Retinal Lesions Kim Son Lett Consultant Ophthalmologist VitreoRetinal







































- Slides: 39

Retinal Lesions Kim Son Lett Consultant Ophthalmologist & Vitreo-Retinal Surgeon Birmingham & Midland Eye Centre Director, Acute Eye & VR Services

Topics �Floaters & Flashes �Posterior Vitreous Detachment �Vitreous Haemorrhage �Retinal Degenerations, Holes & Tears �Retinal Detachment �Retinoschisis �Epiretinal Membrane �Macular Hole

Floaters & Flashes (Field Defect) �V common presentation to Eye Cas �Duration, ? Recent exacerbation �Myopia, -5 & -10 D thresholds �Intra-ocular surgery �Trauma �Medical Hx, eg connective tissue Dx �Family Hx retinal detachment

Floaters & Flashes (2) �Only 20 -30% PVD symptomatic �Floaters alone, 2 -5% breaks �Photopsia alone, 8 -14% breaks �Floaters & photopsia, 11 -18% breaks

Floaters & Flashes (3) Schaeffer’s Sign – tobacco dust Pigmented cells in vitreous Pathognomonic of retinal tear – NO! White cells, RBCs – use red free filter Posterior collapse S shaped post hyaloid face Versions will highlight Indicates PVD

Floaters & Flashes (4) Indentation – not expected of optoms 3 mirror lens In a well dilated eye (use pheny & trop) with a good view may not be much advantage

Floaters and Flashes - Mx �Floater +/ Flashes, no tobacco/# �RD warning, SOS �Symptoms, tobacco, no # �Eye Cas �Asymptomatic, tobacco, no # �Recheck history �Symptoms, tobacco, # �Eye Cas

Posterior Vitreous Detachment �Typically occurs 45 -65 �Virtually 100% prevalence over 85 �Only 20 -30% symptomatic �<10% attenders have #s �Weiss ring �Tobacco dust �Vitreous haemorrhage �Retinal tears / detachment

PVD (2) PVD only RD warning, SOS PVD & VH Eye Cas PVD & #/RD Eye Cas

Birmingham and Midland Eye Centre Date: Vitreo-Retinal Referral Form Referring Hospital: Patient NBM from: Patient name: Addressograph label: Date of birth: Address: Contact number: Presenting symptoms & duration: Floaters Field defect Photopsia Asymptomatic Other history & details Prior intra-ocular surgery Myopia Trauma Family history Examination: OD RAPD OS BC VA IOP Lens status PVD Tobacco dust Vit haem Referring Doctor Contact number Referring Consultant informed? Please complete this form and fax to: 0121 507 4068

Vitreous Haemorrhage VH in 1. 2% of floaters alone VH in 0. 2% of photopsia alone VH in 6% of floaters & photopsia #s in 70% of pts presenting with VH All need to be seen in Eye Cas ? flat periphery (indirect ophthalmoscopy) Ultrasound Systemic Dx? Early Vitrectomy vs Observation

Retinal degenerations �Lattice �White without pressure �Paving/cobble stone

Lattice Degeneration 8 -10% of population Commoner in myopes Overlying pocket of synchitic vitreous May be assoc with holes +/- SRF Progression to RD rare Round hole RD before PVD – slow progression Tear related RD after PVD – rapid progression

WWP & Pavingstone WWP Rarely assoc with GRT Normally no prophylaxis Pavingstone Chorio-retinal atrophy Seen in up to 25% eyes No prophylaxis

Types of Break Horseshoe tears, U-tears Arrowhead tears Operculae Atrophic holes Giant retinal tears Dialysis

What Requires Treatment? Tear vs. hole Size Symptomatic Pigmentation Fellow eye RD H/O cataract extraction 0. 5% routine, 2% PCR RRD Myopia FH Systemic Dx Marfan’s, Stickler’s, Ehlers-Danlos Vitreous traction

Definitions �Separation of neurosensory retina from RPE �Rhegmatogenous 95% �Tractional 4% �Exudative 1%

Why is RD a Problem? �Impaired nutrition to photoreceptors �Retinal vessels vs Choriocapillaris �Altered architecture �Photoreceptor death �Poor vision

Causes of RRD �PVD �Peripheral degenerations �Myopia �Intraocular Sx �Trauma �Inflammation �Retinoschisis �Connective tissue disorders

Symptoms & Signs �Floaters �Photopsia �Field defect �Sudden Lo. V – VH �Anterior uveitis �Tobacco dust �Bullous retina �Retinal corrugation & motion �Breaks

Lincoff’s Laws �Harvey Lincoff �Emeritus Professor, Cornell, NY �Pioneering work on �Cryotherapy �Silicone sponge buckling �Scleral balloon �Perfluorocarbon internal tamponade

ST or SN RRD In 98%, primary break within 1. 5 clock hours of highest border Fluid tracks to opposite side

Total / superior RRD crossing 12 o’clock meridian In 93% primary break is at 12 o’clock or within triangle where apex is at ora serrata and sides extend 1. 5 c. h. either side of 12 o’clock. Break on side of lower detachment

Total RRD Break at 12 o’clock

Inferior RRD In 95% break on side of higher detachment Look along bisecting line

Inferior Bullous RRD Inferior bullae originate from superior break Likely to require indentation which may abolish SRF gutter

Other Considerations �Age �PVD �Phakic or Pseudophakic �Number of breaks �Size of break �Anterior vs. posterior break �Macula on or off �LA or GA

Timing of Surgery �Macula on �Before macula comes off! �Ideally within 24 hrs �Macula off �Normally within 10/7

Principles of Surgery �Close the break �Relieve vitreous traction �Fluid drainage optional

External Approach �Cryobuckle �Encirclage �D-ACE �Indirect ophthalmoscopy skills �Accurate indentation �Buckle selection �Suturing into thin sclera �Trans-scleral fluid drainage

Internal Approach �Pars plana vitrectomy �PVD induction? �Break identification and marking �Retinopexy, scarring time �Fluid-air exchange, heavy liquids �Tamponades �Post-op posturing

Success rates �Primary surgery 80 -90% success �Secondary surgery 70 – 80% success �Rates fall off with each successive procedure

Traction RD Commonest in proliferative diabetic retinopathy Also sickle cell retinopathy V poor prognosis PPV, Delamination, Laser, Tamponade

Exudative RD Rare CNVM commonest Inflammatory disease eg scleritis Neoplasia Vascular anomalies Shifting SRF VR surgery rarely indicated

Degenerative Retinoschisis Present in 5% of population > 20 yrs Often bilateral, hypermetropes Split in outer plexiform layer Transparent Immobile No demarcation line Look for breaks in inner & outer leaves If only inner leaf break, no RD If only outer leaf break, RD v. rare as fluid is very viscous ? Tests to differentiate from RRD

Epiretinal Membrane Scar tissue Semi-opaque Contractile fibrocellular membrane Symptoms & signs Routine referral Surgery only if pt troubled PPV, ERM +/- ILM Peel 2 -3 Snellen line gain

Macular Hole Symptoms & signs Gass classification now defunct Routine referral Surgery elective PPV, ILM Peel, Gas 90 -95% success rate 2 -3 Snellen line gain

Summary �No tobacco dust – don’t panic �Not all retinal defects / degenerations require retinopexy – symptomatic traction is key �Vit haem is high risk �Only mac-on RD is ophthalmic emergency �ERM and MH are routine OPD referrals

Thank You Questions?
 Mr kim son
Mr kim son Vitreoretinal eua
Vitreoretinal eua Mchugh plastic surgery
Mchugh plastic surgery Ecce
Ecce Drug rehab firth
Drug rehab firth Friendly letter sample
Friendly letter sample Lett advokatfirma
Lett advokatfirma Retinal disparity psychology
Retinal disparity psychology Retinal detachment
Retinal detachment On klinika
On klinika Phi phenomenon
Phi phenomenon Binocular disparity depth perception
Binocular disparity depth perception Depth perception ap psychology
Depth perception ap psychology Pragnanz ne demek
Pragnanz ne demek Cortex striata
Cortex striata Wolf jaw retinal detachment
Wolf jaw retinal detachment Retinal ganglion
Retinal ganglion Fusiform initials and ray initials diagram
Fusiform initials and ray initials diagram Advantages of screenless display
Advantages of screenless display Retinal disparity definition psychology
Retinal disparity definition psychology Horseshoe tear
Horseshoe tear Topcon retinal camera
Topcon retinal camera Nursing diagnosis for ngt feeding
Nursing diagnosis for ngt feeding Retinal vessels
Retinal vessels Retinal detachment presentation
Retinal detachment presentation Nursing diagnosis of retinal detachment slideshare
Nursing diagnosis of retinal detachment slideshare Autism nursing diagnosis
Autism nursing diagnosis Retinal migraine
Retinal migraine Optic nerve histology
Optic nerve histology Retinopexy
Retinopexy Monocular depth cues interposition
Monocular depth cues interposition Pie on the floor visual field defect
Pie on the floor visual field defect Pyramidal vs extrapyramidal tract
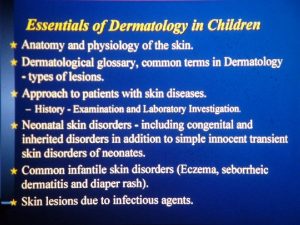
Pyramidal vs extrapyramidal tract Describing skin lesions
Describing skin lesions Esophagus
Esophagus Pustule
Pustule Olneys lesions
Olneys lesions Red nucleus function
Red nucleus function Gingival third vs cervical third
Gingival third vs cervical third Amiante
Amiante