Part1 Impact of Periodontal infection on Systemic Health




- Slides: 37
Part-1 Impact of Periodontal infection on Systemic Health • Prof(Dr) VIVEK Kr. SHARMA 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
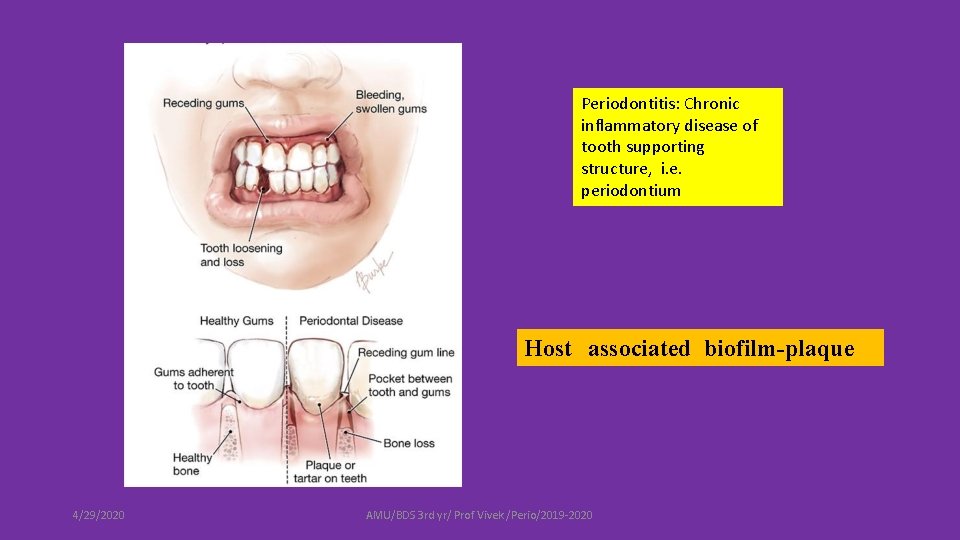
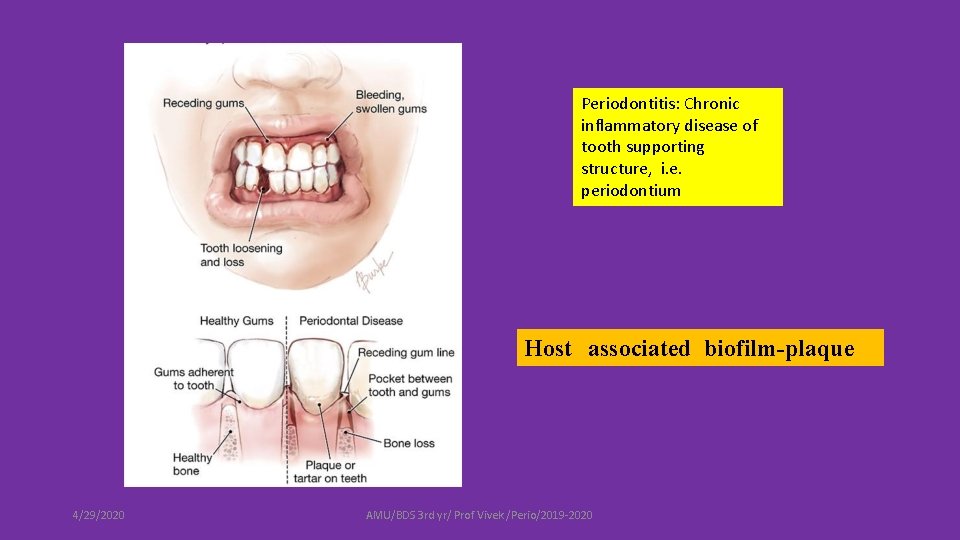
Periodontitis: Chronic inflammatory disease of tooth supporting structure, i. e. periodontium Host associated biofilm-plaque 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
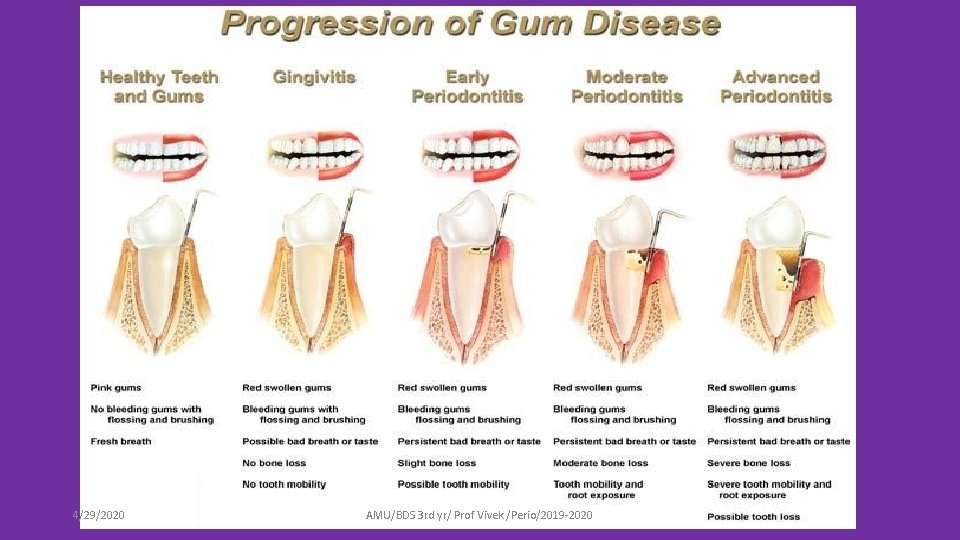
4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
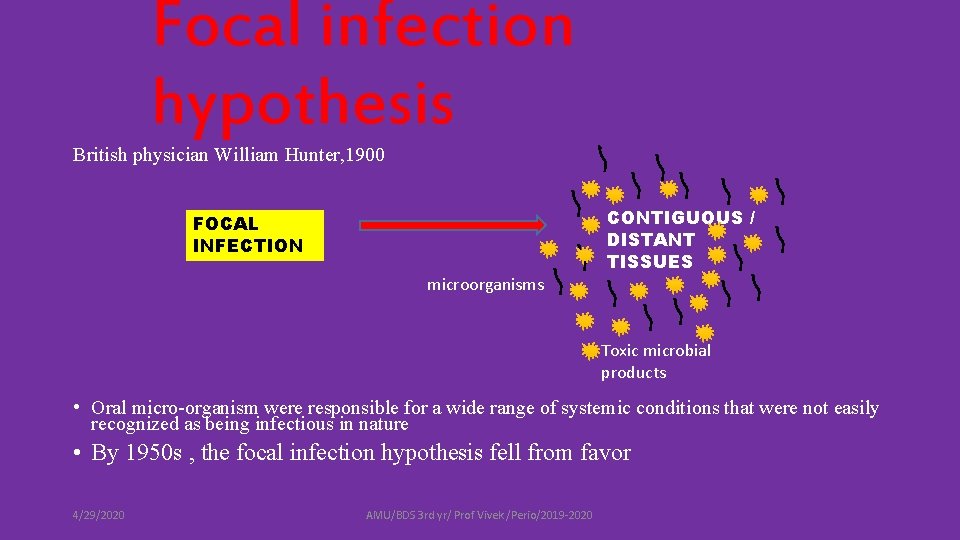
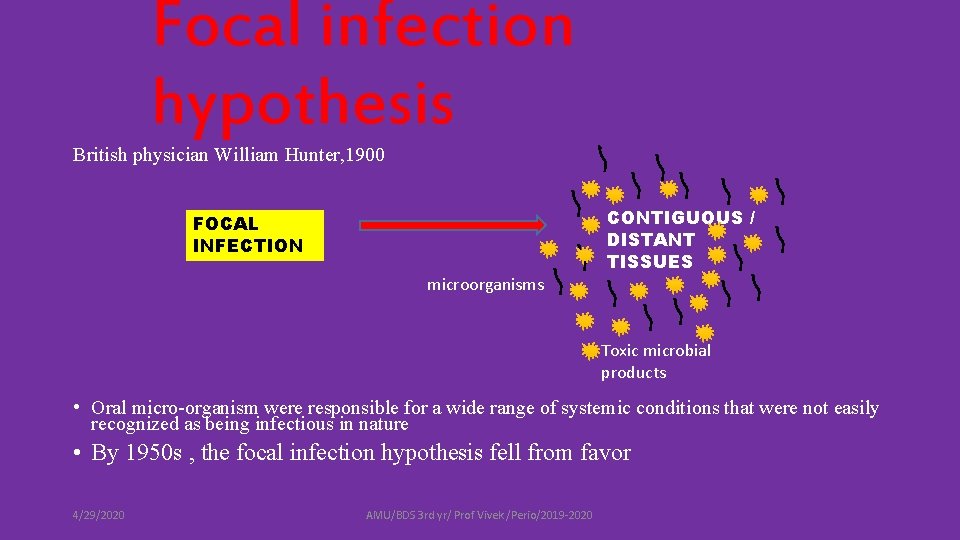
Focal infection hypothesis British physician William Hunter, 1900 CONTIGUOUS / DISTANT TISSUES FOCAL INFECTION microorganisms Toxic microbial products • Oral micro-organism were responsible for a wide range of systemic conditions that were not easily recognized as being infectious in nature • By 1950 s , the focal infection hypothesis fell from favor 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
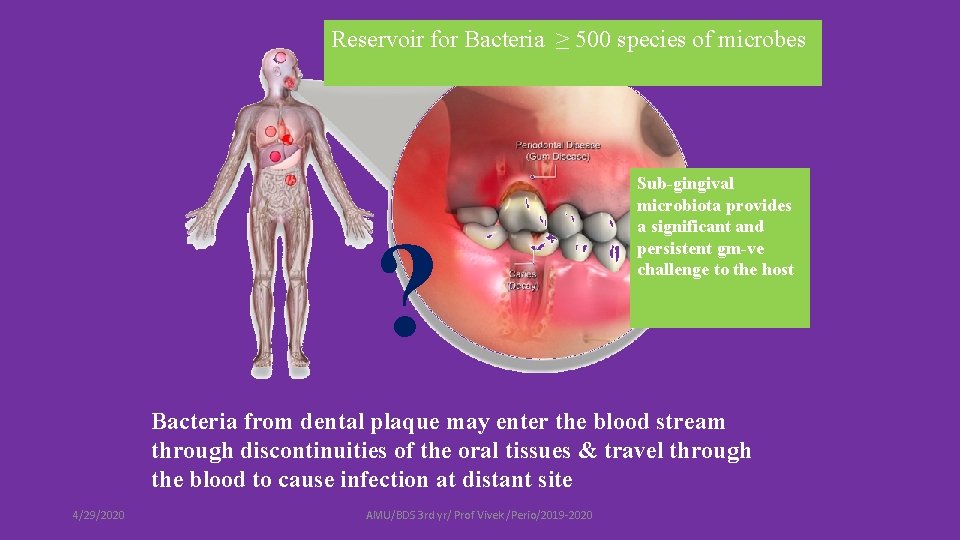
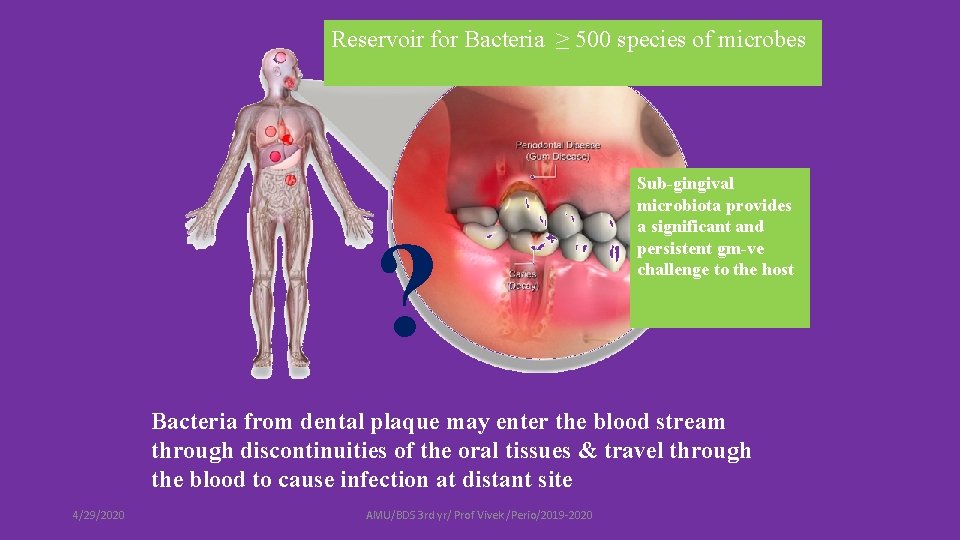
Reservoir for Bacteria ≥ 500 species of microbes ? Sub-gingival microbiota provides a significant and persistent gm-ve challenge to the host Bacteria from dental plaque may enter the blood stream through discontinuities of the oral tissues & travel through the blood to cause infection at distant site 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
Periodontal disease and Mortality • Studies support the association between poor oral health and an increase risk for mortality • Patients with more than 21% alveolar bone loss, the risk of dying was found to be 70% higher than those without bone loss 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
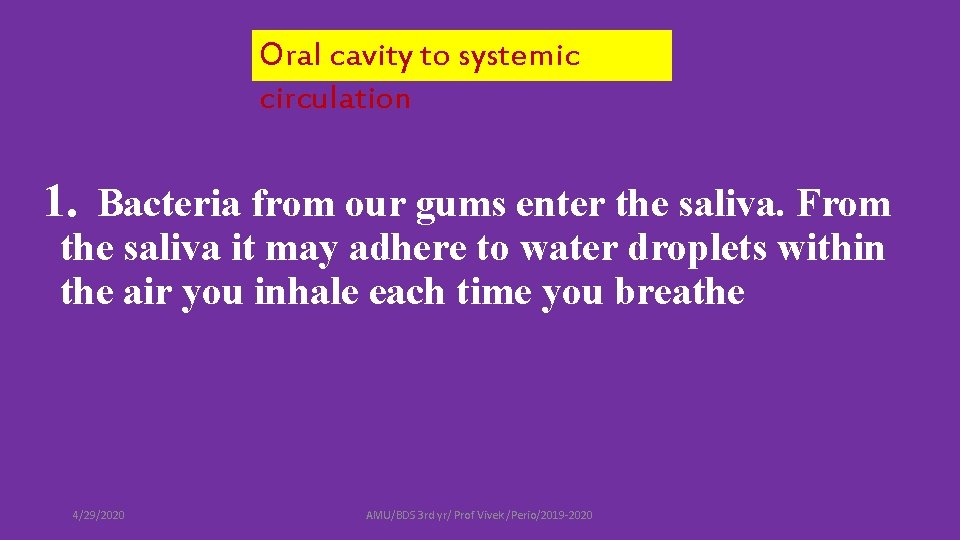
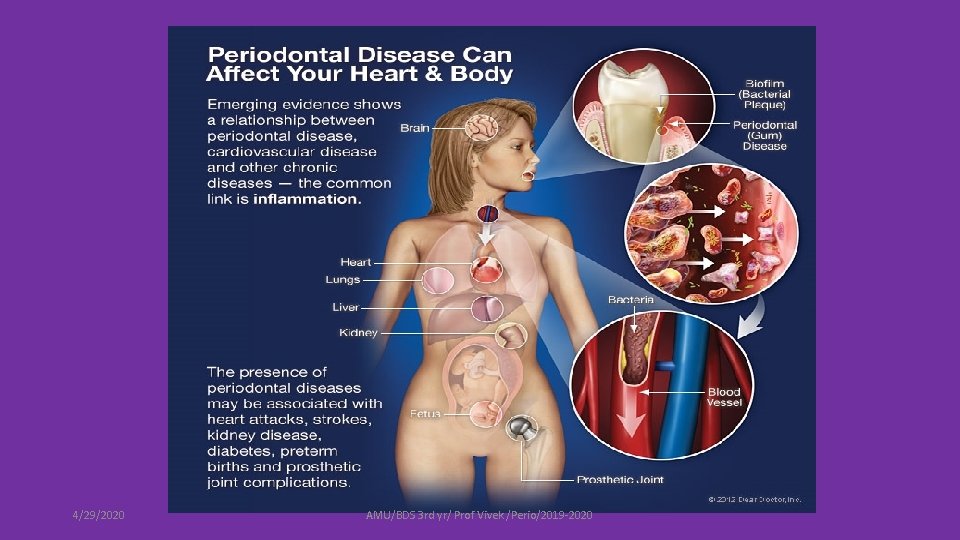
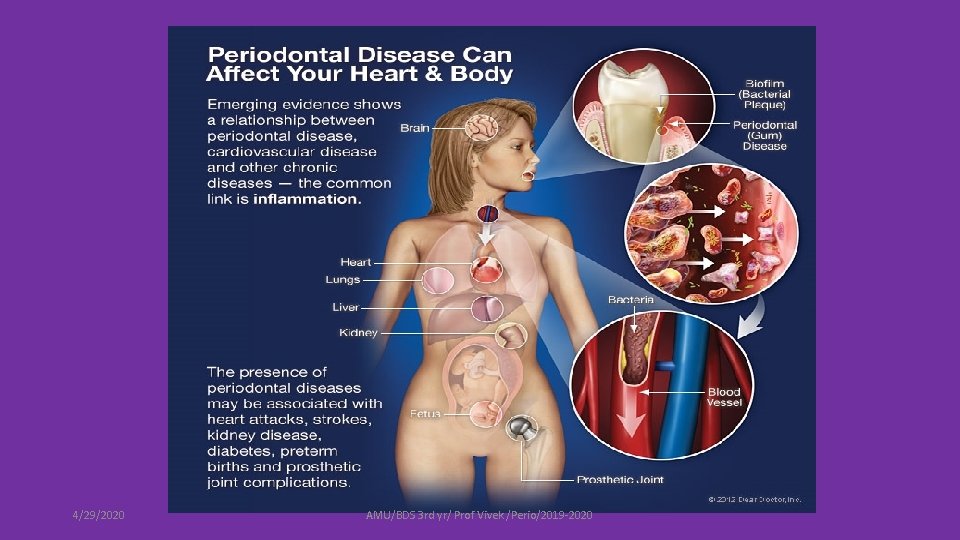
Oral cavity to systemic circulation 1. Bacteria from our gums enter the saliva. From the saliva it may adhere to water droplets within the air you inhale each time you breathe 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
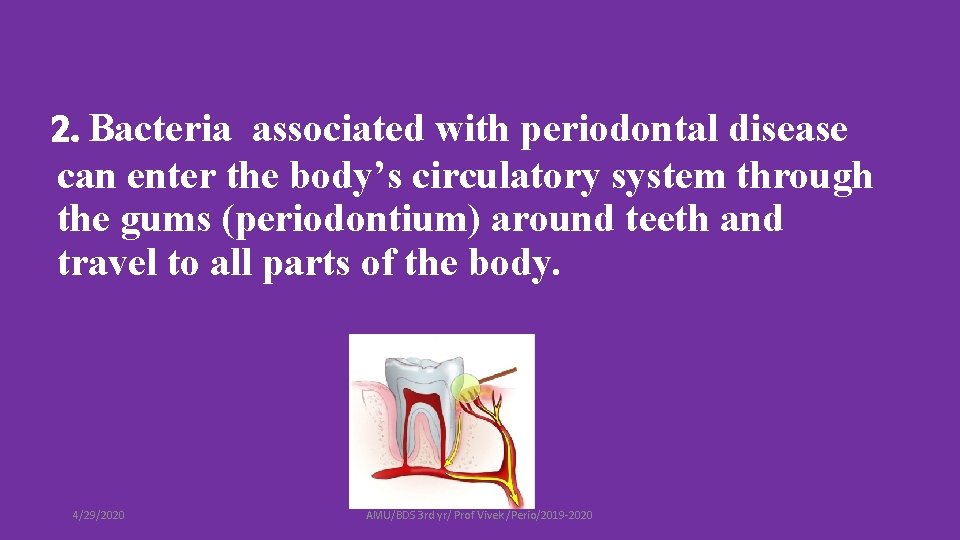
2. Bacteria associated with periodontal disease can enter the body’s circulatory system through the gums (periodontium) around teeth and travel to all parts of the body. 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
3. Inflammation associated with periodontal disease may stimulate a second systemic inflammatory response within the body and contribute to or complicate other disease entities that may have an inflammatory origin. 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020

PERIODONTAL INFLAMMATION Periodontopathogens or their products(LPS) BACTEREMIA Periodonto pathogens Inflammatory mediators(IL-1, IL 6, TNF-ᾳ) LIVER Bacteria induce platelet aggregate, invade endothelium, digest matrix 4/29/2020 IMMUNE RESPONSE C-reactive protein, serum amyloid , fibrinogen TARGET ORGAN AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020 Antibodies to bacteria & to cross -reactive antigens such as heat-shock proteins, T-cells sensitized
4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
ETIOLOGY HOST BACTERIA 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020 TIME
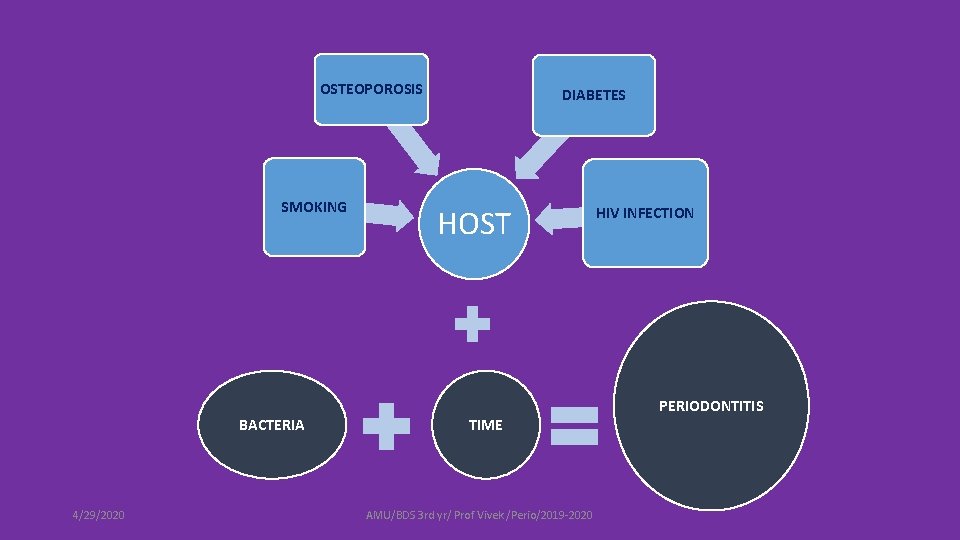
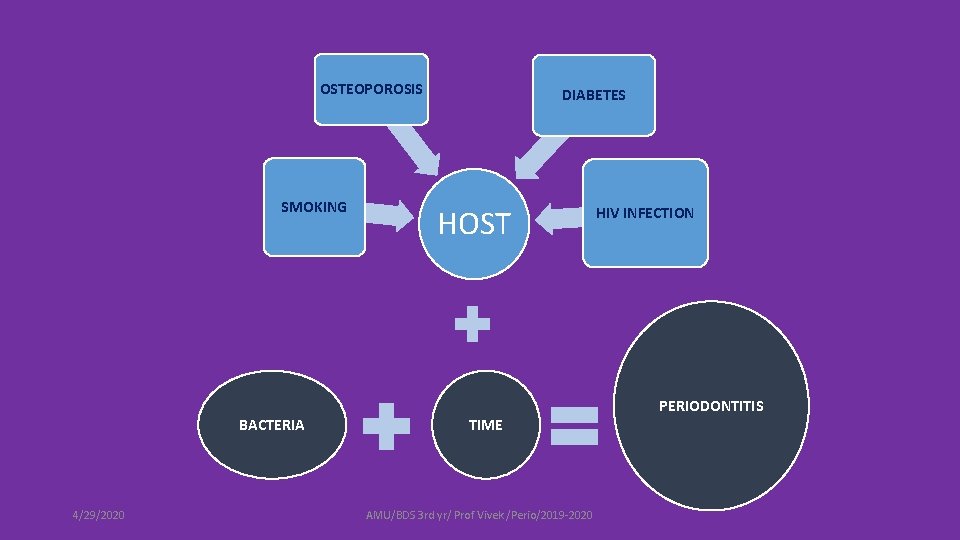
OSTEOPOROSIS SMOKING BACTERIA 4/29/2020 DIABETES HOST TIME AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020 HIV INFECTION PERIODONTITIS

This a two way street Periodontal health /disease Systemic health /disease 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020

SYSTEMIC DISEASE TO ORAL HEALTH SYSTEMIC CONDITION S MAY HAVE EFFECT ON: • Physiological response • Vascular system • Inflammotory response • Immune system • Tissue repair 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
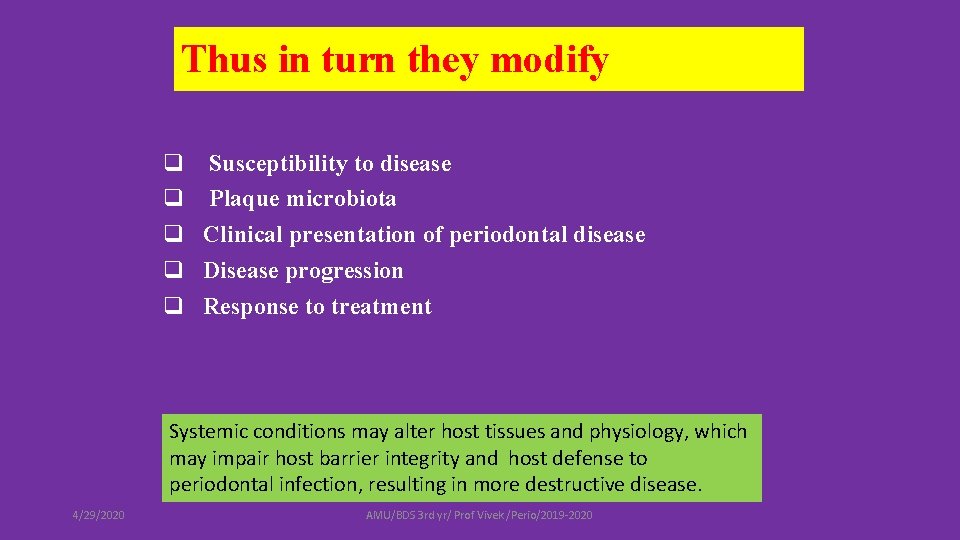
Thus in turn they modify q Susceptibility to disease q Plaque microbiota q Clinical presentation of periodontal disease q Disease progression q Response to treatment Systemic conditions may alter host tissues and physiology, which may impair host barrier integrity and host defense to periodontal infection, resulting in more destructive disease. 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
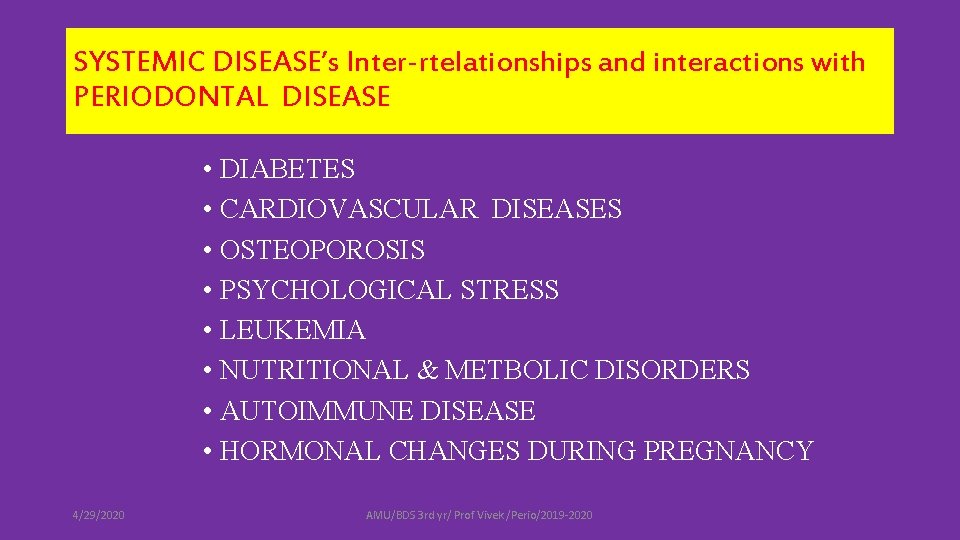
SYSTEMIC DISEASE’s Inter-rtelationships and interactions with PERIODONTAL DISEASE • DIABETES • CARDIOVASCULAR DISEASES • OSTEOPOROSIS • PSYCHOLOGICAL STRESS • LEUKEMIA • NUTRITIONAL & METBOLIC DISORDERS • AUTOIMMUNE DISEASE • HORMONAL CHANGES DURING PREGNANCY 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
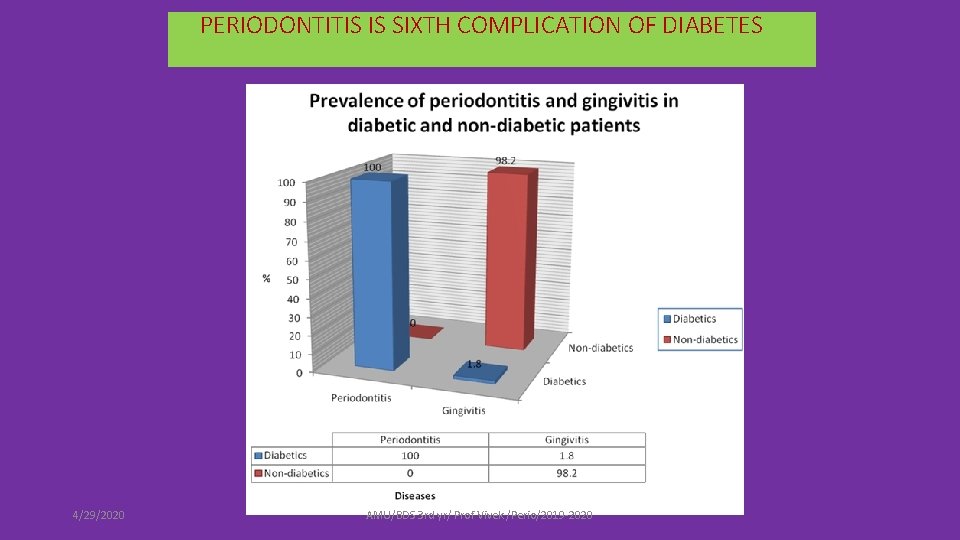
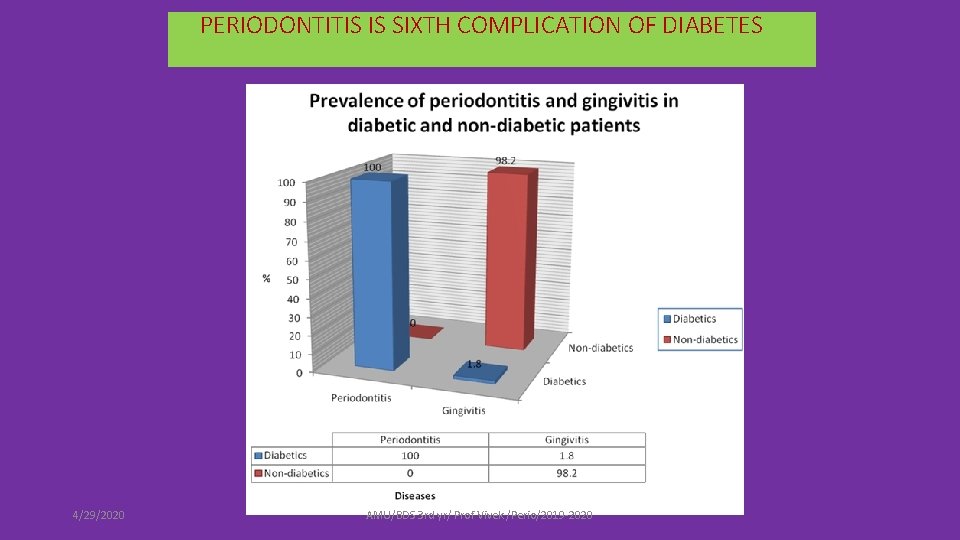
PERIODONTITIS IS SIXTH COMPLICATION OF DIABETES 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020

• Severe gingival inflammation due to diabetes 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
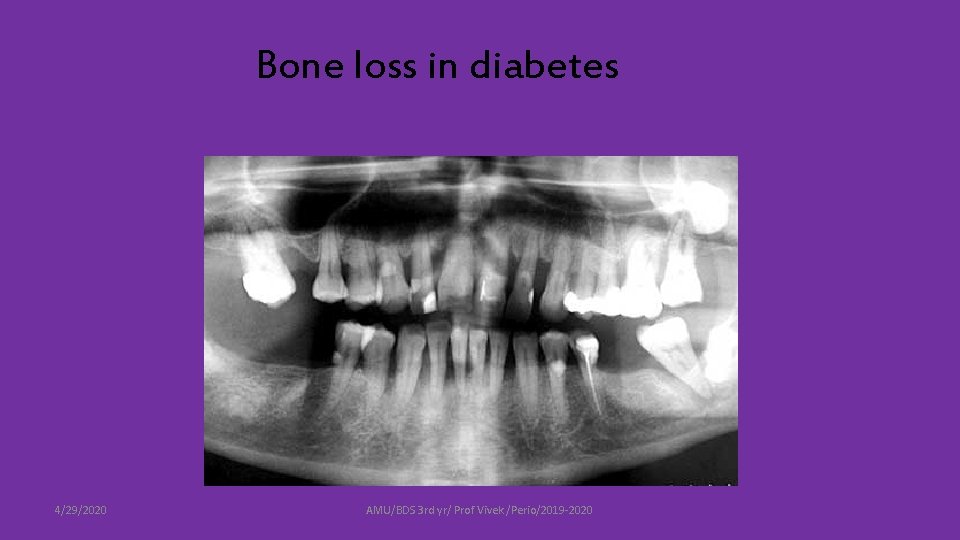
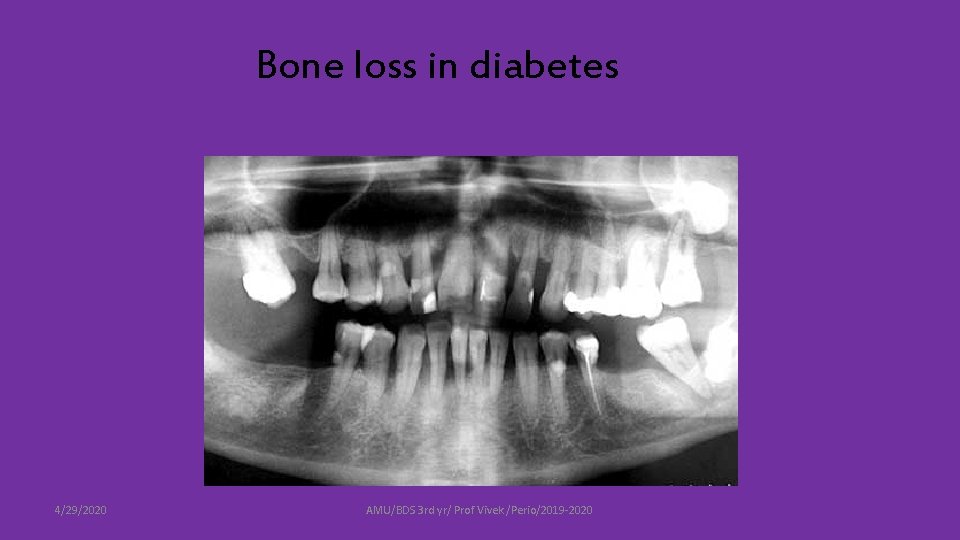
Bone loss in diabetes 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
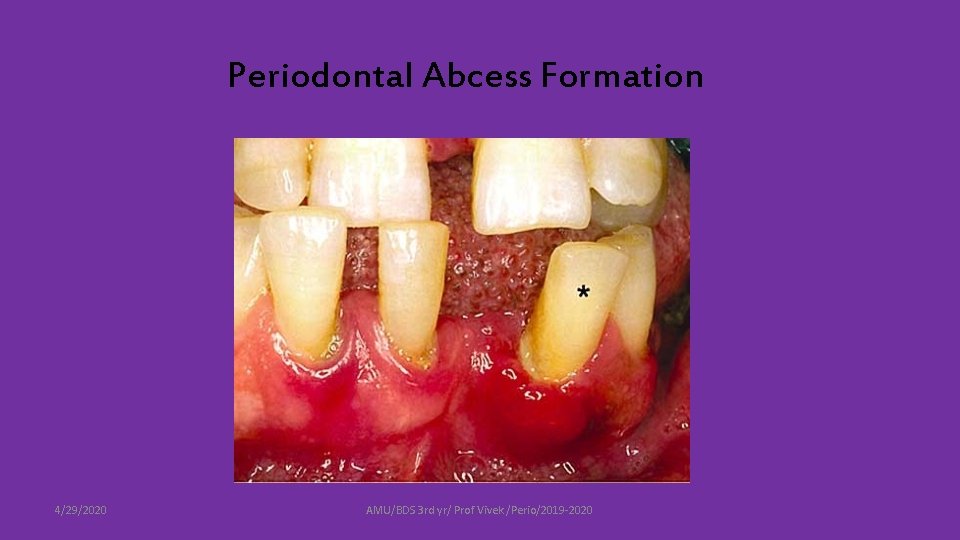
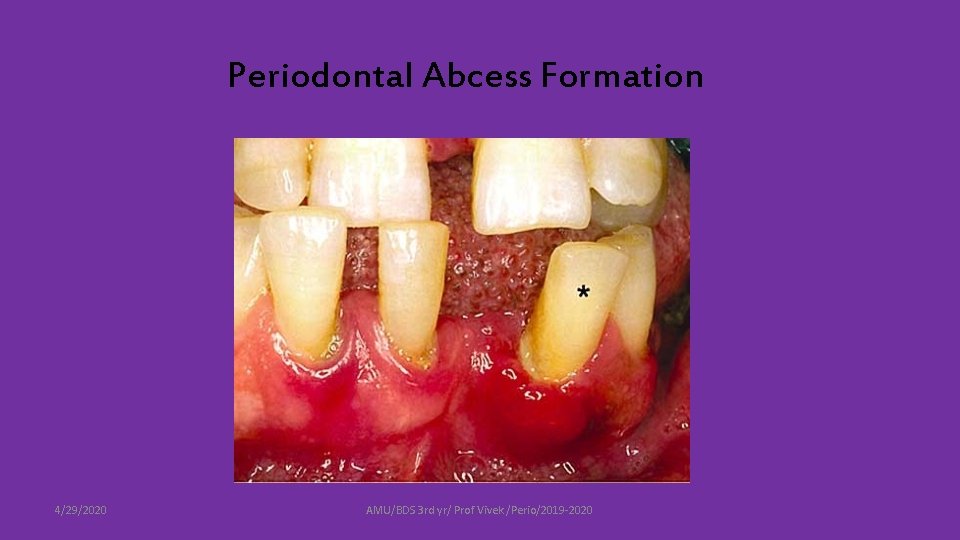
Periodontal Abcess Formation 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
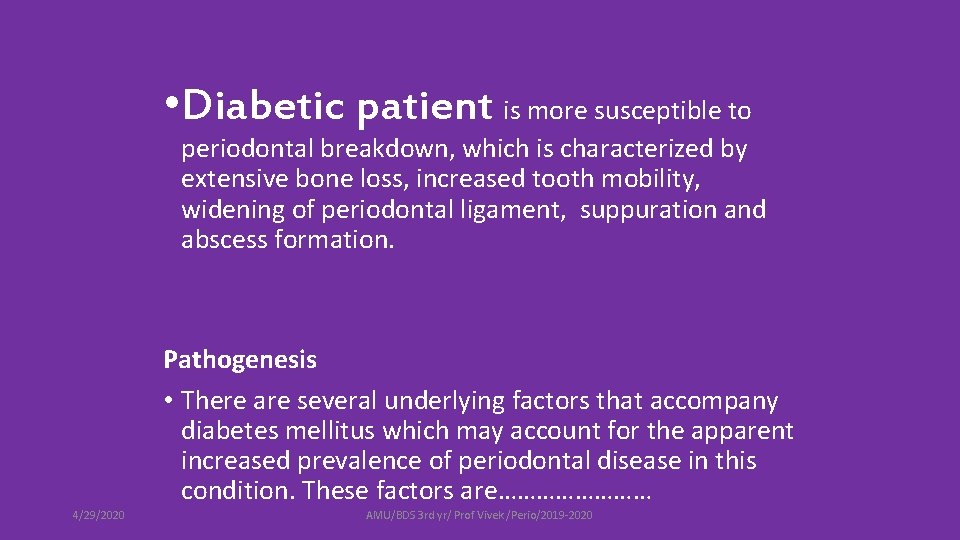
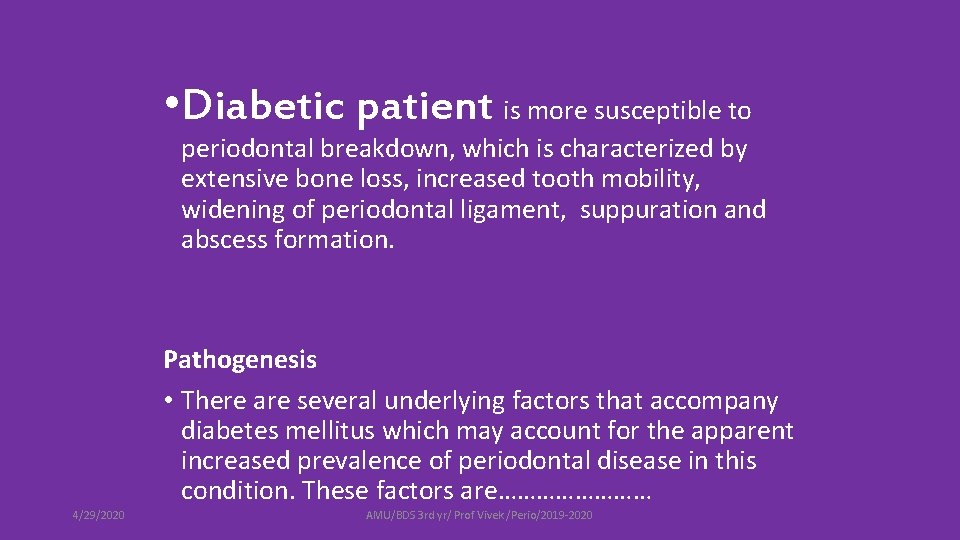
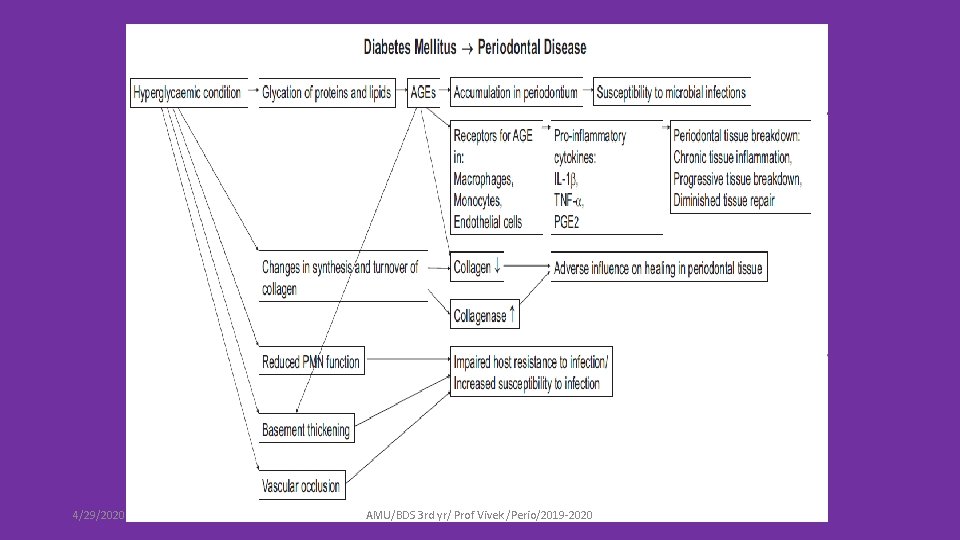
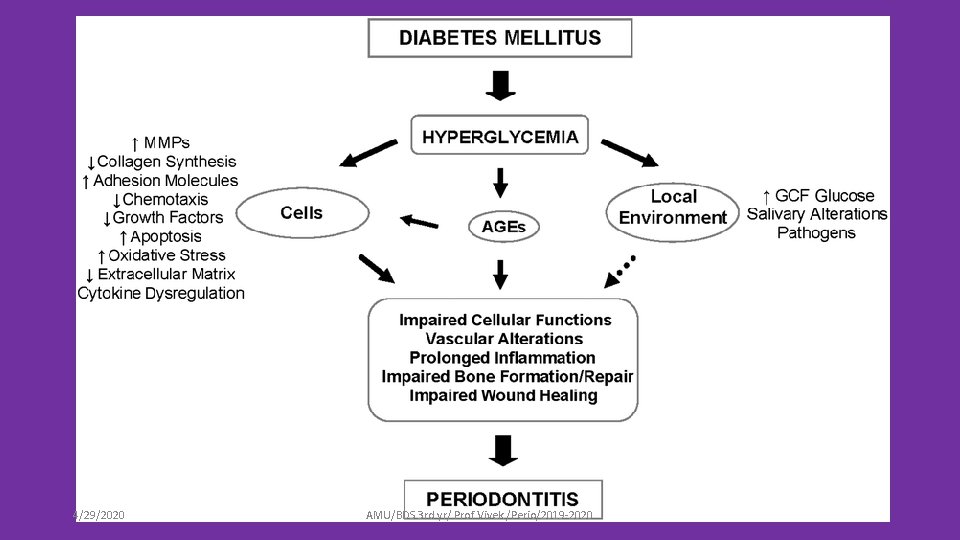
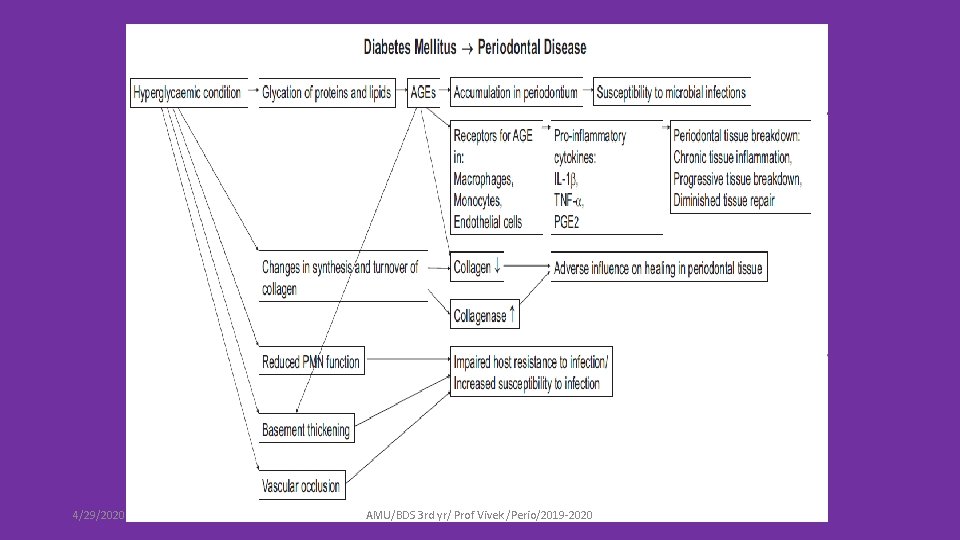
• Diabetic patient is more susceptible to periodontal breakdown, which is characterized by extensive bone loss, increased tooth mobility, widening of periodontal ligament, suppuration and abscess formation. Pathogenesis • There are several underlying factors that accompany diabetes mellitus which may account for the apparent increased prevalence of periodontal disease in this condition. These factors are………… 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
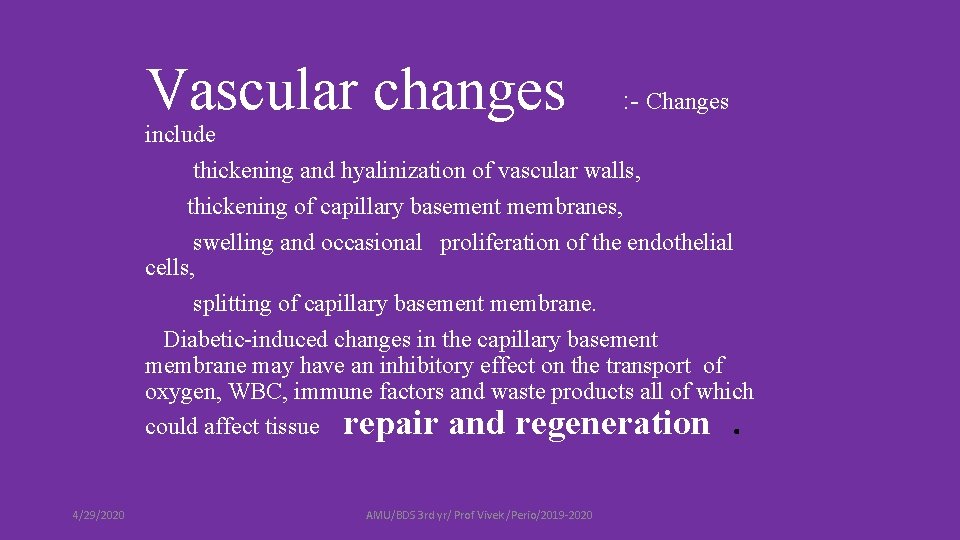
Vascular changes : - Changes include thickening and hyalinization of vascular walls, thickening of capillary basement membranes, swelling and occasional proliferation of the endothelial cells, splitting of capillary basement membrane. Diabetic-induced changes in the capillary basement membrane may have an inhibitory effect on the transport of oxygen, WBC, immune factors and waste products all of which could affect tissue repair and regeneration. 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
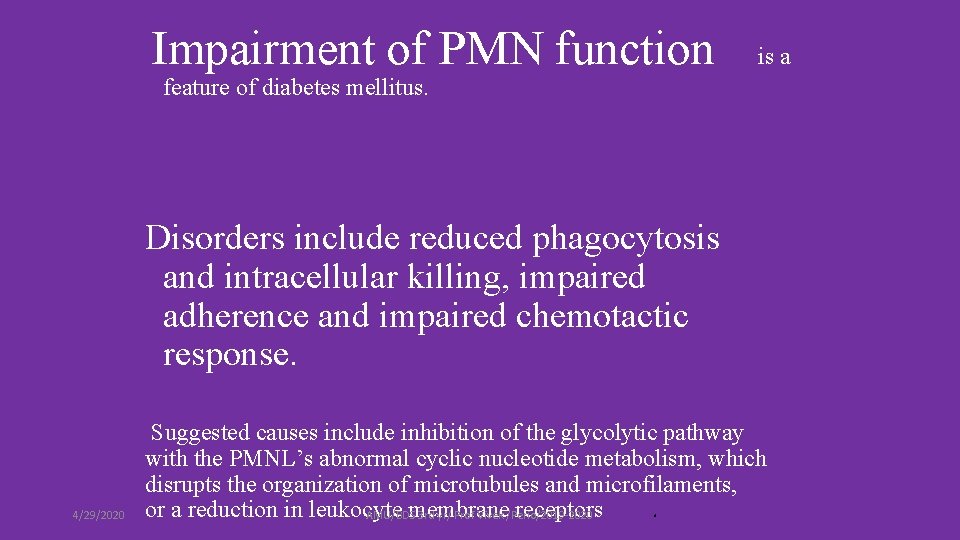
Impairment of PMN function is a feature of diabetes mellitus. Disorders include reduced phagocytosis and intracellular killing, impaired adherence and impaired chemotactic response. 4/29/2020 Suggested causes include inhibition of the glycolytic pathway with the PMNL’s abnormal cyclic nucleotide metabolism, which disrupts the organization of microtubules and microfilaments, or a reduction in leukocyte membrane receptors. AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
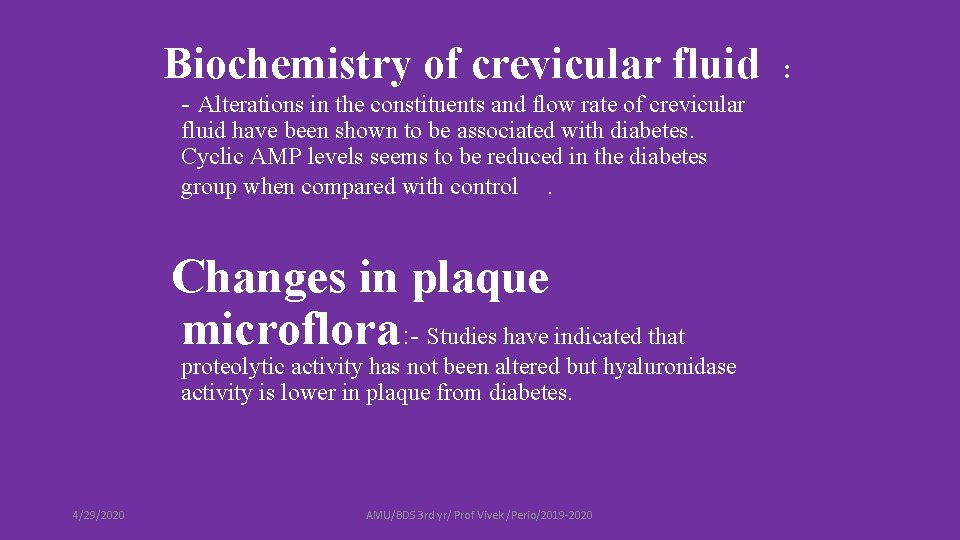
Biochemistry of crevicular fluid - Alterations in the constituents and flow rate of crevicular fluid have been shown to be associated with diabetes. Cyclic AMP levels seems to be reduced in the diabetes group when compared with control. Changes in plaque microflora : - Studies have indicated that proteolytic activity has not been altered but hyaluronidase activity is lower in plaque from diabetes. 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020 :
4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
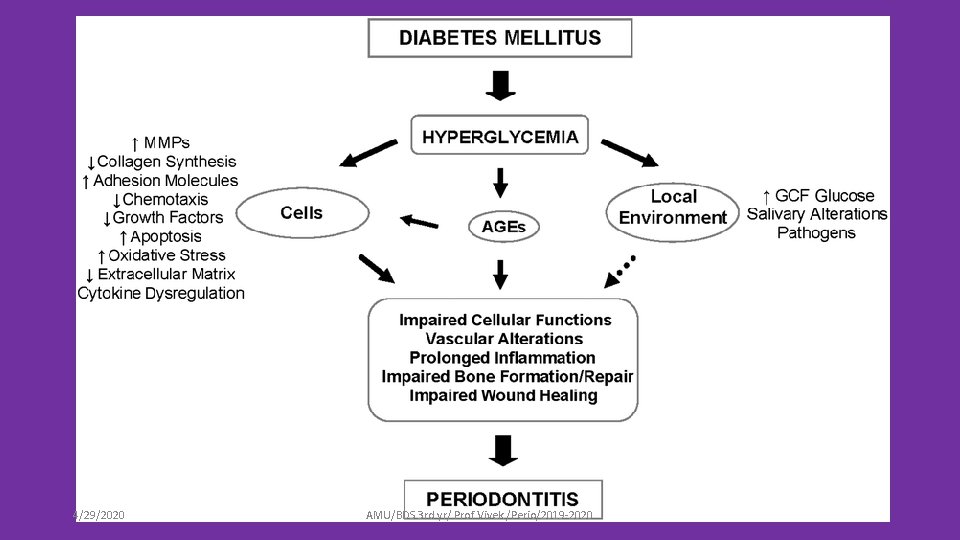
4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
What's the role of periodontal infection and / inflammation in Diabetes status of person ? 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
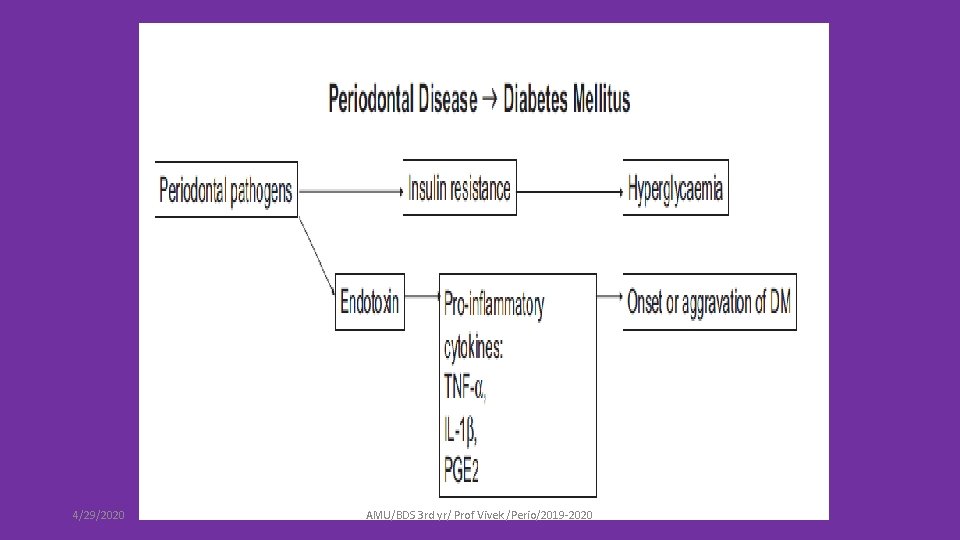
• Evidence has consistently indicated that diabetes is a risk factor for increased severity of gingivitis and periodontitis. Conversely , periodontitis may be a risk factor for worsening glycemic control among patients with diabetes and may increase the risk of diabetic complications. Periodontitis may initiate or propagate insulin resistance in a manner similar to that of obesity, by enhancing activation of the overall systemic immune response initiated by cytokines 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
• Proposed mechanism by which periodontal inflammatory mediators may contribute to the development of insulin resistance in individuals with both type 2 diabetes and periodontitis. 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
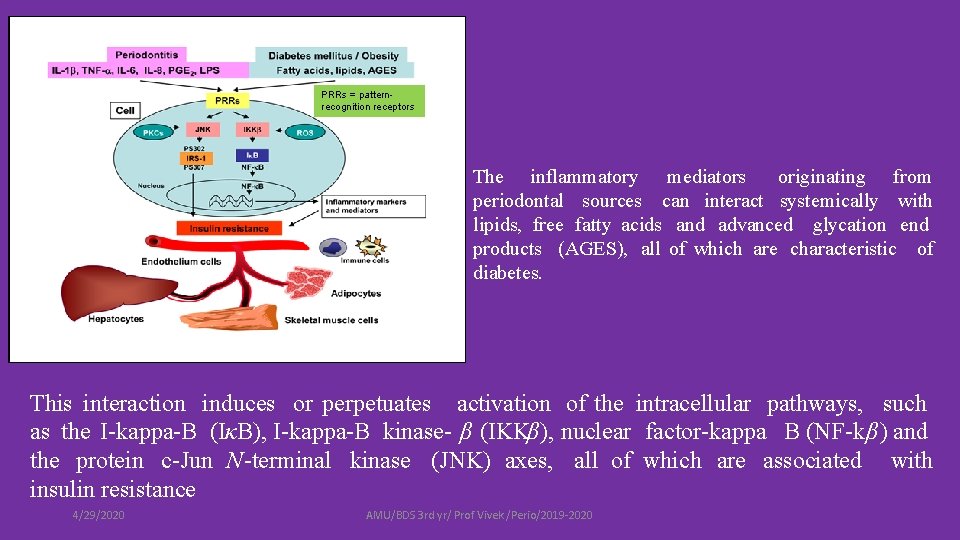
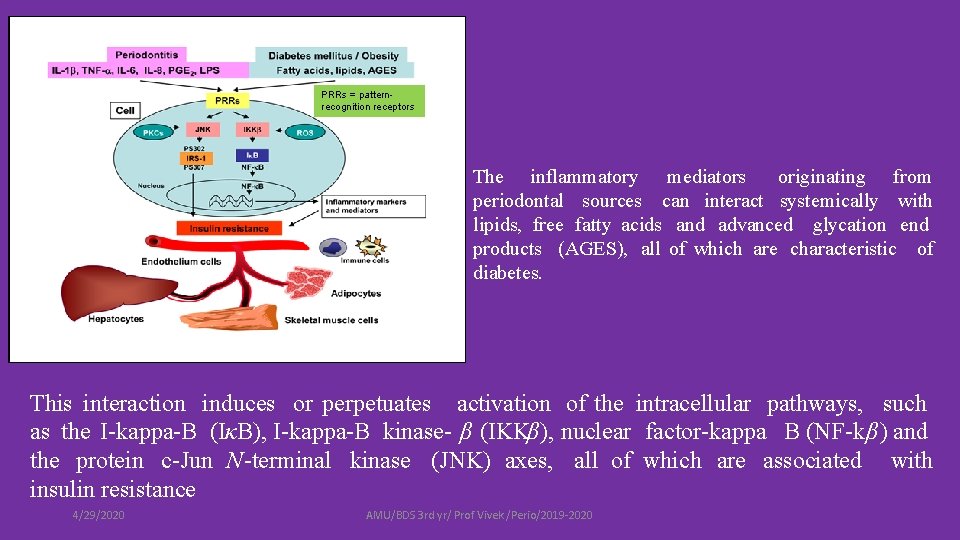
PRRs = patternrecognition receptors The inflammatory mediators originating from periodontal sources can interact systemically with lipids, free fatty acids and advanced glycation end products (AGES), all of which are characteristic of diabetes. This interaction induces or perpetuates activation of the intracellular pathways, such as the I-kappa-B (IκB), I-kappa-B kinase- β (IKKβ), nuclear factor-kappa B (NF-kβ) and the protein c-Jun N-terminal kinase (JNK) axes, all of which are associated with insulin resistance 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
The activation of these inflammatory pathways in immune cells (monocytes or macrophages), endothelium cells, adipocytes, hepatocytes and muscle cells promotes and contributes to an increase in the overall insulin resistance, which makes it difficult to achieve metabolic control in patients with both type 2 diabetes and periodontitis 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
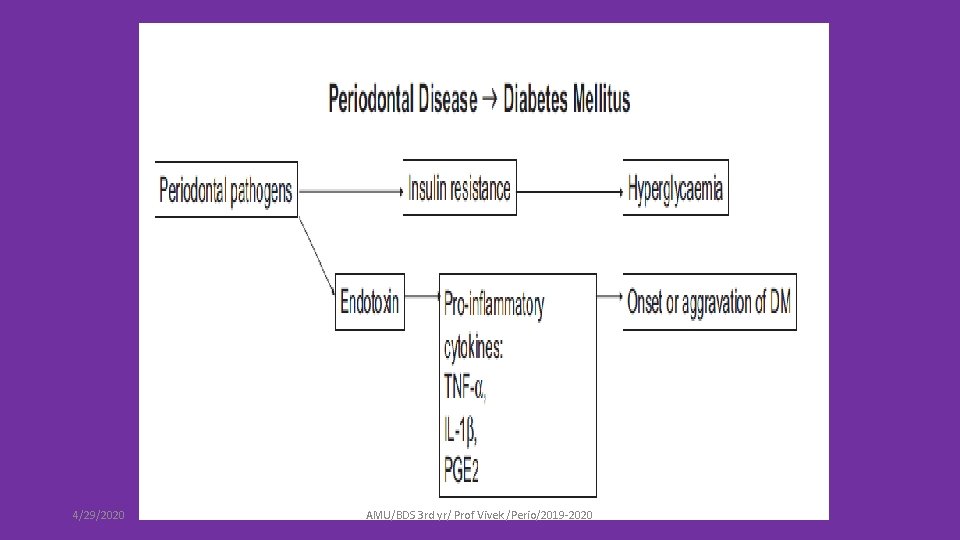
4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
• Given these mechanisms promoting insulin resistance, It seems that in individuals with type 2 diabetes and periodontitis, an elevated chronic systemic inflammatory state induced by periodontal disease may contribute to insulin resistance through a “feed-forward” mechanism, worsening glycemic control. Periodontitis may also contribute to the elevation of serum inflammation mediators through enhanced in vitro production of TNF-α, IL-1β and PGE 2 by monocytes. This may indicate an innate hyper responsiveness of these monocytes to periodontal bacterial challenge. Periodontitis may also play a role through the translocation of gram-negative species and their products from the periodontal biofilm into the circulation and through direct cytokinemia from the gingival crevicular fluid (i. e. , translocation of cytokines from the periodontal space into the circulation). Thus untreated Periodontal disease worsen the diabetes status of patient and vice versa 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020
• Key points • People with poorly controlled diabetes (both type 1 and type 2 diabetes mellitus, both adults and children) must be considered at risk for periodontitis, and people with diabetes should be informed of this risk. • Early diagnosis and prevention are of fundamental importance to avoid the largely irreversible tissue loss that occurs in periodontitis, and early referral of adults and children with poorly controlled diabetes to dental clinicians is indicated for periodontal screening. • Periodontal therapy in patients with diabetes is associated with improvements in glycaemic control (Hb. A 1 c reductions of approximately 0. 4%) that may be clinically relevant in the management of diabetes. • Oral health should be promoted in people with diabetes as an integral component of their overall diabetes management. • Closer collaboration between medical and dental clinical teams is necessary for the joint management of people with diabetes and periodontitis, and contact with dentists is important after the diagnosis of diabetes. 4/29/2020 AMU/BDS 3 rd yr/ Prof Vivek /Perio/2019 -2020 To be continue……………
 Vitamin part1
Vitamin part1 Classification of periodontal instruments
Classification of periodontal instruments Periodontal therapy in female patients
Periodontal therapy in female patients Modifiye stillman
Modifiye stillman Thixotropic theory of pdl
Thixotropic theory of pdl Plaque index
Plaque index Iatrogenic factors in periodontal disease
Iatrogenic factors in periodontal disease Russell periodontal index
Russell periodontal index Fases de la enfermedad periodontal
Fases de la enfermedad periodontal Surgical phase periodontal therapy
Surgical phase periodontal therapy Lanap perio
Lanap perio Rationale for periodontal treatment
Rationale for periodontal treatment Peridonal
Peridonal Paranky
Paranky Periodontal response to external forces
Periodontal response to external forces Periodontal treatment of medically compromised patients
Periodontal treatment of medically compromised patients Anug tedavisi
Anug tedavisi Lima maestra
Lima maestra Margen gingival
Margen gingival Fibres of pdl
Fibres of pdl Birleşim epiteli
Birleşim epiteli Diagnosis of periodontal disease
Diagnosis of periodontal disease Periapical granuloma
Periapical granuloma Lateral periodontal cyst
Lateral periodontal cyst Periodontal abscess
Periodontal abscess Periodontal ligament injection definition
Periodontal ligament injection definition Periodontal disease
Periodontal disease Kista primordial adalah
Kista primordial adalah Dental charting abbreviations
Dental charting abbreviations Periodontal healing
Periodontal healing General principles of periodontal surgery
General principles of periodontal surgery Cavitas oris proprium
Cavitas oris proprium Periodonto de protección
Periodonto de protección Modified widman flap indications
Modified widman flap indications Ligamento periodontal
Ligamento periodontal Periodontal radyoloji
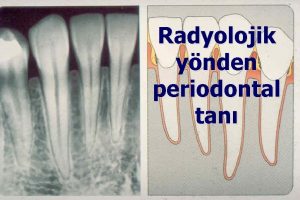
Periodontal radyoloji Alveolar bone
Alveolar bone Periodontal cep
Periodontal cep