Pleural diseases Case Studies Dr JM Nel Department












- Slides: 53
Pleural diseases: Case Studies Dr. JM Nel Department of Pulmonology
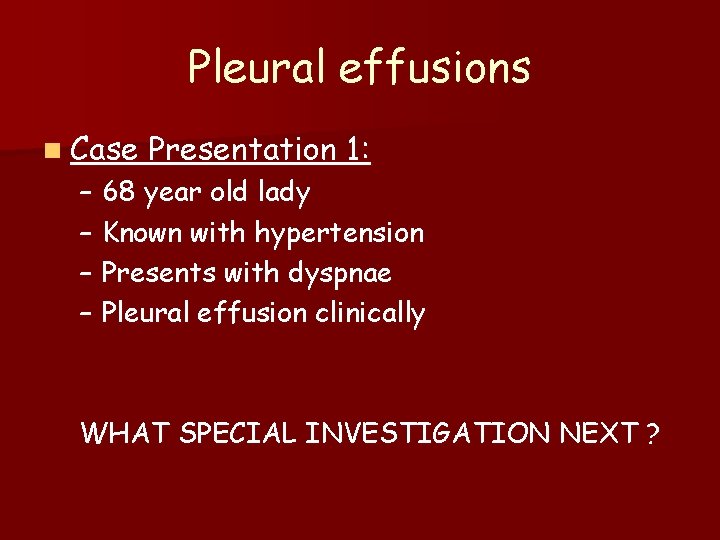
Pleural effusions n Case Presentation 1: – 68 year old lady – Known with hypertension – Presents with dyspnae – Pleural effusion clinically WHAT SPECIAL INVESTIGATION NEXT ?

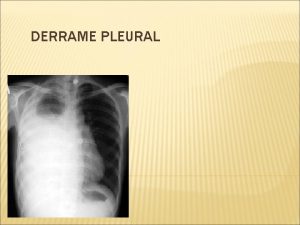
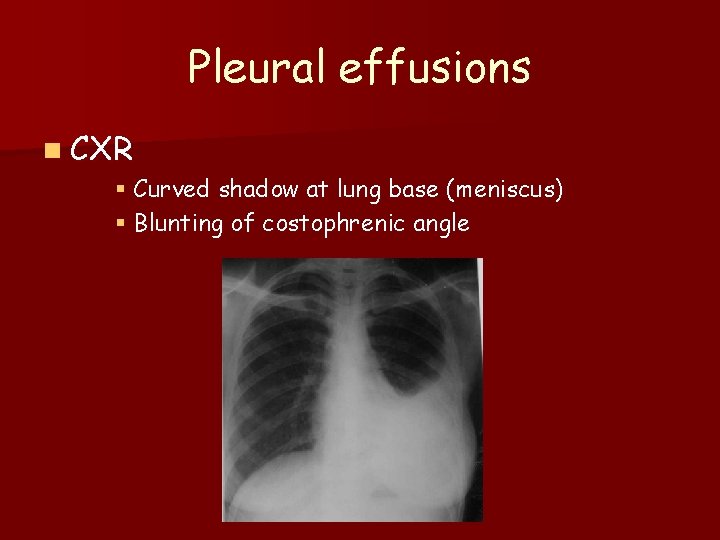
Pleural effusions n CXR § Curved shadow at lung base (meniscus) § Blunting of costophrenic angle
Pleural effusions WHAT NOW ? ? ? n Pleural tap – Transudate – Exudate
Pleural effusions n Pleural fluid features – A. Appearance of fluid – B. Biochemical analysis – C. Gram stain – D. Predominant cells in fluid – E. Other
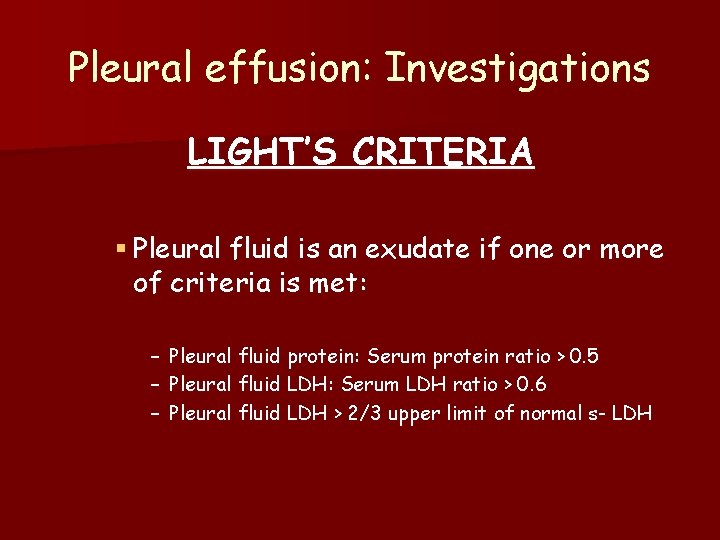
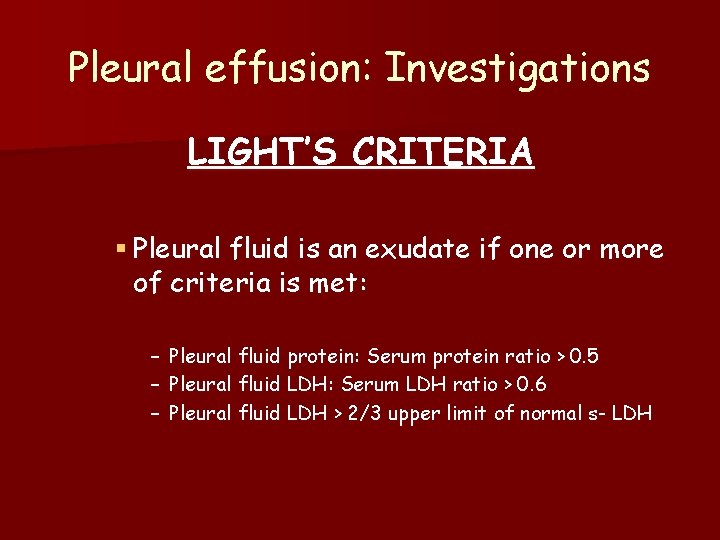
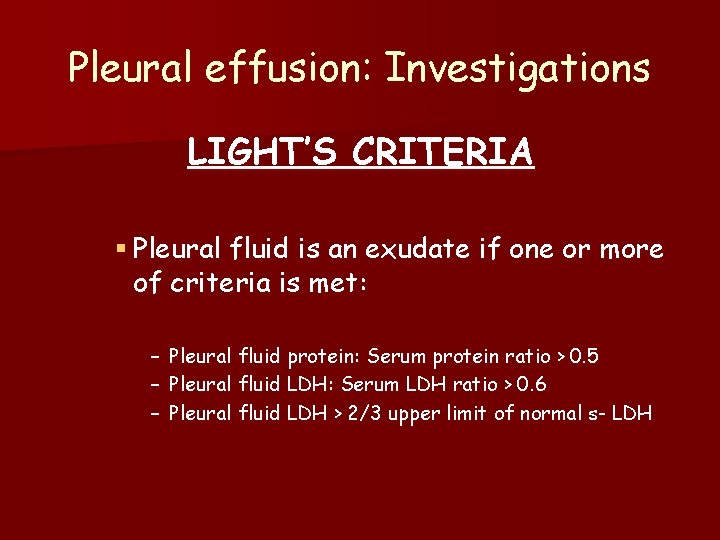
Pleural effusion: Investigations LIGHT’S CRITERIA § Pleural fluid is an exudate if one or more of criteria is met: – – – Pleural fluid protein: Serum protein ratio > 0. 5 Pleural fluid LDH: Serum LDH ratio > 0. 6 Pleural fluid LDH > 2/3 upper limit of normal s- LDH
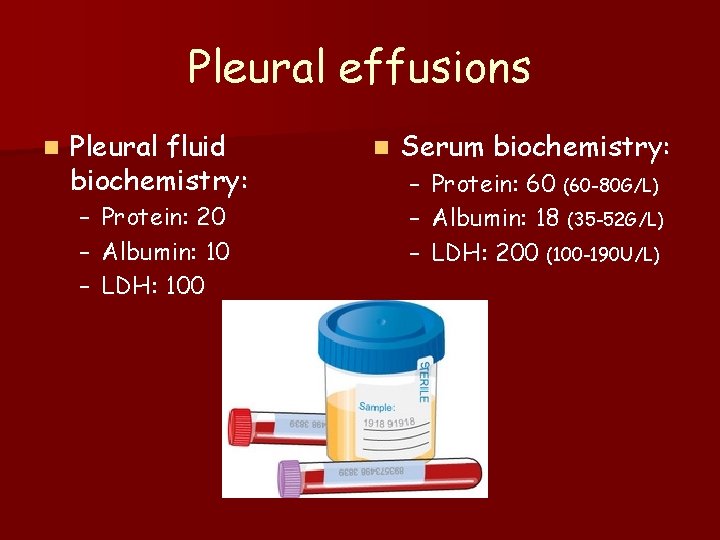
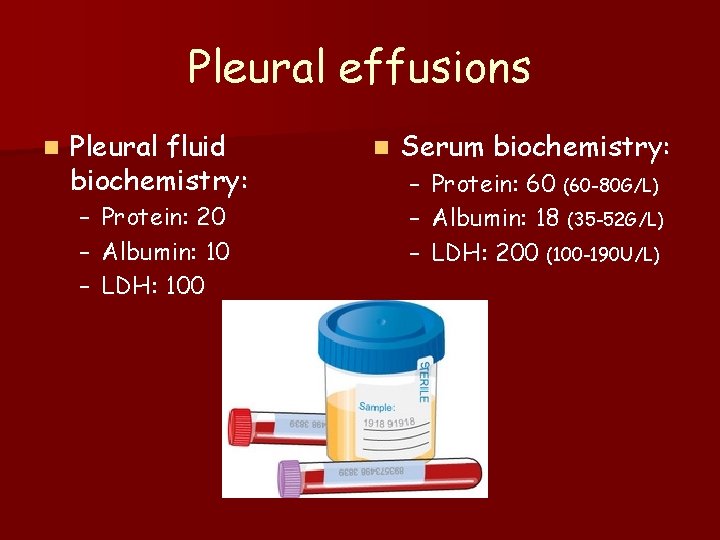
Pleural effusions n Pleural fluid biochemistry: – – – Protein: 20 Albumin: 10 LDH: 100 n Serum biochemistry: – – – Protein: 60 (60 -80 G/L) Albumin: 18 (35 -52 G/L) LDH: 200 (100 -190 U/L)
Pleural effusions TRANSUDATE
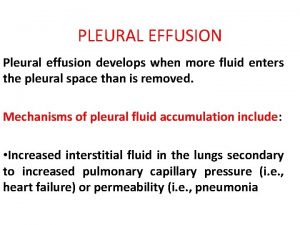
Pleural effusion: Causes n Transudate – Increased hydrostatic pressure § Congestive heart failure – Decreased plasma oncotic pressure § Nephrotic syndrome § Cirrhosis – Movement of transudative ascitic fluid through diaphragm § Cirrhosis

Pleural effusions n Case Presentation 2: – 32 year old man – Presents with fever, pleuritic chest pain and dyspnae – Pleural effusion clinically WHAT SPECIAL INVESTIGATION NEXT ?
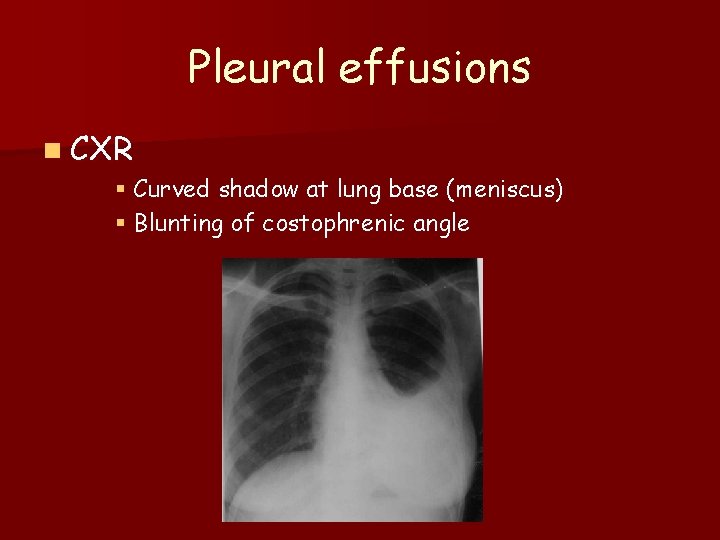
Pleural effusions n CXR § Curved shadow at lung base (meniscus) § Blunting of costophrenic angle

Pleural effusions WHAT NOW ? ? ? n Pleural tap – Transudate – Exudate
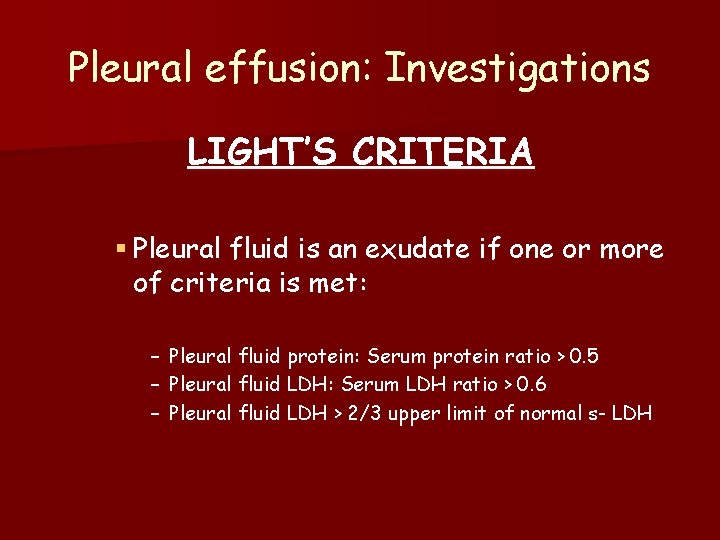
Pleural effusion: Investigations LIGHT’S CRITERIA § Pleural fluid is an exudate if one or more of criteria is met: – – – Pleural fluid protein: Serum protein ratio > 0. 5 Pleural fluid LDH: Serum LDH ratio > 0. 6 Pleural fluid LDH > 2/3 upper limit of normal s- LDH
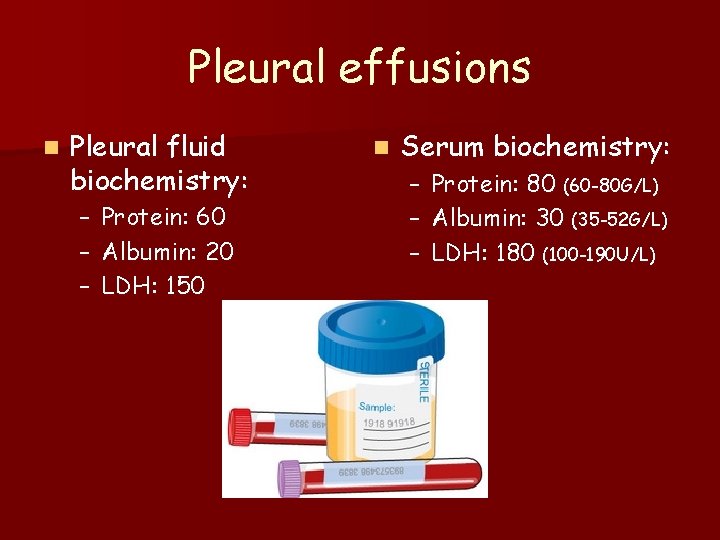
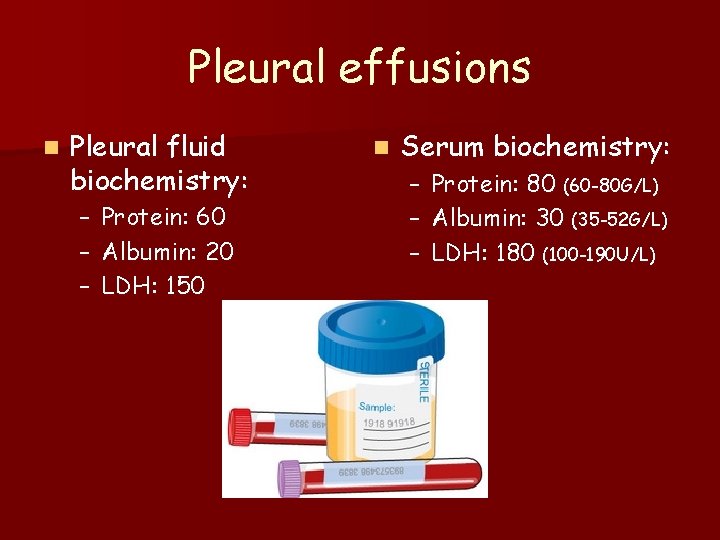
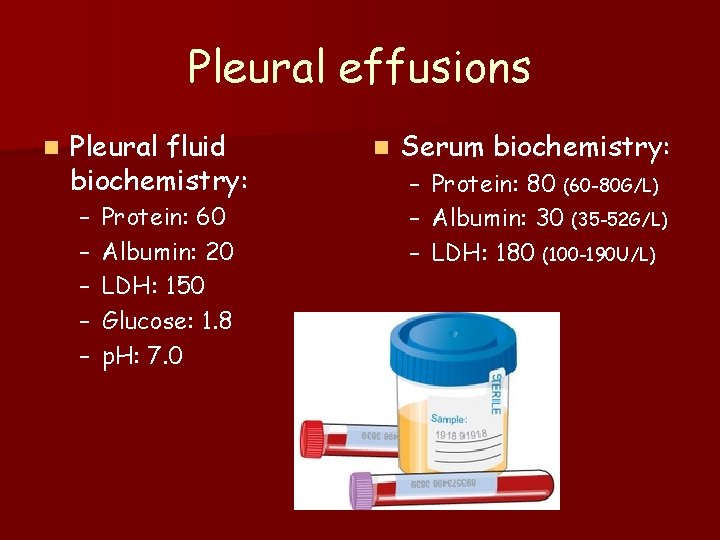
Pleural effusions n Pleural fluid biochemistry: – – – Protein: 60 Albumin: 20 LDH: 150 n Serum biochemistry: – – – Protein: 80 (60 -80 G/L) Albumin: 30 (35 -52 G/L) LDH: 180 (100 -190 U/L)
Pleural effusions EXUDATE
Pleural effusion: Causes n Exudate – Inflammatory § Infection – TB/ Pneumonia § Pulmonary embolus/ infarction § Connective tissue disease – RA/ SLE § Adjacent to subdiaphragmatic disease – Pancreatitis/ Subphrenic abscess – Malignancies
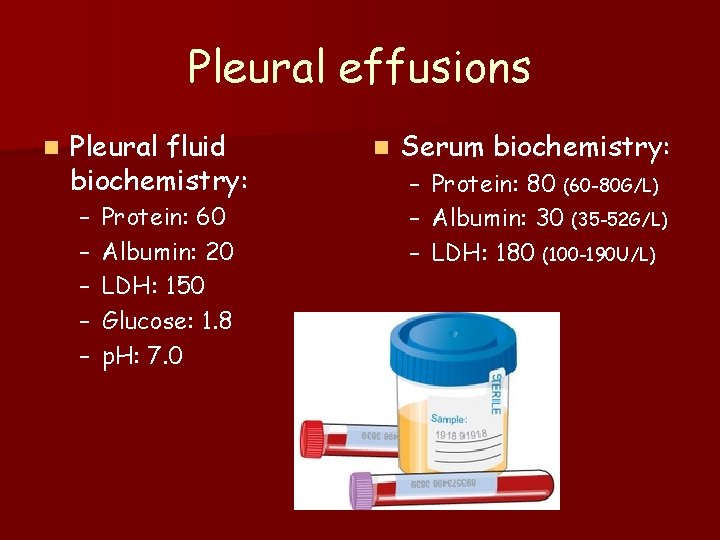
Pleural effusions n Pleural fluid biochemistry: – – – Protein: 60 Albumin: 20 LDH: 150 Glucose: 1. 8 p. H: 7. 0 n Serum biochemistry: – – – Protein: 80 (60 -80 G/L) Albumin: 30 (35 -52 G/L) LDH: 180 (100 -190 U/L)
Pleural effusions EMPYEMA
Empyema: Investigations n Aspiration of pus – Confirmation of empyema § 1. Appearance of fluid: pus § 2. Neutrophils § 3. Positive gram stain § 4. Low p. H < 7. 2 § 5. Low glucose < 3. 3

Pleural effusion: Investigations n E. Other – Low p. H § § § Infection/ Empyema RA/ SLE Malignancy TB Ruptured oesophagus – Low glucose § As low p. H – High ADA
Pulmonary Embolism: Case Studies Dr. JM Nel Department of Pulmonology
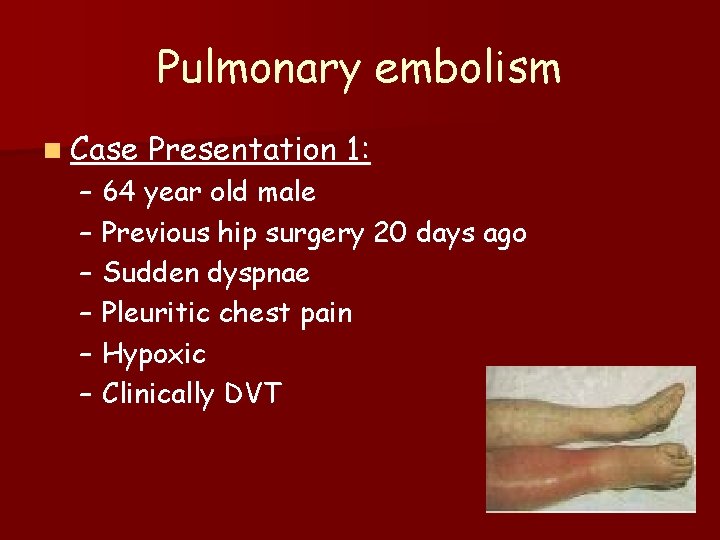
Pulmonary embolism n Case Presentation 1: – 64 year old male – Previous hip surgery 20 days ago – Sudden dyspnae – Pleuritic chest pain – Hypoxic – Clinically DVT
Pulmonary embolism DIFFERENTIAL DIAGNOSIS § Pulmonary embolism § Pneumonia § Pneumothorax § Musculoskeletal chest pain
Pulmonary embolism ASK 3 QUESTIONS – Is the presentation consistent with PE ? – Does the patient have risk factors for PE ? – Is there another diagnosis that can explain the patients presentation ?
Pulmonary embolism WHAT NOW ? ? ?
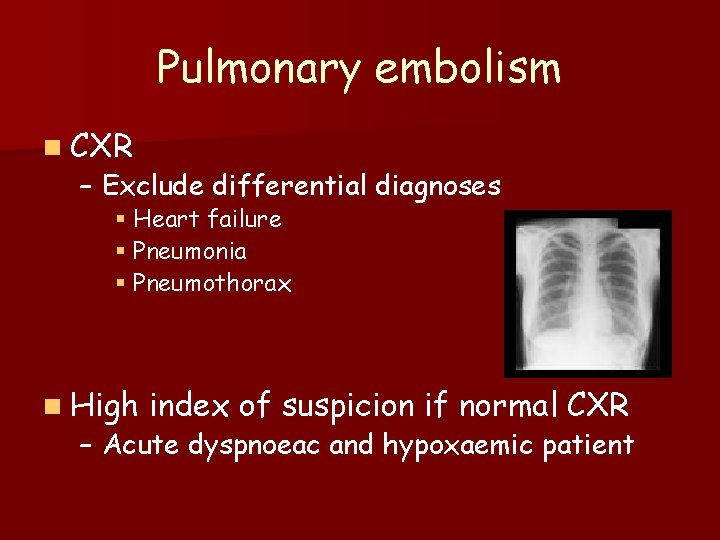
Pulmonary embolism n CXR – Exclude differential diagnoses § Heart failure § Pneumonia § Pneumothorax n High index of suspicion if normal CXR – Acute dyspnoeac and hypoxaemic patient
Pulmonary embolism n ECG – Exclude other differential diagnoses § Acute myocardial infarction § Pericarditis n Most common – Sinus tachycardia
Pulmonary embolism n Arterial n Low bloodgas Pa. O 2
Pulmonary embolism n D- dimer n POSITIVE n Other causes for elevation – Myocardial infarction – Pneumonia – Sepsis
Pulmonary embolism n Heartsonar n Massive PE – Acute dilatation of the right heart – Pulmonary hypertension – Thrombus can be seen n NORMAL n Alternative diagnoses – – – Left ventricular failure Aortic dissection Pericardial tamponade
Pulmonary embolism n Duplex n DVT doppler of legs in leg
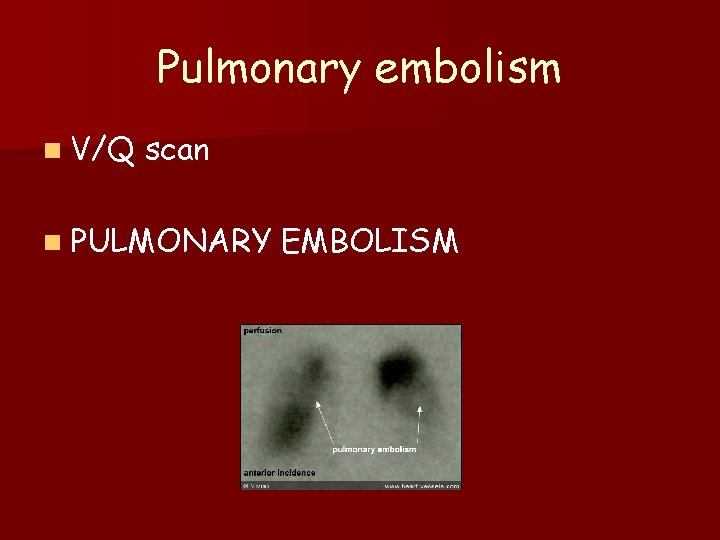
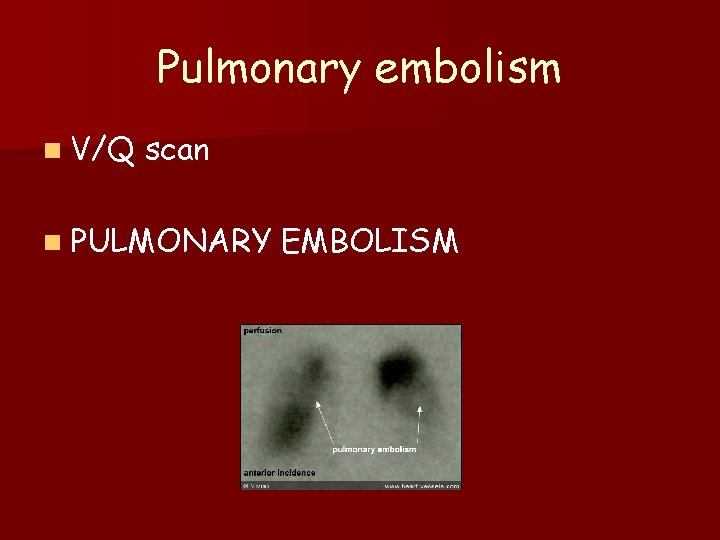
Pulmonary embolism n V/Q scan n PULMONARY EMBOLISM
Pulmonary embolism: Management n General measures – Oxygen for all hyoxaemic patients § Keep arterial oxygen saturation > 90% n Anticoagulation – Clexane 80 mg bd sc § Give at least 5 days – Warfarin – Stop Clexane when INR is > 2
Pulmonary embolism: Management n n HOW LONG DO I TREAT THIS PATIENT WITH WARFARIN ? ? ? 3 Months n Duration of Warfarin therapy – If underlying prothrombotic risk or previous emboli § For life – If identifiable and reversible risk factor § 3 Months – If idiopathic § 6 Months
Pulmonary embolism n Case Presentation 2: – 28 year old lady – Oral contraceptives – 10 hour flight – Sudden dyspnae – BP 90/40 – Loud P 2/ Increased JVP – Hypoxic
Pulmonary embolism DIFFERENTIAL DIAGNOSIS § Massive pulmonary embolism § Myocardial infarction § Pericardial tamponade § Aortic dissection
Pulmonary embolism ASK 3 QUESTIONS – Is the presentation consistent with PE ? – Does the patient have risk factors for PE ? – Is there another diagnosis that can explain the patients presentation ?
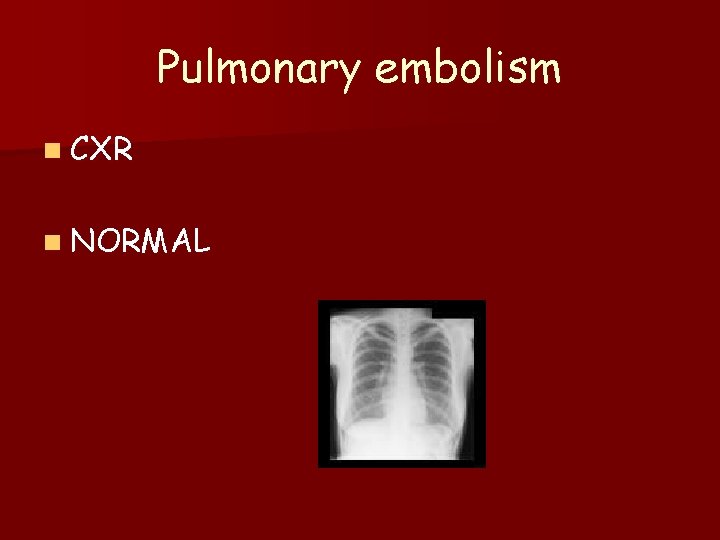
Pulmonary embolism n CXR n NORMAL

Pulmonary embolism n ECG – S 1 Q 3 T 3 – RBBB n Arterial bloodgas – Low Pa. O 2 n D- dimer – POSITIVE

Pulmonary embolism n Heartsonar – Right ventricular dilatation – Increased pulmonary pressure

Pulmonary embolism n CT pulmonary angiography MASSIVE PULMONARY EMBOLISM

Pulmonary embolism: Management n General measures – Oxygen for all hypoxaemic patients § Keep arterial oxygen saturation > 90% – Treat hypotension with IVI fluids n. Thrombolytic – RV dilatation – Low BP therapy

Pulmonary embolism: Management n Complications of thrombolytic therapy – Intracranial haemorrhage – Haemorrhage at other sites – Anaphylaxis
Pulmonary embolism n Case Presentation 3: – 28 year old lady – Oral contraceptives – 10 hour flight – Sudden dyspnae – BP 130/80 – Loud P 2/ Increased JVP – Hypoxic
Pulmonary embolism n CXR n NORMAL
Pulmonary embolism n ECG – S 1 Q 3 T 3 – RBBB n Arterial bloodgas – Low Pa. O 2 n D- dimer – POSITIVE
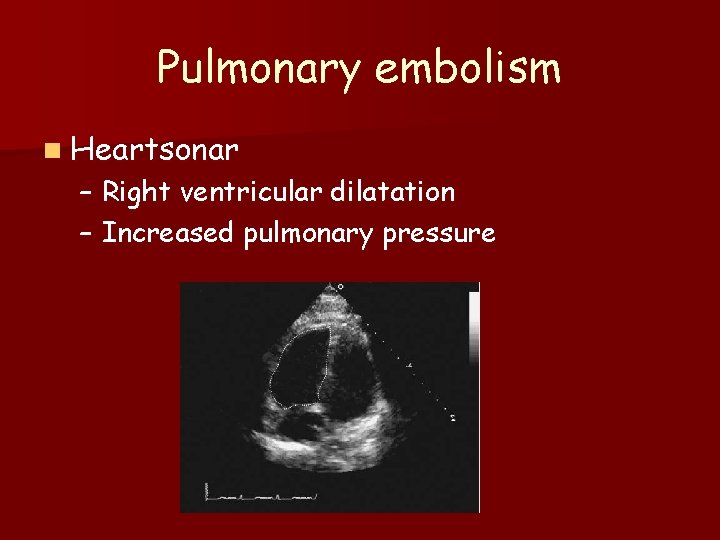
Pulmonary embolism n Heartsonar – Right ventricular dilatation – Increased pulmonary pressure

Pulmonary embolism n CT pulmonary angiography PULMONARY EMBOLISM
Pulmonary embolism n Patient has normal BP n Patient has RV strain SUBMASSIVE PULMONARY EMBOLISM
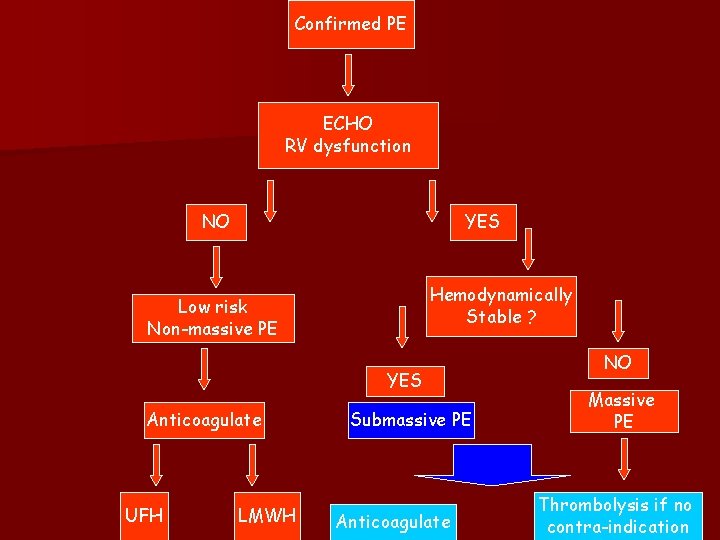
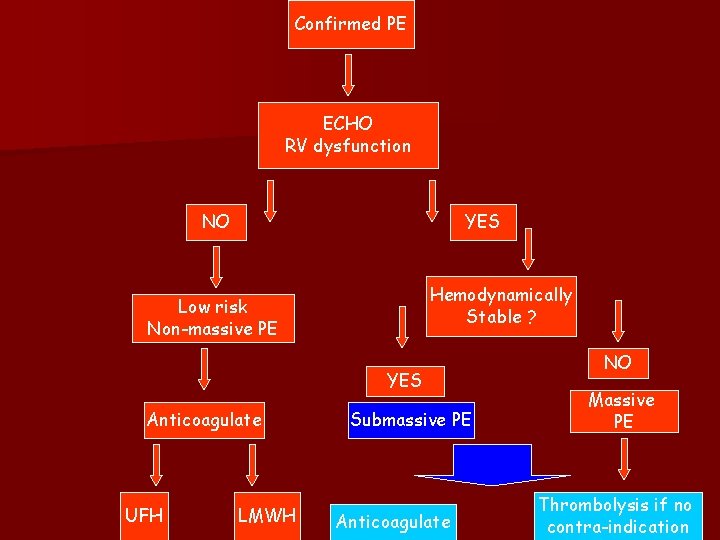
Confirmed PE ECHO RV dysfunction NO YES Hemodynamically Stable ? Low risk Non-massive PE YES Anticoagulate UFH LMWH Submassive PE Anticoagulate NO Massive PE Thrombolysis if no contra-indication

Submassive PE n To thrombolise or not to thrombolise n THAT REMAINS THE QUESTION !!!
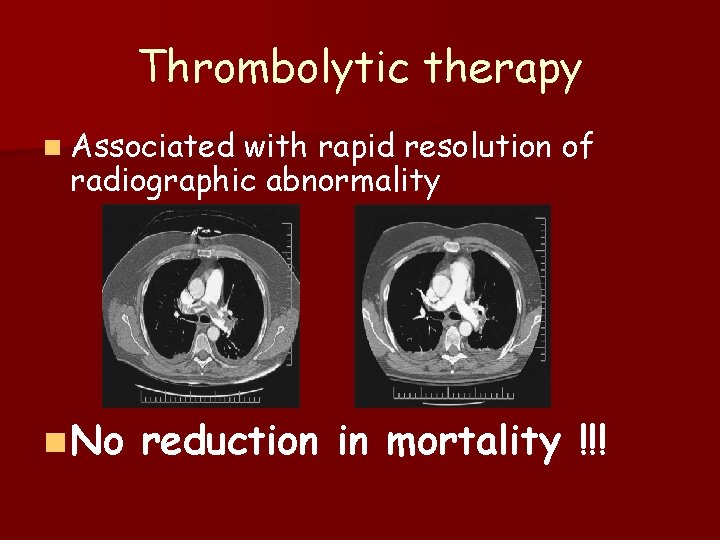
Thrombolytic therapy n Associated with rapid resolution of radiographic abnormality n No reduction in mortality !!!

Thrombolytic therapy n Indicated only in hemodynamically unstable patients !!! – SBP < 90 mm. Hg n All must be followed by therapeutic anticoagulation
 Best case worst case average case
Best case worst case average case Paradigm shift from women studies to gender studies
Paradigm shift from women studies to gender studies Advantages of case studies in psychology
Advantages of case studies in psychology Times 100 business case studies
Times 100 business case studies The times 100 business case studies
The times 100 business case studies Holistic technology in human values
Holistic technology in human values Example of outbreak
Example of outbreak Case series
Case series Eu-gdpr-p
Eu-gdpr-p Gcse geography manchester case study
Gcse geography manchester case study Euthanasia case studies
Euthanasia case studies E procurement case studies
E procurement case studies Types of case studies
Types of case studies Definition of a case study
Definition of a case study Kellogg's crunchy nut bites market research
Kellogg's crunchy nut bites market research Nasa case study
Nasa case study Blood group discrepancy
Blood group discrepancy Organic chemistry case studies
Organic chemistry case studies Nspe board of ethical review cases
Nspe board of ethical review cases Organ donation case studies
Organ donation case studies Jmp case studies
Jmp case studies Case studies of rtos
Case studies of rtos Ferpa case studies
Ferpa case studies Social engineering case studies
Social engineering case studies Plagiarism case study
Plagiarism case study Case studies financial management
Case studies financial management Digital marketing case studies 2012
Digital marketing case studies 2012 @the..porky..maggot:pixeldrain.com/u/vbkr37be
@the..porky..maggot:pixeldrain.com/u/vbkr37be The times 100 business case studies
The times 100 business case studies Ref impact case studies
Ref impact case studies Tanya carmichael
Tanya carmichael Food safety errors: case studies
Food safety errors: case studies Growth hacking case studies
Growth hacking case studies Case study base
Case study base Meniscus sign pleural effusion
Meniscus sign pleural effusion Vocal fermitus
Vocal fermitus What causes tactile fremitus
What causes tactile fremitus What is tactile fremitus
What is tactile fremitus émoussement sac pleural forum
émoussement sac pleural forum Pleural fluid
Pleural fluid Derrame pleural grados
Derrame pleural grados Pleural empyema
Pleural empyema Aspirimi i rrugeve te frymemarrjes
Aspirimi i rrugeve te frymemarrjes Cupola pleurica
Cupola pleurica Pleural effusion color chart
Pleural effusion color chart بیمارستان مدرس
بیمارستان مدرس Indications of intercostal drainage
Indications of intercostal drainage Effusion definition
Effusion definition Light criteria
Light criteria Pleural aspiration site
Pleural aspiration site Serosangineous
Serosangineous Mediastinum structures
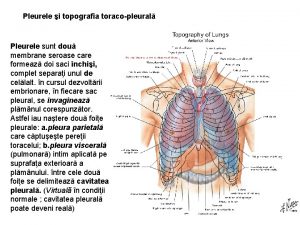
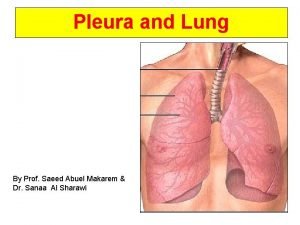
Mediastinum structures Lung pleura
Lung pleura Exsudat transudat
Exsudat transudat