Antifungal Agents Gillian Tufts DNP FNP Fungal Infections



- Slides: 29
Antifungal Agents Gillian Tufts DNP, FNP
Fungal Infections • • Blastomycosis Aspergillus Histoplasmosis Mucor Coccidiodomycosis Cryptococcus Dermatophytes Candida albicans
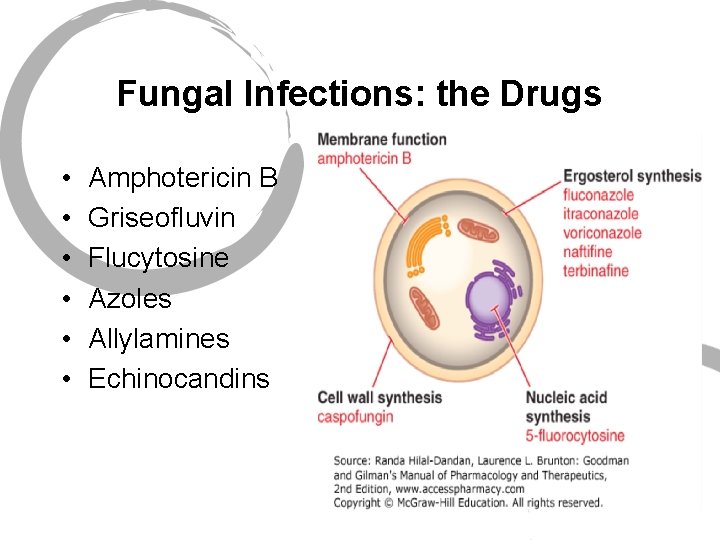
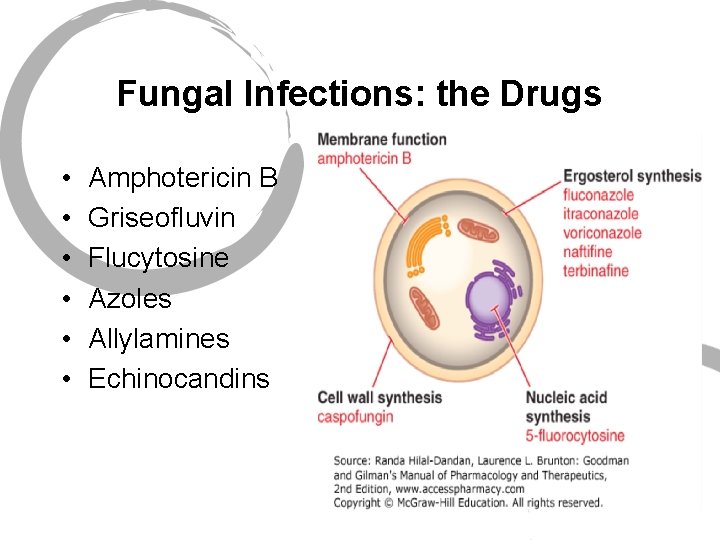
Fungal Infections: the Drugs • • • Amphotericin B Griseofluvin Flucytosine Azoles Allylamines Echinocandins
Azoles • 2 classes • Imidazoles • Ketoconazole • Miconazole (topical) • Clotrimazole (topical) • Butoconazole (topical) • Triazoles • Fluconazole • Itraconazole • Voriconazole • Posaconazole • Terconazole (topical)
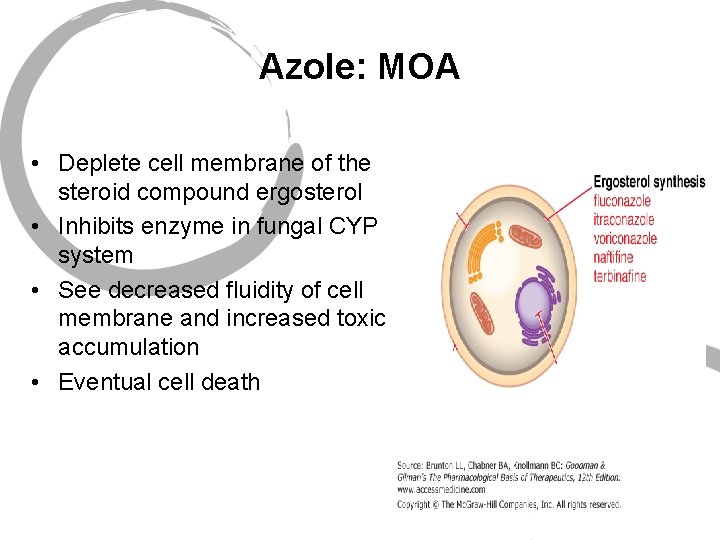
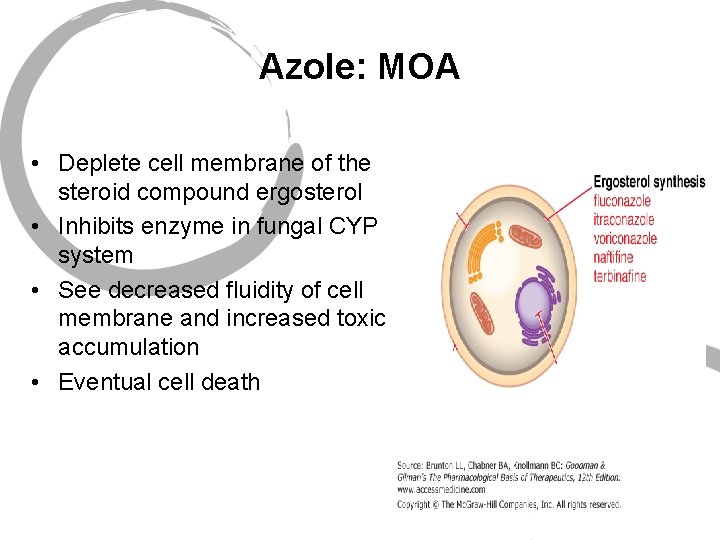
Azole: MOA • Deplete cell membrane of the steroid compound ergosterol • Inhibits enzyme in fungal CYP system • See decreased fluidity of cell membrane and increased toxic accumulation • Eventual cell death
Azoles • Ketoconazole (Nizoral) • First of the azoles • Similar spectrum • Not used much currently
Azoles • Fluconazole (Diflucan) • Spectrum: Candida, Cryptococcus • Resistance with C. glabrata, C. krusei • Alternate: Blastomycosis, Histoplasmosis • Alternate: Onychomycosis • Side effects: generally well tolerated, N/V, headache • ADR: LFT elevation
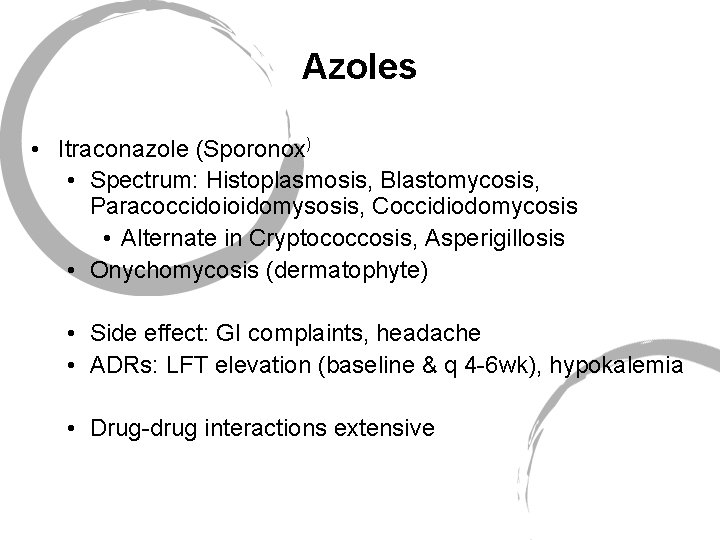
Azoles • Itraconazole (Sporonox) • Spectrum: Histoplasmosis, Blastomycosis, Paracoccidoioidomysosis, Coccidiodomycosis • Alternate in Cryptococcosis, Asperigillosis • Onychomycosis (dermatophyte) • Side effect: GI complaints, headache • ADRs: LFT elevation (baseline & q 4 -6 wk), hypokalemia • Drug-drug interactions extensive
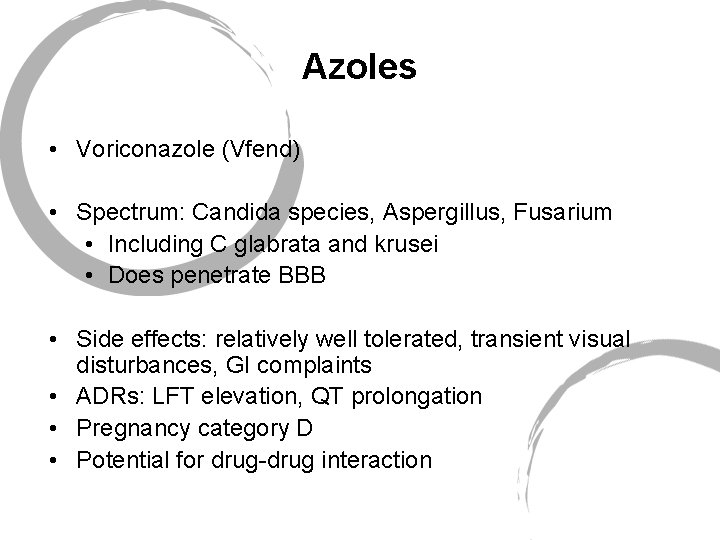
Azoles • Voriconazole (Vfend) • Spectrum: Candida species, Aspergillus, Fusarium • Including C glabrata and krusei • Does penetrate BBB • Side effects: relatively well tolerated, transient visual disturbances, GI complaints • ADRs: LFT elevation, QT prolongation • Pregnancy category D • Potential for drug-drug interaction
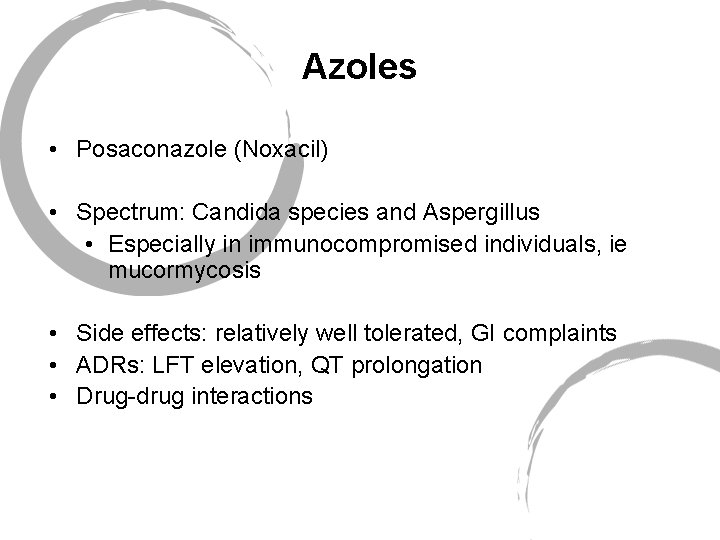
Azoles • Posaconazole (Noxacil) • Spectrum: Candida species and Aspergillus • Especially in immunocompromised individuals, ie mucormycosis • Side effects: relatively well tolerated, GI complaints • ADRs: LFT elevation, QT prolongation • Drug-drug interactions
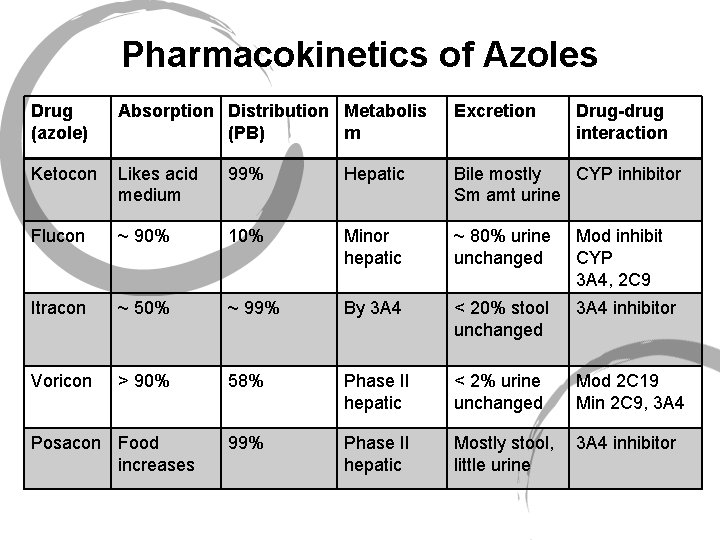
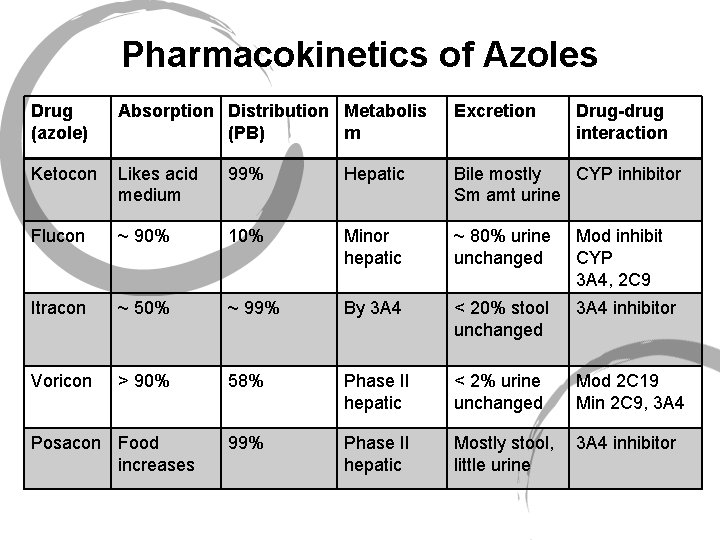
Pharmacokinetics of Azoles Drug (azole) Absorption Distribution Metabolis (PB) m Excretion Ketocon Likes acid medium 99% Hepatic Bile mostly CYP inhibitor Sm amt urine Flucon ~ 90% 10% Minor hepatic ~ 80% urine unchanged Mod inhibit CYP 3 A 4, 2 C 9 Itracon ~ 50% ~ 99% By 3 A 4 < 20% stool unchanged 3 A 4 inhibitor Voricon > 90% 58% Phase II hepatic < 2% urine unchanged Mod 2 C 19 Min 2 C 9, 3 A 4 99% Phase II hepatic Mostly stool, little urine 3 A 4 inhibitor Posacon Food increases Drug-drug interaction
Nystatin • MOA • Similar action to amphotericin B: binds with fungal membrane sterols allowing content leakage and cell death • Poor absorption via intact mucous membranes • Typically used in oral or gastrointestinal fungal infection • Avoid taking at meal times • Prolong medication contact at mucosa • GI distress
Terbinafine (Lamisil) • Spectrum: Dermatophyte, candidiasis • MOA, same as the azoles but different site in pathway • Naftifine (naftin) topical only • Tends to accumulate in the skin, nails, fat tissue • Generally well tolerated: GI SEs, funny taste, transient mild skin itching • ADRs: hepatotoxicity, rarely serious skin rash
Griseofulvin • MOA: though to work through disrupting the microtubule function. This is part of mitosis, alters this process • Spectrum: Dermatophytes • Absorption increased by food, bioavailability up to 75%, also increased with new formulations: • Micro-sized and ultra-microsized • Deposited into keratin precursor cells, only small found in other tissues • HA, N/V, GI, phototoxicity, disulfiram reaction • Drug interactions: Inducer, warfarin, oral contraceptives

Yeast Infections Pharmacologic Management
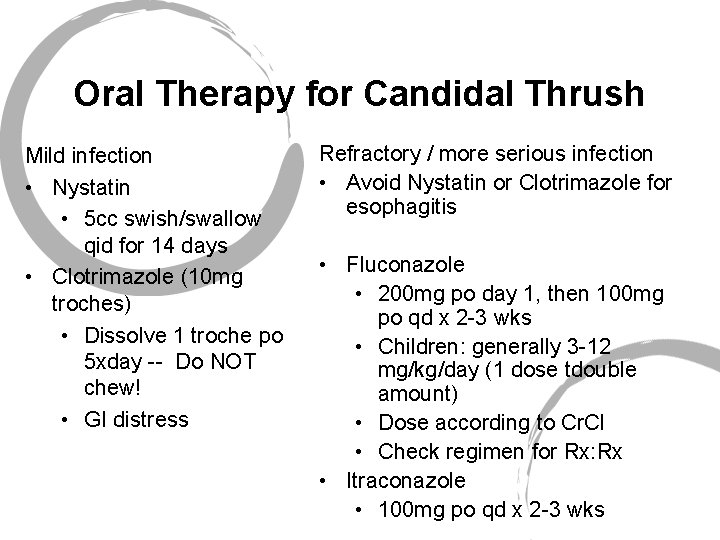
Oral Therapy for Candidal Thrush Mild infection • Nystatin • 5 cc swish/swallow qid for 14 days • Clotrimazole (10 mg troches) • Dissolve 1 troche po 5 xday -- Do NOT chew! • GI distress Refractory / more serious infection • Avoid Nystatin or Clotrimazole for esophagitis • Fluconazole • 200 mg po day 1, then 100 mg po qd x 2 -3 wks • Children: generally 3 -12 mg/kg/day (1 dose tdouble amount) • Dose according to Cr. Cl • Check regimen for Rx: Rx • Itraconazole • 100 mg po qd x 2 -3 wks
Vulvovaginal Candidiasis: Treatment Options OTC Azoles • Butoconazole (Femstat 3™) • Clotrimazole (Gyne-Lotrimin™, Mycelex™) • Miconazole (Monistat 7™) • Tioconazole (Vagistat-1™) Prescription Azoles • Clotrimazole vaginal tablets • Miconazole vaginal suppository (Monistat. TM) • Terconazole (Terazol™): 3 or 7 day cream or suppository • Fluconazole oral tab: 150 mg po x 1, may repeat in 3 -5 d

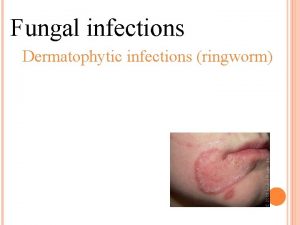
Tinea Infections Pharmacologic Management
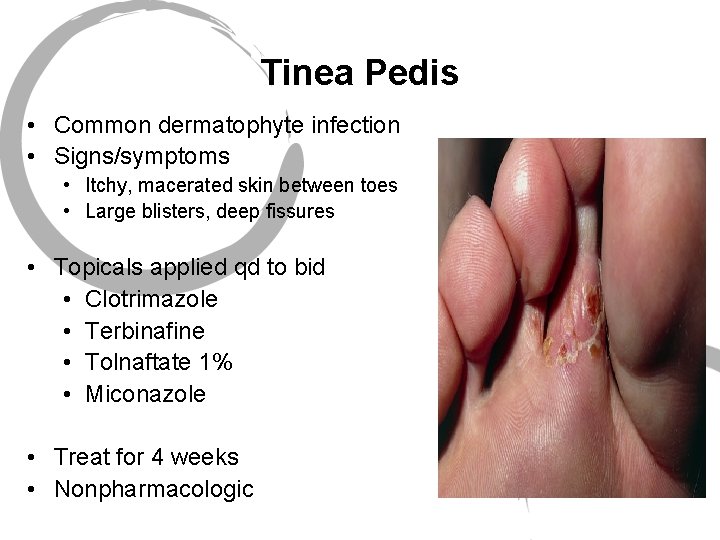
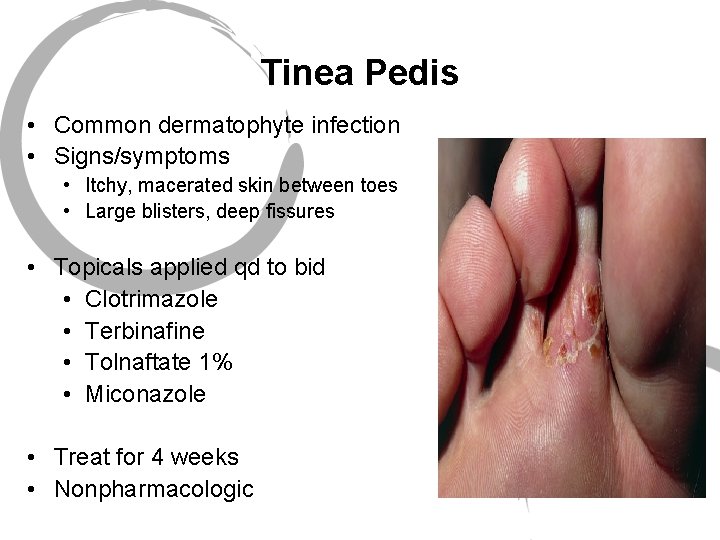
Tinea Pedis • Common dermatophyte infection • Signs/symptoms • Itchy, macerated skin between toes • Large blisters, deep fissures • Topicals applied qd to bid • Clotrimazole • Terbinafine • Tolnaftate 1% • Miconazole • Treat for 4 weeks • Nonpharmacologic
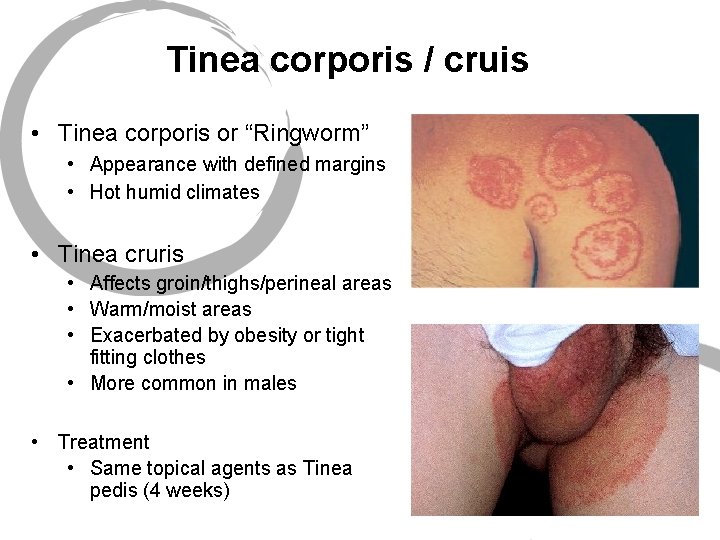
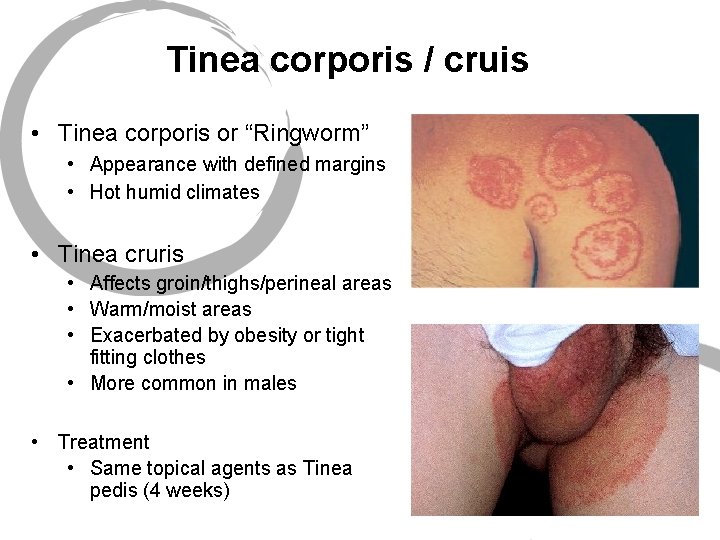
Tinea corporis / cruis • Tinea corporis or “Ringworm” • Appearance with defined margins • Hot humid climates • Tinea cruris • Affects groin/thighs/perineal areas • Warm/moist areas • Exacerbated by obesity or tight fitting clothes • More common in males • Treatment • Same topical agents as Tinea pedis (4 weeks)

Fungal Nail Infections • Tinea unguium or onychomycosis • Topical therapy not effective • Achieve fungicidal concentration within nail • Toe nail thickness > finger nail thickness • Terbinafine • Itraconazole
Fungal Nail Infections • Griseofulvin: cure rates < 20%, relapse 60% • Terbinafine 250 mg daily • Fingernail for 6 weeks • Toenail for 12 weeks • Itraconazole • 200 mg daily for 8 weeks • Pulsatile dosing: 200 mg BID for 1 week/month for 3 mos • Fluconazole (being studied) • 300 mg po q wk x 3 -6 mo (fingers) • 6 -12 mo (toes)
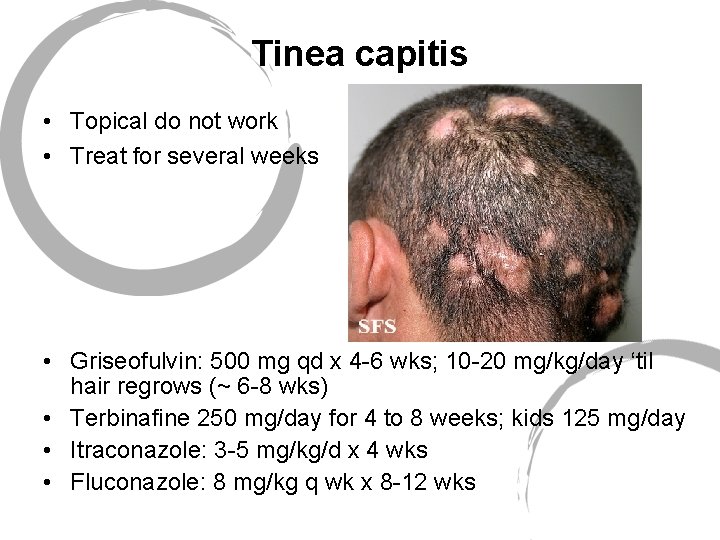
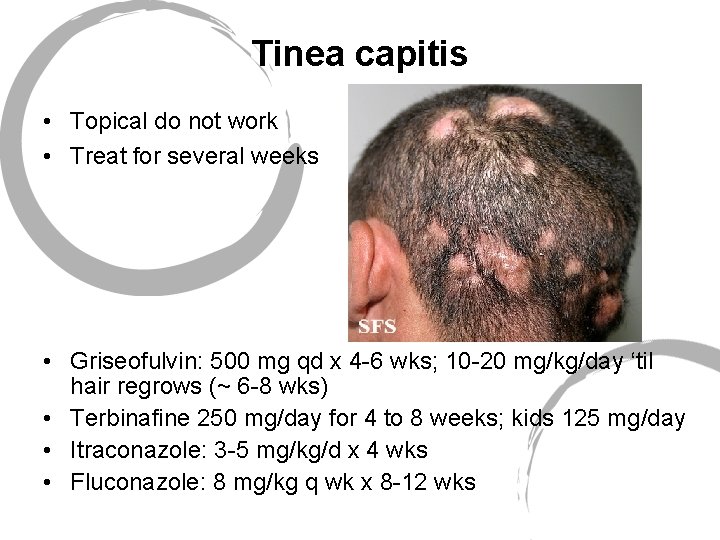
Tinea capitis • Topical do not work • Treat for several weeks • Griseofulvin: 500 mg qd x 4 -6 wks; 10 -20 mg/kg/day ‘til hair regrows (~ 6 -8 wks) • Terbinafine 250 mg/day for 4 to 8 weeks; kids 125 mg/day • Itraconazole: 3 -5 mg/kg/d x 4 wks • Fluconazole: 8 mg/kg q wk x 8 -12 wks
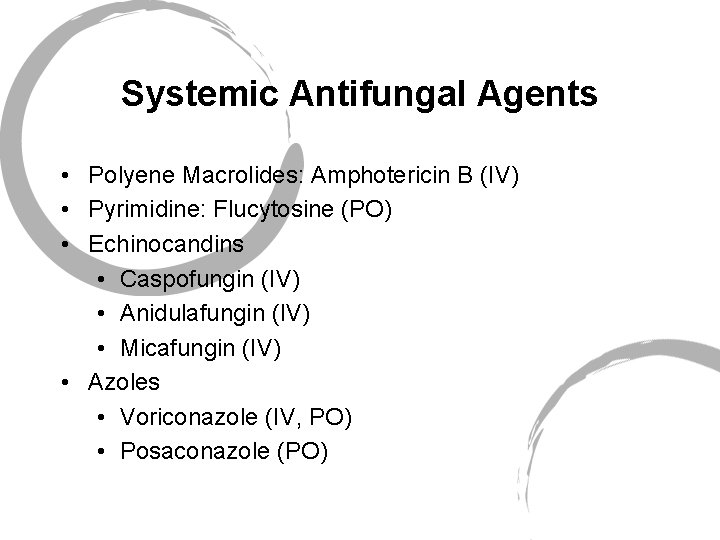
Systemic Antifungal Agents • Polyene Macrolides: Amphotericin B (IV) • Pyrimidine: Flucytosine (PO) • Echinocandins • Caspofungin (IV) • Anidulafungin (IV) • Micafungin (IV) • Azoles • Voriconazole (IV, PO) • Posaconazole (PO)
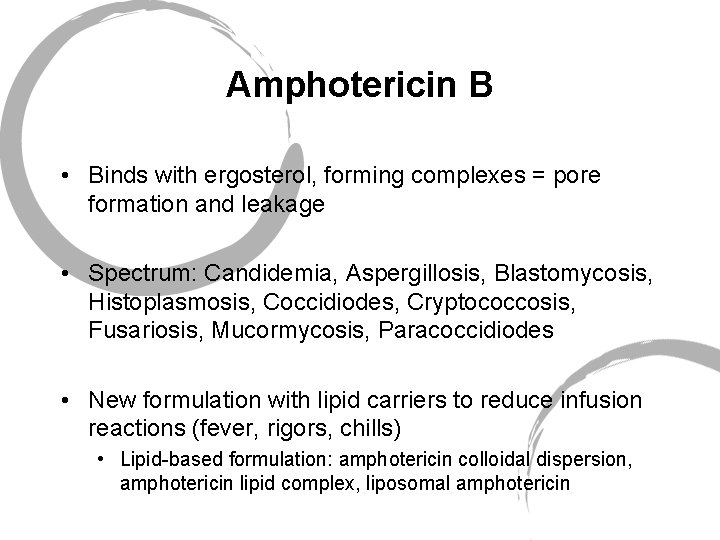
Amphotericin B • Binds with ergosterol, forming complexes = pore formation and leakage • Spectrum: Candidemia, Aspergillosis, Blastomycosis, Histoplasmosis, Coccidiodes, Cryptococcosis, Fusariosis, Mucormycosis, Paracoccidiodes • New formulation with lipid carriers to reduce infusion reactions (fever, rigors, chills) • Lipid-based formulation: amphotericin colloidal dispersion, amphotericin lipid complex, liposomal amphotericin
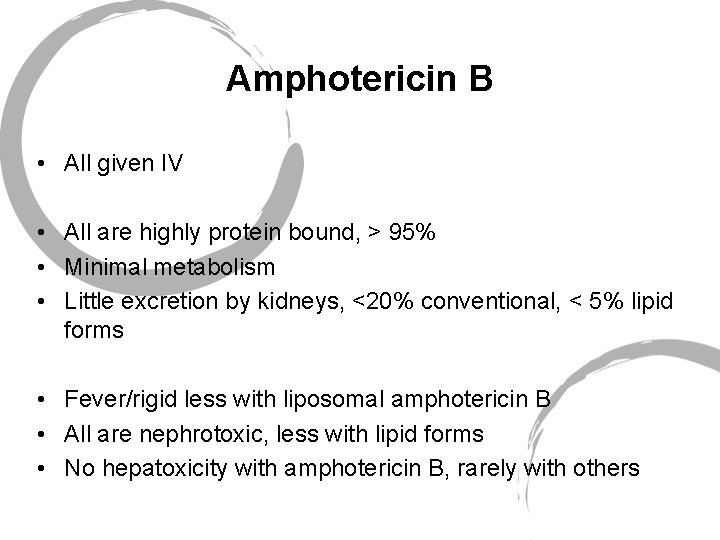
Amphotericin B • All given IV • All are highly protein bound, > 95% • Minimal metabolism • Little excretion by kidneys, <20% conventional, < 5% lipid forms • Fever/rigid less with liposomal amphotericin B • All are nephrotoxic, less with lipid forms • No hepatoxicity with amphotericin B, rarely with others
Flucytosine • Impairs fungal DNA production • Useful in candidia and cryptococcus • Oral agent with good bioavailability • Little protein binding • ~ 80% renal excretion • GI side effects
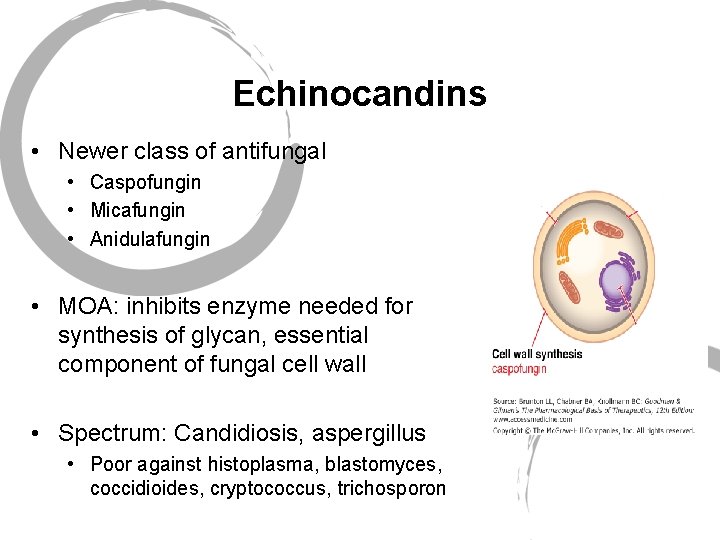
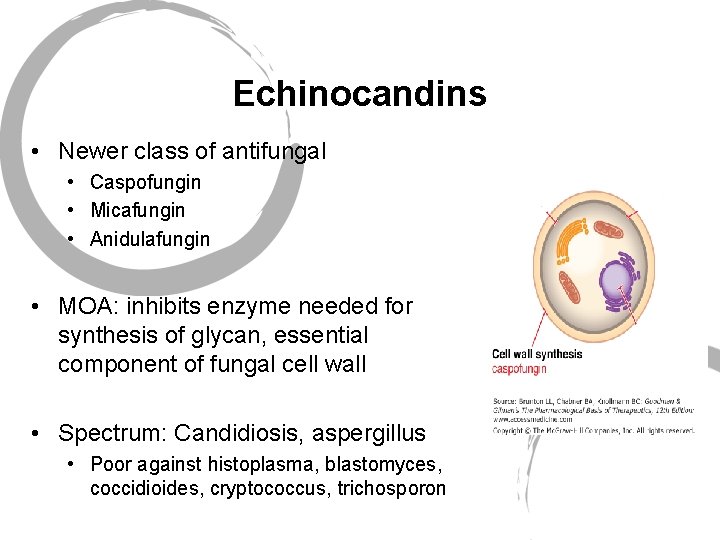
Echinocandins • Newer class of antifungal • Caspofungin • Micafungin • Anidulafungin • MOA: inhibits enzyme needed for synthesis of glycan, essential component of fungal cell wall • Spectrum: Candidiosis, aspergillus • Poor against histoplasma, blastomyces, coccidioides, cryptococcus, trichosporon
Echinocandins • All 3 are large molecules, poor bioavailability = IV administration • All are highly protein bound • None are metabolized by CYP P 450 system • Excretion, negligible unchanged in urine, metabolites in feces and urine • Capsofungin has indication in children 3 mos to 17 yrs • Data available with others
 Fluconazole nursing implications
Fluconazole nursing implications Flucytosine mechanism of action
Flucytosine mechanism of action Classification of antifungal drugs
Classification of antifungal drugs Antifungal sensitivity test
Antifungal sensitivity test Mechanism of action of antifungal drugs
Mechanism of action of antifungal drugs Thrush tablets boots
Thrush tablets boots Bpun unal
Bpun unal Sicodis que es
Sicodis que es Chamberlain fnp practicum handbook
Chamberlain fnp practicum handbook Uca dnp program
Uca dnp program Walden university meditrek
Walden university meditrek Inversion lenta fnp
Inversion lenta fnp Nurse practitioner core competencies
Nurse practitioner core competencies Ocular histoplasmosis
Ocular histoplasmosis Csf analysis interpretation
Csf analysis interpretation Fungal life cycles
Fungal life cycles Fungal nutrition
Fungal nutrition Black mucus
Black mucus Fungal reproduction
Fungal reproduction Single celled fungi
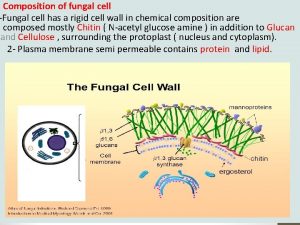
Single celled fungi Fungal cell walls are characteristic in having
Fungal cell walls are characteristic in having Allergic fungal sinusitis treatment
Allergic fungal sinusitis treatment Milady nail diseases and disorders
Milady nail diseases and disorders Nucleariids characteristics
Nucleariids characteristics In what situation should a nail service not be performed
In what situation should a nail service not be performed Fungal phyla
Fungal phyla There fungus among us
There fungus among us Fungi singular
Fungi singular Postpartum infections
Postpartum infections A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes