Pediatric infectious diseases Vaccination programs Prof Dr Gyrgy










- Slides: 53

Pediatric infectious diseases. Vaccination programs Prof. Dr. György Fekete
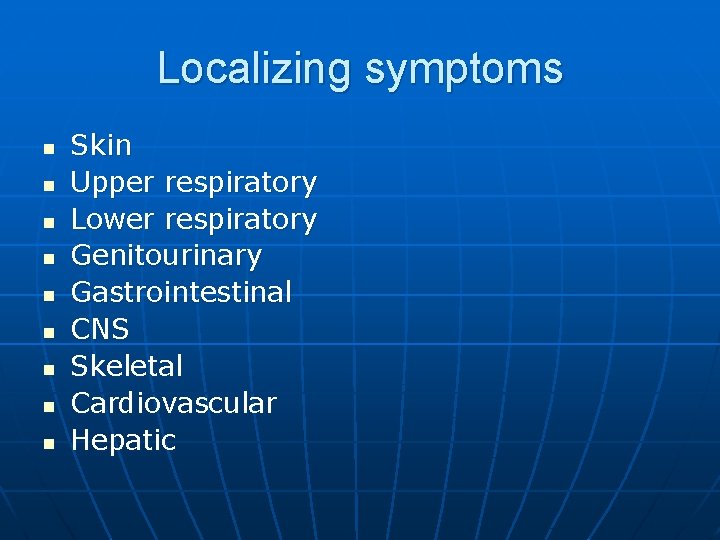
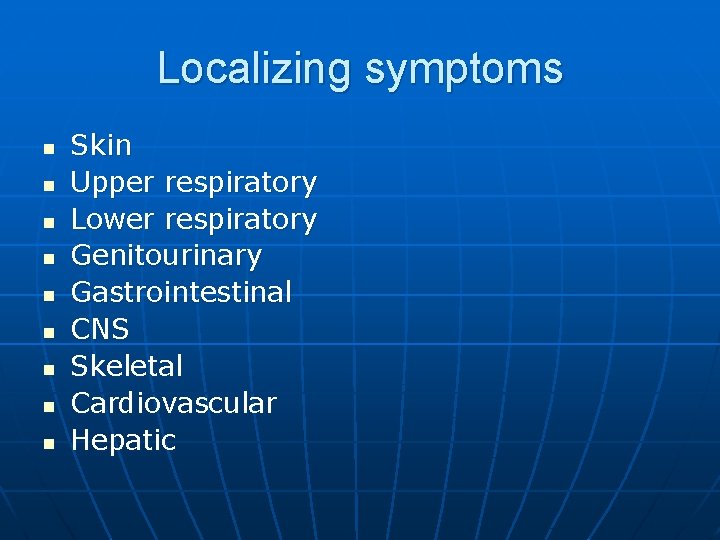
Localizing symptoms n n n n n Skin Upper respiratory Lower respiratory Genitourinary Gastrointestinal CNS Skeletal Cardiovascular Hepatic
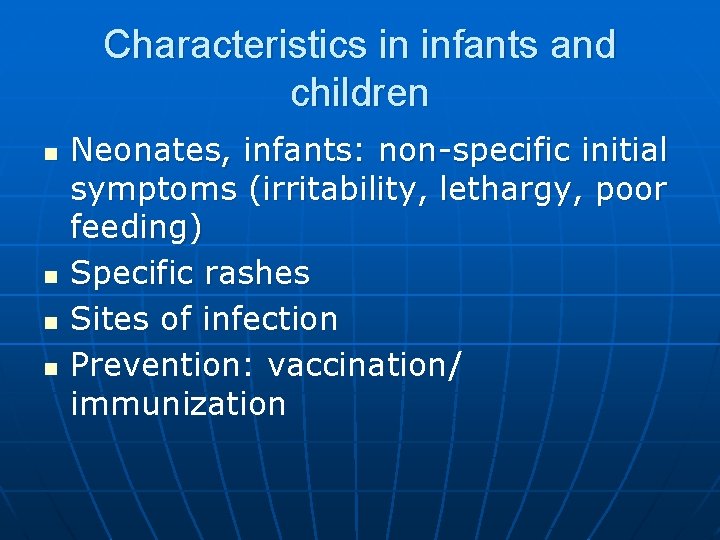
Characteristics in infants and children n n Neonates, infants: non-specific initial symptoms (irritability, lethargy, poor feeding) Specific rashes Sites of infection Prevention: vaccination/ immunization
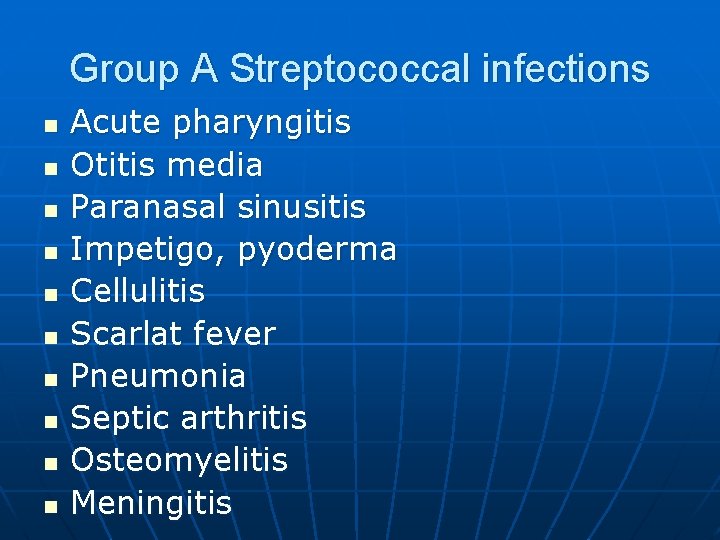
Group A Streptococcal infections n n n n n Acute pharyngitis Otitis media Paranasal sinusitis Impetigo, pyoderma Cellulitis Scarlat fever Pneumonia Septic arthritis Osteomyelitis Meningitis
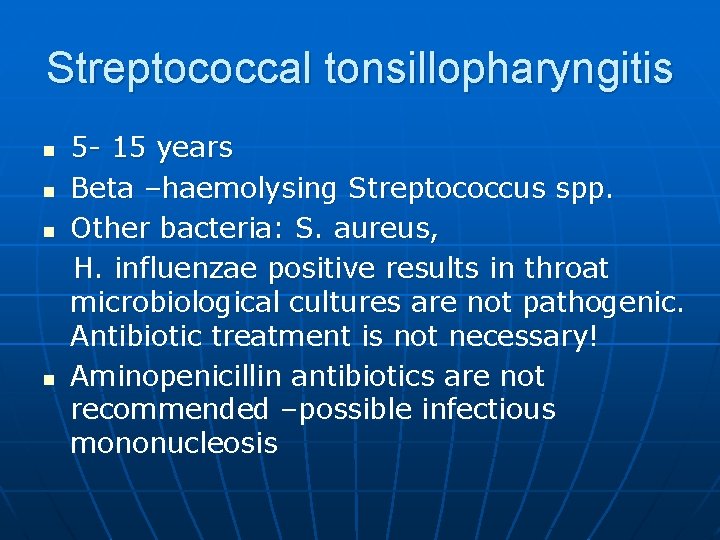
Streptococcal tonsillopharyngitis n n 5 - 15 years Beta –haemolysing Streptococcus spp. Other bacteria: S. aureus, H. influenzae positive results in throat microbiological cultures are not pathogenic. Antibiotic treatment is not necessary! Aminopenicillin antibiotics are not recommended –possible infectious mononucleosis

Tonsillopharyngitis streptococcica n n Diagnosis: microbiology (sensitivity: 90 -95%), streptococcal antigen test (specificity: >95%) Treatment: oral Penicillin, 10 days

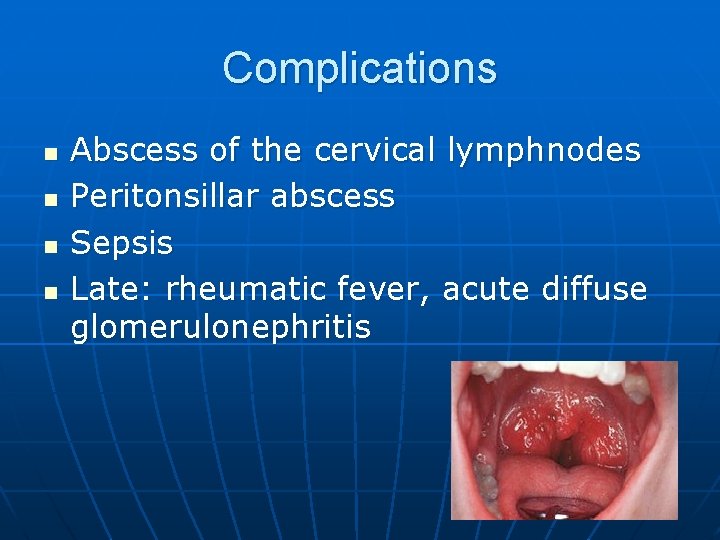
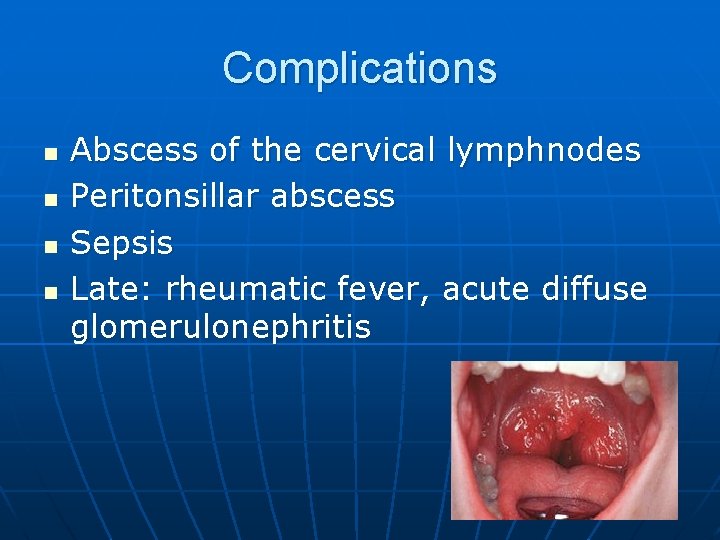
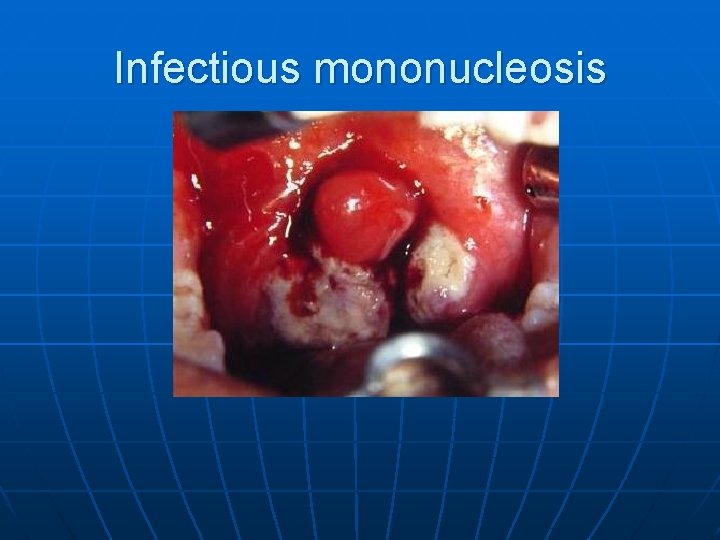
Complications n n Abscess of the cervical lymphnodes Peritonsillar abscess Sepsis Late: rheumatic fever, acute diffuse glomerulonephritis
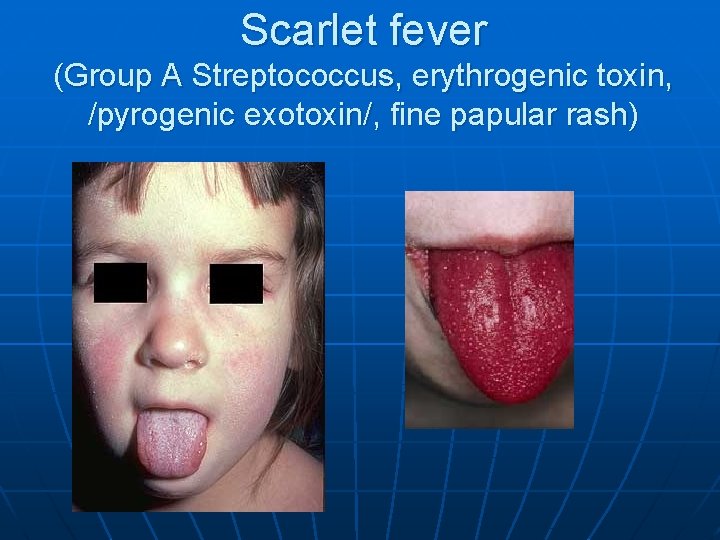
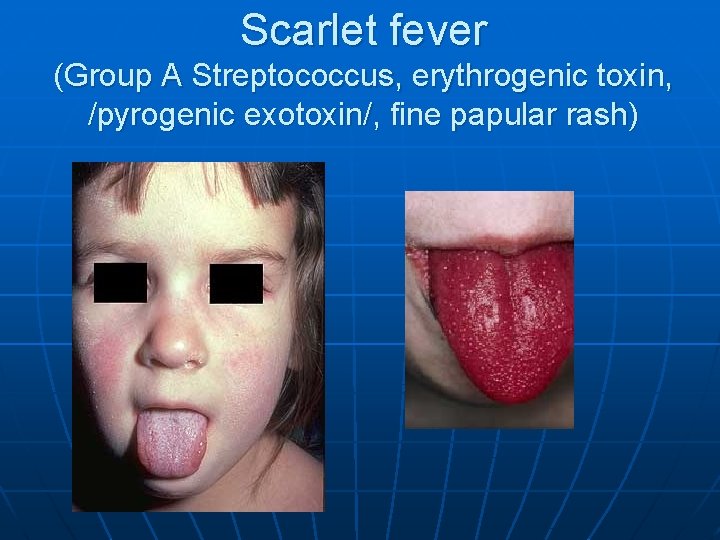
Scarlet fever (Group A Streptococcus, erythrogenic toxin, /pyrogenic exotoxin/, fine papular rash)
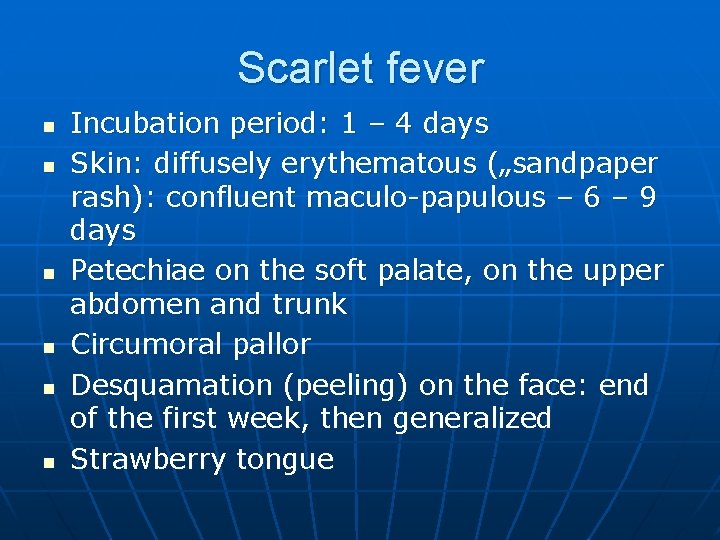
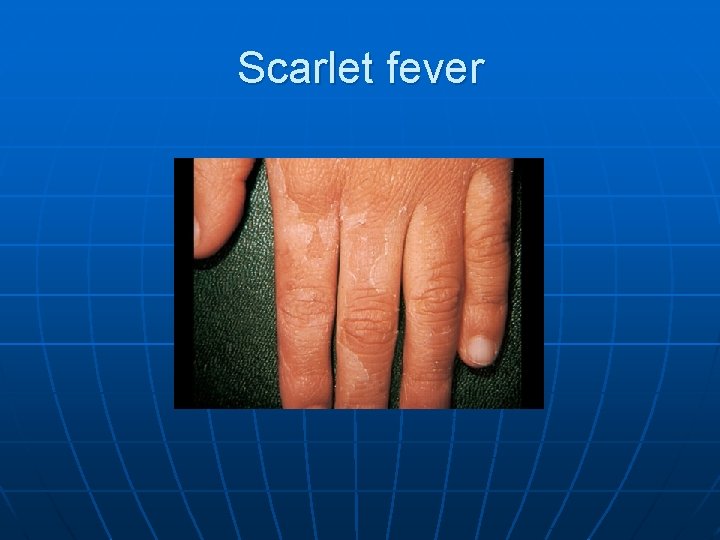
Scarlet fever n n n Incubation period: 1 – 4 days Skin: diffusely erythematous („sandpaper rash): confluent maculo-papulous – 6 – 9 days Petechiae on the soft palate, on the upper abdomen and trunk Circumoral pallor Desquamation (peeling) on the face: end of the first week, then generalized Strawberry tongue

Scarlet fever
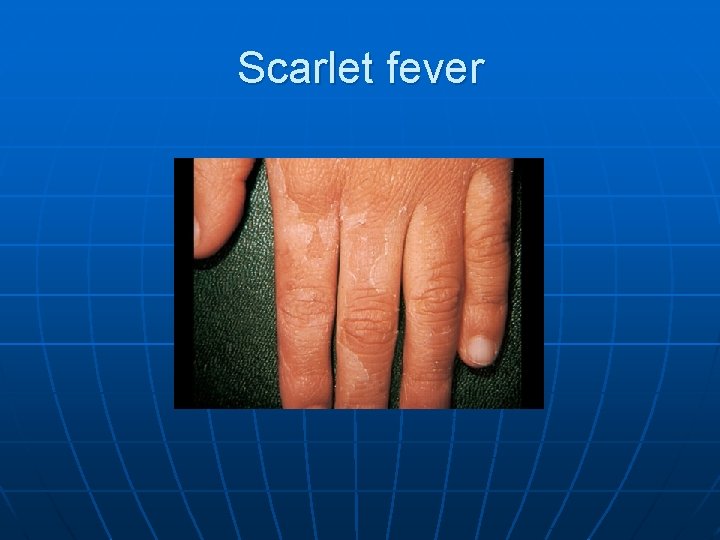
Scarlet fever

Scarlet fever n n Abdominal pain, vomiting Treatment: oral Penicillin, 10 days
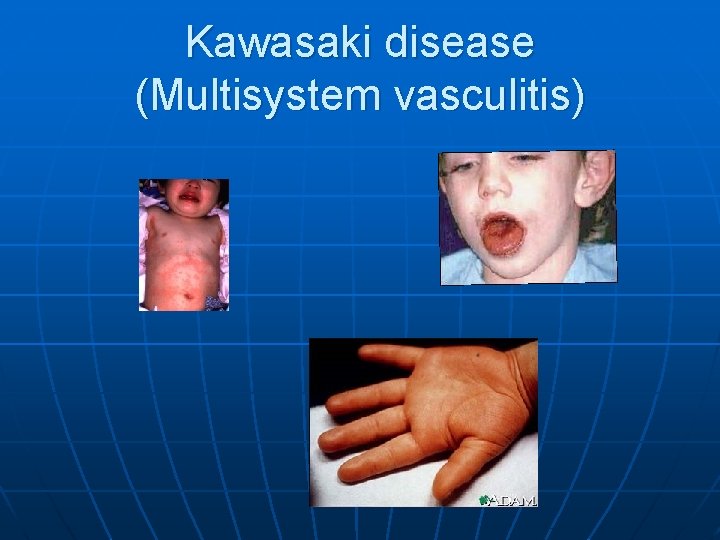
Kawasaki disease (Multisystem vasculitis)
Kawasaki disease n n Coronary aneurism / dilatation < 5 years, incidence: 3 – 6: 100 000 Fever, non – suppurative conjunctivitis, cheilitis, strawberry tongue, polymorphic rash, pharyngitis, lymphadenopathy, peeling on the extremities Treatment: high dose IVIG (2 g/kg bw. ) + aspirin (80 -100 mg/kg bw. )
Erysipelas n n n Superficial and deep inflammation of the skin, demarkated rash Invasive infection Streptococcus pyogenes, Staphylococcus aureus Complication/ infants: sepsis Treatment: penicillin, clindamycin

Erysipelas (Group A Streptococcus, acute cellulitis and lymphangitis)

Impetigo n n Papule, vesiculation, then it breaks Denuded area, covered by a honeycolored crust

Impetigo n n n 2 – 5 years Streptococcus pyogenes Staphylococcus aureus Local treatment Systemic: antibiotic therapy
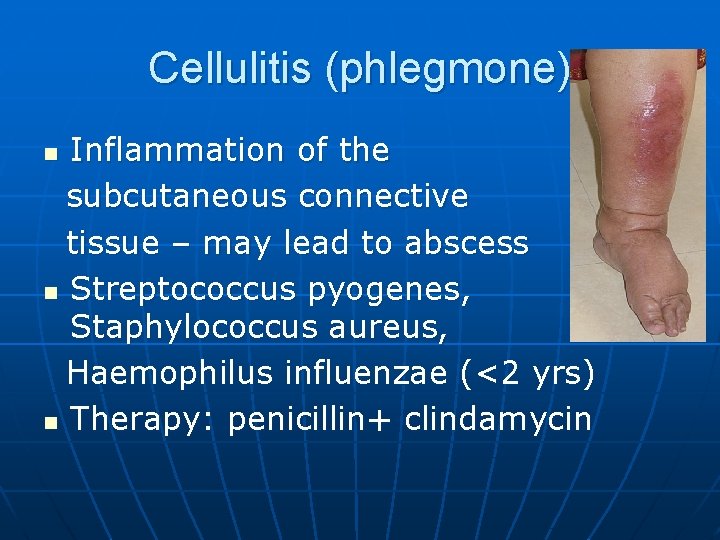
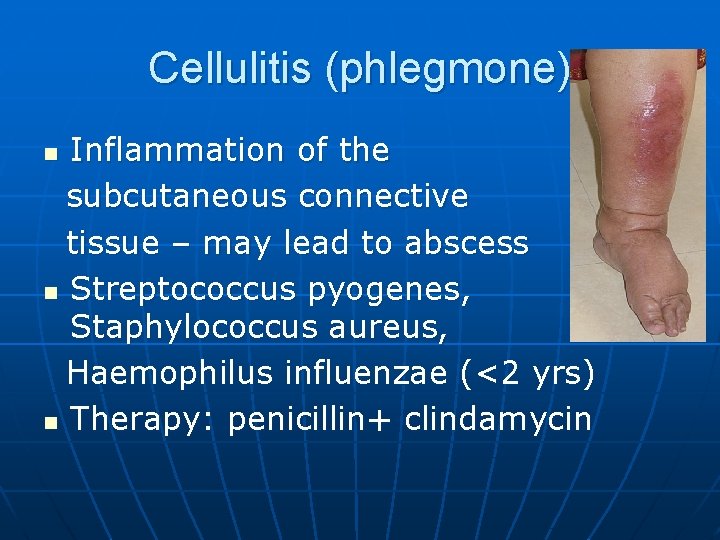
Cellulitis (phlegmone) Inflammation of the subcutaneous connective tissue – may lead to abscess n Streptococcus pyogenes, Staphylococcus aureus, Haemophilus influenzae (<2 yrs) n Therapy: penicillin+ clindamycin n
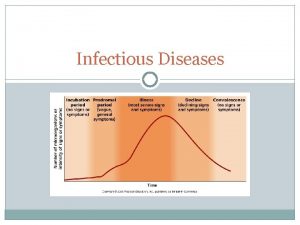
Infectious diseases with rash Stadium incubationis: in generalno symptom n Stadium prodromum: non-specific symptoms n Stadium floritionis n
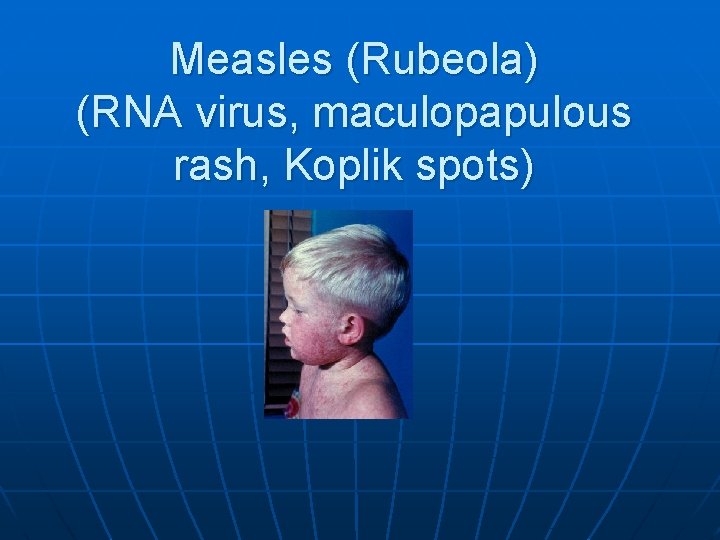
Measles (Rubeola) n n Paramyxovirus, RNA virus 10 -14 days incubation Rash: retroauricular, temporal region, then on the face - maculopapulous exanthemes Complications: encephalitis, cerebellitis, subacute sclerotizing panencephalitis
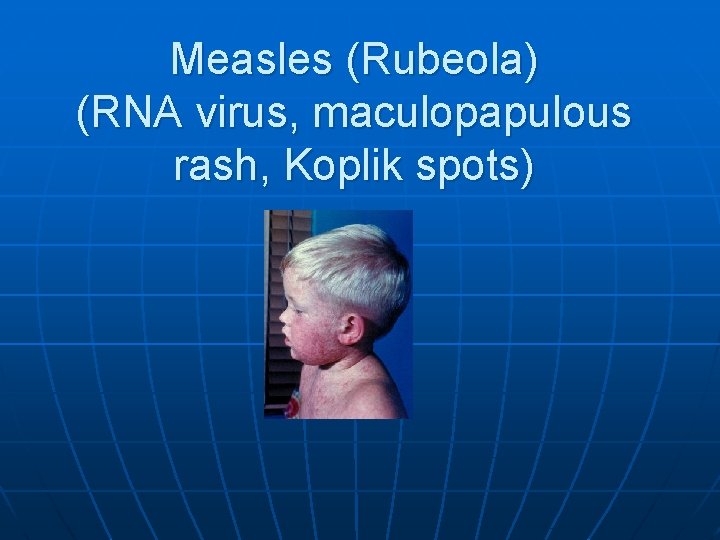
Measles (Rubeola) (RNA virus, maculopapulous rash, Koplik spots)

Measles (Rubeola)
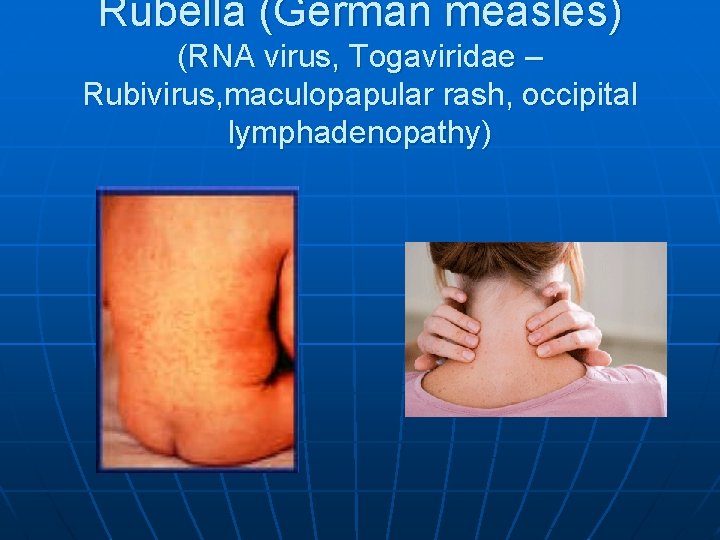
Rubella (German measles) n n Togavirus, RNA Painful lymphadenopathy: retroauricular, cervical, occipital region: Theodor- Klatsch symptom Peeling Congenital rubella syndrome
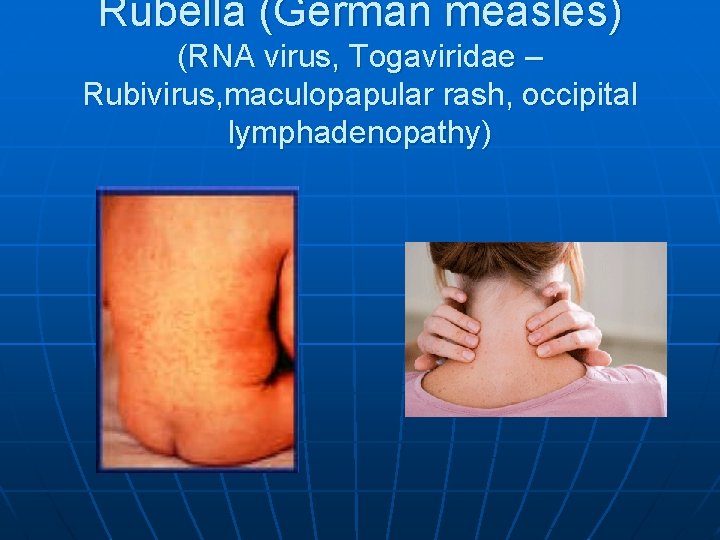
Rubella (German measles) (RNA virus, Togaviridae – Rubivirus, maculopapular rash, occipital lymphadenopathy)
Congenital rubella syndrome n n Infection of seronegative mother during pregnancy Risk of fetal infection • • I. trimenon: 75 -90% II. trimenon: 20 -40% III. trimenon: 25 -50% Fetal lesion n 1 -8. gest. week: 80% 9 -12. gest. week: 30% 13 -20. gest. week: 10%
Congenital rubella syndrome n Gestation • 14 - 60. days: embryopathy – cataracta, microphthalmia, hearing loss, congenital heart disease, microcephalus, thymus hypoplasia Rubella vaccination is prohibited during pregnancy!

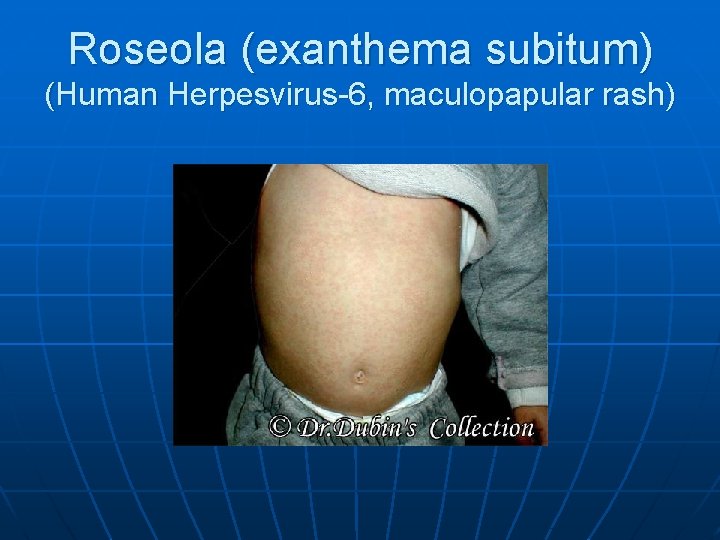
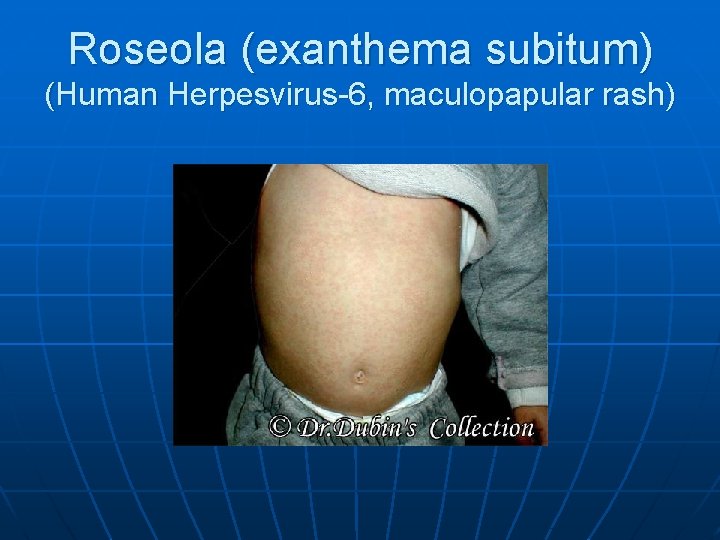
Roseola (exanthema subitum) (Human Herpesvirus-6, maculopapular rash)
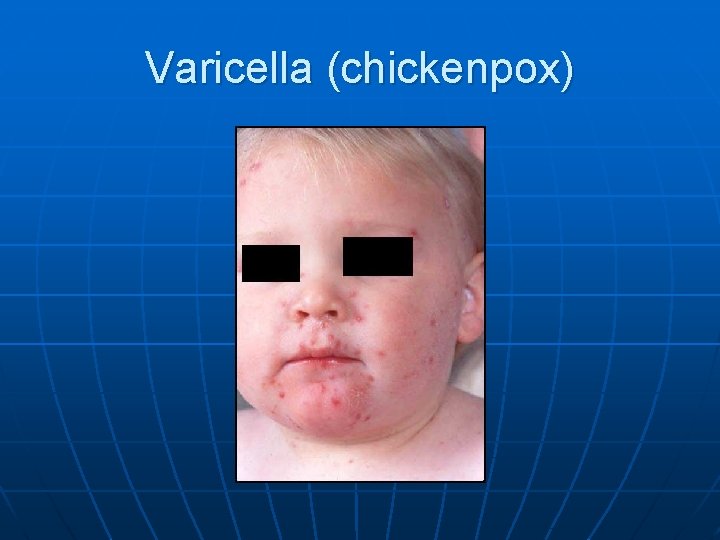
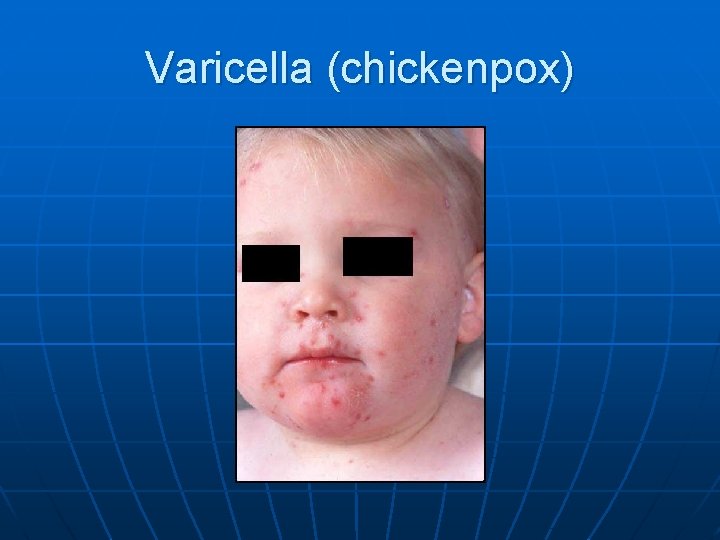
Varicella (chickenpox)
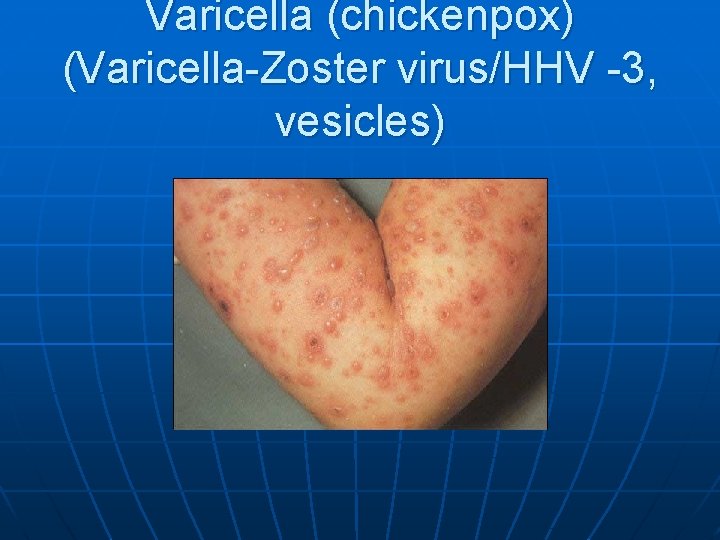
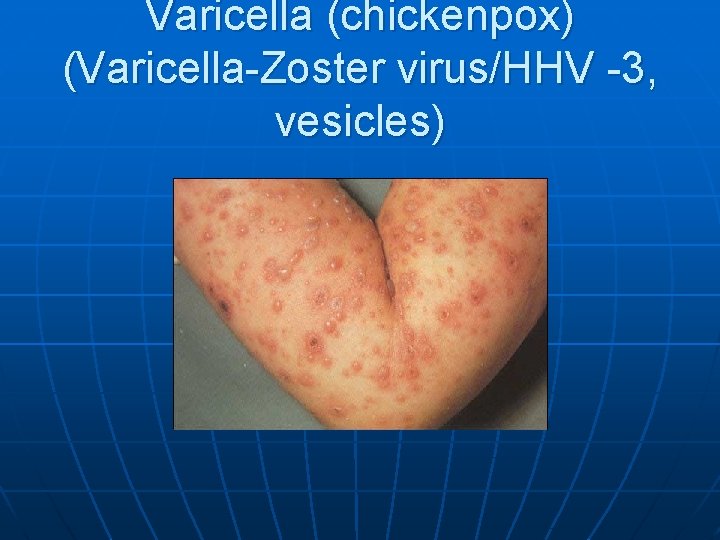
Varicella (chickenpox) (Varicella-Zoster virus/HHV -3, vesicles)
Varicella (chickenpox) n n n Incubation period: 10 – 21 days (1415 days) Complications: secondary bacterial infection – streptococcal toxic shock syndrome Pneumonitis
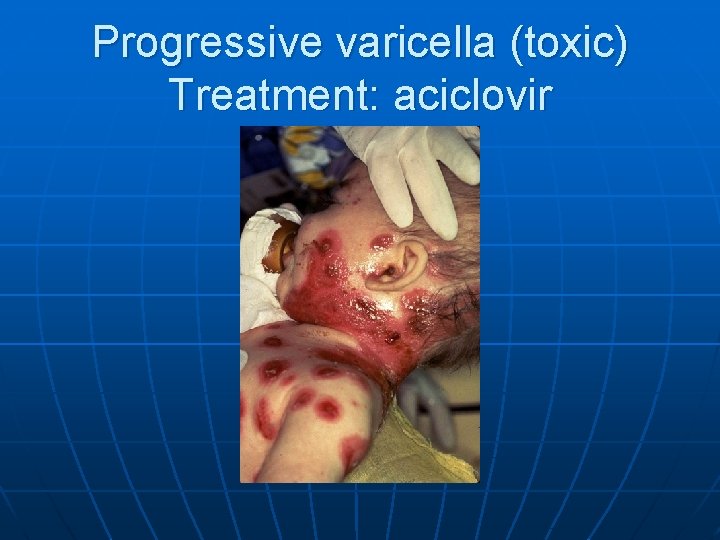
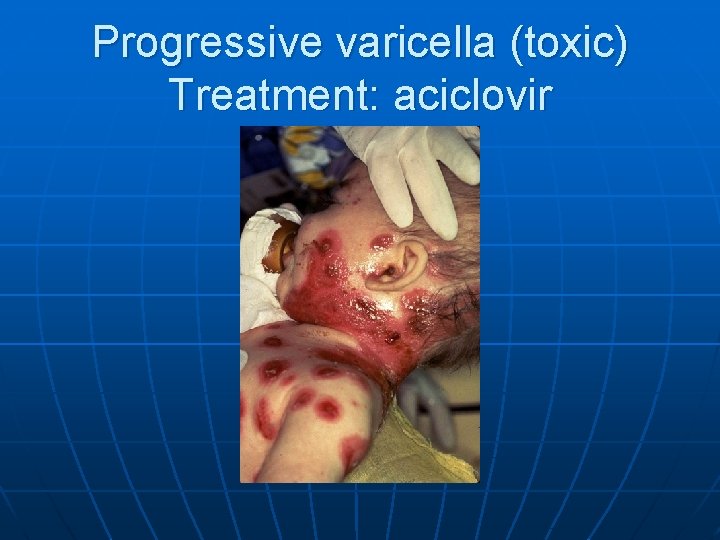
Progressive varicella (toxic) Treatment: aciclovir
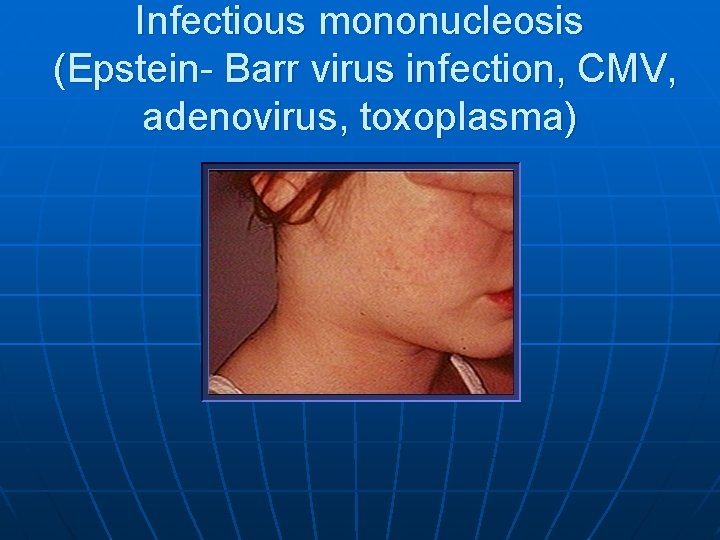
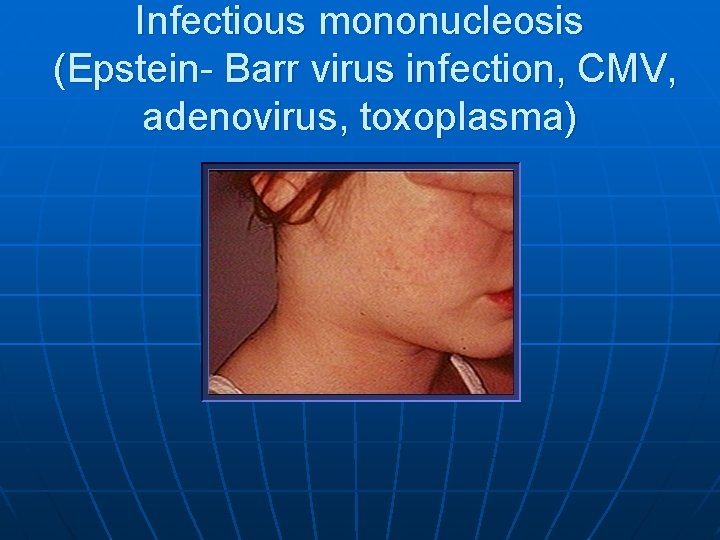
Infectious mononucleosis (Epstein- Barr virus infection, CMV, adenovirus, toxoplasma)
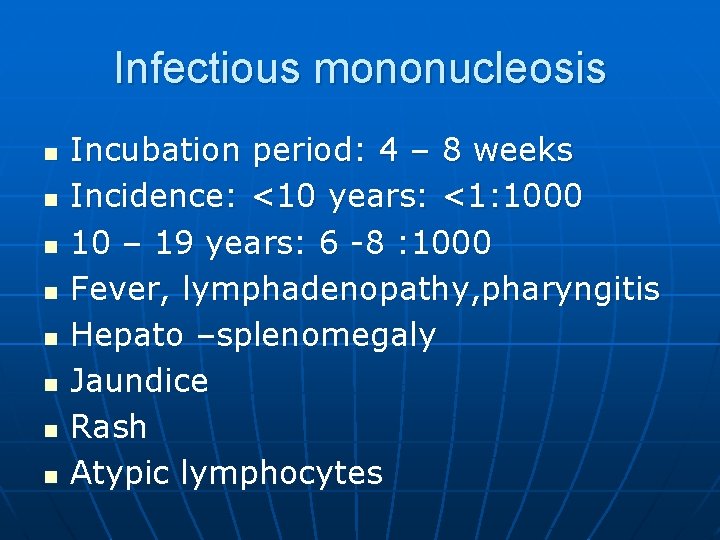
Infectious mononucleosis n n n n Incubation period: 4 – 8 weeks Incidence: <10 years: <1: 1000 10 – 19 years: 6 -8 : 1000 Fever, lymphadenopathy, pharyngitis Hepato –splenomegaly Jaundice Rash Atypic lymphocytes
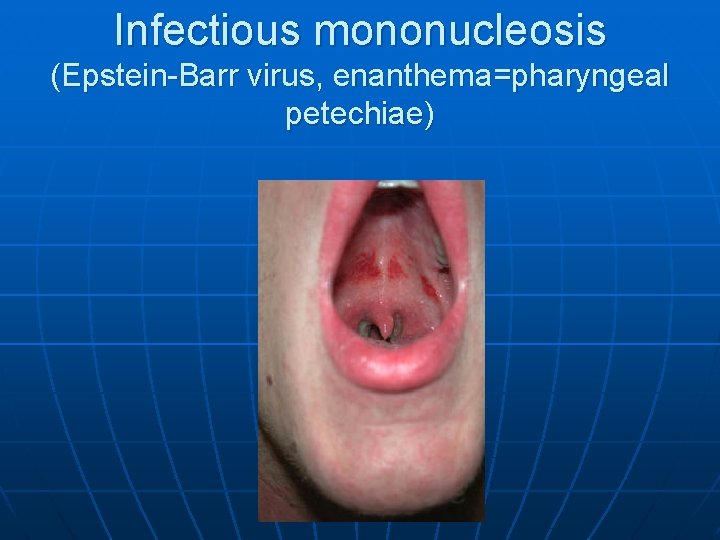
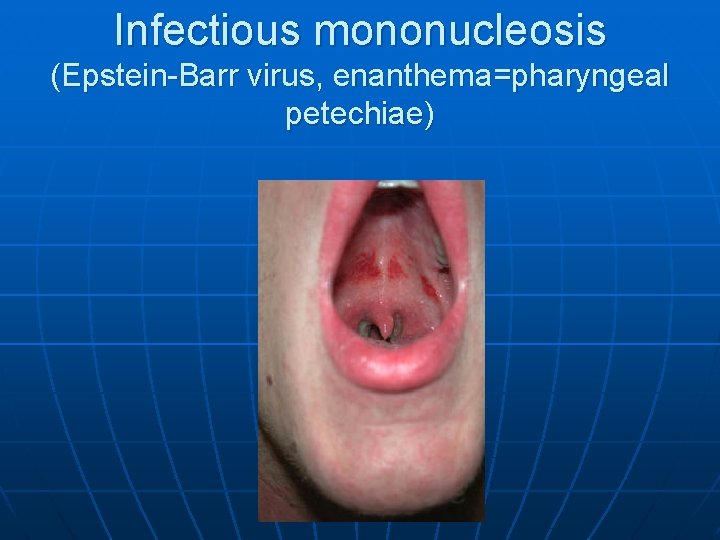
Infectious mononucleosis (Epstein-Barr virus, enanthema=pharyngeal petechiae)
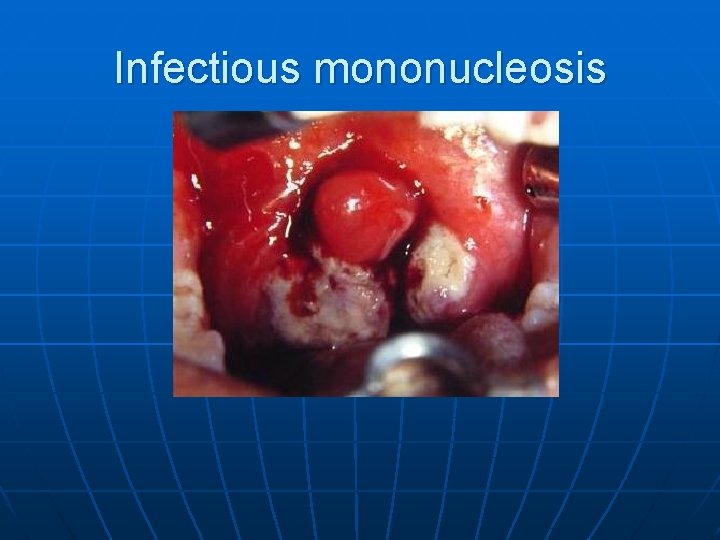
Infectious mononucleosis
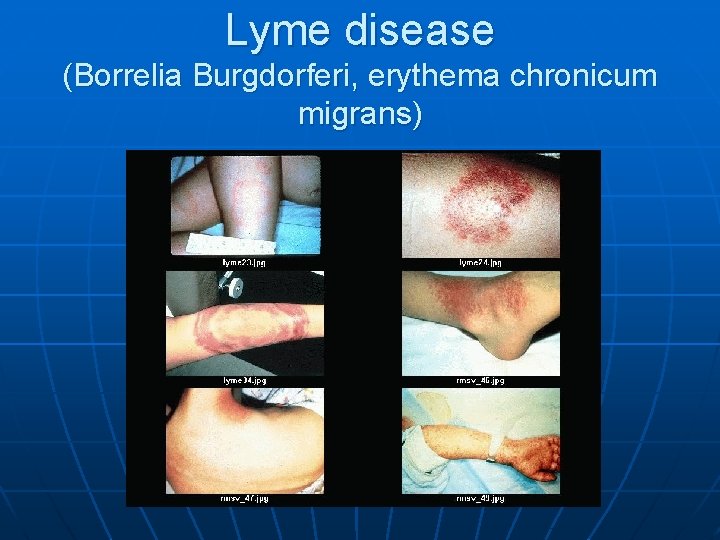
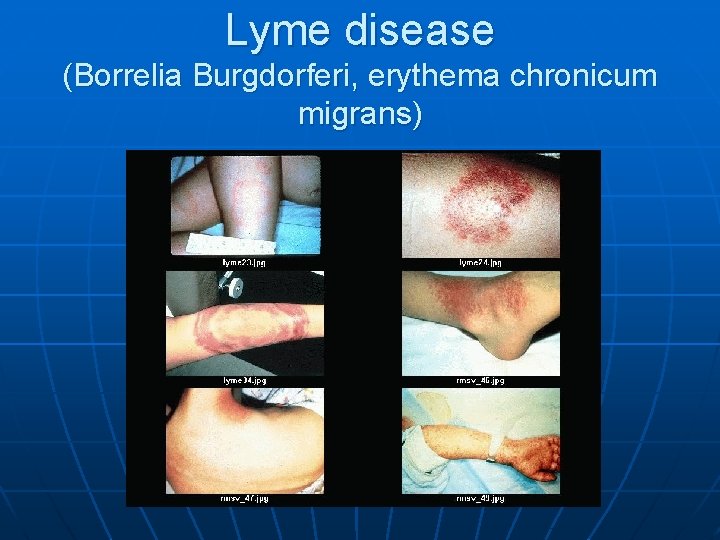
Lyme disease (Borrelia Burgdorferi, erythema chronicum migrans)
Lyme borreliosis n n Skin, joints, CNS, heart Erythema migrans – regional lymphadenopathy Treatment: oral doxycyclin, amoxicillin, cefuroxim-axetil 10 days Ceftriaxon iv.
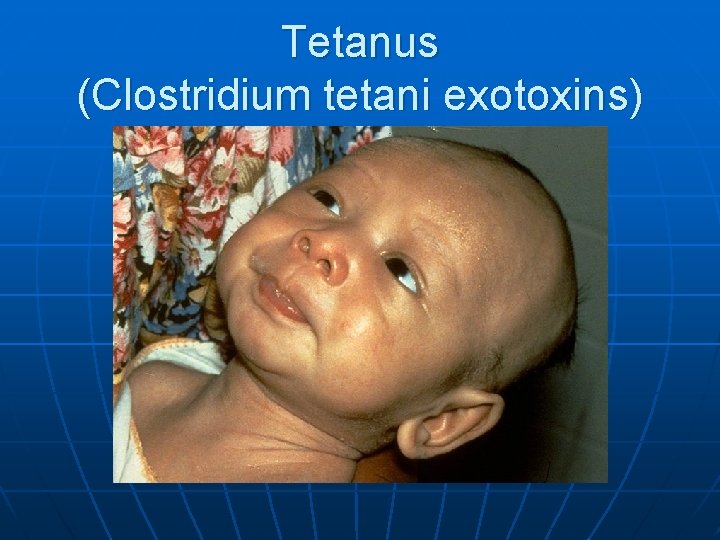
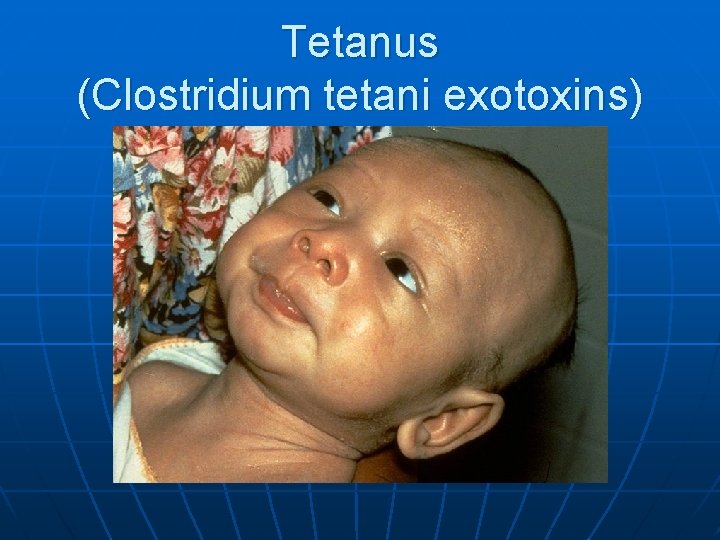
Tetanus (Clostridium tetani exotoxins)
AIDS n n n Occurrence is rare in children 80% intrauterine, intra partum, breast feeding, 10 - 15% blood and blood products, 5% unknown origin Risk of children of HIV infected mother: 20 -40%
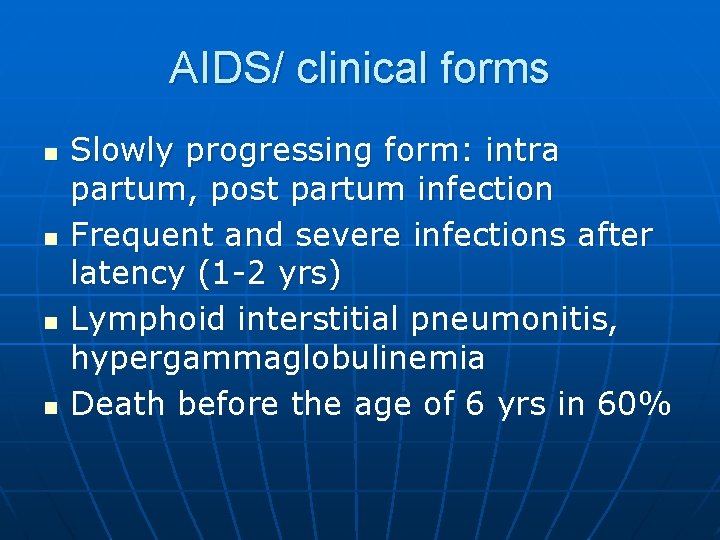
AIDS/ clinical forms n n Slowly progressing form: intra partum, post partum infection Frequent and severe infections after latency (1 -2 yrs) Lymphoid interstitial pneumonitis, hypergammaglobulinemia Death before the age of 6 yrs in 60%
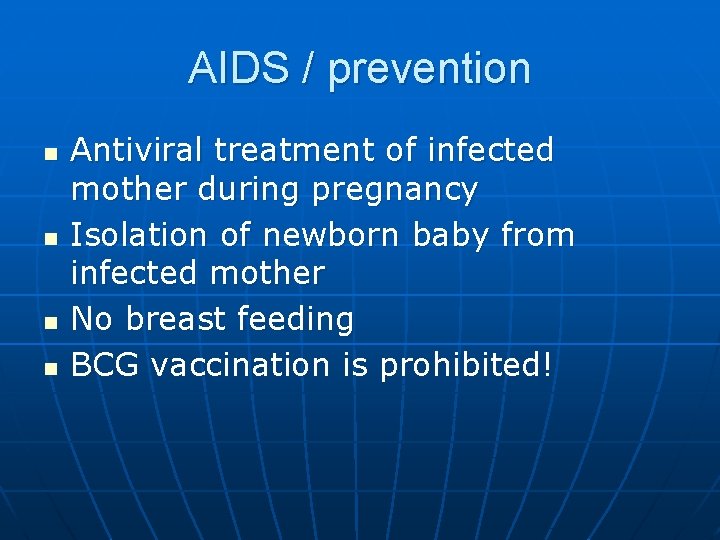
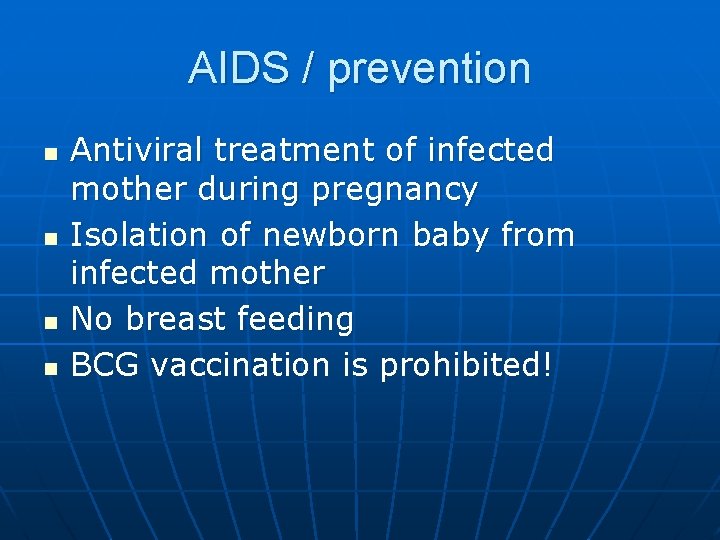
AIDS / prevention n n Antiviral treatment of infected mother during pregnancy Isolation of newborn baby from infected mother No breast feeding BCG vaccination is prohibited!
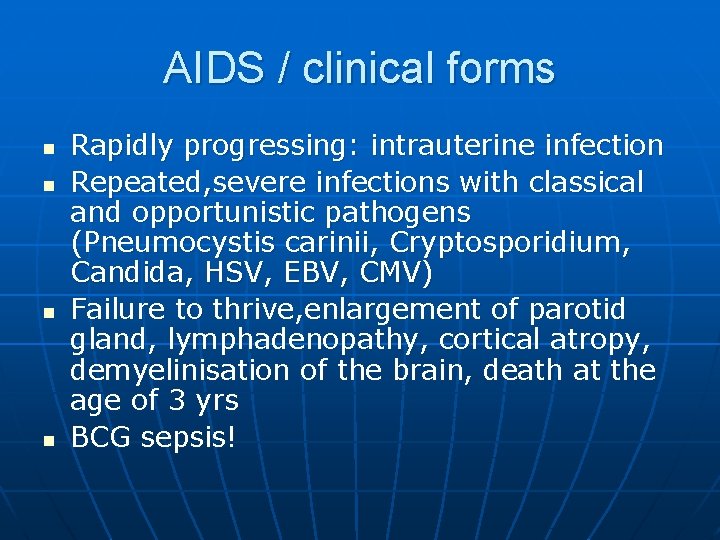
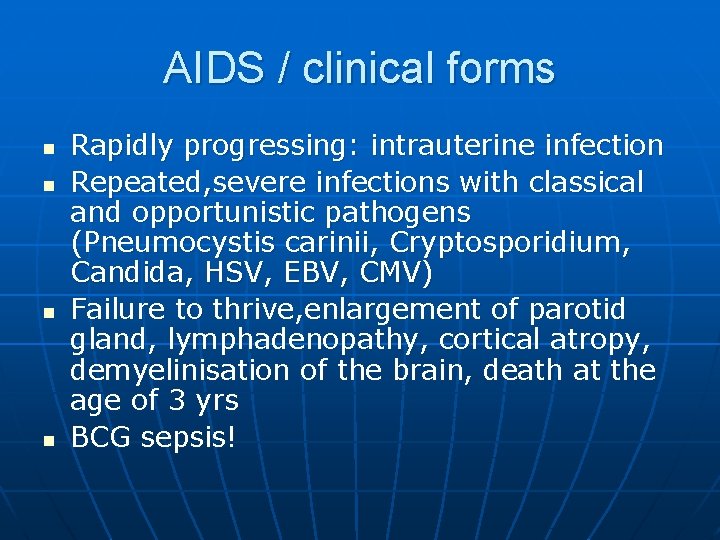
AIDS / clinical forms n n Rapidly progressing: intrauterine infection Repeated, severe infections with classical and opportunistic pathogens (Pneumocystis carinii, Cryptosporidium, Candida, HSV, EBV, CMV) Failure to thrive, enlargement of parotid gland, lymphadenopathy, cortical atropy, demyelinisation of the brain, death at the age of 3 yrs BCG sepsis!
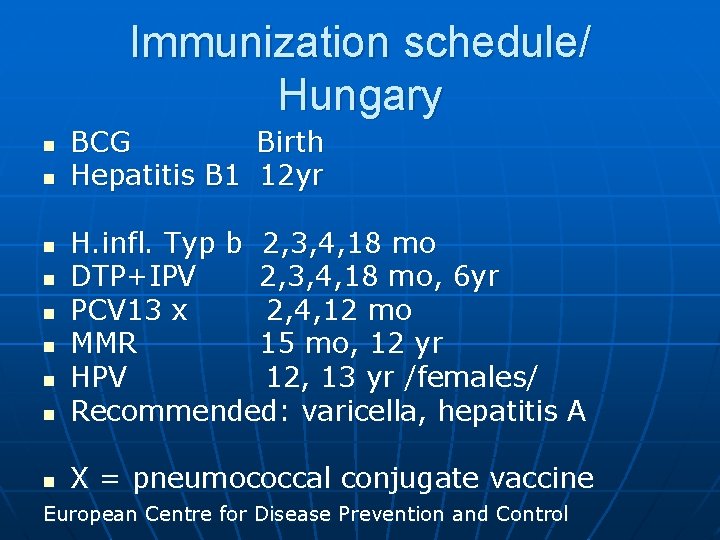
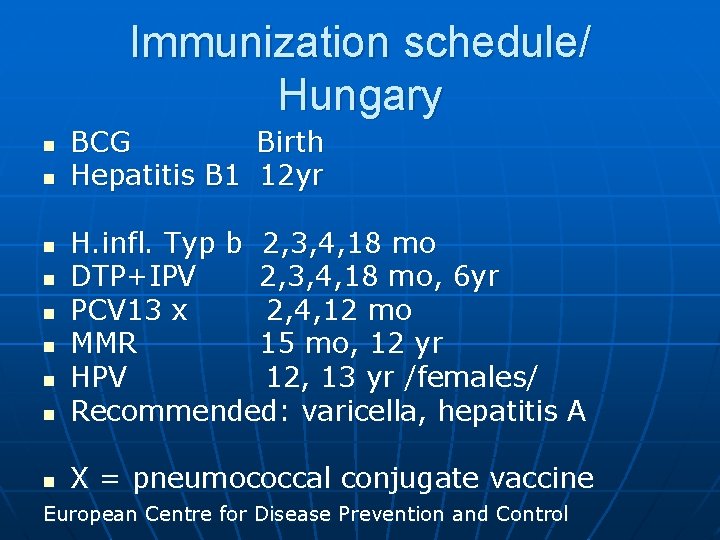
Immunization schedule/ Hungary n n BCG Birth Hepatitis B 1 12 yr n H. infl. Typ b 2, 3, 4, 18 mo DTP+IPV 2, 3, 4, 18 mo, 6 yr PCV 13 x 2, 4, 12 mo MMR 15 mo, 12 yr HPV 12, 13 yr /females/ Recommended: varicella, hepatitis A n X = pneumococcal conjugate vaccine n n n European Centre for Disease Prevention and Control
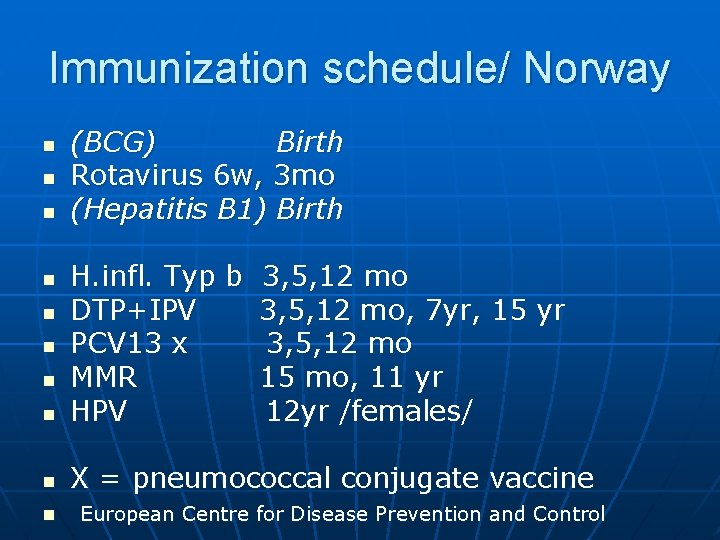
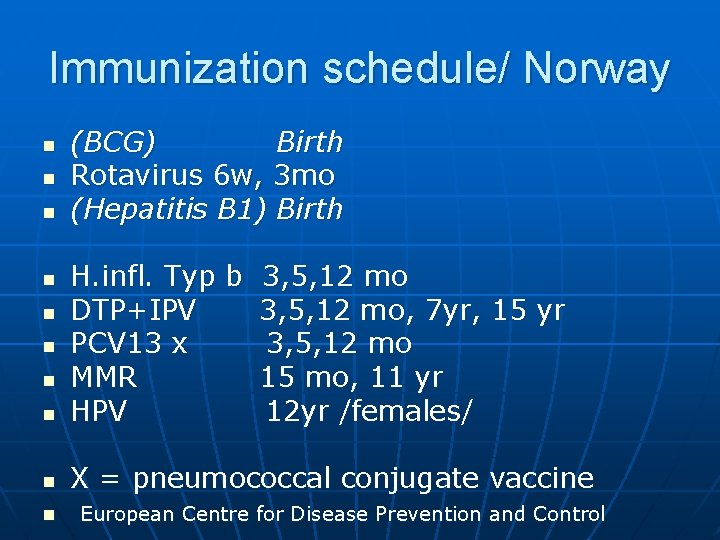
Immunization schedule/ Norway n n n (BCG) Birth Rotavirus 6 w, 3 mo (Hepatitis B 1) Birth n H. infl. Typ b 3, 5, 12 mo DTP+IPV 3, 5, 12 mo, 7 yr, 15 yr PCV 13 x 3, 5, 12 mo MMR 15 mo, 11 yr HPV 12 yr /females/ n X = pneumococcal conjugate vaccine n n n European Centre for Disease Prevention and Control
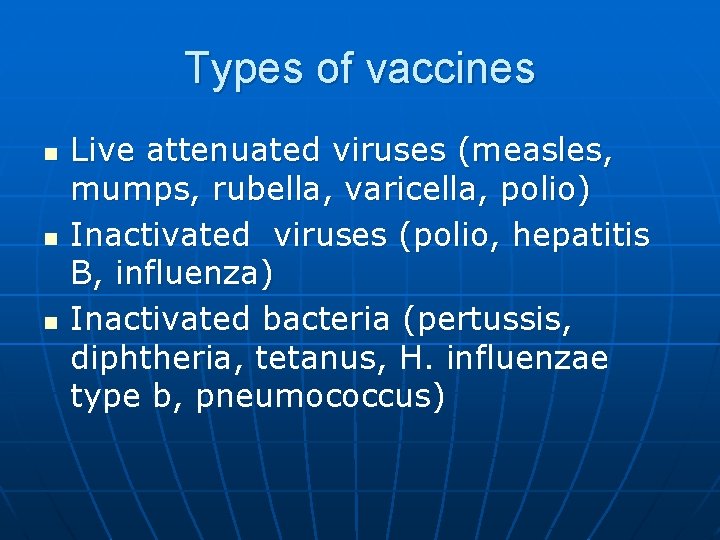
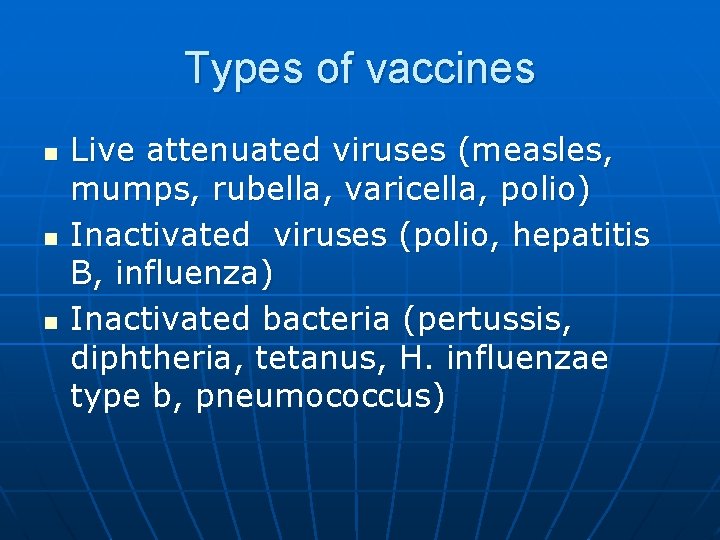
Types of vaccines n n n Live attenuated viruses (measles, mumps, rubella, varicella, polio) Inactivated viruses (polio, hepatitis B, influenza) Inactivated bacteria (pertussis, diphtheria, tetanus, H. influenzae type b, pneumococcus)
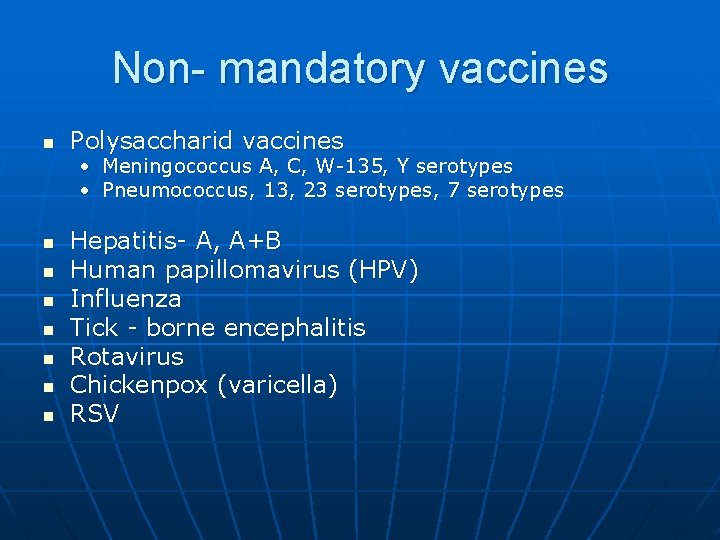
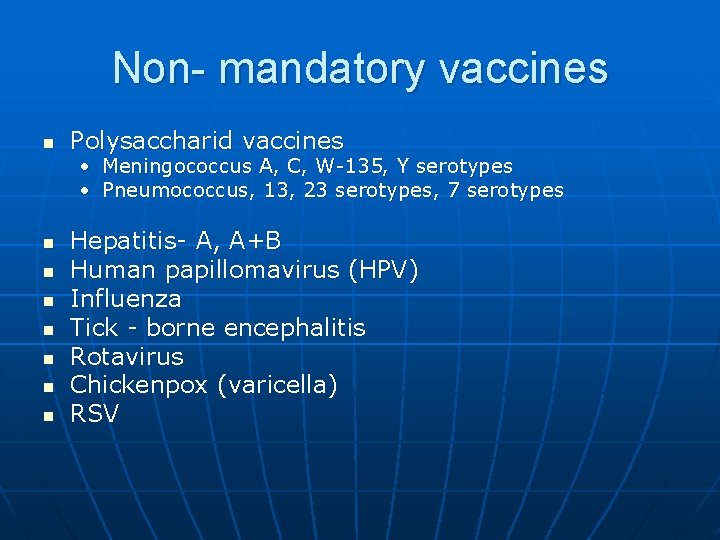
Non- mandatory vaccines n Polysaccharid vaccines • Meningococcus A, C, W-135, Y serotypes • Pneumococcus, 13, 23 serotypes, 7 serotypes n n n n Hepatitis- A, A+B Human papillomavirus (HPV) Influenza Tick - borne encephalitis Rotavirus Chickenpox (varicella) RSV
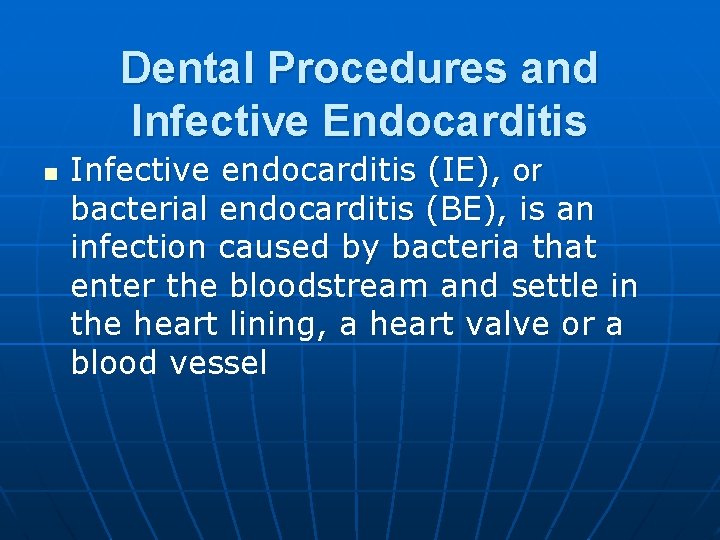
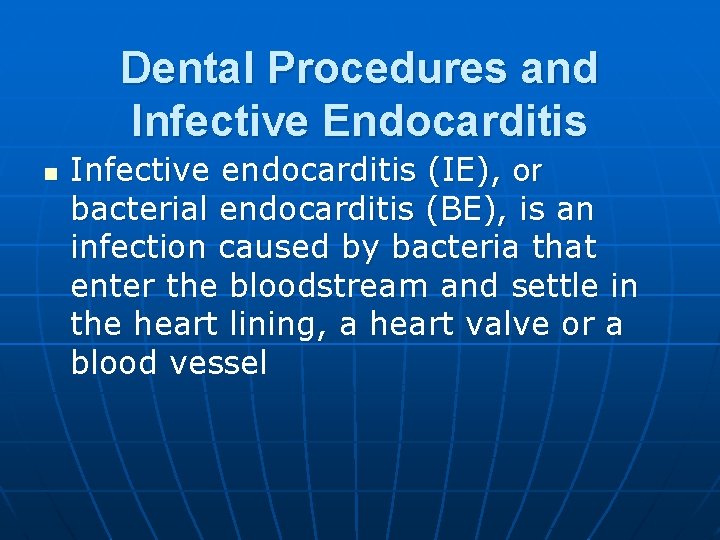
Dental Procedures and Infective Endocarditis n Infective endocarditis (IE), or bacterial endocarditis (BE), is an infection caused by bacteria that enter the bloodstream and settle in the heart lining, a heart valve or a blood vessel
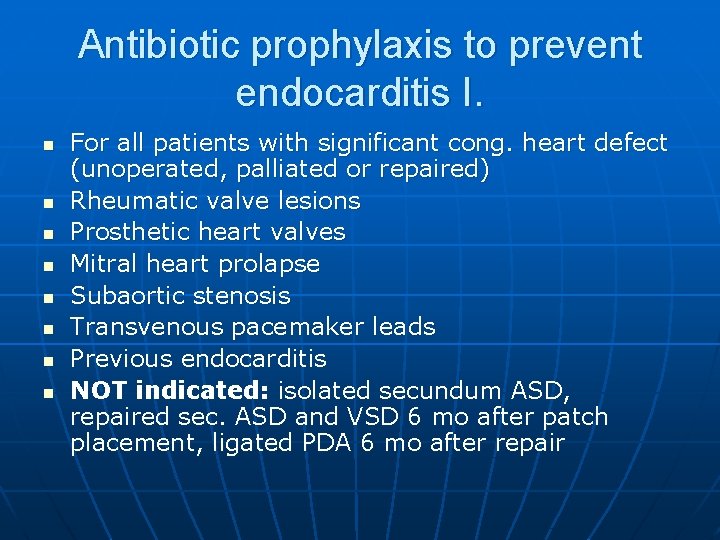
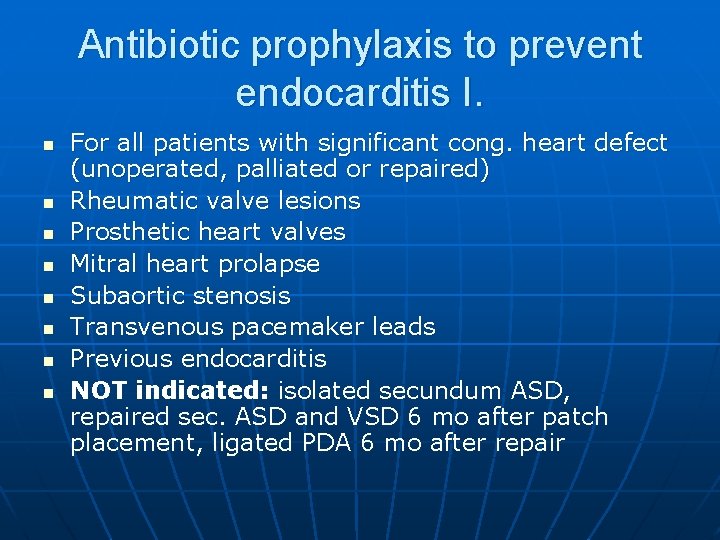
Antibiotic prophylaxis to prevent endocarditis I. n n n n For all patients with significant cong. heart defect (unoperated, palliated or repaired) Rheumatic valve lesions Prosthetic heart valves Mitral heart prolapse Subaortic stenosis Transvenous pacemaker leads Previous endocarditis NOT indicated: isolated secundum ASD, repaired sec. ASD and VSD 6 mo after patch placement, ligated PDA 6 mo after repair
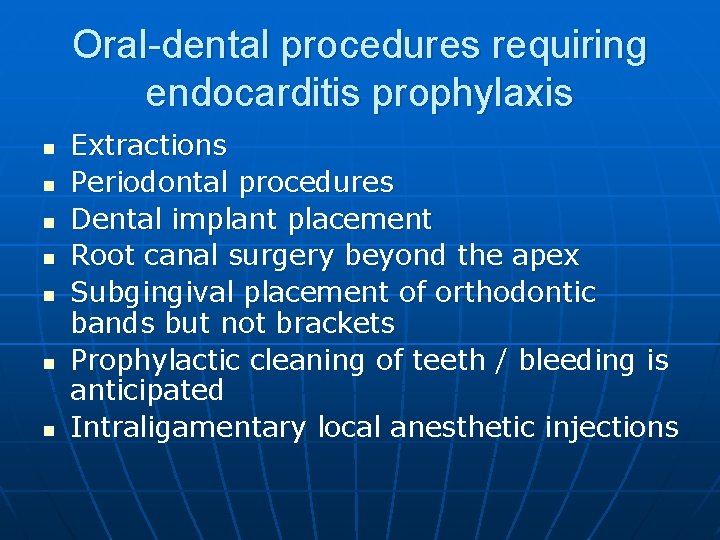
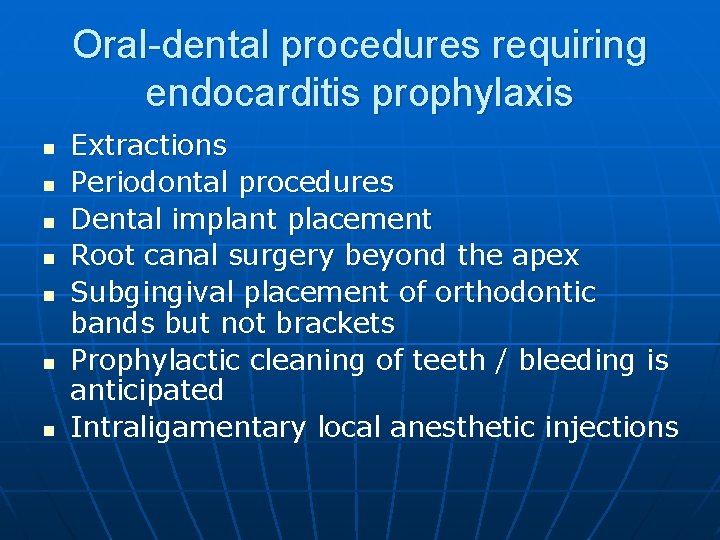
Oral-dental procedures requiring endocarditis prophylaxis n n n n Extractions Periodontal procedures Dental implant placement Root canal surgery beyond the apex Subgingival placement of orthodontic bands but not brackets Prophylactic cleaning of teeth / bleeding is anticipated Intraligamentary local anesthetic injections
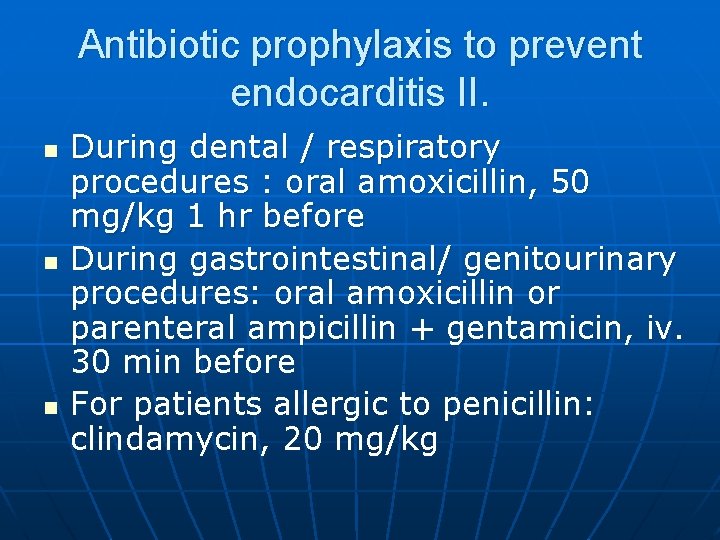
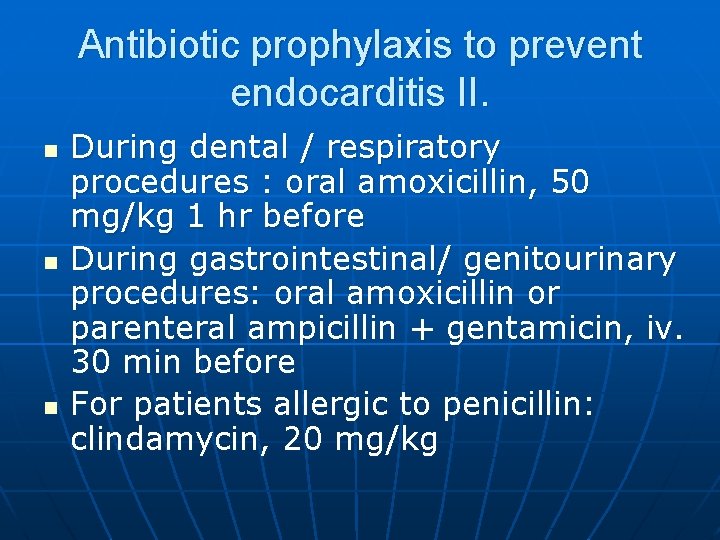
Antibiotic prophylaxis to prevent endocarditis II. n n n During dental / respiratory procedures : oral amoxicillin, 50 mg/kg 1 hr before During gastrointestinal/ genitourinary procedures: oral amoxicillin or parenteral ampicillin + gentamicin, iv. 30 min before For patients allergic to penicillin: clindamycin, 20 mg/kg
 Certain infectious and parasitic diseases
Certain infectious and parasitic diseases Epidemiological triad
Epidemiological triad Caput succedaneum vs kephalhämatom
Caput succedaneum vs kephalhämatom Caput succedaneum vs kephalhämatom
Caput succedaneum vs kephalhämatom Pediatric clinical nurse specialist programs
Pediatric clinical nurse specialist programs Cpmcd full form
Cpmcd full form Difference between spermatogenesis and oogenesis
Difference between spermatogenesis and oogenesis Poultry vaccination schedule
Poultry vaccination schedule Sleeping princesses
Sleeping princesses Vaccination bruxelles
Vaccination bruxelles Ipv vaccine
Ipv vaccine Advantages and disadvantages of vaccines ppt
Advantages and disadvantages of vaccines ppt Vaccination schedule in palestine
Vaccination schedule in palestine Niccolo paganini fingers
Niccolo paganini fingers Mandatory vaccination
Mandatory vaccination Conclusion of immunization
Conclusion of immunization Dog spay perry county
Dog spay perry county Bankeryds vårdcentral influensavaccin
Bankeryds vårdcentral influensavaccin Vaccine vial monitors
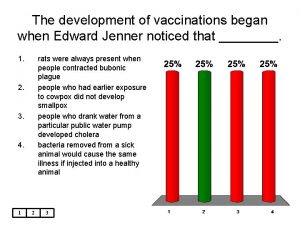
Vaccine vial monitors Edward jenner
Edward jenner 10 rights of medication administration
10 rights of medication administration Hpps logo
Hpps logo Stages of infectious disease
Stages of infectious disease Infectious disease
Infectious disease Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Infectious disease quality controls
Infectious disease quality controls Quizlet
Quizlet Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Infectious mononucleosis
Infectious mononucleosis Types of infection
Types of infection Infectious stunting syndrome
Infectious stunting syndrome Infectious nucleic acid
Infectious nucleic acid Stridor
Stridor Hennepin county infectious disease manual
Hennepin county infectious disease manual Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Lead poisoning
Lead poisoning Smallest infectious agent
Smallest infectious agent Infectious waste management
Infectious waste management X linked diseases
X linked diseases Deficiency chart of macronutrients
Deficiency chart of macronutrients Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Modern lifestyle and hypokinetic diseases
Modern lifestyle and hypokinetic diseases Purulent diseases of lungs and pleura
Purulent diseases of lungs and pleura Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Diseases of the musculoskeletal system
Diseases of the musculoskeletal system Iceberg phenomenon of disease
Iceberg phenomenon of disease What causes genetic diseases
What causes genetic diseases Onychophagy nail disorder
Onychophagy nail disorder An exogenous disease originates outside the body.
An exogenous disease originates outside the body. Nutritional diseases
Nutritional diseases Myth and fallacies about non-communicable diseases
Myth and fallacies about non-communicable diseases Chapter 22 genetics and genetically linked diseases
Chapter 22 genetics and genetically linked diseases Gurus of tqm
Gurus of tqm Albugo eye
Albugo eye