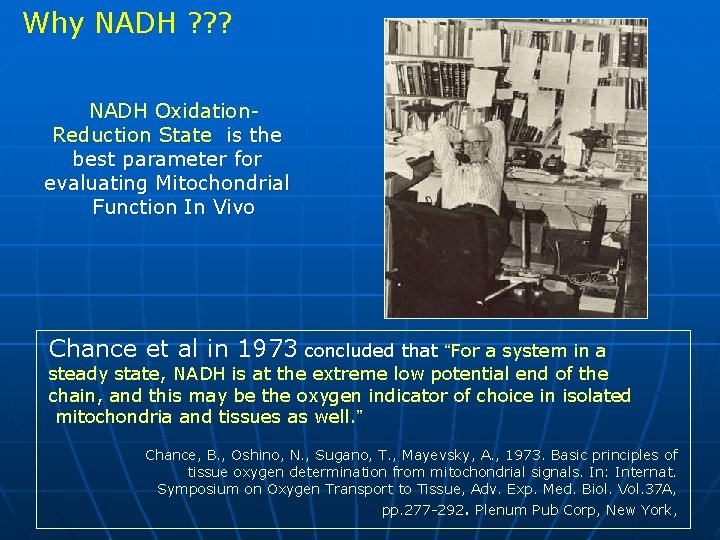
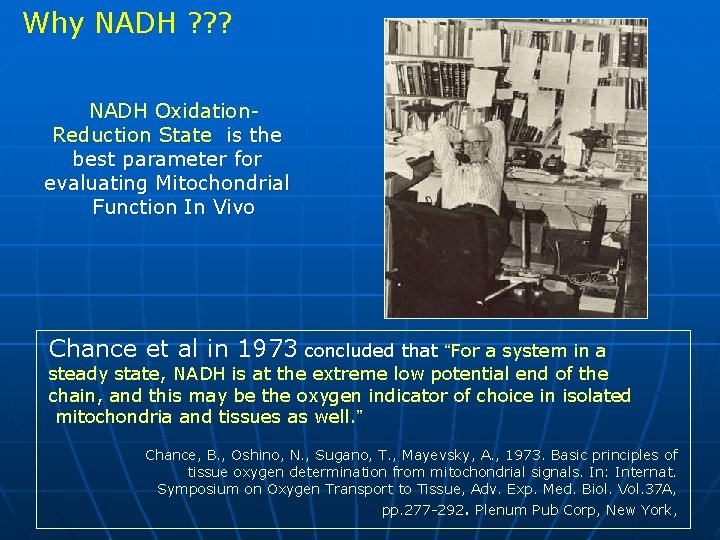
Why NADH ? ? ? NADH Oxidation. Reduction State is the best parameter for evaluating Mitochondrial Function In Vivo Chance et al in 1973 concluded that “For a system in a steady state, NADH is at the extreme low potential end of the chain, and this may be the oxygen indicator of choice in isolated mitochondria and tissues as well. ” Chance, B. , Oshino, N. , Sugano, T. , Mayevsky, A. , 1973. Basic principles of tissue oxygen determination from mitochondrial signals. In: Internat. Symposium on Oxygen Transport to Tissue, Adv. Exp. Med. Biol. Vol. 37 A, pp. 277 -292. Plenum Pub Corp, New York,
Why NADH ? ? ? NADH Oxidation-Reduction State is the best parameter for evaluating Mitochondrial Function In Vivo Lubbers in 1995 concluded that “the most important intrinsic luminescence indicator is NADH, an enzyme of which the reaction is connected with tissue respiration and energy metabolism ” Lubbers, D. W. 1995. Optical sensors for clinical monitoring. Acta Anaesth. Scand. Suppl. 39, 37 -54.
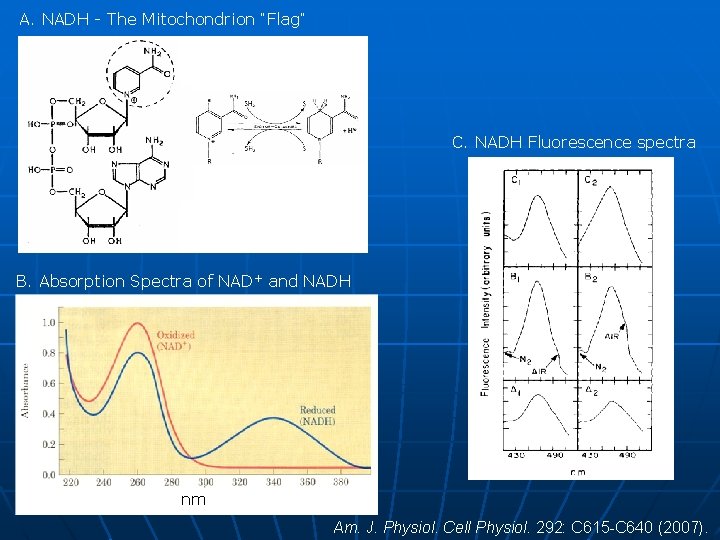
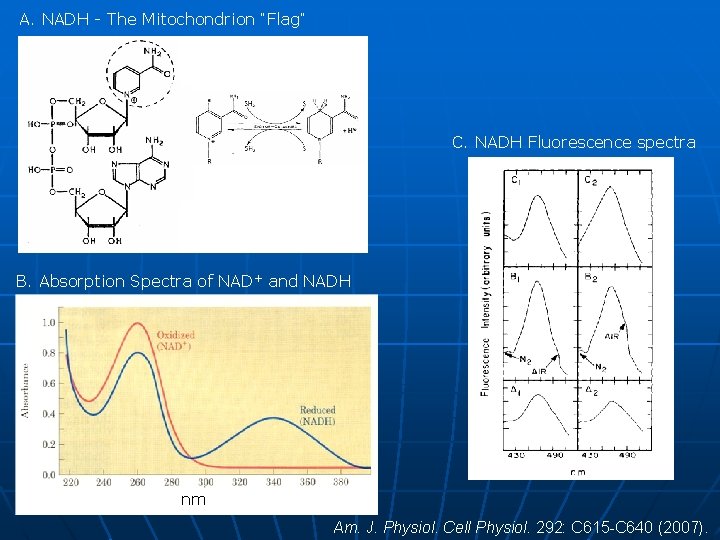
A. NADH - The Mitochondrion “Flag” C. NADH Fluorescence spectra B. Absorption Spectra of NAD+ and NADH nm Am. J. Physiol. Cell Physiol. 292: C 615 -C 640 (2007).
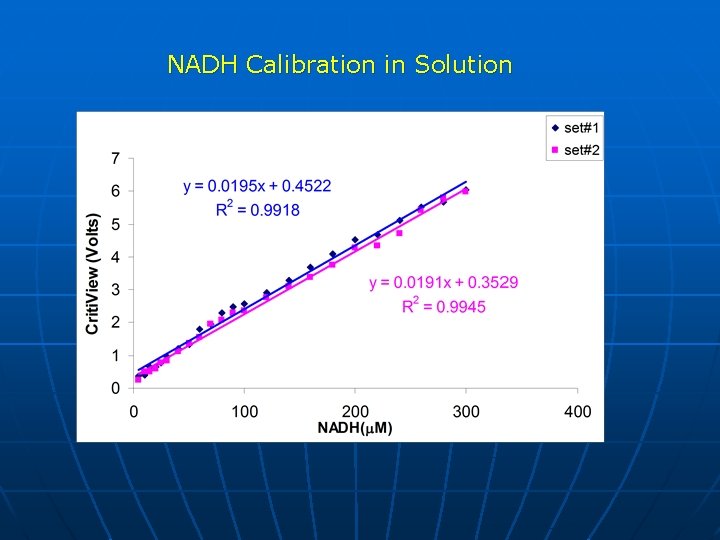
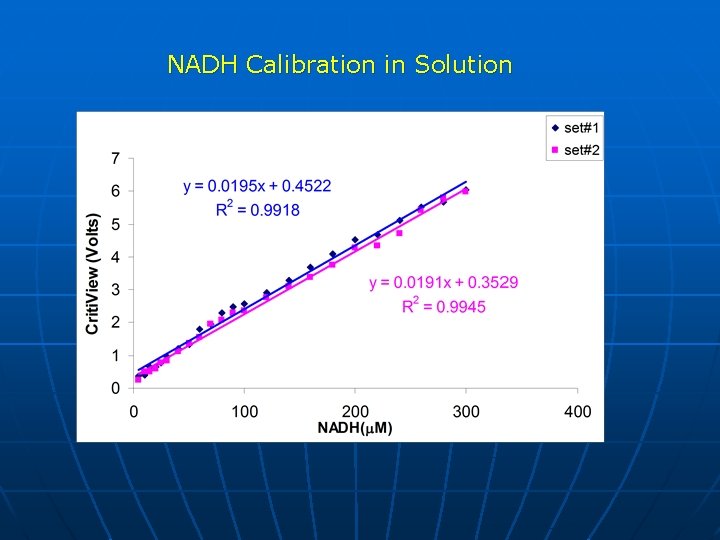
NADH Calibration in Solution
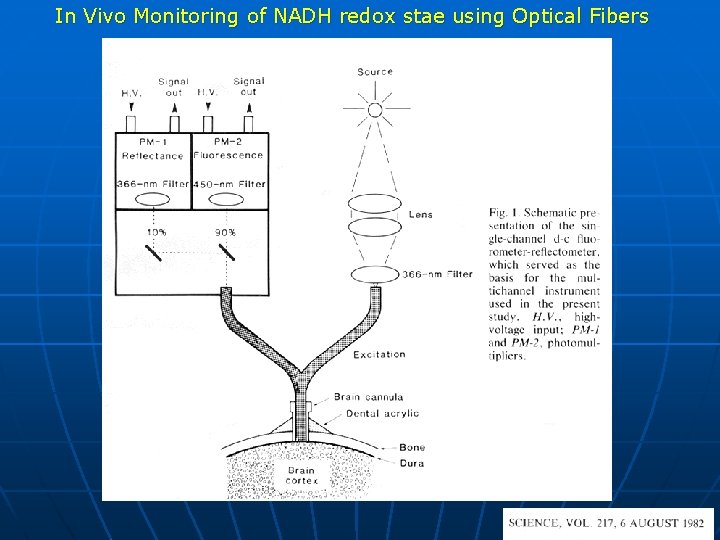
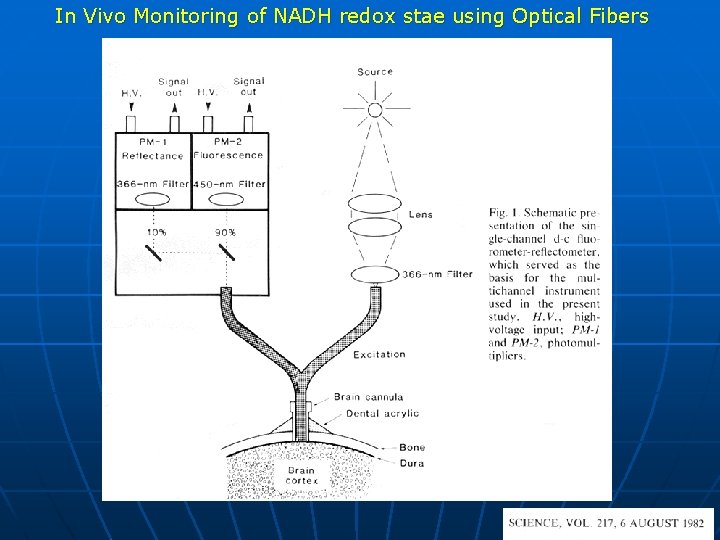
In Vivo Monitoring of NADH redox stae using Optical Fibers
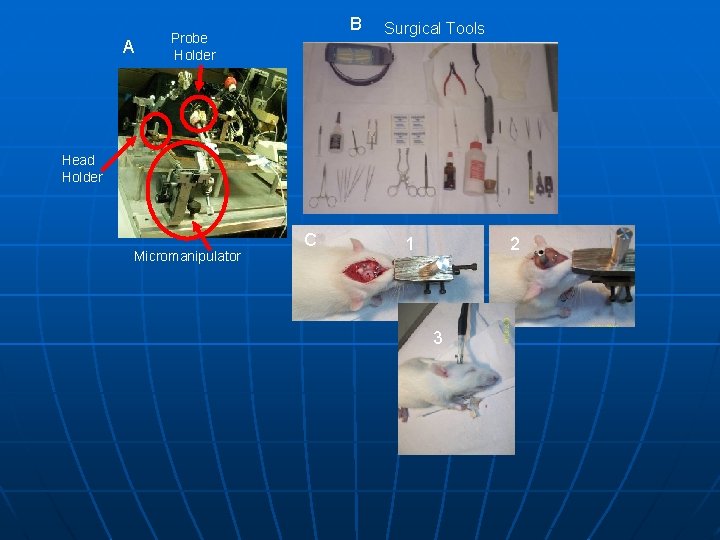
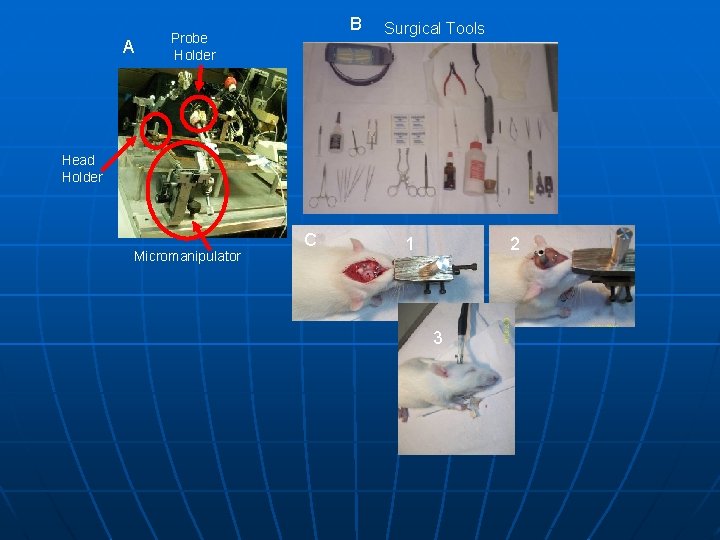
A B Probe Holder Surgical Tools Head Holder Micromanipulator C 2 1 3
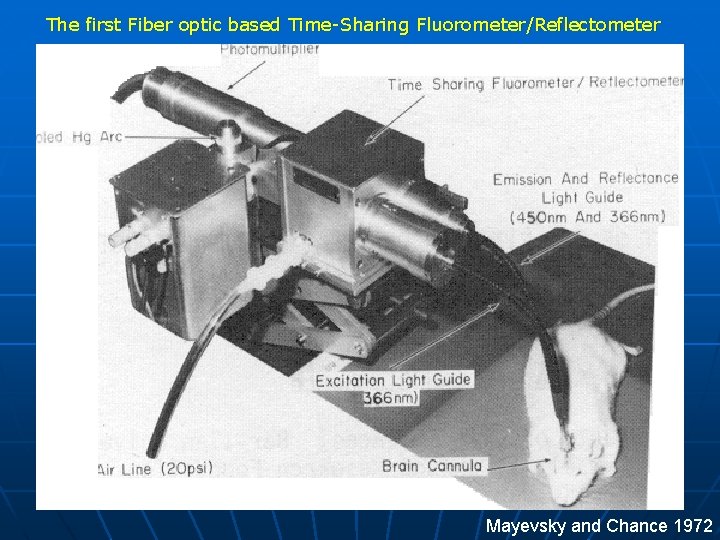
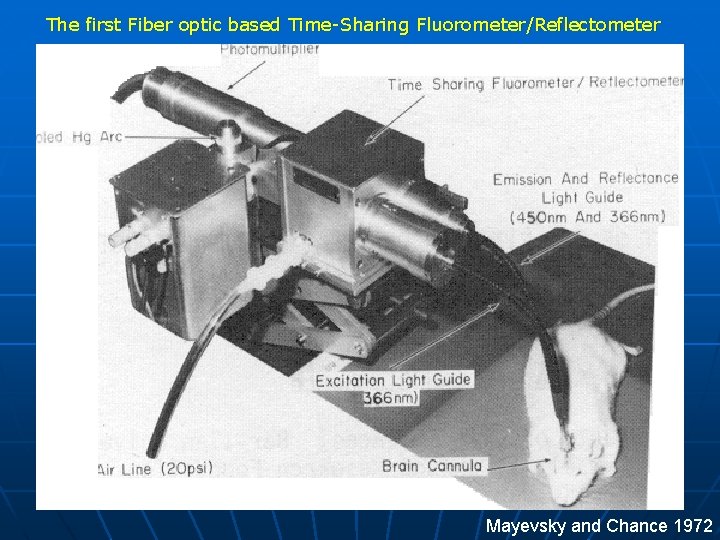
The first Fiber optic based Time-Sharing Fluorometer/Reflectometer Mayevsky and Chance 1972

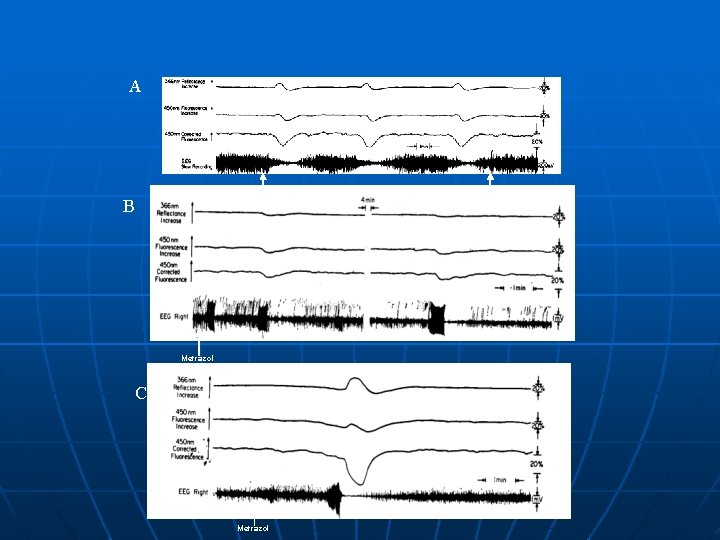
Anoxia A Ref Ischemia 100% Flu 100% CF 100% ECo. G Right B 100 m. V
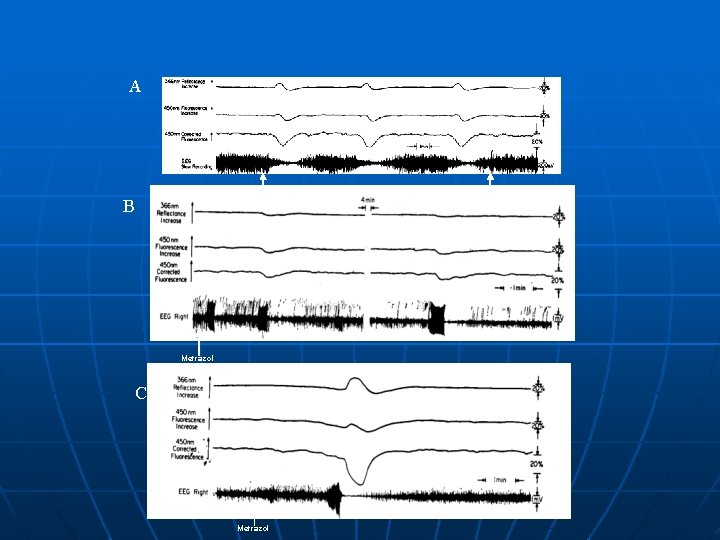
A KCl B Metrazol C Metrazol Na. Cl
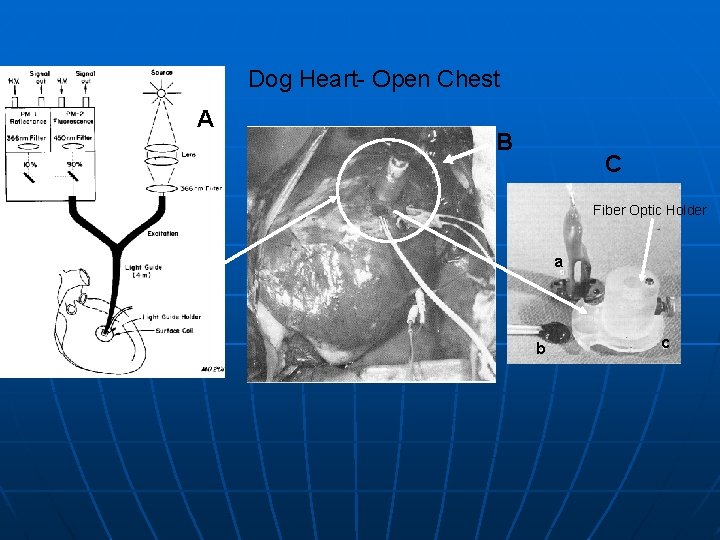
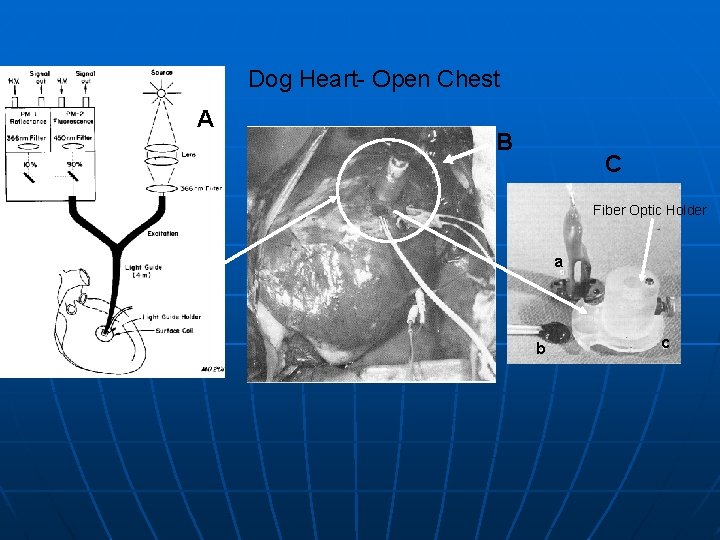
Dog Heart- Open Chest A B C Fiber Optic Holder a b c
A B
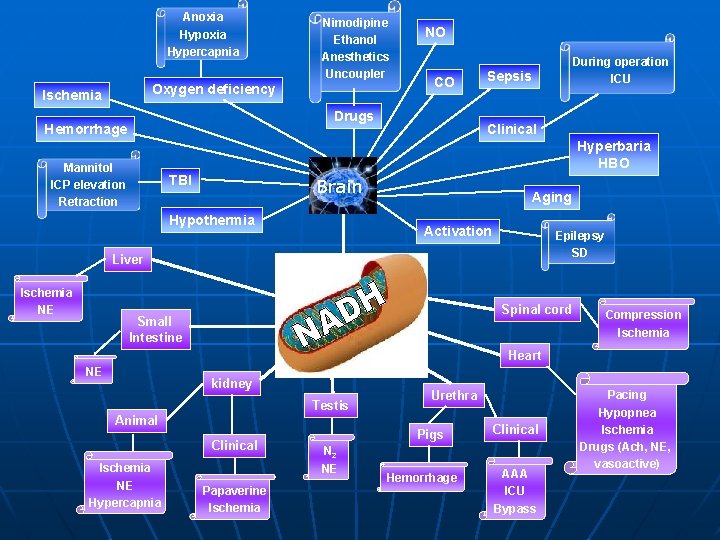
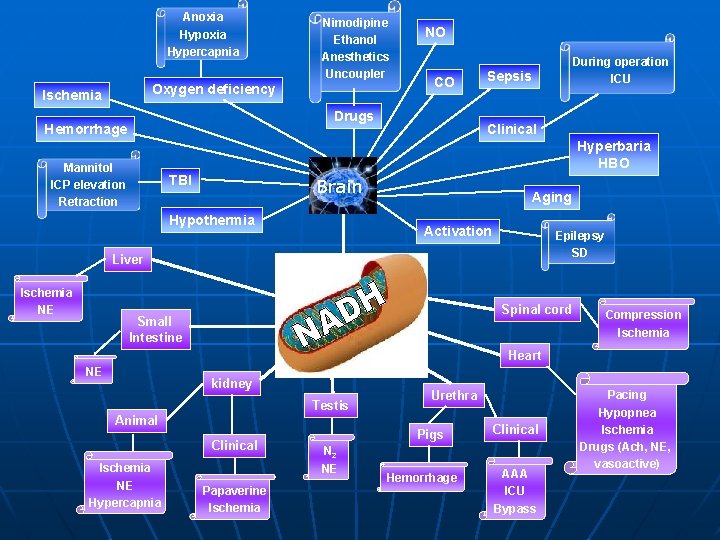
Anoxia Hypercapnia Nimodipine Ethanol Anesthetics Uncoupler Oxygen deficiency Ischemia NO CO Drugs Hemorrhage During operation ICU Sepsis Clinical Hyperbaria HBO Mannitol ICP elevation Retraction TBI Brain Hypothermia Aging Activation Epilepsy SD Liver Ischemia NE Spinal cord Small Intestine Compression Ischemia Heart NE kidney Testis Animal Clinical Ischemia NE Hypercapnia Papaverine Ischemia Urethra Pigs N 2 NE Hemorrhage Clinical AAA ICU Bypass Pacing Hypopnea Ischemia Drugs (Ach, NE, vasoactive)
Multiparametric Monitoring of Tissue Energy Metabolism WHY ?
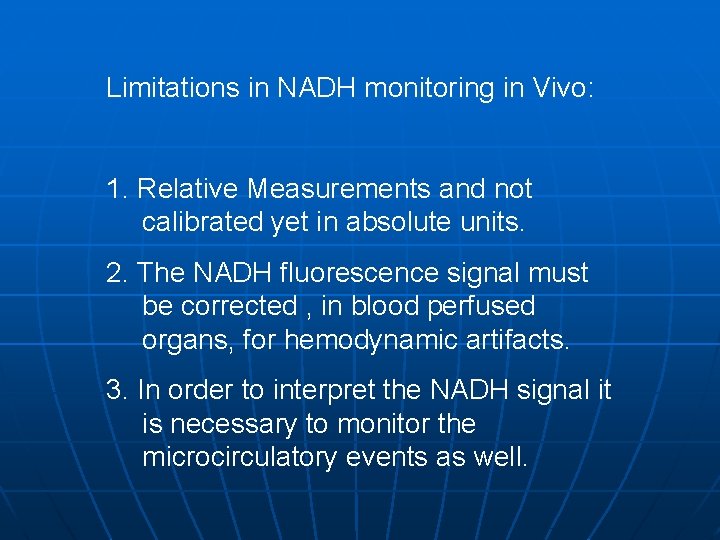
Limitations in NADH monitoring in Vivo: 1. Relative Measurements and not calibrated yet in absolute units. 2. The NADH fluorescence signal must be corrected , in blood perfused organs, for hemodynamic artifacts. 3. In order to interpret the NADH signal it is necessary to monitor the microcirculatory events as well.
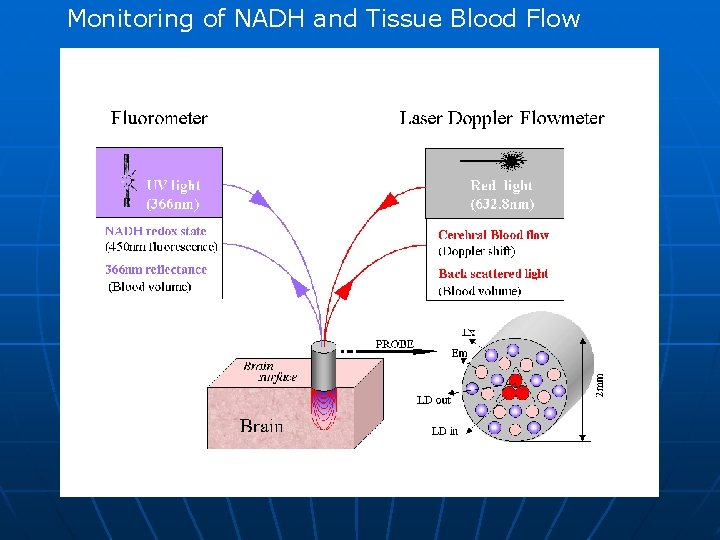
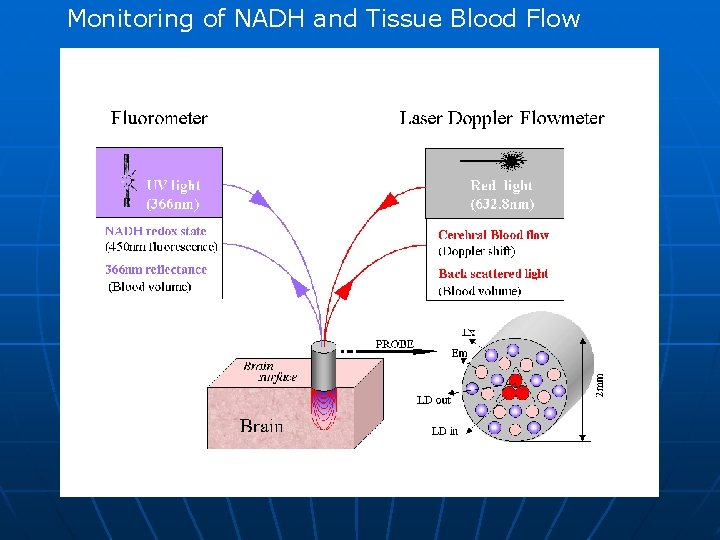
Monitoring of NADH and Tissue Blood Flow
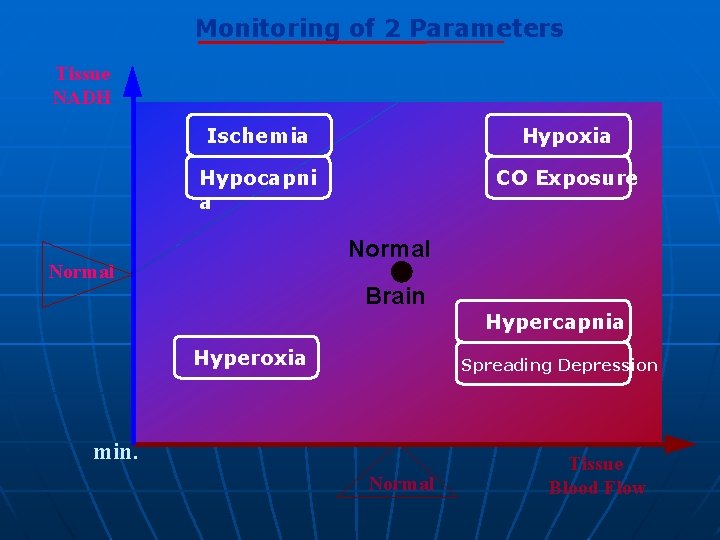
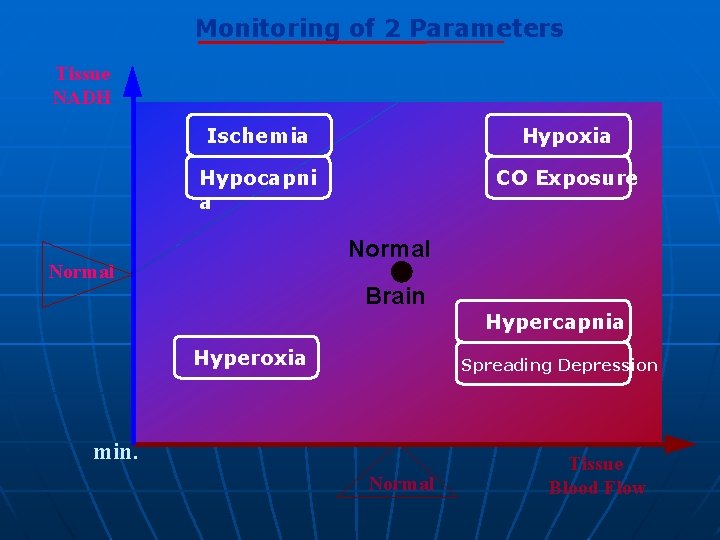
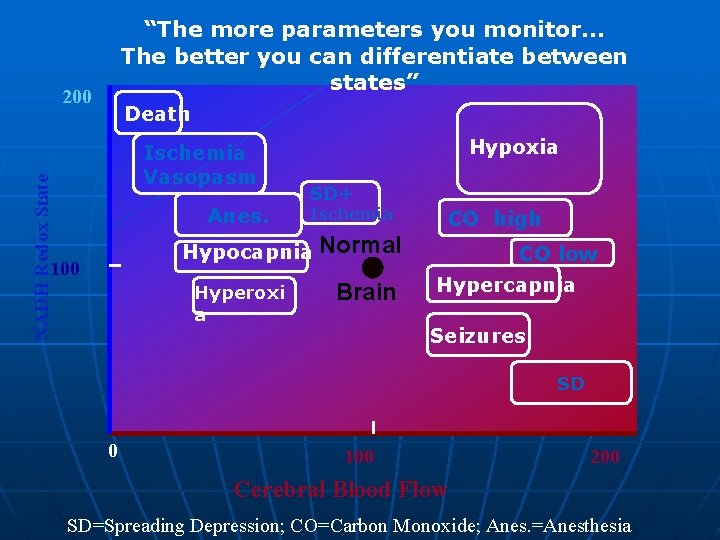
Monitoring of 2 Parameters Tissue NADH Ischemia Hypoxia Hypocapni a CO Exposure Normal Brain Hypercapnia Hyperoxia Spreading Depression min. Normal Tissue Blood Flow
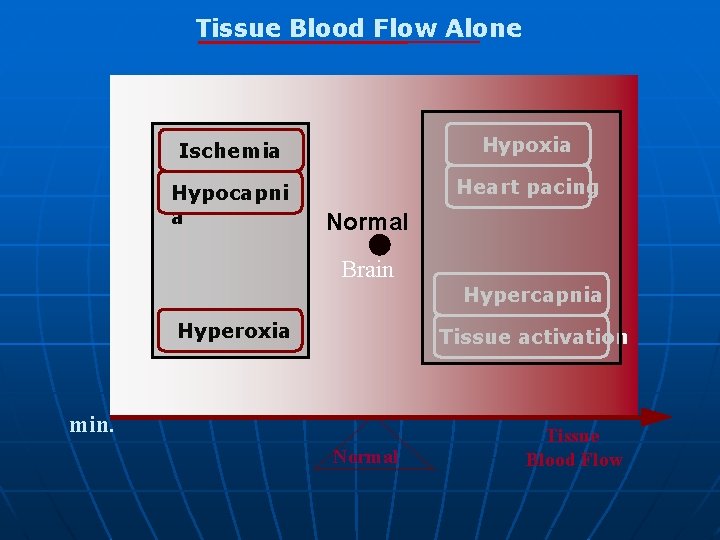
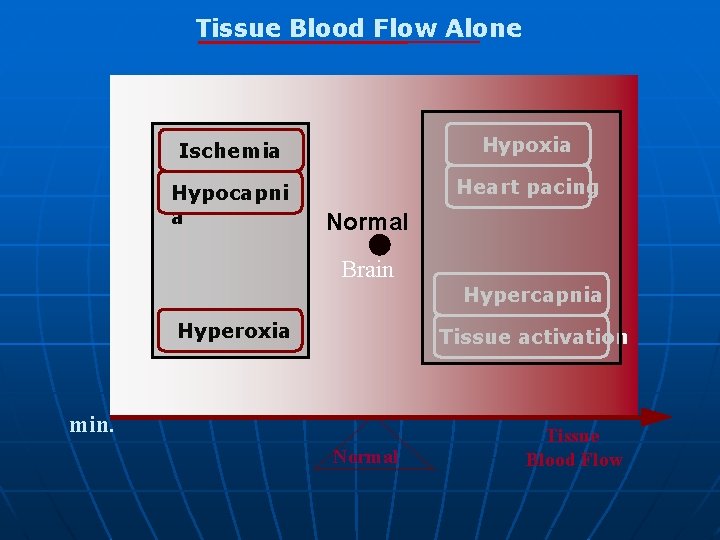
Tissue Blood Flow Alone Ischemia Hypoxia Hypocapni a Heart pacing Normal Brain Hypercapnia Hyperoxia Tissue activation min. Normal Tissue Blood Flow
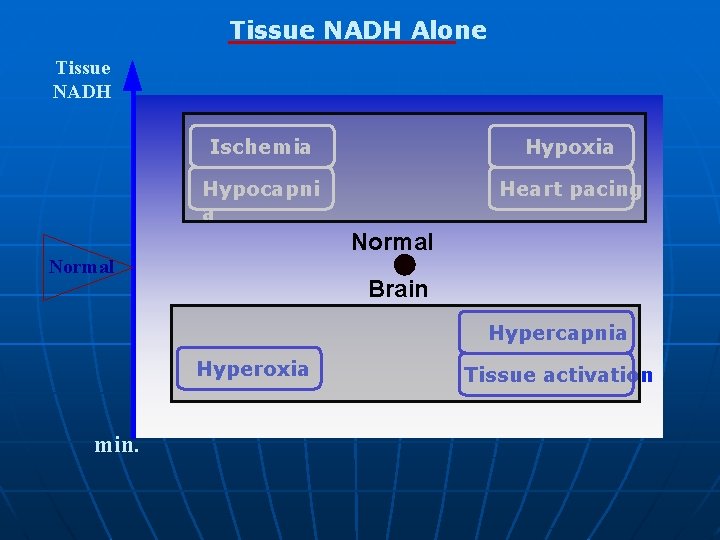
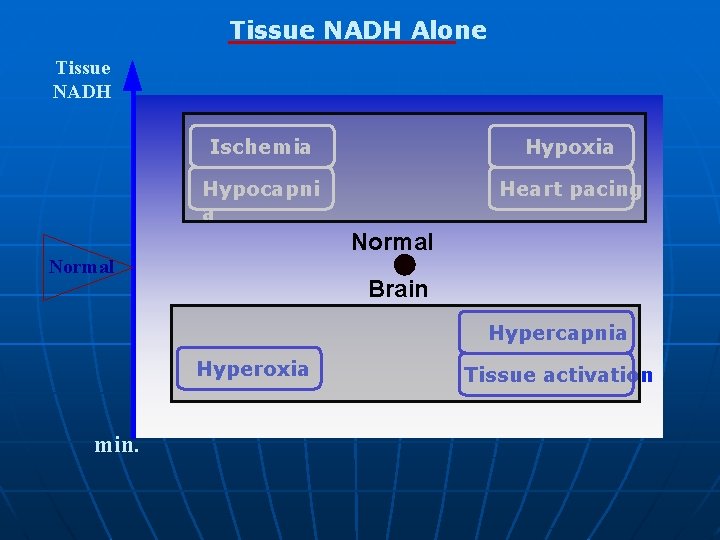
Tissue NADH Alone Tissue NADH Ischemia Hypoxia Hypocapni a Heart pacing Normal Brain Hypercapnia Hyperoxia min. Tissue activation
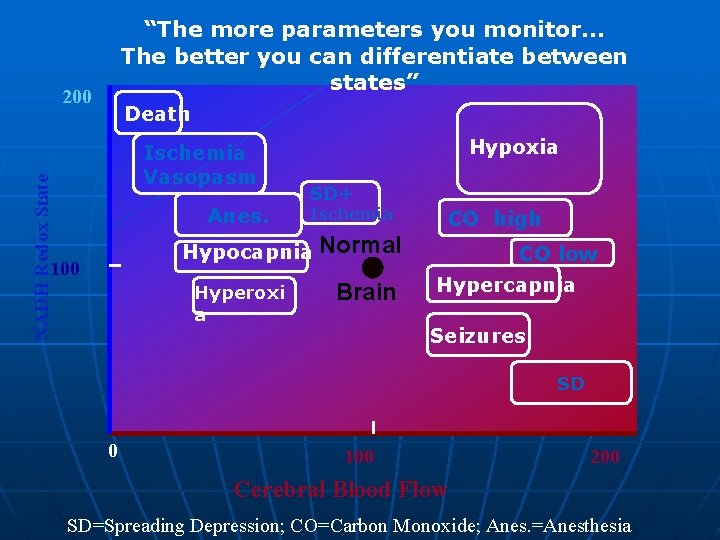
“The more parameters you monitor. . . The better you can differentiate between states” 200 Death NADH Redox State Ischemia Vasopasm Anes. Hypoxia SD+ Ischemia CO high Hypocapnia Normal 100 Hyperoxi a Brain CO low Hypercapnia Seizures SD 0 100 200 Cerebral Blood Flow SD=Spreading Depression; CO=Carbon Monoxide; Anes. =Anesthesia
Multiparametric Monitoring of Tissue Vitality in Vital and Less. Vital organs: Experimental Animal Results
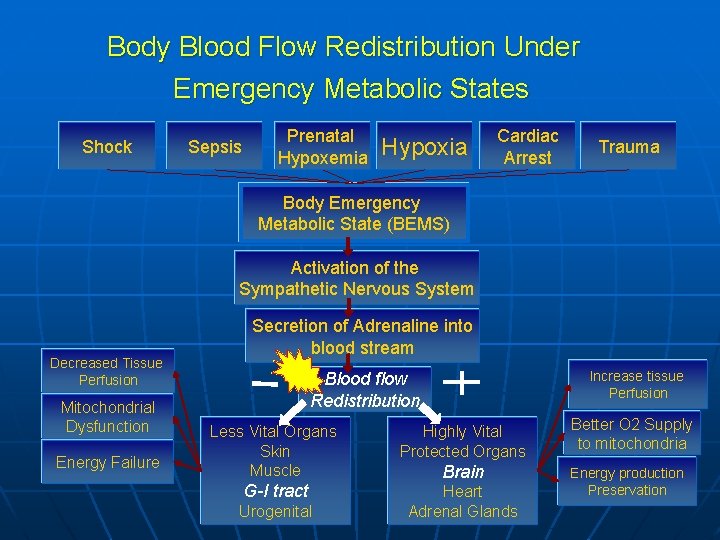
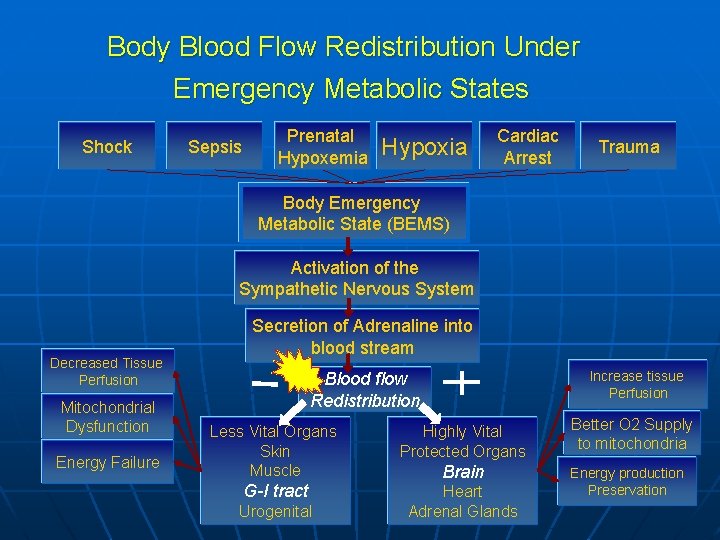
Body Blood Flow Redistribution Under Emergency Metabolic States Shock Sepsis Prenatal Hypoxemia Hypoxia Cardiac Arrest Trauma Body Emergency Metabolic State (BEMS) Activation of the Sympathetic Nervous System Decreased Tissue Perfusion Mitochondrial Dysfunction Energy Failure Secretion of Adrenaline into blood stream Increase tissue Perfusion Blood flow Redistribution Less Vital Organs Skin Muscle Highly Vital Protected Organs G-I tract Heart Adrenal Glands Urogenital Brain Better O 2 Supply to mitochondria Energy production 33 Preservation
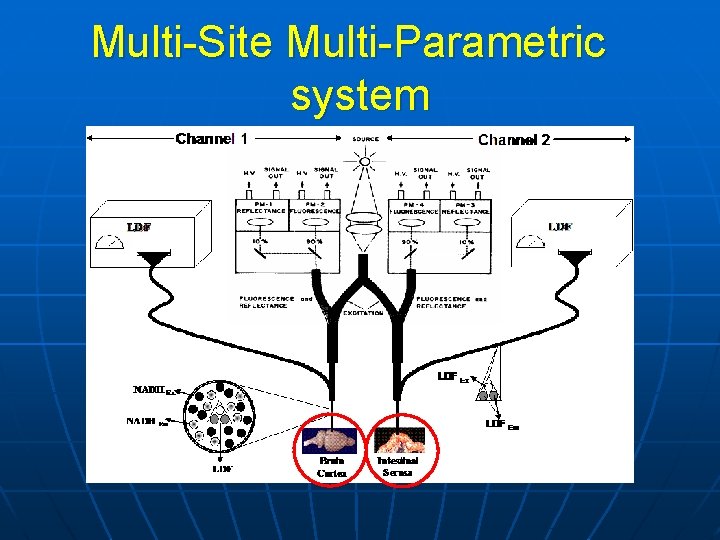
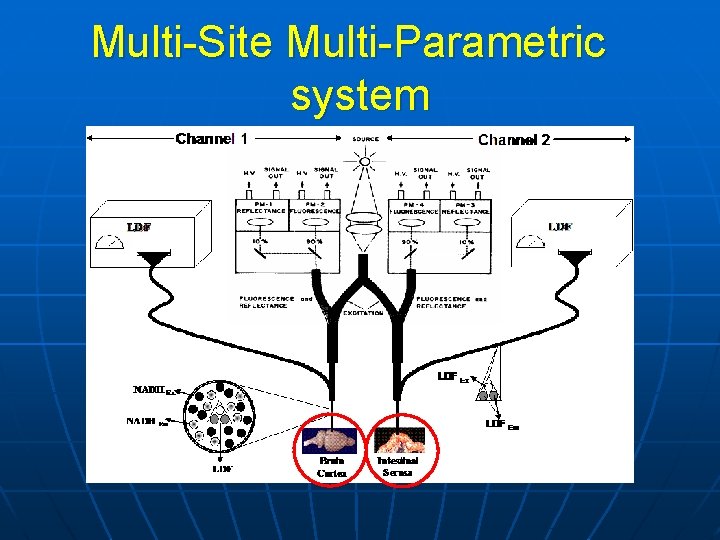
Multi-Site Multi-Parametric system
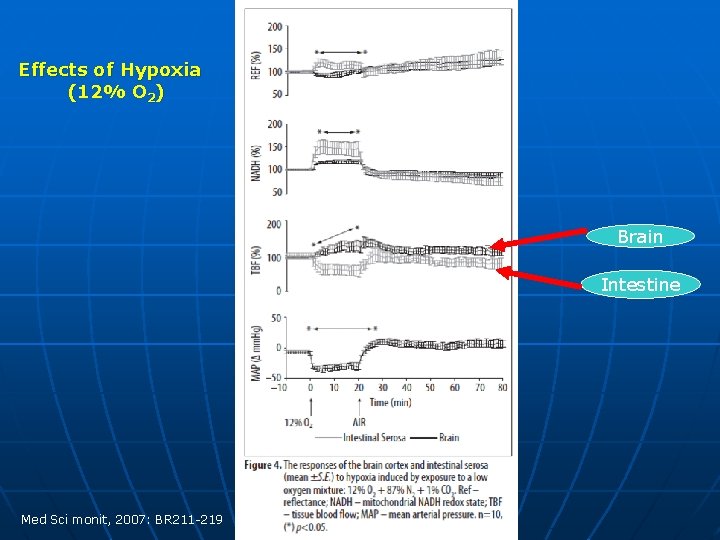
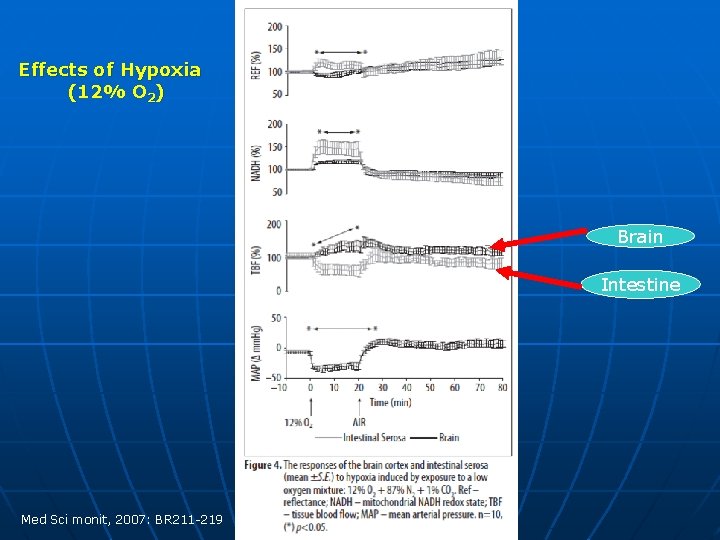
Effects of Hypoxia (12% O 2) Brain Intestine Med Sci monit, 2007: BR 211 -219
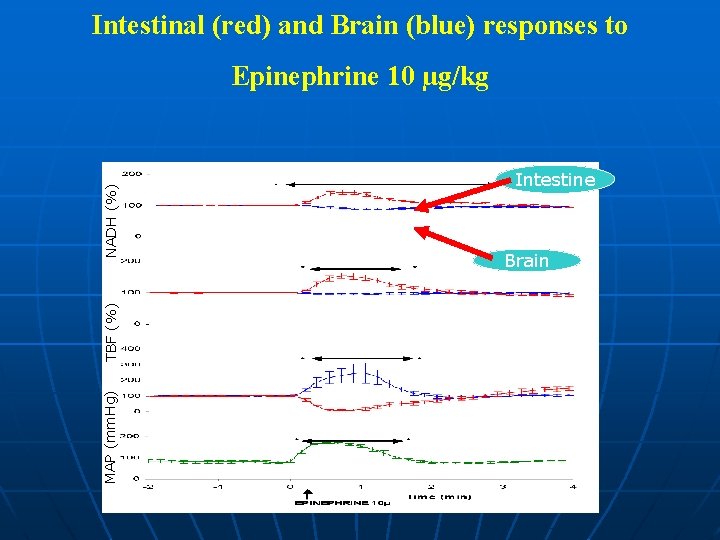
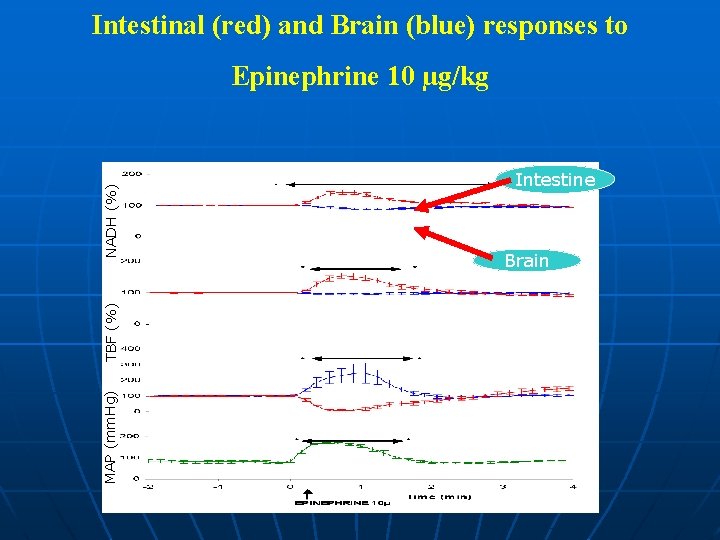
Intestinal (red) and Brain (blue) responses to MAP (mm. Hg) TBF (%) NADH (%) Epinephrine 10 µg/kg Intestine Brain
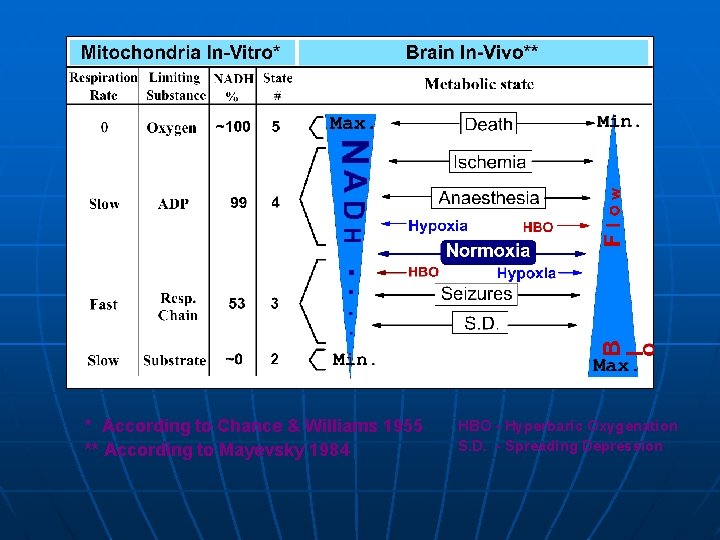
* According to Chance & Williams 1955 ** According to Mayevsky 1984 HBO - Hyperbaric Oxygenation S. D. - Spreading Depression
Critical Clinical Situations Requiring Measurement of Tissue and Body Vitality
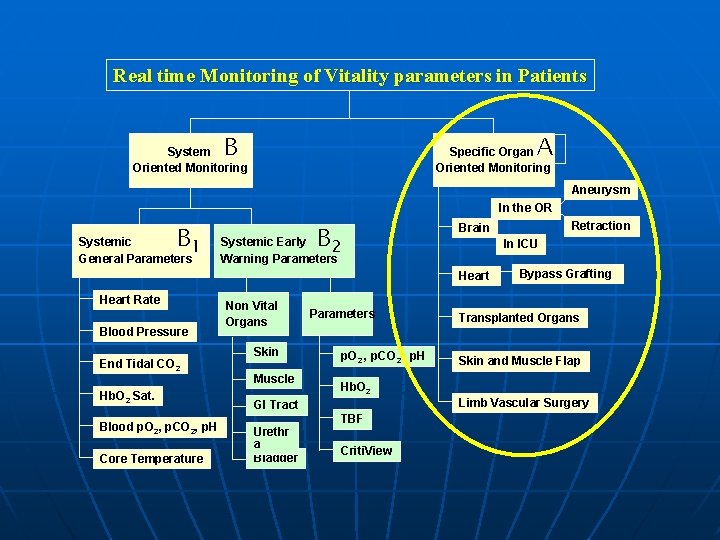
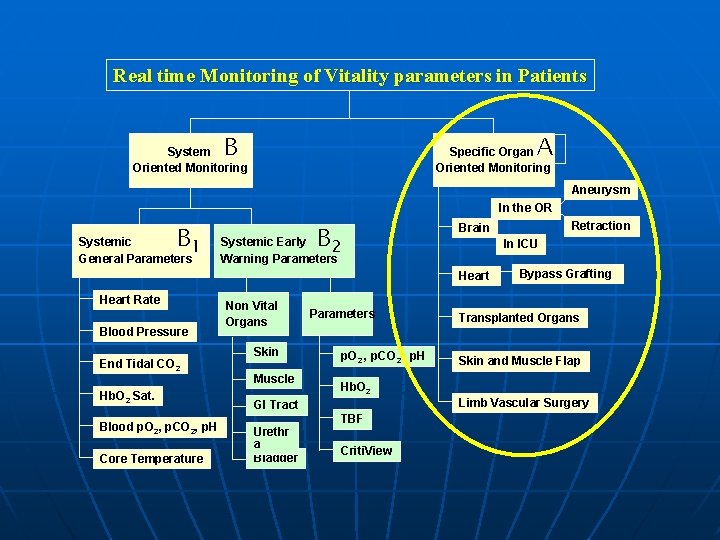
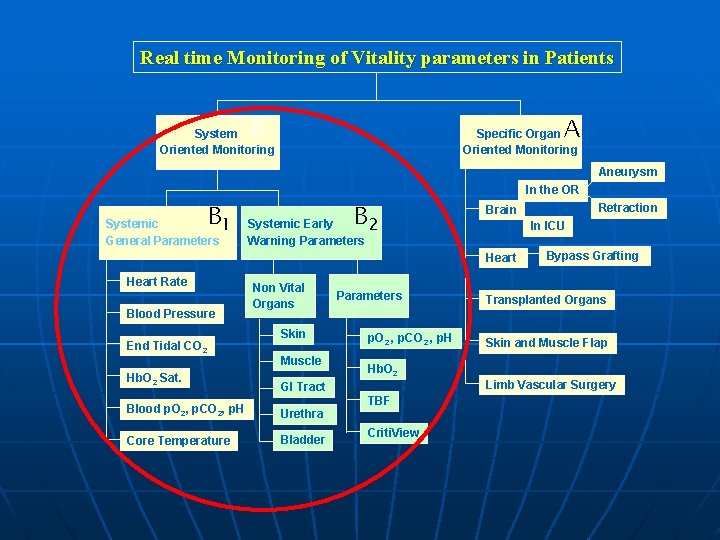
Real time Monitoring of Vitality parameters in Patients A B System Oriented Monitoring Specific Organ Oriented Monitoring Aneurysm In the OR B Systemic 1 General Parameters B Systemic Early 2 Warning Parameters In ICU Heart Rate Blood Pressure End Tidal CO 2 Hb. O 2 Sat. Blood p. O 2, p. CO 2, p. H Core Temperature Non Vital Organs Skin Muscle Parameters p. O 2 , p. CO 2 , p. H Hb. O 2 GI Tract Urethr a Bladder Retraction Brain TBF Criti. View Bypass Grafting Transplanted Organs Skin and Muscle Flap Limb Vascular Surgery
Monitoring of Specific Organ Vitality in Patients
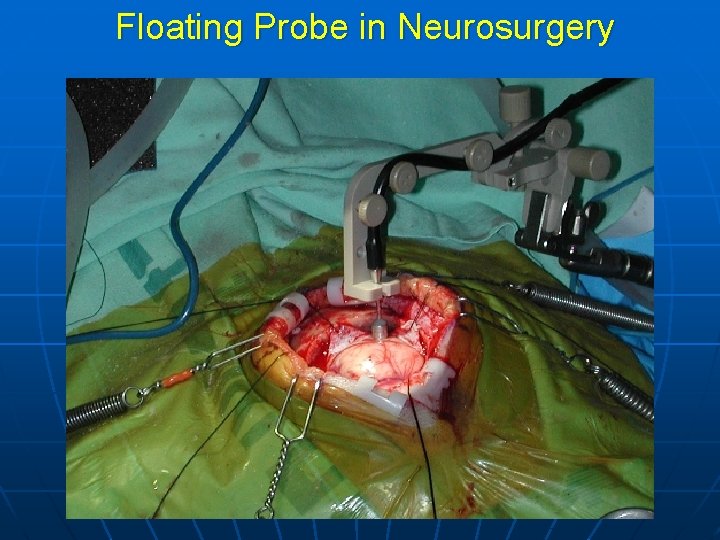
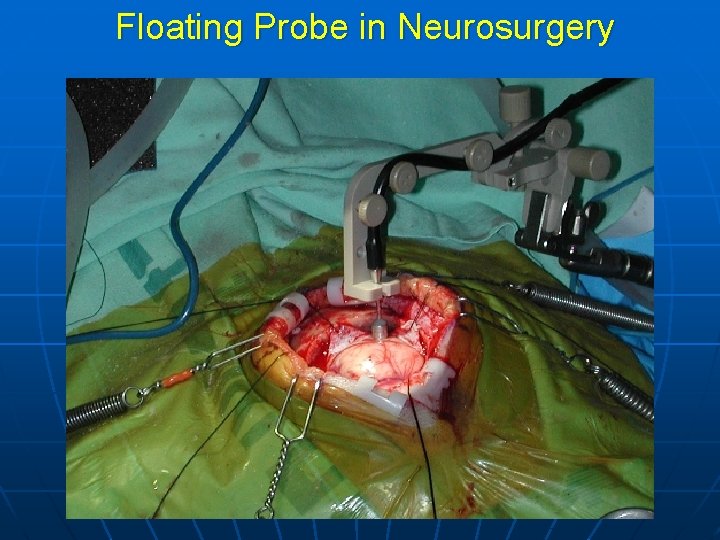
Floating Probe in Neurosurgery
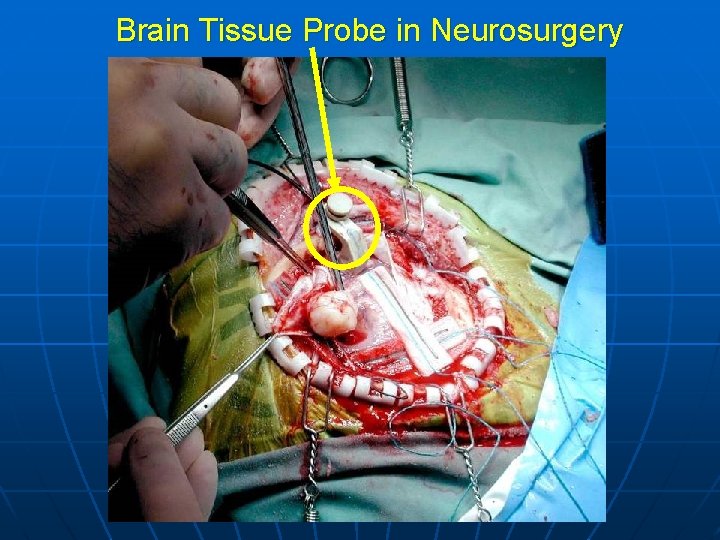
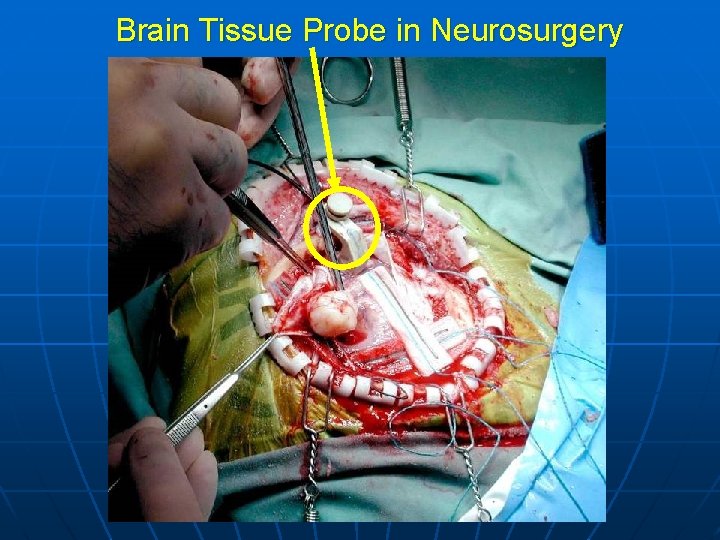
Brain Tissue Probe in Neurosurgery
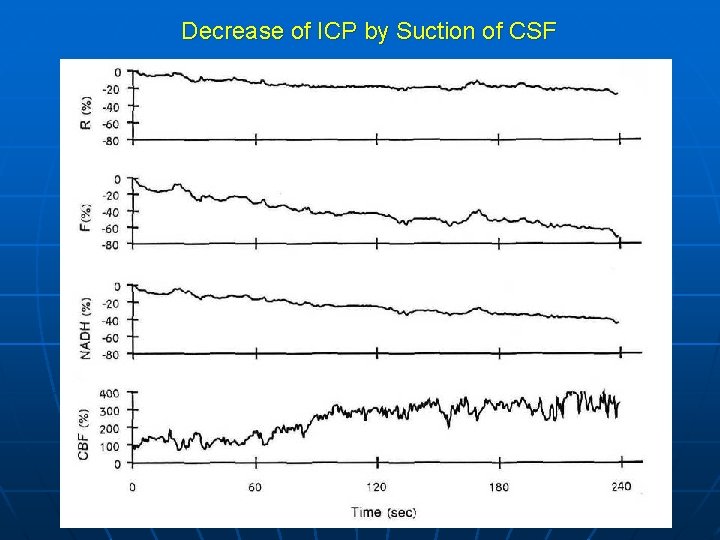
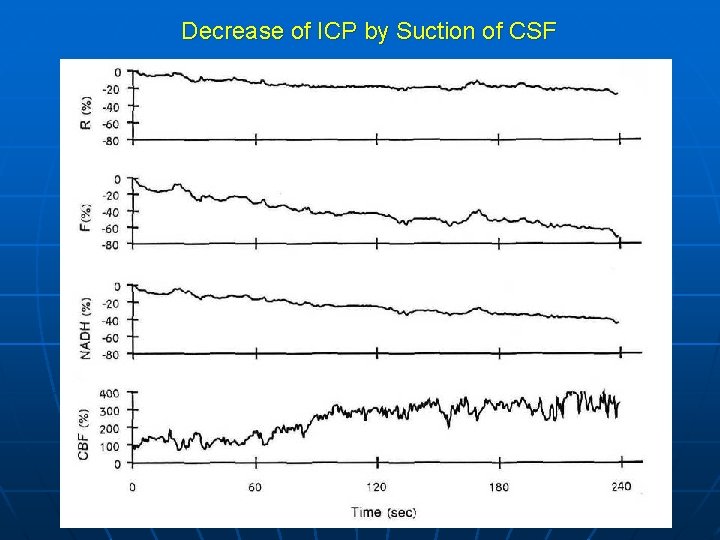
Decrease of ICP by Suction of CSF
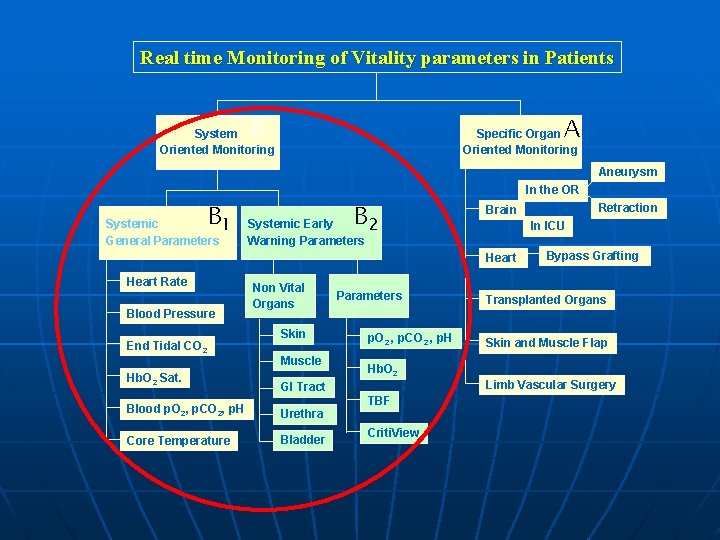
Real time Monitoring of Vitality parameters in Patients A B System Oriented Monitoring Specific Organ Oriented Monitoring Aneurysm In the OR B 1 Systemic General Parameters B 2 Systemic Early Warning Parameters In ICU Heart Rate Blood Pressure End Tidal CO 2 Hb. O 2 Sat. Non Vital Organs Skin Muscle Parameters p. O 2 , p. CO 2 , p. H Hb. O 2 GI Tract Blood p. O 2, p. CO 2, p. H Urethra Core Temperature Bladder TBF Criti. View Retraction Brain Bypass Grafting Transplanted Organs Skin and Muscle Flap Limb Vascular Surgery
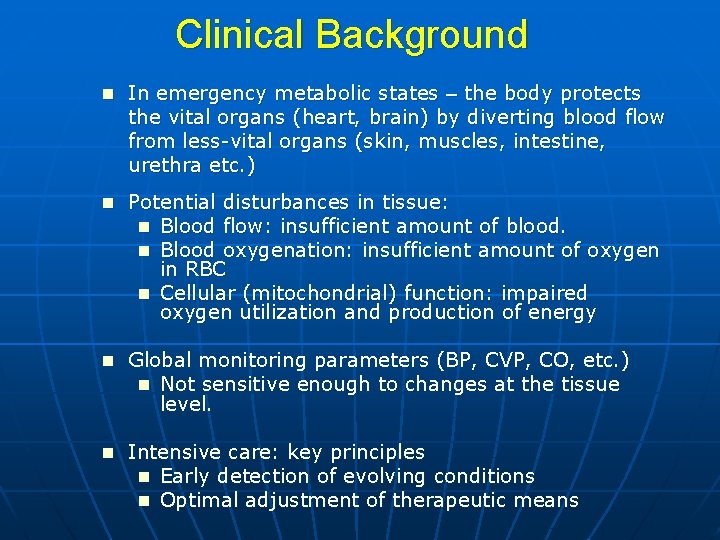
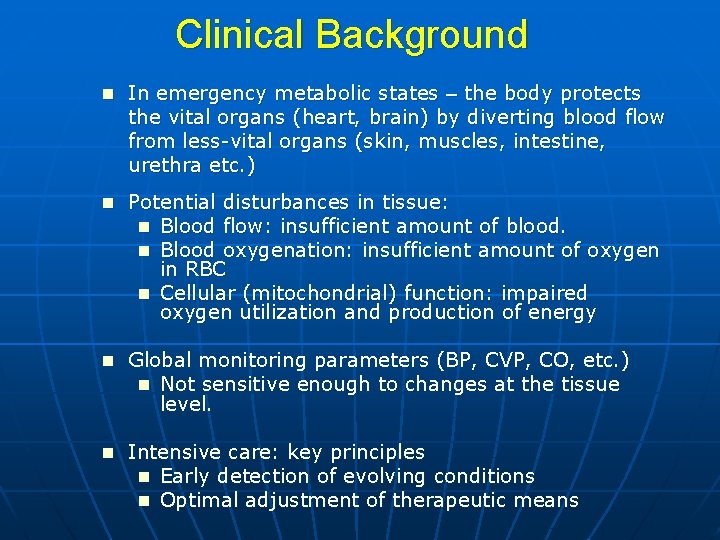
Clinical Background n In emergency metabolic states – the body protects the vital organs (heart, brain) by diverting blood flow from less-vital organs (skin, muscles, intestine, urethra etc. ) n Potential disturbances in tissue: n Blood flow: insufficient amount of blood. n Blood oxygenation: insufficient amount of oxygen in RBC n Cellular (mitochondrial) function: impaired oxygen utilization and production of energy n Global monitoring parameters (BP, CVP, CO, etc. ) n Not sensitive enough to changes at the tissue level. n Intensive care: key principles n Early detection of evolving conditions n Optimal adjustment of therapeutic means
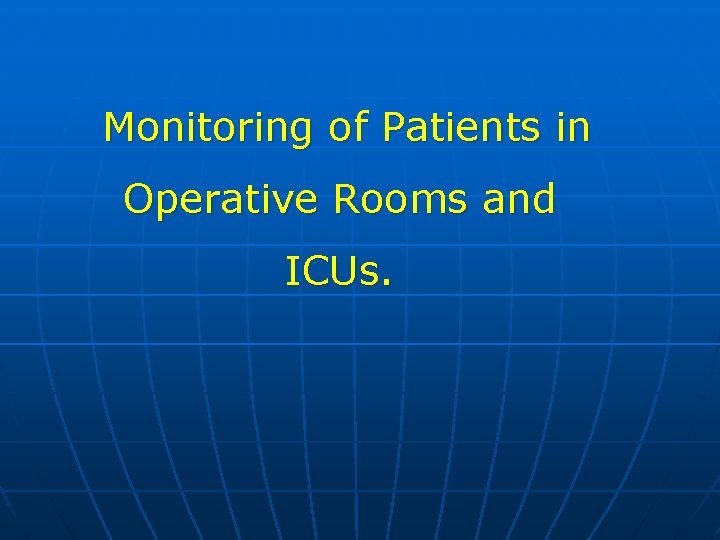
Monitoring of Patients in Operative Rooms and ICUs.
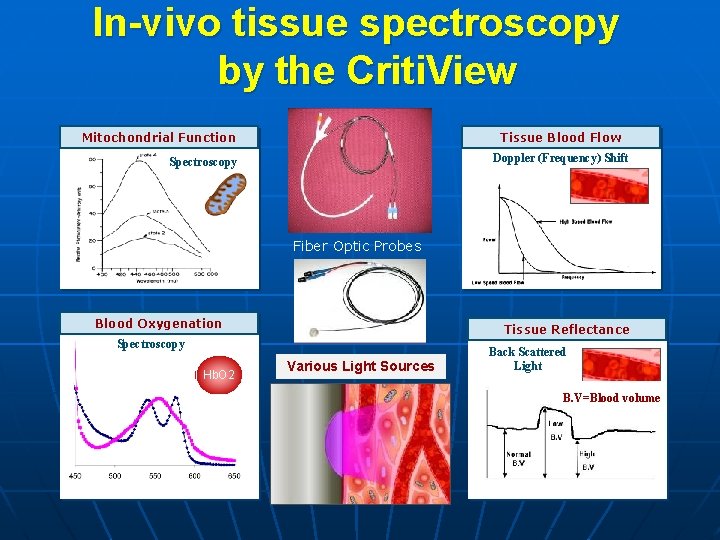
160 Oxygen Partial Pressure (mm. Hg) 150 O 2 End Tidal N 2 CO 2 Heart Rate &ECG Cardiac Output 100 95 Systemic Blood Pressure 100 Systemic Saturation (Pulse Oximetry) Criti. View Microcirculation blood flow and oxygenation 50 20 -30 NADH redox state 1 0 AIR Alveoli Arterial Blood Tissue Intramitochondrial
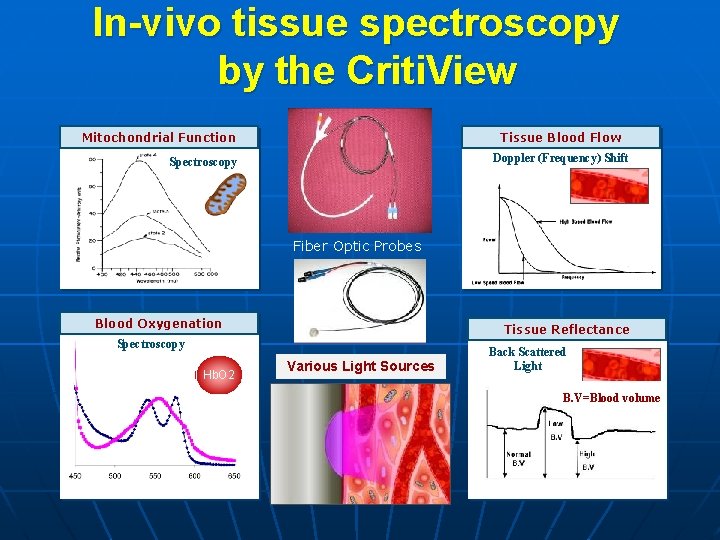
In-vivo tissue spectroscopy by the Criti. View Tissue Blood Flow Mitochondrial Function Doppler (Frequency) Shift Spectroscopy NADH Fiber Optic Probes Blood Oxygenation Tissue Reflectance Spectroscopy Hb. O 2 Various Light Sources Back Scattered Light B. V=Blood volume Wavelength (nm) Time (Sec)
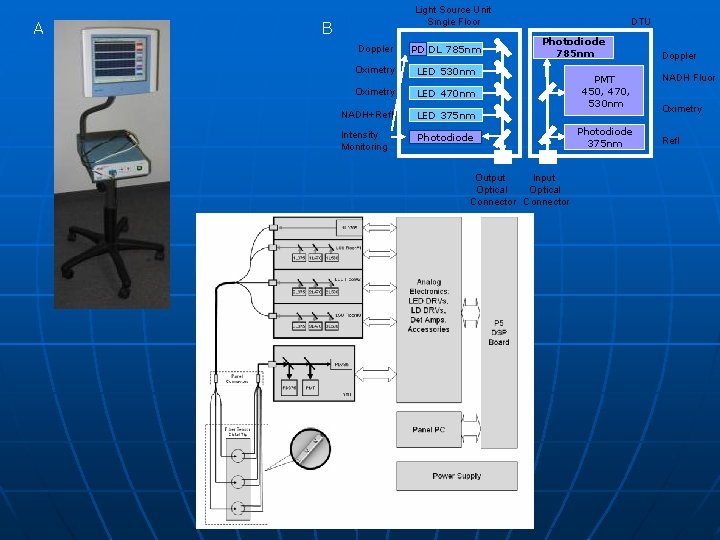
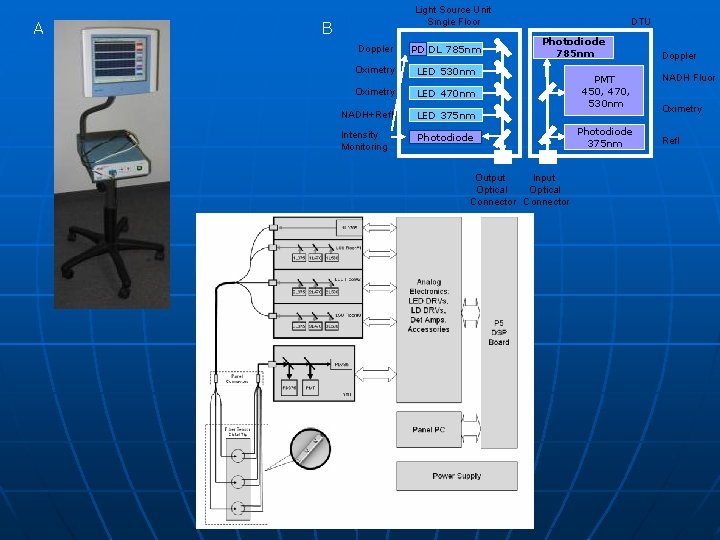
A Light Source Unit Single Floor B Doppler PD DL 785 nm Oximetry LED 530 nm Oximetry LED 470 nm NADH+Refl LED 375 nm Intensity Monitoring Photodiode DTU Photodiode 785 nm Output Input Optical Connector C PMT 450, 470, 530 nm Photodiode 375 nm Doppler NADH Fluor Oximetry Refl
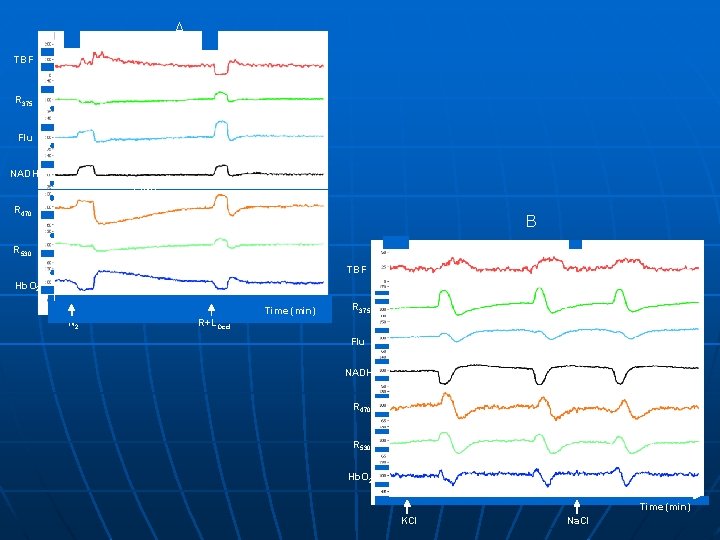
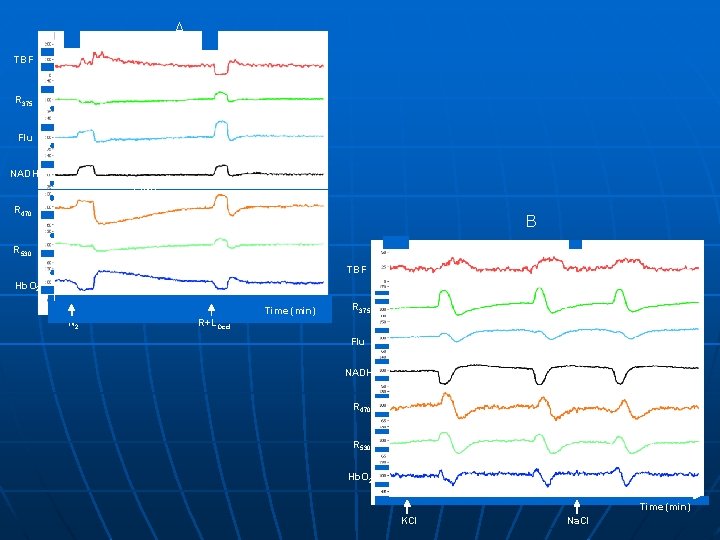
A TBF R 375 Flu NADH 2 min R 470 B R 530 TBF Hb. O 2 Time (min) N 2 R 375 R+LOccl Flu NADH 2 min R 470 R 530 Hb. O 2 Time (min) KCl Na. Cl
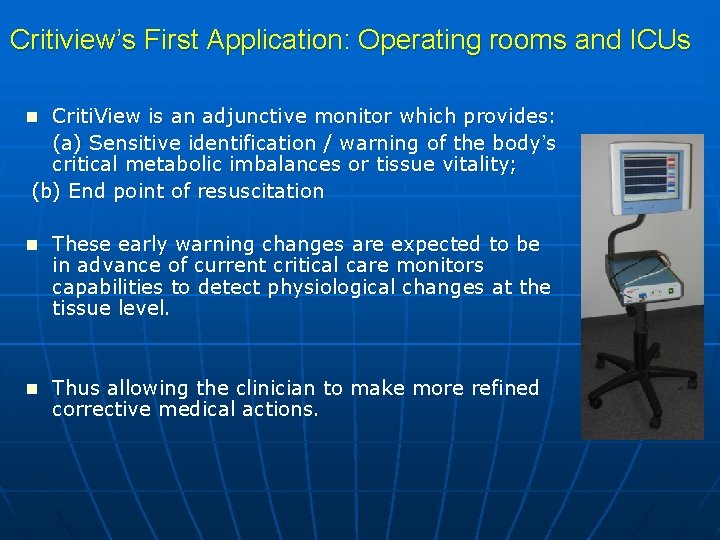
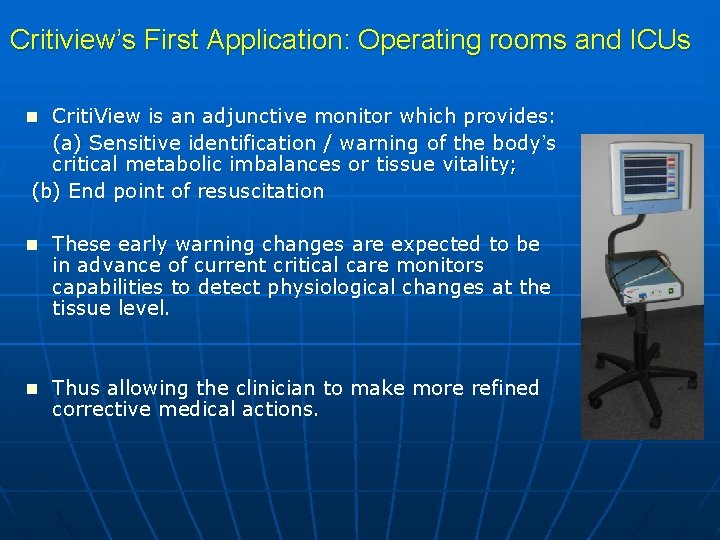
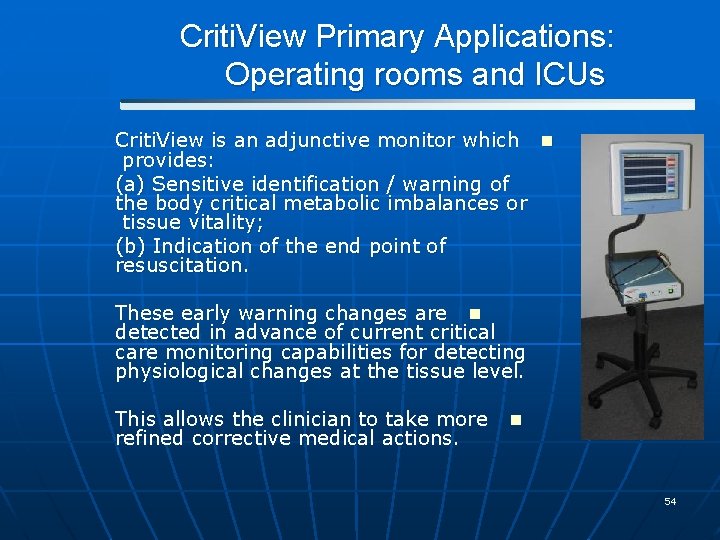
Critiview’s First Application: Operating rooms and ICUs n Criti. View is an adjunctive monitor which provides: (a) Sensitive identification / warning of the body’s critical metabolic imbalances or tissue vitality; (b) End point of resuscitation n These early warning changes are expected to be in advance of current critical care monitors capabilities to detect physiological changes at the tissue level. n Thus allowing the clinician to make more refined corrective medical actions.
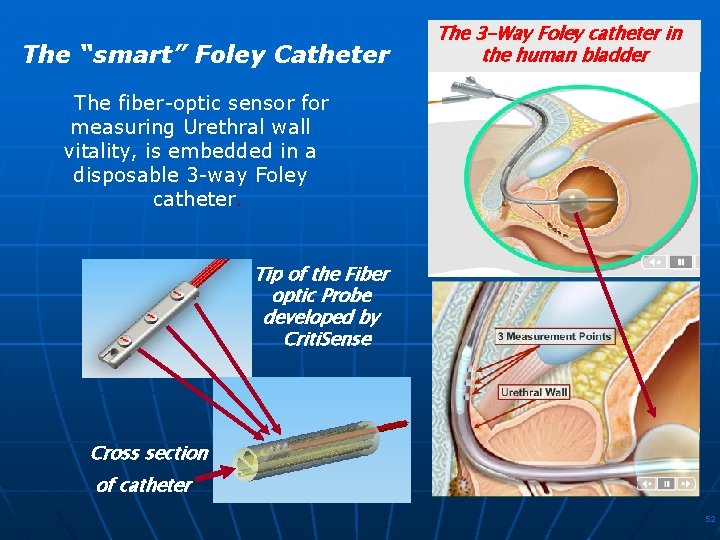
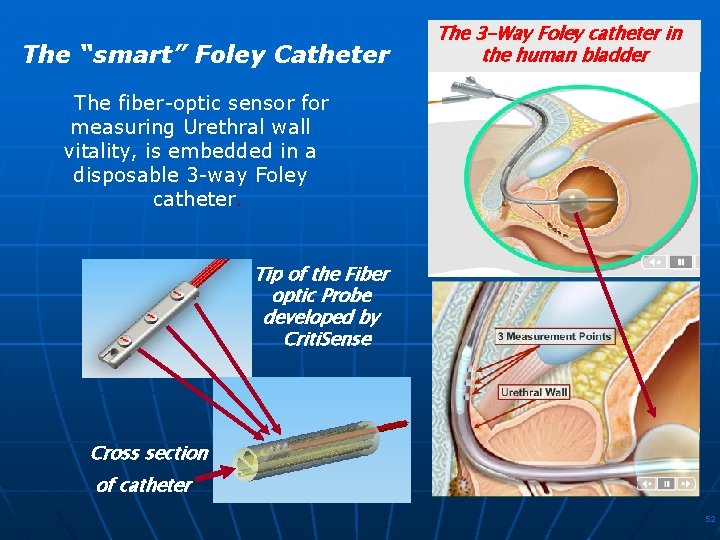
The “smart” Foley Catheter The 3 -Way Foley catheter in the human bladder The fiber-optic sensor for measuring Urethral wall vitality, is embedded in a disposable 3 -way Foley catheter. Tip of the Fiber optic Probe developed by Criti. Sense Cross section of catheter 52
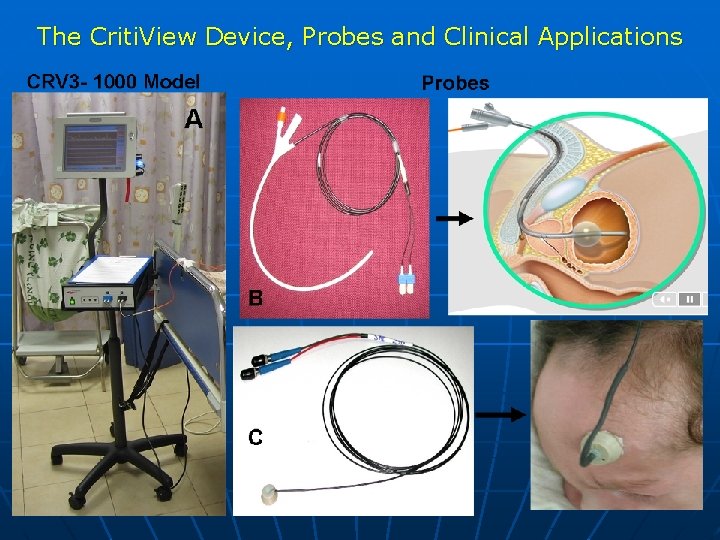
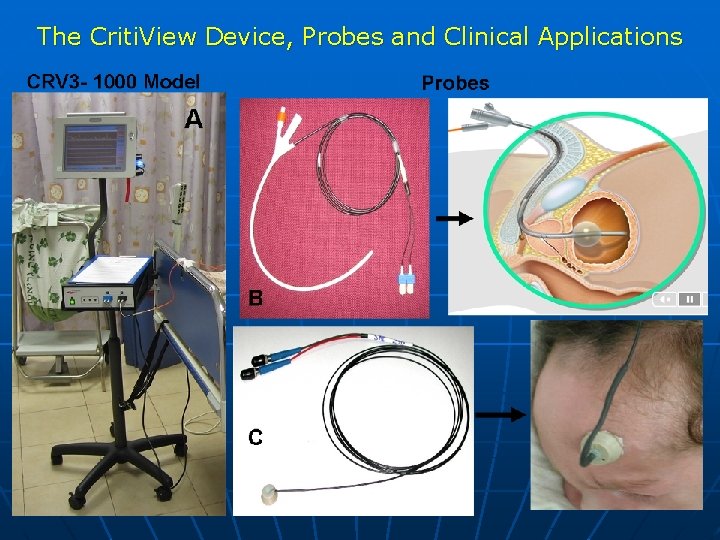
The Criti. View Device, Probes and Clinical Applications
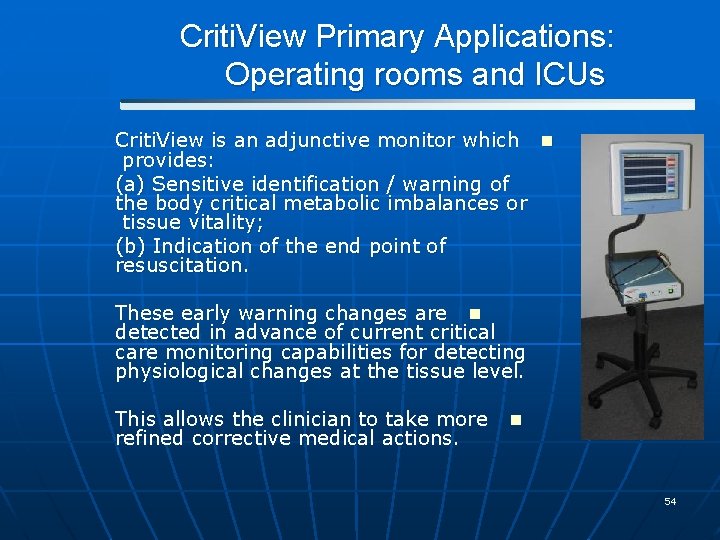
Criti. View Primary Applications: Operating rooms and ICUs Criti. View is an adjunctive monitor which n provides: (a) Sensitive identification / warning of the body critical metabolic imbalances or tissue vitality; (b) Indication of the end point of resuscitation. These early warning changes are n detected in advance of current critical care monitoring capabilities for detecting physiological changes at the tissue level. This allows the clinician to take more n refined corrective medical actions. 54
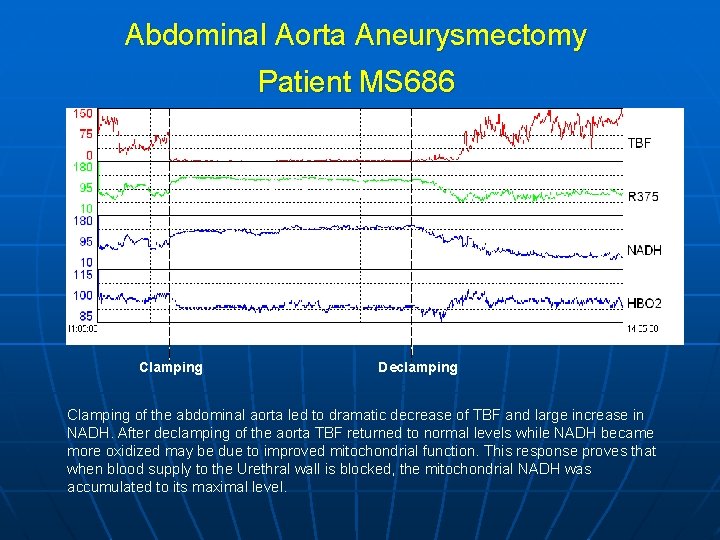
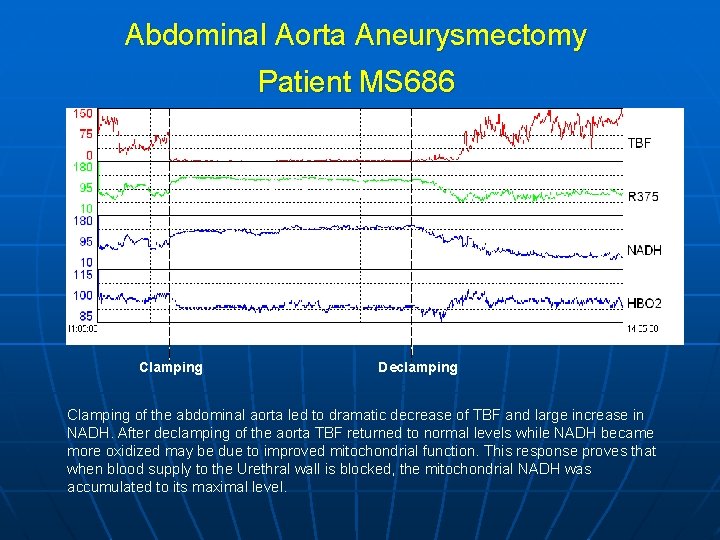
Abdominal Aorta Aneurysmectomy Patient MS 686 10 min Clamping Declamping Clamping of the abdominal aorta led to dramatic decrease of TBF and large increase in NADH. After declamping of the aorta TBF returned to normal levels while NADH became more oxidized may be due to improved mitochondrial function. This response proves that when blood supply to the Urethral wall is blocked, the mitochondrial NADH was accumulated to its maximal level.
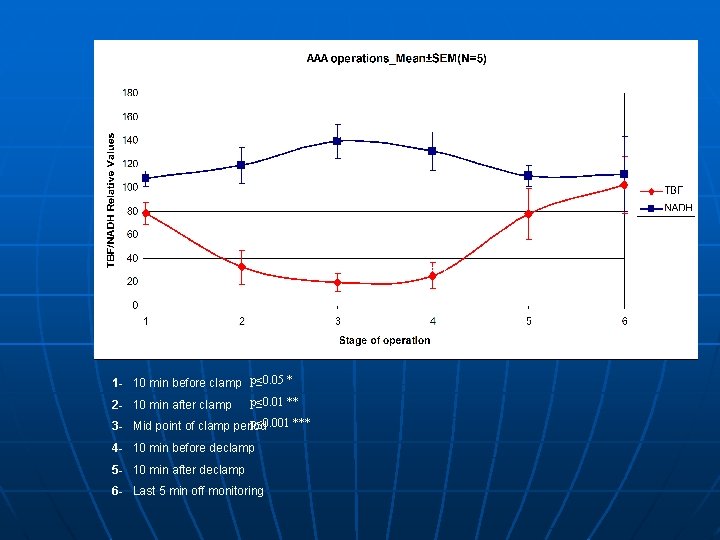
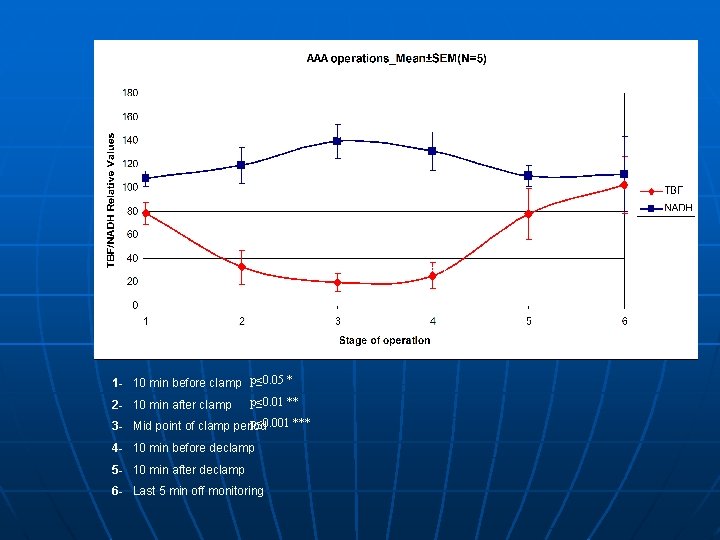
* ** 1 - 10 min before clamp p≤ 0. 05 * 2 - 10 min after clamp p≤ 0. 01 ** p≤ 0. 001 *** 3 - Mid point of clamp period 4 - 10 min before declamp 5 - 10 min after declamp 6 - Last 5 min off monitoring *** **
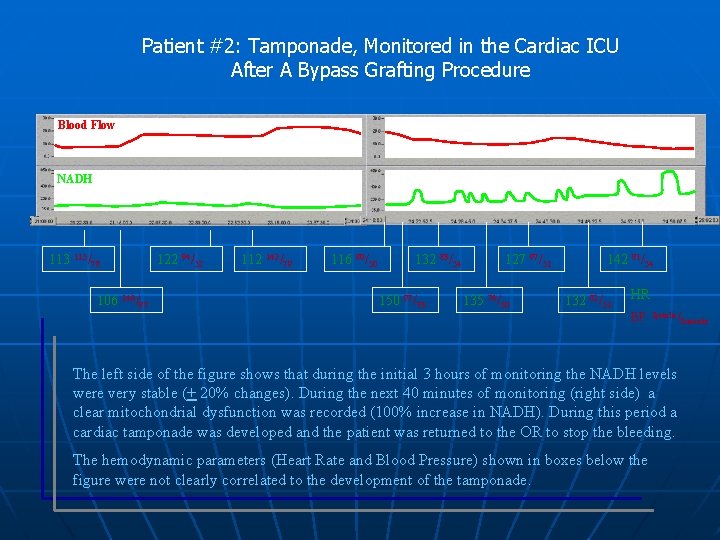
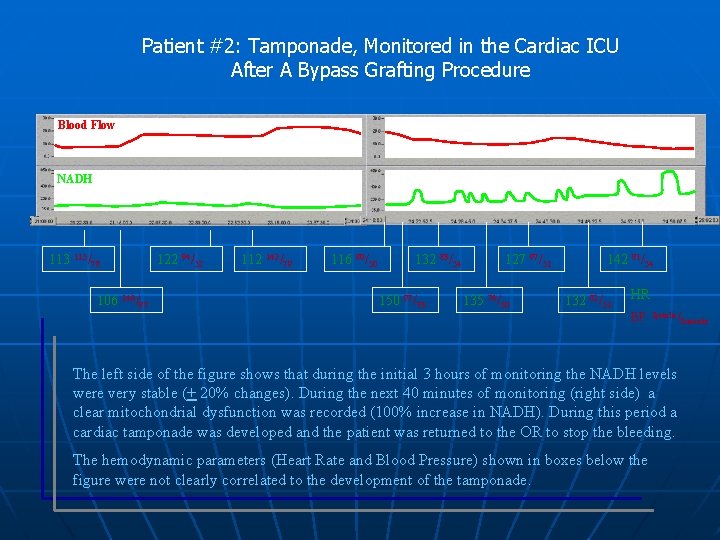
Patient #2: Tamponade, Monitored in the Cardiac ICU After A Bypass Grafting Procedure Blood Flow NADH 113 115/78 106 146/87 122 94/52 112 142/79 116 80/50 132 83/54 150 97/73 127 97/51 135 76/50 142 81/54 132 82/51 HR BP Systolic / The left side of the figure shows that during the initial 3 hours of monitoring the NADH levels were very stable (+ 20% changes). During the next 40 minutes of monitoring (right side) a clear mitochondrial dysfunction was recorded (100% increase in NADH). During this period a cardiac tamponade was developed and the patient was returned to the OR to stop the bleeding. The hemodynamic parameters (Heart Rate and Blood Pressure) shown in boxes below the figure were not clearly correlated to the development of the tamponade. Diastolic
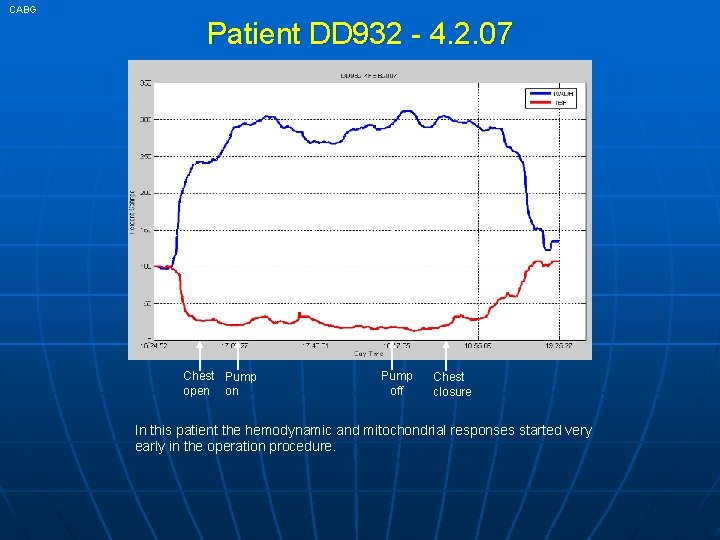
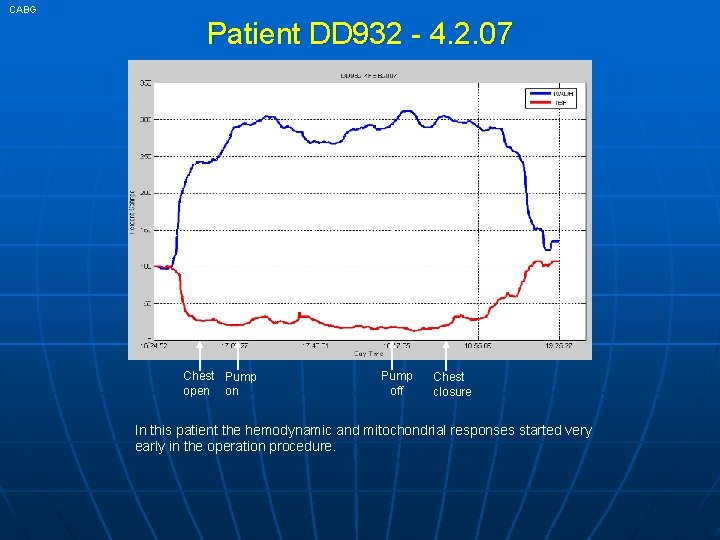
CABG Patient DD 932 - 4. 2. 07 38 min Chest Pump open on Pump off Chest closure In this patient the hemodynamic and mitochondrial responses started very early in the operation procedure.
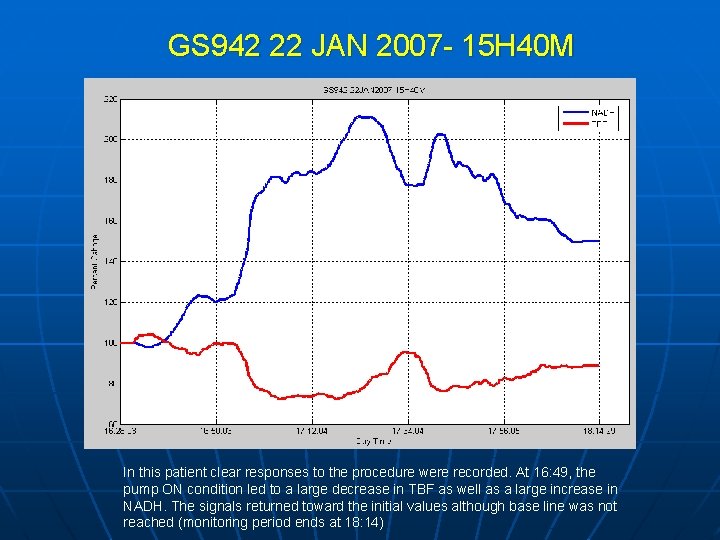
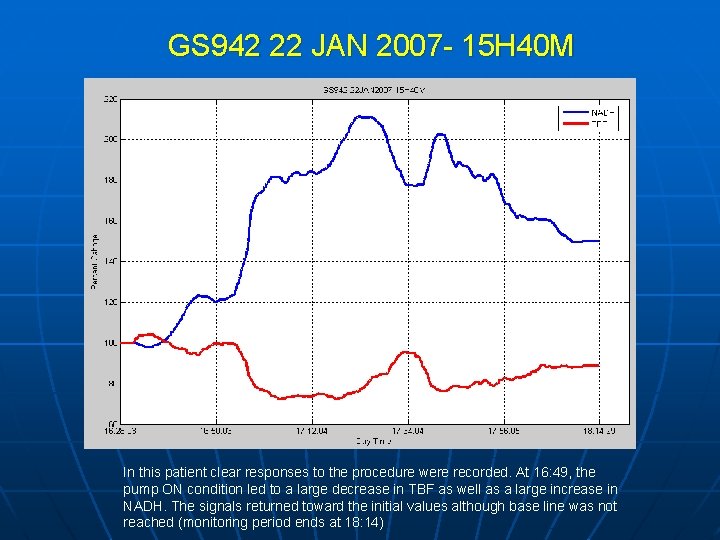
GS 942 22 JAN 2007 - 15 H 40 M 22 min In this patient clear responses to the procedure were recorded. At 16: 49, the pump ON condition led to a large decrease in TBF as well as a large increase in NADH. The signals returned toward the initial values although base line was not reached (monitoring period ends at 18: 14)
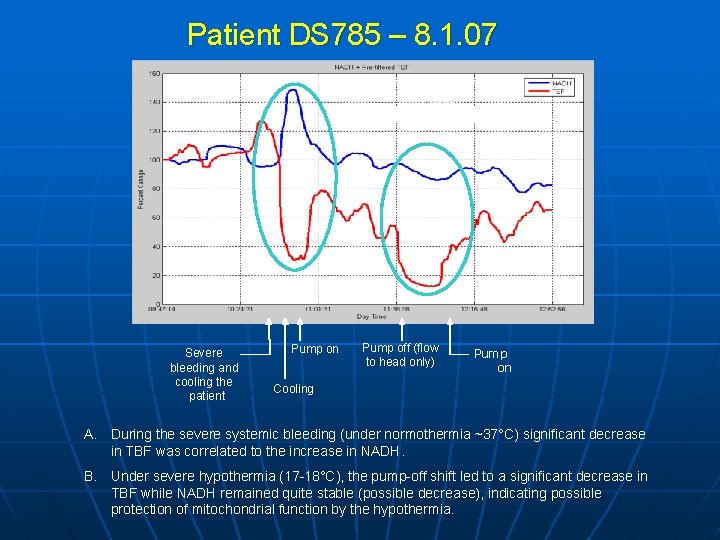
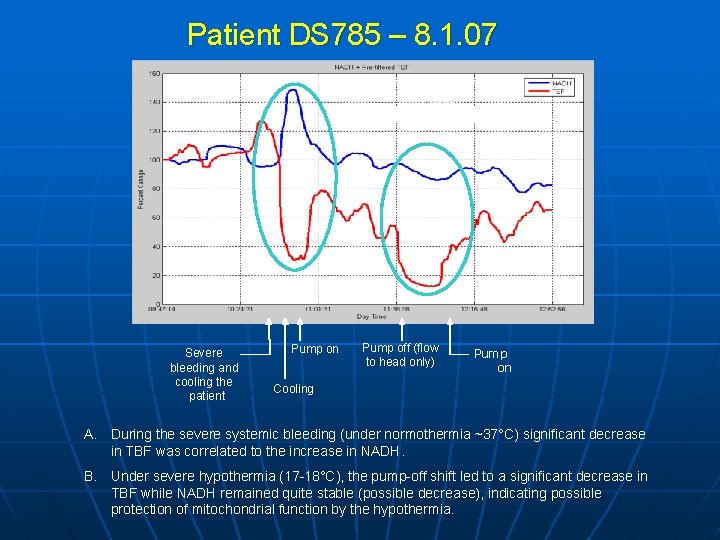
Patient DS 785 – 8. 1. 07 37 min A B Severe bleeding and cooling the patient Pump on Pump off (flow to head only) Pump on Cooling A. During the severe systemic bleeding (under normothermia ~37°C) significant decrease in TBF was correlated to the increase in NADH. B. Under severe hypothermia (17 -18°C), the pump-off shift led to a significant decrease in TBF while NADH remained quite stable (possible decrease), indicating possible protection of mitochondrial function by the hypothermia.
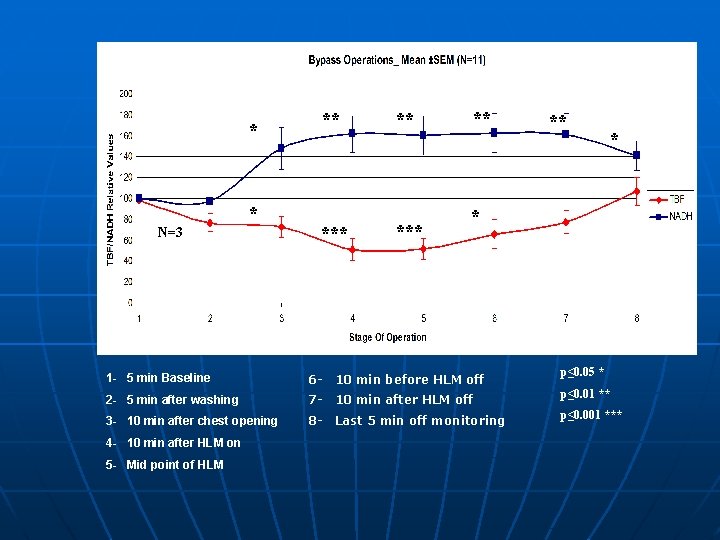
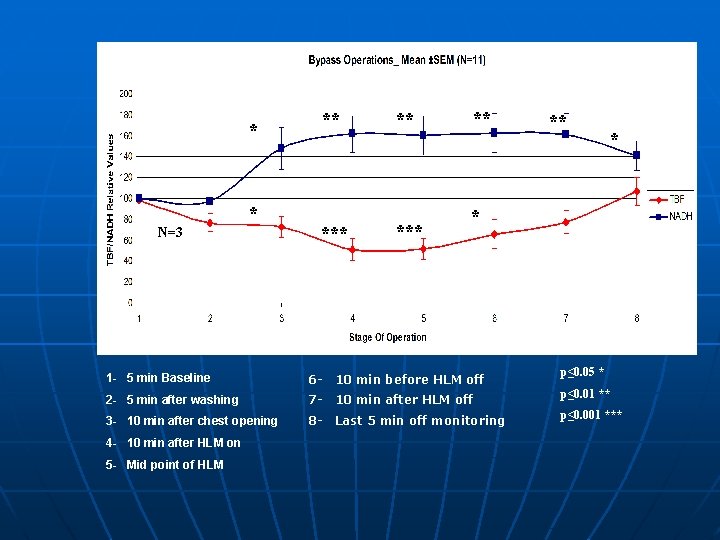
* ** * N=3 *** ** ** * * p≤ 0. 05 * 1 - 5 min Baseline 6 - 10 min before HLM off 2 - 5 min after washing 7 - 10 min after HLM off p≤ 0. 01 ** 3 - 10 min after chest opening 8 - Last 5 min off monitoring p≤ 0. 001 *** 4 - 10 min after HLM on 5 - Mid point of HLM
www. critisense. com Thank You 63