Antifungal Drugs Hamzeh Elayan 2015 1 Types of

- Slides: 20
Antifungal Drugs Hamzeh Elayan, 2015 1
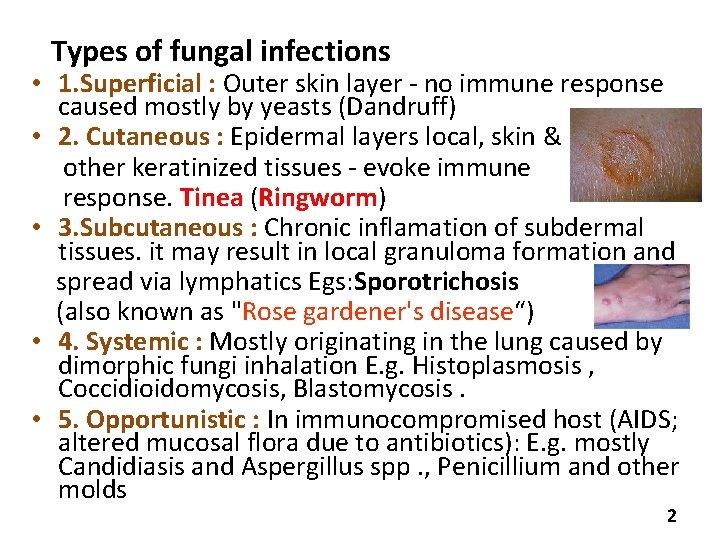
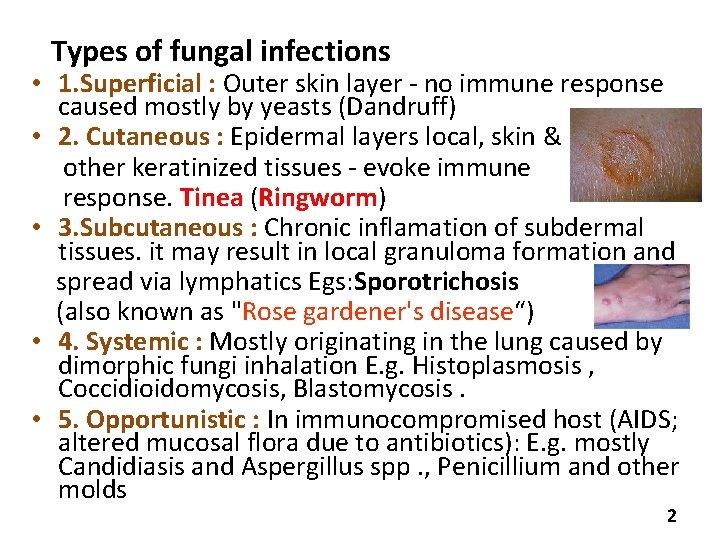
Types of fungal infections • 1. Superficial : Outer skin layer - no immune response caused mostly by yeasts (Dandruff) • 2. Cutaneous : Epidermal layers local, skin & other keratinized tissues - evoke immune response. Tinea (Ringworm) • 3. Subcutaneous : Chronic inflamation of subdermal tissues. it may result in local granuloma formation and spread via lymphatics Egs: Sporotrichosis (also known as "Rose gardener's disease“) • 4. Systemic : Mostly originating in the lung caused by dimorphic fungi inhalation E. g. Histoplasmosis , Coccidioidomycosis, Blastomycosis. • 5. Opportunistic : In immunocompromised host (AIDS; altered mucosal flora due to antibiotics): E. g. mostly Candidiasis and Aspergillus spp. , Penicillium and other molds 2
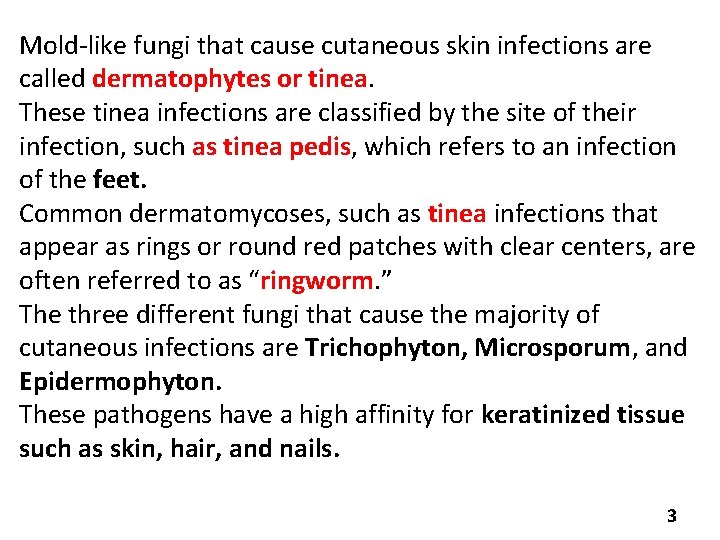
Mold-like fungi that cause cutaneous skin infections are called dermatophytes or tinea. These tinea infections are classified by the site of their infection, such as tinea pedis, which refers to an infection of the feet. Common dermatomycoses, such as tinea infections that appear as rings or round red patches with clear centers, are often referred to as “ringworm. ” The three different fungi that cause the majority of cutaneous infections are Trichophyton, Microsporum, and Epidermophyton. These pathogens have a high affinity for keratinized tissue such as skin, hair, and nails. 3
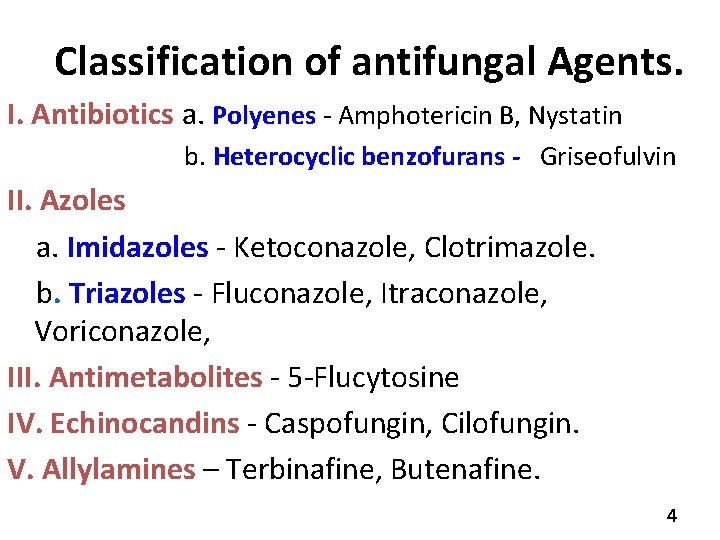
Classification of antifungal Agents. I. Antibiotics a. Polyenes - Amphotericin B, Nystatin b. Heterocyclic benzofurans - Griseofulvin II. Azoles a. Imidazoles - Ketoconazole, Clotrimazole. b. Triazoles - Fluconazole, Itraconazole, Voriconazole, III. Antimetabolites - 5 -Flucytosine IV. Echinocandins - Caspofungin, Cilofungin. V. Allylamines – Terbinafine, Butenafine. 4
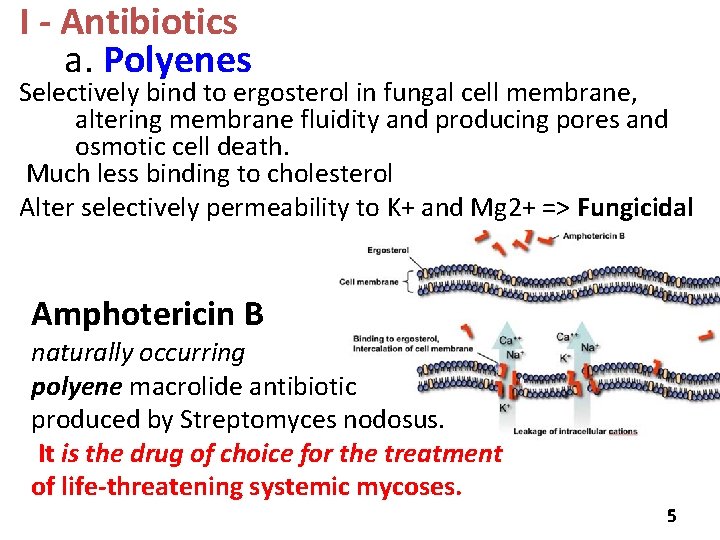
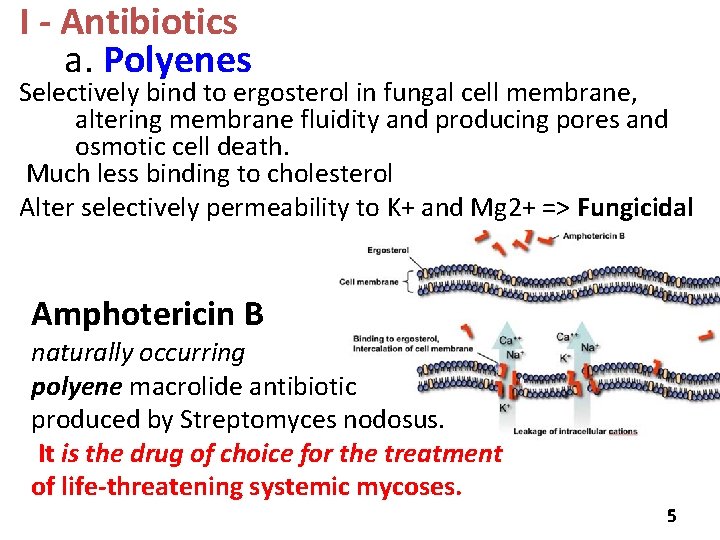
I - Antibiotics a. Polyenes Selectively bind to ergosterol in fungal cell membrane, altering membrane fluidity and producing pores and osmotic cell death. Much less binding to cholesterol Alter selectively permeability to K+ and Mg 2+ => Fungicidal Amphotericin B naturally occurring polyene macrolide antibiotic produced by Streptomyces nodosus. It is the drug of choice for the treatment of life-threatening systemic mycoses. 5
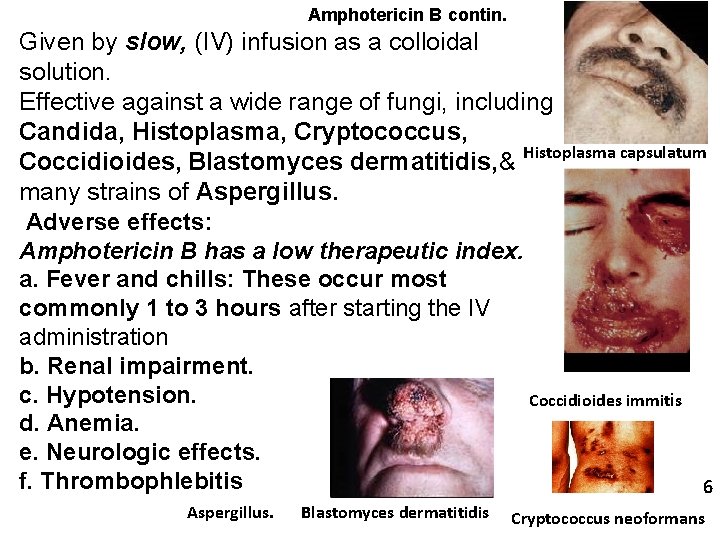
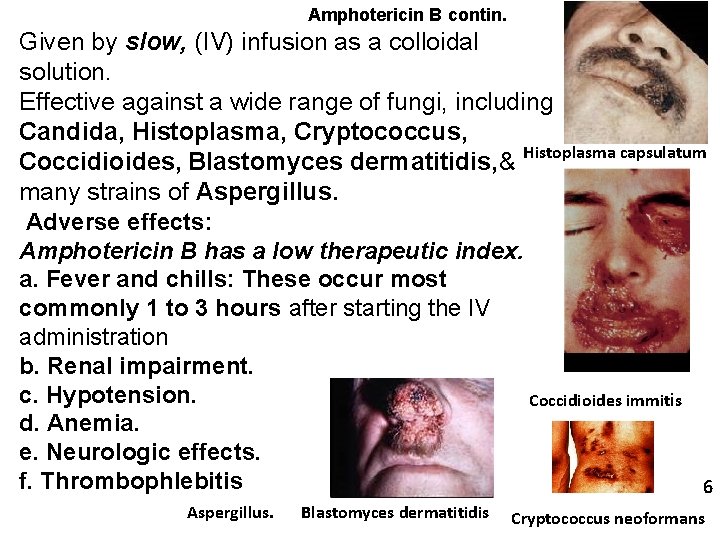
Amphotericin B contin. Given by slow, (IV) infusion as a colloidal solution. Effective against a wide range of fungi, including Candida, Histoplasma, Cryptococcus, Coccidioides, Blastomyces dermatitidis, & Histoplasma capsulatum many strains of Aspergillus. Adverse effects: Amphotericin B has a low therapeutic index. a. Fever and chills: These occur most commonly 1 to 3 hours after starting the IV administration b. Renal impairment. c. Hypotension. Coccidioides immitis d. Anemia. e. Neurologic effects. f. Thrombophlebitis 6 Aspergillus. Blastomyces dermatitidis Cryptococcus neoformans
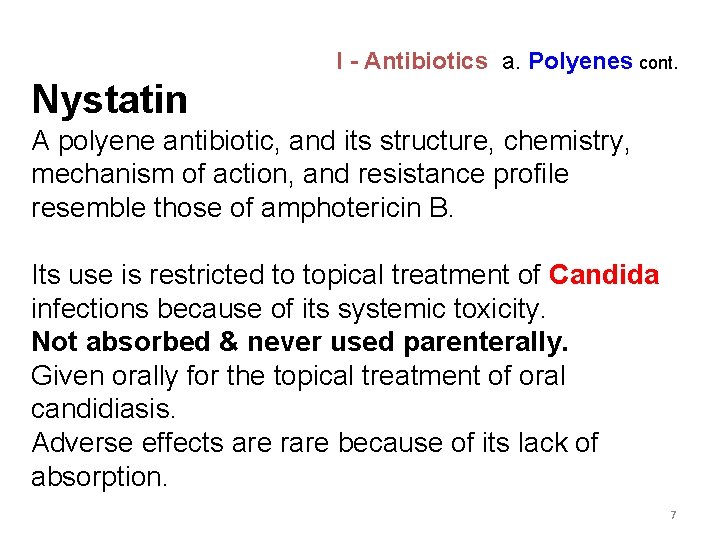
I - Antibiotics a. Polyenes cont. Nystatin A polyene antibiotic, and its structure, chemistry, mechanism of action, and resistance profile resemble those of amphotericin B. Its use is restricted to topical treatment of Candida infections because of its systemic toxicity. Not absorbed & never used parenterally. Given orally for the topical treatment of oral candidiasis. Adverse effects are rare because of its lack of absorption. 7
I - Antibiotics b. Heterocyclic benzofurans Griseofulvin Inhibits fungal growth by binding to microtubules causing disruption of the mitotic spindle and inhibition of fungal mitosis. Given Orally. High fat meal enhances the oral absorption Largely replaced by oral terbinafine for the treatment of infections of the nails but still used for ringworm & dermatophytosis of the skin &hair. Requires treatment of 6 to 12 months & it accumulates in newly synthesized keratin- containing tissue. 8
II. Azoles They inhibit C-14α- demethylase thereby blocking the demethylation of lanosterol to ergosterol. Fungistatic , active against systemic fungi and dermatophytes: fungicidal at higher concentration a. Imidazoles Adverse effects due to inhibition of human gonadal and adrenal steroid synthesis, leading to decreased testosterone and cortisol production. Drug interactions due to inhibition of cyt. P 450 enzymes. Clotrimazole : topical – Candidiasis, tinea 9

Ketoconazole II. Azoles a. Imidazoles cont. First oral -azole , older, and more toxic (mostly replaced by fluconazole and itraconazole) Absorption requires gastric acid (antacids interfere). Poor concentration in CSF Metabolized by Cyt. P 450 enzymes, excretion through the bile. Antifungal spectrum: Oral ketoconazole is active against many fungi, but not aspergillus species. Therapeutic Use : Topical ketoconazole is used to treat tinea sps. (ringworm) & tinea versicolor caused by Malassezia furfur. Oral ketoconazole is used to treat systemic infections, such as coccidiomycosis and histoplasmosis. 10 Also oral, esophageal & mucocutaneous candidiasis
Adverse effects: Ketoconazole, con allergies, GI disturbances are the most common. gynecomastia, decreased libido, impotence, and menstrual irregularities, result from the blocking of androgen and adrenal steroid synthesis. Hepatitis rare. Drug interactions and contraindications: By inhibiting CYP 450, ketoconazole can potentiate the toxicities of drugs. Drugs that decrease gastric acidity can decrease absorption of ketoconazole. Ketoconazole and amphotericin B should not be used together, because the decrease in ergosterol in the fungal membrane reduces the fungicidal action of amphotericin B 11
II. Azoles b. Triazoles Newer, less toxic, more effective Fluconazole The drug of choice for Cryptococcal & coccidial meningitis, & for most candidemias (presence of Candida in the blood), and for coccidioidomycosis (inhaled spores cause pneumonia). Effective against most forms of mucocutaneous candidiasis. orally or IV. Treats vaginal candidiasis in a single oral dose. Absorption not dependent on gastric acidity, penetrates into CSF. poorly metabolized. excreted via the kidney Adverse effects -less endocrine side effects than those with ketoconazole. 12 -Nausea, vomiting, and rashes.
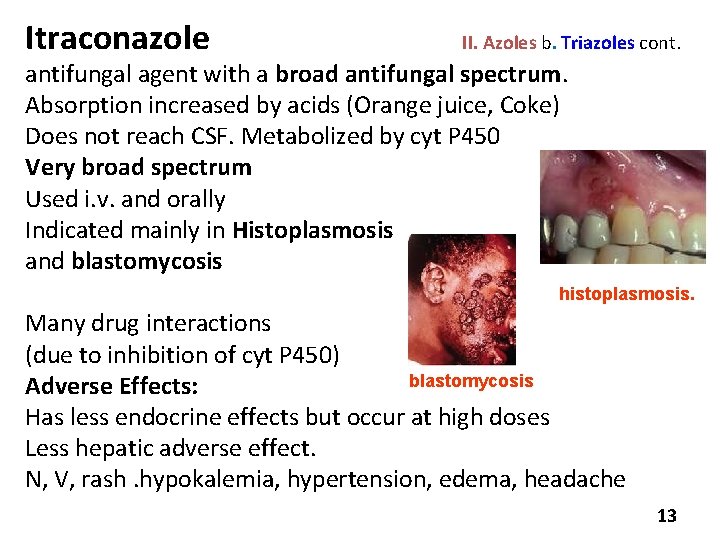
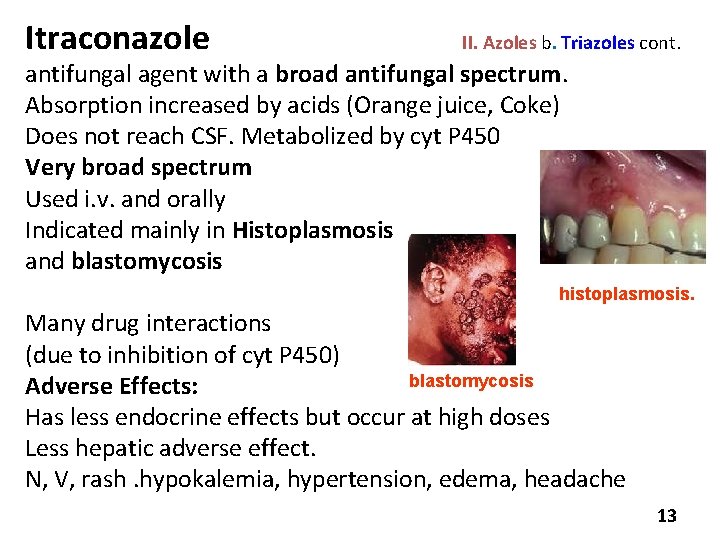
Itraconazole II. Azoles b. Triazoles cont. antifungal agent with a broad antifungal spectrum. Absorption increased by acids (Orange juice, Coke) Does not reach CSF. Metabolized by cyt P 450 Very broad spectrum Used i. v. and orally Indicated mainly in Histoplasmosis and blastomycosis histoplasmosis. Many drug interactions (due to inhibition of cyt P 450) blastomycosis Adverse Effects: Has less endocrine effects but occur at high doses Less hepatic adverse effect. N, V, rash. hypokalemia, hypertension, edema, headache 13
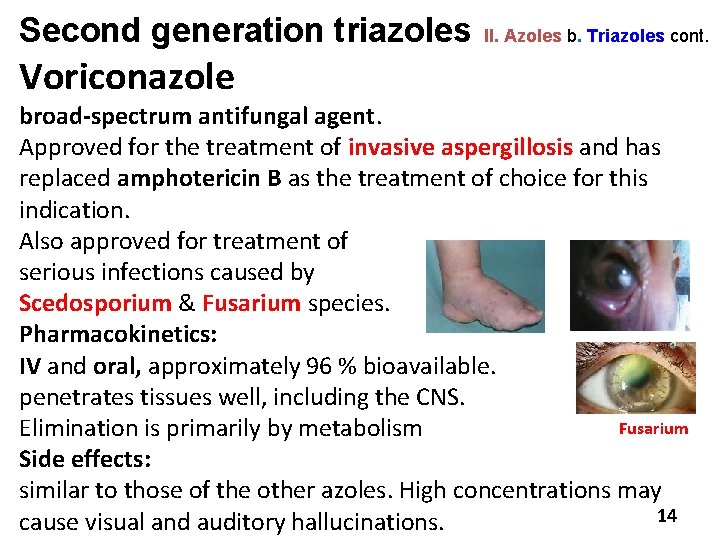
Second generation triazoles Voriconazole II. Azoles b. Triazoles cont. broad-spectrum antifungal agent. Approved for the treatment of invasive aspergillosis and has replaced amphotericin B as the treatment of choice for this indication. Also approved for treatment of serious infections caused by Scedosporium & Fusarium species. Pharmacokinetics: IV and oral, approximately 96 % bioavailable. penetrates tissues well, including the CNS. Fusarium Elimination is primarily by metabolism Side effects: similar to those of the other azoles. High concentrations may 14 cause visual and auditory hallucinations.
Posaconazole II. Azoles b. Triazoles cont. New oral, broad-spectrum antifungal agent Approved in 2006 to prevent Candida and Aspergillus infections in severely immunocompromised patients and for the treatment of oropharyngeal candidiasis. To be effective, posaconazole must be taken with a high fat meal. Side effects: Relatively well tolerated N, V, diarrhea, abdominal pain & headaches. 15
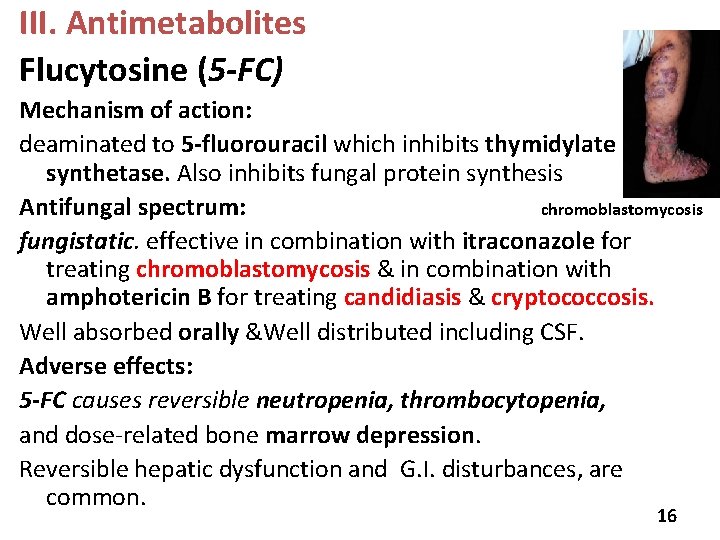
III. Antimetabolites Flucytosine (5 -FC) Mechanism of action: deaminated to 5 -fluorouracil which inhibits thymidylate synthetase. Also inhibits fungal protein synthesis Antifungal spectrum: chromoblastomycosis fungistatic. effective in combination with itraconazole for treating chromoblastomycosis & in combination with amphotericin B for treating candidiasis & cryptococcosis. Well absorbed orally &Well distributed including CSF. Adverse effects: 5 -FC causes reversible neutropenia, thrombocytopenia, and dose-related bone marrow depression. Reversible hepatic dysfunction and G. I. disturbances, are common. 16
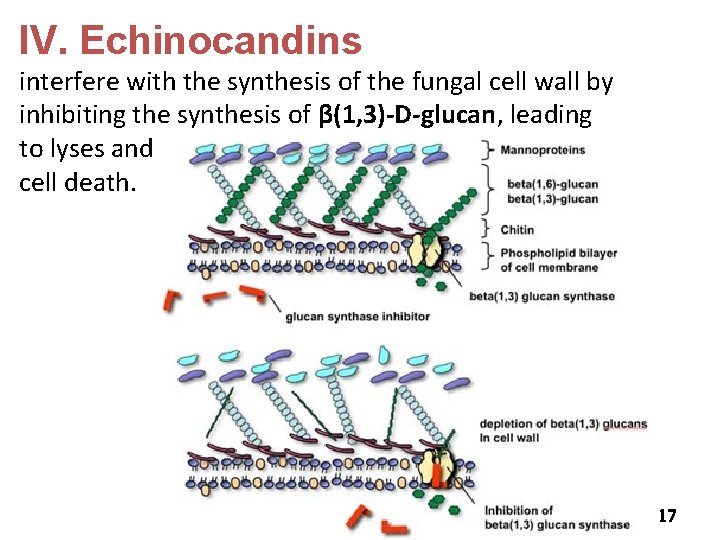
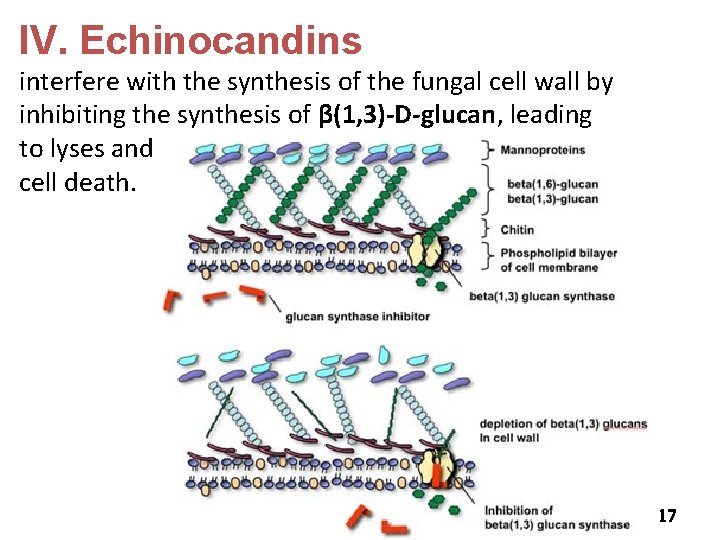
IV. Echinocandins interfere with the synthesis of the fungal cell wall by inhibiting the synthesis of β(1, 3)-D-glucan, leading to lyses and cell death. 17
Caspofungin IV. Echinocandins, cont. Active against Aspergillus & most Candida sps, including species resistant to azoles. Adverse effects fever, rash, nausea, and phlebitis. Flushing due to the release of histamine from mast cells. Caspofungin is a second-line antifungal for those who have failed or cannot tolerate amphotericin B or an azole. Micafungin New member of the echinocandins class of antifungal drugs. Effective against Candida species The dose of micafungin does not need to be adjusted in renal impairment or mild-to-moderate hepatic dysfunction. No drug interactions. 18
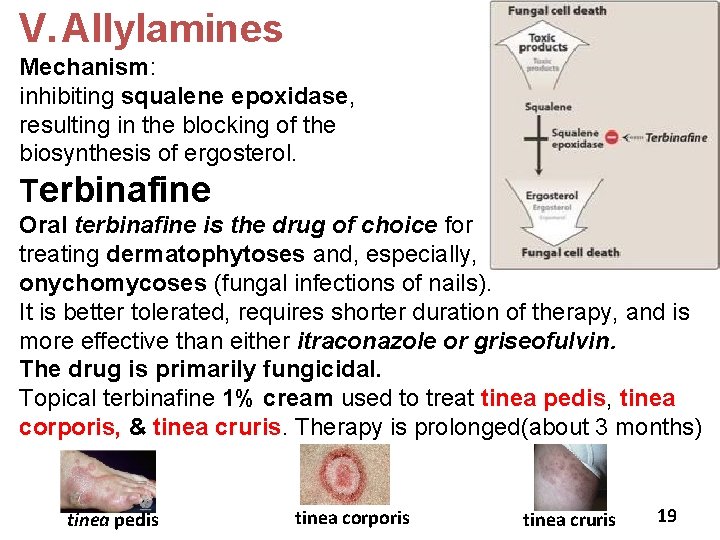
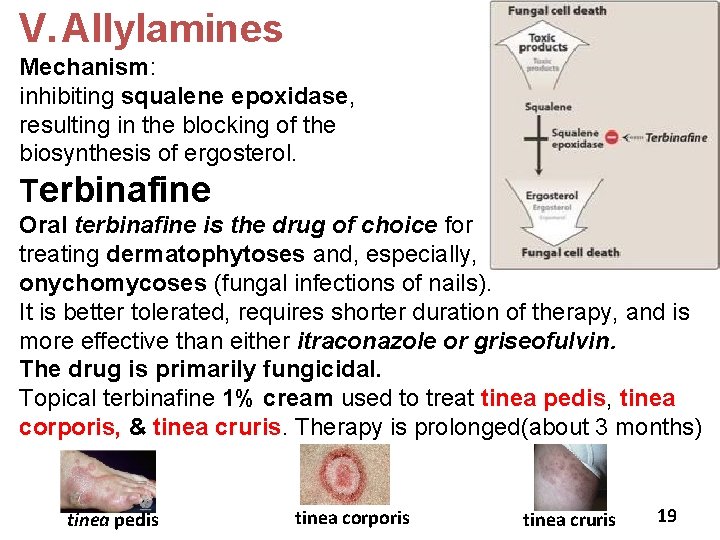
V. Allylamines Mechanism: inhibiting squalene epoxidase, resulting in the blocking of the biosynthesis of ergosterol. Terbinafine Oral terbinafine is the drug of choice for treating dermatophytoses and, especially, onychomycoses (fungal infections of nails). It is better tolerated, requires shorter duration of therapy, and is more effective than either itraconazole or griseofulvin. The drug is primarily fungicidal. Topical terbinafine 1% cream used to treat tinea pedis, tinea corporis, & tinea cruris. Therapy is prolonged(about 3 months) tinea pedis tinea corporis tinea cruris 19
Pharmacokinetics: Terbinafine, cont. oral and topical , bioavailability is 40% (first-pass metabolism). 99% bound to plasma proteins. Deposited in the skin, nails, and fat. Accumulates in breast milk and should not be given to nursing mothers. half-life of 200 to 400 hours extensively metabolized prior to urinary excretion Adverse effects: The most common are GI (diarrhea, dyspepsia, and nausea), headache, and rash. Taste and visual disturbances have been reported. Rarely, terbinafine may cause hepatotoxicity and neutropenia. 20
 Mechanism of action of antifungal drugs
Mechanism of action of antifungal drugs University of science and technology of mazandaran
University of science and technology of mazandaran Antifungal drugs classification
Antifungal drugs classification Flucytosine mechanism of action
Flucytosine mechanism of action Flucytosine mechanism of action
Flucytosine mechanism of action Antifungal sensitivity test
Antifungal sensitivity test Boots clotrimazole cream
Boots clotrimazole cream Types of drugs
Types of drugs Types of drugs
Types of drugs Methods of adulteration of crude drugs
Methods of adulteration of crude drugs The drug basket method is used to dispense medication to.
The drug basket method is used to dispense medication to. Types of drugs
Types of drugs Drug and alcohol jeopardy
Drug and alcohol jeopardy Schedule 1 drugs
Schedule 1 drugs Antithyroid drugs classification
Antithyroid drugs classification Fibrinolytic drugs classification
Fibrinolytic drugs classification Streptokinase دواء
Streptokinase دواء Thrombolytic drugs
Thrombolytic drugs Thrombolytic drugs mechanism of action
Thrombolytic drugs mechanism of action Fibrinolytic drugs
Fibrinolytic drugs British model involved with drugs
British model involved with drugs