Pedal Access in CLI Peter A Soukas MD





- Slides: 49
Pedal Access in CLI Peter A. Soukas, MD, FACC, FSVM, FSCAI, FACP, RPVI Director, Vascular Medicine & Interventional PV Lab Director, Brown Vascular Medicine Fellowship The Miriam & RI Hospitals, Providence, RI Associate Professor of Medicine Brown Medical School

Peter A. Soukas, MD I have no relevant financial relationships related to this presentation
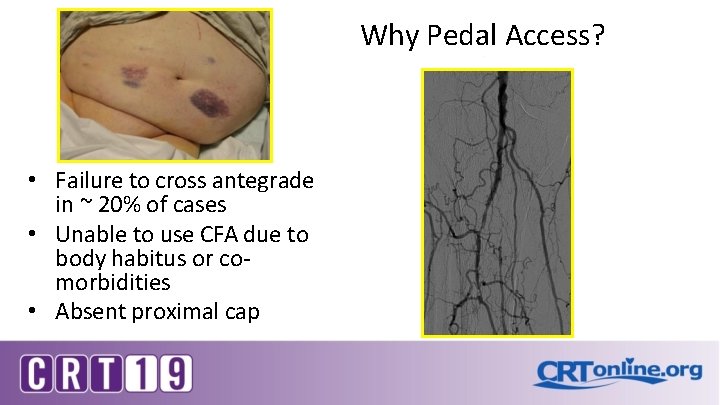
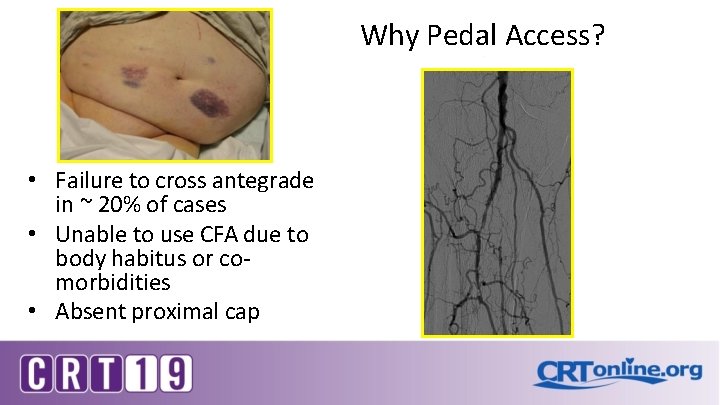
Why Pedal Access? • Failure to cross antegrade in ~ 20% of cases • Unable to use CFA due to body habitus or comorbidities • Absent proximal cap
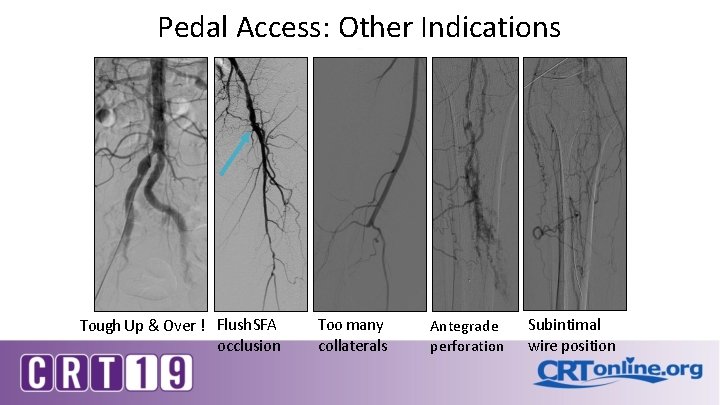
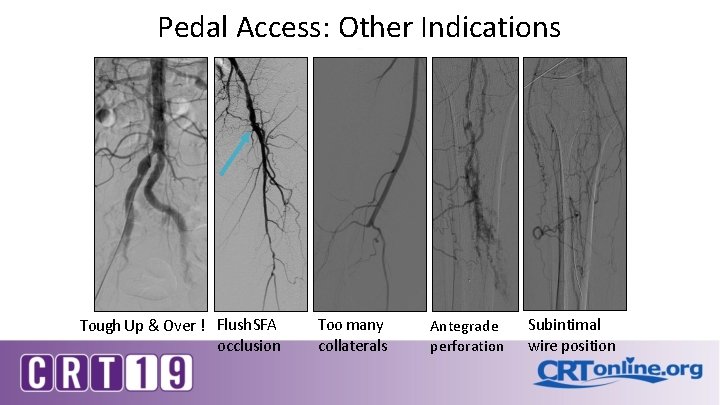
Pedal Access: Other Indications Tough Up & Over ! Flush SFA occlusion Too many collaterals Antegrade perforation Subintimal wire position
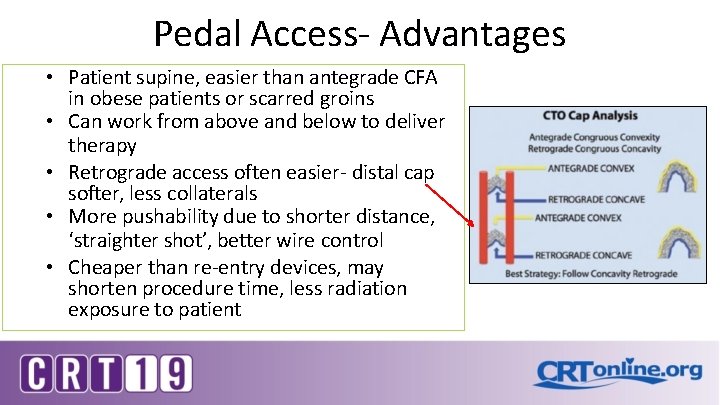
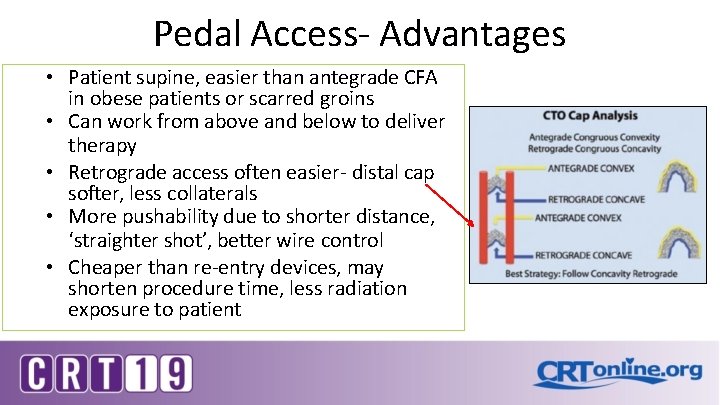
Pedal Access- Advantages • Patient supine, easier than antegrade CFA in obese patients or scarred groins • Can work from above and below to deliver therapy • Retrograde access often easier- distal cap softer, less collaterals • More pushability due to shorter distance, ‘straighter shot’, better wire control • Cheaper than re-entry devices, may shorten procedure time, less radiation exposure to patient
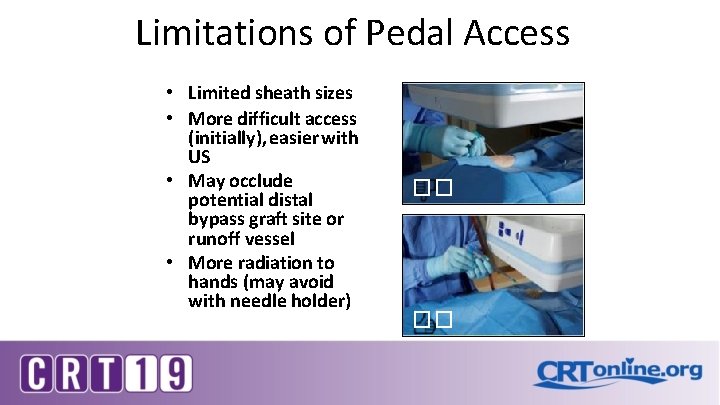
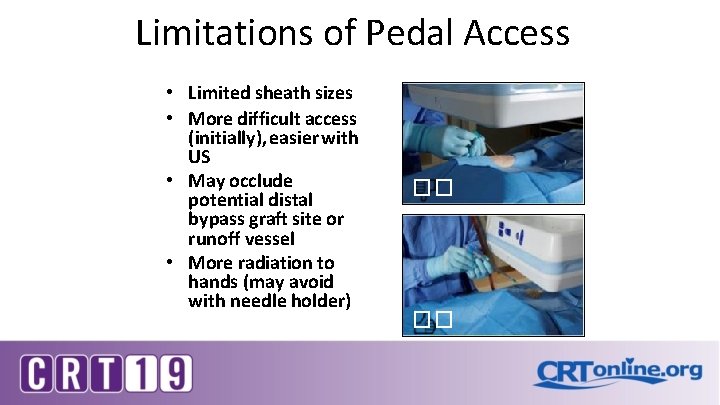
Limitations of Pedal Access • Limited sheath sizes • More difficult access (initially), easier with US • May occlude potential distal bypass graft site or runoff vessel • More radiation to hands (may avoid with needle holder) �� ��
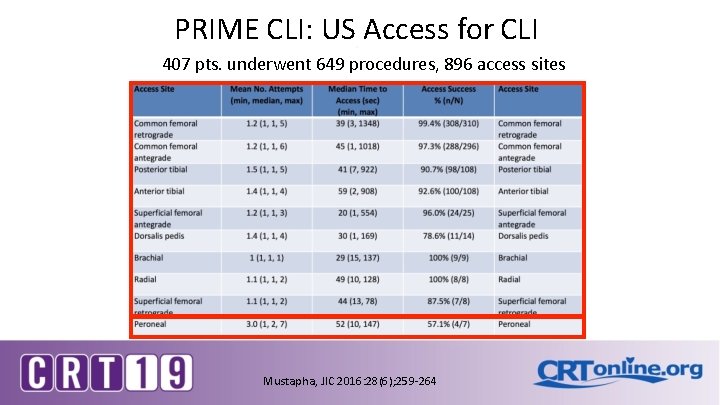
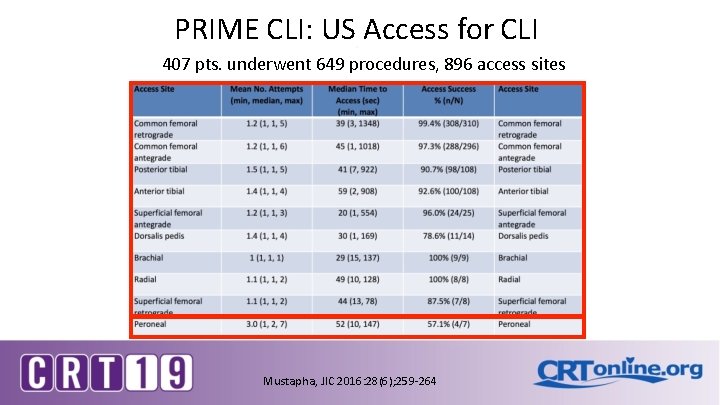
PRIME CLI: US Access for CLI 407 pts. underwent 649 procedures, 896 access sites Mustapha, JIC 2016: 28(6); 259 -264
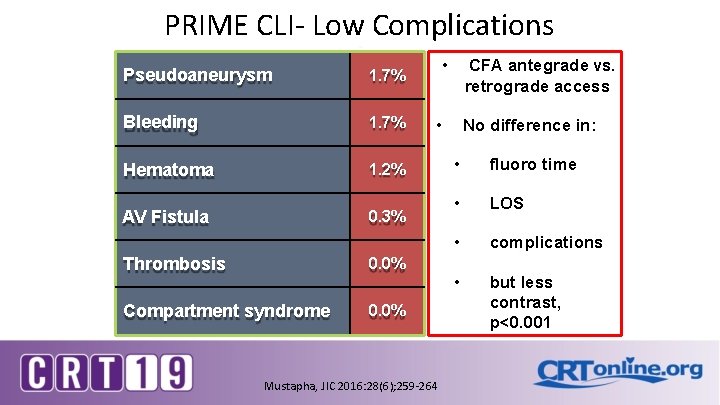
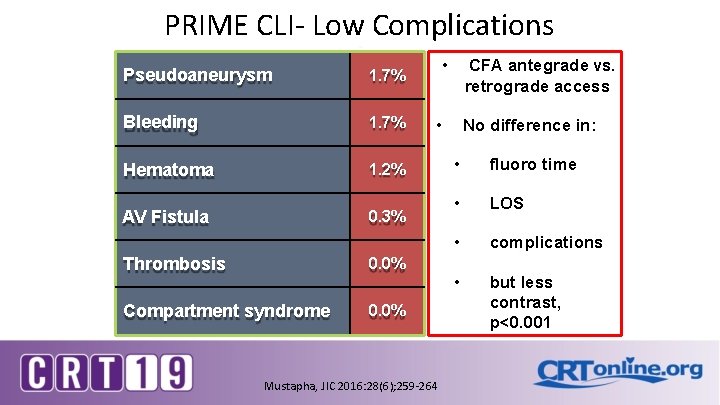
PRIME CLI- Low Complications Pseudoaneurysm 1. 7% Bleeding 1. 7% Hematoma 1. 2% AV Fistula 0. 3% Thrombosis 0. 0% Compartment syndrome 0. 0% • CFA antegrade vs. retrograde access • Mustapha, JIC 2016: 28(6); 259 -264 No difference in: • fluoro time • LOS • complications • but less contrast, p<0. 001
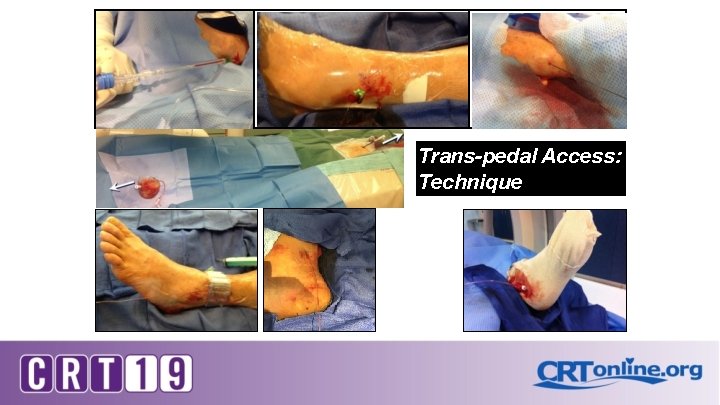
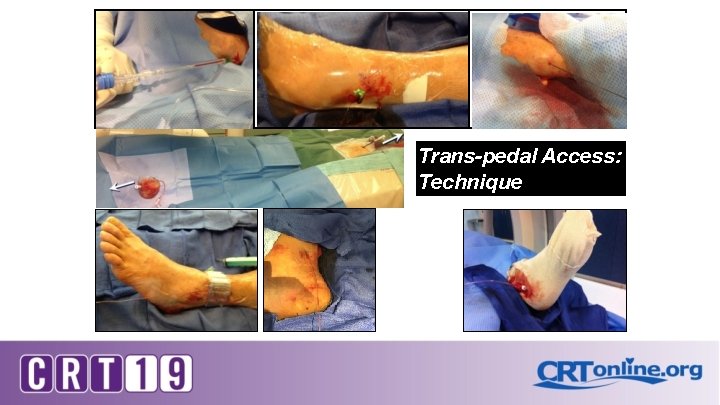
Trans-pedal Access: Technique
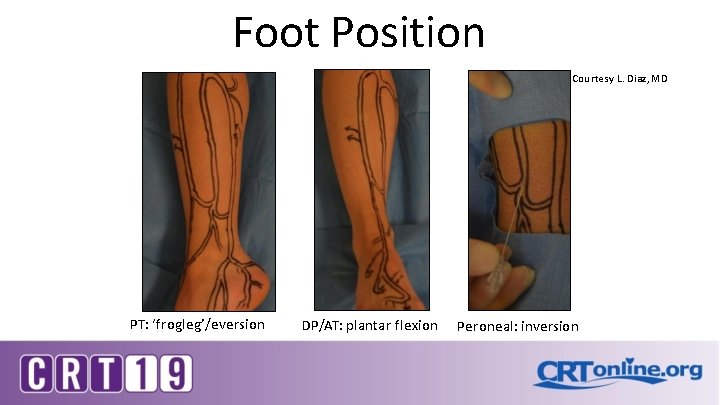
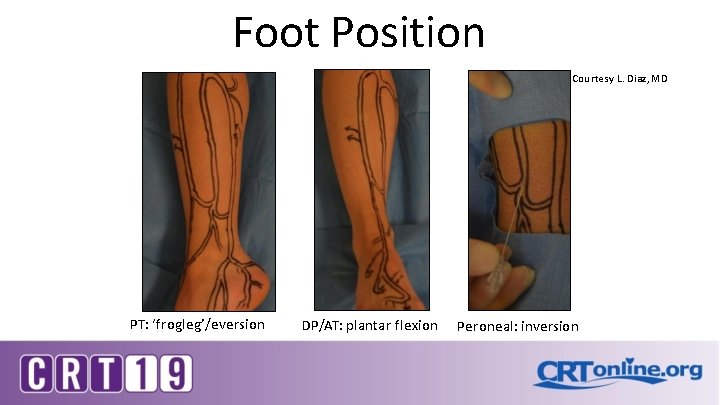
Foot Position Courtesy L. Diaz, MD PT: ‘frogleg’/eversion DP/AT: plantar flexion Peroneal: inversion
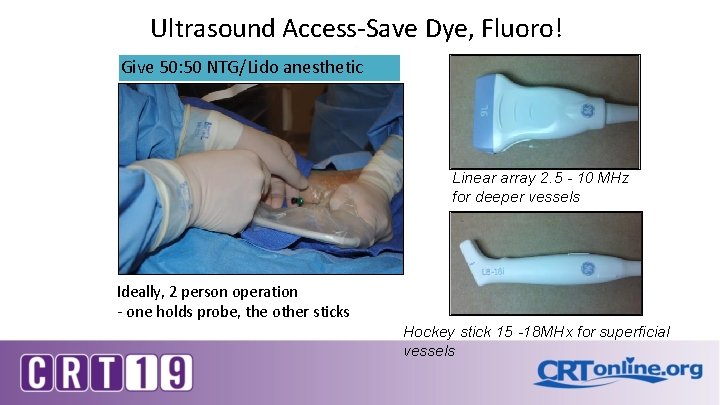
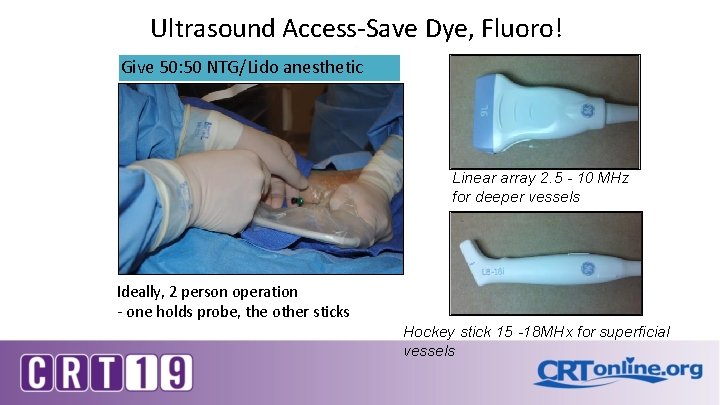
Ultrasound Access-Save Dye, Fluoro! Give 50: 50 NTG/Lido anesthetic Linear array 2. 5 - 10 MHz for deeper vessels Ideally, 2 person operation - one holds probe, the other sticks Hockey stick 15 -18 MHx for superficial vessels
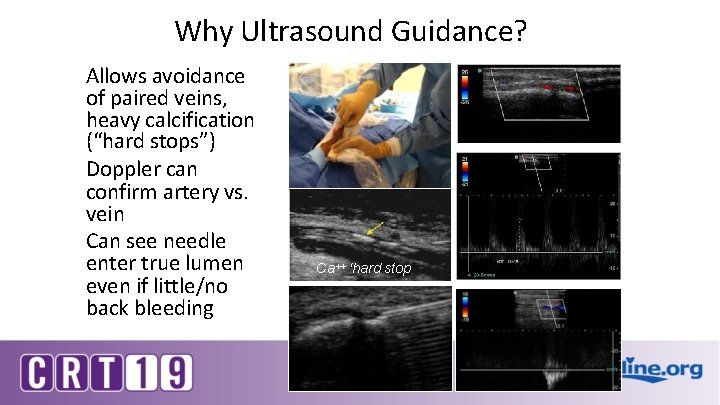
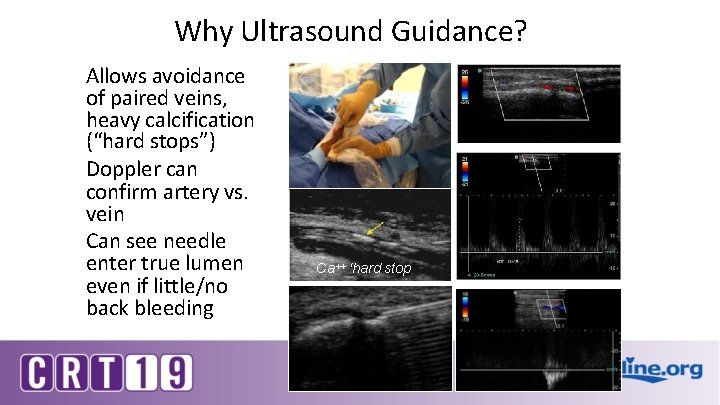
Why Ultrasound Guidance? Allows avoidance of paired veins, heavy calcification (“hard stops”) Doppler can confirm artery vs. vein Can see needle enter true lumen even if little/no back bleeding g color view of arte Ca++ ‘hard stop’ PW artery PW vein needle tering artery
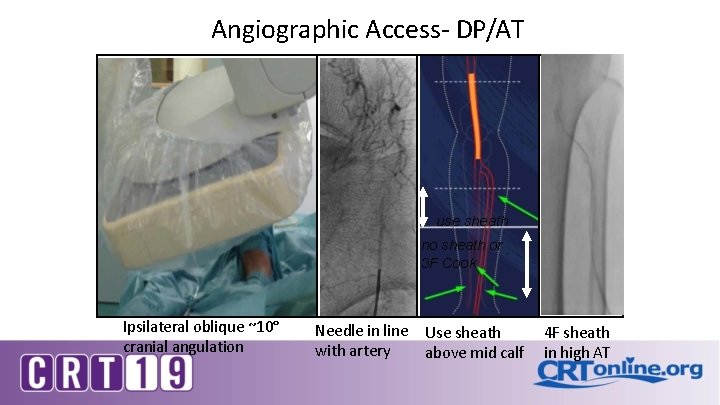
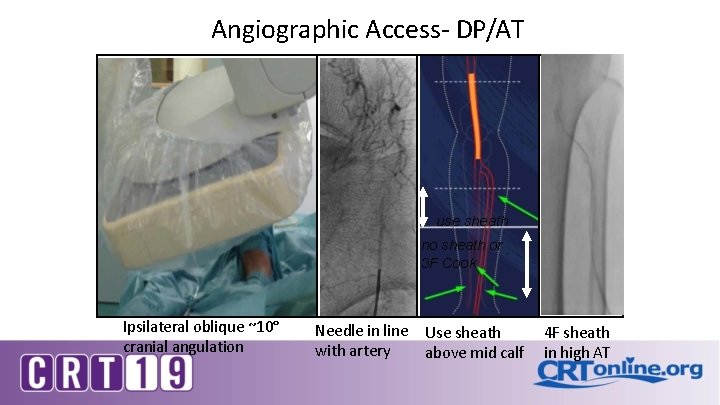
Angiographic Access- DP/AT use sheath no sheath or 3 F Cook Ipsilateral oblique ~10° cranial angulation Needle in line with artery Use sheath above mid calf 4 F sheath in high AT
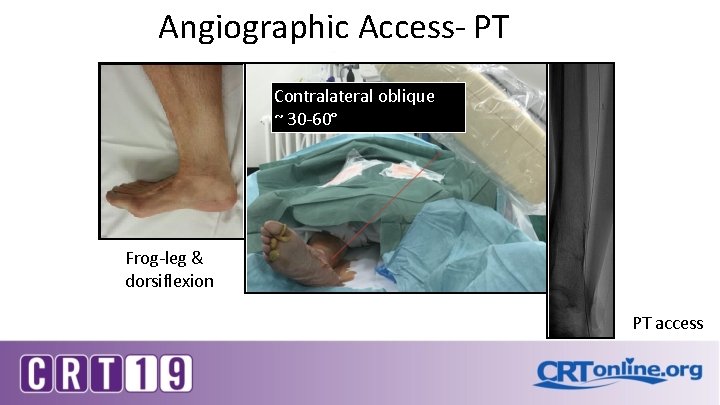
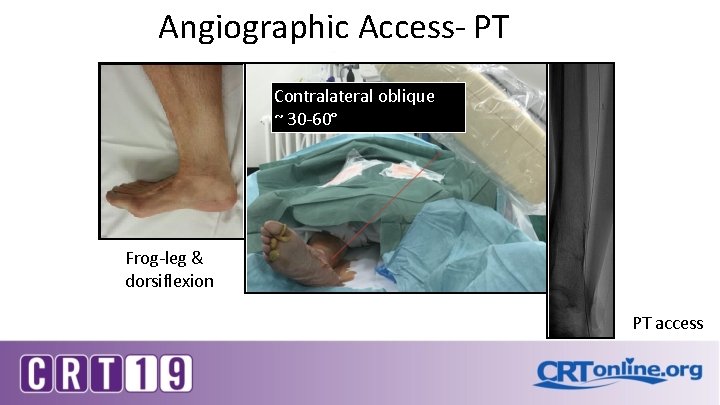
Angiographic Access- PT Contralateral oblique ~ 30 -60° Frog-leg & dorsiflexion PT access
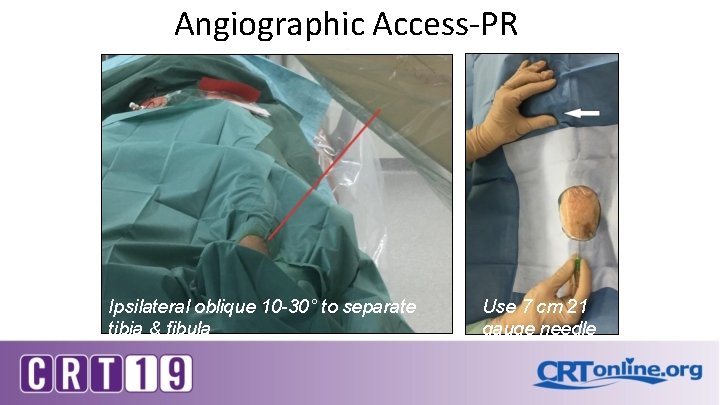
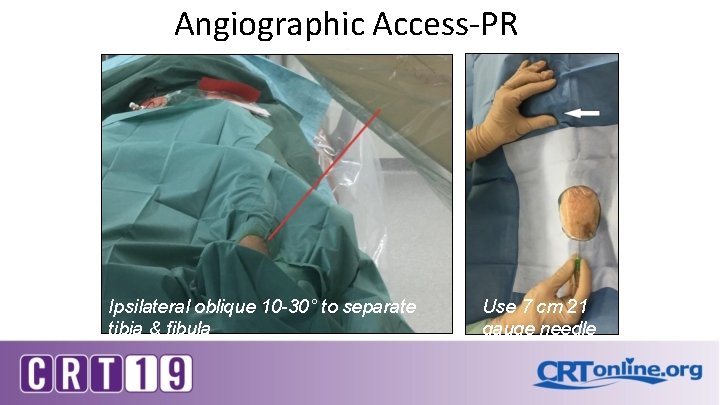
Angiographic Access-PR Ipsilateral oblique 10 -30° to separate tibia & fibula Use 7 cm 21 gauge needle
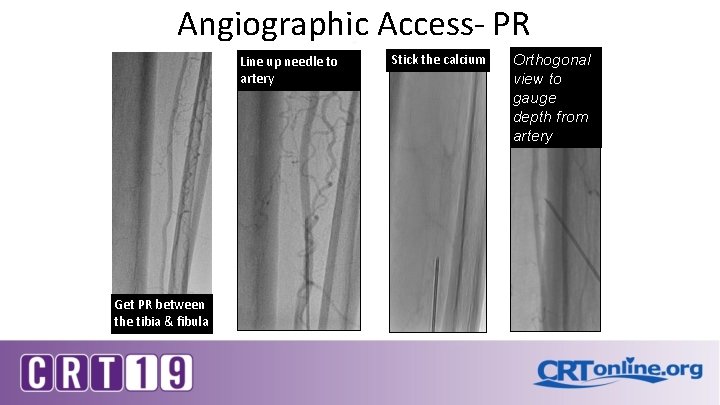
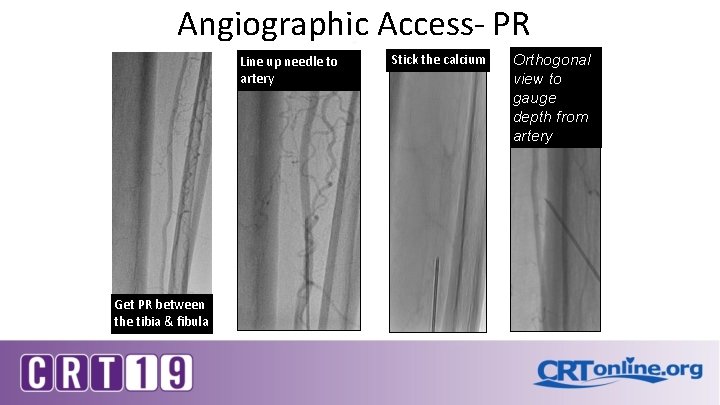
Angiographic Access- PR Line up needle to artery Get PR between the tibia & fibula Stick the calcium Orthogonal view to gauge depth from artery
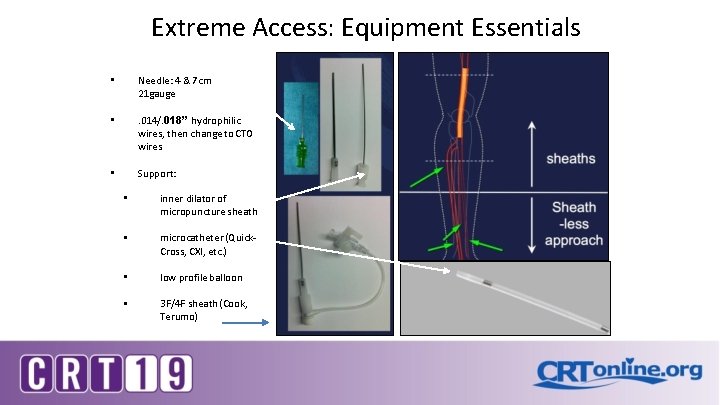
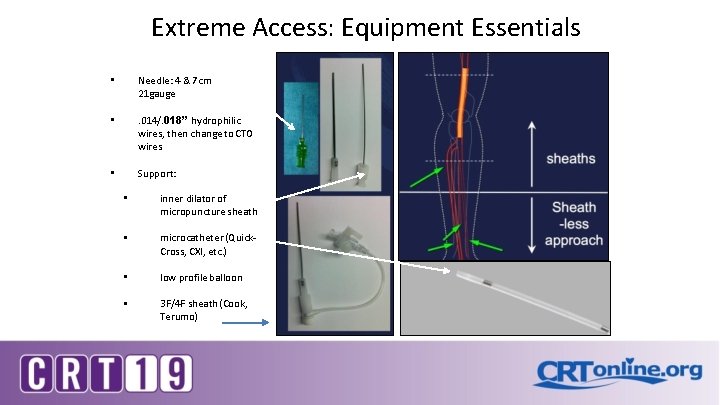
Extreme Access: Equipment Essentials • Needle: 4 & 7 cm 21 gauge • . 014/. 018” hydrophilic wires, then change to CTO wires • Support: • inner dilator of micropuncture sheath • microcatheter (Quick. Cross, CXI, etc. ) • low profile balloon • 3 F/4 F sheath (Cook, Terumo)
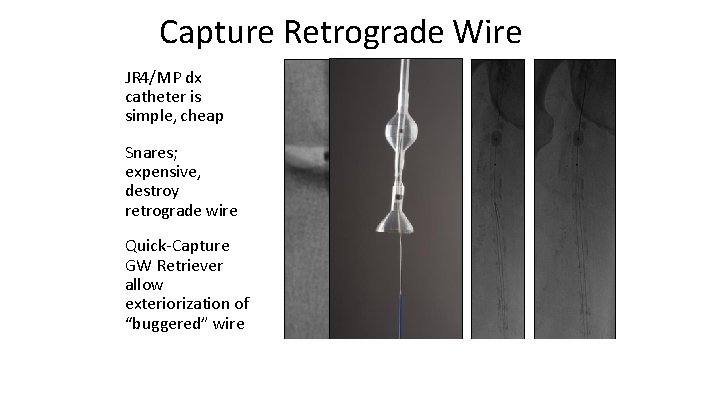
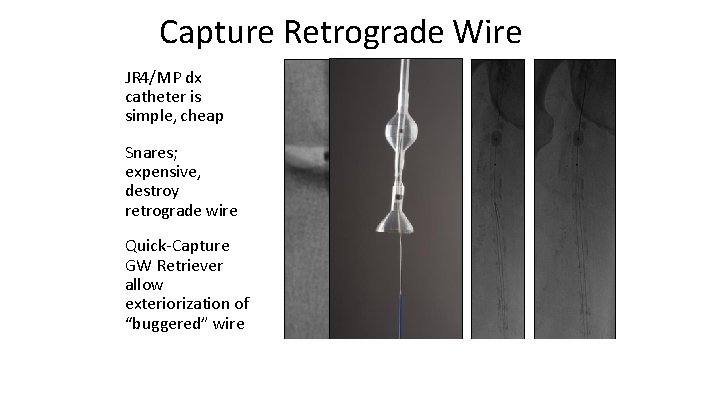
Capture Retrograde Wire JR 4/MP dx catheter is simple, cheap Snares; expensive, destroy retrograde wire Quick-Capture GW Retriever allow exteriorization of “buggered” wire
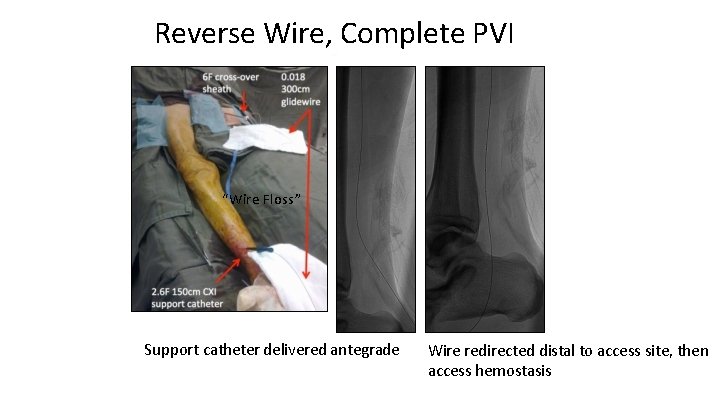
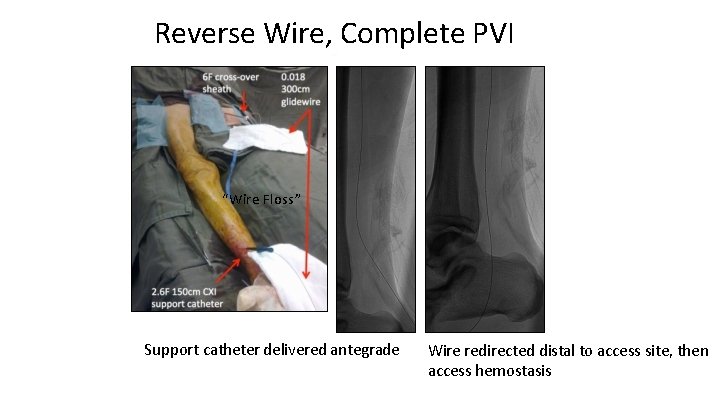
Reverse Wire, Complete PVI “Wire Floss” Support catheter delivered antegrade Wire redirected distal to access site, then access hemostasis
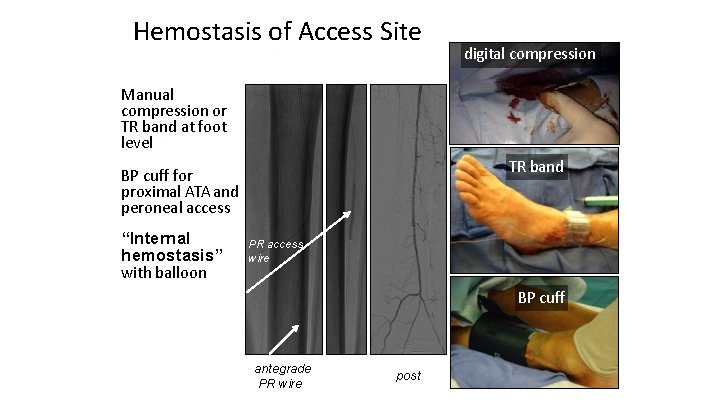
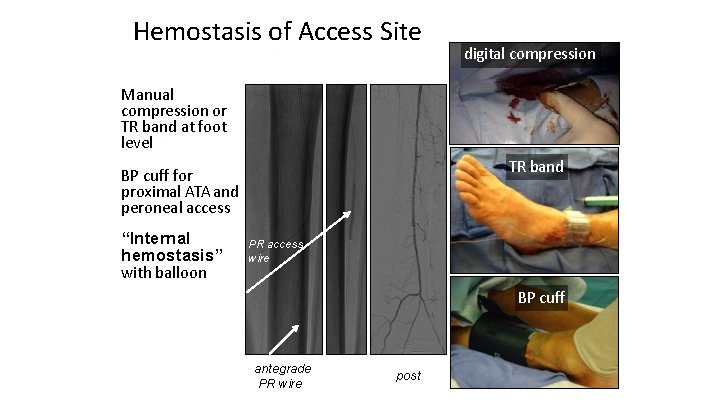
Hemostasis of Access Site digital compression Manual compression or TR band at foot level TR band BP cuff for proximal ATA and peroneal access “Internal hemostasis” with balloon PR access wire BP cuff antegrade PR wire post
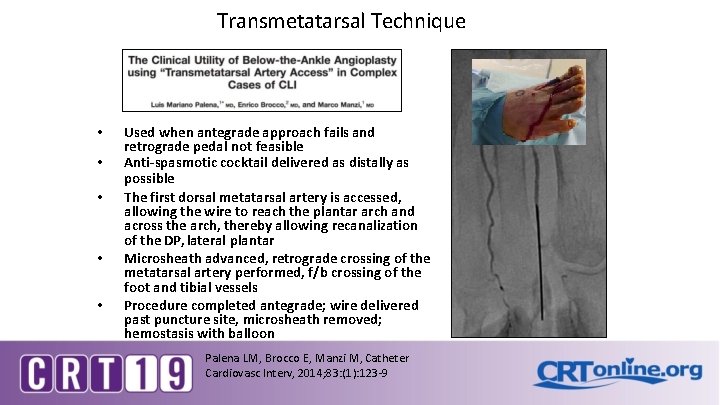
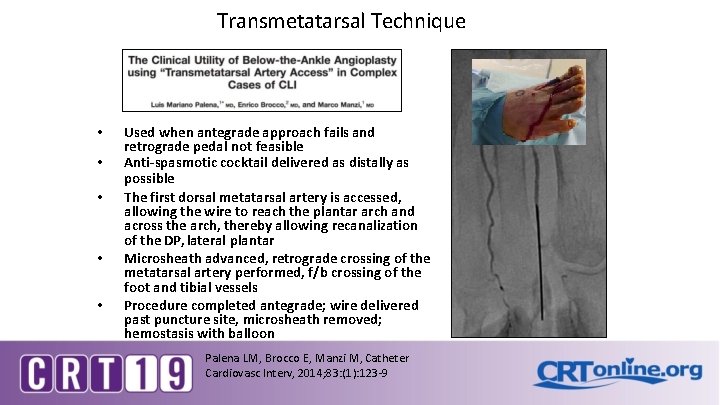
Transmetatarsal Technique • • • Used when antegrade approach fails and retrograde pedal not feasible Anti-spasmotic cocktail delivered as distally as possible The first dorsal metatarsal artery is accessed, allowing the wire to reach the plantar arch and across the arch, thereby allowing recanalization of the DP, lateral plantar Microsheath advanced, retrograde crossing of the metatarsal artery performed, f/b crossing of the foot and tibial vessels Procedure completed antegrade; wire delivered past puncture site, microsheath removed; hemostasis with balloon Palena LM, Brocco E, Manzi M, Catheter Cardiovasc Interv, 2014; 83: (1): 123 -9
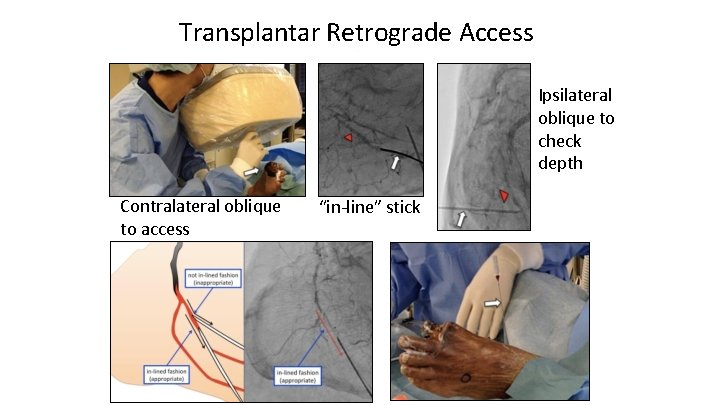
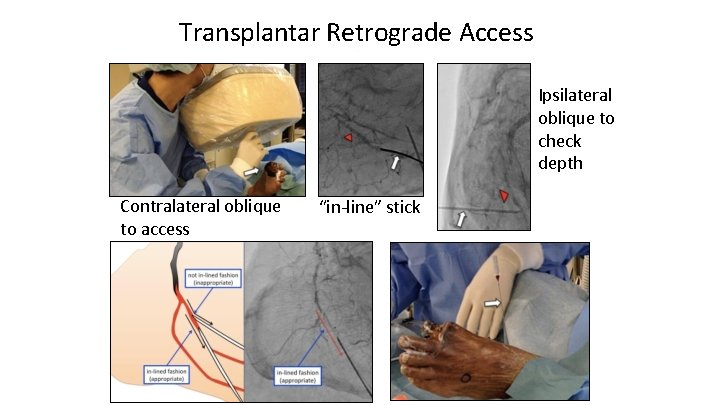
Transplantar Retrograde Access Ipsilateral oblique to check depth Contralateral oblique to access “in-line” stick
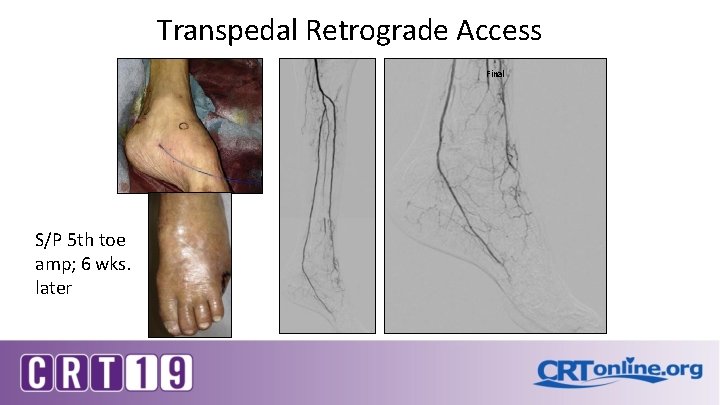
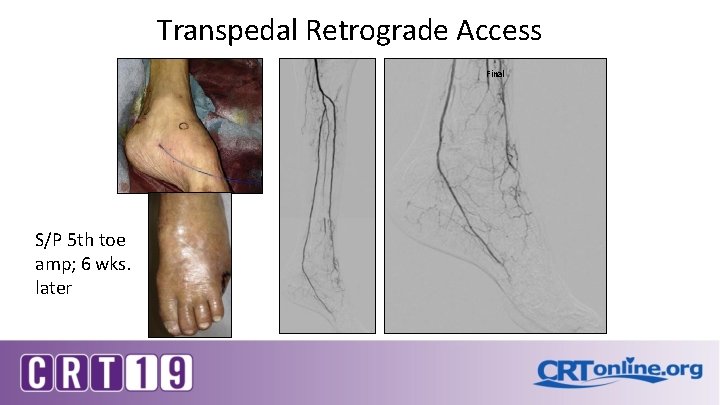
Transpedal Retrograde Access Final S/P 5 th toe amp; 6 wks. later
Extreme Access- Transplantar Obese 63 yo female with IDDM, HBP, HLD, Behcet’s on chronic steroids, CVI, CAD S/P CABG x 2 P/w CLI with NHU left heel and recent left hallux amp for osteo Referred for angiography/PVI due to failed amp site healing and for limb salvage
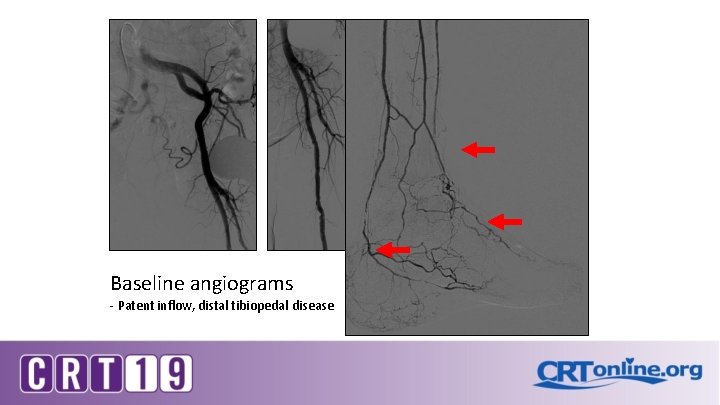
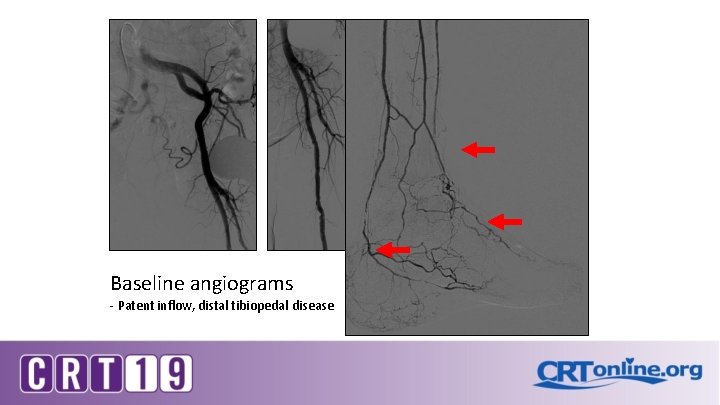
Baseline angiograms - Patent inflow, distal tibiopedal disease
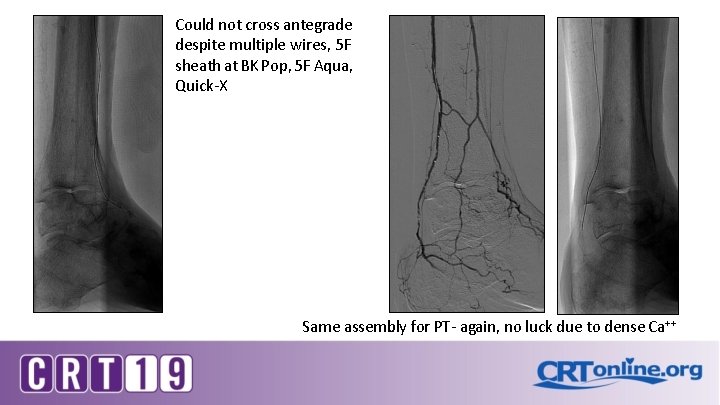
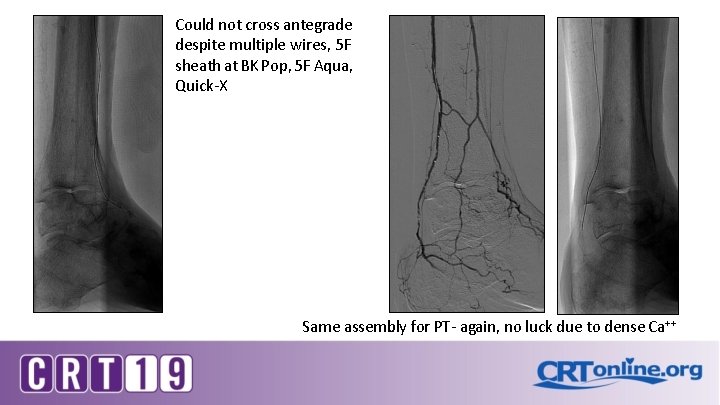
Could not cross antegrade despite multiple wires, 5 F sheath at BK Pop, 5 F Aqua, Quick-X Same assembly for PT- again, no luck due to dense Ca++
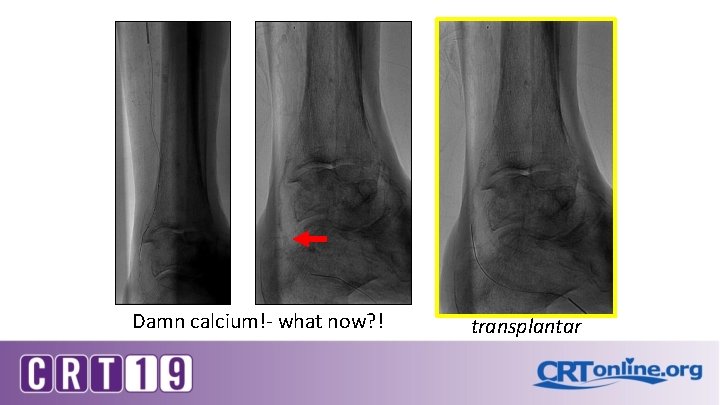
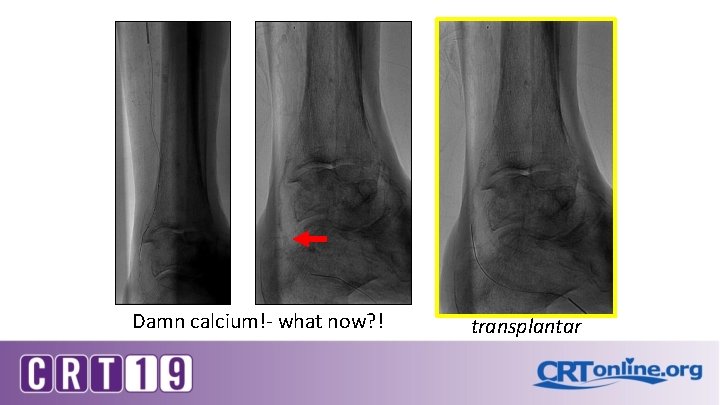
Damn calcium!- what now? ! transplantar

Transplantar wire access
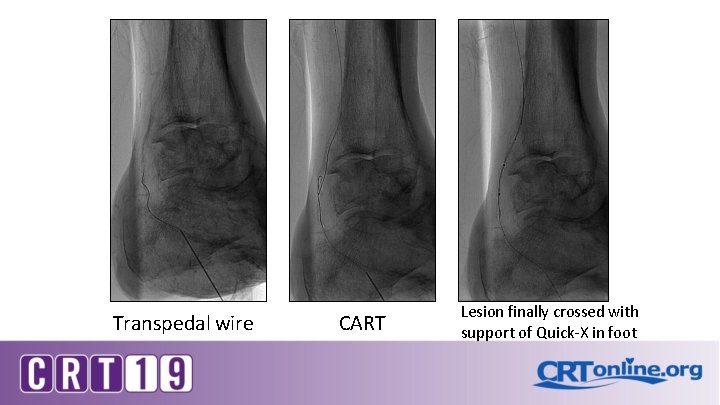
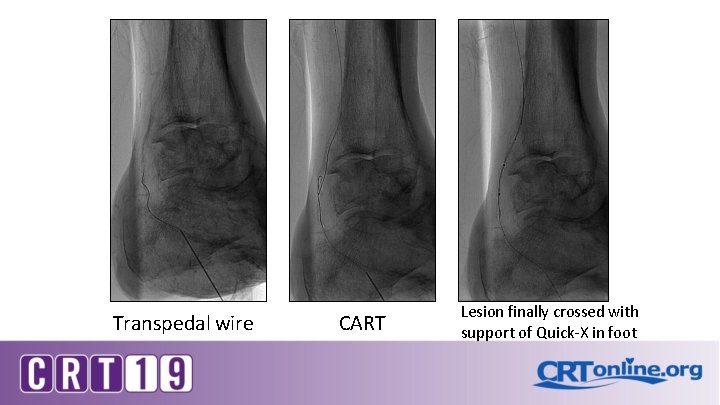
Transpedal wire CART Lesion finally crossed with support of Quick-X in foot

PTA with 2 mm balloon…
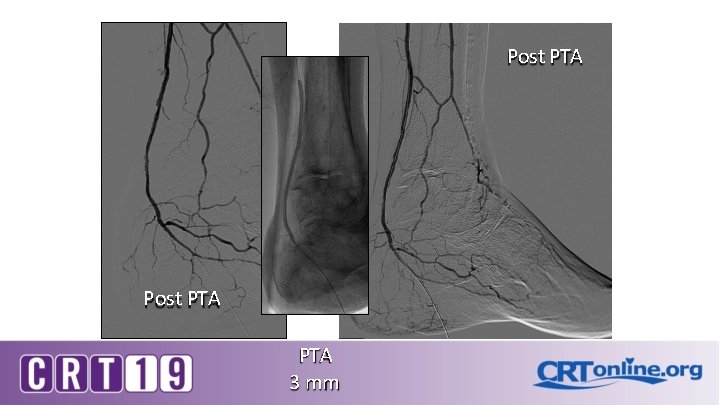
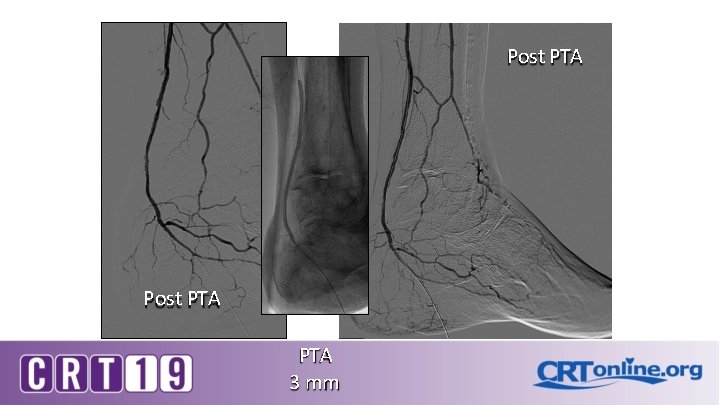
Post PTA PTA 3 mm
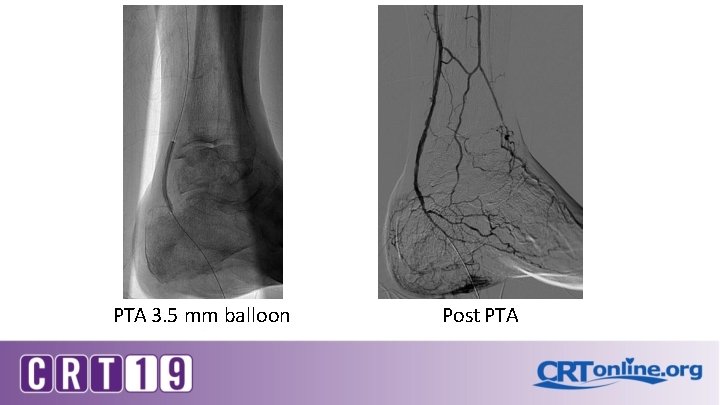
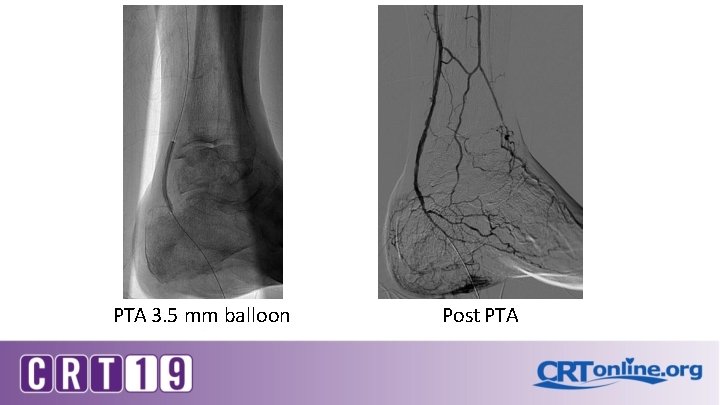
PTA 3. 5 mm balloon Post PTA
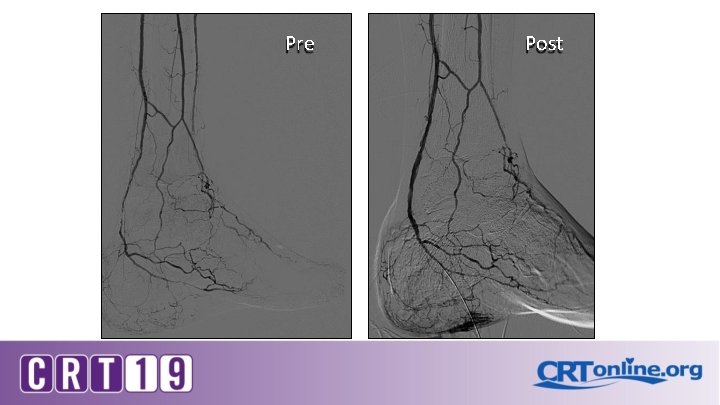
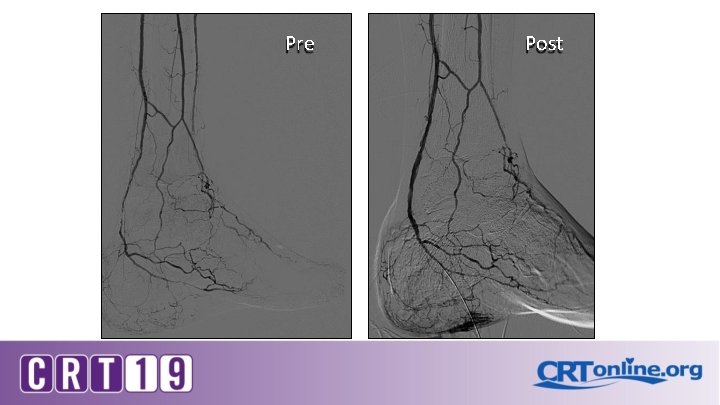
Pre Post
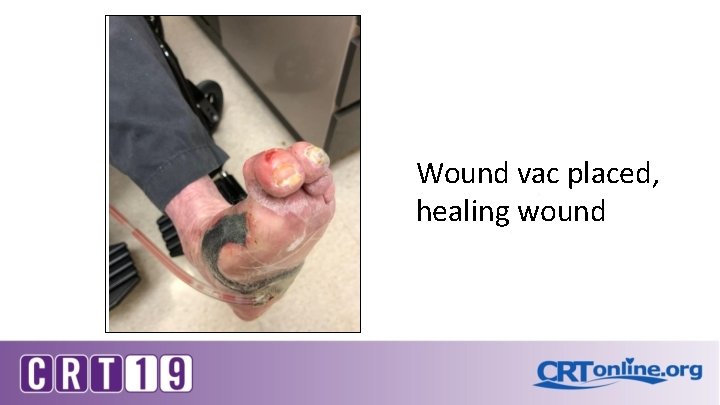
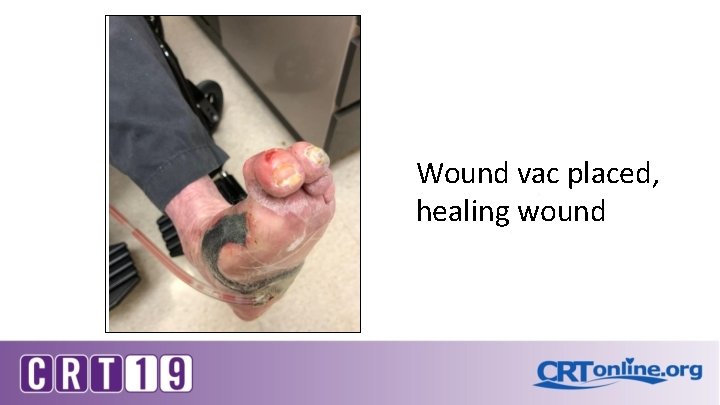
Wound vac placed, healing wound
Case Examples
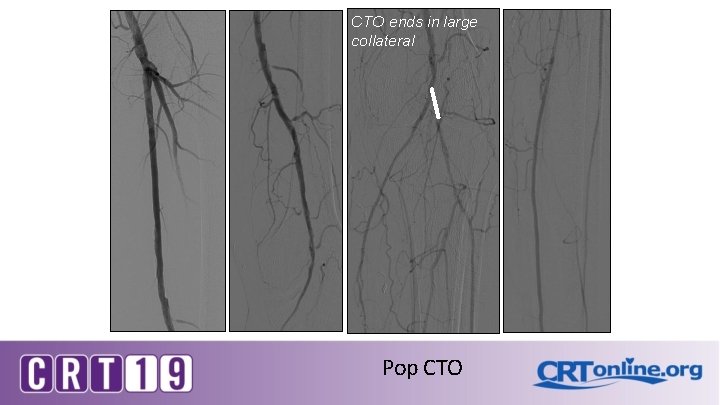
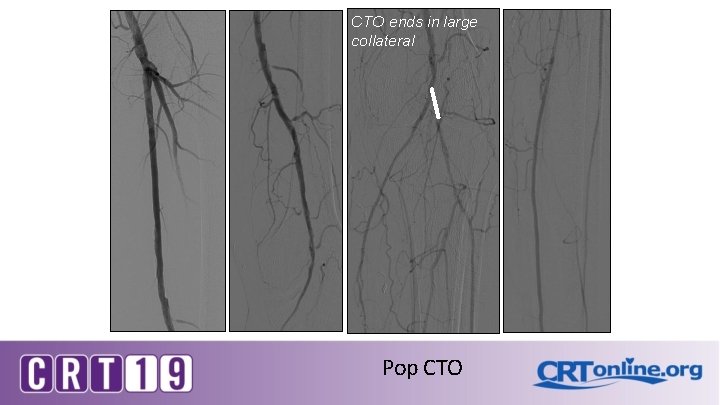
CTO ends in large collateral Pop CTO
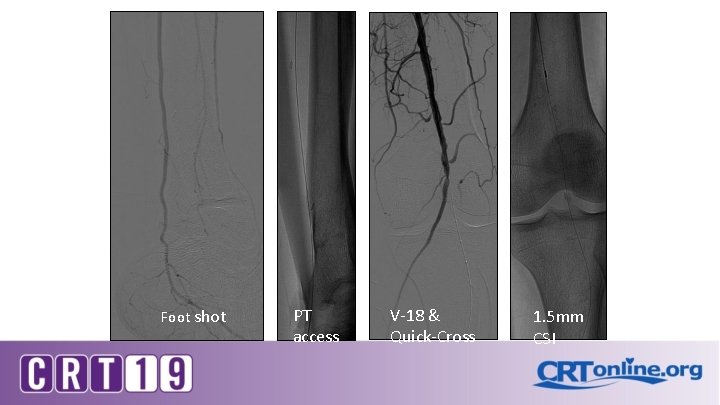
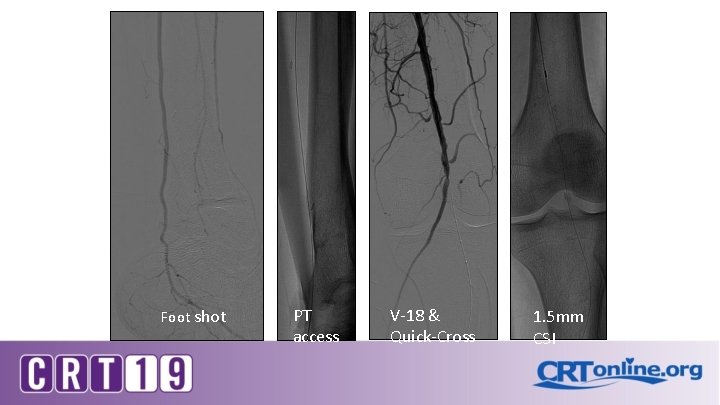
Foot shot PT access V-18 & Quick-Cross 1. 5 mm CSI
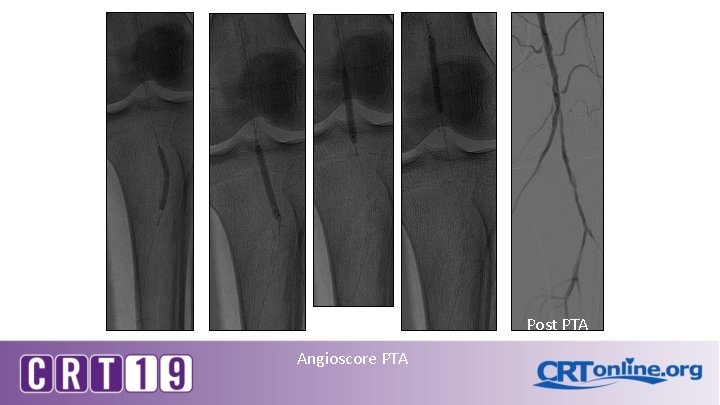
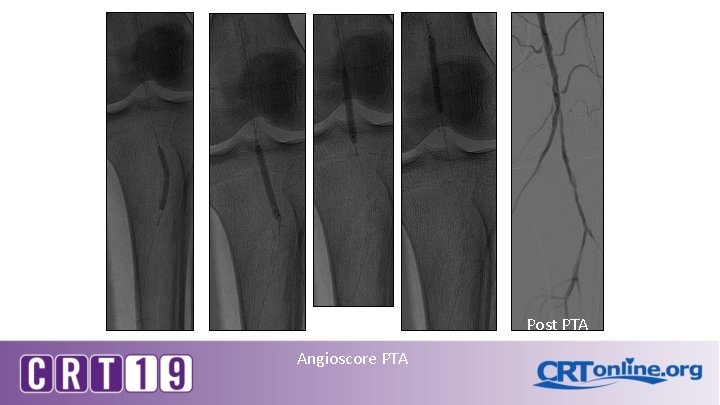
Post PTA Angioscore PTA

DCB Post PTA Supera
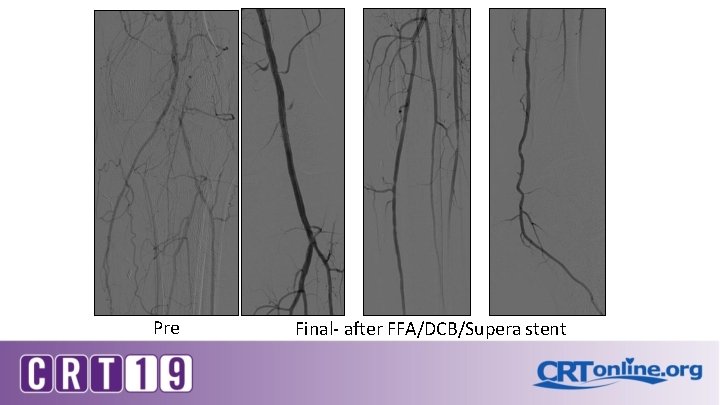
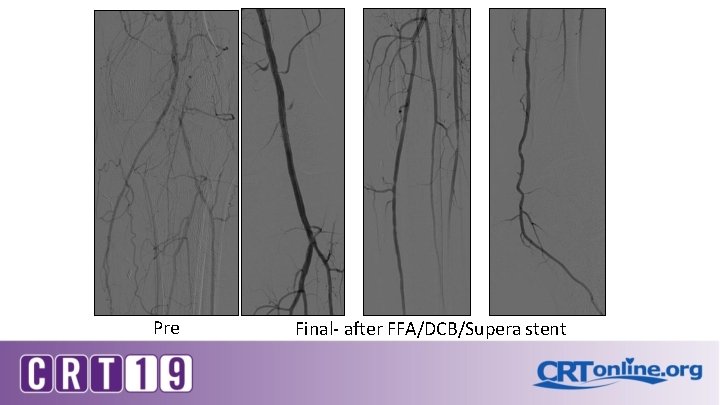
Pre Final- after FFA/DCB/Supera stent
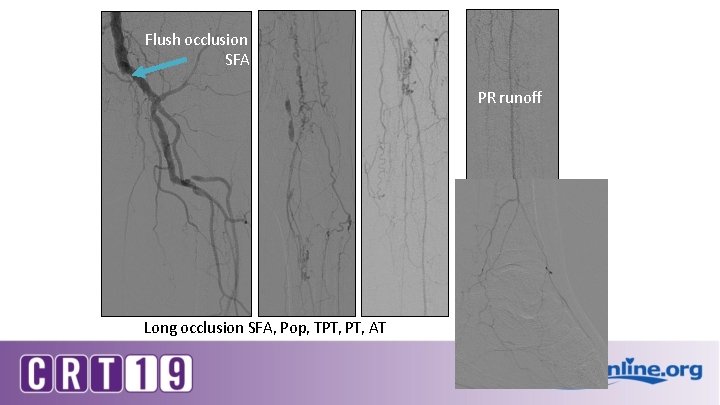
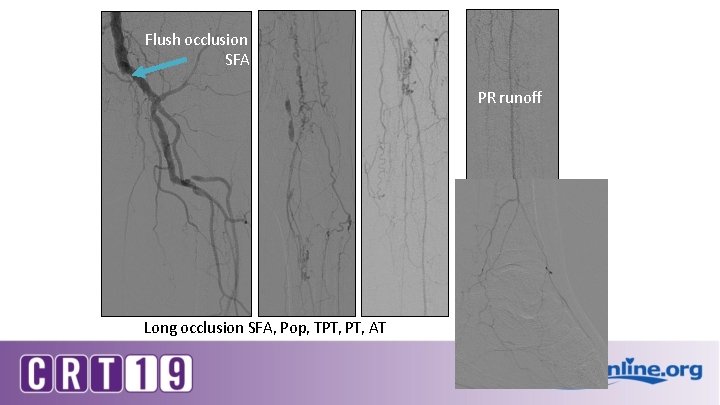
Flush occlusion SFA PR runoff Long occlusion SFA, Pop, TPT, AT
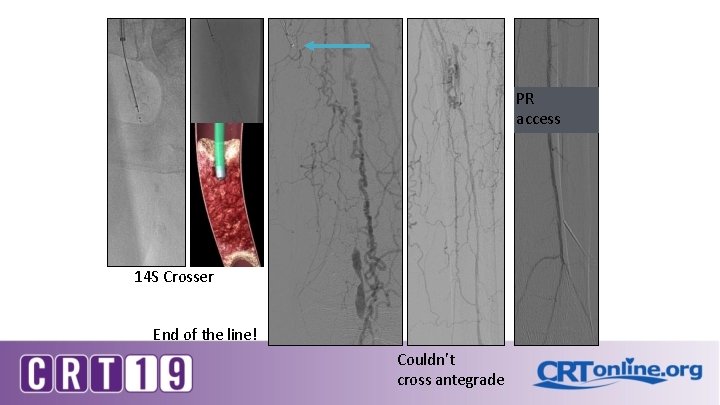
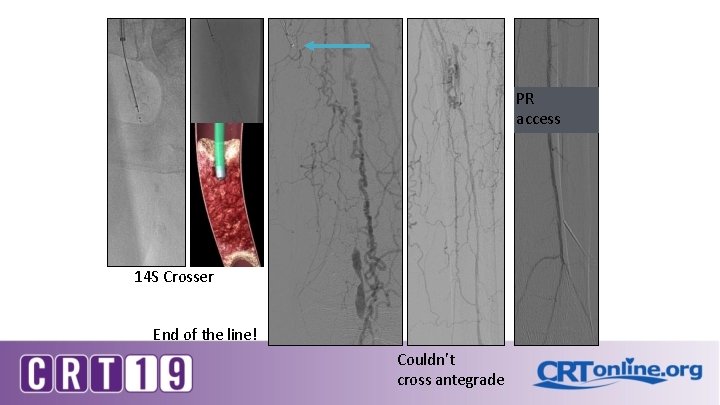
PR access 14 S Crosser End of the line! Couldn’t cross antegrade
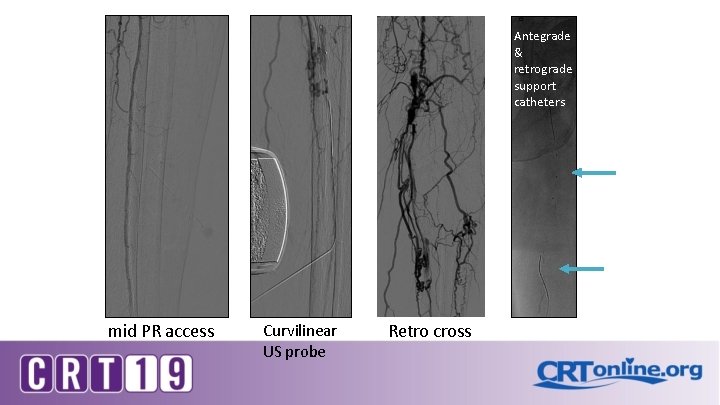
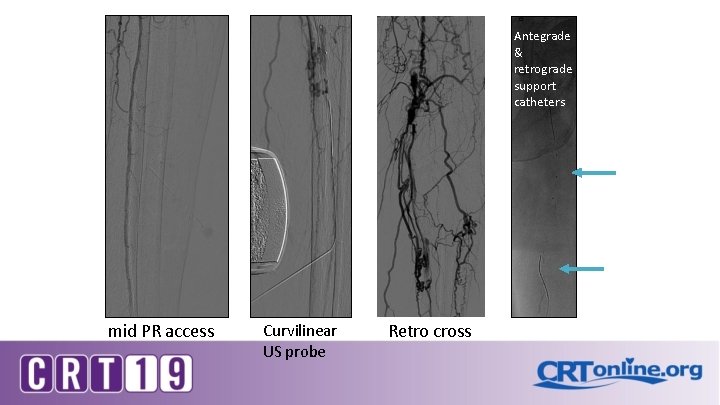
Antegrade & retrograde support catheters mid PR access Curvilinear US probe Retro cross

wire delivered antegrade into PR true lumen Post Yuck Success! balloon hemostasis DCB Supera
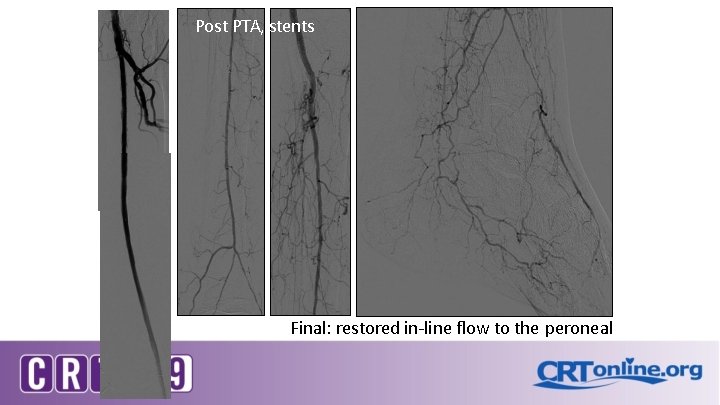
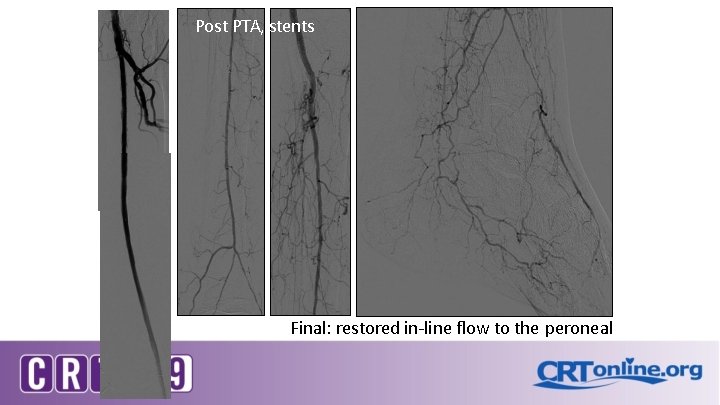
Post PTA, stents Final: restored in-line flow to the peroneal
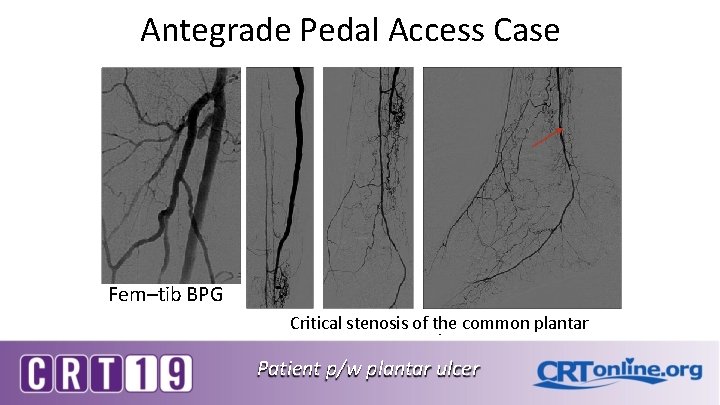
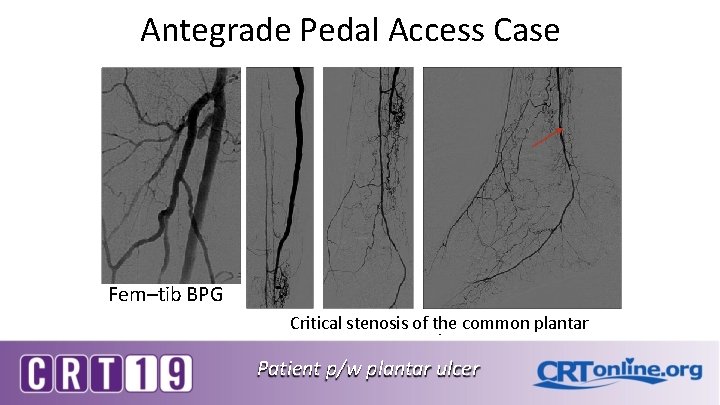
Antegrade Pedal Access Case Fem–tib BPG Critical stenosis of the common plantar Patient p/w plantar ulcer
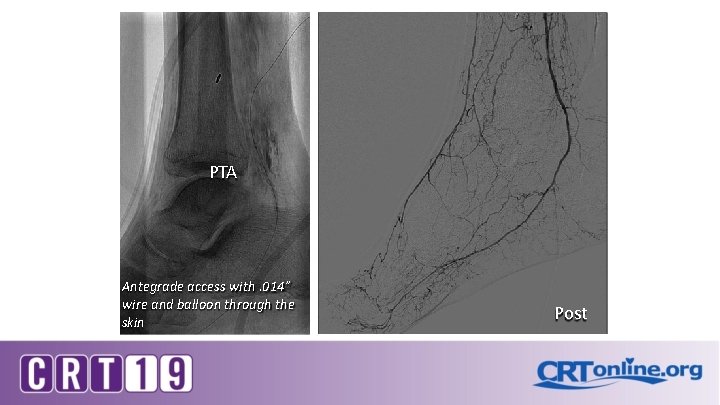
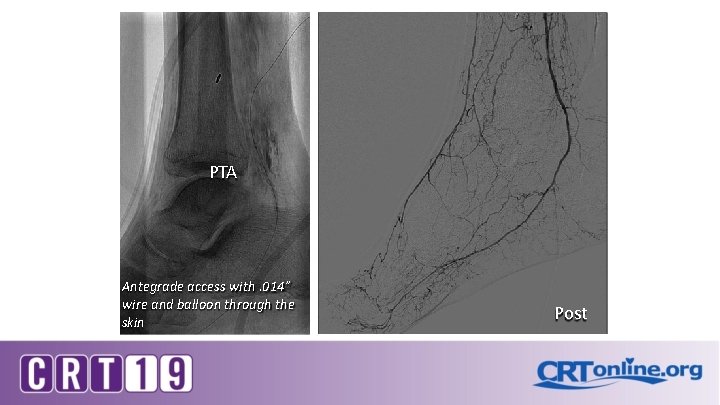
PTA Antegrade access with. 014” wire and balloon through the skin Post
Extreme Access- Conclusions Pedal access is safe, has a high success rate, and is an essential skill for the serious CLI operator Use ultrasound for access, and lots of vasodilators "Extreme” techniques such as transmetatarsal and transplantar will further increase our success rates for treating CLI patients