Pharmacology ANTIFUNGAL DRUG AGENTS Fungal Infections Fungi are



- Slides: 62
Pharmacology ANTI-FUNGAL DRUG AGENTS
Fungal Infections Fungi are a very large and diverse group of microorganisms that compromise both yeast and molds. • Yeast are single-celled fungi that reproduce by budding and are actually very useful organisms. They are used in baking and alcoholic beverages. • Molds are multicellular and are characterized by long, branching filaments called hyphae, which entwine to form a (mat) called a mycelium. Some fungi are part of the normal flora of the skin, mouth, intestines, and vagina. •
Continue The infection caused by a fungus can also be called a mycosis, but there are very few fungi that cause such infections. Those that do are termed pathologic fungi, and the infections they cause range in severity from being mild and superficial to severe and life-threatening.
Continue • • • These infections can be contracted by several different routes: Ingested orally Implanted under the skin after injury They can be inhaled There are four major general types of mycotic infections: Systemic Cutaneous Subcutaneous Superficial
Continue The most severe systemic fungal infections generally afflict persons whose host defenses are compromised. Commonly these are patients who have received organ transplants and are on immunosuppressive drug therapy, cancer patients and AIDS patients. These may result in an over growth of candida albicans, followed by the development of a systemic infection.
Introduction The drugs used to treat fungal infections are called antifungal agents. Systemic mycotic infections and some cutaneous or subcutaneous mycoses are treated with oral or parenterally agents. • One difficulty that has slowed the development of new agents is that frequently the chemical concentrations required for these experimental agents to be effective cannot be tolerated by human beings. •
Continue • • Following is a list of those agents that have met with success in the treatment of systemic and severe cutaneous or subcutaneous mycoses: Amphotericin B Fluconazole Flucytocine Griseofulvin Itraconazole Miconazole Nystatin
Continue • • • Topical antifungal are most commonly used in the treatment of oral and vaginal candisasis. Following is a list of those topical antifungals approved for clinical use: Amphotericin B Butoconazole Ciclopirox Clotrimazole Miconazole Nystatin Terbinavine Sodium thiosulfate Ketoconazole
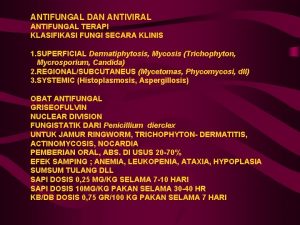
Classification of Drugs The antifungals agents can be broken down in to four major groups based on their chemical structures: Polyenes, e. g Amphotericin B and Nystatin Flucytosine Azoles, e. g Ketoconazole and Miconazole Griseofulvin
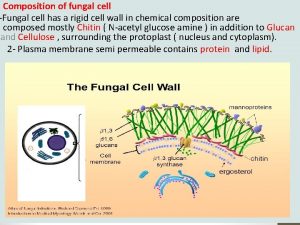
Mechanism of action The mechanisms of action of the various antifungal agents differ depending on which of the four groups of agents they belong to. The polyenes act by binding sterols in the cell membranes of fungi, the main sterol in the fungi is ergosterol. The question is human being has sterol then how do we prevent damage in the human cell?
Continue • The answer of this question polyene antifungal do not bind to human cell membranes, and therefore do not kill human cells, because polyene has stronger affinity for ergosterol than for cholesterol. Once the polyene binds to the ergosterol, a channel forms in the fungal cell membrane that allows potassium and magnesium ions to leak out of the cell. This loss of ions causes fungal cellular metabolism to be altered, and hence death of the cell.
Continue Flucytosine, also known as 5 -fluorocytosine. Once the 5 -fluorouracil is inside the fungal cell, it interferes with DNA synthesis by incorporating itself in to the fungal pathway that produces DNA, with the result that the DNA needed for the fungal cell metabolism is lacking and the cell dies.
Continue Azoles act as either fungistatic or fungicidal agents, depending on their concentration in the fungus. Inhibit production of ergosterol and this allows potassium to escape from the fungi cell membrane and lastly fungi cell dies. • Griseofulvin works by preventing mitosis or reproduction of fungi by binding to microtubules. It has also been proposed that Griseofulvin causes the production of defective DNA, which is then unable to replicate. •
Therapeutic uses used candiasis (oral, vaginal e. t. c) used in Aspergillosis used in histoplasmosis used in fungal septicemia used in Coccidiodomycosis used in cryptococcal meningitis
Aspergillosis Infection caused by the aspergillus fungus or one of it is mold species. Invasive aspergillosis is an opportunistic infection that affects people with immunodeficiencies. the primary infection is usually pneumonia, but the brain, kidney, and heart valves may also be affected. It is treated with I. V amphotericin B or long term oral itracanazole.
Histolasmosis A systemic fungal respiratory disease caused by histoplasma capsulatum. The reservoir for this fungus is in soil with a high organis content, old chicken houses. It is a common opportunistic infection. Signs are fever, anemia, enlarged spleen, leukopenia, adrenal necrosis and pneumonia. The treatment is amphotericin B or ketoconazole.
Coccidiodomycosis Infection with the pathogenic fungus coccidio -immitis. Found in the soil. It is seen in earthquakes, during construction. Persons who inhale the spores may develop active or subclinical infection. Treatment: most patients with primary infection recover with out therapy. Amphotericin B is recommended 1 -3 months.
Blastomycosis Infection caused by inhalation of the conidia of blastomyces dermatitidis. This rare fungal infection may produce inflammatory lesions of the skin (cutaneous), lungs or generalized invasion of skin, bones, CNS, and the kidney. Treatment is amphotericin B and Ketoconazole.

Dermatophytosis It is causes by a fungal parasite that grows the skin of the body, and it is known as dermatophyte fungal infection. They cause skin diseases like eczema, tinea, ringworm. The treatment is Griseofulvin or the azoles and terbinafine.
Chromomycosis A chronic fungal skin infection marked by itching and warty plaques on the skin and subcutaneous swelling of the feet and the legs and other exposed areas. Various fungus have been implicated including phialophora verrucosa. The treatment includes amphotericin B and Flucytosine.
Side-effects • • • Headache Renal toxicity Potassium loss Nausea Vomiting Photosensitivity Anaphylaxis Rash Tachycardia Anorexia Flushing Impotence

Amphotericin B It is obtained from streptomyces nodosus. The polyenes possess a macrocyclic ring, one side of which has several conjugated double bonds and is highly lipophilic, while the other side is hydrophilic with many OH groups. • Amphotericin B is active against a wide range of yeasts and fungi candida albicans, histoplasma capsulatum, cryptococcus neoformans, blastomyces dermatitides, and coccidiodes immitis. • •
Continue Amphotericin isn't orally absorbed. It can be given orally for intestinal candisasis without systemic toxicity. Administered I. V as a suspension made with the help of deoxycholate. It gets widely distributed in the body, but the penetration in CSF is poor.
Continue • • It is metabolized in the liver. It has half life of 15 days. Excretion occurs slowly both in urine and bile, but urinary concentration of active drug is low. Orally can be administered 50 -100 mg QID. For i. v 0. 3 mg/kg or 0. 7 mg/kg. The total dose of amphotericin for majority of cases is 3 -4 g given over 2 -3 months. Intrathecal injection of 0. 5 mg twice weekly has been given in fungal meningitis.
Uses Amphotericin B can be applied topically for oral, vaginal and cutaneous candisasis and otomycosis. • It is the most effective drug for various types of systemic mycosis and is the gold standard of antifungal therapy. However, because of higher toxicity of amphotericin B, the azole antifungals are now preferred in conditions where their efficacy approaches. •
Drug interactions Flucytosine has supra-additive action with amphotericin B in the case of fungi sensitive to fungus. Rifampin and Minocycline , though not antifungal in their own right but potentiate amphotericin action.
Adverse effects Chills Fever Nausea Vomiting Dyspnea Hypokalemia Nephrotoxicity
AMPHOTERICIN B TOXICITY ID/CC: During ward rounds, a 28 year old HIV positive female patient complains that after a period of improvement since her administration 3 days ago, she now feels very sick, with high fever, marked lightheadedness, headache, and myalgias. • HPI: She was admitted because of cryptococcal meningitis and was started on amphotericin B. •
Continue PE: VS: tachycardia (HR 93); hypotension (BP 90/55); fever (39. 3 centigrade); tachypnea. PE: nuchal rigidity resolved, mental status improved. Labs: CBC: mild anemia; normal leukocytes. Lytes: hypokalemia. BUN and creatinine moderately elevated.
Continue Treatment: If the reaction is severe, it may be necessary to lower the dosage of amphotericin B, use a liposomal form, or change to Fluconazole. Antipyretics, antihistamines, and corticosteroids may lessen febrile symptoms; heparin can decrease the risk of thrombophebitis. • Discussion: The mechanism of action of amphotericin B is by binding to ergosterol in fungi and forming membrane pores. Toxicities include arrhythmias, chills and fever, hypotension and nepthrotoxicity. •
Nystatin It is obtained streptomyces nourseia. Nystatin has similar structure with amphotericin B and has the same poreforming mechanism of action. It is too toxic for systemic use and is only used topically. It is not absorbed from skin, mucous membranes, or the gastrointestinal tract.
Continue Nystatin is active against most Candida species and is most commonly used for suppression of local candidal infections. Nystatin is used in the treatment of oropharyngeal thrush, vaginal candidiasis. It is available 1 lac U , 5 lac U vaginal tab, 1 lac U per g for eye ointment. (1 mg = 2000 U). It is available orally as suspension, topically 2% cream.
Griseofulvin is a fungistatic and used is in the treatment of dermatophytosis. Absorption is improved when it is given with fatty foods. Griseofulvin is deposited in newly forming skin where it binds to keratin, protecting the skin from new infection.
Continue It must be administered for 2 -6 weeks for skin and hair infections to allow the replacement of infected keratin by the resistant structures. Nail infections may require therapy for months to allow regrowth of the new protected nail and is often followed by relapse.
Continue It is dose is 125 mg- 250 mg QID with meals, duration depends the location. Body skin: 3 weeks, palms and soles: 4 to 6 weeks, finger nails: 4 to 6 months, toe nails: 8 to 12 months.
Adverse effects and drug interactions Adverse effects include an allergic syndrome much like serum sickness, hepatitis, and drug interactions with warfarin and phenobarbital, oral contraceptives and alcohols. Griseofulvin has been largely replaced by newer antifungal medications such as itraconazole and terbinafine.
Flucytosine is related to fluorouracil (5 -FU). Its spectrum of action is much narrower than that of amphotericin B. It is well absorbed orally. It is poorly protein-bound and penetrates well into all body fluid compartments including the CSF. It is eliminated by glomerular filtration. Toxicity is more likely to occur in AIDS patients and in the presence of renal insufficiency.
Continue Flucytosine is converted intracellularly first to 5 -FU and then to 5 -fluorodeoxyuridine monophosphate (F-d. UMP) and fluorouridine triphosphate (FUTP), which inhibit DNA and RNA synthesis, respectively.
Clinical use Active against Cryptococcus neoformans, some Candida species, and the dematiaceous molds that cause chromoblastomycosis. Clinical use at present is confined to combination therapy, either with amphotericin B for cryptococcal meningitis or with itraconazole for chromoblastomycosis.
Adverse Effects The adverse effects of flucytosine result from metabolism (intestinal flora) to the toxic antineoplastic compound flucytosine. Bone marrow toxicity with anemia, leukopenia, and thrombocytopenia are the most common adverse effects, with derangement of liver enzymes occurring less frequently.
Azoles are synthetic compounds that can be classified as Imidazoles and Triazoles. The Imidazoles consist of Ketoconazole, Miconazole, and Clotrimazole. The triazoles include Itraconazole and Fluconazole.
Continue Azoles are active against many Candida species, Cryptococcus neoformans, the endemic mycoses (blastomycosis, coccidioidomycosis), the dermatophytes, and, Aspergillus infections (itraconazole). Adverse Effects: The azoles are relatively nontoxic.
Adverse effects The most common adverse reaction is minor gastrointestinal upset, Most azoles cause abnormalities in liver enzymes and, very rarely, clinical hepatitis.
Ketoconazole It is the first orally effective broad-spectrum antifungal drug, useful in both dermatophytosis and deep mycosis. Ketoconazole is less selective for fungal P 450 than are the Fluconazole and Itraconazole (inhibit mammalian cytochrome P 450 enzymes). The usual dose is 200 mg o. d or BD, higher doses are some times required. Available 2% shampoo, cream, lotion.
Clinical use it has limited use because of the drug interactions, endocrine side effects, and of its narrow therapeutic range. Oral formulation that is best absorbed at a low gastric p. H. Ketoconazole is used in treatment of mucocutaneous candidiasis and nonmeningeal coccidioidomycosis. It is also used in the treatment of seborrheic dermatitis and pityriasis versicolor (Topical/ shampoo).
Adverse effects First, ketoconazole inhibition of human cytochrome P 450 enzymes interferes with biosynthesis of adrenal and gonadal steroid hormones, producing significant endocrine effects such as gynecomastia, infertility, and menstrual irregularities.
Drug interactions Second, the interaction with P 450 enzymes can alter the metabolism of other drugs, leading to enhance toxicity of those agents: 1. Phenytoin 6. Nifedipine 2. Diazepam 7. cyclosporine 3. Haloperidol 8. Statins 4. Warfarin 9. protease inhibitors 5. Digoxin Ketoconazole rises the blood concentration levels.
Ketoconazole side effects ID/CC: A 23 year old marathon runner visits his sports medicine doctor complaining of unsightly, embarrassing growth of his right breast (GYNECOMASTIA) as well as undue fatigue after training and a slight yellowish hue in the eyes (JAUNDICE).
Continue HPI: Three months ago, he was put on daily oral Ketoconazole because of he had been suffering from a severe, refractory tinea corporis infection. PE: VS: bradycardia; fever (38. 1 centigrade). PE: slight jaundice in conjunctiva, no lymphadenopathy, no neck masses, cardiopulmonary exam normal; no hepatomegaly; examination of skin reveals tinea corporis covering intertriginous areas,
Continue Labs: AST and ALT increased, serum bilirubin level increased. Imaging: US, liver: mildly enlarged liver. Treatment: Discontinue drug; substitute treatment with alternative antifungal (e. g terbinafine).
Continue Discussion: Ketoconazole is an imidazole that inhibits fungal synthesis of ergosterol in membranes. It is used for blastomycosis, coccidiomycosis, histoplasmosis, and candisasis.
Continue Major side effects are hepatic damage, Gynecomastia, impotence (due to inhibition of testosterone synthesis), inhibition of cytochrome P 450, fever, and chills. When taken with antacids or H 2 receptor blockers, it is absorption is decreased. It dramatically increases cyclosporine levels.
Clotrimazole and miconazole are available over-the-counter and are often used for vulvovaginal candidiasis. Oral clotrimazole troches are available for treatment of oral thrush and are a pleasant-tasting alternative to nystatin. In cream form, both agents are useful for dermatophytic infections, including tinea corporis, tinea pedis, and tinea cruris. Absorption is negligible, and adverse effects are rare.
Continue Clotrimazole is effective in the topical treatment of tinea infection like ringworm. It is particularly favored for Vaginitis because of long lasting residual effect after once a daily application, a 7 day course is generally. Clotrimazole is well tolerated by most patients. Clotrimazole is available 1% lotion, cream and powder, 100 mg vaginal tab.

Continue Miconazole is highly efficacious drug for tinea, otomycosis, cutaneous and vulvovaginal candisasis. However, a higher incidence of vaginal irritation is reported in comparison to Clotrimazole , even pelvic cramps have been experienced. Available 100 mg vaginal tab, 1% ear drops, 2% gel and powder, 2% ointment and spray.
Itraconazole is available in an oral formulation and its absorption is increased by food and by low gastric p. H. Undergoes extensive hepatic metabolism. Itraconazole is the azole of choice in the treatment of dermatophytoses and onychomycosis and is the only agent with significant activity against Aspergillus species.
Continue A dose of 200 mg OD-BD with is used for 3 months or more. Dermatophytosis 1 oo-200 mg OD for 7 -15 days. Onchomycosis 200 mg per day for 3 months. Vaginal candisasis 200 mg OD for days.
Drug interactions Oral absorption of Itraconazole is reduced by antacids, H 2 blockers and PPI. Rifampin, Phenobarbitone, phenytoin, Carbamazepine induce Itraconazole metabolism and reduce it is efficacy.
Fluconazole has good cerebrospinal fluid penetration. Can be given by the intravenous or the oral route. Fluconazole has the least effect on hepatic microsomal enzymes. Fluconazole is the azole of choice in the treatment and secondary prophylaxis of cryptococcal meningitis. It is also effective for mucocutaneous candidiasis.
Continue It is primarily excreted unchanged in urine. It has plasma half life of 25 -30 hours. Fluconazole is 94% absorbed and has good oral bioavailability. A single 150 mg oral dose can cure vaginal candisasis. Oral Fluconazole 150 mg per day for 2 weeks iis highly effective oropharyngeal candisasis. Available 50, 100, 150, 200 mg caps, injection.
Drug interactions Phenytoin Astemizole Warfarin Cyclosporine Zidovudine
Continue THANK YOU…
 Mikael ferm
Mikael ferm Essential drug concept in pharmacology
Essential drug concept in pharmacology Fluconazole nursing implications
Fluconazole nursing implications Antifungal drugs classification
Antifungal drugs classification Classification of antifungal drugs
Classification of antifungal drugs Antifungal sensitivity test
Antifungal sensitivity test Mechanism of action of antifungal drugs
Mechanism of action of antifungal drugs Balanitis cream boots
Balanitis cream boots Define adulteration of crude drugs
Define adulteration of crude drugs Fungal phyla
Fungal phyla There's a fungus among us origin
There's a fungus among us origin Fungi
Fungi Bruised nail beds milady
Bruised nail beds milady Csf findings in different meningitis
Csf findings in different meningitis General fungal life cycle
General fungal life cycle Haustorium in fungi
Haustorium in fungi Ocular histoplasmosis
Ocular histoplasmosis Fungal reproduction
Fungal reproduction Fungal cell characteristics
Fungal cell characteristics Allergic fungal sinusitis treatment
Allergic fungal sinusitis treatment Milady chapter 10 nail disorders and diseases
Milady chapter 10 nail disorders and diseases Black mucus
Black mucus Nucleariids characteristics
Nucleariids characteristics Fungal cell wall
Fungal cell wall Haustorium in fungi
Haustorium in fungi Club fungi are morels truffles bracket fungi yeast
Club fungi are morels truffles bracket fungi yeast Examples of club fungi
Examples of club fungi Postpartum infections
Postpartum infections Opportunistic infections
Opportunistic infections Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Salmonella life cycle
Salmonella life cycle Bone and joint infections
Bone and joint infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Methotrexate yeast infection
Methotrexate yeast infection Understanding the mirai botnet
Understanding the mirai botnet Acute gingival infections
Acute gingival infections Neurosiphyllis
Neurosiphyllis Genital infections
Genital infections Opportunistic infections
Opportunistic infections Storch infections
Storch infections Eye infections
Eye infections Genital infections
Genital infections Storch infections
Storch infections Pharmacology module
Pharmacology module Pharmacology newcastle
Pharmacology newcastle Mdi pharmacology
Mdi pharmacology First pass effect in pharmacology
First pass effect in pharmacology Enzyme inducer drugs
Enzyme inducer drugs Glomerular filtration
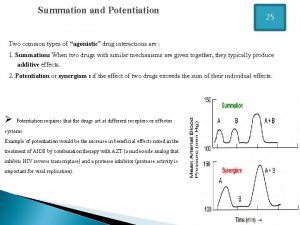
Glomerular filtration Potentiation pharmacology example
Potentiation pharmacology example Pharmacology for veterinary technicians
Pharmacology for veterinary technicians Pharmacology pay
Pharmacology pay Focus on pharmacology essentials for health professionals
Focus on pharmacology essentials for health professionals Therapeutic index
Therapeutic index Chapter 15 diagnostic procedures and pharmacology
Chapter 15 diagnostic procedures and pharmacology Define pharmacology
Define pharmacology First pass effect
First pass effect Potency vs efficacy
Potency vs efficacy Parkinson's disease definition
Parkinson's disease definition Pharmacology chapter 1
Pharmacology chapter 1 Basic & clinical pharmacology
Basic & clinical pharmacology First pass metabolism definition pharmacology
First pass metabolism definition pharmacology Basic principles of pharmacology
Basic principles of pharmacology